Evaluating Commercial Kits for Unidentified Bacteria: A Comprehensive Guide for Researchers and Developers
This article provides a systematic framework for researchers, scientists, and drug development professionals to evaluate and select commercial kits for identifying unknown bacterial isolates.
Evaluating Commercial Kits for Unidentified Bacteria: A Comprehensive Guide for Researchers and Developers
Abstract
This article provides a systematic framework for researchers, scientists, and drug development professionals to evaluate and select commercial kits for identifying unknown bacterial isolates. It explores the foundational principles of bacterial identification technologies, details methodological applications across diverse sample types, offers troubleshooting and optimization strategies for common challenges, and establishes rigorous protocols for kit validation and comparative analysis. By synthesizing current methodologies and emerging trends, this guide aims to enhance diagnostic accuracy, streamline laboratory workflows, and inform strategic decisions in biomedical research and clinical development.
The Evolving Landscape of Bacterial Identification Technologies
The field of bacterial identification has undergone a profound transformation, evolving from traditional biochemistry techniques reliant on phenotypic characteristics to modern platforms that leverage molecular and computational technologies. This shift addresses critical limitations of classical methods, including slow turnaround times, subjective interpretation, and the inability to identify unculturable or rare species [1]. Traditional techniques, such as spectrophotometry and enzyme kinetics described by Michaelis and Menten over a century ago, established the fundamental principles of quantifying biochemical reactions but often lacked the sensitivity and specificity required for precise microbial characterization [2] [1]. The contemporary landscape now integrates these classical principles with high-throughput genomic tools, advanced biosensors, and artificial intelligence, creating a powerful synergy that enhances diagnostic precision and operational efficiency in research and clinical settings [3].
This transition is particularly crucial for evaluating commercial kits in unidentified bacteria research. Modern platforms must demonstrate not only superior analytical performance but also practical advantages in workflow integration, cost-effectiveness, and accessibility. The convergence of traditional biochemical knowledge with digital biomarker tracking through miniaturized, AI-assisted devices represents a new era in translational diagnostics, enabling real-time, data-driven decision-making at the point-of-care [3]. This review objectively compares the performance of traditional biochemical methods against emerging technological platforms, providing researchers with experimental frameworks and data-driven insights to guide their selection of appropriate identification strategies.
Historical Foundation: Traditional Biochemical Approaches
Core Principles and Methodologies
Traditional biochemical identification of bacteria fundamentally relies on detecting specific enzymatic activities or metabolic capabilities through observable phenotypic changes. The theoretical foundation rests upon classical enzymology, particularly the Michaelis-Menten model of enzyme kinetics developed in the early 20th century [2]. This model describes how enzyme-catalyzed reaction rates depend on substrate concentration, characterized by the Michaelis constant (KM) and maximum velocity (Vmax) parameters. These familiar arithmetic concepts from classical enzymology are derived from more fundamental networks of ordinary differential equations (ODEs) describing dynamical systems under mass action approximations [2].
The Briggs-Haldane formulation of Michaelis-Menten kinetics, which assumes the enzyme-substrate complex rapidly achieves a steady state rather than true equilibrium, provides the conceptual framework for many biochemical tests used in bacterial identification [2]. These tests typically involve inoculating bacterial samples into substrates containing specific biochemicals and observing color changes, gas production, or pH shifts that indicate metabolic activity. These methods focus on enzymatic reactions studied under controlled, well-mixed conditions similar to the in vitro approaches that defined early enzymology [2].
Experimental Protocols for Traditional Biochemistry
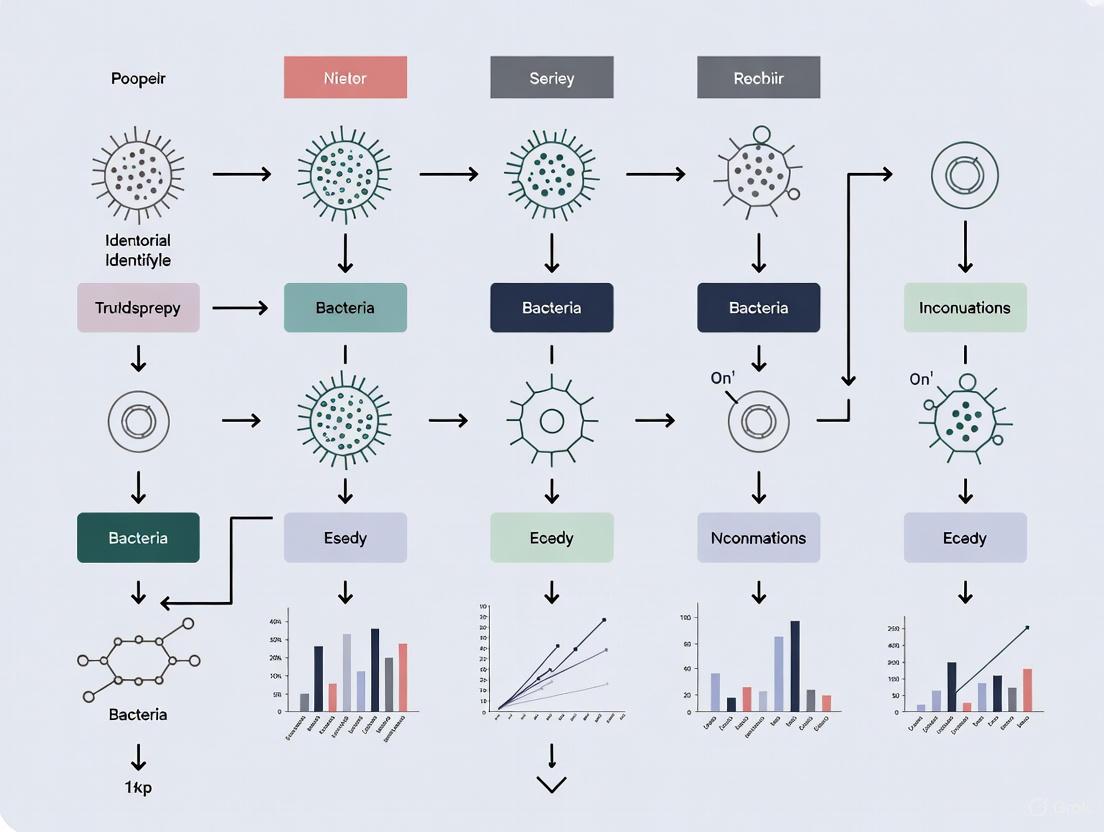
Standard protocols for traditional biochemical identification follow a consistent workflow, represented in the diagram below:
Diagram: Workflow for Traditional Biochemical Bacterial Identification
The specific methodology for a conventional biochemical test panel involves:
- Pure Culture Preparation: Isolate single bacterial colonies on non-selective media and confirm purity through Gram staining and microscopic examination.
- Test System Inoculation: Using sterile technique, prepare a standardized suspension of the bacterial isolate in saline (0.5 McFarland standard). Inoculate each well of a commercial biochemical test panel (e.g., API, VITEK) according to manufacturer specifications.
- Incubation: Seal the test panel and incubate under appropriate atmospheric conditions (aerobic, anaerobic, or microaerophilic) at 35±2°C for 18-48 hours, depending on the expected growth characteristics of the organism.
- Result Interpretation: Following incubation, record color changes in each cup resulting from pH shifts, substrate utilization, or metabolic byproducts. Some tests may require the addition of reagents to visualize specific reactions.
- Identification: Convert the pattern of positive and negative reactions to a numerical code and consult a taxonomic database to determine the most probable species identification, typically expressed with a confidence percentage.
The Scientist's Toolkit: Essential Reagents for Traditional Methods
Table 1: Key Research Reagent Solutions for Traditional Biochemical Identification
| Item | Function | Example Applications |
|---|---|---|
| Selective Media | Suppresses unwanted flora while promoting growth of target bacteria | MacConkey Agar (gram-negative rods), Columbia CNA Agar (gram-positive cocci) |
| Carbohydrate Substrates | Tests fermentation capabilities | Glucose, Lactose, Sucrose in Phenol Red Broth |
| Amino Acid Decarboxylases | Detects amino acid metabolism | Lysine, Ornithine, Arginine decarboxylase tests |
| Enzyme Substrates | Identifies specific enzymatic activities | ONPG (β-galactosidase), Tryptophan (Indole production) |
| Oxidative-Fermentative Media | Differentiates metabolic pathways | Hugh-Leifson OF Basal Medium |
| Commercial Test Panels | Standardized multi-test systems | API 20E, VITEK 2 GN Card |
| KRCA-0008 | KRCA-0008, MF:C30H37ClN8O4, MW:609.1 g/mol | Chemical Reagent |
| 3-Hydroxypentadecane-4-one | 3-Hydroxypentadecane-4-one, MF:C15H30O2, MW:242.40 g/mol | Chemical Reagent |
Modern Platforms: Technological Advancements
Molecular and Mass Spectrometry Approaches
Modern platforms for bacterial identification have largely transitioned to molecular techniques that offer superior speed, specificity, and automation compared to traditional methods. Mass spectrometry (MS), particularly Matrix-Assisted Laser Desorption/Ionization Time-of-Flight (MALDI-TOF), has revolutionized clinical microbiology by enabling rapid identification based on unique protein profiles [1]. This technology generates a characteristic mass spectral fingerprint from bacterial ribosomal proteins, which is compared against an extensive database for identification.
Advanced molecular methods include:
- PCR and Sequencing: Amplification and analysis of conserved genomic regions (e.g., 16S rRNA gene) provides species-level identification, especially valuable for unculturable or fastidious organisms [4].
- Next-Generation Sequencing (NGS): Whole-genome sequencing offers the highest resolution for strain typing and detecting virulence markers, though at higher cost and complexity [1].
- Lab-on-a-Chip (μTAS): Microfluidic platforms miniaturize laboratory processes, enabling portable, rapid testing with minimal sample volumes suitable for point-of-care applications [1].
These technologies demonstrate significant advantages in sensitivity and specificity compared to traditional methods. Mass spectrometry provides up to 1,000 times lower detection levels for some analytes compared to spectrophotometric methods, a critical advantage for early disease diagnosis [1].
Experimental Protocols for Modern Platforms
The workflow for modern bacterial identification using molecular methods follows a distinct pathway:
Diagram: Workflow for Modern Bacterial Identification Platforms
The specific methodology for PCR-based bacterial identification with contamination controls involves:
- Nucleic Acid Extraction: Using a laminar flow hood dedicated to PCR preparation, extract bacterial DNA from pure cultures or clinical samples using a commercial kit. Include extraction controls without sample to monitor reagent contamination.
- PCR Reaction Setup: Prepare reactions under aseptic technique using PCR-grade water and reagents. Include both positive control (bacterial DNA with known sequence) and negative control (no-template water) reactions for every assay run. Reaction components typically include: DNA template, PCR buffer, dNTP mix, forward and reverse primers targeting the 16S rRNA gene, DNA polymerase, and MgClâ‚‚ [4].
- Thermal Cycling: Amplify target sequences using standardized cycling conditions: initial denaturation at 95°C for 2 minutes, followed by 45 cycles of denaturation at 95°C for 30 seconds, annealing at 55°C for 30 seconds, and extension at 72°C for 1 minute, with a final extension at 72°C for 5 minutes [4].
- Amplicon Analysis: Separate PCR products by gel electrophoresis (1% agarose), visualize with SYBRsafe staining, and perform size selection of appropriate bands (approximately 500 bases for the V3-4 region of bacterial 16S rRNA) for sequencing [4].
- Sequencing and Analysis: Submit purified amplicons for Sanger sequencing. Trim sequence ends to remove unidentified bases, ensuring the first and last included base has a quality score ≥20. Query trimmed sequences against the NCBI GenBank database using megablast to identify the closest matches based on percent coverage and identity [4].
Critical Consideration: Contamination in Molecular Methods
A significant challenge in modern bacterial identification, particularly for low-biomass samples, is bacterial DNA contamination of laboratory reagents. Recent research examining nine different commercial PCR enzymes found contaminating bacterial DNA in seven of them, originating from a variety of species [4]. This contamination can lead to false-positive results and erroneous conclusions in microbiome studies. The implementation of rigorous negative controls is therefore essential, and this validation can be achieved using accessible methods like endpoint PCR and Sanger sequencing without requiring expensive high-throughput technologies [4].
The Scientist's Toolkit: Essential Reagents for Modern Platforms
Table 2: Key Research Reagent Solutions for Modern Identification Platforms
| Item | Function | Example Applications |
|---|---|---|
| DNA Extraction Kits | Isolation of high-quality genomic DNA | DNeasy Blood & Tissue Kit, Quick-DNA Fecal/Soil Microbe Kit |
| PCR Master Mixes | Optimized enzymes and buffers for amplification | Platinum Taq DNA Polymerase, Q5 High-Fidelity Master Mix |
| 16S rRNA Primers | Amplification of conserved bacterial regions | 27F/1492R for full-length 16S, V3-4 primers for Illumina |
| Mass Spectrometry Matrix | Energy-absorbing molecules for MALDI-TOF | α-cyano-4-hydroxycinnamic acid (HCCA) |
| Bioinformatic Tools | Analysis of sequencing data | QIIME 2, MEGAN, SPeDE |
| Commercial ID Systems | Integrated identification platforms | Bruker MALDI Biotyper, bioMérieux VITEK MS |
| Lanopepden | Lanopepden, CAS:1152107-25-9, MF:C22H34FN7O4, MW:479.5 g/mol | Chemical Reagent |
| Lappaol F | Lappaol F, CAS:69394-17-8, MF:C40H42O12, MW:714.8 g/mol | Chemical Reagent |
Comparative Performance Analysis
Quantitative Comparison of Method Performance
Table 3: Performance Comparison of Bacterial Identification Methods
| Parameter | Traditional Biochemistry | Mass Spectrometry (MALDI-TOF) | PCR & Sequencing | NGS Platforms |
|---|---|---|---|---|
| Time to Result | 24-48 hours | 10-30 minutes | 4-8 hours | 1-3 days |
| Sample Volume | Medium (1-5 mL) | Low (1 μL) | Low (50-200 μL) | Very Low (<50 μL) |
| Analytical Sensitivity | Moderate | High | Very High | Extremely High |
| Species Discrimination | Fair to Good | Excellent | Excellent | Superior (strain-level) |
| Capital Cost | Low | Medium-High | Medium | High |
| Cost per Test | Low | Low | Medium | High |
| Hands-on Time | High | Low | Medium | Medium-High |
| Database Dependence | Moderate | High | High | High |
| Automation Potential | Low | High | Medium | High |
Analytical Characteristics and Limitations
The performance data reveal distinct advantages and limitations for each methodological approach. Traditional biochemical methods offer cost-effectiveness and operational simplicity but demonstrate limited sensitivity and specificity compared to modern platforms [1]. These limitations become particularly problematic when identifying fastidious organisms or distinguishing between closely related species with similar biochemical profiles.
Mass spectrometry achieves significantly shorter turnaround times (10-30 minutes versus 24-48 hours) while maintaining high accuracy for most common pathogens [1]. However, this technology requires substantial capital investment and struggles with differentiating certain closely related species, such as Shigella and Escherichia coli.
Molecular methods provide the highest sensitivity and specificity, with PCR-based techniques detecting pathogens present in very low numbers that would be missed by traditional culture-based methods [4]. The comprehensive genomic analysis provided by NGS enables strain-level discrimination essential for outbreak investigations, though at higher cost and computational requirements [1].
A critical consideration for molecular methods is reagent contamination, as demonstrated by studies finding bacterial DNA in commercial PCR enzymes [4]. This contamination can significantly impact results in microbiome studies of low-biomass samples, necessitating appropriate negative controls and careful data interpretation.
The evolution from traditional biochemistry to modern platforms represents a paradigm shift in bacterial identification, moving from phenotypic characterization to genotypic analysis. While traditional methods established the fundamental principles of biochemical testing, contemporary technologies offer unprecedented speed, sensitivity, and discrimination capabilities. The optimal approach often involves a complementary strategy, using rapid mass spectrometry for routine identification while reserving molecular methods for complex cases requiring strain-level discrimination.
Future advancements will likely focus on integrating artificial intelligence with portable biosensing technologies to create increasingly automated and accessible diagnostic platforms [3]. These systems will leverage the growing availability of digital biomarkers through wearable devices and miniaturized analytical platforms, potentially enabling real-time monitoring of microbial populations. However, regardless of technological sophistication, proper validation and contamination controls remain essential, as even advanced molecular methods can be compromised by reagent contamination [4]. As the field continues to evolve, the successful integration of traditional biochemical knowledge with cutting-edge technologies will drive the next generation of identification platforms, enhancing both diagnostic precision and global accessibility.
The accurate identification of bacterial isolates is a cornerstone of microbiological research, clinical diagnostics, and drug development. As bacterial resistance and emerging pathogens present ongoing challenges, the reliability of identification methods directly impacts research outcomes and therapeutic strategies. This guide provides an objective comparison of the three core methodological pillars—biochemical, immunological, and molecular techniques—framed within a broader thesis on evaluating commercial kits for unidentified bacteria research. By presenting standardized experimental data and detailed protocols, this article serves as a reference for researchers and scientists in selecting the most appropriate identification pathway for their specific applications.
Bacterial identification methods are characterized by their fundamental principles, targeting different bacterial attributes: metabolic profiles, antigenic structures, and genetic sequences. The following table provides a high-level comparison of these core methodologies.
Table 1: Core Principles of Bacterial Identification Methods
| Feature | Biochemical Methods | Immunological Methods | Molecular Methods |
|---|---|---|---|
| Fundamental Principle | Detection of metabolic enzymes and byproducts | Detection of specific antigen-antibody interactions | Detection of unique nucleic acid sequences |
| Target Analyte | Substrates, enzymes, metabolites (e.g., sugars, proteins) | Surface antigens (e.g., O, H, K antigens), toxins | DNA or RNA sequences (e.g., 16S rRNA, virulence genes) |
| Typical Timeframe | 24-48 hours | Minutes to hours | Several hours to 24 hours |
| Specificity | Moderate to High (species level) | Very High (serotype level) | Very High (strain level possible) |
| Sensitivity | Moderate (requires pure culture) | High | Very High (single copy detection) |
| Key Advantage | Cost-effective, provides functional data | Rapid, can be used for direct detection | High specificity and sensitivity, definitive |
| Primary Limitation | Slow, dependent on bacterial growth | Requires specific antibodies, cross-reactivity | Higher cost, technical expertise required |
The choice among these methods depends on the research question, required speed, specificity, and available resources. Immunological methods leverage the high specificity of antibody-antigen binding, often providing results rapidly, which is crucial in clinical and outbreak settings [5]. Molecular methods, such as PCR, offer high sensitivity and specificity by amplifying and detecting unique genetic markers, making them a powerful tool for identifying unculturable organisms or for genotyping [6]. Biochemical methods, while generally slower, provide valuable information on the metabolic capabilities of the bacterium, which can be functionally relevant.
Experimental Protocols for Core Identification Techniques
Protocol for Immunological Identification via Enzyme Immunoassay (ELISA)
The following workflow details the steps for identifying bacterial antigens using a direct ELISA protocol, a common format in commercial kits.
Detailed Methodology:
- Sample Coating: Dilute the bacterial lysate or suspension in a suitable carbonate-bicarbonate buffer (pH 9.6). Add 100 µL of the solution to each well of a 96-well microtiter plate. Incubate the plate overnight at 4°C to allow antigens to adsorb to the well surface [6].
- Washing: Empty the contents of the wells and wash them three times with 300 µL of a phosphate-buffered saline solution containing a detergent (e.g., 0.05% Tween 20, PBS-T). This removes unbound proteins.
- Blocking: Add 200 µL of a blocking agent (e.g., 1-5% Bovine Serum Albumin or non-fat dry milk in PBS) to each well. Incubate for 1-2 hours at room temperature to cover any unsaturated binding sites on the plastic.
- Primary Antibody Incubation: Remove the blocking solution and add 100 µL of the specific primary antibody (e.g., mouse anti-target bacteria monoclonal antibody) diluted in blocking buffer. Incubate for 1-2 hours at room temperature [6].
- Washing: Wash the plate three times with PBS-T as before.
- Secondary Antibody Incubation: Add 100 µL of an enzyme-conjugated secondary antibody (e.g., Horseradish Peroxidase (HRP)-linked anti-mouse immunoglobulin) diluted in blocking buffer. Incubate for 1-2 hours at room temperature, protected from light [6].
- Washing: Perform a final wash step three times with PBS-T.
- Signal Detection: Prepare the enzyme substrate solution immediately before use. For HRP, Tetramethylbenzidine (TMB) is a common substrate. Add 100 µL of the substrate solution to each well and incubate in the dark for 15-30 minutes.
- Reaction Stopping and Reading: Stop the enzymatic reaction by adding 50 µL of a stop solution (e.g., 1M sulfuric acid for TMB). The color will change from blue to yellow. Immediately measure the absorbance of each well at 450 nm using a microplate reader. A signal significantly higher than the negative control indicates a positive identification.
Protocol for Molecular Identification via Polymerase Chain Reaction (PCR)
The workflow below outlines the key steps for bacterial identification through conventional PCR and result analysis.
Detailed Methodology:
- DNA Extraction: Extract genomic DNA from a pure bacterial culture using a commercial kit. This typically involves enzymatic lysis (e.g., with lysozyme), chemical lysis (with detergents), and mechanical disruption (bead beating). The DNA is then purified from proteins and other contaminants, often through a silica membrane column, and eluted in water or TE buffer [6].
- PCR Reaction Setup: Prepare a PCR master mix on ice to include:
- Nuclease-free water
- PCR Buffer (with MgClâ‚‚)
- dNTPs (deoxynucleotide triphosphates)
- Forward and Reverse Primers (specific to a target gene like 16S rRNA or a virulence gene)
- Thermostable DNA Polymerase (e.g., Taq polymerase) Aliquot the master mix into PCR tubes and add a small volume of the extracted template DNA.
- Thermal Cycling: Place the tubes in a thermal cycler and run a program such as:
- Initial Denaturation: 95°C for 5 minutes.
- Amplification (30-40 cycles):
- Denaturation: 95°C for 30 seconds.
- Annealing: 50-65°C (primer-specific) for 30 seconds.
- Extension: 72°C for 1 minute per kb of amplicon.
- Final Extension: 72°C for 7 minutes.
- Hold: 4°C ∞.
- Amplicon Analysis: Analyze the PCR products using agarose gel electrophoresis. Mix a portion of the PCR product with a loading dye and load it into a well of an agarose gel (1-2%) containing a DNA intercalating dye. Run the gel at a constant voltage alongside a DNA molecular weight ladder. Visualize the gel under UV light. The presence of a band at the expected size confirms the identification of the target bacterium [6].
Performance Data from Experimental Studies
Performance of Immunological and Molecular OT Diagnostics
A 2024 study on ocular toxoplasmosis (OT) provides a direct comparison of serological (immunological) and PCR-based (molecular) techniques, highlighting their relative sensitivities across different sample types. The data demonstrates the critical impact of the sample matrix on test performance [6].
Table 2: Comparison of Diagnostic Techniques for Ocular Toxoplasmosis
| Method | Sample Type | Target | Patient Group | Positivity Rate | Key Finding |
|---|---|---|---|---|---|
| Serology (IFAT/ELISA) | Serum | Anti-T. gondii IgG | Active OT (G1) | Highest Positivity | Effective for systemic confirmation [6] |
| Serology (ELISA) | Tear Fluid | Anti-T. gondii IgA | All Patients (G1-G3) | 9.2% | Less invasive alternative with potential [6] |
| Nested PCR | Blood | GRA7 gene | All Patients | 24.4% | Highest blood-based molecular target [6] |
| Nested PCR | Tear Fluid | B1 gene | All Patients | 15.0% | Highest tear-based molecular target [6] |
Evaluation of Rapid Antigen Tests
A 2022 study on COVID-19 rapid antigen tests (immunological) provides a clear framework for evaluating commercial kit performance against a molecular gold standard, underscoring the influence of viral load.
Table 3: Performance of Two Rapid Antigen Test Kits vs. rRT-PCR
| Test Kit | Sensitivity (Overall) | Specificity (Overall) | Sensitivity (Ct < 25) |
|---|---|---|---|
| SQ RAT | 77.1% (101/131) | 100% (215/215) | > 85% [5] |
| ND RAT | 89.3% (117/131) | 100% (215/215) | > 85% [5] |
Note: rRT-PCR = real-time Reverse Transcription-Polymerase Chain Reaction; Ct = Cycle threshold, a proxy for viral load (lower Ct = higher viral load).
The Scientist's Toolkit: Essential Research Reagent Solutions
Table 4: Key Reagents and Materials for Bacterial Identification
| Item | Function | Example Application |
|---|---|---|
| Specific Antibodies | Bind to unique bacterial surface antigens for detection. | Primary capture/detection antibody in ELISA or Lateral Flow Assays [6]. |
| Oligonucleotide Primers | Short DNA sequences designed to bind and amplify unique bacterial genes. | Amplification of the 16S rRNA gene for species identification via PCR [6]. |
| DNA Polymerase | Enzyme that synthesizes new DNA strands from a template. | Essential component of PCR master mix for target gene amplification [6]. |
| Enzyme Substrates | Compounds converted by an enzyme (e.g., HRP) to produce a detectable signal. | TMB substrate for ELISA, producing a colorimetric change for quantification [6]. |
| Enrichment Broths | Culture media designed to support the growth of specific bacteria. | Selective enrichment of a pathogen from a complex sample prior to DNA extraction or immunoassay. |
| Agarose | Polysaccharide used to create a matrix for separating DNA fragments by size. | Gel electrophoresis to visualize and confirm the size of PCR amplicons [6]. |
| Laquinimod | Laquinimod, CAS:248281-84-7, MF:C19H17ClN2O3, MW:356.8 g/mol | Chemical Reagent |
| Larazotide Acetate | Larazotide Acetate | Tight Junction Regulator | RUO | Larazotide acetate is a synthetic peptide for research into celiac disease and intestinal barrier function. For Research Use Only. Not for human use. |
The comparative data and protocols presented here underscore a central tenet in modern bacteriology: no single method is universally superior. The optimal identification strategy often involves a complementary approach. Immunological tests like ELISA offer robust and rapid screening [5], while molecular techniques like (Nested) PCR provide definitive confirmation with high sensitivity, especially when using optimized genetic targets like GRA7 or B1 [6].
The choice of biological sample (e.g., serum vs. tear fluid) significantly impacts the performance of any method, highlighting the need for thorough validation [6]. For researchers evaluating commercial kits, critical assessment parameters must include sensitivity and specificity against a recognized gold standard, the time-to-result, cost, and the technical skill required. The prozone phenomenon, a rare artifact in immunological tests leading to false negatives, is a reminder that understanding the limitations and potential interferences of any chosen method is crucial for accurate interpretation of results [5]. Ultimately, a strategic combination of these core principles—biochemical, immunological, and molecular—forms the most powerful toolkit for the unambiguous identification of unknown bacteria in research and development.
The global market for bacterial identification tools and detection kits is experiencing a period of robust growth, propelled by the escalating challenge of antimicrobial resistance (AMR), rising incidences of infectious diseases, and stringent safety regulations across healthcare and industrial sectors [7] [8] [9]. This market encompasses a diverse range of technologies, from traditional phenotypic methods to advanced molecular and genotypic systems, all aimed at providing rapid and accurate identification of bacterial pathogens [10]. Key players are actively engaged in innovation and strategic collaborations to enhance their product portfolios and geographic reach [11] [8]. The market is characterized by a distinct shift from conventional culture-based techniques toward rapid, automated, and high-throughput solutions such as MALDI-TOF mass spectrometry, PCR, and next-generation sequencing (NGS), which offer significant reductions in turnaround time from days to hours [8] [10]. North America currently dominates the market landscape, but the Asia-Pacific region is poised to exhibit the highest growth rate in the coming years, driven by improving healthcare infrastructure and growing health awareness [8] [9] [10]. Future growth will be catalyzed by technological advancements, including the integration of artificial intelligence (AI) and machine learning for data analysis, the development of portable point-of-care devices, and the increasing demand for at-home testing kits [7] [8] [12].
The bacterial identification market is a multi-billion dollar industry with strong growth projections through the next decade, though reported figures vary slightly depending on the specific market segment analyzed (e.g., broad bacteriological testing versus specific identification tools).
Table: Global Market Size and Growth Projections
| Market Segment | 2024/2025 Base Value | 2030/2032 Projected Value | CAGR (Compound Annual Growth Rate) | Source |
|---|---|---|---|---|
| Microbial Identification Market | USD 4.55 Billion (2025) | USD 10.01 Billion (2032) | 11.9% | [10] |
| Bacteriological Testing Market | USD 25.83 Billion (2025) | USD 37.26 Billion (2030) | 7.6% | [7] |
| Bacteria Detection Kits Market | ~USD 1.5 Billion (2024) | ~USD 2.9 Billion (2033) | ~8.5% | [13] |
This growth is primarily driven by several key factors:
- Rising Infectious Diseases and AMR: The increasing global burden of infectious diseases and the dire threat of antimicrobial resistance are creating an urgent need for rapid, accurate diagnostics. A report cited that drug-resistant infections could lead to over 39 million direct deaths worldwide in the next 25 years, highlighting the critical role of advanced diagnostics [8].
- Stringent Regulatory Requirements: Governments and regulatory bodies worldwide are enforcing stricter safety standards in the food and beverage, pharmaceutical, and water industries, mandating frequent and reliable microbiological testing [7] [9].
- Technological Advancements: Continuous innovation in molecular diagnostics, automation, and miniaturization is making rapid testing more accessible, cost-effective, and user-friendly, thereby expanding its adoption [8] [10].
Market Segmentation
The bacterial identification market can be segmented by technology, application, end-user, and product type, each with distinct growth dynamics and leading segments.
By Technology
The technology landscape is segmented into traditional and rapid methods, with rapid technologies increasingly dominating due to their speed and accuracy.
Table: Market Segmentation by Technology and Method
| Segmentation Basis | Key Segment | Leading Technology/System | Market Share / Reason for Dominance |
|---|---|---|---|
| Technology [8] | Molecular & Rapid Technologies | MALDI-TOF Mass Spectrometry | Dominated in 2024 due to high speed, low operational cost, and ease of integration into lab workflows [8]. |
| Technology [8] | Molecular & Rapid Technologies | Next-Generation Sequencing (NGS) | Expected fastest growth; can uncover mixed infections and detect unknown strains [8]. |
| Technology [10] | Molecular & Rapid Technologies | PCR | Held a 32.2% share in 2025; valued for high sensitivity, specificity, and broad applicability [10]. |
| Method [10] | Phenotypic Methods | Culture-based, Gram staining, Biochemical tests (e.g., API strips, VITEK) | Held a dominant 35.2% share in 2025; cost-effective, accessible, and used for validation [10]. |
By Application and End-User
Different industries utilize bacterial identification tools to meet specific needs, from clinical diagnostics to quality control.
Table: Key Application Areas and End-Users
| Application Area | Key Drivers and Uses | Growth Notes |
|---|---|---|
| Clinical Diagnostics [8] [9] | Rising patient volumes, need for infection management, and combating AMR. | The largest application segment, led by hospitals and clinics [8] [9]. |
| Food & Beverage Testing [7] [8] | Preventing contamination, complying with safety regulations, and extending product shelf-life. | Expected to be the fastest-growing application segment [8]. |
| Pharmaceutical & Cosmetics [7] | Ensuring microbial safety and quality control of products like biologics and personal care items. | Adoption of rapid testing is increasing for stringent microbial control [7]. |
| Environmental Monitoring [9] | Monitoring water, soil, and air for microbial contamination. | A growing application area for detection kits beyond healthcare [9]. |
By Product Type
The market is also divided by the type of product sold. The instruments segment (e.g., mass spectrometers, PCR systems) accounted for the largest share (45.2%) in 2025, driven by technological advancements and the need for diagnostic accuracy [10]. However, the consumables segment (e.g., reagents, assay kits) also held a dominant position due to their essential, recurring nature in daily lab operations [8]. The software & services segment is projected to grow the fastest as labs increasingly rely on digital platforms for data management and analysis [8].
Key Players and Competitive Landscape
The bacterial identification market features a mix of established multinational corporations and emerging specialized companies. Competition is intense, with players focusing on innovation, partnerships, and mergers and acquisitions to expand their market presence [11] [13].
Table: Key Market Players and Recent Strategic Developments
| Company | Representative Product/Service | Recent Strategic Developments |
|---|---|---|
| bioMérieux | VITEK systems for ID/AST | Received FDA clearance for VITEK COMPACT PRO in March 2025 [8] [10]. |
| Thermo Fisher Scientific | MicroSEQ PCR and Sequencing Kits | Offers kits and libraries for 16S rDNA and fungal identification [14]. |
| Charles River Laboratories | Accugenix NGS Services | Launched Accugenix Next-Generation Sequencing for bacterial and fungal ID in 2023 [8] [10]. |
| QIAGEN | Microbiome WGS SeqSets | Introduced a complete workflow for microbiome research in 2023 [8]. |
| Bruker Corporation | MALDI Biotyper systems | Unveiled advanced fungal and mycobacteria detection solutions in 2023 [10]. |
| Other Notable Players | Various detection kits and instruments | Minerva Biolabs, Charm Sciences, Creative Diagnostics, Sartorius AG [11] [9]. |
Growth Catalysts and Future Outlook
The market's future trajectory will be shaped by several powerful catalysts and emerging trends.
Primary Growth Catalysts
- Technological Advancements: The development of portable, automated, and rapid testing solutions is making advanced diagnostics accessible beyond central laboratories [7] [15]. For instance, AI-powered platforms can now identify bacterial species directly from clinical samples in as little as 5 hours, a process that traditionally took days [8].
- Rising Healthcare Investment: Governments, particularly in the Asia-Pacific region, are investing heavily in upgrading healthcare infrastructure, which includes expanding laboratory capabilities and access to diagnostic tools [9] [10].
- Expanding Point-of-Care (POC) Testing: The trend towards decentralized testing is creating significant demand for portable, user-friendly bacteria detection kits that can deliver immediate results in clinics or remote locations [9].
Emerging Trends
- AI and Predictive Analytics: Integration of AI and machine learning is revolutionizing the market by enhancing the speed and accuracy of pathogen detection, predicting resistance patterns, and enabling real-time outbreak surveillance [7] [8].
- Multiplexing and Multi-Omics: There is a growing focus on developing tests that can detect multiple bacterial pathogens simultaneously (multiplexing) and on combining various testing modalities, such as genomics and metagenomics, for a more comprehensive analysis [7] [15].
- Direct-to-Consumer (DTC) and At-Home Testing: Growing consumer interest in personal health monitoring is fueling the development of at-home microbiome and bacteria testing kits, opening a new distribution channel for the market [12].
Experimental Data and Protocol Comparison
A critical function of commercial kits is the accurate identification of unknown bacterial isolates in a research setting. Below is a detailed comparison of two common genotypic methods.
Table: Comparison of Experimental Protocols for Bacterial ID
| Parameter | 16S rRNA Gene Sequencing (Sanger) [14] | MALDI-TOF Mass Spectrometry [8] |
|---|---|---|
| Principle | Sequencing of the conserved 16S ribosomal RNA gene and comparison to a database. | Analysis of unique protein profiles (primarily ribosomal proteins) from whole cells. |
| Target Molecule | DNA (16S rRNA gene). | Proteins and peptides. |
| Workflow Duration | ~5 hours for sequencing reaction (plus culture time) [14]. | As little as 15 minutes to a few hours [8]. |
| Key Experimental Steps | 1. DNA extraction.2. PCR amplification of 16S gene.3. Purification of PCR product.4. Sequencing reaction.5. Capillary electrophoresis.6. Data analysis against library (e.g., MicroSEQ). | 1. Prepare a thin layer of bacterial colony on target plate.2. Overlay with matrix solution.3. Dry and insert into spectrometer.4. Irradiate with laser to ionize samples.5. Measure time-of-flight of ions.6. Compare resulting spectrum to reference database. |
| Discriminatory Power | Can often discriminate to the species level; full gene (1500 bp) provides higher resolution than partial (500 bp) [14]. | Excellent for species-level identification; may struggle with very closely related species [8]. |
| Throughput | Lower throughput (one to a few samples per run). | Very high throughput (hundreds of samples per run). |
Research Reagent Solutions for 16S rRNA Sequencing
For a typical 16S rRNA sequencing experiment, the following key reagents are required:
- Lysis Buffers and Enzymes: For mechanical or enzymatic breakdown of the bacterial cell wall to release genomic DNA.
- PCR Master Mix: A pre-mixed solution containing a thermostable DNA polymerase, dNTPs, MgClâ‚‚, and reaction buffers optimized for amplifying the 16S rRNA gene [14].
- Specific Primers: Oligonucleotides designed to bind to the conserved regions of the 16S rRNA gene, allowing amplification of the variable regions used for identification [14].
- Purification Kits: For cleaning up the PCR product prior to sequencing to remove excess primers, dNTPs, and enzymes.
- BigDye Terminators or Similar: Fluorescently labeled dideoxynucleotides used in the Sanger sequencing reaction to terminate DNA strand elongation [14].
- Sequence Analysis Software & Database: Bioinformatics tools and curated libraries (e.g., MicroSEQ library with thousands of entries) to compare the obtained sequence for identification [14].
Visual Workflows and Pathways
The following diagrams illustrate the core workflows for the two primary identification methods discussed, providing a clear visual comparison of their processes.
16S rRNA Gene Sequencing Workflow
MALDI-TOF MS Identification Workflow
The rapid evolution of microbial identification technologies is fundamentally transforming the landscape of clinical and research microbiology. The convergence of artificial intelligence (AI), point-of-care (POC) testing, and multiplex assays represents a paradigm shift, offering unprecedented capabilities for identifying unknown bacterial pathogens and combating antimicrobial resistance (AMR). This guide provides an objective comparison of current commercial technologies, evaluating their performance, applications, and limitations within the context of unidentified bacteria research. As AMR continues to threaten global health—projected to claim millions of lives—these emerging tools offer promising avenues for accelerating diagnosis, streamlining therapeutic discovery, and improving patient outcomes [16]. We examine these technologies through the lens of experimental data, providing researchers with a practical framework for selecting appropriate methodologies for their specific investigative needs.
Technology Performance Comparison
The following tables provide a quantitative and qualitative comparison of the primary technology platforms used in modern bacterial identification and analysis.
Table 1: Comparative Analysis of Major Bacterial Identification Technology Platforms
| Technology Platform | Key Functionality | Example Commercial Kits/Systems | Typical Turnaround Time | Key Advantages | Major Limitations |
|---|---|---|---|---|---|
| AI-Driven Discovery Platforms | De novo design & screening of antimicrobial molecules; mines genomic data for novel peptides | Custom algorithms (e.g., from de la Fuente Lab, Stokes Lab) | Weeks (for in silico candidate identification) | Vastly expands searchable chemical space; can design "new-to-nature" antibiotics [16] | Candidates may be difficult to synthesize; requires extensive validation; quality dependent on training data [16] [17] |
| Multiplex Molecular POC Panels | Simultaneous detection of multiple pathogens & antibiotic resistance genes from clinical samples | BioFire FilmArray Panels (BCID, PN plus, ME) [18] [19] [20] | ~1 hour [18] [20] | Rapid results directly impact patient management; high overall agreement (>95%) with SOC [18] | Limited to pre-defined panel targets; may miss novel resistance mechanisms or pathogens not on the panel |
| Rapid Carbapenemase Detection Kits | Detection of genes encoding clinically relevant carbapenemases from bacterial isolates | Check-Direct CPE, eazyplex SuperBug, Xpert Carba-R [21] | < 4 hours | High reliability for major carbapenemase families (KPC, NDM, VIM, OXA-48); fit into local workflows [21] | Variable coverage of OXA-48-like variants and IMP subgroups; requires pure bacterial isolates [21] |
Table 2: Experimental Performance Data of Multiplex POC Testing vs. Standard Methods
| Performance Metric | BioFire FilmArray (POC) | Standard of Care Microbiology Testing (SOCMT) | Notes & Experimental Context |
|---|---|---|---|
| Overall Percent Agreement | 95.8% | (Reference) | Compared to SOCMT for bloodstream, respiratory, and CNS infections in a PICU study (n=111 samples) [18] |
| Positive Percent Agreement (PPA) | 100% | (Reference) | All phenotypically confirmed resistant isolates had corresponding resistance genes detected by FilmArray [18] |
| Negative Percent Agreement (NPA) | 95.6% | (Reference) | Same PICU study context [18] |
| Turnaround Time (TAT) | 1 - 1.5 hours [18] [20] | 48 - 72 hours [18] | Statistically significant reduction (p ≤ 0.001), enabling faster clinical decision-making [18] |
| Pathogen Detection Yield (BAL samples) | 45 pathogens | 21 pathogens | FilmArray identified significantly more pathogens in broncho-alveolar lavage samples (p ≤ 0.0001) [18] |
| Time to Antiviral Treatment | 36 hours faster | (Reference) | Associated with POC testing in adults with respiratory tract infections [20] |
Detailed Experimental Protocols for Technology Evaluation
To ensure the reliability and reproducibility of results when working with these advanced platforms, researchers must adhere to rigorously validated experimental protocols. The following sections detail the methodologies for key applications.
Protocol for Assessing AI-Generated Antimicrobial Candidates
This protocol outlines the workflow for validating AI-generated antibiotic candidates, from in silico design to in vitro testing [16].
- Step 1: Data Curation and Model Training. Assemble a rigorously curated training dataset. For instance, measure Minimum Inhibitory Concentrations (MICs) for thousands of molecules across diverse bacterial strains, holding variables like temperature, pH, and media constant to ensure comparability. Use this data to train machine learning (ML) models, either for virtual screening or generative design [16].
- Step 2: Candidate Generation.
- For Mining Algorithms: Deploy ML models to parse genomic and proteomic databases (e.g., from ancient or modern organisms) to identify sequences with predicted antimicrobial properties [16].
- For Generative Models: Use generative AI models, constrained to synthetically feasible molecular "building blocks," to design novel antibiotic candidates. One such approach generated 46 billion new, tractable compounds [16].
- Step 3: In Vitro Synthesis and Testing. Chemically synthesize the top candidate molecules. Test their antibacterial efficacy against target pathogens (e.g., Acinetobacter baumannii) in vitro by determining MICs. Further evaluate promising candidates in animal infection models (e.g., mouse skin abscess or thigh infection models) [16].
- Step 4: Mechanism of Action Studies. Investigate the candidate's mechanism of action. For antimicrobial peptides, this may involve assays to determine if the compound kills bacteria by depolarizing the cytoplasmic membrane [16].
Protocol for Evaluating Multiplex POC Panels in a Clinical Setting
This methodology describes the evaluation of a multiplex PCR system, like the BioFire FilmArray, against standard culture in a pediatric intensive care unit (PICU) [18].
- Step 1: Sample Collection and Study Design. Conduct a retrospective or quasi-randomized study. Collect matched samples (e.g., blood, broncho-alveolar lavage, cerebrospinal fluid) from patients with suspected infections. For a balanced design, assign patients to intervention (POC testing) and control (standard testing) arms on alternate days [18] [20].
- Step 2: Parallel Testing. Process each sample simultaneously with both methods:
- Standard of Care Microbiology Testing (SOCMT): Culture samples using appropriate media and automated systems (e.g., BACT/ALERT). Identify isolates using standard biochemical tests and perform antimicrobial susceptibility testing per CLSI guidelines [18].
- Multiplex POC Testing: According to manufacturer instructions, load the sample (e.g., 200 μL of respiratory sample or positive blood culture fluid) into the designated FilmArray pouch and run the test on the instrument [18].
- Step 3: Data Analysis. Calculate key performance metrics:
- Overall, Positive, and Negative Percent Agreement between the POC panel and SOCMT. -- Compare turnaround times (TAT) from sample collection to result availability using statistical tests like the chi-square test [18].
- Step 4: Impact Assessment. Analyze the impact of rapid results on antimicrobial stewardship, categorizing changes in therapy (e.g., stop, de-escalate, broaden spectrum, or start antivirals) [18].
Protocol for Testing Commercial Carbapenemase Detection Kits
This protocol evaluates the performance of molecular kits for detecting carbapenemase genes from cultured bacterial isolates [21].
- Step 1: Isolate Panel Preparation. Curate a well-characterized panel of bacterial isolates (e.g., 450 Enterobacteriaceae and Pseudomonas spp.) with previously defined carbapenem resistance mechanisms (e.g., KPC, NDM, VIM, OXA-48-like, IMP) and a set of carbapenemase-negative controls [21].
- Step 2: Kit Testing. Test all isolates using the commercial kits (e.g., Check-Direct CPE, eazyplex SuperBug complete A, Xpert Carba-R) strictly following the manufacturers' protocols for pure bacterial isolates [21].
- Step 3: Resolve Discrepancies. Investigate any discordant results (commercial kit vs. in-house reference method) using an in-house PCR assay followed by amplicon sequencing to definitively identify the carbapenemase allele present [21].
- Step 4: Performance Calculation. For each kit, calculate sensitivity and specificity for detecting each major carbapenemase family. Pay particular attention to the detection of variant enzymes, such as OXA-181, which may not be covered by all kit versions [21].
Visualizing Workflows and Relationships
The integration of these technologies into research and clinical workflows can be visualized through the following diagrams, which outline the logical sequence of steps and functional relationships.
Figure 1: A comparison of traditional microbiology workflows against emerging pathways leveraging POC multiplex PCR and AI-driven discovery.
Figure 2: Functional relationships between core technologies and their primary applications in modern microbiology.
The Scientist's Toolkit: Essential Research Reagents and Materials
Successful implementation of these emerging trends relies on a foundation of specific reagents, instruments, and computational tools.
Table 3: Key Research Reagent Solutions for Emerging Technology Applications
| Item | Function/Application | Example/Notes |
|---|---|---|
| BioFire FilmArray Panels | Syndromic multiplex PCR testing for pathogens and resistance genes directly from samples. | Panels available for Blood Culture ID (BCID), Pneumonia (PN plus), and Meningitis/Encephalitis (ME). Detects organisms and key resistance markers (e.g., mecA, vanA/B, CTX-M, KPC) [18] [19] [20]. |
| Xpert Carba-R Kit | Rapid detection of carbapenemase genes (KPC, NDM, VIM, IMP-1, OXA-48) from bacterial isolates. |
Useful for high-throughput screening of carbapenem-resistant Enterobacteriaceae; limited to predefined targets [21]. |
| Curated MIC & Genomic Datasets | Training data for AI/ML models to predict or design antimicrobial compounds. | Requires standardized, biologically relevant data with variables like pH and temperature controlled for model accuracy [16]. |
| Automated Synthesis Platforms | Physical generation of AI-designed molecular candidates for in vitro validation. | "Robots the size of a microwave" that synthesize molecules from code; essential for closing the AI-design-testing loop [16]. |
| Protein Language Models (pLMs) | AI systems that predict, generate, and optimize functional protein sequences for therapeutic design. | Trained on millions of natural sequences; a powerful tool with significant dual-use biosecurity risks that require safeguards [17]. |
| Larotrectinib Sulfate | Larotrectinib Sulfate, CAS:1223405-08-0, MF:C21H24F2N6O6S, MW:526.5 g/mol | Chemical Reagent |
| Lascufloxacin | Lascufloxacin, CAS:848416-07-9, MF:C21H24F3N3O4, MW:439.4 g/mol | Chemical Reagent |
The integration of AI, point-of-care testing, and multiplex assays is unequivocally reshaping the identification and study of unknown bacteria. Performance data consistently demonstrates that multiplex POC panels offer a significant advantage in speed and diagnostic yield over standard culture, directly impacting antimicrobial stewardship [18] [20]. Meanwhile, AI is breaking decades-long stagnation in antibiotic discovery by exploring vast new chemical spaces [16]. However, each technology presents constraints; POC panels are limited to predefined targets, and AI's promise is contingent on high-quality data and overcoming synthesis challenges [16] [17]. The future of microbial research lies not in using these tools in isolation, but in developing integrated frameworks where rapid diagnostic data feeds into AI-driven discovery platforms, creating a virtuous cycle of innovation to address the pressing challenge of antimicrobial resistance.
Selecting the appropriate DNA manipulation technology is a critical first step in research involving unidentified bacteria. The choice between long-read sequencing, high-throughput automation, and targeted enrichment methods directly impacts the success of genome assembly, functional characterization, and phylogenetic placement. This guide objectively compares leading commercial kits and platforms using published experimental data to help researchers align technological capabilities with specific project requirements, from outbreak investigations to comprehensive microbiome studies.
Comparative Performance of DNA Sequencing and Extraction Technologies
The table below summarizes key performance metrics for different DNA sequencing and extraction technologies based on controlled laboratory evaluations:
Table 1: Performance Comparison of DNA Sequencing and Extraction Technologies
| Technology Category | Specific Kits/Platforms Evaluated | Key Performance Metrics | Optimal Use Cases |
|---|---|---|---|
| Long-Read Sequencing | ONT Q20+ chemistry with:• Ligation Sequencing Kit (SQK-LSK114)• Rapid Barcoding Kit (SQK-RBK114)• DNA Extraction: Maxwell RSC vs. Monarch HMW [22] [23] | • ≥99% raw read accuracy [23]• Assembly length variation: 0.2-38 kb differences vs. reference [23]• Highest output: LSK114/Maxwell (10.65 Gb, 1.76M reads) [23]• Higher N50: NEB HMW DNA with either library kit [23] | • Bacterial outbreak investigations [22]• Complete genome closure [23]• Plasmid and repetitive region analysis [23] |
| High-Throughput Automated Systems | PANA HM9000 Automated System with manufacturer-matched kits [24] | • Concordance rate: 100% for EBV, HCMV, RSV [24]• Precision: CV <5% (intra- & inter-assay) [24]• LoD: 10 IU/mL for EBV/HCMV DNA [24]• Linearity: ∣r∣ ≥0.98 [24] | • Large-scale clinical pathogen screening [24]• Routine nucleic acid testing in clinical labs [24] |
| Targeted NGS with Host Depletion | Custom tNGS panel + novel filtration membrane [25] | • >98% host DNA reduction [25]• 6-8 fold increase in pathogen reads [25]• Covers >330 clinically relevant pathogens [25] | • Bloodstream infections with low pathogen abundance [25]• Samples with high host DNA background [25] |
Detailed Experimental Protocols and Methodologies
Protocol 1: Evaluation of Long-Read Sequencing for Bacterial Genomes
This protocol is adapted from the single-laboratory evaluation of ONT Q20+ chemistry for bacterial outbreak investigations [22] [23].
Sample Preparation:
- Select well-characterized bacterial strains (e.g., Salmonella enterica, Escherichia coli O157:H7) from a defined collection [23].
- Culture bacteria overnight using standard laboratory media appropriate for each strain.
DNA Extraction Methods (Compared):
- Maxwell RSC Cultured Cell DNA Kit: Automated system yielding high DNA concentration but more sheared fragments [23].
- Monarch High Molecular Weight (HMW) DNA Extraction Kit: Manual protocol designed to preserve long DNA fragments [23].
Library Preparation Protocols (Compared):
- Ligation Sequencing Kit (SQK-LSK114): More time-consuming and labor-intensive but produces higher sequencing output [23].
- Rapid Barcoding Sequencing Kit (SQK-RBK114): Faster workflow with fewer steps but generates lower sequencing output [23].
Sequencing and Analysis:
- Utilize ONT R10.4.1 flow cells with Q20+ chemistry [23].
- Perform basecalling and assembly using appropriate bioinformatics tools (e.g., Guppy, Flye).
- Compare assembly statistics: assembly length, contig number, N50, genome completeness, and percentage of ORFs recovered against reference genomes [23].
- Conduct in silico analyses for species identification, serotyping, virulence factors, and phylogenomic clustering [22].
Protocol 2: Comprehensive Validation of Automated High-Throughput Systems
This protocol follows the CLSI-based validation framework for automated nucleic acid detection systems [24].
Sample and Reference Material Sources:
- Use clinically characterized residual samples (e.g., plasma, oropharyngeal swabs) [24].
- Include WHO International Standards and National Reference Materials at defined concentrations [24].
Concordance Rate Assessment (CLSI EP12):
- Test positive and negative clinical samples in parallel on the automated system and a reference RT-qPCR platform [24].
- Calculate positive, negative, and overall concordance rates based on binary outcomes [24].
Accuracy and Linearity Evaluation (CLSI EP09/EP06):
- Dilute WHO standards to five concentration gradients in negative plasma matrix [24].
- Perform extractions and testing in triplicate for each concentration [24].
- Compare mean detected values to theoretical concentrations for accuracy [24].
- Assess linearity by calculating the correlation coefficient (∣r∣) across the dilution series [24].
Precision Testing (CLSI EP05):
- Conduct intra-assay (within-run) and inter-assay (between-run) precision studies [24].
- Report coefficients of variation (CV) for quantitative results [24].
Limit of Detection (LoD) Determination (CLSI EP17):
- Test dilutions of standardized materials at low concentrations [24].
- Establish the lowest concentration detectable in ≥95% of replicates [24].
Stress Testing for Operational Stability:
- Perform continuous operation at full capacity for 168 hours (7 days) [24].
- Monitor system status, error rates, and output quality throughout the testing period [24].
Protocol 3: Targeted NGS with Host DNA Depletion
This protocol implements a novel filtration and tNGS approach for enhanced pathogen detection [25].
Host Cell Depletion Using Specialized Filtration:
- Process blood samples through a human cell-specific filtration membrane.
- This membrane is engineered with surface charge properties to selectively capture nucleated cells, reducing host DNA background by over 98% [25].
Pathogen Concentration and Nucleic Acid Extraction:
- Recover pathogens from the filtrate via centrifugation.
- Extract nucleic acids using standard commercial kits appropriate for the target pathogens (bacterial, viral, fungal).
Targeted Library Preparation:
- Utilize a multiplex tNGS panel covering over 330 clinically relevant pathogens [25].
- The panel employs probe hybridization or multiplex PCR amplification to enrich pathogen-specific sequences [25].
Sequencing and Bioinformatic Analysis:
- Perform sequencing on a high-throughput platform (e.g., Illumina).
- Analyze data using a customized bioinformatics pipeline aligned with the tNGS panel targets.
- Compare results to conventional methods like blood culture and mNGS for validation [25].
Visualizing Technology Selection Pathways
The Scientist's Toolkit: Essential Research Reagent Solutions
Table 2: Key Research Reagents and Their Applications in Bacterial Studies
| Reagent / Kit Name | Primary Function | Application Context |
|---|---|---|
| Monarch HMW DNA Extraction Kit [23] | Extracts high molecular weight DNA with minimal fragmentation | Optimal for long-read sequencing to traverse repetitive regions and improve genome assembly [23] |
| Maxwell RSC Cultured Cell DNA Kit [23] | Automated extraction yielding high concentration DNA | Suitable for rapid processing when maximum read output is prioritized over read length [23] |
| ONT Ligation Sequencing Kit (SQK-LSK114) [23] | Prepares libraries for nanopore sequencing with high output | Ideal for projects requiring complete bacterial genomes and high consensus accuracy [22] [23] |
| ONT Rapid Barcoding Kit (SQK-RBK114) [23] | Rapid library preparation with barcoding for multiplexing | Enables faster turnaround for multiple samples with moderate output requirements [23] |
| Custom tNGS Panels [25] | Enriches sequences from specific pathogens of interest | Focuses sequencing power on predefined targets in complex samples with high host background [25] |
| Host Depletion Filtration Membranes [25] | Selectively removes human cells from clinical samples | Critical for enhancing pathogen detection in blood samples and other host-rich matrices [25] |
| WHO International Standards [24] | Provides standardized reference materials for quantification | Essential for assay validation, accuracy assessment, and cross-platform comparison [24] |
| Lazertinib | Lazertinib, CAS:1903008-80-9, MF:C30H34N8O3, MW:554.6 g/mol | Chemical Reagent |
| LCB 03-0110 | LCB 03-0110|Src/DDR Tyrosine Kinase Inhibitor |
The optimal foundation for unidentified bacteria research depends on a careful alignment of technological capabilities with project-specific goals. Long-read sequencing with Q20+ chemistry offers unparalleled potential for complete genome assembly and accurate strain typing in outbreak investigations. High-throughput automated systems provide exceptional reproducibility and efficiency for large-scale screening applications. Targeted NGS with integrated host depletion strategies enables sensitive detection in challenging sample matrices. By selecting kits and platforms based on the comprehensive performance data and validated protocols presented in this guide, researchers can establish a robust technological foundation capable of supporting their specific research objectives in bacterial characterization and discovery.
A Practical Workflow: From Sample to Identification
The reliability of any molecular analysis in bacterial research, from pathogen detection to whole-genome sequencing, is fundamentally dependent on the initial quality and quantity of the extracted DNA. The extraction method must efficiently lyse tough bacterial cell walls, particularly resilient Gram-positive species, while simultaneously inactivating nucleases and removing contaminants that can inhibit downstream enzymatic reactions [26] [27]. For researchers working with unidentified bacteria, the challenge is magnified; without a priori knowledge of the sample's Gram stain or cell wall properties, the chosen protocol must be robust enough to handle a wide spectrum of bacterial matrices. Inadequate DNA yield, purity, or integrity can lead to failed sequencing runs, inaccurate pathogen detection, and ultimately, erroneous conclusions [28].
The landscape of DNA extraction methodologies ranges from simple, inexpensive in-house protocols to sophisticated, automated commercial kits. While commercial kits offer standardized, quality-controlled reagents, their cost can be prohibitive for large-scale eco-epidemiological studies [26]. Furthermore, the optimal extraction method can vary significantly depending on the specific downstream application, whether it is PCR, metagenomic analysis, or long-read sequencing [29] [28]. This guide provides a comparative evaluation of various DNA extraction methods, supported by experimental data, to empower researchers in selecting and optimizing the ideal protocol for their work with diverse and unidentified bacterial samples.
Comparative Analysis of DNA Extraction Methods and Kits
Performance Metrics Across Commercial Kits and Simple Protocols
To objectively compare the performance of different DNA isolation approaches, researchers typically assess several key parameters: DNA yield (concentration), purity (assessed by absorbance ratios), integrity (fragment size), and, most critically, suitability for downstream applications like qPCR and sequencing. The table below synthesizes experimental findings from multiple studies evaluating various kits and methods on different bacterial samples.
Table 1: Comparative Performance of DNA Extraction Methods for Bacterial Analysis
| Method / Kit Name | Key Principle / Lysis Method | Best For / Sample Type | Reported Performance & Downstream Application Success |
|---|---|---|---|
| Ammonium Hydrolysis [26] | Chemical lysis (Ammonium hydroxide); Can be performed on intact ticks | Cost-effective qPCR: Sub-optimally stored ticks; Large-scale studies | "As good as any other method" for qPCR detection of B. burgdorferi; Low purity (A260/280 ~1.44) but amplifiable. |
| ZymoBIOMICS DNA Miniprep (ZM) [29] [30] | Bead-beating + Silica membrane columns | High Purity DNA: Gram-negative & Gram-positive bacteria; Microbial community standards | Highest purity (A260/230 ≥2.0); Good for Nanopore sequencing and accurate microbial community representation [30]. |
| Nanobind CBB Big DNA (NB) [30] | Magnetic disk for HMW DNA | Longest Read Lengths: Nanopore sequencing; Plasmid recovery | Yielded longest raw read N50 (>8,000 bp for some species); Superior for genome assembly [30]. |
| Fire Monkey HMW-DNA (FM) [30] | Spin-column with high g-force | Genome Assembly: Gram-negative bacteria; Pathogen WGS | Outperformed in genome assembly for Gram-negative bacteria [30]. |
| Quick-DNA HMW MagBead [28] | Magnetic beads for HMW DNA | Metagenomics: Complex mock communities; Fecal/spiked matrices | Best yield of pure HMW DNA; Accurate detection of most species in a complex mock community via Nanopore [28]. |
| NucleoSpin Soil (MNS) [27] | Bead-beating + Silica membrane; Lysozyme option | Ecosystem Microbiotas: Soil, rhizosphere, invertebrate, feces; High diversity samples | Highest alpha diversity estimates; Best contribution to overall sample diversity vs. computationally assembled reference communities [27]. |
| DNeasy Blood & Tissue (QBT) [26] [27] | Silica membrane spin columns | Gram-Positive Bacteria: Efficient lysis of hard-to-lyse cells | Highest extraction efficiency for Gram-positive bacteria in a mock community [27]. |
The Impact of Lysis and Purification Technology
The core differentiators among extraction methods lie in their cell lysis and DNA purification strategies, each with distinct advantages and drawbacks for bacterial analysis.
Lysis Methods: Bead-beating is highly effective for mechanically disrupting tough cell walls, including Gram-positive bacteria, and is crucial for unbiased lysis in diverse microbial communities [28] [27]. However, it can cause DNA shearing, potentially compromising the recovery of high-molecular-weight (HMW) DNA. Enzymatic lysis (e.g., with lysozyme) is a gentler alternative that helps preserve DNA integrity and has been specifically shown to improve the recovery of Gram-positive bacteria [27]. Chemical lysis using detergents or alkaline solutions, like ammonium hydroxide, is simple and low-cost but may result in lower purity DNA that requires careful evaluation for downstream applications [26].
Purification Methods: Silica spin columns are widely used and effective for purifying DNA from a range of contaminants. Magnetic beads offer scalability and are easier to automate, but they carry a risk of bead carryover, which can inhibit downstream enzymes in PCR and sequencing [31]. Phenol-chloroform extraction is a traditional method that can yield high-purity, HMW DNA but involves hazardous chemicals and is less suited for high-throughput or on-site applications [28] [32].
Experimental Protocols for Method Evaluation
To ensure the selected DNA extraction method is fit for purpose, researchers should conduct validation experiments using controls and metrics relevant to their specific goals.
Protocol 1: Evaluating Extraction Efficiency Using a Mock Community
Purpose: To assess the ability of a DNA extraction method to lyse different bacterial cells without bias and recover an accurate microbial profile [28] [27].
- Sample Preparation: Obtain a commercial microbial community standard (e.g., ZymoBIOMICS Microbial Community Standard) with a defined composition of Gram-positive and Gram-negative bacteria. Spike this standard into a sterile matrix that mimics your sample type (e.g., synthetic fecal matter) if needed.
- DNA Extraction: Extract DNA from multiple replicates of the mock community using the methods under evaluation (e.g., Kits A, B, and C).
- Downstream Analysis: Sequence the resulting DNA extracts using a standard platform (e.g., 16S rRNA amplicon sequencing or shotgun metagenomics).
- Data Analysis:
- Calculate Relative Abundances: Determine the relative abundance of each bacterial taxon in the sequenced samples.
- Compare to Expected Ratio: Compare the observed ratio of Gram-negative to Gram-positive bacteria (or the abundance of specific species) to the known ratio in the original standard. A method that deviates significantly from the expected ratio indicates a bias in lysis efficiency [27].
- Assess Community Representation: Evaluate which method recovers the highest number of expected species and most closely matches the defined community structure.
Protocol 2: Assessing DNA Suitability for Long-Read Sequencing
Purpose: To determine if the extracted DNA is of sufficient quantity, purity, and integrity for successful Nanopore sequencing and genome assembly [29] [30].
- DNA Extraction: Extract DNA from a pure culture of a target pathogen or a complex sample using the kits being compared (e.g., HMW-specific kits vs. standard kits).
- Quality Control:
- Quantity and Purity: Measure DNA concentration using fluorometry (Qubit) for accuracy. Assess purity via spectrophotometry (NanoDrop) with A260/A280 and A260/A230 ratios.
- Integrity: Analyze DNA fragment size distribution using gel electrophoresis (e.g., TapeStation) to confirm the presence of HMW DNA.
- Sequencing and Assembly: Perform Nanopore sequencing on a MinION or GridION flow cell. For a pure culture, aim for a target coverage (e.g., 50x).
- Performance Metrics:
- Sequencing Statistics: Calculate raw read length N50 (a measure where 50% of the assembled sequence is contained in reads of this length or longer). Longer N50 values are indicative of better HMW DNA.
- Assembly Metrics: Evaluate the completeness and contiguity of the final assembled genome. A higher quality assembly with fewer contigs and better plasmid recovery indicates a superior extraction method for this application [30].
The Scientist's Toolkit: Essential Reagents and Solutions
Successful DNA extraction relies on a suite of key reagents, each performing a critical function in the workflow.
Table 2: Key Research Reagent Solutions for DNA Extraction
| Reagent / Solution | Function in DNA Extraction |
|---|---|
| Lysis Buffer (with detergents like SDS) | Disrupts lipid membranes and releases cellular contents. |
| Proteinase K | Digests and removes contaminating proteins and nucleases. |
| Lysozyme | Enzymatically degrades the peptidoglycan layer of bacterial cell walls, critical for Gram-positive species [27]. |
| RNase A | Degrades RNA to prevent it from co-purifying with DNA and affecting quantification. |
| Binding Buffer | Creates conditions for DNA to bind to silica matrices (columns or beads). |
| Wash Buffer | Removes salts, proteins, and other impurities while leaving DNA bound. |
| Elution Buffer | A low-salt buffer or water used to release purified DNA from the silica matrix. |
| LDC4297 | LDC4297, MF:C23H28N8O, MW:432.5 g/mol |
| Lefamulin Acetate | Lefamulin Acetate - BC-3781 CAS 1350636-82-6 |
A Workflow for Selecting a DNA Extraction Method
The following diagram summarizes the key decision points for selecting an optimal DNA extraction method based on research objectives, sample type, and technical constraints.
DNA Extraction Method Selection Workflow
No single DNA extraction method is universally superior for all bacterial research scenarios. The optimal choice is a careful balance between research objectives (e.g., diagnostic qPCR vs. complete genome assembly), sample type (e.g., pure culture vs. complex microbiome), and practical constraints (e.g., throughput, cost, and automation needs) [26] [30] [27]. For research on unidentified bacteria, where sample properties are a mystery, a method validated for broad applicability—such as one that efficiently lyses both Gram-positive and Gram-negative cells and yields DNA compatible with the intended downstream application—is paramount.
Looking forward, the field of DNA extraction continues to evolve. Trends for 2025 and beyond point toward increased automation, miniaturization, and tighter integration with sequencing platforms [33]. There is a growing emphasis on developing rapid, gentle protocols that maximize the recovery of ultra-long DNA fragments to fully leverage the power of third-generation sequencing technologies. Furthermore, the development of bead-free purification technologies aims to mitigate the risk of carryover inhibition in sensitive downstream reactions [31]. By understanding the principles and performance data outlined in this guide, researchers can make informed decisions that ensure their sample preparation process provides a solid foundation for reliable and impactful scientific discovery.
Automated systems for bacterial identification (ID) and antibiotic susceptibility testing (AST) are cornerstone technologies in modern clinical and research microbiology. They address the critical need for rapid, accurate results to guide patient treatment and advance scientific research, particularly in the face of rising antimicrobial resistance. This guide provides an objective, data-driven comparison of two major systems: the VITEK 2 (bioMérieux) and the MicroScan (Beckman Coulter) platforms. The evaluation is framed within the broader context of validating commercial kits for research involving unidentified bacteria, a process that demands rigorous assessment of a system's accuracy, database comprehensiveness, and operational workflow.
These systems have evolved from manual biochemical methods, offering increased automation, reduced turnaround times, and standardized interpretation. For researchers, selecting an appropriate system depends on multiple factors, including the diversity of bacterial species in their samples, required throughput, need for susceptibility data, and the operational constraints of the laboratory environment.
VITEK 2 System
The VITEK 2 is a fully automated system that performs bacterial ID and AST using compact, sealed test cards containing 64 microwells. The system utilizes Advanced Colorimetry and kinetic fluorescence measurements to monitor metabolic changes every 15 minutes, enabling rapid results [34] [35]. Its software includes an ADVANCED EXPERT SYSTEM (AES) that analyzes Minimum Inhibitory Concentration (MIC) patterns to detect resistance mechanisms and phenotypes, providing an additional layer of result validation [35].
MicroScan System
The MicroScan system offers both conventional overnight panels and rapid fluorescent panels for ID and AST. The panels evaluated here, such as the Dried Overnight Positive ID Type 3 (PID3) for Gram-positive organisms and Dried Overnight Negative ID Type 2 (NID2) for Gram-negative organisms, are designed for manual inoculation and visual or automated reading. A key feature for low-resource settings is the availability of a customized MSFNPID1 panel that consolidates Gram-negative and Gram-positive test wells on a single panel [36].
Comparative Performance Data
The following tables summarize experimental data from independent studies evaluating the identification accuracy and susceptibility testing performance of both systems.
Table 1: Comparative Identification Accuracy for Gram-Positive Cocci
| Bacterial Species | VITEK 2 (% Correctly Identified) | MicroScan (% Correctly Identified) |
|---|---|---|
| Staphylococcus aureus | 99% (99/100) [34] | Data not available in search |
| Staphylococcus epidermidis | 90% (45/50) [34] | Data not available in search |
| Enterococcus faecalis | 92.7% (51/55) [34] | Data not available in search |
| Enterococcus faecium | 71.4% (20/28) [34] | Data not available in search |
| Streptococcus pneumoniae | 96.9% (64/66) [34] | Data not available in search |
| Overall Gram-positive isolates | 91.4% (351/384) [34] | 85.9% (110/128) [36] |
Table 2: Comparative Identification Accuracy for Gram-Negative Rods
| Bacterial Group/Species | VITEK 2 (% Correctly Identified) | MicroScan (% Correctly Identified) |
|---|---|---|
| Pseudomonas aeruginosa | 91.6% (citation:5] | Data not available in search |
| Acinetobacter baumannii | 76% (19/25) [37] | Data not available in search |
| Stenotrophomonas maltophilia | 100% (27/27) [37] | Data not available in search |
| Overall Gram-negative isolates | Data not available in search | 94.6% (185/195) [36] |
Table 3: Antimicrobial Susceptibility Testing (AST) Performance
| Performance Metric | VITEK 2 (for Gram-positive cocci) | MicroScan (Direct Inoculation from Blood Culture) |
|---|---|---|
| Overall Categorical Agreement | 96% [34] | 92.7% (GPC), 99.5% (Enterobacteria) [38] |
| Very Major Errors | 0.82% [34] | 0.04% (GPC) [38] |
| Major Errors | 0.17% [34] | 0.7% (GPC) [38] |
| Minor Errors | 2.7% [34] | Data not available in search |
Experimental Protocols and Methodologies
The experimental data cited in this guide were generated using standardized methodologies crucial for ensuring reproducible and comparable results. The following protocols detail the key procedures used in the evaluation studies.
Bacterial Strain Selection and Preparation
- Strain Collection: Studies used large collections of clinical isolates from hospitalized patients, ensuring relevance to real-world scenarios. For instance, one VITEK 2 evaluation used 384 clinical isolates of Gram-positive cocci, including Staphylococcus aureus, coagulase-negative staphylococci, Enterococcus spp., and Streptococcus species [34]. The MicroScan study utilized 367 clinical isolates from low-resource settings, encompassing a wide range of Gram-negative and Gram-positive pathogens [36].
- Storage and Subculturing: Isolates were typically stored at -70°C in broth-glycerol mixtures. Prior to testing, they were subcultured twice on appropriate solid media like Columbia agar with 5% sheep blood and grown overnight at 35°C to ensure purity and viability [34].
- Inoculum Standardization: A critical step for both systems is preparing a standardized bacterial suspension. This is done by emulsifying colonies in a saline solution and adjusting the turbidity to match a 0.5 McFarland standard, which approximates 1.5 x 10^8 CFU/mL [34] [38]. The same suspension is often used for both ID and AST panels.
Identification Testing Protocol
- VITEK 2 Inoculation and Loading:
- The standardized suspension is poured into a sterile tube.
- The ID card (e.g., ID-GPC for Gram-positive cocci) is placed in a filler tray.
- The system's vacuum filler automatically draws the suspension into the card's micro-wells.
- The card is sealed and transferred by the instrument to the reader-incubator module, where it is incubated at 35.5°C [34].
- MicroScan Panel Inoculation and Processing:
- The standardized suspension is used to rehydrate the dried substrates in the plastic panel wells.
- The panel is sealed and incubated aerobically at 35°C for 16-24 hours (overnight) [36].
- After incubation, reactions are read either manually by visualizing color changes or automatically using a device like the MicroScan autoSCAN-4 reader.
- The pattern of positive and negative reactions is interpreted by the LabPro software, which compares it to a database for species identification [36].
Antibiotic Susceptibility Testing (AST) Protocol
- VITEK 2 AST: The process is fully integrated. The AST card (e.g., AST-P515 for staphylococci) is filled automatically from the same suspension as the ID card. The system uses kinetic fluorescence measurements to monitor bacterial growth in the presence of antibiotics every 15 minutes, generating a growth curve and calculating the MIC [34].
- Reference Broth Microdilution Method (for validation): As a gold standard for AST validation, the agar or broth microdilution method is performed according to Clinical and Laboratory Standards Institute (CLSI, formerly NCCLS) guidelines [34]. A 0.5 McFarland suspension is used to inoculate a panel containing serial two-fold dilutions of antibiotics. After overnight incubation, the MIC is recorded as the lowest concentration of antibiotic that inhibits visible growth.
Data Analysis and Validation
- Comparative Methods: For identification, system results are compared to those from established methods like API strips (e.g., API Staph, API 20 Strep) supplemented with conventional tests (coagulase, optochin, serological typing) [34].
- Error Rate Calculation: AST results are compared to the reference microdilution method. Discrepancies are categorized as:
Workflow Visualization
The following diagram illustrates the core procedural pathways for both the VITEK 2 and MicroScan systems, highlighting the contrast between full automation and manual steps.
Research Reagent Solutions
This table details the key consumables and reagents essential for operating the VITEK 2 and MicroScan systems, as derived from the evaluated studies.
Table 4: Essential Research Reagents and Materials
| Item Name | System | Function in Protocol |
|---|---|---|
| ID-GPC Card | VITEK 2 | Gram-positive bacterial identification via 46 fluorimetric tests [34]. |
| AST-P515 Card | VITEK 2 | Antibiotic susceptibility testing for staphylococci [34]. |
| Dried Overnight PID3 Panel | MicroScan | Gram-positive bacterial identification via biochemical substrates [36]. |
| Dried Overnight NID2 Panel | MicroScan | Gram-negative bacterial identification via biochemical substrates [36]. |
| MSFNPID1 Panel | MicroScan | Custom panel combining Gram-positive and negative tests for flexibility [36]. |
| 0.45% Saline Solution | Both | Standard diluent for preparing bacterial inoculum [34]. |
| Columbia Agar with 5% Sheep Blood | Both | Standard medium for subculturing and ensuring isolate purity [34]. |
| API Staph / API 20 Strep | Reference | Comparative method for validating system identification results [34]. |
The experimental data demonstrates that both the VITEK 2 and MicroScan systems are capable platforms for bacterial identification, with the choice of system heavily dependent on the specific research context and operational needs.
The VITEK 2 system excels in settings where speed and full automation are priorities. Its ability to provide ID and AST results within a few hours, combined with the sophisticated ADVANCED EXPERT SYSTEM for resistance detection, makes it a powerful tool for high-throughput laboratories [34] [35]. However, its performance can vary by organism, as seen with the lower identification rate for Enterococcus faecium (71.4%) and Acinetobacter baumannii (76%) [34] [37].
The MicroScan system, particularly its dried overnight panels, offers excellent accuracy for Gram-negative rods (94.6%) and good accuracy for Gram-positive cocci (85.9%) [36]. Its strengths include a long shelf life, the flexibility of manual reading, and the availability of a combined panel (MSFNPID1). However, its reliance on overnight incubation and manual steps that can be error-prone represents a trade-off [36]. A critical finding for researchers is that both systems are highly dependent on their internal databases; species not represented in these databases are frequently misidentified [36].
For researchers evaluating commercial kits for unidentified bacteria, this analysis underscores the importance of:
- Database Comprehensiveness: Verify that the system's database covers the taxonomic groups relevant to your research.
- Defining Performance Needs: Balance the need for speed (favoring VITEK 2) against budget, infrastructure, and the need for panel flexibility (where MicroScan may be advantageous).
- Robust Validation: Always employ complementary methods, especially when working with novel or uncommon isolates, to confirm system results.
Both systems represent mature technological solutions that, when selected and validated appropriately, can significantly accelerate and standardize microbiological research.
The accurate identification of bacteria is a cornerstone of research in microbiology, disease diagnosis, and drug development. Commercial identification kits provide standardized, reliable, and accessible methods for this purpose, moving beyond the variability of traditional laboratory techniques. These kits are broadly categorized into phenotypic systems, which identify bacteria based on their biochemical reactions and metabolic properties, and genotypic/proteomic systems, which identify organisms based on their unique genetic or protein signatures [39]. Manual or semi-automated systems, such as API strips, require manual inoculation and observation, while automated systems provide more hands-off operation [40].
This guide objectively compares the performance of the classic API strip system with alternative rapid methods, including molecular PCR kits and the proteomic MALDI-TOF MS technique. The comparison is framed within a research context focused on identifying unknown bacterial isolates, providing experimental data on accuracy, cost, and workflow to help researchers select the most appropriate tool.
Performance Comparison of Identification Methods
The following table summarizes a direct comparison of key identification methods based on experimental studies.
Table 1: Comparative Performance of Bacterial Identification Methods
| Method | Principle | Example / Kit | Relative Accuracy | Sample Throughput | Time to Result | Approx. Cost per Sample | Key Advantage | Key Limitation |
|---|---|---|---|---|---|---|---|---|
| Biochemical (Semi-automated) | Enzyme activity & substrate utilization | API 20E Strip [41] | 96% specificity vs. serotyping [41] | Low to Medium | 18-24 hours [39] | ~$6 [41] | Low initial equipment cost; individual sample testing | Database inaccuracies; cannot differentiate closely related species [39] |
| Genetic (PCR) | Amplification of specific DNA sequences | invA PCR for Salmonella [41], foodproof Salmonella Kit [42] | 100% sensitivity vs. 16S rRNA sequencing [41] | Medium to High | 3-4 hours [41] [42] | <$2 (lab materials) [41] | High sensitivity and specificity; rapid results | High initial equipment investment; requires technical expertise |
| Proteomic (MALDI-TOF MS) | Analysis of ribosomal protein spectra | MALDI-TOF MS [39] | 72.3% species-level concordance with API [39] | High | Minutes per sample [39] | Lower than conventional methods [39] | Extremely fast; high efficiency and precision | Extremely high equipment cost; limited by database size [39] |
Key Experimental Findings from Comparative Studies
- API 20E vs. Molecular Methods: A study identifying Salmonella enterica from swine farms found that the API 20E system, when used at a high likelihood threshold (99.9%), showed excellent agreement with molecular standards. Its sensitivity and specificity were 100% and 96%, respectively, compared to 16S rRNA sequencing, and 96% and 86% compared to serotyping [41]. The study concluded that caution is necessary for likelihoods below 99.9% [41].
- API vs. MALDI-TOF MS: A study on fish digestive content found that MALDI-TOF MS demonstrated a 72.3% concordance with API at the species level [39]. While this shows good agreement, the research highlighted the limitations of the phenotypic API technique compared to the speed and precision of MALDI-TOF MS [39].
Detailed Experimental Protocols
To ensure reproducibility and provide a clear understanding of the methodologies behind the performance data, this section outlines standard protocols for the key techniques.
Protocol for Bacterial Identification Using API 20E Strips
The API 20E system is a standardized gallery of 20 miniature biochemical tests used primarily for identifying Enterobacteriaceae and other Gram-negative rods [41] [40].
Workflow Overview:
Materials:
- API 20E strip (bioMérieux) [41]
- API Suspension Medium [40]
- Incubation chamber (37°C) [40]
- Pure culture of the isolated bacterium [40]
Step-by-Step Procedure:
- Inoculum Preparation: From a pure, fresh culture (18-24 hours old), prepare a bacterial suspension in the sterile suspension medium to a specified turbidity (e.g., 0.5 McFarland standard) [40].
- Strip Inoculation:
- Incubation: Place the inoculated strip in a humidified chamber and incubate at 35-37°C for 18-24 hours [41] [40].
- Reading Results: After incubation, read the reactions. Some tests require the addition of reagents (e.g., Kovac's reagent for indole, Barritt's reagents for VP test) [41] [40]. Record results as positive or negative based on color changes or other visual indicators.
- Identification: Use the reactions to create a 7- or 9-digit profile number. Consult the API database or software to obtain the identification, often given with a percentage probability [40].
Protocol for Bacterial Detection via PCR
PCR-based kits, such as the invA PCR for Salmonella, detect organisms with high specificity by targeting unique genetic sequences [41] [42].
Workflow Overview:
Materials:
- Primers specific to the target (e.g., invA for Salmonella) [41]
- Taq DNA polymerase [41]
- Deoxynucleoside triphosphates (dNTPs) [41]
- PCR buffer (Tris-HCl, KCl, MgCl2) [41]
- Thermocycler [41]
- Gel electrophoresis equipment [41]
Step-by-Step Procedure:
- DNA Extraction: Extract template DNA from a bacterial colony. A common method is to resuspend a colony in sterile water, boil for 5 minutes, and use the supernatant as the template [41]. Commercial kits like the DNeasy Blood and Tissue Kit (QIAGEN) are also highly efficient for this purpose [43].
- Reaction Setup: Prepare a PCR mixture on ice. A typical 25 µL reaction contains:
- 1x PCR Buffer
- 1.5 mM MgCl2
- 250 µM of each dNTP
- 0.4 µM of each forward and reverse primer
- 0.5-1.0 unit of Taq DNA polymerase
- 2 µL of template DNA [41]
- Thermocycling: Place the tubes in a thermocycler and run a program tailored to the primer set. An example program is:
- Initial Denaturation: 94°C for 2-5 minutes
- 30-35 cycles of:
- Denaturation: 94°C for 30 seconds
- Annealing: 55-65°C for 30 seconds (temperature primer-dependent)
- Extension: 72°C for 1 minute
- Final Extension: 72°C for 5-10 minutes [41]
- Amplicon Analysis: Separate the PCR products by gel electrophoresis (e.g., 1.5-2% agarose gel). Visualize the DNA bands under UV illumination after staining with an intercalating dye. A band of the expected size (e.g., 244-bp for invA) indicates a positive result [41] [44].
Essential Research Reagent Solutions
Table 2: Key Materials and Their Functions in Bacterial Identification
| Item | Function in Research | Example / Manufacturer |
|---|---|---|
| DNA Extraction Kit | Isposes high-quality genomic DNA from samples for downstream molecular applications. | DNeasy Blood & Tissue Kit (QIAGEN) [43] |
| Universal 16S rRNA Primers | Amplifies a conserved region of the bacterial 16S rRNA gene, serving as a DNA quality control or for taxonomic identification. | Integrated DNA Technologies [41] |
| Real-time PCR Master Mix | Contains reagents (polymerase, dNTPs, buffer) optimized for quantitative PCR (qPCR), enabling detection and quantification. | Included in kits like foodproof [42] |
| Sterile Paper Points | Minimally invasive tool for collecting biofilm or fluid samples from confined spaces, such as periodontal pockets. | VDW Dental [43] |
| Selective & Differential Media | Supports the growth of target bacteria while inhibiting others and provides visual clues based on metabolic characteristics. | Xylose-lysine-tergitol-4, Brilliant Green agar (Remel) [41] |
| API 20E Strip | Standardized system for biochemical profiling and identification of Enterobacteriaceae and other Gram-negative rods. | API 20E (bioMérieux) [41] [40] |
The choice between semi-automated manual kits and rapid tests is a trade-off between cost, speed, accuracy, and laboratory infrastructure.
- API Strips remain a cost-effective solution for laboratories with low sample volumes and limited capital for large equipment. Their main advantage is the low initial investment and the ability to process samples individually. However, users must be aware of their limitations in differentiating closely related species and should only accept high-likelihood identifications (>99.9%) as reliable [41] [39].
- PCR-based Kits offer superior sensitivity and specificity, with a faster turnaround time than culture-based methods. While the per-test cost can be low, the requirement for a thermocycler and electrophoretic equipment represents a significant initial investment. They are most economical in labs with high sample throughput [41].
- MALDI-TOF MS represents the pinnacle of speed and precision for high-volume laboratories. Despite its high equipment cost, its low per-sample cost and rapid results make it a powerful tool for clinical and research settings that can support the investment [39].
In conclusion, the "best" method is context-dependent. For research focused on unidentified bacteria, a combination of methods may be optimal: using API strips for initial low-cost characterization and employing genetic methods like PCR for definitive confirmation or when high throughput and speed are essential.
The accurate identification of bacteria is a cornerstone of public health, clinical diagnostics, and pharmaceutical quality control. The performance of any downstream molecular analysis, from antimicrobial resistance (AMR) gene detection to whole-genome sequencing, is fundamentally dependent on the initial quality of the extracted bacterial DNA [45] [46]. This guide provides an objective comparison of commercial bacterial DNA extraction kits, summarizing critical experimental data to help researchers select the optimal methodology for their specific sample type—be it clinical, food, water, or pharmaceutical.
Comparative Analysis of Commercial DNA Extraction Kits
A rigorous 2025 comparative study systematically evaluated three leading commercial DNA extraction kits for their performance in isolating genomic DNA from two challenging, multidrug-resistant bacterial pathogens: Pseudomonas aeruginosa and Enterobacter cloacae [46] [47]. The study assessed kits based on DNA yield, purity, and, crucially, the downstream impact on long-read sequencing and AMR determinant detection.
Table 1: Comparison of DNA Extraction Kit Performance Metrics
| Extraction Kit | Average DNA Yield | DNA Integrity/Purity | Sequencing Output | Key Strengths | Optimal Use Cases |
|---|---|---|---|---|---|
| DNeasy UltraClean Microbial Kit (Qiagen) | Up to 4.7x higher than MagAttract [46] | Lower integrity compared to MagAttract [46] | ~50% higher than MagAttract [46] | High yield for ample sequencing | High-throughput AMR surveillance |
| MagAttract HMW DNA Kit (Qiagen) | Lower yield than DNeasy [46] | Higher integrity; more contiguous assemblies [46] | Lower than DNeasy [46] | Superior assembly continuity | Complex genome analysis |
| MagMAX Microbiome Ultra Kit (ThermoFisher) | Not specified | Not specified | Not specified | Comprehensive workflow | Microbiome studies |
The data reveals a clear trade-off: the DNeasy kit provided the highest DNA yield, which translated to a significantly greater sequencing output. In contrast, the MagAttract kit produced DNA with higher integrity, leading to more contiguous genome assemblies [46]. This dichotomy is critical for researchers to consider based on their primary goal—whether it is maximizing data volume or achieving the best possible genome reconstruction.
Table 2: Downstream Impact on AMR Gene Detection (%)
| Extraction Kit + Assembler Combination | Overall AMR Determinants Detected | Efflux Pump Genes Detected |
|---|---|---|
| DNeasy + Flye | 95.2% [46] | Best performance (specific % not provided) [46] |
| MagMAX + Unicycler | 67.8% [46] | Poorest performance (37.5% difference vs. best) [46] |
The choice of bioinformatics tools proved to be as important as the extraction method itself. Across all kits, the Flye assembler consistently outperformed Unicycler, increasing the detection of AMR determinants by 2 to 14 percentage points [46]. The best-performing combination, DNeasy with Flye, successfully detected 95.2% of AMR determinants, while the poorest-performing combination detected only 67.8% [46]. This underscores that a holistic workflow optimization—from extraction to analysis—is essential for reliable results in AMR research.
Experimental Protocols for Kit Evaluation
The following section details the core methodologies used in the comparative study to generate the data presented above. Adherence to such standardized protocols is vital for ensuring reproducible and comparable results when evaluating kit performance.
Bacterial Isolates and DNA Extraction
- Bacterial Strains: The study used clinical isolates of Pseudomonas aeruginosa (n=63) and Enterobacter cloacae (n=96). These are both ESKAPE pathogens known for high levels of antimicrobial resistance and pose significant challenges in clinical care. P. aeruginosa, with its high GC-content (~67%), presents a particular challenge for DNA extraction and sequencing [46] [47].
- Extraction Kits: The three kits evaluated were the MagAttract HMW DNA Kit (Qiagen), the DNeasy UltraClean Microbial Kit (Qiagen), and the MagMAX Microbiome Ultra Nucleic Acid Isolation Kit (ThermoFisher). Extractions were performed according to the manufacturers' instructions [47].
- DNA Quality Control: The quantity and quality of the extracted genomic DNA were assessed using a tripartite approach:
Sequencing and Bioinformatic Analysis
- Library Preparation and Sequencing: Libraries were prepared from the extracted DNA and sequenced using Oxford Nanopore Technologies (ONT) platforms to generate long-read data [46].
- Genome Assembly: The resulting sequencing data was assembled using two different assemblers:
- Unicycler (v.0.5.1)
- Flye (v.2.9.6)
- Assembly Quality Assessment: The quality of the assembled genomes was assessed with QUAST (v.5.3), and genome completeness was evaluated with CheckM (v.1.1.6) [46] [47].
- AMR Determinant Identification: Antimicrobial resistance genes were identified from the assemblies using AMRFinderPlus (v.4.1.19) [47].
Diagram Title: Workflow for DNA Kit Comparison
The Scientist's Toolkit: Essential Research Reagents and Instruments
A successful DNA extraction and analysis workflow relies on a suite of specialized reagents and instruments. The table below details key materials used in the featured comparative study.
Table 3: Key Research Reagent Solutions for Bacterial DNA Analysis
| Item | Function/Description | Specific Examples |
|---|---|---|
| DNA Extraction Kits | Isolate genomic DNA from bacterial samples; protocols vary by kit. | MagAttract HMW DNA Kit (Qiagen), DNeasy UltraClean Microbial Kit (Qiagen), MagMAX Microbiome Ultra Kit (ThermoFisher) [46]. |
| Nucleic Acid Quantification | Accurately measure DNA concentration and purity. | NanoDrop (spectrophotometry), Qubit (fluorometry) [46]. |
| DNA Integrity Analysis | Assess the size distribution and quality of extracted DNA. | Agilent TapeStation 2200 (capillary electrophoresis) [46]. |
| Sequencing Platform | Generate long-read sequencing data for genome assembly. | Oxford Nanopore Technologies (ONT) platforms [46]. |
| Bioinformatics Tools | Assemble sequences, assess quality, and identify resistance genes. | Flye/Unicycler (assembly), QUAST (quality), CheckM (completeness), AMRFinderPlus (AMR genes) [46]. |
| LEI105 | LEI105 | LEI105 is a potent, selective DAGL-α/β inhibitor that reduces 2-AG levels. For Research Use Only. Not for human or veterinary diagnostic or therapeutic use. |
| LEM-14 | LEM-14, MF:C25H26N4O4S, MW:478.6 g/mol | Chemical Reagent |
Application Across Sample Types
The principles of kit selection and workflow optimization must be adapted to the unique challenges presented by different sample matrices.
Clinical Samples
Clinical microbiology is undergoing a rapid transformation with the integration of novel technologies to shorten the time-to-result for pathogen identification and AST [45]. While traditional phenotypic AST remains the gold standard, molecular methods like those described in this guide are becoming indispensable. For instance, rapid molecular tests like the Streck ARM-D Kits can detect specific resistance genes (e.g., for carbapenemases, ESBLs) directly from bacterial isolates, aiding antibiotic stewardship programs [48]. Furthermore, deep learning approaches are being developed to automate the identification of bacteria from Gram-stained clinical smears, a process known as Microbiological Rapid On-Site Evaluation (M-ROSE), which can provide critical references for diagnosis within hours [49].
Pharmaceutical and Water Analysis
In the pharmaceutical industry, water is a critical raw material used in drug formulation, equipment cleaning, and as a solvent [50] [51]. The quality of pharmaceutical water (e.g., Water for Injection, WFI) is stringently regulated by pharmacopeias like the USP and EP to ensure it is free from microorganisms and endotoxins [50] [52]. While this guide focuses on bacterial DNA extraction from isolates, the detection of bacterial contamination in pharmaceutical water systems is a related and vital application. The market for pharmaceutical water is growing significantly, driven by the expansion of the biopharmaceutical industry and rising demand for biologics and biosimilars, which require ultra-pure water in their manufacturing [51] [52]. The principles of selecting a DNA extraction kit that maximizes yield or integrity would directly apply to environmental monitoring programs within a pharmaceutical facility, where detecting low levels of contamination is crucial.
The selection of a bacterial DNA extraction kit is a consequential decision that ripples through all subsequent analytical steps. The experimental data clearly demonstrates that no single kit is superior in all metrics; instead, the choice hinges on the research objectives. For projects prioritizing the highest possible detection rate of AMR determinants, such as in genomic epidemiology and surveillance, a kit optimized for high DNA yield paired with a modern assembler like Flye is recommended [46]. Conversely, research requiring the most accurate genome reconstruction may benefit from a kit that prioritizes DNA integrity, even at the cost of lower yield. Researchers must therefore align their selection with their specific goals, whether working with clinical, food, water, or pharmaceutical samples, to ensure the reliability and accuracy of their findings in the critical fight against unidentified and multidrug-resistant bacteria.
In the field of clinical and food microbiology, the rapid and accurate identification of pathogenic bacteria is a cornerstone of effective diagnostics and subsequent therapeutic intervention. The broader thesis of evaluation commercial kits in unidentified bacteria research centers on systematically comparing the performance, reliability, and practical applicability of different diagnostic platforms. This guide provides an objective comparison of several advanced methodologies, including Matrix-Assisted Laser Desorption/Ionization Time-of-Flight Mass Spectrometry (MALDI-TOF MS) systems and a novel molecular technique, by presenting supporting experimental data on their identification accuracy, speed, and limitations. The findings are critical for researchers, scientists, and drug development professionals who rely on precise microbiological data.
Performance Comparison of Microbial Identification Systems
The following tables summarize the quantitative performance data of different microbial identification systems as reported in recent studies. This data allows for a direct comparison of their efficacy.
Table 1: Performance of Direct MALDI-TOF MS Identification from Positive Blood Cultures [53]
This table details the performance of a simplified, rapid MALDI-TOF MS method for identifying microorganisms directly from positive blood culture bottles, without prior isolation on routine media. The study analyzed 128 microorganisms.
| Microorganism Type | Identified to Species Level | Identified to Genus Level | Misidentified | Not Identified |
|---|---|---|---|---|
| All Organisms | 97 (75.8%) | 4 (3.1%) | 3 (2.3%) | 24 (18.8%) |
| Gram-Negative Bacteria | 55 (90.16%) | 2 (3.28%) | - | 4 (6.56%)* |
| Gram-Positive Bacteria | 38 (69.1%) | - | 2 (3.6%)* | 15 (27.3%) |
| Yeasts | 4 (33.3%) | 1 (8.3%) | 2 (16.7%)* | 5 (41.7%) |
*Note: The values for misidentified and not identified Gram-Negative bacteria, and for identified to genus level and misidentified Gram-Positive bacteria, were aggregated in the source. The table above distributes the aggregated figures for a complete view based on the original data context. The "Not Identified" count for Gram-Negative Bacteria includes organisms that were not identified or misidentified. [53]
Table 2: Comparative Identification of Raw Milk Bacteria by Two MALDI-TOF MS Systems [54]
This study compared the identification performance of two commercial MALDI-TOF MS systems, the Bruker Microflex LT Biotyper and the Zybio EXS2600, using 1,130 bacterial isolates from raw milk.
| Identification Level | Bruker Biotyper | Zybio EXS2600 |
|---|---|---|
| To Species Level | 73.63% | 74.43% |
| To Genus Level Only | 20.97% | 16.86% |
| Not Identified | 5.40% | 8.71% |
Table 3: Key Features of a Novel Rapid PCR-Based Identification and Quantification Method [55]
This table summarizes the core attributes of a novel real-time PCR-based method (Tm mapping method) that can identify and quantify unknown pathogenic bacteria in a blood sample within four hours.
| Feature | Description |
|---|---|
| Time to Result | Within 4 hours of sample collection. |
| Key Innovation | Quantification of unknown bacteria in a clinical sample, adjusted for the 16S rRNA operon copy number. |
| Method Core | Tm mapping method using bacterial universal primers and a real-time PCR system. |
| Critical Reagent | Eukaryote-made thermostable DNA polymerase, free from bacterial DNA contamination. |
| Application | Suggested as a novel biomarker for estimating the severity of microbial infection and monitoring therapeutic effect. |
Experimental Protocols for Key Methodologies
This protocol describes a simplified processing method for positive blood cultures.
- Sample Collection: 4.0 mL of blood is taken from a positive blood culture bottle (BD BACTEC FX40 or BacT/ALERT System) that shows a single organism in a direct Gram-stained film.
- Centrifugation: The sample is transferred to a tube containing a plasma separation gel and centrifuged at 3000 g for 10 minutes.
- Washing: The supernatant is discarded, and the precipitate is resuspended in 1.0 mL of deionized water.
- Target Spotting: 1 µL of the suspension is spotted in triplicate on a MALDI-TOF MS target plate.
- Matrix Application:
- For bacteria, 1 µL of alpha-cyano-4-hydroxycinnamic acid (CHCA) matrix solution is added to each spot and left to dry completely.
- For yeast, 0.5 µL of formic acid (FA) is added to the spot and allowed to evaporate before adding 1 µL of CHCA matrix solution.
- MS Analysis: The target plate is analyzed using the Vitek MS V3.2 system (bioMérieux). Quality control is performed with E. coli ATCC 8739.
- Interpretation: Identification is based on a confidence score provided by the software. A score of 95-99.9% is considered high for species-level identification, and 90-94% for genus-level.
This protocol was used for the comparative identification of raw milk bacteria.
- Protein Extraction: Protein extraction is performed using the standard formic acid/acetonitrile protocol.
- Target Preparation: The prepared extracts (1 µL) are applied to a steel 96-spot plate and left to dry. The sample is then coated with 1 µL of a matrix solution (HCCA) and dried at room temperature. Bacteria from the same colony are applied onto two separate spots on the same plate for each system.
- Analysis with Bruker System: The target is analyzed with a Microflex LT MALDI-TOF MS in positive linear mode (mass range: 2000–20000 m/z). Spectra are recorded and identified using MBT Compass software (database: 10830 entries).
- Analysis with Zybio System: The same target is analyzed with an EXS2600 MALDI-TOF MS in positive linear mode (same mass range). Spectra are recorded and identified using System Ex-Accuspec software (database: ~15,000 entries).
- Identification Criteria: For both systems, a score ≥ 2.000 indicates species-level identification, a score between 1.700-1.999 indicates genus-level, and a score < 1.700 is an identification failure.
This protocol enables identification and quantification within four hours of blood collection.
- Bacterial DNA Extraction: Bacterial DNA is extracted directly from 2 mL of a whole blood sample. The sample is centrifuged at low speed (100×g, 5 min) to pellet red blood cells, and the supernatant with the buffy coat is used. Lysis uses Proteinase K and small beads to maximize efficiency.
- Nested PCR: The extracted DNA is used as a template for a nested PCR with seven bacterial universal primer sets. The PCR uses a eukaryote-made thermostable DNA polymerase to avoid false positives from bacterial DNA contamination.
- Tm Value Acquisition: The seven PCR amplicons are analyzed to acquire their melting temperature (Tm) values.
- Tm Mapping: The seven Tm values are mapped in two dimensions, creating a unique species-specific "Tm mapping shape." This shape is compared to a database for identification.
- Quantification: A standard curve is formed using Ct values from three quantification standards (E. coli DNA with known concentrations). The bacterial concentration is first calculated as E. coli equivalents and then corrected based on the 16S rRNA operon copy number of the identified pathogen.
Visualized Workflows and Signaling Pathways
The following diagrams, generated with Graphviz, illustrate the logical workflows of the key experimental protocols described.
Direct MALDI-TOF MS Identification Workflow
Tm Mapping Method Identification and Quantification
The Scientist's Toolkit: Essential Research Reagents and Materials
Table 4: Key Research Reagent Solutions for Featured Experiments
This table details essential materials and their functions as used in the protocols cited in this guide.
| Item | Function/Application | Relevant Experiment |
|---|---|---|
| VITEK MS V3.2 (bioMérieux) | MALDI-TOF MS system for rapid microbial identification using spectral protein profiling. | Direct ID from Blood Cultures [53] |
| MALDI Biotyper (Bruker Daltonics) | MALDI-TOF MS system for microbial identification; compared against Zybio system. | Comparative Milk Bacteria Analysis [54] |
| EXS2600 (Zybio) | MALDI-TOF MS system for microbial identification; compared against Bruker system. | Comparative Milk Bacteria Analysis [54] |
| Alpha-Cyano-4-Hydroxycinnamic Acid (CHCA) | Matrix solution for MALDI-TOF MS; co-crystallizes with the sample for laser desorption/ionization. | Direct ID from Blood Cultures, Comparative Analysis [53] [54] |
| Formic Acid | Used in sample preparation, especially for yeasts, to enhance protein extraction and spectral quality. | Direct ID from Blood Cultures [53] |
| Eukaryote-Made Thermostable DNA Polymerase | A recombinant DNA polymerase produced in yeast, free from bacterial DNA contamination, enabling sensitive and reliable bacterial universal PCR. | Novel Rapid PCR-Based Method [55] |
| Bacterial Universal Primers | Primer sets targeting conserved regions (e.g., in 16S rRNA gene) to amplify a broad range of bacterial species for identification. | Novel Rapid PCR-Based Method [55] |
| Plasma Separation Gel | Used in centrifugation to separate plasma and cells from positive blood cultures for cleaner sample preparation. | Direct ID from Blood Cultures [53] |
| Leniolisib | Leniolisib|PI3Kδ Inhibitor|CAS 1354690-24-6 | |
| Lesinurad Sodium | Lesinurad Sodium, CAS:1151516-14-1, MF:C17H13BrN3NaO2S, MW:426.3 g/mol | Chemical Reagent |
Solving Common Challenges in Bacterial Identification
Troubleshooting Low DNA Yield and Purity from Complex Samples
In unidentified bacteria research, the initial step of DNA extraction is a critical determinant of success for all downstream molecular applications, including next-generation sequencing (NGS), polymerase chain reaction (PCR), and metagenomic analysis. The fundamental challenge researchers face is that complex samples—such as soil, stool, blood, and subgingival biofilms—contain not only the target microbial cells but also numerous potent PCR inhibitors like humic acids, hemoglobin, and bilirubin. Furthermore, the diverse cellular structures of bacteria, particularly the thick peptidoglycan layer in Gram-positive species, necessitate robust lysis methods that can simultaneously preserve DNA integrity. Inefficient lysis or incomplete removal of these contaminants directly leads to the common problems of low DNA yield and purity, which can compromise assay sensitivity, produce biased microbial diversity data, and ultimately hinder research progress. This guide provides a systematic comparison of commercial DNA extraction kits, empowering scientists to select the optimal methodology for overcoming these ubiquitous challenges.
Comparative Evaluation of Commercial DNA Extraction Kits
To objectively assess performance, we summarize findings from two independent studies that evaluated different DNA extraction kits for challenging sample types. The first study directly compared three kits for isolating DNA from subgingival biofilm samples collected on single paper points, a scenario characterized by extremely low sample volume [43]. The second study evaluated kits for detecting bacterial pathogens in whole blood, a complex medium rich in PCR inhibitors [56].
Table 1: Performance Comparison of DNA Extraction Kits from Subgingival Biofilm Samples [43]
| Kit Name | Manufacturer | Primary Lysis Method | Total dsDNA Yield (from healthy sites) | Bacterial DNA Yield (qPCR) | Cost per Prep (€) | Time per Prep (min) |
|---|---|---|---|---|---|---|
| DNeasy Blood & Tissue Kit | QIAGEN | Enzymatic & Chemical | Highest | Highest | 4.48 | ~150 |
| NucleoSpin Tissue Mini | MACHEREY‑NAGEL | Enzymatic & Chemical | Intermediate | Intermediate | 3.48 | ~90 |
| ZymoBIOMICS DNA Miniprep | ZYMO RESEARCH | Mechanical (Bead Beating) | Lowest | Lowest | 6.51 | ~120 |
Table 2: Performance Comparison of DNA Extraction Kits from Whole Blood Samples [56]
| Kit Name | Technology | Automation | Accuracy for E. coli | Accuracy for S. aureus | Specificity |
|---|---|---|---|---|---|
| GraBon System | Magnetic Bead (with bacterial isolation) | Full | 76.5% | 77.5% | 100% |
| K-SL DNA Extraction Kit | Magnetic Bead (with bacterial isolation) | Manual | 77.5% | 67.5% | 100% |
| QIAamp DNA Blood Mini Kit | Silica Column | Manual | 65.0% | 67.5% | 100% |
Key Insights from Comparative Data
- Lysis Mechanism is Crucial: The superior performance of the DNeasy Blood & Tissue Kit for subgingival biofilms underscores the efficacy of combined enzymatic and chemical lysis for this sample type [43]. Conversely, for tough Gram-positive bacteria in blood, the automated GraBon system's vigorous mechanical lysis via a rotating tip proved most effective for S. aureus [56].
- The Inhibitor Removal Advantage: Magnetic bead-based systems (K-SL and GraBon) that include a bacterial isolation step prior to lysis demonstrated significantly higher accuracy for E. coli detection in blood than the standard column-based method. This pre-lysis purification effectively separates bacteria from PCR inhibitors present in whole blood, leading to cleaner extracts and more reliable downstream detection [56].
- Sample Volume and DNA Concentration: The GraBon system's ability to process a larger initial sample volume (500 µL vs. 200 µL) and elute DNA in a relatively small volume (100 µL) provides a concentration effect that enhances detection sensitivity for low-abundance targets, a critical factor in sepsis diagnosis [56].
Detailed Experimental Protocols for Performance Evaluation
To ensure the reproducibility of the comparative data presented, this section outlines the key methodologies employed in the cited studies.
This protocol is designed for minimal sample input, simulating conditions where sample material is precious or limited.
- Sample Collection and Preparation: Subgingival biofilm samples are collected by inserting a single sterile paper point (e.g., VDW Dental, 29 mm, size 50) into the periodontal pocket for 15 seconds. Supragingival surfaces must be dried and isolated with cotton rolls to avoid contamination. The paper point is then transferred to a sterile 1.5 mL microcentrifuge tube and immediately frozen in liquid nitrogen, with long-term storage at -80°C.
- Cell Lysis and DNA Extraction (DNeasy Blood & Tissue Kit):
- Sample Wash: Employ a "pipe-in-pipe" method to wash sample material from the paper point. Add 1 mL of nuclease-free water and 12 glass beads (1.7–2.1 mm) to the tube. Shake at 14,000 rpm for 5 minutes.
- Pellet Bacteria: Pierce the bottom of the tube, place it into a 5 mL collection tube, and centrifuge at 4,000 × g for 1 minute. Transfer the flow-through to a new 1.5 mL tube and pellet the microbial cells by centrifuging at 10,000 × g for 15 minutes.
- Enzymatic Lysis: Resuspend the pellet in 180 µL of enzymatic lysis buffer. Follow the kit's standard protocol for "Purification of Total DNA from Animal Tissues," which includes an incubation step with Proteinase K.
- DNA Binding and Elution: Bind the DNA to the DNeasy Mini spin column, wash with the provided buffers, and elute the purified DNA in 100 µL of Buffer AE.
- DNA Quantification and Quality Control:
- Total Double-Stranded DNA (dsDNA): Quantify using a fluorometric method like the Qubit dsDNA HS Assay, which is highly specific for dsDNA.
- Bacterial DNA: Quantify via qPCR using universal primers targeting the bacterial 16S rRNA gene.
- Human DNA (Contamination): Quantify via qPCR using primers specific for the human GAPDH gene.
This protocol highlights a method optimized for removing PCR inhibitors from complex blood samples.
- Sample Preparation: Use 200 µL of whole blood, either fresh or from residual complete blood count (CBC) samples.
- DNA Extraction (K-SL DNA Extraction Kit - Manual Magnetic Bead Method):
- Bacterial Isolation: The kit uses magnetic beads to specifically isolate and concentrate intact bacterial cells from the whole blood sample. This crucial first step separates bacteria from hemoglobin and other PCR inhibitors.
- Cell Lysis: Lyse the isolated bacteria. The K-SL kit uses a gentle tube-mixing lysis method.
- DNA Binding and Elution: Bind the released DNA to magnetic beads. Wash the beads to remove residual contaminants, and elute the pure DNA in 100 µL of elution buffer.
- DNA Extraction (GraBon - Automated Magnetic Bead Method):
- The GraBon system automates the entire process using the same reagents as the K-SL kit.
- Its key differentiator is a more aggressive motor-driven rotating plastic tip for vortexing during the lysis step, which is particularly effective for disrupting the tough cell walls of Gram-positive bacteria like S. aureus.
- The system processes 500 µL of sample and elutes the DNA in 100 µL, providing a 5-fold concentration effect.
- Downstream Analysis: The extracted DNA is analyzed by real-time PCR using species-specific primers for pathogens like Escherichia coli and Staphylococcus aureus to determine detection accuracy.
Workflow Diagram: Kit Selection for Complex Samples
The following diagram illustrates the decision-making process for selecting an appropriate DNA extraction method based on sample type and research goals.
The Scientist's Toolkit: Essential Research Reagent Solutions
Successful DNA extraction from complex samples relies on a suite of specialized reagents and instruments. The table below details key solutions referenced in the comparative studies.
Table 3: Key Research Reagent Solutions for DNA Extraction from Complex Samples
| Item Name | Function/Application | Key Feature/Benefit |
|---|---|---|
| DNeasy Blood & Tissue Kit (QIAGEN) [57] | DNA purification from blood, tissues, Gram-positive & negative bacteria. | Reliable silica-membrane technology; optimized protocols for diverse samples; phenol/chloroform-free. |
| DNeasy 96 PowerSoil Pro Kit (QIAGEN) [58] | High-throughput microbial DNA isolation from soil, stool, sediment. | PowerBead Pro Plates for homogenization; Inhibitor Removal Technology (IRT) for humic acids, heme, etc. |
| NucleoSpin Tissue Mini Kit (MACHEREY‑NAGEL) [43] [59] | DNA purification from animal tissues, including specialized protocols for dental swabs. | Cost-effective; includes pre-lysis protocol for dental swab/paper point samples. |
| ZymoBIOMICS DNA Miniprep Kit (ZYMO RESEARCH) [43] | DNA isolation from microbial communities in various samples. | Incorporates mechanical bead beating for efficient lysis of tough cells. |
| K-SL DNA Extraction Kit (KingoBio) [56] | Bacterial DNA extraction from whole blood. | Magnetic bead-based bacterial isolation step to remove PCR inhibitors prior to lysis. |
| BashingBeads (in ZymoBIOMICS Kit) [43] | Mechanical cell disruption via bead beating. | Ultra-high density beads for efficient lysis of microbial cell walls. |
| Proteinase K | Enzymatic digestion of proteins and nucleases. | Critical for efficient sample lysis and inactivation of DNases that degrade target DNA. |
| Inhibitor Removal Technology (IRT) | Chemical removal of common PCR inhibitors. | Specialized buffers to remove humic substances (soil) and heme/bilirubin (blood/stool). |
| Levofloxacin sodium | Levofloxacin sodium, CAS:872606-49-0, MF:C18H19FN3NaO4, MW:383.3 g/mol | Chemical Reagent |
| PIM-447 dihydrochloride | PIM-447 dihydrochloride, MF:C24H25Cl2F3N4O, MW:513.4 g/mol | Chemical Reagent |
Addressing Suboptimal Transformation Efficiency and Growth Issues
Working with unidentified or difficult-to-culture bacteria presents significant challenges in molecular microbiology. Two of the most frequent obstacles researchers encounter are suboptimal transformation efficiency and poor bacterial growth, which can stall critical research projects and delay discoveries. Transformation efficiency—the ability to introduce foreign DNA into a host bacterium—is fundamental to genetic manipulation, protein expression, and synthetic biology applications. Similarly, successful cultivation relies on providing appropriate nutritional and environmental conditions that mirror a bacterium's natural habitat. Overcoming these limitations requires a systematic approach to selecting and optimizing commercial research kits, which vary considerably in their mechanisms, performance characteristics, and suitability for specific bacterial species and research goals. This guide provides an objective, data-driven comparison of available solutions to help researchers troubleshoot these persistent issues, framed within the broader context of optimizing commercial kits for unidentified bacteria research.
Comparative Analysis of Commercial Kits and Reagents
Whole-Genome Amplification Kits for Low-Input Samples
When DNA yield is insufficient for downstream sequencing applications, Whole-Genome Amplification (WGA) kits provide a solution, but their performance characteristics vary significantly. A 2025 systematic evaluation of four commercial WGA platforms using 100-pg and 1-ng DNA inputs revealed distinct performance profiles suited to different analytical endpoints [60].
Table 1: Performance Comparison of Whole-Genome Amplification Kits
| Platform (Manufacturer) | Amplification Technology | Key Strength | Primary Limitation | Optimal Application |
|---|---|---|---|---|
| REPLI-g (Qiagen) | Multiple Displacement Amplification | Highest DNA yield | Significant amplification bias and allelic dropout under ultra-low-input conditions | Applications requiring maximum DNA quantity but less concerned with bias |
| PicoPLEX (Takara Bio) | Modified MALBAC | Most accurate quantification for chimerism and CNV | Lower performance in allelic balance preservation | Quantitative applications: chimerism analysis, CNV detection |
| SurePlex (Illumina) | Modified MALBAC | Intermediate performance across all metrics | Not superior in any single category | General-purpose use when balanced performance is acceptable |
| ResolveDNA (BioSkryb Genomics) | Primary Template-Directed Amplification (PTA) | Lowest allelic dropout rates; best preservation of allelic balance | Less accurate for copy number variation | Applications where allelic fidelity is essential: SNP detection, variant analysis |
The study found that ResolveDNA showed the lowest allelic dropout (ADO) rates across input levels, whereas PicoPLEX offered the most accurate quantification for chimerism and copy number variation (CNV) [60]. REPLI-g had the highest DNA yield but exhibited marked amplification bias and ADO under ultra-low-input conditions. This comparative data indicates that platform selection must be tailored to specific analytical requirements rather than seeking a universal solution.
DNA Extraction Kit Efficiency for Microbial Biomass
Efficient DNA extraction is particularly challenging with small sample volumes typical in periodontal or environmental microbiome research. A 2025 pilot study compared three commercial DNA extraction kits for analyzing subgingival biofilm samples collected on single paper points (<10 μL volume) [43]. The results demonstrated significant differences in extraction efficiency that could substantially impact downstream analyses.
Table 2: DNA Extraction Kit Performance for Low-Biomass Samples
| Kit (Manufacturer) | Cell Lysis Method | Total dsDNA Yield (Healthy Sites) | Bacterial DNA Yield (16S qPCR) | Cost per Extraction (€) | Processing Time (min) |
|---|---|---|---|---|---|
| DNeasy Blood & Tissue (QIAGEN) | Enzymatic & Chemical | Significantly higher than both other kits | Significantly higher than both other kits in periodontitis sites | 4.48 | ~150 |
| NucleoSpin Tissue Mini (MACHEREY-NAGEL) | Enzymatic & Chemical | Intermediate | Intermediate | 3.48 | ~90 |
| ZymoBIOMICS DNA Miniprep (ZYMO RESEARCH) | Mechanical Bead Beating | Lowest | Lowest | 6.51 | ~120 |
Among the tested kits, the DNeasy Blood and Tissue Kit demonstrated the highest efficiency, yielding significantly more total dsDNA in samples from healthy sites compared to both other kits and in samples from periodontitis-affected sites compared to one kit [43]. Bacterial DNA yields were also significantly higher with the DNeasy Kit compared to one of the other kits in both health conditions. These findings suggest that for low-biomass samples, enzymatic and chemical lysis (as used in the DNeasy kit) may be more efficient than mechanical bead beating for bacterial DNA recovery.
Competent Cell Transformation Efficiencies
Cloned competent cells represent another critical factor in transformation efficiency, with significant variations in performance between products. The global cloned competent cells market offers formulations with transformation efficiencies ranging from 10â· to 10â¹ transformants per microgram of DNA, with some advanced formulations pushing toward 1 billion CFUs/ml [61].
The market segmentation reveals distinct preferences in competent cell types and applications. While the 100×100μl and 50×100μl segments dominate due to their versatility and widespread use in routine cloning, specialized strains are increasingly available for challenging applications like toxic/unstable DNA cloning and phage display library construction [61]. For subcloning and routine cloning applications, standard competent cells with efficiencies of 10â·-10⸠transformants/μg are generally sufficient. However, for high-throughput cloning or difficult constructs, premium cells with efficiencies exceeding 10â¹ transformants/μg may be necessary despite their higher cost.
Experimental Protocols for Kit Validation
Protocol for Evaluating DNA Extraction Kits from Low-Biomass Samples
Based on the methodology from the comparative pilot study of DNA extraction kits [43], the following protocol can be used to validate kit performance for low-biomass bacterial samples:
Sample Collection: Collect bacterial biomass using appropriate methods (e.g., sterile paper points for biofilm, filtration for liquid samples, swabs for surfaces). For comparative studies, divide samples equally across kits being tested.
Cell Lysis:
- Enzymatic/Chemical Lysis (DNeasy Kit): Resuspend samples in 180 μL enzymatic lysis buffer (Tris-Cl, sodium EDTA, Triton X-100, lysozyme) and incubate with proteinase K according to manufacturer protocols.
- Mechanical Lysis (ZymoBIOMICS Kit): Use bead beating with ultra-high density BashingBeads and lysis solution containing EDTA. Vortex at maximum speed for 1 minute, followed by a 5-minute pause, repeating this cycle five times.
DNA Purification: Follow manufacturer instructions for DNA binding to columns, washing steps, and elution. Use consistent elution volumes (e.g., 100 μL) across kits for accurate comparison.
DNA Quantification:
- Measure total DNA yield by UV absorption at 260 nm using a spectrophotometer.
- Quantify double-stranded DNA (dsDNA) yield using fluorometric measurements (e.g., Qubit fluorometer).
- Perform quantitative PCR with universal 16S rRNA primers to specifically assess bacterial DNA recovery.
Quality Assessment: Evaluate DNA purity via A260/A280 and A260/A230 ratios, and assess integrity through gel electrophoresis or automated electrophoresis systems.
Workflow for Assessing Whole-Genome Amplification Performance
The performance evaluation of WGA platforms followed a systematic approach to assess multiple performance metrics under standardized conditions [60]:
Diagram 1: WGA Performance Evaluation Workflow
This comprehensive assessment revealed that each platform demonstrated specific strengths and limitations depending on analytical endpoints [60]. Modified MALBAC-based platforms (PicoPLEX, SurePlex) performed optimally when quantitative accuracy was critical, such as in chimerism or CNV analysis, whereas PTA-based WGA (ResolveDNA) was preferred when allelic fidelity was essential.
Innovative Approaches for Growth Optimization
Machine Learning for Culture Media Prediction
For growth issues with unidentified bacteria, traditional culture medium selection relying on empirical knowledge or trial and error often proves inefficient. The MediaMatch tool represents an innovative approach to this challenge, using machine learning to predict appropriate culture media based on 16S rRNA sequences [62].
The system employs 45 binary classification models built using the XGBoost algorithm with data on culture media from the MediaDive database combined with microbial 16S rRNA sequences [62]. The models use k-mer frequencies from 16S rRNA sequences as features, with labels indicating whether bacteria can grow in specific media. This approach has demonstrated strong predictive performance, with accuracies ranging from 76% to 99.3%, and F1 scores for most models exceeding 90% [62].
Diagram 2: MediaMatch Predictive Workflow
Emerging Technologies in Bacterial Research
The field of bacterial research is witnessing several technological advances that address transformation and growth challenges:
CRISPR and refactoring-based strategies can activate silent biosynthetic genes, potentially revealing new growth requirements or metabolic capabilities in unculturable bacteria [63].
Cell-free biosynthesis bypasses biosynthetic limitations of natural products, allowing study of bacterial metabolic pathways without the need for cultivation [63].
Big data and artificial intelligence can generate novel structures and predict biological relevance, including optimal growth conditions for difficult-to-culture species [63].
Digital PCR and microfluidic-based kits enable miniaturization, reducing reagent costs and improving portability for field applications [64].
The Scientist's Toolkit: Essential Research Reagent Solutions
Table 3: Key Research Reagent Solutions for Bacterial Transformation and Growth Studies
| Reagent Category | Specific Examples | Function & Application | Performance Considerations |
|---|---|---|---|
| High-Efficiency Competent Cells | Cloned competent cells (20×100μl, 50×100μl, 100×100μl formats) [61] | DNA cloning and transformation; available as chemically or electrocompetent cells | Transformation efficiencies range from 10ⷠto 10⹠transformants/μg DNA; specialized strains available for toxic/unstable DNA |
| DNA Extraction Kits | DNeasy Blood & Tissue (QIAGEN), ZymoBIOMICS DNA Miniprep (Zymo Research), NucleoSpin Tissue Mini (MACHEREY-NAGEL) [43] | Isolation of high-quality genomic DNA from bacterial cultures or environmental samples | Lysis method (enzymatic, chemical, mechanical) significantly impacts yield from low-biomass samples |
| Whole-Genome Amplification Kits | REPLI-g (Qiagen), PicoPLEX (Takara Bio), ResolveDNA (BioSkryb Genomics) [60] | Genome amplification from low-input DNA for sequencing applications | Performance varies by application: allelic fidelity vs. quantitative accuracy for CNV/chimerism |
| Culture Media Prediction Tools | MediaMatch algorithm [62] | Predicts optimal culture media for bacterial growth based on 16S rRNA sequences | Achieves 76-99.3% accuracy in predicting growth on specific media types |
| Specialized Cloning Kits | Various vendor-specific kits [65] | Simplify molecular cloning workflows (TA cloning, Gibson assembly, restriction enzyme-based) | Efficiency varies by cloning method; modern kits emphasize speed and seamless cloning |
Addressing suboptimal transformation efficiency and growth issues requires careful selection and validation of commercial kits based on specific research needs rather than assuming universal performance across products. The comparative data presented in this guide demonstrates that kit performance varies significantly across different applications—what excels for whole-genome amplification may underperform for DNA extraction from low-biomass samples.
Looking toward 2026, the DNA amplification kit sector is expected to continue evolving with increased vendor consolidation and pricing strategies shifting toward value-based models emphasizing performance and support [66]. Technological advancements will likely focus on automation compatibility, higher throughput capabilities, and integration with digital platforms and AI-driven data analysis [64] [66]. For bacterial research specifically, the integration of machine learning approaches for culture media prediction represents a promising direction to overcome one of the most persistent challenges in microbiology—culturing the unculturable.
By applying the systematic comparison frameworks and validation protocols outlined in this guide, researchers can make evidence-based decisions in selecting and optimizing commercial kits, ultimately overcoming the common challenges of suboptimal transformation efficiency and bacterial growth issues that impede progress in microbiological research and drug development.
Resolving Weak, Indeterminate, or Incorrect Identification Results
Accurate microbial identification is a cornerstone of clinical diagnostics and microbiological research. However, scientists often encounter weak, indeterminate, or incorrect results, which can delay critical decisions in patient treatment and drug development. These challenges stem from various factors, including the limitations of individual technological platforms, sample preparation complexities, and the inherent difficulties of analyzing polymicrobial or low-biomass samples. This guide objectively compares the performance of contemporary commercial identification kits and methodologies. By evaluating supporting experimental data within a structured framework, it aims to provide researchers with the evidence needed to select appropriate tools and implement strategies that enhance the reliability of bacterial identification in research settings.
Comparative Performance Analysis of Identification Methods
The following table summarizes key performance metrics from recent studies for a range of identification technologies, highlighting their respective strengths and limitations in resolving ambiguous results.
| Method / Kit Name | Technology Principle | Reported Species-Level Accuracy | Time to Result | Key Strengths | Major Limitations / Sources of Indeterminate Results |
|---|---|---|---|---|---|
| SepsiTyper Kit [67] | Direct MS identification from broth (MALDI-TOF MS) | High in monomicrobial samples | ~1 day faster than conventional methods [67] | Reduced turnaround time; high species-level accuracy for monomicrobial cultures [67] | Lower accuracy in polymicrobial samples; requires centrifugation and washing steps [67] |
| FilmArray BCID2 Panel [67] | Multiplex PCR (Molecular) | Outperformed in polymicrobial cases [67] | ~1 day faster than conventional methods [67] | Excellent for polymicrobial detection; detects resistance genes; minimal hands-on time [67] | Limited to pre-defined targets on the panel; cannot discover novel species [67] |
| 16S rRNA PCR & Sequencing [68] | DNA Sequencing | Foundational for identification of non-culturable organisms [68] | Several hours to days (includes PCR and sequencing) [68] | Broad-range identification; gold standard for phylogenetic studies; useful for difficult-to-identify isolates [68] | Requires validation; may not distinguish between highly similar species; requires bioinformatics expertise [68] |
| REIMS Metabolomic Profiling [69] | Mass Spectrometry (Metabolites/Lipids) | Identified 359 taxon-specific markers (TSMs) across 233 species [69] | Near-real-time (minutes) [69] | Untargeted, universal detection; can identify bacteria directly in complex tissues [69] | High-cost instrumentation; emerging technology; validation needed for clinical samples [69] |
| RapID Systems [70] | Biochemical Enzyme Reactions | Accurately identify >400 organisms [70] | < 4 hours [70] | Rapid; low-tech; extensive database [70] | Relies on pure culture and bacterial metabolism; can be subjective [70] |
Experimental Protocols for Key Comparisons
Protocol: Benchmarking Rapid ID/AST from Blood Cultures
This protocol, adapted from a 2025 study, is designed to compare the performance of rapid diagnostic methods against conventional culture in a simulated laboratory workflow [67].
- Sample Preparation: Collect positive blood culture broths (e.g., Bact/ALERT FA/FN Plus) flagged by a microbial detection system. Perform Gram staining to exclude yeast and Gram-positive bacilli. Include both monomicrobial and polymicrobial samples [67].
- Methodology:
- Rapid Identification (performed in parallel):
- Conventional Method (Reference): Subculture broths onto solid media. Identify isolated colonies using standard MALDI-TOF MS after overnight incubation [67].
- Data Analysis: Calculate species-level and genus-level identification accuracy for each rapid method against the conventional method reference. Analyze turnaround time from time of blood culture positivity to result reporting [67].
Protocol: Validating ID with 16S rRNA and Biochemical Tests
This protocol employs a reverse approach, using 16S rRNA sequencing for initial identification followed by customized biochemical validation, which is ideal for resolving discrepancies [68].
- Sample Preparation: Isolate bacteria from a source (e.g., root nodules, clinical sample). Purify cultures on appropriate agar plates [68].
- Methodology:
- Molecular Identification: Perform colony PCR using universal 16S rRNA primers (e.g., 530F and 1492R). Clean up PCR products and sequence them. Analyze sequences against a database (e.g., NCBI BLAST) for identification [68].
- Hypothesis-Driven Biochemical Verification: Based on the 16S rRNA identification result, design a tailored panel of biochemical tests to confirm the identity of the isolate. For example, if identified as a Rhizobium, tests for growth on specific carbon sources or nitrogen fixation phenotypes can be used [68].
- Data Analysis: Confirm that the results of the bespoke biochemical tests are consistent with the expected phenotype of the species identified by sequencing. This confirms the identity and resolves indeterminate or weak biochemical results [68].
Visualization of Workflows and Resolution Pathways
Diagram 1: Comparative Experimental Workflow
Diagram 2: Pathway for Resolving Indeterminate Results
The Scientist's Toolkit: Essential Research Reagents & Materials
The following table details key reagents and materials critical for executing the experiments and comparisons described in this guide.
| Item Name | Function / Application | Example Use Case |
|---|---|---|
| SepsiTyper Kit (Bruker Daltonics) [67] | Sample preparation kit for direct identification from positive blood cultures using MALDI-TOF MS. | Enables rapid ID from blood culture broth, bypassing subculture. |
| FilmArray BCID2 Panel (bioMérieux) [67] | Multiplex PCR panel for detection of pathogens and antimicrobial resistance genes directly from blood culture. | Rapid, targeted detection in polymicrobial infections. |
| Universal 16S rRNA Primers [68] | PCR amplification of the 16S rRNA gene for sequencing and phylogenetic analysis. | Broad-range identification of bacterial isolates. |
| DNeasy UltraClean Microbial Kit (Qiagen) [46] | Extraction of high-quality genomic DNA from microbial cultures for downstream sequencing. | Preparing DNA for 16S rRNA sequencing or WGS. |
| RapID Systems (Thermo Fisher) [70] | Manual biochemical test panels for enzymatic identification of bacteria. | Low-cost, rapid verification of isolate identity. |
| MagAttract HMW DNA Kit (Qiagen) [46] | Extraction of high-molecular-weight DNA suitable for long-read sequencing. | Preparing DNA for advanced genomic studies (e.g., AMR detection). |
Resolving weak, indeterminate, or incorrect identification results requires a systematic and often multi-platform approach. As the comparative data shows, no single method is infallible; mass spectrometry excels in monomicrobial samples, molecular panels offer speed and specificity for targeted pathogens, and 16S rRNA sequencing provides a broad-based identification capability. The path to a definitive result often lies in leveraging these technologies as complementary tools. Implementing the outlined workflows and resolution pathways, which emphasize the use of orthogonal methods for verification, will significantly enhance the accuracy and reliability of bacterial identification. This rigorous, evidence-based framework is essential for advancing research and ensuring the integrity of findings in microbiology and drug development.
This guide objectively compares the performance of various commercial kits and methods used for identifying unidentified bacteria in research, focusing on the critical roles of control strains and strict protocol adherence.
The accurate identification of bacterial isolates is a cornerstone of microbiological research, clinical diagnostics, and drug development. This process often relies on a suite of commercial kits for biochemical testing and genetic analysis. However, the performance of these kits must be rigorously evaluated using well-characterized control strains, and the results are highly dependent on strict adherence to standardized protocols. This guide synthesizes findings from comparative studies to provide a clear framework for selecting and using these essential tools, ensuring that data generated in one lab is reproducible and reliable in another.
The Scientist's Toolkit: Essential Research Reagents and Materials
The following table details key reagents and their functions in the process of bacterial identification, providing a foundation for understanding the experimental comparisons that follow [71] [72].
| Item | Function in Bacterial Identification |
|---|---|
| API Coryne System | A commercial biochemical identification kit that uses micro-metabolite tests to generate a profile for coryneform and other bacteria [71]. |
| 16S rRNA Gene Primers | Oligonucleotides designed to amplify specific regions of the 16S rRNA gene, which serves as a molecular clock for phylogenetic analysis and species identification [71]. |
| rpoB Gene Primers | Oligonucleotides for amplifying the RNA polymerase beta-subunit gene, which can provide higher resolution than 16S rRNA for distinguishing closely related species [71]. |
| Silica-Matrix DNA Kits | Kits that purify genomic and plasmid DNA via binding to a silica membrane, especially effective for maintaining the yield of small plasmids [72]. |
| Anion Exchange Resin Kits | An alternative DNA purification technology that uses a charge-based binding matrix [72]. |
| Precipitation-Based DNA Kits | Kits that use salt and alcohol to precipitate nucleic acids; may deplete smaller plasmids (<5 kb) [72]. |
| American Type Culture Collection (ATCC) Strains | A primary global source for well-characterized, authenticated control strains used for quality assurance and method validation [73]. |
Comparative Analysis of Bacterial Identification Methods
A pivotal study directly compared the effectiveness of three commercial biochemical identification kits and three nucleic acid amplification tests for identifying a diverse set of 50 coryneform bacteria isolates, including 12 well-characterized control strains [71]. The performance data is summarized below.
Table 1: Performance Comparison of Identification Methods for Coryneform Bacteria [71]
| Identification Method | Type | Principle | Correct Species ID of Control Strains | Key Limitations |
|---|---|---|---|---|
| API Coryne System | Phenotypic/Biochemical | Micro-metabolite profiling | 75.0% (9/12 strains) | Limited by database scope; cannot differentiate some genospecies. |
| 16S rRNA Gene Sequencing | Genotypic/Sequence Analysis | Amplification and sequencing of conserved gene | 75.0% (9/12 strains) | Database pollution from uncharacterized strains; limited species-level resolution. |
| rpoB Gene Sequencing | Genotypic/Sequence Analysis | Amplification and sequencing of housekeeping gene | Not specified (lower than others) | Severely limited by the small number of reference sequences in databases. |
| Other Commercial Kits (2) | Phenotypic/Biochemical | Not specified | 33.3% - 58.3% | Performance varies significantly by kit and database. |
This comparative study revealed several critical insights. First, the API Coryne system and 16S rRNA gene sequencing were the most sensitive techniques, correctly identifying 75% of control strains to the species level [71]. All strains that generated a high-confidence result from these methods were correctly identified. Second, a major limitation for both phenotypic and genotypic methods is database comprehensiveness. Biochemical kits failed to identify species not included in their databases, while genetic sequencing was complicated by the presence of sequence data from uncultivated and uncharacterized organisms in public databases [71]. Finally, the correlation between identifications produced by different classification systems was poor, especially for clinical isolates, underscoring the need for a polyphasic approach to identification [71].
Comparison of DNA Extraction Kits for Genomic Analysis
The choice of DNA extraction method can profoundly impact downstream genetic analysis, such as next-generation sequencing. A study of six commercial kits for extracting DNA from Klebsiella pneumoniae compared methods based on silica-matrix binding, anion exchange resin, and differential precipitation (salting out) [72].
Table 2: Impact of DNA Extraction Kit Chemistry on Sequencing Results [72]
| Extraction Chemistry | Principle | Effect on Sequencing Coverage | Key Finding Regarding Plasmids |
|---|---|---|---|
| Matrix Binding (Silica or Anion Exchange) | DNA binds to a matrix, impurities are washed away, DNA is eluted. | Minimal effect on sequencing quality and coverage across replicons. | Maintained consistent representation; no significant depletion. |
| Differential Precipitation (Salting Out) | Proteins are precipitated, DNA remains in solution and is salted out. | Minimal effect on overall sequencing quality. | Apparent depletion of small plasmids (<5 kb), leading to higher copy-number estimates via sequencing than qPCR. |
The study concluded that while the choice of kit had little effect on overall sequencing quality and coverage across large, drastically different replicons (like the chromosome versus large plasmids), there was a notable exception: precipitation-based methods appeared to deplete small plasmids [72]. This highlights that the selection of a DNA extraction kit is not one-size-fits-all; the research objective must guide the choice. If the goal is comprehensive plasmid sequencing, a silica-matrix or anion exchange-based kit is superior.
Experimental Protocols for Method Validation
Protocol: Validating Identification Methods Using Control Strains
This protocol outlines the steps for assessing the performance of any bacterial identification method, based on the comparative study methodology [71].
- Strain Selection: Select a panel of well-characterized control strains from a reputable culture collection (e.g., ATCC, DSMZ). The panel should include species relevant to your research and, if possible, strains known to be difficult to identify.
- Parallel Testing: Subject all control strains to the identification methods being compared (e.g., API Coryne, 16S rRNA sequencing, rpoB sequencing) simultaneously and under standardized conditions.
- Data Analysis: For each method and strain, record the identification result and the confidence level provided by the system (e.g., "excellent identification," "low discrimination").
- Calculation of Accuracy: Calculate the percentage of control strains correctly identified to the species level by each method. Strains producing a low-confidence result should be noted separately.
Protocol: Evaluating DNA Extraction Kits for Sequencing
This protocol describes how to compare the efficiency of DNA extraction kits, particularly for sequencing applications involving multiple replicons [72].
- Standardized Culture: Grow a control bacterial strain (e.g., Klebsiella pneumoniae known to harbor chromosomes and plasmids of various sizes) in a standardized culture.
- Parallel Extraction: Divide the bacterial culture into aliquots and extract genomic DNA using each kit under evaluation, strictly following the manufacturers' instructions.
- Quality and Quantity Assessment: Measure the concentration and purity (A260/A280) of the extracted DNA from all kits.
- Downstream Analysis: Subject the extracted DNA from all kits to the same downstream analysis, such as MiSeq sequencing.
- Comparative Bioinformatics: Map the sequencing reads to a reference genome for the control strain. Analyze and compare the coverage depth and uniformity across all replicons (chromosome, large plasmids, small plasmids) for the DNA extracted with each different kit.
Workflow and Signaling Pathways
The following diagram illustrates the logical workflow for selecting and applying quality control measures in bacterial identification, integrating the roles of control strains and the comparative data on different methods.
Diagram 1: A workflow for bacterial identification integrating method selection and control strains.
Ensuring Protocol Adherence in Research
Measuring and ensuring provider adherence to research protocols is a critical but methodologically challenging aspect of quality control. The table below summarizes the primary methods for measuring adherence, their advantages, and their disadvantages, which researchers should consider when designing and conducting studies [74].
Table 3: Methods for Measuring Protocol Adherence in Research [74]
| Method | Key Advantage | Key Disadvantage | Underlying Assumption |
|---|---|---|---|
| Direct Observation | Considered the gold standard; most accurate data. | Highly time-consuming and resource-intensive; prone to observer and Hawthorne effect (behavior change when observed). | Observers are well-trained and opportunities for adherence are clearly predefined. |
| Self-Reporting | Inexpensive and easy to administer to a large sample. | Subjective and prone to significant overestimation due to social desirability bias. | The measuring instrument (questionnaire) is reliable and validated, and participants feel safe to report truthfully. |
| Electronic Monitoring | Provides objective data and allows tracking over time. | High initial and maintenance costs; can be prone to device failure. | A washout period for the "novelty effect" is observed, and all ethical requirements for activity tracking are met. |
| Documentation Review | Easy, inexpensive, and can be done independently. | Provides only indirect data on adherence; cannot verify the quality of the original action. | The documents are accurate and complete records of the actions taken. |
To reduce the risk of bias when measuring adherence, especially in multi-center trials, researchers must ensure that all necessary resources for adherence are available, check that the protocols align with local guidelines, and confirm that the guidelines are not the subject of a recent quality improvement project that could temporarily inflate adherence rates [74].
Optimizing for Fastidious, Slow-Growing, or Mixed Cultures
The accurate and timely identification of pathogens is a cornerstone of effective clinical microbiology. This process is particularly challenging when dealing with fastidious, slow-growing, or mixed bacterial cultures, which can lead to diagnostic delays and compromise patient care. Conventional culture-based methods, while considered the gold standard, often require 48–72 hours for results and may fail to detect pathogens with stringent growth requirements or in patients with prior antibiotic exposure [75]. The evolution of molecular diagnostics offers promising alternatives. This guide evaluates the performance of a rapid multiplex PCR (mPCR) assay against traditional culture methods, providing researchers and drug development professionals with critical data to inform their diagnostic toolkit.
Comparative Analysis: mPCR vs. Conventional Culture
The following analysis is based on a 2025 multicenter study evaluating a Respiratory Pathogens Multiplex Nucleic Acid Diagnostic Kit against bacterial culture using 728 bronchoalveolar lavage fluid (BALF) specimens [75].
Table 1: Overall Diagnostic Performance of mPCR vs. Culture [75]
| Metric | Value | Notes |
|---|---|---|
| Total Specimens | 728 | 51 specimens excluded due to invalid results. |
| Culture Positivity Rate | 14.15% (103/728) | Reference standard for bacterial detection. |
| mPCR Positivity Rate | 86.3% (628/728) | Detected ≥1 pathogen; includes viral targets. |
| Positive Percentage Agreement (PPA) | 84.6% (95% CI: 76.6-92.6%) | Versus culture for bacterial targets. |
| Negative Percentage Agreement (NPA) | 96.5% (95% CI: 96.0-97.1%) | Versus culture for bacterial targets. |
| Semi-quantitative Concordance | 79.3% (283/357) | In culture-positive specimens. |
| Samples with Multiple Pathogens | 19.8% (144/728) | mPCR detected 2-4 pathogens; culture detected two pathogens in only 0.5% of samples. |
Table 2: Pathogen Detection Concordance with Ct-Value Threshold (Ct <30) [75]
| Pathogen | Conventional Culture | mPCR (Ct <30) | Key Finding |
|---|---|---|---|
| Pseudomonas aeruginosa | 5.63% | 6.6% | Improved concordance when applying Ct threshold. |
| Klebsiella pneumoniae | 5.36% | 5.63% | Improved concordance when applying Ct threshold. |
| Streptococcus pneumoniae | 0.96% | 7.14% | Largest discrepancy; mPCR more sensitive. |
| Haemophilus influenzae | 0.55% | 4.12% | mPCR detected at a significantly higher rate. |
| Staphylococcus aureus | 0.82% | 2.34% | mPCR detected at a significantly higher rate. |
| Legionella pneumophila | Not specified | Not specified | No significant difference in detection (P ≥0.05). |
Key Insight from Data: The mPCR kit demonstrated a significantly higher overall detection rate. However, a strong correlation was observed between low Cycle Threshold (Ct) values (≤30) and culture positivity, suggesting Ct values can help differentiate active infection from colonization or non-viable DNA [75].
Experimental Protocols
- Specimen Inoculation: BALF specimens were inoculated onto selective and differential media using calibrated loops to achieve semi-quantitative results.
- Growth Media:
- Blood Agar: A nutrient-rich medium for broad-spectrum bacterial cultivation, optimal for Gram-positive cocci like Staphylococcus aureus and Streptococcus pneumoniae.
- Chocolate Agar: Enriched with NAD and hemin to support fastidious organisms, specifically targeting Haemophilus influenzae.
- HE Agar (Hektoen Enteric Agar): A selective medium for isolating Gram-negative bacilli, critical for detecting Pseudomonas aeruginosa and Klebsiella pneumoniae.
- Incubation and Identification: Inoculated media were incubated at 35°C in a 5% CO₂ atmosphere for up to three days. Pure colonies were analyzed using MALDI-TOF MS for pathogen identification.
- Kit: Respiratory Pathogens Multiplex Nucleic Acid Diagnostic Kit.
- Platforms: Hongshi SLAN-96P or Life Technologies QuantStudio 5.
- Targets: Six bacterial (P. aeruginosa, K. pneumoniae, S. aureus, S. pneumoniae, H. influenzae, L. pneumophila) and six viral targets (Influenza A/B, RSV, Adenoviruses, Human rhinovirus, Mycoplasma pneumoniae).
- Process: A closed, pouch-based system that integrates nucleic acid extraction, amplification, and detection from approximately 1mL of raw sample.
- Time-to-Result: Approximately 75 minutes.
- Analysis: A positive result was defined as a Ct value less than 39. For improved specificity versus culture, a Ct value of less than 30 was applied.
Diagnostic Workflow and Data Interpretation
The diagram below illustrates the integrated diagnostic pathway and the logical relationship for interpreting mPCR results in the context of culture.
Diagram 1: Integrated diagnostic pathway for pathogen identification.
The Scientist's Toolkit: Essential Research Reagents & Materials
Table 3: Key Reagents and Materials for Pathogen Identification Research [75]
| Item | Function in Research |
|---|---|
| Bronchoalveolar Lavage Fluid (BALF) | A critical clinical specimen obtained via bronchoscopy, representing lower respiratory tract contents for analysis. |
| Selective Culture Media (Blood, Chocolate, HE Agar) | Support the growth of specific pathogen types while inhibiting others, enabling isolation and semi-quantitative analysis. |
| Multiplex PCR Kit (Pathogen-Specific) | Enables simultaneous amplification and detection of multiple pathogen-specific DNA/RNA targets from a single sample. |
| Automated PCR Analysis System | Instruments that automate the thermal cycling and fluorescence detection processes for precise and reproducible PCR results. |
| MALDI-TOF MS | Matrix-Assisted Laser Desorption/Ionization Time-of-Flight Mass Spectrometry for rapid, accurate microbial identification from cultured colonies. |
The rapid multiplex PCR assay presents a formidable complementary tool to conventional culture for identifying fastidious, slow-growing, or mixed cultures. Its primary advantages are speed (approximately 75 minutes) and high sensitivity, especially for pathogens like Streptococcus pneumoniae and Haemophilus influenzae. However, culture remains essential for antimicrobial susceptibility testing. The strategic application of a Ct-value threshold (Ct ≤30) can enhance the clinical relevance of mPCR results by correlating with viable, culture-positive organisms. For researchers and clinicians, an integrated protocol that leverages the speed of mPCR and the viability data of culture represents the most robust approach for advancing diagnostic accuracy in complex clinical and research scenarios.
Ensuring Accuracy: Validation Protocols and Performance Benchmarks
In the field of unidentified bacteria research, the selection and validation of commercial kits are critical for generating reliable, reproducible data. The process requires a rigorous framework that assesses both analytical performance—the technical capability of the method itself—and biological relevance—its effectiveness in detecting and identifying microbial agents within complex samples. This guide provides a structured approach for evaluating commercial kits, focusing on DNA extraction as a foundational step, and establishes a validation paradigm that integrates principles from bioanalytical chemistry and biomolecular research. By applying this framework, researchers can make informed comparisons between commercially available alternatives, ensuring that their chosen methodologies are fit-for-purpose in both exploratory research and applied drug development contexts.
Foundational Principles: Analytical versus Bioanalytical Validation
A critical first step in designing a validation framework is understanding the distinction between analytical and bioanalytical methods, as their validation procedures differ significantly.
Analytical Methods are used to determine quality parameters (identity, purity, content, potency) of a pharmaceutical product itself, such as a drug substance or finished drug product. They are typically performed under Good Manufacturing Practices (GMP) and are governed by the harmonized ICH Q2(R2) guideline. [76]
Bioanalytical Methods are used for the quantitative determination of drugs, their metabolites, or biomarkers in biological matrices such as blood, serum, plasma, urine, or tissue samples. [77] [76] They are primarily applied in pharmacological, bioavailability, bioequivalence, pharmacokinetic, and toxicology studies, often conducted under Good Laboratory Practices (GLP). [77] A key characteristic is that the analyte (e.g., a drug or, in this context, bacterial DNA) is measured within a complex biological milieu.
Research involving the identification of bacteria from biological samples (e.g., subgingival biofilm, tissue) falls into the bioanalytical category because the target is measured from within a biological matrix. [43] Consequently, the validation framework must address challenges like selectively isolating the microbial DNA from a background of human DNA and other contaminants.
The Validation Workflow: From Method Selection to Data Presentation
A rigorous validation follows a structured lifecycle from development through to performance verification. The workflow below outlines the key stages for establishing a method suitable for evaluating commercial kits in bacteria research.
Stages of the Validation Lifecycle
Method Development: This initial phase involves creating a reliable analytical method. Key activities include defining the method's purpose, conducting a literature review, selecting techniques, and optimizing parameters like sample preparation and operating conditions. [78] For DNA extraction from bacteria, this includes selecting the appropriate lysis method (enzymatic, mechanical, chemical) for the target cell wall type (Gram-positive vs. Gram-negative).
Method Qualification: This stage involves an initial evaluation and characterization of the method's performance as an analytical tool. [78] It assesses core parameters such as specificity, precision, accuracy, linearity, and the lower limits of detection and quantitation (LOD/LOQ) to establish that the method is fundamentally sound.
Method Validation: This is the formal process of demonstrating that the method is suitable for its intended purpose, providing documented evidence that it meets predefined acceptance criteria. [79] [78] This is a comprehensive assessment of validation parameters, often required for regulatory submissions. For bioanalytical methods, stability studies of the analyte in the biological matrix are particularly critical. [76]
Continued Method Performance Verification: After validation, the method's performance is regularly monitored during routine use through system suitability tests and quality control samples to ensure ongoing reliability and consistency. [78]
Core Validation Parameters for Assessment
The following parameters form the cornerstone of the validation framework, providing a standardized set of criteria for kit comparison. [79] [78]
Analytical Parameters
- Specificity/SELECTIVITY: The ability of the method to unambiguously distinguish and measure the analyte (bacterial DNA) in the presence of other components, such as human DNA, proteins, enzymes, or PCR inhibitors that may be co-extracted from the sample. [79]
- Accuracy: The closeness of agreement between the measured value (e.g., DNA concentration) and a reference value. This can be assessed by spiking a known quantity of bacteria into a sample and determining the recovery rate. [78]
- Precision: The degree of agreement among a series of measurements from multiple sampling of the same homogeneous sample. It is usually expressed as relative standard deviation (RSD) and can be measured at repeatability (within-day) and intermediate precision (between-day, between-analyst) levels. [79] [78]
- Linearity and Range: The linearity of an analytical procedure is its ability to obtain test results that are directly proportional to the concentration of the analyte. The range is the interval between the upper and lower concentrations for which linearity, accuracy, and precision have been demonstrated. [79]
- Limit of Detection (LOD) and Quantitation (LOQ): The LOD is the lowest amount of analyte that can be detected, but not necessarily quantified. The LOQ is the lowest amount that can be quantified with acceptable accuracy and precision. [79] [78] This is crucial for detecting low-biomass bacterial populations.
- Robustness: A measure of the method's capacity to remain unaffected by small, deliberate variations in method parameters (e.g., lysis time, temperature, elution volume), indicating its reliability during normal usage. [79]
Biological Parameters
- Efficiency in a Complex Matrix: The kit's performance when processing real-world biological samples (e.g., subgingival biofilm, sputum, tissue) rather than pure bacterial cultures. This evaluates its ability to handle inhibitors and complex substrates. [43]
- Bacterial DNA Yield: The total amount of microbial DNA recovered from a standardized sample, often quantified using fluorometric methods (e.g., Qubit dsDNA assay) which are more specific than UV absorbance. [43]
- Purity of Recovered DNA: The presence of contaminants (e.g., proteins, salts) that can inhibit downstream applications like PCR. This is commonly assessed by UV absorbance ratios (A260/A280 and A260/A230). [43]
- Stability: The integrity and usability of the extracted DNA after storage under various conditions (e.g., -80°C, freeze-thaw cycles). For bioanalytical methods, stability is a paramount parameter. [79] [76]
Experimental Data: A Pilot Comparison of DNA Extraction Kits
A recent pilot study compared three commercial DNA extraction kits for their efficiency in isolating microbial gDNA from single paper point samples of subgingival biofilm, a relevant scenario for low-biomass and complex bacterial samples. [43] The experimental workflow and results provide a model for a comparative kit evaluation.
Experimental Protocol
- Sample Collection: Subgingival biofilm samples were collected from participants using sterile paper points, inserted into the periodontal pocket for 15 seconds. [43]
- Storage: Samples were immediately frozen in liquid nitrogen and stored at -80°C until processing. [43]
- DNA Extraction: The following kits were used according to manufacturers' instructions, with minor protocol-specific adjustments: [43]
- NucleoSpin Tissue Mini Kit (MN): Based on enzymatic and chemical lysis.
- ZymoBIOMICS DNA Miniprep Kit (ZB): Based on mechanical lysis (bead beating) and chemical lysis.
- DNeasy Blood & Tissue Kit (QB): Based on enzymatic and chemical lysis, with a pre-wash step to separate sample material from the paper point.
- DNA Quantification: Total DNA yield was measured via UV absorbance (NanoDrop). Double-stranded DNA (dsDNA) yield was measured using a fluorometric assay (Qubit). Bacterial DNA yield was specifically quantified via qPCR with universal 16S rRNA primers. [43]
The following table summarizes the key performance data from the pilot study, providing a clear comparison of the kits' efficiencies. [43]
Table 1: Performance Comparison of DNA Extraction Kits from Subgingival Biofilm
| Kit Name | Manufacturer | Primary Lysis Method | Total dsDNA Yield (Health / Periodontitis) | Bacterial DNA Recovery (via qPCR) | Approx. Cost per Extraction (€) | Avg. Processing Time (min) |
|---|---|---|---|---|---|---|
| DNeasy Blood & Tissue | QIAGEN | Enzymatic & Chemical | Highest | Significantly Higher | 4.48 | ~150 |
| NucleoSpin Tissue Mini | MACHEREY-NAGEL | Enzymatic & Chemical | Intermediate | Intermediate | 3.48 | ~90 |
| ZymoBIOMICS DNA Miniprep | ZYMO RESEARCH | Mechanical & Chemical | Lower | Lower | 6.51 | ~120 |
Note: Data adapted from a pilot study with a limited sample size (n=6 participants). The DNeasy Kit demonstrated significantly higher efficiency in both healthy and periodontitis-affected sites compared to at least one other kit. [43]
The Scientist's Toolkit: Essential Research Reagents & Materials
A standardized set of materials and reagents is essential for executing a controlled validation study. The table below details key items used in the featured experimental protocol. [43]
Table 2: Essential Research Reagents and Materials for DNA Extraction Validation
| Item | Function in the Experiment |
|---|---|
| Sterile Paper Points | For consistent and minimally invasive collection of subgingival biofilm samples. |
| Enzymatic Lysis Buffer | Contains enzymes (e.g., proteinase K, lysozyme) to break down bacterial cell walls and human proteins. |
| Chemical Lysis Buffer | Contains detergents (e.g., SDS) and chelating agents (e.g., EDTA) to dissolve lipids and inactivate nucleases. |
| Bashing Beads | Used in mechanical lysis to physically disrupt tough bacterial cell walls via vigorous vortexing. |
| Binding Silica Membrane/Column | selectively binds DNA while allowing contaminants like proteins and salts to be washed away. |
| Wash Buffers | Typically contain ethanol to remove salts and other impurities without eluting the DNA from the membrane. |
| Elution Buffer | A low-salt buffer or nuclease-free water used to release purified DNA from the binding membrane. |
| Nuclease-Free Water | Used for preparing solutions and eluting DNA to prevent degradation by environmental nucleases. |
| Proteinase K | A broad-spectrum protease critical for digesting proteins and degrading nucleases that could degrade DNA. |
Data Presentation and Visualization Guidelines
Effective communication of validation data is paramount. The choice between tables and graphs depends on the type of data and the message to be conveyed. [80] [81]
- Use Tables to present large amounts of data or when the message requires precise numerical values. A well-designed table should have clearly defined categories, units, and a concise caption. [81] For example, summary statistics for accuracy and precision across multiple concentration levels are best presented in a table.
- Use Data Plots to show relationships, trends, or comparisons. For continuous data (e.g., DNA concentration), use box plots to display the central tendency, spread, and outliers of different kit groups. Scatterplots are ideal for demonstrating linearity between theoretical and measured concentrations. [81] Avoid using bar graphs for continuous data as they can obscure the underlying data distribution. [81]
Designing a rigorous validation framework for commercial kits in unidentified bacteria research requires a systematic approach that integrates bioanalytical principles with practical experimental testing. By defining key validation parameters, implementing a structured workflow, and employing standardized protocols for comparative evaluation, researchers can generate robust, reliable data to guide their selection of the most fit-for-purpose kit. The comparative data presented here, while from a pilot study, highlights how such a framework can reveal significant differences in kit performance, ultimately ensuring the quality and reproducibility of scientific findings in both academic research and drug development.
Comparative Analysis of Leading Commercial Kits and Platforms
The accurate identification of unidentified bacteria is a cornerstone of microbiological research, impacting fields from clinical diagnostics to drug development. The validity of this research hinges on the initial steps of genomic DNA (gDNA) extraction and subsequent analysis. The selection of appropriate commercial kits and platforms is therefore not merely a procedural detail but a critical determinant of experimental success. This guide provides an objective comparison of leading solutions, framing the evaluation within the broader thesis that optimal performance is context-dependent, varying with sample type, biomass, and intended analytical method. It is designed to equip researchers and scientists with the data and protocols necessary to make informed decisions in their investigations.
Comparative Evaluation of DNA Extraction Kits
The efficiency of DNA extraction is a primary source of bias in microbial studies, especially with challenging samples like those with low biomass or complex cellular walls. The following section compares three commercially available DNA extraction kits, evaluating their performance based on yield, quality, and practicality.
Key Commercial Kits & Experimental Performance
A 2025 pilot study systematically evaluated three commercial DNA extraction kits for their efficiency in isolating microbial gDNA from small-volume subgingival biofilm samples collected on single paper points [43]. The kits were selected to represent a broad spectrum of lysis approaches: enzymatic, chemical, and mechanical.
Table 1: Comparison of DNA Extraction Kit Features and Performance [43]
| Kit Name | Manufacturer | Primary Lysis Method | Total dsDNA Yield (Health) | Total dsDNA Yield (Periodontitis) | Elution Volume (µL) | Cost per Extraction (€) | Processing Time (min) |
|---|---|---|---|---|---|---|---|
| DNeasy Blood & Tissue | QIAGEN | Enzymatic & Chemical | Highest | Highest | 100-200 | 4.48 | ~150 |
| NucleoSpin Tissue Mini | MACHEREY‑NAGEL | Enzymatic & Chemical | Intermediate | Intermediate | 60-100 | 3.48 | ~90 |
| ZymoBIOMICS DNA Miniprep | ZYMO RESEARCH | Mechanical (Bead Beating) | Lower | Lower | 50-100 | 6.51 | ~120 |
The performance data reveals that the DNeasy Blood and Tissue Kit (QIAGEN) demonstrated the highest efficiency, yielding significantly more total double-stranded DNA (dsDNA) in samples from both healthy and periodontitis-affected sites compared to the other kits [43]. This suggests that for the low-biomass environment of a healthy periodontal pocket, its enzymatic and chemical lysis protocol is particularly effective at liberating DNA.
Conversely, a separate 2025 study on neonatal gut microbiota found that bead-beating kits consistently outperformed a non-bead-beating QIAamp kit [82]. This highlights the thesis that the "best" kit is sample-dependent; mechanical disruption may be crucial for breaking open tough environmental or gut bacterial cell walls, while enzymatic lysis may be sufficient for other sample types.
Detailed Experimental Protocol for Kit Evaluation
The following methodology is adapted from the 2025 pilot study to provide a reproducible framework for evaluating DNA extraction kits [43].
1. Sample Collection:
- Material: Sterile paper points (e.g., VDW Dental, 29 mm, size 50).
- Procedure: Isolate the tooth with cotton rolls and dry the supragingival surface. Insert a single sterile paper point into the periodontal pocket (or other target site) for 15 seconds.
- Handling: Transfer the paper point immediately to a sterile 1.5 mL tube and rapidly freeze in liquid nitrogen. Store at -80°C until processing.
2. DNA Extraction Protocols:
- DNeasy Blood & Tissue Kit (QIAGEN): A "pipe-in-pipe" washing method is recommended for paper points. Add 1 mL nuclease-free water and 12 glass beads to the tube and shake at 14,000 rpm for 5 min. Pierce the tube bottom, place it in a 5 mL tube, and centrifuge at 4,000 × g for 1 min. Pellet the flow-through and resuspend in 180 µL enzymatic lysis buffer. Then, follow the manufacturer's protocol for Gram-positive bacteria and "Purification of Total DNA from Animal Tissues," eluting in 100 µL Buffer AE [43].
- NucleoSpin Tissue Mini Kit (MACHEREY‑NAGEL): Follow the manufacturer's support protocol for dental swabs. Use the pipette method to separate the lysis solution from the paper point. Elute the DNA in 100 µL elution buffer BE [43].
- ZymoBIOMICS DNA Miniprep Kit (ZYMO RESEARCH): Follow the standard protocol with enhanced mechanical lysis. Vortex the sample with BashingBeads on maximum speed for 1 minute, followed by a 5-minute pause. Repeat this cycle five times. Elute the DNA in 100 µL DNase/RNase-free water [43].
3. DNA Quantification and Quality Control:
- Total DNA Yield: Measure UV absorption at 260 nm using a spectrophotometer (e.g., NanoDrop).
- dsDNA Yield: Use a fluorometric method (e.g., Qubit dsDNA HS Assay) for a more accurate quantification of intact, double-stranded DNA.
- Bacterial DNA Quantification: Perform qPCR with universal primers targeting the bacterial 16S rRNA gene to determine the proportion of bacterial DNA in the total yield [43].
Figure 1: Generalized DNA extraction workflow from sample collection to final elution, highlighting the primary lysis method divergence.
Analysis of Microbial Identification Platforms
Beyond DNA extraction, the choice of an identification platform is critical for data generation. The market offers a range of technologies, each with strengths tailored to specific applications.
Table 2: Leading Microbial Identification Platforms and Their Applications [83] [84]
| Vendor / Platform | Key Technology | Optimal Use-Case | Key Features |
|---|---|---|---|
| BioMérieux | MALDI-TOF, Automated Systems | Clinical Diagnostics | High speed, regulatory-compliant, validated for clinical pathogens. |
| Thermo Fisher Scientific | Next-Generation Sequencing (NGS), qPCR | Research & Development | Detailed microbial characterization, resistance gene detection, high-resolution genomics. |
| Bruker Corporation | MALDI-TOF Mass Spectrometry | Clinical & Industrial Labs | Rapid identification of bacteria, fungi, and yeasts via protein fingerprints. |
| Charm Sciences / 3M | Immunoassays, Rapid Tests | Food Safety & Environmental Testing | High-throughput, ease-of-use, rapid results for field and production environments. |
| Hach / Neogen | Portable Molecular & Biochemical | Field Testing & On-Site Analysis | Portability for quick results outside traditional lab settings. |
The global microbial identification market, driven by the infectious disease burden and food safety concerns, is anticipated to grow from USD 4.69 billion in 2025 to USD 10.31 billion by 2035 [84]. This growth is fueled by technological advancements. Next-Generation Sequencing (NGS) allows for comprehensive genomic analysis, detecting pathogens and resistance genes with high precision, which is invaluable for outbreak investigation and research [84]. Matrix-Assisted Laser Desorption/Ionization-Time of Flight (MALDI-TOF) Mass Spectrometry has revolutionized routine diagnostics by providing rapid, economical identification of microorganisms based on unique protein profiles, significantly reducing turnaround times in clinical labs [84]. Emerging trends point towards the integration of AI and machine learning for enhanced accuracy and predictive capabilities, as well as the development of portable, microfluidics-based devices for point-of-care testing in resource-limited environments [83] [84].
The Scientist's Toolkit: Essential Research Reagents & Materials
Successful microbial identification relies on a suite of essential materials and reagents. The following table details key components used in the featured experiments and the broader field.
Table 3: Essential Research Reagent Solutions for Microbial DNA Analysis
| Item | Function / Description | Example Use in Protocol |
|---|---|---|
| Sterile Paper Points | Minimally invasive tool for collecting subgingival biofilm and crevicular fluid. | Inserted into periodontal pocket for 15 seconds to absorb sample [43]. |
| Proteinase K | Broad-spectrum serine protease that digests histones and denatures proteins. | Used in enzymatic lysis buffers to degrade cellular proteins and nucleases [43]. |
| BashingBeads / Lysing Matrix | High-density beads for mechanical disruption of tough microbial cell walls. | Critical in bead-beating kits for homogenizing samples and ensuring complete lysis [43] [82]. |
| Silica Membrane Columns | selectively bind nucleic acids in the presence of high-concentration salt buffers. | Used in all three evaluated kits for purifying DNA from lysates during extraction [43]. |
| Universal 16S rRNA Primers | Short DNA sequences that bind to conserved regions of the bacterial 16S gene. | Used in qPCR to quantify bacterial DNA load and profile community structure [43]. |
| Fluorometric dsDNA Dye | A dye that fluoresces upon binding to double-stranded DNA but not single-stranded DNA or RNA. | Provides a highly accurate measurement of intact DNA yield (e.g., Qubit assay) [43]. |
Figure 2: A decision-flow diagram to guide the selection of appropriate DNA extraction and identification technologies based on sample type and research requirements.
This comparative analysis underscores that there is no single "best" kit or platform for all scenarios in unidentified bacteria research. The experimental data clearly shows that the QIAGEN DNeasy Blood and Tissue Kit was superior for low-volume subgingival biofilm samples, whereas other studies emphasize the necessity of bead-beating-based kits like ZymoBIOMICS or PowerSoil for tougher cell walls in stool samples [43] [82]. Similarly, the choice between a rapid MALDI-TOF system for clinical diagnostics and a deep-sequencing NGS platform for research depends entirely on the project's goals. Therefore, researchers must frame their selection within the specific context of their sample type, biomass, required resolution, and operational constraints to ensure the generation of robust and reliable data.
The accurate identification of microorganisms is a cornerstone of microbiological research, clinical diagnostics, and drug development. As technological advancements introduce increasingly sophisticated analytical methods, the rigorous benchmarking of new techniques against established gold standards becomes paramount for validating their performance and establishing their appropriate applications. In commercial kits for unidentified bacteria research, understanding the relative strengths and limitations of available methods ensures reliable results and informed methodological selections. This comparison guide provides an objective evaluation of three fundamental approaches—culture-based methods, polymerase chain reaction (PCR), and liquid chromatography-tandem mass spectrometry (LC-MS/MS)—framed within the context of method validation and performance benchmarking.
The process of benchmarking typically involves a method comparison experiment where results from a candidate method are compared against a comparator method, often one that has already been approved or is considered a reference standard [85]. This process is central to regulatory acceptance and scientific validation, providing critical data on sensitivity, specificity, and overall reliability. For microbial identification, the choice of benchmark method depends significantly on the intended application, as tests valued for population screening may prioritize different performance characteristics than those intended for tracking pathogen dynamics over time [85].
Performance Comparison at a Glance
The following table summarizes the key characteristics, performance metrics, and typical applications of the three gold standard methods discussed in this guide, providing a quick reference for researchers.
Table 1: Comparative overview of culture, PCR, and LC-MS/MS methods for microbial identification
| Feature | Culture-Based Methods | PCR-Based Methods | LC-MS/MS-Based Proteomics |
|---|---|---|---|
| Basis of Identification | Phenotypic characteristics (morphology, physiology, biochemistry) [86] | Genetic markers (16S rRNA gene, species-specific DNA sequences) [86] | Protein and peptide profiles (specific peptide markers) [87] |
| Typical Timeframe | 2-5 days to over a week [86] | Several hours to 1-2 days [88] | Several hours to 1 day [87] |
| Throughput | Low to moderate | High | High |
| Sensitivity & Specificity | High specificity but lower sensitivity for unculturable or fastidious organisms [86] | High sensitivity and specificity (e.g., 80-100% PPA for PCR kits) [88] [85] | High sensitivity and specificity (e.g., 0.01% detection of adulterants) [87] |
| Key Quantitative Metrics | Not inherently quantitative; based on phenotypic observation | Ct (Cycle threshold) values; Positive Percent Agreement (PPA); Negative Percent Agreement (NPA) [88] [85] | Limit of Detection (LOD)/Limit of Quantification (LOQ); Recovery (Accuracy: 80-107%); Precision (RSD: 5-10%) [87] |
| Primary Applications | Gold standard for viability; teaching fundamental microbiology skills [89] | Rapid, specific detection of pathogens; epidemiological studies [86] [88] | High-throughput biomarker discovery; detection in complex matrices; authentication of origin [90] [91] [87] |
| Main Limitations | Time-consuming; cannot identify non-culturable organisms [86] | Requires prior knowledge of target sequences; potential for false positives [87] | High instrument cost; requires expert operation and data analysis [90] |
Detailed Experimental Protocols and Benchmarking Data
Culture-Based Methods: The Foundational Benchmark
Experimental Protocol: The Bacterial Unknowns Project A classic microbiology project involves identifying two unknown bacteria (one Gram-positive, one Gram-negative) from a predefined list of species through a series of diagnostic tests, embodying the core principles of culture-based identification [89].
- Isolation and Staining: The first step is streaking the mixed sample onto solid media to achieve isolated pure colonies. This is followed by Gram staining to determine the Gram status and morphology of each isolate [89].
- Biochemical Testing: Isolates are subjected to a panel of biochemical assays. A minimum of five tests is typically required for confirmation. Common tests include [89]:
- Triple Sugar Iron (TSI) Agar: Assesses carbohydrate fermentation and hydrogen sulfide production.
- Litmus Milk Media: Determines various metabolic reactions in milk.
- Urea Broth: Tests for the enzyme urease.
- Phenol Red Broths: Evaluate fermentation of different carbohydrates.
- Mannitol Salt Agar: A selective and differential medium for staphylococci.
- Analysis: Results from the tests are compared to known metabolic profiles of bacteria to deduce their identity and rule out other species [89].
Benchmarking Context: While this method is foundational, it is time-consuming and labor-intensive, taking several days [86]. Its utility as a benchmark lies in its ability to confirm viability and provide phenotypic information that molecular methods cannot. However, its limitations have driven the adoption of molecular techniques for faster and more precise identification [86].
PCR-Based Methods: The Molecular Gold Standard
Experimental Protocol: Evaluating Commercial RT-PCR Kits A study evaluating seven commercial RT-PCR kits for COVID-19 detection provides a robust framework for benchmarking molecular diagnostics [88].
- Sample Preparation: Known positive (n=40) and negative (n=10) samples are characterized using a reference WHO protocol. Positive samples should include a range of viral loads (high and low) as indicated by Ct values [88].
- Nucleic Acid Extraction: RNA is extracted from viral transport media using a standardized viral DNA/RNA kit on an automated extraction instrument [88].
- PCR Amplification: A 25μL reaction is prepared using the kit's master mix, primers, and probes. Thermocycling is performed as per the manufacturer's instructions, typically involving reverse transcription followed by 40 amplification cycles [88].
- Data Analysis: Results are interpreted based on the kit's prescribed Ct value cut-off (e.g., <40 is positive). Sensitivity is calculated based on the kit's ability to detect weak positive samples (Ct >30) [88].
Benchmarking Data from Kit Comparison: The following table summarizes the performance of selected commercial PCR kits from a comparative study, illustrating how benchmarking data is typically presented [88].
Table 2: Performance evaluation of selected commercial RT-PCR kits on pooled samples
| Kit Name | Manufacturer | Target Genes | Sensitivity on Weak Positives (Ct >30) | Remarks |
|---|---|---|---|---|
| TRUPCR SARS-CoV-2 Kit | Black Bio | E, N, RdRP | 100% | Recommended for pooled testing |
| TaqPath COVID-19 Kit | Thermo Fisher | S, N, ORF1ab | 100% | Recommended for pooled testing |
| Allplex 2019-nCoV Assay | Seegene | E, N, RdRP | 100% | Recommended for pooled testing |
| Fosun COVID-19 RT-PCR Kit | Fosun | E, N, ORF1ab | 90% | - |
| LabGun COVID-19 RT-PCR Kit | Lab Genomics | E, RdRP | 85% | - |
| Patho detect COVID-19 Kit | My Lab | E, RdRP | 75% | - |
The same study highlighted that kits with 100% sensitivity on weak positive samples were deemed most suitable for pooled sample testing, a key finding for operational benchmarking [88].
LC-MS/MS-Based Proteomics: The Emerging High-Throughput Technique
Experimental Protocol: Gelatin Source Identification via Specific Peptide Markers An LC-MS/MS method for identifying bovine and porcine gelatin in food products demonstrates a proteomic approach to species authentication, a principle applicable to bacterial identification [87].
- Protein Digestion: Gelatin samples are digested into peptides using trypsin, following standard protocols for protein reduction and alkylation [87].
- LC-MS/MS Analysis with MRM: Digested peptides are separated by liquid chromatography. The mass spectrometer is operated in Multiple Reaction Monitoring (MRM) mode, targeting specific precursor and product ion transitions for peptide markers unique to bovine (e.g., GEAGPSGPAGPTGAR) and porcine gelatin [87].
- Quantification and Validation: The method is validated at multiple concentration levels. Key performance metrics include [87]:
- Accuracy (Recovery): 80% - 107%.
- Precision (Relative Standard Deviation): 5.16% - 9.97%.
- Linearity (R²): ≥ 0.99.
- Limit of Quantification (LOQ): As low as 0.01% for gelatin adulteration.
Benchmarking Against PCR: This study directly compared LC-MS/MS with PCR, finding the LC-MS/MS method to be highly sensitive and capable of providing results within 4 hours. A key advantage noted was the ability of LC-MS/MS to detect multiple species simultaneously in a single run without prior knowledge of the specific targets, unlike PCR which typically requires separate assays for each species [87].
Experimental Protocol: Benchmarking DIA Workflows in Proteomics For broader proteomic applications, such as biomarker discovery, benchmarking involves comparing data processing workflows using samples of known composition.
- Benchmark Sample Preparation: Mixtures of proteome digests from different species (e.g., human, yeast, E. coli) are prepared in defined ratios to create samples with known, expected fold changes in protein abundance [92].
- Data Acquisition: Samples are analyzed using the LC-MS/MS workflow (e.g., Data-Independent Acquisition - DIA) [92].
- Data Processing and Benchmark Analysis: The raw data is processed through software like DIA-NN. The output is analyzed with a specialized R script (e.g., LFQ_bout) that calculates summary statistics, including coefficients of variation (CV), asymmetry factors, and confusion matrices, to evaluate quantification accuracy by comparing measured fold changes to expected values [92].
Workflow Visualization
The following diagrams illustrate the logical workflow and key decision points for each of the three gold standard methods.
Diagram 1: Culture-based identification involves isolation and phenotypic testing.
Diagram 2: PCR-based identification relies on genetic amplification and detection.
Diagram 3: LC-MS/MS identification uses protein separation and mass analysis.
The Scientist's Toolkit: Essential Research Reagent Solutions
Successful execution of the described methodologies requires specific reagents and tools. The following table details key solutions for the featured experiments.
Table 3: Essential research reagents and their functions in microbial identification
| Research Reagent Solution | Function | Example Application Context |
|---|---|---|
| Selective & Differential Media | Allows isolation and preliminary identification based on growth and metabolic reactions. | Mannitol Salt Agar for selecting Staphylococcus species [89]. |
| Specific Peptide Markers | Unique amino acid sequences used as targets for unambiguous identification of proteins and their source organisms. | Identifying bovine vs. porcine gelatin via markers like GEAGPSGPAGPTGAR [87]. |
| LC-MS/MS Internal Standards | Known compounds added to correct for variability in sample preparation and instrument response, ensuring quantification accuracy. | Using stable isotope-labeled peptides for precise quantification in proteomic workflows [93]. |
| Primers and Probes | Short, specific nucleic acid sequences that bind to complementary target DNA regions to enable amplification and detection. | Targeting the E, N, and RdRP genes for SARS-CoV-2 detection in PCR kits [88]. |
| Reference Proteomes/Databases | Curated collections of protein sequences used to identify peptides from MS/MS spectra by database searching. | Using canonical Swiss-Prot subsets of UniProt reference proteomes for human, yeast, and E. coli [92]. |
| Trypsin | A proteolytic enzyme that cleaves proteins at specific amino acids (lysine and arginine) to generate peptides for LC-MS/MS analysis. | Digesting gelatin or bacterial proteins into peptides for downstream proteomic analysis [87]. |
Assessing Sensitivity, Specificity, and Limit of Detection
In the field of unidentified bacteria research, the accuracy and reliability of diagnostic tests are paramount. The performance of commercial detection kits is quantitatively assessed through three fundamental metrics: sensitivity, specificity, and limit of detection (LOD). These parameters form the cornerstone for evaluating the clinical validity and analytical robustness of any diagnostic tool, guiding researchers in selecting the most appropriate kit for their specific application. Sensitivity reflects the test's ability to correctly identify true positives, while specificity measures its capacity to correctly identify true negatives [94]. The LOD defines the lowest concentration of an analyte that can be reliably distinguished from a blank sample, representing the ultimate detection capability of the assay [95] [96]. A comprehensive understanding of these metrics, supported by well-designed experimental data, is essential for researchers and drug development professionals who rely on precise bacterial identification to advance public health and therapeutic development.
Defining the Core Metrics
Sensitivity and Specificity
In diagnostic testing, sensitivity and specificity are prevalence-independent test characteristics that describe the intrinsic accuracy of a test [94].
- Sensitivity (True Positive Rate): This is the probability that a test result will be positive when the disease is present. Mathematically, it is defined as the number of true positives divided by the total number of actually sick individuals (true positives + false negatives) [97] [94]. A test with high sensitivity is crucial for "ruling out" a disease, as it minimizes the chance of false negatives. In a clinical or research setting, this is particularly important when the consequence of missing a true positive is severe [94].
- Specificity (True Negative Rate): This is the probability that a test result will be negative when the disease is not present. It is calculated as the number of true negatives divided by the total number of actually well individuals (true negatives + false positives) [97] [94]. A test with high specificity is valuable for "ruling in" a disease, as it minimizes false positives. This is especially critical when a positive test result leads to further invasive testing, expense, or stigma for the patient [94].
There is an inherent trade-off between sensitivity and specificity; adjusting the test cutoff point to increase one will typically decrease the other [97] [94].
Limit of Detection (LOD)
The Limit of Detection is a key measure of analytical sensitivity. The International Organization for Standardization (ISO) defines the LOD as the lowest true net concentration of a component that will lead, with a high probability (typically 1-β, where β is the risk of a false negative), to the conclusion that the component is present [96]. Determining the LOD involves managing two types of statistical errors [96]:
- Type I Error (α): The risk of a false positive, i.e., concluding an analyte is present when it is not.
- Type II Error (β): The risk of a false negative, i.e., failing to detect an analyte that is present.
The clinical and laboratory standards institute (CLSI) guideline EP17 provides a standardized method for determining the LOD, which involves first establishing the Limit of Blank (LoB) and then the LOD [95]. The relationships and calculations between these concepts are outlined in the diagram below.
In chromatographic and other analytical methods, a common practical approach for estimating the LOD is the signal-to-noise ratio (S/N) method, where the LOD is often defined as the concentration that yields a signal three times the height of the background noise [96].
Experimental Comparison of Commercial Kits
Case Study: SARS-CoV-2 Serology Kits
A 2025 study provides a robust model for kit comparison by evaluating three commercial ELISA kits for detecting SARS-CoV-2 antibodies in animal sera, using a pseudovirus neutralization test (pVNT) as the reference gold standard [98]. This experimental design mirrors the challenges faced in unidentified bacteria research, where a definitive diagnostic standard must be established.
Experimental Protocol:
- Sample Collection: 101 serum samples from six animal species (cats, dogs, ferrets, wild boar, goats, and lions) were used to assess cross-species applicability [98].
- Reference Method: A pVNT, which can be performed in BSL-2 laboratories and simulates virus entry and infection, was used as the confirmatory test for neutralizing antibodies [98].
- Index Tests: The three ELISA kits were:
- ELISA-1:
cPass SARS-CoV-2 Neutralization Antibody Detection Kit(Genscript). A competitive ELISA detecting neutralizing antibodies against the Receptor Binding Domain (RBD) [98]. - ELISA-2:
SARS-CoV-2 NeutraLISA kit(EUROIMMUN). Also a competitive ELISA targeting RBD neutralizing antibodies [98]. - ELISA-3:
ID Screen SARS-CoV-2 Double Antigen Multi-species assay(IDVET). A double-antigen ELISA detecting total antibodies against the Nucleoprotein (N) [98].
- ELISA-1:
- Analysis: Results from each ELISA were compared against the pVNT results to calculate diagnostic performance metrics [98].
Results and Comparative Data: The study's findings, which highlight the impact of target antigen and kit design on performance, are summarized in the table below.
Table 1: Performance Comparison of Three Commercial SARS-CoV-2 ELISA Kits
| Kit Name | Target Antigen | Assay Format | Diagnostic Performance (vs. pVNT) | Key Findings |
|---|---|---|---|---|
| ELISA-1 (cPass) | RBD | Competitive ELISA | Highest diagnostic performance; most reliable for initial screening | Superior sensitivity for detecting seropositive animals; RBD target offers higher specificity [98] |
| ELISA-2 (NeutraLISA) | RBD | Competitive ELISA | Lower sensitivity than ELISA-1 | Demonstrated lower capability to detect true positives compared to ELISA-1 [98] |
| ELISA-3 (ID Screen) | Nucleoprotein (N) | Double-Antigen ELISA | Lower sensitivity for detecting seropositive animals | N protein is more conserved, potentially leading to cross-reactivity with other coronaviruses [98] |
This case study demonstrates that even kits targeting the same pathogen can exhibit significantly different performance based on the chosen antigen and test methodology. The RBD of the spike protein was found to provide greater specificity for SARS-CoV-2 compared to the more conserved nucleoprotein, a critical consideration when developing or selecting tests for novel bacterial species where cross-reactivity is a concern [98].
Case Study: SARS-CoV-2 Molecular Detection Kits
Another relevant study compared the analytical sensitivity (LOD) of various SARS-CoV-2 molecular detection kits approved by the National Medical Products Administration [99]. This study highlights the importance of independently verifying manufacturer claims.
Experimental Protocol: The study utilized armored RNA reference materials to evaluate the LOD of multiple kits based on rRT-PCR and other molecular detection assays. This approach provides a standardized and safe way to compare performance across different platforms [99].
Results and Comparative Data: The study found that the percentage of samples requiring retesting increased as the viral concentration decreased, with 23.08% of samples at a concentration of 781 copies/mL needing retesting. Importantly, 93% of the rRT-PCR kits evaluated had an LOD of less than 1000 copies/mL, while the LOD for other molecular detection kits ranged from 68 to 2264 copies/mL [99]. This variance underscores the necessity for researchers to base kit selection on independently verified performance data rather than manufacturer specifications alone.
The Scientist's Toolkit: Essential Reagents and Materials
Successful diagnostic evaluation and research in bacteriology require a suite of core reagents and materials. The following table details key solutions and their functions in a typical workflow.
Table 2: Key Research Reagent Solutions for Diagnostic Assay Evaluation
| Item | Function in the Experiment |
|---|---|
| Reference Materials | Certified standards (e.g., armored RNA, purified antigens) used to calibrate assays, determine the LOD, and ensure accuracy across different laboratories and experiments [99]. |
| Gold Standard Reagents | Components for the definitive test method (e.g., for pVNT: pseudoviruses, cell lines, reporter systems). This provides the benchmark against which new or commercial kits are validated [98]. |
| Assay Kits & Components | Commercial kits or in-house assay components including pre-coated plates, specific antigens (e.g., RBD, N protein), conjugated antibodies, and substrate solutions for detection [98]. |
| Sample Diluents & Buffers | Solutions used to dilute samples and standards to a workable concentration, maintain pH, and minimize non-specific binding to ensure assay stability and reproducibility. |
| Control Panels | Characterized positive and negative control samples, crucial for validating each run of an experiment, monitoring assay performance over time, and calculating sensitivity and specificity [98] [94]. |
Experimental Design and Workflow
A rigorous experimental workflow for assessing sensitivity, specificity, and LOD is crucial for generating reliable, comparable data. The following diagram and protocol outline a generalized approach suitable for evaluating commercial kits for bacterial detection.
Detailed Experimental Protocol:
- Define the Gold Standard: The first and most critical step is to establish a definitive method for confirming the presence or absence of the target bacterium. This could be culture-based methods, genome sequencing, or an already-validated high-complexity test. The performance of all commercial kits will be judged against this standard [98] [97].
- Assemble a Characterized Sample Panel: Collect a sufficient number of well-characterized samples. This panel should include samples with known positive status (true positives) and known negative status (true negatives), covering a range of expected bacterial loads or analyte concentrations. The sample size must be adequate to provide statistically meaningful results [98].
- Establish the Limit of Detection (LOD):
- Prepare a dilution series of the target bacterium or its specific marker (e.g., a purified antigen or nucleic acid) in a relevant matrix.
- Analyze multiple replicates (a minimum of 10 is recommended, 20-60 for robust validation) at each concentration level, including a blank (matrix only) [95] [96].
- Calculate the LOD using established formulas, such as
LOD = LoB + 1.645(SD_low concentration sample), where the Limit of Blank (LoB) is first determined from the blank measurements [95].
- Execute Index Tests with Commercial Kits: Run all samples in the characterized panel using the commercial kits under evaluation. This should be performed in a blinded manner, where the operator is unaware of the gold standard results to prevent bias. Strictly adhere to the manufacturer's instructions for each kit [98].
- Compare Results and Construct a Contingency Table: Compare the results from each commercial kit to the results from the gold standard. Tally the outcomes into a 2x2 table, classifying them as True Positives (TP), False Positives (FP), True Negatives (TN), and False Negatives (FN) [97] [94].
- Calculate Performance Metrics:
The objective evaluation of commercial detection kits through rigorous assessment of sensitivity, specificity, and LOD is a fundamental practice in modern unidentified bacteria research. As demonstrated by the comparative studies, the choice of target antigen and assay format directly influences test performance. Researchers must employ standardized experimental protocols, utilize well-characterized sample panels, and use a definitive gold standard to generate reliable data. By systematically applying these principles, scientists and drug development professionals can make informed decisions, select the most fit-for-purpose diagnostic tools, and ultimately contribute to more accurate bacterial identification and effective public health responses.
For researchers identifying unknown bacteria, selecting the right methodology involves a critical evaluation of cost, throughput, and automation. This guide compares conventional biochemical methods, molecular diagnostics, and modern high-throughput kits to inform laboratory decision-making.
The table below compares the core identification methodologies for unnamed bacteria, highlighting their key performance metrics.
| Methodology | Typical Cost per Sample | Time to Result | Throughput Potential | Key Differentiators |
|---|---|---|---|---|
| Conventional Biochemical Panels [100] | Low (85% lower reagent cost) [100] | 24-72 hours | Low (Manual, serial processing) | Gold standard; high labor input; lower speed. [100] |
| Automated Molecular Detection (e.g., associated with CM) [101] | Higher initial investment | Hours (Enables therapeutic adequacy in a short time) [101] | High (Amenable to automation) | Cost-effective; reduces deaths and resistant infections; dominant in CEA. [101] |
| High-Throughput Kits (e.g., NAxtra protocol) [102] | Low-cost and cost-effective [102] | Fast (14 min for 96 samples on a robot) [102] | Very High (288 samples in one run) [102] | Designed for automation; superior for low-microbial biomass samples. [102] |
Experimental Protocols for Key Data
The comparative data in the summary table is derived from published experimental procedures. The following sections detail the protocols used to generate this critical performance data.
Protocol for Abbreviated Biochemical Algorithm
This protocol, evaluated in a 2010 study, demonstrates a cost-reduced conventional method. [100]
- Sample Preparation: Bacterial pathogens are primarily isolated on blood agar and MacConkey agar.
- Primary Tests: Isolates are subjected to oxidase and indole tests. Lactose fermentation is inferred from colonial morphology on MacConkey agar.
- Confirmation: A limited set of conventional biochemical tests is used for genus-level confirmation, specifically avoiding extensive commercial panels.
- Outcome Measurement: Accuracy is determined by comparing results to commercial identification kits. Cost and technologist time are tracked and compared to full biochemical panels. [100]
Protocol for High-Throughput Nucleic Acid Extraction and Sequencing
This modern protocol, detailed in a 2025 study, is designed for bacterial microbiota profiling, including the identification of unnamed bacteria in a mixture. [102]
- Sample Collection: Nasopharyngeal aspirates, nasal swabs, and saliva samples are collected.
- Automated Nucleic Acid Extraction: The NAxtra magnetic nanoparticle-based kit is used. The process is automated on a liquid handling robot (e.g., Tecan Fluent), with an input volume of 100 µl and an elution volume of 80 µl.
- Library Preparation & Sequencing: The V3-V4 region of the 16S rRNA gene is amplified via a two-step PCR procedure. Final libraries are sequenced on an Illumina MiSeq platform with 300 bp paired-end reads.
- Bioinformatic Analysis: Demultiplexed FASTQ files are processed in QIIME2. Sequences are denoised into Amplicon Sequence Variants (ASVs) using DADA2 and classified taxonomically against the SILVA database. [102]
Workflow and Cost-Benefit Logic
The following diagram illustrates the logical pathway for selecting a bacterial identification method based on project goals and resource constraints, leading to the associated cost-benefit outcome.
The Scientist's Toolkit: Essential Research Reagents & Materials
This table details key materials and technologies used in the featured experiments and their critical functions.
| Item | Function in Research |
|---|---|
| NAxtra Nucleic Acid Kit [102] | A fast, low-cost, high-throughput magnetic nanoparticle-based method for extracting total nucleic acid from low-microbial biomass samples. |
| Liquid Handling Robot [102] | (e.g., Tecan Fluent) Automates the nucleic acid extraction process, enabling high throughput (e.g., 288 samples per run) and rapid results. |
| 16S rRNA Gene Sequencing [102] | A culture-independent method for bacterial identification and microbiota profiling by sequencing the hypervariable regions of the 16S ribosomal RNA gene. |
| Illumina MiSeq Platform [102] | A next-generation sequencing system used for mid-throughput sequencing of prepared 16S rRNA libraries. |
| Magnetic Nanoparticles [102] | The core of certain extraction protocols, they bind nucleic acids in the presence of a magnetic field, allowing for purification and automation. |
| Biochemical Test Panels [100] | A series of substrates and media used to determine the metabolic capabilities of a bacterial isolate for genus-level identification. |
| Total Cost of Ownership (TCO) [103] [104] | A financial estimate to determine the direct and indirect costs of a system or method over its entire lifecycle, beyond the initial purchase price. |
Conclusion
The effective evaluation of commercial kits for unidentified bacteria is paramount for advancing biomedical and clinical research. A strategic approach that combines a deep understanding of foundational technologies, rigorous application of methodological workflows, proactive troubleshooting, and comprehensive validation is essential for success. The future of bacterial identification lies in the adoption of rapid, high-throughput, and integrated technologies like next-generation sequencing and AI-driven analysis. Researchers must prioritize validation and cross-comparison to ensure data reliability, ultimately accelerating drug discovery, improving patient diagnostics, and strengthening public health defenses against emerging bacterial threats.
References
- 1. Advancing clinical biochemistry: addressing gaps and driving ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12011881/]
- 2. Classic and contemporary approaches to modeling ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC2932968/]
- 3. The convergence of traditional and digital biomarkers ... [https://www.sciencedirect.com/science/article/pii/S0956566323003299]
- 4. Bacterial DNA Contamination of Commercial PCR Enzymes [https://pmc.ncbi.nlm.nih.gov/articles/PMC12029200/]
- 5. Performance Evaluation of Two Kinds of Rapid Antigen ... [https://pubmed.ncbi.nlm.nih.gov/36912313/]
- 6. Comparison of immunological and molecular methods ... - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC10846737/]
- 7. Bacteriological Testing Market Size, Share, Trends - 2030 [https://www.marketsandmarkets.com/Market-Reports/bacteriological-testing-market-238062451.html]
- 8. Bacterial ID Tools Market Trends and Regional Growth ... [https://www.towardshealthcare.com/insights/bacterial-id-tools-market-sizing]
- 9. Bacteria Detection Kits Market Analysis by Size, Share & ... [https://www.theinsightpartners.com/reports/bacteria-detection-kits-market]
- 10. Microbial Identification Market Size and Trends, 2025-2032 [https://www.coherentmarketinsights.com/industry-reports/microbial-identification-market]
- 11. Bacteria Detection Kits Market Partnering Deals of Key ... [https://www.openpr.com/news/3466096/bacteria-detection-kits-market-partnering-deals-of-key-players]
- 12. Microbiome Testing Kit Market Report 2025 [https://www.researchandmarkets.com/reports/6178241/microbiome-testing-kit-market-report?srsltid=AfmBOopOatsytwhbgLN2sv2iU0ra9Y6kLORFxRks5GUnWDYV1gz-e00M]
- 13. Bacteria Detection Kits Market Insights 2025: Key Metrics ... [https://www.linkedin.com/pulse/bacteria-detection-kits-market-insights-2025-zflqc/]
- 14. Microbial Identification Kits and Libraries [https://www.thermofisher.com/us/en/home/life-science/bioproduction/contaminant-and-impurity-testing/microbial-identification/kits-libraries.html]
- 15. Bacteria Detection Kits Future-proof Strategies [https://www.archivemarketresearch.com/reports/bacteria-detection-kits-324768]
- 16. Harnessing AI to Revolutionize Antibiotic Discovery [https://asm.org/articles/2025/august/ai-next-frontier-antibiotic-discovery]
- 17. Without Safeguard, AI-Bio Integration Risks Accelerating ... [https://www.frontiersin.org/journals/microbiology/articles/10.3389/fmicb.2025.1734561/full]
- 18. Comparison of a Point-of-Care FilmArray Test to Standard-of ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC9029956/]
- 19. Comparative Evaluation of a multiplex PCR panel for high ... [https://www.sciencedirect.com/science/article/pii/S1201971225003698]
- 20. Multiplex PCR point of care testing versus routine, laboratory ... [https://bmcinfectdis.biomedcentral.com/articles/10.1186/s12879-017-2784-z]
- 21. Evaluation of Three Commercial Assays for Rapid ... [https://pubmed.ncbi.nlm.nih.gov/25630646/]
- 22. Single Laboratory Evaluation of the Q20+ Nanopore ... [https://pubmed.ncbi.nlm.nih.gov/39595947/]
- 23. Single Laboratory Evaluation of the Q20+ Nanopore ... [https://www.mdpi.com/1422-0067/25/22/11877]
- 24. Comprehensive performance evaluation of a high ... [https://www.frontiersin.org/journals/microbiology/articles/10.3389/fmicb.2025.1609142/full]
- 25. a novel filtration and targeted next-generation sequencing ... [https://www.frontiersin.org/journals/microbiology/articles/10.3389/fmicb.2025.1538265/full]
- 26. Making the best of a bad sample: Comparison of DNA and... extraction [https://pmc.ncbi.nlm.nih.gov/articles/PMC12121741/]
- 27. Comparison of DNA extraction methods on different ... [https://www.nature.com/articles/s41598-024-59086-4]
- 28. Comparison of 6 DNA extraction methods for isolation ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10401787/]
- 29. Comparative evaluation of commercial DNA isolation ... [https://pubmed.ncbi.nlm.nih.gov/39532954/]
- 30. Comparative evaluation of commercial DNA isolation ... [https://www.nature.com/articles/s41598-024-78066-2]
- 31. Optimizing Sample Preparation for DNA Extraction [https://dpxtechnologies.com/optimizing-sample-preparation-for-dna-extraction/]
- 32. Protocol for efficient recovery of high-quality DNA from ... [https://pubmed.ncbi.nlm.nih.gov/41025248/]
- 33. Top DNA /RNA Extraction Kits Companies & How to Compare Them... [https://www.linkedin.com/pulse/top-dnarna-extraction-kits-companies-how-compare-them-wsmdc]
- 34. Evaluation of the VITEK 2 System for Identification and ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC130656/]
- 35. VITEK® 2 | Pioneering Diagnostics - bioMerieux [https://www.biomerieux.com/us/en/our-offer/clinical-products/vitek-2.html]
- 36. Evaluation of MicroScan Bacterial Identification Panels for ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC7922174/]
- 37. Evaluation of the VITEK 2 System for the Identification and ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC88326/]
- 38. Direct inoculation method using BacT/ALERT 3D and BD ... [https://www.sciencedirect.com/science/article/abs/pii/S073288931200096X]
- 39. Investigation of Carriers of Salmonella and Other Hydrogen ... [https://www.mdpi.com/2076-2615/14/22/3247]
- 40. Commercial Kits | MI - Microbiology [https://microbiology.mlsascp.com/commercial-kits.html]
- 41. Comparison of API 20E and invA PCR for Identification ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC1594722/]
- 42. foodproof® Salmonella Detection Kit [https://www.hygiena.com/food-safety/pathogen-detection/salmonella/foodproof-salmonella-detection-kit]
- 43. Comparative pilot study of three commercial kits ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12372513/]
- 44. Cell Culture Contamination / Bacteria Detection / Onar ... [https://minervabiolabs.us/bacteria-detection-kits/1219-onar-bacteria.html]
- 45. Advances in Rapid Identification and Susceptibility Testing ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC5391540/]
- 46. Comparison of three commercial DNA extraction kits and ... [https://pubmed.ncbi.nlm.nih.gov/41177336/]
- 47. Comparison of three commercial DNA extraction kits and ... [https://www.sciencedirect.com/science/article/abs/pii/S0167701225002337]
- 48. Antibiotic Resistance Kits - Streck [https://www.streck.com/products/molecular/antibiotic-resistance-kits/]
- 49. A Clinical Bacterial Dataset for Deep Learning in ... [https://www.nature.com/articles/s41597-024-03370-5]
- 50. Pharmaceutical Water Market Size to Reach USD 99.30 ... [https://www.precedenceresearch.com/pharmaceutical-water-market]
- 51. Pharmaceutical Water Market Size & Opportunities, 2025- ... [https://www.coherentmarketinsights.com/industry-reports/pharmaceutical-water-market]
- 52. Global Pharmaceutical Water Market 2025–2034 [https://www.custommarketinsights.com/report/pharmaceutical-water-market/]
- 53. Rapid and cost-effective identification of microorganisms from ... [https://bmcinfectdis.biomedcentral.com/articles/10.1186/s12879-025-11129-5]
- 54. Comparative analysis of milk bacteria by two MALDI-MS ... [https://www.nature.com/articles/s41598-025-21019-0]
- 55. Novel rapid method for identifying and quantifying ... [https://www.nature.com/articles/s41598-023-50864-0]
- 56. Comparison evaluation of bacterial DNA extraction ... [https://www.nature.com/articles/s41598-025-87225-y]
- 57. DNeasy Blood & Tissue Kits | DNA Purification [https://www.qiagen.com/us/products/discovery-and-translational-research/dna-rna-purification/dna-purification/genomic-dna/dneasy-blood-and-tissue-kit]
- 58. DNeasy 96 PowerSoil Pro Kit [https://www.qiagen.com/us/products/discovery-and-translational-research/dna-rna-purification/dna-purification/microbial-dna/dneasy-96-powersoil-pro-kit]
- 59. NucleoSpin Tissue, Mini kit for DNA from cells and tissue [https://www.mn-net.com/nucleospin-tissue-mini-kit-for-dna-from-cells-and-tissue-740952.50]
- 60. Performance Evaluation of Whole-Genome Amplification ... [https://pubmed.ncbi.nlm.nih.gov/41277018/?utm_source=FeedFetcher&utm_medium=rss&utm_campaign=None&utm_content=10MSL6XygFtCE0XpaQpog-pEt8342fXkY9lzrR7q6H0wVRyEa2&fc=None&ff=20251124065242&v=2.18.0.post22+67771e2]
- 61. Consumer Trends in cloned competent cells Market 2025- ... [https://www.datainsightsmarket.com/reports/cloned-competent-cells-1495254]
- 62. MediaMatch: Prediction of Bacterial Growth on Different ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12495271/]
- 63. Emerging strategies to enhance microbial natural product– ... [https://www.sciencedirect.com/science/article/pii/S0958166925001132]
- 64. DNA Amplification Kit Strategic Roadmap: Analysis and ... [https://www.archivemarketresearch.com/reports/dna-amplification-kit-293020]
- 65. Top DNA Cloning Kit Companies & How to Compare Them ... [https://www.linkedin.com/pulse/top-dna-cloning-kit-companies-how-compare-them-2025-iljvf/]
- 66. Top DNA Amplification Kit Companies & How to Compare ... [https://www.linkedin.com/pulse/top-dna-amplification-kit-companies-how-compare-them-efykf]
- 67. Comparative Assessment of Rapid Identification and ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12113830/]
- 68. An Alternative Approach to “Identification of Unknowns†[https://pmc.ncbi.nlm.nih.gov/articles/PMC4690567/]
- 69. Universal, untargeted detection of bacteria in tissues using ... [https://www.nature.com/articles/s41467-024-55457-7]
- 70. Biochemical ID Panels | Thermo Fisher Scientific - US [https://www.thermofisher.com/us/en/home/industrial/microbiology/microbial-identification/biochemical-identification/biochemical-id-panels.html]
- 71. Identification of clinical coryneform bacterial isolates: comparison of biochemical methods and sequence analysis of 16S rRNA and rpoB genes - PubMed [https://pubmed.ncbi.nlm.nih.gov/18160450/]
- 72. Comparison of six commercial kits to extract bacterial chromosome and plasmid DNA for MiSeq sequencing - PubMed [https://pubmed.ncbi.nlm.nih.gov/27312200/]
- 73. Bacterial Strains: Choosing the Right One for Research [https://bitesizebio.com/55858/bacterial-strains-for-lab/]
- 74. Recommendation and protocol compliance: “Yes, I do†may ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC7529399/]
- 75. Multicenter evaluation of fast multiplex PCR for detection ... [https://www.frontiersin.org/journals/cellular-and-infection-microbiology/articles/10.3389/fcimb.2025.1643991/full]
- 76. Analytical versus bioanalytical method validation [https://mpl.loesungsfabrik.de/en/english-blog/method-validation/analytical-vs-bioanalytical-method-validation]
- 77. Distinctions Between Analytical and Bioanalytical Test ... [https://www.bioprocessintl.com/bioanalytical-methods/distinctions-between-analytical-and-bioanalytical-test-methods]
- 78. What are the differences and key steps in Analytical ... [https://resources.eirgenix.com/blog/method_dev_qual_validation]
- 79. Bioanalytical method validation: An updated review - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC3658022/]
- 80. Presenting data in tables and charts - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC4008059/]
- 81. Scientific Data Presentation: a Picture Is Worth a Thousand ... [https://www.aje.com/arc/scientific-data-presentation-picture-worth-thousand-words]
- 82. Comparative evaluation of DNA extraction protocols for ... [https://www.sciencedirect.com/science/article/pii/S2950194625001669]
- 83. Top Microbial Analyzers Companies & How to Compare ... [https://www.linkedin.com/pulse/top-microbial-analyzers-companies-how-compare-them-rkcrc]
- 84. Microbial Identification Market Size, Share & Trends 2025- ... [https://www.futuremarketinsights.com/reports/microbial-identification-market]
- 85. A Central Requirement for New Test Methods [https://dcndx.com/insights/method-comparison-experiment-central-requirement-new-test-methods/]
- 86. Advances in Chemical and Biological Methods to Identify ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC6560418/]
- 87. A comprehensive quantitative LC-MS/MS method for rapid ... [https://www.sciencedirect.com/science/article/abs/pii/S096399692401682X]
- 88. Evaluation of seven commercial RTâ€PCR kits for COVIDâ€19 ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC7753435/]
- 89. An Instructor's Ultimate Assessment: The Bacterial ... [https://asm.org/articles/2016/august/teaching-microbiology-52]
- 90. Integrating LC-MS/MS proteomics with liquid biopsy platforms [https://pmc.ncbi.nlm.nih.gov/articles/PMC12358695/]
- 91. Review of Liquid Chromatography-Mass Spectrometry-Based ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC8878692/]
- 92. Multispecies Benchmark Analysis for LC-MS/MS Validation ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10845134/]
- 93. What are the Best Practices of LC-MS/MS Internal ... [https://www.nebiolab.com/what-are-the-best-practices-of-lc-ms-internal-standards/]
- 94. Sensitivity and specificity [https://en.wikipedia.org/wiki/Sensitivity_and_specificity]
- 95. Limit of Blank, Limit of Detection and Limit of Quantitation [https://pmc.ncbi.nlm.nih.gov/articles/PMC2556583/]
- 96. The Limit of Detection [https://www.chromatographyonline.com/view/limit-detection]
- 97. Sensitivity, Specificity, Positive Predictive Value, and ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC8156826/]
- 98. Comparison of Three Commercial ELISA Kits for Detection of ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12116064/]
- 99. Comparison of analytical sensitivity of SARS-CoV-2 ... [https://www.sciencedirect.com/science/article/pii/S1201971221006767]
- 100. A cost-effective method for the presumptive identification of ... [https://pubmed.ncbi.nlm.nih.gov/20350223/]
- 101. Cost-Effectiveness of Molecular Method Diagnostic for ... [https://www.sciencedirect.com/science/article/pii/S2212109921001163]
- 102. A preliminary evaluation of a fast, low-cost, and high ... [https://www.nature.com/articles/s41598-024-84682-9]
- 103. Understanding the Total Cost of Ownership(TCO) of Test ... [https://testrigor.com/blog/understanding-the-total-cost-of-ownershiptco-of-test-automation/]
- 104. What does TCO Look Like in Automation? A Practical ... [https://smart-robotics.io/total-cost-of-ownership-in-automation/]