Nutrient Gradients and Bacterial Persistence: Mechanisms, Models, and Therapeutic Targeting in Biofilms
This article synthesizes current research on how nutrient gradients within biofilms drive the formation of antibiotic-tolerant persister cells, a major cause of chronic and recurrent infections.
Nutrient Gradients and Bacterial Persistence: Mechanisms, Models, and Therapeutic Targeting in Biofilms
Abstract
This article synthesizes current research on how nutrient gradients within biofilms drive the formation of antibiotic-tolerant persister cells, a major cause of chronic and recurrent infections. It explores the foundational molecular mechanisms, including the stringent response and toxin-antitoxin systems, activated by nutrient limitation. The content details advanced methodological approaches, from experimental models to mathematical simulations, used to study these heterogeneous environments. Furthermore, it examines the challenges in eradicating persisters and evaluates emerging therapeutic strategies that target nutrient-driven persistence. Aimed at researchers and drug development professionals, this review provides a comprehensive framework for understanding and combating biofilm-associated treatment failures.
The Biofilm Environment: How Nutrient Gradients Create Persister Cell Sanctuaries
Architectural and Physiological Heterogeneity in Biofilms
Biofilms are structured microbial communities embedded in a self-produced extracellular polymeric substance (EPS) matrix, representing the predominant mode of bacterial life [1] [2]. Their architecture is not uniform but is characterized by profound spatial and physiological heterogeneity, which arises from the complex interplay between microbial metabolism and environmental gradients [3] [4]. This heterogeneity is a critical determinant of biofilm function, influencing everything from metabolic efficiency to resilience against antimicrobial agents.
Within the context of antimicrobial therapy failure, the relationship between nutrient gradients and the formation of antibiotic-tolerant persister cells is of paramount importance. As biofilms mature, the consumption of nutrients by cells in outer layers creates chemical gradients, leading to nutrient limitation in the biofilm interior [3] [4]. This spatial variation in resource availability drives the differentiation of subpopulations with distinct physiological states, including dormant persister cells that can survive antibiotic challenges and lead to chronic or recurrent infections [5] [6]. Understanding these dynamics is essential for developing effective strategies against biofilm-associated infections, particularly those involving medical implants where nutrient availability is often restricted.
Architectural Foundations of Biofilm Heterogeneity
Structural Composition and Matrix Architecture
The biofilm architecture is a complex, three-dimensional arrangement comprising microbial cells and a matrix of extracellular polymeric substances. The EPS matrix typically constitutes over 90% of the biofilm's dry mass, creating a cohesive environment that immobilizes cells and facilitates adhesion to surfaces [2]. This matrix is compositionally diverse, containing:
- Exopolysaccharides (e.g., alginate in Pseudomonas aeruginosa, polysaccharide intercellular adhesin in staphylococci) providing structural scaffolding [2]
- Extracellular DNA (eDNA) contributing to structural integrity and facilitating horizontal gene transfer [7]
- Proteins and enzymes functioning in nutrient acquisition and matrix remodeling [2]
- Lipids influencing hydrophobicity and barrier functions [7]
- Inorganic ions like calcium and magnesium that cross-link polymer networks [2]
The matrix is organized into two distinct layers: an outer loosely bound EPS (LB-EPS) layer with reduced adhesive capacity, and an inner tightly bound EPS (TB-EPS) layer where 97-98% of proteins are concentrated, creating a tightly packed environment around the cells [2].
Developmental Stages Establishing Heterogeneity
Biofilm formation progresses through defined developmental stages that establish the foundation for heterogeneity:
- Initial Reversible Attachment: Free-floating planktonic cells adhere to preconditioned surfaces through weak interactions (van der Waals forces, electrostatic interactions) and microbial structures like pili [1].
- Irreversible Attachment: Cells begin producing EPS, facilitating strong attachment and initiating microcolony formation [1].
- Maturation: Development of complex three-dimensional structures with characteristic architectural features like the honeycomb pattern observed in Pantoea sp. YR343 biofilms [8].
- Dispersion: Controlled release of cells from the biofilm to colonize new surfaces [1].
Table 1: Key Components of the Biofilm Extracellular Matrix
| Matrix Component | Primary Functions | Examples |
|---|---|---|
| Exopolysaccharides | Structural scaffolding, adhesion, protection | Alginate, Psl, Pel in P. aeruginosa; PIA in staphylococci [2] |
| Extracellular DNA (eDNA) | Structural cohesion, genetic exchange, immune activation | DNA from lysed cells [7] |
| Proteins & Enzymes | Structural integrity, nutrient processing, matrix degradation | Extracellular adhesion protein in S. aureus [9] |
| Lipids | Hydrophobicity, barrier function | Not specified in search results |
| Inorganic Ions | Polymer cross-linking, matrix stabilization | Calcium, magnesium ions [2] |
Gradient-Driven Physiological Heterogeneity
Resource Gradients and Metabolic Specialization
The three-dimensional architecture of biofilms impedes uniform diffusion of molecules, leading to the formation of physical and chemical gradients that serve as primary drivers of physiological heterogeneity [3] [4]. Oxygen, often the most critical gradient, typically decreases with depth from the biofilm surface, creating stratified microenvironments with distinct redox potentials [3]. This oxygenation gradient establishes a fundamental trend in microbial physiology, favoring aerobic metabolisms near the surface and anaerobic pathways in the interior regions.
These resource gradients promote metabolic differentiation and division-of-labor within the biofilm community [3]. For instance, in Escherichia coli biofilms, cells in the anoxic lower layers ferment glucose and produce acetate, which then diffuses upward to be consumed by aerobic cells in the oxic zone [3]. This cross-feeding optimizes resource utilization and enhances the overall fitness of the community. Similar metabolic cooperation occurs in oral biofilms, where early colonizers like Streptococcus spp. consume oxygen, creating anaerobic niches that support later colonizers including periodontal pathogens [7].
Metal Ion Gradients and Their Physiological Impact
Metal availability represents another crucial dimension of gradient-induced heterogeneity, significantly influencing biofilm development and function [9]. Bacteria have evolved sophisticated regulatory systems to maintain metal homeostasis, including metal-responsive transcriptional regulators like Fur (iron), Zur (zinc), and Mur (manganese) [9]. The host employs nutritional immunity, sequestering essential metals to limit bacterial growth, which in turn triggers adaptive responses in biofilms.
Table 2: Metal-Mediated Regulation of Biofilm Formation
| Metal | Regulatory System | Observed Effect on Biofilms | Example Organisms |
|---|---|---|---|
| Iron (Fe) | Fur (Ferric Uptake Regulator) | Iron limitation induces biofilm formation through increased secretion of adhesion proteins (Eap, Emp) [9] | Staphylococcus aureus, Pseudomonas aeruginosa [9] |
| Zinc (Zn) | Zur (Zinc Uptake Regulator) | Zinc-regulated biofilm formation [9] | Bacillus anthracis [9] |
| Manganese (Mn) | Mur (Manganese Uptake Regulator) | Manganese uptake regulates quorum sensing and biofilm formation [9] | Burkholderia cenocepacia, Enterococcus faecalis [9] |
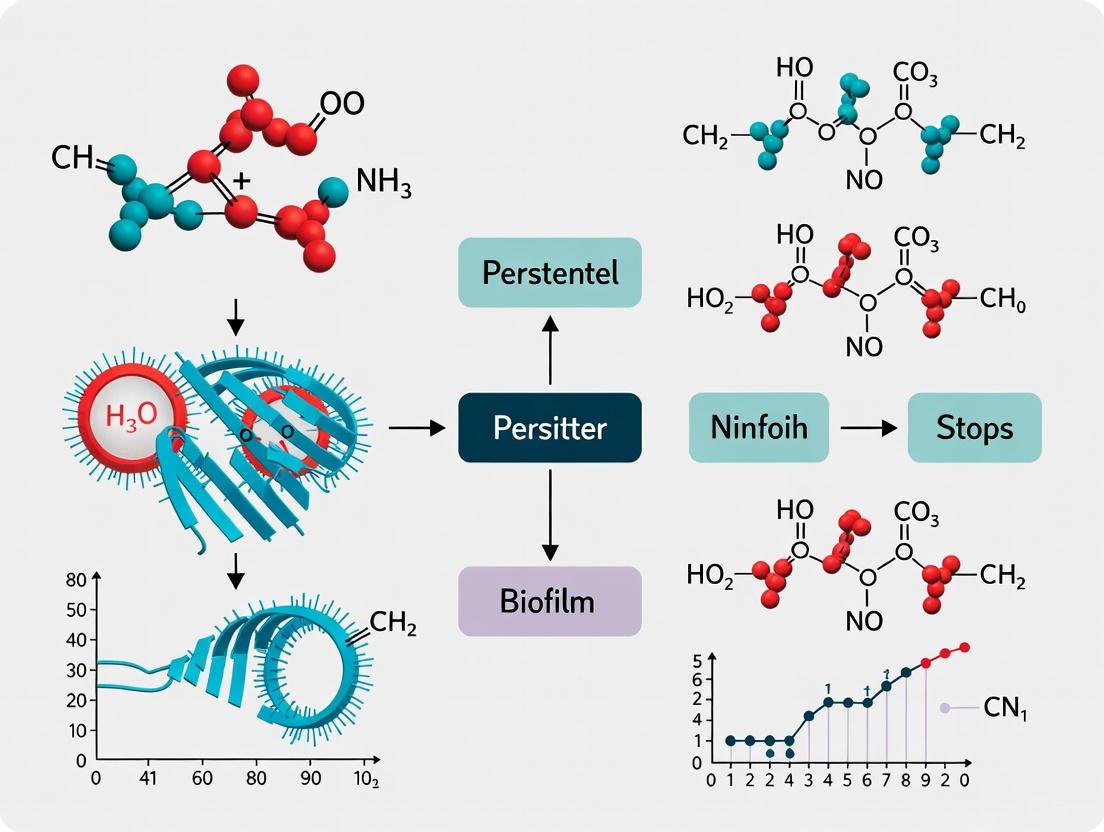
The following diagram illustrates how nutrient and metal gradients create heterogeneous microenvironments that drive physiological adaptations and persister cell formation within biofilms:
Mechanisms Linking Nutrient Gradients to Persister Formation
Physiological Basis of Persister Cells
Persisters represent a small subpopulation of bacterial cells that exhibit high tolerance to lethal doses of antibiotics without undergoing genetic resistance mutations [5]. This tolerance is non-heritable and reversible, distinguishing it from conventional antibiotic resistance. When antibiotic treatment ceases, persisters can resuscitate and regenerate a population with susceptibility profiles identical to the original one [5]. Biofilms are particularly effective at generating persisters, with frequencies 10 to 1000 times higher than observed in planktonic cultures [5].
The formation of persisters is closely linked to reduced metabolic activity and dormancy states. Since most antibiotics target active cellular processes like cell wall synthesis, protein production, and DNA replication, slowing or halting these processes provides a protective effect [5] [4]. In biofilms, nutrient gradients naturally create heterogeneous metabolic conditions, with cells in nutrient-deprived regions transitioning toward dormancy and consequently developing increased antibiotic tolerance [5] [6].
Molecular Mechanisms of Persistence
Multiple molecular mechanisms contribute to persister formation in response to nutrient gradients:
- Toxin-Antitoxin (TA) Modules: These systems consist of stable toxins and unstable antitoxins. Under stress conditions, antitoxins are degraded, freeing toxins to inhibit essential processes like DNA replication and protein translation, inducing dormancy [5].
- Stringent Response: Nutrient limitation triggers (p)ppGpp signaling, which reprograms cellular metabolism away from growth and toward maintenance, promoting persistence [5].
- Stress Response Systems: DNA damage (SOS response) and oxidative stress responses activate protective mechanisms that can contribute to antibiotic tolerance [5].
- Efflux Pumps: Enhanced drug efflux activity can reduce intracellular antibiotic concentrations, though this mechanism is more associated with resistance than tolerance [5].
- Quorum Sensing: Cell-to-cell communication systems regulate collective behaviors and can influence persister formation through population-dependent signaling [5].
The following diagram illustrates the molecular pathways through which nutrient limitation triggers persister cell formation:
Experimental Methodologies for Studying Biofilm Heterogeneity
Advanced Imaging Techniques
Understanding biofilm heterogeneity requires methodologies capable of resolving structural and physiological variations across multiple spatial scales:
- Large Area Automated Atomic Force Microscopy (AFM): This technique enables high-resolution imaging over millimeter-scale areas, capturing spatial heterogeneity and cellular morphology during early biofilm formation. Automated scanning with machine learning-assisted image stitching allows visualization of features like flagellar coordination and honeycomb patterning in Pantoea sp. YR343 biofilms [8].
- Confocal Laser Scanning Microscopy (CLSM): Provides three-dimensional imaging of biofilm architecture while preserving native structure. When combined with fluorescent staining, it reveals different microbial species occupying distinct ecological niches and the spatial organization of metabolic activity [7].
- Microfluidics with Single-Cell Microscopy: Custom microfluidic devices enable precise control of nutrient fluctuations while monitoring individual cell growth. This approach revealed that E. coli exhibits a distinct "fluctuation-adapted" physiology that enhances growth under rapid nutrient changes compared to predictions from steady-state models [10].
Molecular and Analytical Approaches
- Metabolic Flux Analysis: Using techniques like 13C metabolic flux analysis, researchers can track nutrient utilization pathways in different biofilm regions, revealing cross-feeding interactions such as acetate production in anaerobic zones and consumption in aerobic regions [3].
- Transcriptomics and Proteomics: These methods identify gene expression and protein production patterns across biofilm subpopulations, highlighting physiological adaptations to local microenvironments [4].
- Mathematical Modeling: Continuum models that couple nutrient transport with dynamics of proliferative bacteria, persisters, and EPS matrix components provide theoretical frameworks for understanding how nutrient availability controls the balance between active growth and dormancy [6].
Table 3: Methodologies for Analyzing Biofilm Heterogeneity
| Methodology | Key Applications | Technical Advantages | Limitations |
|---|---|---|---|
| Large Area Automated AFM | Nanoscale topography, cellular morphology, flagellar interactions [8] | High resolution under physiological conditions; nanomechanical property mapping [8] | Limited to surface features; requires specialized equipment and analysis [8] |
| Confocal Laser Scanning Microscopy | 3D architecture, spatial organization, species distribution [7] | Non-destructive optical sectioning; compatible with live-cell imaging and fluorescent probes [7] | Resolution limited by light diffraction; potential phototoxicity [7] |
| Microfluidics with Single-Cell Analysis | Growth dynamics under controlled nutrient fluctuations, physiological heterogeneity [10] | Precise environmental control; high-temporal resolution; single-cell data [10] | Technical complexity; potential surface effects on cell behavior [10] |
| Mathematical Modeling | Prediction of persister dynamics, nutrient gradient effects, treatment outcomes [6] | Integrates complex processes; enables hypothesis testing and prediction [6] | Requires parameterization and validation; simplifications may limit biological accuracy [6] |
The Scientist's Toolkit: Key Research Reagents and Materials
Table 4: Essential Research Reagents and Materials for Biofilm Heterogeneity Studies
| Reagent/Material | Function/Application | Specific Examples |
|---|---|---|
| PFOTS-Treated Glass Surfaces | Controlled hydrophobic surfaces for studying initial attachment dynamics [8] | Used in AFM studies of Pantoea sp. YR343 biofilm assembly [8] |
| Custom Microfluidic Devices | Precise control of nutrient fluctuations with single-cell imaging capability [10] | PDMS devices for E. coli growth under minute-scale nutrient oscillations [10] |
| Fluorescent Stains and Probes | Visualization of live/dead cells, metabolic activity, and specific matrix components | SYTO dyes for nucleic acids, FITC-conjugated lectins for polysaccharides [7] |
| Metal Chelators | Investigation of metal limitation effects on biofilm formation and physiology | Iron chelators inducing slime production in S. epidermidis [9] |
| Specific Nutrient Media | Creating defined nutritional environments and gradients | LB media at varying concentrations (0.1%-2%) for fluctuation experiments [10] |
| Atomic Force Microscopy Probes | High-resolution topographical imaging and nanomechanical measurements | Sharp silicon tips for visualizing bacterial flagella and EPS matrix [8] |
| Quorum Sensing Inhibitors | Interruption of cell-cell communication to study its role in heterogeneity | AHL analogs for blocking quorum sensing in Gram-negative bacteria [7] |
| MI-503 | MI-503, MF:C28H27F3N8S, MW:564.6 g/mol | Chemical Reagent |
| Mimopezil | Mimopezil, CAS:180694-97-7, MF:C23H23ClN2O3, MW:410.9 g/mol | Chemical Reagent |
Architectural and physiological heterogeneity in biofilms represents a fundamental survival strategy that emerges from the interaction between microbial communities and their spatially structured environments. The nutrient gradients that develop within biofilms directly drive the formation of metabolically diverse subpopulations, including antibiotic-tolerant persister cells that contribute to therapeutic failure and chronic infections. Understanding these relationships requires sophisticated methodological approaches that span from nanoscale imaging to computational modeling.
The implications of this heterogeneity extend significantly to clinical practice, particularly in the context of medical device-related infections where nutrient limitations are common. Traditional antibiotic therapies often fail because they primarily target metabolically active cells while overlooking the dormant persister populations that reside in nutrient-deprived regions of biofilms. Future therapeutic strategies may need to consider manipulating nutrient availability or targeting the molecular mechanisms that drive persistence to achieve more effective biofilm control. As research continues to unravel the complex relationships between gradient-driven heterogeneity and treatment outcomes, new opportunities will emerge for combating persistent biofilm-associated infections.
Spatial Gradients of Carbon, Oxygen, and Metabolites
In the structured environment of a microbial biofilm, the consumption of nutrients and oxygen by surface-layer cells creates chemical gradients that penetrate the depths of the community. These spatial gradients of carbon, oxygen, and metabolites are not merely a consequence of biofilm growth; they are fundamental organizers of microbial physiology and a critical driving force behind the formation of antibiotic-tolerant persister cells [3] [5]. This phenomenon presents a major challenge in treating chronic infections, as these dormant, tolerant cells are responsible for relapse and therapeutic failure [11] [5].
Understanding the mechanisms of gradient formation and their physiological consequences is essential for developing novel anti-biofilm strategies. This guide provides a technical overview of the principles, measurement methodologies, and implications of chemical gradients within biofilms, with a specific focus on their role in fostering bacterial persistence.
The Formation and Architecture of Biofilm Gradients
Fundamentals of Gradient Formation
Biofilms are structured as complex, three-dimensional communities encased in an extracellular polymeric substance (EPS) matrix. This matrix, composed of exopolysaccharides, proteins, and extracellular DNA, acts as a diffusion barrier, significantly hindering the free movement of molecules [3] [12]. The combination of this physical barrier and the collective metabolic activity of the microbial population establishes steep chemical gradients from the biofilm-fluid interface to the substratum.
- Oxygen Gradients: Oxygen, often the most rapidly consumed substrate, is typically depleted within the first few tens to hundreds of micrometers from the biofilm surface [3]. This creates distinct aerobic, microaerophilic, and anaerobic zones.
- Carbon and Nutrient Gradients: The availability of carbon sources and other nutrients decreases with depth, as they are consumed by cells in outer layers [3] [13].
- Metabolite Gradients: Waste products and metabolic by-products (e.g., organic acids, fermentation products) accumulate in the biofilm interior, creating additional environmental stresses [3].
The diagram below illustrates the structural and chemical heterogeneity within a mature biofilm.
Physiological Heterogeneity and Metabolic Stratification
Spatial gradients create a patchwork of microenvironments with distinct physiological states. This heterogeneity is a key survival strategy, allowing the biofilm community to utilize resources efficiently through a division-of-labor [3].
A classic example is metabolic cross-feeding in Escherichia coli biofilms. Cells in the anoxic lower layers ferment glucose and produce acetate. This acetate then diffuses upwards and serves as a carbon source for aerobic cells in the oxic zone of the biofilm [3]. This functional stratification optimizes energy production and biomass yield from the available substrates.
Quantitative Characterization of Gradients
The specific physical and chemical properties of a biofilm's environment directly influence the steepness and impact of these gradients. The table below summarizes key parameters and their quantitative effects.
Table 1: Key Parameters Influencing Biofilm Gradient Formation and Metabolic Activity
| Parameter | Impact on Gradients & Metabolism | Experimental Evidence |
|---|---|---|
| Specific Surface Area | Non-linear impact on carbon metabolic rate; mass transfer limitations can cause activity to peak at a threshold (e.g., 5000-7500 m²/m³) and then decline [14]. | Study using carriers with different specific surface areas (1,900 - 12,500 m²/m³) incubated in lakes; metabolic activity measured via BIOLOG ECO microplates [14]. |
| Oxygen Concentration | Primary determinant of overall chemistry and microbial physiology; creates zones with distinct electron acceptors [3] [15]. | Metagenomic data from Baltic Sea sediments showed oxygen and salinity as the main drivers of functional gene composition [15]. |
| Carbon Source Transition | Diauxic shifts (e.g., glucose to acetate) stimulate persister formation via a ppGpp-dependent pathway [13]. | Colony biofilm assays on membranes; persisters enumerated after ofloxacin/ampicillin exposure pre- and post-glucose exhaustion [13]. |
| Carrier C:N Ratio | Correlates with diversity of nutrient transport and carbon metabolism genes in benthic environments [15]. | Large-scale spatial correlation of sediment C/N ratio with metagenomic functional profiles [15]. |
| Nutrient Limitation | Directly induces dormancy; also causes time-dependent growth arrest, indirectly increasing persistence [16]. | Individual-based modeling (IbM) simulating nutrient, oxygen, and time-dependent dormancy mechanisms [16]. |
Methodologies for Studying Gradients and Persistence
Investigating the relationship between spatial gradients and persister formation requires a combination of sophisticated techniques. The following workflow outlines an integrated experimental approach.
Experimental Protocols
Carbon Source Transition Assay in Colony Biofilms
This protocol is designed to directly test the effect of nutrient shifts on persister formation within a biofilm structure [13].
- Biofilm Growth: Grow E. coli colony biofilms on polyethersulfone (PES) membranes placed on M9 minimal agar plates containing a primary carbon source (e.g., 10-60 mM glucose).
- Monitor Growth: Aseptically remove membranes at intervals, vortex in PBS, and measure OD₆₀₀ to track growth. Exhaustion of the primary carbon source is indicated by a plateau in OD.
- Induce Transition: At specific time points before and after carbon source exhaustion, samples are taken for persister enumeration.
- Persister Measurement: Resuspend biofilm cells from membranes and expose to a high concentration of a fluoroquinolone (e.g., 10 μg/mL ofloxacin) or a β-lactam (e.g., 750 μg/mL ampicillin) for 5 hours.
- Enumeration: Serially dilute the antibiotic-treated suspension and spot on LB agar plates. Count colony-forming units (CFU) after incubation. Persisters are the cells that survive this antibiotic exposure.
Metabolic Activity Profiling via BIOLOG ECO Microplates
This method assesses the functional metabolic diversity of biofilms grown under different conditions, such as on carriers with varying specific surface areas [14].
- Biofilm Collection and Homogenization: Separate biofilm from its carrier via ultrasonic oscillation and suspend in sterile physiological saline (0.85% NaCl).
- Standardization: Dilute the biofilm suspension until the optical density at 590 nm (OD₅₉₀) reaches 0.05.
- Inoculation and Incubation: Transfer 150 μL of the standardized suspension into each well of a BIOLOG ECO microplate, which contains 31 different carbon sources and a control well. Incubate at 25°C in the dark for up to 7 days.
- Data Acquisition: Measure the OD₅₉₀ of each well every 12-24 hours using a microplate reader.
- Data Analysis:
- Calculate the Average Well Color Development (AWCD) for each plate:
AWCD = Σ(Ci - R) / n, whereCiis the absorbance of a sample well,Ris the absorbance of the control well, andnis the number of substrates (31). - Fit the AWCD over time to a logistic growth curve to model metabolic activity kinetics.
- Calculate diversity indices like the Shannon-Wiener index (H') to assess the community's metabolic versatility.
- Calculate the Average Well Color Development (AWCD) for each plate:
The Scientist's Toolkit: Research Reagent Solutions
The following table details essential materials and their applications in biofilm gradient and persister research.
Table 2: Essential Research Reagents and Tools for Biofilm Gradient Studies
| Reagent / Tool | Function & Application | Key Characteristics |
|---|---|---|
| BIOLOG ECO Microplates | Community-level physiological profiling; measures carbon source utilization potential of a biofilm community [14]. | Contains 31 different carbon sources; tetrazolium dye color change indicates metabolic activity. |
| Polyethersulfone (PES) Membranes | Support surface for growing colony biofilms, allowing controlled nutrient delivery from underlying agar [13]. | 0.2 μm pore size, 25 mm diameter; inert and non-degradable. |
| M9 Minimal Salts Agar | Defined medium for biofilm growth, essential for conducting controlled carbon transition experiments [13]. | Allows precise control over carbon source type and concentration. |
| Confocal Laser Scanning Microscope (CLSM) | Non-invasive, real-time 3D visualization of biofilm architecture, cell viability, and spatial organization using fluorescent tags [7] [12]. | Enables optical sectioning of live biofilms without disruption. |
| Atomic Force Microscope (AFM) | Provides nanomechanical data (adhesion, elasticity) of biofilm surfaces and single cells [12]. | Can operate in liquid environments, providing physiologically relevant data. |
| Microfluidic Devices | Simulates dynamic fluid flow and nutrient conditions; allows high-resolution study of biofilm heterogeneity and antimicrobial penetration [16] [12]. | Enables precise environmental control and real-time imaging. |
| CRISPR-Cas9 / CRISPRi | Targeted gene editing (knockout) or interference (knockdown) to investigate function of specific genes in persistence (e.g., TA modules, ppGpp synthases) [11] [12]. | Provides precise molecular tools for mechanistic studies. |
| Minocycline hydrochloride | Minocycline Hydrochloride | High-purity Minocycline Hydrochloride for research. Explore its antibiotic and non-antibiotic mechanisms in biomedical studies. For Research Use Only. Not for human consumption. |
| Mirogabalin Besylate | Mirogabalin Besylate|High-Purity α2δ Ligand | Mirogabalin besylate is a novel, selective α2δ ligand for neuropathic pain research. This product is For Research Use Only. Not for human or veterinary diagnostic or therapeutic use. |
Connecting Gradients to Persister Cell Formation
The heterogeneous microenvironments created by spatial gradients are a primary source of persister cells in biofilms. The following diagram synthesizes the major mechanisms linking these gradients to phenotypic tolerance.
Key Mechanistic Insights
- Nutrient Transitions as a Trigger: The shift from a preferred carbon source (like glucose) to a secondary one (like acetate) as it is depleted in the biofilm is a potent stimulus for persister formation. This diauxic transition activates the stringent response via the signaling molecule (p)ppGpp, which orchestrates a massive reprogramming of cellular metabolism towards a dormant, tolerant state [13].
- Dormancy and Active Tolerance: A prevailing hypothesis is that gradient-driven starvation pushes cells into a dormant state with drastically reduced growth and metabolic activity, rendering them insensitive to antibiotics that target active cellular processes [11] [5]. However, persistence is not synonymous with dormancy. Active mechanisms, such as efflux pumps and stress responses (e.g., oxidative stress response), also contribute to tolerance in biofilm subpopulations [5].
- The Role of Toxin-Antitoxin (TA) Modules: Under stress conditions, degradation of labile antitoxins leads to the release of free toxins. These toxins can disrupt essential processes like translation and replication, thereby inducing a dormant state that is a hallmark of many persister cells [11] [5].
Spatial gradients of carbon, oxygen, and metabolites are non-genetic, self-organizing principles that generate phenotypic heterogeneity and antibiotic tolerance in biofilms. The deep, nutrient-limited, and anaerobic zones of a biofilm serve as reservoirs for dormant persister cells, which are largely responsible for the recalcitrance of chronic infections.
Future research and therapeutic development must move beyond traditional antimicrobials that target growing cells. Effective strategies will require a dual approach: first, disrupting the gradient structure itself, perhaps by enhancing diffusion or applying metabolic inhibitors that target multiple physiological states simultaneously; and second, directly eradicating the persister subpopulation by exploiting their unique physiology, such as their low metabolic state or specific stress pathways. A deep, quantitative understanding of biofilm gradients is therefore not just an academic pursuit but a critical pathway to overcoming one of the most significant challenges in modern infectious disease management.
The stringent response, a universal bacterial stress adaptation mechanism, is orchestrated by the signaling molecules guanosine tetraphosphate and pentaphosphate, collectively known as (p)ppGpp. This master regulator extensively rewires bacterial physiology by reprogramming transcriptional networks and cellular metabolic processes. Within structured biofilm communities, nutrient gradients create heterogeneous microenvironments that trigger (p)ppGpp accumulation, leading to bacterial growth arrest and promoting the formation of antibiotic-tolerant persister cells. This technical review examines the core molecular mechanisms of (p)ppGpp signaling, with particular emphasis on its role as a critical mediator connecting nutrient limitation to persister formation in biofilms—a key driver of chronic and recurrent infections. We synthesize current experimental evidence, quantitative relationships, and methodological approaches to provide researchers with a comprehensive framework for investigating this fundamental bacterial survival pathway.
The stringent response represents one of the most crucial global regulatory systems in bacteria, enabling rapid adaptation to environmental stresses, particularly nutrient limitation. Central to this response are the hyperphosphorylated guanosine nucleotides ppGpp (guanosine pentaphosphate) and pppGpp (guanosine tetraphosphate), collectively termed (p)ppGpp and historically known as "magic spot". These signaling molecules function as bacterial alarmones that coordinate cellular physiology by redirecting resources from proliferation to maintenance and survival [17].
In clinical contexts, (p)ppGpp signaling gains particular significance due to its direct involvement in bacterial pathogenesis, host invasion, and antibiotic tolerance [17]. The stringent response is activated not only during nutrient starvation but also in response to diverse environmental cues including oxygen variation, pH downshift, osmotic shock, temperature shift, and even light exposure in phototrophic bacteria [17]. This versatile signaling system enables bacterial pathogens to withstand antibiotic therapy and establish persistent infections, making it a compelling target for novel antimicrobial strategies.
Molecular Mechanisms of (p)ppGpp Synthesis and Regulation
Enzymatic Control of (p)ppGpp Homeostasis
Cellular (p)ppGpp levels are primarily regulated by enzymes belonging to the RelA/SpoT homolog (RSH) family, which are highly conserved across bacterial species [17]. These enzymes can be categorized based on their domain architecture and functional capabilities:
- Long RSH enzymes: Bifunctional proteins containing both synthetase and hydrolase domains. In Gamma-proteobacteria like Escherichia coli, this function is divided between RelA (primarily synthetase activity) and SpoT (weak synthetase but strong hydrolase activity) [17] [18].
- Short RSH enzymes: Monofunctional enzymes including small alarmone synthetases (SAS) and small alarmone hydrolases (SAH) that provide additional regulatory layers in certain bacterial species [17].
The regulation of (p)ppGpp synthesis is triggered by specific environmental stimuli. RelA is activated by uncharged tRNA molecules that accumulate during amino acid starvation, while SpoT responds to diverse stresses including fatty acid limitation, carbon starvation, and oxidative stress [17] [19].
Table 1: Enzymatic Regulators of (p)ppGpp Homeostasis Across Bacterial Species
| Enzyme | Organism Type | Primary Function | Activating Signals |
|---|---|---|---|
| RelA | Gamma-proteobacteria | (p)ppGpp synthesis | Uncharged tRNA (amino acid starvation) |
| SpoT | Gamma-proteobacteria | (p)ppGpp hydrolysis (primary); weak synthesis | Fatty acid limitation, carbon starvation, oxidative stress |
| Rel | Gram-positive bacteria, Mycobacteria | Bifunctional (synthesis and hydrolysis) | Multiple nutrient stresses |
| SAS (Small Alarmone Synthetases) | Various bacteria | (p)ppGpp synthesis | Specialized environmental cues |
| SAH (Small Alarmone Hydrolases) | Various bacteria | (p)ppGpp hydrolysis | Cellular (p)ppGpp concentration |
Molecular Effectors and Transcriptional Reprogramming
(p)ppGpp exerts its profound physiological effects through direct interactions with key cellular targets:
- RNA polymerase (RNAP): In Gammaproteobacteria, (p)ppGpp binds directly to the RNAP, often with its cofactor DksA, to differentially regulate transcription. This binding induces allosteric changes that inhibit stable RNA synthesis while activating amino acid biosynthesis and stress response genes [19] [18].
- Transcription factors: (p)ppGpp can modulate the activity of various transcription factors, including the GTP-sensing regulator CodY, thereby indirectly influencing gene expression [18].
- Metabolic enzymes: Direct inhibition of enzymes involved in nucleotide synthesis (e.g., DNA primase) and other central metabolic processes [17].
The diagram below illustrates the core (p)ppGpp signaling pathway and its physiological outcomes:
Quantitative Relationships in (p)ppGpp Signaling
Graded Nature of the Stringent Response
Recent research has revealed that the stringent response operates not as a binary on/off switch but as a graded system where (p)ppGpp accumulation and transcriptional responses are proportional to stress severity [19]. This continuum model explains how bacteria can fine-tune their adaptation to varying degrees of nutrient limitation.
Table 2: Dose-Dependent Effects of (p)ppGpp Accumulation in Pseudomonas aeruginosa PA14
| SHX Concentration | Stringent Response Level | (p)ppGpp Increase (Fold) | Growth Rate (Doublings/Hour) | Differentially Expressed Genes |
|---|---|---|---|---|
| 100 µM | Mild | 1.33x | 0.40 | 227 (~4% of genome) |
| 500 µM | Intermediate | 1.39x | 0.26 | 1,197 (~20% of genome) |
| 1000 µM | Acute | 1.48x | Severe perturbation | 1,508 (~25% of genome) |
The quantitative relationship between (p)ppGpp levels and growth rate follows a strong negative correlation (R² = 0.95), demonstrating the precision of this regulatory system [19]. Transcriptomic analysis reveals that increasing (p)ppGpp concentrations engage cellular processes in a layer-by-layer manner, with more severe stress conditions recruiting additional genes into the response network [19].
Phenotypic Outcomes of (p)ppGpp Signaling
The functional consequences of (p)ppGpp accumulation manifest differently across bacterial species and environmental contexts:
Table 3: Phenotypic Consequences of (p)ppGpp Signaling Across Bacterial Species
| Bacterial Species | Phenotypic Outcomes | Relationship to Persistence |
|---|---|---|
| Escherichia coli | Inhibition of DNA replication; Multidrug tolerance in biofilms; Transient growth arrest | Direct role in persister formation during nutrient transitions [17] [13] |
| Pseudomonas aeruginosa | Dose-dependent motility suppression; Enhanced biofilm formation; Antibiotic tolerance | Promotes antimicrobial tolerance under biofilm conditions [19] |
| Yersinia enterocolitica | Copositive regulation with DksA for motility, antibiotic resistance, oxidative stress tolerance | Synergistic actions with other regulators in persistence [18] |
| Clavibacter michiganensis | Reduced ribosomal gene expression; Enhanced biofilm synthesis; Increased production of cell-wall degrading enzymes | Mediates virulence and survival in host environment [20] |
| Pseudomonas putida | Stimulation of biofilm dispersal under nutrient limitation | Coordinates exit from biofilm lifestyle [21] |
Methodologies for Investigating (p)ppGpp-Dependent Persister Formation
Experimental Induction of Stringent Response
Researchers have developed multiple approaches to induce and study (p)ppGpp-mediated persister formation:
Serine Hydroxamate (SHX) Treatment
- Principle: SHX is a serine analog that inhibits seryl-tRNA synthetase, causing accumulation of uncharged tRNA and activating RelA-dependent (p)ppGpp synthesis [19].
- Protocol:
- Grow P. aeruginosa PA14 cultures to exponential phase (OD₆₀₀ ~0.2-0.4)
- Add SHX at concentrations ranging from 10-1000 µM to induce varying stringent response levels
- Incubate for 30 minutes at growth temperature
- Measure (p)ppGpp accumulation via thin-layer chromatography or HPLC
- Assess persister levels by antibiotic challenge assays
- Applications: Ideal for studying dose-dependent effects of (p)ppGpp on transcriptomics and persister formation [19].
Temperature-Sensitive valS Allele System
- Principle: Utilizing a temperature-sensitive valyl-tRNA synthetase (valSts) to controllably induce tRNA charging limitation and (p)ppGpp accumulation [22].
- Protocol:
- Grow E. coli MG1655valSts at permissive temperature (30°C)
- Shift to semi-permissive temperature (36.6-37°C) to partially inactivate ValS
- Monitor ppGpp levels over time (peaks at ~10 minutes post-shift)
- Assess persister frequency by antibiotic challenge at different time points
- Applications: Enables single-cell analysis of persister formation, survival, and resuscitation using live microscopy [22].
Carbon Source Transition Model
- Principle: Diauxic shifts between preferred and secondary carbon sources naturally induce (p)ppGpp accumulation and persister formation [13].
- Protocol:
- Grow E. coli colony biofilms on membranes placed on M9 minimal agar with primary carbon source
- Monitor growth until near-exhaustion of primary carbon source (FCOD₆₀₀ ~30)
- Verify carbon source depletion with glucose assay kits
- Measure persister levels before and after carbon source exhaustion
- Compare with relA/spoT mutants to confirm (p)ppGpp dependence
- Applications: Models nutrient gradient effects in biofilms; identifies persister formation pathways relevant to in vivo conditions [13].
The experimental workflow for studying nutrient transition-induced persistence is illustrated below:
The Scientist's Toolkit: Essential Research Reagents
Table 4: Key Reagents for Investigating (p)ppGpp-Dependent Persister Formation
| Reagent/Condition | Function/Application | Example Usage |
|---|---|---|
| Serine Hydroxamate (SHX) | Chemical inducer of amino acid starvation | Dose-dependent induction of stringent response [19] |
| valSts (temperature-sensitive valS) | Genetic system for controlled tRNA charging limitation | Single-cell analysis of persister formation dynamics [22] |
| Colony biofilm system with PES membranes | Controlled nutrient delivery and transition studies | Modeling nutrient gradient effects in biofilms [13] |
| relA/spoT deletion mutants | Genetic dissection of (p)ppGpp synthesis pathways | Determining pathway specificity in persister formation [17] [13] |
| RpoS-mCherry fusion | Fluorescent reporter for (p)ppGpp activation | Single-cell tracking of stringent response activation [22] |
| QUEEN-7µ ATP sensor | FRET-based ATP concentration measurement | Correlating metabolic state with persistence [22] |
| TA promoter-YFPunstable fusions | Reporter for toxin-antitoxin system activation | Monitoring stochastic TA activation in single cells [22] |
| HPLC / TLC methods | Quantitative (p)ppGpp measurement | Precise quantification of alarmone levels [19] |
| Mivebresib | Mivebresib, CAS:1445993-26-9, MF:C22H19F2N3O4S, MW:459.5 g/mol | Chemical Reagent |
| Setileuton tosylate | Setileuton tosylate, CAS:1137737-87-1, MF:C29H25F4N3O7S, MW:635.6 g/mol | Chemical Reagent |
(p)ppGpp in Biofilm Persistence and Therapeutic Implications
Nutrient Gradients and Heterogeneous Persister Formation
Within biofilms, nutrient availability follows spatial gradients that create heterogeneous microenvironments. Cells in nutrient-depleted regions experience stress conditions that trigger (p)ppGpp accumulation, leading to heterogeneous persister formation throughout the biofilm structure [17] [6]. Mathematical modeling confirms that nutrient limitation produces a high and sustained proportion of persister cells even when overall biomass is reduced, whereas nutrient-rich conditions support reversion to proliferative growth [6].
The (p)ppGpp-mediated persister formation in biofilms involves coordinated regulation of multiple cellular processes:
- Metabolic reprogramming: Downregulation of energy-intensive processes including ribosome biogenesis, nucleotide synthesis, and oxidative phosphorylation [19]
- Toxin-antitoxin system modulation: Activation of specific TA modules that promote dormancy in subpopulations of cells [17] [23]
- Cell envelope modifications: Changes in membrane permeability and transport systems that reduce antibiotic uptake [17]
- DNA supercoiling regulation: Inhibition of DNA gyrase leading to reduced DNA replication and transcription [17]
Interplay with Other Persistence Mechanisms
(p)ppGpp does not function in isolation but interacts with multiple cellular pathways to regulate persistence. Research in E. coli has revealed complex genetic interactions between (p)ppGpp and 15 known persister genes, which can be categorized into five relationship types: dependent, positive reinforcement, antagonistic, epistasis, and irrelevant [23]. These interactions are further modulated by bacterial culture age, antibiotic class, and cell concentration, highlighting the contextual nature of persistence mechanisms.
Notably, the relationship between (p)ppGpp and persistence is not always straightforward. Single-cell studies have demonstrated that while high population-level (p)ppGpp correlates with increased persister frequencies, there is no direct correlation between (p)ppGpp levels and antibiotic tolerance at the single-cell level, emphasizing the importance of stochasticity in persister formation [22].
Therapeutic Perspectives and Targeting Strategies
The central role of (p)ppGpp in bacterial persistence makes it an attractive target for novel therapeutic interventions. Several strategic approaches have emerged:
- Direct (p)ppGpp synthesis inhibitors: Small molecules that target RelA/SpoT enzymes to prevent alarmone accumulation during stress [17]
- Stringent response disruptors: Compounds that interfere with (p)ppGpp-RNAP interactions or downstream signaling events [17]
- Combination therapies: Anti-persister agents that target (p)ppGpp-mediated pathways alongside conventional antibiotics [11]
- Nutrient modulation approaches: Strategies that manipulate environmental conditions to prevent persistent state induction [6]
Recent evidence suggests that targeting (p)ppGpp signaling may enhance the efficacy of conventional antibiotics against biofilm-associated infections, potentially addressing the clinical challenge of chronic and recurrent infections [17] [11]. As our understanding of the nuanced role of (p)ppGpp in bacterial pathogenesis continues to evolve, so too will opportunities for therapeutic intervention in persistent infections.
The Role of Toxin-Antitoxin (TA) Modules in Stress-Induced Dormancy
Toxin-antitoxin (TA) systems are genetic elements ubiquitous in bacteria and archaea, functioning as sophisticated stress-responsive survival circuits. This review delves into the molecular mechanisms of type II TA modules, emphasizing their critical role in inducing bacterial dormancy and antibiotic tolerance, particularly within the nutrient-graded environments of biofilms. Within biofilms, heterogenous nutrient distribution creates micro-niches that actively trigger TA systems, leading to a dormant, persister subpopulation responsible for chronic infections and therapeutic failures. We synthesize current understanding of TA system operation, present quantitative data on their distribution and function, and provide detailed methodologies for their study. The focus on biofilm nutrient gradients provides a critical context for understanding persister formation, offering insights for developing novel anti-persister therapeutic strategies.
Toxin-antitoxin (TA) systems are genetic modules composed of a stable toxin protein and a labile antitoxin (a protein or RNA) that neutralizes the toxin under normal growth conditions [24]. Under stress conditions, such as nutrient limitation, antibiotic exposure, or oxidative stress, the antitoxin is rapidly degraded, freeing the toxin to act on its cellular target and induce a state of growth arrest and dormancy [5]. This physiological state is characterized by a drastic reduction in metabolism, protecting the bacterial cell from stressors that typically target active cellular processes.
This stress-induced dormancy is intrinsically linked to the formation of bacterial persisters—a small subpopulation of genetically susceptible cells that exhibit multidrug tolerance without acquired resistance [11] [25]. Persisters are phenotypically variant, non-growing, or slow-growing cells that can survive high doses of antibiotics and regrow once the antibiotic pressure is removed, leading to recurrent and chronic infections [11] [5]. The ability of TA systems to orchestrate this reversible dormancy positions them as a cornerstone of bacterial persistence, especially in structured environments like biofilms where stress gradients are common.
Classification and Molecular Mechanisms of Type II TA Systems
Among the various types of TA systems, type II is the most well-characterized class. These systems are defined by proteinaceous toxins and antitoxins that form a stable complex. Under normal conditions, the antitoxin binds to and neutralizes the toxin. Environmental stressors trigger the degradation of the antitoxin by specific proteases, unleashing the toxin to act on its target [24].
The table below summarizes the primary functional targets and roles of key type II TA systems implicated in bacterial persistence.
Table 1: Key Type II Toxin-Antitoxin Systems and Their Functions
| TA System | Toxin Target & Mechanism | Primary Role in Persistence | Representative Organisms |
|---|---|---|---|
| VapBC | Ribonuclease activity; inhibits protein synthesis [26] | Dormancy induction, stress response, biofilm formation [24] [26] | Mycobacterium tuberculosis, M. bovis [26] |
| MazEF | Ribonuclease activity; cleaves cellular mRNA [24] | Dormancy induction, programmed cell death [24] | E. coli, M. tuberculosis [24] |
| RelBE | Ribonuclease activity; inhibits protein translation [24] | Dormancy induction, stringent response [24] | E. coli, numerous pathogens [24] |
| HigBA | Ribonuclease activity [24] | Dormancy induction, biofilm formation [24] | Pseudomonas aeruginosa, E. coli |
| ParDE | DNA gyrase poison; inhibits DNA replication [24] | Dormancy induction, plasmid maintenance [24] | E. coli, P. aeruginosa |
| CcdAB | DNA gyrase poison; inhibits DNA replication [24] | DNA repair, dormancy induction [24] | E. coli |
| DarTG | ADP-ribosyltransferase; modifies DNA [24] | DNA repair pathways [24] | E. coli |
The molecular interplay within a type II TA system can be visualized as a regulatory circuit that responds to external stress. The following diagram illustrates the core pathway of stress-induced dormancy via a type II TA module.
TA Systems, Nutrient Gradients, and Persister Formation in Biofilms
The biofilm microenvironment is characterized by chemical and nutrient gradients that arise from the consumption of nutrients and oxygen by cells in the outer layers and the limited diffusion of these molecules through the extracellular polymeric substance (EPS) matrix [5]. This creates a heterogeneous structure with distinct micro-niches: nutrient-replete, fast-growing cells at the biofilm periphery, and nutrient-deprived, slow-growing or non-growing cells in the interior core.
This physiological heterogeneity is a primary driver of persister formation within biofilms. Bacteria residing in the nutrient-limited interior experience starvation stress, which serves as a key environmental trigger for the activation of TA systems [5]. The subsequent induction of dormancy in these subpopulations renders them highly tolerant to antibiotics. It is estimated that biofilms can contain 10 to 1000 times more persisters than their planktonic counterparts, explaining the recalcitrance of biofilm-associated infections to antimicrobial treatment [5].
The connection between nutrient gradients, TA system activation, and the resulting population heterogeneity is summarized in the following workflow.
Quantitative Analysis of TA Systems in Pathogens
The abundance and conservation of TA systems vary across bacterial pathogens, reflecting their adaptation to different environmental niches and stress challenges. The table below compiles quantitative data on the distribution of type II TA families in several clinically relevant bacteria, highlighting their potential role in persistence and virulence.
Table 2: Quantitative Distribution of Type II TA Systems in Bacterial Pathogens
| Bacterial Species | VapBC Count | MazEF Count | RelBE Count | Other Key Systems | Key Reference |
|---|---|---|---|---|---|
| Mycobacterium tuberculosis | ~50 subfamilies [26] | ~10 types [26] | ~3 types [26] | ParDE, DarTG | [26] |
| Escherichia coli | Present [24] | Present (e.g., MazF) [24] | Present (e.g., RelE) [24] | HigBA, YafQ-DinJ | [24] |
| Pseudomonas aeruginosa | Present (e.g., VapC) [24] | Present | Present | HigBA, ParDE | [24] [11] |
| Methanocaldococcus jannaschii | Present (VapB-VapC) [24] | - | - | - | [24] |
Experimental Protocols for Investigating TA Systems
Studying TA systems requires a multidisciplinary approach combining molecular biology, microbiology, and biochemical techniques. Below are detailed protocols for key experiments used to characterize TA system function and their role in persistence.
Protocol: Assessing Persister Levels via Antibiotic Kill Curves
Purpose: To quantify the fraction of antibiotic-tolerant persister cells in a bacterial population, such as one derived from a biofilm [11].
Methodology:
- Culture Preparation: Grow the bacterial strain to the desired phase (e.g., stationary phase, or disaggregate a mature biofilm). For biofilms, grow them in a suitable model (e.g., Calgary biofilm device, flow cell) for 3-5 days.
- Antibiotic Exposure: Expose the bacterial population to a high concentration of a bactericidal antibiotic (e.g., 100x MIC of a fluoroquinolone or an aminoglycoside). Ensure the antibiotic concentration is sufficient to kill all growing cells.
- Viability Counting: At predetermined time intervals (e.g., 0h, 3h, 6h, 24h), remove aliquots, serially dilute them, and plate them on antibiotic-free agar plates.
- Data Analysis: Count the colony-forming units (CFU) after incubation. A biphasic kill curve—a rapid initial drop in viability followed by a plateau—indicates the presence of a persister subpopulation. The CFU count at the plateau represents the persister frequency.
Protocol: Molecular Docking of TA Complexes
Purpose: To predict and analyze the binding interactions and stability between toxin and antitoxin proteins, which can reveal the functional impact of mutations [26].
Methodology:
- Protein Structure Preparation: Obtain 3D structures of the toxin and antitoxin proteins from experimental data (e.g., PDB) or generate homology models using tools like AlphaFold.
- Molecular Docking: Use a docking program such as HADDOCK 2.4 (High Ambiguity Driven biomolecular DOCKing) to model the TA complex.
- Define active and passive residues based on known interaction sites or mutagenesis data.
- HADDOCK will generate an ensemble of possible complex structures.
- Analysis of Docking Results: Analyze the generated models using key parameters:
- HADDOCK Score: A combined energy score where more negative values indicate stronger binding affinity.
- RMSD (Root Mean Square Deviation): Measures the structural deviation of the complex; lower values indicate a more stable complex.
- Van der Waals Energy & Electrostatic Energy: Contributions from different intermolecular forces.
- Buried Surface Area (BSA): The surface area hidden upon complex formation; larger BSA often correlates with stronger binding.
- Validation: Compare docking results between wild-type and mutant proteins (e.g., M. tuberculosis vs. M. bovis VapC3) to infer the functional consequences of sequence variations [26].
The Scientist's Toolkit: Essential Research Reagents
The following table lists key reagents, tools, and their applications for researching TA systems and persistence.
Table 3: Essential Research Reagents for TA System and Persister Studies
| Reagent / Tool | Function / Application | Example Use Case |
|---|---|---|
| HADDOCK 2.4 Software | Biomolecular docking to model protein-protein interactions [26] | Predicting binding stability of VapB-VapC complex in M. tuberculosis [26] |
| AlphaFold | Protein structure prediction from amino acid sequence [26] | Generating 3D models of toxin proteins for docking studies [26] |
| UCSF ChimeraX | Molecular visualization and analysis [26] | Visualizing and comparing structural models of TA complexes [26] |
| pNDM-220 Vector | Plasmid for controlled gene expression [11] | Overexpressing VapC toxin to induce growth arrest in E. coli [11] |
| Calgary Biofilm Device | High-throughput cultivation of biofilms [5] | Generating standardized biofilm samples for antibiotic tolerance assays [5] |
| Fluoroquinolone Antibiotics | Inducers of DNA damage and SOS response [25] | Selecting for and studying persisters in biofilm populations [25] |
| MK2-IN-1 hydrochloride | MK2-IN-1 hydrochloride, MF:C27H26Cl2N4O2, MW:509.4 g/mol | Chemical Reagent |
| Ibrexafungerp | Ibrexafungerp | Ibrexafungerp is a first-in-class triterpenoid antifungal for research. It inhibits glucan synthase. For Research Use Only. Not for human use. |
Toxin-antitoxin systems are master regulators of bacterial stress response, directly linking environmental cues like nutrient scarcity in biofilms to the phenotypic switch into a dormant, persistent state. The structured heterogeneity of biofilms provides an ideal environment for the stochastic and triggered activation of these modules, creating a reservoir of antibiotic-tolerant cells that drive chronic and relapsing infections. A deep understanding of the specific TA systems activated by biofilm nutrient gradients, their molecular targets, and their regulatory networks is paramount. Future research must leverage the experimental frameworks and tools outlined here to dissect these pathways, with the ultimate goal of identifying and developing novel therapeutic agents that can effectively eradicate persister cells and resolve stubborn biofilm infections.
Metabolic Transitions and Diauxic Shifts as Persister Triggers
Bacterial persisters, a subpopulation of cells capable of surviving antibiotic treatment without genetic mutation, pose a significant challenge in treating chronic and biofilm-associated infections. This technical guide explores the central role of metabolic transitions, specifically diauxic shifts, as critical environmental triggers for persister cell formation. Within the context of biofilm biology, nutrient gradients create heterogeneous microenvironments that promote a bet-hedging strategy where subpopulations enter a dormant, persistent state. We detail the molecular mechanisms underpinning this phenomenon, summarize key quantitative findings, provide experimental methodologies for studying nutrient-induced persistence, and visualize the core signaling pathways. This resource aims to equip researchers and drug development professionals with the foundational knowledge and technical protocols necessary to advance therapeutic strategies against persistent infections.
Bacterial persisters are genetically susceptible, slow-growing or non-growing phenotypic variants that survive exposure to bactericidal antibiotics and can regrow once the stress is removed [11]. These cells are now recognized as a major contributor to chronic and recurrent infections, including those associated with medical implants and cystic fibrosis [27] [11]. While persisters can form stochastically, a significant body of evidence demonstrates that environmental cues, particularly nutrient availability and metabolic shifts, are potent inducers of this transient, high-tolerance state [13].
In structured environments like biofilms, bacteria encounter steep nutrient gradients. Cells at the periphery consume preferred nutrients, leaving less favorable substrates for cells in the interior [13]. This heterogeneity is a hallmark of the biofilm lifestyle and creates ideal conditions for persister formation. The transition from one carbon source to another, known as a diauxic shift, has been specifically identified as a metabolic stressor that stimulates a persister formation pathway in Escherichia coli biofilms [13]. Understanding these nutrient-dependent mechanisms is therefore crucial for the development of more effective treatments for persistent biofilm infections, framing the core thesis that nutrient gradients are a fundamental environmental driver of persister formation.
Molecular Mechanisms Linking Metabolic Shifts to Persistence
The bacterial response to nutrient transitions is a highly coordinated process involving key signaling molecules and genetic regulators that ultimately lead to growth arrest and antibiotic tolerance.
The Central Role of ppGpp and the Stringent Response
The alarmone guanosine tetraphosphate (ppGpp) serves as a central mediator of bacterial persistence in response to nutrient stress [28] [13]. During nutrient limitation or carbon source transitions, ppGpp is synthesized by RelA and SpoT. This alarmone dramatically reprograms cellular metabolism by binding to RNA polymerase and activating stress response sigma factors like RpoS, leading to the downregulation of energy-intensive processes such as DNA replication, protein synthesis, and cell division [28]. This reallocation of resources induces a state of dormancy or reduced metabolic activity, which is the hallmark of persister cells. Data from both planktonic and biofilm studies confirm that ppGpp is indispensable for persister formation in response to diauxic shifts [13].
Toxin-Antitoxin (TA) Systems and Growth Arrest
Toxin-Antitoxin (TA) systems are tightly linked to persistence and are often activated downstream of the ppGpp-mediated stringent response [28]. These systems typically consist of a stable toxin that disrupts an essential cellular process (e.g., translation) and a labile antitoxin that neutralizes the toxin. Under stress conditions, proteases like Lon are activated, leading to the degradation of the antitoxin and freeing the toxin to act. Key TA systems implicated in persistence include:
- MqsR/MqsA: The MqsR toxin cleaves mRNA at a 5'-GCU site, effectively shutting down translation and inducing dormancy [28].
- TisB/IstR-1: The TisB toxin decreases the proton motive force and ATP levels, rendering the cell dormant and tolerant to multiple antibiotic classes [28].
While overexpression of many toxins increases persistence, deletion of specific TA pairs, such as mqsRA and tisAB-istR, has been shown to reduce persister numbers, confirming their functional role [28].
Nutrient Transitions as a Specific Trigger
Research has demonstrated that the exhaustion of a primary carbon source (e.g., glucose) and the subsequent transition to a secondary carbon source is a potent stimulus for persister formation in E. coli biofilms [13]. This diauxic transition activates a pathway dependent on ppGpp and specific nucleoid-associated proteins (NAPs) like FIS and HU. The proposed mechanistic cascade is as follows: nutrient transition → ppGpp accumulation → activation of NAPs → expression/activation of toxin components from TA systems → growth arrest and persistence. This pathway highlights how a common metabolic event in structured communities can directly lead to the formation of antibiotic-tolerant cells.
The diagram below illustrates the core signaling pathway from nutrient transition to persister cell formation.
Quantitative Data on Nutrient-Induced Persistence
Experimental data quantifying persister formation in response to metabolic stresses is critical for understanding the phenomenon. The following table consolidates key quantitative findings from investigations into diauxic shifts and carbon source transitions.
Table 1: Quantitative Data on Persister Formation Induced by Metabolic Transitions
| Organism | Metabolic Transition / Condition | Key Genetic Factors | Effect on Persistence (Fold Change) | Reference |
|---|---|---|---|---|
| E. coli | Diauxic carbon shift in biofilms | Wild-type | Significant increase post-glucose exhaustion | [13] |
| E. coli | Diauxic carbon shift in biofilms | ΔrelA (ppGpp synthase) | Elimination of transition-induced persistence | [13] |
| E. coli | Diauxic carbon shift in biofilms | Δfis, Δhu (NAPs) | Decreased persistence | [13] |
| E. coli | Overproduction of RelE toxin | N/A | Up to 10,000-fold increase | [28] |
| E. coli | Isolation of dormant cells via FACS | — | 20-fold greater persistence to ofloxacin | [28] |
The data underscore that diauxic shifts are a potent trigger for persistence, a process heavily dependent on the ppGpp pathway and its downstream effectors. The dramatic increase in persistence upon toxin overproduction further supports the involvement of TA systems, which are often regulated by these central metabolic signals.
Experimental Protocols for Investigating Metabolic Persistence
To study persister formation in the context of nutrient transitions, robust and reproducible experimental methodologies are required. Below is a detailed protocol for assessing persister levels in response to a diauxic shift in E. coli biofilms, based on established methods [13].
Biofilm Growth and Carbon Transition Assay
Key Materials:
- Bacterial Strain: E. coli MG1655 (wild-type and relevant mutants, e.g., ΔrelA).
- Growth Media: M9 minimal salts medium, supplemented with a primary carbon source (e.g., 15-60 mM glucose).
- Solid Support: Polyethersulfone (PES) membranes (0.2 µm pore size, 25 mm diameter).
- Agar Plates: M9 minimal agar plates containing the desired carbon source(s).
Procedure:
- Inoculum Preparation: Grow an overnight culture of the target strain in M9 media with a low concentration of glucose (e.g., 10 mM).
- Biofilm Initiation: Dilute the overnight culture to an OD600 of 0.01 in fresh M9 media with 15 mM carbon content. Inoculate 100 µL aliquots onto sterile PES membranes placed on M9 minimal agar plates containing a higher concentration of glucose (e.g., 60 mM).
- Growth Monitoring: Incubate plates at 37°C. Periodically aseptically remove membranes, vortex in PBS, and measure OD600 to monitor growth. Growth is reported as Fold Change in OD600 (FCOD600).
- Inducing Diauxic Shift: Persister measurements are taken at two critical points:
- Before glucose exhaustion: At FCOD600 ~6.
- After glucose exhaustion: At FCOD600 ~30. Glucose exhaustion can be confirmed using a commercial glucose assay kit.
- Persister Measurement:
- Harvest biofilm cells from membranes at the specified time points.
- Treat the cell suspension with a high concentration of a bactericidal antibiotic (e.g., 10 µg/mL ofloxacin or 750 µg/mL ampicillin) for 5 hours. The antibiotic concentration must be on the second, concentration-independent phase of the kill curve.
- After antibiotic exposure, serially dilute the cells, spot onto drug-free LB agar plates, and incubate overnight to enumerate Colony Forming Units (CFUs).
- The number of CFUs remaining after 5 hours of antibiotic exposure represents the persister cell count.
The experimental workflow for this protocol is visualized below.
Research Reagent Solutions
The following table lists essential materials and reagents for executing the described experiments, along with their critical functions.
Table 2: Essential Research Reagents for Studying Nutrient-Dependent Persistence
| Reagent / Material | Function / Application | Example / Note |
|---|---|---|
| PES Membranes | Provides a solid, non-invasive surface for growing colony biofilms. | Pall Corporation, 0.2 µm pore size, 25 mm diameter. |
| M9 Minimal Salts | Defined minimal medium base for precise control of nutrient availability. | Allows specific supplementation with carbon sources. |
| Carbon Sources (Glucose, etc.) | To create controlled nutrient environments and induce diauxic shifts. | Use high-purity grades for consistent results. |
| Amplex Red Glucose Assay Kit | Quantitatively measure glucose concentration in the biofilm environment. | Critical for confirming the point of carbon source exhaustion. |
| Bactericidal Antibiotics (Ofloxacin, Ampicillin) | To kill non-persister cells and selectively enumerate the persister population. | Concentration must be optimized to be on the second phase of the kill curve. |
| Flow Cytometer | Analyze and sort bacterial subpopulations based on metabolic activity (e.g., using GFP reporters). | Can be used with ribosomal promoters to isolate dormant cells [28]. |
Discussion and Therapeutic Implications
The direct link between metabolic transitions and bacterial persistence provides a framework for understanding why chronic infections are so difficult to eradicate. Biofilms, with their inherent nutrient gradients, are factories for generating persister cells through the ppGpp-dependent pathway detailed above [13] [6]. This mechanistic understanding opens up new avenues for therapeutic intervention.
Rather than relying solely on traditional antibiotics that target active cellular processes, novel strategies are being explored. These include:
- Preventing Persister Formation: Targeting the ppGpp signaling pathway or TA systems to block the entry into dormancy [27].
- Eradicating Dormant Persisters: Using compounds that disrupt membrane integrity or corrupt essential processes in a metabolism-independent manner, such as membrane-targeting agents or compounds that activate uncontrolled protein degradation (e.g., ADEP4) [27].
- Synergistic Approaches: Combining metabolic modulators that force persister cells to resuscitate with conventional antibiotics to enhance killing [27].
In conclusion, metabolic transitions and diauxic shifts are not merely physiological events but are pivotal ecological triggers for the persister state within biofilms. Future research focusing on disrupting these specific metabolic signaling pathways holds great promise for developing more effective treatments against recalcitrant biofilm infections.
From Bench to Model: Techniques for Quantifying Nutrient-Linked Persistence
The study of biofilms in structured, colony-type systems is fundamental to understanding microbial physiology in environments that mirror natural and clinical settings. A core principle governing these communities is the formation of physical and chemical gradients, which arise from metabolic activity and diffusion limitations within the aggregated biomass [3]. These gradients are not merely a consequence of growth; they actively shape the physiological heterogeneity of the population, influencing everything from primary metabolism to the emergence of transiently tolerant sub-populations known as persisters [3] [29]. The interplay between gradient formation and physiology has far-reaching consequences for human health, particularly in the context of chronic infections and antibiotic treatment failure [3] [30]. This guide details the experimental systems that enable researchers to dissect these complex relationships, with a specific focus on methodologies that control nutrient delivery to probe the mechanisms of persister formation.
Key Experimental Methodologies for Colony Biofilms
A range of techniques has been developed to cultivate and analyze colony biofilms, allowing for precise control over the environment and detailed observation of community structure and function. The following table summarizes the primary systems in use.
Table 1: Overview of Key Colony Biofilm Experimental Systems
| Experimental System | Core Principle | Key Readouts & Applications | Notable Advantages |
|---|---|---|---|
| Membrane-Based Colony Biofilms [29] | Cells grown on a porous membrane atop solid agar, allowing nutrient diffusion from below. | Persister assays, gene expression analysis, metabolic studies. | Simplicity and reliability; ideal for studying nutrient transitions from a primary to a secondary carbon source [29]. |
| Microfluidic Devices [30] | Traps for growing microcolonies with continuous media flow from one side, creating controlled nutrient gradients. | Real-time imaging of growth and gene expression, response to dynamic antibiotic regimens. | Enables high-resolution, spatiotemporal analysis of gradient-driven phenomena in a biofilm-like environment [30]. |
| Pipe Loop Samplers [31] | Closed-loop flow-through systems with removable material coupons to simulate plumbing or industrial piping. | Biomass quantification, disinfectant efficacy testing, material biofilm growth potential. | Directly applicable to industrial and public health settings (e.g., drinking water distribution systems) [31]. |
| Macro-Colony Imaging (Mesoscopy) [32] | Use of specialized optics (e.g., Mesolens) to image large, intact colonies at high resolution. | Visualization of internal colony architecture, such as intra-colony channels for nutrient transport. | Reveals emergent structural features of mature colonies without destructive processing [32]. |
Detailed Protocol: Membrane-Based Colony Biofilm for Nutrient Transition Studies
This protocol, adapted from Amato & Brynildsen (2014), is specifically designed to investigate how nutrient shifts stimulate persister formation [29].
- Preparation of Inoculum:
- Grow the bacterial strain (e.g., E. coli MG1655) overnight for 16 hours in a defined minimal medium (e.g., M9) with a primary carbon source (e.g., 10 mM glucose).
- Biofilm Establishment:
- Dilute the overnight culture into fresh M9 medium containing a limiting concentration of the primary carbon source (e.g., 2.5-15 mM glucose) to an OD₆₀₀ of 0.01.
- Inoculate 100 µL aliquots onto sterile, polyethersulfone (PES) membranes (0.2 µm pore size, 25 mm diameter) positioned on M9 minimal agar plates.
- The agar should contain a high concentration (e.g., 60 mM) of the secondary carbon source to be studied (e.g., fumarate) or no carbon as a control.
- Growth and Monitoring:
- Incubate the plates at 37°C.
- Monitor growth by aseptically removing membranes at intervals, vortexing in phosphate-buffered saline (PBS) for 1 minute to dislodge cells, and measuring the OD₆₀₀ of the suspension.
- Inducing Nutrient Transition and Sampling Persisters:
- The primary carbon source (glucose) in the inoculum is exhausted after a predictable number of doublings, forcing a transition to the secondary source in the agar.
- Sample persisters at two critical time points: 1) prior to glucose exhaustion (e.g., FCOD₆₀₀ = 6), and 2) after glucose exhaustion and the transition is underway (e.g., FCOD₆₀₀ = 30) [29].
- For persister assays, dislodge cells from the membrane, treat with a high concentration of antibiotic (e.g., ofloxacin) for a set period, wash, and plate on solid media to count surviving colony-forming units (CFUs).
Detailed Protocol: Microfluidic Device for Spatial Gradient Analysis
This system allows for real-time observation of gradient formation and its consequences [30].
- Device Fabrication and Preparation:
- Fabricate a microfluidic device containing deep (e.g., 170 µm) traps for cell growth, connected to nutrient supply channels.
- Inoculation and Growth:
- Load a bacterial strain, potentially carrying fluorescent reporters for genes of interest (e.g., tetracycline resistance operon), into the device traps.
- Continuously perfuse the supply channels with fresh growth medium. Nutrients diffuse into the trap, creating a gradient from the open edge to the interior.
- Real-Time Imaging and Analysis:
- Use time-lapse microscopy to monitor colony development.
- Particle Image Velocimetry (PIV) can be applied to time-lapse images to calculate cell movement and growth rates throughout the colony [30].
- Fluorescence signals reveal the spatial pattern of gene expression in response to the nutrient gradient or to subsequent challenges, such as the introduction of antibiotics via the supply channels.
Quantitative Assessment of Biofilms
The quantitative evaluation of biofilm mass, viability, and metabolic activity is crucial. Different methods offer distinct advantages and are suited to different research questions.
Table 2: Quantitative Methodologies for Biofilm Analysis
| Methodology | What It Measures | Typical Data Output | Considerations |
|---|---|---|---|
| XTT Reduction Assay [33] | Metabolic activity of cells within the biofilm matrix via tetrazolium salt reduction. | Colorimetric readout (Absorbance at 490nm). | Accurate measure of cellular viability and vitality; more reproducible for Vibrionaceae than CV staining [33]. |
| Colony Forming Units (CFU) [33] [31] | Number of culturable/culturable bacteria. | CFU per unit area or volume. | Measures viability but is labor-intensive; does not account for viable but non-culturable (VBNC) cells [31]. |
| Crystal Violet (CV) Staining [33] | Total adhered biomass (cells and matrix). | Colorimetric readout (Absorbance at 562nm). | Semi-quantitative; cannot differentiate between live and dead cells. |
| Flow Cytometry (FCM) [31] | Total bacterial cell count using fluorescent nucleic acid stains (e.g., Syto 9). | Cell count per unit area or volume. | Provides rapid, automated total cell counting; does not distinguish viability without specific stains. |
| Confocal Scanning Laser Microscopy (CSLM) [31] | 3D architecture, biomass, and spatial distribution of live/dead cells. | Biomass volume, thickness, roughness. | Allows in situ analysis of biofilm structure; requires specialized equipment and expertise. |
| Dry Cell Mass [33] | Total dry weight of the biofilm. | Mass (e.g., µg). | Direct measurement but is low-throughput and requires large amounts of biofilm. |
Connecting Nutrient Gradients to Persister Formation: A Pathway Analysis
Nutrient transitions, particularly diauxic shifts, have been identified as a direct stimulus for persister formation in biofilms [29]. The pathway involves key regulators that sense and respond to metabolic stress.
Diagram 1: Nutrient stress to persister formation pathway.
The pathway outlined in the diagram can be broken down as follows:
- Stimulus: A carbon source transition, such as the exhaustion of a preferred sugar like glucose, acts as a nutrient stress signal [29].
- Central Mediator: This stress activates the RelA enzyme, leading to a rapid accumulation of the alarmone ppGpp [29]. This molecule is a central mediator of the stringent response and has been strongly implicated in bacterial persistence across multiple studies.
- Effectors: Elevated ppGpp levels lead to changes in the expression and activity of Nucleoid-Associated Proteins (NAPs), such as FIS and HU [29]. These proteins play a critical role in orchestrating large-scale changes in gene expression and chromosome organization.
- Phenotype: The action of these NAPs promotes the entry of a sub-population of cells into the persister state, a slow-growing or dormant phenotype characterized by multi-drug tolerance [29].
The Scientist's Toolkit: Essential Research Reagents and Materials
Successful research in this field relies on a suite of specific reagents, strains, and tools.
Table 3: Key Research Reagent Solutions for Biofilm and Persister Studies
| Reagent/Material | Function/Application | Specific Examples & Notes |
|---|---|---|
| PES Membranes | Support for colony biofilm growth; allows diffusion of nutrients from underlying agar. | 0.2 µm pore size, 25 mm diameter; sterile [29]. |
| Defined Minimal Media (M9) | Provides controlled environment for studying specific nutrient effects. | Can be supplemented with defined carbon sources (e.g., glucose, fumarate) at varying concentrations [29]. |
| XTT/Menadione Solution | Colorimetric assay to measure metabolic activity and viability of biofilm cells. | XTT is reduced by metabolically active cells to an orange formazan product; Menadione acts as an electron-coupling agent [33]. |
| Microfluidic Device | Creates spatially structured microcolonies with defined nutrient gradients for real-time imaging. | Custom-built devices with cell traps and media supply channels [30]. |
| Fluorescent Reporter Plasmids | Visualizing gene expression patterns in space and time within biofilms. | e.g., two-color reporters for resistance genes (TetR-GFP, TetA-mCherry) [30]. |
| ppGpp0 Mutant Strain | Genetic tool to study the role of the stringent response. | E. coli strain lacking both RelA and SpoT enzymes, unable to produce ppGpp [29]. |
| NAP Mutant Strains | Genetic tools to dissect the role of specific nucleoid-associated proteins. | Isogenic mutants in genes such as fis and hupA/hupB (HU) [29]. |
| MKC3946 | MKC3946, MF:C21H20N2O3S, MW:380.5 g/mol | Chemical Reagent |
| ML352 | ML352, MF:C21H29N3O4, MW:387.5 g/mol | Chemical Reagent |
The experimental systems detailed here—from simple membrane colonies to sophisticated microfluidic devices—provide a powerful toolkit for unraveling the causal links between controlled nutrient delivery, gradient formation, and the resulting physiological heterogeneity in biofilms. The quantitative methodologies and specific reagents outlined enable rigorous investigation into the mechanisms underlying one of biofilm's most clinically relevant properties: the formation of antibiotic-tolerant persister cells. By applying these structured approaches, researchers can generate reproducible data that deepens our understanding of biofilm pathophysiology and informs the development of novel anti-biofilm therapeutic strategies.
Single-Cell Analysis and Fluorescence Imaging of Microenvironments
Biofilms are structured microbial communities embedded in a self-produced extracellular matrix and are a major source of persistent infections in clinical and industrial settings [34] [11]. Their remarkable tolerance to antimicrobial treatment stems not only from physical barrier properties but also from profound physiological heterogeneity among constituent cells, particularly the presence of persister cells [11]. These persisters are genetically susceptible, non-growing, or slow-growing bacterial cells that survive antibiotic exposure and other environmental stresses, serving as a reservoir for infection relapse after treatment cessation [11].
A primary driver of this heterogeneity is the establishment of nutrient and chemical gradients within the biofilm's three-dimensional structure [35]. As nutrients diffuse from the exterior to the interior, and metabolic waste products accumulate, distinct microenvironments emerge that profoundly influence bacterial physiology [35]. Research has demonstrated that nutrient limitation is a key environmental cue triggering the formation of persister cells [36] [6]. Understanding these microenvironments and their effects on single-cell phenotypes is therefore critical for developing more effective strategies to combat biofilm-associated infections.
This technical guide details advanced methodologies for quantifying biofilm microenvironmental gradients and correlating them with single-cell physiological states, providing researchers with the tools to unravel the spatial and functional architecture of biofilms.
Technical Approaches for Microenvironment and Single-Cell Analysis
Fluorescence Imaging of Microenvironmental Gradients
Chemical gradients within biofilms create microenvironments where local conditions differ substantially from the surrounding solution. Measuring these gradients is essential for understanding the conditions that promote persister formation [35].
- Ratiometric Nanoparticle Sensors: A powerful approach for pH mapping utilizes ratiometric core-shell silica nanoparticle sensors (C dot sensors). These nanoparticles contain a pH-insensitive reference dye (e.g., Cy5) in the core and a pH-sensitive dye (e.g., Fluorescein isothiocyanate, FITC) in the shell [35]. The ratio of the two fluorescence signals allows quantitative pH mapping independent of local sensor concentration.
- Critical Size for Biofilm Penetration: Studies reveal that sensor size is critical for homogeneous biofilm staining. While 70-nm and 30-nm particles show limited penetration, 10-nm-diameter C dot sensors successfully generate high-resolution 3D maps of biofilm pH, revealing heterogeneous pH profiles ranging from 5 to >7 [35].
- Protocol for pH Gradient Imaging:
- Sensor Preparation: Synthesize 10-nm C dot sensors via a modified Stöber silica synthesis, incorporating Cy5 in the core and FITC in the shell [35].
- Biofilm Staining: Grow biofilms for 7-8 days in appropriate culture dishes. Approximately 9 hours before imaging, add C dot sensors to a concentration of 50 nM and stir continuously for 4 hours [35].
- Sample Washing: 5 hours prior to imaging, wash biofilms twice with fresh medium to remove unbound nanoparticles.
- Image Acquisition: Perform 3D tomographic imaging using a confocal fluorescence microscope. Collect emission signals for both the pH-sensitive (FITC) and pH-insensitive (Cy5) channels [35].
- Data Processing: Calculate the ratiometric signal (FITC/Cy5) for each voxel and convert to pH values using a pre-established calibration curve [35].
Table 1: Nanoparticle Sensors for Microenvironment Imaging
| Sensor Type | Target Analyte | Size | Key Feature | Application in Biofilms |
|---|---|---|---|---|
| C Dot Sensor [35] | pH | 10 nm | Ratiometric (FITC/Cy5); core-shell structure | High-resolution 3D mapping of pH microenvironments |
| C-SNARF-4 [35] | pH | Molecular Dye | Ratiometric fluorescent dye | Measuring pH microenvironments; can interact with biofilm components |
Single-Cell Transcriptomics in Biofilms
Bacterial single-cell RNA sequencing (scRNA-seq) has emerged as a transformative technology for deconvoluting the transcriptional heterogeneity of biofilms without the need for cultivation [37] [38].
- Technical Challenge and Solution: The overwhelming abundance of ribosomal RNA (rRNA >95%) in bacterial total RNA poses a major challenge for mRNA capture. Recent methodological advances, such as BaSSSh-seq and RiboD-PETRI, have successfully addressed this through efficient rRNA depletion [37] [38].
- BaSSSh-seq Protocol:
- Cell Fixation and Permeabilization: Cells are fixed and permeabilized to allow entry of reagents while preserving cellular integrity [37].
- Split-Pool Barcoding: RNA transcripts from individual cells are labeled with a unique combination of oligonucleotide barcodes over three rounds of reverse transcription and ligation in a multi-well plate. This labels the cellular origin of each transcript [37].
- rRNA Depletion: An enzyme-free subtraction hybridization method is used to deplete rRNA-derived cDNAs, significantly enriching for mRNA sequences [37].
- Library Preparation and Sequencing: The processed cDNA is amplified and prepared for high-throughput sequencing [37].
- Performance: RiboD-PETRI, for instance, can increase mRNA detection rates from ~8% to over 90%, enabling the identification of distinct biofilm subpopulations based on unique gene expression signatures [38]. This approach can identify markers like PdeI, which is associated with cell-surface attachment subpopulations and elevated cyclic di-GMP levels that promote persister formation [38].
Table 2: Bacterial Single-Cell RNA-Seq Methods
| Method Name | Barcoding Approach | rRNA Depletion Strategy | Reported mRNA Detection Rate | Key Application |
|---|---|---|---|---|
| BaSSSh-seq [37] | Split-pool barcoding | Subtractive hybridization | Not explicitly quantified, but enables transcriptome-wide coverage | Identifying transcriptional heterogeneity in S. aureus biofilms and response to immune cells |
| RiboD-PETRI [38] | Combinatorial barcoding (PETRI-seq) | Ribosomal RNA-derived cDNA depletion (RiboD) with probes and magnetic beads | Up to 92% | Identifying biofilm subpopulations and marker genes like PdeI |
| microSPLiT [38] | Split-pool barcoding | Poly A polymerase | ~7% | Profiling bacterial populations |
| M3-seq [38] | Not specified | RNase H | ~65% | Profiling bacterial populations |
| BacDrop [38] | Not specified | RNase H | ~61% | Profiling bacterial populations |
Quantitative 3D Image Analysis with BiofilmQ
To extract robust quantitative data from 3D fluorescence images of biofilms, specialized computational tools are required. BiofilmQ is a software tool designed for the automated and high-throughput quantification, analysis, and visualization of biofilm properties in three-dimensional space and time [39].
- Workflow:
- Biofilm Segmentation: The biofilm biovolume is identified from 3D images using automatic, semi-manual, or imported segmentation [39].
- Image Cytometry: For images without single-cell resolution, the segmented biovolume is dissected into a cubical grid (user-defined size). Each cube is treated as a "pseudocell" object [39].
- Parameter Quantification: For each cube, BiofilmQ calculates up to 49 structural, textural, and fluorescence properties, as well as its spatial context (e.g., distance to biofilm surface) [39].
- Data Visualization: The software includes built-in capabilities to visualize the quantified data, enabling direct correlation of local microenvironment conditions with cellular phenotypes [39].
- Application: This tool allows researchers to spatiotemporally quantify the expression of key genes (e.g., matrix genes) and correlate them with the localization of their corresponding proteins and structural features within the same biofilm [39].
Integrated Experimental Workflow
Combining these techniques provides a comprehensive view of the relationship between nutrient gradients and cell fate. The following workflow integrates the key techniques described in this guide.
Diagram: Integrated Workflow for Correlating Microenvironments with Single-Cell Phenotypes
This integrated experimental pipeline enables researchers to directly link heterogeneous microenvironments within biofilms to the emergence of specific, hard-to-treat cellular states.
The Scientist's Toolkit: Essential Research Reagents and Materials
Table 3: Key Reagents and Materials for Biofilm Microenvironment Analysis
| Item | Function/Description | Example Use Case |
|---|---|---|
| C Dot Nanoparticle Sensors [35] | Ratiometric, core-shell silica nanoparticles for quantitative pH sensing. | Mapping pH gradients in E. coli and wastewater biofilms with high spatial resolution. |
| Fixative and Permeabilization Reagents [37] [38] | Chemicals (e.g., paraformaldehyde, methanol) to fix and permeabilize cells for in situ barcoding. | Preparing bacterial cells for single-cell RNA-seq protocols like BaSSSh-seq and RiboD-PETRI. |
| Oligonucleotide Barcodes [37] [38] | Unique DNA barcodes for labeling cellular origin of RNA transcripts. | Enabling multiplexing of thousands of single cells in scRNA-seq workflows. |
| rRNA Depletion Probes [37] [38] | Sets of DNA oligonucleotides reverse complementary to rRNA sequences. | Enriching for mRNA in bacterial scRNA-seq libraries to drastically improve detection rates. |
| Viability Stains (e.g., RSG) [40] | Fluorescent dyes reporting cellular metabolic activity (redox potential). | Differentiating active, mid-active, and inactive (dead) subpopulations in biofilms via imaging flow cytometry. |
| BiofilmQ Software [39] | Image cytometry software for 3D quantification and visualization of biofilm properties. | Automating the analysis of biofilm architecture and internal heterogeneity from 3D microscopy images. |
| ML365 | ML365, MF:C22H20N2O3, MW:360.4 g/mol | Chemical Reagent |
| ML-792 | ML-792, MF:C21H23BrN6O5S, MW:551.4 g/mol | Chemical Reagent |
The combination of advanced fluorescence imaging, single-cell transcriptomics, and sophisticated computational analysis provides an unprecedented window into the complex world of biofilms. These techniques enable researchers to move beyond bulk measurements and understand how spatial variations in the physical and chemical microenvironment, particularly nutrient gradients, drive phenotypic heterogeneity and the formation of recalcitrant persister cells. By applying the integrated workflows and methodologies detailed in this guide, scientists and drug development professionals can identify new, targeted strategies to disrupt the pathways leading to persistence, ultimately leading to more effective therapies for persistent biofilm-associated infections.
Leveraging Individual-Based Models (IbM) to Simulate Phenotypic Switching
Individual-Based Models (IbM) have emerged as a powerful computational approach for simulating the complex dynamics of phenotypic switching in bacterial biofilms. Unlike traditional continuum models that treat bacterial populations as homogeneous entities, IbM represents each cell as an autonomous agent with unique characteristics and behaviors. This technical guide explores how IbM frameworks can elucidate the critical relationship between nutrient gradients and persister cell formation—a key mechanism underlying biofilm antibiotic tolerance. By integrating spatial constraints, nutrient diffusion, and single-cell response mechanisms, IbM provides unprecedented insights into the emergence of phenotypic heterogeneity in biofilm environments. This whitepaper details fundamental principles, methodological frameworks, and practical applications of IbM for researchers and drug development professionals seeking to combat persistent biofilm-associated infections.
The Clinical Challenge of Biofilm Persistence
Biofilm-associated infections represent a significant clinical challenge, particularly on medical implants, where they account for over a quarter of all healthcare-associated infections [6]. The resilience of biofilms to antibiotic treatment stems from two distinct mechanisms: genetic resistance and phenotypic tolerance. While resistance involves heritable genetic changes that enable bacteria to grow despite antibiotic presence, tolerance represents a transient, non-genetic adaptation where persister cells survive antibiotic exposure without replicating [6]. These persister cells are typically located in nutrient-deprived regions of the biofilm and are protected by the extracellular polymeric substance (EPS) matrix, creating protected niches that facilitate chronic infections.
The formation of persister cells is fundamentally linked to phenotypic switching—a process where genetically identical cells transition between different physiological states in response to environmental cues. This switching enables a subpopulation of cells to enter a dormant or slow-growing state that is tolerant to conventional antibiotics, which primarily target metabolically active cells. Understanding and modeling these switching dynamics is crucial for developing effective therapeutic strategies against persistent biofilm infections.
Limitations of Traditional Modeling Approaches
Traditional mathematical models of biofilm dynamics often overlook the critical role of nutrient-dependent phenotypic switching between proliferative and persister states [6]. Continuum models, which treat biofilms as homogeneous masses, cannot capture how environmental conditions control the balance between active growth and dormancy, which is central to biofilm persistence. Without this mechanism, models fail to accurately predict treatment outcomes or identify optimal intervention strategies.
Partial differential equation (PDE)-based models have been extensively used to simulate spatiotemporal dynamics of biofilms but often rely on simplifications such as uniform EPS properties and constant fluid viscosity, which may not reflect biological variability [6]. Similarly, cellular automaton (CA) models incorporate key biological mechanisms but face limitations due to stochastic nature of biomass redistribution, which can introduce algorithmic artefacts and reduce biological interpretability [6]. These limitations highlight the need for more sophisticated modeling approaches that can capture the emergent behaviors arising from individual cell interactions and environmental responses.
Individual-Based Modeling: Core Principles and Advantages
Fundamental Concepts of IbM
Individual-Based Models (IbM), also known as agent-based models, represent a paradigm shift in biofilm modeling by treating each bacterial cell as a discrete entity with its own set of rules and characteristics. In IbM frameworks, every cell is modeled as an autonomous agent that responds to local environmental conditions according to predefined behavioral rules. This bottom-up approach allows for the natural emergence of complex population-level behaviors from simple individual-level interactions.
The key components of an IbM system include:
- Autonomous agents: Individual cells with defined properties (size, metabolic state, genetic makeup)
- Behavioral rules: Algorithms governing growth, division, movement, and phenotypic changes
- Local environment: Spatial representation of nutrient concentrations, signaling molecules, and physical constraints
- Interaction mechanisms: Rules for cell-cell and cell-environment interactions
Unlike continuum models that use averaged population parameters, IbM tracks the fate of individual cells over time, enabling the simulation of heterogeneity that arises from stochastic events and positional advantages within the biofilm structure.
Advantages for Studying Phenotypic Switching
IbM offers several distinct advantages for investigating phenotypic switching in biofilms:
Spatial Heterogeneity Capture: IbM naturally incorporates spatial gradients of nutrients, oxygen, and signaling molecules, which are critical drivers of phenotypic switching [41]. The models can represent how cells in different biofilm regions experience varying microenvironments, leading to distinct phenotypic states.
Emergent Behavior Modeling: Complex population dynamics, such as the formation of persister cell niches, emerge naturally from individual cell decisions based on local conditions, rather than being prescribed in the model [41].
Multi-Scale Integration: IbM can bridge molecular-level mechanisms (e.g., toxin-antitoxin systems) with population-level outcomes, providing insights into how single-cell decisions impact overall biofilm resilience [16].
Stochasticity Incorporation: Phenotypic switching often involves probabilistic events at the cellular level, which can be directly implemented in IbM through stochastic rules for state transitions [16].
These advantages make IbM particularly suited for investigating the relationship between nutrient gradients and persister formation, as the models can directly simulate how local variations in nutrient availability trigger switching mechanisms at the single-cell level.
Modeling Nutrient Gradients and Persister Formation
Implementing Nutrient Diffusion and Consumption
A critical component of IbM for biofilm studies is the accurate representation of nutrient transport and consumption. Most models implement nutrient dynamics through reaction-diffusion equations that simulate how nutrients diffuse from the bulk fluid and are consumed by cells based on their metabolic state and local concentration.
The general form of these equations is:
∂S/∂t = D∇²S - f(X,S)
Where S is nutrient concentration, D is diffusion coefficient, X is biomass density, and f(X,S) represents consumption by cells [6] [16].
Advanced IbM frameworks like CROMICS explicitly model how crowding conditions affect nutrient diffusion, demonstrating that biomass accumulation significantly reduces metabolite mobility when cells occupy more than 14% of the volume fraction [42]. This reduction creates steeper nutrient gradients that promote phenotypic switching in nutrient-deprived regions.
Table 1: Key Parameters for Nutrient Dynamics in Biofilm IbM
| Parameter | Symbol | Typical Value Range | Unit | Biological Significance |
|---|---|---|---|---|
| Nutrient diffusion coefficient | D | 4.5×10â»â¶ - 2.0×10â»â´ | m²/day | Determines nutrient penetration depth |
| Maximum consumption rate | qmax | 15-75 | (gCOD/gCOD)/day | Metabolic activity of active cells |
| Half-saturation constant | KS | 20 | gCOD/m³ | Nutrient concentration at half-maximal uptake |
| Yield coefficient | Y | 0.5 | gCOD/gCOD | Biomass produced per nutrient consumed |
Source: Adapted from [16] [42]
Modeling Phenotypic Switching Mechanisms
IbM can implement various hypothesized mechanisms of persister formation, each with distinct implications for spatial distribution and biofilm response to treatment:
Stochastic Switching: Cells randomly transition between susceptible and persister states with fixed probabilities, independent of environmental conditions [16].
Nutrient-Dependent Switching: Transition rates depend on local nutrient concentration, with switching to persister state accelerated when nutrients fall below critical thresholds [6] [16].
Antibiotic-Induced Switching: Presence of antibiotics triggers transition to persistent state as a stress response [43].
Time-Dependent Switching: Cells switch to persistent state after prolonged growth arrest, implementing a "timer" mechanism [16].
In nutrient-dependent switching models, transition rates typically follow threshold-based functions:
[ k{S→P} = \begin{cases} k{max} & \text{if } S \leq S{critical} \ k{min} & \text{if } S > S_{critical} \end{cases} ]
Where ( k{S→P} ) is the switching rate from susceptible to persister state, S is local nutrient concentration, and ( S{critical} ) is the threshold nutrient level that triggers persistence [6].
Table 2: Experimentally Derived Switching Parameters for Common Pathogens
| Bacterial Species | Switching Type | Switching Rate (per hour) | Persister Fraction | Critical Nutrient Threshold |
|---|---|---|---|---|
| Pseudomonas aeruginosa | Nutrient-dependent | 0.001-0.01 | 0.1-1% | 20 gCOD/m³ |
| Escherichia coli | Stochastic | 0.0001-0.001 | 0.01-0.1% | N/A |
| Bacillus subtilis | (p)ppGpp-mediated | 0.005-0.05 | 0.1-10% | Variable |
Source: Adapted from [16] [44] [45]
Implementation Frameworks and Methodologies
Computational Framework for Biofilm IbM
Implementing an IbM for biofilm studies requires integration of multiple computational components:
Cell Representation: Bacterial cells are typically modeled as spherocylindrical particles with defined length and diameter that grow by polar elongation [46]. For example, Pseudomonas putida has been represented with an initial aspect ratio L*â‚€ = 2.6 [46].
Growth and Division: Cell growth follows Monod kinetics, where the growth rate depends on local nutrient availability:
[ \frac{dmi}{dt} = mi \mu{max} \frac{CS}{CS + KS} ]
Where ( mi ) is the mass of cell i, ( \mu{max} ) is the maximal specific growth rate, ( CS ) is local substrate concentration, and ( KS ) is the half-saturation constant [43].
Mechanical Interactions: As cells grow and divide, they exert forces on neighboring cells. A "shoving algorithm" is commonly used to resolve overlapping cells by displacing them until no overlaps remain [43] [16].
Nutrient Field: Nutrients diffuse from the bulk liquid and are consumed by cells based on their metabolic state and local concentration, creating dynamic gradients that evolve with biofilm development.
Experimental Protocols for Model Parameterization and Validation
Protocol 1: Parameterizing Phenotypic Switching Rates
Culture Preparation: Grow bacterial cultures to mid-exponential phase in defined media with varying nutrient concentrations (e.g., 10-100% of standard nutrient load) [16].
Persister Induction: Expose subcultures to nutrient limitation by transferring to nutrient-depleted media or allowing growth into stationary phase [44].
Time-Kill Assays: Treat cultures with bactericidal antibiotics at 10-100× MIC and plate samples at regular intervals to determine surviving fractions [43] [44].
Switching Rate Calculation: Estimate switching rates from the proportion of persisters before and after nutrient shifts using mathematical fitting procedures [16].
Single-Cell Validation: Use microfluidic devices with time-lapse microscopy to track phenotypic switching in individual cells under controlled nutrient gradients [44].
Protocol 2: Spatial Mapping of Persister Distributions
Biofilm Cultivation: Grow biofilms in flow cells or on membrane filters under defined nutrient conditions [16].
Sectioning and Staining: Cryo-section biofilms and stain with viability markers combined with persister-specific reporters (e.g., toxin-antitoxin fusion proteins) [16].
Image Analysis: Use confocal microscopy to reconstruct three-dimensional maps of persister locations relative to nutrient gradients measured with fluorescent nutrient analogs [16].
Model Validation: Compare spatial patterns of persister formation in experimental biofilms with IbM predictions using spatial correlation analysis [16].
Case Studies and Research Applications
Optimizing Antibiotic Treatment Regimens
IbM has demonstrated significant utility in optimizing antibiotic dosing strategies against persistent biofilm infections. A recent agent-based model investigated periodic versus continuous antibiotic dosing and found that properly tuned periodic dosing could reduce the total antibiotic dose required for effective treatment by nearly 77% [43].
The model simulated biofilm growth with persister formation dependent on both substrate availability and antibiotic presence. By aligning treatment intervals with the dynamics of persister resuscitation, the optimized regimen allowed time for persisters to revert to susceptible states between antibiotic pulses, significantly improving overall killing efficiency [43]. This approach demonstrates how IbM can identify treatment strategies that would be difficult to discover through experimental trial-and-error alone.
Mapping Spatial Organization of Persister Niches
IbM simulations have revealed how different switching mechanisms produce distinct spatial patterns of persister cells within biofilms:
- Stochastic switching produces randomly distributed persisters throughout the biofilm [16]
- Nutrient-dependent switching concentrates persisters in the nutrient-deprived biofilm interior [6] [16]
- Oxygen-dependent switching localizes persisters in anoxic regions [16]
- Time-dependent switching distributes persisters based on cellular age and growth history [16]
These spatial patterns have profound implications for treatment efficacy, as persisters in different locations may be exposed to varying antibiotic concentrations due to diffusion limitations and presence of chemical gradients within the biofilm.
Table 3: Research Reagent Solutions for Persister Studies
| Reagent/Category | Specific Examples | Function/Application | Considerations |
|---|---|---|---|
| Bacterial Strains | P. aeruginosa PAO1, E. coli MG1655, B. subtilis 168 | Model organisms for persistence studies | Genetic tractability, relevance to infections |
| Persistence Reporters | GFP fusions to toxin-antitoxin systems, (p)ppGpp biosensors | Visualize persister cells and signaling dynamics | May alter native persistence mechanisms |
| Nutrient Probes | FRET-based nutrient sensors, fluorescent glucose analogs | Map nutrient gradients in biofilms | Potential perturbation of native nutrient uptake |
| Antibiotics | Vancomycin, ciprofloxacin, kanamycin at 10-100× MIC | Persister time-kill assays | Concentration-dependent effects on switching |
| Microfluidic Devices | PDMS chips with controlled flow and nutrient gradients | Single-cell persistence dynamics | Technical complexity of setup and operation |
Source: Adapted from [43] [16] [44]
Exploring Evolutionary Dynamics
Beyond immediate treatment optimization, IbM provides a platform for investigating long-term evolutionary dynamics of persistence. Models can simulate how repeated antibiotic treatments select for strains with altered switching rates or mechanisms, potentially informing strategies to suppress the emergence of high-persistence mutants.
For example, models incorporating multiple TA modules can explore how spontaneous mutations affect the network of persistence regulation, potentially identifying fragile points in the regulatory circuitry that could be targeted by future anti-persistence drugs [45].
Practical Implementation Guide
Software and Computational Tools
Several computational platforms facilitate IbM implementation for biofilm studies:
iDynoMiCS: An open-source IbM framework specifically designed for microbial communities, incorporating nutrient diffusion, cell growth, and mechanical interactions [41].
NetLogo: A versatile agent-based modeling environment with a lower entry barrier, suitable for prototyping and educational applications [43].
BacSim: An individual-based model for bacterial biofilms that has been continuously developed and refined for over two decades [41].
Custom MATLAB/Python Implementations: Many research groups develop custom solutions using general-purpose scientific computing languages, providing maximum flexibility at the cost of development time.
When selecting a modeling platform, researchers should consider factors including computational efficiency for the desired population size, flexibility in implementing novel mechanisms, compatibility with experimental data formats, and availability of analysis and visualization tools.
Parameter Estimation and Sensitivity Analysis
Successful IbM implementation requires careful parameter estimation and sensitivity analysis:
Literature Review: Compile parameter values from published experimental studies, noting the specific conditions under which they were measured [16] [42].
Experimental Calibration: Conduct targeted experiments to measure critical parameters that are poorly characterized in literature, particularly those related to phenotypic switching rates [16].
Sensitivity Analysis: Systematically vary parameters within plausible ranges to identify which have the greatest impact on model outcomes, focusing refinement efforts on the most influential parameters [42].
Uncertainty Quantification: Use statistical approaches such as Bayesian calibration to quantify uncertainty in parameter estimates and model predictions [43].
Particular attention should be paid to parameters governing nutrient diffusion, growth kinetics, and phenotypic switching rates, as these most strongly influence persister formation dynamics in nutrient gradients.
Emerging Trends and Technologies
The field of IbM for phenotypic switching is rapidly evolving, with several promising directions:
Multi-Scale Integration: Future models will more effectively bridge molecular mechanisms (e.g., TA module dynamics, (p)ppGpp signaling) with cellular and population-level behaviors [44] [45].
Integration with Omics Data: Incorporating transcriptomic, proteomic, and metabolomic data will enhance the biological fidelity of models and enable more accurate predictions of persister metabolism [41].
Host-Pathogen Interactions: Extending IbM to include immune cells and host tissue interactions will improve models of in vivo biofilm infections [41].
Machine Learning Integration: Combining IbM with machine learning approaches for parameter optimization, pattern recognition, and model reduction will enhance computational efficiency and predictive power.
High-Performance Computing: Leveraging parallel computing architectures will enable simulation of larger biofilms with more detailed molecular mechanisms, moving toward whole-biofilm virtual twins.
Individual-Based Models represent a powerful methodology for elucidating the complex relationship between nutrient gradients and phenotypic switching in bacterial biofilms. By explicitly representing individual cells and their responses to local environmental conditions, IbM provides unique insights into the emergence of persister cells that underlie biofilm antibiotic tolerance. The integration of experimental data with computational models creates a virtuous cycle of hypothesis generation and testing, accelerating our understanding of persistence mechanisms and the development of more effective anti-biofilm strategies.
As experimental techniques for single-cell analysis continue to advance and computational power grows, IbM will play an increasingly central role in bridging molecular mechanisms with population dynamics, ultimately contributing to improved clinical outcomes for biofilm-associated infections. For researchers and drug development professionals, mastering IbM approaches provides a competitive edge in the ongoing battle against antimicrobial tolerance.
Continuum Models Integrating Nutrient Transport with Persister Dynamics
Biofilm-associated infections, particularly on medical implants, represent a significant clinical challenge due to their recalcitrance to antibiotic treatment. A key factor underlying this resilience is the presence of bacterial persister cells—dormant, phenotypic variants that exhibit transient tolerance to antimicrobials without genetic resistance [11] [28]. The formation and maintenance of these persister cells are profoundly influenced by local nutrient availability within the biofilm microenvironment [47] [13] [6]. Traditional biofilm models have largely overlooked the critical role of nutrient-dependent phenotypic switching between proliferative and persister states, creating a knowledge gap in our understanding of biofilm persistence mechanisms [47] [6]. This whitepaper explores the development and application of advanced continuum models that explicitly integrate nutrient transport dynamics with persister cell formation, providing a powerful computational framework for predicting therapeutic intervention points and developing novel treatment strategies for chronic biofilm infections.
Theoretical Foundations of Nutrient-Persister Dynamics
Persister Cell Biology and Nutrient Gradients
Persister cells represent a transient, non-genetic phenotypic variant characterized by metabolic dormancy and extraordinary antibiotic tolerance [11] [28]. Unlike resistant bacteria that grow in the presence of antibiotics, persister cells do not grow when exposed to antimicrobials but can resume growth once the stress is removed [28]. These cells are predominantly found in nutrient-deprived regions of biofilms where limited nutrient availability triggers a dormancy response [47] [6].
The metabolic heterogeneity of persisters is complex, spanning a continuum from completely dormant (Type I) to slow-growing (Type II) states [11]. This heterogeneity is directly influenced by local environmental conditions, particularly nutrient concentration gradients that naturally develop in biofilms due to differential consumption rates from the periphery to the core [47] [13]. As nutrient availability decreases, bacteria employ various sensing mechanisms to activate stress response pathways that ultimately lead to persister formation [13] [6].
Mathematical Framework for Continuum Modeling
Continuum models represent biofilms as continuous materials and describe their evolution using partial differential equations that capture mass conservation and reaction-diffusion dynamics [6]. The fundamental components of these models include:
- Nutrient transport governed by diffusion-reaction equations
- Biomass dynamics for different cellular subpopulations
- Phenotypic switching rates dependent on local nutrient concentrations
- Extracellular polymeric substance (EPS) production and distribution
The general form of the reaction-diffusion equation for nutrients is:
∂C/∂t = ∇·(D∇C) - R(C,B)
Where C is nutrient concentration, D is the diffusion coefficient, and R(C,B) represents nutrient consumption by biomass B [6].
Table 1: Key Variables in Continuum Models of Biofilm-Persister Dynamics
| Variable | Description | Units |
|---|---|---|
| C | Nutrient concentration | mmol/L |
| Bâ‚ | Active bacterial biomass | g/L |
| Bâ‚š | Persister bacterial biomass | g/L |
| B_d | Dead bacterial biomass | g/L |
| E | EPS concentration | g/L |
| D | Effective diffusion coefficient | cm²/s |
| μ_max | Maximum growth rate | 1/h |
| K_s | Half-saturation constant | mmol/L |
Core Model Components and Implementation
Governing Equations and Phenotypic Switching
Advanced continuum models incorporate multiple biomass components that interact through nutrient-dependent processes. The dynamics of proliferative bacteria (Bâ‚), persisters (Bâ‚š), dead cells (B_d), and extracellular polymeric substance (E) are governed by a system of partial differential equations [47] [6]:
∂Bâ‚/∂t = ∇·(DB∇Bâ‚) + μmax(C/(Ks + C))Bâ‚ - kap(C)Bâ‚ + kpa(C)Bâ‚š - kdBâ‚
∂Bₚ/∂t = ∇·(DB∇Bₚ) + kap(C)B₠- k_pa(C)Bₚ
∂E/∂t = ∇·(DE∇E) + γμmax(C/(Ks + C))B₠- kedE
A critical innovation in recent models is the implementation of dual-threshold switching between proliferative and persister phenotypes based on local nutrient concentration [47]. The switching rates kap (active to persister) and kpa (persister to active) are piecewise functions of nutrient concentration C:
kap(C) = kapmax when C < Clow kap(C) = kapmin when C > Chigh
kpa(C) = kpamin when C < Clow kpa(C) = kpamax when C > Chigh
This formulation allows the model to capture adaptive responses across nutrient-poor, intermediate, and nutrient-rich regimes [47].
Numerical Implementation and Computational Tools
Implementing these continuum models requires specialized numerical methods and computational tools. The biofilmFoam toolbox, based on OpenFOAM, provides an efficient framework for simulating these processes in complex geometries by coupling advection-diffusion equations with reaction source terms [48]. Key implementation considerations include:
- Spatial discretization using finite volume methods
- Time integration with adaptive step-sizing for stiffness handling
- Parameter estimation from experimental data
- Validation against experimental biofilm systems
Simulations typically reveal that nutrient limitation produces a high and sustained proportion of persister cells even when overall biomass is reduced, while nutrient-rich conditions support reversion to proliferative growth and lead to greater total biomass [47]. The models also predict that persister populations peak at specific times that vary with nutrient availability, identifying critical intervention windows for antimicrobial therapy [47].
Experimental Validation and Methodologies
Linking Model Predictions with Experimental Observations
Continuum models of nutrient-persister dynamics must be validated against empirical data to ensure biological relevance. Key experimental findings that support model predictions include:
- Carbon source transitions in E. coli biofilms stimulate persister formation through pathways involving ppGpp and nucleoid-associated proteins [13]
- Nutrient-limited regions in biofilms exhibit higher proportions of antibiotic-tolerant cells [47] [6]
- Spatial heterogeneity in metabolic activity correlates with persister distribution patterns [13] [6]
Table 2: Experimental Methods for Validating Nutrient-Persister Models
| Methodology | Application | Key Insights |
|---|---|---|
| Colony biofilm system with controlled nutrient availability [13] | Quantifying persister formation during nutrient transitions | Diauxic shifts stimulate persister formation via ppGpp signaling |
| Fluorescence-activated cell sorting (FACS) of dormant cells [28] | Isolation and transcriptional analysis of persister subpopulations | Dormant cells show elevated expression of toxin-antitoxin system genes |
| Microelectrode measurements of nutrient gradients [6] | Spatial mapping of oxygen and nutrient concentrations in biofilms | Steep nutrient gradients correlate with spatial heterogeneity in metabolic activity |
| Transcriptional reporters (e.g., GFP) [13] | Monitoring metabolic activity and stress response in situ | Nutrient limitation triggers stringent response and dormancy programs |
Protocol: Carbon Source Transition Assay in E. coli Biofilms
This protocol details the experimental methodology for investigating nutrient-dependent persister formation in biofilms, adapted from [13].
Materials and Reagents
Table 3: Essential Research Reagents for Nutrient-Persister Experiments
| Reagent/Equipment | Function | Specifications |
|---|---|---|
| Polyethersulfone (PES) membranes | Support for colony biofilm growth | 0.2 μm pore size, 25 mm diameter |
| M9 minimal medium | Defined growth medium | Supplemented with carbon sources |
| Amplex Red Glucose Kit | Quantifying glucose consumption | Fluorometric measurement |
| Ofloxacin/Ampicillin | Antibiotics for persister enumeration | Concentration: 10 μg/mL and 750 μg/mL respectively |
| Flow cytometer | Analysis of transcriptional reporters | Capable of GFP detection |
Procedure
Strain Preparation: Inoculate E. coli MG1655 from -80°C stock into LB medium and grow for 4 hours at 37°C with shaking at 250 rpm.
Overnight Culture: Dilute the culture 1:100 into 2 mL of 10 mM glucose M9 media and grow overnight for 16 hours at 37°C with shaking.
Biofilm Initiation: Dilute the overnight culture into fresh M9 media containing 15 mM carbon content to OD₆₀₀ = 0.01. Inoculate 100 μL aliquots onto sterile PES membranes positioned on M9 minimal agar plates containing 60 mM carbon source.
Growth Monitoring: Incubate plates at 37°C. Periodically monitor growth by aseptically removing PES membranes, vortexing in 2 mL of sterile PBS for 1 minute, and measuring OD₆₀₀.
Persistence Measurements: At specified growth phases (before and after glucose exhaustion), enumerate persisters by determining colony forming units after exposure to 10 μg/mL ofloxacin or 750 μg/mL ampicillin for 5 hours.
Nutrient Measurement: Quantify glucose concentration in biofilm samples using the Amplex Red Glucose/Glucose Oxidase Kit according to manufacturer instructions.
Data Analysis: Calculate persister frequency as the ratio of CFU after antibiotic treatment to total CFU before treatment. Correlate persister levels with nutrient availability and growth phase.
Molecular Mechanisms and Signaling Pathways
The molecular underpinnings of nutrient-dependent persister formation involve complex signaling networks that translate nutrient limitation into phenotypic switching.
ppGpp-Mediated Stringent Response
The central mediator of nutrient stress response in bacteria is the guanosine tetraphosphate (ppGpp) alarmone, which accumulates during nutrient limitation and activates the stringent response [28] [13]. ppGpp is synthesized by RelA and SpoT enzymes in response to amino acid starvation and other stresses [28]. Elevated ppGpp levels:
- Redirect cellular resources from growth to maintenance
- Activate toxin-antitoxin (TA) systems through proteolytic degradation of antitoxins
- Modulate RNA polymerase activity to alter gene expression profiles
- Promote dormancy entry through metabolic shutdown
Toxin-Antitoxin Systems and Persister Formation
Toxin-antitoxin systems constitute a key mechanistic link between nutrient sensing and persister formation [28]. These systems typically consist of a stable toxin that disrupts essential cellular processes and a labile antitoxin that inhibits toxin activity. Under nutrient-rich conditions, antitoxins neutralize toxins, but during nutrient limitation, activated proteases (e.g., Lon) degrade antitoxins, freeing toxins to induce dormancy [28].
Key TA systems implicated in nutrient-dependent persistence include:
- MqsR/MqsA: MqsR toxin cleaves most cellular transcripts at 5'-GCU sites, dramatically reducing translation
- TisB/IstR-1: TisB toxin decreases proton motive force and ATP levels, inducing energy collapse
- HipA/HipB: HipA phosphorylates translation factor EF-Tu, inhibiting protein synthesis
Implications for Therapeutic Development
The integration of nutrient transport with persister dynamics in continuum models provides valuable insights for developing novel anti-biofilm strategies. Key implications include:
- Timed interventions: Models identify critical windows when persister populations are most vulnerable, suggesting pulsed antibiotic regimens could improve efficacy [47]
- Nutrient modulation: Strategic manipulation of nutrient availability could prevent persister formation or force resuscitation for antibiotic susceptibility [47] [6]
- Combination therapies: Targeting both nutrient pathways and cellular dormancy mechanisms may provide synergistic effects [11] [49]
Continuum models that accurately capture the spatiotemporal dynamics of nutrient-persister relationships represent powerful tools for optimizing these therapeutic approaches and predicting their outcomes across different biofilm microenvironments.
Continuum models integrating nutrient transport with persister dynamics represent a significant advancement in biofilm modeling, addressing a critical gap in understanding how environmental cues govern phenotypic heterogeneity and treatment failure. By explicitly coupling nutrient gradients with phenotypic switching mechanisms, these models provide unprecedented insights into the spatiotemporal dynamics of biofilm persistence and identify novel intervention strategies. Future model development should focus on incorporating multi-species interactions, host-pathogen dynamics, and more sophisticated representations of metabolic networks to further enhance predictive capabilities and clinical relevance.
Linking Model Predictions with Experimental Validation
The persistence of chronic biofilm-associated infections represents a significant challenge in clinical practice. A key factor underlying this resilience is the presence of bacterial persister cells—dormant, phenotypic variants that exhibit remarkable tolerance to conventional antibiotic treatments without possessing genetic resistance mutations [11]. While numerous studies have investigated either mathematical modeling or experimental aspects of biofilm biology, integrating these approaches remains essential for advancing both fundamental understanding and therapeutic development.
This technical guide examines the critical intersection between predictive mathematical modeling and empirical experimental validation within the specific context of nutrient gradient effects on persister formation. We focus specifically on how nutrient availability within biofilm microenvironments drives phenotypic switching between proliferative and persister states—a relationship with profound implications for infection control strategies [6]. For researchers and drug development professionals, mastering this model-experiment integration provides a powerful framework for identifying key therapeutic windows and developing more effective treatments for persistent biofilm infections.
Mathematical Modeling of Nutrient-Persister Dynamics
Foundation of Continuum Biofilm Models
Continuum models provide a well-established framework for simulating biofilm dynamics by treating bacterial populations and extracellular components as continuous fields. These models typically describe system evolution using partial differential equations that account for mass conservation, reaction kinetics, and transport phenomena [6]. In the context of nutrient-persister dynamics, a representative continuum model tracks multiple interacting components:
- Proliferative bacterial cells (B_p): Metabolically active cells responsible for biofilm growth
- Persister cells (B_s): Dormant, antibiotic-tolerant phenotypic variants
- Dead cells (B_d): Non-viable biomass
- Extracellular polymeric substances (EPS): Matrix components providing structural integrity
- Nutrient concentration (c): Rate-limiting substrate governing growth and phenotypic switching
The spatiotemporal dynamics of these components emerge from coupled reaction-diffusion processes, with nutrient gradients developing naturally from the balance between diffusion and consumption.
Incorporating Phenotypic Switching
A critical advancement in contemporary biofilm modeling involves implementing nutrient-dependent phenotypic switching between proliferative and persister states [6]. Unlike earlier models that treated persistence as static, modern approaches define switching rates as functions of local nutrient concentration through threshold-based mechanisms:
- High nutrient conditions: Promote switching from persister to proliferative state
- Low nutrient conditions: Trigger transition from proliferative to persister state
- Critical threshold values: Define boundaries between nutrient regimes
This implementation enables models to capture the essential adaptation of biofilms to fluctuating environmental conditions, particularly the shift toward dormancy under nutrient scarcity that characterizes many chronic infections.
Table 1: Key Variables in Nutrient-Dependent Biofilm Models
| Variable | Description | Units | Typical Range |
|---|---|---|---|
| B_p | Proliferating biomass concentration | mg/cm³ | 0-20 |
| B_s | Persister biomass concentration | mg/cm³ | 0-5 |
| c | Nutrient concentration | mM | 0-10 |
| k_switch→persister | Switching rate to persister state | 1/h | 0.001-0.1 |
| k_switch→proliferative | Switching rate to proliferative state | 1/h | 0.01-0.5 |
| c_low | Lower nutrient threshold for persister formation | mM | 0.05-0.2 |
| c_high | Upper nutrient threshold for proliferative growth | mM | 0.5-2.0 |
Model Predictions on Nutrient Gradients
Simulations based on these mechanistic models generate several fundamental predictions regarding nutrient-persister relationships:
- Spatial organization: Nutrient gradients generate heterogeneous persister distributions, with higher persister proportions in nutrient-depleted biofilm regions [6]
- Temporal dynamics: Persister populations peak at specific timepoints that vary with nutrient availability, creating critical intervention windows [6]
- Biomass relationship: Nutrient limitation produces high persister proportions even when total biomass is reduced, whereas nutrient-rich conditions support greater biomass but lower persister fractions [6]
- Intervention implications: Treatments that modulate nutrient availability may effectively manipulate persister dynamics and enhance antibiotic efficacy
Figure 1: Nutrient-dependent phenotypic switching mechanism between proliferative and persister states. High nutrient conditions promote active proliferation, while nutrient limitation triggers transition to dormant, tolerant persister cells [6].
Experimental Validation Approaches
Quantifying Biofilm Architecture and Composition
Validating model predictions requires sophisticated methodologies for characterizing biofilm spatial organization and compositional heterogeneity:
- Confocal laser scanning microscopy (CLSM): Enables non-destructive, three-dimensional imaging of biofilm architecture
- Fluorescent reporter systems: Employ tissue-specific promoters fused to fluorescent proteins to visualize persister cells in situ
- Image analysis pipelines: Extract quantitative data on biomass distribution, spatial patterns, and microcolony morphology
- Cell sorting techniques: Isolate persister subpopulations for subsequent transcriptomic or proteomic analysis
These techniques collectively enable researchers to map the spatial correlation between nutrient gradients and persister formations predicted by mathematical models [50].
Measuring Nutrient Gradients
Experimental quantification of nutrient gradients presents technical challenges due to the microscale of biofilms and the need for spatial resolution:
- Microsensor technology: Provides direct measurement of chemical gradients (Oâ‚‚, pH, specific nutrients) with micrometer spatial resolution
- Fluorescent nutrient analogs: Enable visualization of nutrient distribution and uptake patterns
- Ratiometric fluorescent reporters: Genetically encoded biosensors that respond to specific metabolite concentrations
- Mass spectrometry imaging: Maps spatial distributions of metabolites and nutrients within biofilm sections
These approaches have confirmed the presence of steep nutrient gradients within biofilms, particularly in thicker, more developed structures where diffusion limitations become significant [6].
Correlating Biomass with Susceptibility
A crucial aspect of experimental validation involves testing the model-predicted relationship between biofilm biomass, nutrient status, and antimicrobial susceptibility. Systematic analysis reveals that the correlation between biofilm biomass and antibiotic susceptibility is highly variable and influenced by multiple factors [51]:
- Microbial species and strain-specific traits
- Antibiotic class and mechanism of action
- Biofilm cultivation conditions and nutrient environment
- Quantification methodologies (crystal violet staining, resazurin viability assay, colony-forming units)
This complexity underscores the importance of standardized protocols and multi-factorial experimental designs when validating model predictions [51].
Table 2: Experimental Methods for Biofilm-Persister Analysis
| Method Category | Specific Techniques | Parameters Measured | Limitations |
|---|---|---|---|
| Spatial Analysis | CLSM, FISH, SEM/TEM | 3D architecture, cell localization | Sample processing artifacts |
| Chemical Imaging | Microsensors, FLIM, MALDI-MSI | Nutrient gradients, metabolite distribution | Limited temporal resolution |
| Compositional Analysis | Flow cytometry, RNA-seq, Proteomics | Persister gene expression, protein profiles | Potential state changes during processing |
| Functional Assays | CFU counting, viability staining, antibiotic challenge | Survival fractions, killing kinetics | Difficulty maintaining in situ conditions |
Integrated Protocols for Model Validation
Protocol: Nutrient Manipulation and Persister Quantification
This protocol provides a methodology for experimentally testing model predictions regarding nutrient effects on persister formation:
Materials:
- Modified continuous flow cell system with controlled nutrient delivery
- Appropriate bacterial strains with selective markers
- Defined growth media with varying nutrient compositions
- Antibiotics for persister selection (typically 10-100× MIC)
- Cell dispersal reagents (sonication, enzymatic treatment)
Procedure:
- Cultivate biofilms under defined nutrient conditions in flow cells for 48-72 hours
- Implement nutrient shift experiments by switching media composition
- At designated timepoints, harvest biofilms and disperse cells mechanically and enzymatically
- Treat dispersed cells with high concentrations of relevant antibiotics for 3-5 hours
- Wash antibiotic and plate serial dilutions on nutrient agar
- Quantify surviving colony-forming units (persisters)
- Perform parallel analysis using live/dead staining and microscopy
Validation Metrics:
- Persister fraction = (CFU after antibiotic treatment) / (total CFU before treatment)
- Spatial distribution of cell states via fluorescent reporters
- Correlation between nutrient depletion zones and persister locations
Protocol: High-Throughput Screening of Anti-Persister Compounds
This protocol enables experimental testing of therapeutic strategies predicted by mathematical models to target nutrient-induced persisters:
Materials:
- 96-well plate biofilm cultivation system
- Library of candidate anti-persister compounds
- Resazurin viability dye or similar metabolic indicator
- Crystal violet staining solution for biomass quantification
- Automated imaging system if available
Procedure:
- Grow biofilms in 96-well plates for 24-48 hours under nutrient-limited conditions
- Treat mature biofilms with compound libraries across concentration gradients
- Include combination therapies with conventional antibiotics
- Assess viability using resazurin reduction assays after compound exposure
- Quantify total biomass using crystal violet staining
- Calculate specific anti-persister efficacy normalized to biomass
- Confirm results with traditional CFU-based persister assays
Validation Metrics:
- Persister eradication efficiency = 1 - (CFU after treatment / CFU before treatment)
- Biomass reduction percentage
- Minimum biofilm eradication concentration (MBEC)
Figure 2: Iterative workflow for integrating mathematical modeling with experimental validation. This cyclic approach enables refinement of both theoretical frameworks and empirical methods [6] [11].
The Scientist's Toolkit: Essential Research Reagents
Table 3: Key Research Reagents for Nutrient-Persister Investigations
| Reagent Category | Specific Examples | Research Application | Technical Considerations |
|---|---|---|---|
| Fluorescent Reporters | GFP, RFP, CFP variants under persister-specific promoters | Visualizing persister cells in situ | Potential metabolic burden, promoter specificity |
| Metabolic Indicators | Resazurin, CTC, SYTOX stains | Differentiating active vs. dormant cells | Dye penetration limitations in thick biofilms |
| Matrix Degradation Enzymes | DNase I, dispersin B, proteinase K | Dispersing biofilms for cell counting | Potential impact on cell viability |
| Nutrient Sensors | FRET-based metabolite biosensors, microelectrodes | Quantifying nutrient gradients | Calibration requirements, spatial resolution limits |
| Phenotypic Switching Inducers | Carbon starvation media, spent media extracts | Controlled induction of persistence | Batch-to-batch variability |
| Anti-Persister Compounds | ADEP4, pyrazinamide, membrane-targeting agents [52] | Evaluating eradication strategies | Cytotoxicity considerations for therapeutic development |
| Mobocertinib | Mobocertinib|High-Quality EGFR Inhibitor|RUO | Mobocertinib is a potent, irreversible EGFR exon 20 insertion mutation inhibitor. For Research Use Only. Not for human or veterinary diagnostic or therapeutic use. | Bench Chemicals |
| Molibresib Besylate | Molibresib Besylate, CAS:1895049-20-3, MF:C28H28ClN5O5S, MW:582.1 g/mol | Chemical Reagent | Bench Chemicals |
Discussion and Future Directions
The integration of mathematical modeling with experimental validation represents a powerful paradigm for advancing our understanding of nutrient-dependent persister formation in biofilms. Several key insights emerge from this synthesis:
First, the predictive capability of mechanistic models provides a framework for designing more informative experiments. Models can identify critical parameter spaces and temporal windows that might otherwise be overlooked in purely empirical approaches [6]. Conversely, experimental data grounds mathematical abstractions in biological reality, revealing unanticipated complexities that drive model refinement.
Second, the iterative nature of this integration accelerates scientific discovery. Initial model predictions guide experimental design, while experimental results inform parameterization and structural improvements to models. This cyclic process progressively enhances both theoretical understanding and methodological sophistication.
Looking forward, several emerging technologies promise to further strengthen this integration:
- Single-cell omics technologies will enable detailed characterization of persister physiology and heterogeneity
- Advanced in situ imaging provides increasingly sophisticated spatial and temporal resolution of biofilm dynamics
- Machine learning approaches can identify complex patterns in large datasets generated by both models and experiments [53]
- Microfluidic systems with precise environmental control allow more rigorous testing of model predictions [50]
For researchers and therapeutic developers, mastering this integrated approach offers a pathway to more effective strategies for combating persistent biofilm infections. By leveraging models to identify critical intervention points and experiments to validate therapeutic approaches, the field can move toward treatments that specifically target the nutrient-responsive mechanisms underlying biofilm resilience.
Overcoming Technical and Biological Hurdles in Persister Eradication
Challenges in Penetrating Biofilm Architecture for Nutrient or Drug Delivery
The structured microbial communities known as biofilms represent a predominant mode of bacterial life and a significant challenge in clinical and industrial settings. These aggregates of microbial cells, encased in a self-produced matrix of extracellular polymeric substances (EPS), demonstrate remarkable resilience to antimicrobial agents and environmental stresses [1] [54]. This resilience is intrinsically linked to the biofilm's complex architecture, which imposes formidable barriers to the penetration of both nutrients and therapeutic compounds. Within the context of a broader investigation into nutrient gradient effects on persister cell formation, understanding these penetration challenges becomes paramount. The spatial organization of biofilms creates heterogeneous microenvironments where steep physical and chemical gradients dictate microbial physiology, leading to the emergence of dormant, tolerant subpopulations that evade conventional treatments [3] [11]. This technical review examines the fundamental barriers within biofilm architecture, the experimental methodologies for studying penetration, and the emerging strategies to overcome these delivery challenges.
Biofilm Architecture and Formation
Structural Components of the Biofilm Matrix
The biofilm matrix is a complex, dynamic assemblage of biopolymers that constitutes the primary physical barrier to penetration. This extracellular polymeric substance (EPS) can comprise over 90% of the biofilm's dry mass [54] and is composed of polysaccharides, lipids, proteins, and extracellular DNA (eDNA) [1] [55]. The specific composition varies significantly based on microbial species, nutrient availability, and environmental conditions [54]. This matrix is not merely a static scaffold but a functional, evolving component continuously remodeled through production and degradation by matrix housekeeping enzymes in response to environmental cues [56].
Table 1: Major Components of the Biofilm Extracellular Matrix
| Matrix Component | Primary Functions | Impact on Penetration |
|---|---|---|
| Polysaccharides | Structural integrity, adhesion, water retention | Creates viscous diffusion barrier, may chelate antimicrobials |
| Extracellular DNA (eDNA) | Structural support, cation sequestration, genetic exchange | Binds cationic antimicrobials (e.g., aminoglycosides), increases density |
| Proteins | Enzymatic activities, structural support | May degrade antimicrobial compounds, contribute to adhesion |
| Lipids | Hydrophobic regions, signaling | Creates hydrophobic barriers affecting compound solubility |
The Biofilm Lifecycle
Biofilm development follows a structured progression through distinct stages:
- Initial Reversible Attachment: Planktonic cells adhere to conditioned surfaces via weak interactions (van der Waals forces, electrostatic interactions) [1].
- Irreversible Attachment: Production of EPS strengthens attachment, transitioning to a sessile lifestyle [1] [54].
- Microcolony Formation & Maturation: Cells proliferate, forming structured communities with characteristic architecture (e.g., mushroom-shaped structures in P. aeruginosa) [54]. Signaling molecules like cyclic diguanylate monophosphate (c-di-GMP) promote this sessile lifestyle [54].
- Dispersion: Active or passive release of cells or clusters to colonize new niches, completing the lifecycle [54].
The following diagram illustrates the key developmental stages and the resulting biofilm architecture with its associated penetration barriers:
Diagram 1: Biofilm lifecycle and mature architecture creating penetration barriers.
Fundamental Barriers to Penetration in Biofilms
Physical and Chemical Barriers
The EPS matrix acts as a formidable physical barrier through several mechanisms. Its dense, viscous structure significantly retards the diffusion of antimicrobial molecules, often preventing lethal concentrations from reaching embedded cells [54]. Certain antibiotics, particularly positively charged aminoglycosides, can bind to negatively charged biopolymers like eDNA within the matrix, effectively neutralizing them before they reach their cellular targets [57] [54]. Furthermore, the matrix may contain extracellular enzymes capable of inactivating or degrading antimicrobial compounds [54].
Beyond the EPS, the host environment contributes additional barriers. In respiratory infections, the airway mucus gel layer traps inhaled particles and pathogens, transporting them out via ciliary beating [57]. In diseases like cystic fibrosis (CF) and chronic obstructive pulmonary disease (COPD), this mucus becomes pathologically thick and viscous, with reduced pore sizes (often < 100 nm) that severely restrict nanoparticle access to underlying biofilms [57]. Neutrophil extracellular traps (NETs), released by infiltrating immune cells, further increase mucus viscoelasticity and contribute to the physical shield protecting biofilms from antimicrobials [57] [54].
Physiological Heterogeneity and Persister Cell Formation
As depicted in Diagram 1, metabolic gradients within the biofilm architecture lead to profound physiological heterogeneity. The primary consumption of oxygen by cells in the outer layers creates oxygen concentration gradients that decrease with depth [3]. This results in subzones with distinct microbial physiologies: metabolically active cells in oxygen-rich areas and slow-growing or dormant persister cells in nutrient-poor, anoxic regions [3] [11] [6].
Persisters are non-growing or slow-growing, genetically drug-susceptible bacteria that survive antibiotic exposure and can regrow after its removal, underlying many chronic and relapsing infections [11]. This phenotypic tolerance is distinct from genetic resistance and is a direct consequence of the heterogeneous microenvironment shaped by penetration-limited nutrient gradients. Mathematical models that couple nutrient transport with bacterial dynamics confirm that nutrient limitation produces a high and sustained proportion of persister cells, even when overall biomass is reduced [6].
Table 2: Quantitative Analysis of Biofilm Penetration Barriers
| Barrier Type | Measurable Impact | Experimental Evidence |
|---|---|---|
| Diffusion Limitation | Up to 1000-fold increase in antibiotic resistance compared to planktonic cells [57] | Altered diffusion coefficients for antibiotics through EPS matrices |
| Matrix Binding | Significant reduction in aminoglycoside bioavailability due to eDNA binding [54] | Fluorescence correlation spectroscopy showing reduced mobility |
| Metabolic Gradients | Formation of ~10-40% persister cells in nutrient-poor zones [11] [6] | Microelectrode measurements of Oâ‚‚ gradients; reporter strains showing heterogeneous gene expression |
| Mucus Barrier | Pore sizes < 100 nm in CF sputum, restricting nanoparticle diffusion [57] | Multiple particle tracking showing reduced nanoparticle mobility |
Experimental Methods for Assessing Biofilm Penetration
Quantitative Biofilm Characterization Techniques
Researchers employ diverse methodologies to quantify biofilm growth and assess penetration. Classical methods include colony forming unit (CFU) counting to determine viable cell numbers and crystal violet staining to measure total biofilm biomass [58]. More advanced techniques offer real-time monitoring and higher resolution:
- ATP Bioluminescence: Measures metabolically active cells through adenosine triphosphate quantification [58].
- Quartz Crystal Microbalance: Detects mass accumulation on surfaces in real-time by measuring changes in resonance frequency [58].
- Flow-based Cell Counting (Coulter counting, flow cytometry): Provides automated enumeration of cells from homogenized biofilms, though cannot differentiate live/dead cells without specific stains [58].
Morphological and Chemical Characterization
Understanding biofilm architecture requires techniques that reveal structural details:
- Scanning Electron Microscopy (SEM): Provides high-resolution, detailed images of biofilm surface topology [58].
- Confocal Scanning Laser Microscopy (CSLM): Enables non-invasive, three-dimensional visualization of hydrated biofilms, often using fluorescent markers to distinguish live/dead cells or specific matrix components [58].
- Spectroscopic Methods: Fourier-transform infrared (FTIR) and Raman spectroscopy can characterize the chemical composition of the EPS matrix [58].
The following workflow integrates these methods into a coherent experimental pipeline for evaluating anti-penetration strategies:
Diagram 2: Experimental workflow for assessing penetration and efficacy.
The Scientist's Toolkit: Key Reagents and Materials
Table 3: Essential Research Reagents for Biofilm Penetration Studies
| Reagent/Material | Function in Research | Specific Application Examples |
|---|---|---|
| Crystal Violet | Stains total biofilm biomass | Quantitative assessment of biofilm formation in microtiter plate assays [58] |
| Resazurin (Alamar Blue) | Metabolic activity indicator | Measures cell viability without biofilm disruption [58] |
| SYTO 9/Propidium Iodide | Nucleic acid stains for live/dead differentiation | Confocal microscopy visualization of cell viability spatial distribution [58] |
| DNase I | Degrades extracellular DNA (eDNA) in matrix | Disrupts matrix integrity to enhance antimicrobial penetration [54] |
| Dispersin B | Glycoside hydrolase targeting polysaccharide matrix | Induces biofilm dispersal; studies matrix role in protection [54] |
| Mucin-based Hydrogels | Simulates pathological mucus barrier | In vitro testing of drug delivery system penetration through mucus [57] |
| Fluorescently-labeled Dextrans | Diffusion tracers of varying sizes | Quantifies pore size and diffusion barriers in biofilm/mucus [57] |
| Momipp | MOMIPP|Methuosis Inducer|Caspase-Independent Cell Death | MOMIPP is a potent inducer of methuosis, a non-apoptotic cell death. This indolyl-chalcone is for research into apoptosis-resistant cancer pathways. For Research Use Only. Not for human or veterinary use. |
| MP-A08 | MP-A08, MF:C27H25N3O4S2, MW:519.6 g/mol | Chemical Reagent |
Emerging Strategies to Overcome Penetration Barriers
Nanotechnology-Based Delivery Systems
Nanoparticles (NPs) offer promising approaches to circumvent biofilm penetration barriers. Their small size, high surface area, and modifiable surfaces enable improved diffusion through EPS and mucus matrices [57] [55]. Key nanocarriers under investigation include:
- Metal and Metal Oxide Nanoparticles (e.g., silver, zinc oxide): Intrinsic antimicrobial activity combined with drug delivery capability [55].
- Liposomes: Phospholipid bilayers that can encapsulate both hydrophilic and hydrophobic antibiotics, fusing with bacterial membranes to enhance delivery [55].
- Polymeric Nanoparticles: Biodegradable particles (e.g., PLGA) allowing sustained release and surface functionalization for targeted delivery [57] [55].
- Solid Lipid Nanoparticles: Offer improved stability and high payload capacity for lipophilic compounds [55].
These nanosystems can be engineered to be smaller than the mesh pore size of mucus (enabling mucopenetration) or to exhibit minimal adhesion to mucus components (mucoinert) through surface PEGylation [57].
Adjunctive Therapies and Alternative Approaches
Combination strategies that disrupt the biofilm matrix simultaneously with antimicrobial delivery show enhanced efficacy:
- EPS-degrading Enzymes: DNase I to break down eDNA networks or glycoside hydrolases to target polysaccharides can compromise matrix integrity and enhance penetration of co-administered antimicrobials [54].
- Quorum Sensing Inhibitors: Interfere with bacterial cell-to-cell communication systems that coordinate biofilm behaviors, potentially reducing matrix production and increasing susceptibility [59].
- Physical Methods: Ultrasound creates cavitation bubbles that can disrupt biofilm integrity, while ultraviolet (UVC) or visible violet/blue light inactivates microorganisms through DNA damage or reactive oxygen species generation [1] [56].
The challenges in penetrating biofilm architecture for nutrient or drug delivery stem from a multifaceted defense system incorporating physical diffusion barriers, chemical interactions, and physiological heterogeneity. The extracellular matrix acts as a molecular sieve and deactivation zone, while the resulting nutrient gradients drive the formation of treatment-resistant persister cells. Overcoming these barriers requires sophisticated approaches that address both the physical penetration limitations and the biological heterogeneity. Emerging strategies leveraging nanotechnology, matrix-disrupting enzymes, and combination therapies show promise in enhancing delivery efficacy. Future research should continue to integrate mathematical modeling with experimental validation to optimize interventions that can effectively navigate the complex topography of biofilms and ultimately overcome the recalcitrance of biofilm-associated infections.
Limitations of Conventional Antibiotics Against Dormant Cells
The efficacy of conventional antibiotics is fundamentally constrained by their limited activity against dormant bacterial cells, a phenomenon that poses significant challenges in treating chronic and recurrent infections. While antibiotic resistance has garnered substantial attention, the problem of bacterial persistence represents a distinct therapeutic hurdle. Persisters are metabolically inactive phenotypic variants that can survive antibiotic exposure without undergoing genetic resistance mutations [11] [28]. These cells exist in a transient, non-growing or slow-growing state that protects them from antibiotics that typically target active cellular processes, only to resume growth after treatment cessation, leading to relapsing infections [60].
This technical review examines the limitations of conventional antibiotics against dormant cells within the specific context of nutrient gradient effects on persister formation in biofilms. Understanding these mechanisms is critical for researchers and drug development professionals working to overcome treatment failures in persistent infections such as tuberculosis, recurrent urinary tract infections, and biofilm-associated conditions [11]. The following sections analyze the molecular basis of antibiotic failure, the role of biofilm microenvironments, and the experimental approaches driving discovery in this field.
Molecular Mechanisms of Antibiotic Failure Against Dormant Cells
Fundamental Distinctions: Persistence Versus Resistance
Bacterial persistence differs fundamentally from antibiotic resistance, both mechanistically and therapeutically. Antibiotic resistance involves stable genetic changes that enable bacteria to grow in the presence of antibiotics, typically through specific mechanisms such as drug inactivation, target modification, enhanced efflux, or reduced permeability [60] [61]. In contrast, antibiotic persistence represents a transient, phenotypically tolerant state where dormant cells survive antibiotic exposure despite maintaining genetic susceptibility to the drug [11]. This distinction has profound clinical implications: while resistance is specific to particular drug classes, persistence confers broad tolerance to diverse antibiotics, complicating treatment strategies [60].
The table below summarizes key differences between antibiotic resistance and persistence:
Table 1: Comparative Analysis of Antibiotic Resistance and Persistence
| Characteristic | Antibiotic Resistance | Antibiotic Persistence |
|---|---|---|
| Genetic basis | Stable genetic mutations | Transient phenotypic variation |
| Heritability | Stable across generations | Reversible; not inherited |
| Population size | Entire population | Small subpopulation (typically 0.1%-1%) |
| Mechanism | Target modification, drug inactivation, efflux pumps | Dormancy, reduced metabolic activity, active efflux |
| Drug specificity | Often drug-class specific | Broad, multi-drug tolerance |
| Concentration dependence | Survive at above-MIC concentrations | Survive at both above- and below-MIC concentrations |
| Clinical manifestation | Treatment failure from outset | Relapsing infections after initial treatment success |
Mechanisms Underlying Antibiotic Tolerance in Dormant Cells
Passive Tolerance Through Cellular Dormancy
The primary mechanism protecting persister cells from antibiotic killing is greatly reduced metabolic activity, which diminishes the efficacy of antibiotics that target active cellular processes [28]. Most conventional antibiotics require bacterial cells to be actively growing to exert their lethal effects. For instance, β-lactam antibiotics target cell wall synthesis in actively dividing bacteria, while aminoglycosides require active uptake and interaction with functional ribosomes [11]. In dormant persisters, these processes are minimal or suspended, creating a passive defense mechanism against antibiotic-mediated killing [62].
A 2025 study challenged the conventional view that only a small subset of hyper-resilient "persister" bacteria survive antibiotic treatment [63]. Instead, researchers found that under nutrient-scarce conditions mimicking infection environments, the majority of bacterial populations can survive antibiotic exposure due to slowed growth. As lead researcher Professor Dirk Bumann explained, "Under nutrient-scarce conditions, bacteria grow very slowly. This may seem good at first, but is actually a problem because most antibiotics only gradually kill slowly growing bacteria" [63].
Active Defense Mechanisms in Persister Cells
Contrary to the traditional view of persisters as entirely passive, recent research reveals they employ active defense mechanisms to enhance their survival. One significant finding is that some persister cells maintain enhanced efflux pump activity even in their dormant state, actively expelling antibiotics from the cell interior [62]. This combination of passive dormancy and active efflux creates a formidable barrier to antibiotic efficacy.
Additionally, persister cells utilize sophisticated molecular mechanisms to maintain their dormant state and coordinate population survival. Key among these are:
Toxin-Antitoxin (TA) Modules: These genetic elements consist of a stable toxin that disrupts essential cellular processes and a labile antitoxin that neutralizes the toxin [28]. Under stress conditions, antitoxins are degraded, allowing toxins to induce dormancy. Type II TA systems are particularly important, where protein antitoxins inhibit protein toxins through direct binding [11]. The HipA toxin, for instance, inhibits translation by phosphorylating elongation factor EF-Tu, while MqsR cleaves cellular mRNAs, effectively halting growth [28] [60].
Stringent Response and ppGpp Signaling: Nutrient limitation triggers the stringent response, mediated by the alarmone guanosine tetraphosphate (ppGpp) [28] [60]. ppGpp acts as a central regulator of bacterial persistence, dramatically reprogramming cellular metabolism toward dormancy by redirecting transcription away from growth-related genes toward stress response and maintenance pathways [60] [29].
Nutrient Gradients and Persister Formation in Biofilms
Biofilm Microenvironments as Persister Nurseries
Biofilms represent a primary source of persistent infections in clinical settings, with their structured communities of bacteria encased in an extracellular matrix providing ideal conditions for persister formation [11] [3]. The physical and chemical heterogeneity within biofilms creates microenvironments that strongly influence bacterial physiology and antibiotic tolerance [3]. Biofilm architecture leads to resource gradients including oxygen, nutrients, and metabolic waste products that vary spatially and temporally within the community [3].
The matrix itself contributes to antibiotic tolerance by imposing a diffusion barrier that limits antibiotic penetration, though this appears secondary to the physiological changes induced by gradient formation [3]. As nutrients become depleted in deeper biofilm regions, cells enter slowed or arrested growth states that inherently protect them from antibiotic killing [63]. This gradient-induced physiological heterogeneity means that biofilm subpopulations experience different microenvironments, leading to division-of-labor where some cells maintain active growth while others enter persistent states [3].
Nutrient Transitions as Persister Induction Signals
Nutrient transitions represent a specific stimulus for persister formation within biofilms. Research has demonstrated that diauxic carbon source shifts actively stimulate persister formation in Escherichia coli biofilms through a pathway involving ppGpp and nucleoid-associated proteins (FIS and HU) [29]. This finding is particularly significant because nutrient transitions occur naturally in biofilms as peripheral cells consume preferred substrates, leaving less favorable nutrients for interior cells [29].
The metabolic reprogramming during nutrient transitions involves redirecting cellular resources from growth to maintenance, effectively inducing a dormant state that protects against antibiotic killing [29]. This mechanism demonstrates that persistence is not merely a stochastic phenomenon but can be actively triggered by environmental cues commonly encountered in infection sites.
Table 2: Quantitative Data on Antibiotic Survival in Bacterial Persisters
| Bacterial Species | Antibiotic Challenge | Survival Rate (%) | Key Tolerance Mechanism | Experimental Context |
|---|---|---|---|---|
| Salmonella enterica | Multiple antibiotics | Majority of population | Nutrient starvation-induced slow growth | Mouse infection model [63] |
| Escherichia coli | Ampicillin | Up to 1% (hipA7 mutant) | Toxin-antitoxin module (HipBA) activation | Planktonic culture [11] |
| Escherichia coli | Ofloxacin | 20-fold increase in survival | Dormancy via MqsR toxin mRNA cleavage | Fluorescence-activated cell sorting [28] |
| Pseudomonas aeruginosa | Multiple antibiotics | 100x higher after long-term treatment | Biofilm-induced persistence, not MIC change | Clinical isolates from long-term treatment [60] |
| Escherichia coli | Multiple antibiotics | Significant increase | Carbon source transition via ppGpp/NAP pathway | Colony biofilms [29] |
Experimental Approaches for Studying Persister Cells
Methodologies for Investigating Nutrient Gradient Effects
Research into nutrient gradient effects on persister formation requires specialized methodologies that replicate key aspects of biofilm environments while allowing controlled experimentation:
Colony Biofilm Systems: These models employ bacteria grown on semi-permeable membranes placed on agar plates, enabling precise control over nutrient availability while maintaining biofilm-like community structures [29]. This approach allows researchers to introduce specific nutrient transitions and monitor subsequent physiological responses.
Real-Time Single-Cell Analysis: Advanced imaging techniques combined with fluorescent reporter systems enable monitoring of persister dynamics at single-cell resolution [63]. This methodology revealed that traditional persistence assays underestimate surviving bacteria and falsely suggest hyper-resilient subpopulations [63].
Chemical Gradient Microfluidics: Microfabricated devices create stable nutrient gradients across bacterial populations, permitting high-resolution observation of how localized microenvironments influence persister formation [60].
The diagram below illustrates a representative experimental workflow for studying nutrient transition effects on persister formation in biofilms:
The Scientist's Toolkit: Essential Research Reagents and Methods
Investigating persister formation in response to nutrient gradients requires specialized reagents and methodologies. The following table compiles key experimental resources used in foundational studies:
Table 3: Essential Research Reagents and Methods for Persister Studies
| Reagent/Method | Function/Application | Representative Use |
|---|---|---|
| PES Membranes | Support for colony biofilm growth | Provides semi-permeable surface for controlled nutrient diffusion in biofilm studies [29] |
| GFP Reporter Systems | Visualizing gene expression and protein localization | Monitoring promoter activity and protein expression in single cells during nutrient transitions [29] |
| ppGpp Mutants (ΔrelA, ΔspoT) | Investigating stringent response mechanisms | Dissecting role of alarmone signaling in persistence during nutrient limitation [60] [29] |
| TA System Mutants | Determining toxin-antitoxin module contributions | Establishing molecular pathways for dormancy induction (e.g., hipA, mqsR mutants) [28] [60] |
| Carbon Source Variants | Creating controlled nutrient transitions | Inducing diauxic shifts that stimulate persister formation (e.g., glucose to fumarate) [29] |
| Fluorescence-Activated Cell Sorting (FACS) | Isolating subpopulations based on metabolic activity | Separating dormant versus active cells for transcriptomic and proteomic analysis [28] |
| Microfluidic Gradient Devices | Establishing stable nutrient gradients | Creating controlled microenvironments to study spatial aspects of persistence [60] |
Visualization of Key Signaling Pathways in Persister Formation
The molecular pathways connecting nutrient sensing to persister formation involve interconnected signaling systems that integrate environmental cues with physiological responses. The diagram below illustrates the primary pathway through which nutrient limitations lead to antibiotic tolerance:
This pathway illustrates how nutrient limitation initiates a cascade of molecular events culminating in antibiotic tolerance. The process begins with nutrient sensing and activation of stress responses, leading to ppGpp accumulation—the central mediator of the stringent response [60]. ppGpp then coordinates multiple downstream effects, including activation of toxin-antitoxin systems through Lon-mediated antitoxin degradation and modulation of nucleoid-associated proteins (NAPs) that reorganize chromosomal DNA and global transcription patterns [28] [29]. These changes collectively drive metabolic downshifting and enhanced efflux activity, establishing a dormant cellular state capable of surviving antibiotic exposure [62].
The limitations of conventional antibiotics against dormant bacterial cells represent a fundamental challenge in infectious disease management. The mechanisms underlying this tolerance—particularly in the context of nutrient gradient-induced persistence in biofilms—highlight the need for innovative therapeutic approaches that target the unique biology of persister cells.
Future research directions should focus on: (1) developing compounds that disrupt ppGpp-mediated stringent response signaling; (2) creating efflux pump inhibitors specifically designed to function against dormant cells; (3) designing combination therapies that simultaneously target both active and dormant bacterial subpopulations; and (4) exploiting metabolic priming strategies that force persisters out of dormancy before antibiotic administration.
The growing understanding of how nutrient gradients drive persister formation in biofilms provides promising targets for next-generation antimicrobials that could potentially overcome the limitations of conventional antibiotics and address the clinical challenge of relapsing, persistent infections.
Bacterial persister cells and biofilms represent a critical therapeutic challenge, contributing significantly to chronic and recalcitrant infections. This review examines two promising strategic approaches to eradicate these treatment-refractory bacterial populations: membrane-targeting antimicrobial agents and precision-activated prodrug systems. The development of these strategies is contextualized within the fundamental understanding that nutrient gradients within biofilms drive phenotypic heterogeneity, including the formation of dormant, antibiotic-tolerant persister cells. We synthesize recent advances in compound discovery, delivery platforms, and mechanistic insights, providing a technical guide for researchers aiming to develop novel anti-persister therapeutics. The article integrates quantitative efficacy data, detailed experimental methodologies, and visual schematics of mechanisms and workflows to serve as a comprehensive resource for drug development professionals.
Bacterial biofilms are structured microbial communities encased in a self-produced extracellular polymeric substance (EPS) matrix, constituting a protected mode of growth that is highly tolerant to antimicrobials and host immune responses [1] [54]. A key factor in biofilm resilience is the presence of persister cells—dormant, non-growing phenotypic variants that exhibit exceptional tolerance to conventional antibiotics, which typically target active cellular processes [64] [65].
The formation and distribution of persisters within biofilms are not random but are intrinsically linked to heterogeneous microenvironmental conditions created by the biofilm structure. Nutrient and oxygen gradients generate distinct physiological zones, compelling subpopulations of bacteria to enter a metabolically dormant state in nutrient-deprived regions [3] [6]. This nutrient-dependent phenotypic switching is a fundamental survival strategy, allowing the biofilm community to withstand starvation and other stresses [65]. Consequently, effective anti-biofilm strategies must account for and target these specialized, dormant subpopulations and overcome the physical barrier of the EPS matrix.
Membrane-Targeting Antimicrobial Agents
Traditional antibiotics often fail against persisters due to their reliance on bacterial growth for efficacy. Membrane-active compounds present a compelling alternative by targeting the fundamental structural integrity of the bacterial membrane, a mechanism that is effective independently of bacterial metabolic state.
Mechanism of Action and Selectivity
Membrane-targeting agents like the repurposed anthelmintic drug bithionol kill methicillin-resistant Staphylococcus aureus (MRSA) persisters by disrupting the lipid bilayer of bacterial membranes [64]. The key to their therapeutic potential is selective disruption of bacterial membranes over mammalian membranes. All-atom molecular dynamics simulations demonstrate that bithionol penetrates and embeds in bacterial-mimic lipid bilayers but is excluded from cholesterol-rich mammalian-mimic lipid bilayers [64]. The insertion of bithionol into bacterial membranes increases membrane fluidity, causes rapid permeabilization, and leads to cell death, correlating directly with its antipersister potency.
Quantitative Efficacy of Bithionol
Table 1: Efficacy Profile of Bithionol Against MRSA
| Strain / Model | Condition | Metric | Result |
|---|---|---|---|
| MRSA MW2 | Exponential Phase | MIC | 0.5 - 2 µg/mL [64] |
| MRSA MW2 | Exponential Phase | Killing Kinetics (10x MIC) | Eradicated ~10â· CFU/mL within 3 h [64] |
| MRSA MW2 | Planktonic Persisters | Eradication (32x MIC) | Complete eradication within 2 h [64] |
| MRSA MW2 | Biofilm Persisters | Eradication (32x MIC) | Complete eradication within 24 h [64] |
| VRSA VRS1 | Planktonic Persisters | Activity (32x MIC) | Significant killing; superior to linezolid & daptomycin [64] |
| Mouse Model | Chronic Deep-Seated MRSA | Combination with Gentamicin | Effective reduction of bacterial burdens [64] |
Experimental Protocol: Evaluating Membrane-Targeting Agents
Objective: To assess the efficacy of a membrane-targeting compound against bacterial persister cells in planktonic and biofilm states.
Materials:
- Bacterial Strains: e.g., MRSA strain MW2, VRSA strain VRS1.
- Test Compound: e.g., Bithionol (CAS No. 97-18-7).
- Control Antibiotics: Vancomycin, daptomycin, linezolid.
- Media: Cation-adjusted Mueller-Hinton broth (CA-MHB) for MIC and killing kinetics.
- Specialized Reagents: SYTOX Green stain for membrane permeability assessment.
Methodology:
- Persister Cell Preparation:
- Minimum Inhibitory Concentration (MIC): Determine MIC against exponentially growing cells using standard broth microdilution according to CLSI guidelines [64].
- Time-Kill Kinetics Assay:
- Expose persister preparations (planktonic or biofilm) to the test compound at multiples of the MIC (e.g., 10x, 32x).
- Incubate and sample at predetermined time points (e.g., 0, 2, 3, 6, 24 h).
- Quantify viable counts by plating serial dilutions on agar and enumerating CFU/mL [64].
- Mechanistic Studies:
- Membrane Permeability: Incubate bacteria with SYTOX Green and the test compound. Monitor fluorescence increase over time, as SYTOX Green fluoresces upon binding to DNA after membrane disruption [64].
- Transmission Electron Microscopy (TEM): Fix treated and untreated cells, embed, section, and visualize to observe ultrastructural damage to membranes [64].
Diagram Title: Selective Mechanism of Membrane-Targeting Antimicrobials
Prodrug Strategies for Targeted Biofilm Eradication
Prodrug approaches aim to achieve localized activation of antimicrobials at the infection site, mitigating systemic toxicity and enabling the use of higher effective doses precisely where needed.
Enzyme-Prodrug Therapy (EPT) and Surface-Mediated Activation
EPT is a two-stage strategy involving a localized enzyme that activates a systemically administered inert prodrug. A specific adaptation for implants is Substrate-Mediated Enzyme Prodrug Therapy (SMEPT), where the activating enzyme is immobilized on the biomaterial surface [66].
Glucuronide Prodrugs of Fluoroquinolones: Stable prodrugs for ciprofloxacin and moxifloxacin were synthesized using a self-immolative linker (SIL) based on p-hydroxybenzyl alcohol (PHBA) to bridge the glucuronic acid mask and the antibiotic [66]. This design ensures stability in circulation and specific activation by β-glucuronidase (β-Glu) enzyme coatings on the implant.
Biorthogonal Catalytic Activation: An alternative approach uses abiotic catalysts, such as palladium nanosheets (PdNS), embedded in hydrogel coatings on implants [67]. These catalysts activate propargylated fluoroquinolone prodrugs (e.g., Cipro-Pro 2, Moxi-Pro 1) via depropargylation reactions directly at the implant surface, preventing biofilm formation.
Quantitative Efficacy of Prodrug Systems
Table 2: Efficacy Profile of Fluoroquinolone Prodrugs
| Prodrug / System | Test Model | Key Metric | Performance |
|---|---|---|---|
| Cipro-Pro 2 (N-modified) | S. aureus (Planktonic) | MIC | >64 µg/mL (vs. Ciprofloxacin MIC = 0.5 µg/mL) [67] |
| Moxi-Pro 1 (N-modified) | S. aureus (Planktonic) | MIC | >64 µg/mL (vs. Moxifloxacin MIC = 0.06 µg/mL) [67] |
| Cipro-Pro 2 (N-modified) | S. aureus Biofilm | MBIC | 8-fold higher than parent ciprofloxacin [67] |
| Moxi-Pro 1 (N-modified) | S. aureus Biofilm | MBIC | >60-fold higher than parent moxifloxacin [67] |
| PdNS-90 Hydrogel + Moxi-Pro 1 | S. aureus Biofilm Prevention | Biofilm Inhibition | ~90% reduction vs. control [67] |
| Enzyme Coating + Glucuronide Prodrug | Planktonic Bacteria | Zone of Inhibition | Pronounced bacterial growth inhibition around coated biomaterial [66] |
Experimental Protocol: Developing and Testing Catalytic Prodrug Systems
Objective: To synthesize and evaluate the efficacy of a Pd-catalyzed prodrug system for preventing biofilm formation on coated surfaces.
Materials:
- Prodrugs: Synthesized Cipro-Pro 2 or Moxi-Pro 1 (propargylated fluoroquinolones) [67].
- Catalyst: Pd(0) Nanosheets (PdNS), synthesized using tungsten hexacarbonyl (W(CO)₆) and citric acid [67].
- Coating Substrate: Agarose hydrogel.
- Bacterial Strain: Staphylococcus aureus.
- Analytical Tools: HPLC, Mass Spectrometry (MS) for prodrug conversion analysis.
Methodology:
- Synthesis of Pd Nanosheets (PdNS):
- Use W(CO)₆ as a reducing agent and poly-(vinylpyrrolidone) (PVP) as a stabilizer in a water/methanol mixture.
- Vary the amount of citric acid (e.g., 90 mg vs. 170 mg) to control nanosheet size (e.g., ~17 nm vs. ~9 nm edge length) [67].
- Characterize size and morphology via Transmission Electron Microscopy (TEM) and High-Angle Annular Dark-Field Scanning TEM (HAADF-STEM).
- Prodrug Synthesis and Validation:
- Modify fluoroquinolone antibiotics (ciprofloxacin, moxifloxacin) at the secondary amine with a propargyl moiety via a self-immolative linker [67].
- Confirm loss of antibiotic activity (MIC, MBIC) and lack of cytotoxicity (e.g., using HepG2 cells).
- Catalytic Activity and Release Kinetics:
- Load PdNS into agarose hydrogels.
- Quantify prodrug conversion using a fluorescent reporter (e.g., pro-coumarin) or direct quantification of active antibiotic release via HPLC/MS [67].
- Biofilm Prevention Assay:
- Coat surfaces with PdNS-loaded hydrogel.
- Treat with prodrug (e.g., 5 µM) for 0-8 hours.
- Inoculate with S. aureus and incubate for 24 hours to allow biofilm formation.
- Quantify biofilm biomass using a metabolic dye like CellTiter-Blue [67].
Diagram Title: Prodrug Activation on Implant Surface to Prevent Biofilms
The Scientist's Toolkit: Key Research Reagents and Materials
Table 3: Essential Reagents for Anti-Persister and Anti-Biofilm Research
| Reagent / Material | Function / Application | Specific Examples / Notes |
|---|---|---|
| Membrane-Targeting Compounds | To kill persister cells via membrane disruption. | Bithionol, nTZDpa, synthetic retinoids. Check for selectivity against mammalian membranes [64]. |
| Propargylated Prodrugs | Inactive precursors for localized activation. | Cipro-Pro 2, Moxi-Pro 1. Require custom synthesis with a self-immolative linker [67]. |
| Palladium Nanosheets (PdNS) | Abiotic catalyst for biorot-hogonal prodrug activation on surfaces. | Synthesized using W(CO)₆ and citric acid. Size can be tuned by varying reactant ratios [67]. |
| β-Glucuronidase (β-Glu) | Enzyme for activating glucuronide-based prodrugs in EPT. | Can be immobilized on biomaterial surfaces for SMEPT [66]. |
| SYTOX Green | Fluorescent nucleic acid stain for assessing membrane integrity/permeability. | Fluorescence increases upon entering cells with compromised membranes [64]. |
| Extracellular Polymeric Substances (EPS) | Matrix components to study antibiotic penetration and binding. | eDNA, polysaccharides (PIA/PNAG), proteins. Can bind antibiotics like aminoglycosides [1] [54]. |
The relentless challenge of biofilm-associated and chronic infections demands innovative strategies that move beyond conventional antibiotic paradigms. Membrane-targeting agents and precision-activated prodrug systems represent two highly promising, mechanistically distinct avenues to address the core problems of physiological heterogeneity, dormancy, and physical protection in biofilms. The critical role of nutrient gradients in driving persister formation underscores the necessity for such targeted approaches. Future success in this field will rely on the continued integration of mechanistic biology, sophisticated materials science, and rigorous in vitro and in vivo validation, as exemplified by the strategies and methodologies detailed in this review.
Bacterial persisters are growth-arrested, dormant phenotypic variants found in essentially all bacterial populations that exhibit tolerance to high doses of conventional antibiotics without genetic mutation [52] [27]. These metabolically quiescent cells can survive antibiotic exposure and regenerate bacterial populations once treatment ceases, posing a critical challenge in treating chronic and biofilm-associated infections [11]. In biofilm environments, nutrient gradients create heterogeneous microenvironments that significantly influence persister dynamics [11]. The outer layers of biofilms, with greater access to nutrients, typically contain metabolically active cells, while oxygen and nutrient depletion in deeper zones induces a dormant state, fostering higher persister formation [11]. This spatial distribution of metabolic states within biofilms, driven by nutrient gradients, establishes reservoirs of recalcitrant cells that contribute to chronic infections and treatment failure [68]. Understanding these microenvironments is fundamental to developing strategies that disrupt persister formation and reactivation mechanisms.
Current Strategies for Persister Control
Direct Killing Approaches
Direct killing strategies target growth-independent cellular structures in persister cells, primarily focusing on membrane disruption and protein degradation [52] [27]. These approaches are particularly valuable as they bypass the need for metabolic activity in target cells.
Table 1: Compounds for Direct Killing of Persister Cells
| Compound Class | Example Agents | Mechanism of Action | Target Pathogens |
|---|---|---|---|
| Membrane-Targeting Compounds | XF-70, XF-73, SA-558 | Disrupt cell membrane integrity; some generate ROS | S. aureus [52] |
| Nanoparticle Systems | Hb-Naf@RBCM NPs, C-AgND | Disrupt membrane and EPS layer; deliver antimicrobials | S. aureus biofilms [52] |
| Protein Degradation Activators | ADEP4 | Activates ClpP protease, causing uncontrolled protein degradation | Broad-spectrum [52] |
| Antimetabolites | Pyrazinamide (active form: pyrazinoic acid) | Disrupts membrane energetics; triggers PanD degradation | M. tuberculosis [52] |
The therapeutic potential of membrane-active compounds can be limited by off-target toxicity against mammalian membranes [52]. Consequently, research continues to identify persister-specific targets that enable selective eradication without host cell damage.
Inhibition of Persister Formation
Preventing the formation of persister cells represents a proactive strategy for combating bacterial tolerance. Several approaches target the metabolic and signaling pathways that drive the transition to dormancy.
Table 2: Strategies to Inhibit Persister Formation
| Strategy | Key Agents/Approaches | Mechanism | Evidence |
|---|---|---|---|
| Metabolic Modulation | Pheromone cCf10 | Reduces (p)ppGpp alarmone accumulation | Enterococcus faecalis [52] |
| Hâ‚‚S Pathway Targeting | CSE inhibitors, Hâ‚‚S scavengers | Reduce endogenous Hâ‚‚S that protects under stress | S. aureus, P. aeruginosa, E. coli [52] |
| Membrane Potential Disruption | Pinaverium bromide (PB) | Disrupts proton motive force (PMF), generates ROS | Reduced persister formation [52] |
| Fatty Acid Interventions | Undecanoic acid, lauric acid | Reduce persister formation through undefined mechanisms | Multiple species [52] |
| Quorum Sensing Inhibition | Benzamide-benzimidazole compounds, brominated furanones | Inhibit QS regulators (e.g., MvfR), reduce persistence | P. aeruginosa [52] |
These preventive strategies are particularly relevant in biofilm contexts, where quorum sensing and metabolic heterogeneity drive persister formation in response to nutrient gradients and population density [52] [68].
Synergistic Combination Therapies
Combination approaches that enhance the efficacy of conventional antibiotics against persisters represent one of the most promising near-term strategies. These therapies typically work by disrupting persister membranes or metabolic homeostasis to facilitate antibiotic uptake and activity.
Membrane Permeabilizers: Compounds including MB6, synthetic retinoids (CD437, CD1530), bithionol, and nTZDpa bind to and disrupt bacterial membrane integrity, increasing uptake of co-administered antibiotics like gentamicin [52]. These combinations have demonstrated strong activity against MRSA persisters [52].
Peptide Enhancers: Engineered peptides such as polymyxin B nonapeptide (PMBN) and its derivative SPR741 function through membrane disruption, while modified antibiotics like Pentobra (tobramycin with added transporter sequence) demonstrate enhanced penetration into persister cells [52].
Antibiotic Combinations: Specific antibiotic pairings show synergistic effects against persisters. Ciprofloxacin-vancomycin, daptomycin-tobramycin, and tobramycin-vancomycin combinations resulted in 2 to 256-fold reductions in MICs against S. aureus clinical isolates and significantly reduced persister fractions in time-kill assays [69].
Diagram 1: Mechanism of synergistic combination therapy for eradicating bacterial persister cells.
Nutrient Gradients and Persister Dynamics in Biofilms
Physiological Heterogeneity in Biofilms
Biofilms exhibit remarkable physiological heterogeneity largely driven by nutrient and oxygen gradients [11]. This microenvironmental variation creates distinct subpopulations with different metabolic states and persistence capabilities:
- Type I Persisters: Form in response to external environmental triggers such as nutrient limitation in stationary phase or specific stress signals within biofilm depth gradients [11].
- Type II Persisters: Arise spontaneously through stochastic switching to slow-growth states independent of external cues, maintaining the ability to divide slowly and revert to normal growth [11].
The metabolic diversity of persisters extends beyond this simple classification, forming a continuum from "shallow" to "deep" persistence states, with deeper dormancy associated with increased antibiotic tolerance [11]. This hierarchy correlates with position within biofilm nutrient gradients, where deeply located cells experience more severe nutrient restriction.
Experimental Models for Nutrient Gradient Studies
Investigating persister dynamics under nutrient gradient conditions requires specialized experimental approaches that mimic the biofilm microenvironment:
Biofilm Persister Isolation Protocol:
- Grow P. aeruginosa strains to exponential and stationary phases in appropriate media [68]
- Establish biofilms on suitable substrates (e.g., peg lids, flow cells) for 24-48 hours
- Treat biofilms with 5× MIC of ciprofloxacin or colistin for 3.5 hours [68]
- Disaggregate biofilms enzymatically or mechanically
- Plate serial dilutions on nutrient agar for colony counting after 24-48 hours incubation
- Calculate persister fractions by comparing CFU counts before and after antibiotic treatment [68]
This protocol can be adapted to study nutrient gradient effects by establishing biofilms of different thicknesses or using gradient plate systems that create defined nutrient concentration profiles.
Diagram 2: Nutrient gradient effects on persister cell formation and distribution within bacterial biofilms.
Experimental Protocols for Persister Research
Quantitative Persister Fraction Assay
Accurately quantifying persister fractions requires standardized methodologies that account for the dynamic nature of persister populations:
Time-Kill Assay Protocol:
- Grow bacterial cultures to desired growth phase (exponential or stationary) in appropriate medium [68]
- Prepare antibiotic solutions at target concentrations (typically 5-100× MIC)
- Treat cultures with antibiotics for varying durations (0-24 hours)
- At each time point, remove aliquots, wash to remove antibiotics, and perform serial dilutions
- Plate dilutions on antibiotic-free media and incubate for 24-48 hours
- Count CFUs and calculate persister fractions as surviving cells per initial population [69]
Mathematical Modeling: A two-state model can be applied where normal cells (N) die at rate μ and switch to persister state at rate α, while persister cells (P) switch to normal state at rate β but do not die during antibiotic treatment [70]. This model enables calculation of switching rates and intrinsic persister fractions independent of experimental timing.
Biofilm Disruption and Persister Elimination Assay
Evaluating anti-persister strategies in biofilm contexts requires specialized protocols:
- Grow biofilms for 24-72 hours on appropriate substrates (peg lids, flow cells) [68]
- Treat pre-formed biofilms with test compounds at specified concentrations (e.g., 100× MIC) for 4-24 hours [69]
- Disrupt biofilms using sonication or enzymatic treatment
- Plate serial dilutions for CFU counting to determine surviving persister fractions
- Assess biofilm disruption by crystal violet staining or confocal microscopy
Research Reagent Solutions
Table 3: Essential Research Reagents for Persister Studies
| Reagent/Category | Specific Examples | Function/Application | Research Context |
|---|---|---|---|
| Membrane-Targeting Compounds | XF-73, SA-558, synthetic retinoids (CD437, CD1530) | Disrupt persister membranes, enable antibiotic uptake | MRSA persister eradication [52] |
| TA System Modulators | relBE, vapBC expression systems | Study toxin-antitoxin mediated persistence mechanisms | P. aeruginosa biofilm persister analysis [68] |
| Hâ‚‚S Pathway Modulators | CSE inhibitors, Hâ‚‚S scavengers | Block bacterial Hâ‚‚S-mediated stress protection | Persister prevention in multiple pathogens [52] |
| Quorum Sensing Inhibitors | Benzamide-benzimidazole compounds, brominated furanones | Inhibit QS-regulated persister formation | P. aeruginosa persister reduction [52] |
| Synergistic Antibiotic Combinations | Ciprofloxacin-vancomycin, daptomycin-tobramycin | Enhanced killing through dual mechanisms | S. aureus persister reduction [69] |
| Metabolic Disruptors | Nitric oxide (NO), pinaverium bromide | Alter bacterial metabolism, reduce persistence | Prevention of persister formation [52] |
The complex interplay between nutrient gradients, biofilm microenvironments, and persister cell dynamics presents both challenges and opportunities for therapeutic intervention. Successful eradication of persistent infections will likely require multi-pronged approaches that consider the spatial and metabolic heterogeneity of bacterial populations. Future research directions should focus on identifying persister-specific targets within nutrient-deprived biofilm regions, developing compounds that exploit metabolic vulnerabilities in dormant cells, and optimizing combination therapies that prevent persister formation while effectively eliminating existing reservoirs. The continued refinement of experimental models that accurately replicate in vivo nutrient gradients will be essential for translating promising anti-persister strategies from laboratory research to clinical application.
Addressing Heterogeneity in Persister Metabolic States and Depth of Dormancy
Bacterial persisters, a subpopulation of cells capable of surviving antibiotic treatment without genetic resistance, represent a significant challenge in treating persistent infections. Their formation and survival are profoundly influenced by heterogeneous microenvironments within biofilms, particularly nutrient gradients [11] [3]. Far from being a uniform population of dormant cells, persisters exhibit a striking diversity in their metabolic states and depth of dormancy, forming a continuum from shallowly dormant, metabolically active cells to deeply dormant, viable but non-culturable (VBNC) cells [11] [71]. This heterogeneity is primarily driven by spatial and temporal variations in nutrient availability, oxygen concentration, and other environmental stresses within the biofilm architecture [3] [29]. Understanding this complexity is crucial for developing effective therapeutic strategies against chronic biofilm-based infections. This technical guide synthesizes current knowledge on the characteristics, formation mechanisms, and experimental approaches for studying persister heterogeneity in the context of nutrient gradients, providing researchers and drug development professionals with a framework to target this resilient bacterial subpopulation.
Classifying Persister States: From Metabolic Activity to Dormancy Depth
Established Classification Systems
Persister cells are broadly categorized based on their formation triggers and physiological characteristics. Type I persisters form during the stationary phase in response to environmental stresses such as nutrient starvation [72]. Type II persisters are spontaneously generated throughout the exponential phase due to stochastic fluctuations in gene expression [72]. A third category, Type III or "specialized persisters," exhibits persistence mechanisms specific to particular antibiotics without necessarily undergoing slow growth or significant metabolic reduction prior to antibiotic exposure [72].
The Metabolic and Dormancy Continuum
Beyond these categories, persisters exist along a dynamic spectrum of metabolic activity and dormancy depth, challenging the traditional view of persisters as uniformly dormant [11] [71].
- Metabolic Diversity: Persisters display varying degrees of metabolic activity. Some are metabolically quiescent (non-growing), while others exhibit slow metabolism and growth [11]. Recent transcriptomic evidence confirms that persister cells can actively produce RNA and adapt their gene expression profiles to enhance survival, indicating significant metabolic activity despite antibiotic exposure [71].
- Dormancy Hierarchy: A hierarchy of persistence levels exists within a "persister continuum." Some cells exhibit "shallow persistence" with relatively weak tolerance, while others display "deep persistence" with profound dormancy and enhanced survival capabilities [11]. The most extremely dormant states are classified as viable but non-culturable (VBNC), where cells remain viable but cannot be cultured by standard laboratory methods [11].
Table 1: Spectrum of Persister Metabolic States and Dormancy Depth
| State Classification | Metabolic Activity | Growth Status | Key Characteristics | Cultivability |
|---|---|---|---|---|
| Shallow Persistence | Moderate to low | Slow-growing | Retains significant transcriptional activity; quicker resuscitation | Cultivable |
| Moderate Persistence | Low | Non-growing or severely slow-growing | Reduced but detectable metabolism; delayed resuscitation | Cultivable |
| Deep Persistence | Very low to undetectable | Non-growing | Profound dormancy; high tolerance to multiple stresses | Cultivable |
| VBNC State | Dormant with minimal activity | Non-growing | Extreme dormancy; requires specific signals for resuscitation | Non-cultivable |
Mechanisms Driving Heterogeneity in Biofilms
The Central Role of Nutrient Gradients
The physical and chemical structure of biofilms generates microenvironments that are the primary drivers of persister heterogeneity [3]. Nutrient availability, especially oxygen, serves as the principal factor influencing microbial physiology [3]. In biofilms, the source of oxygen is typically the interface with the environment, leading to decreasing concentrations with depth. This creates oxic zones near the surface and anoxic or reduced zones in the interior, supporting distinct metabolic processes [3]. This resource gradient leads to physiological differentiation and a division-of-labor within the community [3]. For instance, computational and experimental studies of E. coli biofilms predict and validate metabolic cross-feeding: cells in the lower, anoxic regions ferment glucose and produce acetate, which then diffuses upward to be respired by cells in the oxic zone [3].
Molecular Mechanisms of Persister Formation and Survival
The cellular response to nutrient limitation and other stresses is mediated by sophisticated molecular mechanisms that induce dormancy.
- The Stringent Response and ppGpp: The alarmone guanosine tetraphosphate (ppGpp) is a central mediator of bacterial persistence [28] [29]. Produced in response to nutrient limitation and other stresses, ppGpp triggers a global transcriptional reprogramming known as the stringent response, shifting the cell toward a non-growing state and activating persistence pathways [28] [29]. Research shows that carbon source transitions in E. coli biofilms stimulate persister formation through a pathway dependent on ppGpp and nucleoid-associated proteins (NAPs) like FIS and HU [29].
- Toxin-Antitoxin (TA) Systems: TA systems are key genetic elements that induce a dormant state [28]. They typically consist of a stable toxin that disrupts essential cellular processes (e.g., translation via mRNA degradation) and a labile antitoxin that neutralizes the toxin. Under stress, proteases such as Lon degrade the antitoxin, freeing the toxin to act. For example, the MqsR toxin cleaves most cellular transcripts, rendering the cell dormant by halting translation, while the TisB toxin decreases proton motive force and ATP levels [28].
- Environmental Sensing and Phenotypic Switching: Persister formation is not purely stochastic; it is also influenced by environmental cues. Computational models demonstrate that biofilms employing environment-dependent switching strategies—such as inducing persistence in response to low substrate or the presence of antibiotics—exhibit enhanced survival and recovery after antibiotic treatment compared to those using constant stochastic switching [65]. This ability to sense and respond to the local microenvironment fine-tunes the level of persistence within different biofilm regions.
The following diagram illustrates the core signaling pathway through which nutrient gradients trigger persister formation.
Core Pathway from Nutrient Stress to Persister Formation
Experimental Approaches for Analyzing Heterogeneity
Methodologies for Isolation and Characterization
Investigating persister heterogeneity requires methodologies capable of isolating and characterizing subpopulations based on their metabolic activity and dormancy depth.
- Fluorescence-Activated Cell Sorting (FACS): This is a powerful technique for isolating persister subpopulations. A standard protocol involves using a GFP reporter under the control of a ribosomal promoter [28]. Metabolically inactive cells with diminished fluorescence can be separated from active cells via FACS, allowing for downstream analysis like transcriptomics [28].
- Transcriptomic Analysis: RNA sequencing of persisters isolated at multiple time points after antibiotic exposure reveals major shifts in gene network activity, demonstrating their metabolic activity and adaptation over time [71]. This approach can identify genes consistently upregulated in persisters, providing insights into survival mechanisms.
- Colony Biofilm Model for Nutrient Control: This ex vivo method allows for precise control of nutrient availability to biofilm cells [29]. Bacteria are inoculated onto polyethersulfone (PES) membranes positioned on agar plates containing defined carbon sources. This setup enables the study of persister formation in response to specific nutrient transitions, such as a diauxic shift from glucose to fumarate [29].
Table 2: Key Experimental Models for Studying Persister Heterogeneity
| Experimental Model | Key Feature | Application in Persister Research | Reference Organism |
|---|---|---|---|
| Colony Biofilm on PES Membrane | Exogenous control of nutrient availability | Studying persister formation in response to defined carbon source transitions | Escherichia coli [29] |
| Individual-Based Model (IBM) | Simulates individual cell behavior in a biofilm | Testing environment-dependent switching strategies (constant, substrate-, antibiotic-dependent) | In silico [65] |
| Continuum Mathematical Model | Couples nutrient transport with population dynamics | Predicting how nutrient-dependent phenotypic switching affects persister populations and biofilm resilience | In silico [6] |
The Scientist's Toolkit: Essential Research Reagents
Table 3: Key Reagents and Tools for Persister Heterogeneity Research
| Reagent / Tool | Function / Target | Experimental Utility |
|---|---|---|
| Ribosomal Promoter GFP Reporter | Reports on ribosomal activity and protein synthesis potential | FACS-based isolation of metabolically inactive/dormant cells [28] |
| PES (Polyethersulfone) Membranes | Provides a solid support for biofilm growth | Enables colony biofilm formation and transfer between different nutrient agars [29] |
| Lon Protease Inhibitors | Targets Lon protease, which degrades type II TA system antitoxins | Probing the role of TA systems in persister formation [28] |
| ppGpp Analogs / RelA SpoT Mutants | Modulates the stringent response | Elucidating the role of ppGpp in nutrient transition-induced persistence [28] [29] |
| Specific TA System Mutants (e.g., ΔmqsR, ΔtisB) | Gene deletion in specific toxin-antitoxin modules | Determining the contribution of individual TA systems to persistence in planktonic vs. biofilm growth [28] |
The following workflow outlines a key experimental protocol for investigating nutrient transition effects on persisters.
Workflow for Nutrient Transition Assay
Implications for Therapeutic Development
The heterogeneity of persister metabolic states and dormancy depth necessitates a multi-pronged therapeutic approach. Strategies must move beyond traditional growth-active antibiotics to include agents that target dormant cells or manipulate their physiological state.
- Direct Killing of Persisters: This strategy targets growth-independent cellular structures. Examples include membrane-targeting compounds like XF-73 and SA-558, which cause cell lysis, and the prodrug Pyrazinamide, which disrupts membrane energetics in Mycobacterium tuberculosis persisters [52] [27]. ADEP4 activates the ClpP protease, leading to uncontrolled protein degradation even in dormant cells [52] [27].
- Inhibiting Persister Formation: Targeting the molecular triggers of persistence can prevent cells from entering the tolerant state. Inhibitors of H2S biogenesis or quorum-sensing interference molecules can reduce persister formation and potentiate the effect of conventional antibiotics [52] [27].
- Synergistic Killing by Reactivation: "Awakening" persisters from dormancy can re-sensitize them to traditional antibiotics. This can be achieved by disrupting persistence maintenance mechanisms or using compounds that increase membrane permeability, thereby enhancing antibiotic uptake [52] [27].
Mathematical models that incorporate nutrient-dependent phenotypic switching, as described in [6], are invaluable for predicting the efficacy of these strategies and identifying critical intervention windows during biofilm treatment.
The heterogeneity of bacterial persisters, driven by nutrient gradients and other microenvironmental factors within biofilms, is a fundamental aspect of their biology that complicates treatment. The continuum of metabolic states and dormancy depths, governed by mechanisms like the stringent response and TA systems, requires a sophisticated and nuanced research approach. The experimental frameworks and tools detailed in this guide—from advanced isolation techniques and ex vivo models to computational simulations—provide a pathway for deciphering this complexity. Embracing this heterogeneous paradigm is essential for the scientific community to develop the next generation of anti-persister therapeutics that can effectively target the entire spectrum of dormant cells and ultimately overcome chronic biofilm infections.
Evaluating Therapeutic Strategies and Clinical Implications
Comparative Analysis of Direct vs. Indirect Anti-Persister Compounds
Bacterial persisters are a subpopulation of growth-arrested, dormant cells that exhibit remarkable tolerance to conventional antibiotic treatments despite being genetically susceptible [11] [27]. These cells underlie the recalcitrance of chronic and persistent infections, leading to treatment failures and relapses [25] [73]. The formation of persisters is significantly influenced by heterogeneous microenvironments, particularly the nutrient gradients within biofilms. As nutrients become limited in deeper biofilm layers, bacterial metabolism slows, triggering a transition to a dormant state that protects them from antibiotics that target active cellular processes [11] [25].
Addressing this challenge requires therapeutic strategies that either directly target dormant persisters or indirectly manipulate their physiology. Direct anti-persister compounds typically target growth-independent cellular structures, such as membranes, to induce lethal damage [27] [52]. In contrast, indirect strategies focus on preventing persister formation, resuscitating dormant cells to re-sensitize them to conventional antibiotics, or exploiting other vulnerabilities [27]. This review provides a comparative analysis of these distinct approaches, evaluating their mechanisms, experimental validation, and application within the context of nutrient-influenced biofilm persistence.
Direct Anti-Persister Strategies: Mechanisms and Compounds
Direct strategies are characterized by their action on cellular targets that remain vulnerable even in metabolically inactive cells. Their primary advantage lies in their independence from bacterial metabolic state, allowing them to kill persisters without the need for cellular activation [27].
Key Mechanisms of Direct Compounds
- Cell Membrane Disruption: This is the most common mechanism for direct killing. Many compounds physically disrupt the integrity of the bacterial cell membrane, leading to leakage of cellular contents, loss of membrane potential, and ultimately, cell lysis [27] [52]. Membrane damage can also generate lethal levels of reactive oxygen species (ROS) [27]. Compounds like XF-73, SA-558, and thymol triphenylphosphine conjugates (TPP-Thy3) function primarily through this mechanism [27] [52].
- Protein Degradation: Some compounds hijack or activate proteolytic systems to cause uncontrolled degradation of essential proteins. ADEP4, for instance, binds to and activates the ClpP protease, leading to the ATP-independent degradation of over 400 intracellular proteins. This includes enzymes critical for metabolic recovery, rendering the cells unable to resuscitate [27] [52].
- Membrane Energetics Disruption: Pyrazinamide (PZA), a cornerstone drug for tuberculosis, is a prodrug converted to pyrazinoic acid (POA) by bacterial amidases. POA disrupts membrane energetics and targets enzymes like PanD, triggering its degradation and crippling coenzyme A biosynthesis [11] [27] [52].
Table 1: Characteristics of Direct Anti-Persister Compounds
| Compound Class/Name | Primary Target | Proposed Mechanism of Action | Key Evidence/Model |
|---|---|---|---|
| XF-70, XF-73 | Cell Membrane | Disrupts membrane integrity; generates ROS upon light activation [27]. | Effective against non-dividing S. aureus; time-kill assays in stationary phase cultures [27] [52]. |
| SA-558 | Cell Membrane | Synthetic cation transporter that disrupts bacterial homeostasis, leading to autolysis [27]. | Killing curves against S. aureus persisters; disruption of membrane potential measured fluorometrically [27]. |
| ADEP4 | ClpP Protease | Binds and activates ClpP, causing uncontrolled protein degradation [27] [52]. | Synergy with rifampicin; eradication of S. aureus persisters in vitro; reduced bacterial load in a mouse thigh infection model [27]. |
| Pyrazinamide (PZA) | Membrane Energetics & PanD | Disrupts membrane potential and binds PanD, triggering its ClpC1-ClpP-mediated degradation [27]. | Critical for shortening TB therapy; effective against non-replicating M. tuberculosis; defined acid pH assay conditions [11] [27]. |
| Cationic Silver Nanodroplets (C-AgND) | Cell Membrane & EPS | Interacts with negatively charged EPS and bacterial membranes, causing physical damage [27]. | Effective against S. aureus persisters within biofilms; confocal microscopy showing reduced biofilm viability [27]. |
Experimental Protocols for Evaluating Direct Compounds
Protocol 1: Time-Kill Assay Against Stationary-Phase Persisters
- Objective: To quantify the killing efficacy of a direct compound against non-growing persister cells.
- Procedure:
- Culture Preparation: Grow the bacterial strain (e.g., S. aureus or E. coli) to stationary phase (e.g., 24-48 hours) to enrich for persisters [27] [74].
- Compound Exposure: Treat the culture with the test compound at a predetermined concentration (e.g., 10-100x MIC). Include an untreated control.
- Viability Assessment: At defined time intervals (e.g., 0, 2, 6, 24 hours), remove aliquots, perform serial dilution, and plate on drug-free agar.
- Data Analysis: Count colony-forming units (CFUs) after incubation. Plot log10(CFU/mL) versus time to generate killing curves. A direct compound will show a rapid, concentration-dependent decrease in viable count without a distinct persistent plateau [27] [74].
Protocol 2: Membrane Integrity Assay
- Objective: To confirm membrane disruption as the mechanism of action.
- Procedure:
- Cell Staining: Incubate a stationary-phase bacterial culture with a fluorescent dye pair such as SYTO9 and propidium iodide (PI). SYTO9 stains all cells green, while PI penetrates only cells with compromised membranes, staining them red and reducing green fluorescence.
- Treatment and Measurement: Treat the stained cells with the test compound.
- Analysis: Use fluorescence spectrometry or flow cytometry to measure the shift in fluorescence. An increase in red/green fluorescence ratio indicates membrane damage [27].
Indirect Anti-Persister Strategies: Mechanisms and Compounds
Indirect strategies aim to manage the persister problem by altering their formation or dormant state, rather than killing them directly. These approaches often seek to sensitize persisters to conventional antibiotics [27].
Key Mechanisms of Indirect Compounds
- Inhibiting Persister Formation: This strategy targets the molecular pathways that initiate dormancy. For example, nitric oxide (NO) acts as a metabolic disruptor that can prevent entry into a persistent state [27]. Inhibitors of hydrogen sulfide (H₂S) biogenesis, such as cystathionine γ-lyase (CSE) inhibitors, have also been shown to reduce persister formation in S. aureus and P. aeruginosa by compromising a key defense system against oxidative stress [27] [52].
- Reactivating Persisters ("Wake-Up" Strategy): Compounds that force persisters to exit dormancy and resume metabolic activity can make them vulnerable again to traditional antibiotics. This can be achieved by disrupting the proton motive force (PMF) or by interfering with stringent response signaling [27].
- Quorum Sensing Interference: Quorum sensing (QS) molecules can influence persister levels in a population. Inhibiting QS regulators, for instance with benzamide-benzimidazole compounds that target MvfR in P. aeruginosa, can reduce persister formation without affecting growth [27].
- Synergistic Killing with Antibiotics: Several compounds function by weakening cellular defenses, thereby allowing conventional antibiotics to penetrate and kill persisters. Membrane-active compounds like MB6, CD437, and SPR741 disrupt membrane integrity, increasing the uptake of antibiotics like gentamicin into otherwise impermeable dormant cells [27] [52].
Table 2: Characteristics of Indirect Anti-Persister Compounds and Strategies
| Compound/Strategy | Primary Target/Mechanism | Effect on Persisters | Key Evidence/Model |
|---|---|---|---|
| CSE Inhibitors | Hâ‚‚S Biogenesis | Reduces persister formation; potentiates antibiotics [27]. | Reduced persister counts in S. aureus and P. aeruginosa; synergy with aminoglycosides demonstrated in checkerboard assays [27] [52]. |
| Nitric Oxide (NO) | Bacterial Metabolism | Metabolic disruptor that inhibits persister formation [27]. | Reduction in E. coli and P. aeruginosa persister levels upon co-administration with antibiotics [27]. |
| Quorum Sensing Inhibitors | MvfR Regulon & AHLs | Reduces persister formation by interfering with bacterial communication [27]. | Brominated furanones and other QSIs reduce persister formation in P. aeruginosa without inhibiting growth [27]. |
| Membrane Permeabilizers (e.g., MB6, SPR741) | Cell Membrane Integrity | Disrupts membrane, increasing uptake of co-administered antibiotics [27] [52]. | Strong synergy with gentamicin against MRSA persisters; shown by time-kill assays where combination leads to sterilization [27]. |
| Pheromone cCf10 | (p)ppGpp Alarmone | Inhibits Enterococcus faecalis persister formation by reducing alarmone accumulation [27]. | Maintains metabolic activity; reduces persister frequency in specific assays [27]. |
Experimental Protocols for Evaluating Indirect Compounds
Protocol 1: Persister Formation Inhibition Assay
- Objective: To determine if a compound can prevent the formation of persisters upon exposure to a stressor.
- Procedure:
- Co-Incubation: Grow a bacterial culture to mid-log phase. Add the test compound (at a sub-inhibitory concentration) and a known persister-inducing stressor (e.g., a low concentration of a bacteriostatic antibiotic).
- Induction and Treatment: After several hours of induction, treat the culture with a high concentration of a bactericidal antibiotic (e.g., 100x MIC of a fluoroquinolone) for a set period to kill non-persisters.
- Viability Assessment: Wash the cells to remove antibiotics, serially dilute, and plate to count surviving CFUs.
- Data Analysis: Compare the number of surviving persisters in the test group to a control group (stressor only). A significant reduction indicates the test compound inhibits persister formation [27].
Protocol 2: Synergy Checkerboard Assay
- Objective: To quantify the synergistic interaction between an indirect compound and a conventional antibiotic.
- Procedure:
- Microtiter Plate Setup: Prepare a 96-well plate with a two-dimensional dilution series. Vary the concentration of the antibiotic along the rows and the concentration of the indirect compound along the columns.
- Inoculation: Inoculate each well with a standardized suspension of stationary-phase bacteria or a pre-formed biofilm.
- Incubation and Analysis: Incubate the plate and measure bacterial growth (OD600) or viability (ATP-based assays). Calculate the Fractional Inhibitory Concentration Index (FICI). A FICI of ≤0.5 indicates synergy [27] [52].
The Scientist's Toolkit: Key Research Reagents
Table 3: Essential Reagents for Anti-Persister Research
| Reagent / Material | Function in Experimental Workflow |
|---|---|
| Stationary-Phase Cultures | Source of Type I (non-growing) persister cells for in vitro assays [11] [27]. |
| Biofilm Reactors (e.g., Calgary Device, Flow Cells) | Models nutrient gradients and generates biofilm-associated persisters for physiologically relevant testing [7] [25]. |
| SYTO9/Propidium Iodide (LIVE/DEAD BacLight) | Fluorescent dyes used in conjunction with fluorescence microscopy or flow cytometry to assess cell membrane integrity and viability [27]. |
| ATP-based Viability Assays | Measures metabolically active cells, useful for quantifying persister resuscitation after indirect "wake-up" treatment [27]. |
| Microtiter Plates (96-well) | Standard platform for high-throughput screening of compound libraries and for performing synergy checkerboard assays [27]. |
Conceptual Workflows and Pathway Diagrams
Workflow for Differentiating Direct and Indirect Anti-Persister Activity
The following diagram illustrates a logical experimental workflow to determine a compound's mechanism of action.
Nutrient Gradients and Persister Signaling in Biofilms
This diagram conceptualizes how nutrient gradients within a biofilm influence physiological states and trigger molecular pathways leading to persistence, highlighting potential intervention points.
The comparative analysis of direct and indirect anti-persister strategies reveals a complementary set of tools for combating persistent infections. Direct compounds, such as membrane disruptors and uncontrolled proteolysis activators, offer the decisive advantage of killing persisters in their dormant state, providing a "sterilizing" effect crucial for eradicating biofilms [27] [52]. Their primary challenge lies in potential off-target toxicity against host membranes [27]. Indirect strategies, including persister formation inhibitors and synergistic sensitizers, offer a more nuanced approach. They can potentiate existing antibiotics and reduce the reservoir of tolerant cells, potentially lowering the evolutionary pressure for full resistance [27] [73].
The efficacy of both strategies is profoundly influenced by the biofilm microenvironment. Nutrient gradients create a spectrum of metabolic activity, from active cells at the biofilm periphery to deeply dormant persisters in the core [11] [25]. This heterogeneity suggests that the most effective therapeutic approach may be combination therapy, utilizing direct compounds to eliminate the recalcitrant core and indirect agents to prevent reformation or sensitize shallow persisters at the periphery. Future research must continue to elucidate the complex molecular pathways triggered by nutrient limitation to identify novel, high-value targets for both direct and indirect interventions, ultimately paving the way for more effective treatments for chronic biofilm-associated infections.
Within the broader context of research on nutrient gradient effects on persister formation in biofilms, the transition from theoretical modeling to experimental validation is a critical step. Mathematical models, particularly those incorporating nutrient-dependent phenotypic switching, provide testable hypotheses about the spatiotemporal dynamics of persister cells [47] [16]. However, these predictions require rigorous validation through carefully designed in vitro and ex vivo studies that replicate the complex microenvironment of biofilms. This guide details the experimental frameworks and methodologies necessary to bridge computational predictions with biological validation, enabling researchers to confirm model accuracy and identify potential therapeutic windows for targeting persistent infections.
The challenge in persister studies lies in their phenotypic heterogeneity and the technical difficulties in detecting these rare, dormant cells within heterogeneous populations. As nutrient gradients within biofilms directly influence the formation and distribution of persister cells [47] [16], validation experiments must replicate these conditions to generate meaningful data. This technical guide consolidates current methodologies for persister survival studies, with particular emphasis on approaches that can directly inform and refine nutrient-gradient models of biofilm-associated infections.
Integrating Mathematical Models with Experimental Design
Key Model Predictions Requiring Experimental Validation
Contemporary mathematical models of biofilm dynamics generate specific, testable predictions about persister formation and survival. The nutrient-dependent switching model proposed by Mandal et al. offers a valuable framework for experimental design, suggesting that local nutrient concentration controls phenotypic switching between proliferative and persister states through two distinct thresholds [47]. This model predicts several quantitatively verifiable phenomena: that nutrient limitation produces a high and sustained proportion of persisters even when overall biomass is reduced, that persister populations peak at times varying with nutrient availability, and that these peaks coincide with critical turning points in biofilm growth that may represent optimal intervention windows [47].
Earlier individual-based models (IbM) have proposed four primary hypotheses for dormant cell formation—stochastic processes, nutrient-dependent, oxygen-dependent, and time-dependent mechanisms—each generating distinct spatiotemporal distributions of persisters within growing biofilms [16]. These competing hypotheses can be discriminated through experimental manipulation of bulk nutrient or oxygen concentrations followed by careful mapping of persister distributions [16]. For researchers focused on nutrient gradient effects, validating the spatial correlation between nutrient penetration depth, metabolic activity zones, and persister localization represents a particularly high priority.
Experimental Variables for Nutrient Gradient Manipulation
Table 1: Key experimental variables for manipulating nutrient gradients in persister studies
| Variable Category | Specific Parameters | Measurement Techniques | Relevance to Model Validation |
|---|---|---|---|
| Nutrient Composition | Carbon source type (e.g., glucose, glutamate), concentration, limitation | Chemical assays, biosensors | Tests nutrient-dependent switching thresholds [47] |
| Gradient Establishment | Flow rate, reactor type (flow cell, drip flow), biofilm age | Microsensor profiling, computational fluid dynamics | Validates spatial distribution predictions [16] |
| Environmental Stressors | Oxygen tension, pH, temperature, metabolic byproducts | Oxygen microsensors, pH indicators | Discriminates between formation mechanisms [16] |
| Temporal Dynamics | Treatment timing, duration, nutrient shift experiments | Time-lapse imaging, kill curves | Correlates persister peaks with growth turning points [47] |
Experimental Methodologies for Persister Survival Studies
In Vitro Model Systems for Biofilm Persistence
In vitro systems allow controlled manipulation of specific variables hypothesized to influence persister formation. The selection of an appropriate model system depends on the specific research question and the spatial resolution required for validation.
Biofilm Cultivation Systems: Several established systems enable the study of persisters under defined nutrient gradients. Flow cell reactors generate nutrient gradients similar to those found in natural environments and medical implant infections, allowing real-time monitoring of spatial organization [47]. For higher-throughput screening, drip flow reactors or calgary biofilm devices provide a compromise between nutrient gradient formation and experimental scalability. Batch culture systems with controlled nutrient depletion offer the simplest approach for studying temporal dynamics of persister formation without complex spatial gradients [16].
Nutrient Gradient Manipulation: To specifically test nutrient-dependent hypotheses, researchers can systematically vary bulk nutrient concentrations while monitoring persister formation through time-kill assays [16]. More sophisticated approaches involve the use of membrane-based gradient systems or microfluidic devices that generate stable, quantifiable nutrient gradients for high-resolution spatial mapping of persister distributions in relation to nutrient availability [47].
Ex Vivo and In Vivo Model Systems
While in vitro systems offer control and reproducibility, ex vivo and in vivo models provide critical validation under more clinically relevant conditions. The optimized murine lung infection model for Pseudomonas aeruginosa represents a sophisticated approach for studying antibiotic tolerance in settings that mimic human disease [75]. In this model, bacteria are embedded in seaweed alginate beads to mimic the biofilm environment and installed in the lower respiratory tract via intratracheal instillation, followed by antibiotic treatment through nasal droplets [75].
For correlation with in vitro findings, researchers can employ the time-kill assay methodology, which has demonstrated positive correlation between in vitro persistence levels and survival in animal models [75]. This validation is crucial for establishing the clinical relevance of mechanisms identified through in vitro studies. The murine model also enables the testing of potential antipersister therapies and the study of persistence mechanisms in biologically complex environments [75].
Persister Detection and Quantification Methods
Accurate detection and quantification of persister cells remains technically challenging due to their low frequency and metabolic heterogeneity. The most widely accepted method involves time-kill curves with high concentrations of bactericidal antibiotics, typically using the minimum duration for killing 99.99% of cells (MDK99.99) as a quantitative measure of persistence levels [11] [76]. This approach reveals the characteristic biphasic killing kinetics where the majority of cells die rapidly while a small persister subpopulation survives extended antibiotic exposure [11].
For spatial mapping of persisters within biofilms, researchers can employ dormancy-labeling strategies such as the Sps1 protein marker system developed for Cryptococcus neoformans, which enables direct detection and isolation of dormant fungal subpopulations in complex environments [76]. Similar approaches for bacterial systems typically combine fluorescent viability markers with metabolic indicators to identify subpopulations with reduced metabolic activity.
Table 2: Key reagents and methodologies for persister detection and quantification
| Reagent/Method | Application | Technical Considerations | References |
|---|---|---|---|
| Time-kill assays | Quantification of persister frequency using MDK99.99 | Requires high antibiotic concentrations; biphasic kinetics confirm persistence | [11] [76] |
| Live/dead staining (e.g., SYTO9/propidium iodide) | Differentiation of viable and non-viable cells | May not detect metabolically inactive but viable persisters | [76] |
| Dormancy-specific markers (e.g., Sps1 in C. neoformans) | Specific detection of dormant subpopulations | Limited availability of specific markers for bacterial systems | [76] |
| Metabolic indicators (e.g., CTC reduction, GFP reporters) | Assessment of metabolic activity | Correlates with but does not definitively identify persisters | [16] |
| Microfluidic cultivation | Single-cell dynamics under controlled conditions | Technically demanding; enables real-time monitoring | [16] |
Validation of Nutrient-Dependent Phenotypic Switching
Experimental Design for Nutrient Threshold Validation
The mathematical model proposed by Mandal et al. specifically predicts that switching rates between proliferative and persister phenotypes depend on local nutrient concentration through two thresholds, enabling adaptation across nutrient-poor, intermediate, and nutrient-rich regimes [47]. Validating this prediction requires experimental designs that systematically manipulate nutrient availability while monitoring phenotypic switching in real time.
A recommended approach involves cultivating biofilms under defined nutrient conditions, then subjecting them to nutrient shifts while monitoring persister formation through time-kill assays at multiple time points. This experimental paradigm can identify critical nutrient thresholds that trigger increased phenotypic switching. Complementary approaches using fluorescent reporter systems fused to promoters of persister-related genes can provide single-cell resolution data on switching dynamics in response to nutrient gradients [47] [16].
Correlation of Spatial Distributions
Individual-based models generate explicit predictions about the spatial distribution of persisters within biofilms growing under different nutrient conditions [16]. Validating these predictions requires techniques that preserve spatial information while identifying persister cells. One approach combines cryosectioning of biofilms with viability staining after antibiotic exposure to map persister locations relative to the biofilm structure [16]. Alternatively, in situ hybridization techniques targeting persister-associated transcripts or the use of strain libraries with persister-specific promoters driving fluorescent reporters can provide spatial data without disrupting biofilm architecture.
The Scientist's Toolkit: Essential Research Reagents and Solutions
Table 3: Key research reagent solutions for persister survival studies
| Reagent Category | Specific Examples | Function/Application | Technical Notes |
|---|---|---|---|
| Bacterial Strains | E. coli HM22 (hipA7), P. aeruginosa PA14, Clinical isolates | High-persistence mutants for increased yield; diverse isolates for generality | hipA7 allele in E. coli HM22 provides high persistence [77] |
| Culture Media Components | Defined minimal media, Specific carbon sources, Gradient-forming gels | Controlled nutrient environment; establishment of reproducible gradients | Enables testing of nutrient-dependent hypotheses [16] |
| Antibiotics for Selection | Tobramycin, Ampicillin, Ciprofloxacin, Drug combinations | Persister isolation through killing of non-persister cells | Tobramycin used at high doses (120 mg/kg) in murine models [75] |
| Viability Stains | SYTO9/propidium iodide, CTC, FUN-1, Resazurin | Differentiation of viable/non-viable cells; metabolic activity assessment | Complementary approaches provide more reliable quantification [76] |
| Molecular Biology Tools | Fluorescent reporter plasmids, Antibodies for protein detection, qPCR reagents | Monitoring gene expression; protein localization; transcriptional responses | Reporters enable real-time monitoring of phenotypic switching [47] |
| Biofilm Disruption Reagents | DNase I, Dispersin B, Proteases, Mechanical disruption | Harvesting cells from biofilms for enumeration | Enzymatic treatment preserves viability better than mechanical alone |
Data Interpretation and Integration with Computational Models
The ultimate goal of these validation experiments is to refine mathematical models and generate testable hypotheses about therapeutic interventions. Successful validation requires quantitative comparisons between predicted and observed persister frequencies, distributions, and dynamics under varying nutrient conditions. Discrepancies between model predictions and experimental data should be viewed as opportunities to identify missing biological mechanisms rather than failures of either approach.
For the nutrient gradient effects central to this research, particular attention should be paid to how well models predict the fraction of persisters in different biofilm regions defined by their local nutrient environment. The iterative process of model refinement and experimental validation will ultimately yield more accurate predictors of persister behavior and identify the most promising approaches for targeting these recalcitrant cell populations in clinical settings [47] [16].
Pyrazinamide (PZA) serves a unique role in tuberculosis (TB) therapy by specifically targeting non-replicating, drug-tolerant Mycobacterium tuberculosis persister cells. This case study examines PZA's mechanism of action within the context of nutrient gradient effects on persister formation in biofilms. We explore how PZA's ability to disrupt coenzyme A metabolism and synergize with host-derived oxidative stress provides exceptional sterilizing activity, ultimately shortening TB treatment duration. The analysis integrates current molecular insights with experimental approaches for investigating PZA efficacy, highlighting its critical position in modern TB regimens and future therapeutic development.
The lengthy treatment required for tuberculosis, typically a minimum of six months using first-line drugs, presents significant challenges for global TB control and patient adherence. This prolonged therapy is necessary due to the presence of bacterial persisters—metabolically heterogeneous, non-growing or slow-growing bacterial subpopulations that survive antibiotic exposure despite being genetically susceptible [78] [11]. These persisters exhibit phenotypic tolerance rather than heritable resistance, and their progeny remain fully drug-susceptible upon regrowth [78]. In TB infections, persisters underlie chronicity, relapse, and the requirement for lengthy, multi-drug regimens.
The formation of mycobacterial persisters is deeply intertwined with host microenvironments and nutrient heterogeneity. Within granulomas and biofilms, M. tuberculosis encounters varied conditions including oxygen gradients, nutrient starvation, acidic pH, and immune pressures [78] [79]. These conditions create a spectrum of metabolic states, from actively replicating to completely dormant bacilli, with differential susceptibility to antibiotics [78]. The "Yin-Yang" model of bacterial persistence conceptualizes this as a continuum where growing (Yang) and non-growing (Yin) subpopulations coexist and interconvert [78] [11]. This heterogeneity necessitates drugs that target both replicating and non-replicating populations—a role uniquely fulfilled by pyrazinamide.
Pyrazinamide: A Unique Anti-Persister Drug
Historical Context and Clinical Importance
Pyrazinamide occupies a special position in TB therapy as the only first-line drug specifically effective against non-replicating persister populations. Its inclusion in combination therapy in the 1970s demonstrated the dramatic ability to shorten treatment duration from 9-12 months to the current 6-month standard, while significantly reducing relapse rates [80]. This established PZA as a "sterilizing" drug capable of eliminating persisters that survive other antibiotics, making it indispensable in both drug-susceptible and multidrug-resistant TB regimens [80].
Unlike other TB drugs, PZA exhibits conditional activity—showing weak bacteriostatic activity in standard culture conditions but potent bactericidal activity in the acidic environment within phagosomes and in vivo [80] [81]. This discrepancy between in vitro and in vivo efficacy long puzzled researchers and complicated mechanistic studies.
Activation and Resistance
PZA is a prodrug that requires conversion to its active form, pyrazinoic acid (POA), by the bacterial enzyme pyrazinamidase/nicotinamidase (PZase) encoded by the pncA gene [80]. This activation step is crucial for anti-mycobacterial activity. Consequently, the predominant mechanism of clinical PZA resistance involves loss-of-function mutations in pncA, which prevent conversion of PZA to POA [80]. These mutations occur throughout the pncA coding sequence and account for approximately 70% of PZA-resistant clinical isolates [80].
Molecular Mechanisms of PZA Against Persisters
Proposed Models of Action
Research has yielded several models for PZA's mechanism of action, with growing evidence supporting multiple complementary pathways:
3.1.1 Coenzyme A Disruption Mounting evidence indicates that POA disrupts coenzyme A (CoA) biosynthesis through interaction with aspartate decarboxylase (PanD) [81]. This disruption depletes intracellular CoA pools, affecting numerous metabolic processes dependent on this essential cofactor. Supporting this model:
- CoA intermediate supplementation antagonizes PZA action
- Mutations in panD associate with POA resistance
- CoA-dependent pathways are crucial for persistent cell metabolism [81]
3.1.2 Protonophore Activity The protonophore model proposes that PZA/POA acts as a weak acid proton shuttle that disrupts membrane potential and cytoplasmic pH homeostasis [80]. Under this model:
- PZA diffuses into the cell and is converted to POA
- POA anion is exported but reprotonated in acidic extracellular environments
- HPOA re-enters the cell and dissociates, releasing protons and acidifying the cytoplasm
- This cyclic process collapses the proton motive force and depletes cellular energy [80]
However, this model faces challenges as acidic pH is not strictly required for PZA activity under all conditions [80].
3.1.3 Synergy with Host Oxidative Stress Recent evidence reveals that PZA synergizes with host-derived reactive oxygen species (ROS) to enhance killing [81]. This synergistic activity helps explain the discrepancy between PZA's weak in vitro activity and potent in vivo efficacy:
- POA complexes with iron can catalyze hydroxyl radical formation from Hâ‚‚Oâ‚‚
- Sub-inhibitory PZA and Hâ‚‚Oâ‚‚ concentrations become bactericidal in combination
- PZA efficacy is diminished in infection models with impaired macrophage activation
- Thiol oxidation appears to be a key driver of this synergistic effect [81]
Table 1: Comparison of Proposed PZA Mechanisms of Action
| Mechanism | Key Components | Supporting Evidence | Limitations/Challenges |
|---|---|---|---|
| Coenzyme A Disruption | PanD (aspartate decarboxylase), CoA biosynthesis | panD mutations confer resistance; CoA intermediates antagonize PZA | Does not fully explain pH dependence of activity |
| Protonophore Activity | pH gradient, membrane potential, proton shuttling | Disruption of cytoplasmic pH; energy depletion | Acidic pH not absolutely required in all conditions |
| Oxidative Stress Synergy | Host ROS, iron complexes, hydroxyl radicals | Potentiation with Hâ‚‚Oâ‚‚; required ROS for macrophage activity | Mechanism of interaction with bacterial metabolism unclear |
PZA Activity in Biofilm and Nutrient Gradient Contexts
Nutrient transitions and heterogeneous microenvironments in biofilms serve as potent inducers of bacterial persistence [29]. As nutrients become depleted in biofilm subzones, bacilli activate stress responses that promote transition to non-replicating states. The stringent response mediated by (p)ppGpp and nucleoid-associated proteins have been implicated in this persister formation pathway [29]. PZA appears particularly effective against populations experiencing these metabolic stresses, potentially through its disruption of CoA-dependent pathways essential for metabolic adaptation.
The relationship between nutrient gradients, persistence, and PZA activity can be visualized as follows:
Experimental Approaches and Methodologies
Assessing PZA Susceptibility and Persister Formation
4.1.1 Time to Detection (TTD) Persister Assay Recent research has developed a TTD assay using the BD BACTEC MGIT 960 system to quantify persister formation after PZA exposure [82]. This method detects viable bacilli that survive antibiotic pressure, even at concentrations far exceeding MIC values.
Protocol Summary:
- Inoculate M. tuberculosis H37Rv in MGIT tubes containing various PZA concentrations (including 20×MIC)
- Load tubes into BACTEC MGIT 960 system for continuous monitoring
- Record time until positive growth detection indicating persister regrowth
- Compare TTD across concentrations to assess persister formation dynamics
- Even at high PZA concentrations (20×MIC), not all bacteria are killed, demonstrating persister formation [82]
4.1.2 In Vitro Synergy with Oxidative Stress To evaluate PZA-ROS synergistic interactions [81]:
Protocol Summary:
- Grow M. tuberculosis to mid-exponential phase in 7H9 medium (pH 5.8)
- Add PZA (200 µg/mL) or vehicle control and incubate for 3 days
- Expose aliquots to geometric concentration series of Hâ‚‚Oâ‚‚
- Plate for CFU enumeration after treatment
- Include controls with diamide (thiol oxidant) to test thiol stress potentiation
- For macrophage models: Use IFN-γ activated macrophages and include ROS inhibition controls
Single-Cell Analysis of Persister Dynamics
Advanced microfluidic devices enable visualization of persister cell histories and heterogenous responses [83]. The Membrane-Covered Microchamber Array (MCMA) allows:
- Enclosure of individual cells in 0.8-µm deep microchambers
- Monolayer bacterial growth with flexible medium control
- Tracking of >10ⶠindividual cells before/during antibiotic exposure
- Correlation of pre-exposure growth status with survival outcomes
Table 2: Quantitative Data on PZA Efficacy and Persister Formation
| Parameter | Values/Measurements | Experimental Context | Source |
|---|---|---|---|
| PZA MIC | Variable with pH; activity increases at pH 5.8 | M. tuberculosis in culture | [80] |
| Persister Fractions | 10â»â¶ to 10â»Â³ of population | Various bacterial species and antibiotics | [83] |
| PZA Resistance Rate | ~70% with pncA mutations | Clinical isolates | [80] |
| Treatment Shortening | 3 months reduction | Clinical trials with PZA | [80] |
| Synergistic Killing | Bactericidal with sub-MIC Hâ‚‚Oâ‚‚ | M. tuberculosis culture | [81] |
Research Toolkit: Essential Reagents and Methods
Table 3: Key Research Reagents for PZA and Persister Studies
| Reagent/Resource | Function/Application | Key Features |
|---|---|---|
| BD BACTEC MGIT 960 | Automated PZA susceptibility and persister detection | Measures time to detection; enables high-throughput screening |
| Microfluidic MCMA | Single-cell persister history tracking | Enables visualization of >10ⶠindividual cells; membrane-controlled environment |
| PZA/Panalogues | Mechanism of action studies | Prodrug requires bacterial activation; structural variants probe specificity |
| Hâ‚‚Oâ‚‚/Diamide | Oxidative stress synergy studies | Diamide specifically induces thiol oxidation; Hâ‚‚Oâ‚‚ mimics phagosomal ROS |
| pH-controlled media | Conditional PZA activity assessment | Acidic pH (5.5-6.0) induces PZA susceptibility in culture models |
| CoA intermediates | Pathway rescue experiments | Test CoA disruption mechanism; include β-alanine, pantothenate |
| IFN-γ activated macrophages | Host-pathogen interaction models | Produce ROS relevant to in vivo PZA activity; bridge in vitro-in vivo gap |
Pyrazinamide remains a cornerstone of TB therapy due to its unique activity against non-replicating persister populations that survive other antibiotics. Its mechanisms—particularly CoA metabolism disruption and synergy with host oxidative stress—provide crucial anti-persister activity within the heterogeneous microenvironment of biofilms and granulomas where nutrient gradients drive persistence.
Future research should focus on:
- Developing more potent PZA analogs with improved safety and efficacy
- Exploiting the PZA-ROS synergy for host-directed therapies
- Targeting persister formation pathways induced by nutrient transitions
- Optimizing combination regimens that maximize PZA's anti-persister activity
Understanding PZA's action within the framework of nutrient gradient effects on persistence provides valuable insights for developing more effective therapies against chronic bacterial infections and biofilm-associated diseases.
Assessing the Efficacy of Combination Therapies Against Biofilm Infections
Biofilms are complex, surface-attached microbial communities embedded in a self-produced matrix of extracellular polymeric substances (EPS), which act as a protective barrier [1]. This structure is a primary factor in the difficulty of treating biofilm-associated infections, as it provides physical and physiological resistance to antimicrobial agents and the host immune system [84] [1]. A critical component of this resistance is the presence of bacterial persisters—a subpopulation of genetically drug-susceptible, non-growing, or slow-growing bacteria that can survive antibiotic exposure and other environmental stresses [11]. After the stress is removed, persisters can regrow, leading to relapse of the infection [11] [60]. The formation and survival of persisters are heavily influenced by heterogeneity within the biofilm, particularly the establishment of nutrient gradients [11]. Spatial gradients of nutrients and oxygen create varied microenvironments, driving a subset of bacteria into a dormant, persistent state that is recalcitrant to conventional antibiotics that typically target active cellular processes [11] [60]. This interplay between biofilm architecture, nutrient limitation, and persister formation represents a significant obstacle in clinical practice and frames the critical need for innovative therapeutic strategies, such as combination therapies, designed to penetrate biofilms and target all bacterial subpopulations [84].
The Scientific Basis: Nutrient Gradients and Persister Formation in Biofilms
The structured environment of a biofilm is not uniform. As the community matures, consumption of nutrients and oxygen by cells on the periphery creates diffusion limitations, leading to spatial gradients of these essential compounds [11]. This results in heterogeneous microenvironments, including areas deep within the biofilm that are nutrient-depleted and hypoxic [60].
Bacteria residing in these harsh, nutrient-poor niches undergo profound physiological adaptations to survive. One key survival strategy is the induction of a dormant or slow-growing state, which is the hallmark of bacterial persisters [11] [60]. This dormancy is orchestrated by several interconnected molecular mechanisms, which are activated in response to nutrient stress and other environmental cues. The table below summarizes the core mechanisms linking nutrient gradients to persister formation.
Table 1: Core Mechanisms of Persister Formation Induced by Nutrient Gradients
| Mechanism | Key Elements | Role in Persistence |
|---|---|---|
| Stringent Response [11] [60] | ppGpp, RelA, SpoT | Triggered by amino acid starvation; leads to global reprogramming of gene expression, downregulating energy-intensive processes (like translation) and promoting dormancy. |
| Toxin-Antitoxin (TA) Modules [11] [60] | HipA/HipB, HokB, ObgE | Environmental stress triggers degradation of the antitoxin, freeing the toxin to inhibit essential cellular processes (e.g., translation, membrane potential), inducing growth arrest. |
| Reduced Metabolic Activity [60] | Downregulated TCA cycle | In inner biofilm regions, low metabolism prevents production of reactive oxygen species, a key component of antibiotic-induced killing, enhancing survival. |
The relationship between spatial location and persistence is complex. While the "fortress model" suggests that the nutrient-limited core of the biofilm is a sanctuary for persisters, some studies indicate that cells at the periphery, with better access to nutrients, can also form robust, persistent subpopulations [60]. This highlights the phenotypic heterogeneity within biofilms and the need for therapies that can address multiple bacterial states simultaneously. The following diagram illustrates the logical progression from nutrient gradient formation to the development of therapeutic tolerance.
Emerging Combination Therapies: Mechanisms and Targets
Monotherapy with conventional antibiotics often fails against biofilm infections because it cannot simultaneously disrupt the physical EPS barrier, eradicate dormant persisters, and kill actively growing cells. Combination therapies are designed to overcome this by leveraging synergistic effects between agents with complementary mechanisms of action [84] [1]. Current research focuses on several strategic approaches, categorized by their primary target.
Table 2: Categories of Combination Therapies for Biofilm Eradication
| Therapy Category | Key Components | Mechanism of Action | Example Combinations |
|---|---|---|---|
| EPS-Targeting + Antibiotics [84] [1] | Enzymes (Dornase alfa, Dispersin B), Chelators, Nanoparticles | Degrades the structural matrix (e.g., eDNA, polysaccharides), enhancing antibiotic penetration into the biofilm. | Enzyme-based therapy + Antibiotic washes [84] |
| Anti-Virulence + Antibiotics [84] | Quorum Sensing Inhibitors (e.g., cinnamoyl hydroxamates), Anti-biofilm peptides (CRAMP-34) | Disrupts bacterial communication (QS) and virulence without killing, reducing pathogenicity and sensitizing bacteria to antibiotics. | QS inhibitor + reduced dose antibiotic [84] |
| Metabolic Stimulants + Antibiotics [11] | Metabolites, Carbon sources | "Wakes up" dormant persisters by stimulating metabolic activity, making them vulnerable to killing by conventional antibiotics. | Specific metabolites + Aminoglycosides [11] |
| Nanomaterial-Based + Antibiotics [84] [1] | Biogenic Zinc Nanoparticles (ZnNPs), Gold Nanoparticles | Physically disrupts biofilm structure, generates reactive oxygen species, and can be used for targeted drug delivery. | ZnNPs + Antibiotics [84] |
| Non-Antibiotic Adjuvants + Antibiotics [84] | Ibuprofen, Simvastatin, Statins, Natural Compounds (crocetin) | Has intrinsic anti-virulence properties, reduces biofilm formation, and can enhance the efficacy of standard antibiotics. | Ibuprofen + Antibiotic vs. S. aureus [84] |
The workflow for developing and testing these therapies typically follows a multi-stage process, from in vitro validation to advanced in vivo models, as outlined below.
Experimental Protocols for Efficacy Assessment
Robust and standardized experimental protocols are essential for accurately evaluating the efficacy of novel combination therapies. The following sections provide detailed methodologies for key assays.
Biofilm Cultivation and Treatment
- Biofilm Growth Model: Grow biofilms in relevant in vitro models such as:
- Static 96-well plates: For high-throughput screening of anti-biofilm compounds [1].
- Flow-cell systems: To study biofilms under shear stress conditions that more closely mimic physiological environments (e.g., urinary catheters) [85] [1].
- Use standardized media and incubation times (e.g., 24-48 hours) appropriate for the bacterial species.
- Treatment Application: Prepare fresh solutions of the test compounds. For combination therapy, apply them simultaneously or in a pre-determined sequence. Include controls:
- Untreated biofilm (negative control).
- Biofilm treated with a known effective antibiotic (positive control).
- Vehicle control (e.g., DMSO).
- Incubation: Incubate the biofilms with the treatments for a specified period (e.g., 4-24 hours) under conditions optimal for bacterial growth.
Assessment of Biofilm Viability and Biomass
- Viability Staining and Quantification:
- Gently wash the biofilm to remove non-adherent cells and antibiotics.
- Stain using a fluorescent viability kit, such as:
- SYTO9/Propidium Iodide (PI): SYTO9 labels all cells (green), while PI penetrates only membrane-compromised dead cells (red).
- Alternative Staining (Calcein AM/TMA-DPH): Calcein AM indicates esterase activity in live cells, while TMA-DPH labels biomass, offering enhanced consistency across species [84].
- Quantify fluorescence using a microplate reader or, for spatial analysis, confocal microscopy.
- Biomass Staining (Crystal Violet):
- Fix the biofilm with methanol or ethanol.
- Stain with 0.1% crystal violet solution for 15-20 minutes.
- Wash off excess stain, solubilize the bound stain with acetic acid or ethanol, and measure the optical density at 570-600 nm [1].
Advanced 3D Image Analysis with BiofilmQ
For a spatially resolved analysis of biofilm structure and composition after treatment, follow these steps [85]:
- Image Acquisition: Acquire 3D image stacks of the stained biofilms using a confocal laser scanning microscope.
- Software Segmentation:
- Import the 3D image stack into BiofilmQ.
- Identify the biovolume of the biofilm using one fluorescence channel (e.g., a general biomass stain). BiofilmQ offers automatic (e.g., Otsu, Ridler-Calvard) or semi-manual thresholding with immediate visual feedback to ensure accurate segmentation.
- Image Cytometry:
- If single-cell segmentation is not possible due to resolution, dissect the biofilm biovolume into a cubical grid. The cube size can be adjusted to approximate cell volume for microcolonies or to analyze multicell regions in larger colonies.
- BiofilmQ will compute dozens of cytometric properties for each cube, including fluorescence intensity, local density, and distance to the biofilm surface.
- Data Analysis and Visualization:
- Analyze the quantified data to determine parameters such as:
- Global Parameters: Total biovolume, mean thickness, surface area, and roughness.
- Internal Parameters: Spatial distribution of live/dead cells, gradient of metabolic activity, and correlation between different fluorescence reporters (e.g., matrix components vs. viability).
- Use BiofilmQ's inbuilt visualization tools to create editable figures showing the spatial effects of the treatment within the biofilm architecture.
- Analyze the quantified data to determine parameters such as:
The Scientist's Toolkit: Essential Reagents and Materials
Table 3: Key Research Reagent Solutions for Biofilm and Persister Studies
| Reagent/Material | Function/Application | Example Use-Case |
|---|---|---|
| Calcein AM & TMA-DPH [84] | A two-dye staining system for assessing biofilm viability (Calcein AM for live cells) and residual biomass (TMA-DPH). | An alternative to SYTO9/PI staining; provides enhanced consistency and sensitivity for viability assays across different bacterial species. |
| Cinnamoyl Hydroxamates [84] | Synthetic small-molecule inhibitors of bacterial Quorum Sensing (QS). | Used in combination with reduced antibiotic doses to disarm bacterial virulence and prevent resistance development in P. aeruginosa. |
| Iminosugars (e.g., PDIA) [84] | A class of synthetic compounds with biofilm-inhibitory properties. | Evaluated in an in vivo wound infection mouse model to treat biofilm-associated skin infections caused by S. aureus and P. aeruginosa. |
| Biogenic Zinc Nanoparticles (ZnNPs) [84] | Green-synthesized nanoparticles with antimicrobial and antibiofilm activity. | Used as sustainable, multifunctional agents against both planktonic and biofilm-forming states of various pathogens. |
| BiofilmQ Software [85] | Image cytometry tool for automated, high-throughput 3D quantification and visualization of biofilm-internal properties. | To analyze spatiotemporal effects of treatments on biofilm architecture, gene expression, and matrix component localization. |
| Dornase Alfa (DNase) [84] [1] | An enzyme that degrades extracellular DNA (eDNA), a key component of the biofilm matrix. | Applied to disrupt the biofilm structure, facilitating the penetration of co-administered antibiotics. |
| Anti-biofilm Peptide (CRAMP-34) [84] | A peptide that promotes biofilm disassembly from within by enhancing bacterial motility. | Used to induce dispersion of A. lwoffii biofilms, making the cells more susceptible to eradication. |
The transition from laboratory findings to clinical trial design represents a critical juncture in therapeutic development for persistent bacterial infections. This whitepaper examines the current scientific understanding of nutrient gradient effects on persister cell formation in biofilms, detailing the mechanistic pathways involved and proposing standardized methodologies for both basic research and clinical translation. By integrating quantitative data on bacterial persistence mechanisms with practical experimental protocols, we provide a framework for researchers and drug development professionals to bridge the gap between bench discoveries and bedside applications, with particular emphasis on targeting the unique metabolic adaptations of biofilm-associated persister cells.
Bacterial persisters are a subpopulation of genetically drug-susceptible, quiescent (non-growing or slow-growing) cells that survive antibiotic exposure and other stress conditions, only to regrow once the stress is removed, thereby causing recurrent infections [11]. Unlike antibiotic resistance, which involves stable genetic mutations, persistence is a transient, phenotypic tolerance that enables bacteria to survive lethal antibiotic concentrations without undergoing genetic change [60]. This phenomenon was first identified by Joseph Bigger in 1944 when he observed that a small subpopulation of Staphylococcus survived penicillin treatment [60] [11]. The recurrence of bacterial infectious diseases is closely associated with these bacterial persisters, which can escape antibiotic treatment by entering a metabolic state of low activity through various mechanisms including biofilm formation, toxin-antitoxin modules, the stringent response, and the SOS response [60].
The presence of persister cells poses significant challenges for treating chronic and persistent infections such as tuberculosis, urinary tract infections, and biofilm-associated infections in immunocompromised patients [60] [11]. In clinical settings, persisters underlie problems of relapse infections after treatment, drug resistance development, and biofilm infections [11]. The failure of antibiotic treatment may not be solely due to resistance, as persistence may also play a significant role, particularly in cases where antibiotic concentrations fluctuate periodically during treatment [60].
Nutrient Gradients and Persister Formation: Mechanisms and Pathways
Biofilm Microenvironments as Niches for Persister Formation
Biofilms are complex, surface-attached microbial communities encased in an extracellular polymeric substance (EPS) matrix that provides physical protection for embedded bacteria [1]. The architectural complexity of biofilms creates heterogeneous microenvironments with gradients of nutrients, oxygen, pH, and metabolic waste products [1]. This spatial organization generates distinct ecological niches that significantly influence bacterial behavior and phenotype, including the formation of persister cells [60] [1].
Within mature biofilms, cells at the periphery typically have better access to nutrients, while those in the core experience nutrient limitation and hypoxia [60] [1]. This nutrient heterogeneity creates ideal conditions for persister formation, as nutrient starvation serves as a key environmental trigger for the transition to a dormant, persistent state [29]. The physical structure of the biofilm matrix itself acts as a barrier that imped antibiotic penetration while simultaneously creating the nutrient gradients that stimulate persistence mechanisms [60] [1].
Molecular Mechanisms of Nutrient-Induced Persistence
The Central Role of Stringent Response and ppGpp
The stringent response represents a conserved global transcriptomic adaptation to environmental stress, particularly nutrient starvation, and plays a fundamental role in persister formation [60]. This response is mediated by the signaling molecule guanosine tetraphosphate (ppGpp), which is controlled by Rel/Spo homolog and small alarmone synthetase proteins [60]. When bacterial cells encounter nutrient limitation, particularly amino acid starvation, ppGpp accumulates and triggers a dramatic reprogramming of cellular metabolism, redirecting resources away from growth and division and toward maintenance and survival pathways [60] [29].
ppGpp serves as a central mediator of bacterial persistence by integrating multiple stress signals and coordinating the transition to dormancy [29]. It modulates cellular processes through direct interaction with target proteins and by regulating transcription through association with RNA polymerase [60]. The pivotal role of ppGpp in persistence has been demonstrated in Escherichia coli, where carbon source transitions stimulate persister formation through a pathway dependent on the ppGpp synthase RelA and nucleoid-associated proteins (NAPs) such as FIS and HU [29].
Toxin-Antitoxin Modules and Persistence Regulation
Toxin-antitoxin (TA) modules represent another key mechanism underlying bacterial persistence in response to nutrient stress [60]. These genetic elements consist of a toxin protein that inhibits essential cellular processes (such as translation, replication, or membrane integrity) and a corresponding antitoxin that neutralizes the toxin's activity [60]. Under favorable growth conditions, toxins and antitoxins form stable complexes; however, nutrient stress triggers the degradation of antitoxins, freeing toxins to induce cellular dormancy [60].
TA modules are categorized into eight types (I-VIII) based on the nature and mode of action of their antitoxin components [60]. Type I systems utilize antisense RNA molecules that inhibit toxin translation, while Type II systems, the most extensively studied, employ protein antitoxins that bind and inhibit protein toxins [60]. In E. coli, the HipA toxin phosphorylates glutamyl-tRNA synthetase, thereby inhibiting translation and triggering growth arrest, while multiple TA modules act synergistically to promote persistence during exponential growth phase [60]. The activation of TA modules is intimately connected to nutrient sensing pathways, with the Lon protease playing a crucial role in antitoxin degradation under starvation conditions [60].
Table 1: Key Molecular Mechanisms in Nutrient-Induced Persister Formation
| Mechanism | Key Components | Role in Persistence | Response to Nutrient Gradients |
|---|---|---|---|
| Stringent Response | ppGpp, RelA, SpoT | Induces dormancy via metabolic shutdown | Activated by amino acid and carbon starvation |
| Toxin-Antitoxin Modules | HipBA, MazEF, RelBE | Growth arrest through targeting essential cellular processes | Antitoxin degradation under nutrient stress |
| Nucleoid-Associated Proteins | FIS, HU, H-NS | Chromosome organization and gene regulation | Expression modulated by nutrient availability |
| Biofilm Matrix | Extracellular polymeric substances (EPS) | Physical barrier creating nutrient heterogeneity | Limits nutrient diffusion, creating gradients |
Quantitative Analysis of Nutrient Gradient Effects on Persistence
Experimental Models for Studying Nutrient Gradients and Persistence
Research into nutrient gradients and persister formation has employed various experimental models that replicate key aspects of biofilm environments. The colony biofilm model has proven particularly valuable for investigating how nutrient transitions influence persistence [29]. In this system, bacteria are grown on polyethersulfone (PES) membranes positioned on agar plates containing defined nutrient compositions, allowing precise control over nutrient availability and transitions [29].
This approach enables researchers to simulate the nutrient gradients encountered in natural biofilm environments, where peripheral cells consume preferred nutrients, leaving less favorable substrates for cells in deeper layers [29]. By manipulating the carbon sources available in the agar substrate and monitoring bacterial growth and persister formation, researchers have demonstrated that diauxic shifts (transitions between preferred and secondary carbon sources) serve as potent inducers of bacterial persistence [29].
Other models include flow-cell systems that permit real-time observation of biofilm development under controlled nutrient conditions, as well as microfluidic devices that enable the creation of defined nutrient gradients and high-resolution analysis of single-cell responses [60]. Each model offers distinct advantages for investigating specific aspects of nutrient gradient effects on persistence, with the colony biofilm system providing exceptional control over nutrient transitions while maintaining physiological relevance to in vivo biofilm communities [29].
Quantitative Data on Nutrient Transitions and Persister Frequencies
Experimental studies have generated quantitative data linking specific nutrient conditions to persister frequencies. Research using the colony biofilm model with E. coli has demonstrated that carbon source transitions significantly increase persister formation [29]. Specifically, diauxic shifts from glucose to secondary carbon sources such as fumarate stimulate persister formation through a pathway requiring the ppGpp synthase RelA and nucleoid-associated proteins FIS and HU [29].
Table 2: Quantitative Effects of Nutrient Conditions on Persister Formation in E. coli Biofilms
| Nutrient Condition | Persister Frequency | Key Regulatory Factors | Experimental System |
|---|---|---|---|
| Continuous glucose | Baseline (reference) | N/A | Colony biofilm |
| Glucose to fumarate transition | Significantly increased | ppGpp, RelA, FIS, HU | Colony biofilm |
| Stationary phase | 100-fold higher than exponential | ppGpp, TA modules | Planktonic culture |
| Biofilm vs planktonic | Up to 1000-fold higher in biofilms | Multiple mechanisms | Comparative studies |
The importance of nutrient transitions is further highlighted by research showing that the proportion of persisters in isolated Pseudomonas aeruginosa from long-term treatment patients receiving periodic high-concentration antibiotics was 100 times higher than during early treatment stages, without significant changes in minimum inhibitory concentration (MIC) [60]. This clinical observation supports the laboratory findings that nutrient fluctuations and antibiotic exposure both contribute to enhanced persister formation in biofilm-associated infections.
Experimental Protocols and Methodologies
Colony Biofilm Model for Nutrient Transition Studies
The colony biofilm system provides a robust methodology for investigating nutrient transitions and persister formation under controlled conditions. The following protocol has been validated for studying carbon source transitions in E. coli biofilms [29]:
Bacterial strains and growth conditions:
- Use E. coli MG1655 as wild-type strain.
- Grow cells from -80°C stock for 4 hours in LB medium.
- Dilute 1:100 into 2 mL of 10 mM glucose M9 minimal media.
- Grow overnight for 16 hours at 37°C with shaking at 250 rpm.
Biofilm establishment:
- Dilute overnight culture into fresh M9 media containing 15 mM carbon content to OD600 of 0.01.
- Inoculate 100 μL aliquots onto sterile polyethersulfone (PES) membranes (0.2 μm pore size, 25 mm diameter).
- Position membranes on M9 minimal agar plates containing either 60 mM carbon content, no carbon, or LB.
- Incubate plates at 37°C for desired duration.
Growth monitoring:
- Aseptically remove PES membranes from agar at designated time points.
- Vortex in 2 mL of sterile PBS for 1 minute.
- Measure OD600 of resulting cell suspensions.
- Report growth as fold change in OD600 (FCOD600).
Carbon transition assay:
- Sample persisters prior to glucose exhaustion (FCOD600 ~14) at FCOD600 = 6.
- Sample persisters after glucose exhaustion at FCOD600 = 30.
- Compare persister frequencies between different nutrient conditions.
Persister quantification:
- Treat biofilm cells with lethal antibiotic concentrations (e.g., 5× MIC of ciprofloxacin or ampicillin).
- Determine viable counts by plating serial dilutions.
- Calculate persister frequency as CFU/mL after antibiotic treatment divided by CFU/mL before treatment.
High-Throughput Single-Cell Analysis Techniques
Advanced microscopy and microfluidic techniques enable detailed investigation of persister formation at the single-cell level:
Microscopy of colony biofilms:
- Use bacterial strains chromosomally modified with fluorescent reporter constructs (e.g., GFP under control of specific promoters).
- Grow biofilms as described above with appropriate inducer (e.g., 2 mM IPTG for PT5-GFP constructs).
- Analyze biofilm architecture and gene expression patterns using fluorescence microscopy.
- Correlate spatial position within biofilm with nutrient gradients and persister markers.
Microfluidic systems:
- Implement microfluidic devices with controlled nutrient gradient generation.
- Monitor single-cell responses to defined nutrient shifts in real time.
- Track cell division, growth rates, and persistence events at single-cell resolution.
- Combine with time-lapse microscopy for dynamic analysis.
Flow cytometry analysis:
- Dissociate biofilm cells at different growth phases.
- Stain with fluorescent dyes reporting metabolic activity (e.g., CFDA), membrane potential (e.g., DiOCâ‚‚(3)), or redox state.
- Sort subpopulations for further analysis or persister enrichment.
The following workflow diagram illustrates the key experimental approach for investigating nutrient gradient effects on persister formation:
The Scientist's Toolkit: Essential Research Reagents and Materials
Table 3: Essential Research Reagents for Nutrient Gradient and Persister Studies
| Reagent/Material | Specifications | Application/Function |
|---|---|---|
| Polyethersulfone (PES) Membranes | 0.2 μm pore size, 25 mm diameter | Support for colony biofilm growth with controlled nutrient diffusion |
| M9 Minimal Media | Standard formulation with defined carbon sources | Controlled nutrient environment for biofilm studies |
| Carbon Sources | Glucose, fumarate, succinate, etc. (various concentrations) | Creating nutrient transitions and diauxic shifts |
| Antibiotics | Ciprofloxacin, ampicillin, tobramycin, etc. (at 5× MIC) | Persister selection and quantification |
| Fluorescent Reporters | GFP, RFP under appropriate promoters | Visualization of gene expression and spatial organization |
| ppGpp Detection Kits | HPLC standards, antibody-based detection | Monitoring stringent response activation |
| Microfluidic Devices | Custom designs for gradient generation | Single-cell analysis under controlled nutrient gradients |
| Viability Stains | CFDA, propidium iodide, SYTO dyes | Assessment of metabolic activity and membrane integrity |
Translational Framework: From Mechanistic Insights to Clinical Trial Design
Therapeutic Targeting of Nutrient-Induced Persistence Pathways
The mechanistic understanding of nutrient gradient effects on persister formation reveals several promising therapeutic strategies for combating persistent infections:
Stringent Response Inhibitors: Small molecules targeting ppGpp synthesis or function could prevent the transition to dormancy triggered by nutrient gradients. Compounds that inhibit RelA/SpoT activity or mimic ppGpp antagonists may sensitize persisters to conventional antibiotics [60] [29].
TA Module Modulators: Agents that stabilize toxin-antitoxin complexes or prevent toxin activation could maintain bacterial growth during antibiotic exposure. Alternatively, controlled activation of specific toxins might induce bacterial apoptosis or growth arrest in a manner that prevents regrowth [60].
Biofilm Disruption Strategies: Approaches that disrupt biofilm architecture or nutrient gradient formation could reduce persister formation. This includes enzymes that degrade EPS matrix components, compounds that interfere with quorum sensing, or methods that enhance nutrient penetration into biofilm depths [1].
Metabolic Stimulation Approaches: "Awakening" persisters from dormancy through provision of specific metabolites or signaling molecules could sensitize them to conventional antibiotics. This approach requires precise timing to avoid widespread regrowth before antibiotic clearance [29].
Clinical Trial Design Considerations for Anti-Persister Therapies
Developing effective clinical trials for anti-persister therapies requires addressing several unique challenges:
Patient Stratification:
- Identify patient populations with high likelihood of persister-mediated infections (e.g., cystic fibrosis, chronic UTI, device-related infections).
- Develop biomarkers for persister burden, such as specific metabolic signatures or transcriptional profiles.
- Implement enrichment strategies to select patients most likely to benefit from persister-targeting approaches.
Endpoint Selection:
- Include relapse rates as primary endpoints, not just initial clearance.
- Consider time-to-relapse as key efficacy measure.
- Incorporate patient-reported outcomes relevant to chronic infection burden.
Trial Design Considerations:
- Implement randomized withdrawal designs after initial eradication therapy.
- Consider add-on designs where persister-targeting agents are tested in combination with standard care.
- Include extended follow-up periods to detect late relapses.
Combination Therapy Strategies:
- Develop rational combinations targeting multiple persistence mechanisms simultaneously.
- Sequence treatments to first awaken persisters followed by conventional antibiotics.
- Consider cyclic therapy approaches to prevent adaptation.
The following diagram illustrates the key signaling pathway through which nutrient gradients trigger persister formation, highlighting potential therapeutic intervention points:
The translation of laboratory findings on nutrient gradient effects and persister formation into effective clinical trial designs represents a promising frontier in combating persistent bacterial infections. By leveraging detailed mechanistic understanding of how nutrient heterogeneity within biofilms triggers persistence pathways, researchers can develop targeted strategies to eliminate this recalcitrant bacterial subpopulation. The integrated approach presented in this whitepaper—combining robust experimental models, molecular mechanism elucidation, and strategic therapeutic development—provides a framework for bridging the critical gap between basic research discoveries and clinical applications. As our understanding of bacterial persistence continues to evolve, so too will our ability to design innovative clinical trials that effectively address the challenge of recurrent and chronic infections, ultimately improving patient outcomes across a spectrum of infectious diseases.
Conclusion
Nutrient gradients are a fundamental and inherent feature of biofilms that directly orchestrate the formation and spatial distribution of persister cells. Understanding the interplay between environmental cues, such as carbon source transitions and starvation, and molecular mechanisms like the ppGpp-mediated stringent response provides a critical roadmap for innovation. The integration of sophisticated mathematical models with advanced experimental methodologies is essential to decode the spatiotemporal dynamics of persistence. Future research must focus on translating this knowledge into clinically viable strategies that disrupt the formation and maintenance of persister cells. Promising avenues include developing compounds that target dormant cell physiology, exploiting metabolic pathways to re-sensitize persisters, and designing smart treatment regimens informed by computational models. Ultimately, targeting the nutrient-driven pathways of persistence holds the key to overcoming chronic biofilm infections and mitigating the global threat of antimicrobial resistance.
References
- 1. Biofilms: structure, resistance mechanism, emerging control ... [https://pubs.rsc.org/en/content/articlehtml/2025/pm/d5pm00094g]
- 2. What We Still Don't Know About Biofilms—Current ... [https://www.mdpi.com/2036-7481/16/2/46]
- 3. Gradients and consequences of heterogeneity in biofilms [https://pmc.ncbi.nlm.nih.gov/articles/PMC9590228/]
- 4. Dissecting cell heterogeneities in bacterial biofilms and ... [https://www.sciencedirect.com/science/article/abs/pii/S1369527424000262]
- 5. Persisters of Bacterial Biofilms [https://www.intechopen.com/chapters/1211701]
- 6. Mathematical modelling of nutrient-dependent biofilm ... [https://arxiv.org/html/2509.18065v1]
- 7. Formation, architecture, and persistence of oral biofilms [https://www.frontiersin.org/journals/microbiology/articles/10.3389/fmicb.2025.1602962/full]
- 8. Analysis of biofilm assembly by large area automated AFM [https://www.nature.com/articles/s41522-025-00704-y]
- 9. Forging biofilms: metal-induced microbial responses in biofilm ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12632276/]
- 10. A distinct growth physiology enhances bacterial ... [https://www.nature.com/articles/s41467-021-23439-8]
- 11. Bacterial persisters: molecular mechanisms and ... [https://www.nature.com/articles/s41392-024-01866-5]
- 12. New Methodologies as Opportunities in the Study of Bacterial ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12114119/]
- 13. Nutrient Transitions Are a Source of Persisters in Escherichia ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC3965526/]
- 14. Effects of Specific Surface Area of Artificial Carriers on ... [https://www.mdpi.com/2073-4441/14/17/2735]
- 15. Microbial functional genes are driven by gradients in sediment ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC9377124/]
- 16. Mathematical modeling of dormant cell formation in ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC4446547/]
- 17. (p)ppGpp and Its Role in Bacterial Persistence [https://pmc.ncbi.nlm.nih.gov/articles/PMC7508602/]
- 18. Similar and Divergent Roles of Stringent Regulator (p) ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC9769547/]
- 19. (p)ppGpp imposes graded transcriptional changes to ... [https://www.nature.com/articles/s41522-025-00795-7]
- 20. Bacterial alarmone (p)ppGpp mediates the pathogenicity of ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12455917/]
- 21. The stringent promotes response dispersal in Pseudomonas... biofilm [https://pubmed.ncbi.nlm.nih.gov/29273811/]
- 22. Birth and Resuscitation of (p)ppGpp Induced Antibiotic ... [https://www.nature.com/articles/s41598-019-42403-7]
- 23. Variable Persister Gene Interactions with (p)ppGpp for ... [https://www.frontiersin.org/journals/microbiology/articles/10.3389/fmicb.2017.01795/full]
- 24. Type II toxin-antitoxin systems as stress-responsive ... [https://pubmed.ncbi.nlm.nih.gov/40970936/]
- 25. Bacterial Persister Cells and Development of Antibiotic ... - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC11335562/]
- 26. Comparative in silico analysis of vapBC3 toxin-antitoxin ... [https://www.nature.com/articles/s41598-025-24448-z]
- 27. Mini review: Persister cell control strategies - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC12568461/]
- 28. Bacterial Persister Cell Formation and Dormancy - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC3837759/]
- 29. Nutrient Transitions Are a Source of Persisters in Escherichia ... [https://journals.plos.org/plosone/article?id=10.1371/journal.pone.0093110]
- 30. Nutrient Gradients Mediate Complex Colony-Level ... [https://www.frontiersin.org/journals/microbiology/articles/10.3389/fmicb.2022.740259/full]
- 31. Comparison of biofilm cell quantification methods for ... [https://www.sciencedirect.com/science/article/abs/pii/S0167701217302786]
- 32. Intra-colony channels in E. coli function as a nutrient uptake ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC7490401/]
- 33. Comparative analysis of quantitative methodologies for ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC5035616/]
- 34. Incorporating toxin hypothesis into a mathematical model ... [https://www.sciencedirect.com/science/article/abs/pii/S0022519307002639]
- 35. Functional Tomographic Fluorescence of pH... Imaging [https://pmc.ncbi.nlm.nih.gov/articles/PMC2786433/]
- 36. Biofilm formation is correlated with low nutrient and simulated ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10009688/]
- 37. Bacterial single-cell RNA sequencing captures biofilm ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11585574/]
- 38. An improved bacterial single-cell RNA-seq reveals biofilm ... [https://elifesciences.org/articles/97543]
- 39. Quantitative image analysis of microbial communities with ... [https://www.nature.com/articles/s41564-020-00817-4]
- 40. Imaging Flow Cytometry to Study Biofilm-Associated ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC8659131/]
- 41. Agent Based Models of Polymicrobial Biofilms and the ... [https://www.mdpi.com/2076-2607/9/2/417]
- 42. The influence of the crowding assumptions in biofilm simulations [https://journals.plos.org/ploscompbiol/article?id=10.1371/journal.pcbi.1009158]
- 43. Optimization of periodic treatment strategies for bacterial ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11003776/]
- 44. A shared alarmone–GTP switch controls persister ... [https://www.nature.com/articles/s41564-025-02015-6]
- 45. Molecular mechanism and application of emerging ... [https://bmcmicrobiol.biomedcentral.com/articles/10.1186/s12866-024-03628-3]
- 46. Computer simulation study of early bacterial biofilm ... [https://www.nature.com/articles/s41598-018-23524-x]
- 47. Mathematical modelling of nutrient-dependent biofilm ... [https://arxiv.org/abs/2509.18065]
- 48. Micro-continuum modeling of biofilm growth coupled with ... [https://www.sciencedirect.com/science/article/pii/S2352711024003819]
- 49. Bacterial Persister Cells and Development of Antibiotic ... [https://www.frontierspartnerships.org/journals/british-journal-of-biomedical-science/articles/10.3389/bjbs.2024.12958/full]
- 50. Cell adhesion and fluid flow jointly initiate genotype spatial ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC5901778/]
- 51. Is Increased Biofilm Formation Associated with Decreased ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12566419/]
- 52. Mini review: Persister cell control strategies [https://www.frontiersin.org/journals/pharmacology/articles/10.3389/fphar.2025.1706115/full]
- 53. A machine learning framework for the prediction and ... [https://www.sciencedirect.com/science/article/pii/S2667318525000133]
- 54. Mechanisms of antimicrobial resistance in biofilms [https://www.nature.com/articles/s44259-024-00046-3]
- 55. Nanotechnology in combating biofilm: A smart and ... [https://www.frontiersin.org/journals/microbiology/articles/10.3389/fmicb.2022.1028086/full]
- 56. A Collection and Analysis of Simplified Data for a Better ... [https://www.mdpi.com/2076-2607/13/9/2048]
- 57. Nanotechnology-Based Drug Delivery Systems to Control ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10674810/]
- 58. Quantitative and Qualitative Assessment Methods for Biofilm ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC6133255/]
- 59. Biofilm, resistance, and quorum sensing: The triple threat in ... [https://www.sciencedirect.com/science/article/pii/S2950194625003462]
- 60. Recent Advances in Bacterial Persistence Mechanisms - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC10531727/]
- 61. The Global Challenge of Antimicrobial Resistance [https://pmc.ncbi.nlm.nih.gov/articles/PMC12284435/]
- 62. ä¼‘çœ ç»†èŒç»†èƒžä¸çš„ä¸»åŠ¨å¤–æŽ’â€”â€”å¯¹æŠ—ç”Ÿç´ è€è¯æ€§çš„新认识。 [https://suppr.wilddata.cn/browses/detail/pubmed/28363336]
- 63. Why antibiotics can fail even against non-resistant bacteria [https://www.sciencedaily.com/releases/2025/02/250205130936.htm]
- 64. A selective membrane-targeting repurposed antibiotic with ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC6697817/]
- 65. How do environment-dependent switching rates between ... [https://www.nature.com/articles/s41522-018-0049-2]
- 66. Combatting implant-associated biofilms through localized ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC6176123/]
- 67. A Pd-labile fluoroquinolone prodrug efficiently prevents biofilm ... [https://pubs.rsc.org/en/content/articlehtml/2024/ob/d4ob00014e]
- 68. Isolation of persister cells within the biofilm and relative ... [https://www.sciencedirect.com/science/article/pii/S2213716521002630]
- 69. Synergistic effect of antibiotic combinations on ... [https://www.sciencedirect.com/science/article/pii/S2590207522000028]
- 70. Quantitative analysis of persister fractions suggests different ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC3682893/]
- 71. Antibiotic persisters are metabolically active, non-growing ... [https://www.sciencedirect.com/science/article/pii/S0924857924003029]
- 72. From Dormancy to Eradication: Strategies for Controlling ... [https://www.mdpi.com/2304-8158/14/6/1075]
- 73. Antibiotic resistance and persistence—Implications for human ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC7726816/]
- 74. Persisters—as elusive as ever - PMC - PubMed Central - NIH [https://pmc.ncbi.nlm.nih.gov/articles/PMC4939303/]
- 75. In Vitro Persistence Level Reflects In Vivo Antibiotic ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10269860/]
- 76. Persister cells in human fungal pathogens - Research journals [https://journals.plos.org/plospathogens/article?id=10.1371/journal.ppat.1013483]
- 77. A rational approach to discovering new persister control ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12406675/]
- 78. Targeting Persisters for Tuberculosis Control - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC3346619/]
- 79. Mycobacterial biofilms: A therapeutic target against ... [https://www.sciencedirect.com/science/article/pii/S2405844024080344]
- 80. The Bewildering Antitubercular Action of Pyrazinamide - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC7062198/]
- 81. Oxidative stress drives potent bactericidal activity of ... [https://elifesciences.org/reviewed-preprints/105614]
- 82. Mycobacterium Tuberculosis Persister Cell Formation after ... [https://zoonoses-journal.org/index.php/2024/09/10/mycobacterium-tuberculosis-persister-cell-formation-after-pyrazinamide-exposure/]
- 83. Observation of persister cell histories reveals diverse ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12074638/]
- 84. Editorial: Fighting microbial biofilms: novel therapeutics ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12423030/]
- 85. Quantitative image analysis of microbial communities with ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC7840502/]