SOS Response and Antibiotic Tolerance: Mechanisms, Therapeutic Targeting, and Future Directions
This article provides a comprehensive analysis of the complex relationship between the bacterial SOS response and antibiotic tolerance for researchers and drug development professionals.
SOS Response and Antibiotic Tolerance: Mechanisms, Therapeutic Targeting, and Future Directions
Abstract
This article provides a comprehensive analysis of the complex relationship between the bacterial SOS response and antibiotic tolerance for researchers and drug development professionals. It explores the foundational mechanisms of this inducible DNA repair system, detailing how its activation by diverse antibiotic classes can promote survival, mutagenesis, and resistance dissemination. The content covers advanced methodological approaches for studying SOS dynamics, examines challenges in therapeutic targeting—including paradoxical SOS-independent resistance pathways—and offers a comparative analysis of strategies to suppress this evolvability mechanism. By synthesizing foundational knowledge with recent findings on non-canonical resistance pathways, this review aims to inform the development of next-generation antibacterial adjuvants designed to counteract tolerance and resistance.
The SOS Response: A Bacterial Survival Mechanism Against Antibiotic Stress
The SOS response is a conserved global regulatory network in prokaryotes that addresses DNA damage through coordinated expression of DNA repair genes. This inducible system, first articulated by Evelyn Witkin and detailed by Miroslav Radman, represents the first coordinated stress response to be elucidated in bacteria [1]. The core regulatory mechanism hinges on the interaction between two key proteins: the LexA repressor and the RecA coprotease. Within the context of antibiotic resistance research, understanding this mechanism is paramount. The SOS response promotes genetic diversity through error-prone repair, facilitating the evolution of antibiotic resistance [1] [2]. This technical guide examines the LexA repression and RecA-mediated derepression mechanisms, detailing their operational dynamics and profound implications for antimicrobial resistance development.
Core Regulatory Mechanism
The SOS response regulation is a precisely timed process that maintains genomic integrity while balancing mutagenic risks. Under normal growth conditions, the LexA protein functions as the master transcriptional repressor for the SOS regulon. LexA forms a homodimer through its C-terminal domain, while its N-terminal domain binds specifically to a 20-base-pair consensus sequence known as the SOS box within the promoter regions of SOS genes [3]. The canonical SOS box sequence is a near-perfect palindrome: TACTG(TA)5CAGTA [3]. The strength of LexA binding varies across genes due to deviations from this consensus sequence, allowing for graded gene expression during the response [1].
The triggering event for SOS induction occurs when DNA damage, such as that caused by UV radiation or antibiotics like ciprofloxacin, generates single-stranded DNA (ssDNA) regions at stalled replication forks [1] [3]. RecA protein binds to this ssDNA in an ATP-dependent fashion, forming a nucleoprotein filament referred to as RecA* [3]. This activated RecA* filament facilitates the autocleavage of LexA at a specific Ala84-Gly85 peptide bond, located within the linker region connecting its two domains [3]. LexA self-cleavage inactivates its DNA-binding capacity and exposes degradation signals, leading to ClpXP and Lon protease-mediated degradation [3]. The resulting decrease in cellular LexA concentration derepresses SOS genes according to their binding affinity for LexA, with weakly bound genes expressing first and strongly bound genes expressing later in the response sequence [1].
Table 1: Key Components of the SOS Core Regulatory Mechanism
| Component | Function | Activation/Cleavage Characteristics |
|---|---|---|
| LexA Repressor | Transcriptional repressor; binds SOS boxes in promoter regions of ~50 genes | Homodimer with N-terminal DNA-binding domain and C-terminal catalytic domain; undergoes self-cleavage between Ala84-Gly85 |
| RecA Coprotease | DNA strand exchange protein; nucleoprotein filament formation on ssDNA | ATP-dependent binding to ssDNA forms RecA*; stimulates LexA autocleavage |
| SOS Box | LexA binding operator sequence (5'-TACTG(TA)5CAGTA-3') | Palindromic consensus; binding affinity varies with deviation from consensus |
| ssDNA | Primary inducing signal | Generated at stalled replication forks; RecA nucleoprotein filament platform |
Connection to Antibiotic Tolerance and Resistance
The SOS response contributes significantly to antibiotic resistance through multiple mechanisms that enhance bacterial survival and genetic adaptation. Error-prone DNA polymerases induced during the late SOS response constitute a primary pathway for resistance development. DNA polymerases IV (DinB) and V (UmuD'â‚‚C) facilitate translesion synthesis across damaged DNA templates at the cost of increased mutation rates, a phenomenon termed the "mutator phenotype" or hypermutation [2] [3]. This elevated mutation frequency accelerates the acquisition of resistance-conferring mutations in genes encoding antibiotic targets [2].
Research demonstrates that SOS-inducing antibiotics like ciprofloxacin and even non-antibiotic agents like zidovudine trigger this mutator phenotype in vivo. Experimental data from rabbit intestinal infection models show that exposure to these induces significantly increases resistance frequencies to unrelated antibiotics including rifampin, minocycline, and fosfomycin [2]. Beyond genetic resistance, the SOS response promotes phenotypic tolerance through mechanisms such as the tisB-istR toxin-antitoxin system, which induces persister cell formation—a transient, non-replicating state that protects a bacterial subpopulation from antibiotic killing [1].
The SOS response also facilitates horizontal gene transfer by activating integron recombination systems. Sub-inhibitory concentrations of antibiotics (1/2 MIC to 1/4 MIC) induce recA expression, which in turn activates integrase expression in class 1 and class 2 integrons, promoting capture and expression of antibiotic resistance gene cassettes [4]. Recent findings reveal alternative resistance pathways where RecA deficiency unexpectedly accelerates β-lactam resistance evolution through SOS-independent mechanisms involving impaired DNA repair and reactive oxygen species accumulation, highlighting the complex interplay between DNA repair systems and resistance development [5].
Table 2: SOS Response Role in Antibiotic Resistance Mechanisms
| Resistance Mechanism | SOS Component Involved | Experimental Evidence |
|---|---|---|
| Hypermutation | DNA Pol IV (DinB), Pol V (UmuDC) | 2-4 log increase in rifampin/minocycline resistance frequency after ciprofloxacin/zidovudine exposure [2] |
| Integron Recombination | RecA-mediated intI activation | Sub-MIC ciprofloxacin, ampicillin, kanamycin induce recA and intI2 expression; peak at day 3 of induction [4] |
| Phenotypic Persistence | TisB toxin expression | DNA damage-induced persister cell formation via tisB-istR system [1] |
| SOS-Independent Resistance | RecA deficiency with β-lactams | 20-fold MIC increase to ampicillin in ΔrecA E. coli within 8 hours; stable resistance after 7-day passage [5] |
Experimental Approaches and Methodologies
In Vitro SOS Induction and Hypermutation Assay
Purpose: To quantify SOS-induced hypermutation leading to antibiotic resistance [2].
Method Details:
- Bacterial Strains: Enteropathogenic E. coli strains (e.g., B171-8, E22) or clinical isolates containing integrons (e.g., Proteus mirabilis) [2] [4].
- SOS Induction: Expose mid-log phase cultures to sub-inhibitory concentrations of SOS-inducing agents (e.g., 1/4-1/2 MIC ciprofloxacin, 0.2 μg/mL mitomycin C, or 0.4-0.6 μg/mL zidovudine) for 8-24 hours [2] [4].
- Mutation Frequency Analysis: Plate induced cultures on antibiotic selection plates (rifampin 100 μg/mL, minocycline 10-12 μg/mL, or fosfomycin 300 μg/mL). Count resistant colonies after 24-48 hours incubation [2].
- SOS Inhibition Testing: Include zinc acetate (0.3-0.5 mM) in parallel experiments to assess SOS inhibition, using iron sulfate or manganese chloride as negative controls [2].
- Calculation: Mutation frequency = (CFU on antibiotic plate) / (total CFU on non-selective plate).
Key Considerations: Rifampin-resistant colonies typically appear within 24h, while minocycline-resistant colonies may require 48h incubation for visible growth [2]. Use multiple biological replicates (≥3) due to potential "jackpot" effects in mutation distribution [2].
Gene Expression Analysis During SOS Induction
Purpose: To measure temporal expression patterns of SOS regulon genes under antibiotic stress [4].
Method Details:
- Strain Preparation: Construct clinical isolate-derived strains containing functional or non-functional integrons via recombinant plasmids (e.g., pACYC184-based with chloramphenicol resistance) transformed into E. coli TOP10 [4].
- Induction Protocol: Subject strains to continuous induction with 1/2 MIC and 1/4 MIC antibiotics (ciprofloxacin, ampicillin, kanamycin) or 0.2 μg/mL mitomycin C for 8 days with daily subculturing in fresh antibiotic-containing media [4].
- Sampling Timepoints: Collect samples at days 1, 3, and 8 for RNA extraction and qRT-PCR analysis [4].
- Gene Targets: Quantify expression of recA, lexA, integron integrase (intI2), and resistance gene cassettes (dfrA1, sat2, aadA1) [4].
- Normalization: Use housekeeping genes (e.g., 16S rRNA) as internal controls for relative quantification.
Key Considerations: Expression peaks typically occur at day 3, with slight decline by day 8 [4]. Include antibiotic susceptibility testing (Kirby-Bauer or MIC determination) pre- and post-induction to correlate expression changes with resistance phenotypes [4].
In Vivo SOS Response in Infection Models
Purpose: To validate SOS-induced resistance development in biologically relevant environments [2].
Method Details:
- Animal Model: Rabbit ligated ileal loop model inoculated with enteropathogenic E. coli (e.g., strain E22) [2].
- SOS Induction: Directly inject SOS-inducing agents (e.g., 0.4-0.6 μg/mL zidovudine or ciprofloxacin) into intestinal loops [2].
- Sample Collection: Aspirate intestinal fluid after 8-12 hours for bacterial enumeration and resistance frequency determination [2].
- Analysis: Plate intestinal fluid dilutions on selective antibiotic plates to quantify resistance frequency development in vivo [2].
- Inhibition Studies: Co-administer zinc acetate (0.3 mM) with SOS inducers to assess SOS blockade in vivo [2].
Key Considerations: Account for background microbiota in uninfected control loops. Fluid accumulation measurement validates infection establishment [2].
SOS Pathway Regulation
The Scientist's Toolkit
Table 3: Essential Research Reagents for SOS Response Studies
| Reagent/Cell Line | Specifications & Function | Application Examples |
|---|---|---|
| E. coli TOP10 | F- mcrA Δ(mrr-hsdRMS-mcrBC) φ80 lacZΔM15 ΔlacX74 recA1 araΔ139 Δ(ara-leu)7697 galU galK rpsL endA1 nupG; general cloning host | Plasmid propagation for integron studies [4] |
| E. coli JW2669-1 | ΔrecA::kan from Coli Genetic Stock Centre (CGSC); recA-deficient strain | SOS-independent resistance mechanisms [5] |
| Rabbit EPEC E22 | Enteropathogenic E. coli strain adapted to rabbit infection model | In vivo SOS response in intestinal environment [2] |
| Proteus mirabilis 5b/7b | Clinical isolates with functional (5b) and non-functional (7b) class 2 integrons | Integrase expression and recombination studies [4] |
| pACYC184 Vector | Cloning vector, P15A origin, chloramphenicol resistance (cat gene) | Construction of integron-containing recombinant plasmids [4] |
| SOS-Inducing Agents | Ciprofloxacin (1/4-1/2 MIC), Mitomycin C (0.2 μg/mL), Zidovudine (0.4-0.6 μg/mL) | Direct SOS pathway activation in experimental systems [2] [4] |
| SOS Inhibitors | Zinc acetate (0.3-0.5 mM); blocks RecA filament formation | Negative control for SOS-specific effects [2] |
| Selection Antibiotics | Rifampin (100 μg/mL), Minocycline (10-12 μg/mL), Fosfomycin (300 μg/mL) | Quantifying mutation frequencies and resistance development [2] |
| Orismilast | Orismilast, CAS:1353546-86-7, MF:C19H15Cl2F2NO7S, MW:510.3 g/mol | Chemical Reagent |
| Letermovir | Letermovir|CMV DNA Terminase Inhibitor|Research Only | Letermovir is a CMV DNA terminase complex inhibitor for research use only (RUO). Not for human consumption. Explore its unique mechanism and applications. |
SOS Experimental Workflow
The core regulatory mechanism of LexA repression and RecA-mediated derepression represents a sophisticated bacterial adaptation system that directly influences antibiotic resistance evolution. The precise molecular interplay between these regulators determines the timing and magnitude of DNA repair responses, balancing error-free and error-prone repair pathways. Contemporary research reveals that targeting this system, particularly through RecA inhibition with compounds like zinc, presents a promising adjuvant strategy for extending antibiotic efficacy. However, the emergence of SOS-independent resistance mechanisms in recA-deficient backgrounds underscores the remarkable adaptability of bacterial pathogens. Future therapeutic development must account for these parallel pathways while exploiting vulnerabilities in the SOS response to combat the escalating antimicrobial resistance crisis.
The bacterial SOS response is a conserved DNA damage repair network that is critically implicated in bacterial survival, antibiotic tolerance, and the evolution of resistance. This inducible system senses genotoxic stress and coordinates a multifaceted cellular response aimed at DNA repair. A comprehensive understanding of SOS response triggers and activation mechanisms is paramount for developing novel therapeutic strategies to counteract antimicrobial resistance. This whitepaper details the primary inducers of the SOS response, the molecular mechanisms of its activation, and its direct consequences on antibiotic efficacy and resistance development, providing a technical guide for researchers and drug development professionals.
The SOS response is a tightly regulated genetic network controlled by the key regulators RecA and LexA. Under normal physiological conditions, the LexA repressor protein binds to specific DNA sequences (SOS boxes) in the promoter regions of SOS genes, suppressing their transcription [6]. The SOS regulon in Escherichia coli comprises over 48 genes involved in various DNA repair processes, cell division control, and mutagenesis [7].
Genotoxic stress leads to the accumulation of single-stranded DNA (ssDNA), which can result from replication fork stalling or direct DNA damage. RecA protein monomers polymerize on this ssDNA, forming nucleoprotein filaments (RecA*) in an ATP-dependent process. These activated filaments facilitate the autocleavage of the LexA repressor, alleviating transcriptional repression and inducing the expression of SOS genes [7] [6]. This sequence of events enables cells to repair DNA damage, but also promotes error-prone repair and other adaptations linked to antibiotic resistance.
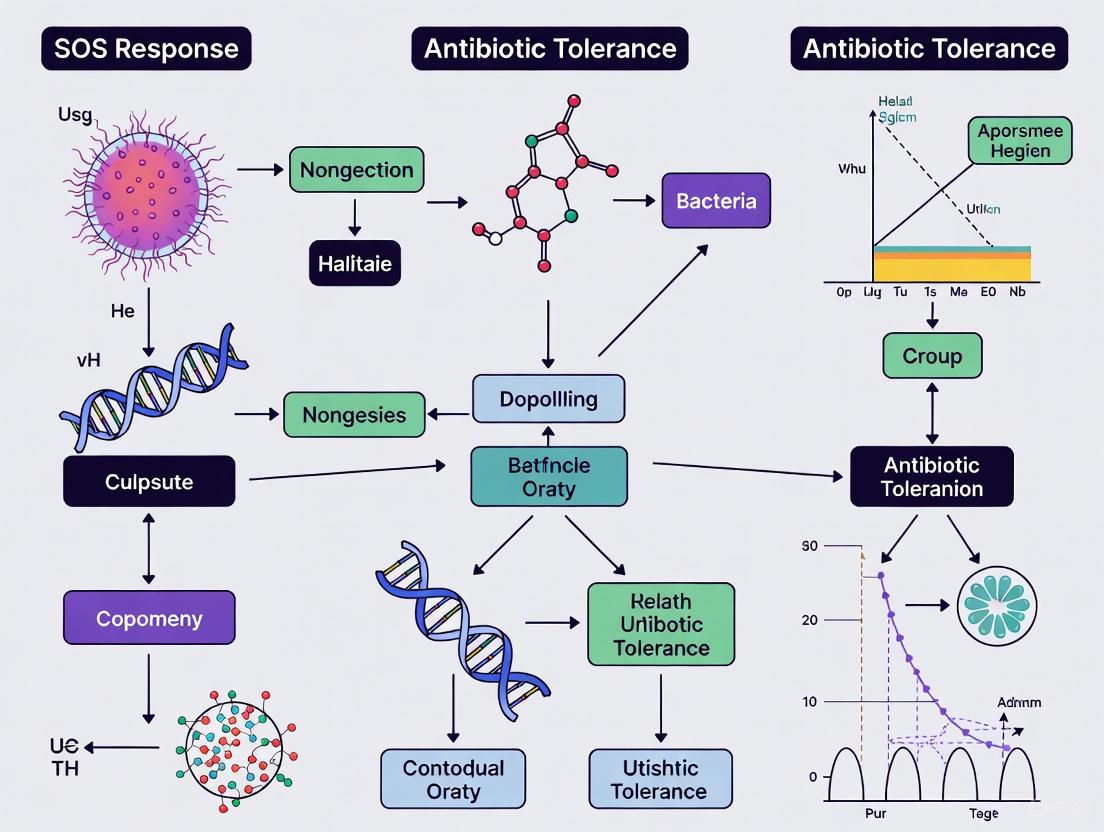
The following diagram illustrates this core regulatory circuit:
Figure 1. The Core SOS Response Regulatory Circuit. Genotoxic stress leads to ssDNA formation, triggering RecA filament assembly and LexA repressor cleavage. This derepresses the SOS regulon, driving diverse cellular phenotypes with significant implications for antibiotic resistance.
Triggers of the SOS Response
The SOS response can be activated by a wide array of physical agents, chemical compounds, and antibiotic classes that directly or indirectly cause DNA damage or disrupt DNA replication.
Direct DNA-Damaging Agents
- UV Radiation: Causes cyclobutane pyrimidine dimers and (6-4) photoproducts that stall replication forks, generating ssDNA and activating RecA.
- Mitomycin C (MMC): A potent DNA crosslinker that induces severe DNA damage, leading to a hyper-induced SOS response with up to 100-fold increase in SOS gene expression (sulA, recN) [7].
- Reactive Oxygen Species (ROS): Antibiotic-induced oxidative stress generates superoxide radicals (Oâ‚‚â»), hydrogen peroxide (Hâ‚‚Oâ‚‚), and hydroxyl radicals (OH•) that cause DNA lesions, indirectly activating SOS [6].
Antibiotic Classes and Their Induction Mechanisms
Different antibiotic classes trigger the SOS response through distinct primary mechanisms, as summarized in Table 1.
Table 1: SOS Response Induction by Major Antibiotic Classes
| Antibiotic Class | Primary Target | SOS Induction Mechanism | Key Evidence |
|---|---|---|---|
| Fluoroquinolones (e.g., Ciprofloxacin) | DNA gyrase, Topoisomerase IV | Direct DNA double-strand breaks via stabilized enzyme-DNA cleavage complexes [8] [9]. | 14-20 fold increase in sulA and recN expression; significant induction of conjugative transfer elements [7] [9]. |
| β-Lactams (e.g., Ampicillin, Cefotaxime) | Penicillin-binding proteins (cell wall synthesis) | Indirect via DpiBA two-component system; impaired cell wall integrity signals through DpiA to disrupt replication [6] [5]. | 5-fold SOS gene induction; significant increase in plasmid conjugation frequency independent of SOS levels [7]. |
| Aminoglycosides (e.g., Kanamycin) | 30S ribosomal subunit | Indirect through electron transport chain disruption, increased ROS production, and subsequent oxidative DNA damage [8] [6]. | Increased killing rates in DSBR-deficient strains; SOS-mediated mutagenesis observed [8]. |
| Trimethoprim | Dihydrofolate reductase | Indirect via nucleotide pool depletion and replication stress; induces promutagenic SOS response [8]. | DSBR defects dampen SOS induction and increase killing rates [8]. |
Beyond these established pathways, recent research reveals surprising complexity in SOS induction. The methylated adenine recognition and restriction (Mrr) endonuclease can trigger SOS under hyperpressure conditions [6]. Furthermore, the CcdAB toxin-antitoxin system activates SOS through a mechanism similar to quinolones, where CcdB poisons DNA gyrase [6].
Quantitative Experimental Data: Antibiotic Effects on SOS and Conjugation
The relationship between antibiotic-induced SOS response and plasmid conjugation frequency is complex and not always correlated. Research demonstrates that different antibiotics varying in their primary mechanisms of action can differentially impact the SOS response and conjugative transfer.
Table 2: SOS Induction and Conjugation Frequency Across Antibiotic Treatments
| Antibiotic Treatment | SOS Gene Fold-Change | tra Gene Fold-Change | Conjugation Frequency | Proposed Mechanism |
|---|---|---|---|---|
| Cefotaxime (β-lactam) | ~5x increase [7] | Increased [7] | Significantly increased [7] | SOS-independent; likely via increased expression of transfer and pilus proteins [7]. |
| Ciprofloxacin (Quinolone) | 14-20x increase [7] | Unaffected [7] | Unaffected [7] | Strong SOS induction without conjugation promotion; suggests distinct regulatory pathways. |
| Mitomycin C (DNA crosslinker) | ~100x increase [7] | Increased [7] | Significantly increased [7] | Hyper-induction of both SOS and conjugation apparatus. |
| Combination (CTX + MMC) | High induction [7] | Upregulated [7] | Not significantly different from untreated [7] | Saturation effect or potential negative regulatory cross-talk. |
The data reveal that SOS induction levels and conjugation frequency are uncorrelated, suggesting the involvement of alternative regulatory pathways in antibiotic-induced conjugation [7]. For instance, cefotaxime increases conjugation with minimal SOS induction, while ciprofloxacin triggers strong SOS response without affecting conjugation.
Essential Methodologies for SOS Response Research
Measuring SOS Activity and Gene Expression
Flow Cytometry with GFP Reporters:
- Protocol: Utilize reporter strains where SOS-responsive promoters (e.g., sulA, recN, lexA) drive GFPmut2 or GFPmut3 expression. Grow cultures to mid-exponential phase (OD₆₀₀ ≈ 0.8) in appropriate media with inducers. For intracellular pH standardization, dilute samples in pH-buffered PBS with sodium benzoate (60 mM) to collapse ΔpH. Analyze fluorescence from ≥10,000 cells/sample using a flow cytometer [10].
- Key Considerations: GFPmut3 is preferred for pH-sensitive measurements due to its excitation spectrum. Maintain 200 µM arabinose for high cytoplasmic GFP expression [10].
Quantitative PCR (qPCR):
- Protocol: Extract RNA from antibiotic-exposed and control cells at mid-exponential phase using a commercial kit. Treat with DNase I, reverse transcribe to cDNA, and perform qPCR using primers for SOS genes (sulA, recN) and housekeeping genes. Express data as fold-change using the 2^(-ΔΔCt) method [7].
- Application: Used to demonstrate a 5-fold (sulA, recN) increase with cefotaxime and 14-20 fold increase with ciprofloxacin [7].
Assessing Genetic Outcomes
Mutation Frequency and Rate Analysis:
- Fluctuation Test (Luria-Delbrück): Plate 96 independent cultures on selective media (e.g., rifampicin) with/without antibiotic pre-treatment. Count resistant colonies to determine mutation frequency distribution. Use non-parametric statistical tests (Kruskal-Wallis) and maximum likelihood estimation (MLE) to calculate mutation rates, distinguishing between selective enrichment and increased mutagenesis [5].
- Application: Identified that ampicillin treatment in ΔrecA strains enriches pre-existing resistant mutants rather than increasing general mutagenesis [5].
Conjugation Frequency Assay:
- Protocol: Mix donor and recipient strains at a standardized ratio (e.g., 1:1). Expose to sub-MIC antibiotics during mating. Plate serial dilutions on selective media to count transconjugants. Calculate transfer frequency as transconjugants per donor [7].
- Key Finding: Cefotaxime and mitomycin C increase conjugation frequency, while ciprofloxacin does not, despite strong SOS induction [7].
The Scientist's Toolkit: Key Research Reagents
Table 3: Essential Reagents for SOS Response Research
| Reagent / Tool | Function / Feature | Research Application | Key References |
|---|---|---|---|
| KEIO Collection | Single-gene knockout mutants in E. coli BW25113. | Source of isogenic strains (e.g., ΔrecA, ΔfumC) for phenotypic comparison. | [10] [11] |
| ASKA Library | Complete E. coli ORF library for protein expression. | Complementation experiments (e.g., RecA expression in ΔrecA mutant). | [10] |
| pCP20 Plasmid | FLP recombinase source for antibiotic marker excision. | Removal of Kaná´¿ cassettes after gene knockout via FRT site recombination. | [8] [11] |
| λRED Recombinase System | Plasmid (e.g., pKD46) for homologous recombination. | Targeted gene disruption and allele replacement via PCR products. | [8] [12] |
| SOS-GFP Reporter Plasmids | GFP under control of SOS promoters (sulA, recN). | Real-time monitoring of SOS induction via flow cytometry or microscopy. | [10] |
| LexA Cleavage Variants | LexA mutants with altered cleavage rates (e.g., S119A, E86P). | Generating strains with constitutively repressed or hyper-induced SOS. | [12] |
| Levistolide A | Levistolide A, CAS:88182-33-6, MF:C24H28O4, MW:380.5 g/mol | Chemical Reagent | Bench Chemicals |
| Emapticap pegol | Lexaptepid Pegol | Lexaptepid pegol is a pegylated anti-hepcidin Spiegelmer® for research on anemia of chronic disease. For Research Use Only. Not for human use. | Bench Chemicals |
SOS-Independent Resistance and Therapeutic Targeting
Recent findings demonstrate that antibiotic resistance can evolve through SOS-independent pathways. recA-deficient E. coli exposed to β-lactams rapidly develop stable, multi-drug resistance via a two-step mechanism: (1) recA deletion impairs DNA repair and downregulates antioxidant defenses, increasing reactive oxygen species (ROS) and genetic instability; (2) antibiotic pressure selectively enriches resistant mutants from this hypermutable population [13] [5]. This repair-redox axis represents a significant, alternative pathway for resistance evolution.
These insights have spurred investigation into SOS pathway inhibition as an antibacterial adjuvant strategy. Key approaches include:
- RecA Inhibition: Small molecules like suramin disrupt RecA nucleoprotein filament formation and ATP hydrolysis, preventing LexA cleavage and SOS induction [6].
- LexA Cleavage Inhibition: Compounds such as 5-amino-1-(carbamoylmethyl)-1H-1,2,3-triazole-4-carboxamide scaffold-based molecules prevent LexA autoproteolysis [6].
- Combination Therapies: Co-targeting SOS with other stress pathways (e.g., ΔfumC/ΔrecA double mutants) significantly enhances susceptibility to cephalosporins and quinolones [11]. Zinc acetate can block SOS-induced hypermutation to rifampin and minocycline in vivo [2].
The following diagram synthesizes the relationship between antibiotic triggers, SOS activation, and resistance outcomes, highlighting potential therapeutic intervention points:
Figure 2. SOS Response Triggers, Outcomes, and Therapeutic Interventions. Multiple pathways converge on SOS activation, promoting resistance through mutagenesis and gene transfer. SOS-independent pathways and pharmacological inhibitors represent emerging therapeutic frontiers.
The SOS response represents a critical bacterial survival mechanism against genotoxic stress, including that imposed by diverse antibiotic classes. While the RecA-LexA axis constitutes the core regulatory pathway, recent research reveals surprising complexity, including SOS-independent resistance mechanisms and the uncoupling of SOS induction from phenotypes like conjugation. A deep understanding of these triggers and mechanisms provides the foundation for innovative therapeutic strategies. Targeting the SOS response and its associated pathways with adjuvant compounds presents a promising approach to potentiate existing antibiotics, suppress resistance development, and extend the lifespan of our current antimicrobial arsenal.
The SOS response is a conserved, global transcriptional network in prokaryotes that is activated in response to DNA damage. Originally identified in Escherichia coli as an inducible system for responding to ultraviolet (UV) radiation, this sophisticated DNA repair system represents the first coordinated stress response to be elucidated in bacteria [1] [3]. While this pathway provides a survival advantage by enabling bacteria to cope with DNA damage, its induction has significant consequences for antibiotic resistance research. The error-prone nature of key SOS-controlled DNA repair mechanisms accelerates bacterial evolution under antimicrobial pressure, facilitating the development of resistance phenotypes [14] [2] [6]. This technical guide examines the molecular machinery of the SOS regulon, with particular emphasis on its error-prone repair systems and their contribution to the antimicrobial resistance crisis, providing experimental methodologies and resources crucial for researchers targeting this pathway.
Molecular Mechanism of the SOS Response
Core Regulatory Circuit: LexA and RecA
The SOS regulatory system operates through a precisely controlled molecular circuit centered on two key proteins: LexA and RecA. Under normal growth conditions, the LexA repressor protein binds to a specific DNA sequence known as the SOS box within the promoter regions of genes comprising the SOS regulon, effectively repressing their transcription [1] [3]. The SOS box consensus sequence is a near-palindromic 20-base-pair operator (TACTG(TA)5CAGTA) [3].
The activation trigger occurs when DNA damage results in the accumulation of single-stranded DNA (ssDNA) regions, typically generated when DNA polymerase stalls at replication forks blocked by template lesions [1] [3]. The RecA protein binds to these ssDNA regions in an ATP-dependent fashion, forming a nucleoprotein filament referred to as RecA [1] [15]. This activated RecA complex facilitates the autocleavage of the LexA repressor at a specific Ala84-Gly85 bond, inactivating its DNA-binding capacity and targeting it for proteolytic degradation by ClpXP and Lon proteases [3]. With LexA repression lifted, the SOS genes are sequentially derepressed according to the affinity of their respective SOS boxes for LexA [1].
The following diagram illustrates this core regulatory pathway:
Temporal Regulation of the SOS Response
The SOS response exhibits sophisticated temporal regulation, with genes induced in a specific sequence based on their LexA binding affinity and cellular priorities [1] [3]. The following table summarizes this phased induction pattern:
Table 1: Temporal Regulation of SOS Gene Induction
| Induction Phase | Timing | Key Genes Induced | Gene Functions | Repair Fidelity |
|---|---|---|---|---|
| Early | Immediate | uvrA, uvrB, uvrD |
Nucleotide excision repair | Error-free |
recA, recN |
Homologous recombination | Error-free | ||
| Middle | Intermediate | polB (Pol II), dinB (Pol IV) |
Translesion synthesis | Error-prone |
sulA |
Cell division inhibition | - | ||
| Late | Delayed/Persistent Damage | umuC, umuD (Pol V) |
Translesion synthesis | Highly error-prone |
Genes with weak SOS boxes (e.g., lexA, recA, uvrA, uvrB) are fully induced even with mild DNA damage, prioritizing error-free repair mechanisms like nucleotide excision repair (NER) [1]. If initial repair attempts fail and DNA damage persists, further reduction in LexA concentration leads to expression of genes with stronger SOS boxes (e.g., sulA, umuD, umuC), resulting in error-prone translesion synthesis and potentially mutagenic outcomes [1] [3].
Error-Prone DNA Polymerases and the Mutasome Complex
Biochemical Characterization of SOS DNA Polymerases
The mutagenic potential of the SOS response primarily resides in three inducible DNA polymerases that conduct translesion synthesis (TLS) - replicating past DNA lesions that would stall the accurate replicative polymerase [3] [15]. These specialized polymerases exhibit reduced fidelity but greater flexibility in accommodating damaged DNA templates.
Table 2: Error-Prone SOS DNA Polymerases
| Polymerase | Gene | Induction Kinetics | Catalytic Subunit | Error Rate | Primary Lesion Bypass |
|---|---|---|---|---|---|
| Pol II | polB |
Middle | PolB (single subunit) | Moderate | Extension from mispaired primer termini |
| Pol IV | dinB |
Middle | DinB (single subunit) | 10â»Â³ - 10â»â´ | Bulky adducts, fork rescue |
| Pol V | umuDC |
Late | UmuC | 10â»Â² - 10â»Â³ | Abasic sites, UV photoproducts |
Pol V Mutasome: Structure and Activation
DNA polymerase V represents the primary SOS mutagenic polymerase, responsible for the majority of damage-induced mutations [15]. Its activation requires a complex, multi-step process resulting in the formation of the pol V mutasome:
- Transcription and Translation: The
umuDCoperon is transcribed and translated following LexA cleavage, producing UmuD and UmuC proteins [15]. - Post-Translational Modification: UmuD undergoes RecA-facilitated autocleavage to form UmuD' [15].
- Complex Assembly: UmuD'â‚‚ forms a complex with UmuC (UmuD'â‚‚C) [15].
- RecA Transfer: A RecA monomer is transferred from the 3'-proximal tip of the RecA* nucleoprotein filament to UmuD'â‚‚C [15].
- ATP Binding: The UmuD'â‚‚C-RecA complex binds ATP to form the active mutasome (pol V Mut = UmuD'â‚‚C-RecA-ATP) [15].
The resulting mutasome complex is capable of DNA synthesis across both damaged and undamaged DNA templates, with its mutagenic potential tightly constrained through four regulatory levels: (1) temporal control via targeted proteolysis; (2) spatial sequestration of UmuC on the cell membrane; (3) intrinsic DNA-dependent ATPase activity; and (4) conformational regulation depending on RecA positioning [15].
The biochemical activity of pol V Mut is significantly enhanced by interaction with the β-sliding processivity clamp, which serves dual stabilizing roles: canonical tethering at the primer-3'-terminus and inhibition of pol V Mut's ATPase to reduce mutasome-DNA dissociation rates [15].
SOS Response in Antibiotic Resistance and Tolerance
Mechanisms Linking SOS to Resistance Acquisition
The SOS response contributes to antibiotic resistance through multiple interconnected mechanisms that present significant challenges in clinical settings:
Hypermutation and Mutator Phenotype: Induction of error-prone DNA polymerases (Pol II, IV, and V) increases mutation rates by 100-fold or more, creating a "mutator phenotype" that accelerates the acquisition of resistance-conferring mutations [1] [2]. This elevated mutation frequency directly facilitates the evolution of resistance to antibiotics like rifampin, minocycline, and fosfomycin [2].
Horizontal Gene Transfer: SOS induction promotes the transfer of resistance genes through conjugation and transformation, facilitating the spread of resistance determinants across bacterial populations [3] [6].
Biofilm Formation and Persistence: SOS activation enhances biofilm formation and promotes the generation of bacterial persister cells - dormant variants that exhibit multidrug tolerance - through toxin-antitoxin systems like TisB-IstR [1] [6].
Stress Response Integration: The SOS response interacts with other stress responses (oxidative stress, envelope stress) through shared regulators and overlapping gene networks, creating a coordinated defense system against antimicrobial agents [14] [6].
SOS-Independent Resistance Pathways
Recent research has revealed intriguing SOS-independent resistance mechanisms, particularly in response to β-lactam antibiotics. Studies demonstrate that recA-deficient E. coli can rapidly develop stable, multi-drug resistance after a single exposure to ampicillin [5]. This paradoxical finding suggests an alternative pathway where RecA deletion impairs DNA repair and downregulates base excision repair while concurrently repressing antioxidative defense genes. The resulting oxidative environment leads to excessive accumulation of reactive oxygen species (ROS), promoting mutation and enriching resistant clones under antibiotic selection pressure [5].
Experimental Analysis of SOS Response
Key Methodologies and Protocols
In Vitro SOS Induction and Mutation Frequency Assay
Purpose: Quantify SOS-induced hypermutation and its contribution to antibiotic resistance development [2].
Protocol:
- Bacterial Strains: Use appropriate E. coli strains (e.g., EPEC E22, B171-8) or target pathogens.
- SOS Induction: Expose mid-log phase cultures to subinhibitory concentrations of SOS-inducing agents:
- Ciprofloxacin: 0.01-0.05 μg/mL (strain-dependent)
- Zidovudine: 10-50 μg/mL
- Co-treatment Conditions: Include experimental groups with SOS inhibitors:
- Zinc acetate: 0.1-0.5 mM
- Iron sulfate or manganese chloride: 0.1-0.5 mM (as negative controls)
- Mutation Selection: Plate induced cultures on antibiotic selection plates after 18-24 hours induction:
- Rifampin: 100 μg/mL
- Minocycline: 6-12 μg/mL (incubate 48 hours for colony development)
- Fosfomycin: 25-50 μg/mL
- Frequency Calculation: Calculate mutation frequency as (CFU on selective media) / (total CFU on non-selective media) [2].
In Vivo Rabbit Intestinal Loop Model
Purpose: Evaluate SOS-induced hypermutation in a physiologically relevant environment [2].
Protocol:
- Surgical Preparation: Anesthetize rabbits and exteriorize small intestine.
- Loop Creation: Ligate 4-5 cm intestinal segments, leaving vascularization intact.
- Inoculation: Inject into each loop:
- Test: 10⸠CFU EPEC E22 + SOS inducer (zidovudine 0.4-0.6 μg/mL or ciprofloxacin)
- Control: 10⸠CFU EPEC E22 alone
- Inhibition test: Add zinc acetate (0.3 mM) to inhibitor group
- Incubation: Maintain loops for 8 hours in situ.
- Sample Collection: Aspirate intestinal fluid, serially dilute, and plate on selective antibiotics.
- Analysis: Calculate in vivo mutation frequencies and compare to parallel in vitro experiments [2].
Genotoxicity Testing (SOS Chromotest)
Purpose: Rapid colorimetric assessment of compound genotoxicity through SOS induction [1].
Protocol:
- Engineered Strain: Use E. coli with lacZ gene under control of SOS-responsive promoter, plus uvrA mutation (excision repair deficient) and rfa mutation (LPS-deficient for improved chemical permeability) [1].
- Exposure: Incurate strain with test compounds for 2-4 hours.
- Substrate Addition: Add lactose analog that produces colored compound when cleaved by β-galactosidase.
- Quantification: Measure color development spectrophotometrically; intensity correlates with SOS induction level and genotoxic potential [1].
Research Reagent Solutions
Table 3: Essential Research Reagents for SOS Response Studies
| Reagent/Category | Specific Examples | Function/Application | Experimental Notes |
|---|---|---|---|
| SOS Inducers | Ciprofloxacin, Zidovudine | Direct DNA damage or inhibition of replication | Use subinhibitory concentrations (e.g., 0.01-0.05 μg/mL ciprofloxacin) |
| SOS Inhibitors | Zinc acetate, Suramin, p-Coumaric acid | Block RecA function or LexA cleavage | Zinc (0.1-0.5 mM) specifically inhibits SOS-induced hypermutation |
| Bacterial Strains | E. coli EPEC E22, B171-8, JW2669-1 (ΔrecA) | Model organisms for SOS studies | Rabbit EPEC E22 essential for in vivo intestinal loop models |
| Selection Antibiotics | Rifampin, Minocycline, Fosfomycin | Detect resistance emergence through mutation | Minocycline requires 48h incubation for colony development |
| Plasmid Constructs | recA complementation vector | Genetic rescue experiments | Native promoter ensures physiological expression levels |
| Detection Systems | SOS chromotest strain (uvrA-, rfa-) | High-throughput genotoxicity screening | Colorimetric readout via β-galactosidase activity |
Therapeutic Targeting of the SOS Response
The SOS pathway represents a promising target for antimicrobial adjuvants that could extend the efficacy of existing antibiotics. Several inhibitory approaches have been identified:
- RecA Inhibition: Small molecules like suramin disrupt RecA filament formation and ATP hydrolysis, preventing LexA autocleavage and SOS induction [6].
- LexA Stabilization: Compounds such as 5-amino-1-(carbamoylmethyl)-1H-1,2,3-triazole-4-carboxamide scaffold derivatives inhibit LexA autoproteolysis [6].
- Zinc Supplementation: Physiological concentrations of zinc acetate (0.1-0.5 mM) specifically inhibit SOS-induced hypermutation without affecting bacterial growth, showing efficacy in both in vitro and in vivo models [2].
- Natural Compounds: Plant-derived phenolics like p-coumaric acid exhibit dual antibacterial and SOS-inhibitory activity [6].
The following diagram illustrates the experimental workflow for evaluating SOS inhibition:
Combining SOS inhibitors with conventional antibiotics represents a promising strategy to reduce the emergence of resistance during treatment, potentially extending the clinical lifespan of valuable antimicrobial agents [2] [6].
The SOS regulon represents a sophisticated bacterial adaptation system that presents both challenges and opportunities in antibiotic resistance research. Its error-prone DNA repair polymerases, particularly those assembled into the pol V mutasome complex, serve as significant drivers of bacterial evolution under antimicrobial pressure. The experimental frameworks and reagent tools outlined in this technical guide provide foundation for advancing research in this critical area. As the understanding of SOS-independent resistance mechanisms grows, simultaneous targeting of multiple bacterial stress response pathways may offer the most promising approach for mitigating the ongoing antimicrobial resistance crisis.
Linking SOS Activation to Antibiotic Tolerance and Persister Cell Formation
The SOS response, a conserved bacterial DNA damage repair pathway, has been identified as a pivotal mechanism in the development of antibiotic tolerance and persister cell formation. This in-depth technical review examines the molecular interplay between SOS activation and bacterial survival strategies, highlighting how this response facilitates the emergence of phenotypically tolerant subpopulations that withstand antibiotic treatment. Within the broader context of antibiotic tolerance research, understanding SOS-mediated persistence provides critical insights for addressing chronic and relapsing infections. We consolidate current experimental data, methodological frameworks, and emerging therapeutic approaches targeting this pathway, providing researchers and drug development professionals with a comprehensive resource for advancing anti-persister strategies.
Bacterial persisters are a subpopulation of genetically drug-susceptible cells that enter a transient, slow-growing or dormant state, enabling them to survive high-dose antibiotic exposure and potentially cause relapse infections [16]. These cells differ from resistant bacteria in that they do not possess genetic resistance mutations and return to antibiotic susceptibility upon regrowth [16]. Persisters are increasingly recognized as a critical factor in chronic and biofilm-associated infections that are difficult to eradicate with conventional antibiotics [17] [16].
The SOS response represents a fundamental bacterial survival mechanism coordinated by the RecA-LexA regulatory system [18]. When bacterial DNA is damaged, RecA protein polymerizes on single-stranded DNA (RecA*), triggering LexA repressor auto-cleavage and derepression of SOS genes [18]. This pathway activates a temporally regulated DNA repair cascade, beginning with high-fidelity repair mechanisms and progressing to error-prone translesion synthesis polymerases when damage persists [18]. Beyond its canonical DNA repair function, the SOS response influences multiple aspects of bacterial pathogenesis, including biofilm formation, virulence, and importantly, antibiotic tolerance and persistence [18].
Molecular Mechanisms Linking SOS to Persistence
Core SOS Signaling Pathway
The SOS pathway initiates when DNA damage generates single-stranded DNA (ssDNA) regions, typically through replication fork stalling or direct DNA strand breaks. RecA binding to ssDNA forms nucleoprotein filaments (RecA) that facilitate LexA repressor autocleavage. LexA inactivation derepresses approximately 50 SOS genes in *Escherichia coli, including DNA repair enzymes, error-prone polymerases, and cell division inhibitors [18].
Figure 1: SOS Response Pathway Leading to Persister Formation. DNA damage triggers RecA activation and LexA cleavage, enabling SOS gene expression that promotes both DNA repair and persistence mechanisms.
SOS-Regulated Persistence Mechanisms
The SOS response promotes persistence through several molecular mechanisms:
Toxin-Antitoxin System Activation: The E. coli TisB/IstR module is the first documented SOS-regulated toxin-antitoxin system directly involved in persister formation [18]. TisB toxin expression disrupts membrane potential and reduces metabolism, inducing a dormant state.
Cell Division Inhibition: SOS-induced SulA protein halts cell division by inhibiting FtsZ polymerization, preventing chromosomal segregation in damaged cells and contributing to dormancy [18].
Error-Prone Repair and Mutagenesis: SOS-induced DNA polymerases (PolII, PolIV, PolV) increase mutation rates during stress, potentially generating genetic diversity that favors persistence and resistance development [18].
Biofilm Enhancement: SOS response promotes biofilm formation through RecA-dependent mechanisms, creating protected environments with elevated persister frequencies [18].
Interplay with Other Stress Responses
The SOS pathway integrates signals from multiple stress response systems:
Stringent Response: Nutrient starvation triggers (p)ppGpp production, which stalls replication forks and induces SOS via ssDNA accumulation [18].
Oxidative Stress: Reactive oxygen species (ROS) cause DNA damage directly and indirectly via impaired antioxidant defenses in RecA-deficient cells [5].
General Stress Response: RpoS and RpoH sigma factors regulate SOS components, connecting DNA damage to broader stress adaptation [18].
Quantitative Analysis of SOS-Mediated Persistence
Experimental Killing Kinetics Data
Time-kill assays reveal distinct kinetic patterns in SOS-proficient and deficient strains, characterized by multiphasic killing with persistent subpopulations.
Table 1: Time-Kill Parameters for E. coli Exposed to β-Lactam Antibiotics (10× MIC)
| Parameter | Piperacillin-Tazobactam | Cefotaxime | Meropenem | Ciprofloxacin |
|---|---|---|---|---|
| Bacteriostatic Phase (min) | 66.2 (60.6-71.7) | 57.4 (49.8-65.0) | 43.3 (37.8-48.8) | Absent |
| Half-Life, First Kill Phase (min) | 2.9 (2.5-3.4) | 3.3 (2.9-3.7) | 4.6 (4.0-5.2) | 4.4 (3.9-4.9) |
| MDK99 (min) | 162 (149-175) | 151 (137-165) | 149 (134-164) | 115 (105-125) |
| Persister Proportion (cells/10âµ CFU) | 57 (32-82) | 44 (24-64) | 153 (104-202) | 32 (18-46) |
Data derived from mathematical modeling of time-kill curves [19]. Values represent means with 95% confidence intervals. MDK99: Minimum duration for killing 99% of the population.
SOS-Deficient Mutant Analysis
Table 2: Resistance Development in RecA-Deficient E. coli After Single Antibiotic Exposure
| Parameter | Wild Type E. coli | ΔrecA E. coli | Complemented ΔrecA |
|---|---|---|---|
| Baseline MIC (μg/mL ampicillin) | 5.0 | 5.0 | 5.0 |
| MIC After 8h Exposure (μg/mL) | 5.0 | 100.0 | 5.0 |
| Resistance Development Time | >3 weeks | 2 days | >3 weeks |
| Mutation Rate (per culture) | 1.2 × 10â»â¸ | 3.5 × 10â»â¸ | 1.3 × 10â»â¸ |
| ROS Accumulation | Baseline | 4.2-fold increase | Baseline |
| Resistance Stability | N/A | Stable after 7 days passage | N/A |
Data compiled from experimental evolution studies [5]. ROS: Reactive oxygen species.
Experimental Methodologies
Time-Kill Assay Protocol for Persister Quantification
Principle: This gold-standard method characterizes antibiotic killing kinetics and persister frequencies by monitoring bacterial viability over time under lethal antibiotic concentrations [19].
Procedure:
- Inoculum Preparation: Grow test strains to mid-log phase (OD₆₀₀ ≈ 0.5) in appropriate rich medium under standardized conditions.
- Antibiotic Exposure: Add antibiotic at 10× MIC concentration to 10ⶠCFU/mL bacterial suspension.
- High-Frequency Sampling: Collect samples every 15 minutes for the first 90 minutes, then at 2, 4, 6, 8, and 24 hours.
- Viability Assessment: Serially dilute samples in neutralization buffer, plate on antibiotic-free media, and enumerate CFUs after 24-48 hours incubation.
- Control Cultures: Include untreated growth controls and sterility controls.
Data Analysis:
- Plot logâ‚â‚€ CFU/mL versus time to visualize killing kinetics
- Apply mathematical modeling to determine parameters:
- Nâ‚€: Initial inoculum size
- Tâ‚€: Duration of bacteriostatic phase
- kâ‚/kâ‚‚: Kill rates for rapid/slow phases
- p: Proportion of persister cells
- Calculate MDK₉₉: Time required for 2-log (99%) reduction
Technical Considerations:
- Standardize growth phase and medium composition across experiments
- Include appropriate reference strains (e.g., E. coli ATCC 25922)
- Use fresh antibiotic solutions prepared according to CLSI guidelines
- Account for antibiotic carryover during plating [19]
SOS Response Activation Assay
Principle: Measure SOS induction using reporter constructs or transcriptional analysis of SOS regulon genes.
Procedure:
- Reporter Strains: Utilize recA-gfp or sulA-lacZ transcriptional fusions
- Antibiotic Exposure: Apply subinhibitory and bactericidal concentrations
- Monitoring: Measure fluorescence (GFP) or enzyme activity (β-galactosidase) over time
- Transcript Analysis: Quantify recA, lexA, umuC, umuD mRNA via RT-qPCR
Alternative Approach: Monitor RecA-GFP fusion protein localization to DNA damage foci [18].
Research Reagent Solutions
Table 3: Essential Research Tools for SOS and Persistence Studies
| Reagent/Category | Specific Examples | Function/Application | Experimental Considerations |
|---|---|---|---|
| Bacterial Strains | E. coli MG1655 (WT), JW2669-1 (ΔrecA), P. aeruginosa PAO1, S. aureus strain Evans | Isogenic pairs for genetic studies; clinical tolerant isolates | Verify genotype; monitor culture stability; use appropriate biosafety |
| Antibiotics | Ampicillin, Ciprofloxacin, Meropenem, Piperacillin-Tazobactam | SOS inducers; persistence challenges | Prepare fresh solutions; validate concentrations via MIC testing |
| Reporter Systems | recA-gfp, sulA-lacZ, lexA-venus | Real-time SOS activation monitoring | Optimize promoter strength; control for growth effects |
| DNA Damaging Agents | Mitomycin C, UV irradiation, Norfloxacin | Positive controls for SOS induction | Titrate for sublethal concentrations; include recovery periods |
| Mutation Detection | Rifampicin resistance assay, Whole genome sequencing | Quantify mutation frequencies; identify resistance mutations | Use multiple independent cultures; sufficient statistical power |
| ROS Detection | Hâ‚‚DCFDA, MitoSOX Red | Measure reactive oxygen species | Include oxidation controls; minimize dye exposure to light |
Therapeutic Implications and Future Directions
SOS-Targeted Anti-Persister Strategies
The mechanistic link between SOS response and persistence presents promising therapeutic targets:
RecA Inhibitors: Small molecules disrupting RecA nucleoprotein filament formation could suppress SOS-mediated persistence without increasing mutation rates [5].
TA System Modulators: Compounds targeting TisB-IstR or similar SOS-regulated toxin-antitoxin systems might prevent dormancy entry [18].
Combination Therapies: SOS inhibitors paired with conventional antibiotics show potential for eradicating persister populations in biofilms [17] [16].
Anti-Biofilm Agents: Disrupting SOS-mediated biofilm development could reduce persister niches and improve antibiotic penetration [17].
Experimental Workflow for SOS-Persistence Drug Screening
Figure 2: SOS-Targeted Drug Screening Workflow. Sequential approach for identifying compounds that inhibit SOS-mediated persistence while characterizing efficacy and resistance potential.
The SOS response represents a critical nexus in bacterial survival strategies, functionally linking DNA damage repair to antibiotic tolerance and persister cell formation. This mechanistic connection provides both explanatory power for clinical treatment failures and promising avenues for therapeutic intervention. As research methodologies advance, particularly in single-cell analysis and high-throughput screening, our understanding of SOS-mediated persistence continues to refine. Targeting this pathway offers substantial potential for mitigating chronic and biofilm-associated infections, representing a crucial frontier in overcoming antibiotic tolerance challenges. Future research should prioritize translational development of SOS inhibitors and their optimized integration into conventional antibiotic regimens to address the persistent threat of recalcitrant bacterial infections.
The global spread of antibiotic resistance represents one of the most significant challenges to modern public health. While vertical gene transfer propagates resistance within bacterial lineages, horizontal gene transfer (HGT) enables the dissemination of resistance genes across diverse bacterial species, dramatically accelerating this process. Among HGT mechanisms, conjugative plasmid transfer serves as a primary pathway for spreading antibiotic resistance genes among bacterial populations.
The SOS response is a conserved bacterial DNA damage repair system that has garnered significant attention for its potential role in accelerating resistance evolution. This inducible response regulates over 50 genes in Escherichia coli and is primarily controlled by the LexA repressor and RecA inducer proteins [3]. Under normal growth conditions, LexA dimers bind to specific operator sequences (SOS boxes), repressing transcription of SOS regulon genes. Upon DNA damage, single-stranded DNA (ssDNA) accumulates and binds RecA, forming nucleoprotein filaments that stimulate LexA self-cleavage, thereby derepressing the SOS regulon [3] [20].
This technical review examines the complex relationship between the SOS response and the dissemination of antibiotic resistance via conjugation, focusing on mechanistic insights, experimental approaches, and implications for therapeutic development within the broader context of antibiotic tolerance research.
The SOS Response: Molecular Mechanisms and Regulation
Core Regulatory Circuit
The SOS response employs a finely-tuned regulatory circuit centered on RecA and LexA:
- Induction: DNA damage leads to replication fork stalling and ssDNA accumulation
- RecA Activation: ssDNA binding facilitates RecA filament formation (RecA*)
- LexA Cleavage: RecA* stimulates self-cleavage of LexA repressor
- Derepression: LexA inactivation allows expression of SOS genes [3] [20]
Temporal Regulation of SOS Genes
The SOS response unfolds in temporally regulated phases:
- Early phase: Error-free repair mechanisms (e.g., nucleotide excision repair via UvrAB)
- Intermediate phase: Homologous recombination (RecA, RecN), cell division inhibition (SulA)
- Late phase: Error-prone translesion synthesis (Pol IV, Pol V) [3]
This temporal regulation ensures that mutagenic polymerases are only expressed when damage is extensive and persistent, balancing survival against mutagenic cost [3].
SOS Response in Conjugation and Resistance Dissemination
Conjugation-Induced SOS Activation
Conjugative DNA transfer represents a natural physiological trigger for SOS induction. During conjugation, plasmid DNA enters recipient cells as single-stranded DNA, which directly activates the RecA-LexA SOS pathway [21]. This connection creates a potential feedback loop where conjugation stimulates SOS response, which may in turn enhance genetic adaptability.
Evidence demonstrates that broad-host-range conjugative plasmids (R388, R6Kγ, RP4) induce SOS response in both E. coli and V. cholerae recipient cells [21]. However, some narrow-host-range plasmids encode anti-SOS factors (e.g., PsiB) that alleviate this induction, suggesting co-evolution between plasmids and bacterial hosts to modulate SOS activation [21].
SOS-Mediated Mutagenesis and Resistance Evolution
The SOS response contributes to antibiotic resistance through multiple mechanisms:
- Induced mutagenesis: Error-prone polymerases (Pol IV, Pol V) increase mutation rates, generating resistance mutations [22] [2]
- Hypermutation: SOS-induced mutator phenotypes can increase acquisition of resistance mutations by 100-1000 fold under antibiotic stress [2]
- Integron activation: SOS response upregulates integron integrase expression, promoting cassette rearrangements that can assemble resistance genes [21]
Recent work reveals that SOS-induced mutagenesis primarily occurs during recovery phases after antibiotic exposure, requiring active transcription, translation, and energy availability [23]. This timing is crucial for therapeutic strategies aimed at blocking resistance development.
SOS-Independent Resistance Pathways
Surprisingly, some resistance pathways operate independently of canonical SOS mechanisms. Research demonstrates that recA deletion mutants can still develop rapid β-lactam resistance through alternative pathways involving:
- ROS accumulation: Impaired antioxidant defenses in ΔrecA mutants
- Compromised DNA repair: Increased mutational supply
- Antibiotic selection: Selective enrichment of resistant variants [5]
This SOS-independent evolution highlights the complexity of resistance mechanisms and the challenges for therapeutic interventions.
Quantitative Analysis of SOS-Inducing Compounds
Antibiotic Effects on SOS Induction and Conjugation
Table 1: Comparative Effects of Antibiotics on SOS Response and Conjugation Frequencies
| Antibiotic | Class | SOS Induction (fold-change) | tra Gene Expression | Conjugation Frequency | Primary Mechanism |
|---|---|---|---|---|---|
| Cefotaxime | β-lactam | 5x [7] | Increased [7] | Significantly increased [7] | Cell wall damage, indirect DNA stress |
| Ciprofloxacin | Fluoroquinolone | 14-20x [7] | Unaffected [7] | No significant change [7] | Direct DNA damage via gyrase inhibition |
| Mitomycin C | DNA cross-linker | ~100x [7] | Increased [7] | Significantly increased [7] | Direct DNA cross-linking |
| Zidovudine | Nucleoside analog | Moderate [2] | Not tested | Not tested | DNA chain termination |
SOS Response Modulation Strategies
Table 2: Experimental Approaches for SOS Pathway Modulation
| Target | Intervention | Effect | Experimental Evidence |
|---|---|---|---|
| RecA | Zinc acetate | Inhibits SOS induction | Blocks ciprofloxacin-induced rifampin resistance in vivo [2] |
| LexA | 5-amino-1-(carbamoylmethyl)-1H-1,2,3-triazole-4-carboxamide | Inhibits self-cleavage | Reduces SOS-mediated mutagenesis [22] |
| RecA | Suramin-like compounds | Disassembles RecA-ssDNA filaments | Inhibits SOS response activation [22] |
| RecBCD | NSAC1003 (sulfanyltriazolobenzimidazole) | Binds RecB/RecD ATP sites | Alters DNA repair and recombination [22] |
| SSB | Small molecules | Disrupts SSB protein interfaces | Interferes with replication and recombination [22] |
Experimental Approaches and Methodologies
Assessing SOS Response Induction
Protocol: Reporter-Based SOS Quantification
Strain Construction:
- Utilize reporter strains with SOS-promoter fusions (e.g., PrecA-gfp, PsulA-lacZ)
- PrecA-gfp plasmid (pUA66-PrecA-gfp) enables fluorescence-based SOS monitoring [23]
Treatment Conditions:
- Expose bacterial cultures to subinhibitory antibiotic concentrations (½ MIC)
- Include positive controls (e.g., mitomycin C) and negative controls
- For UV induction: expose mid-exponential phase cells in thin films (Petri dishes) to UV light (2-32 minutes) [23]
Measurement:
- Monitor fluorescence (GFP) or β-galactosidase activity at regular intervals
- Correlate SOS induction with mutagenesis rates (e.g., rifampin resistance frequency) [23]
Conjugation Frequency Assay
Protocol: Plasmid Transfer Quantification
Strain Preparation:
- Grow donor (plasmid-carrying) and recipient (plasmid-free) strains separately to mid-exponential phase
- Use selective markers to distinguish strains (e.g., antibiotic resistance, chromosomal markers)
Mating Conditions:
- Mix donor and recipient cells at optimal ratios (typically 1:10 donor:recipient)
- Incubate for conjugation (1-4 hours, 37°C)
- Include test groups with SOS-inducing compounds and appropriate controls [7]
Selection and Enumeration:
- Plate on selective media that counterselects donors while selecting for transconjugants
- Calculate conjugation frequency as transconjugants per recipient cell [7]
Tra Gene Expression:
- Parallel samples for qPCR analysis of transfer genes (traF, traM) [7]
Mutagenesis Rate Determination
Protocol: Fluctuation Test for Mutation Rates
Culture Setup:
- Inoculate multiple (96+) independent cultures from small inocula
- Grow to saturation with/without SOS-inducing treatments [5]
Selection:
- Plate entire cultures on selective media (e.g., rifampicin 500 μg/mL)
- Plate appropriate dilutions on non-selective media for total counts [23]
Calculation:
- Use maximum likelihood estimation (MLE) or MSS maximum likelihood method
- Compare mutation rates between treatment groups and controls [5]
The Scientist's Toolkit: Essential Research Reagents
Table 3: Key Reagents for SOS and Conjugation Research
| Reagent/Category | Specific Examples | Function/Application | Key Features |
|---|---|---|---|
| Reporter Plasmids | pUA66-PrecA-gfp [23] | SOS response quantification | GFP under recA promoter control |
| sfiA::lacZ, recN::lacZ [21] | SOS response detection | β-galactosidase-based reporters | |
| SOS-Inducing Compounds | Mitomycin C [7] | Positive control for SOS | Strong DNA cross-linker |
| Ciprofloxacin [7] [2] | DNA damage-induced SOS | Gyrase inhibitor | |
| Cefotaxime [7] | Indirect SOS induction | β-lactam antibiotic | |
| SOS Inhibitors | Zinc acetate [2] | RecA inhibition | Blocks SOS induction in vivo |
| LexA cleavage inhibitors [22] | Prevent SOS derepression | Small molecule inhibitors | |
| Suramin analogs [22] | RecA-ssDNA disruption | Filament disassembly | |
| Genetic Tools | ΔrecA strains [7] [5] | SOS-deficient mutants | Eliminates SOS induction |
| LexA non-cleavable mutants [7] | Constitutive SOS repression | LexA S119A mutation | |
| SOS* hyper-induced mutants [7] | Constitutive SOS activation | LexA E74V, S119A, P176L, I188T | |
| Selection Markers | Rifampicin [2] [23] | Mutation frequency determination | Selects for rpoB mutations |
| Antibiotic combinations | Transconjugant selection | Counterselects donor strains | |
| LH1306 | LH1306: PD-1/PD-L1 Inhibitor for Cancer Immunotherapy | LH1306 is a small molecule immune checkpoint inhibitor targeting the PD-1/PD-L1 pathway. For Research Use Only. Not for human or veterinary diagnostic or therapeutic use. | Bench Chemicals |
| Liafensine | Liafensine, CAS:1198790-53-2, MF:C24H22N4, MW:366.5 g/mol | Chemical Reagent | Bench Chemicals |
Research Implications and Future Directions
The relationship between SOS response and conjugative resistance dissemination presents both challenges and opportunities for antimicrobial development. Several key implications emerge from current research:
Therapeutic Implications
- SOS Inhibition: Combining antibiotics with SOS inhibitors may reduce resistance development
- Timing Considerations: Interventions targeting recovery phases may effectively block mutagenesis [23]
- Ecological Impacts: Environmental stressors (heavy metals, biocides) can promote SOS-mediated resistance spread [24]
Research Gaps and Opportunities
While significant progress has been made, important questions remain:
- Plasmid-Specific Effects: How do different plasmid types modulate and respond to SOS induction?
- In Vivo Dynamics: How does SOS-mediated transfer operate in complex microbial communities and host environments?
- Alternative Pathways: What are the relative contributions of SOS-dependent and independent mechanisms in clinical settings?
Future research should prioritize translational applications, including validating SOS inhibition strategies in clinically relevant models and developing approaches that account for the complex interplay between bacterial stress responses and horizontal gene transfer in diverse environments.
Investigating SOS Dynamics: Tools and Models for Resistance Research
Reporter Systems for Real-Time SOS Response Monitoring
The bacterial SOS response is a critical DNA damage repair system that is increasingly recognized for its role in antimicrobial resistance (AMR) and tolerance. As the global AMR crisis intensifies—associated with 4.95 million global deaths annually—understanding and monitoring cellular stress responses like the SOS pathway has become paramount in antibiotic research and development [25]. Real-time reporter systems allow researchers to visualize and quantify the dynamics of this response in living cells, providing invaluable insights into the relationship between antibiotic-induced stress, bacterial survival mechanisms, and the evolution of resistance. This technical guide details the core principles, quantitative data, and experimental methodologies for implementing these powerful tools within a research framework focused on the SOS response and antibiotic tolerance.
The SOS Response: Core Pathway and Link to Antibiotic Tolerance
The SOS response is a conserved bacterial regulatory network activated by DNA damage. The core pathway consists of two key players: the LexA repressor protein and the RecA nucleoprotein filament.
- In the absence of DNA damage, LexA binds to operator regions (SOS boxes) in the promoter sequences of SOS genes, repressing their transcription.
- Upon DNA damage, single-stranded DNA (ssDNA) gaps accumulate. RecA monomers bind to this ssDNA, forming nucleoprotein filaments (RecA). This activated RecA facilitates the autocleavage of the LexA repressor.
- LexA cleavage de-represses the SOS regulon, allowing the transcription of over 40 genes involved in DNA repair, mutagenesis, and cell division arrest.
- Once DNA repair is complete, RecA* filaments disassemble, allowing intact LexA to reaccumulate and repress the SOS regulon once more.
The connection to antibiotic tolerance is multifaceted. Some bactericidal antibiotics, notably fluoroquinolones, induce DNA damage directly or indirectly. The resulting SOS response can elevate mutation rates through the induction of error-prone DNA polymerases (e.g., Pol IV, Pol V), thereby accelerating the evolution of heritable resistance [25]. Furthermore, the SOS response can contribute to a transient, non-heritable multidrug tolerance by promoting growth arrest and the formation of persister cells—dormant bacterial subpopulations that survive antibiotic treatment [25]. Consequently, inhibiting the SOS response has been proposed as a strategy to enhance the efficacy of existing antibiotics and curb resistance evolution. Research shows that transient inhibition of host RecA activity can increase the efficiency of CRISPR-Cas-based selection in genome editing, underscoring its functional importance [26].
The following diagram illustrates this core pathway and its implications.
Quantitative Data on Reporter System Performance
The performance of an SOS reporter system is critical for data reliability. Key parameters include dynamic range, sensitivity, and response time. The table below summarizes quantitative data for commonly used and engineered SOS promoter systems.
Table 1: Performance Characteristics of SOS Reporter Promoters
| Promoter | Key Regulated Gene | Reported Dynamic Range (Fold Induction) | Response Time (Post-induction) | Key Features and Applications |
|---|---|---|---|---|
| PsulA | sulA (Cell division inhibitor) | 50 - 100+ | 20 - 40 min | Strong, late gene; high output signal; ideal for high-sensitivity detection [26] |
| PrecA | recA (DNA repair protein) | 10 - 20 | 10 - 20 min | Early gene; fast response; useful for kinetic studies [26] |
| PuvrA | uvrA (Nucleotide excision repair) | 15 - 30 | 15 - 30 min | Reliable, intermediate response; general DNA damage reporting |
| PumuC | umuC (Error-prone polymerase) | 5 - 15 | 30 - 60 min | Late gene; linked directly to mutagenesis; studies on resistance evolution [26] |
The choice of reporter protein (e.g., GFP, RFP, Luciferase) also significantly impacts performance. The following table compares these options.
Table 2: Comparison of Reporter Proteins for Real-Time Monitoring
| Reporter Protein | Detection Modality | Relative Brightness | Maturation Half-Time | Advantages | Disadvantages |
|---|---|---|---|---|---|
| GFP | Fluorescence | High | ~10-40 min | Easy detection, widely used | Background from autofluorescence |
| RFP | Fluorescence | Medium | ~60 min | Reduced cellular autofluorescence | Slower maturation |
| Luciferase | Bioluminescence | Low | N/A | Extremely low background, high sensitivity | Requires substrate addition |
| Venus (YFP) | Fluorescence | Very High | ~2-5 min | Fast maturation for kinetics | Photobleaching potential |
Experimental Protocols for Key Applications
Protocol 1: Monitoring SOS Induction During Antibiotic Treatment
This protocol details how to use an SOS reporter construct to quantify the induction level in response to antibiotic stress.
Strain Preparation:
- Transform the E. coli strain of interest with a plasmid containing a fluorescent protein (e.g., GFP) under the control of a strong SOS-dependent promoter like PsulA.
- Prepare an overnight culture in a suitable medium with the necessary antibiotics for plasmid maintenance.
Antibiotic Exposure and Measurement:
- Dilute the overnight culture 1:100 in fresh, pre-warmed medium and grow to mid-exponential phase (OD600 ≈ 0.3-0.5).
- Split the culture into aliquots. Treat the experimental aliquot with the desired antibiotic (e.g., Ciprofloxacin at 2x MIC). Maintain an untreated control.
- Immediately transfer 150-200 µL of each culture into a 96-well microplate with a clear, flat bottom.
- Place the plate in a pre-warmed plate reader and initiate kinetic measurements. Monitor every 5-10 minutes for 3-6 hours.
- Measurements: OD600 (biomass) and Fluorescence (Ex/Em: ~488/510 nm for GFP).
Data Analysis:
- Normalize the fluorescence readings of each well to its corresponding OD600 to calculate Arbitrary Fluorescence Units (AFU).
- Plot normalized fluorescence (AFU) versus time.
- Calculate the Fold Induction as (Maximum AFU in treated sample) / (Average AFU in untreated control).
Protocol 2: Measuring SOS-Driven Mutation Rates and Enrichment
This method leverages reporters to quantify how the SOS response influences mutation rates, a key driver of resistance.
Genetic Tool Setup:
- Use a strain harboring both the SOS reporter (e.g., PumuC-GFP) and a mutation reporter, such as a counter-selectable plasmid or a chromosomal allele that confers resistance upon mutation (e.g., rifampicin resistance, RifR).
Selection and Screening:
- Subject the bacterial culture to sub-inhibitory concentrations of an antibiotic known to induce the SOS response (e.g., Ciprofloxacin at 0.5x MIC) for a defined period.
- Plate the cultures on agar plates containing rifampicin to select for mutants. Also, plate on non-selective agar to determine the total viable count.
- In parallel, analyze the culture by flow cytometry to determine the percentage of cells that exhibited a high SOS response (GFP-positive) during the antibiotic exposure.
Analysis:
- Calculate the mutation frequency as (Number of RifR colonies) / (Total viable count).
- Correlate the mutation frequency with the percentage of SOS-induced cells. Studies show that bioenergetic stress, which can be induced by antibiotics, potentiates resistance evolution via enhanced ROS production and mutagenic break repair, processes linked to the SOS response [25].
The workflow for these integrated protocols is summarized below.
The Scientist's Toolkit: Essential Research Reagents
Successful implementation of SOS reporter assays requires a suite of reliable reagents and genetic tools. The table below catalogs key solutions for building and deploying these systems.
Table 3: Essential Research Reagents for SOS Response Studies
| Reagent / Tool | Function / Description | Example Application / Rationale |
|---|---|---|
| PsulA-GFP Reporter Plasmid | High-sensitivity plasmid-based reporter for SOS induction. | Detecting subtle changes in SOS activation; ideal for flow cytometry and microscopy. |
| RecA Inhibitor (e.g., RecA56) | Dominant-negative mutant RecA protein that incorporates into and inhibits wild-type RecA filaments [26]. | Experimentally suppressing the SOS response to confirm its role in a phenotype (e.g., persistence). |
| Error-Prone Polymerase Mutants | Strains with deletions in umuC or dinB genes. |
Determining the contribution of SOS-induced mutagenesis to antibiotic resistance evolution. |
| Mitomycin C | A direct DNA cross-linking agent. | Positive control for strong, reliable induction of the SOS response. |
| Fluoroquinolone Antibiotics | Induce DNA double-strand breaks by inhibiting DNA gyrase and topoisomerase IV. | Physiological inducer of the SOS response in antimicrobial research [25]. |
| Bioenergetic Stress Inducers (pF1, pNOX) | Plasmids for constitutive ATP hydrolysis (pF1) or NADH oxidation (pNOX) to induce bioenergetic stress [25]. | Investigating the link between metabolic stress, SOS response, and antibiotic persistence/resistance. |
| Licogliflozin | Licogliflozin|SGLT1/SGLT2 Inhibitor|For Research | Licogliflozin is a potent dual SGLT1 and SGLT2 inhibitor for research of metabolic diseases. This product is For Research Use Only. Not for human or veterinary diagnostic or therapeutic use. |
| Lifirafenib | Lifirafenib, CAS:1446090-79-4, MF:C25H17F3N4O3, MW:478.4 g/mol | Chemical Reagent |
Advanced Research and Future Perspectives
Research continues to reveal the complex interplay between the SOS response and other cellular stress pathways. For instance, bioenergetic stress—a state of impaired cellular energy status—has been shown to potentiate both antibiotic resistance evolution and persistence. This stress increases ROS production, leading to oxidative DNA damage that can further stimulate the SOS response and stress-induced mutagenesis [25]. Furthermore, bioenergetic stress can enhance persister cell formation via the stringent response, creating another pathway to antibiotic tolerance that may interact with SOS-mediated dormancy [25].
Future developments in reporter systems will likely focus on multi-channel reporters that can simultaneously monitor the SOS response, metabolic activity (e.g., ATP levels), and redox state (ROS) in single cells. This will provide a systems-level view of bacterial physiology under antibiotic stress. Additionally, the integration of SOS reporters with CRISPR-Cas-based genome editing techniques is a powerful combination. As demonstrated, managing the SOS response through transient inhibition of RecA enhances the efficiency of CRISPR-Cas selection in recombineering, by preventing recA-mediated evasion of Cas9-induced lethality [26]. This synergy between reporters and genetic tools will accelerate both fundamental research and the development of anti-resistance strategies.
Genomic and Proteomic Approaches to Characterize SOS Mutagenesis
The bacterial SOS response is a conserved DNA damage repair system that plays a critically underappreciated role in the development of antimicrobial resistance. Initially characterized as a response to ultraviolet (UV) radiation, this complex regulatory network is now known to be activated by various classes of antibiotics, particularly those causing DNA damage or replication stress [27] [2]. The mutagenic phase of the SOS response is largely mediated by error-prone DNA polymerases, with DNA polymerase V (Pol V) being primarily responsible for the approximately 100-fold increase in DNA damage-induced chromosomal mutations [27]. This SOS-induced mutagenesis generates genetic diversity that can lead to antibiotic tolerance and resistance, presenting a significant challenge in clinical settings. Understanding the molecular mechanisms underlying SOS mutagenesis through genomic and proteomic approaches provides crucial insights for developing novel therapeutic strategies to combat antimicrobial resistance.
The core SOS response mechanism involves RecA nucleoprotein filaments (RecA*) forming on single-stranded DNA (ssDNA) generated at stalled replication forks. These active filaments facilitate autocleavage of the LexA repressor, derepressing approximately 40 genes involved in DNA repair and mutagenesis [27] [7]. During prolonged stress conditions, the error-prone polymerase Pol V (composed of UmuD'â‚‚C) is activated, enabling translesion DNA synthesis (TLS) that bypasses DNA damage at the cost of increased mutation rates [27]. This desperate survival strategy allows bacterial populations to evolve resistance to antibiotics, making the SOS response a potentially valuable target for adjuvant therapies aimed at curbing resistance development.
Molecular Mechanisms of SOS-Induced Mutagenesis
Core Regulatory Components
The SOS response is governed by a precise regulatory cascade that ensures appropriate cellular reactions to DNA damage:
RecA Nucleoprotein Filaments (RecA*): RecA binds to single-stranded DNA with ATP to form active nucleoprotein filaments that serve as the central activation signal for the SOS response. These filaments act as coproteases that stimulate LexA and UmuD autocleavage [27]. The RecA filament footprint covers one monomer per three nucleotides, extending bound DNA by 50% with six RecA monomers per helical turn [27].
LexA Repressor: In unstressed cells, LexA dimers bind to SOS boxes in promoter regions, repressing transcription of SOS genes. Following DNA damage, RecA* facilitates LexA autocleavage, derepressing the regulon [27] [7]. The SOS regulon includes over 40 genes in Escherichia coli involved in various DNA repair pathways [7].
DNA Polymerase V (Pol V): Composed of UmuD'â‚‚ and UmuC, Pol V is the primary enzyme responsible for SOS-induced mutagenesis. This error-prone polymerase catalyzes translesion DNA synthesis across various DNA lesions, often inserting incorrect nucleotides and generating mutations [27]. Pol V is strictly regulated to prevent genomic mutation overload and is only activated during the later phases of the SOS response.
Error-Prone Translesion Synthesis
SOS mutagenesis occurs primarily through Pol V-mediated translesion synthesis, which allows replication to proceed past DNA lesions that would otherwise stall replication forks. Unlike accurate DNA polymerases, Pol V can incorporate nucleotides opposite damaged templates but does so with significantly reduced fidelity [27]. The activation of Pol V requires both RecA-mediated cleavage of UmuD to UmuD' and subsequent interaction with RecA for catalytic stimulation [27]. This multistep activation process ensures that error-prone synthesis is only employed when accurate repair mechanisms are insufficient.
Recent studies have revealed that Pol V-mediated mutagenesis exhibits distinct sequence context preferences. Whole-genome sequencing approaches have demonstrated that SOS-induced mutations show strong strand bias and sequence specificity, with G:C to C:G transversions being particularly highly induced (up to 160-fold above wild-type levels) [28]. Approximately 60% of these transversions occur at the middle base of 5′GGC3′+5′GCC3′ sites, despite these sequences representing only 8% of G:C base pairs in the genome [28].
Figure 1: SOS Response Pathway Leading to Mutagenesis and Antibiotic Resistance. The cascade begins with DNA damage and progresses through RecA filament formation, leading to LexA cleavage and derepression of SOS genes, including error-prone DNA polymerases that ultimately generate mutations conferring antibiotic resistance.*
Genomic Methodologies for SOS Mutagenesis Characterization
Mutation Accumulation with Whole-Genome Sequencing
Mutation accumulation (MA) experiments coupled with whole-genome sequencing (WGS) provide a powerful approach for comprehensively characterizing SOS-induced mutagenesis without the selection biases inherent in phenotype-based assays. In this methodology, bacterial strains are passaged through repeated single-cell bottlenecks, allowing nearly neutral mutations to accumulate over time [28]. Subsequent whole-genome sequencing of evolved lineages enables identification of mutations across all genomic contexts, revealing the full spectrum and distribution of SOS-induced genetic changes.
Key Protocol Steps:
- Strain Construction: Generate SOS-constitutive strains (e.g., recA730 or ΔlexA) in a ΔsulA background to prevent lethal filamentation [28]
- Mutation Accumulation Lines: Establish multiple independent lines (typically 50-100) and subject them to repeated single-colony transfers
- DNA Extraction: Harvest genomic DNA from endpoints of each MA line
- Whole-Genome Sequencing: Sequence genomes using high-coverage Illumina or PacBio platforms
- Variant Calling: Identify mutations relative to ancestral reference genome
- Mutation Spectrum Analysis: Categorize mutations by type (transitions, transversions, indels) and sequence context
This approach has revealed that SOS-constitutive expression increases base-pair substitution rates approximately 30-fold, with transversions being particularly highly induced compared to transitions [28]. The mutation spectrum shows significant sequence context dependence, with G:C to C:G transversions exhibiting extreme sequence specificity.
Genomic Analysis of Antibiotic-Induced SOS Responses
Genomic approaches are also employed to study SOS activation following antibiotic exposure. RNA sequencing (RNA-seq) provides transcriptome-wide quantification of SOS gene induction, while targeted sequencing of mutation hotspots reveals specific mutational patterns induced by different antibiotic classes.
Experimental Workflow for Antibiotic-Induced Mutagenesis:
- Antibiotic Exposure: Expose bacterial cultures to subinhibitory concentrations of SOS-inducing antibiotics (e.g., ciprofloxacin, zidovudine)
- Variant Selection: Plate exposed cultures on antibiotic-containing media to select for resistant mutants
- Resistant Clone Sequencing: Sequence whole genomes or specific resistance loci (e.g., gyrA, gyrB, rpoB) from resistant colonies
- Mutation Pattern Analysis: Compare mutation spectra between antibiotic-treated and control populations
This approach has demonstrated that SOS-inducing antibiotics like ciprofloxacin and zidovudine increase resistance frequencies to multiple antibiotic classes, including rifampin, minocycline, and fosfomycin [2]. The mutation profiles differ from spontaneously arising mutations, displaying the characteristic transversion bias associated with Pol V activity.
Table 1: Mutation Rates Under SOS-Constitutive Conditions Revealed by MA/WGS
| Mutation Type | Fold Increase Over Wild-Type | Sequence Context Bias | Primary Polymerase Responsible |
|---|---|---|---|
| G:C → C:G Transversions | 160-fold | 60% at 5′GGC3′/5′GCC3′ sites | Pol V |
| G:C → T:A Transversions | 70-fold | Multiple hotspots | Pol V, Pol IV |
| A:T → T:A Transversions | 40-fold | Leading-strand template bias | Pol V |
| A:T → C:G Transversions | 30-fold | Lagging-strand template bias | Pol V |
| All Transversions | 60-fold (average) | Strand-biased | Pol V, Pol IV |
| Small Indels | 13-fold | - | Pol IV |
Analysis of Horizontal Gene Transfer
Genomic methodologies also facilitate investigation of SOS-mediated horizontal gene transfer, another mechanism contributing to antibiotic resistance dissemination. Whole-genome sequencing of transconjugants can identify mobilized resistance elements and their genomic integration sites [9]. Comparative genomics of pre- and post-transfer strains reveals the extent of genetic exchange facilitated by SOS induction.
Proteomic Approaches for SOS Response Characterization
Mass Spectrometry-Based Proteomics
Proteomic approaches provide crucial insights into SOS response dynamics by quantifying protein expression changes, post-translational modifications, and protein-protein interactions following DNA damage. Mass spectrometry (MS)-based proteomics has emerged as the primary technology for comprehensive protein characterization, enabling simultaneous monitoring of hundreds of SOS-related proteins.
Liquid Chromatography-Mass Spectrometry (LC-MS) Protocol for SOS Proteomics:
- Sample Preparation:
- Grow bacterial cultures with/without SOS-inducing agents (e.g., ciprofloxacin)
- Harvest cells at appropriate time points (e.g., exponential phase)
- Lyse cells and extract proteins
- Protein Digestion:
- Reduce and alkylate cysteine residues
- Digest proteins with trypsin
- Liquid Chromatography:
- Separate peptides using reverse-phase LC
- Mass Spectrometry Analysis:
- Analyze eluting peptides using high-resolution MS (e.g., Orbitrap instruments)
- Use data-dependent acquisition for untargeted discovery proteomics
- Data Processing:
- Identify proteins using database search algorithms (MaxQuant)
- Perform label-free quantification using software such as Perseus
This approach has revealed that RecA inactivation in clinical E. coli isolates under ciprofloxacin pressure leads to significant downregulation of proteins involved in DNA repair (DinG, DinI), nucleotide metabolism (GarL, PsuG, PsuK), and transport systems (CysP, UgpB) [29]. Simultaneously, stress response proteins (Hpf, IbpB) and translation factors (TufB, RpmH) show increased expression, indicating global metabolic rewiring when SOS function is compromised.
Single-Cell Proteomics
While technically challenging due to the small protein content of individual bacterial cells, emerging single-cell proteomics (SCP) approaches promise to reveal heterogeneity in SOS response activation within bacterial populations [30]. Techniques like Single-Cell ProtEomics by Mass Spectrometry (SCoPE-MS) and nanospray desorption electrospray ionization (nano-DESI) enable protein measurement from individual cells, potentially identifying subpopulations with differential SOS activation that may serve as reservoirs for resistance development.
Bacterial SCP Workflow Challenges:
- Low Protein Content: Single bacterial cells contain approximately 50-500 fg of protein, requiring extreme sensitivity
- Sample Preparation: Specialized microfluidic or nanopatterning systems needed for bacterial manipulation
- MS Sensitivity Requirements: High-efficiency ionization and advanced mass analyzers essential for detection
- Data Analysis: Specialized computational pipelines for low-input proteomic data
Despite these challenges, bacterial SCP represents the frontier for understanding how cell-to-cell variation in SOS protein expression influences population-level resistance development.
Table 2: Key Proteomic Changes in Clinical E. coli Isolates with Suppressed SOS Response Under Ciprofloxacin Treatment
| Protein Category | Representative Proteins | Expression Change (ΔrecA vs WT) | Functional Implications |
|---|---|---|---|
| DNA Repair | RecA, DinG, DinI, PriS | Decreased | Impaired DNA damage repair and mutagenesis |
| Nucleotide Metabolism | GarL, PsuG, PsuK | Decreased | Altered nucleotide precursor synthesis |
| Transport Systems | CysP, UgpB, YebG | Decreased | Reduced nutrient uptake |
| Stress Response | Hpf, IbpB | Increased | Protein aggregation protection |
| Translation | TufB, RpsQ, RpmH | Variable | Altered protein synthesis capacity |
Integrated Multi-Omics Experimental Design
Comprehensive characterization of SOS mutagenesis requires integration of genomic and proteomic approaches within unified experimental frameworks. The following section outlines a recommended workflow for simultaneous monitoring of mutational outcomes and protein expression dynamics during SOS induction.
Concurrent Genomic and Proteomic Profiling Protocol
Phase 1: Strain Selection and Preparation
- Select clinical isolates representing relevant resistance phenotypes and sequence types
- Generate isogenic ΔrecA mutants for SOS suppression controls
- Pre-culture strains in appropriate media to exponential growth phase
Phase 2: Antibiotic Exposure and Sampling
- Expose biological replicates to sub-MIC concentrations of SOS-inducing antibiotics (e.g., ½ MIC ciprofloxacin)
- Include untreated controls and RecA-deficient strains
- Collect samples at multiple time points (0, 15, 30, 60, 120 minutes) for:
- Genomic DNA extraction (whole-genome sequencing)
- RNA extraction (transcriptomic analysis)
- Protein extraction (proteomic analysis)
- Phenotypic assays (mutation frequency, survival rates)
Phase 3: Multi-Omics Data Generation
- Genomics: Whole-genome sequencing of pre- and post-exposure populations to identify mutations
- Transcriptomics: RNA sequencing to quantify SOS gene expression dynamics
- Proteomics: LC-MS/MS to measure protein abundance and modifications
Phase 4: Data Integration and Analysis
- Correlate mutation spectra with expression changes in DNA repair pathways
- Identify protein biomarkers predictive of mutator phenotypes
- Map temporal relationships between SOS induction and mutation accumulation
Figure 2: Integrated Multi-Omics Workflow for SOS Mutagenesis Characterization. The experimental design incorporates clinical isolates with isogenic controls, antibiotic exposure, multi-timepoint sampling, and concurrent genomic/proteomic analyses to comprehensively profile SOS-mediated adaptation.
The Scientist's Toolkit: Essential Research Reagents
Table 3: Essential Research Reagents for SOS Mutagenesis Studies
| Reagent/Category | Specific Examples | Function/Application | Key Characteristics |
|---|---|---|---|
| SOS-Inducing Agents | Ciprofloxacin, Mitomycin C, Zidovudine | Induce SOS response via DNA damage or replication stress | Subinhibitory concentrations (½ MIC) for mutation studies |
| SOS Reporter Systems | recA-gfp, sulA-gfp fusions | Visualize and quantify SOS activation at single-cell level | Enable monitoring of heterogeneity in SOS induction |
| Genetic Tools | ΔrecA mutants, lexA(Def) mutants, ΔumuDC mutants | Dissect specific SOS pathway components | Essential for establishing causal relationships |
| Antibiotic Resistance Selection | Rifampin, Minocycline, Fosfomycin | Measure mutation frequencies and resistance development | Different mechanisms reveal spectrum of mutational effects |
| Proteomic Standards | Stable isotope-labeled reference peptides | Quantify protein abundance changes in mass spectrometry | Enable precise quantification across samples |
| SOS Inhibitors | Zinc acetate | Suppress SOS response and reduce mutagenesis | Potential adjuvant therapeutic candidates |
| DNA Repair Assays | Antibody against UmuD', RecA, LexA | Monitor protein cleavage and activation states | Western blot analysis of SOS activation dynamics |
| Lifitegrast Sodium | Lifitegrast Sodium, CAS:1119276-80-0, MF:C29H23Cl2N2NaO7S, MW:637.5 g/mol | Chemical Reagent | Bench Chemicals |
| Lisavanbulin dihydrochloride | Lisavanbulin dihydrochloride, CAS:1387574-54-0, MF:C26H31Cl2N9O3, MW:588.5 g/mol | Chemical Reagent | Bench Chemicals |
Discussion and Research Implications
The integration of genomic and proteomic approaches has significantly advanced our understanding of SOS mutagenesis mechanisms and their contribution to antibiotic resistance development. Genomic methodologies, particularly mutation accumulation with whole-genome sequencing, have revealed the striking sequence context dependence of SOS-induced mutations and the profound increase in specific transversion types [28]. Meanwhile, proteomic approaches have illuminated the complex network of protein expression changes that facilitate mutagenic bypass and cellular adaptation under antibiotic pressure [29].
A critical insight from recent studies is the heterogeneity in SOS response activation among clinical isolates, which occurs despite remarkable sequence conservation in RecA and LexA regulators [31]. This phenotypic variation in SOS induction correlates with different propensities for resistance development, suggesting that strain-specific differences in SOS regulation significantly influence evolutionary trajectories under antibiotic selection. Proteomic analyses have further revealed that SOS suppression produces strain-dependent expression changes affecting diverse cellular processes beyond DNA repair, including nucleotide metabolism, transport systems, and stress response pathways [29].
Unexpectedly, recent research has also identified SOS-independent pathways to resistance, particularly in RecA-deficient backgrounds exposed to β-lactam antibiotics [5]. In these contexts, RecA deletion impairs DNA repair and represses antioxidative defense genes, leading to reactive oxygen species accumulation that promotes mutation and resistance development through alternative mechanisms. This finding highlights the complexity of bacterial adaptation and the importance of comprehensive omics approaches for capturing the full repertoire of resistance strategies.
From a therapeutic perspective, characterizing SOS mutagenesis through genomic and proteomic approaches identifies potential targets for adjuvant therapies aimed at curbing resistance development. Zinc acetate has emerged as a promising SOS inhibitor that reduces mutation frequencies in vitro and in vivo [2], while other strategies targeting RecA function or error-prone polymerase activity show potential for enhancing antibiotic efficacy. As antimicrobial resistance continues to pose grave threats to public health, understanding and intervening in SOS-mediated mutagenesis represents a crucial frontier in maintaining the effectiveness of existing antibiotics.
Adaptive Laboratory Evolution (ALE) Models for Studying Resistance Emergence
Adaptive Laboratory Evolution (ALE) has emerged as a powerful experimental framework for studying the fundamental processes driving the emergence of antibiotic resistance in bacteria. By simulating natural selection through controlled serial culturing, ALE promotes the accumulation of beneficial mutations, leading to the emergence of specific adaptive phenotypes. This approach bypasses the complexities inherent in rational genetic engineering while providing critical insights into evolutionary pathways [32]. Within this context, the relationship between ALE experiments and the bacterial SOS response—a conserved stress response to DNA damage—has become a focal point for understanding how antibiotic tolerance develops and stabilizes in bacterial populations. The SOS response, orchestrated primarily by the RecA and LexA proteins, represents a crucial mechanism that bacteria employ to manage DNA damage, but it also serves as a pathway for accelerating evolutionary adaptation under antibiotic pressure [2] [9].
The growing prevalence of multidrug-resistant pathogens has intensified the need to understand the genetic and physiological mechanisms underlying resistance development. ALE methodologies provide a controlled environment to observe these processes in real-time, allowing researchers to map genotype-phenotype relationships and identify causal mutations [33]. When framed within investigations of the SOS response, ALE becomes particularly valuable for deciphering how antibiotic-induced stress signals translate into genetic changes that confer survival advantages. This technical guide explores the core principles, methodologies, and applications of ALE models with specific emphasis on their utility for studying resistance emergence through SOS-related pathways, providing researchers with both theoretical foundations and practical protocols for implementing these approaches.
Theoretical Foundation: Linking ALE, SOS Response, and Resistance Development
Core Principles of Adaptive Laboratory Evolution
Adaptive Laboratory Evolution harnesses biology's innate capacity for self-optimization through natural selection under defined selective pressures. In practice, ALE involves subjecting microbial populations to controlled serial passages under specific environmental conditions—such as sublethal antibiotic concentrations—over numerous generations. This process enriches for spontaneous beneficial mutations that enhance fitness in the selective environment [33]. The major advantage of ALE over targeted genetic engineering approaches lies in its ability to identify unexpected adaptive solutions that might not be intuitively designed, often revealing novel genetic interactions and compensatory mutations that contribute to complex phenotypes like antibiotic resistance.
With the integration of whole-genome sequencing, automation, and bioinformatics, ALE has transformed into a powerful platform for connecting selectable phenotypes to underlying genotypes [33]. The typical ALE workflow encompasses four key components: (1) Robotics and Automation - enabling high-throughput experimentation with large population sizes and individually-addressable experiments; (2) Process Control Software - ensuring tight experimental control and reproducibility; (3) Suites of Modules - applying different selection pressures relevant to the research question; and (4) Bioinformatics - including mutation databases for rapid dissemination and interpretation of results, cloud-based mutation calling pipelines with quality control, and genome-scale models to predict and interpret evolution outcomes [33].
The SOS Response Pathway: Mechanism and Regulation
The SOS response represents a conserved bacterial stress response triggered primarily by DNA damage. This pathway activates when single-stranded DNA (ssDNA) accumulates in the bacterial cell, often as a result of antibiotic-induced DNA damage or replication fork stalling. The molecular mechanism begins with RecA protein coating ssDNA and forming nucleoprotein filaments that facilitate autocleavage of the LexA repressor protein [2]. LexA cleavage de-represses approximately 50 genes involved in DNA damage tolerance, including error-prone DNA polymerases (DNA pol II, IV, and V), DNA repair proteins, and cell division inhibitors [9].
This coordinated response presents a double-edged sword in the context of antibiotic resistance: while it promotes DNA repair and survival under stress, it also markedly increases mutation rates through the induction of error-prone polymerases—a phenomenon termed the "mutator phenotype" or "hypermutation" [2]. This enhanced genetic variability provides a larger pool of mutations from which antibiotic-resistant clones can emerge. The SOS response can be induced by various environmental factors and antibiotics, particularly fluoroquinolones like ciprofloxacin, but also by β-lactam antibiotics through less direct mechanisms involving impaired cell wall synthesis mediated by the DpiBA two-component signal system [34] [35].
Figure 1: SOS Response Pathway Induced by Antibiotic Stress. The pathway illustrates how antibiotic-induced DNA damage triggers the SOS response through RecA filament formation and LexA cleavage, leading to expression of error-prone DNA polymerases and ultimately contributing to resistance development.
Interplay Between ALE and SOS Response Studies
ALE experiments provide an ideal framework for investigating the SOS response's role in resistance development because they allow direct observation of evolutionary trajectories under controlled conditions. Researchers can design ALE studies that specifically probe SOS-mediated mutagenesis by using known SOS-inducing antibiotics (e.g., ciprofloxacin) or by employing bacterial strains with genetically modified SOS pathways (e.g., recA deletions) [34] [35]. The serial passage format of ALE enables researchers to monitor the timing and order of resistance mutations, potentially distinguishing between SOS-dependent and SOS-independent mechanisms.
The relationship between ALE and SOS response research is synergistic: ALE experiments reveal how SOS activation influences evolutionary outcomes, while understanding SOS mechanisms helps interpret mutational patterns observed in ALE studies. This intersection has proven particularly valuable for identifying factors that accelerate resistance development and for testing interventions that might suppress resistance emergence. For instance, studies have demonstrated that zinc can inhibit the SOS-induced emergence of antibiotic resistance in vivo, suggesting potential therapeutic approaches for constraining resistance evolution [2].
Experimental Design and Methodologies
Core ALE Experimental Framework
A well-designed ALE experiment requires careful consideration of multiple parameters to ensure meaningful results. The foundational ALE methodology involves serially transferring microbial cultures into fresh medium at defined intervals, maintaining consistent selective pressure throughout the experiment. The frequency of transfer is typically determined by the microbial growth rate, with passages occurring during mid- to late-exponential phase to maintain continuous growth under selection [36]. For Escherichia coli, a model organism in ALE studies, passage sizes significantly impact evolutionary outcomes, as they affect the efficiency of producing and fixing beneficial mutations [36].
The basic ALE protocol consists of several key steps: (1) Strain selection and preconditioning - selecting appropriate bacterial strains, sometimes with genetic modifications relevant to the SOS pathway; (2) Environment design - establishing growth conditions and selective pressures; (3) Serial passage - repeatedly transferring cultures to maintain exponential growth; (4) Monitoring - tracking population dynamics and phenotypic changes; (5) Sampling - preserving evolving populations at intervals for later analysis; and (6) Endpoint analysis - characterizing evolved populations through genotypic and phenotypic assessments [36] [33].
Figure 2: ALE Experimental Workflow. The diagram outlines the key steps in a standard ALE experiment, from initial strain selection through serial passage under selective pressure to final genomic and phenotypic analysis of evolved populations.
Specialized Methodologies for SOS Response Studies
Investigating the relationship between SOS response and resistance emergence requires specialized methodological approaches that go beyond standard ALE protocols. These include:
SOS-Inducing Conditions: Researchers can apply antibiotics known to trigger the SOS response at subinhibitory concentrations. Fluoroquinolones (e.g., ciprofloxacin) directly cause DNA breaks and are potent SOS inducers [2] [9]. β-lactam antibiotics (e.g., ampicillin) induce the SOS response through impaired cell wall synthesis mediated by the DpiBA two-component system [35]. Non-antibiotic SOS inducers like the antiretroviral drug zidovudine can also be employed to isolate DNA damage effects from antibiotic-specific killing mechanisms [2].
Genetic Manipulation of SOS Pathways: Isogenic bacterial strains with modifications in key SOS pathway genes allow researchers to test specific hypotheses about SOS involvement. Common approaches include:
- recA deletion mutants to eliminate SOS response capability
- lexA non-cleavable mutants to create constitutively repressed SOS pathways
- Fluorescent reporter strains where SOS-responsive promoters drive fluorescent protein expression for real-time monitoring of SOS induction [35]
In vivo ALE Models: While many ALE studies occur in vitro, animal models provide critical insights into SOS-mediated resistance evolution in physiologically relevant environments. The rabbit model of intestinal infection with enteropathogenic Escherichia coli has been successfully used to demonstrate that SOS-inducing drugs trigger the mutator phenotype response in vivo, resulting in increased antibiotic resistance frequencies [2].
Quantitative Measurements and Analytical Approaches
Robust quantification of evolutionary changes is essential for interpreting ALE experiments focused on resistance emergence. Key measurements include:
Minimum Inhibitory Concentration (MIC) Determinations: Standard broth microdilution or agar dilution methods to quantify changes in antibiotic susceptibility throughout evolution experiments [34] [35].
Mutation Frequency and Rate Calculations: Using fluctuation analysis to quantify the emergence of resistance mutations. This typically involves measuring the frequency of rifampin-resistant colonies in multiple independent cultures and applying mathematical models like the Luria-Delbrück test to distinguish between selective enrichment and induced mutagenesis [35].
Whole-Genome Sequencing: Identifying mutations that accumulate during ALE experiments through next-generation sequencing of evolved isolates compared to ancestral strains. This approach has revealed that drug resistance-associated mutations rapidly appear in resistant bacterial genomes, with specific mutations in genes like ampC, ftsI, and acrB associated with different resistance mechanisms [34] [35].
SOS Activation Assays: Quantifying SOS induction through reporter systems or molecular markers like RecA protein levels. Researchers can track the timing and magnitude of SOS activation relative to resistance emergence.
Key Experimental Findings and Data Synthesis
SOS-Dependent Resistance Emergence
Substantial evidence demonstrates that SOS response activation accelerates the development of antibiotic resistance through multiple mechanisms. Beaber et al. (2004) established that the SOS response promotes horizontal dissemination of antibiotic resistance genes through conjugative elements [9]. This work showed that SetR, a repressor encoded by the SXT integrating conjugative element, represses activators of SXT transfer, but SOS induction alleviates this repression. Consequently, antibiotics like ciprofloxacin that induce the SOS response simultaneously promote the spread of resistance genes through mobile genetic elements.
Further studies have quantified the impact of SOS-induced hypermutation on resistance frequencies. Research using a rabbit intestinal infection model demonstrated that exposure to SOS-inducing drugs like ciprofloxacin or zidovudine significantly increased the emergence of resistance to multiple antibiotics including rifampin, minocycline, and fosfomycin [2]. This effect was observed both in vitro and in vivo, with zinc supplementation shown to inhibit SOS-induced emergence of resistance, suggesting a potential therapeutic approach for suppressing resistance development.
Table 1: SOS-Dependent Resistance Emergence in E. coli
| Inducing Condition | Resistance Measured | Fold Increase | Experimental System | Key Mechanism |
|---|---|---|---|---|
| Ciprofloxacin (0.015 μg/mL) | Rifampin resistance | ~10-fold | In vitro, EPEC E22 | Hypermutation via error-prone polymerases |
| Zidovudine (0.6 μg/mL) | Minocycline resistance | ~100-fold | Rabbit intestinal loop | SOS-induced mutator phenotype |
| Ciprofloxacin (0.1× MIC) | SXT conjugative transfer | ~100-fold | In vitro, V. cholerae | Derepression of conjugation genes |
SOS-Independent Resistance Mechanisms
Surprisingly, recent research has revealed that resistance can emerge rapidly even in the absence of a functional SOS response. Studies with E. coli recA deletion mutants demonstrated a 20-fold increase in ampicillin MIC within just 8 hours after a single exposure to the antibiotic [34] [35]. This SOS-independent resistance development occurred through a different mechanism involving impaired DNA repair and downregulated base excision repair pathways, coupled with repression of antioxidative defense genes. The resulting accumulation of reactive oxygen species (ROS) promoted mutagenesis and resistance development, indicating that genetic instability can arise through multiple cellular pathways.
This SOS-independent resistance demonstrates distinct properties compared to SOS-dependent mechanisms. Once established, the resistance remains stable and can be passed to subsequent generations even in the absence of antibiotic pressure [35]. Complementation with functional recA restored the wild-type sensitivity phenotype, confirming the specific role of RecA deletion in enabling this rapid resistance evolution. The resistance spectrum differed as well, with recA mutants showing increased MICs not only to β-lactams but also to unrelated antibiotics like rifampicin, indicating a multidrug resistance phenotype [34].
Table 2: Comparative Analysis of SOS-Dependent vs. SOS-Independent Resistance
| Characteristic | SOS-Dependent Resistance | SOS-Independent Resistance |
|---|---|---|
| Key regulators | RecA, LexA, error-prone DNA polymerases | ROS accumulation, anti-oxidant pathway repression |
| Time scale | Develops over multiple generations | Rapid emergence (hours) |
| Mutation rate | Increased ~10-100 fold | Increased ~10-20 fold |
| Stability | May be unstable without continued selection | Remains stable after establishment |
| Genetic requirements | Functional RecA protein | RecA deletion or inhibition |
| Resistance spectrum | Often specific to inducing antibiotic | Frequently multidrug resistance |
ALEsim and Computational Approaches
The optimization of ALE experiments has been significantly advanced through computational tools like ALEsim, a simulator developed to model and optimize ALE experimental designs [36]. This computational approach has helped researchers identify suboptimal elements of traditional ALE protocols, particularly highlighting that passage sizes typically employed in serial passage batch culture ALE experiments lead to inefficient production and fixation of beneficial mutations. Through simulation-based optimization, ALE experiments can be designed to generate greater fitness gains in accelerated timeframes, pushing the limits of what adaptive laboratory evolution can achieve.
ALEsim has also facilitated the derivation of fundamental evolutionary parameters, such as the beneficial mutation rate for E. coli, estimated at 10â»â¶.â¹ to 10â»â¸.â´ mutations per cell division [36]. These quantitative insights help researchers design ALE experiments with appropriate population sizes and selection strengths to reliably capture evolutionary adaptation events. The integration of such computational tools with experimental ALE frameworks represents a powerful approach for systematically investigating complex phenomena like SOS-mediated resistance emergence.
Essential Research Tools and Reagents
Successful implementation of ALE experiments for studying resistance emergence requires specific research tools and reagents. The following table summarizes key resources mentioned in the literature:
Table 3: Research Reagent Solutions for ALE Studies on Resistance Emergence
| Reagent/Resource | Specifications | Application/Function | Example Sources |
|---|---|---|---|
| E. coli Strains | MG1655 (wild-type), JW2669-1 (ΔrecA), EPEC E22 | Model organisms for evolution experiments | CGSC, ATCC |
| SOS-Inducing Antibiotics | Ciprofloxacin, Ampicillin, Penicillin G, Carbenicillin | Selective pressure and SOS pathway activation | Commercial suppliers |
| Non-Antibiotic Inducers | Zidovudine (0.4-0.6 μg/mL) | SOS induction without direct antibacterial effects | Pharmaceutical sources |
| SOS Inhibitors | Zinc acetate (0.3 mM) | Suppression of SOS-induced hypermutation | Chemical suppliers |
| Selection Antibiotics | Rifampin, Minocycline, Fosfomycin | Measuring resistance emergence frequencies | Commercial suppliers |
| Growth Media | LB broth, M9 minimal medium | Culture maintenance and experimental evolution | Standard formulations |
| Automation Systems | Robotic liquid handlers, Bioreactors | High-throughput serial passaging | Various manufacturers |
| Sequencing Platforms | Illumina, Nanopore | Whole-genome sequencing of evolved isolates | Commercial services |
Adaptive Laboratory Evolution represents a powerful methodology for investigating the emergence of antibiotic resistance, particularly when focused on the role of the SOS response pathway. The experimental findings synthesized in this technical guide demonstrate that bacteria employ multiple genetic strategies to evolve resistance under antibiotic pressure, with both SOS-dependent and SOS-independent mechanisms contributing to this process. The relationship between these pathways is complex, with potential interactions and compensatory effects that warrant further investigation.
Future research directions in this field include developing more sophisticated ALE frameworks that integrate real-time monitoring of SOS activation during evolution experiments, potentially through fluorescent reporter systems. There is also a need to explore the potential therapeutic implications of these findings, such as whether SOS inhibitors like zinc could be deployed alongside antibiotics to suppress resistance emergence in clinical settings. Additionally, expanding ALE approaches to microbial communities rather than single species may provide insights into how SOS-mediated resistance emergence occurs in more ecologically relevant contexts.
As antibiotic resistance continues to pose grave threats to public health, ALE models offer valuable experimental systems for understanding—and potentially intervening in—the evolutionary processes that drive resistance development. The integration of these approaches with molecular analyses of SOS response activation provides a particularly promising path toward deciphering the complex relationship between antibiotic stress, genetic adaptation, and resistance emergence.
High-Throughput Screening for SOS Inhibitors and Therapeutic Adjuvants
The bacterial SOS response is a DNA damage repair network that is strongly implicated in both survival and acquired drug resistance under antimicrobial stress [12]. This widely conserved pathway is activated by many antibiotics and plays a central role in promoting bacterial survival and the evolution of resistance under antibiotic stress [12]. The SOS pathway consists of a set of genes under the control of the RecA and LexA proteins [12]. LexA is a dual-function repressor protease that blocks transcription of SOS genes in the absence of stress. When bacteria experience genotoxic stress, RecA polymerizes along exposed single-stranded DNA (ssDNA), forming activated nucleoprotein filaments (RecA*) that stimulate LexA to undergo autoproteolysis, leading to derepression of SOS effector genes [12]. The induced SOS effector genes facilitate adaptation to antibiotic stress through high-fidelity DNA damage repair initially, but under higher damage levels, error-prone processes emerge including translesion DNA polymerases that increase mutagenesis [12]. Given its role in adaptation and acquired resistance, the SOS response has emerged as an attractive therapeutic target that might potentiate our current antibiotic arsenal [12] [37].
Table 1: Key Molecular Targets in the SOS Response Pathway
| Target Protein | Function | Therapeutic Rationale | Validation Status |
|---|---|---|---|
| RecA | Master regulator, forms nucleoprotein filament | Central to SOS activation; inhibition blocks LexA cleavage | Genetic studies show recA deletion increases antibiotic sensitivity [12] |
| LexA | Repressor protease, controls SOS gene expression | Preventing self-cleavage maintains repression of SOS genes | Uncleavable LexA variants block SOS response and mutagenesis [22] |
| AddAB/RecBCD | DNA repair complexes, initiate homologous recombination | Inhibition blocks DNA repair and SOS activation | Genetic knockouts increase efficacy of DNA-damaging antibiotics [37] |
| Pol IV/Pol V | Error-prone DNA polymerases | Source of mutagenesis during SOS response | Inhibition reduces mutation rates and resistance emergence [22] |
Molecular Mechanisms of the SOS Response and Resistance Evolution
Core SOS Pathway Regulation
The SOS response is a finely-tuned regulatory network that activates when bacteria experience genotoxic stress from antibiotics such as fluoroquinolones [5] [37]. The pathway initiates with RecA protein binding to single-stranded DNA to form an activated nucleoprotein filament (RecA) [37]. This RecA filament then binds the LexA repressor protein, triggering LexA autocleavage and derepressing SOS box genes [37]. This leads to expression of error-prone DNA polymerases, additional LexA repressor protein, and DNA gyrase subunits [37]. The entire process represents a coordinated cellular defense mechanism that promotes survival at the cost of increased mutagenesis.
SOS-Independent Resistance Mechanisms
While the SOS pathway represents a major mechanism for resistance evolution, recent research has revealed alternative pathways for rapid resistance development. Surprisingly, Escherichia coli lacking RecA can still rapidly develop stable β-lactam resistance (20-fold MIC increase within 8 hours) after a single exposure to ampicillin [5]. This SOS-independent mechanism involves two distinct evolutionary forces: increased mutational supply and antibiotic-driven selection [5]. RecA deletion impairs DNA repair and downregulates base excision repair pathways while concurrently repressing transcription of antioxidative defense genes [5]. This dual impairment leads to excessive accumulation of reactive oxygen species (ROS), which promotes emergence of resistance-conferring mutations through increased genetic instability [5].
Diagram 1: SOS and SOS-Independent Resistance Pathways
High-Throughput Screening Approaches for SOS Inhibitors
The PubChem database, hosted by the National Center for Biotechnology Information (NCBI), represents the largest public chemical data source, containing over 60 million unique chemical structures and 1 million biological assays from more than 350 contributors [38]. This repository consists of three primary databases: Substance, Compound, and BioAssay, each serving distinct functions in HTS data management [38]. For researchers targeting SOS response inhibitors, PubChem provides standardized access to screening results through multiple interfaces, including manual web portal queries and automated programmatic access via the PubChem Power User Gateway (PUG) system [38].
HTS Data Retrieval Protocols
Manual Data Retrieval from PubChem:
- Access the PubChem Compound search tool at: https://pubchem.ncbi.nlm.nih.gov/search/search.cgi
- Select the appropriate search tab and enter identifier information (chemical name, SMILES, InChIKey, etc.)
- From the compound summary page, scroll to "BioAssay Results"
- Click "Refine/Analyze" and select "Go To Bioactivity Analysis Tool"
- Download the bioassay information as a plain text file [38]
Automated Data Retrieval for Large Datasets: For screening larger compound libraries (>1,000 compounds), automated querying through PubChem PUG-REST (Representational State Transfer) interface is recommended [38]. This system uses constructed URLs containing four parts: base, input, operation, and output. The input section specifies the target database and identifier information, while the operation designates the information to be retrieved (e.g., "assaysummary" for HTS data) [38]. This approach enables integration with programming languages including Java, Python, Perl, and C# for high-throughput data retrieval.
Master HTS Database Download: For comprehensive analysis requiring the complete PubChem database, File Transfer Protocol (FTP) access is available to download all three databases in multiple formats including Abstract Syntax Notation (ASN), CSV, JavaScript Object Notation (JSON), and Extensible Markup Language (XML) [38].
Table 2: HTS Data Sources for SOS Inhibitor Discovery
| Resource | Data Type | Content Relevance | Access Method |
|---|---|---|---|
| PubChem BioAssay | Screening results | SOS inhibition assays, RecA/LexA targeted screens | Web portal, PUG-REST, FTP [38] |
| ChEMBL | Bioactive molecules | Curated SAR data for known SOS inhibitors | Web services, database downloads |
| BindingDB | Binding affinities | Protein-ligand interaction data for RecA/LexA | Web interface, data exports |
| Comparative Toxicogenomics Database (CTD) | Chemical-gene interactions | SOS pathway gene expression modulation | Custom queries, batch downloads |
Experimental Validation of SOS Inhibitors
Structural-Activity Relationship Studies
Comprehensive structure-activity relationship (SAR) studies have been conducted on known SOS inhibitor scaffolds to identify key pharmacophoric groups. Investigation of the IMP-1700 scaffold, a known inhibitor of the mutagenic SOS response, has revealed critical structural requirements for activity [37]. Systematic variation of the phenyl ring, thiourea linker, quinolone substructure, carboxylic acid, and N-alkyl substituent has led to the development of OXF-077, the most potent analogue reported to date in this series [37]. This compound demonstrates significant suppression of ciprofloxacin resistance emergence in Staphylococcus aureus, validating the SOS inhibition strategy for combating antimicrobial resistance [37].
Target Validation and Resistance Studies
Genetic studies provide compelling evidence for RecA and LexA as therapeutic targets. E. coli strains with mutations in recA or lexA genes spanning the full spectrum of SOS activity levels have been systematically analyzed to measure bacterial susceptibility and induced mutation rates across different antibiotic classes [12]. Significant changes in minimum inhibitory concentrations (MICs) are largely confined to DNA-damaging antibiotics, with strains containing constitutively repressed SOS response impacted to a greater extent than hyperactivated strains [12]. Additionally, antibiotic-induced mutation rates are suppressed when SOS activity is reduced across a wider spectrum of antibiotics [12].
Diagram 2: HTS Workflow for SOS Inhibitor Discovery
Research Reagent Solutions for SOS Inhibition Studies
Table 3: Essential Research Tools for SOS Inhibitor Development
| Reagent/Category | Specifications | Research Application | Example Use |
|---|---|---|---|
| SOS Reporter Strains | E. coli or S. aureus with SOS-promoter fusions to fluorescent proteins | Primary HTS for SOS inhibitory activity | Quantifying LexA derepression inhibition [12] |
| RecA/LexA Mutant Panels | Isogenic strains with varying SOS activity (hypoactive to hyperactive) | Target validation and mechanism studies | Systematic analysis of antibiotic susceptibility [12] |
| Biochemical Assay Kits | Purified RecA, LexA, AddAB/RecBCD proteins | In vitro inhibition profiling | Direct target engagement assessment [37] |
| Antibiotic Panels | DNA-damaging (e.g., ciprofloxacin) and non-DNA-damaging agents | Synergy studies with SOS inhibitors | Determining adjuvant potential [12] [37] |
| HTS-Compatible Assays | β-galactosidase, luciferase, or fluorescence-based SOS reporters | Large-scale compound screening | Primary identification of SOS inhibitor hits [38] |
| Resistance Evolution Systems | Serial passage or chemostat-based selection | Measuring resistance suppression | Evaluating SOS inhibitors on resistance development [37] |
Protocols for Key SOS Inhibition Experiments
SOS Response Inhibition Assay Protocol
Objective: Quantify inhibition of SOS response activation using reporter strains.
- Culture SOS reporter strains (e.g., E. coli with sulA-gfp fusion) to mid-log phase in appropriate medium.
- Distribute cultures into 96-well or 384-well microplates containing test compounds.
- Induce SOS response with sub-inhibitory concentrations of ciprofloxacin (0.1-0.5 × MIC).
- Incubate with shaking at 37°C for 3-4 hours.
- Measure fluorescence (excitation 485 nm, emission 535 nm) using plate reader.
- Calculate percentage inhibition relative to untreated controls and no-antibiotic baseline.
- Confirm cytotoxicity through parallel viability assessment (OD600 or resazurin reduction) [12] [37].
Resistance Emergence Suppression Protocol
Objective: Evaluate SOS inhibitors' ability to suppress antibiotic resistance development.
- Prepare wild-type and SOS-deficient strains in cation-adjusted Mueller-Hinton broth.
- Expose to single concentration of β-lactam antibiotic (e.g., ampicillin at 10 × MIC) for 8 hours.
- Plate serial dilutions on antibiotic-free medium to determine survival rates.
- Islete individual colonies and determine MIC values for parent antibiotics.
- Assess stability of resistance by serial passage in antibiotic-free medium for 7 days.
- Compare resistance emergence frequencies between treatment conditions [5].
Synergy Testing with DNA-Damaging Antibiotics
Objective: Quantify adjuvant potential of SOS inhibitors with conventional antibiotics.
- Perform checkerboard microdilution assays with SOS inhibitors and DNA-damaging antibiotics.
- Prepare serial dilutions of both compounds in 96-well plates.
- Inoculate with standardized bacterial suspension (5 × 10^5 CFU/mL).
- Incubate at 37°C for 18-24 hours.
- Determine fractional inhibitory concentration (FIC) index using the formula: FIC index = (MIC of drug A in combination/MIC of drug A alone) + (MIC of drug B in combination/MIC of drug B alone).
- Interpret results: FIC index ≤0.5 indicates synergy; >0.5-4 indicates indifference; >4 indicates antagonism [12] [37].
The strategic inhibition of the bacterial SOS response represents a promising adjuvant approach to combat the escalating crisis of antimicrobial resistance. High-throughput screening methodologies, coupled with comprehensive SAR studies, have yielded potent inhibitors such as OXF-077 that demonstrate significant suppression of resistance evolution [37]. The integration of public data resources like PubChem with robust experimental validation protocols provides a solid foundation for advancing SOS-targeted therapeutic strategies. As the silent pandemic of AMR continues to surge globally - with one in six bacterial infections now resistant to standard antibiotics according to recent WHO surveillance - innovative approaches that preserve the efficacy of existing antibiotics through resistance suppression become increasingly vital [39]. Future directions will likely involve combining SOS inhibitors with conventional antibiotics in clinical settings, developing narrow-spectrum agents that minimize microbiome disruption, and leveraging artificial intelligence for accelerated discovery of next-generation therapeutics targeting bacterial adaptive mechanisms [40].
Analyzing Mutation Spectra and Frequencies in SOS-Active Populations
The bacterial SOS response is a conserved DNA damage repair system that plays a critically important role in antibiotic tolerance and the evolution of resistance. This inducible stress response is activated when antibiotics cause DNA damage directly or indirectly through the production of reactive oxygen species (ROS) [14]. The paradigm has been that the SOS response, with RecA as its master regulator, serves as a key facilitator of resistance evolution, particularly for DNA-damaging antibiotics like fluoroquinolones [5]. However, emerging research reveals more complex relationships, demonstrating that resistance can evolve rapidly through SOS-independent mechanisms and that mutation spectra analysis provides powerful insights for predicting resistance trajectories [13] [41]. This technical guide examines contemporary methodologies for analyzing mutation spectra within the context of SOS response research, providing experimental frameworks and analytical tools to advance antibiotic resistance investigations.
The significance of this research area extends to clinical applications, as mutational signature analysis of patient samples is emerging as a promising diagnostic tool that may predict multidrug resistance and guide precision-based medical care [41]. Furthermore, understanding these pathways opens potential therapeutic avenues, as demonstrated by the development of small molecules that suppress the evolution of antibiotic resistance in bacteria through SOS response inhibition [42].
Core Mechanisms: SOS and Alternative Pathways to Resistance
The Canonical SOS Response Pathway
The canonical SOS response pathway represents a tightly regulated DNA repair system in Gram-negative bacteria. When DNA damage occurs, single-stranded DNA (ssDNA) regions accumulate and trigger the activation of RecA nucleofilaments. The activated RecA facilitates the self-cleavage of the LexA repressor, derepressing approximately 50 genes involved in DNA repair, mutagenesis, and cell division control [14]. This network enables bacteria to survive antibiotic-induced DNA damage but simultaneously increases genetic instability that can accelerate resistance development.
The critical components of this pathway include:
- RecA: Master regulator and recombinase that initiates SOS response
- LexA: Transcriptional repressor that undergoes self-cleavage during SOS induction
- DNA damage: Primarily double-strand breaks caused directly or indirectly by antibiotics
- SOS-regulated genes: Diverse network including error-prone polymerases, recombination, and repair functions
SOS-Independent Resistance Mechanisms
Recent research has revealed surprising SOS-independent pathways to resistance, particularly in RecA-deficient strains. Contrary to conventional wisdom, E. coli lacking RecA can develop stable, high-level β-lactam resistance (20-fold MIC increase within 8 hours) after a single antibiotic exposure [13] [5]. This pathway operates through a "repair-redox axis" wherein RecA deletion impairs both DNA repair and antioxidative defense mechanisms.
The key mechanistic components include:
- Impaired DNA repair: Base excision repair pathways are downregulated in ΔrecA strains
- Antioxidant repression: Transcription of antioxidative defence genes is repressed
- ROS accumulation: Elevated reactive oxygen species promote mutagenesis
- Selection enrichment: Antibiotic pressure selectively enriches rare resistant mutants
This repair-redox axis creates a hypermutable population that serves as a substrate for rapid resistance evolution under antibiotic selection, demonstrating that genetic instability can arise through alternative pathways when the canonical SOS response is compromised [13].
Figure 1: Comparative pathways of canonical SOS-dependent and SOS-independent evolution of antibiotic resistance.
Methodological Approaches for Mutation Spectrum Analysis
Experimental Evolution and Resistance Profiling
Adaptive Laboratory Evolution (ALE) provides a powerful approach for studying mutation spectra under controlled antibiotic selection pressure. The following protocol outlines a standardized method for tracking resistance evolution:
Bacterial Strains and Culture Conditions
- Utilize isogenic wild-type and SOS pathway mutant strains (e.g., ΔrecA, ΔlexA)
- Include complementation strains with plasmid-borne recA to verify specificity
- Maintain strains in appropriate medium with necessary selective antibiotics
Evolution Experiment Protocol
- Inoculate biological replicates (minimum n=3) in fresh medium
- Expose to sub-MIC and supra-MIC antibiotic concentrations in parallel
- For β-lactams: Use 10× MIC (e.g., 50 µg/mL ampicillin for E. coli)
- Treatment duration: 4.5-8 hours per cycle for acute exposure studies
- Daily passage protocol:
- Transfer surviving populations to fresh medium with antibiotic
- Preserve aliquots at each passage for retrospective analysis
- Continue for predetermined cycles (typically 10-21 days) or until resistance emerges
- Monitor population dynamics:
- Measure optical density to track growth kinetics
- Determine MIC at regular intervals using microbroth dilution
- Assess survival rates through colony-forming unit (CFU) counts
Resistance Stability Assessment
- Passage resistant isolates in antibiotic-free medium for 7+ days
- Monitor MIC retention to distinguish stable genetic changes from transient adaptations
- Evaluate cross-resistance to other drug classes to identify multidrug resistance
This ALE approach successfully demonstrated that ΔrecA E. coli develops stable, high-level β-lactam resistance within hours compared to days in wild-type strains [5].
Mutational Signature Analysis Framework
Comprehensive mutation spectrum analysis requires specialized bioinformatic workflows. The nSPECTRa pipeline provides a reusable framework for characterizing mutation spectra across populations and species [43].
Core Analytical Workflow:
Figure 2: Bioinformatic workflow for mutation spectrum analysis.
Key Normalization Considerations:
- Account for ancestral k-mer frequencies in reference genomes
- Apply median of ratios normalization to control for total mutation burden differences
- Correct for sequencing depth and coverage variation
- Adjust for population structure and phylogenetic relationships
Advanced Analytical Features:
- Trinucleotide context analysis (96 possible mutation types)
- Detection of multi-nucleotide polymorphisms (MNPs) and sequential dinucleotide mutations (SDMs)
- Cosine similarity analysis to compare with reference mutational signatures
- Machine learning classification (e.g., gradient boosting with SHAP interpretation)
This framework enabled the identification of a distinct MMR-deficient mutational signature in Pseudomonas aeruginosa characterized by enriched C>T and T>C transitions, particularly in NCC, NCG, CTN, and GTN contexts [41].
Quantitative Data on Mutation Spectra and Resistance
Mutation Rates and Resistance Evolution Kinetics
Table 1: Comparative analysis of mutation rates and resistance evolution across genetic backgrounds
| Strain/Background | Baseline Mutation Rate | Post-Antibiotic Mutation Rate | Time to Resistance | Resistance Stability |
|---|---|---|---|---|
| E. coli WT | 1.0× (reference) | 1.2-2.0× | 14-21 days | Stable |
| E. coli ΔrecA | 2.5-4.0× | 5.0-8.0× (high variance) | 2 days (β-lactams) | Stable across 7+ days |
| P. aeruginosa WT | 1.0× (reference) | 1.5-3.0× | 10+ passages | Variable |
| P. aeruginosa ΔmutS | 300× (hypermutator) | 300-500× | 2-4 passages | Stable |
Data compiled from [13] [5] [41]
Characteristic Mutational Signatures
Table 2: Mutation signatures associated with DNA repair deficiencies across species
| Repair Defect | Enriched Mutations | Trinucleotide Context Preferences | Species Conservation |
|---|---|---|---|
| MMR deficiency | C>T and T>C transitions | NCC, NCG (C>T); CTN, GTN (T>C) | Conserved across domains |
| SOS induction | C>T, C>A, T>C | Varied, context-dependent | Species-specific |
| recA deletion | C>A, T>A, insertions | No strong context preference | Limited data |
| Base excision repair impairment | Oxidative damage signatures | GCA, GCC (8-oxoG contexts) | Conserved in bacteria |
Data compiled from [13] [43] [41]
The data reveal that MMR-deficient bacteria display a highly conserved mutational signature dominated by C>T and T>C transitions, with specific trinucleotide context preferences that distinguish them from other repair deficiencies. This signature shows cosine similarity of 0.65-0.80 with MMR-deficient human tumors, indicating deep evolutionary conservation of mutational processes [41].
Research Toolkit: Essential Reagents and Methodologies
Key Research Reagent Solutions
Table 3: Essential research reagents for SOS and mutation spectrum studies
| Reagent/Method | Specific Example | Research Application | Technical Notes |
|---|---|---|---|
| SOS inhibitors | OXF-077 small molecule | Suppresses SOS response; reduces resistance evolution | Most potent SOS inhibitor reported; restores sensitivity in resistant strains |
| MMR-deficient strains | P. aeruginosa mutS::Tn, mutL::Tn | Hypermutation and MDR acquisition studies | 300-fold increase in mutation rate; rapid resistance development |
| recA-deficient strains | E. coli ΔrecA (JW2669-1 from CGSC) | SOS-independent pathway analysis | Verified knockout; used in complementation studies |
| Adaptive evolution platforms | Cyclic ALE with antibiotic pressure | Modeling resistance evolution in lab | Treatment cycles: 4.5-8h antibiotic exposure followed by outgrowth |
| Mutational signature analysis | nSPECTRa workflow (Nextflow) | Comparative mutation spectra analysis | Handles ancestral allele inference, SNV/SDM spectra, normalization |
| Variant calling pipelines | Custom WGS analysis with recurrent mutation detection | Identifies de novo mutations in evolved clones | Requires high-quality sequencing; sensitive to coverage depth |
| L-Moses | L-Moses|PCAF/GCN5 Bromodomain Inhibitor|Research Use Only | Bench Chemicals | |
| LMT-28 | LMT-28, MF:C17H29NO4, MW:311.4 g/mol | Chemical Reagent | Bench Chemicals |
Data compiled from [13] [5] [42]
Discussion and Research Implications
The integration of mutation spectrum analysis with SOS response research provides powerful insights into the evolutionary trajectories of antibiotic resistance. The emerging paradigm recognizes that while the SOS response represents a crucial pathway for stress-induced mutagenesis, alternative mechanisms like the repair-redox axis in RecA-deficient backgrounds can facilitate equally rapid resistance evolution [13] [5]. This has profound implications for therapeutic strategies aimed at suppressing resistance evolution.
From a technical perspective, standardized workflows like nSPECTRa that account for trinucleotide context and recurrent mutations enable robust comparison of mutational signatures across studies and species [43]. The conserved nature of MMR-deficient signatures between bacteria and humans suggests fundamental evolutionary conservation in mutational processes that transcend biological domains [41].
For the drug development community, these findings highlight two complementary strategies: first, SOS inhibitors like OXF-077 represent promising adjuvants for preventing resistance evolution during antibiotic therapy [42]; second, mutational signature analysis of clinical isolates could enable predictive diagnostics for identifying strains prone to multidrug resistance development [41]. As sequencing costs continue to decline, the integration of mutation spectrum analysis into clinical microbiology workflows offers exciting possibilities for personalized antibiotic therapy tailored to the evolutionary potential of infecting pathogens.
Future research directions should focus on expanding mutational signature databases across diverse bacterial pathogens, developing point-of-care tools for signature analysis, and optimizing combination therapies that simultaneously target bacterial viability and suppress resistance evolution.
Challenges in SOS Response Inhibition and Paradoxical Resistance
The SOS response, orchestrated by the RecA/LexA regulatory axis, has long been considered a cornerstone of bacterial antibiotic resistance evolution. This inducible DNA repair system activates in response to antibiotic-induced DNA damage, facilitating survival and mutagenesis that can lead to stable resistance. However, emerging research reveals that bacteria can rapidly evolve multi-drug resistance through sophisticated SOS-independent pathways. This mechanistic divergence challenges the primacy of the canonical SOS response and reveals a complex network of alternative adaptation strategies. Understanding these parallel evolutionary routes is critical for developing next-generation antimicrobial strategies that anticipate and counter bacterial adaptation in all its forms.
This technical review examines the molecular machinery, experimental evidence, and therapeutic implications of SOS-independent antibiotic resistance. We synthesize findings from recent studies that delineate how bacteria leverage oxidative stress management, gene amplification events, and constitutive stress response pathways to achieve resistance without SOS activation. For researchers and drug development professionals, these insights reveal new vulnerabilities that could be targeted to suppress resistance evolution more comprehensively.
Fundamental Mechanisms of SOS-Independent Resistance
The Repair-Redox Axis: Mutational Supply Through Oxidative Stress
A paradigm-shifting study demonstrated that Escherichia coli lacking RecA can develop stable, multi-drug resistance 20-fold above baseline MIC following a single 8-hour exposure to ampicillin [13] [5]. This accelerated resistance evolution occurs through a two-step mechanism that bypasses canonical SOS signaling entirely.
Step 1: Dual Impairment Creates a Hypermutable State
- DNA Repair Deficiency: RecA deletion intrinsically compromises homologous recombination repair, downregulating base excision repair pathways and creating a DNA repair deficit [13].
- Antioxidant Suppression: Simultaneously, RecA deficiency represses transcription of antioxidative defense genes, leading to excessive accumulation of reactive oxygen species (ROS) [5].
- Synergistic Effect: This dual impairment establishes a hypermutable cellular environment where elevated ROS causes increased DNA damage while repair capacity is diminished [13].
Step 2: Selective Enrichment of Resistant Variants
- Ampicillin treatment does not alter survival rates between wild-type and ΔrecA strains but selectively enriches for rare pre-existing mutants in the RecA-deficient, ROS-elevated background [5].
- Resistant clones emerge from this population through selection rather than antibiotic-induced mutagenesis, with resistance remaining stable after antibiotic removal [13] [5].
Table 1: Key Experimental Findings Supporting the Repair-Redox Axis
| Experimental Observation | Quantitative Result | Significance | Citation |
|---|---|---|---|
| Resistance development time | Reduced from 3 weeks to 2 days in ΔrecA vs. wild-type | Demonstrates accelerated evolution | [5] |
| MIC increase after single exposure | 20-fold increase within 8 hours | Shows rapid resistance development | [13] [5] |
| Mutation rate in ΔrecA with ampicillin | Significant increase in estimated mutation rate | Confirms increased mutational supply | [5] |
| Resistance stability | Maintained for 7 days without antibiotic | Indicates stable genetic resistance | [5] |
| Complementation effect | Restored wild-type sensitivity in complemented strain | Validates RecA-specific mechanism | [5] |
Gene Amplification: Dynamic Copy Number Variation
Gene amplification represents a powerful SOS-independent pathway to antibiotic resistance through reversible increases in gene copy number. This mechanism generates rapid, dose-dependent resistance through tandem duplication of genomic regions containing resistance determinants [44].
Formation and Dynamics:
- Amplification occurs through an initial duplication event followed by RecA-dependent or RecA-independent expansion, with frequencies at individual loci ranging from ~10â»Â² to ~10â»â¶ in unselected cultures [44].
- In S. Typhimurium, gene duplications occur at some genomic location in approximately 10% of unselected cells, making this a highly accessible adaptation route [44].
Resistance Mechanisms via Amplification:
- Efflux Pump Overexpression: CC398 lineage Staphylococcus aureus evolves fluoroquinolone resistance through amplification of the norA efflux pump gene, with copy numbers increasing 3-24-fold [44].
- Target Bypass: Amplifications can provide alternative, low-affinity targets that bypass antibiotic action [44].
- Enzyme Overproduction: Increased copy number of antibiotic-modifying enzymes directly neutralizes antibiotic activity [44].
Clinical Relevance:
- Amplification-mediated resistance exhibits heteroresistance, where only a subpopulation displays resistance, complicating diagnostics and treatment [44].
- This resistance is typically unstable without selective pressure, creating dynamic, reversible adaptation that evades conventional detection methods [44].
Alternative Stress Response Pathways
Beyond the repair-redox axis and gene amplification, bacteria employ additional SOS-independent stress responses that contribute to antibiotic resistance:
- Envelope Stress Responses: Activated by antibiotics damaging the cell envelope, these responses upregulate repair mechanisms and efflux pumps in Gram-negative bacteria [14].
- Oxidative Stress Response: Induced by ROS-generating antibiotics, this system enhances bacterial survival through detoxification enzymes [14].
- Heat Shock Response: Triggered by antibiotics causing protein misfolding, this pathway refolds or degrades damaged proteins [14].
Experimental Approaches and Methodologies
RecA Deficiency and Resistance Evolution Protocols
Bacterial Strains and Culture Conditions:
- Strains: E. coli MG1655 (wild-type) and isogenic ΔrecA mutant; validation with JW2669-1 ΔrecA strain from Coli Genetic Stock Centre [5].
- Growth Conditions: Standard lysogeny broth (LB) medium, 37°C with shaking [5].
- Antibiotic Exposure: Single exposure to 50 μg/mL ampicillin (10× MIC) for 8 hours; additional testing with penicillin G (1 mg/mL) and carbenicillin (200 μg/mL) [5].
Resistance Assessment Methodology:
- MIC Determination: Broth microdilution following CLSI guidelines pre- and post-exposure [5].
- Stability Testing: Daily passage in antibiotic-free medium for 7 days with periodic MIC assessment [5].
- Complementation Assay: recA gene expressed from native promoter on plasmid in ΔrecA strain [5].
Mutation Rate Quantification:
- Fluctuation Analysis: 96 independent cultures per condition assessed for rifampicin-resistant CFUs [5].
- Statistical Models: Luria-Delbrück distribution analysis with Maximum Likelihood Estimation (MLE) for mutation rate calculation [5].
- Poisson Fit Assessment: Goodness-of-fit testing to determine selection versus mutagenesis dominance [5].
Gene Amplification Detection Methods
Experimental Evolution Setup:
- Selection Protocol: Stepwise increase in antibiotic concentration or single high-concentration challenge [44].
- Population Analysis: Profile analysis of subpopulations with different resistance levels to detect heteroresistance [44].
Genomic Analysis Techniques:
- qPCR: Copy number quantification of target genes in resistant isolates [44].
- Whole-Genome Sequencing: Read depth analysis to identify amplified regions [44].
- Stability Assessment: Passage in antibiotic-free medium with periodic resistance monitoring [44].
Table 2: Essential Research Reagents for Investigating SOS-Independent Resistance
| Reagent/Category | Specific Examples | Research Application | Key Function |
|---|---|---|---|
| Bacterial Strains | E. coli MG1655 ΔrecA, JW2669-1 ΔrecA | Resistance evolution studies | RecA-deficient background |
| Antibiotics | Ampicillin, ciprofloxacin, penicillin G, carbenicillin | Selective pressure application | Resistance induction |
| Plasmids | recA complementation vector | Genetic rescue experiments | Mechanism confirmation |
| ROS Detection Probes | DCFH-DA, Hâ‚‚DCFDA | Oxidative stress measurement | ROS quantification |
| Mutation Reporter Systems | Rifampicin resistance assay | Mutation frequency analysis | Mutational supply measurement |
| Gene Expression Tools | qPCR primers for DNA repair and antioxidant genes | Transcriptional profiling | Pathway analysis |
| Selection Markers | Antibiotic resistance cassettes | Strain construction and maintenance | Genetic manipulation |
Research Visualization: Signaling Pathways and Experimental Workflows
The Repair-Redox Axis in SOS-Independent Resistance
Diagram 1: Repair-Redox Axis in SOS-Independent Resistance. This pathway illustrates how RecA deletion creates a hypermutable state through dual impairment of DNA repair and antioxidant defenses, leading to ROS accumulation and increased genetic diversity that is subsequently enriched by antibiotic selection.
Gene Amplification-Mediated Resistance
Diagram 2: Gene Amplification Resistance Pathway. This workflow shows how initial gene duplications lead to tandem amplifications that create heteroresistant populations, with antibiotic selection enriching high-copy-number subpopulations that confer resistance through multiple mechanisms.
Therapeutic Implications and Future Directions
Combating SOS-Independent Resistance
The existence of robust SOS-independent resistance pathways necessitates re-evaluation of current anti-resistance strategies. While SOS inhibition shows promise for countering resistance to DNA-damaging antibiotics like fluoroquinolones [42], this approach would be ineffective against β-lactam resistance evolving through the repair-redox axis [13] [5]. Combination therapies targeting both SOS-dependent and independent pathways offer a more comprehensive approach.
Promising Therapeutic Strategies:
- ROS Potentiation: Compounds that further increase oxidative stress could push bacteria beyond a viability threshold in repair-deficient backgrounds [13].
- Amplification Stabilizers: Agents that maintain amplification-associated fitness costs could prevent resistance reversion [44].
- Efflux Pump Inhibitors: Broad-spectrum inhibitors could counter both SOS-mediated and amplification-mediated efflux overexpression [44] [14].
- Horizontal Transfer Blockers: Conjugation inhibitors remain valuable despite the mechanistic divergence between SOS response and plasmid transfer [45].
Research Priorities and Methodological Considerations
Future research should prioritize several key areas to advance our understanding of SOS-independent resistance:
Technical Advancements:
- Development of real-time amplification tracking systems to monitor copy number dynamics during treatment [44].
- Advanced ROS imaging with single-cell resolution to quantify heterogeneity in oxidative stress [13] [5].
- High-throughput screening for compounds that specifically target repair-deficient, ROS-elevated bacteria [13].
Conceptual Frameworks:
- Integrated models of how SOS-independent pathways interact with canonical resistance mechanisms [46].
- Clinical studies correlating bacterial stress response states with treatment outcomes [14].
- Evolutionary studies examining trade-offs between resistance stability and adaptability in different pathways [44].
The mechanistic divergence between SOS-dependent and independent resistance pathways reveals the remarkable adaptability of bacterial pathogens. By mapping these alternative evolutionary routes, we can develop more resilient antimicrobial strategies that anticipate bacterial countermoves and maintain therapeutic efficacy in the face of evolving resistance.
The SOS response, a conserved DNA damage repair system in bacteria, has long been a target for therapeutic strategies aimed at curbing antibiotic resistance evolution. The central hypothesis posits that inhibiting this inducible mutagenic response would suppress the emergence of resistance. However, recent research reveals a paradoxical phenomenon: genetic or pharmacological inhibition of the SOS response can, under certain conditions, accelerate the development of resistance through alternative, SOS-independent pathways. This whitepaper synthesizes emerging evidence on this paradox, highlighting how RecA deficiency creates a cellular environment of elevated genetic instability through impaired DNA repair and dysregulated redox homeostasis. We present quantitative data from key studies, detailed experimental methodologies, and visualizations of the underlying mechanisms. For researchers in antibiotic tolerance and drug development, these findings necessitate a re-evaluation of SOS-targeting therapeutic approaches and underscore the complexity of bacterial adaptive evolution.
The SOS response is the primary DNA damage response network in prokaryotes, orchestrated by the RecA and LexA proteins [1]. Under normal growth conditions, the LexA repressor binds to operator regions (SOS boxes), suppressing the transcription of over 40 genes involved in DNA repair, mutagenesis, and cell division [27] [1]. Genotoxic stress, such as that caused by UV radiation or antibiotics, leads to the formation of single-stranded DNA (ssDNA) gaps. RecA protein monomers nucleate onto this ssDNA in an ATP-dependent process, forming activated nucleoprotein filaments (RecA*) that facilitate the autocleavage of LexA [27] [1]. This de-represses the SOS regulon, enabling error-free repair processes in the early phase and, under sustained damage, error-prone translesion synthesis (TLS) mediated by low-fidelity DNA polymerases like Pol V (UmuD'â‚‚C) [27].
Given that the error-prone phase of the SOS response significantly contributes to bacterial mutagenesis [27], its inhibition has been proposed as a promising strategy to combat antibiotic resistance. The rationale is straightforward: by co-administering an SOS inhibitor with a DNA-damaging antibiotic, one could reduce the mutation rate and thus slow the evolution of resistance. This review examines the unsettling evidence that challenges this straightforward rationale, presenting the "RecA Paradox" wherein SOS inhibition can inadvertently foster genetic instability and accelerate resistance through alternative pathways.
Quantitative Evidence of the Paradox: SOS Inhibition and Accelerated Resistance
Contrary to the established paradigm, recent findings demonstrate that RecA deletion can lead to the rapid evolution of antibiotic resistance. The following table summarizes key quantitative data from a seminal 2025 study investigating β-lactam resistance in E. coli [13] [5].
Table 1: Quantitative Evidence of Accelerated Resistance in recA-Deficient E. coli
| Metric | Wild Type (MG1655) | ΔrecA Mutant | Experimental Conditions |
|---|---|---|---|
| Time to Resistance (ALE) | ~3 weeks | ~2 days | Cyclic daily exposure to ampicillin (50 µg/mL) [5] |
| MIC Increase | Minimal | 20-fold | Single 8-hour exposure to ampicillin (50 µg/mL) [5] |
| Resistance Stability | N/A | Remained stable after 7-day passaging in antibiotic-free medium [5] | |
| Baseline Mutation Rate | Baseline | 2.5-fold increase (vs. WT) | Calculated from Rifampicin resistance frequency [5] |
| Mutation Rate with Ampicillin | No significant change | 9.5-fold increase (vs. untreated ΔrecA) | Calculated after 8-hour ampicillin exposure [5] |
| Resistance to Other β-lactams | Sensitive | Rapid resistance emergence | Single 8-hour exposure to Penicillin G or Carbenicillin [5] |
This data underscores a rapid and stable evolution of resistance in the absence of the canonical SOS response. The significant increase in the mutation rate of the ΔrecA strain, even without antibiotic pressure, points to a fundamental loss of genetic stability. The enrichment of resistant mutants following ampicillin exposure highlights a powerful selection process acting on this hypermutable population.
Experimental Protocols for Investigating the RecA Paradox
To enable replication and further investigation of this phenomenon, we detail the core methodologies from the cited studies.
Protocol for Single-Exposure Ampicillin Resistance Evolution
This protocol is adapted from Zhang et al. (2025) to demonstrate the rapid emergence of resistance in ΔrecA strains [5].
- Objective: To induce and isolate ampicillin-resistant clones from a ΔrecA strain following a single, short-term antibiotic exposure.
- Materials:
- Bacterial Strains: Wild-type E. coli MG1655 and its isogenic ΔrecA mutant.
- Media: Lysogeny Broth (LB) liquid and solid agar plates.
- Antibiotics: Ampicillin stock solution. Ampicillin-containing LB agar plates (e.g., 50 µg/mL, 100 µg/mL, 200 µg/mL).
- Procedure:
- Inoculum Preparation: Grow overnight cultures of WT and ΔrecA strains in antibiotic-free LB.
- Antibiotic Challenge: Sub-culture the overnight cultures 1:100 into fresh LB containing 50 µg/mL ampicillin. Incubate with shaking at 37°C for 8 hours.
- Plating and Isolation: After 8 hours, serially dilute the cultures in sterile saline and plate onto LB agar plates containing a range of ampicillin concentrations (e.g., 0, 50, 100, and 200 µg/mL).
- Incubation and Analysis: Incubate the plates for 16-24 hours at 37°C. Count the colony-forming units (CFUs) on each plate. Resistant clones will be visible on plates with ampicillin concentrations far exceeding the baseline MIC.
- MIC Confirmation: Purify putative resistant colonies and determine the minimum inhibitory concentration (MIC) for ampicillin using standard broth microdilution methods.
- Stability Assay: Passage the resistant isolates daily in antibiotic-free LB for 7 days. After the final passage, re-test the MIC to confirm stability.
Protocol for Measuring Mutation Rates via Fluctuation Assay
The following Luria-Delbrück fluctuation assay protocol was used to quantify mutation rates in [5].
- Objective: To determine the rate of mutation to rifampicin resistance in WT and ΔrecA strains.
- Materials:
- Bacterial Strains: WT and ΔrecA.
- Media: LB liquid and LB agar plates supplemented with 100 µg/mL rifampicin.
- Procedure:
- Inoculation: Prepare 96 independent 1 mL cultures of LB for each strain. Inoculate each culture with a low number of cells (~100-1000) to ensure they arise from independent founder colonies.
- Outgrowth: Incubate the 96-well plates statically at 37°C until the cultures reach saturation.
- Plating: From each independent culture, plate the entire volume onto LB-rifampicin plates to select for resistant mutants.
- Viable Count: Serially dilute and plate a subset of the cultures onto plain LB plates to determine the total number of viable cells per culture.
- Analysis: Count the number of rifampicin-resistant colonies from each independent culture. Use statistical models, such as the Ma-Sandri-Sarkar Maximum Likelihood Estimator (MLE), to calculate the mutation rate based on the distribution of resistant mutants across the 96 independent cultures [5].
Mechanisms Underpinning the Paradox: The Repair-Redox Axis
The experimental data indicates that the paradoxical emergence of resistance is not a random event but is driven by a defined molecular pathway. The core mechanism involves a dual impairment caused by RecA deletion, leading to a crisis of genetic instability.
The following diagram illustrates the key signaling pathway and logical relationships that define the RecA Paradox.
Diagram 1: The Repair-Redox Axis of SOS-Independent Resistance. This pathway illustrates how RecA deficiency impairs DNA repair and antioxidant defenses, leading to ROS accumulation and increased mutagenesis. Antibiotic pressure then selects for resistant mutants from this diverse population.
As shown in Diagram 1, the absence of RecA has two major consequences that converge to increase mutational supply. First, it directly impairs high-fidelity DNA repair pathways, including the Base Excision Repair (BER) pathway, compromising the cell's ability to correct endogenous DNA damage [13] [5]. Second, RecA deletion leads to the transcriptional repression of key antioxidative defense genes. This dual impairment results in the excessive accumulation of reactive oxygen species (ROS), which cause oxidative DNA damage and further increase the mutation load [13] [5]. In this hypermutable background, antibiotic treatment does not need to induce mutations itself; instead, it acts as a powerful selective agent that enriches for pre-existing or newly generated resistant mutants, leading to the rapid evolution of stable resistance.
The Scientist's Toolkit: Key Research Reagents
Research into the RecA Paradox and SOS-independent mechanisms requires specific genetic tools, bacterial strains, and assay reagents. The following table catalogues essential materials used in the featured studies.
Table 2: Key Research Reagents for Investigating SOS-Independent Resistance
| Reagent / Material | Function / Application | Example from Literature |
|---|---|---|
| ΔrecA Mutant Strains | Isogenic mutant to study phenotypes specifically caused by the absence of RecA, excluding SOS response. | E. coli MG1655 ΔrecA; JW2669-1 from CGSC [5]. |
| SOS Reporter Constructs | Measure SOS induction levels quantitatively, typically by fusing SOS promoters (e.g., sulA, recN) to reporter genes (e.g., gfp, lacZ). | qPCR measurement of sulA and recN mRNA levels [7]. |
| SOS Constitutive Mutants | Strains with genetically altered SOS regulators to study effects of varying SOS activity levels independent of external inducers. | LexA E86P (enhanced auto-cleavage); LexA S119A (cleavage-deficient) [7]. |
| recA Complementation Plasmid | Plasmid expressing recA under its native promoter; used to confirm that observed ΔrecA phenotypes are due to recA loss and not secondary mutations. | Plasmid introduced into ΔrecA restored wild-type sensitivity [5]. |
| ROS Detection Probes | Chemical probes (e.g., H₂DCFDA, DHR123) for fluorescent detection and quantification of intracellular reactive oxygen species. | Used to demonstrate ROS accumulation in ΔrecA strain [5]. |
| Antibiotics for Selection | Antibiotics from different classes to probe for cross-resistance and multidrug resistance phenotypes. | Ampicillin, Penicillin G, Carbenicillin (β-lactams); Ciprofloxacin (FQ); Mitomycin C (DNA cross-linker) [7] [5]. |
| Longdaysin | Longdaysin, MF:C16H16F3N5, MW:335.33 g/mol | Chemical Reagent |
Discussion and Research Implications
The discovery of SOS-independent pathways to resistance represents a paradigm shift with immediate implications for antimicrobial research and development.
- Re-evaluating SOS-Targeting Therapeutics: The initial therapeutic premise that inhibiting RecA or the SOS response would slow resistance evolution is incomplete. While it may be effective against SOS-dependent resistance mechanisms (e.g., to fluoroquinolones), this strategy could inadvertently promote resistance to other antibiotic classes, such as β-lactams, by activating the repair-redox axis [13] [5]. Future drug development must account for the specific antibiotic partner and the potential for paradoxical outcomes.
- The Role of Non-Mutational Resistance: Beyond genetic resistance, the SOS response is linked to phenotypic tolerance mechanisms, such as persister cell formation via toxin-antitoxin systems [1]. The relationship between SOS inhibition and these non-genetic survival strategies requires further exploration, as it may represent an additional layer of complexity in treatment failures.
- Broader Context of DNA Damage Responses: The existence of the RecA Paradox underscores the robustness and redundancy of bacterial stress responses. Cells possess multiple, sometimes compensatory, DDRs [46]. Targeting a single pathway may not be sufficient to halt adaptive evolution and may reveal or exacerbate other vulnerabilities.
The "RecA Paradox" illuminates a critical complexity in the battle against antibiotic resistance. While the SOS response is a well-documented driver of mutagenesis and resistance, its inhibition is not a silver bullet. Evidence now compellingly shows that RecA deficiency can trigger an alternative route to resistance via a repair-redox axis that elevates mutation supply and facilitates the rapid selection of resistant clones. This finding necessitates a more nuanced approach to adjuvant therapies that target bacterial stress responses. Future strategies must consider the potential for pathway redundancy and paradoxical effects, moving beyond single-target approaches toward combination therapies that simultaneously address genetic instability, redox homeostasis, and the selective pressure of antibiotics. For researchers in the field, this paradox opens new avenues of investigation into the fundamental principles of bacterial evolution and the development of more resilient antibacterial treatment protocols.
Reactive Oxygen Species (ROS) Accumulation in DNA Repair-Deficient Strains
Reactive oxygen species (ROS) represent a critical junction between DNA damage repair pathways and the development of antibiotic tolerance. A growing body of evidence demonstrates that deficiencies in key DNA repair pathways, particularly in the context of a compromised SOS response, lead to the accumulation of intracellular ROS, which in turn drives mutagenesis and antibiotic resistance evolution through oxidative stress-mediated mechanisms. This whitepaper synthesizes current research quantifying ROS accumulation in DNA repair-deficient strains, delineates the underlying molecular pathways, and presents standardized experimental methodologies for investigating this relationship. The findings have profound implications for understanding bacterial adaptation to antimicrobial stress and identifying novel therapeutic targets to combat antibiotic resistance.
The integrity of cellular DNA is continuously challenged by endogenous and exogenous agents that cause damage, necessitating robust repair mechanisms. Reactive oxygen species (ROS)—including superoxide (O₂•â»), hydrogen peroxide (Hâ‚‚Oâ‚‚), and hydroxyl radicals (•OH)—are particularly problematic as they function as both byproducts and instigators of genomic instability [47] [48]. While ROS can directly damage DNA, lipids, and proteins, they also serve as signaling molecules in stress response pathways [49]. The relationship between DNA repair capacity and ROS homeostasis is bidirectional: DNA damage can induce ROS production, and conversely, impaired ROS scavenging can exacerbate DNA damage.
Within antibiotic resistance research, the SOS response represents a canonical bacterial reaction to genotoxic stress, coordinating DNA repair, mutagenesis, and survival. However, recent investigations reveal an alternative, SOS-independent pathway to resistance fueled by ROS accumulation in DNA repair-compromised strains [5] [50]. This whitepaper examines the mechanistic basis for ROS accumulation in repair-deficient backgrounds, its quantitative assessment, and its direct implications for antibiotic resistance evolution.
Mechanisms of ROS Accumulation in Repair-Deficient Strains
Impaired Repair and Chronic Oxidative Stress
Deficiencies in base excision repair (BER) and nucleotide excision repair (NER) pathways create a cellular environment prone to chronic oxidative stress. In Saccharomyces cerevisiae, strains deficient in both BER and NER (BER-/NER-) spontaneously accumulate approximately 800-fold more oxidative DNA damage than wild-type counterparts, correlating with substantially increased intracellular ROS [47] [51]. This persistent DNA damage overwhelms the cell's repair capacity, leading to a cycle of genomic instability and ROS production that is not directly related to cell death but functions as a generalized stress response [47] [49].
SOS Response Deficiency and Antioxidant Downregulation
In bacterial systems, disruption of the SOS response master regulator RecA creates a paradoxical scenario that accelerates antibiotic resistance evolution. Escherichia coli lacking recA (ΔrecA) exhibits a dual impairment: compromised DNA repair capability coupled with transcriptional repression of antioxidative defense genes [5]. This dual impairment leads to excessive ROS accumulation, which promotes mutagenesis and enriches for resistance-conferring mutations under antibiotic selection pressure. The finding that recA deficiency increases mutational supply through ROS-mediated mechanisms reveals an SOS-independent evolutionary pathway to multi-drug resistance [5].
Signaling Pathway Activation
DNA damage-induced ROS activates specific stress response pathways. In yeast, the transcription factor Yap1—a major activator of the oxidative stress response—translocates to the nucleus following exposure to the DNA alkylating agent methyl methanesulfonate (MMS) [47] [49]. This relocalization mirrors the response to direct H₂O₂ exposure and confirms ROS signaling activation in response to genotoxic stress. Yap1 nuclear accumulation leads to upregulated expression of ROS-scavenging enzymes, representing the cell's attempt to reestablish redox balance despite persistent DNA damage.
Diagram 1: Molecular mechanism of ROS accumulation in DNA repair-deficient strains and its consequences.
Quantitative Analysis of ROS Accumulation
ROS Levels in Repair-Deficient Yeast Strains
Research using isogenic Saccharomyces cerevisiae strains with defined DNA repair deficiencies demonstrates a clear dose-dependent increase in intracellular ROS following exposure to DNA damaging agents.
Table 1: ROS Accumulation in DNA Repair-Deficient S. cerevisiae Strains
| Strain Genotype | DNA Repair Deficiency | Treatment | ROS Level Increase | Measurement Method |
|---|---|---|---|---|
| Wild-type (WT) | None | MMS (0.025%) | ~1.5-fold | DHR123 fluorescence |
| WT | None | UV-C (50 J/m²) | ~1.8-fold | DHR123 fluorescence |
| BER- (ntg1Δ ntg2Δ apn1Δ) | Base excision repair | MMS (0.025%) | ~2.3-fold | DHR123 fluorescence |
| NER- (rad1Δ) | Nucleotide excision repair | UV-C (50 J/m²) | ~2.5-fold | DHR123 fluorescence |
| BER-/NER- (ntg1Δ ntg2Δ apn1Δ rad1Δ) | Combined BER and NER | Spontaneous (no treatment) | Significant increase vs. WT | DHR123 fluorescence |
Data derived from [47] and [51].
Bacterial RecA Deficiency and Resistance Evolution
In Escherichia coli, deletion of recA accelerates resistance evolution through ROS-mediated mutagenesis, with measurable impacts on resistance development.
Table 2: Antibiotic Resistance Evolution in E. coli ΔrecA Strain
| Strain | Treatment | Resistance Development Time | MIC Increase | Intracellular ROS | Mutation Rate |
|---|---|---|---|---|---|
| Wild-type | Ampicillin (single exposure) | >3 weeks | 4-fold | Baseline | ~1.5 × 10â»â¹ |
| ΔrecA | Ampicillin (single exposure) | 2 days | 20-fold | Significantly elevated | ~4.2 × 10â»â¹ |
| ΔrecA + recA complement | Ampicillin (single exposure) | >3 weeks | 4-fold | Near baseline | ~1.6 × 10â»â¹ |
| ΔsodA (ROS elimination deficient) | Amoxicillin (prolonged) | Accelerated vs. WT | ~64 µg/mL by day 20 | Elevated | Increased |
| ΔkatE (ROS elimination deficient) | Enrofloxacin (prolonged) | Accelerated vs. WT | ~16 µg/mL by day 20 | Elevated | Increased |
Data compiled from [5] and [50].
Experimental Protocols for Assessing ROS in Repair-Deficient Strains
Protocol 1: Yeast Intracellular ROS Quantification Using Fluorescent Dyes
This protocol adapts methodologies from [47] and [49] for measuring DNA damage-induced ROS in Saccharomyces cerevisiae.
Materials:
- Isogenic yeast strains with defined DNA repair deficiencies (WT, BER-, NER-, BER-/NER-)
- YPD media (1% yeast extract, 2% peptone, 2% dextrose)
- DNA damaging agents: Methyl methanesulfonate (MMS), Hâ‚‚Oâ‚‚
- ROS-sensitive fluorescent dyes: Dihydrorhodamine 123 (DHR123)
- Phosphate-buffered saline (PBS)
- Flow cytometer or fluorescence microplate reader
Procedure:
- Cell Culture: Grow yeast strains in YPD media at 30°C to mid-log phase (OD₆₀₀ ≈ 0.5-0.7).
- Genotoxic Treatment: Divide cultures and treat with varying concentrations of DNA damaging agents:
- MMS: 0%-0.05% (v/v) for 2 hours
- Hâ‚‚Oâ‚‚: 0-2 mM for 1 hour
- UV-C irradiation: 0-50 J/m²
- ROS Staining: Harvest cells by centrifugation (3,000 × g, 5 minutes). Wash with PBS and resuspend in PBS containing 5 µg/mL DHR123.
- Incubation: Incubate stained cells in dark at 30°C for 30 minutes.
- Measurement: Analyze fluorescence using flow cytometry (excitation 488 nm, emission 525-530 nm) or fluorescence microplate reader.
- Data Analysis: Express results as fold-increase in fluorescence relative to untreated control cells. Perform statistical analysis using Student's t-test or ANOVA with post-hoc testing.
Troubleshooting Notes:
- Include catalase (100 U/mL) controls to confirm ROS-specific fluorescence.
- Use ROS scavengers (e.g., N-acetylcysteine) as negative controls.
- Ensure consistent cell density across samples as density affects fluorescence readings.
Protocol 2: Bacterial ROS Measurement During Antibiotic Exposure
This protocol is adapted from [5], [50], and [52] for quantifying ROS in bacterial strains under antibiotic selection.
Materials:
- E. coli strains: Wild-type (MG1655), ΔrecA, and complemented strains
- Additional ROS elimination-deficient strains (ΔsodA, ΔsodB, ΔkatE, ΔsoxR, ΔsoxS)
- LB broth and agar
- Antibiotics: Ampicillin, enrofloxacin, kanamycin
- ROS detection probe: 2',7'-Dichlorodihydrofluorescein diacetate (Hâ‚‚DCFDA)
- Flow cytometry equipment
- Anaerobic chamber (for anaerobic control experiments)
Procedure:
- Culture Preparation: Grow bacterial strains overnight in LB broth at 37°C with shaking (200 rpm).
- Subculture: Dilute overnight cultures 1:100 in fresh LB and grow to mid-log phase (OD₆₀₀ ≈ 0.4-0.6).
- Antibiotic Exposure: Add sub-MIC concentrations of antibiotics:
- Ampicillin: 5-50 µg/mL (depending on strain MIC)
- Enrofloxacin: 0.005-0.05 µg/mL
- Kanamycin: 5-25 µg/mL
- Time-Course Sampling: Collect samples at 0, 1, 2, 3, 4, 5, and 6 hours post-treatment.
- ROS Staining: For each time point, harvest 1 mL culture, wash with PBS, and resuspend in PBS containing 10 µM H₂DCFDA.
- Incubation: Incubate in dark at 37°C for 30 minutes.
- Flow Cytometry: Analyze approximately 10,000 events per sample using flow cytometry (FITC channel).
- Data Analysis: Calculate geometric mean fluorescence intensity for each sample. Compare ROS production kinetics between strains and treatments.
Validation Experiments:
- Include thiourea (ROS scavenger, 10-20 mM) treated controls to confirm ROS-specific signals.
- Perform anaerobic culture experiments to verify oxygen-dependent ROS production.
- Conduct survival assays in parallel to correlate ROS levels with cell viability.
Diagram 2: Experimental workflow for assessing ROS accumulation in DNA repair-deficient strains.
The Scientist's Toolkit: Essential Research Reagents
Table 3: Key Research Reagents for Studying ROS in DNA Repair-Deficient Strains
| Reagent/Category | Specific Examples | Function/Application | Key Research Findings |
|---|---|---|---|
| DNA Repair-Deficient Strains | S. cerevisiae BER-/NER- (ntg1Δ ntg2Δ apn1Δ rad1Δ); E. coli ΔrecA | Models for studying repair deficiency consequences | BER-/NER- yeast accumulate 800× more oxidative DNA damage [51]; ΔrecA E. coli shows accelerated resistance evolution [5] |
| ROS Detection Probes | Dihydrorhodamine 123 (DHR123), Hâ‚‚DCFDA | Fluorescent detection of intracellular ROS | Dose-dependent ROS increase measured post-DNA damage [47] [52] |
| ROS Scavengers/Modulators | Thiourea, N-acetylcysteine | Experimental control of ROS levels | Thiourea decelerates resistance development [50] |
| SOS Response Inhibitors | OXF-077 | Suppresses SOS-mediated mutagenesis | Suppresses evolution of quinolone resistance [42] |
| Genotoxic Agents | Methyl methanesulfonate (MMS), Hâ‚‚Oâ‚‚, UV-C | Induce specific DNA damage types | MMS treatment causes Yap1 nuclear relocalization [47] |
| Antibiotics for Selection | β-lactams, Fluoroquinolones, Aminoglycosides | Selective pressure for resistance evolution | Bactericidal antibiotics induce ROS; bacteriostatic tetracycline does not [50] |
| Antioxidant-Deficient Strains | ΔsodA, ΔsodB, ΔkatE | Models for impaired ROS elimination | Accelerated resistance development under antibiotic pressure [50] |
Research Implications and Future Directions
The relationship between DNA repair deficiency and ROS accumulation presents both challenges and opportunities in antimicrobial research. The findings that RecA-deficient bacteria rapidly develop antibiotic resistance through ROS-mediated mechanisms necessitate a reevaluation of therapeutic strategies that target the SOS response [5] [7]. While SOS inhibition remains conceptually attractive for limiting resistance evolution, complementary approaches must address the alternative pathways that emerge under repair-deficient conditions.
Promising research directions include:
- Combination Therapies: Pairing existing antibiotics with ROS modulators or DNA repair inhibitors to exploit the vulnerability of repair-deficient strains [22] [42].
- Diagnostic Applications: Leveraging ROS dynamics as quantitative indicators of antibiotic susceptibility, as demonstrated in the ROS-AST (ROS-based antibiotic susceptibility testing) method that correlates peak ROS accumulation with minimal inhibitory concentration [52].
- Evolutionary Control: Identifying intervention points during the reversible phase of resistance evolution before mutations become fixed, potentially through ROS monitoring during antibiotic treatment [50] [52].
The mechanistic understanding of how DNA repair deficiencies alter cellular redox balance provides a framework for developing next-generation antimicrobials that specifically target the repair-redox axis to suppress resistance evolution while enhancing the efficacy of existing antibiotics.
Antibiotic-Specific Variations in SOS Induction and Conjugation Promotion
The global rise of antimicrobial resistance (AMR) represents one of the most severe threats to modern medicine, with drug-resistant infections contributing to millions of deaths annually [53]. The dissemination of antibiotic resistance genes occurs not only through clonal expansion but also via horizontal gene transfer, with bacterial conjugation serving as a critical mechanism for the spread of resistance determinants among bacterial populations [7] [53]. Understanding the environmental and pharmacological factors that regulate conjugation is therefore essential for controlling the AMR crisis.
The bacterial SOS response, a conserved DNA damage repair system, has been historically implicated in the regulation of horizontal gene transfer. This pathway is activated by genotoxic stresses, including those induced by various classes of antibiotics, which trigger the RecA-LexA mediated signaling cascade [7] [11]. However, emerging research reveals a more complex relationship, demonstrating that antibiotic-induced SOS response and conjugation promotion do not always correlate directly, suggesting the involvement of additional, SOS-independent pathways [7]. This technical guide synthesizes current research on antibiotic-specific variations in SOS induction and conjugation promotion, providing researchers with comprehensive experimental data, methodologies, and conceptual frameworks to advance this critical field of study.
Core Mechanisms: SOS Response and Conjugative Transfer
The SOS Response Pathway
The SOS response is the primary bacterial DNA damage repair system, coordinated by the key regulators RecA and LexA. Under normal conditions, LexA represses the SOS regulon by binding to specific SOS-box sequences in the promoter regions of target genes. Upon exposure to genotoxic stress (e.g., antibiotics, UV light), single-stranded DNA (ssDNA) accumulates and associates with RecA and ATP, forming RecA–ssDNA–ATP filaments (RecA*). This complex stimulates the autocleavage of LexA, derepressing the SOS regulon and initiating DNA repair processes [7] [11].
The SOS regulon encompasses over 48 genes in Escherichia coli, including those involved in nucleotide excision repair (e.g., uvrA), homologous recombination (e.g., recA), and error-prone transfusion synthesis (e.g., umuDC, dinB) [7]. The sulA gene, also SOS-regulated, acts as a cell division inhibitor that provides time for DNA repair before replication resumes. While this system typically facilitates high-fidelity DNA repair, sustained damage can lead to the expression of error-prone polymerases that increase mutagenesis rates, potentially accelerating the evolution of antibiotic resistance [7] [11].
Conjugative Plasmid Transfer
Conjugative transfer of plasmids between bacteria represents a fundamental mechanism for the dissemination of antibiotic resistance genes. This process requires the expression of transfer (tra) and pilus (pil) genes, which facilitate the formation of a type IV secretion system necessary for intercellular DNA transfer [7]. The genetic regulation of these systems varies among plasmid incompatibility groups, creating complex interplay between chromosomal stress responses like SOS and plasmid-encoded transfer machinery.
Recent evidence suggests that certain antimicrobial agents can enhance conjugative plasmid transfer frequencies, though the ability to induce conjugation appears to depend on both the antibiotic class and the specific resistance genes carried by the plasmid [7] [25]. The potential connection between SOS-mediated upregulation and plasmid transfer has therefore become a significant focus of AMR research.
Figure 1: SOS Response Pathway and Potential Links to Conjugation. The core SOS signaling cascade begins with antibiotic-induced DNA damage, leading to RecA activation, LexA cleavage, and subsequent expression of DNA repair genes. The dashed line indicates the potential, context-dependent connection to conjugation activation.
Antibiotic-Specific Effects on SOS and Conjugation
Quantitative Variations Across Antibiotic Classes
Groundbreaking research has demonstrated that different classes of antibiotics vary significantly in their ability to induce the SOS response and promote conjugative transfer. These variations suggest distinct mechanistic pathways that may operate independently of one another.
Table 1: Antibiotic-Specific Induction of SOS Response and Conjugation Frequency
| Antibiotic | Class | Primary Mechanism | SOS Induction (sulA expression) | tra Gene Expression | Conjugation Frequency |
|---|---|---|---|---|---|
| Cefotaxime | β-lactam | Cell wall synthesis inhibition | ~5-fold increase [7] | Significantly induced [7] | Significantly increased [7] |
| Ciprofloxacin | Fluoroquinolone | DNA gyrase inhibition | ~14-fold increase [7] | Unaffected [7] | Unaffected [7] |
| Mitomycin C | Antitumor antibiotic | DNA crosslinker | ~100-fold increase [7] | Significantly induced [7] | Significantly increased [7] |
Notably, cefotaxime induces conjugation with only minimal SOS induction, while ciprofloxacin triggers substantial SOS response without affecting conjugation frequencies. Mitomycin C, a potent DNA crosslinker, hyper-induces both systems [7]. This dissociation between SOS response levels and conjugation promotion highlights the complexity of these regulatory networks and suggests that SOS-independent pathways significantly contribute to antibiotic-induced conjugation.
SOS-Independent Resistance Mechanisms
Recent evidence confirms the existence of SOS-independent pathways to antibiotic resistance. Studies demonstrate that E. coli lacking RecA can rapidly develop stable β-lactam resistance (20-fold MIC increase within 8 hours) after a single ampicillin exposure [13]. This alternative pathway involves two distinct evolutionary forces: increased mutational supply and antibiotic-driven selection.
In RecA-deficient strains, impaired DNA repair and downregulated base excision repair pathways concurrent with repression of antioxidative defence genes lead to excessive accumulation of reactive oxygen species (ROS). This oxidative environment promotes genetic instability and creates a selective landscape favoring the expansion of resistant clones, demonstrating the repair-redox axis as a key determinant of bacterial evolvability under antimicrobial stress [13].
Bioenergetic stress represents another SOS-independent mechanism that potentiates antimicrobial resistance and persistence. When ATP consumption exceeds production, decreasing the ATP/ADP ratio and adenylate energy charge, bacteria experience bioenergetic stress that accelerates fluoroquinolone resistance evolution via enhanced ROS production, mutagenic break repair, and transcription-coupled repair [25].
Experimental Approaches and Methodologies
Establishing SOS Response Mutant Strains
To systematically investigate the relationship between SOS response levels and conjugation frequencies, researchers have developed a series of isogenic E. coli MG1655 mutants with SOS responses ranging from constitutively inactive to hyper-induced states [7].
Protocol: Construction of SOS Mutant Series
- Start with wild-type E. coli MG1655 harboring the plasmid of interest (e.g., pTF2, an IncI1 plasmid carrying blaCTX-M-1).
- Generate SOS-inactivated mutants:
- ΔrecA: Eliminates the LexA auto-cleavage inducer
- LexA S119A: Expresses a non-cleavable LexA mutant
- Generate SOS-enhanced mutants:
- LexA E86P: Increases the rate of LexA auto-cleavage
- SOS: A spontaneously occurring hyper-induced mutant with multiple *lexA mutations (E74V, S119A, P176L, I188T)
- Complement mutants with wild-type lexA gene (e.g., SOS*_C) to confirm phenotype restoration [7].
These engineered strains enable researchers to dissect the specific contributions of the SOS response to conjugation apart from other antibiotic-induced effects. The SOS* mutant, for instance, exhibits dramatic upregulation of SOS genes (47- and 128-fold increases in sulA and recN expression, respectively) without significant growth impairment [7].
Measuring Conjugation Frequencies
Standardized conjugation assays are essential for quantifying plasmid transfer rates under different antibiotic treatments.
Protocol: Conjugation Frequency Assay
- Prepare donor and recipient strains: Use donor strain carrying the conjugative plasmid (e.g., IncI1 or IncFII plasmids with blaCTX-M resistance genes) and a plasmid-free recipient strain with appropriate selection markers.
- Grow cultures to mid-exponential phase (OD~600~ ≈ 0.5) in appropriate media.
- Mix donor and recipient cells at a standardized ratio (typically 1:10 donor:recipient) and concentrate if necessary.
- Spot mixture on filters placed on non-selective agar plates, with or without sub-inhibitory antibiotic concentrations (½ MIC).
- Incubate for conjugation to occur (typically 4-8 hours at 37°C).
- Resuspend cells and plate serial dilutions on selective media to quantify:
- Donor cells (antibiotic selecting for plasmid)
- Recipient cells (antibiotic selecting for chromosomal marker)
- Transconjugants (selecting for both markers)
- Calculate conjugation frequency as the number of transconjugants per recipient cell [7].
This methodology allows for direct comparison of how different antibiotics and genetic backgrounds affect plasmid transfer efficiency.
Gene Expression Analysis
Quantitative assessment of SOS gene and tra gene expression provides mechanistic insights into the regulatory networks governing conjugation.
Protocol: Gene Expression Analysis via qPCR
- Treat bacterial cultures with sub-inhibitory concentrations of antibiotics (½ MIC) or appropriate controls.
- Collect samples at mid-exponential phase for RNA extraction.
- Extract total RNA using commercial kits with DNase treatment to remove genomic DNA contamination.
- Synthesize cDNA using reverse transcriptase with random hexamers or gene-specific primers.
- Perform quantitative PCR using SYBR Green or TaqMan chemistry with primers specific for:
- SOS genes (sulA, recN)
- Conjugation genes (traF, traM)
- Housekeeping genes (rpoB, gyrB) for normalization
- Analyze data using the comparative C~T~ method (2^-ΔΔCT^) to calculate fold-changes in gene expression [7].
This approach confirmed that cefotaxime and mitomycin C induced both SOS genes and tra genes, while ciprofloxacin induced only SOS genes without affecting tra gene expression [7].
Figure 2: Experimental Workflow for Assessing SOS and Conjugation. The methodology involves parallel tracks for gene expression analysis and conjugation assays following antibiotic treatment of appropriately engineered bacterial strains.
Research Reagent Solutions
Table 2: Essential Research Reagents for SOS and Conjugation Studies
| Reagent/Category | Specific Examples | Function/Application |
|---|---|---|
| Bacterial Strains | E. coli MG1655 (wild-type) [7] | Base genetic background for mutant construction |
| KEIO collection mutants [11] | Source of single-gene knockout mutants (ΔrecA, ΔfumC, etc.) | |
| Clinical isolates (e.g., ST131) [11] | Validation in clinically relevant strains | |
| SOS Mutant Series | ΔrecA, LexA S119A [7] | SOS-inactivated strains |
| LexA E86P, SOS* [7] | SOS-enhanced strains | |
| Plasmids | IncI1 plasmids (e.g., pTF2) [7] | Model conjugative plasmids with resistance genes |
| IncFII plasmids with blaCTX-M [7] | Alternative incompatibility groups for comparison | |
| Antibiotics | Cefotaxime [7] | β-lactam inducer of conjugation |
| Ciprofloxacin [7] | Fluoroquinolone inducer of SOS only | |
| Mitomycin C [7] | Potent SOS hyper-inducer | |
| Molecular Biology Tools | pCP20 plasmid [11] | Kanamycin cassette excision |
| pKOBEG plasmid [11] | Arabinose-inducible recombinase for gene replacement | |
| Analytical Assays | LC-MS/MS [25] | Metabolomic profiling and energy charge measurements |
| NAD/NADH-Glo Assay [25] | Quantification of redox state | |
| Droplet microfluidics [54] | Single-cell MIC and heteroresistance studies |
Therapeutic Implications and Future Directions
The mechanistic divergence between SOS induction and conjugation promotion has significant implications for developing strategies to combat antimicrobial resistance. Research indicates that targeting the SOS response alone may be insufficient to prevent antibiotic-induced conjugation, since alternative pathways can activate transfer genes [7]. Combination approaches that address both SOS-dependent and SOS-independent mechanisms show greater promise.
Studies demonstrate that co-targeting the SOS response with metabolic pathways like the tricarboxylic acid (TCA) cycle significantly enhances antibiotic susceptibility. For example, double mutants lacking both recA and fumC (encoding a fumarase) show dramatically increased sensitivity to cephalosporins and quinolones compared to single mutants [11]. This approach has been validated in both laboratory strains and clinical E. coli ST131 isolates, suggesting broad applicability [11].
Inhibitors of the generalized stress response, such as dequalinium, have shown strong ability to inhibit SOS-mediated biofilm formation, while zinc acetate directly inhibits RecA activity [55]. These compounds represent promising adjuvants for combination therapies aimed at reducing the emergence and spread of resistance.
Future research directions should focus on elucidating the precise SOS-independent pathways that activate conjugation under antibiotic stress, developing specific inhibitors of key regulators in these pathways, and validating combination therapies in clinically relevant models. The integration of single-cell technologies, such as droplet microfluidics [54], with multi-omics approaches will further advance our understanding of the heterogeneous responses to antibiotic treatment within bacterial populations.
The relationship between antibiotic-induced SOS response and conjugation promotion exhibits significant antibiotic-class specificity, with clear dissociations observed between SOS induction levels and plasmid transfer frequencies. This mechanistic divergence underscores the complexity of bacterial stress responses and highlights the limitations of targeting single pathways to prevent resistance dissemination. A comprehensive understanding of both SOS-dependent and SOS-independent mechanisms, particularly those involving metabolic reprogramming and bioenergetic stress, will be essential for developing next-generation therapeutic strategies effective against multidrug-resistant pathogens. The experimental frameworks and methodologies outlined in this technical guide provide researchers with the essential tools to advance this critical area of antimicrobial research.
The bacterial SOS response represents a compelling target for innovative combination therapies aimed at combating antibiotic resistance. This conserved DNA repair system, activated by antibiotic-induced damage, plays a pivotal role in bacterial survival, mutagenesis, and resistance acquisition [6]. When DNA damage occurs, single-stranded DNA accumulates and activates RecA, which stimulates the autocleavage of the LexA repressor, derepressing SOS genes [6]. This cascade promotes DNA repair but also increases mutation rates and antibiotic tolerance through error-prone polymerases and other mechanisms.
Targeting this system presents unique timing and dosage challenges that require precise pharmacological optimization. The SOS response's central role in resistance evolution makes its inhibition a promising strategy for enhancing antibiotic efficacy. This technical guide examines current approaches for optimizing SOS-targeting combination therapies, integrating fundamental mechanisms with practical dosage considerations for research and development professionals.
SOS Response Mechanisms and Resistance Dynamics
Core SOS Pathway and Antibiotic Induction
The SOS pathway activates through a finely-tuned molecular mechanism. Under normal conditions, LexA represses approximately 40 genes comprising the SOS regulon. DNA damage generates single-stranded DNA (ssDNA) regions that recruit RecA, forming nucleoprotein filaments that facilitate LexA cleavage [6]. This de-repression upregulates DNA repair proteins (e.g., UvrA, UmuC, UmuD) while simultaneously inducing error-prone translesion synthesis polymerases (DNA pol IV and V) that increase mutagenesis and resistance development [2].
Antibiotics induce the SOS response through diverse mechanisms:
- Fluoroquinolones (e.g., ciprofloxacin) directly cause DNA double-strand breaks by inhibiting DNA gyrase and topoisomerase IV [13]
- β-lactams (e.g., ampicillin) activate the DpiBA two-component system through impaired cell wall synthesis, indirectly inducing SOS [5]
- General bactericidal antibiotics generate reactive oxygen species (ROS) that cause DNA damage, triggering the response [6]
SOS-Independent Resistance Pathways
Recent evidence reveals surprising complexity in resistance mechanisms. Contrary to established models, RecA-deficient E. coli can rapidly develop stable, heritable β-lactam resistance (20-fold MIC increase within 8 hours) through SOS-independent pathways [13] [5]. This alternative pathway involves impaired base excision repair and downregulated antioxidant defenses, leading to ROS accumulation and increased mutagenesis [13]. This redundancy underscores the importance of multi-target approaches in combination therapy design.
Table 1: SOS Response Components as Therapeutic Targets
| Component | Function | Therapeutic Targeting Approach | Experimental Evidence |
|---|---|---|---|
| RecA | DNA strand exchange, LexA co-protease activation | Direct inhibition (e.g., suramin), gene inactivation | ΔrecA mutants show reduced resistance evolution to fluoroquinolones [6] |
| LexA | Transcriptional repressor of SOS regulon | Inhibition of autoproteolysis | Small molecule inhibitors identified through screening [6] |
| DNA pol IV/V | Error-prone translesion synthesis | Specific inhibitor development | SOS-induced hypermutation requires these polymerases [2] |
| ROS Detoxification Systems | Neutralize reactive oxygen species | Adjuvants that increase oxidative stress | RecA deficiency represses antioxidative genes, increasing ROS [13] |
Combination Therapy Strategies and Experimental Evidence
SOS Inhibition with Conventional Antibiotics
Co-targeting the SOS response with conventional antibiotics represents a promising strategy for enhancing antibacterial efficacy and suppressing resistance. Several approaches have demonstrated success:
RecA Inhibition with Antibiotics Zinc acetate (0.3-0.5 mM) effectively suppresses ciprofloxacin-induced SOS hypermutation to rifampin, minocycline, and fosfomycin in vitro and in rabbit intestinal infection models [2]. This combination reduces mutation frequencies by 10-100 fold without significantly altering antibiotic MICs, suggesting purely anti-mutagenic effects.
Dual Pathway Disruption Simultaneous disruption of SOS and other DNA damage response pathways shows enhanced effects. ΔfumC/ΔrecA and ΔaidB/ΔrecA double mutants exhibit significantly increased susceptibility to cephalosporins and quinolones compared to single mutants [56]. This approach targets both the primary SOS pathway and secondary adaptive responses involving TCA cycle metabolites and alkylation repair.
Timing Considerations for Combination Therapies
The temporal sequence of administration critically influences combination therapy outcomes:
Preemptive SOS Inhibition Administering SOS inhibitors before or concurrently with antibiotics maximizes prevention of resistance development. In rabbit intestinal models, zinc co-administration with ciprofloxacin or zidovudine prevented enrichment of resistant mutants [2].
Exploiting SOS-Independent Pathways In RecA-deficient backgrounds, rapid resistance evolution occurs through alternative mechanisms. These findings suggest that effective combination therapies must address both SOS-dependent and independent pathways, potentially requiring different timing protocols [13].
Table 2: Experimental Evidence for SOS-Targeting Combinations
| Antibiotic Class | SOS-Targeting Agent | Experimental Model | Key Findings | Dosage Considerations |
|---|---|---|---|---|
| Fluoroquinolones (Ciprofloxacin) | Zinc acetate | In vitro (E. coli), Rabbit intestinal infection | Reduced resistance frequency to rifampin, minocycline, fosfomycin by 10-100× | 0.3-0.5 mM zinc with 0.1× MIC ciprofloxacin [2] |
| β-lactams (Ampicillin) | recA gene deletion | In vitro (E. coli) adaptive evolution | 20× MIC increase in 8 hours in ΔrecA via SOS-independent pathway | Single exposure to 50 μg/mL (10× MIC) ampicillin [13] |
| Cephalosporins, Quinolones | ΔfumC/ΔrecA double mutation | In vitro (E. coli BW25113, ST131 clinical isolate) | Enhanced susceptibility compared to single ΔrecA mutant | Strain-dependent MIC reductions [56] |
| Multiple Classes | Suramin | In vitro (E. coli) | Inhibits RecA-mediated strand exchange and LexA cleavage | 50-200 μM suramin with sub-MIC antibiotics [6] |
Experimental Protocols and Methodologies
In Vitro SOS Inhibition and Resistance Monitoring
Checkerboard Susceptibility Testing This standard method evaluates antibiotic-SOS inhibitor interactions:
- Prepare serial dilutions of both compounds in Mueller-Hinton broth in 96-well plates
- Inoculate with ~5×10^5 CFU/mL of target bacteria
- Incubate 18-24 hours at 35°C
- Determine Fractional Inhibitory Concentration (FIC) indices: FIC index = (MIC of drug A in combination/MIC of drug A alone) + (MIC of drug B in combination/MIC of drug B alone)
- Interpret results: FIC ≤0.5 = synergy; >0.5-4 = additive/indifferent; >4 = antagonism [56]
Mutation Frequency Analysis Quantify resistance emergence under combination treatment:
- Expose bacterial cultures (~10^8 CFU) to sub-MIC antibiotics ± SOS inhibitors for 8-24 hours
- Plate serial dilutions on non-selective and antibiotic-containing media
- Calculate mutation frequency = (CFU on antibiotic media)/(total CFU)
- Compare treated vs. untreated controls; zinc typically reduces mutation frequency 10-100 fold [2]
In Vivo Validation Models
Rabbit Intestinal Loop Model This system assesses SOS inhibition in a clinically relevant setting:
- Anesthetize rabbits and create ligated intestinal loops
- Inject ~10^7 CFU of enteropathogenic E. coli with/without SOS inducers (e.g., ciprofloxacin, zidovudine) and SOS inhibitors (e.g., zinc)
- After 18-24 hours, collect intestinal fluid and determine bacterial counts and resistance frequencies
- Compare treatment groups; zinc acetate (0.3 mM) significantly reduces in vivo resistance development [2]
Quantitative Data Analysis and Dosage Optimization
Exposure-Response Relationships
Effective combination therapy requires careful dosage optimization based on exposure-response relationships. Model-informed approaches include:
Population Pharmacokinetic-Pharmacodynamic Modeling This methodology correlates drug exposure with antibacterial effects and resistance suppression:
- Collect time-concentration data for both antibiotic and SOS inhibitor
- Measure bacterial killing and resistance emergence across concentration ranges
- Develop mathematical models predicting optimal dosing regimens
- Identify exposure thresholds for resistance prevention [57]
Clinical Utility Index Frameworks Quantitatively integrate efficacy and toxicity data:
- Define weights for key outcomes (e.g., bactericidal activity = 0.4, resistance prevention = 0.4, toxicity = 0.2)
- Score each dosage regimen across these parameters
- Calculate weighted sums to identify optimal balance
- Validate predictions in appropriate models [58]
Dosage Considerations for Specific Combinations
Zinc-Antibiotic Combinations
- Zinc acetate (0.3-0.5 mM) effectively inhibits SOS without significant toxicity
- Higher concentrations may cause nonspecific effects
- Timing critical: must be present during antibiotic exposure to prevent hypermutation [2]
RecA Inhibitor Dosing
- Suramin (50-200 μM) shows concentration-dependent SOS inhibition
- Requires balancing RecA inhibition with potential off-target effects
- Optimal ratios with antibiotics must be empirically determined [6]
Research Reagent Solutions
Table 3: Essential Research Tools for SOS-Combination Studies
| Reagent/Cell Line | Key Application | Considerations for Use |
|---|---|---|
| KEIO Collection E. coli Mutants (ΔrecA, ΔlexA, DNA polymerase mutants) | Mechanistic studies of SOS pathway components | Confirm genotype; complementation strains recommended [56] |
| Clinical Isolate Panels (including ST131 E. coli, MDR P. aeruginosa) | Validation in diverse genetic backgrounds | Account for strain-specific differences in SOS regulation [56] |
| SOS Reporter Constructs (e.g., sulA-gfp, recA-lux) | Real-time monitoring of SOS induction | Correlate expression with resistance phenotypes [2] |
| Zinc Acetate (200-500 mM stock solutions) | SOS inhibition in physiological models | Filter sterilize; prepare fresh to avoid precipitation [2] |
| Suramin (10-100 mM stocks in DMSO or water) | Small molecule RecA inhibition | Monitor off-target effects at higher concentrations [6] |
| In Vivo Model Systems (rabbit intestinal loop, mouse infection models) | Therapeutic efficacy validation | Species-specific differences in metal ion pharmacology [2] |
Signaling Pathways and Experimental Workflows
SOS Response Pathway and Therapeutic Inhibition
Combination Therapy Experimental Workflow
Optimizing combination therapies that target the SOS response requires meticulous attention to timing, dosage, and bacterial strain characteristics. Key principles emerge from current research: effective combinations must address both SOS-dependent and independent resistance pathways; SOS inhibitors should be present during initial antibiotic exposure to prevent resistance enrichment; and dosage optimization requires model-informed approaches that balance efficacy with safety.
Future work should focus on developing more specific SOS inhibitors with improved pharmacological properties, validating optimized combinations in clinically relevant models, and exploring connections between SOS inhibition and other resistance mechanisms such as efflux pump regulation and biofilm formation. The integration of SOS-targeting strategies with other innovative approaches, including collateral sensitivity-based treatments [59], represents a promising avenue for developing robust combination therapies that outpace bacterial evolution.
Therapeutic Strategies: Validating SOS Response as an Antibiotic Adjuvant Target
Comparative Analysis of SOS Inhibition Across Antibiotic Classes
The bacterial SOS response is a conserved DNA damage repair network that is pivotal for bacterial survival under genotoxic stress. Its activation, initiated by antibiotics that cause DNA damage directly or indirectly, promotes mutagenesis, horizontal gene transfer, and the evolution of antibiotic resistance. Inhibiting the SOS response has emerged as a promising strategy to counteract antibiotic resistance. This review analyzes the feasibility and effectiveness of SOS inhibition across different antibiotic classes, situating this approach within the broader research on antibiotic tolerance. We synthesize recent findings to compare the dependency of various antibiotics on the SOS response for resistance development, evaluate the consequences of SOS inhibition, and discuss the implications for combination therapies.
The SOS Response Pathway and Its Role in Antibiotic Resistance
Core Mechanism of the SOS Response
The SOS response is a finely regulated genetic circuit for DNA damage repair in prokaryotes. Under normal conditions, the LexA repressor protein binds to specific DNA sequences (SOS boxes), suppressing the transcription of over 48 genes in the SOS regulon [7]. Genotoxic stress, such as that induced by certain antibiotics, leads to the accumulation of single-stranded DNA (ssDNA). This recruits RecA, which forms nucleoprotein filaments (RecA*) that facilitate the autocleavage of LexA [7]. LexA inactivation derepresses the SOS regulon, initiating DNA repair through high-fidelity mechanisms involving genes like uvrA (nucleotide excision repair) and recA (homologous recombination). Under severe, persistent damage, error-prone polymerases (e.g., umuDC, dinB) are transcribed, increasing mutagenesis and the potential for resistance development [7].
SOS Activation and Resistance Mechanisms
Antibiotics induce the SOS response through diverse mechanisms, which in turn fuels resistance via several pathways:
- Induction of Mutagenesis: Error-prone SOS polymerases introduce mutations across the genome, which can confer resistance [60].
- Enhancement of Horizontal Gene Transfer: The SOS response can upregulate the transfer of mobile genetic elements, such as plasmids and integrons, disseminating resistance genes [61].
- Modulation of Integron Rearrangement: SOS activation induces the expression of integrases in class 1 integrons, catalyzing cassette rearrangements that can unlock silent resistance genes [61].
Table 1: Antibiotic Classes and Their Mechanisms of SOS Induction
| Antibiotic Class | Example | Primary Mechanism of SOS Induction | Resistance Outcome Linked to SOS |
|---|---|---|---|
| Fluoroquinolones | Ciprofloxacin | Direct DNA damage via DNA gyrase inhibition [7] | Increased mutation frequency, potential for resistance development [60] |
| β-Lactams | Cefotaxime, Ampicillin | Indirect; via impaired cell wall synthesis and activation of stress responses [7] [5] | Plasmid conjugation, potential integrase-mediated gene cassette rearrangement [7] [61] |
| DNA Crosslinkers | Mitomycin C | Direct DNA damage causing crosslinks [7] | Hyper-induction of SOS, plasmid conjugation [7] |
Comparative Analysis of SOS Dependence Across Antibiotic Classes
The relationship between antibiotic stress and the SOS response is complex and varies significantly by antibiotic class. This variability dictates the potential utility of SOS inhibition as an adjuvant strategy.
Fluoroquinolones
Fluoroquinolones, like ciprofloxacin, directly cause DNA double-strand breaks by inhibiting DNA gyrase, potently inducing the SOS response [7]. Studies show a clear dependency on RecA and the SOS pathway for resistance evolution following fluoroquinolone exposure.
- Evidence for SOS-Dependence: In Pseudomonas aeruginosa, deletion of
recAsignificantly reduced resistance development to fluoroquinolones [5]. - Limitations of SOS Inhibition: While SOS inhibition reduces resistance, it does not eliminate the primary bactericidal activity of the drug. Furthermore, exposure to sub-inhibitory concentrations (SICs) of ciprofloxacin can significantly upregulate
recAexpression and increase mutation frequencies in pathogens like Proteus spp., fostering cross-resistance [60].
β-Lactam Antibiotics
β-lactams target cell wall synthesis and can indirectly induce the SOS response, but the functional consequences for resistance are more nuanced and often plasmid-dependent.
- SOS-Independent Conjugation: A key study found that β-lactams like cefotaxime could induce plasmid conjugation without a strong correlation to the level of SOS induction. Genetic SOS mutants (from constitutively inactive to hyper-induced) showed no direct link between SOS activity and conjugation frequency for IncI1 and IncFII plasmids [7]. This suggests that cefotaxime-induced conjugation is an SOS-independent phenomenon.
- SOS-Independent Mutational Resistance: Contrary to established paradigms, β-lactam resistance can evolve rapidly and stably in E. coli lacking
recA[5]. A single exposure to ampicillin drove a 20-fold increase in MIC in ΔrecAstrains through an SOS-independent mechanism. This pathway involves impaired DNA repair and repressed antioxidant defenses, leading to reactive oxygen species (ROS) accumulation and selection of resistant mutants [5].
Table 2: Comparative Consequences of SOS Inhibition by Antibiotic Class
| Antibiotic Class | Effect of SOS/RecA Inhibition on Resistance Development | Key Evidence and Underlying Mechanism |
|---|---|---|
| Fluoroquinolones | Reduces resistance evolution [5] | SOS is a primary pathway for error-prone repair and mutagenesis after direct DNA damage. |
| β-Lactams | Variable effect; can accelerate resistance via alternative pathways [5] | SOS inhibition impairs DNA repair and downregulates base excision repair/antioxidant genes, leading to ROS accumulation and increased mutational supply. Antibiotic pressure then selects for resistant mutants. |
| Aminoglycosides | Limited direct evidence; may induce SOS indirectly via ROS production [14] | Proposed indirect induction through oxidative stress; role in resistance development requires further characterization. |
Divergent and Convergent Pathways to Resistance
The evidence reveals two broad evolutionary paths to antibiotic resistance:
- SOS-Dependent Pathways: Prevalent with direct DNA-damaging agents like fluoroquinolones, where SOS-induced mutagenesis is a key driver of resistance.
- SOS-Independent Pathways: Prominent in some responses to β-lactams, where inhibition of the SOS response creates a genetic and oxidative background that paradoxically accelerates the selection of resistance through alternative mechanisms [5].
The following diagram summarizes these two major pathways and the consequence of SOS inhibition.
Experimental Approaches for Studying SOS Inhibition
Key Methodologies and Protocols
Research in this field relies on specific genetic tools and phenotypic assays to dissect the SOS response.
- Construction of SOS Genetic Mutants: A series of isogenic strains with varying SOS activity levels is crucial. This includes:
- Δ
recAstrain: Eliminates the inducer of LexA auto-cleavage. - LexA S119A mutant: A non-cleavable LexA variant, constitutively repressing the SOS regulon.
- LexA E86P mutant: A hyper-cleavable LexA variant leading to constitutive SOS induction.
- SOS* mutant: A strain with multiple mutations in
lexAresulting in SOS hyper-induction without growth defects [7].
- Δ
- Conjugation Assay Protocol:
- Donor and recipient strains are grown to mid-exponential phase.
- Donors are exposed to sub-MIC levels of antibiotic (e.g., ½ MIC cefotaxime, mitomycin C) or left untreated.
- Donors and recipients are mixed at a specific ratio and incubated on filters.
- Cells are resuspended and plated on selective media to count transconjugants (recipients that received the plasmid) and donor/recipient controls.
- Conjugation frequency is calculated as transconjugants per recipient [7].
- Mutation Frequency Assay (Rifampicin Resistance):
- Multiple independent bacterial cultures are grown with and without sub-MIC antibiotics.
- Cultures are plated on agar containing rifampicin and on non-selective agar.
- Mutation frequency is calculated as the number of rifampicin-resistant colonies divided by the total viable count [60] [5].
- Data distribution is analyzed using fluctuation analysis (e.g., Luria-Delbrück) to distinguish between induced mutagenesis and selection of pre-existing mutants [5].
The Scientist's Toolkit: Essential Research Reagents
Table 3: Key Reagents for SOS Response and Inhibition Research
| Reagent / Tool | Function/Description | Application in Research |
|---|---|---|
| ΔrecA mutant strain | Isogenic strain lacking the master regulator RecA. | Serves as a genetic proxy for SOS inhibition to study SOS-dependent phenotypes [7] [5]. |
| LexA repressor mutants | Strains with non-cleavable (S119A) or hyper-cleavable (E86P) LexA. | Used to create constitutively inactive or active SOS states, respectively, to study regulon effects [7]. |
| SOS reporter fusions | Genetic fusions of SOS gene promoters (e.g., sulA, recN) to fluorescent proteins or luciferase. |
Allows quantitative, real-time measurement of SOS induction in response to antibiotics [7]. |
| Sub-MIC antibiotics | Antibiotics used at sub-inhibitory concentrations (e.g., ¼, ½ MIC). | Used to study stress-induced effects like SOS activation, mutagenesis, and horizontal gene transfer without killing the entire culture [7] [60]. |
| Class 1 integron-bearing plasmid | A mobile genetic element containing an integrase gene with a LexA-binding SOS box. | Used to study the role of the SOS response in catalyzing integrase-mediated cassette rearrangements and resistance gene acquisition/expression [61]. |
Discussion and Clinical Implications
The comparative analysis reveals that SOS inhibition is not a universally effective strategy against antibiotic resistance. Its utility is highly context-dependent, determined by the antibiotic class, the genetic background of the bacterium, and the specific resistance mechanism in play.
Therapeutic Potential and Limitations: Targeting the SOS response could be a potent adjuvant for fluoroquinolone therapy by reducing mutagenesis-driven resistance. However, for β-lactams, where resistance often arises through SOS-independent mechanisms like ROS-driven mutagenesis and selection, SOS inhibition may be ineffective or even counterproductive [5]. This underscores the necessity for a nuanced, mechanism-based approach to combination therapies.
Future Research Directions: Key unanswered questions include the identification of biomarkers that predict whether a bacterial infection will evolve resistance via SOS-dependent or independent routes. Furthermore, a deeper mechanistic understanding of the "repair-redox axis" [5]—the interplay between DNA repair systems and oxidative stress in
recA-deficient backgrounds—could reveal new targets for thwarting resistance across multiple antibiotic classes.
Inhibition of the SOS response presents a double-edged sword in the fight against antibiotic resistance. While it effectively suppresses resistance evolution following treatment with direct DNA-damaging antibiotics, it can unexpectedly facilitate resistance to cell-wall agents through alternative, stress-induced pathways. This comparative analysis underscores that successful therapeutic strategies must be tailored to the specific antibiotic and its corresponding bacterial stress response network. A one-size-fits-all approach to SOS inhibition is unlikely to succeed. Future efforts must focus on mapping the complex interplay between different antibiotic classes and bacterial survival pathways to develop intelligent combination therapies that preempt resistance evolution.
Validating SOS Suppression in Fluoroquinolone vs. β-Lactam Treatments
The bacterial SOS response is a conserved DNA repair network that is activated by antibiotic-induced genotoxic stress. Its role in promoting mutation rates and horizontal gene transfer has made it a promising target for suppressing the evolution of antimicrobial resistance (AMR) [62] [63]. The core regulatory mechanism involves the RecA protein, which, upon sensing DNA damage, facilitates the autocleavage of the LexA repressor, thereby derepressing dozens of genes involved in DNA repair, mutagenesis, and cell division [62] [63]. While the paradigm that SOS inhibition suppresses resistance is well-established for DNA-damaging antibiotics like fluoroquinolones, emerging research reveals a more complex relationship, particularly with cell-wall targeting β-lactams [5] [35]. This guide synthesizes current experimental data and protocols to validate SOS suppression strategies across these antibiotic classes, providing a technical framework for researchers and drug development professionals.
Core Concepts: Divergent Resistance Dynamics
Established Role in Fluoroquinolone Resistance
Fluoroquinolones directly cause DNA double-strand breaks by inhibiting DNA gyrase and topoisomerase IV, potently inducing the SOS response [62]. Consequently, inhibiting this response effectively hampers resistance development.
- Key Evidence: Deleting the
recAgene in E. coli significantly reduces the rate of resistance development to ciprofloxacin, enrofloxacin, and moxifloxacin [64]. The SOS response is crucial for the induction of error-prone DNA polymerases (Pol IV and Pol V), which increase mutagenesis and the probability of resistance-conferring mutations [62]. - Therapeutic Application: The small molecule OXF-077, an SOS response inhibitor, suppresses the evolution of ciprofloxacin resistance in MRSA and resensitizes resistant bacteria to the antibiotic [42].
Paradoxical Role in β-Lactam Resistance
Unexpectedly, SOS suppression does not universally impede resistance evolution. Studies in E. coli show that ΔrecA mutants can develop stable, multi-drug resistance to ampicillin after a single 8-hour exposure—a 20-fold MIC increase occurring 2-3 days faster than in wild-type strains [5] [35].
- Proposed Mechanism: This SOS-independent pathway involves a two-step evolutionary process:
- Increased Mutational Supply: RecA deficiency impairs DNA repair and downregulates base excision repair and antioxidative defence genes, leading to excessive accumulation of reactive oxygen species (ROS) and elevated mutation rates [5] [35].
- Antibiotic-Driven Selection: Ampicillin treatment selectively enriches rare, pre-existing resistant mutants from this genetically unstable population [5] [35].
- Key Distinction: Complementation with a functional
recAplasmid restores ampicillin sensitivity, confirming the phenomenon is directly linked to RecA loss and not a general fitness cost [5].
Table 1: Comparative Summary of SOS Suppression Effects
| Feature | Fluoroquinolones (e.g., Ciprofloxacin) | β-Lactams (e.g., Ampicillin) |
|---|---|---|
| Primary Drug Target | DNA gyrase/Topoisomerase IV [62] | Penicillin-Binding Proteins (cell wall synthesis) [53] |
| SOS Induction | Direct, via DNA damage [62] | Indirect, via impaired cell wall synthesis [5] |
Effect of recA Deletion on Resistance Evolution |
Impairs or delays resistance [65] [64] | Accelerates resistance (SOS-independent pathway) [5] [35] |
| Key Resistance Mutations | gyrA, gyrB, parC, parE [64] |
P<sub>ampC</sub>, ftsI (PBP3), acrB [66] |
| Role of ROS | Contributes to SOS induction and mutagenesis [62] | Central to mutagenesis in ΔrecA background [5] [35] |
Experimental Validation Protocols
Validating SOS Suppression in Fluoroquinolone Treatments
Objective: To confirm that SOS suppression slows the development of fluoroquinolone resistance.
Protocol:
- Strains and Culture:
Experimental Evolution:
- Subject all strains to serial passaging in sub-MIC concentrations of the target fluoroquinolone (e.g., ciprofloxacin, enrofloxacin) [64].
- Daily, inoculate fresh medium containing an antibiotic concentration typically set at 2-4x the MIC of the previous day's culture. Monitor growth for 24-hour periods.
- Continue this for a set number of transfers (e.g., 14-30 cycles) or until a predefined resistance breakpoint is reached [64].
Analysis and Endpoints:
- Phenotypic Monitoring: Determine the MIC of evolved populations every few transfers against the selecting antibiotic and other classes to check for multi-drug resistance.
- Genetic Validation: Sequence whole genomes of endpoint populations and isolated clones. Analyze for mutations in known resistance loci (e.g.,
gyrA,parC) and compare the mutational spectra and rates between wild-type andΔrecAstrains [64].
The following workflow outlines the key steps for validating SOS suppression in fluoroquinolone treatments:
Investigating SOS-Independent β-Lactam Resistance
Objective: To characterize the rapid, SOS-independent evolution of β-lactam resistance in ΔrecA mutants.
Protocol:
- Single Exposure and Isolation:
Stability Assessment:
- Passage the resistant isolates in antibiotic-free medium for 7-10 days.
- Periodically check the MIC of ampicillin to determine if resistance is stable [5].
Mechanistic Profiling:
- ROS Quantification: Use a fluorescent probe like H2DCFDA to measure intracellular ROS levels in treated and untreated
ΔrecAcells versus wild-type controls [5] [35]. - Mutation Rate Analysis: Perform a fluctuation test. Inoculate multiple (e.g., 96) independent cultures, grow them, and plate on rifampicin-containing plates to count rifampicin-resistant mutants. Calculate mutation rates using maximum likelihood estimation [5].
- Transcriptomics: Conduct RNA-seq on
ΔrecAresistant isolates to analyze differential expression of DNA repair and antioxidant defence genes compared to the wild-type [35] [66].
- ROS Quantification: Use a fluorescent probe like H2DCFDA to measure intracellular ROS levels in treated and untreated
The pathway below illustrates the proposed mechanism for SOS-independent β-lactam resistance:
The Scientist's Toolkit: Essential Research Reagents
Table 2: Key Reagents for SOS and Resistance Studies
| Reagent / Tool | Function / Application | Example Use Case |
|---|---|---|
ΔrecA Mutant Strains |
Isogenic host deficient in SOS response activation; essential control. | Comparing resistance evolution between WT and SOS-deficient backgrounds [5] [64]. |
| Complementation Plasmid | Plasmid carrying functional recA gene; confirms phenotype is due to recA loss. |
Restoring SOS function to validate target specificity [5]. |
| SOS Inhibitor (e.g., OXF-077) | Small molecule that suppresses the SOS response. | Co-administration with antibiotics to assess resistance suppression [42]. |
| Fluorescent ROS Probe (e.g., H₂DCFDA) | Detects and quantifies intracellular reactive oxygen species. | Measuring oxidative stress in ΔrecA mutants under antibiotic pressure [5] [35]. |
| RNA-seq Kits | For whole transcriptome analysis of bacterial cultures. | Profiling gene expression changes in DNA repair and antioxidant pathways [35] [66]. |
Discussion and Research Outlook
The divergent effects of SOS suppression underscore that the relationship between DNA damage, stress responses, and resistance evolution is antibiotic-class specific. Targeting the SOS response remains a potent strategy for fluoroquinolones but may have unintended consequences for β-lactam treatments. Future research should focus on several key areas, including the clinical relevance of the ROS-driven resistance pathway in pathogenic bacteria beyond E. coli, and the development of combination therapies that simultaneously target the SOS response and mitigate oxidative stress. Furthermore, high-throughput screening for compounds that disrupt the "repair-redox axis" could identify novel anti-evolvability drugs. A nuanced, mechanism-based understanding is paramount for designing the next generation of antimicrobial adjuvants.
The escalating crisis of antimicrobial resistance represents one of the most significant challenges to global public health in the 21st century [67]. As bacteria continue to evolve mechanisms to withstand antibiotic pressure, understanding the evolutionary trade-offs between resistance acquisition and bacterial fitness becomes paramount for developing novel therapeutic strategies. This technical guide examines the fundamental relationship between resistance costs and compensatory mutations, with specific emphasis on the SOS response system as a central regulator of bacterial adaptation.
The SOS response, an inducible DNA repair system, serves as a critical pathway for bacterial survival under antibiotic-induced stress [18] [6]. While this system enables DNA damage repair, it simultaneously promotes genetic diversity, hypermutation, and horizontal gene transfer—processes that accelerate the development of antibiotic resistance [18] [6]. However, these advantages often come with inherent fitness costs that shape evolutionary trajectories through compensatory mutations [68]. This complex interplay represents a crucial frontier in antimicrobial research, offering potential targets for adjuvant therapies aimed at curtailing resistance development.
The SOS Response: Core Pathway and Antibiotic Resistance Implications
Molecular Mechanisms of SOS Activation
The SOS response constitutes a sophisticated DNA damage repair system controlled primarily by the LexA repressor and RecA inducer proteins [18] [6]. Under normal conditions, LexA binds to SOS operator sites, repressing the transcription of more than 50 genes involved in DNA repair [18]. When DNA damage occurs, single-stranded DNA (ssDNA) fragments accumulate, prompting RecA polymerization onto these segments and forming nucleoprotein filaments [18]. This activated RecA* complex facilitates LexA autocleavage, derepressing the SOS regulon and initiating a coordinated DNA repair cascade [18] [6].
The temporal regulation of SOS activation ensures appropriate response kinetics: initial induction of high-fidelity repair mechanisms precedes error-prone translesion DNA synthesis mediated by specialized polymerases (PolII, PolIV, and PolV) [18]. These low-fidelity polymerases enable replication past irreparable DNA lesions but introduce mutations that contribute to genetic diversification and resistance development [18].
Figure 1: SOS Response Pathway Activation and Consequences. The diagram illustrates the sequential molecular events following antibiotic-induced DNA damage, culminating in both DNA repair and potential resistance development through error-prone repair mechanisms.
SOS-Inducing Antibiotic Agents
Multiple antibiotic classes trigger SOS activation through direct or indirect DNA damage:
- Fluoroquinolones: Directly cause DNA double-strand breaks by inhibiting DNA gyrase and topoisomerase IV [69] [18]
- β-lactams: Indirectly induce SOS via the DpiBA two-component system that responds to cell wall stress [6] [70]
- Aminoglycosides: Generate reactive oxygen species (ROS) that cause oxidative DNA damage [67] [6]
Beyond antibiotics, numerous other pharmaceuticals including anticancer drugs, antivirals, and antidepressants demonstrate SOS-inducing capabilities, highlighting the broad exposure potential in clinical settings [71].
Quantifying Fitness Costs of Resistance Mechanisms
Plasmid-Mediated Resistance Costs
Horizontal gene transfer via plasmids represents a primary route for antibiotic resistance dissemination, but imposes significant fitness burdens on bacterial hosts [68] [72]. The molecular mechanisms underlying these costs extend beyond simple metabolic burden to encompass specific genetic conflicts.
Table 1: Fitness Costs Associated with Plasmid Carriage
| Cost Category | Molecular Mechanism | Experimental Evidence | Impact on Growth Rate |
|---|---|---|---|
| Specific Genetic Conflicts | Plasmid-induced SOS activation leading to prophage expression and toxin production [68] [72] | P. fluorescens with pQBR103/pQBR57 plasmids showed tailocin-mediated toxicity [68] | 15-25% reduction [68] |
| Metabolic Burden | Resource diversion for plasmid replication, maintenance, and gene expression [68] | Analysis of plasmid size, copy number, and gene expression effects [68] | Variable (dose-dependent) [68] |
| Membrane Disruption | Conjugative pilus expression compromising membrane integrity [68] | Increased phage susceptibility and osmosensitivity [68] | 10-20% reduction [68] |
Chromosomal Mutation Fitness Costs
Chromosomal resistance mutations frequently impair essential cellular functions, creating selective pressure for compensatory evolution:
Table 2: Fitness Costs of Chromosomal Resistance Mutations
| Resistance Mechanism | Associated Cost | Compensatory Pathway | Experimental System |
|---|---|---|---|
| Target Modification | Reduced enzymatic efficiency or substrate binding affinity [67] | Second-site suppressor mutations [67] | E. coli rpoB mutations (rifampicin resistance) [67] |
| Membrane Transport | Impaired nutrient uptake or disrupted proton motive force [67] | Regulatory adjustments to transport systems [67] | Porin mutations in Gram-negative bacteria [67] |
| SOS Hyperactivation | Energy diversion, cell filamentation, reduced replication [18] [6] | Modulation of RecA/LexA regulation [18] | E. coli under fluoroquinolone exposure [18] |
Compensatory Mutations: Molecular Mechanisms and Experimental Evidence
Plasmid-Host Compensation Pathways
Compensatory evolution rapidly ameliorates plasmid-associated fitness costs through specific genetic solutions:
Figure 2: Plasmid Compensation Pathways. Genetic conflicts following plasmid acquisition can be resolved through mutations occurring on either the bacterial chromosome or the plasmid itself, restoring bacterial fitness.
Experimental evolution studies in Pseudomonas fluorescens demonstrated that single mutations could completely overcome the fitness costs of large plasmids (pQBR103, 425 kb; pQBR57, 307 kb) [68]. Chromosomal mutations targeted the gacA/S global regulatory system or the hypothetical protein PFLU4242, while plasmid-based compensation occurred through mutations in a lambda repressor-like protein (PQBR57_0059) [68]. These findings indicate that specific genetic conflicts, rather than general metabolic burden, primarily drive plasmid fitness costs.
SOS-Independent Resistance Evolution
Paradoxically, RecA deletion can accelerate resistance development under certain conditions, revealing complex evolutionary trade-offs:
Recent investigations demonstrate that E. coli ΔrecA mutants develop β-lactam resistance 20-fold faster than wild-type strains following single-dose ampicillin exposure [70]. This SOS-independent pathway involves:
- Hindrance of DNA repair pathways
- Transcriptional repression of antioxidative response genes
- Excessive ROS accumulation promoting mutagenesis
- Stable, heritable resistance mutations in genes including PampC, ftsI, and acrB [70]
This phenomenon illustrates the multifactorial nature of resistance evolution and highlights how compensatory mechanisms can exploit alternative genetic routes when primary pathways are compromised.
Experimental Approaches and Methodologies
Assessing SOS-Mediated Resistance Costs
Protocol 1: SOS Activation Kinetics Under Antibiotic Stress
- Bacterial Strains: Wild-type vs. ΔrecA or ΔlexA mutants (isogenic backgrounds) [11]
- Antibiotic Exposure:
- SOS Activity Measurement:
- Fitness Assessment:
Protocol 2: Compensatory Mutation Selection and Identification
- Experimental Evolution Design:
- Compensated Strain Identification:
- Mutation Mapping:
The Scientist's Toolkit: Essential Research Reagents
Table 3: Key Reagents for Resistance Trade-off Studies
| Reagent Category | Specific Examples | Application/Function | Experimental Context |
|---|---|---|---|
| SOS Reporters | PrecA-gfp fusion constructs [71] | Quantitative SOS induction kinetics | Real-time monitoring of DNA damage response [71] |
| Genetic Tools | pKOBEG plasmid (Red recombinase) [11] | Targeted gene inactivation | Construction of isogenic mutants (ΔrecA, ΔfumC, ΔaidB) [11] |
| SOS Inhibitors | Zinc salts, nitric oxide donors, dequalinium [71] | RecA filamentation blockade | SOS pathway inhibition studies [71] |
| Antibiotic Classes | Ciprofloxacin, ampicillin, mitomycin C [11] [71] | SOS response induction | DNA damage generation and resistance selection [11] [71] |
| Molecular Assays | Qubit Flex fluorometry, SybrSafe DNA stain [71] | Nucleic acid quantification and visualization | Extracellular DNA release measurement [71] |
Research Implications and Therapeutic Applications
SOS-Targeted Adjuvant Strategies
Inhibiting the SOS response presents a promising approach for enhancing antibiotic efficacy and reducing resistance emergence:
- Zinc salts and nitric oxide donors: Prevent RecA binding to ssDNA, blocking SOS initiation [71] [6]
- Dequalinium: Suppresses σs-mediated general stress response, indirectly modulating SOS activation [71]
- Suramin: Interacts with RecA to inhibit SOS induction through ATP competition [6]
- p-Coumaric acid: Disrupts RecA filament formation and LexA autoproteolysis [6]
Combining SOS inhibitors with conventional antibiotics significantly enhances susceptibility in multidrug-resistant pathogens, including E. coli, P. aeruginosa, and K. pneumoniae [71] [6]. For instance, zinc salts reduce ciprofloxacin MIC by 4-8 fold in SOS-hyperinducing strains [71].
Evolutionary-Based Treatment Approaches
Understanding resistance trade-offs enables novel therapeutic strategies:
- Collateral sensitivity cycling: Exploiting evolutionary trade-offs where resistance to one drug increases susceptibility to another [67]
- Plasmid curing therapies: Utilizing plasmid fitness costs to selectively target resistant strains [68] [72]
- Anti-evolution drugs: Compounds specifically targeting mutagenesis pathways like SOS-induced hypermutation [18] [6]
The evolutionary trade-offs between antibiotic resistance acquisition and bacterial fitness costs represent a dynamic battlefield with profound implications for antimicrobial therapy. The SOS response stands as a central regulator in this balance, simultaneously enabling bacterial survival under antibiotic stress while creating vulnerabilities through fitness burdens and compensatory requirements. The precise molecular mechanisms underlying these trade-offs—from specific genetic conflicts in plasmid-host interactions to SOS-mediated hypermutation—provide promising targets for next-generation antimicrobial adjuvants.
Future research directions should focus on mapping the complete network of genetic interactions governing resistance costs, developing high-throughput methods to quantify evolutionary trade-offs in clinical isolates, and translating mechanistic insights into combination therapies that exploit bacterial evolutionary vulnerabilities. As the resistance crisis intensifies, leveraging these fundamental evolutionary principles may prove essential for extending the utility of our existing antibiotic arsenal and managing treatment failures in clinical settings.
In Vivo Model Validation of SOS-Targeted Anti-Resistance Strategies
The bacterial SOS response, a conserved DNA repair network, is a promising therapeutic target for curbing the evolution of antibiotic resistance. While in vitro studies have firmly established that SOS inhibition can suppress resistance emergence, validation in physiologically relevant in vivo models is a critical step in translating these findings. This whitepaper synthesizes current evidence on in vivo model validation for SOS-targeted strategies, highlighting the use of a rabbit model of intestinal infection to demonstrate that SOS-inducing antibiotics trigger a mutator phenotype in vivo, and that this effect can be mitigated by co-administration of zinc. The document provides a detailed experimental framework for in vivo validation, including protocols, key reagents, and data analysis techniques, serving as a technical guide for researchers aiming to advance anti-evolution strategies toward clinical application.
The SOS response is a conserved bacterial stress response activated by DNA damage, often induced by antibiotic treatment. This pathway, regulated by the RecA and LexA proteins, controls over 40 genes involved in DNA repair, error-prone translesion synthesis, and horizontal gene transfer. The induction of this response facilitates the acquisition of resistance mutations and the dissemination of resistance genes, making it a compelling target for anti-resistance strategies [22]. The core premise is that by inhibiting the SOS response, the mutation rate and genetic adaptability of bacteria under antibiotic pressure can be reduced, thereby preserving the efficacy of existing antibiotics.
Most foundational research on SOS-mediated resistance has been conducted in vitro. These studies have demonstrated that SOS-inducing antibiotics like ciprofloxacin promote a "mutator phenotype" or hypermutation, increasing the acquisition of resistance to multiple antibiotic classes [73]. Furthermore, genetic disruption of the recA gene, the master regulator of the SOS response, has been shown to sensitize bacteria to antibiotics and reduce resistance development in laboratory strains [29]. However, the in vivo environment presents complex challenges, including host immune factors, tissue-specific microenvironments, and population dynamics, which can significantly alter bacterial behavior. Therefore, validation in a living host is an indispensable step in evaluating the therapeutic potential of SOS-targeted strategies.
Core In Vivo Evidence and Quantitative Data
The transition from in vitro concepts to in vivo validation is exemplified by a key study that quantified the effects of SOS-inducing drugs in a live animal model [73]. This research provided critical proof-of-concept that the SOS response can be targeted to reduce resistance evolution in an infected host.
Crane et al. (2021) used a rabbit model of intestinal infection with enteropathogenic Escherichia coli (EPEC) strain E22. The investigators demonstrated that antibiotics known to induce the SOS response in vitro (ciprofloxacin and zidovudine) also triggered the mutator phenotype in vivo. This was measured by a significant increase in the emergence of antibiotic-resistant E. coli to three unrelated antibiotics: rifampin, minocycline, and fosfomycin. Crucially, the study showed that co-administration of zinc was able to inhibit the SOS response and consequently reduce the emergence of antibiotic resistance in the infected rabbits [73]. Zinc acts as a potent inhibitor of RecA protein function, specifically by blocking its ATPase activity and preventing the filamentation on single-stranded DNA that is required for LexA repressor cleavage [22].
Table 1: Quantitative Data from Key In Vivo Validation Study
| Experimental Variable | Model System | Pathogen | Key Measured Outcome | Result |
|---|---|---|---|---|
| Ciprofloxacin exposure | Rabbit intestinal infection | Enteropathogenic E. coli E22 | Emergence of resistance to rifampin, minocycline, fosfomycin | Increased resistance emergence [73] |
| Zidovudine exposure | Rabbit intestinal infection | Enteropathogenic E. coli E22 | Emergence of resistance to rifampin, minocycline, fosfomycin | Increased resistance emergence [73] |
| Zinc co-administration | Rabbit intestinal infection | Enteropathogenic E. coli E22 | SOS-induced emergence of antibiotic resistance | Inhibition of resistance emergence [73] |
This body of work validates two critical points for the field: first, that the SOS-mediated resistance phenomenon is relevant in a live host, and second, that pharmacological inhibition of the SOS response in this setting is a viable strategy to slow resistance evolution.
Detailed Experimental Protocol for In Vivo Validation
This section outlines a comprehensive methodology for validating SOS-targeted anti-resistance strategies in an animal model, based on established approaches and incorporating best practices.
Animal Model and Infection Setup
- Animal Species: New Zealand White rabbits.
- Infection Model: Intestinal infection model. Rabbits are inoculated with a standardized inoculum (e.g., 10^8 CFU) of a well-characterized bacterial strain, such as enteropathogenic E. coli (EPEC) strain E22, via oral gavage [73].
- Justification: The rabbit model for EPEC closely mimics human intestinal disease, providing a relevant niche for studying bacterial evolution under antibiotic pressure.
Experimental Groups and Dosing
Animals should be randomly assigned into several experimental groups to allow for direct comparisons:
- Infected, untreated control: Receives vehicle only.
- SOS-inducing antibiotic: Treated with an antibiotic like ciprofloxacin.
- SOS inhibitor + SOS-inducing antibiotic: Treated with both the SOS-inducing antibiotic and the SOS inhibitor (e.g., zinc).
- SOS inhibitor alone: To assess the compound's impact on bacterial load and host health in the absence of antibiotic treatment.
Dosing should be determined based on prior pharmacokinetic/pharmacodynamic (PK/PD) studies to achieve clinically relevant drug exposures at the site of infection.
Sample Collection and Analysis
- Sample Collection: At defined timepoints post-treatment (e.g., daily), fecal samples or intestinal contents are collected.
- Bacterial Enumeration: Serial dilution and plating of samples to determine the total bacterial load.
- Resistance Frequency Analysis: To quantify the emergence of resistance, sample aliquots are plated on agar containing a target antibiotic (e.g., rifampin, minocycline, fosfomycin) at a pre-defined concentration (e.g., 4x MIC). The frequency of resistance is calculated as the number of CFU on the antibiotic plate divided by the total CFU on the non-selective plate [73].
- Whole-Genome Sequencing: Isolated resistant colonies should be subjected to whole-genome sequencing to confirm that resistance is due to mutation and not contamination, and to identify the genetic basis of resistance [29].
The following diagram illustrates the core mechanism of the SOS response and the logical pathway for its inhibition, which is the focus of the in vivo validation strategies discussed in this protocol.
The Scientist's Toolkit: Research Reagent Solutions
Successfully conducting in vivo validation requires a suite of well-characterized reagents and tools. The table below details essential materials for these experiments.
Table 2: Key Research Reagents for In Vivo SOS Response Studies
| Reagent / Tool | Function / Purpose | Example & Notes |
|---|---|---|
| SOS-Inducing Antibiotic | To create DNA damage and activate the SOS response in the target pathogen. | Ciprofloxacin (fluoroquinolone) [73]. Zidovudine (nucleoside analogue) is also used [73]. |
| SOS Pathway Inhibitor | To pharmacologically block the SOS response and test the anti-evolution strategy. | Zinc acetate (inhibits RecA filamentation and ATPase activity) [73] [22]. |
| Isogenic recA Mutant Strain | Control to confirm SOS-dependence of observed effects; provides genetic validation of pharmacological inhibition. | E. coli with recA gene knockout (e.g., JW2669-1 from CGSC) [13] [5]. |
| Selective Agar Plates | To quantify the frequency of resistant mutants emerging in vivo. | Mueller-Hinton Agar supplemented with a target antibiotic (e.g., Rifampin at 4x MIC) [73]. |
| Clinical Isolate Panel | To assess the strategy's efficacy across diverse, clinically relevant genetic backgrounds. | Panels of E. coli clinical isolates, including high-risk clones (e.g., ST131) with varying resistance phenotypes [29]. |
Critical Considerations and Future Directions
While the validation of SOS inhibition in vivo is promising, several complexities must be addressed in future research.
Strain-Dependent Variability: Proteomic studies have revealed that suppression of the SOS response (via
recAdeletion) leads to extensive, strain-dependent changes in protein expression in clinical isolates of E. coli [29]. This suggests that the physiological consequences of SOS inhibition can vary significantly across different bacterial strains, which may impact the efficacy and off-target effects of SOS-targeted therapies.SOS-Independent Resistance Pathways: Research has uncovered that rapid evolution of multi-drug resistance can occur through SOS-independent mechanisms. In E. coli lacking
recA, β-lactam resistance emerged rapidly due to a compromised DNA repair system and an accumulation of reactive oxygen species (ROS), which increased the mutational supply [13] [5]. This highlights a potential limitation of targeting only the SOS pathway and suggests that combination strategies may be necessary to fully suppress resistance evolution.In Vivo Workflow and Translational Gaps: The overall workflow for transitioning an SOS-targeted strategy from concept to in vivo validation involves multiple stages, as summarized below. A major translational gap is the need for more potent and specific small-molecule RecA/LexA inhibitors suitable for clinical use.
Future work should focus on identifying and optimizing more potent SOS inhibitors, testing these strategies in a wider range of infection models (e.g., pneumonia, sepsis), and exploring combinations with antibiotics that have low metabolic dependencies to preempt the evolution of both tolerance and resistance [74].
Benchmarking SOS Inhibitors Against Conventional Antimicrobial Stewardship
The global antimicrobial resistance (AMR) crisis is exacerbated by the ability of bacteria to rapidly evolve resistance mechanisms, rendering treatments ineffective. Forecasts estimate that upwards of 169 million global deaths will be associated with AMR between 2025 and 2050 [75]. While conventional antimicrobial stewardship programs (ASPs) focus on optimizing antibiotic use to reduce resistance selection, they primarily address exogenous factors without targeting the fundamental molecular pathways that drive resistance evolution within the bacterial cell.
The SOS response represents a conserved bacterial stress response pathway activated by DNA damage, often triggered by antibiotic exposure. This pathway coordinates DNA repair but also induces error-prone DNA polymerases that increase mutation rates—a phenomenon termed "hypermutation" [2] [22]. Crucially, this mutator phenotype accelerates the acquisition of resistance mutations and facilitates horizontal gene transfer, serving as a key engine for resistance development [6]. Targeting the SOS response with inhibitory compounds thus presents a novel therapeutic strategy that could complement traditional stewardship approaches by addressing the intrinsic molecular mechanisms of resistance evolution.
This review provides a technical benchmark comparing emerging SOS inhibition strategies against conventional ASP frameworks, evaluating their potential synergy for combating multi-drug resistant pathogens.
The SOS Response: Molecular Mechanisms and Role in Resistance
Core Pathway Mechanics
The SOS response is a conserved DNA damage response pathway in bacteria, primarily regulated by the RecA-LexA interaction [22] [6]. Under normal conditions, the LexA repressor protein binds to SOS promoter sequences (SOS boxes), suppressing the expression of approximately 40 genes involved in DNA repair. DNA damage leads to single-stranded DNA (ssDNA) formation, which activates RecA nucleoprotein filaments. Activated RecA facilitates LexA autocleavage, derepressing the SOS regulon [22].
Induced genes include those encoding nucleotide excision repair proteins, homologous recombination factors, and error-prone translesion synthesis (TLS) DNA polymerases (Pol IV and Pol V). These TLS polymerases replicate damaged DNA with reduced fidelity, directly contributing to the hypermutation that generates antibiotic resistance mutations [2] [22].
Resistance Mechanisms Facilitated by SOS Activation
SOS response activation promotes antibiotic resistance through multiple molecular mechanisms:
Hypermutation and Mutator Phenotype: Induction of error-prone DNA polymerases (Pol IV and V) increases mutation rates by 10- to 100-fold, accelerating the emergence of de novo resistance mutations [2] [22]. In vivo studies demonstrate that SOS-inducing drugs like ciprofloxacin increase resistance frequencies to unrelated antibiotics including rifampin, minocycline, and fosfomycin [2].
Horizontal Gene Transfer: SOS activation promotes conjugation, transformation, and transduction efficiency. The RecA-LEXA system regulates integron cassette shuffling and natural competence in some species, facilitating the acquisition of pre-evolved resistance genes [6].
Biofilm Formation and Persistence: SOS response induction enhances biofilm formation and promotes the generation of persister cells—metabolically dormant variants that exhibit multidrug tolerance and contribute to chronic infections [6].
Direct Resistance Gene Expression: Some resistance determinants are directly regulated by LexA cleavage. For example, the expression of certain antibiotic-inactivating enzymes and efflux pump components can be upregulated during SOS induction [6].
Conventional Antimicrobial Stewardship: Frameworks and Limitations
Quantitative and Qualitative Evaluation Methods
ASP effectiveness relies on standardized metrics for monitoring antibiotic consumption and prescribing quality as shown in Table 1 [76].
Table 1: Antimicrobial Use Evaluation Metrics in Stewardship Programs
| Metric Category | Specific Measures | Implementation Examples | Limitations |
|---|---|---|---|
| Quantitative Use Metrics | Defined Daily Dose (DDD); Days of Therapy (DOT) | WHO AWaRe classification; CDC SAAR | DDD inaccurate in renal impairment/pediatric patients; DOT requires patient-level data |
| Qualitative Use Assessment | Guideline adherence; Appropriate indication/duration/therapy de-escalation | Prospective audit with feedback; Pre-authorization requirements | Resource-intensive; Inter-institutional variability in standards |
| Antibiotic Spectrum Optimization | AWaRe category consumption (Access vs. Watch vs. Reserve) | Formulary restrictions; Automatic conversion pathways | Does not address molecular resistance mechanisms |
Limitations of Conventional Stewardship
While ASPs reduce inappropriate antibiotic selection and duration, they face fundamental limitations:
Reactive Rather Than Proactive: ASPs primarily address resistance after emergence through antibiotic optimization, without preventing the genetic evolution driving resistance [76].
Incomplete Resistance Prevention: Even optimal antibiotic use cannot prevent SOS-mediated hypermutation induced by non-antibiotic SOS inducers (e.g., antiviral drugs, antidepressants, herbicides) [77].
Narrow Mechanistic Scope: Traditional stewardship focuses on antibiotic-bacteria interaction without targeting bacterial stress responses that accelerate resistance evolution [6].
SOS Inhibition as a Novel Therapeutic Strategy
Molecular Targets and Inhibitor Compounds
SOS pathway inhibition targets key regulatory nodes to block hypermutation and resistance gene transfer while potentially enhancing antibiotic efficacy. Major targets and their inhibitors are summarized in Table 2 [22] [6].
Table 2: SOS Response Inhibitor Targets and Experimental Compounds
| Target Protein | Inhibitor Compounds | Mechanism of Action | Experimental Evidence |
|---|---|---|---|
| RecA | Zinc acetate, Suramin, Peptide inhibitors (e.g., 4E1) | Disassembles RecA-ssDNA filaments; Inhibits ATPase activity; Blocks LexA cleavage | Zinc blocked SOS-induced resistance in rabbit infection model [2]; Suramin inhibits RecA-mediated strand exchange [6] |
| LexA | Boron-containing compounds, 5-amino-1-(carbamoylmethyl)-1H-1,2,3-triazole-4-carboxamide | Inhibits LexA autoproteolysis; Maintains SOS repression | Identified through high-throughput screening; Limited in vivo data [22] |
| SSB Protein | Small molecules (under characterization) | Disrupts SSB protein-protein interactions | Early research stage; disrupts replication and recombination [22] |
| Pol V (UmuDâ‚‚C) | RecA mutant proteins (e.g., RecAD112R/N113R) | Interferes with Mutasome formation | Reduces SOS mutagenesis in E. coli [22] |
Experimental Validation of SOS Inhibition
In Vitro and In Vivo Efficacy
SOS inhibitors demonstrate significant potential in experimental models:
Zinc Acetate Efficacy: In a rabbit intestinal infection model with enteropathogenic E. coli, co-administration of zinc acetate inhibited ciprofloxacin-induced SOS response, reducing resistance emergence to rifampin, minocycline, and fosfomycin. Zinc specifically blocked the mutator phenotype without general antibacterial effects [2].
Synergistic Antibiotic Enhancement: Combined inactivation of SOS response (recA deletion) with metabolic pathway disruption (fumarase fumC deletion) significantly increased susceptibility to cephalosporins and quinolones in E. coli laboratory and clinical strains, demonstrating the potential of dual-pathway targeting [11].
RecA Inhibition Specificity: The anti-trypanosomal drug suramin inhibits three discrete RecA activities: ssDNA binding, ATP hydrolysis, and strand exchange. This multi-mechanistic inhibition effectively blocks SOS induction [6].
Diagnostic Applications
Beyond therapeutic applications, SOS response components serve as biomarkers for rapid antimicrobial susceptibility testing. Relative quantification of recA gene expression after ciprofloxacin exposure accurately distinguishes susceptible from resistant strains of Y. pestis, B. anthracis, and ESKAPE pathogens within 15-60 minutes—significantly faster than conventional growth-based methods [78].
Experimental Protocols for SOS Inhibition Research
Hypermutation Frequency Assay
Purpose: Quantify SOS-induced mutator phenotype and inhibitor efficacy [2].
Methodology:
- Grow bacterial cultures (e.g., E. coli E22) with sub-MIC concentrations of SOS-inducing antibiotic (ciprofloxacin at 0.1 µg/mL) ± SOS inhibitor (zinc acetate at 0.3 mM)
- Plate serial dilutions on non-selective media for total CFU count and antibiotic-containing media (rifampin at 100 µg/mL or minocycline at 10-12 µg/mL)
- Incubate plates (24h for rifampin; 48h for minocycline)
- Calculate resistance frequency = (CFU on antibiotic plate)/(total CFU)
Validation: Effective SOS inhibitors reduce resistance frequency by ≥10-fold compared to inducer-only controls [2].
RecA-LexA Interaction Reporter Assay
Purpose: Monitor SOS pathway activation and inhibition using transcriptional fusions [77].
Methodology:
- Utilize E. coli reporter strain (e.g., JLM281) with recA or other SOS gene promoter fused to lacZ
- Expose to SOS inducers (zidovudine, bleomycin, ciprofloxacin) ± inhibitors
- Measure β-galactosidase activity colorimetrically
- Calculate induction ratio relative to untreated controls
Applications: Compound screening; ICâ‚…â‚€ determination for SOS inhibitors [77].
In Vivo Intestinal Loop Model
Purpose: Evaluate SOS inhibitor efficacy in physiologically relevant environment [2].
Methodology:
- Rabbit intestinal ligated loop model infected with enteropathogenic E. coli
- Direct injection of SOS inducer (ciprofloxacin, zidovudine) ± inhibitor (zinc acetate) into loops
- After 18-24h, collect intestinal fluid and bacteria
- Plate serial dilutions on selective antibiotics to quantify resistance frequency
- Compare treatment groups to untreated control loops
Advantages: Models human gastrointestinal infections where resistance frequently emerges [2].
Comparative Analysis: SOS Inhibition vs. Conventional Stewardship
The table below benchmarks SOS inhibition against conventional ASP approaches across key parameters.
Table 3: Benchmarking SOS Inhibition Against Conventional Stewardship
| Parameter | Conventional Stewardship | SOS Inhibition | Potential Synergy |
|---|---|---|---|
| Primary Mechanism | Optimize antibiotic selection, dosing, duration | Block bacterial stress response, hypermutation, HGT | Stewardship reduces selective pressure; inhibitors block genetic adaptation |
| Resistance Prevention | Manages existing resistance | Prevents de novo resistance emergence | Comprehensive resistance management |
| Therapeutic Index | N/A (administrative/procedural) | Requires demonstration of selectivity over host pathways | Adjuvant approach enhances existing antibiotics |
| Implementation Level | Institutional/population level | Individual patient/pathogen level | Multi-level intervention strategy |
| Development Stage | Clinically implemented, guidelines established | Preclinical research, candidate optimization | Near-term: biomarker applications; Long-term: combination therapies |
The Scientist's Toolkit: Essential Research Reagents
Table 4: Key Reagents for SOS Response Research
| Reagent Category | Specific Examples | Research Application | Key Features |
|---|---|---|---|
| SOS-Inducing Compounds | Ciprofloxacin, Mitomycin C, Zidovudine, Bleomycin | Positive controls for SOS activation; Hyper-mutation assays | DNA damage via distinct mechanisms; Titratable induction levels |
| SOS Reporter Strains | E. coli JLM281 (recA-lacZ), GFP transcriptional fusions | Quantifying SOS pathway activation; Inhibitor screening | Sensitive, quantitative readout; Compatible with high-throughput formats |
| SOS Inhibitors | Zinc acetate, Suramin, LexA autoproteolysis inhibitors | Mechanism of action studies; Combination therapy testing | Various targets (RecA, LexA); Different chemical scaffolds |
| Genetic Tools | recA knockout strains (e.g., JW2669-1), Complementation plasmids | Establishing SOS-deficient backgrounds; Genetic rescue experiments | Clear phenotypic comparisons; Controlled genetic background |
| Animal Models | Rabbit intestinal loop infection, Mouse systemic infection models | In vivo efficacy assessment; Pharmacokinetic studies | Physiologically relevant environments; Host-pathogen interactions |
SOS response inhibition represents a paradigm-shifting approach that addresses the molecular drivers of antibiotic resistance evolution. While conventional antimicrobial stewardship remains essential for optimizing antibiotic use and reducing selective pressure, it cannot prevent the genetic adaptations facilitated by bacterial stress responses. SOS inhibitors provide a targeted strategy to suppress hypermutation and horizontal gene transfer—complementing existing stewardship frameworks.
The experimental evidence for SOS inhibition continues to accumulate, from zinc-mediated blockade of resistance emergence in animal models to diagnostic applications using recA expression as a rapid susceptibility biomarker. Future therapeutic development should focus on optimizing the selectivity and pharmacokinetics of SOS inhibitory compounds, particularly for use as antibiotic adjuvants. Combining molecular inhibition of resistance evolution with conventional stewardship principles offers a comprehensive strategy to address the multifaceted challenge of antimicrobial resistance, potentially extending the clinical lifespan of existing antibiotics while mitigating the emergence of future resistance.
Conclusion
The bacterial SOS response represents a double-edged sword, serving as a crucial DNA damage response system while simultaneously accelerating the evolution of antibiotic resistance. Key takeaways reveal that while SOS induction promotes mutagenesis, tolerance, and resistance gene dissemination, its complete inhibition may trigger alternative resistance pathways through ROS accumulation and impaired DNA repair. The relationship is highly context-dependent, varying by antibiotic class and bacterial genetic background. Future directions must focus on precisely timed SOS modulation rather than blanket inhibition, development of specific RecA and error-prone polymerase inhibitors, and combination therapies that exploit the vulnerabilities of SOS-deficient bacteria. For clinical translation, research should prioritize identifying biomarkers for SOS activity in infections and designing adjuvants that suppress resistance evolution without compromising bacterial eradication, ultimately extending the lifespan of existing antibiotics.
References
- 1. SOS response [https://en.wikipedia.org/wiki/SOS_response]
- 2. Role of the SOS Response in the Generation of Antibiotic ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC8373240/]
- 3. The SOS system: A complex and tightly regulated response to ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC6590174/]
- 4. The expression regulation of recA gene and bacterial class ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12425958/]
- 5. Fast evolution of SOS-independent multi-drug resistance in ... [https://elifesciences.org/articles/95058]
- 6. The central role of the SOS DNA repair system in ... [https://www.sciencedirect.com/science/article/abs/pii/S0024320520313151]
- 7. Mechanistic divergence between SOS response activation ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12211044/]
- 8. Defects in DNA doubleâ€strand break repair resensitize ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC9500592/]
- 9. SOS response promotes horizontal dissemination of ... [https://www.nature.com/articles/nature02241]
- 10. Antibiotic-induced DNA damage results in a controlled loss ... [https://www.nature.com/articles/s41598-020-76426-2]
- 11. Frontiers | Combined inactivation of the SOS response with TCA fumarases and the adaptive response enhances antibiotic susceptibility against Escherichia coli [https://www.frontiersin.org/journals/microbiology/articles/10.3389/fmicb.2025.1570764/full]
- 12. Systematically Altering Bacterial SOS Activity under Stress Reveals Therapeutic Strategies for Potentiating Antibiotics - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC4980697/]
- 13. Fast evolution of SOS-independent multi-drug resistance in ... [https://pubmed.ncbi.nlm.nih.gov/40631979/]
- 14. Antibiotic-induced stress responses in Gram-negative ... [https://pubmed.ncbi.nlm.nih.gov/40053699/]
- 15. The SOS - Error V Mutasome and β-Sliding... Prone DNA Polymerase [https://pmc.ncbi.nlm.nih.gov/articles/PMC8147279/]
- 16. Bacterial persisters: molecular mechanisms and ... [https://www.nature.com/articles/s41392-024-01866-5]
- 17. Bacterial Persister Cells and Development of Antibiotic ... - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC11335562/]
- 18. The DNA Damage Inducible SOS Response Is a Key ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC7417476/]
- 19. Antibiotic tolerance and persistence in clinical isolates of ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12403604/]
- 20. The DNA Damage Inducible SOS Response Is a Key ... [https://www.frontiersin.org/journals/microbiology/articles/10.3389/fmicb.2020.01785/full]
- 21. Conjugative DNA Transfer Induces the Bacterial SOS ... [https://journals.plos.org/plosgenetics/article?id=10.1371/journal.pgen.1001165]
- 22. Targeting evolution of antibiotic resistance by SOS response ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC7843400/]
- 23. Exploring the links between SOS response, mutagenesis, and ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11064565/]
- 24. Dissemination mechanisms of unique antibiotic resistance ... [https://www.sciencedirect.com/science/article/abs/pii/S0043135424019304]
- 25. Bioenergetic stress potentiates antimicrobial resistance ... [https://www.nature.com/articles/s41467-025-60302-6]
- 26. Managing the SOS Response for Enhanced CRISPR-Cas ... [https://pubmed.ncbi.nlm.nih.gov/28915012/]
- 27. A New Model for SOS-induced Mutagenesis: How RecA ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC2874081/]
- 28. New complexities of SOS-induced “untargeted ... [https://www.sciencedirect.com/science/article/abs/pii/S1568786420300975]
- 29. Impact of suppression of the SOS response on protein ... [https://www.frontiersin.org/journals/microbiology/articles/10.3389/fmicb.2024.1379534/full]
- 30. Bacterial Proteomics and Antibiotic Resistance Identification [https://pmc.ncbi.nlm.nih.gov/articles/PMC12655617/]
- 31. Heterogeneity of SOS response expression in clinical ... [https://www.sciencedirect.com/science/article/pii/S1368764624000451]
- 32. Advances in adaptive laboratory evolution applications for ... [https://www.sciencedirect.com/science/article/pii/S2405805X25001085]
- 33. ( Adaptive ) | Systems Biology Research... Laboratory Evolution ALE [https://systemsbiology.ucsd.edu/adaptive-laboratory-evolution-ale]
- 34. Fast Evolution of SOS-Independent Multi-Drug Resistance ... [https://elifesciences.org/reviewed-preprints/95058v1]
- 35. Fast evolution of SOS-independent multi-drug resistance in ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12240585/]
- 36. A Model for Designing Adaptive Experiments Laboratory Evolution [https://pubmed.ncbi.nlm.nih.gov/28159796/]
- 37. Development of an inhibitor of the mutagenic SOS response ... [https://pubs.rsc.org/en/content/articlehtml/2024/sc/d4sc00995a]
- 38. Accessing the High Throughput Screening Data Landscape [https://pmc.ncbi.nlm.nih.gov/articles/PMC5613246/]
- 39. Antibiotic resistance surges globally, UN health agency warns [https://news.un.org/en/story/2025/10/1166087]
- 40. Harnessing AI-Powered Computational Drug Design to ... [https://www.sciencedirect.com/science/article/pii/S3050787125001301]
- 41. Mutational signature analysis predicts bacterial ... [https://www.nature.com/articles/s41467-024-55206-w]
- 42. New small molecule found to suppress the evolution ... [https://www.ox.ac.uk/news/2024-05-23-new-small-molecule-found-suppress-evolution-antibiotic-resistance-bacteria]
- 43. The evolution and convergence of mutation spectra across ... [https://www.nature.com/articles/s42003-025-08181-x]
- 44. Antibiotic resistance mediated by gene amplifications [https://www.nature.com/articles/s44259-024-00052-5]
- 45. Mechanistic divergence between SOS response activation ... [https://pubmed.ncbi.nlm.nih.gov/40434128/]
- 46. SOS-independent bacterial DNA damage responses [https://www.sciencedirect.com/science/article/pii/S1369527423000607]
- 47. DNA Damage-induced Reactive Oxygen Species (ROS) ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC2643028/]
- 48. ROS and the DNA damage response in cancer - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC6859528/]
- 49. DNA damage-induced reactive oxygen species (ROS) ... [https://www.sciencedirect.com/science/article/abs/pii/S0891584908004267]
- 50. Reactive oxygen species accelerate de novo acquisition of ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10679899/]
- 51. Chronic Oxidative DNA Damage Due to DNA Repair ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC2519736/]
- 52. Reactive oxygen species as quantitative indicator of ... [https://www.sciencedirect.com/science/article/abs/pii/S1001074225002293]
- 53. The Global Challenge of Antimicrobial Resistance [https://pmc.ncbi.nlm.nih.gov/articles/PMC12284435/]
- 54. Ciprofloxacin pre-exposure influences individual cell MIC ... [https://www.nature.com/articles/s41598-025-17157-0]
- 55. Rapid assembly of biofilms from DNA released by SOS ... [https://www.nature.com/articles/s41598-025-96943-2]
- 56. Combined inactivation of the SOS response with TCA ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12098349/]
- 57. FDA-AACR Strategies for Optimizing Dosages for Oncology ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12536354/]
- 58. Key Considerations for Improving Dosage Optimization in ... [https://www.aacr.org/blog/2025/10/03/key-considerations-for-improving-dosage-optimization-in-oncology/]
- 59. Drug combinations targeting antibiotic resistance [https://www.nature.com/articles/s44259-024-00047-2]
- 60. The SOS Response Activation and the Risk of Antibiotic ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11720175/]
- 61. Evidence for Induction of Integron-Based Antibiotic Resistance ... [https://journals.plos.org/plospathogens/article?id=10.1371/journal.ppat.1002778]
- 62. SOS response and its regulation on the fluoroquinolone ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC4701512/]
- 63. Staphylococcus aureus SOS response: Activation, impact, and ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11442139/]
- 64. Fluoroquinolone-specific resistance trajectories in E. coli ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11748515/]
- 65. Differential proteomics of the SOS response and RecA ... [https://www.sciencedirect.com/science/article/pii/S0924857924003364]
- 66. Fast Evolution of SOS-Independent Multi-Drug Resistance ... [https://elifesciences.org/reviewed-preprints/95058v1/pdf]
- 67. Mechanisms of Antibiotic Resistance - PMC - PubMed Central [https://pmc.ncbi.nlm.nih.gov/articles/PMC4888801/]
- 68. Plasmid fitness costs are caused by specific genetic ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC8544851/]
- 69. TisB enables antibiotic in Salmonella by... | PLOS Pathogens tolerance [https://journals.plos.org/plospathogens/article?id=10.1371/journal.ppat.1013498]
- 70. Fast Evolution of SOS -Independent Multi-Drug Resistance in Bacteria [https://elifesciences.org/reviewed-preprints/95058v2]
- 71. SOS-Inducing Drugs Trigger Nucleic Acid Release and Biofilm ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10967838/]
- 72. Overcoming the cost of plasmid carriage [https://www.nature.com/articles/s41579-021-00657-x]
- 73. Role of the SOS Response in the Generation of Antibiotic ... [https://pubmed.ncbi.nlm.nih.gov/33875437/]
- 74. Modulating the evolutionary trajectory of tolerance using ... [https://www.nature.com/articles/s41467-022-30272-0]
- 75. The role of bacterial metabolism in antimicrobial resistance [https://pmc.ncbi.nlm.nih.gov/articles/PMC12173792/]
- 76. Quantitative and qualitative evaluation of antimicrobial usage [https://pmc.ncbi.nlm.nih.gov/articles/PMC11076899/]
- 77. Role of Extracellular DNA in Bacterial Response to SOS- ... [https://www.mdpi.com/2079-6382/12/4/649]
- 78. Relative quantification of the recA gene for antimicrobial ... [https://www.nature.com/articles/s41598-024-52937-0]