Targeting Metabolic Heterogeneity in Persister Cells: From Mechanisms to Therapeutic Breakthroughs
Persister cells, a dormant subpopulation in both bacterial and cancer contexts, exhibit profound metabolic heterogeneity, which is a key driver of antibiotic and chemotherapy treatment failure.
Targeting Metabolic Heterogeneity in Persister Cells: From Mechanisms to Therapeutic Breakthroughs
Abstract
Persister cells, a dormant subpopulation in both bacterial and cancer contexts, exhibit profound metabolic heterogeneity, which is a key driver of antibiotic and chemotherapy treatment failure. This article synthesizes the latest research on the non-genetic mechanisms underlying this metabolic diversity, exploring its origins in stochastic gene expression, epigenetic reprogramming, and dynamic feedback loops. We critically evaluate advanced single-cell technologies for profiling persister metabolism and systematically review emerging therapeutic strategies designed to exploit these metabolic vulnerabilities. By integrating foundational concepts with methodological advances and translational applications, this review provides a comprehensive resource for researchers and drug development professionals aiming to overcome the challenge of treatment relapse in chronic infections and cancer.
Unraveling the Origins and Molecular Drivers of Metabolic Heterogeneity
FAQ: Understanding Persister Cells
What exactly are persister cells? Persister cells are a subpopulation of cells within an isogenic culture that enter a temporary, non-growing, or slow-growing dormant state, enabling them to survive exposure to high doses of drugs or other environmental stresses without possessing heritable genetic resistance. Upon removal of the stress, these cells can resuscitate and regenerate a susceptible population [1] [2].
How do persister cells differ from resistant cells? The key difference lies in the mechanism of survival. Resistant cells have genetic mutations that allow them to grow in the presence of a drug, and this resistance is heritable. Persister cells, in contrast, are genetically identical to their susceptible siblings and survive through non-genetic, phenotypic mechanisms like dormancy; their tolerance is not passed on to the next generation of cells once they resume growth [3] [2].
Why are persister cells a critical problem in both infectious disease and oncology? In bacterial infections, persisters are a major cause of chronic and relapsing infections (e.g., tuberculosis, cystic fibrosis-related infections) and are implicated in the development of genetic antibiotic resistance [3] [2]. In cancer, drug-tolerant persister (DTP) cells contribute to tumor relapse and the emergence of acquired resistance to targeted therapies and chemotherapies, representing a significant barrier to a cure [1].
What is the role of metabolic heterogeneity in persister cells? Even within an isoclonal population, individual cells can exhibit significant variation in their metabolic states. This metabolic heterogeneity is a fundamental driver of persistence. It acts as a "bet-hedging" strategy, ensuring that a subset of cells with a specific, slow-metabolizing phenotype will survive a sudden environmental stress, such as antibiotic or anti-cancer drug exposure [4].
How can I experimentally isolate and study persister cells? A standard method is to treat a mid-log phase bacterial culture with a high concentration of a bactericidal antibiotic (e.g., a fluoroquinolone or an aminoglycoside) for several hours. The surviving cells, which are typically 0.001% to 1% of the total population, are considered persisters. These can be quantified by plating for colony-forming units (CFUs) after drug exposure [2]. For cancer DTPs, cells are exposed to targeted or chemotherapeutic agents, and the surviving, often dormant, subpopulation is analyzed [1].
Troubleshooting Common Experimental Challenges
Issue: Low or Inconsistent Persister Cell Yields
Potential Causes and Solutions:
- Cause: Inconsistent growth phase of the starter culture.
- Solution: Always use cultures grown to the same optical density (e.g., mid-log phase) and ensure highly reproducible growth conditions, including media, temperature, and shaking speed [2].
- Cause: Inadequate drug concentration or exposure time.
- Solution: Perform a kill curve experiment to establish the minimum drug concentration and exposure time that kills >99.9% of the population. Use a freshly prepared, high-quality drug solution [2].
- Cause: Environmental stressors inducing unintended persistence.
- Solution: Avoid temperature fluctuations, nutrient shifts, or oxygen limitation immediately before and during the persister assay.
Issue: High Variability in Results Between Replicates
Potential Causes and Solutions:
- Cause: Stochastic nature of persister formation.
- Solution: Increase the number of biological replicates (n ≥ 6 is often recommended) to account for the inherent randomness of the phenotype [4].
- Cause: Clumping of cells leading to uneven drug exposure.
- Solution: Vortex and/or briefly sonicate the culture before treatment to ensure a single-cell suspension. Take multiple samples for CFU plating during the dilution steps.
- Cause: Contamination.
- Solution: Maintain strict aseptic technique and regularly check for microbial contamination.
Key Signaling Pathways and Mechanisms
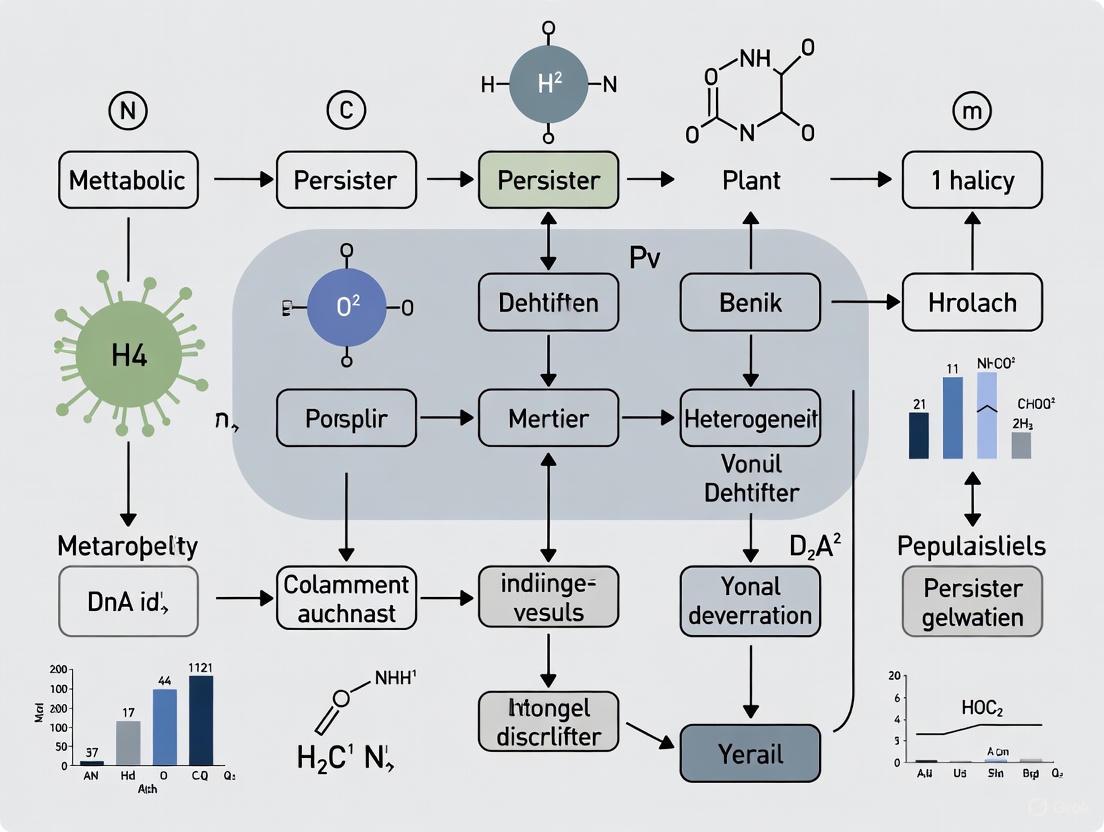
The following diagram illustrates the core pathways and regulatory interactions involved in the formation and survival of bacterial persister cells, integrating mechanisms like toxin-antitoxin systems, stringent response, and metabolic shutdown.
Experimental Protocols for Persister Research
Protocol 1: Isolation of Bacterial Persisters via Antibiotic Killing
Principle: A high dose of a bactericidal antibiotic is used to kill the vast majority of growing cells, leaving behind the non-growing, tolerant persister population for downstream analysis [2].
Procedure:
- Grow culture: Inoculate bacteria in appropriate liquid medium (e.g., LB) and incubate with shaking until mid-log phase (OD₆₀₀ ~0.5).
- Treat with antibiotic: Add a high concentration of a bactericidal antibiotic (e.g., 100x MIC of ciprofloxacin or 100 µg/mL of ampicillin). Continue incubation.
- Sample and quantify: At specific time points (e.g., 0, 2, 5, 24 hours), remove aliquots of the culture.
- Wash and plate: Wash the samples 2-3 times with sterile PBS or saline to remove the antibiotic. Perform serial dilutions and plate on drug-free agar plates.
- Count colonies: After overnight incubation, count the colonies to determine the number of viable persister cells (CFU/mL).
Key Reagents:
- Liquid growth medium
- Bactericidal antibiotic (e.g., Ciprofloxacin, Ampicillin)
- Phosphate Buffered Saline (PBS)
- Drug-free solid agar plates
Protocol 2: Profiling Metabolic Heterogeneity Using Genetically Encoded Biosensors
Principle: Fluorescent biosensors allow real-time tracking of metabolite levels (e.g., ATP, NADH) in single cells, revealing the metabolic heterogeneity that underpins persister formation [4].
Procedure:
- Engineer biosensor strain: Transform bacteria with a plasmid expressing a FRET-based or transcription factor-based biosensor for a metabolite of interest (e.g., ATP).
- Prepare sample: Grow the sensor strain to mid-log phase and mount a small volume on an agarose pad for live-cell microscopy.
- Image acquisition: Use a fluorescence microscope with appropriate filters and settings to capture images of the bacterial population at high resolution.
- Image analysis: Use image analysis software (e.g., ImageJ, CellProfiler) to quantify the fluorescence intensity of the biosensor in individual cells.
- Data interpretation: Plot the distribution of fluorescence intensities across the population. A broad or multimodal distribution indicates significant metabolic heterogeneity.
Key Reagents:
- Genetically encoded metabolite biosensor plasmids
- Selective antibiotics for plasmid maintenance
- Agarose
- Live-cell imaging compatible growth medium
Research Reagent Solutions
Table: Essential Reagents for Persister Cell Research
| Reagent / Tool | Primary Function | Example Application |
|---|---|---|
| Bactericidal Antibiotics (Ciprofloxacin, Ampicillin) | Kill growing cells to isolate the non-growing persister subpopulation. | Primary isolation of persisters from bacterial cultures [2]. |
| Genetically Encoded Biosensors (e.g., for ATP, NADH) | Enable real-time, single-cell measurement of metabolite levels and dynamics. | Quantifying metabolic heterogeneity and identifying low-metabolism subpopulations [4]. |
| Fluorescence-Activated Cell Sorter (FACS) | Isolate subpopulations of cells based on specific fluorescence signals (e.g., from biosensors or dye staining). | Sorting and collecting metabolically high vs. low cells for downstream 'omics' analysis or culture [4]. |
| Metabolic Dyes (e.g., CTC for respiration, SYTOX for viability) | Probe the metabolic activity and membrane integrity of cells at a single-cell level. | Distinguishing between dormant, active, and dead cells in a population. |
| ClpP Activators (e.g., ADEP4) | Activate the ClpP protease, leading to uncontrolled protein degradation. | Directly killing persister cells by degrading essential proteins in a growth-independent manner [3]. |
| Membrane-Targeting Compounds (e.g., XF-73, SA-558) | Directly disrupt bacterial cell membrane integrity, causing cell lysis. | Eradicating persisters by targeting a structure that is essential regardless of growth state [3]. |
Bacterial persisters are a subpopulation of cells that exhibit multidrug tolerance, enabling them to survive antibiotic treatment without genetic resistance mutations [2] [5]. These cells are not inherently resistant but exist in a transient, phenotypically distinct state characterized by reduced metabolic activity and growth arrest [6] [7]. The core metabolic features of persisters—quiescence, stress signaling, and energy shifts—represent a significant challenge in treating persistent and biofilm-associated infections [2]. Understanding this metabolic heterogeneity is crucial for developing therapeutic strategies that can effectively target these recalcitrant cells.
Persisters demonstrate remarkable phenotypic heterogeneity, including metabolic diversity, variation in persistence levels, and differences in colony sizes [2]. This heterogeneity exists on a continuum, with some persisters exhibiting "deep" persistence (strong persistence ability) while others demonstrate "shallow" persistence (weak persistence ability) [2]. The metabolic state of persister cells is not fixed but changes dynamically with environmental conditions, creating a complex landscape for researchers to navigate [2]. This technical support center provides troubleshooting guidance and experimental protocols to address the specific challenges faced by investigators studying metabolic heterogeneity in persister cell populations.
Frequently Asked Questions (FAQs) on Persister Metabolism
FAQ 1: What fundamentally distinguishes persister cells from resistant bacteria at the metabolic level?
Persister cells are characterized by phenotypic tolerance without genetic resistance, while resistant bacteria possess genetic mutations that allow growth in the presence of antibiotics [5]. The key distinction lies in the minimum inhibitory concentration (MIC)—persisters exhibit an unchanged MIC but survive antibiotic treatment due to a higher minimum duration to kill 99% of the population (MDK99) [5]. Metabolically, persisters typically exist in a slow-growing or non-growing state with reduced metabolic activity, whereas resistant bacteria continue to grow and replicate normally in the presence of antibiotics [6]. When persister cells regrow without antibiotics, their progeny regain susceptibility identical to the parental population [5].
FAQ 2: How does metabolic quiescence enable antibiotic tolerance?
Most bactericidal antibiotics target active cellular processes such as cell wall synthesis, protein production, and DNA replication [6]. Metabolic quiescence allows persisters to avoid these targets through:
- Reduced proton motive force (PMF): Limits uptake of aminoglycoside antibiotics [6]
- Diminished metabolic activity: Decreases antibiotic target corruption [5]
- Downregulated energy production: Low ATP levels reduce activity of antibiotics whose lethality depends on energy metabolism [7] This dormant or slow-metabolizing state is reversible, allowing resumption of growth once antibiotic pressure is removed [2].
FAQ 3: What are the primary metabolic pathways involved in persister formation?
Multiple interconnected pathways regulate persister formation:
- Stringent response: Mediated by the alarmone (p)ppGpp in response to nutrient stress [8]
- Toxin-antitoxin (TA) modules: Act as effectors of ppGpp-induced persistence [8]
- Energy metabolism shifts: Alterations in TCA cycle, ATP production, and proton motive force [7]
- Central carbon metabolism regulation: Changes in glycolysis, pentose phosphate pathway, and amino acid biosynthesis [4] [7] These pathways form a complex regulatory network that responds to both stochastic triggers and environmental cues [2] [8].
Troubleshooting Common Experimental Challenges
Table 1: Troubleshooting Guide for Persister Metabolism Studies
| Challenge | Potential Causes | Solutions | Supporting Techniques |
|---|---|---|---|
| Low persister yields | Insufficient stress induction; inadequate culture conditions; improper antibiotic selection | Extend stationary phase incubation; use biofilm models; optimize antibiotic concentration and treatment duration | Population killing curves; MIC/MDC determinations [5] |
| Inconsistent metabolic measurements | Persister heterogeneity; contamination with normal cells; unstable metabolic state | Implement robust persister isolation; use single-cell approaches; standardize recovery protocols | Microfluidics with membrane-covered microchamber arrays [9]; flow cytometry with sorting [4] |
| Difficulty characterizing metabolic fluxes | Low persister numbers; rapid metabolic changes during isolation; technical limitations | Employ 13C-isotopolog profiling; use genetically encoded biosensors; apply NanoSIMS | Isotopolog profiling [7]; FRET-based metabolite biosensors [4]; nanoscale secondary ion mass spectrometry [4] |
| Poor response to metabolite supplementation | Impermeable metabolites; incorrect concentration; incompatible with antibiotic mechanism | Test metabolite analogs with better permeability; optimize concentration ranges; match metabolites to antibiotic class | Phenotype microarrays [7]; fluorescent dye-based reductase assays [7] |
| Inadequate separation of persisters | Incomplete killing of non-persisters; antibiotic concentration too low; treatment duration insufficient | Use lytic antibiotics for selection; employ unstable GFP variants; implement fluorescence-activated cell sorting | Unstable GFP-based separation [7]; antibiotic selection protocols [2] |
Advanced Protocol: Single-Cell Analysis of Persister Metabolism Using Microfluidics
Background: Traditional bulk measurements mask the metabolic heterogeneity of persister populations. This protocol utilizes microfluidic devices to track metabolic states of individual persister cells before, during, and after antibiotic treatment [9].
Materials:
- Microfluidic device with membrane-covered microchamber array (MCMA)
- E. coli MG1655 or other target strain
- Antibiotics: ampicillin (200 µg/mL) and ciprofloxacin (1 µg/mL)
- Fluorescence microscopy system with environmental control
- Genetically encoded metabolite biosensors (as needed)
Procedure:
- Device Preparation: Fabricate MCMA with 0.8-µm deep microchambers on glass coverslips [9]
- Cell Loading: Introduce exponential or stationary phase bacterial cells into microchambers
- Medium Control: Establish controlled medium flow above membrane for rapid exchange (within 5 minutes)
- Antibiotic Treatment: Expose cells to lethal antibiotic concentrations (e.g., 12.5×MIC ampicillin or 32×MIC ciprofloxacin)
- Time-Lapse Imaging: Monitor individual cells throughout treatment and recovery phases
- Data Analysis: Track growth history, morphological changes, and resuscitation dynamics of surviving persisters
Expected Results: Recent studies using this approach revealed that most persisters from exponentially growing populations were actively growing before antibiotic treatment, showing heterogeneous survival dynamics including continuous growth with L-form-like morphologies, responsive growth arrest, or post-exposure filamentation [9].
Troubleshooting Tip: For improved cell viability during extended imaging, ensure proper nutrient exchange through the semipermeable membrane and maintain appropriate temperature and humidity control throughout the experiment.
Key Signaling Pathways in Persister Metabolism
The Central Role of ppGpp in Persister Metabolism
The following diagram illustrates the ppGpp-mediated stringent response pathway, a central regulator of metabolic shifts in persister formation:
Diagram 1: ppGpp-Mediated Stringent Response in Persister Formation (76 characters)
The (p)ppGpp-mediated stringent response serves as a master regulator connecting nutrient stress to persister formation [8]. This pathway is activated by various metabolic stresses including glucose starvation and amino acid depletion, leading to increased ppGpp production through RelA activation [7]. Elevated ppGpp levels trigger multiple downstream effects:
- TA system activation: ppGpp induces toxin-antitoxin modules such as HipA, which phosphorylates glutamyl-tRNA synthetase (GltX), inhibiting tRNA loading and further amplifying the stringent response [7]
- Metabolic reprogramming: Direct inhibition of DNA gyrase and RNA polymerase reduces biosynthetic activities [7]
- Energy metabolism shift: Downregulation of TCA cycle and ATP-generating pathways conserves energy [7]
In Pseudomonas aeruginosa, nutrient limitation activates a ppGpp-dependent mechanism directing cells to a state of increased antibiotic tolerance [7]. Similarly, in Staphylococcus aureus, permanent ppGpp synthesis leads to growth inhibition and facilitates persistent infections [7].
Metabolic Activation Strategies for Anti-Persister Interventions
The "wake and kill" strategy aims to reverse metabolic dormancy to resensitize persisters to conventional antibiotics:
Diagram 2: Metabolic Activation Strategy to Eradicate Persisters (67 characters)
This approach leverages the correlation between bacterial metabolic rate and efficacy of bactericidal antibiotics [6]. Key metabolites can stimulate and disrupt metabolic dormancy mechanisms:
- Sugar metabolites: Mannitol restores proton motive force and enhances aminoglycoside uptake [6]
- Central carbon metabolites: Pyruvate promotes gentamicin uptake against antibiotic-resistant Vibrio alginolyticus [6]
- Amino acids: L-valine promotes phagocytosis to kill multidrug-resistant bacterial pathogens [6]
- Nucleotides: Exogenous adenosine and/or guanosine enhances tetracycline sensitivity [6]
Research Reagent Solutions for Persister Metabolism Studies
Table 2: Essential Research Reagents for Persister Metabolism Investigations
| Reagent/Category | Specific Examples | Research Application | Key Function |
|---|---|---|---|
| Metabolite Biosensors | FRET-based sensors; Transcription factor-based reporters; RNA aptamer systems | Real-time monitoring of metabolite dynamics in single cells | Couple metabolite concentrations to fluorescent outputs for quantification [4] |
| Isotopic Tracers | 13C-labeled glucose; 15N-labeled ammonium | Metabolic flux analysis in persister populations | Enable isotopolog profiling to determine pathway activities [7] |
| Metabolic Modulators | Carbonyl cyanide m-chlorophenylhydrazone (CCCP); Metabolites (mannitol, pyruvate) | Manipulate energy states and test "wake and kill" strategies | Modulate proton motive force and metabolic activity [6] [7] |
| Microfluidic Systems | Membrane-covered microchamber arrays (MCMA); Single-cell cultivation devices | Single-cell analysis of persister formation and resuscitation | Enable tracking of individual cell histories before and after antibiotic exposure [9] |
| Separation Tools | Unstable GFP variants; Fluorescence-activated cell sorting | Isolation of persister subpopulations from heterogeneous cultures | Enable separation of persisters from non-persisters for targeted analysis [7] |
Quantitative Analysis of Persister Metabolic Features
Table 3: Metabolic Parameters in Different Persister Subpopulations
| Metabolic Parameter | Type I Persisters | Type II Persisters | Growing Persisters | Measurement Techniques |
|---|---|---|---|---|
| Growth Rate | Non-growing | Slow-growing (0.001-0.01 hâ»Â¹) | Variable, but detectable division | Single-cell tracking; Time-lapse microscopy [2] [9] |
| ATP Levels | Severely reduced (~5% of normal) | Moderately reduced (~20% of normal) | Near normal with fluctuations | Luciferase-based assays; Fluorescent biosensors [7] |
| Proton Motive Force | Significantly diminished | Partially reduced | Variable, can be restored | Membrane potential-sensitive dyes; FRET reporters [6] |
| Antibiotic Survival Rate | High (up to 1% of population) | Moderate (0.1-0.001% of population) | Lower but significant (0.01-0.0001%) | Killing curves with 12.5×MIC ampicillin or 32×MIC ciprofloxacin [9] |
| Resuscitation Time | Longer lag phase (hours to days) | Shorter lag phase (minutes to hours) | Minimal lag phase (immediate growth) | Microfluidic monitoring after antibiotic removal [9] |
The data presented in Table 3 highlights the continuum of metabolic states in persister populations, from deeply dormant Type I persisters to the recently characterized growing persisters observed in single-cell studies [2] [9]. This heterogeneity underscores the importance of using multiple complementary approaches to fully capture the metabolic diversity of persister cells.
The core metabolic features of bacterial persisters—quiescence, stress signaling, and energy shifts—represent a complex adaptive response that enables survival under antibiotic pressure. Understanding these features at both population and single-cell levels is crucial for developing effective strategies against persistent infections. The experimental approaches and troubleshooting guidance provided here address key challenges in persister metabolism research, from isolation and characterization to targeted intervention.
Future research directions should focus on:
- Developing more sensitive tools for real-time metabolic monitoring in single persister cells
- Elucidating the precise molecular mechanisms linking metabolic states to antibiotic tolerance
- Translating metabolic activation strategies into clinically viable treatments
- Exploring interspecies differences in persister metabolism across clinically relevant pathogens
As research in this field advances, the integration of single-cell technologies with metabolic analysis will continue to reveal the intricate heterogeneity of persister populations, ultimately guiding the development of novel therapeutic approaches that can overcome antibiotic tolerance.
Within clonal microbial populations, even isogenic cells grown in identical environments display significant phenotypic variation. This heterogeneity, driven by the inherent stochasticity of biochemical reactions, presents a substantial challenge in combating persistent infections. Molecular noise—random fluctuations in gene expression—and metabolic heterogeneity—cell-to-cell variations in metabolite levels and fluxes—are critical underlying factors. Research into bacterial persisters, which are dormant, drug-tolerant cells responsible for chronic and relapse infections, is particularly affected by this variability [2]. The stochastic nature of gene expression means that even carefully controlled experiments generate data with substantial cell-to-cell variation, complicating interpretation and requiring specialized troubleshooting approaches. This technical support center addresses the specific experimental challenges and frequently asked questions that arise when investigating these phenomena.
FAQs: Core Concepts and Technical Challenges
Q1: What is the fundamental difference between intrinsic and extrinsic noise in gene expression?
- Intrinsic noise originates from the random, inherent fluctuations in the biochemical processes of transcription and translation of a specific gene. These fluctuations cause independent variation in the expression of two identical genes within the same cell [10] [11].
- Extrinsic noise stems from global, cell-wide fluctuations in factors such as the concentrations of RNA polymerases, ribosomes, or metabolic resources. These variations affect the expression of all genes in a cell in a correlated manner [10] [11].
Q2: How does stochastic gene expression contribute to metabolic heterogeneity in bacterial persisters?
Gene expression is a fundamentally stochastic process characterized by transcriptional bursting, where mRNA molecules are produced in random, pulse-like events [10] [12]. This noise propagates into metabolism because variations in the expression of metabolic enzymes cause cell-to-cell differences in metabolic fluxes and metabolite levels [4] [13]. In persister cells, this can lead to subpopulations with distinct metabolic states, such as metabolic quiescence or slow growth, enabling survival under antibiotic stress [2]. This metabolic heterogeneity is now recognized as a key mechanism underlying bacterial persistence and biofilm-related treatment failures [4] [2].
Q3: My single-cell RNA sequencing data shows a high number of zero-expression values ("dropouts") for a gene of interest. Is this a technical failure?
Not necessarily. While some zero counts are technical artifacts, a significant portion often reflects true biological silence due to transcriptional bursting [12]. Genes transition stochastically between active transcriptional states and inactive, silent states. A zero count in a viable cell can indicate it was captured during a silent phase. This natural variability can be leveraged analytically, as in the single-cell Stochastic Gene Silencing (scSGS) method, which compares active and silent cell subpopulations to infer gene function without genetic perturbation [12].
Troubleshooting Guides
Troubleshooting Experimental Noise Quantification
This guide addresses common issues when quantifying gene expression noise using dual-fluorescent reporter systems [11].
| Problem | Possible Cause | Solution |
|---|---|---|
| No correlation in control | Global cellular factors (extrinsic noise) are overwhelming the signal. | Verify cell health and growth conditions; ensure reporters are genomically integrated at identical loci to minimize copy number variation. |
| Excessive independent variation | High intrinsic noise or poor experimental calibration. | Check promoter strength; use a stronger promoter to increase expression levels and potentially reduce the coefficient of variation. |
| Low signal-to-noise ratio | Fluorescent proteins are maturing slowly or are unstable. | Use faster-folding fluorescent protein variants (e.g., sfGFP); include proper controls to account for protein half-life. |
| Unexpected bimodality | The promoter may be in a bistable network or the population contains multiple cell states. | Analyze the population for cell cycle stage or other physiological heterogeneity; consider using time-lapse microscopy to track single cells over time. |
Troubleshooting Metabolic Heterogeneity Measurements
This guide assists with challenges in assessing cell-to-cell metabolic variation, relevant to studying persister cell subpopulations [4] [13].
| Problem | Possible Cause | Solution |
|---|---|---|
| Uninterpretable biosensor data | The biosensor kinetics are too slow for the metabolic dynamics, or the sensor is saturated. | Characterize biosensor response time in vivo; use ratiometric FRET-based biosensors for more quantitative measurements [4]. |
| High background in metabolite detection | Non-specific signal or autofluorescence interfering with measurement. | Include control strains lacking the biosensor; use mass spectrometry-based techniques (e.g., NanoSIMS) for specific, label-free metabolite quantification [4]. |
| Metabolite distributions are always unimodal | The assay may not be sensitive enough to detect rare metabolic subpopulations. | Increase the number of cells analyzed; use fluorescence-activated cell sorting (FACS) to pre-enrich for rare cells based on a marker before metabolic analysis. |
| Inability to link metabolic state to persistence | Lack of a direct readout connecting a metabolic flux to persister cell viability. | Employ combination assays: sort cells based on a metabolic biosensor (e.g., for ATP) and then subject the sorted populations to antibiotic challenge to quantify persister frequency [4] [2]. |
Key Experimental Protocols & Data
Protocol: Quantifying Intrinsic and Extrinsic Noise with a Dual-Reporter System
This protocol quantifies noise using two fluorescent proteins under identical promoters [10] [11].
- Step 1: Strain Construction. Genomically integrate two expression cassettes into the cell. Each cassette must use an identical promoter to drive the expression of two different fluorescent proteins (e.g., CFP and YFP). Ensure the integration sites are genomically neutral and equidistant from the origin of replication to control for gene copy number effects.
- Step 2: Cultivation and Flow Cytometry. Grow the strain under the defined experimental conditions to mid-exponential phase. Analyze a minimum of 10,000 individual cells using a flow cytometer equipped with lasers and filters appropriate for CFP and YFP.
- Step 3: Data Analysis. For each cell
i, you will have a fluorescence intensity for CFP (C_i) and YFP (Y_i).- Calculate the total noise for a protein (e.g., CFP):
η²_total = ⟨C²⟩ / ⟨C⟩² - 1, where⟨⟩denotes the population mean. - Calculate the extrinsic noise (
η²_ext) from the correlation between CFP and YFP across the population:η_ext ≈ cov(C, Y) / (⟨C⟩⟨Y⟩). - Calculate the intrinsic noise (
η²_int) from the uncorrelated variation:η_int ≈ η²_total - η²_ext.
- Calculate the total noise for a protein (e.g., CFP):
Quantitative Foundations of Heterogeneity
The table below summarizes key quantitative relationships identified in research on stochastic gene expression and metabolic heterogeneity.
| Parameter or Relationship | Quantitative Value or Correlation | Experimental System | Significance |
|---|---|---|---|
| Noise vs. Expression Variation | Significant correlation (Predictive model, SVR, achieved high fidelity) [14] | S. cerevisiae | Population-level expression variation can serve as a proxy for single-cell stochastic noise. |
| Promoter Type and Noise | TATA-box containing genes show higher and more predictable noise levels [14] | S. cerevisiae | Specific promoter architectures are major determinants of stochastic gene expression. |
| Metabolic Gene Promoters | Controlled by noisier promoters compared to essential genes [4] | E. coli | Suggests evolutionary tuning to allow large metabolic heterogeneity for bet-hedging. |
| Protein Copy Number | ~10% of repressors and ~50% of activators have ≤10 copies per cell [11] | E. coli | Low abundance of key regulators ensures system-wide susceptibility to molecular noise. |
Essential Visualizations
Quantifying Gene Expression Noise
Origins of Metabolic Heterogeneity
The Scientist's Toolkit: Research Reagent Solutions
| Reagent or Tool | Function in Research | Key Consideration |
|---|---|---|
| Dual-Fluorescent Reporter Plasmids | Quantifying intrinsic vs. extrinsic noise by expressing CFP and YFP from identical promoters [11]. | Ensure genomic integration at neutral, matched loci to avoid position effects. |
| Genetically Encoded Metabolite Biosensors | Dynamic, single-cell quantification of metabolite levels (e.g., FRET-based sensors, transcription factor-based reporters) [4]. | Validate sensor response time and dynamic range in your specific model organism and condition. |
| Support Vector Regression (SVR) Models | In silico prediction of gene expression noise levels based on population-level expression variation data [14]. | Requires a large compendium of gene expression data across many conditions for training. |
| Microfluidics & Time-Lapse Microscopy | Monitoring gene expression dynamics and metabolic heterogeneity in single cells over multiple generations [10]. | Essential for distinguishing between deep and shallow persister states based on duration of dormancy [2]. |
| scSGS Computational Framework | Leveraging transcriptional bursting patterns in scRNA-seq data to infer gene function without knockout [12]. | Identifies "SGS-responsive genes" by comparing cells in active vs. silenced transcriptional states for a target gene. |
| cl-387785 | cl-387785, CAS:253310-44-0, MF:C18H13BrN4O, MW:381.2 g/mol | Chemical Reagent |
| Paritaprevir | Paritaprevir, CAS:1221573-85-8, MF:C40H43N7O7S, MW:765.9 g/mol | Chemical Reagent |
The Role of Epigenetic Reprogramming and Transcriptional Plasticity in Cancer DTPs
What are Drug-Tolerant Persister (DTP) cells and why are they a problem in cancer therapy?
Drug-Tolerant Persister (DTP) cells are a rare subpopulation of cancer cells that survive standard-of-care therapies not through stable genetic resistance, but via reversible, non-genetic adaptations [15]. Acting as clinically occult reservoirs, DTP cells persist after treatment, seeding relapse long after the visible tumour has regressed [15]. This phenomenon is a major obstacle to achieving durable cancer remission.
The concept was inspired by bacterial persisters first described by Bigger and later identified in cancer by Sharma et al. in EGFR-mutant non-small cell lung cancer (NSCLC) models treated with EGFR inhibitors [15]. DTPs exhibit a spectrum of adaptive traits including epigenetic reprogramming, transcriptional memory, translational remodelling, metabolic shifts, and therapy-induced mutagenesis across diverse tumour types and treatments [15].
How do DTPs differ from other resistant cell types?
Unlike genetically resistant clones or cancer stem cells (CSCs), DTPs are characterized by their transient, reversible nature and emergence from genetically identical cell populations under therapeutic pressure [15]. Table 1 compares DTPs with other cell states.
Table 1: Characteristic Comparison of DTPs and Related Cell States
| Characteristic | DTPs | Genetically Resistant Cells | Cancer Stem Cells (CSCs) | Senescent Cells |
|---|---|---|---|---|
| Cell Fraction | Rare subset | Subset (context-dependent) | Subset (context-dependent) | Variable (often large fractions) |
| Growth State | Slow-cycling or quiescent | Proliferating | Self-renewing | Quiescent |
| Treatment Requirement | Induced by lethal treatment | No | No | Context-dependent |
| Genetic Dependency | No | Yes | Partial | Partial |
| Reversibility | Yes, upon drug removal | No | Yes | Irreversible |
| Primary Mechanism | Non-genetic adaptation | Genetic mutations | Stemness programs | Stress-induced arrest |
Molecular Mechanisms & Troubleshooting
What epigenetic mechanisms drive DTP formation and maintenance?
Epigenetic reprogramming serves as a key mechanism enabling cancer cells to acquire stem-like characteristics and drive therapeutic resistance [16]. This involves dynamic alterations to histone modifications and chromatin architecture in response to environmental stimuli like drug exposure [16].
The "writer-reader-eraser" framework governs histone modification dynamics [17] [18]:
- Writers (e.g., HATs, HMTs) add chemical groups to histones
- Erasers (e.g., HDACs, KDMs) remove these modifications
- Readers (e.g., proteins with bromodomains, chromodomains) interpret these marks
In DTPs, this equilibrium is disrupted, creating transcriptionally permissive chromatin regions at genes associated with stemness while silencing differentiation genes [16].
Table 2: Key Epigenetic Regulators Implicated in DTP States
| Epigenetic Regulator | Type | Function in DTPs | Therapeutic Targeting |
|---|---|---|---|
| EZH2 | Writer (HMT) | Represses differentiation genes via H3K27me3 | Tazemetostat (EPZ-6438) [17] |
| BRD4 | Reader | Binds acetylated histones at super-enhancers | BET inhibitors (RO6870810) [17] [19] |
| HDACs | Erasers | Remove acetyl groups, promoting chromatin compaction | HDAC inhibitors [17] |
| DNMTs | Writers | DNA methylation silencing of tumor suppressors | DNMT inhibitors [18] |
| KDM family | Erasers | Demethylate histones, altering gene expression | KDM inhibitors in development [18] |
What experimental approaches can detect and characterize DTP epigenetic states?
Protocol 1: Profiling DTP Epigenetic Landscapes
Materials Required:
- Drug-tolerant cells from appropriate cancer model
- HDAC or BET inhibitors as positive controls
- Antibodies for ChIP (H3K27ac, H3K4me3, H3K27me3)
- Single-cell RNA-sequencing reagents
- ATAC-sequencing reagents
Methodology:
- DTP Generation: Treat cancer cells with relevant targeted therapy (e.g., EGFR inhibitors for NSCLC, BRAF inhibitors for melanoma) for 7-14 days at clinically relevant concentrations [15].
- Epigenetic Profiling:
- Perform ChIP-seq for activation (H3K27ac, H3K4me3) and repression (H3K27me3) marks
- Conduct ATAC-seq to map chromatin accessibility
- Implement single-cell RNA-seq to resolve heterogeneity
- Data Analysis: Identify differentially accessible regions and super-enhancers driving DTP identity [19].
Troubleshooting Guide:
- Low DTP yield: Optimize drug concentration and treatment duration; use viability dyes to isolate persistent cells
- High background in ChIP: Include appropriate negative control regions and validate antibody specificity
- Poor single-cell sequencing data: Check cell viability before loading (>90% recommended)
Diagram 1: Epigenetic Regulation of DTP State. Therapy-induced signals rewire the epigenetic landscape through writer, eraser, and reader proteins, creating permissive chromatin at stemness genes and repressive chromatin at differentiation loci.
Metabolic Heterogeneity & Analysis
How does metabolic heterogeneity influence DTP epigenetics?
Metabolic reprogramming is an evolutionarily conserved strategy for cells facing stress [20]. Cancer cells rewire their metabolism to support energy production and biosynthetic precursors, which directly influences the epigenetic landscape through metabolite availability [20].
Key metabolic-epigenetic connections:
- ATP-dependent chromatin remodeling: Energy status directly affects chromatin modifier activity
- Metabolites as cofactors: α-KG, SAM, Acetyl-CoA, and NAD+ levels regulate epigenetic enzyme function
- Oxidative stress: Impacts epigenetic regulation through redox-sensitive transcription factors
Protocol 2: Assessing Metabolic Heterogeneity in DTP Populations
Materials Required:
- Seahorse XF Analyzer and consumables
- Metabolic modulators (oligomycin, FCCP, rotenone, 2-DG)
- Stable isotope tracers (^13C-glucose, ^15N-glutamine)
- LC-MS equipment for metabolomics
- Fluorescent glucose and nutrient sensors
Methodology:
- Metabolic Flux Analysis:
- Use Seahorse XF Analyzer to measure OCR (oxidative phosphorylation) and ECAR (glycolysis)
- Calculate metabolic phenotypes using basal and stressed conditions
- Stable Isotope Tracing:
- Feed DTPs with ^13C-glucose or ^15N-glutamine
- Track isotope incorporation into TCA intermediates and epigenetic cofactors (acetyl-CoA, SAM)
- Single-Cell Metabolic Profiling:
- Use fluorescent reporters for glucose uptake, mitochondrial membrane potential
- Correlate with epigenetic markers via imaging
Table 3: Metabolic Parameters in DTPs vs. Treatment-Naive Cells
| Metabolic Parameter | DTP Cells | Treatment-Naive Cells | Measurement Technique |
|---|---|---|---|
| Glycolytic Rate | Variable (context-dependent) | Typically high | Seahorse ECAR, ^13C-glucose tracing |
| Oxidative Phosphorylation | Often elevated | Variable | Seahorse OCR, mitochondrial staining |
| ATP Levels | Maintained despite stress | High | Luminescent assays, biosensors |
| Acetyl-CoA Production | Reprogrammed | Growth-associated | LC-MS, enzymatic assays |
| SAM Availability | Altered | Normal | Mass spectrometry |
Troubleshooting Guide:
- Inconsistent flux measurements: Normalize to cell number; ensure consistent pretreatment conditions
- Poor isotope incorporation: Optimize tracer concentration and duration
- Metabolite instability: Use rapid quenching methods and maintain cold chain
Diagram 2: Metabolic-Epigenetic Crosstalk in DTPs. Core metabolic pathways generate essential cofactors and energy that directly regulate epigenetic modifications, creating a feedback loop that maintains the DTP state.
Technical Challenges & Solutions
How can we overcome transcriptional heterogeneity in DTP studies?
DTP populations exhibit significant heterogeneity, with multiple phenotypic states coexisting within the same tumor [15]. For instance, single-cell RNA sequencing has shown that DTPs with mesenchymal-like and luminal-like transcriptional states can coexist within breast cancers [15].
Solutions:
- Single-cell multi-omics: Combine scRNA-seq with scATAC-seq to link transcriptional states with chromatin accessibility
- Lineage tracing: Use DNA barcoding to track clonal fates after treatment
- Spatial transcriptomics: Map DTP niches within tumor architectures
What are common pitfalls in DTP experimental models?
Most DTP studies rely heavily on in vitro or ex vivo models, limiting their physiological relevance [15]. Recent efforts have begun to explore minimal residual disease in vivo, including through patient-derived xenografts (PDXs), but these models often lack immune components and don't capture broader systemic influences [15].
Improved Model Systems:
- Patient-derived organoids (PDOs): Maintain tumor heterogeneity and microenvironment cues
- Immunocompetent models: Include relevant immune populations
- 3D culture systems: Better mimic tissue architecture and nutrient gradients
Therapeutic Strategies & Reagents
What therapeutic approaches target DTP epigenetic vulnerabilities?
Combination therapies that target both bulk tumor cells and DTP populations show the most promise. The reversibility of epigenetic modifications makes them particularly attractive drug targets [17] [18].
Research Reagent Solutions:
Table 4: Essential Reagents for Targeting DTP Epigenetic Mechanisms
| Reagent Category | Specific Examples | Function/Application | Key Considerations |
|---|---|---|---|
| Epi-drug Inhibitors | Tazemetostat (EZH2i), RO6870810 (BETi), Vorinostat (HDACi) | Target specific epigenetic regulators | Use combination approaches to prevent adaptation |
| MET Inhibitors | TGF-β pathway inhibitors, RTK inhibitors | Reverse EMT plasticity | Context-dependent effects |
| Metabolic Modulators | OXPHOS inhibitors, glycolysis inhibitors | Target DTP energy metabolism | Monitor compensatory pathways |
| PROTAC Degraders | BET-PROTACs, HDAC-PROTACs | Selective protein degradation | Optimize dosing schedules |
| Differentiation Agents | Retinoids, epigenetic primers | Force DTPs out of quiescence | Sequential therapy timing |
Protocol 3: Epi-drug Combination Screening
Materials Required:
- DTP-enriched cell populations
- Epigenetic drug library (HDACi, BETi, EZH2i, DNMTi)
- Viability and apoptosis assays
- Senescence biomarkers (SA-β-gal, γH2AX)
- Drug efflux pump inhibitors
Methodology:
- Primary Screening: Test single agents and combinations in DTP-enriched cultures
- Mechanistic Validation: Assess target engagement (western, qPCR), chromatin changes (ChIP)
- Functional Outcomes: Measure colony formation, tumorsphere formation, drug withdrawal recovery
- In Vivo Validation: Use PDX models with biomarker readouts
Troubleshooting Guide:
- Rapid resistance to single agents: Implement rational combinations from outset
- Poor in vivo efficacy: Consider pharmacokinetic issues, optimize dosing schedule
- Toxicity concerns: Explore intermittent dosing or lower doses in combinations
Future Directions & Advanced Applications
How can AI and multi-omics advance DTP targeting?
The convergence of high-throughput omics technologies and Artificial Intelligence (AI) is revolutionizing drug repositioning strategies, offering new precision tools to identify histone-targeted therapies for solid tumors [17]. AI-driven multi-omics integration is reshaping therapeutic opportunities by uncovering novel drug–target–patient associations with unprecedented accuracy [17].
Emerging Approaches:
- Computational drug repurposing: Leverage known safety profiles of existing drugs for new epigenetic applications
- Patient stratification biomarkers: Identify epigenetic signatures predictive of DTP formation
- Dynamic epigenetic monitoring: Track minimal residual disease through liquid biopsies
What are the key unanswered questions in DTP biology?
Critical research gaps include:
- How do DTPs relate to other cancer cell states (CSCs, senescent cells)?
- What mechanisms govern DTP emergence, persistence, and reactivation?
- How do organ-specific macroenvironments shape DTP behaviors?
- Can we develop reliable biomarkers for clinical detection and monitoring?
The integration of AI, multi-omics, and targeting of chromatin remodelers may herald a transformative shift in cancer management, bridging the gap between biological insights and therapeutic innovation to address the challenge of DTP-driven treatment resistance and relapse.
Frequently Asked Questions (FAQs)
Q1: What are the primary molecular mechanisms that contribute to metabolic heterogeneity in bacterial persister populations? Metabolic heterogeneity in persister populations is driven by several key mechanisms:
- Stochastic Gene Expression: Noise in the expression of metabolic enzymes and global regulators leads to cell-to-cell variation in metabolic states, even in isogenic populations [21] [4].
- Alarmone (p)ppGpp Signaling: This central stress response alarmone triggers a global reprogramming of transcription, downregulating proliferative processes like ribosome synthesis and upregulating stress survival pathways, which can vary between cells [22] [21] [23].
- Toxin-Antitoxin (TA) Module Activation: Under stress, labile antitoxins are degraded, allowing stable toxins to inhibit essential processes like translation and replication, inducing a dormant, persistent state [24].
- Asymmetric Partitioning: During cell division, cellular components like protein aggregates or transcription factors can be asymmetrically distributed, leading to immediate metabolic differences in daughter cells [4].
Q2: How do ppGpp signaling mechanisms differ between major bacterial classes like Proteobacteria and Firmicutes? The molecular mechanisms of ppGpp signaling are unexpectedly diverse [22]:
- In Proteobacteria (e.g., E. coli): ppGpp directly binds to two sites on RNA polymerase (RNAP), often in concert with the transcription factor DksA, to allosterically regulate hundreds of genes [22].
- In Firmicutes (e.g., Bacillus subtilis): ppGpp indirectly regulates transcription by binding to and inhibiting enzymes involved in GTP synthesis and salvage. This repression of cellular GTP levels indirectly inhibits transcription from promoters that use GTP for initiation, such as those for rRNA [22].
Q3: What is the functional relationship between (p)ppGpp and Toxin-Antitoxin systems in persister formation? (p)ppGpp and TA systems are interconnected components of the stress response network that promote persistence.
- Stringent Response Activation: Nutrient starvation and other stresses trigger a sharp increase in (p)ppGpp levels, initiating the stringent response [22] [21].
- TA System Regulation: The (p)ppGpp-mediated stress signal can lead to the activation of specific TA modules. For instance, in some Firmicutes, ppGpp directly allosterically regulates the transcription repressor PurR, which controls purine biosynthesis genes [22]. Furthermore, the stringent response leads to a general shutdown of translation and a reduction in ATP levels, which can prevent the synthesis of labile antitoxins and promote their degradation, thereby freeing toxins to induce growth arrest and persistence [21] [24].
Q4: Beyond persister formation, what other physiological roles do TA systems play in bacterial pathogens? TA systems are multifunctional and contribute significantly to bacterial pathogenesis through several roles [24]:
- Biofilm Formation: Chromosomally encoded TA modules are involved in the development and maintenance of biofilms, which protect bacteria from antibiotics and host immune responses [24].
- Anti-Phage Defense: Through abortive infection, some TA systems are activated in phage-infected cells, leading to altruistic cell death before the phage can replicate, thus protecting the bacterial population [24].
- Stabilization of Genetic Elements: Plasmid-encoded TA systems function as "addiction modules" via post-segregational killing, ensuring the plasmid is inherited by daughter cells [24].
Troubleshooting Guides
Issue: Low or Inconsistent Persister Cell Frequencies in Stationary-Phase Cultures
Potential Causes and Solutions:
| Potential Cause | Diagnostic Experiments | Recommended Solution |
|---|---|---|
| Inconsistent culture conditions | Monitor growth phase precisely using optical density (OD). Ensure consistent media, temperature, and shaking speed across experiments. | Standardize the inoculum, growth medium, and flask volume-to-medium ratio. Harvest cultures at the same specific OD for stationary-phase studies. |
| Inadequate stress induction | Quantify (p)ppGpp levels directly via mass spectrometry or use a fluorescent reporter to confirm stringent response activation [21]. | Use a defined starvation medium (e.g., for carbon, phosphate, or amino acids) to ensure robust and reproducible (p)ppGpp production. |
| Genetic drift or contamination | Streak for single colonies and re-validate genotype, especially for strains with mutations in stress response pathways (e.g., relA, spoT, dksA, rpoS). |
Use fresh colony inoculum from a frozen stock and perform periodic whole-genome sequencing to check for suppressor mutations. |
Issue: Failure to Detect TA System Toxin Activity or Protein Expression
Potential Causes and Solutions:
| Potential Cause | Diagnostic Experiments | Recommended Solution |
|---|---|---|
| Unstable antitoxin counteraction | Co-express the toxin and antitoxin genes from an inducible system. Use Western blotting with specific antibodies to check for toxin and antitoxin protein stability. | Use a tightly regulated, titratable expression system (e.g., arabinose- or rhamnose-inducible) for the toxin gene alone. Induce for short durations to prevent complete growth inhibition. |
| Insufficient stress for TA activation | Measure mRNA levels of the TA operon under different stress conditions (e.g., antibiotic treatment, nutrient starvation) using RT-qPCR. | Apply a defined stressor known to activate the specific TA system. For some systems, this may require adding an antibiotic that induces the SOS response or carbon starvation. |
| Toxin target specificity | Review literature on the toxin's known molecular target (e.g., mRNA, tRNA, ribosomes, DNA gyrase) [24]. | Use a specific biochemical assay to detect the toxin's activity. For example, for an mRNA interferase toxin, detect mRNA cleavage fragments. |
Key Data Tables
Table 1: ppGpp-Mediated Transcription Regulatory Mechanisms Across Bacterial Species
| Bacterial Species / Group | Mechanism of Action | Key Effector Molecules | Primary Transcriptional Outcome | Key Supporting Evidence |
|---|---|---|---|---|
| Escherichia coli (Proteobacteria) | Direct binding to RNA Polymerase | ppGpp, DksA, RNAP | Represses ~750 genes (e.g., rRNA, tRNA); Activates amino acid biosynthetic genes [22] | RNA-seq with ppGpp-binding site RNAP mutants [22] |
| Bacillus subtilis (Firmicutes) | Indirect regulation via GTP pool control | ppGpp, GTP biosynthesis enzymes (e.g., Gmk, HprT) | Represses rRNA promoters dependent on GTP for initiation [22] | Measurement of GTP levels and rRNA expression in ppGpp^0^ mutants [22] |
| Francisella tularensis | Direct modulation of a transcription activator | ppGpp, MglA, SspA | Activates virulence gene expression [22] | Characterization of tripartite transcription factor complex binding to RNAP [22] |
| Firmicutes | Allosteric regulation of a transcription repressor | ppGpp, PurR | Derepression of purine biosynthesis genes [22] | Biochemical assays showing ppGpp binding to PurR [22] |
Table 2: Classification and Functions of Major Toxin-Antitoxin System Types
| TA Type | Antitoxin Nature | Mechanism of Antitoxin Action | Toxin Target / Mechanism | Physiological Role(s) |
|---|---|---|---|---|
| I | Antisense RNA | Binds toxin mRNA, inhibiting translation [24] | Membrane integrity / pore formation [24] | Plasmid maintenance, persistence [24] |
| II | Protein | Binds and neutralizes toxin protein [24] | Translation (mRNA cleavage), DNA replication, Cell wall synthesis [24] | Persistence, biofilm formation, phage defense [24] |
| III | RNA | Binds and neutralizes toxin protein directly [24] | Translation inhibition [24] | Persistence, phage defense [24] |
| IV | Protein | Protects the toxin's target [24] | Cytoskeleton assembly (FtsZ) [24] | Persistence [24] |
| V | Protein | Cleaves toxin mRNA [25] | Membrane integrity [25] | Not specified in sources |
| VI | Protein | Tags toxin for proteolytic degradation [24] | Not specified in sources | Not specified in sources |
| VII | RNA | Possibly cleaves toxin mRNA [24] | tRNA acceptor stem inhibition [25] | Not specified in sources |
| VIII | Protein | OligoAMPylation of HEPN RNase [25] | tRNA pyrophosphorylation [25] | Growth control via alarmone signaling [25] |
Experimental Protocols
Protocol: Measuring (p)ppGpp Levels in Bacterial Cultures Using Thin-Layer Chromatography (TLC)
Objective: To quantitatively assess the intracellular levels of the alarmones ppGpp and pppGpp in response to stress, providing a direct readout of stringent response activation.
Principle: Bacterial cells are metabolically labeled with radioactive ^32^P-orthophosphate. Upon induction of stress, nucleotides are extracted and separated via polyethyleneimine (PEI)-cellulose TLC. The (p)ppGpp spots are visualized and quantified using a phosphorimager.
Materials:
- Strains: Wild-type and relevant mutant (e.g.,
relAorrelA spoT) bacterial strains. - Media: MOPS-based defined medium.
- Radioactive Isotope: ^32^P-orthophosphate.
- Stress Inducer: A defined amino acid analog (e.g., serine hydroxamate) or antibiotic.
- Extraction Solution: 2M formic acid, kept on ice.
- TLC Plate: PEI-cellulose F plastic-backed plates.
- Chromatography Solvent: 1.5 M KH~2~PO~4~, pH 3.6.
- Equipment: Phosphorimager or X-ray film.
Procedure:
- Grow and Label: Grow bacterial cultures to mid-exponential phase (OD~600~ ~0.4) in MOPS medium. Add ^32^P-orthophosphate (e.g., 50 μCi/mL) and incubate for at least one generation.
- Induce Stress: Split the culture. To one half, add the stress inducer (e.g., 500 μg/mL serine hydroxamate). The other half serves as an uninduced control.
- Quench and Extract: At specific time points (e.g., 0, 5, 15, 30 minutes post-induction), take 100 μL aliquots and transfer to microcentrifuge tubes containing 50 μL of ice-cold 2M formic acid. Incubate on ice for 30 minutes. Centrifuge at high speed for 5 minutes.
- Spot and Separate: Spot 2-5 μL of the supernatant onto a PEI-cellulose TLC plate. Air dry completely. Develop the TLC plate in the 1.5 M KH~2~PO~4~ solvent until the solvent front is near the top.
- Visualize and Quantify: Air dry the plate. Expose it to a phosphorimager screen overnight. Identify (p)ppGpp spots by comparing their migration to known standards (ATP typically runs near the front, while ppGpp and pppGpp migrate slower). Quantify the spot intensities and normalize to the GTP spot for each sample.
Troubleshooting:
- High Background: Ensure the TLC plate is completely dry before development. Use fresh chromatography solvent.
- No Signal: Confirm the activity of the ^32^P-orthophosphate. Verify that the stressor effectively induces the stringent response in your strain.
Protocol: Evaluating Toxin-Induced Persistence via Ectopic Expression
Objective: To determine the direct contribution of a specific TA system toxin to antibiotic persistence by quantifying the increase in persister cells upon toxin overexpression.
Principle: The toxin gene is cloned under a tightly regulated, inducible promoter. Induction of toxin expression halts the growth of most cells, inducing a dormant state. The culture is then treated with a high concentration of a bactericidal antibiotic. Only dormant, toxin-induced persisters will survive. After antibiotic removal and toxin repression, the surviving cells can resume growth.
Materials:
- Plasmids: pBAD-TOX (toxin gene under arabinose control), pBAD-Empty (control vector).
- Strains: An E. coli strain with the appropriate genetic background.
- Media: LB broth and LB agar plates.
- Inducers/Repressors: 20% L-Arabinose (inducer), 20% D-Glucose (repressor).
- Antibiotics: A bactericidal antibiotic (e.g., 100 μg/mL ampicillin or 10 μg/mL ofloxacin).
Procedure:
- Transform and Grow: Transform the pBAD-TOX and pBAD-Empty plasmids into the target strain. Grow overnight cultures from single colonies in LB with the appropriate antibiotic.
- Induce Toxin Expression: Dilute overnight cultures 1:1000 into fresh LB with antibiotic. Grow to mid-exponential phase (OD~600~ ~0.4). Split each culture into two. To one subculture, add arabinose (0.2%) to induce toxin expression. To the other, add glucose (0.2%) to keep the toxin repressed. Incubate for 1-2 hours.
- Apply Antibiotic Stress: Take a sample from each subculture, serially dilute it, and plate on LB-glucose plates to determine the total viable count (TVC) before antibiotic addition. To the remaining culture, add the bactericidal antibiotic. Incubate for 3-5 hours.
- Quantify Persisters: After antibiotic treatment, pellet the cells, wash twice with fresh LB to remove the antibiotic, and resuspend in LB-glucose to repress further toxin expression. Serially dilute and plate on LB-glucose plates to determine the number of surviving cells (persisters).
- Calculate Persister Frequency: Persister frequency = (TVC after antibiotic treatment / TVC before antibiotic treatment).
Troubleshooting:
- No Colonies After Induction: The toxin may be too potent. Titrate the inducer concentration (e.g., use 0.02%, 0.002% arabinose) or reduce the induction time.
- High Persistence in Control: Ensure the control plasmid does not contain a toxin gene. Use a fresh, high-concentration antibiotic stock to ensure killing of non-persister cells.
Signaling Pathway Diagrams
ppGpp Signaling Network
Toxin-Antitoxin System Regulation
The Scientist's Toolkit: Research Reagent Solutions
Table 3: Essential Reagents for Studying ppGpp, TA Systems, and Persister Metabolism
| Reagent / Tool | Category | Primary Function / Application | Key Considerations |
|---|---|---|---|
| Serine Hydroxamate | Metabolic Inhibitor | Induces amino acid starvation, leading to RelA-dependent (p)ppGpp synthesis. Useful for synchronized stringent response induction. | Concentration and duration of treatment must be optimized to avoid complete growth arrest. |
| pBAD/araC Expression System | Genetic Tool | Tightly regulated, titratable system for controlled overexpression of toxin genes or other stress-related proteins. | Use glucose for full repression. Titrate arabinose concentration to find a sub-lethal level for persistence studies. |
| Fluorescent (p)ppGpp Reporters | Biosensor | Allows single-cell, real-time monitoring of (p)ppGpp dynamics in live cells using flow cytometry or microscopy. | Reveals population heterogeneity in stress response activation [21]. |
| ^32^P-Orthophosphate | Radioactive Tracer | Metabolic labeling for direct detection and quantification of (p)ppGpp and other nucleotides via TLC. | Requires facilities for radioactive work. Provides the most direct measurement of alarmone levels. |
| Lon Protease Mutant Strains | Bacterial Strain | Used to study TA systems where the antitoxin is degraded by the Lon protease. Stabilizes the antitoxin, preventing toxin activation. | Helps confirm the role of specific protease pathways in TA module regulation. |
| ATP-based Cell Viability Assays | Metabolic Assay | Measures cellular ATP levels as a proxy for metabolic activity and viability, crucial for identifying dormant persister cells [21]. | More rapid than CFU plating but correlates with metabolic state rather than direct cultivability. |
| Fluorescent Protein Fusions (GFP/mCherry) | Reporter | Tags proteins of interest (e.g., antitoxins) or promoters to monitor expression localization and dynamics at single-cell level. | Enables visualization of heterogeneity and subcellular localization in real-time. |
| BI-9627 | BI-9627, MF:C16H19F3N4O2, MW:356.34 g/mol | Chemical Reagent | Bench Chemicals |
| AS601245 | AS601245, CAS:861411-83-8, MF:C20H16N6S, MW:372.4 g/mol | Chemical Reagent | Bench Chemicals |
Conceptual Foundations: Understanding Metabolic Multimodality
What is metabolic multimodality and why is it important in persister cell research?
Metabolic multimodality refers to the phenomenon where bacterial populations exhibit multiple distinct metabolic phenotypes despite genetic identity. In persister cell research, this is crucial because persister cells form a multi-drug tolerant subpopulation within an isogenic bacterial culture that can survive antibiotic treatment. These cells are genetically susceptible but temporarily reside in a slow- or non-growing state, and their formation is strongly influenced by metabolic state transitions. Metabolic multimodality enables bacterial populations to employ bet-hedging strategies, where some cells maintain active metabolism while others enter dormant states, ensuring population survival under fluctuating stress conditions like antibiotic exposure [7] [2].
How do unimodal and bimodal distributions relate to metabolic heterogeneity?
Unimodal distributions represent a continuum of protein levels or metabolic activity across a population, where cells have similar phenotypes with variations about the mean levels. In contrast, bimodal distributions feature two distinct subpopulations with different phenotypic states optimized for different environments. In bacterial persistence, populations often display bimodality, maintaining a small subpopulation of dormant cells in addition to normally growing cells. This bimodality can be advantageous in environments with distinct stress levels, allowing populations to maintain diversity without imposing high metabolic costs on all cells [26].
What key metabolic pathways are involved in persister cell formation?
Several core metabolic pathways and regulators play essential roles in persister formation:
- Toxin-Antitoxin (TA) Systems: These systems comprise a toxin that blocks essential cellular functions and an antitoxin that counteracts the toxin. They act as key regulators of persister formation, often activated by nutrient limitation and stress [7].
- Stringent Response and ppGpp: The alarmone ppGpp is a central mediator of the stringent response to nutrient starvation. It influences persister levels by activating TA systems and other regulatory factors, leading to metabolic downshift and growth arrest [7].
- Energy Metabolism: Enzymes involved in ubiquinone biosynthesis and the TCA cycle contribute to intracellular ATP pools, and their perturbation affects persister levels. Interestingly, both inhibition and enhancement of ATP synthesis have been shown to influence persister formation in different contexts [7].
- Central Carbon Metabolism: Studies using 13C-isotopolog profiling have demonstrated active glycolysis, TCA cycle, and pentose phosphate pathway in Staphylococcus aureus persisters challenged with antibiotics, indicating these pathways remain active but potentially redirected in some persister types [7].
Table 1: Key Metabolic Pathways in Persister Formation
| Metabolic Pathway/Component | Role in Persister Formation | Experimental Evidence |
|---|---|---|
| Toxin-Antitoxin (TA) Systems | Induces growth arrest and dormancy in response to stress | Gene knockout studies show decreased persister levels [7] |
| Stringent Response (ppGpp) | Mediates response to nutrient starvation; activates TA systems | ppGpp overexpression increases antibiotic tolerance [7] |
| TCA Cycle & Energy Production | Generates ATP; modulates persistence through energy status | Mutants in sucB (TCA cycle) show altered persistence [7] |
| Proton Motive Force (PMF) | Maintains membrane potential for energy production | PMF disruption by TisB increases persister levels [7] |
Troubleshooting Guides: Common Experimental Challenges
How can I effectively isolate and study persister cell metabolism?
A major challenge in persister research is the natural heterogeneity of bacterial populations and the fact that antibiotics used to isolate persisters alter their naïve metabolic state. Furthermore, persisters typically represent only a small subpopulation, making it difficult to distinguish their metabolism from non-persisters [7].
Solution: Implement specialized isolation and analysis techniques:
- Use lytic antibiotics or unstable GFP-variants to separate persister and non-persister cells before metabolic analysis [7].
- Apply 13C-isotopolog profiling to track metabolic fluxes in persister populations. This technique involves feeding 13C-labeled substrates and analyzing labeling patterns in metabolic intermediates to deduce relative pathway activities without measuring absolute metabolite concentrations [7].
- Utilize phenotype microarrays combined with fluorescent dyes to assay reductase activity as a proxy for overall metabolic activity [7].
Why does my population show unimodal instead of bimodal distributions in stress response?
The emergence of bimodal versus unimodal distributions depends on environmental conditions. Bimodality is typically favored in environments that alternate between two distinct stress levels (e.g., low and high stress), while unimodality becomes more beneficial when there is noise in the environment or multiple intermediate stress conditions [26].
Solution:
- Carefully control environmental parameters to create well-defined alternating conditions if bimodality is desired.
- If studying natural environments where unimodality predominates, focus on characterizing the breadth and shape of the unimodal distribution, as a broader distribution can still enhance population survival in fluctuating conditions [26].
- Consider that unimodal distributions may be a more straightforward bet-hedging strategy for surviving in realistic, noisy environments with multiple stress levels [26].
How can I integrate multi-omics data to understand metabolic heterogeneity?
The volume and heterogeneity of multi-omics data (transcriptomics, proteomics, metabolomics) can be challenging to synthesize into actionable insights [27].
Solution: Implement an integrated systems biology approach:
- Use Genome-Scale Metabolic Models (GSMMs) as a framework for integrating multi-omic data. GSMMs provide a mechanistic foundation that bridges genotype and phenotype by incorporating prior biological knowledge [28].
- Apply multimodal machine learning to analyze combined omics datasets. Machine learning can deconstruct biological complexity and extract relevant patterns from heterogeneous data [27] [28].
- Employ tools like the Automated Recommendation Tool (ART) that leverage machine learning to provide predictive models and recommendations for future experiments based on multi-omics data [27].
What methods can characterize metabolic states in persister subpopulations?
Solution: Deploy single-cell or population-level methodologies:
- Single-cell RNA sequencing reveals cellular heterogeneity and relationships between tumor microenvironment and drug resistance in persistent cell populations [29].
- Flux Balance Analysis (FBA) generates metabolic fluxes based on growth rate maximization assumptions, which can serve as a foundation for predicting proteomics and metabolomics data [27].
- Class Activation Maps (CAMs) technology visualizes features in pathological samples associated with specific metabolic or immune states, helping correlate spatial organization with functional states [29].
Experimental Protocols: Key Methodologies
Protocol: 13C-Isotopolog Profiling for Persister Metabolic Flux Analysis
Purpose: To identify active metabolic pathways in persister cells by tracing labeled carbon atoms through metabolic networks [7].
Reagents and Equipment:
- 13C-labeled carbon source (e.g., 13C-glucose)
- Appropriate antibiotic for persister selection
- Quenching solution (cold methanol)
- Metabolite extraction buffers
- Gas chromatography-mass spectrometry (GC-MS) or LC-MS system
- Data analysis software for isotopolog distribution
Procedure:
- Grow bacterial culture to desired growth phase (stationary phase cultures typically have higher persister levels).
- Challenge culture with appropriate antibiotic to kill non-persisters.
- Harvest persister cells by centrifugation and washing.
- Resuspend persisters in medium containing 13C-labeled carbon source.
- Incubate for specific time intervals to allow metabolite incorporation.
- Quench metabolism rapidly with cold methanol.
- Extract intracellular metabolites.
- Analyze metabolite extracts using GC-MS or LC-MS.
- Determine isotopolog distributions (mass distributions due to 13C incorporation).
- Map isotopolog patterns to metabolic pathway activities.
Expected Results: Stationary phase S. aureus persisters challenged with daptomycin showed active biosynthesis of amino acids with labeling patterns indicating active glycolysis, TCA cycle, and pentose phosphate pathway [7].
Protocol: Flux Balance Analysis with Multi-omics Integration
Purpose: To predict metabolic fluxes and generate biologically plausible multi-omics data for testing algorithms and computational tools [27].
Reagents and Equipment:
- Genome-scale metabolic model (e.g., iJO1366 for E. coli)
- COBRApy toolbox or similar constraint-based modeling software
- Omics Mock Generator (OMG) library for synthetic data generation
- Computing environment (Python/Jupyter notebooks)
Procedure:
- Formulate the FBA optimization problem to maximize biomass production:
- Maximize Vbiomass
- Subject to: Σj Sij Vj = 0 (mass balance)
- lbj ≤ Vj ≤ ub_j (flux constraints)
- Set exchange reaction constraints based on experimental conditions.
- Solve the linear programming problem to obtain flux distributions.
- Generate time series data by running batch simulations:
- For each time point, run FBA
- Update extracellular metabolite concentrations based on exchange fluxes
- Continue until carbon source is exhausted
- Derive proteomics data assuming protein expression is linearly related to fluxes.
- Generate metabolomics data assuming metabolite concentrations are proportional to sum of absolute incoming and outgoing fluxes.
Expected Results: The OMG library produces synthetic multi-omics data including fluxes, proteomics, and metabolomics that are biologically plausible though computationally generated, useful for testing analysis pipelines [27].
Signaling Pathways and Metabolic Networks
Figure 1: Metabolic Signaling in Persister Formation
Research Reagent Solutions
Table 2: Essential Research Reagents for Metabolic Multimodality Studies
| Reagent/Tool | Function | Application Examples |
|---|---|---|
| 13C-labeled substrates | Tracing metabolic fluxes through pathways | Isotopolog profiling to identify active pathways in persisters [7] |
| COBRApy toolbox | Constraint-based reconstruction and analysis of metabolic networks | Flux Balance Analysis for predicting metabolic fluxes [27] |
| Omics Mock Generator (OMG) | Generates synthetic multi-omics data based on metabolic models | Testing algorithms and computational tools without expensive experimental data [27] |
| Automated Recommendation Tool (ART) | Machine learning library for predictive biology | Recommending next strain designs based on multi-omics data [27] |
| Experiment Data Depot (EDD) | Open source repository for experimental data and metadata | Storing and managing multi-omics experimental data [27] |
| Class Activation Maps (CAMs) | Visualizing features in images that drive AI decisions | Identifying pathological features associated with metabolic states [29] |
Advanced Tools and Techniques for Profiling and Targeting Metabolic States
In the study of bacterial infections, a significant challenge lies in understanding and eradicating persister cells—a subpopulation of genetically susceptible bacteria that enter a transient, slow-growing or dormant state to survive antibiotic treatment [2] [7]. These cells are a primary cause of chronic and recurrent infections, as they exhibit phenotypic heterogeneity, meaning individual cells within a clonal population can exist in diverse metabolic states even under identical environmental conditions [4] [30]. This metabolic heterogeneity is now recognized as a fundamental bet-hedging strategy, ensuring that some cells survive unforeseen stresses, and poses a major obstacle for effective therapeutic interventions [4] [2].
Addressing this challenge requires advanced analytical techniques capable of probing metabolism at the single-cell level. This technical support center focuses on three pivotal methodologies: fluorescent biosensors for real-time monitoring of metabolites and pathways in live cells; Nanoscale Secondary Ion Mass Spectrometry (NanoSIMS) for mapping isotopic enrichment with ultra-high spatial resolution; and isotopolog profiling for tracing metabolic fluxes within central carbon metabolism. The following sections provide detailed troubleshooting guides, experimental protocols, and reagent solutions to empower researchers in deploying these powerful tools to dissect the metabolic enigma of persister cells.
Core Analytical Techniques: Principles and Workflows
The table below summarizes the key characteristics of the three primary single-cell metabolic analytics techniques.
Table 1: Comparison of Core Single-Cell Metabolic Analytical Techniques
| Technique | Key Principle | Spatial Resolution | Metabolic Information | Key Advantage | Primary Limitation |
|---|---|---|---|---|---|
| Fluorescent Biosensors | Couples metabolite concentration to a fluorescent output [4] | Diffraction-limited (~200 nm) | Real-time dynamics of specific metabolites (e.g., ATP, c-di-GMP) [30] | Compatible with live-cell imaging and high-throughput flow cytometry [4] [30] | Requires genetic manipulation; limited to a few analytes simultaneously [4] |
| NanoSIMS | Sputters sample surface with primary ions to generate secondary ions for mass spectrometry [31] | ~50 nm [32] [33] | Elemental and isotopic composition (e.g., 13C/12C, 15N/14N) [34] [32] | Ultra-high spatial resolution; can be combined with stable isotope labeling and other microscopy techniques [34] [31] | Requires high vacuum, chemical fixation; measures atoms, not intact molecules [34] |
| Isotopolog Profiling | Tracks incorporation of 13C from labeled nutrients (e.g., glucose) into metabolic intermediates [7] | Bulk population or, recently, single-cells via coupling to NanoSIMS | Relative fluxes through metabolic pathways (e.g., glycolysis, TCA cycle) [7] | Provides quantitative flux data for entire metabolic networks [7] | Traditionally a bulk technique; single-cell version requires complex sample preparation and analysis [34] |
Visualizing Workflows and Pathways
The following diagrams outline the general workflows for key experiments and the central signaling pathways involved in persistence.
Frequently Asked Questions (FAQs) & Troubleshooting
General Experimental Design
Q: My persister population is extremely rare. How can I ensure I am analyzing true persisters and not just resistant mutants?
A true persister, when resuscitated, will generate a population that is as susceptible to the antibiotic as the original parent strain [2] [7]. After isolating surviving cells following antibiotic treatment, you must regrow them in fresh medium without antibiotic and re-check their susceptibility. The regrown culture should have a Minimum Inhibitory Concentration (MIC) identical to the original, pre-treatment population. An elevated MIC indicates the presence of resistant mutants, which should be excluded from persister-specific metabolic studies [2].
Q: What is the best way to isolate persisters for downstream metabolic analysis like isotopolog profiling?
This is a major technical challenge, as the isolation method itself can alter the persister's metabolic state. Using lytic antibiotics (e.g., β-lactams) that kill growing cells but leave persisters intact is a common strategy [7]. For flow cytometry-based sorting, unstable GFP variants expressed under growth-promoting promoters can be used to distinguish and sort non-fluorescent, non-growing persisters from the larger, fluorescent, growing population [30]. Critically, any isolation protocol should be validated and completed as quickly as possible to minimize changes to the persister metabolome.
Biosensor-Specific Issues
Q: The fluorescence signal from my FRET-based ATP biosensor is weak and noisy. What could be wrong?
First, verify the sensor's expression and health of your cells. Ensure the biosensor is expressed from an appropriate, well-characterized plasmid or chromosomal locus. Check for cell lysis or stress, which can deplete ATP and cause a low signal [30]. Second, optimize your imaging conditions. Confirm that your microscope lasers and filters are correctly aligned for the specific donor and acceptor fluorophores. High noise can result from photobleaching; reduce laser power and exposure time, or use an oxygen-scavenging system in your imaging medium to mitigate this. Finally, ensure you are using the correct emission ratio calculation, as this ratiometric measurement is less sensitive to changes in biosensor concentration than single-wavelength intensity [30].
Q: How many different cell types or metabolic states can I track at once using fluorescent biosensors?
The number is limited by the spectral overlap of fluorophores. In a standard confocal microscope setup, you can typically distinguish 3-4 biomarkers simultaneously plus a nuclear counterstain [34]. To overcome this, "multi-reporter" constructs have been developed that use combinatorial labeling and sequential imaging to expand the number of distinguishable targets [30]. For instance, different RNA transcripts can be visualized in the same cell using sequential rounds of multiplexed FISH (par-seqFISH) [30].
NanoSIMS-Specific Issues
Q: My NanoSIMS analysis shows poor counting statistics for 13C, making it hard to detect enrichment above natural abundance. How can I improve this?
This is a common issue, especially when looking for small enrichments [34]. Several factors can be addressed:
- Increase Labeling: Use a higher enrichment of the stable isotope (e.g., [U-13C] glucose) and/or extend the labeling time to incorporate more tracer into the biomass.
- Optimize Sputtering: Ensure the sample is adequately implanted with Cs+ from the primary ion beam, as this is required for good ionization yield [34]. Using Scanning Electron Microscopy (SEM) for correlation, rather than Transmission Electron Microscopy (TEM), leaves more material available for sputtering and can improve results [34].
- Acquisition Time: Increase the measurement time per pixel to collect more ions, though this requires a trade-off with total analysis area and time.
Q: I can see the isotopic ratio in my data, but how do I know which subcellular compartment I'm measuring?
This requires correlative microscopy [34]. The power of NanoSIMS is fully realized when combined with other imaging modalities. You must first image your sample with a technique that provides organelle-level structural context, such as:
- Confocal Microscopy: If using fluorescent antibodies, to identify cell types [34].
- Electron Microscopy (EM): To provide the high-resolution contrast needed to identify membranes, mitochondria, and other organelles [34] [31]. These correlative images are then overlain with the NanoSIMS isotope map to pinpoint the location of the isotopic enrichment.
Isotopolog Profiling-Specific Issues
Q: My 13C-labeling pattern from a persister sample is inconsistent. What are potential sources of heterogeneity?
Inconsistency can stem from two main sources:
- Technical Heterogeneity: Inadequate separation of persisters from non-persisters before analysis. If your sample is contaminated with a significant number of normal cells, their dominant metabolic signal will mask the persister-specific signature [7].
- Biological Heterogeneity: Persisters themselves are a metabolically diverse continuum, comprising both completely dormant (Type I) and slow-growing (Type II) cells [2] [7]. It is therefore expected that subpopulations of persisters will exhibit different metabolic fluxes and thus different labeling patterns. This is not noise, but real biological information that may require single-cell techniques like NanoSIMS to resolve [34] [7].
Essential Research Reagent Solutions
The table below catalogs key reagents and their critical functions in single-cell metabolic studies of persisters.
Table 2: Key Research Reagents for Single-Cell Metabolic Analytics
| Reagent / Tool | Function | Example Application | Key Considerations |
|---|---|---|---|
| Non-depleting Fluorescent Antibodies [34] | In vivo labeling of specific cell surface markers (e.g., CD68 for macrophages) for cell type identification. | Identifying tumour-associated immune cells in a complex microenvironment for subsequent NanoSIMS analysis [34]. | Must recognize an extracellular epitope; limited by the number of spectrally distinct fluorophores. |
| Stable Isotope Labels (e.g., [U-13C] Glucose, 15N-Glutamine) [34] [7] | Tracer compounds to track nutrient uptake and utilization through metabolic pathways. | Studying the incorporation of glucose-derived carbon into specific cell types in murine tumour models [34]. | Chemical fixation can cause loss of soluble components; NanoSIMS only measures atoms, not molecular context [34]. |
| Genetically Encoded Biosensors (e.g., QUEEN, iATPSnFR, Riboswitch-based) [30] | Real-time reporting of specific intracellular metabolite levels (e.g., ATP, c-di-GMP) in live cells. | Quantifying heterogeneity in energy status across a clonal population under antibiotic stress [30]. | Requires genetic tractability; can perturb native protein function or localization. |
| Click Chemistry Probes (e.g., OPP, FUNCAT) [31] [30] | Labeling of nascent macromolecules (proteins, peptidoglycan) for visualization of biosynthesis rates. | Measuring single-cell translation rates in Gram-positive bacteria during antibiotic treatment [30]. | May not be compatible with all bacterial species (e.g., OPP with Gram-negatives). |
| Toxin-Antitoxin System Mutants [2] [7] | Genetic models to dissect molecular mechanisms linking stress response to persistence. | Elucidating the role of HipA-mediated ppGpp synthesis or TisB-mediated PMF reduction in persister formation [7]. | Effects can be strain and condition-dependent. |
Mathematical Modeling of Metabolic Fluxes and Heterogeneity Origins
The Scientist's Toolkit: Research Reagent Solutions
The following table details key reagents and materials essential for conducting experiments in metabolic flux analysis and investigating metabolic heterogeneity in persister cells.
| Item Name | Function/Explanation |
|---|---|
| Uniformly Labeled [U-¹³C] Glucose | A tracer substrate used in ¹³C-MFA to track carbon atoms through central metabolic pathways like glycolysis and the TCA cycle, enabling flux quantification [35]. |
| ¹³C-Labelled Tracers (e.g., ¹³C-CO₂, ¹³C-NaHCO₃) | Labeled substrates used to study specific metabolic routes or autotrophic carbon fixation pathways [35]. |
| Genetically Encoded Metabolite Biosensors | Tools coupling concentrations of a specific metabolite (e.g., ATP, amino acids) to a quantitative fluorescent output, allowing assessment of metabolic heterogeneity via live cell imaging or flow cytometry [4]. |
| Mass Spectrometry (MS) Instrumentation | The gold standard technique for versatile and quantitative metabolite assessment. It is used to measure labeling patterns in ¹³C-MFA and, in forms like NanoSIMS, to study metabolic heterogeneity at single-cell resolution [35] [4]. |
| Nuclear Magnetic Resonance (NMR) Spectroscopy | A technique used in carbon-labeled experiments to identify and quantify isotope distribution in metabolites, providing complementary data to MS [35]. |
| Anti-Persister Compounds (e.g., Pyrazinamide) | Drugs used to target and kill dormant bacterial persisters. Pyrazinamide is a canonical example crucial for shortening tuberculosis therapy [2]. |
| XL228 | XL228, CAS:952306-27-3, MF:C22H31N9O, MW:437.5 g/mol |
| JTV-519 hemifumarate | JTV-519 hemifumarate, MF:C54H68N4O8S2, MW:965.3 g/mol |
Frequently Asked Questions (FAQs)
Q1: What is the core difference between metabolic flux analysis (MFA) and flux balance analysis (FBA)?
- A: MFA is typically a smaller-scale model focused on the central carbon metabolism (e.g., glycolysis, TCA cycle). It can be supported by experimental data from stable isotope tracers to determine in vivo metabolic fluxes [35].
- A: FBA is a older, mathematical approach that uses a large-scale model of the entire metabolism (up to thousands of reactions). It is a predictive in silico model that assumes a metabolic steady state but does not typically use experimental tracer data [35].
Q2: Why is ¹³C the most common stable isotope used in fluxomics?
- A: ¹³C is universally present in all bioorganic molecules. Furthermore, its natural relative abundance (about 1.11%) is high compared to other stable isotopes like ²H or ¹âµN, making it highly suitable for tracing carbon atoms through metabolic networks [35].
Q3: What are the primary molecular origins of metabolic heterogeneity in an isogenic bacterial population?
- A: Metabolic heterogeneity arises from several mechanisms:
- Molecular Noise: Stochastic (random) variations in the transcription and translation of metabolic enzymes lead to cell-to-cell differences in enzyme abundance and, consequently, metabolite levels [4].
- Positive Feedback Loops: Regulatory architectures where a metabolic product enhances its own production can, under molecular noise, push cells into multiple stable states with distinct metabolic phenotypes (multimodality) [4].
- Asymmetric Partitioning: During cell division, low-copy-number cellular components like certain transcription factors or large enzyme complexes can be unevenly distributed between daughter cells, leading to inherited differences in metabolic activity [4].
Q4: How do "persister" cells differ from "antibiotic-resistant" cells?
- A: Persister cells are genetically drug-susceptible but exist in a transiently quiescent or slow-growing state, which allows them to survive antibiotic exposure without genetic mutation. Once the antibiotic is removed, they can regrow and remain sensitive to the drug [2].
- A: Antibiotic-resistant cells have acquired genetic mutations (or genes) that allow them to grow in the presence of the antibiotic, for example, by enzymatically inactivating the drug or modifying the drug's target site [2].
Experimental Protocols & Workflows
Protocol for ¹³C-Metabolic Flux Analysis (¹³C-MFA)
This is a standard workflow for determining metabolic fluxes at the isotopic steady state [35].
- Pre-culture and Steady-State Setup: Grow cells in a non-labeled medium until a metabolic steady state is achieved, where all metabolic fluxes remain constant over time.
- Introduction of Tracer: Replace the medium with one containing a ¹³C-labeled substrate (e.g., [U-¹³C] glucose).
- Cell Cultivation: Continue cultivation until the isotopic steady state is reached. This is when the isotope labeling patterns in intracellular metabolites become static. Note: This can take several hours to a day for mammalian cells [35].
- Rapid Quenching and Metabolite Extraction: Quickly quench metabolic activity (e.g., using cold methanol) and extract intracellular and extracellular metabolites.
- Sample Analysis: Analyze the labeling patterns (isotopomer distribution) of the metabolites using Mass Spectrometry (MS) or NMR Spectroscopy [35].
- Computational Modeling and Flux Estimation: Input the measured labeling data and extracellular flux rates (e.g., substrate uptake, product secretion) into a computational model of the metabolic network. Software tools (e.g., INCA, OpenFLUX) are used to find the set of intracellular fluxes that best fit the experimental data [35].
Workflow for 13C-MFA at Isotopic Steady State
Protocol for Investigating Metabolic Heterogeneity in Persisters
This protocol outlines a combined approach to study cell-to-cell metabolic variation in a persister population.
- Persister Induction: Expose a stationary-phase bacterial culture or a biofilm to a high concentration of a bactericidal antibiotic (e.g., ampicillin or ciprofloxacin) for several hours. This will kill the growing cells and enrich for the non-growing, tolerant persisters [2].
- Persister Isolation and Washing: Wash the culture thoroughly to remove the antibiotic. The surviving persisters can be collected for analysis [2].
- Single-Cell Metabolic Assessment (Choose One):
- Option A (Biosensors): Use a genetically encoded fluorescent biosensor (e.g., FRET-based or transcription-factor-based) to monitor the levels of a specific metabolite (e.g., ATP) in single, live cells via microscopy or flow cytometry [4].
- Option B (NanoSIMS): Pulse-label the persister population with a stable isotope (e.g., ¹âµN or ¹³C). Then, use Nanoscale Secondary Ion Mass Spectrometry (NanoSIMS) to achieve high-resolution imaging and quantification of the isotope incorporation in individual cells, revealing heterogeneity in metabolic activity [4].
- Data Analysis and Correlation: Analyze the single-cell data (fluorescence intensity or isotope ratio) to determine the distribution of metabolic activity across the population. Correlate this heterogeneity with survival outcomes or other phenotypic traits.
Troubleshooting Guides
Table: Common ¹³C-MFA Issues and Solutions
| Problem | Possible Causes | Suggested Solutions |
|---|---|---|
| Poor Fit of Model to Data | Incorrect metabolic network reconstruction; failure to reach true isotopic steady state; measurement errors. | Verify network stoichiometry; confirm isotopic steady state with time-course measurements; check instrument calibration and sample processing [35]. |
| Low Signal-to-Noise in MS Data | Insufficient cell biomass; low enrichment of ¹³C label; metabolite degradation during extraction. | Increase culture scale; optimize labeling time and tracer concentration; optimize quenching/extraction protocol for metabolite stability [35]. |
| Inability to Resolve Specific Fluxes | Network gaps around certain metabolites; lack of measurements for key extracellular fluxes. | Perform complementary experiments with different tracer molecules (e.g., [1,2-¹³C] glucose); ensure accurate measurement of uptake and secretion rates [35]. |
Table: Challenges in Persister Metabolic Heterogeneity Studies
| Problem | Possible Causes | Suggested Solutions |
|---|---|---|
| Low Persister Yield | Incorrect antibiotic concentration or exposure time; insufficient stationary-phase culture. | Titrate antibiotic to find minimal killing concentration (e.g., 99.9% kill); ensure culture is in true stationary phase for Type I persister induction [2]. |
| High Technical Noise in Single-Cell Measurements | Biosensor response time too slow; photobleaching in microscopy; low counting statistics in NanoSIMS. | Use faster-responding biosensors (e.g., FRET-based or RNA aptamers); optimize imaging conditions; ensure adequate measurement time per cell in NanoSIMS [4]. |
| Difficulty Linking Heterogeneity to Mechanism | The observed heterogeneity is a consequence, not a cause, of persistence; multiple overlapping mechanisms. | Combine metabolic measurements with genetic tools (e.g., knockouts of putative persistence genes) to establish causal relationships [4] [2]. |
Connecting Heterogeneity to Persistence: A Conceptual Workflow
Understanding how metabolic heterogeneity contributes to bacterial persistence requires integrating the tools and protocols above. The following diagram outlines a logical framework for this investigation.
Linking Metabolic Heterogeneity to Persister Formation
Lineage Tracing and Barcoding to Map Pre-Existing versus Induced Persister States
Frequently Asked Questions (FAQs)
Q1: What is the core difference between "pre-existing" and "induced" persister states in the context of metabolic heterogeneity?
A1: Pre-existing persisters are phenotypic variants that exist stochastically in a population prior to drug treatment. These cells often arise from spontaneous metabolic heterogeneity, such as stochastic fluctuations in enzyme expression leading to subpopulations with different metabolic activities (e.g., slow-growing, acetate-secreting cells vs. fast-growing, CO2-secreting cells) [36]. In contrast, induced persisters are a distinct state triggered directly by environmental stress, such as antibiotic exposure, which can cause a coordinated metabolic shift, for example, toward fatty acid oxidation or antioxidant upregulation, as a survival response [37] [15]. The relationship between metabolic heterogeneity and these persister states is summarized in the table below.
Table 1: Characteristics of Pre-Existing vs. Induced Persister States
| Feature | Pre-Existing Persisters | Induced Persisters |
|---|---|---|
| Origin | Spontaneous, stochastic variation in isogenic populations [36] | Triggered by external stressors (e.g., therapy, nutrient limitation) [15] |
| Primary Driver | Non-genetic, phenotypic heterogeneity [37] | Adaptive response to lethal stress [15] |
| Metabolic State | Can be deeply dormant or slow-cycling [2] | Often involves a programmed metabolic shift (e.g., to fatty acid oxidation) [37] |
| Therapeutic Implication | Population is pre-armed for survival; requires targeting dormant cell mechanisms | Population is dynamically adapting; requires disrupting adaptive pathways |
Q2: How can lineage tracing experimentally distinguish between these two origins?
A2: Lineage tracing techniques, particularly those using high-complexity expressed barcodes, allow researchers to track the fate of individual cell lineages over time. By applying these tools, one can determine if persisters that survive treatment regrow from lineages that were already slow-cycling or metabolically distinct before treatment (pre-existing), or if they arise from many different lineages that underwent a uniform adaptive response after treatment (induced) [37]. For instance, the "Watermelon" system uses lentiviral barcoding to simultaneously trace a cell's clonal origin and its proliferative state, revealing that cycling and non-cycling persisters can originate from distinct lineages with pre-programmed transcriptional and metabolic states [37].
Q3: What are the most common technical challenges when performing single-cell persister recovery assays?
A3: Key challenges and their solutions are outlined in the table below.
Table 2: Troubleshooting Common Issues in Persister Assays
| Problem | Potential Cause | Solution |
|---|---|---|
| No persister plateau is reached in time-kill assays | Antibiotic concentration is too low or treatment duration is insufficient. | Confirm the Minimal Inhibitory Concentration (MIC) and use an antibiotic concentration of at least 10x MIC. Perform a time-kill assay first to determine the treatment duration needed to eliminate susceptible cells [38]. |
| High background growth in recovery phases | Inadequate antibiotic removal or carryover. | Ensure proper dilution (often 1:1000 or greater) and washing steps after antibiotic treatment to prevent carryover [38]. |
| Excessive variability between replicates | Inconsistent culture conditions or cell preparation. | Standardize growth media, incubation times, and cell harvesting methods. Use OD measurements corrected to a McFarland standard for consistent inoculum preparation [38]. |
| Failure to detect rare persister subpopulations | Insufficient analytical sensitivity or sampling depth. | Employ single-cell resolution methods like time-lapse microscopy or high-complexity barcoding to capture rare, transient states [37] [38]. |
Q4: Why is metabolic heterogeneity a critical factor in persister cell research, and how can it be measured?
A4: Metabolic heterogeneity means that not all persisters are in the same dormant state; they exist in a continuum of metabolic activity, from deeply quiescent to slow-cycling [2]. This diversity is critical because different metabolic states (e.g., reliance on glycolysis vs. fatty acid oxidation) may require different eradication strategies [37] [39]. For example, in cancer, cycling persisters upregulate antioxidant programs and shift to fatty acid oxidation, making them vulnerable to disruption of these specific pathways [37]. Measurement techniques include:
- Spatial Metabolomics: Techniques like MALDI mass spectrometry imaging (MALDI-MSI) can map the spatial distribution of metabolites within a tumor or bacterial biofilm, identifying distinct metabolic tumor subpopulations (MTSs) and quantifying heterogeneity using indices like Simpson's diversity index [39].
- Flow Injection Mass Spectrometry (FI-MS): Allows for simultaneous detection of intracellular metabolites and strain-specific protein barcodes, linking metabolic phenotype to genotype in a high-throughput manner [40].
- Single-Cell RNA Sequencing (scRNA-seq): Can infer metabolic states by revealing the transcriptional programs of individual persister cells, showing coexistence of different phenotypic states within a population [15].
Experimental Protocols
Protocol 1: Determining the Minimal Inhibitory Concentration (MIC) and Time-Kill Curve for Persister Isolation
This protocol is fundamental for establishing the conditions to isolate a pure persister population [38].
Key Resources:
- Culture Media: Lysogeny broth (LB) or other appropriate medium.
- Antibiotic Stock Solution: Prepared in sterile milli-Q water or as recommended (e.g., 10 mg/mL for amikacin). Filter-sterilize.
- Equipment: 96-well plates, spectrophotometer, incubator shaker.
Procedure:
- Susceptibility Test (MIC Determination):
- Correct the optical density (OD625) of an overnight bacterial culture to 0.08-0.1 in 10 mM MgSO4 to achieve a turbidity equivalent to a 0.5 McFarland standard (~1.5 x 10^8 cells/mL).
- Dilute this suspension 1:200 in fresh medium to get ~5 x 10^5 cells/mL.
- Add 150 µL of the inoculum mixture to columns 1-11 of a 96-well plate. Use column 12 for a negative control (medium only).
- In column 1, add 150 µL of inoculum mixed with antibiotic at 2x the highest concentration you wish to test.
- Perform a two-fold serial dilution from column 1 to column 10.
- Column 11 serves as a positive growth control (inoculum, no antibiotic).
- Incubate the plate for 16-20 hours at the appropriate temperature.
- Measure the OD595. The MIC is the lowest antibiotic concentration that inhibits growth, defined as an OD value below 10% of the positive control [38].
- Time-Kill Assay (Persister Plateau):
- Treat a culture with a high concentration of antibiotic (e.g., ≥10x MIC).
- At regular time intervals, take samples, wash or dilute extensively to remove the antibiotic, and plate on drug-free solid medium to enumerate viable Colony Forming Units (CFUs).
- Plot the log(CFU) over time. The initial rapid kill phase will be followed by a slower decline or a plateau—this represents the persister population. The duration to reach this plateau is your required treatment time for subsequent persister experiments [38].
Protocol 2: Lineage Tracing with High-Complexity Barcodes using the "Watermelon" System
This methodology enables the simultaneous tracking of clonal origin, proliferative status, and transcriptional state of persister cells [37].
Key Resources:
- Barcoding Library: A high-complexity lentiviral library (e.g., Watermelon library) containing expressed barcodes.
- Target Cells: Cancer cell line of interest (e.g., EGFR-mutant NSCLC).
- Drugs: The therapeutic agent being studied (e.g., targeted therapy like EGFR inhibitors).
Procedure:
- Library Transduction: Infect your target cell population at a low Multiplicity of Infection (MOI) with the lentiviral barcode library to ensure each cell receives a unique, heritable genetic barcode.
- Expansion and Treatment: Expand the transduced population to establish stable lineages. Treat the population with the drug of interest for a duration determined from your time-kill curve.
- Sorting and Analysis:
- Use Fluorescence-Activated Cell Sorting (FACS) to separate the heterogeneous persister population into subpopulations of interest based on reporters (e.g., cycling vs. non-cycling).
- Recover genomic DNA and RNA from the sorted populations.
- Use high-throughput sequencing to read out the DNA barcodes, which reveal clonal lineage.
- Perform single-cell RNA sequencing (scRNA-seq) on the same populations to reveal transcriptional programs.
- Data Integration: Correlate the clonal barcode information with the transcriptional and phenotypic data. This allows you to determine if, for example, all cycling persisters emerged from a specific set of pre-existing lineages with a distinct metabolic signature (e.g., upregulated antioxidant genes) [37].
Diagram 1: Watermelon System Workflow for tracing persister lineages.
Research Reagent Solutions
Table 3: Essential Tools for Lineage Tracing and Persister Research
| Reagent / Tool | Function | Example & Notes |
|---|---|---|
| High-Complexity DNA Barcode Library | Uniquely labels individual cells, allowing clonal fate to be tracked over time. | Watermelon Lentiviral Library [37]: Expressed barcodes enable simultaneous lineage and state tracing. |
| Fluorescent Reporter Constructs | Reports on cell state (e.g., proliferation, stress) in live cells. | FUCCI (Fluorescent Ubiquitination-based Cell Cycle Indicator): Distinguishes cycling from non-cycling (persister) cells. |
| Site-Specific Recombinase Systems | Provides permanent, heritable genetic labeling for lineage tracing in vivo. | Cre-loxP and Dre-rox: Can be used for sparse labeling or multicolour confetti systems to visualize clonal dynamics [41]. |
| Protein-Based Barcodes | Enables high-throughput identification of strains and simultaneous metabolomic profiling. | Ubiquitin-based Barcodes [40]: Readable by mass spectrometry (FI-MS), allowing parallel strain ID and metabolite measurement. |
| Mass Spectrometry Imaging (MSI) | Spatially resolves metabolic heterogeneity within tissue or biofilm contexts. | MALDI-FT-ICR MS [39]: Maps metabolite distributions and identifies metabolic tumor subpopulations linked to survival. |
Signaling Pathways and Metabolic Networks in Persister Formation
Understanding the molecular pathways that define persister states is key to developing targeted interventions. The following diagram integrates key mechanisms from both cancer and bacterial models to show the logical flow from stress to persister formation.
Diagram 2: Core pathways in persister cell formation.
High-Throughput Screening for Anti-Persister Compounds and Synergistic Combinations
Core Concepts: Persister Cells and Screening Fundamentals
What are persister cells and why are they a problem in drug screening?
Answer: Persister cells are dormant, non-growing phenotypic variants found within genetically susceptible bacterial populations. They are not genetically mutant but exhibit transient, high-level tolerance to conventional antibiotics that target active cellular processes like cell wall synthesis, DNA replication, and protein synthesis. Their dormant nature means they do not metabolize drugs effectively, allowing them to survive treatment and cause chronic, relapsing infections [42] [43]. In screening, this poses a fundamental problem: traditional High-Throughput Screening (HTS) assays are biased toward identifying compounds that inhibit growing bacteria, causing them to miss agents that kill this dormant subpopulation [44].
How does metabolic heterogeneity impact persister cell research?
Answer: Metabolic heterogeneity refers to the significant cell-to-cell variation in metabolite levels and metabolic activity within an isogenic bacterial population, even under identical environmental conditions [4]. This heterogeneity is a fundamental driver of the persister phenotype.
- Bet-Hedging: The population ensures some cells (persisters) survive a future stress, like antibiotic exposure, by maintaining metabolic variability.
- Screening Challenge: This variation means a persister population is not uniform. A compound that kills one persister sub-type might be ineffective against another, complicating the identification of universally effective anti-persister therapies. Screening assays must therefore be designed to account for this spectrum of metabolic states [4].
What is the basic principle of High-Throughput Screening (HTS) for anti-persister compounds?
Answer: HTS utilizes robotics, data processing software, and sensitive detectors to rapidly test thousands of compounds for a desired biological activity [45]. For anti-persister drug discovery, the core principle is to shift from growth-inhibition assays to assays that measure direct killing of non-growing, antibiotic-tolerant bacteria. This requires specific protocols, such as maintaining cells in a starved state to enrich for and stabilize the persister phenotype during screening [44].
Troubleshooting Experimental Protocols
How do I generate a high-concentration, stable population of persister cells for screening?
Problem: Low yield or instability of the persister population during assay setup, leading to high background noise and false negatives.
Solution: Utilize a carbon-free starvation protocol to stabilize the dormant phenotype [44]. Protocol: Generating Staphylococcus aureus Persisters for HTS
- Culture Preparation: Grow a stationary-phase culture of S. aureus.
- Key Step - Starvation: Transfer the stationary-phase culture to a carbon-free minimal medium before antibiotic exposure. This prevents metabolic resuscitation and maintains the persister state.
- Antibiotic Selection: Expose the starved culture to a high concentration of ciprofloxacin (e.g., 50× MIC) for 24 hours. This kills all growing cells.
- Harvesting: Centrifuge the culture, wash the pellet to remove antibiotics, and resuspend in an appropriate buffer. The resulting population is highly enriched for persister cells that tolerate the antibiotic challenge [44].
Troubleshooting Tip: If persister yield is low, verify the growth phase of the pre-culture and ensure the absence of any carbon source in the minimal medium during antibiotic exposure.
Problem: Difficulty in distinguishing and tracking the small subpopulation of resuscitating persisters within a heterogeneous mixture of dead and VBNC cells.
Solution: Implement a flow cytometry-based protein dilution method [46]. Protocol: Flow Cytometry-Based Resuscitation Assay
- Genetic Engineering: Use an E. coli strain harboring a chromosomally integrated, IPTG-inducible fluorescent protein (e.g., mCherry) cassette.
- Labeling: Grow the pre-culture in the presence of IPTG to induce high fluorescence in all cells.
- Antibiotic Treatment: Treat the labeled culture with ampicillin. Growing cells will lyse and lose fluorescence, while persisters and VBNC cells remain intact and fluorescent.
- Resuscitation and Detection: Wash away the antibiotic and IPTG, then resuspend cells in fresh media. Analyze by flow cytometry over time.
- Interpretation: Resuscitating persisters will dilute their fluorescent protein as they divide, appearing as a subpopulation with decreasing fluorescence intensity. VBNC cells will retain high, constant fluorescence but will not divide [46].
Troubleshooting Tip: Include a no-antibiotic control to establish the baseline fluorescence decay profile for normal growing cells. Ensure the flow cytometer is calibrated for consistent fluorescence measurement.
What are the established methods for quantifying synergy in antibiotic combinations?
Problem: How to determine if two drugs act synergistically against persister cells, rather than just additively.
Solution: Employ standardized reference models and indices to quantify synergy [47]. Protocol: Checkerboard Assay and Synergy Calculation
- Checkerboard Setup: In a 96-well plate, serially dilute Antibiotic A along the rows and Antibiotic B along the columns.
- Inoculation: Inoculate each well with a standardized bacterial suspension (~10^5 CFU/mL).
- Incubation and Analysis: Incubate the plate and determine the Minimum Inhibitory Concentration (MIC) for each antibiotic alone and in combination.
- Calculate FIC Index: The Fractional Inhibitory Concentration Index (FICI) is calculated as follows:
- FIC of Antibiotic A = (MIC of A in combination) / (MIC of A alone)
- FIC of Antibiotic B = (MIC of B in combination) / (MIC of B alone)
- FICI = FICA + FICB
- Interpretation:
Troubleshooting Tip: For persister studies, perform time-kill assays with synergistic combinations against stationary-phase cells, as a reduction in log(CFU) followed by a plateau is indicative of persister survival [48].
FAQ: Data Analysis and Interpretation
How should I handle artifacts and non-specific signals in qHTS data?
Answer: Implement a rigorous data analysis pipeline that integrates counter-screens.
- Identify Common Artifacts: These include compound auto-fluorescence, direct interaction with the assay reporter gene (e.g., luciferase inhibition), and general cytotoxicity, which can mimic or mask true on-target activity [49].
- Counter-Screens: Run all library compounds through additional assays to measure auto-fluorescence and cytotoxicity under identical conditions.
- Data Integration: Use a pipeline that evaluates the primary qHTS readout alongside counter-screen data. A signal in the primary assay that is explained by a signal in a counter-screen (e.g., cytotoxicity) should be discounted as a non-specific artifact [49].
What are the major strategies for controlling persister cells?
Answer: Strategies can be categorized into direct and indirect killing approaches, as summarized below [42].
Table 1: Major Persister Control Strategies
| Strategy | Mechanism of Action | Key Examples | Advantages/Limitations |
|---|---|---|---|
| Direct Killing | Targets growth-independent cellular structures. | ||
| Membrane Targeting | Disrupts cell membrane integrity, causes lysis. | XF-73, SA-558, synthetic peptides [42] | Advantage: Does not require metabolic activity. Limitation: Potential for off-target toxicity to host membranes. |
| Protease Activation | Activates uncontrolled protein degradation. | ADEP4 (activates ClpP protease) [42] | Advantage: Effective against dormant cells. Limitation: Resistance can develop. |
| Indirect Killing | Alters the physiological state of the persister cell. | ||
| Preventing Formation | Reduces entry into dormancy. | CSE inhibitors, H2S scavengers, nitric oxide [42] | Advantage: Prevents problem at source. Limitation: Requires precise understanding of formation pathways. |
| Resuscitation & Sensitization | Wakes persisters, making them susceptible to conventional antibiotics. | Metabolic disruptors, membrane permeabilizers [42] | Advantage: Leverages existing antibiotics. Limitation: Timing of antibiotic administration is critical. |
Essential Research Reagent Solutions
Table 2: Key Reagents for Anti-Persister HTS
| Reagent / Tool | Function in HTS | Key Considerations |
|---|---|---|
| Carbon-Free Minimal Medium [44] | Maintains persister cells in a dormant, starved state during screening to prevent regrowth and stabilize the phenotype. | Essential for generating a uniform, high-tolerance population. |
| Fluorescent Protein Expression System [46] | Enables real-time, single-cell tracking of persister resuscitation via flow cytometry (e.g., using a dilution method). | Allows differentiation between persisters and VBNC cells. |
| Genetically Encoded Metabolite Biosensors [4] | Reports on metabolite levels and dynamics in single cells, allowing correlation of metabolic state with persistence. | Crucial for investigating metabolic heterogeneity. |
| Membrane-Permeabilizing Agents [42] | Used in combination therapies to disrupt the persister cell membrane and facilitate uptake of co-administered antibiotics. | Examples: synthetic retinoids (CD437), PMBN. |
Workflow and Pathway Visualizations
What are persister cells?
Persister cells are a subpopulation of genetically drug-susceptible bacteria that exist in a quiescent (non-growing or slow-growing) state, enabling them to survive antibiotic exposure and other stress conditions. After stress removal, these cells can regrow while remaining susceptible to the same stress, distinguishing them from fully resistant bacteria. Persisters underlie the challenges of treating chronic and persistent infections, relapses after treatment, and biofilm-associated infections [2].
How does metabolic heterogeneity contribute to persistence?
Bacterial populations display significant metabolic heterogeneity even under identical environmental conditions. This variability arises from multiple mechanisms, including molecular noise in metabolic enzyme expression, positive feedback loops, and asymmetric partitioning of cellular components during cell division. This "bet-hedging" strategy ensures that some subpopulations will survive unexpected stress conditions, such as antibiotic exposure [4].
Key characteristics of persister cells:
- Metabolic diversity: Persisters exhibit different metabolic states, from complete quiescence to slow metabolism
- Persistence continuum: A hierarchy exists from "shallow" to "deep" persistence states
- Reversibility: Unlike genetic resistance, persistence is a transient, phenotypic state
- Relationship to VBNC: The deepest persisters can become viable but non-culturable (VBNC) [2]
Fundamental Principles of Metabolic Priming
What is metabolic priming?
Metabolic priming involves preconditioning cells by manipulating cellular metabolism to force persister cells out of their dormant state and into a metabolically active, vulnerable state. This technique has emerged as a valuable tool for studying cellular processes related to energy metabolism, particularly those associated with persister cell survival [50].
Why does metabolic priming work against persisters?
Contrary to the long-standing belief that persisters are completely metabolically dormant, recent evidence demonstrates that antibiotic persisters remain metabolically active and can adapt their transcriptome to enhance survival. Transcriptomic analysis of E. coli persisters shows consistent upregulation of specific genes following antibiotic exposure, indicating ongoing metabolic activity that can be exploited through priming strategies [51].
Troubleshooting Guides
FAQ: Why can't I consistently generate persister cells for my metabolic priming experiments?
Problem: Inconsistent persister cell yields across experiments.
Solution:
- Standardize growth conditions: Persister formation is highly dependent on growth phase. Late stationary phase cultures (24-48 hours) typically yield higher persister numbers, particularly type I persisters that are highly resilient [2] [20].
- Control metabolic pre-history: The metabolic state of the inoculum culture dramatically affects persister formation. Use consistent pre-culture conditions including medium composition, temperature, and shaking speed.
- Validate antibiotic killing kinetics: Perform time-kill curves to confirm the characteristic biphasic pattern where the majority of cells die rapidly while a small persister subpopulation survives.
- Check antibiotic concentration: Use bactericidal (not bacteriostatic) antibiotics at concentrations 5-10× MIC to ensure efficient killing of non-persister cells.
Table 1: Common Problems in Persister Generation and Solutions
| Problem | Possible Causes | Solution |
|---|---|---|
| Low persister frequency | Wrong growth phase, insufficient stress | Use late stationary phase cultures (24-48h), confirm stress with stress markers |
| No biphasic killing | Antibiotic concentration too low, wrong antibiotic class | Use cidal antibiotics at 5-10× MIC, verify MIC values regularly |
| High variability between replicates | Inconsistent inoculum, metabolic drift | Use single-colony inoculum, limit culture passages, control temperature precisely |
| Contamination | Antibiotic degradation, improper technique | Filter-sterilize antibiotics, use fresh stocks, verify sterility controls |
FAQ: How do I confirm that metabolic priming is actually altering persister cell metabolism?
Problem: Difficulty in verifying metabolic state changes in persister cells.
Solution:
- Direct metabolic measurements:
- Monitor oxygen consumption rate (OCR) as an indicator of oxidative phosphorylation. Primed cells typically show increased OCR [52].
- Measure ATP levels using luciferase-based assays. While some persisters may have lower ATP than growing cells, they maintain detectable levels that may change with priming [20].
- Transcriptomic analysis:
- Perform RNA sequencing on sorted persister populations before and after priming.
- Look for upregulation of energy metabolism genes (TCA cycle, electron transport chain) and downregulation of anabolic pathways [20].
- Functional assays:
- Use metabolic potentiators like aminoglycosides that only kill metabolically active cells. Successful priming should increase aminoglycoside susceptibility [20].
- Monitor resumption of growth after priming using automated growth curve analysis.
Experimental Protocol: Validating Metabolic Priming Through Respiration Changes
Materials:
- Persister cell population
- Fresh medium with priming compounds
- Oxygen consumption rate (OCR) measurement system (e.g., Seahorse XF Analyzer)
- Carbon source known to induce metabolism (e.g., succinate, mannitol)
Procedure:
- Generate persisters from late stationary phase cultures (48h) using standard methods.
- Isolate persisters by antibiotic selection and washing.
- Resuspend persisters in fresh medium with priming compounds.
- Measure baseline OCR.
- Add metabolic substrates and monitor OCR changes over 2-4 hours.
- Compare primed vs. unprimed persisters.
- Correlate OCR changes with increased antibiotic susceptibility.
Expected Results: Successfully primed persisters should show significantly increased OCR (potentially nearly doubling within 24h as shown in fibroblast studies) and become susceptible to killing by conventional antibiotics [52].
FAQ: What are the most effective metabolic targets for priming persister cells?
Problem: Identifying which metabolic pathways to target for effective priming.
Solution: Focus on these key metabolic pathways based on recent research:
Table 2: High-Value Metabolic Targets for Persister Priming
| Metabolic Target | Rationale | Example Priming Agents | Expected Outcome |
|---|---|---|---|
| CRP/cAMP signaling | Global regulator that redirects metabolism from anabolism to oxidative phosphorylation in persisters | cAMP analogs, carbon sources that activate cAMP production | Increased TCA cycle activity, enhanced proton motive force |
| TCA cycle | Essential for energy metabolism in persister survival | Succinate, malate, other TCA intermediates | Increased ATP production, enhanced aminoglycoside uptake |
| Electron transport chain (ETC) | Maintains membrane potential in persisters | Menaquinone precursors, terminal electron acceptors | Increased proton motive force, improved antibiotic penetration |
| ATP synthase | Critical for energy production in persistent cells | ADP/ATP ratio manipulation | Energy depletion or restoration depending on strategy |
| Stringent response | Regulates transition to dormant state | (p)ppGpp analogs, inhibitors of RelA/SpoT | Reversal of dormancy, resumption of growth |
The CRP/cAMP complex represents a particularly promising target, as it redirects persister cell metabolism from anabolism to oxidative phosphorylation, making them vulnerable to antibiotics [20].
Metabolic Priming Experimental Protocols
Core Protocol: CRP/cAMP-Mediated Metabolic Priming
Principle: The Crp/cAMP complex serves as a global metabolic regulator that redirects persister cell metabolism from anabolic pathways to oxidative phosphorylation, increasing their susceptibility to antibiotics [20].
Materials:
- Late stationary phase bacterial culture (48h)
- cAMP analogs (e.g., 8-bromo-cAMP, dibutyryl-cAMP)
- Carbon sources: succinate (10mM), mannitol (10mM), or other Crp/cAMP-inducing carbon sources
- Appropriate antibiotics for susceptibility testing
- Metabolic inhibitors as controls (e.g., sodium azide, cyanide)
Procedure:
- Persister isolation:
- Grow bacteria to late stationary phase (48h)
- Treat with bactericidal antibiotic (5-10× MIC, 3-5h)
- Wash 3× with sterile saline or buffer to remove antibiotic
- Confirm persister isolation by plating and colony counting
Metabolic priming:
- Resuspend persister cells in fresh medium containing:
- Experimental: 5mM cAMP analog + inducing carbon source
- Control 1: Inducing carbon source alone
- Control 2: Non-inducing carbon source
- Control 3: cAMP analog alone
- Incubate 1-2h at 37°C with aeration
- Resuspend persister cells in fresh medium containing:
Susceptibility testing:
- Treat primed persisters with target antibiotic
- Sample at 0, 1, 2, 4, 8, and 24h for viability counts
- Calculate log-reduction in viability compared to controls
Validation:
- Measure cAMP levels if possible
- Monitor gene expression of Crp/cAMP-regulated genes
- Assess metabolic activity via ATP levels or respiration rates
Expected Results: Persisters treated with both cAMP analog and inducing carbon source should show significantly enhanced killing (2-4 log reduction) compared to controls, indicating successful metabolic priming.
Protocol: Energy Metabolism-Targeted Priming
Principle: Persister cells maintain energy metabolism through TCA cycle, electron transport chain, and ATP synthase activity. Disrupting or hyperactivating these pathways can create vulnerability [20].
Materials:
- Persister cells isolated as above
- TCA cycle intermediates (succinate, fumarate, α-ketoglutarate)
- ETC manipulation compounds (menadione, cyanide, azide)
- ATP synthase inhibitors (oligomycin, DCCD)
- Aminoglycoside antibiotics for susceptibility testing
Procedure:
- Isolate persister cells as described above.
- Divide into treatment groups:
- TCA cycle activation: 10mM succinate + 10mM α-ketoglutarate
- ETC activation: 1mM menadione
- ATP synthase modulation: 10µM oligomycin
- Combined approach: TCA intermediates + menadione
- Negative control: Buffer only
- Incubate 1h at 37°C.
- Assess metabolic activation via:
- Oxygen consumption rate
- ATP levels
- Membrane potential dyes
- Challenge with aminoglycoside antibiotic (e.g., gentamicin 10× MIC).
- Determine viability over time.
Troubleshooting Notes:
- If priming fails, verify that your persister population is derived from late stationary phase.
- Test multiple carbon sources as effectiveness varies by bacterial species.
- Include controls for osmotic stress from compound additions.
Table 3: Research Reagent Solutions for Metabolic Priming Studies
| Reagent Category | Specific Examples | Function in Metabolic Priming | Key Considerations |
|---|---|---|---|
| cAMP signaling modulators | 8-bromo-cAMP, dibutyryl-cAMP, forskolin | Activate Crp/cAMP complex, shift metabolism to OXPHOS | Membrane permeability varies by analog; use at 1-5mM |
| Carbon source primers | Succinate, mannitol, fumarate, malate | Induce Crp/cAMP signaling, provide metabolic substrates | Effectiveness is species-dependent; test multiple sources |
| Metabolic inhibitors | Sodium azide, cyanide, oligomycin, 2,4-DNP | Disrupt energy metabolism, validate priming mechanisms | Use at sub-inhibitory concentrations for priming studies |
| Metabolic activity probes | Resazurin, CTC, TMRM, BCECF-AM | Measure metabolic activation, membrane potential, pH | Verify probe penetration in persisters; may require loading optimization |
| Energy status assays | BacTiter-Glo, ATPlite, NAD/NADH kits | Quantify ATP levels, energy charge, redox state | Compare to exponential phase controls for normalization |
| Gene expression tools | crp/cya deletion strains, CRP overexpression plasmids | Validate Crp/cAMP dependence in priming | Use multiple strains to confirm generalizability |
| Antibiotic potentiators | Aminoglycosides, fluoroquinolones | Kill metabolically active primed persisters | Use at sub-MIC concentrations to detect enhanced killing |
Visualization of Metabolic Priming Concepts
Metabolic Priming of Bacterial Persisters
CRP/cAMP Metabolic Regulation Network
Experimental Workflow for Metabolic Priming
Advanced Applications and Future Directions
How can I apply metabolic priming to my specific bacterial pathogen?
While much foundational work has been done in E. coli and M. tuberculosis, the principles of metabolic priming can be adapted to other pathogens:
- Identify conserved pathways: The CRP/cAMP system, TCA cycle, and ETC are highly conserved across bacterial species.
- Test species-specific carbon sources: Determine which carbon sources most effectively activate metabolism in your pathogen.
- Validate with genetic tools: Use knockout strains to confirm the necessity of specific pathways in priming efficacy.
- Adapt to infection models: Transition from in vitro to in vivo models to assess priming in physiologically relevant environments.
What are the emerging targets in metabolic priming?
Recent research has identified several promising directions:
- Combination with efflux pump inhibitors: Simultaneously increase metabolic activity and block antibiotic extrusion.
- Immunometabolic priming: Enhance immune cell activity alongside bacterial metabolic activation for dual targeting.
- Species-specific pathway targeting: Identify unique metabolic dependencies in pathogens like M. tuberculosis and P. aeruginosa.
- Diagnostic applications: Develop metabolic activation profiles as biomarkers for persistent infections.
The field continues to evolve as we better understand the complex metabolic heterogeneity within persister populations and develop more sophisticated strategies to exploit these vulnerabilities for therapeutic benefit.
Exploiting Unique Metabolites and Surface Antigens for Selective Targeting
This technical support center provides troubleshooting and methodological guidance for researchers focusing on the selective targeting of persister cell populations. Persisters are non-growing or slow-growing, genetically drug-susceptible cells that survive antibiotic exposure and other stresses, contributing to chronic and relapsing infections [2]. A key characteristic of these populations is metabolic heterogeneity—significant cell-to-cell variation in metabolic activity even within an isogenic population [4]. This heterogeneity enables "bet-hedging," ensuring that some subpopulations survive future stresses [4]. The strategic exploitation of unique metabolites and surface antigens that arise from this heterogeneity is a promising avenue for developing more effective therapies against persistent infections.
Foundational Knowledge: FAQs
FAQ 1: What are bacterial persisters and why are they a problem for treatment? Bacterial persisters are a subpopulation of cells that enter a dormant or slow-growing state within a larger, genetically identical population. They are not antibiotic-resistant mutants but survive antibiotic treatment due to their low metabolic activity. The core problem is that after antibiotic treatment is stopped, these persister cells can regrow, leading to relapse of the infection. They are a major culprit behind treatment failure in chronic and biofilm-associated infections, such as tuberculosis, recurrent urinary tract infections, and Lyme disease [2].
FAQ 2: What is metabolic heterogeneity and what causes it in bacterial populations? Metabolic heterogeneity refers to the cell-to-cell variation in metabolite levels and metabolic activity observed even in an isoclonal population of bacteria grown under uniform laboratory conditions [4]. Several molecular and cellular mechanisms drive this heterogeneity:
- Molecular Noise: Stochastic (random) variations in the transcription and translation of metabolic enzymes lead to differences in their abundance, which in turn affects metabolite levels [4].
- Positive Feedback Loops: Bistable systems, where a positive feedback loop pushes cells into one of two stable metabolic states, can create distinct subpopulations. The classic example is the E. coli lac operon [4].
- Asymmetric Partitioning: During cell division, cellular components like low-copy-number enzymes or transcription factors can be unevenly distributed to daughter cells, leading to immediate or generational differences in metabolic activity [4].
FAQ 3: How can we target persister cells if they are metabolically dormant? While persisters are often dormant, their dormancy is not absolute, and their unique metabolic state can be exploited. Strategies include:
- Targeting Metabolic Pathways: Identifying and disrupting low-level metabolic functions essential for persister survival or reactivation.
- Targeting Surface Antigens: Discovering unique surface proteins or other structures that are expressed on persister cells and using them as a handle for targeted delivery of antibacterial agents.
- Using Metabolic Biosensors: Employing genetically encoded tools to identify, isolate, and study metabolically distinct subpopulations for further analysis [4].
Methodologies and Experimental Protocols
This section provides detailed protocols for key experiments in persister cell research.
Protocol: Isolation and Characterization of Persister Cells
Objective: To obtain a pure population of persister cells from a stationary-phase culture and characterize their metabolic heterogeneity.
Materials:
- Bacterial culture (e.g., E. coli, S. aureus, M. tuberculosis)
- Appropriate liquid growth medium
- High-concentration antibiotic (e.g., 100x MIC of a fluoroquinolone or β-lactam)
- Phosphate-Buffered Saline (PBS), sterile
- Centrifuge and tubes
- Flow cytometer or cell sorter
Procedure:
- Grow Stationary-Phase Culture: Inoculate bacteria in liquid medium and incubate with shaking until the culture reaches stationary phase (typically 24-48 hours). The stationary phase is enriched for Type I persisters (induced by nutrient starvation) [2].
- Treat with High-Concentration Antibiotic: Add a high concentration of a bactericidal antibiotic to the culture. The exact concentration and treatment time must be optimized for each bacterial strain but typically lasts 4-6 hours. This step kills all growing cells, leaving only non-growing persisters [2].
- Wash and Re-suspend: Centrifuge the culture to pellet the cells. Carefully discard the supernatant containing the antibiotic. Wash the pellet twice with sterile PBS to remove all traces of the antibiotic. Finally, re-suspend the pellet in fresh PBS or medium.
- Characterize Metabolic Heterogeneity:
- Using Metabolic Biosensors: If available, use a strain expressing a genetically encoded FRET-based biosensor for a key metabolite (e.g., ATP). Analyze the cells via flow cytometry to reveal the distribution of metabolic states within the persister population [4].
- Using Dye-Based Assays: Stain the persister population with fluorescent dyes that report on metabolic activity (e.g., CTC for electron transport chain activity) and membrane potential. Flow cytometry analysis will show a heterogeneous profile, confirming the presence of subpopulations with varying metabolic states.
Troubleshooting:
- Low Persister Yield: Ensure the culture has truly entered stationary phase. Extend the incubation time or confirm growth has plateaued by measuring optical density.
- Contamination with Growing Cells: Verify the antibiotic concentration is sufficiently high (e.g., 100x MIC) and that the antibiotic is active. Consider using two different classes of antibiotics in succession.
Protocol: Targeted Metabolomic Analysis of Persister Populations
Objective: To quantitatively measure the levels of a defined set of metabolites from a purified persister cell sample.
Materials:
- Purified persister cell sample
- Metabolite extraction solvent (e.g., 80% methanol)
- Isotopically labeled internal standards for each target metabolite
- Liquid Chromatography-Mass Spectrometry (LC-MS) system with a triple quadrupole mass spectrometer
- Nitrogen gas
Procedure:
- Rapid Metabolite Extraction: Transfer the persister cell sample to a tube containing pre-chilled (-20°C) extraction solvent. The high solvent-to-sample ratio and low temperature instantly quench metabolic activity. Vortex vigorously for 1 minute.
- Add Internal Standards: Spike the sample with a known quantity of isotopically labeled internal standards (e.g., 13C- or 15N-labeled amino acids). These standards correct for variations in sample preparation and ion suppression during MS analysis [53].
- Pellet Debris: Centrifuge the sample at high speed (e.g., 16,000 x g) for 15 minutes at 4°C to pellet protein and cell debris.
- Collect Supernatant: Transfer the clear supernatant containing the metabolites to a new vial.
- Concentrate Sample: Evaporate the solvent under a stream of nitrogen gas. Re-constitute the dried metabolite pellet in a solvent compatible with the LC-MS analysis.
- LC-MS/MRM Analysis:
- Chromatography: Inject the sample onto the LC column to separate metabolites based on polarity.
- Mass Spectrometry: Use the triple quadrupole MS in Multiple Reaction Monitoring (MRM) mode. For each target metabolite, the first quadrupole (Q1) selects the specific precursor ion (parent mass), the second (Q2) fragments it, and the third (Q3) selects a unique fragment ion (product mass). This two-stage mass filtering provides high specificity and sensitivity for absolute quantification [53].
- Data Analysis: Quantify metabolites by comparing the peak areas of the target metabolites to the peak areas of their corresponding isotopically labeled internal standards. Use calibration curves for absolute quantification.
Troubleshooting:
- Poor Chromatography: Ensure the LC system is well-maintained and the column is not degraded. Optimize the mobile phase gradient for the metabolites of interest.
- High Background Noise: Check for contamination in solvents or tubes. Use high-purity (HPLC/MS-grade) solvents.
The Scientist's Toolkit: Research Reagent Solutions
Table 1: Essential Research Reagents for Investigating Persister Cell Metabolism and Targeting.
| Reagent/Category | Function/Description | Key Considerations |
|---|---|---|
| Genetically Encoded Biosensors (e.g., FRET-based) | Enable real-time monitoring of specific metabolite levels (e.g., ATP, NADH) in live, single cells [4]. | Crucial for revealing metabolic heterogeneity; requires genetic engineering of the target organism. |
| Mass Spectrometry Platforms | NanoSIMS: Provides subcellular resolution for imaging metabolic incorporation of stable isotopes [4]. LC-MS/MS: Gold standard for versatile and quantitative metabolite profiling from bulk samples [53] [54]. | NanoSIMS is excellent for spatial mapping but requires specialized sample preparation. LC-MS/MS is the workhorse for targeted metabolomics. |
| Isotopically Labeled Internal Standards | (e.g., 13C-glucose, 15N-glutamine). Used as internal spikes in metabolomics for absolute quantification and to trace metabolic flux in pathways [53]. | Essential for accurate quantification in targeted metabolomics to correct for matrix effects and ion suppression. |
| Cell-Penetrating Peptides (CPPs) | Oligopeptides that can deliver cargos (drugs, probes) across cell membranes. Can be engineered for targeted delivery [55]. | Can be modified with pH-sensitive or enzyme-cleavable linkers to achieve selective activation in the unique microenvironment of persisters [55]. |
| Antibiotics for Persister Isolation | Bactericidal antibiotics like fluoroquinolones and β-lactams, used at high concentrations (e.g., 100x MIC) to kill growing cells and enrich for persisters [2]. | The choice of antibiotic depends on the bacterial strain and its mode of action must target growing cells. |
| A-966492 | A-966492, MF:C18H17FN4O, MW:324.4 g/mol | Chemical Reagent |
| Serabelisib | Serabelisib, CAS:1428967-74-1, MF:C19H17N5O3, MW:363.4 g/mol | Chemical Reagent |
Data Presentation and Visualization
Table 2: Summary of Key Metabolomic and Phenotypic Heterogeneity Concepts.
| Concept | Description | Measurement Technique |
|---|---|---|
| Metabolic Heterogeneity | Cell-to-cell variation in metabolite levels and dynamics within an isoclonal population [4]. | Single-cell methods: FRET biosensors + Flow Cytometry, NanoSIMS [4]. |
| Type I Persisters | Non-growing, metabolically stagnant persisters induced by external stress (e.g., stationary phase) [2]. | Isolation via antibiotic treatment of stationary phase cultures [2]. |
| Type II Persisters | Slow-growing, metabolically slow persisters that arise spontaneously without external cues [2]. | More challenging to isolate; often studied via microfluidics and time-lapse microscopy. |
| Targeted Metabolomics | Measurement of a predefined set of chemically characterized metabolites. Provides absolute quantification [56] [53]. | LC-MS/MRM with isotopically labeled internal standards [53]. |
| Untargeted Metabolomics | Global analysis of all measurable metabolites in a sample, both known and unknown. Used for hypothesis generation [56] [54]. | NMR or high-resolution LC-MS; requires complex data processing [56]. |
Pathway and Workflow Visualizations
Diagram 1: Origins and Targeting of Metabolic Heterogeneity in Persisters
Diagram 2: Targeted Metabolomics Workflow for Persister Analysis
Overcoming Technical and Biological Challenges in Persister Research
Addressing the Transient and Rare Nature of Persister Cells in Experimental Workflows
FAQs and Troubleshooting Guides
FAQ 1: What are the defining characteristics of persister cells, and how do they differ from resistant or tolerant cells?
Answer: Persister cells are a small subpopulation of cells that survive bactericidal or chemotherapeutic treatments through transient, non-genetic mechanisms. Their key characteristic is reversible drug tolerance; when the treatment is removed and the cells are re-cultured, their progeny regain drug sensitivity.
The table below clarifies the critical distinctions between resistance, tolerance, and persistence.
Table 1: Distinguishing Resistance, Tolerance, and Persistence
| Feature | Antibiotic/Chemotherapy Resistance | Antibiotic/Chemotherapy Tolerance | Antibiotic/Chemotherapy Persistence |
|---|---|---|---|
| Definition | Inherited ability to grow in the presence of a drug [57] | Transient ability of the entire population to survive longer drug exposure [58] [57] | Transient ability of a subpopulation to survive drug exposure [59] [57] |
| Genetic Basis | Stable genetic mutations [2] | Can be genetic or non-genetic [57] | Non-genetic, phenotypic heterogeneity [2] [60] |
| Killing Curve | Monophasic, shifted MIC [57] | Monophasic, but slower killing (increased MDK99) [58] [57] | Biphasic, with a persistent subpopulation surviving [38] [58] [57] |
| Minimum Inhibitory Concentration (MIC) | Increased [58] [57] | Unchanged [58] [57] | Unchanged [57] |
FAQ 2: How can I reliably isolate and quantify persister cells given their low abundance?
Answer: Reliable quantification requires carefully designed time-kill assays and precise counting techniques. The core principle is to expose a culture to a high concentration of a bactericidal drug and monitor the decline in viable cells over time.
Experimental Protocol: Time-Kill Assay for Persister Quantification [38]
- Determine MIC: First, establish the Minimum Inhibitory Concentration (MIC) for the drug and bacterial strain/cancer model you are using [38].
- Apply Lethal Dose: Treat a culture with an antibiotic concentration significantly above the MIC (e.g., 10-100x MIC) to ensure rapid killing of non-persister cells [38] [58].
- Sample Over Time: At regular intervals, remove samples, wash to remove the drug, and plate for viable colony counts (CFUs).
- Identify the "Persister Plateau": The killing curve will show a rapid initial drop followed by a flattening plateau. The cell count at this plateau represents the persister subpopulation [38] [58].
Troubleshooting Tip: A common issue is the failure to observe a clear biphasic curve.
- Potential Cause: The drug concentration is too low or the treatment duration is insufficient, failing to kill all non-persister cells.
- Solution: Ensure the antibiotic concentration is sufficiently high (at least 10x MIC) and continue treatment until the kill curve stabilizes, indicating the "persister plateau" has been reached [38].
FAQ 3: The heterogeneity of persister cell states is a major research challenge. How can I account for this in my experimental design?
Answer: Metabolic and phenotypic heterogeneity is a fundamental feature of persister populations. Acknowledging this requires moving beyond bulk population analyses to single-cell or single-cell-informed techniques [59] [4].
- Embrace Single-Cell Technologies: Utilize methods like single-cell RNA sequencing (scRNA-seq) to characterize the diverse transcriptional states within a persister population. Studies in breast cancer and melanoma have shown that persisters with different phenotypic states (e.g., mesenchymal-like, luminal-like) can coexist [59].
- Incorporate Lineage Tracing: Combine molecular profiling with DNA barcoding to track the fates of individual cells and their progeny after treatment. This reveals how genetically identical cells diverge into different persister states [59].
- Monitor Long-Term Dynamics: Understand that persister states are not fixed. A cell's metabolic state and drug tolerance can fluctuate over time and in response to changing environmental conditions [2].
FAQ 4: What are the best practices for studying persister cell regrowth and relapse?
Answer: Studying regrowth requires monitoring cells after the removal of the drug stressor. Key parameters to track are recovery kinetics and heterogeneity in regrowth at the single-cell level.
Experimental Protocol: Assessing Single-Cell Persister Recovery [38]
- Eliminate Drug: After a time-kill assay, remove the antibiotic by washing and centrifugation or by diluting the culture into fresh, drug-free medium.
- Monitor Recovery: Use methods like spectrophotometry (OD measurements) to track population-level regrowth kinetics.
- Analyze Single-Cell Physiology: Employ flow cytometry or time-lapse microscopy to analyze heterogeneity in recovery. This can reveal subpopulations that resume growth immediately versus those that remain dormant for extended periods [38].
Troubleshooting Tip: Recovery results are inconsistent between replicates.
- Potential Cause: Inconsistent removal of the drug or failure to document the precise growth phase and environmental conditions of the pre-treatment culture, which heavily influence persister levels [38].
- Solution: Standardize the culture conditions (e.g., always use stationary-phase cultures if studying triggered persistence) and ensure drug removal is complete and consistent.
FAQ 5: What are the emerging strategies to target and eradicate persister cells?
Answer: The clinical goal is to identify "anti-persister" compounds that can kill this dormant subpopulation. Strategies include:
- Combination Therapies: Use standard-of-care drugs alongside agents that target persister-specific vulnerabilities. For example, in EGFR-mutant NSCLC, HDAC inhibitors can trigger caspase-independent cell death in DTPs that survive EGFR-targeted therapy [59].
- Targeting Dormancy Mechanisms: Develop drugs that disrupt the metabolic, epigenetic, or stress-response pathways that maintain the persister state (e.g., targeting the integrated stress response) [61] [60].
- Forcing Deeper Dormancy: A novel approach is to push persister cells into an even deeper, irreversible dormant state (a Viable But Non-Culturable state), preventing them from ever regrowing and causing relapse [58].
Experimental Protocols & Workflows
Core Protocol: A Systematic Workflow for Persister Cell Isolation and Characterization
The following diagram outlines a generalized experimental workflow for persister cell research, integrating steps from bacterial and cancer persister studies.
Key Experimental Considerations
- Standardization is Critical: Persister levels are highly sensitive to culture conditions (growth phase, medium, temperature). Maintain strict consistency for reproducible results [38] [62].
- Appropriate Controls: Always include an untreated control culture to account for natural cell death and normal growth dynamics.
- Confirm Reversibility: Verify that the isolated surviving cells are true persisters by demonstrating that the progeny of regrown cultures are as drug-sensitive as the original parental population [57].
The Scientist's Toolkit: Research Reagent Solutions
Table 2: Essential Reagents and Materials for Persister Cell Research
| Item | Function/Application | Key Considerations |
|---|---|---|
| Lysogeny Broth (LB) / Appropriate Cell Culture Medium | Standard culture medium for maintaining bacterial/cancer cell populations. | Medium composition can dramatically influence persister levels; use consistent batches [38]. |
| Bactericidal Antibiotics / Chemotherapeutic Agents | Primary selective agent for eliminating non-persister cells. | Use at concentrations significantly above the MIC (e.g., 10-100x). Confirm drug stability during assay [38] [58]. |
| Phosphate-Buffered Saline (PBS) or 10mM MgSOâ‚„ | Used for washing cells and diluting samples for viable plating. | Essential for effectively removing antibiotics before recovery phase assays [38]. |
| 96-well Plates & Breathable Membranes | Used for high-throughput MIC determination and time-kill assays. | Breathable membranes allow for aeration during prolonged incubation [38]. |
| Flow Cytometer with Cell Sorter | Analysis of population heterogeneity and isolation of specific persister subpopulations. | Enables sorting based on viability dyes, reporter constructs, or metabolic activity [4] [2]. |
| Single-Cell RNA Sequencing Kit | Profiling the transcriptional heterogeneity of persister populations. | Crucial for understanding the spectrum of cell states and identifying potential therapeutic targets [59]. |
| Incubation Monitoring System (e.g., CM20) | Automated, label-free monitoring of cell growth and confluency inside an incubator. | Reduces disturbance to cells, minimizes phototoxicity, and provides quantitative growth data for consistent passaging and recovery timing [63]. |
| Bizine | Bizine, MF:C18H23N3O, MW:297.4 g/mol | Chemical Reagent |
| Quinupristin mesylate | Quinupristin mesylate, MF:C54H71N9O13S2, MW:1118.3 g/mol | Chemical Reagent |
Conceptual Framework: Mechanisms and Therapeutic Targeting
The following diagram summarizes the key biological mechanisms that contribute to persister cell formation and survival, highlighting potential points for therapeutic intervention.
Distinguishing Metabolic Heterogeneity from Genetic Resistance Mechanisms
Fundamental Concepts: FAQs for the Researcher
FAQ 1: What is the core difference between genetic resistance and metabolic heterogeneity in the context of antibiotic persistence?
Answer: Genetic resistance is a heritable trait that enables bacteria to grow in the presence of an antibiotic, typically characterized by an increase in the Minimum Inhibitory Concentration (MIC). In contrast, metabolic heterogeneity refers to non-heritable, phenotypic variation within an isogenic population, leading to a subpopulation of cells (persisters) that survive antibiotic treatment without a change in MIC. Their survival is grounded in a transient, often dormant, physiological state [64] [2].
FAQ 2: How do persisters, which exhibit metabolic heterogeneity, differ from genetically resistant bacteria?
Answer: The distinctions are summarized in the table below.
| Feature | Genetic Resistance | Metabolic Heterogeneity (Persisters) |
|---|---|---|
| Heritability | Heritable and stable | Non-heritable and transient [64] |
| Effect on MIC | Increases MIC [64] | Does not alter MIC [64] |
| Mechanism | Genetic mutations (e.g., in drug target or efflux pumps) [64] | Phenotypic switch (e.g., dormancy, toxin-antitoxin modules, reduced metabolism) [2] [6] |
| Population Size | Entire population | Small subpopulation [64] |
| Role in Infection | Treatment failure due to growth | Relapse and chronic infections due to survival and regrowth [2] |
FAQ 3: What are the primary molecular mechanisms that drive metabolic heterogeneity and persister formation?
Answer: Multiple interconnected mechanisms can induce a dormant, persistent state, including:
- Toxin-Antitoxin (TA) Modules: Under stress, unstable antitoxins are degraded, allowing toxins to disrupt vital processes like translation and replication, inducing dormancy [2] [6].
- Stringent Response: Nutrient starvation triggers the accumulation of (p)ppGpp, a global alarmone that dramatically reprograms cellular metabolism away from growth and toward maintenance [2] [6].
- Metabolic Noise and Feedback: Stochastic (random) fluctuations in the expression of metabolic enzymes and positive feedback loops in metabolic networks (e.g., the Lac operon) can generate distinct metabolic states between identical cells [4].
Experimental Protocols & Troubleshooting
This section provides methodologies for key experiments and solutions to common problems.
Protocol: Isolation and Quantification of Persisters
Objective: To isolate and enumerate the persister subpopulation from a bacterial culture after antibiotic exposure.
Materials:
- Mid-log phase bacterial culture
- Suitable bactericidal antibiotic (e.g., ampicillin, ofloxacin)
- Phosphate-Buffered Saline (PBS)
- Cell culture centrifuge
- Automated cell counter or materials for serial dilution and plating
Methodology:
- Culture Standardization: Grow the bacterial strain to mid-log phase (OD600 ~0.4-0.6).
- Antibiotic Exposure: Treat the culture with a high concentration of the antibiotic (typically 10-100x MIC) for a defined period (e.g., 3-5 hours).
- Drug Removal: Centrifuge the sample, discard the supernatant containing the antibiotic, and wash the cell pellet twice with PBS.
- Viability Count: Resuspend the pellet in fresh media. Perform serial dilutions and spot plate on antibiotic-free agar plates. Alternatively, use an automated cell counter with viability staining.
- Calculation: The number of Colony Forming Units (CFUs) that regrow represents the persister population [2].
Troubleshooting Guide: Common Experimental Challenges
Problem: Inconsistent persister counts between replicates.
- Potential Cause: Inhomogeneous mixing during culture growth or antibiotic exposure.
- Solution: Ensure consistent and vigorous shaking during all incubation steps. Use biological replicates (n≥3) and report the mean and standard deviation [64].
Problem: No persisters are detected after treatment.
- Potential Cause: Antibiotic concentration is too high or exposure time is too long.
- Solution: Titrate the antibiotic concentration and duration of exposure. Use a time-kill assay to establish the killing kinetics and identify the point where the kill curve plateaus, indicating the persister subpopulation [2].
Problem: Inability to distinguish between slow growth and true persistence.
- Potential Cause: Regrowth from a dormant state can be misinterpreted.
- Solution: Use microscopy or flow cytometry with fluorescent dyes that report on metabolic activity (e.g., CTC for respiration) to confirm a metabolically dormant state prior to antibiotic addition [4] [65].
Data Interpretation: Quantitative Analysis
The following table summarizes key metabolic parameters that can distinguish between susceptible, resistant, and persistent cell states.
| Metabolic Parameter | Susceptible Population | Resistant Mutants | Persister Subpopulation |
|---|---|---|---|
| ATP Levels | High | High | Significantly reduced [4] [6] |
| Proton Motive Force (PMF) | High | High | Collapsed [6] |
| Respiratory Activity | High | Variable | Dormant or very low [6] |
| Central Carbon Metabolite Pools | Active and balanced | Altered but active | Imbalanced and heterogeneous [4] |
| Ribosome Content | High | High | Asymmetrically partitioned, often low [4] |
Therapeutic Strategies and the "Wake and Kill" Approach
A promising strategy to combat persisters is metabolite-driven metabolic reprogramming, often called the "wake and kill" approach [6]. This involves using specific metabolites to reactivate the dormant metabolism of persisters, thereby re-sensitizing them to conventional antibiotics.
The following diagram illustrates the core signaling pathways and regulatory relationships involved in persister cell formation and potential intervention points.
Diagram: Signaling pathways in persister formation and the "Wake and Kill" intervention strategy.
The Scientist's Toolkit: Essential Research Reagents
The table below lists key reagents and their applications for studying metabolic heterogeneity and persistence.
| Research Reagent / Tool | Primary Function | Application in Persistence Research |
|---|---|---|
| Fluorescent Biosensors (e.g., FRET-based) | Real-time monitoring of specific metabolite levels (e.g., ATP, NADH) in live cells [4]. | Quantifying metabolic heterogeneity at single-cell resolution using flow cytometry or live-cell imaging [4]. |
| Stable Isotope Tracers (e.g., ¹³C-Glucose) | Tracing atom fate through metabolic pathways (Stable Isotope-Resolved Metabolomics - SIRM) [65]. | Mapping active vs. inactive metabolic networks in persisters compared to normal cells [65]. |
| Metabolite Adjuvants (e.g., Pyruvate, Mannitol) | Serve as exogenous carbon sources to stimulate bacterial metabolism [6]. | Used in "wake and kill" strategies to resuscitate persisters and restore their sensitivity to aminoglycosides and other antibiotics [6]. |
| Viability Stains (e.g., CTC, CFDA) | Differentiating metabolically active from inactive cells. | Identifying and isolating the dormant persister subpopulation prior to molecular analysis [65]. |
| Grazoprevir | Grazoprevir|HCV NS3/4A Protease Inhibitor | Grazoprevir is a potent, second-generation NS3/4A protease inhibitor for hepatitis C virus (HCV) research. This product is for Research Use Only (RUO). Not for human or veterinary use. |
| Davercin | Davercin, CAS:11054-95-8, MF:C38H65NO14, MW:759.9 g/mol | Chemical Reagent |
Navigating the Reversibility and Dynamic State Transitions of Persisters
Frequently Asked Questions (FAQs)
Q1: What fundamentally distinguishes a persister cell from a resistant cell?
Persister cells are not genetically resistant mutants. They survive antibiotic or anticancer therapy through reversible, non-genetic adaptations that often involve a transient slowdown in metabolism or growth. Once the treatment pressure is removed, persisters can revert to a treatment-sensitive state and regrow. In contrast, resistant cells have acquired stable genetic mutations that allow them to grow in the presence of the drug, and this trait is heritable. The key distinction lies in the reversibility of the tolerant phenotype in persisters versus the stability of the resistant phenotype [66] [67].
Q2: Why is metabolic heterogeneity a critical factor in persister cell populations?
Even within an isogenic population, individual cells can exhibit significant variations in their metabolic states. This metabolic heterogeneity acts as a "bet-hedging" strategy for the population. When a sudden stress like antibiotic treatment occurs, a sub-population of cells may already be in a slow-growing or dormant metabolic state that coincidentally tolerates the drug. This pre-existing heterogeneity means the population doesn't need to "sense" the stress to adapt; a surviving fraction is already present [4]. In cancer, metabolic heterogeneity within tumors is linked to worse survival and can influence the local immune response, complicating treatment efforts [39].
Q3: What are the primary mechanisms that trigger the entry into a persister state?
Entry into the persister state can be stochastic (random) or induced by environmental stressors. Key triggers and mechanisms include:
- Stress Signaling: Nutrient limitation, oxidative stress, or DNA damage can activate stringent response pathways and toxin-antitoxin modules, leading to growth arrest [68] [67].
- Epigenetic Reprogramming: In cancer, drug-tolerant persisters (DTPs) often show reversible changes in histone modifications (e.g., by KDM5A demethylase or EZH2 methyltransferase) that alter chromatin structure and gene expression, promoting survival [66].
- Metabolic Rewiring: A shift from glycolysis to oxidative phosphorylation (OXPHOS) and fatty acid oxidation is common. This reduces reactive oxygen species (ROS) accumulation and supports survival in a low-energy state [66].
Q4: How can I experimentally isolate and study bacterial persister cells?
A standard method involves using a time-kill assay. You treat a stationary-phase bacterial culture with a high concentration of an antibiotic (typically 10x or more above the MIC) for a prolonged period. The majority of susceptible cells die, and the remaining viable cells, which can be quantified by plating and counting colony-forming units (CFUs), are considered the persister fraction [38]. The protocol below outlines the steps for assessing persister cell recovery.
Q5: What strategies are being explored to target and eradicate persister cells?
Since persisters are tolerant to conventional antibiotics that target growth, new strategies focus on growth-independent vulnerabilities:
- Direct Killing: Using membrane-targeting agents (e.g., cationic peptides, certain synthetic compounds) to disrupt cell integrity, or prodrugs like pyrazinamide that disrupt membrane energetics in dormant Mycobacterium tuberculosis [42].
- Preventing Persistence: Inhibiting pathways essential for entry into persistence, such as Hâ‚‚S biogenesis or quorum-sensing systems that regulate multicellular behaviors [42].
- Awakening and Killing: Forcing persisters to exit dormancy using metabolic stimulants (e.g., specific carbon sources, metabolites) to sensitize them to conventional antibiotics [42].
Troubleshooting Experimental Guides
Problem 1: Inconsistent Persister Cell Counts in Time-Kill Assays
Potential Causes and Solutions:
- Cause: Inaccurate determination of the Minimal Inhibitory Concentration (MIC).
- Solution: Precisely determine the MIC for your bacterial strain and antibiotic combination using a standardized broth microdilution method [38]. Re-check the MIC regularly.
- Cause: Antibiotic degradation or instability during the long treatment period.
- Solution: Confirm antibiotic stability under your experimental conditions (temperature, media). Consider replenishing the antibiotic if the treatment lasts more than 24 hours.
- Cause: Incomplete removal of the antibiotic before plating for CFU counts, leading to carryover effects.
- Solution: Perform adequate washing steps by centrifuging the cell culture and resuspending the pellet in fresh, antibiotic-free media or buffer. Use a sufficient volume and number of washes [38].
Problem 2: Failure to Induce or Detect Cancer Drug-Tolerant Persister (DTP) Cells
Potential Causes and Solutions:
- Cause: The drug concentration used is insufficiently lethal or exposure time is too short.
- Cause: The model system lacks the cellular heterogeneity present in tumors.
- Solution: Move beyond simple 2D cell lines. Use 3D culture systems, patient-derived organoids (PDOs), or in vivo models that better recapitulate the tumor microenvironment and its inherent heterogeneity, which is a breeding ground for DTPs [59].
- Cause: Analysis methods are not sensitive enough to detect a rare DTP population.
Experimental Protocol: Assessing Bacterial Persister Recovery Kinetics
This protocol, adapted from Wilmaerts et al., details the steps to obtain and analyze the recovery of bacterial persister cells at the single-cell level [38].
1. Determine Minimal Inhibitory Concentration (MIC)
- Prepare a two-fold dilution series of your antibiotic in a 96-well plate containing the bacterial inoculum.
- Incubate for 16-20 hours.
- The MIC is the lowest antibiotic concentration that completely inhibits visible growth (OD measurement) [38].
2. Perform Time-Kill Assay to Isolate Persisters
- Treat a stationary-phase bacterial culture with a high concentration of antibiotic (e.g., 10x MIC).
- Take samples at various time points, wash to remove the antibiotic, and plate serial dilutions to determine the number of viable persister cells (CFUs).
- Continue until the kill curve reaches a plateau, indicating the remaining population is enriched in persisters [38].
3. Monitor Persister Recovery
- Dilute the antibiotic-treated culture to a level where individual persister cells are physically separated.
- Incubate in fresh, antibiotic-free media and monitor the recovery of individual cells using time-lapse microscopy or by measuring bulk culture growth (OD) over time [38].
- Use flow cytometry with viability stains or metabolic dyes to assess the physiological states of the recovering cells.
Key Experimental Parameters for Common Bacteria
Table 1: Example parameters for persister assays with E. coli and amikacin.
| Parameter | Example for E. coli BW25113 & Amikacin [38] | General Consideration |
|---|---|---|
| Growth Phase | Stationary Phase | Persister frequency is often highest in stationary phase. |
| Antibiotic Conc. | 100 µg/mL (12.5x MIC) | Use at least 10x the MIC to ensure killing of non-persisters. |
| Treatment Duration | Until kill curve plateaus | Varies by strain/antibiotic; can be several hours to days. |
| Recovery Media | Lysogeny Broth (LB) | Use rich media to support the recovery of dormant cells. |
Research Reagent Solutions
Table 2: Essential reagents and their functions in persister cell research.
| Reagent / Tool | Function / Application | Key Details |
|---|---|---|
| HDAC Inhibitors(e.g., Entinostat) | Epigenetic Modulator | Reverses drug tolerance in cancer DTPs by altering chromatin accessibility; used in combination therapies [66]. |
| Membrane-Targeting Agents(e.g., XF-73, SA-558) | Direct Persister Killing | Disrupts bacterial cell membrane integrity, effective against dormant cells; some induce ROS generation [42]. |
| OXPHOS Inhibitors(e.g., IACS-010759) | Metabolic Disruptor | Targets the shifted metabolic state of cancer DTPs reliant on oxidative phosphorylation; in clinical trials [66]. |
| Hâ‚‚S Biosynthesis Inhibitors | Prevention of Persistence | Reduces persister formation in bacteria like S. aureus and P. aeruginosa by blocking a key defense pathway [42]. |
| FRET-based Metabolite Biosensors | Single-Cell Metabolic Analysis | Genetically encoded tools for real-time, dynamic monitoring of metabolite levels in individual live cells [4]. |
| NanoSIMS(Nanoscale Secondary Ion Mass Spectrometry) | Spatial Metabolomics | Provides high-resolution subcellular imaging of metabolic heterogeneity and nutrient uptake in microbial populations [4]. |
Visualizing Persister State Transitions and Key Pathways
The following diagrams illustrate the dynamic lifecycle of a persister cell and the core metabolic shifts that support its survival.
Persister Cell Lifecycle
Metabolic Shift in Persisters
Core Concepts and Troubleshooting
Frequently Asked Questions (FAQs)
Q1: What is the fundamental difference between a persister cell and a viable but non-culturable (VBNC) cell? A1: Both are dormant, stress-tolerant subpopulations, but a key operational difference lies in their ability to revive on standard culture media. Persister cells can be resuscitated and will start dividing again at normal growth rates once the stressor (e.g., an antibiotic) is removed, regenerating a population with a similar persister fraction [69]. In contrast, VBNC cells have transiently lost the ability to grow on standard culture media and require special complex media to regain culturability [69]. Some researchers argue that the VBNC state may not represent a separate phenotype and should be considered under the broader umbrella of persistence [69].
Q2: Why are persister cells particularly problematic in the context of intracellular bacterial pathogens (IBPs)? A2: Persister formation is linked to recalcitrant chronic infections caused by pathogens like Myobacterium tuberculosis and Chlamydia species [69]. These persistent IBPs have been found almost exclusively in vacuolar compartments (e.g., pathogen-containing vacuoles or inclusions) rather than in the host cell's cytosol [69]. This specific intracellular niche appears to offer a more favorable environment for entering the persistent state, which is poorly understood but may be connected to the unique metabolic environment within the vacuole.
Q3: How does cellular heterogeneity impact the study of persister cell populations? A3: Cellular heterogeneity means that an average measurement taken from a whole population can be misleading. A population may contain rare but functionally important subpopulations, like persisters, which are masked by the majority [70]. For instance, an ensemble measurement might suggest a graded response to a stimulus, while single-cell analysis could reveal an all-or-nothing commitment within individual cells [70]. Therefore, models based solely on population averages may not accurately represent the biology of any single cell, including persisters, and can hinder the development of accurate clinical models and effective treatments.
Q4: What are the main advantages of using 3D tumor models over traditional 2D cultures in drug screening? A4: 3D models (e.g., spheroids, organoids) more closely mimic the in vivo tumor environment. Compared to 2D monolayers, 3D cultures better retain the original tumor's genetic and phenotypic heterogeneity and incorporate crucial cell-cell and cell-matrix interactions that are absent in 2D [71]. Cells in 3D environments also show morphology, gene expression, and drug sensitivity profiles that are more physiologically relevant, which is critical as cells in 2D often have higher and less accurate proliferation rates and drug sensitivities [72]. This leads to more reliable data for predicting drug efficacy in clinical trials.
Troubleshooting Common Experimental Challenges
Table 1: Troubleshooting Guide for Model Systems
| Problem | Potential Cause | Suggested Solution |
|---|---|---|
| Low persister cell yield in in vitro assays. | Lack of appropriate metabolic stress trigger. | Induce a carbon source transition (diauxie); ensure the presence of the stringent response alarmone (p)ppGpp [73]. |
| Inconsistent results between laboratories when using Patient-Derived Cancer Cells (PDCCs). | Genetic and phenotypic drift in culture; loss of tumor heterogeneity. | Use lower-passage cells; transition from 2D to 3D culture models (spheroids, organoids) that better maintain original tumor characteristics [71]. |
| Poor formation or structural integrity of 3D tumor spheroids. | Suboptimal self-aggregation conditions; lack of necessary structural support. | Utilize scaffold-free methods like the hanging drop technique or nanoimprinted scaffolds to promote spheroid formation via self-aggregation [72]. |
| Failure to recapitulate key biofilm properties in in vitro models. | Oversimplified model unable to capture environmental heterogeneity (e.g., nutrient, oxygen gradients). | Implement advanced models like microfluidic devices ("biofilm-on-a-chip") that allow for dynamic flow and the creation of nutrient/oxygen gradients, influencing metabolism and creating persister niches [74]. |
| High variability in hydrogel-based 3D cultures. | Batch-to-batch variability of natural hydrogels (e.g., Matrigel). | Consider using synthetic or recombinant hydrogels (e.g., BioSilk functionalized with RGD peptide) for greater control over composition and mechanical properties [72]. |
Detailed Experimental Protocols
Protocol: Inducing Persister Heterogeneity via a Single Metabolic Stress
This protocol is adapted from a study investigating the formation of persisters to different antibiotics in response to a carbon source transition (diauxie) in E. coli [73].
1. Primary Objective: To generate and isolate ampicillin-tolerant persister cells through a controlled metabolic shift.
2. Study Design:
- Type: Laboratory in vitro experiment.
- Strain: Escherichia coli (e.g., K-12 strain).
- Controls: Include a non-stressed control population growing exponentially in a single carbon source.
3. Materials and Reagents:
- Growth Medium: M9 minimal medium.
- Carbon Sources: Glucose and a secondary carbon source (e.g., lactose, arabinose).
- Antibiotic: Ampicillin sodium salt.
- Equipment: Shaking incubator, spectrophotometer for measuring optical density (OD), centrifuge, sterile plates or flasks.
4. Step-by-Step Procedure: 1. Inoculation and Pre-culture: Inoculate E. coli from a single colony into M9 minimal medium supplemented with a limiting concentration of glucose (e.g., 0.1% w/v). Grow overnight at 37°C with shaking. 2. Dilution and Growth: Dilute the overnight culture 1:100 into fresh M9 medium with the same limiting glucose concentration. Grow until the culture reaches mid-exponential phase (OD600 ~0.3-0.5). 3. Metabolic Stress Induction: Add a second, non-preferred carbon source to the culture. The culture will enter diauxie, pausing growth as it switches its metabolic machinery from consuming glucose to the second carbon source. 4. Persister Formation: Incubate the culture for the duration of the diauxic lag phase (typically 1-2 hours). Monitor growth by OD600 to confirm the growth pause. 5. Antibiotic Selection: Add a high concentration of ampicillin (e.g., 100 μg/mL) to the culture to kill non-persister cells. Continue incubation for a defined period (e.g., 3-5 hours). 6. Persister Isolation: Wash the antibiotic-treated cells by centrifugation (e.g., 10,000 rpm for 5 minutes) and resuspend in fresh, antibiotic-free M9 medium to remove the antibiotic. 7. Viability Assessment: Plate serial dilutions of the resuspended cells on LB agar plates to determine the number of colony-forming units (CFUs) that represent the resuscitated persister population.
5. Key Technical Notes:
- This pathway for ampicillin persister formation requires the stringent response and the enzyme RelA for synthesizing the alarmone (p)ppGpp [73].
- The tolerance mechanism involves a broad inhibition of peptidoglycan biosynthesis [73].
- The level of (p)ppGpp required for persister formation can vary depending on the antibiotic's mode of action; higher synthesis is needed for ampicillin persisters compared to ofloxacin persisters [73].
Protocol: Establishing Patient-Derived 3D Tumor Spheroids
This protocol outlines the generation of scaffold-free 3D tumor spheroids, a foundational model for studying tumor heterogeneity and drug response [71] [72].
1. Primary Objective: To create three-dimensional, multicellular tumor spheroids directly from patient-derived cancer cells (PDCCs) for use in drug sensitivity assays.
2. Study Design:
- Type: In vitro 3D cell culture.
- Cell Source: PDCCs obtained via surgical resection, fine needle aspiration, or liquid biopsy [71].
3. Materials and Reagents:
- Cells: Dissociated patient-derived tumor cells.
- Medium: Serum-free medium appropriate for the tumor type, supplemented with necessary growth factors.
- Equipment: Ultra-low attachment (ULA) 96-well U-bottom plates or hanging drop plates, standard cell culture incubator, brightfield microscope.
4. Step-by-Step Procedure: 1. Cell Preparation: Dissociate the patient tumor tissue or PDCC culture into a single-cell suspension. Determine cell viability using trypan blue exclusion. 2. Seeding: - ULA Plate Method: Seed cells at an optimized density (e.g., 1,000-10,000 cells per well, depending on cell type) into the U-bottom plates. The non-adhesive surface forces cells to aggregate. - Hanging Drop Method: Suspend the cell solution in drops from the lid of a culture dish. Gravity causes the cells to settle and aggregate at the bottom of the drop. 3. Spheroid Formation: Culture the plates in a 37°C, 5% CO2 incubator. Spheroids will typically form within 24-72 hours. 4. Monitoring: Use brightfield microscopy daily to monitor spheroid formation, morphology, and size. Representative images can be taken at 40x total magnification [71]. 5. Experimental Use: Once mature (typically after 3-7 days), spheroids can be used for drug testing. Add compounds directly to the wells and monitor for changes in morphology, size, or viability.
5. Key Technical Notes:
- The success of spheroid formation relies on the inherent ability of the cells to self-aggregate [72].
- This method is simple, reproducible, and scalable, making it suitable for high-throughput drug screening [72].
- Compared to 2D monolayers, these 3D models better maintain tumor-specific heterogeneity and more accurate drug response profiles [71].
The Scientist's Toolkit: Research Reagent Solutions
Table 2: Essential Reagents for Featured Experiments
| Item | Function/Application | Example & Notes |
|---|---|---|
| Ultra-Low Attachment (ULA) Plates | Facilitates scaffold-free 3D spheroid formation by preventing cell adhesion. | Corning Costar Spheroid Microplates. Critical for generating uniform tumor spheroids from PDCCs [71]. |
| Natural Hydrogels | Provides a biologically active 3D scaffold that mimics the extracellular matrix (ECM). | Matrigel (basement membrane extract). Contains ECM proteins and growth factors, but batch-to-batch variability can be an issue [72]. |
| Recombinant Hydrogels | Offers a defined, reproducible synthetic ECM for 3D culture with tunable properties. | BioSilk (recombinant silk functionalized with RGD adhesion peptide). Provides control over stiffness and composition [72]. |
| Microfluidic Devices | Creates dynamic, gradient-rich environments to model complex systems like biofilms and tumor microenvironments. | OrganoPlate (for 3D perfusion culture). Allows for co-culture and mimics nutrient/waste transport and shear stress [74] [71]. |
| Stringent Response Inducers | Triggers the (p)ppGpp-mediated stress pathway leading to growth arrest and persister formation. | Carbon source transition (e.g., glucose to lactose). A key metabolic stress for generating persister heterogeneity in bacterial populations [73]. |
Key Workflow and Pathway Diagrams
Metabolic Stress-Induced Persister Formation
This diagram illustrates the core pathway by which a single metabolic stress (diauxie) triggers the formation of persisters tolerant to different antibiotics, highlighting shared and unique genetic elements [73].
Workflow for Establishing Patient-Derived 3D Models
This diagram outlines the key decision points and methods for establishing advanced 3D culture models from patient tumors, bridging the gap between 2D culture and in vivo reality [71].
Challenges in Translating In Vitro Metabolic Findings to In Vivo Relevance
Why do my in vitro metabolic stability results often underpredict the actual in vivo clearance?
A common challenge in drug discovery is the underprediction of in vivo hepatic clearance (CLh) from in vitro intrinsic clearance (CLint, in vitro) data. This discrepancy can arise from several factors, and understanding them is key to improving predictions.
- Limitations of Traditional In Vitro Systems: Short-lived enzyme activity in conventional systems like liver microsomes and hepatocyte suspensions makes it difficult to accurately measure clearance for low-turnover compounds, often resulting in underprediction [75].
- Omission of Critical Biological Factors: Simple in vitro systems may not account for the influence of plasma protein binding or the role of uptake transporters. For instance, the absence of albumin in hepatocyte incubations has been identified as a reason for the underprediction of clearance for compounds that are substrates for uptake transporters [75].
- The Complexity of Glucuronidation: For drugs metabolized via glucuronidation (a major Phase II pathway), relying solely on microsomal data can lead to significant underprediction. This is because the in vivo disposition of glucuronidated metabolites is also influenced by efflux/uptake transporters, enterohepatic recycling, and deglucuronidation reactions, which are not fully captured in basic microsomal assays [76].
Table 1: Factors Leading to Underprediction of In Vivo Clearance and Potential Solutions
| Factor | Impact on Prediction | Potential Solution |
|---|---|---|
| Low-Turnover Compounds | Conventional assays lack sensitivity for slow metabolism, leading to inaccurate CLint, in vitro [75]. | Use extended incubation systems (e.g., hepatocyte relay, 3D co-cultures) [75]. |
| Plasma Protein Binding | Omitting binding proteins in vitro can alter free drug concentration and perceived clearance [75]. | Incorporate human serum albumin into uptake transporter assays [75]. |
| Transporter Effects | Absent in microsomal systems; can be rate-limiting in vivo [76] [75]. | Use transporter-transfected systems or plated hepatocytes. |
| Phase II Metabolism | Microsomal data alone often underpredict glucuronidation clearance [76]. | Use hepatocytes, which have higher phase II activity [76] [75]. |
How does metabolic heterogeneity in bacterial persister populations affect the translation of in vitro findings?
Metabolic heterogeneity is a hallmark of bacterial persister cells—dormant, drug-tolerant subpopulations that cause chronic and relapsing infections. This heterogeneity poses a significant challenge for in vitro to in vivo translation.
- Diverse Metabolic States: Persisters are not a uniform group. They exist on a continuum of metabolic states, from completely dormant ("deep persisters") to slowly metabolizing ("shallow persisters"). In vitro tests that measure average metabolic activity across a population can miss these critical subpopulations that survive antibiotic treatment in vivo [2].
- Multiple Mechanisms of Heterogeneity: This variability arises from several cell-inherent mechanisms:
- Molecular Noise: Stochastic fluctuations in the expression of metabolic enzymes and regulators can lead to cell-to-cell differences in metabolite levels and metabolic fluxes [4] [13].
- Positive Feedback Loops: Systems like the lac operon can create bistability, leading to distinct subpopulations with high and low metabolic activity from a genetically identical culture [4].
- Asymmetric Partitioning: During cell division, cellular components like protein aggregates or transcription factors can be unevenly distributed to daughter cells, creating immediate differences in their metabolic potential [4].
Diagram 1: Origins of metabolic heterogeneity in persister cells and its clinical consequence of antibiotic tolerance.
What advanced in vitro models can improve predictions for low-clearance compounds and complex biology?
To overcome the limitations of traditional models, several advanced in vitro systems have been developed.
- Long-Lived Hepatocyte Models: The hepatocyte relay method and 3D co-culture systems allow for longer incubation times (from hours to days), enabling more accurate determination of CLint, in vitro for low-clearance compounds that are slowly metabolized [75].
- Physiologically Based Pharmacokinetic (PBPK) Modeling: This computational approach is a powerful strategy for drugs like those undergoing glucuronidation. PBPK models can incorporate and integrate complex in vivo processes, including simultaneous enzyme kinetics, transporter effects, and organ-level physiology, leading to more robust predictions of pharmacokinetics and potential drug-drug interactions [76].
- Complex In Vitro Systems: Models such as organoids and organs-on-a-chip more closely mimic human disease and physiology. These systems, which can include 3D structures and multiple cell types, offer higher clinical biomimicry and can better predict the human response to a new drug compared to simple static models or animal studies [77].
Table 2: Comparison of Advanced Models for Improved In Vitro-In Vivo Translation
| Model | Key Application | Key Advantage | Consideration |
|---|---|---|---|
| Hepatocyte Relay / 3D Cultures | Accurate CLint for low-turnover drugs [75]. | Extended viability and metabolic activity [75]. | More complex protocol; higher cost. |
| PBPK Modeling | Integrating metabolism & transporter data (e.g., glucuronidation) [76]. | Models full-body physiology; predicts DDIs [76]. | Requires high-quality input data. |
| Organs-on-a-Chip | Disease modeling, biomarker discovery. | Dynamic flow; mimics tissue-tissue interfaces [77]. | Still emerging; standardization needed. |
How can I account for the role of transporters in Phase II metabolism during in vitro experiments?
Transporters are a critical yet often overlooked factor in the disposition of phase II metabolites.
- The Transport-Metabolism Interplay: Many glucuronide metabolites are substrates for efflux transporters like MRPs (Multidrug Resistance-Associated Proteins). If a glucuronide is formed in the liver but efficiently exported into the bile, it may not be detected in a simple metabolic stability assay using microsomes, which lack these transporters. This can lead to a significant underestimation of the metabolic rate [76].
- A Proposed Framework: The Transport-Glucuronidation Classification System: Research suggests classifying compounds based on the kinetics of both their glucuronidation and the transport of the resulting glucuronide. This system helps determine whether the overall elimination process is limited by the metabolic step or the transporter step, which is crucial for selecting the right experimental tools and achieving better in vivo predictions [76].
Diagram 2: The interplay between hepatic glucuronidation and efflux transporters, a key challenge in IVIVE.
The Scientist's Toolkit: Key Research Reagent Solutions
Table 3: Essential Materials and Tools for Metabolic Translation Studies
| Research Reagent / Tool | Function in Experimental Design |
|---|---|
| Cryopreserved Hepatocytes | Gold standard for estimating hepatic CLint; retain phase I/II metabolism and transporter activity [76] [75]. |
| Transporter-Transfected Cell Lines | Used to isolate and study the specific role of uptake (e.g., OATPs) and efflux (e.g., MRPs, BCRP) transporters [76]. |
| Human Liver Microsomes (HLMs) | Contains cytochrome P450s and UGT enzymes for initial metabolic stability and reaction phenotyping studies [78]. |
| LC-UV-MSn Mass Spectrometry | Technology for identifying and quantifying metabolites formed in vitro and in vivo, crucial for building metabolic profiles [79] [78]. |
| PBPK Software | (e.g., GastroPlus, Simcyp Simulator) Platforms for building integrated models that incorporate in vitro data to predict in vivo PK [76]. |
| Genetically Encoded Biosensors | Enable real-time monitoring of metabolite levels (e.g., ATP) in live cells, allowing assessment of metabolic heterogeneity [4]. |
Frequently Asked Questions (FAQs)
FAQ 1: What are the primary sources of technical noise when integrating single-cell multi-omics data from bacterial persisters? Technical noise primarily arises from the inherent heterogeneity of bacterial populations and the technical challenges of isolating persister cells. Using antibiotics to isolate persisters alters their naïve metabolic state, making true metabolic measurements difficult [7]. Furthermore, each omics data type (e.g., transcriptomics, proteomics) has a unique data structure, scale, and noise profile, challenging harmonization. For instance, a gene detected at the RNA level may be missing in the protein dataset due to differences in methodological sensitivity [80] [81].
FAQ 2: Why is it difficult to correlate transcriptomic data with metabolic activity in persister cells? A downregulation of metabolic genes is often observed in transcriptome patterns of persisters, but this does not necessarily mean metabolism has ceased [7]. Metabolic activity can be uncoupled from transcription; for example, isotopolog profiling of Staphylococcus aureus persisters challenged with daptomycin revealed active de novo biosynthesis of amino acids and an active TCA cycle, despite the cells being in a drug-tolerant state [7]. This demonstrates the critical need to directly measure metabolic fluxes rather than relying solely on transcriptional data.
FAQ 3: What computational strategies can integrate data from different omics layers that were not collected from the same cell? For this "unmatched" or "diagonal" integration, where omics data come from different cells, tools like GLUE (Graph-Linked Unified Embedding) use graph variational autoencoders and prior biological knowledge to anchor and align cells from different modalities into a co-embedded space [80]. Other methods like Pamona and UnionCom use manifold alignment to achieve similar integration from different single cells [80].
FAQ 4: How can I account for the strong batch effects often present in public reference atlases? Frameworks like Φ-Space use a linear factor modeling approach (Partial Least Squares Regression) that can remove unwanted variation, making it robust against batch effects in reference data without needing additional correction steps [82]. For more general batch correction, tools such as Harmony or Liger can be applied during the normalization step of your analysis pipeline [83].
Troubleshooting Guides
Table 1: Common Data Integration Issues and Solutions
| Problem Area | Specific Issue | Potential Solution |
|---|---|---|
| Experimental Design | Low RNA yield from persister cells leading to poor library quality. | Perform a pilot experiment to optimize cell input and PCR cycles. Use positive control RNA with mass similar to your samples (e.g., 1-10 pg) [84]. |
| Cell Isolation & Lysis | Carryover of media, EDTA, or divalent cations that interfere with reverse transcription. | Wash and resuspend cells in EDTA-, Mg²âº-, and Ca²âº-free PBS before processing. When using FACS, sort cells directly into lysis buffer containing RNase inhibitor [84]. |
| Data Preprocessing | High ambient RNA or multiplet rates in data. | Use computational tools in pipelines like Seurat or Scanpy to filter ambient RNA and doublets. Platforms with image-based cell isolation (e.g., cellenONE) can reduce multiplets from the start [85] [83]. |
| Multi-omics Integration | Difficulty integrating matched multi-omics data (e.g., RNA and protein from the same cell). | Use matched integration tools like Seurat v4 (weighted nearest neighbor) or MOFA+ (factor analysis) to leverage the cell itself as an anchor [80]. |
| Biological Interpretation | Translating integrated data into actionable biological insight for persister metabolism. | Use pathway and network analysis on the integrated output. Supervised integration methods like DIABLO can help relate multi-omics data directly to a phenotypic outcome like drug tolerance [81]. |
Detailed Protocol: Metabolic Profiling of Persister Cells
This protocol outlines a methodology for investigating the active metabolism of bacterial persister cells by combining selective isolation with ¹³C-isotopolog profiling [7].
1. Persister Cell Isolation:
- Culture and Treatment: Grow the bacterial culture to stationary phase, as this stage typically has higher persister levels [7].
- Antibiotic Challenge: Treat the culture with a high concentration of a bactericidal antibiotic (e.g., daptomycin, tobramycin) for a sufficient duration to kill the majority of the population.
- Washing: Remove the antibiotic thoroughly by washing the surviving cells with an appropriate buffer. These survivor cells are enriched for persisters.
2. ¹³C-Isotopolog Profiling:
- Pulse Labeling: Resuspend the isolated persister cells in a medium containing a ¹³C-labeled carbon source (e.g., [U-¹³C]glucose).
- Incubation: Allow the cells to metabolize the labeled substrate for a defined period.
- Metabolite Extraction: Quench metabolism rapidly (e.g., using cold methanol) and extract intracellular metabolites.
3. Data Acquisition and Analysis:
- Mass Spectrometry: Analyze the metabolite extracts using Gas Chromatography- or Liquid Chromatography-Mass Spectrometry (GC/LC-MS).
- Flux Analysis: Determine the ¹³C-labeling patterns (isotopologs) in key metabolic intermediates (e.g., amino acids, TCA cycle metabolites). The distribution of labels reveals the relative activities of pathways like glycolysis, the pentose phosphate pathway, and the TCA cycle in persister cells [7].
Persister Cell Metabolic Signaling
Single-Cell Multi-Omics Integration Workflow
Research Reagent Solutions
Table 2: Essential Materials for Single-Cell Persister Analysis
| Item | Function in the Context of Persister Research |
|---|---|
| EDTA-/Cation-Free PBS | To wash and resuspend cells without interfering with downstream enzymatic reactions (e.g., reverse transcription) during single-cell library prep [84]. |
| RNase Inhibitor | Preserves RNA integrity during cell sorting and lysis, which is critical for obtaining high-quality transcriptomic data from low-input persister samples [84]. |
| ¹³C-labeled Substrates (e.g., Glucose) | Allows for isotopolog profiling to measure metabolic fluxes and pathway activities directly in persister cell populations, moving beyond static transcriptomic data [7] [4]. |
| Lysis Buffer with CDS Primer | A specialized buffer for FACS-sorting single cells that immediately begins cell lysis and primes cDNA synthesis, maximizing yield from the tiny amount of RNA in one cell [84]. |
| Genetically Encoded Biosensors | For live-cell imaging and tracking of specific metabolites (e.g., ATP) at the single-cell level, helping to link metabolic heterogeneity to the persister phenotype [4]. |
Evaluating Therapeutic Strategies and Their Clinical Translation Potential
What are the primary mechanisms of direct killing agents, and why are they relevant to persister cell research?
Persister cells are dormant, non-growing bacterial variants that are tolerant to conventional antibiotics, which typically target active cellular processes. This metabolic heterogeneity within bacterial populations is a major cause of chronic and relapse infections [3] [2]. Direct killing agents offer a solution by targeting growth-independent cellular structures. Their primary mechanisms are:
- Membrane Disruption: Physically damaging the bacterial cell membrane, leading to cell lysis and death [3] [86].
- Protein Degradation: Activating proteases to cause uncontrolled degradation of essential cellular proteins, preventing cellular recovery [3].
These mechanisms are crucial for eradicating persister cells because they do not require the target cells to be metabolically active [3].
Troubleshooting Guides
FAQ 1: My membrane-disruptive agent shows excellent efficacy in planktonic cultures but fails against biofilm-based persisters. What could be wrong?
Potential Cause: The extracellular polymeric substance (EPS) of biofilms acts as a diffusion barrier, sequestering the agent and preventing it from reaching the bacterial membranes [3].
Solutions:
- Utilize Combination Therapy: Co-administer with EPS matrix degrading enzymes (e.g., DNase I to degrade extracellular DNA) to enhance penetration [3].
- Employ Nano-carriers: Use delivery systems like red blood cell membrane-coated nanoparticles, which have been shown to interact with EPS and improve delivery of antimicrobials to persisters within biofilms [3].
- Check Agent Molecular Weight: Large, hydrophobic agents may have difficulty penetrating the biofilm. Consider switching to smaller, cationic peptides or peptidomimetics that can better navigate the biofilm matrix.
FAQ 2: I am observing high cytotoxicity in my mammalian cell models with a novel membrane-disruptive peptide. How can I improve its selectivity?
Potential Cause: The peptide may have a high binding affinity for zwitterionic mammalian membranes (rich in phosphatidylcholine) in addition to anionic bacterial membranes [86] [87].
Solutions:
- Modify Physicochemical Parameters: Adjust the peptide's hydrophobicity. Excessive hydrophobicity often correlates with increased hemolytic activity. Reduce it to a moderate level (e.g., <40% hydrophobic residues).
- Optimize Charge and Amphipathicity: Ensure the peptide has a strong net positive charge (+4 to +9) to enhance electrostatic binding to anionic bacterial surfaces. Refine its amphipathic structure to maximize interaction with bacterial membranes while minimizing interaction with mammalian membranes [86] [88].
- Perform Binding Affinity Assays: Use Surface Plasmon Resonance (SPR) to quantitatively measure the peptide's binding affinity (KD) for liposomes mimicking bacterial vs. mammalian membranes. Select peptides with high selectivity for bacterial membrane models [87].
FAQ 3: My protease activator (e.g., ADEP4) is effective in vitro, but bacterial populations eventually resume growth after treatment. How can I prevent this regrowth?
Potential Cause: ADEP4 activates the ClpP protease, leading to uncontrolled protein degradation. However, some persisters may survive if the protein degradation is not comprehensive enough to eliminate all proteins essential for "wake-up" [3].
Solutions:
- Implement Combination Therapy: Combine ADEP4 with a conventional antibiotic (e.g., rifampicin). ADEP4 breaks down the proteins necessary for persister regrowth, while the antibiotic kills any cells that exit dormancy. This synergy can lead to complete eradication [3].
- Optimize Dosing and Timing: Ensure the concentration of ADEP4 is sufficient to fully saturate ClpP and maintain it throughout the critical "wake-up" period. Perform time-kill curves to determine the optimal treatment duration.
- Screen for Resistance: Monitor for mutations in the clpP gene that may confer resistance. Using combination therapy from the outset can mitigate the outgrowth of such mutants.
The Scientist's Toolkit: Research Reagent Solutions
Table 1: Essential Reagents for Studying Direct Killing Agents
| Reagent / Tool | Function / Application | Key Considerations |
|---|---|---|
| Liposomes (LUVs/GUVs) | Synthetic model membranes for studying peptide-lipid interactions and mechanism of action (e.g., dye leakage assays) [87]. | Can be tailored with bacterial (e.g., PG, CL) or mammalian (e.g., PC) lipids to test selectivity. |
| SYTOX Green / PI | Membrane-impermeant nucleic acid stains. Used in flow cytometry or fluorometry to quantify loss of membrane integrity in bacterial cells [87]. | SYTOX Green offers higher sensitivity and quantum yield than Propidium Iodide (PI). |
| DiSC3(5) Dye | A membrane potential-sensitive dye used to detect membrane depolarization in real-time [87]. | Requires pre-loading of bacteria and optimization of cell density and dye concentration. |
| NPN (N-phenyl-1-napthylamine) | A fluorescent dye used to assess outer membrane permeability in Gram-negative bacteria [87]. | Increased fluorescence indicates disruption of the outer membrane. |
| ADEP4 | Acyldepsipeptide that activates the ClpP protease, leading to uncontrolled protein degradation and death of persister cells [3]. | Most effective when used in combination with other antibiotics to prevent regrowth. |
| Pyrazinamide (PZA) | A prodrug (active form: pyrazinoic acid) used against M. tuberculosis persisters. Disrupts membrane energetics and targets PanD for degradation [3]. | Requires acidic environment for optimal activity. A key example of a clinically approved anti-persister drug. |
Experimental Protocols & Data Analysis
Protocol 1: Dye Leakage Assay for Membrane Disruption
Objective: To quantify the membrane-disruptive activity of an agent using carboxyfluorescein-loaded liposomes [87].
Workflow:
- Liposome Preparation: Prepare large unilamellar vesicles (LUVs) from a 7:3 molar ratio of phosphatidylglycerol (PG) and phosphatidylethanolamine (PE) in a buffer containing 70 mM carboxyfluorescein.
- Remove Free Dye: Separate the dye-loaded liposomes from unencapsulated dye using gel filtration (e.g., Sephadex G-50).
- Baseline Measurement: In a 96-well plate, add liposomes to buffer and measure baseline fluorescence (λex/~492 nm, λem/~517 nm). Carboxyfluorescein is self-quenched at high concentration, so signal is low.
- Add Test Agent: Add your membrane-disruptive agent to the wells. Include a positive control (e.g., 0.1% Triton X-100 for 100% leakage) and a negative control (buffer only).
- Monitor Leakage: Measure fluorescence over time (e.g., 60 minutes). As the agent disrupts the liposome membrane, carboxyfluorescein is released and diluted, causing a de-quenching and increase in fluorescence.
- Calculate % Leakage: % Leakage = [(Fsample - Finitial) / (FTriton - Finitial)] × 100.
Diagram 1: Dye leakage assay workflow.
Protocol 2: Flow Cytometry Assay for Membrane Integrity
Objective: To distinguish and quantify populations of permeabilized and intact bacterial cells after treatment with a membrane-disruptive agent using SYTOX Green [87].
Workflow:
- Culture and Treat Bacteria: Grow bacteria to mid-log phase. Treat a sample with your test agent for a desired time. Include an untreated control.
- Stain with SYTOX Green: Add SYTOX Green nucleic acid stain to both treated and untreated samples at a final concentration of 1 µM.
- Incubate: Incubate samples in the dark for 10-15 minutes.
- Run Flow Cytometry: Analyze samples using a flow cytometer. Use the untreated population to set a gate for SYTOX Green-negative (intact membrane) cells.
- Analyze: The percentage of cells in the SYTOX Green-positive population (fluorescent) corresponds to cells with compromised membranes.
Table 2: Key Parameters for SYTOX Green Flow Cytometry
| Parameter | Recommended Setting | Purpose / Note |
|---|---|---|
| Laser | Blue (488 nm) | Standard excitation for SYTOX Green. |
| Detection Filter | FL1 / 530/30 nm | Standard emission filter for green fluorescence. |
| Concentration | 0.5 - 1 µM | Optimize to minimize background in untreated control. |
| Incubation Time | 10 - 15 min | Protect from light during incubation. |
| Gating Strategy | FSC vs. SSC to select bacterial population, then FL1 histogram. | Exclude debris and aggregates. |
Table 3: Summary of Direct Killing Agents and Their Efficacy
| Agent / Class | Target | Model Organism | Reported Efficacy (Quantitative) | Key Experimental Condition |
|---|---|---|---|---|
| XF-73 [3] | Cell Membrane | S. aureus | Effective against non-dividing and slow-growing cells. | Disrupts cell membrane; generates ROS upon light activation. |
| ADEP4 + Rifampicin [3] | ClpP Protease | S. aureus | Complete eradication of persisters in vitro. | Combination therapy. ADEP4 causes ATP-independent protein degradation. |
| Pyrazinamide (PZA) [3] [2] | Membrane Energetics / PanD | M. tuberculosis | Key drug for shortening TB therapy; targets persisters. | Prodrug activated to pyrazinoic acid in acidic environment. |
| Cationic Silver Nanoparticles (C-AgND) [3] | Cell Membrane / EPS | S. aureus (in biofilms) | Effective killing of persisters within biofilms. | Nanocarrier interacts with negatively charged EPS for delivery. |
| LL-37 [89] [90] | Cell Membrane | Broad-spectrum | Kills 90% of E. coli in 90-120 min, P. aeruginosa in 5-30 min [88]. | Human cathelicidin; also has immunomodulatory functions. |
| Polymer Nanocomposite [3] | Cell Membrane | S. aureus | Exhibits anti-persister effects. | Organo-soluble antimicrobial polymer. |
Frequently Asked Questions (FAQs)
FAQ 1: What is the fundamental difference between a bacterial persister and an antibiotic-resistant bacterium? Bacterial persisters and antibiotic-resistant bacteria are distinct subpopulations. Persisters are genetically drug-susceptible but exist in a transient, slow-growing or non-growing state that allows them to tolerate antibiotic exposure without genetic mutation. In contrast, resistant bacteria have acquired genetic mutations that allow them to grow in the presence of antibiotics, often by modifying the drug's target, inactivating the drug, or pumping it out [2] [91]. This difference is crucial because persisters are linked to chronic, relapsing infections and are not effectively targeted by conventional antibiotics.
FAQ 2: How do "wake-up" strategies circumvent the problem of metabolic heterogeneity in persister populations? Metabolic heterogeneity means a persister population contains cells at different levels of dormancy (shallow to deep persistence) [2]. "Wake-up" strategies aim to force these dormant cells back into an active metabolic state, making them vulnerable again to traditional antibiotics. Research shows that an optimal lag time exists for waking up; waking too soon may expose cells to lingering antibiotics, while waking too late forfeits growth opportunities. Evolving or administering strategies that align wake-up times with the cessation of antibiotic stress can effectively target this heterogeneous population [92].
FAQ 3: Why are anti-virulence approaches considered a promising alternative to traditional bactericidal antibiotics? Anti-virulence therapies, or "pathoblockers," disarm pathogens by targeting their virulence factors—molecules required to cause disease—instead of killing the bacteria or stopping their growth [93] [94]. This approach exerts less selective pressure for resistance development, as it does not directly threaten bacterial survival. It also preserves the host's beneficial microbiome because the therapy is specific to the pathogen's virulence mechanisms. These strategies can target factors like toxins, adhesion molecules, biofilm formation, and quorum-sensing systems [93] [94] [95].
FAQ 4: What are common reasons for the failure of quorum-sensing inhibition assays, and how can this be addressed? A major reason for false positives in quorum-sensing inhibition assays is that test compounds may non-specifically interfere with the reporter system's biochemistry (e.g., GFP or luciferase activity) rather than the quorum-sensing regulation itself [95]. To address this, the concept of Specific Quorum Sensing-Disrupting Activity (AQSI) was developed. The AQSI parameter is calculated by comparing the percent inhibition of a quorum-sensing-regulated reporter to the percent inhibition of a control reporter that is independent of quorum sensing. This normalization helps reliably identify true inhibitors [95].
Troubleshooting Guides
Table 1: Troubleshooting Anti-Virulence Compound Screening
| Problem | Possible Cause | Solution |
|---|---|---|
| High hit rate in initial QS inhibitor screen | Non-specific inhibition of reporter protein (e.g., GFP) or general cellular toxicity [95]. | Implement a control reporter strain not regulated by QS and calculate the AQSI value to identify specific inhibitors [95]. |
| Lack of correlation between in vitro and in vivo efficacy | The virulence factor targeted may not be critical in the infection model, or compound may have poor pharmacokinetics. | Validate target essentiality in the host environment; check compound stability, bioavailability, and dosing regimen. |
| Rapid loss of compound efficacy | Potential emergence of resistance to the anti-virulence compound, as seen in some Pseudomonas aeruginosa studies [94]. | Consider combination therapies that target multiple virulence pathways or pair with low-dose conventional antibiotics. |
Table 2: Troubleshooting Persister "Wake-Up" Experiments
| Problem | Possible Cause | Solution |
|---|---|---|
| Inconsistent persister resuscitation after wake-up stimulus | High degree of metabolic heterogeneity within the persister pool; some cells are in a deeper dormant state (VBNC) and do not respond [2]. | Characterize the depth of dormancy; consider using multiple, sequential wake-up stimuli or metabolic primers to target different subpopulations. |
| Wake-up strategy does not re-sensitize persisters to antibiotics | The wake-up trigger may not fully restore metabolic activity or the antibiotic's target pathway. | Verify metabolic reactivation by measuring RNA production or energy status [51]. Test antibiotic class with a different mechanism of action. |
| Failure to isolate a pure persister population for testing | Standard methods may not fully remove all viable, non-persister cells. | Use a more rigorous protocol with high-dose, bactericidal antibiotic exposure for an extended period, followed by thorough washing [2]. |
The Scientist's Toolkit: Research Reagent Solutions
Table 3: Key Reagents for Indirect Eradication Research
| Reagent / Tool | Function in Research | Example Application |
|---|---|---|
| Quorum Sensing Reporter Strains | Report on the activity of quorum-sensing systems via a measurable output (e.g., luminescence, GFP) [95]. | Screening for QS inhibitors; quantifying virulence factor expression. |
| Specific Antivirulence Activity (AAV) Metric | A normalized parameter to distinguish true virulence inhibitors from non-specific toxic compounds [95]. | Validating hits from high-throughput virulence inhibitor screens. |
| Photoimmuno-antimicrobial Conjugates (e.g., SA–IR700) | Target-specific antibodies conjugated to a photosensitizer for precise microbial eradication [96]. | Selective killing of pathogen persisters in a mixed culture without disrupting commensals. |
| Metabolic Activity Probes | Measure the metabolic state of cells (e.g., ATP levels, membrane potential, RNA production) [51]. | Differentiating and characterizing subpopulations within heterogeneous persister cultures. |
Experimental Protocols & Workflows
Protocol 1: Evaluating "Wake-Up" Compounds for Antibiotic Re-sensitization
Objective: To test if a candidate compound can wake up bacterial persisters and restore their susceptibility to a conventional antibiotic.
Persister Isolation:
- Grow the bacterial culture to stationary phase (enriched for Type I persisters) or mid-exponential phase (for spontaneous Type II persisters).
- Expose the culture to a high concentration of a bactericidal antibiotic (e.g., ampicillin or ciprofloxacin) for a duration sufficient to kill all growing cells (typically 3-5 hours).
- Centrifuge the culture, discard the supernatant, and wash the pellet thoroughly with fresh media or buffer to remove the antibiotic. This pellet constitutes the enriched persister population [2].
Wake-Up and Eradication Assay:
- Resuspend the persister pellet in fresh media.
- Divide the suspension into aliquots:
- Control 1: Persisters + media only.
- Control 2: Persisters + antibiotic only.
- Test Group: Persisters + wake-up compound + antibiotic.
- Incubate the cultures for a set period (e.g., 4-24 hours).
Viability Assessment:
- Serially dilute the cultures and spot them on antibiotic-free agar plates.
- Count the colony-forming units (CFU) after incubation.
- A significant reduction in CFU in the "Test Group" compared to "Control 2" indicates successful wake-up and eradication.
The logic of this strategy is summarized below:
Protocol 2: Screening for Specific Quorum-Sensing Inhibitors (QSIs)
Objective: To identify compounds that specifically inhibit a quorum-sensing (QS) system without general anti-growth effects.
Strain Preparation:
- QS Reporter Strain: A strain where a key virulence gene (e.g., for toxin production) is fused to a reporter like gfp or luc.
- Constitutive Control Strain: A strain where the same reporter is expressed from a promoter not regulated by QS.
Compound Screening:
- In a multi-well plate, add both strains to separate wells containing serial dilutions of the test compound.
- Incubate the plates until the control strain (without compound) reaches mid-exponential phase and shows strong QS-induced reporter signal.
Signal Measurement and Analysis:
- Measure the optical density (OD) to monitor growth.
- Measure the reporter signal (e.g., fluorescence or luminescence).
- For each compound concentration, calculate:
%Inhibition_QS-regulated = 100 * (1 - (Signal_QS / Signal_QS_control))%Inhibition_QS-independent = 100 * (1 - (Signal_control / Signal_control_control))
- Calculate the Specific Antivirulence Activity (AAV):
AAV = %Inhibition_QS-regulated / %Inhibition_QS-independent[95]. - Compounds with high AAV values (>>1) are specific QS inhibitors, while those with AAV near 1 are likely non-specific.
The workflow for reliable QSI identification is as follows:
Conceptual Framework for Addressing Metabolic Heterogeneity
The following diagram illustrates the core challenge of metabolic heterogeneity in persister populations and the two main indirect eradication strategies discussed in this guide.
Comparative Analysis of Anti-Persister Efficacy Across Bacterial and Cancer Models
Frequently Asked Questions (FAQs)
FAQ 1: What is the fundamental difference between antibiotic resistance and bacterial persistence? Antibiotic resistance is a genetically inherited trait that allows bacteria to grow in the presence of an antibiotic, typically leading to a higher minimum inhibitory concentration (MIC). In contrast, bacterial persistence is a reversible, non-genetic phenotype where a small subpopulation of dormant or slow-growing cells survives antibiotic treatment without a change in MIC. Persisters can resume growth once the antibiotic pressure is removed, often causing relapsing infections [2] [97] [98].
FAQ 2: How do Drug-Tolerant Persister (DTP) cells in cancer differ from fully resistant cancer cells? Cancer DTPs survive therapy through reversible, non-genetic adaptations such as epigenetic reprogramming, metabolic shifts, and quiescence. They are not selected clones but can revert to a drug-sensitive state upon therapy withdrawal. In contrast, fully resistant cancer cells typically possess stable genetic mutations that confer a permanent growth advantage under treatment. DTPs act as a reservoir that can eventually give rise to resistant populations [59] [15] [99].
FAQ 3: Why do standard antibiotics and chemotherapies often fail against persister cells? Standard bactericidal antibiotics and many chemotherapies primarily target actively growing cells. Persister cells, both bacterial and cancer, evade these treatments by entering a state of metabolic dormancy or slowed proliferation, thereby avoiding the cellular processes these drugs corrupt. This is not a failure of drug binding but a failure of the cell to engage the lethal mechanism [100] [6] [101].
FAQ 4: What is the "wake and kill" strategy, and how is it being implemented? The "wake and kill" (or reactivation) strategy involves forcing persister cells out of their dormant state to make them vulnerable again to conventional antimicrobials or chemotherapeutics. In bacteria, this is achieved using metabolites (e.g., mannitol, pyruvate) to reactivate metabolism. In cancer, epigenetic drugs (e.g., HDAC inhibitors) or targeted agents are used to reverse the dormant DTP state, followed by a conventional cytotoxic drug [100] [6] [99].
FAQ 5: How does the tumor microenvironment (TME) contribute to cancer DTP formation? The TME promotes DTP formation through various mechanisms. Hypoxic regions and nutrient deprivation within the tumor can induce a quiescent state. Additionally, signaling from cancer-associated fibroblasts (CAFs) and other stromal cells, such as the secretion of Hepatocyte Growth Factor (HGF), provides pro-survival signals that help cancer cells withstand therapy [99] [101].
Troubleshooting Common Experimental Challenges
Challenge 1: Low and Variable Persister Cell Yields
- Problem: The proportion of persisters isolated is inconsistent, making experiments unreliable.
- Solution:
- For Bacterial Persisters: Standardize the growth phase of your inoculum. Persister levels are highest in stationary phase cultures. Use mid-log phase cultures for Type II (spontaneous) persister studies and stationary phase for Type I (stress-induced) persisters [2]. For biofilm-derived persisters, allow biofilms to mature fully before treatment [98].
- For Cancer DTPs: Ensure treatment duration and drug concentration are optimized for your specific cell line. DTPs are often observed after prolonged exposure (72-144 hours) to concentrations 100-fold the IC50 [101]. Confirm the presence of DTPs by demonstrating reversibility—washing out the drug should allow colonies to re-grow.
Challenge 2: Differentiating Between True Persisters and Resistant Mutants
- Problem: It is difficult to confirm that surviving cells are phenotypically tolerant persisters and not genetically resistant mutants.
- Solution:
- Re-culture Assay: The gold-standard test is to re-culture the surviving cells in drug-free media and then re-challenge them with the same drug. Persisters will re-establish a population with a similar killing curve as the parent strain, while resistant mutants will show a consistently higher survival rate [2] [97].
- Genomic Analysis: Sequence surviving populations to check for known resistance-conferring mutations. A lack of such mutations supports a persister phenotype.
Challenge 3: Inefficient Eradication of Biofilm-Embedded Persisters
- Problem: Antimicrobials fail to penetrate and kill persisters within a biofilm matrix.
- Solution:
- Utilize Nano-strategies: Employ nanoparticles functionalized with biofilm matrix-degrading enzymes (e.g., DNase I to break down extracellular DNA). Their small size enhances penetration. For example, cationic polymers like PS+(triEG-alt-octyl) loaded onto polydopamine nanoparticles have shown enhanced diffusion and efficacy against biofilm persisters [100].
- Combination Therapy: Use a two-step approach: first, a dispersing agent (e.g., a quorum-sensing inhibitor) to disrupt the biofilm structure, followed by a conventional antibiotic or a anti-persister nanoagent [98].
Key Experimental Protocols
Protocol: Generating and Isulating Bacterial Persisters via Antibiotic Killing Curve
This protocol is fundamental for obtaining a purified population of bacterial persisters for downstream analysis [2] [97].
- Culture Preparation: Grow the bacterial strain of interest to the desired phase (e.g., mid-log or stationary) in appropriate liquid medium.
- Antibiotic Challenge: Add a high concentration of a bactericidal antibiotic (e.g., ampicillin at 10x MIC) to the culture. Ensure proper controls (no antibiotic) are included.
- Incubation and Sampling: Incubate the culture under standard conditions. Take samples at regular intervals (e.g., 0, 2, 4, 8, 24 hours).
- Viable Count Plating: Serially dilute each sample and plate on drug-free agar plates. This step is critical; plating on drug-free media allows persisters to grow.
- Calculation: Count the colony-forming units (CFUs) after incubation. Plot the log(CFU/mL) versus time to generate a biphasic killing curve. The surviving population after 24 hours is highly enriched for persisters.
- Persister Isolation: Harvest the cells from the 24-hour time point by centrifugation and washing to remove the antibiotic. The resulting pellet can be used for subsequent experiments.
Protocol: Assessing the "Wake and Kill" Efficacy in Cancer DTPs
This protocol evaluates the ability of a candidate drug to reactivate DTPs and re-sensitize them to chemotherapy [99] [101].
- DTP Induction: Treat a sensitive cancer cell line (e.g., EGFR-mutant PC9 for NSCLC) with a high dose of a targeted therapy (e.g., 1 µM Erlotinib) for 5-7 days. Refresh the drug and medium every 2-3 days.
- Confirm Quiescence: Verify the induction of a quiescent state using a flow cytometry-based assay for Ki67 (a proliferation marker) or by staining with a fluorescent dye like CFSE that dilutes with cell division.
- "Wake and Kill" Treatment:
- Group 1 (Control): DTPs with fresh medium only.
- Group 2 (Kill only): DTPs with the original chemotherapy.
- Group 3 (Wake and Kill): DTPs with the reactivating agent (e.g., an HDAC inhibitor like Entinostat) combined with the original chemotherapy.
- Viability Assessment: After 72-96 hours of treatment, assess cell viability using a resazurin (Alamar Blue) assay or by performing clonogenic survival assays.
- Data Interpretation: A significant reduction in viability in Group 3 compared to Groups 1 and 2 indicates successful reactivation and killing of DTPs.
Comparative Efficacy Data
Table 1: Quantitative Efficacy of Selected Anti-Persister Formulations Across Models
| Agent / Formulation | Model System | Target Persister Type | Key Mechanism of Action | Reported Efficacy | Citation |
|---|---|---|---|---|---|
| Caff-AuNPs | In vitro, Planktonic & Biofilm | Bacterial (Gram+ & Gram-) | Direct physical disruption of cell membranes/mature biofilms | Potent bactericidal activity against dormant cells | [100] |
| AuNC@ATP | In vitro, Planktonic | Bacterial (Gram-) | Enhanced bacterial membrane permeability; disrupts outer membrane protein folding | ~7-log reduction in persister populations | [100] |
| MPDA/FeOOH-GOx@CaP Microspheres | Prosthetic Joint Infection | Bacterial (e.g., S. aureus) | ROS generation via Fenton-like reaction in acidic biofilm microenvironment | Effective eradication of S. aureus and S. epidermidis persisters | [100] |
| PS+(triEG-alt-octyl)PDA NPs | In vitro, Bacterial Biofilm | Bacterial | "Wake and Kill": Reactivates persisters via electron transport chain, then disrupts membranes | Potent antibiofilm activity, clearing persistent biofilms | [100] |
| Entinostat (HDACi) + EGFRi | EGFR-mutant NSCLC (Cancer) | Cancer DTP | Epigenetic modulation; reverses repressive chromatin state to re-sensitize | Overcomes reversible resistance in clinical evaluation | [99] |
| IACS-010759 (OXPHOSi) | Relapsed/Refractory AML & Solid Tumors (Cancer) | Cancer DTP | Inhibits oxidative phosphorylation, targeting DTP metabolic dependency | Preliminary clinical activity; suppresses OXPHOS in patient biopsies | [99] |
Table 2: The Scientist's Toolkit: Key Research Reagent Solutions
| Reagent / Material | Category | Primary Function in Persister Research | Example Application |
|---|---|---|---|
| Caffeine-functionalized Gold Nanoparticles (Caff-AuNPs) | Nanomaterial | Directly disrupts bacterial cell membranes and biofilms physically, independent of metabolic state. | Eradicating planktonic and biofilm-associated bacterial persisters [100]. |
| Adenosine Triphosphate-functionalized Gold Nanoclusters (AuNC@ATP) | Nanomaterial | Increases membrane permeability and disrupts protein folding in Gram-negative bacterial persisters. | Achieving high-log reduction of Gram-negative persister populations [100]. |
| Mesoporous Polydopamine (MPDA) | Nanomaterial Core | Serves as a scaffold for growing catalysts and loading drugs; can enhance biofilm penetration. | Core component of ROS-generating microspheres for joint infection models [100]. |
| Histone Deacetylase Inhibitors (e.g., Entinostat) | Small Molecule Inhibitor | Reverses epigenetic silencing by altering chromatin structure, "waking up" cancer DTPs. | Used in combination with targeted therapies to overcome reversible drug tolerance in cancer [99]. |
| Oxidative Phosphorylation Inhibitors (e.g., IACS-010759) | Small Molecule Inhibitor | Targets the shifted metabolic state of cancer DTPs, which often rely on mitochondrial OXPHOS. | Eliminating DTPs in AML and solid tumor models by inducing metabolic crisis [99]. |
| Mannitol / Pyruvate | Metabolite | Acts as a metabolic re-activator ("wake" signal) by restoring proton motive force in bacterial persisters. | Pre-treatment to sensitize bacterial persisters to aminoglycoside antibiotics [6]. |
Signaling Pathways and Workflows
Bacterial Anti-Persister Nanoagent Action
Diagram Title: Bacterial Anti-Persister Nanoagent Action
Cancer DTP State Transition & Intervention
Diagram Title: Cancer DTP State Transition & Intervention
Frequently Asked Questions (FAQs)
Q1: What are the key characteristics of persister cells that make them resistant to standard antibiotic or chemotherapeutic treatments? Persister cells are a subpopulation of genetically drug-susceptible cells that enter a transient, non-growing or slow-growing state. This quiescence allows them to survive exposure to high concentrations of antibiotics or chemotherapeutic agents that kill their actively growing counterparts. Their key characteristics include metabolic heterogeneity, dormancy, and non-heritable antibiotic tolerance, meaning the survival trait is not passed genetically to offspring but is a phenotypic switch [2] [64]. This state is a "bet-hedging" strategy that protects bacterial populations from environmental stresses.
Q2: Why is Pyrazinamide (PZA) effective against bacterial persisters when many other antibiotics fail? Unlike most antibiotics that target actively growing cells, Pyrazinamide is a unique anti-tuberculosis drug that preferentially targets dormant Mycobacterium tuberculosis persisters [102]. Its active form, pyrazinoic acid, disrupts essential cellular processes that are critical for bacterial survival under stress conditions, such as energy metabolism and the trans-translation system required for protein quality control during starvation [102]. This makes PZA a cornerstone of combination therapy for tuberculosis, as it shortens treatment duration by eradicating this refractory subpopulation [2] [102].
Q3: What are the common reasons for the failure of combination therapies targeting persister cells in experimental models? The failure of combination therapies in experiments can often be attributed to several factors:
- Inadequate Model Systems: Using in vitro models that do not fully recapitulate the metabolic heterogeneity and complex microenvironments (e.g., biofilms, nutrient gradients) found in vivo [2] [64].
- Incorrect Dosing and Timing: Administering drugs at doses or sequences that do not account for the slow metabolic state of persisters. For instance, a drug that requires active cell division may be ineffective if given before a metabolic inhibitor that induces stasis.
- Unaddressed Pathogen Diversity: Failing to account for the continuum of persister states, from "shallow" to "deep" dormancy, which may have different susceptibilities to various drugs [2].
Q4: How can I validate that a metabolic inhibitor is effectively sensitizing cancer persister cells to chemotherapy? Validation requires a multi-faceted approach:
- Direct Cell Viability Assays: Use long-term colony-forming unit (CFU) counts or regrowth assays after removal of the drugs, rather than just short-term viability stains, to confirm eradication [2] [64].
- Metabolic Profiling: Measure key metabolic parameters (e.g., ATP levels, oxygen consumption rate, glycolytic flux) to confirm the inhibitor is hitting its intended target and shifting the cell's metabolic state [103].
- In Vivo Confirmation: Test the combination in relevant animal models. The efficacy of a combination must be demonstrated in a complex physiological environment where factors like drug penetration and immune response play a role [64].
Q5: What controls are essential when testing antibiotic-metabolic inhibitor combinations against bacterial biofilms? Essential controls include:
- Planktonic Cell Control: Test the combination on free-floating, non-biofilm cells of the same strain to distinguish biofilm-specific effects.
- Vehicle Control: Account for any effect of the solvent used to dissolve the inhibitors.
- Single-Agent Controls: Include wells treated with the antibiotic alone and the metabolic inhibitor alone to demonstrate the synergy of the combination.
- Viability Staining: Combine CFU counts with staining methods (e.g., LIVE/DEAD stains) to visualize the spatial distribution of live and dead cells within the biofilm architecture.
Troubleshooting Guides
Issue: High Background Regrowth in Persister Killing Assays
Problem: After treating a bacterial culture with a bactericidal antibiotic and plating for CFUs, a high number of colonies regrow, making it difficult to distinguish between a true reduction in persisters and simple antibiotic decay or inadequate killing.
Solution:
- Confirm Drug Stability: Ensure the antibiotic remains stable and active for the entire duration of the experiment. Use chemical assays to verify concentration if necessary.
- Optimize Drug Concentration and Time: Perform a time-kill curve with a high, clinically relevant concentration of the antibiotic (e.g., 10x MIC) to establish the baseline killing kinetics for your specific strain [2].
- Include Appropriate Controls: Always include a "no treatment" control and a "drug alone" control for any combination therapy. For the persister assay, after antibiotic exposure, wash cells or use an antidote (e.g., penicillinase for β-lactams) to inactivate the antibiotic before plating, ensuring that regrowth is not due to carry-over effects [64].
- Use Deep Well Plates for Regrowth: When monitoring regrowth in liquid media, use deep well plates with sufficient aeration to prevent anaerobic conditions that can independently affect growth rates.
Issue: Inconsistent Results with Metabolic Inhibitors in Cell Culture
Problem: The sensitizing effect of a metabolic inhibitor on chemotherapy-resistant cancer persister cells varies significantly between experimental replicates.
Solution:
- Standardize "Persister" Generation: The method for generating the persister-like population must be highly consistent. For example, if using high-dose chemotherapy to enrich for persisters, ensure the dose, duration, and cell density are identical across replicates.
- Characterize Metabolic State: Do not assume the inhibitor is working. Use a extracellular flux analyzer to directly measure the metabolic shift (e.g., from oxidative phosphorylation to glycolysis) upon inhibitor application in your specific cell line.
- Verify Inhibitor Efficacy and Specificity: Use Western blotting or other functional assays to confirm that the inhibitor is effectively blocking its intended pathway (e.g., phosphorylation status of key pathway components).
- Control for Cell Cycle Heterogeneity: Since persistence is linked to quiescence, use flow cytometry to analyze cell cycle distributions in your treated populations. Inconsistencies may arise from varying proportions of G0/G1 phase cells.
Issue: Combination Therapy Fails in an In Vivo Model
Problem: A drug combination that showed strong synergy in eradicating persisters in vitro has no effect or a diminished effect in a mouse infection or xenograft model.
Solution:
- Check Pharmacokinetics/Pharmacodynamics (PK/PD): The most common cause of in vivo failure is inadequate drug exposure. Measure the plasma and tissue levels of both drugs to ensure they reach the target site at a sufficient concentration and for the required time to be effective. The dosing regimen may need adjustment from in vitro conditions [64].
- Assess Tumor Penetration or Biofilm Accessibility: Drugs may not adequately penetrate the core of a tumor or a biofilm where the most dormant persisters reside. Use imaging or other techniques to assess drug distribution.
- Consider the Host Microenvironment: The in vivo environment may neutralize the drug (e.g., local pH affecting drug activity) or the host immune response may be a confounding factor. Using immunocompromised models for cancer studies can help isolate drug-specific effects.
Experimental Protocols
Protocol 1: Time-Kill Assay for Antibiotic-Persister Combinations
Objective: To determine the synergistic killing effect of an antibiotic combined with a metabolic inhibitor against bacterial persisters.
Materials:
- Late-log or stationary phase bacterial culture (e.g., S. aureus, E. coli)
- Test antibiotic (e.g., Ciprofloxacin)
- Test metabolic inhibitor (e.g., CCCP - a protonophore that disrupts membrane potential)
- Sterile Phosphate Buffered Saline (PBS)
- Liquid growth media (e.g., Mueller-Hinton Broth)
- Agar plates
- Microcentrifuge tubes and shaking incubator
Method:
- Prepare Inoculum: Adjust the bacterial culture to a standardized density (e.g., ~10^8 CFU/mL) in fresh media.
- Treatment Setup: Aliquot the inoculum into four tubes:
- Tube A (Control): No drug addition.
- Tube B (Antibiotic Only): Add antibiotic at a predetermined concentration (e.g., 10x MIC).
- Tube C (Inhibitor Only): Add the metabolic inhibitor at a sub-inhibitory concentration.
- Tube D (Combination): Add both the antibiotic and the metabolic inhibitor.
- Incubate: Incubate all tubes under optimal growth conditions with shaking.
- Sample and Quantify: At time points 0, 2, 4, 6, 8, and 24 hours, remove aliquots from each tube.
- Serially dilute the samples in PBS.
- Plate appropriate dilutions onto agar plates.
- Incubate plates for 24-48 hours and count CFUs.
- Analyze: Plot the log10 CFU/mL versus time for each condition. Synergy is demonstrated when the killing in the combination tube (D) is significantly greater than the most effective single agent.
Protocol 2: Metabolic Profiling of Cancer Persister Cells
Objective: To characterize the metabolic state of chemotherapy-induced persister cells and validate the action of metabolic inhibitors.
Materials:
- Cancer cell line (e.g., A549, MCF-7)
- Chemotherapeutic agent (e.g., Cisplatin)
- Metabolic inhibitor (e.g., 2-Deoxy-D-glucose, 2-DG, a glycolytic inhibitor)
- Seahorse XF Analyzer culture plates and cartridges
- Assay media (XF base medium supplemented with glucose, glutamine, pyruvate)
- ATP-based viability assay kit
- Flow cytometer
Method:
- Generate Persister Cells: Treat a log-phase cancer cell culture with a high dose of chemotherapy for 48-72 hours. Wash away the drug and allow a "recovery period" in fresh media for 5-7 days. The surviving, non-proliferating cells are enriched for persisters.
- Seahorse XF Cell Mito Stress Test:
- Seed persister-enriched and control cells into a Seahorse XF cell culture plate.
- On the day of the assay, replace media with Seahorse XF assay media.
- Load cartridge with compounds to measure Oxygen Consumption Rate (OCR) and Extracellular Acidification Rate (ECAR) – proxies for oxidative phosphorylation and glycolysis, respectively. Standard compounds include Oligomycin, FCCP, and Rotenone/Antimycin A.
- Run the assay on the Seahorse XF Analyzer.
- Validate with Inhibitor: Treat persister cells with the metabolic inhibitor (e.g., 2-DG) and repeat the Seahorse assay or measure ATP levels to confirm a drop in energy production.
- Correlate with Viability: In parallel, perform a cell viability assay (e.g., CellTiter-Glo) to link the metabolic shift induced by the inhibitor to cell death, especially when combined with a low-dose chemotherapy.
Data Presentation
Table 1: Example In Vitro Data from a Time-Kill Assay Against Staphylococcus aureus Persisters This table illustrates the type of quantitative data needed to demonstrate synergy between an antibiotic and a metabolic inhibitor.
| Treatment Condition | CFU/mL at 0h (log10) | CFU/mL at 24h (log10) | Log Reduction (0-24h) |
|---|---|---|---|
| Growth Control (No drug) | 8.0 | 9.2 | -1.2 (growth) |
| Ciprofloxacin (10x MIC) Only | 8.0 | 5.5 | 2.5 |
| Metabolic Inhibitor X Only | 8.0 | 7.9 | 0.1 |
| Ciprofloxacin + Inhibitor X | 8.0 | 2.5 | 5.5 |
Interpretation: The combination treatment results in a significantly greater log reduction (>3 logs) compared to the most effective single agent (Ciprofloxacin, 2.5 logs), indicating a synergistic killing effect against the persister population.
Table 2: Key Reagent Solutions for Persister Cell Research This table lists essential materials and their functions for studying metabolic heterogeneity and combination therapies.
| Research Reagent / Tool | Function & Application in Persister Research |
|---|---|
| Pyrazinamide (PZA) | A first-line anti-tuberculosis drug used as a positive control for its unique ability to kill dormant M. tuberculosis persisters by disrupting energy metabolism and trans-translation [102]. |
| Glycolytic Inhibitors (e.g., 2-DG) | Blocks glycolysis by inhibiting hexokinase. Used to starve cells of ATP derived from glycolysis and to test if persisters rely on this metabolic pathway for survival [103]. |
| Uncouplers (e.g., CCCP) | Collapses the bacterial proton motive force (PMF). Used to study the role of membrane energetics in persistence and to sensitize cells to aminoglycosides which require PMF for uptake [2] [103]. |
| Seahorse XF Analyzer | An instrument for live-cell metabolic profiling. Critically used to measure OCR and ECAR to characterize the metabolic phenotype (oxidative vs. glycolytic) of persister cells before and after treatment [103]. |
| Viability Stains (e.g., LIVE/DEAD BacLight) | A fluorescent dye kit that distinguishes live (with intact membranes) from dead cells. Used in conjunction with CFU counts to assess the viability of persisters within biofilms or populations without relying on regrowth. |
| CRISPR-Cas Systems | A gene-editing tool. Used to knock out genes suspected to be involved in persister formation (e.g., toxin-antitoxin modules, metabolic regulators) to validate their function [103]. |
Signaling Pathways and Workflows
Diagram: Mechanism of Persister Formation and Targeted Eradication. This diagram illustrates how environmental stressors trigger the formation of a heterogeneous persister population with distinct metabolic states. Key molecular mechanisms underlying their survival are targeted by combination therapies like Pyrazinamide and metabolic inhibitors to achieve eradication.
Diagram: Experimental Workflow for Validating Combination Therapies. This flowchart outlines the key steps for generating, characterizing, and testing combination therapies against persister cells, highlighting critical checkpoints and optimization loops.
Benchmarking Novel Compounds Against Standard-of-Care Treatments
What is the primary challenge in treating diseases characterized by metabolic heterogeneity, such as cancer? The primary challenge is the presence of drug-tolerant persister (DTP) cells. These are a sub-population of tumor cells that survive initial treatment by entering a slow-cycling or quiescent state, often through non-genetic mechanisms like profound metabolic reprogramming. This metabolic heterogeneity allows them to evade standard-of-care (SOC) therapies, leading to disease relapse [104].
Why is it crucial to benchmark new compounds against SOC treatments in this context? Benchmarking is essential to determine whether a novel compound offers a genuine advantage over existing treatments. A new drug may be highly effective against bulk tumor cells, but if it fails to target the metabolically adapted DTP cell population, it will ultimately fail to produce a durable clinical response. Effective benchmarking must, therefore, evaluate compound efficacy not just on general cytotoxicity, but specifically on the eradication of these persistent sub-populations [104].
Experimental Design & Protocols
Protocol 1: Generating and Isating Drug-Tolerant Persister (DTP) Cells
Objective: To establish an in vitro model of a residual disease population for subsequent compound testing [104].
Materials:
- HER2-positive gastric cancer cell line (e.g., NCI-N87)
- Standard cell culture reagents and equipment
- SOC drug: Trastuzumab
- Phosphatase inhibitors (e.g., sodium orthovanadate)
- RIPA lysis buffer
- BCA protein assay kit
- SDS-PAGE and Western blot apparatus
- Antibodies for HER2, pHER2, and β-Actin
Methodology:
- Culture Expansion: Grow cancer cells to 70-80% confluence under standard conditions.
- SOC Treatment: Treat cells with a clinically relevant dose of Trastuzumab (e.g., 10 µg/mL) for a sustained period (e.g., 2-3 weeks).
- DTP Enrichment: The majority of cells will die. Replace the drug-containing medium regularly until a population of slow-growing, adherent DTP cells emerges.
- Model Validation: Confirm the DTP phenotype by analyzing key signaling pathways. As detailed in Table 1, DTP cells often show altered signaling despite SOC treatment.
Table 1: Key Signaling Pathway Adaptations in DTP Cells
| Pathway/Component | Change in DTP Cells | Functional Consequence |
|---|---|---|
| HER2 Signaling | Persistent or reactivated phosphorylation | Sustained survival signals despite targeted therapy [104] |
| PI3K/AKT/mTOR | Alternative activation | Bypasses HER2 blockade to promote cell growth and inhibit apoptosis [104] |
| RAS/RAF/MEK/ERK | Upregulated | Drives proliferation and survival independently of the primary target [104] |
| Metabolic State | Shift towards quiescence & stress tolerance | Reduces dependency on pathways targeted by SOC drugs [104] |
Protocol 2: Spatial Metabolomics to Decode Metabolic Heterogeneity
Objective: To spatially resolve the metabolic landscape of tumor tissue following treatment, identifying unique adaptations in DTP cell niches [105].
Materials:
- Frozen tissue sections (e.g., from patient-derived xenograft models)
¹³C-labeled yeast extract(Key Reagent: serves as a universal internal standard for normalization and relative quantification) [105]Matrix-assisted laser desorption/ionization (MALDI)mass spectrometerSCILS Labsoftware (for data processing and imaging analysis) [106]
Methodology:
- Sample Preparation: Treat tumor-bearing models with SOC or novel compounds. Harvest and snap-freeze tissues. Cryosection tissues onto slides.
- Internal Standard Application: Uniformly spray the
¹³C-labeled yeast extractover the tissue sections. This allows for robust normalization of data across different tissue regions and samples [105]. - Data Acquisition: Perform spatial metabolomics imaging using a
MALDI-mass spectrometer. The technology's principle is outlined in the workflow below. - Data Analysis: Process the raw data using
SCILS Labsoftware. Use it to perform segmentation analysis, which clusters pixels with similar metabolic profiles, thereby identifying distinct metabolic regions (e.g., DTP niches) without prior histological knowledge [106].
Spatial Metabolomics Workflow: From tissue preparation to data visualization.
Protocol 3: Profiling Compound Binding Kinetics with COOKIE-Pro
Objective: To comprehensively evaluate the binding kinetics and selectivity of novel covalent inhibitors across the entire proteome, identifying on-target engagement and potential off-target effects [107].
Materials:
- Ramos cell line (or other relevant cell lines)
COOKIE-Proassay reagentsTMT multiplex labelingkitLiquid Chromatography-Mass Spectrometry (LC-MS/MS)systemCustom MATLAB algorithmsfor data fitting
Methodology:
- Two-Step Incubation: Incubate permeable cells with the covalent inhibitor at varying concentrations and times. This is followed by a second incubation with a matching desthiobiotin probe to label the remaining, unoccupied binding sites [107].
- Proteomic Processing: Lyse cells, digest proteins, and label peptides with a
TMT multiplex kitfor high-throughput quantitative proteomics viaLC-MS/MS[107]. - Kinetic Parameter Calculation: Use developed
MATLAB algorithmsto fit the occupancy data and calculate the inactivation rate (kinact) and the inhibitor constant (KI) for thousands of cysteine sites across the proteome simultaneously [107].
The Scientist's Toolkit: Essential Research Reagents
Table 2: Key Reagents for DTP and Metabolic Heterogeneity Research
| Research Reagent | Function & Application |
|---|---|
| ¹³C-labeled Yeast Extract | A universal internal standard for spatial metabolomics that enables robust relative quantification and cross-sample comparison of hundreds of metabolites [105]. |
| Desthiobiotin Probes | Specially designed chemical probes used in the COOKIE-Pro method to tag unoccupied protein sites, allowing for proteome-wide profiling of covalent inhibitor binding [107]. |
| TMT Multiplex Kits | Reagents for tandem mass tag (TMT) labeling that enable the simultaneous quantification of proteins from multiple experimental conditions in a single LC-MS/MS run, increasing throughput and reducing batch effects [107]. |
| SCILS Lab Software | A commercial software package specifically designed for analyzing mass spectrometry imaging data. It is crucial for spatial clustering, metabolite visualization, and identifying metabolically distinct regions [106]. |
Data Analysis & Interpretation
How do I quantify and compare the efficacy of a novel compound versus a SOC treatment? A comprehensive benchmarking analysis should generate a multi-parameter dataset. The table below summarizes key quantitative metrics to collect.
Table 3: Quantitative Benchmarking of Novel Compound vs. SOC
| Metric | SOC Treatment | Novel Compound | Significance |
|---|---|---|---|
| IC50 (Bulk Cells) | e.g., 5 nM | e.g., 2 nM | Measures potency against the main tumor population. |
| DTP Cell Viability (%) | e.g., 65% | e.g., 20% | Critical metric. Lower viability indicates superior efficacy against the persistent population [104]. |
| Metabolic Heterogeneity (Spatial Entropy) | e.g., High | e.g., Low | Calculated from spatial metabolomics data. A reduction suggests the compound normalizes the metabolic landscape [105]. |
| Selectivity Index (kinact/KI) | e.g., 9.15 x 10â´ Mâ»Â¹sâ»Â¹ | e.g., 7.06 x 10âµ Mâ»Â¹sâ»Â¹ | From COOKIE-Pro. A higher value indicates more potent and selective binding to the intended target over off-targets [107]. |
Troubleshooting FAQs
FAQ 1: Our novel compound shows excellent efficacy against bulk tumor cells but fails to reduce DTP cell viability. What could be the reason? This is a common issue indicating that the compound's mechanism of action may not address the specific survival pathways utilized by DTPs. We recommend:
- Profile Metabolic Dependencies: Use the spatial metabolomics protocol (2.2) to identify the specific energy and biosynthetic pathways (e.g., lysine uptake, UDP-GlcNAc levels) that are active in the DTP niches within your model [105]. This can reveal therapeutic vulnerabilities.
- Check for Signaling Reactivation: Perform Western blotting on your isolated DTP cells (from Protocol 2.1) to see if alternative pathways like PI3K/AKT/mTOR or RAS/RAF/MEK/ERK are reactivated, providing a bypass survival signal [104].
FAQ 2: The spatial metabolomics data shows high technical variation, making it difficult to interpret biological differences. How can we improve data quality? The key to robust quantification in spatial metabolomics is a superior normalization strategy.
- Implement Universal Internal Standards: Adopt the method of using a
¹³C-labeled yeast extractas an internal standard. This approach has been proven to outperform traditional normalization methods, correcting for matrix effects and enabling more sensitive detection of true biological changes, such as those in stroke-affected brain regions [105].
FAQ 3: We are concerned that our novel covalent inhibitor might have off-target effects. How can we systematically evaluate this before moving to in vivo studies? Traditional assays are insufficient for proteome-wide off-target profiling.
- Adopt Proteome-Wide Kinetic Profiling: Utilize the
COOKIE-Promethod (Protocol 2.3). This technique moves beyond simple binding identification to actually measure the binding kinetics (kinact/KI) for thousands of potential targets across the proteome in a single experiment. This allows you to objectively rank off-targets by their engagement strength and make informed decisions on compound optimization for selectivity [107].
Assessing Therapeutic Windows and Off-Target Toxicity of Anti-Persister Agents
Frequently Asked Questions (FAQs) and Troubleshooting
Q1: Why are anti-persister agents that target fundamental structures like cell membranes often associated with a narrow therapeutic window? How can this be mitigated?
A: Agents that directly disrupt bacterial membranes (e.g., synthetic cation transporters, thymol conjugates) are highly effective because their action is independent of bacterial metabolic activity [3]. However, their fundamental mechanism of action—disrupting lipid bilayers—poses a high risk of off-target toxicity against mammalian cells, which inherently narrows the therapeutic window [3]. This is a central challenge in their development.
- Troubleshooting Tip: If your in vitro screening indicates high cytotoxicity (e.g., low selectivity index), consider these strategies:
- Explore Combination Therapy: Use lower, sub-lethal concentrations of the membrane-targeting agent to permeabilize the persister cells, thereby sensitizing them to a conventional antibiotic. This can achieve eradication while reducing the required dose of the toxic agent [3] [108].
- Leverage Formulation: Utilize nanoparticle-based delivery systems (e.g., red blood cell membrane-coated nanoparticles) to improve targeted delivery to infection sites, potentially reducing systemic exposure and toxicity [3].
Q2: Our "wake-and-kill" strategy, using metabolites to resuscitate persisters, is not consistently potentiating antibiotic efficacy across all persister sub-populations. What could be the cause?
A: This issue directly reflects the metabolic heterogeneity of persister populations. The "wake-and-kill" approach relies on stimulating specific metabolic pathways to activate antibiotic uptake mechanisms [6]. Failure suggests that the exogenous metabolite you are using may not be the correct carbon or energy source for every persister subtype in your model.
- Troubleshooting Guide:
- Problem: Inconsistent potentiation of aminoglycosides.
- Potential Cause: The persister population contains metabolically distinct subtypes (e.g., some reliant on glycolysis, others on the TCA cycle) [109].
- Solution: Profile the metabolic state of your persister population. Test a panel of different metabolites (e.g., pyruvate, sugars, amino acids like L-valine) known to stimulate divergent metabolic pathways [6]. Combining metabolites may be necessary to cover a broader spectrum of the dormant population.
Q3: We observe that knocking out global metabolic regulators (like Crp/cAMP) reduces persister formation, but also severely impairs general bacterial fitness. Is this a viable therapeutic target?
A: This is a key consideration. Targeting master regulators like Crp/cAMP, which redirects metabolism from anabolism to oxidative phosphorylation in persisters, is effective at reducing persistence but can have pleiotropic effects [109]. The viability of such a target depends on the strategy.
- Recommendation: Instead of aiming to knockout the regulator entirely, focus on fine-tuning its activity. The goal should be to identify downstream effectors or specific interactions that are disproportionately critical for persister metabolism but less so for normal bacterial growth. This approach may help in designing inhibitors that disrupt persistence mechanisms with a wider therapeutic window than targeting the core regulator itself.
Q4: How can we accurately assess the therapeutic window of a new anti-persister compound in pre-clinical models?
A: A robust assessment requires a multi-tiered approach:
- In Vitro Determination: First, establish the Minimum Biofilm Eradication Concentration (MBEC) against persister-rich biofilms and the cytotoxic concentration 50 (CC50) against relevant mammalian cell lines (e.g., hepatocytes, kidney cells). Calculate a preliminary Selectivity Index (SI = CC50 / MBEC) [3] [110].
- In Vivo Validation: Move to animal models of chronic infection (e.g., catheter-associated biofilm models, chronic lung infection models) [110]. The therapeutic window is defined by the dose range between the lowest dose that significantly reduces bacterial burden and the dose that induces observable toxicological effects.
- Pharmacokinetic/Pharmacodynamic (PK/PD) Analysis: Measure compound concentration at the site of infection versus plasma concentration over time. A favorable window is indicated by sustained anti-persister concentrations at the infection site that remain below toxic plasma levels [110].
Quantitative Data on Anti-Persister Strategies and Toxicity
The table below summarizes the primary strategies for combating persister cells, their mechanisms, and inherent challenges related to therapeutic windows.
Table 1: Anti-Persister Strategies and Associated Challenges
| Strategy | Mechanism of Action | Advantages | Limitations & Toxicity Concerns |
|---|---|---|---|
| Direct Killing (Membrane Targeting) | Disrupts bacterial membrane integrity, causes lysis and ROS generation [3]. | Independent of bacterial growth state or metabolic activity [3]. | High risk of off-target toxicity to mammalian membranes, limiting therapeutic potential [3]. |
| "Wake-and-Kill" (Metabolic Potentiation) | Uses metabolites (e.g., sugars, L-valine) to resuscitate persisters, making them susceptible to traditional antibiotics [6]. | Leverages existing antibiotic libraries; can delay resistance [6]. | Efficacy is highly dependent on the metabolic heterogeneity of the persister population; local metabolite delivery in vivo is challenging [6]. |
| Inhibiting Persister Formation | Alters bacterial communication (QS) or inhibits stress responses (e.g., Hâ‚‚S biogenesis) to reduce persister formation [3]. | Bacteria-specific targets; reduces antibiotic tolerance at its source [3]. | May not be effective against already-formed persisters; potential to exert evolutionary pressure [3]. |
| Synergistic Antibiotic Combinations | Pairs antibiotics with strongly and weakly metabolism-dependent (SDM/WDM) activities to kill both active and dormant cells [108]. | Can eradicate entire populations with dose-sparing effects, potentially widening the therapeutic window [108]. | Optimal combinations are pathogen and context-specific; interactions are not detectable in standard growth inhibition assays [108]. |
Key Signaling Pathways in Persister Metabolism and Eradication
The following diagram illustrates the core metabolic pathways involved in persister cell survival and the points of intervention for "wake-and-kill" strategies, which are central to addressing metabolic heterogeneity.
Metabolic Pathways in Persister Eradication. This diagram shows how exogenous metabolites can reprogram the metabolism of a heterogeneous persister population, reversing dormancy and facilitating antibiotic-mediated killing. The Crp/cAMP complex and (p)ppGpp-mediated stringent response are key regulators. Interventions (blue nodes) force metabolic activation, enhancing the TCA cycle and Electron Transport Chain (ETC). This increases the Proton Motive Force (PMF), which drives the uptake of antibiotics like aminoglycosides, leading to cell death [6] [109].
The Scientist's Toolkit: Essential Research Reagents
Table 2: Key Reagents for Anti-Persister Metabolic Research
| Reagent | Function in Experiment | Key Consideration |
|---|---|---|
| CFDA / PI Staining Kit | Flow cytometry-based isolation of persister cells by differentiating membrane integrity and esterase activity [111] [112]. | Allows for isolation of pure persister populations without using antibiotics, preventing stress-response induction during isolation [112]. |
| Lysozyme & Osmotic Lysis Solutions | Key components of antibiotic-free persister isolation protocols, enzymatically degrading cell walls of non-persisters [112]. | Can be optimized to differentiate between Type I (stationary phase) and Type II (spontaneous) persisters [112]. |
| Specific Metabolites (e.g., Pyruvate, L-Valine, Mannitol) | Used in "wake-and-kill" assays to resuscitate metabolically dormant persisters and potentiate aminoglycoside activity [6]. | Metabolite choice is critical; screening a panel is recommended to account for metabolic heterogeneity in the persister population [6]. |
| Membrane-Targeting Compounds (e.g., XF-73, SA-558) | Positive controls for direct, metabolism-independent killing of persister cells via membrane disruption [3]. | Useful for benchmarking, but often exhibit high cytotoxicity in mammalian cell assays, highlighting the therapeutic window challenge [3]. |
| Hâ‚‚S Biosynthesis Inhibitors (e.g., CSE Inhibitors) | Investigational tools to inhibit persister formation by blocking a key bacterial stress defense system [3]. | Reduces persister formation and can potentiate conventional antibiotics, offering a prophylactic or combination approach [3]. |
Experimental Protocol: Metabolite Potentiation of Antibiotics
This protocol details a standard method for assessing the efficacy of a "wake-and-kill" strategy, a key technique for probing persister metabolic heterogeneity.
Aim: To determine if an exogenous metabolite can re-sensitize bacterial persisters to a specific antibiotic.
Procedure:
- Persister Enrichment:
- Inoculate bacteria in a suitable broth and grow to the desired phase (e.g., late stationary phase for high persister numbers) [109].
- Alternatively, treat a mid-log phase culture with a high concentration of a bactericidal antibiotic (e.g., a fluoroquinolone) for 3-5 hours. Centrifuge and wash the pellet to remove the antibiotic [111].
Metabolite Potentiation Assay:
- Resuspend the persister-enriched pellet in a minimal buffer or medium.
- Divide the suspension into the following treatment groups in a 96-well plate:
- Group 1: Buffer only (Control for viability).
- Group 2: Metabolite only (e.g., 10 mM Pyruvate [6]).
- Group 3: Antibiotic only (e.g., Gentamicin at a relevant concentration).
- Group 4: Metabolite + Antibicide.
- Incubate the plate under appropriate conditions for 4-24 hours.
Viability Assessment:
- Serially dilute the cultures at the end of the incubation period.
- Spot the dilutions onto nutrient-rich agar plates.
- Count the colony-forming units (CFUs) after 24-48 hours of growth.
Data Analysis:
- Compare the log-reduction in CFU/mL between Group 3 (Antibiotic only) and Group 4 (Metabolite + Antibiotic).
- A statistically significant greater reduction in Group 4 indicates successful metabolite-mediated potentiation of the antibiotic, suggesting the metabolite successfully altered the metabolic state of the persisters [6].
Conclusion
Metabolic heterogeneity in persister cells is not a peripheral observation but a central, targetable axis of treatment failure. The synthesis of research across bacterial and cancer systems reveals conserved principles: metabolic diversity arises from both pre-existing stochastic variation and dynamic induction by therapy, creating a resilient continuum of cell states. Future progress hinges on developing more physiologically relevant models that capture host-microenvironment interactions, advancing dynamic single-cell metabolic imaging in vivo, and designing clinical trials that specifically evaluate anti-persister strategies. Successfully targeting this heterogeneity—by either forcing vulnerable metabolic states or exploiting fixed metabolic vulnerabilities—holds the key to eradicating the persister reservoir and achieving durable cures for persistent infections and cancer.
References
- 1. Cancer drug-tolerant persister cells: from biological questions to clinical opportunities | Nature Reviews Cancer [https://www.nature.com/articles/s41568-024-00737-z]
- 2. Bacterial persisters: molecular mechanisms and ... [https://www.nature.com/articles/s41392-024-01866-5]
- 3. Mini review: Persister cell control strategies - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC12568461/]
- 4. Bacterial Metabolic Heterogeneity: Origins and Applications in ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC7485380/]
- 5. Definitions and guidelines for research on antibiotic ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC7136161/]
- 6. Metabolite-driven reprogramming of bacterial persisters [https://www.sciencedirect.com/science/article/abs/pii/S1368764625001256]
- 7. Metabolic aspects of bacterial persisters - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC4205924/]
- 8. Molecular Mechanisms Underlying Bacterial Persisters [https://www.sciencedirect.com/science/article/pii/S0092867414002979]
- 9. Observation of persister cell histories reveals diverse ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12074638/]
- 10. Stochastic gene expression and its consequences - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC3118044/]
- 11. 15. The noisy, noisy nature of gene expression [https://biocircuits.github.io/chapters/15_noise.html]
- 12. Gene function revealed at the moment of stochastic ... [https://www.nature.com/articles/s42003-025-07530-0]
- 13. Metabolic heterogeneity in clonal microbial populations [https://www.sciencedirect.com/science/article/pii/S1369527417301935]
- 14. Gene expression variations are predictive for stochastic noise [https://pmc.ncbi.nlm.nih.gov/articles/PMC3025572/]
- 15. Drug-tolerant persister cells in cancer: bridging the gaps ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12623778/]
- 16. Epigenetic reprogramming as the nexus of cancer ... [https://link.springer.com/article/10.1007/s12672-025-04085-8]
- 17. Multi-omics based and AI-driven drug repositioning for ... [https://translational-medicine.biomedcentral.com/articles/10.1186/s12967-025-06856-x]
- 18. Epigenetic regulators in cancer therapy and progression [https://www.nature.com/articles/s41698-025-01003-7]
- 19. Transcriptional Condensates: Epigenetic Reprogramming ... [https://www.mdpi.com/2072-6694/17/19/3148]
- 20. Unraveling CRP/cAMP-mediated metabolic regulation in ... [https://elifesciences.org/articles/99735]
- 21. Advances in linking single cell bacterial stress response to ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC9899315/]
- 22. Diverse molecular mechanisms of transcription regulation by ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC9304144/]
- 23. Frontiers | Molecular Mechanisms of Bacterial Clinical Pathogens... [https://www.frontiersin.org/research-topics/11176/molecular-mechanisms-of-bacterial-clinical-pathogens-tolerance-and-persistence-under-stress-conditions-tolerant-and-persister-cells]
- 24. Bacterial toxin-antitoxin modules: classification, functions, and ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC8610362/]
- 25. Biology and evolution of bacterial toxin–antitoxin systems [https://www.nature.com/articles/s41579-021-00661-1]
- 26. Phenotypic Diversity Using Bimodal and Unimodal ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC4881231/]
- 27. Multiomics Data Collection, Visualization, and Utilization ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC7902046/]
- 28. A Practical Guide to Integrating Multimodal Machine ... [https://pubmed.ncbi.nlm.nih.gov/35604554/]
- 29. Multi-modal characterization of metabolic and immune ... [https://www.nature.com/articles/s41698-025-01092-4]
- 30. Single-Cell Technologies to Study Phenotypic ... [https://www.mdpi.com/2076-2607/9/11/2277]
- 31. Novel Secondary Ion Mass Spectrometry Methods for the ... [https://www.frontiersin.org/journals/behavioral-neuroscience/articles/10.3389/fnbeh.2020.00124/full]
- 32. Single-Cell Analysis with NanoSIMS [https://dekaslab.stanford.edu/research/single-cell-analysis-nanosims]
- 33. NanoSIMS 50L [https://www.cameca.com/products/sims/nanosims]
- 34. A Multimodal Imaging Pipeline to Decipher Cell-Specific ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC7617660/]
- 35. Metabolic flux analysis: a comprehensive review on sample ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC9449821/]
- 36. Metabolic heterogeneity in microbial populations [https://www.ideals.illinois.edu/items/103401]
- 37. Cycling cancer persister cells arise from lineages with distinct programs [https://pubmed.ncbi.nlm.nih.gov/34381210/]
- 38. Protocol for assessing single-cell persister recovery ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11015153/]
- 39. Metabolic heterogeneity in tumor cells impacts immunology in ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11812363/]
- 40. Intact protein barcoding enables one-shot identification of ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11704613/]
- 41. Next generation lineage tracing and its applications ... [https://www.nature.com/articles/s41540-025-00542-w]
- 42. Mini review: Persister cell control strategies [https://www.frontiersin.org/journals/pharmacology/articles/10.3389/fphar.2025.1706115/full]
- 43. Strategies to Combat Multidrug-Resistant and Persistent ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC7168131/]
- 44. A high-throughput assay identifies molecules with ... [https://pubmed.ncbi.nlm.nih.gov/38995832/]
- 45. High Throughput Screening (HTS) [https://www.atcc.org/the-science/drug-discovery/high-throughput-screening]
- 46. Flow-cytometry analysis reveals persister resuscitation ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC7346475/]
- 47. Current Methods for Quantifying Drug Synergism - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC7010330/]
- 48. Synergistic effect of antibiotic combinations on ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC8844754/]
- 49. A Quantitative High-Throughput Screening Data Analysis ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC9540341/]
- 50. Metabolic Priming as a Tool in Redox and Mitochondrial ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10215850/]
- 51. Antibiotic persisters are metabolically active, non-growing ... [https://www.sciencedirect.com/science/article/pii/S0924857924003029]
- 52. Metabolic priming alters the morphology and ... [https://pubmed.ncbi.nlm.nih.gov/41220916/]
- 53. Targeted Metabolomics - PMC - PubMed Central - NIH [https://pmc.ncbi.nlm.nih.gov/articles/PMC3334318/]
- 54. Small molecule metabolites: discovery of biomarkers and ... [https://www.nature.com/articles/s41392-023-01399-3]
- 55. Recent advances in selective and targeted drug/gene delivery ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC9807432/]
- 56. Targeted vs Untargeted Metabolomics [https://www.metabolon.com/blog/targeted-vs-untargeted-metabolomics/]
- 57. Definitions and guidelines for research on antibiotic ... [https://www.nature.com/articles/s41579-019-0196-3]
- 58. Combatting persister cells: The daunting task in post- ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10250163/]
- 59. Drug-tolerant persister cells in cancer: bridging the gaps ... [https://www.nature.com/articles/s41467-025-66376-6]
- 60. Non-genetic Drug Tolerance Mechanisms [https://www.forbeckforums.org/forums/non-genetic-drug-tolerance-mechanisms]
- 61. Persistence, Apoptosis, and Minimal Residual Disease [https://www.forbeckforums.org/forums/persistence-apoptosis-and-minimal-residual-disease]
- 62. Seeding, Subculturing, and Maintaining Cells [https://www.thermofisher.com/us/en/home/references/gibco-cell-culture-basics/maintaining-cultured-cells.html]
- 63. Accelerating Experimental Success Using a Systematic ... [https://evidentscientific.com/en/learn/white-papers/success-systematic-cell-culture-workflow]
- 64. Phenotypic heterogeneity in persisters: a novel 'hunker' ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC8767447/]
- 65. Resolving Metabolic Heterogeneity in Experimental Models of ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC7345423/]
- 66. Drug-tolerant persister cell in cancer: reversibility ... [https://www.frontiersin.org/journals/pharmacology/articles/10.3389/fphar.2025.1612089/full]
- 67. sciencedirect.com/topics/neuroscience/ persister - cell [https://www.sciencedirect.com/topics/neuroscience/persister-cell]
- 68. Bacterial Persister Cells and Development of Antibiotic ... - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC11335562/]
- 69. Frontiers | Persistence of Intracellular Bacterial Pathogens—With a Focus on the Metabolic Perspective [https://www.frontiersin.org/journals/cellular-and-infection-microbiology/articles/10.3389/fcimb.2020.615450/full]
- 70. Cellular heterogeneity: when do differences make a difference? - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC2918286/]
- 71. Advancements and challenges in culturing patient-derived ... [https://www.frontiersin.org/journals/lab-on-a-chip-technologies/articles/10.3389/frlct.2025.1663420/full]
- 72. Applications of Tumor Cells in an In Vitro 3D Environment [https://www.mdpi.com/2076-3417/13/18/10349]
- 73. Persister Heterogeneity Arising from a Single Metabolic Stress - PubMed [https://pubmed.ncbi.nlm.nih.gov/26255847/]
- 74. In Vitro Models of Bacterial Biofilms: Innovative Tools to ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10004855/]
- 75. Recent developments in in vitro and in vivo models for ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC8381685/]
- 76. Challenges and Opportunities with Predicting in Vivo Phase II ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC5613675/]
- 77. In Vitro to In Vivo Translation in Lead Optimization [https://www.sygnaturediscovery.com/news-and-events/blog/in-vitro-to-in-vivo-translation-in-lead-optimization/]
- 78. Study on In Vitro Metabolism and In Vivo Pharmacokinetics of ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC9320654/]
- 79. Metabolomics and lipidomics strategies in modern drug ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10543515/]
- 80. A Guide to Multi-omics Integration Strategies [https://frontlinegenomics.com/a-guide-to-multi-omics-integration-strategies/]
- 81. Multi-Omics: Challenges and Solutions [https://bigomics.ch/blog/key-challenges-in-multi-omics-data-integration/]
- 82. continuous phenotyping of single-cell multi-omics data - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC12482742/]
- 83. A Guide to Single-Cell Multiomics Data Analysis [https://www.bdbiosciences.com/en-us/learn/science-thought-leadership/blogs/single-cell-multiomics-data-analysis-guide]
- 84. 5 tips for successful single-cell RNA-seq [https://www.takarabio.com/about/bioview-blog/tips-and-troubleshooting/5-tips-to-make-your-single-cell-rna-seq-experiments-a-success?srsltid=AfmBOoqHR_ekUO1Jq9RZ929MoyEqDuFFEZtZhPfp_q59tqaIDzQfSUrr]
- 85. The Technical Foundations of Single-Cell Omics [https://www.cellenion.com/designing-for-discovery/]
- 86. Membrane-disruptive peptides/peptidomimetics-based ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC8463292/]
- 87. Mode-of-Action of Antimicrobial Peptides: Membrane ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC8757789/]
- 88. Antimicrobial peptides: mechanism of action, activity and ... [https://mmrjournal.biomedcentral.com/articles/10.1186/s40779-021-00343-2]
- 89. Antimicrobial Peptides: Diversity, Mechanism of Action ... - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC5871973/]
- 90. Antimicrobial Mechanisms and Clinical Application ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC9104849/]
- 91. Mechanisms and Strategies for Effective Eradication [https://pubmed.ncbi.nlm.nih.gov/38940498/]
- 92. When to wake up? The optimal waking-up strategies for ... - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC7904209/]
- 93. Anti-virulence therapeutic strategies against bacterial ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC9719373/]
- 94. Recent Advances in Anti-virulence Therapeutic Strategies ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC6454102/]
- 95. Specific Antivirulence Activity, A New Concept for Reliable ... [https://www.sciencedirect.com/science/article/abs/pii/S0167779916000226]
- 96. Antimicrobial strategy for targeted elimination of different ... [https://www.nature.com/articles/s42003-022-03586-4]
- 97. Recent Advances in Bacterial Persistence Mechanisms - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC10531727/]
- 98. Bacterial Persister Cells and Development of Antibiotic ... [https://www.frontierspartnerships.org/journals/british-journal-of-biomedical-science/articles/10.3389/bjbs.2024.12958/full]
- 99. Drug-tolerant persister cell in cancer - PubMed Central - NIH [https://pmc.ncbi.nlm.nih.gov/articles/PMC12391116/]
- 100. Antibacterial nanoagents: an emerging arsenal against ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12537890/]
- 101. Targeting Drug-Tolerant Persister Cancer Cells [https://www.mdpi.com/1999-4923/17/11/1428]
- 102. ç»“æ ¸ç—… è¯ æ²» 物 的过去ã€çŽ°çŠ¶åŠæœªæ¥ - PMC ç–— [https://pmc.ncbi.nlm.nih.gov/articles/PMC10262004/]
- 103. 的分å机 抗 åŠ ç”Ÿ èŒç–ç•¥ ç´ è€ è¯ æ€§ 制 抑 [https://ccj.pku.edu.cn/article/info?aid=375603514]
- 104. 综述:针对è€è¯æ€§æŒä¹…细胞以克æœHER2阳性胃癌的 ... [https://www.ebiotrade.com/newsf/2025-11/20251124083759878.htm]
- 105. 王罡ç¦ç ”究员在《Nature Metabolism》å‘表空间代谢组å¦é¢†åŸŸ ... [https://bydrug.pharmcube.com/news/detail/5a4b8730d73e374154ee01188dd174ad]
- 106. 常è§é—®é¢˜ - 质谱多组å¦å¹³å°_创新生命科å¦æœåŠ¡ [https://testhome.aptbiotech.com/problem/category0_8]
- 107. COOKIE-Pro:蛋白质组尺度共价抑制剂结åˆåŠ¨åŠ›å¦åˆ†æž ... [https://www.ebiotrade.com/newsf/2025-10/20251001031513678.htm]
- 108. Eradicating Bacterial Persisters with Combinations of ... [https://www.sciencedirect.com/science/article/pii/S2451945620303378]
- 109. Unraveling CRP/cAMP-mediated metabolic regulation in ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12237405/]
- 110. Fighting bacterial persistence: Current and emerging anti- ... [https://www.sciencedirect.com/science/article/abs/pii/S1368764618300232]
- 111. Isolation and characterization of persisters of the pathogenic ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11166702/]
- 112. Novel Protocol for Persister Cells Isolation | PLOS One [https://journals.plos.org/plosone/article?id=10.1371/journal.pone.0088660]