Comparative Mechanisms of Bacterial Persister Formation: From Molecular Pathways to Therapeutic Innovation
This article provides a comprehensive analysis of the mechanisms underlying bacterial persister cell formation across major pathogenic species.
Comparative Mechanisms of Bacterial Persister Formation: From Molecular Pathways to Therapeutic Innovation
Abstract
This article provides a comprehensive analysis of the mechanisms underlying bacterial persister cell formation across major pathogenic species. Tailored for researchers, scientists, and drug development professionals, it synthesizes foundational knowledge on shared and species-specific pathways, including toxin-antitoxin modules, the stringent response, and biofilm-mediated tolerance. It further explores advanced methodologies for persister research, current challenges in therapeutic development, and a comparative evaluation of persistence strategies in organisms such as Escherichia coli, Pseudomonas aeruginosa, Mycobacterium tuberculosis, and Salmonella. The review concludes by outlining future directions for overcoming treatment failures in chronic and recurrent infections, aiming to bridge the gap between basic research and clinical application.
Defining the Dormant Threat: Core Concepts and Universal Pathways in Persister Formation
The relentless challenge of treating bacterial infections stems not only from the well-known phenomenon of antibiotic resistance but also from the more elusive concept of antibiotic persistence. While both enable bacterial survival under antimicrobial treatment, they represent fundamentally distinct survival strategies with critical implications for therapeutic outcomes and public health [1] [2]. Antibiotic resistance refers to heritable genetic changes that enable bacteria to grow in the presence of antibiotics, typically through mechanisms that prevent the drug from binding to its target or actively remove it from the cell [3]. In contrast, bacterial persistence describes a transient, non-heritable phenotypic state in which a small subpopulation of genetically susceptible cells enters a dormant or slow-growing state, thereby surviving antibiotic exposure without genetic alteration [4] [5].
This distinction is clinically paramount: resistant strains lead to treatment failure against which alternative antibiotics must be sought, while persister cells underlie chronic, relapsing infections that resume after treatment cessation, complicating conditions such as tuberculosis, cystic fibrosis, and biofilm-associated infections [1] [2]. Understanding the mechanistic differences between these phenomena is thus essential for developing effective therapeutic strategies to combat persistent infections.
Table 1: Fundamental Distinctions Between Antibiotic Resistance and Persistence
| Characteristic | Antibiotic Resistance | Antibiotic Persistence |
|---|---|---|
| Genetic Basis | Heritable genetic mutations or acquired resistance genes [3] | Non-heritable, phenotypic variation without genetic change [4] |
| Population Effect | Entire population grows in antibiotic presence [4] | Small subpopulation (0.001-1%) survives but does not grow during treatment [5] [6] |
| MIC Change | Minimum Inhibitory Concentration (MIC) increased [3] | MIC unchanged; population exhibits tolerance [1] |
| Reversibility | Stable and irreversible | Transient and reversible upon antibiotic removal [2] |
| Clinical Impact | Treatment failure requiring alternative drugs | Chronic, relapsing infections after treatment [1] |
Molecular Mechanisms: Contrasting Pathways to Survival
Genetic Foundations of Antibiotic Resistance
Antibiotic resistance emerges through specific genetic alterations that enable bacteria to neutralize, exclude, or modify antimicrobial agents. These mechanisms include: (1) * enzymatic inactivation* of antibiotics, such as β-lactamases that hydrolyze β-lactam antibiotics; (2) target modification that reduces antibiotic binding affinity; (3) reduced permeability of cellular envelopes through porin alterations; and (4) active efflux of antibiotics via membrane transporters [3] [7]. These resistance determinants can be acquired through horizontal gene transfer or emerge via selective pressure from mutations in chromosomal genes, resulting in stable, heritable resistance that enables growth under antibiotic pressure [7].
Phenotypic Basis of Bacterial Persistence
Persister cells survive antibiotic treatment not through genetic resistance mechanisms but via phenotypic switching to a dormant or slow-growing state [4]. This transition is mediated by diverse molecular mechanisms that include:
Toxin-Antitoxin (TA) Systems: These genetic modules consist of a stable toxin that disrupts essential cellular processes (e.g., translation, DNA replication) and a labile antitoxin that neutralizes the toxin [4]. Under stress conditions, activation of toxins such as HipA, MqsR, and TisB induces a dormant state by inhibiting translation through mRNA cleavage or reducing ATP levels [4] [5]. For instance, MqsR cleaves mRNA at GCU sites, dramatically reducing cellular translation and inducing dormancy [4].
Stringent Response: Nutrient limitation and other stresses trigger the accumulation of the alarmone (p)ppGpp, which redirects cellular resources from growth to maintenance, promoting a persistent state [4].
Reduced Metabolism: Persisters exhibit downregulated metabolic activity, particularly in central carbon metabolism and energy production, which protects them from antibiotics that corrupt active cellular processes [1] [5].
These mechanisms collectively enable a small bacterial subpopulation to enter a transient, drug-tolerant state without genetic alteration, distinguishing persistence from genuine resistance.
Detection Methodologies: Experimental Approaches for Discrimination
Establishing Persistence: The Time-Kill Assay
The gold standard for detecting persister cells is the time-kill curve assay, which demonstrates the characteristic biphasic killing pattern where the majority of cells die rapidly while a small subpopulation survives prolonged antibiotic exposure [6].
Table 2: Key Experimental Protocols for Distinguishing Resistance and Persistence
| Method | Protocol Overview | Interpretation of Results |
|---|---|---|
| Time-Kill Curve Assay | Expose bacterial culture to bactericidal antibiotic; plate samples at intervals (1, 3, 5, 7, 20h) after washing away antibiotic; count CFUs [6] | Biphasic killing curve indicates persistence; subpopulation survives without regrowth during treatment [5] [6] |
| Minimum Inhibitory Concentration (MIC) | Standard broth microdilution following EUCAST/CLSI guidelines [6] | Elevated MIC indicates resistance; unchanged MIC with survival in time-kill indicates persistence [1] |
| Population Analysis Profile (PAP) | Plate serial dilutions of culture on antibiotic gradient plates; enumerate colonies after 24-48h incubation | Resistant mutants grow at high concentrations; persisters show small subpopulation surviving across concentrations |
Detailed Protocol for Time-Kill Assy:
- Grow bacterial cultures to mid-log phase (OD600 ≈ 0.2-0.3) in appropriate broth [6].
- Add bactericidal antibiotic at high concentration (typically 10-100× MIC) [6].
- Incubate at 37°C with shaking.
- At predetermined timepoints (e.g., 1, 3, 5, 7, and 20 hours), remove aliquots and wash cells with sterile saline to remove antibiotic [6].
- Perform serial dilutions and plate on antibiotic-free agar.
- Count colonies after 24-48 hours incubation and plot log CFU/mL versus time.
- Include antibiotic-free control to monitor normal growth [6].
Distinguishing Genetic Resistance
To confirm whether survival stems from resistance or persistence, researchers must:
- Determine MIC values for surviving cells - persisters will exhibit unchanged MIC compared to original population [1].
- Subculture surviving cells in antibiotic-free medium, then re-challenge with the same antibiotic - persister descendants regain sensitivity while resistant mutants maintain resistance [4] [2].
- Perform genetic analysis to identify resistance mutations or genes in surviving populations [7].
Mechanistic Pathways of Persister Formation and Awakening
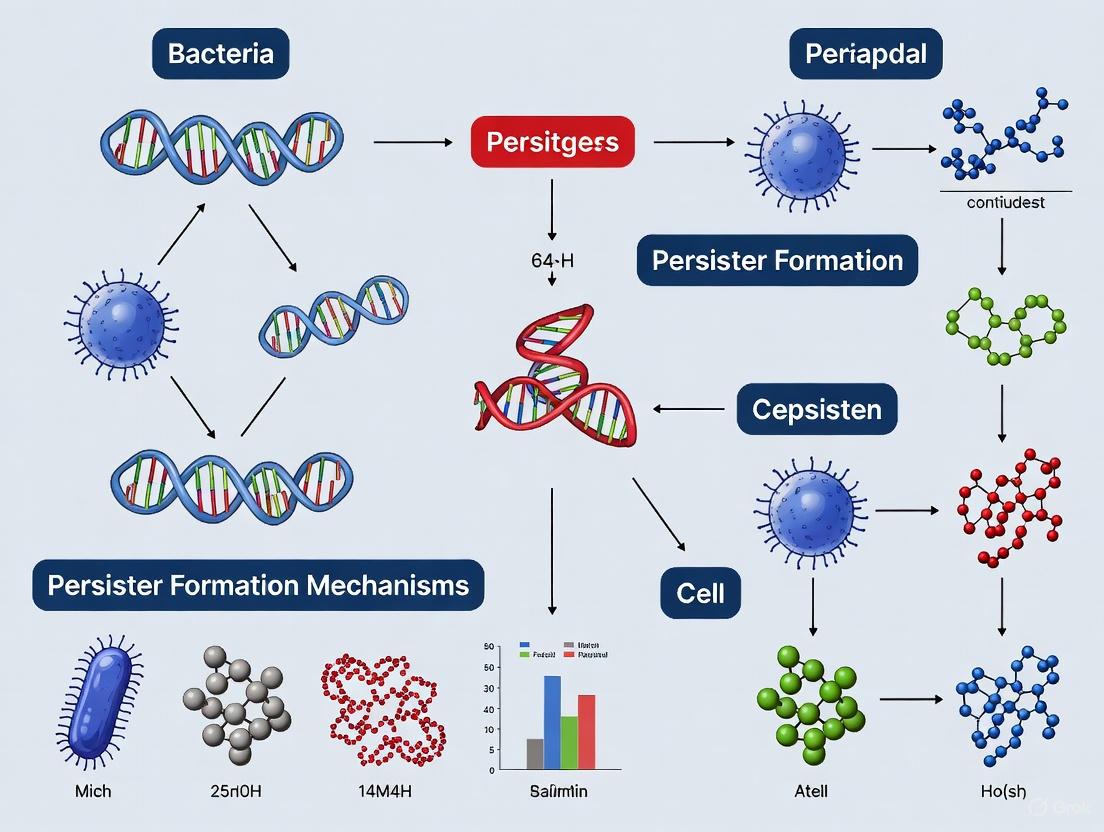
The formation and resuscitation of persister cells can be visualized as a dynamic cycle of entry into and exit from the persistent state. The following diagram illustrates the key regulatory pathways and environmental triggers that govern these transitions:
Diagram 1: Regulatory pathways of persister cell formation and awakening. Environmental stressors trigger persistence through toxin-antitoxin systems and (p)ppGpp signaling, leading to metabolic shutdown. Awakening occurs stochastically or in response to environmental signals.
Research Toolkit: Essential Reagents and Methodologies
Table 3: Essential Research Reagents and Tools for Studying Persistence and Resistance
| Reagent/Technique | Specific Examples | Research Application |
|---|---|---|
| Bactericidal Antibiotics | Ciprofloxacin (0.1 mg/mL), Gentamicin (0.1-0.4 mg/mL) [6] | Time-kill assays to distinguish persisters via biphasic killing curves [6] |
| Culture Media | Mueller-Hinton Agar/Broth, Luria-Bertani (LB) Broth [6] | Standardized antimicrobial susceptibility testing and bacterial cultivation |
| Molecular Biology Reagents | PCR primers for persistence genes (mazF, hipA, relE) [6] | Detection of toxin-antitoxin system genes associated with persistence |
| Antibiotic Susceptibility Testing | EUCAST/CLSI recommended discs and concentrations [6] | Determination of MIC values to distinguish resistance from persistence |
| DNA Sequencing Technologies | Whole-genome sequencing, long-read sequencing (e.g., PacBio, Nanopore) [7] | Identification of genetic mutations conferring bona fide resistance |
| Fluorescence-Activated Cell Sorting (FACS) | GFP reporters under ribosomal promoters [4] | Isolation of dormant cells based on reduced metabolic activity |
Interplay and Clinical Implications
While distinct phenomena, persistence and resistance interact in clinically significant ways. Persister cells can serve as a reservoir for resistance development by surviving antibiotic treatment and accumulating resistance mutations during transient growth phases [2]. This dynamic is particularly problematic in biofilm-associated infections, where persisters are enriched and protected within the biofilm structure [3] [2].
Therapeutic strategies must address both mechanisms simultaneously. Promising approaches include:
- Combination therapies that pair conventional antibiotics with compounds that disrupt persistence mechanisms [1].
- Anti-biofilm agents that enhance antibiotic penetration and target the protected niches where persisters reside [3] [2].
- Metabolic stimulation to "awaken" persisters before antibiotic administration, making them vulnerable to treatment [5].
Understanding the distinctions and interactions between phenotypic persistence and genetic resistance remains crucial for developing more effective treatments for persistent bacterial infections and addressing the ongoing antibiotic crisis.
Bacterial persisters are a subpopulation of genetically drug-susceptible, quiescent cells that survive exposure to lethal stresses, including antibiotics, and can regrow once the stress is removed [1] [8]. These cells are not antibiotic-resistant mutants but rather phenotypic variants that exhibit transient tolerance [8] [9]. Their presence is a significant clinical challenge, underlying chronic, relapsing infections such as tuberculosis, recurrent urinary tract infections, and biofilm-associated infections [1] [8]. The "Dormancy Spectrum" concept refers to the continuum of metabolic states that persisters can occupy, ranging from shallow to deep dormancy [1]. This guide objectively compares the classical types of persisters—Type I and Type II—and introduces the emerging concept of stress-induced, active tolerance mechanisms that some classifications refer to as Type III persisters.
Comparative Analysis of Persister Types
The following table summarizes the core characteristics of the primary persister types, providing a clear, at-a-glance comparison for researchers.
Table 1: Comparative Characteristics of Bacterial Persister Types
| Feature | Type I Persisters | Type II Persisters | Type III Persisters (Stress-Induced) |
|---|---|---|---|
| Primary Inducer | External environmental triggers (e.g., stationary phase, carbon starvation) [1] [10] | Spontaneous, stochastic switching during active growth [1] [10] | Specific environmental stresses (e.g., DNA damage, oxidative stress) [5] |
| Formation Kinetics | Programmed, synchronized response to a signal [10] | Continuous, stochastic formation throughout growth [10] | Induced rapidly in response to a specific stressor [5] |
| Metabolic State | Non-growing or metabolically stagnant [1] | Slow-growing or metabolically attenuated [1] | Can exhibit targeted inactivation of cellular processes without global dormancy [5] |
| Key Molecular Mechanisms | Stringent response, (p)ppGpp accumulation, RpoS [4] | Stochastic variation in toxin-antitoxin (TA) system expression (e.g., HipA) [10] [4] | SOS response (e.g., TisB), membrane depolarization, active efflux pumps [5] [11] |
| Typical Proportion in Population | Can be a significant fraction (e.g., in stationary phase) [4] | A very small fraction (e.g., 1 in 10^5–10^6 in E. coli) [10] | Variable, depends on the nature and intensity of the stress [5] |
| Regrowth Kinetics | Synchronized, upon removal of the inducing signal [10] | Stochastic awakening [10] | Awakening can be stochastic or triggered by environmental cues [5] |
Molecular Mechanisms and Signaling Pathways
The formation of persister cells is governed by a complex network of biochemical pathways. The diagram below illustrates the key signaling pathways and their logical relationships for Type I, II, and III persister formation.
Diagram 1: Signaling Pathways in Persister Formation. This diagram maps the primary molecular pathways leading to the formation of Type I (induced by external triggers), Type II (stochastic), and Type III (stress-induced) persister cells. Key processes include the stringent response, toxin-antitoxin system imbalance, and specific stress responses like the SOS pathway.
Detailed Pathway Analysis
Type I Pathways: The stringent response is a master regulator of Type I persistence. Nutrient limitation leads to the rapid accumulation of the alarmone (p)ppGpp, which orchestrates a dramatic reprogramming of cellular metabolism [4]. This includes shutting down ribosome synthesis and activating the general stress response sigma factor RpoS, collectively pushing the cell into a dormant, tolerant state [4].
Type II Pathways: The formation of Type II persisters is largely driven by the stochastic overexpression of toxin proteins from chromosomal Toxin-Antitoxin (TA) systems. In a small subset of cells, random fluctuations in gene expression can lead to a temporary imbalance where a toxin (e.g., HipA, MqsR, RelE) overwhelms its cognate labile antitoxin [10] [4]. These toxins then inhibit vital processes like translation (e.g., MqsR cleaves mRNA) or ATP production, inducing a dormant state [4].
Type III Pathways: Emerging research highlights that dormancy is not always required for tolerance. Some cells survive through active, targeted mechanisms induced by stress [5]. For example, DNA damage from fluoroquinolone antibiotics activates the SOS response, which upregulates the type I TA toxin TisB [11]. TisB integrates into the membrane, disrupting the proton motive force (PMF) and causing ATP depletion. This directly protects the cell by reducing antibiotic uptake (e.g., of aminoglycosides) and corrupting the drug's target [5] [11].
Experimental Protocols for Persister Research
Protocol 1: Isolation and Quantification of Persisters
The gold standard for measuring persistence is the biphasic killing curve assay [8].
- Culture Preparation: Grow a bacterial culture to the desired growth phase (e.g., mid-logarithmic or stationary phase). For Type I persisters, an inoculum from stationary phase is often used [4].
- Antibiotic Challenge: Expose the culture to a lethal concentration of a bactericidal antibiotic (e.g., 5-10x MIC of ampicillin or ciprofloxacin). Maintain the culture under growth conditions with aeration.
- Viable Count Enumeration:
- At time zero (immediately before antibiotic addition) and at regular intervals thereafter (e.g., 1h, 2h, 4h, 8h, 24h), remove aliquots from the culture.
- Wash the cells to remove the antibiotic by centrifugation and resuspension in fresh phosphate-buffered saline (PBS) or medium.
- Serially dilute the samples and spot or plate them onto antibiotic-free LB agar plates.
- Incubate the plates for 16-48 hours until colonies appear.
- Data Analysis: Plot the number of colony-forming units (CFU) per milliliter against time. The plot will show a rapid initial killing phase (death of normal cells) followed by a plateau or a much slower second killing phase (survival of persisters). The persister frequency is calculated as the CFU/mL at the plateau divided by the initial CFU/mL [8].
Protocol 2: Single-Cell Analysis of Type II Persisters
This protocol, based on Balaban et al. (2004), allows for the direct observation of stochastic persister formation and awakening [10].
- Microfluidic Setup: Use a microfluidic device designed to trap and continuously perfuse fresh medium over individual bacterial cells.
- Cell Loading and Monitoring: Load a dilute culture of bacteria into the device. Continuously flow fresh, rich medium through the device to encourage growth. Monitor cell division in real-time using time-lapse microscopy.
- Antibiotic Exposure and Identification: After a period of growth, switch the medium to one containing a high concentration of a bactericidal antibiotic (e.g., ampicillin). Continue perfusion and observation. Normal, growing cells will lyse. Cells that were non-growing or slow-growing at the time of antibiotic application will not lyse and are identified as persisters.
- Awakening Kinetics: After a defined period, switch back to antibiotic-free medium. Monitor the trapped, surviving persister cells to record the time at which they resume division ("awakening"). This demonstrates the stochastic and reversible nature of the Type II persister state [10].
The Scientist's Toolkit: Essential Research Reagents
The table below details key reagents and their applications in persister cell research, providing a practical resource for experimental design.
Table 2: Key Reagents for Persister Cell Research
| Reagent / Tool | Function in Research | Application Example |
|---|---|---|
| Ciprofloxacin / Ofloxacin | DNA-damaging antibiotics (fluoroquinolones) that induce the SOS response. | Used to study stress-induced (Type III) persistence and the role of the TisB toxin [11]. |
| Ampicillin | A bactericidal β-lactam antibiotic that inhibits cell wall synthesis. | Commonly used in biphasic killing assays to isolate and enumerate persisters, as it effectively kills growing cells [4]. |
| HipA7 Mutant Strain | A gain-of-function mutant in the HipA toxin of E. coli. | Serves as a high-persistence (Hip) model strain, producing ~1000x more Type II persisters than wild-type, useful for mechanistic studies [10]. |
| Fluorescence-Activated Cell Sorting (FACS) | A technique to isolate cell subpopulations based on fluorescence. | Used with a GFP reporter under a ribosomal promoter to isolate dormant, non-fluorescent persister cells from a larger population for transcriptomic analysis [4]. |
| Lon Protease Mutant | A mutant deficient in the ATP-dependent protease Lon. | Used to study Type II TA systems, as Lon degrades labile protein antitoxins; its deletion reduces persistence by preventing toxin activation [4]. |
Understanding the distinctions and overlaps between Type I, II, and III persisters is critical for developing effective therapies against chronic infections. While Type I and II represent different routes to a dormant, multidrug-tolerant state, Type III mechanisms suggest that active cellular responses can also confer tolerance without global shutdown. Future research must focus on identifying the specific inducers and molecular effectors of these pathways during human infection. The redundancy in persister formation mechanisms poses a significant challenge, implying that combination therapies targeting multiple pathways simultaneously will be essential to eradicate these resilient cells. The experimental tools and comparative data provided in this guide offer a foundation for such advanced therapeutic development.
Toxin-antitoxin (TA) modules are small genetic operons ubiquitous in bacterial genomes, functioning as master regulators of bacterial persistence across diverse species [12]. These universal molecular triggers consist of a stable toxin protein that can inhibit essential cellular processes and a corresponding labile antitoxin that neutralizes the toxin's activity [12] [13]. Under normal growth conditions, antitoxins effectively counteract their cognate toxins; however, during environmental stress such as antibiotic exposure, nutrient limitation, or immune system attack, antitoxins are rapidly degraded, allowing toxins to induce a transient dormant state [12] [14]. This dormancy creates persister cells—metabolically inactive variants that survive lethal antibiotic treatment despite genetic susceptibility, contributing significantly to chronic and recurrent infections [1] [15].
The abundance and diversity of TA modules vary considerably across bacterial pathogens, with notable enrichment in persistent pathogens like Mycobacterium tuberculosis, which carries 88 TA modules, compared to only 5 in the relatively fast-growing non-pathogen Mycobacterium smegmatis [12]. This correlation between TA module abundance and pathogenic persistence underscores their clinical importance as key regulators of bacterial survival strategies. This guide provides a systematic comparison of TA module functions, distributions, and experimental approaches across major bacterial species, offering researchers a comprehensive resource for investigating these universal molecular triggers of persistence.
TA Module Classification and Comparative Mechanisms
TA systems are currently classified into eight distinct types (I-VIII) based on the nature of the antitoxin and its mechanism of toxin neutralization [12] [16]. This classification reflects the remarkable diversity of molecular strategies bacteria employ to regulate persistence activation.
Table 1: Classification of Toxin-Antitoxin Systems and Their Mechanisms
| Type | Toxin Nature | Antitoxin Nature | Mechanism of Neutralization | Key Features |
|---|---|---|---|---|
| I | Protein | RNA (antisense) | Antitoxin RNA binds toxin mRNA, inhibiting translation [16] [13] | First discovered type; post-transcriptional regulation [14] |
| II | Protein | Protein | Antitoxin protein binds and inhibits toxin directly [12] [16] | Most extensively studied; transcriptional autoregulation [12] [17] |
| III | Protein | RNA | Antitoxin RNA binds toxin protein directly [16] | RNA-protein interaction; macromolecular complex formation [16] |
| IV | Protein | Protein | Antitoxin competes with toxin for target binding [16] | Substrate competition rather than direct toxin binding [16] |
| V | Protein | Protein | Antitoxin cleaves toxin mRNA [16] | Enzymatic RNA degradation as neutralization mechanism [16] |
| VI | Protein | Protein | Antitoxin mediates proteolytic degradation of toxin [16] | Promotes toxin destruction via proteolysis [16] |
| VII | Protein | Protein | Antitoxin enzymatically neutralizes toxin activity [16] | Recently described enzymatic neutralization mechanism [16] |
| VIII | RNA | RNA (antisense) | Antitoxin RNA binds toxin RNA directly [16] | RNA-RNA interaction; both components are RNAs [16] |
Type II TA systems represent the most extensively characterized and abundant class, particularly in pathogenic bacteria [16]. These systems feature protein antitoxins that typically contain two functional domains: a DNA-binding domain for transcriptional regulation and a toxin-binding domain that directly inhibits toxin activity through protein-protein interaction [12] [17]. The regulatory sophistication of type II systems is exemplified by "conditional cooperativity," where the toxin acts as a corepressor or derepressor depending on the cellular toxin:antitoxin ratio, creating a finely tuned responsive system [18].
Table 2: Distribution of Major Type II TA Families Across Bacterial Pathogens
| TA Family | Primary Toxin Target | Key Bacterial Species | Pathophysiological Role |
|---|---|---|---|
| VapBC | Translation (mRNA cleavage) [12] | M. tuberculosis (50 loci), P. aeruginosa [12] [16] | Major TA family; stress adaptation, persistence [12] |
| MazEF | Translation (mRNA cleavage) [12] | E. coli, M. tuberculosis (10 loci), S. aureus [12] [13] | Programmed cell death, stress response [12] |
| RelBE | Translation (ribosome-dependent mRNA cleavage) [12] | E. coli, V. cholerae [12] | Nutrient stress response, persistence [12] |
| HipBA | Translation (EF-Tu phosphorylation) [12] | E. coli (hipA7 mutants show 1000× higher persistence) [14] | High-persistence mutants, multidrug tolerance [14] |
| ParDE | DNA replication (gyrase inhibition) [12] | E. coli, various pathogens [12] | Plasmid maintenance, stress response [12] |
| CcdAB | DNA replication (gyrase inhibition) [12] | E. coli (F-plasmid) [12] | Plasmid stabilization, post-segregational killing [12] |
| HigBA | Translation [12] | P. aeruginosa, E. coli [16] | Biofilm formation, antibiotic tolerance [16] |
| Hha/TomB | Unknown | P. aeruginosa [16] | Recently identified in pan-genome analysis [16] |
The following diagram illustrates the fundamental operational principles shared across TA system types, highlighting how environmental stress triggers the activation of toxins and subsequent persistence formation:
Species-Specific TA Module Distribution and Functional Specialization
The distribution and abundance of TA modules vary dramatically across bacterial species, reflecting adaptation to specific environmental niches and pathogenic lifestyles. Pathogenic species typically harbor significantly more TA modules than their non-pathogenic relatives, suggesting an important role in virulence and host adaptation [12].
Mycobacterium tuberculosis
M. tuberculosis represents an extreme example of TA module enrichment, with 88 identified TA modules that contribute to its remarkable ability to establish persistent infections [12]. This abundance contrasts sharply with the relatively fast-growing Mycobacterium smegmatis, which possesses only 5 TA modules [12]. The M. tuberculosis TA arsenal includes 50 VapBC family systems and 10 MazEF family systems, providing multiple redundant pathways to enter dormancy during antibiotic treatment or immune system pressure [12]. This extensive TA network likely explains the pathogen's exceptional capacity for latent infection and treatment recalcitrance.
Pseudomonas aeruginosa
Pan-genome analysis of P. aeruginosa has revealed a diverse TA repertoire that includes both well-characterized and novel systems [16]. Beyond established type II systems like ParAB, RelBE, HigBA, and MazEF, genomic mining has identified previously unreported TA modules in this species, including hok-sok, cptA-cptB, cbeA-cbtA, tomB-hha, and ryeA-sdsR [16]. Importantly, approximately 16% of antibiotic resistance genes in P. aeruginosa are located near TA modules, suggesting potential co-regulation or coordinated dissemination through mobile genetic elements [16]. This genetic architecture facilitates the development of multidrug-resistant persistent infections, particularly in clinical settings.
Escherichia coli
E. coli possesses more than ten well-characterized type II TA systems, including relE-relB, yoeB-yefM, hipA-hipB, and mqsR-mqsA, which have served as models for understanding TA regulation and function [17]. The hipBA system is particularly notable, as hipA7 mutants produce persisters at a frequency of 1% compared to 0.0001% in wild-type strains when exposed to ampicillin [14]. This 10,000-fold increase in persistence frequency demonstrates the critical role specific TA loci play in mediating antibiotic tolerance. Research in E. coli has also revealed that the simultaneous deficiency of five or more type II TA modules significantly reduces persister formation during exponential growth phase, indicating functional redundancy across multiple systems [14].
Other Bacterial Pathogens
TA modules have been identified and characterized in numerous other pathogens with varying persistence capabilities. Xenorhabdus nematophila, an entomopathogen, possesses 39 TA modules that facilitate survival in insects through the formation of non-replicating persisters [12]. Clinical isolates of Staphylococcus aureus show varied TA system distributions, though evidence suggests their role in persistence may differ from Gram-negative organisms [14]. Additionally, well-characterized TA systems exist in non-human pathogens including Agrobacterium tumefasciens, Erwinia amylovora, Xanthomonas species, and Acetobacter pasteurianus, indicating the universal conservation of these mechanisms across the bacterial kingdom [12].
Experimental Approaches for TA System Investigation
Genomic Mining and Bioinformatics Analysis
Advanced genomic approaches enable comprehensive identification of TA modules across bacterial species. As demonstrated in P. aeruginosa research, reassembling genomes from sequencing data (e.g., from NCBI SRA database) allows detection of abundant TA homologs [16]. Subsequent pan-genome analysis across thousands of isolates reveals TA diversity and distribution patterns. Bioinformatic tools like TADB2 provide curated TA sequences and annotations, though current databases show a strong bias toward type II systems due to research focus [16]. Essential reagents for these approaches include:
Table 3: Research Reagent Solutions for TA System Studies
| Research Reagent | Function/Application | Example Use |
|---|---|---|
| TADB2 Database | Curated TA sequence database | Reference for identifying known TA modules and families [16] |
| BRET Assay Components | Bioluminescence Resonance Energy Transfer | High-throughput screening of TA protein interactions [19] |
| Lon Protease | ATP-dependent protease | Studying antitoxin degradation in type II systems [14] |
| RNA-Seq | Transcriptome profiling | Monitoring TA gene expression dynamics [17] |
| Microfluidic Culture | Single-cell analysis | Observing persister formation and resuscitation [1] |
| Fluorescent Protein Fusions | Protein localization and interaction | Visualizing toxin-antitoxin dynamics in live cells [19] |
Molecular Interaction Methodologies
Bioluminescence Resonance Energy Transfer (BRET) provides a powerful high-throughput screening method for investigating TA protein interactions and identifying compounds that disrupt these interactions [19]. In this approach, the epsilon antitoxin gene is fused to luciferase (Luc-epsilon) and the zeta toxin gene to GFP (zeta-GFP), enabling quantification of interaction dynamics through energy transfer measurements [19]. Molecular dynamics studies can further predict critical residues involved in toxin-antitoxin interactions, such as Asp18 and/or Glu22 in the epsilon-zeta system, which can be validated through site-directed mutagenesis [19].
The following diagram illustrates a generalized experimental workflow for investigating TA systems, from identification to functional characterization:
Mathematical Modeling of TA Dynamics
Mathematical modeling provides valuable insights into TA system dynamics and their relationship to persistence. Ordinary differential equation (ODE) models can describe the core regulatory logic of type II TA systems, incorporating key features such as toxin and antitoxin production rates, complex formation, and toxin-induced growth modulation [17]. These models typically account for the fundamental characteristics of TA systems: toxin and antitoxin are expressed by neighboring genes; toxins are more stable than antitoxins; the TA complex inhibits its own production; and toxin presence inhibits cell growth [17].
Stochastic models that include conditional cooperativity demonstrate how rare, extreme stochastic spikes in free toxin levels can create persister cells, with spike amplitude determining persister state duration [18]. These models reveal that free toxin levels are primarily controlled through toxin sequestration in TA complexes of various stoichiometry rather than by gene regulation alone [18]. Parameterizing these models with experimental data from specific TA pairs allows quantitative comparison of system dynamics across different bacterial species and environmental conditions [17].
TA Modules as Therapeutic Targets
The central role of TA modules in bacterial persistence makes them attractive targets for novel antibacterial strategies [12] [19]. Proposed approaches include artificial activation of toxin activity through compounds that disrupt toxin-antitoxin interactions, acceleration of antitoxin degradation, repression of antitoxin transcription or translation, and delivery of recombinant toxin RNA/DNA [16] [19]. Successful proof-of-concept studies have demonstrated the feasibility of these approaches. For example, in the Streptococcus pyogenes pSM19035-encoded epsilon-zeta TA system, a compound that disrupts the epsilon-zeta interaction could serve as an effective antimicrobial agent by freeing the zeta toxin to induce growth arrest [19].
Additional strategies include activating Lon protease to degrade antitoxins more rapidly or using antisense oligonucleotides to target antitoxin RNAs in type I systems [16]. The relatively narrow phylogenetic distribution of some TA systems offers potential for species-specific antimicrobial development, potentially minimizing disruption to beneficial microbiota [16]. As mathematical models improve predictions of TA system dynamics across bacterial species, targeted therapeutic interventions can be designed to activate these universal molecular triggers specifically in pathogenic contexts, potentially overcoming the limitations of conventional antibiotics against persistent infections.
Bacterial persistence represents a significant challenge in treating chronic infections, as persister cells can survive antibiotic treatment without genetic resistance [1] [4]. These dormant bacterial subpopulations exhibit remarkable tolerance to antimicrobial agents through metabolic dormancy and phenotypic heterogeneity [1] [20]. Central to this survival mechanism is the stringent response, masterfully orchestrated by the guanosine nucleotides (p)ppGpp (guanosine pentaphosphate and tetraphosphate) [21] [22]. This review comprehensively examines the role of (p)ppGpp as the primary regulator of bacterial dormancy, comparing its function across bacterial species and contextualizing its influence within the broader framework of persistence mechanisms.
The stringent response constitutes an evolutionarily conserved adaptation to nutrient limitation and environmental stresses [23]. When activated, it triggers a profound transcriptional reprogramming that shifts cellular priorities from growth and proliferation to survival and maintenance [24]. This response is characterized by the rapid accumulation of (p)ppGpp, which serves as a master regulatory alarmone that coordinates bacterial physiology to enhance survival under adverse conditions [21] [25]. Understanding the precise mechanisms through which (p)ppGpp influences entry into dormancy provides critical insights for developing novel therapeutic strategies against persistent infections.
Molecular Mechanisms of (p)ppGpp Signaling
(p)ppGpp Synthesis and Hydrolysis
The metabolism of (p)ppGpp is governed by enzymes belonging to the RelA/SpoT homolog (RSH) family [21] [23]. In Escherichia coli, a model Gram-negative organism, this system comprises two principal enzymes: RelA, which functions primarily as a (p)ppGpp synthetase, and SpoT, a bifunctional enzyme possessing both synthetic and hydrolytic capabilities [23] [25]. These enzymes meticulously maintain cellular (p)ppGpp concentrations, ensuring appropriate responses to environmental cues.
RelA is ribosome-associated and becomes activated upon binding of uncharged tRNA to the ribosomal A-site during amino acid starvation [25]. This activation triggers the synthesis of (p)ppGpp from GTP/GDP and ATP [21]. In contrast, SpoT responds to diverse stress signals, including fatty acid starvation, carbon source limitation, and oxidative stress [21] [25]. The functional diversity of RSH enzymes across bacterial species significantly influences how different pathogens regulate their stringent responses [21].
Table: (p)ppGpp Metabolic Enzymes Across Bacterial Species
| Organism | Enzyme Type | Synthetic Function | Hydrolytic Function | Primary Activators |
|---|---|---|---|---|
| Escherichia coli (Gram-negative) | RelA | Primary synthetase | Non-functional | Amino acid starvation (uncharged tRNA) |
| SpoT | Weak synthetase | Primary hydrolase | Fatty acid starvation, carbon limitation | |
| Gram-positive bacteria | Rel | Bifunctional (both activities) | Bifunctional (both activities) | Multiple nutrient limitations |
| Various pathogens | SAS (Small Alarmone Synthetase) | Monofunctional synthetase | None | Stress-specific signals |
(p)ppGpp-Mediated Transcriptional Regulation
(p)ppGpp exerts its profound effects on bacterial physiology through sophisticated mechanisms of transcriptional control. In Gamma-proteobacteria including E. coli and Pseudomonas aeruginosa, (p)ppGpp binds directly to the RNA polymerase (RNAP), often with the cofactor DksA, to modify promoter specificity and stability [24] [25]. This interaction preferentially represses stable RNA transcription (rRNA and tRNA) while activating stress response genes [21] [24].
The regulatory influence of (p)ppGpp extends beyond RNAP interaction. In many Gram-positive bacteria, (p)ppGpp indirectly controls transcription by modulating cellular GTP pools [25]. High (p)ppGpp levels inhibit enzymes involved in GTP biosynthesis, thereby reducing GTP concentrations that in turn affect transcription factors like CodY that sense nutrient sufficiency [25]. This mechanism enables a coordinated shutdown of anabolic processes during nutrient limitation.
Recent findings in P. aeruginosa demonstrate that (p)ppGpp implements a graded transcriptional response proportional to stress severity rather than a simple binary switch [24]. Under mild stress conditions (100 μM SHX), approximately 4% of the genome shows differential expression, while acute stress (1000 μM SHX) reprograms up to 25% of all genes [24]. This layered response enables precise physiological adjustments matched to environmental challenges.
Diagram: The (p)ppGpp Signaling Pathway and Its Role in Bacterial Persistence. This diagram illustrates how various environmental stressors activate RSH enzymes, leading to (p)ppGpp accumulation and subsequent physiological changes that promote dormancy and antibiotic tolerance.
Comparative Analysis of (p)ppGpp Function Across Bacterial Species
Gram-negative Bacteria
In Escherichia coli, (p)ppGpp accumulation triggers a comprehensive physiological transformation that promotes survival under adverse conditions. The alarmone directly inhibits DNA primase, effectively halting DNA replication initiation [21]. Simultaneously, it represses rRNA and tRNA synthesis through direct interaction with RNA polymerase, reducing the protein synthesis capacity of the cell [21]. These coordinated actions induce a state of metabolic quiescence that underlies antibiotic tolerance [21] [4].
Pseudomonas aeruginosa exhibits a graded response to (p)ppGpp accumulation that correlates with stress severity [24]. At low concentrations, (p)ppGpp primarily suppresses motility and pyocyanin production, promoting a transition to sessile lifestyle. Intermediate levels upregulate biofilm-related genes while downregulating virulence factors. High (p)ppGpp concentrations induce multidrug tolerance in biofilm populations through comprehensive transcriptional reprogramming affecting up to 25% of the genome [24]. This sophisticated layering of responses enables precise adaptation to environmental challenges.
In Salmonella enterica, (p)ppGpp is essential for intracellular survival within acidified vacuoles of macrophages [21]. (p)ppGpp-deficient mutants show severely impaired persistence in mouse infection models, highlighting the critical role of the stringent response in bacterial pathogenesis [21].
Gram-positive Bacteria
Gram-positive organisms typically possess a single bifunctional RSH enzyme (Rel) that combines both synthetic and hydrolytic activities [21] [22]. This architectural difference from the Gram-negative system may reflect alternative regulatory strategies for persistence formation. Additionally, Gram-positive bacteria frequently employ GTP pool modulation as a key regulatory mechanism, where (p)ppGpp inhibits GTP synthesis, thereby affecting cellular processes controlled by GTP-sensitive transcription factors [25].
Table: Comparative Analysis of (p)ppGpp-Mediated Persistence Mechanisms
| Mechanistic Feature | E. coli | P. aeruginosa | Gram-positive Bacteria |
|---|---|---|---|
| RSH Enzyme Architecture | Two enzymes: RelA (synthetase) and SpoT (bifunctional) | Similar to E. coli | Single bifunctional Rel enzyme |
| Primary Transcriptional Control | Direct RNAP binding with DksA | Direct RNAP binding with DksA | GTP pool modulation & CodY regulation |
| Metabolic Consequences | Inhibition of DNA primase; rRNA repression | Graded transcriptional response | Reduced GTP pools; ribosomal shutdown |
| Persistence Induction | Toxin-antitoxin activation; metabolic arrest | Biofilm-enhanced tolerance; motility suppression | Stress adaptation; sporulation in some species |
| Virulence Modulation | Host invasion capability | Quorum sensing integration; virulence factor regulation | Virulence gene expression control |
Interplay Between (p)ppGpp and Other Persistence Mechanisms
Toxin-Antitoxin (TA) Systems
(p)ppGpp plays an integral role in the activation and regulation of toxin-antitoxin (TA) modules, which constitute another fundamental mechanism of bacterial persistence [21] [22]. These systems typically consist of a stable toxin that disrupts essential cellular processes and a labile antitoxin that counteracts the toxin's effects [4] [22]. Under stress conditions, (p)ppGpp signaling promotes the activation of TA systems through both direct and indirect mechanisms.
The HipAB system represents a well-characterized example of (p)ppGpp-TA system integration [22]. The HipA toxin functions as a protein kinase that phosphorylates and inhibits glutamyl-tRNA synthetase (GltX), resulting in uncharged tRNA accumulation that activates RelA-mediated (p)ppGpp synthesis [22]. This creates a self-reinforcing cycle where TA system activation amplifies the stringent response, which in turn promotes further persistence induction.
Other TA systems, including MqsR/MqsA and TisB/IstR-1, are similarly interconnected with (p)ppGpp signaling [4]. The MqsR toxin functions as an mRNA interferase that cleaves cellular transcripts at GCU sites, effectively halting translation and inducing dormancy [4]. The TisB toxin dissipates the proton motive force and reduces ATP levels, creating a metabolically dormant state [4]. (p)ppGpp influences the expression and activity of these systems, creating a coordinated network of persistence mechanisms.
Biofilm Formation and Metabolic Adaptation
(p)ppGpp serves as a critical regulator of biofilm formation across multiple bacterial species [21] [24]. In both E. coli and P. aeruginosa, (p)ppGpp-deficient strains exhibit severely impaired biofilm development and enhanced antibiotic sensitivity [21]. The alarmone promotes biofilm formation through multiple pathways, including exopolysaccharide production, adhesion expression, and quorum sensing integration [24] [22].
Within biofilms, bacterial cells encounter gradients of nutrients and oxygen that create microenvironments with varying metabolic activity [20]. (p)ppGpp enables bacterial adaptation to these heterogeneous conditions by implementing a spatially coordinated stringent response [24]. Cells in nutrient-poor regions of biofilms exhibit elevated (p)ppGpp levels, resulting in reduced metabolic activity and enhanced antibiotic tolerance compared to their nutrient-replete counterparts [20].
The metabolic control exerted by (p)ppGpp extends to energy metabolism regulation. The alarmone modulates ATP production through effects on oxidative phosphorylation and carbon metabolism pathways [24] [20]. Reduced ATP levels contribute to persistence by promoting the formation of protein aggregates (aggresomes) that sequester essential enzymes for replication, transcription, and translation [22]. This aggregation mechanism establishes a self-reinforcing dormant state that can persist even after stress removal.
Experimental Approaches for Studying (p)ppGpp-Mediated Persistence
Key Methodologies and Protocols
Research on (p)ppGpp and bacterial persistence employs a diverse array of experimental approaches designed to quantify persistence levels, measure alarmone concentrations, and manipulate the stringent response. The following protocols represent standardized methodologies in the field.
Amino Acid Starvation Induction Using Serine Hydroxamate (SHX):
- Grow bacterial cultures to mid-exponential phase (OD600 ≈ 0.3-0.5) in appropriate medium [24]
- Add SHX at concentrations ranging from 100-1000 μM to induce mild to acute stringent response [24]
- Incubate for 30 minutes to allow (p)ppGpp accumulation
- Monitor growth inhibition and (p)ppGpp levels
- For transcriptomic studies, collect cells after 30 minutes of SHX treatment for RNA extraction and sequencing [24]
(p)ppGpp Quantification Method:
- Extract nucleotides from bacterial cultures using cold formic acid (0.5 M final concentration) [24]
- Separate nucleotides via polyethyleneimine-cellulose thin-layer chromatography
- Develop chromatography in 1.5 M KH2PO4 buffer (pH 3.6)
- Visualize and quantify (p)ppGpp spots using phosphorimaging or autoradiography
- Normalize (p)ppGpp levels to total guanine nucleotide pool (ppGpp + pppGpp + GTP) [24]
Persister Cell Isolation and Quantification:
- Grow cultures to desired growth phase (exponential or stationary)
- Treat with bactericidal antibiotics at 5-10× MIC for 3-5 hours
- Remove antibiotics by washing or dilution
- Plate on fresh medium to enumerate surviving colony-forming units (CFUs)
- Calculate persister frequency as (CFU after antibiotic treatment / total CFU before treatment) × 100 [1] [4]
The Scientist's Toolkit: Essential Research Reagents
Table: Key Research Reagents for Studying (p)ppGpp-Mediated Persistence
| Reagent/Category | Specific Examples | Function/Application |
|---|---|---|
| Stringent Response Inducers | Serine Hydroxamate (SHX) | Induces amino acid starvation via seryl-tRNA synthetase inhibition [24] |
| L-1,4-Diaminobutyrate | Lysine starvation analog for stringent response induction | |
| Analytical Tools | Polyethyleneimine-cellulose TLC plates | Separation and quantification of (p)ppGpp nucleotides [24] |
| HPLC-MS systems | High-sensitivity detection and quantification of alarmones | |
| Genetic Tools | relA/spoT knockout strains | Study (p)ppGpp-deficient phenotypes [21] [23] |
| (p)ppGpp0 strains (ΔrelA ΔspoT) | Complete (p)ppGpp-null mutants for functional studies [21] | |
| SAS/SAH expression vectors | Investigate small alarmone synthetase/hydrolase functions [21] | |
| Detection Assays | RNAP binding assays | Measure (p)ppGpp-RNAP interactions using EMSA or SPR |
| Transcriptomic microarrays/RNA-seq | Comprehensive analysis of stringent response regulons [24] |
Diagram: Experimental Workflow for (p)ppGpp Research. This diagram outlines the key methodological steps for investigating the role of (p)ppGpp in bacterial persistence, from strain preparation through final analysis.
Therapeutic Implications and Future Perspectives
The central role of (p)ppGpp in bacterial persistence makes it an attractive therapeutic target for combating chronic and recurrent infections [21] [22]. Innovative treatment strategies focusing on (p)ppGpp inhibition or modulation represent promising approaches to enhance the efficacy of conventional antibiotics.
One strategic approach involves developing small molecule inhibitors that target (p)ppGpp synthesis or function [21]. Compounds that inhibit RelA/SpoT synthetase activity could prevent the induction of the stringent response, thereby reducing persister formation and sensitizing bacteria to antibiotic treatment [21] [20]. Alternatively, molecules that activate (p)ppGpp hydrolase activity could accelerate alarmone turnover, limiting its physiological effects [23].
Metabolite-based adjuvant therapy represents another promising strategy [20]. Specific metabolites, including mannitol, pyruvate, and certain amino acids, can reactivate metabolic processes in persistent cells, restoring their susceptibility to antibiotics [20]. For instance, mannitol has been shown to enhance aminoglycoside sensitivity in P. aeruginosa biofilms by restoring proton motive force and drug uptake [20]. Similarly, exogenous adenosine and guanosine can increase tetracycline sensitivity against persister cells [20].
A more comprehensive understanding of the graded response mechanism of (p)ppGpp signaling [24] opens possibilities for fine-tuned interventions that modulate rather than completely abolish the stringent response. Such approaches might avoid potential resistance development associated with complete pathway inhibition while still effectively reducing persistence rates.
As research advances, targeting (p)ppGpp-mediated persistence holds significant promise for addressing the ongoing challenge of antibiotic treatment failure in chronic infections. The integration of (p)ppGpp inhibitors with conventional antibiotics may provide a synergistic strategy to eradicate bacterial populations completely, preventing relapses and reducing the emergence of genetic resistance.
Bacterial persisters are a transient, non-growing, and phenotypically variant subpopulation within a genetically susceptible strain that exhibits remarkable tolerance to high doses of conventional antibiotics. These cells are not resistant mutants but can resume growth once antibiotic pressure ceases, leading to recurrent infections and therapeutic failure [26] [1]. Critically, the biofilm lifestyle provides an ideal sanctuary for the formation and protection of these persister cells. Biofilms are structured microbial communities encased in a self-produced extracellular polymeric substance (EPS) matrix that adhere to biotic or abiotic surfaces [27]. This matrix creates a protected microenvironment where gradients of nutrients, oxygen, and metabolic waste products generate physiological heterogeneity, fostering the emergence and survival of persisters [26] [28]. The synergy between biofilms and persisters represents a major clinical challenge, underlying approximately 80% of chronic bacterial infections that are recalcitrant to standard antibiotic therapies [26] [29]. This review systematically compares the mechanisms by which biofilm structures and metabolic pathways collaboratively protect persister cells across major bacterial pathogens, providing a foundational analysis for antimicrobial development.
Comparative Architecture: Biofilm Structures Across Pathogens
The architectural complexity of biofilms varies significantly across bacterial species, influencing their capacity to harbor persisters. The protective EPS matrix composition differs notably between Gram-positive and Gram-negative pathogens, though all share common functional characteristics that contribute to persistence.
Table 1: Comparative Biofilm Matrix Components and Persister Protection Mechanisms in ESKAPE Pathogens
| Pathogen | Key Matrix Components | Structural Features | Primary Persister Protection Mechanisms |
|---|---|---|---|
| Pseudomonas aeruginosa | Pel, Psl alginate, eDNA, proteins | Mushroom-shaped microcolonies (glucose) or flat structures (citrate) | Matrix barrier delaying antibiotic penetration; steep oxygen gradient creating anaerobic niches [28] |
| Staphylococcus aureus | PIA/PNAG, protein/eDNA, fibrin, amyloid fibers | Polysaccharide, protein-based, fibrin-dependent, or amyloid structures | Multiple biofilm archetypes adapt to environmental conditions; fibrin shield from immune recognition [28] [29] |
| Klebsiella pneumoniae | Capsular polysaccharide, cellulose, poly-N-acetylglucosamine | Strong biofilm former with high matrix production | Enhanced biofilm formation correlates with carbapenem resistance; matrix impedes antibiotic diffusion [30] |
| Acinetobacter baumannii | Extracellular polysaccharides, proteins, eDNA | Robust biofilm architecture on abiotic surfaces | High-level resistance to cephalosporins and carbapenems linked to biofilm capability [30] |
| Enterococcus faecium | Polysaccharides, proteins | Hospital-adapted biofilm formation on medical devices | High multi-drug resistance rates (90%) within biofilm populations [30] |
The biofilm lifecycle proceeds through defined stages—initial attachment, irreversible attachment, microcolony formation, maturation, and dispersion—each contributing differently to persister dynamics [28]. Initial attachment involves reversible adhesion to preconditioned surfaces through weak interactions like van der Waals forces and electrostatic interactions [27]. During irreversible attachment, bacteria produce EPS that anchors them firmly to the surface and to each other. The maturation phase establishes the three-dimensional architecture with characteristic water channels that facilitate nutrient distribution and waste removal [27] [31]. Crucially, the biofilm interior develops chemical gradients of nutrients and oxygen that create heterogeneous microenvironments with varying metabolic activities [26]. This physiological heterogeneity is fundamental to persister development, as subpopulations in nutrient-deprived, oxygen-limited regions enter dormant or slow-growing states that are tolerant to antibiotics [26] [28].
Figure 1: The Biofilm Lifecycle and Persister Formation. Biofilms develop through a structured lifecycle that creates protective niches for persister cells, particularly in deep layers where nutrient and oxygen gradients induce dormancy.
Molecular Mechanisms of Persister Formation and Maintenance
Signaling Pathways and Genetic Regulation
Persister formation within biofilms is regulated by sophisticated molecular mechanisms that respond to environmental stresses and population dynamics. These mechanisms can be stochastic (arising spontaneously in a subset of cells) or triggered in response to environmental cues such as nutrient limitation, antibiotic exposure, or oxidative stress [26] [1].
Figure 2: Molecular Pathways Governing Persister Formation in Biofilms. Multiple interconnected signaling pathways respond to environmental stresses by inducing cellular changes that lead to the dormant, antibiotic-tolerant persister state.
The toxin-antitoxin (TA) modules represent a fundamental persistence mechanism, consisting of stable toxin proteins that inhibit essential cellular processes and unstable antitoxins that neutralize them [26]. Under stress conditions, antitoxins are degraded, freeing toxins to induce dormancy by targeting processes like DNA replication, protein translation, and cell wall synthesis [26]. The hipA toxin in Escherichia coli phosphorylates glutamyl-tRNA synthetase, inhibiting translation and leading to growth arrest, while the E. coli hokB toxin forms pores in the membrane, causing depolarization and ATP leakage that promotes persistence [32].
The stringent response, mediated by the alarmone (p)ppGpp, serves as a global regulator of bacterial persistence [32]. Under nutrient starvation, (p)ppGpp accumulates and reprograms cellular metabolism by downregulating ribosomal RNA and protein synthesis while upregulating stress response genes [32]. This response promotes dormancy and activates TA modules, creating a multi-layered defense mechanism. In P. aeruginosa, (p)ppGpp works with the GTPase Obg to activate transcription of the hokB toxin, linking nutrient sensing directly to persistence pathways [32].
Quorum sensing (QS) represents a population-density coordination system that significantly influences persister formation in biofilms [26] [33]. Bacteria release and detect signaling molecules called autoinducers that accumulate as cell density increases. At critical thresholds, these signals trigger collective behavioral changes, including enhanced biofilm formation and persistence mechanisms [29]. In P. aeruginosa, the LasI/LasR and RhlI/RhlR systems using N-acyl-homoserine lactones (AHLs) regulate pyocyanin production and biofilm maturation, while Staphylococcus aureus uses the Agr system with autoinducing peptides to control virulence and persistence [29]. QS inhibition has been shown to reduce persister formation, demonstrating its critical role in population-wide tolerance [34].
Metabolic Heterogeneity and Dormancy
The physiological heterogeneity within biofilms creates a spectrum of metabolic states, from actively growing to deeply dormant cells, which is fundamental to antibiotic tolerance [26] [28]. This metabolic stratification occurs along nutrient and oxygen gradients, with cells in the biofilm interior experiencing limited nutrient availability and hypoxia [26]. These conditions trigger metabolic reprogramming that reduces cellular activity, decreasing the efficacy of antibiotics that target active processes like cell wall synthesis, DNA replication, and protein translation [26] [1].
Energy metabolism plays a crucial role in persister formation, with fluctuations in Krebs cycle enzymes and ATP levels driving phenotypic variation [32]. Reduced intracellular ATP correlates with increased persistence, as many antibiotics require active cellular processes and energy-dependent uptake for efficacy [26]. Additionally, the accumulation of protein aggregates due to ATP depletion has been linked to deeper dormancy states, with the molecular chaperones DnaK and ClpB required for disaggregation and resuscitation [32].
Table 2: Experimental Evidence for Biofilm-Enhanced Persister Formation Across Bacterial Species
| Bacterial Species | Experimental Findings | Biofilm vs. Planktonic Persister Ratio | Key Identified Mechanisms |
|---|---|---|---|
| Pseudomonas aeruginosa | Biofilms contain up to 1% persisters after antibiotic treatment | 10-1000× higher in biofilm | TA modules, (p)ppGpp signaling, reduced metabolic activity, efflux pumps [26] |
| Staphylococcus aureus | MRSA biofilms show high tolerance to vancomycin and rifampicin | ~100× higher in biofilm | Multiple biofilm archetypes, fibrin shield, protein/eDNA matrix [28] |
| Escherichia coli | Stationary-phase biofilms exhibit increased multidrug tolerance | 10-100× higher in biofilm | hipBA TA module, SOS response, oxidative stress protection [1] |
| Mycobacterium tuberculosis | Pyrazinamide specifically targets dormant persisters in granulomas | N/A (caseous lesions) | Acidic environment activates pyrazinoic acid production disrupting membrane energetics [1] [34] |
| Klebsiella pneumoniae | Strong biofilm formers show correlation with carbapenem resistance | Significant correlation (p<0.05) | EPS matrix barrier, enzymatic degradation of antibiotics [30] |
Experimental Models and Methodologies for Studying Biofilm Persisters
Standardized Protocols for Persister Isolation and Quantification
Research on biofilm persisters requires specialized methodologies that account for the structural and physiological complexity of these communities. The microtiter plate biofilm formation assay represents a fundamental approach for quantifying biofilm formation capability and isolating persisters [30]. In this protocol, bacteria are grown in 96-well plates under static conditions for 24-48 hours to allow biofilm development on the well walls. Following incubation, non-adherent cells are removed by gentle washing, and biofilms are treated with high concentrations of bactericidal antibiotics (e.g., 10-100× MIC) for 3-24 hours [30]. The surviving persister population is then quantified by disrupting the biofilm through sonication or scraping, followed by serial dilution and plating on nutrient agar for colony-forming unit enumeration [26] [30].
The chemostat model with continuous flow provides a more dynamic system for studying biofilm development and persister formation under controlled nutrient conditions [28]. This approach allows researchers to simulate the natural gradients that occur in biofilms while maintaining constant growth parameters. For more sophisticated spatial analysis, the Calgary Biofilm Device (MBEC assay) enables high-throughput testing of multiple antimicrobial conditions against biofilms grown on pegs [28]. Confocal laser scanning microscopy (CLSM) with fluorescent viability stains (e.g., SYTO9/propidium iodide) provides direct visualization of the three-dimensional distribution of live, dead, and persister cells within the biofilm architecture, revealing localized niches where persisters accumulate [31].
The Scientist's Toolkit: Essential Research Reagents
Table 3: Essential Research Reagents for Biofilm Persister Studies
| Reagent/Category | Specific Examples | Experimental Function | Application Notes |
|---|---|---|---|
| Biofilm Growth Systems | 96-well microtiter plates, Calgary Biofilm Device (MBEC), flow cells | Standardized platforms for reproducible biofilm cultivation under static or dynamic conditions | Flow cells best mimic natural environments; microtiter plates allow high-throughput screening [30] [28] |
| Viability Stains | SYTO9/propidium iodide (LIVE/DEAD), CTC (5-cyano-2,3-ditolyl tetrazolium chloride) | Differentiation of live, dead, and metabolically active cells in biofilms | LIVE/DEAD staining combined with CLSM enables 3D spatial mapping of persister niches [31] |
| Matrix Disruption Agents | DNase I, dispersin B, proteinase K, glycoside hydrolases | Enzymatic breakdown of specific EPS components to study matrix protection mechanisms | Used to investigate matrix contribution to antibiotic tolerance and persister survival [28] |
| Stress Inducers | Carbon starvation media, hydrogen peroxide, acidified media, sub-MIC antibiotics | Controlled induction of persistence pathways to study regulatory mechanisms | Enable synchronized persister formation for mechanistic studies [1] [34] |
| Specialized Antimicrobials | Pyrazinamide, ADEP4, colistin, membrane-targeting compounds | Agents with demonstrated activity against persister cells and dormant populations | Used as positive controls and to study persister killing mechanisms [34] |
Emerging Control Strategies and Therapeutic Approaches
The unique biology of biofilm-protected persisters necessitates innovative treatment approaches beyond conventional antibiotics. These strategies can be broadly categorized into those targeting persister cells directly and those preventing persister formation or reactivating dormant cells to sensitize them to traditional antibiotics.
Direct killing approaches focus on growth-independent cellular targets, particularly the cell membrane. Membrane-targeting agents like 2D-24, XF-70, XF-73, and SA-558 disrupt membrane integrity, causing depolarization, ATP leakage, and ultimately cell lysis independent of metabolic state [34]. Similarly, the anti-tuberculosis drug pyrazinamide (PZA) specifically targets dormant M. tuberculosis persisters by disrupting membrane energetics when activated to pyrazinoic acid in acidic environments [1] [34]. ADEP4 activates the ClpP protease, causing uncontrolled protein degradation in dormant cells, while silver nanoparticle-shelled nanodroplets (C-AgND) interact with negatively charged EPS components to reach and kill persisters within biofilms [34].
Indirect strategies aim to prevent persister formation or reactivate dormant cells. Quorum sensing inhibitors like benzamide-benzimidazole compounds and brominated furanones disrupt cell-to-cell communication, reducing persister formation without affecting growth [34]. Inhibitors of hydrogen sulfide (H₂S) biogenesis and nitric oxide (NO) donors act as metabolic disruptors that prevent entry into dormancy [34]. Membrane-potentiating compounds such as MB6, CD437, and polymyxin B nonapeptide increase membrane permeability, enhancing uptake of conventional antibiotics like gentamicin to achieve synergistic killing of persisters [34].
Novel delivery systems including red blood cell membrane-coated nanoparticles (Hb-Naf@RBCM NPs) and engineered phages show promise for targeted delivery of antimicrobials to biofilm environments, overcoming penetration barriers [34]. Combination therapies that integrate multiple approaches—such as matrix-degrading enzymes to enhance antibiotic penetration with membrane-active compounds to increase susceptibility—represent the most promising direction for eradicating biofilm-associated persister cells [32] [34].
The sanctuary provided by biofilms for persister cells represents a critical frontier in combating chronic and recurrent bacterial infections. The structural protection of the EPS matrix combined with metabolic heterogeneity creates specialized niches where dormant, antibiotic-tolerant subpopulations can evade treatment and reseed infections. While significant progress has been made in understanding the molecular mechanisms underlying persistence, including TA modules, (p)ppGpp signaling, and quorum sensing, the redundancy of these pathways presents both challenges and opportunities for therapeutic intervention.
Future research should prioritize the development of standardized models that better recapitulate the complexity of in vivo biofilms, including multispecies communities and host-pathogen interactions. The integration of advanced techniques such as single-cell RNA sequencing with spatial mapping within biofilms will provide unprecedented resolution of persister heterogeneity and metabolic states. From a therapeutic perspective, combination approaches that simultaneously target structural biofilm components, persistence pathways, and reactivate dormant cells hold the greatest promise for overcoming the recalcitrance of biofilm-associated infections. As our understanding of the intricate relationship between biofilm structures and persistence mechanisms deepens, so too will our ability to develop effective strategies against these resilient bacterial sanctuaries.
Advanced Tools and Models: Deciphering Persistence from Single Cells to Host Environments
The study of bacterial persister cells—dormant, phenotypic variants that survive antibiotic treatment—is fundamentally a challenge of analyzing cellular heterogeneity. Traditional bulk-cell analysis methods mask the rare, transient events that lead to persistence, making single-cell technologies indispensable for this field. The convergence of microfluidic technologies for high-throughput, controlled single-cell manipulation and live-cell imaging for dynamic, real-time phenotypic observation is revolutionizing our understanding of persister formation mechanisms across bacterial species. This guide objectively compares the performance, capabilities, and experimental requirements of these pivotal technologies, providing researchers with the data needed to select the optimal approach for their investigations into bacterial persistence.
Technology Performance Comparison
Microfluidic Platforms for Single-Cell Analysis
Microfluidic systems create a customized microenvironment for precise cell manipulation with spatio-temporal control, making them powerful tools for isolating and studying rare bacterial persisters. [35] [36] These platforms leverage channels with dimensions of tens to hundreds of micrometers, comparable to cellular scales, enabling high-throughput spatial segregation of single cells. [37] [38]
Table 1: Comparison of Single-Cell Isolation Technologies for Persister Studies
| Technology | Throughput | Efficiency | Cell Viability | Key Advantage for Persistence Research | Primary Limitation |
|---|---|---|---|---|---|
| Limiting Dilution | Medium | Low (~37% max) | High [37] | Simplicity, low cost [37] | Statistical randomness, low throughput [37] |
| Laser Capture Microdissection (LCM) | Low | High | Low (often requires fixation) [37] | In-situ isolation from complex samples [37] | Low throughput, compromises cell integrity [37] |
| Micromanipulation | Low | High | High [37] | Targeted isolation of specific cells [37] | Manual process limits throughput [37] |
| Fluorescence-Activated Cell Sorting (FACS) | High (up to 70,000 cells/sec) [37] | Medium | Low (shear force, laser damage) [37] | Rapid screening of fluorescently labeled cells [35] | Bulky, expensive, cannot process low cell counts [37] [35] |
| Microfluidic Platforms | High (thousands of cells) | Variable by design | High (gentle isolation) [37] | Precise microenvironment control, high-throughput temporal monitoring [35] [36] | Complex fabrication, requires specialized equipment [35] |
Table 2: Performance Metrics of Microfluidic Modalities for Single-Cell Analysis
| Microfluidic Type | Throughput | Temporal Resolution | Integration with Live Imaging | Best Application in Persistence Research |
|---|---|---|---|---|
| Microchamber/Chip-based | Medium-High | Minutes to hours | Excellent [37] | Long-term tracking of persister formation and resuscitation |
| Droplet-based | Very High (thousands) | Seconds to minutes | Moderate [38] | High-throughput screening of rare persister cells in populations |
| Active Microfluidics | Medium | High (real-time) | Excellent [35] | Dynamic response to antibiotic pulses at single-cell level |
Live-Cell Imaging Modalities for Dynamic Single-Cell Analysis
Live-cell imaging provides the essential temporal dimension to persister studies, enabling direct observation of phenotypic transitions that precede persistence formation.
Table 3: Performance Comparison of Live-Cell Imaging Modalities
| Imaging Modality | Penetration Depth | Sensitivity | Temporal Resolution | Advantages for Persistence Studies | Limitations |
|---|---|---|---|---|---|
| Fluorescence Imaging | Poor [39] | 10⁻⁹-10⁻¹² mol/L [39] | Seconds-minutes [39] | No substrate required; wide range of fluorescent proteins [39] | Phototoxicity, photobleaching, autofluorescence [39] |
| Bioluminescence Imaging | Fair [39] | 10⁻¹⁵-10⁻¹⁷ mol/L [39] | Minutes [39] | High sensitivity, low background, no phototoxicity [39] | Requires substrate, lower spatial resolution [39] |
| Phase-Contrast/ Brightfield | Good (in vitro) | N/A | Seconds | Label-free, minimal cellular perturbation | Limited molecular specificity |
Experimental Protocols for Single-Cell Persistence Studies
Integrated Microfluidics with Live-Cell Imaging for Persister Formation Analysis
Objective: To track the formation and resuscitation of bacterial persister cells at single-cell resolution under controlled antibiotic exposure.
Protocol Workflow:
Detailed Methodology:
Bacterial Strain Preparation:
- Engineer reporter strains with fluorescent protein expression under constitutive promoters (e.g., GFP, mCherry) or stress-responsive promoters (e.g., SOS response). For bioluminescence imaging, introduce luciferase genes (Fluc, Rluc, Gluc). [39]
- Culture bacteria to specific growth phases (exponential vs. stationary), as persistence frequency varies significantly. [1] [14]
Microfluidic Device Operation:
- For microchamber chips: Use hydrodynamic cell trapping or single-cell printing to gently isolate individual bacteria into microchambers. [37] Continuous media flow maintains nutrient supply and enables precise antibiotic introduction.
- For droplet microfluidics: Encapsulate single cells in picoliter-sized water-in-oil droplets. This creates isolated bioreactors enabling high-throughput parallel analysis while eliminating cross-contamination. [38]
- For active microfluidics: Utilize optical tweezers, dielectrophoresis, or acoustic waves to position and manipulate individual cells for long-term observation. [35]
Antibiotic Treatment and Imaging:
- Introduce bactericidal antibiotics (e.g., fluoroquinolones, aminoglycosides) at clinically relevant concentrations via precisely controlled flow rates.
- Perform time-lapse imaging using automated microscopy systems. For fluorescence, capture images at intervals (e.g., every 10-30 minutes) to minimize photodamage. For bioluminescence, longer exposures may be necessary due to lower signal intensity. [39]
- Continue imaging for 24-72 hours to capture both killing and resuscitation phases.
Data Extraction and Analysis:
- Use single-cell tracking software to quantify key parameters: time to persistence formation, resuscitation kinetics, and morphological changes.
- Calculate persistence frequency as the percentage of cells surviving antibiotic treatment after 24-48 hours that subsequently resume growth.
- Correlate persistence events with pre-existing cellular features (e.g., growth rate, expression level of stress response reporters).
High-Throughput scRNA-seq of Bacterial Persisters
Objective: To identify transcriptional heterogeneity underlying persister formation using single-cell RNA sequencing.
Protocol Workflow:
Detailed Methodology:
Persister Enrichment:
- Treat bacterial cultures with high concentrations of bactericidal antibiotics (e.g., 10-100× MIC of ampicillin or ofloxacin) for 3-5 hours. [14]
- Wash cells to remove antibiotics and collect surviving persister cells. Include appropriate controls (untreated cells).
Single-Cell Isolation and Library Preparation:
- Use commercial droplet microfluidics platforms (10× Chromium or BD Rhapsody) to partition individual cells into nanoliter droplets with barcoded beads. [38] [40]
- Perform cell lysis within droplets, capturing mRNA on barcoded beads.
- Reverse transcribe RNA to create cDNA libraries with cell-specific barcodes.
Sequencing and Data Analysis:
- Sequence libraries using high-throughput sequencing platforms (Illumina).
- Process data through established pipelines (Cell Ranger, Seurat) for quality control, normalization, and clustering.
- Apply clustering algorithms (e.g., SC3, PhenoGraph) to identify distinct transcriptional states. [41]
- Perform differential expression analysis to identify genes upregulated in persister subpopulations (e.g., toxin-antitoxin modules, stress response genes, metabolic regulators). [14]
Key Signaling Pathways in Bacterial Persistence
Bacterial persistence is regulated by interconnected molecular pathways that control metabolic dormancy and stress adaptation. Single-cell analysis has been instrumental in revealing heterogeneity in the activation of these pathways within isogenic populations.
Pathway Dynamics at Single-Cell Level:
Toxin-Antitoxin (TA) Systems: Single-cell studies reveal bistable expression of TA modules (e.g., HipBA, MazEF), where stochastic toxin activation in a subset of cells induces dormancy. [14] Type II TA systems are most abundant, with toxins targeting essential cellular processes like translation and DNA replication. [14]
Stringent Response: Nutrient limitation triggers ppGpp accumulation, which reprograms cellular metabolism toward dormancy. Microfluidic studies show heterogeneous ppGpp levels within populations, correlating with persistence probability. [14]
SOS Response: Antibiotic-induced DNA damage activates the RecA-LexA pathway. Live-cell imaging of SOS reporters demonstrates variable induction timing and intensity among individual cells, influencing survival outcomes. [39] [14]
Biofilm Association: Bacterial persisters are highly enriched in biofilms, where extracellular polymeric substances (EPS) provide physical protection and create nutrient gradients that induce dormancy. [1] [2] Microfluidic biofilm models enable real-time observation of spatial organization and heterogeneity in metabolic activity.
The Scientist's Toolkit: Essential Research Reagents and Materials
Table 4: Key Research Reagent Solutions for Single-Cell Persistence Studies
| Reagent/Material | Function | Application Examples |
|---|---|---|
| Polydimethylsiloxane (PDMS) | Elastomeric polymer for microfluidic device fabrication; transparent, gas-permeable, biocompatible [37] [36] | Long-term bacterial culture on-chip; observation of persister resuscitation [37] |
| Fluorescent Reporter Plasmids | Visualize gene expression and protein localization in live cells (e.g., GFP, mCherry, tdTomato) [39] | SOS response reporters (recA::gfp); promoter activity of persistence genes (hipA::mCherry) [39] |
| Bioluminescence Reporter Systems | Monitor gene expression with high sensitivity and low background (e.g., Fluc, Rluc, Gluc) [39] | Stress response studies in deep tissue models; low-abundance gene expression in persisters [39] |
| Barcoded Beads (10× Chromium, BD Rhapsody) | Capture mRNA from single cells for sequencing; unique molecular identifiers | High-throughput scRNA-seq of persister subpopulations; transcriptional heterogeneity analysis [38] [40] |
| Antibiotic Tolerance Assay Kits | Standardized reagents for persister quantification and characterization | Comparison of persistence levels across bacterial strains; screening of anti-persister compounds |
The integration of microfluidics and live-cell imaging has transformed our ability to study bacterial persistence at single-cell resolution, revealing unprecedented heterogeneity in phenotypic responses to antibiotic stress. Microfluidic platforms excel in high-throughput, controlled single-cell manipulation, while live-cell imaging provides essential dynamic information about persister formation and resuscitation. The choice between these technologies depends on specific research goals: microfluidic approaches are ideal for high-throughput screening and transcriptional analysis of persister subpopulations, while live-cell imaging is optimal for kinetic studies of persistence development and molecular pathway dynamics. As these technologies continue to converge and advance, they will undoubtedly accelerate the discovery of novel therapeutic strategies to combat persistent bacterial infections.
Transposon insertion sequencing (Tn-seq) represents a powerful genome-wide technology that has revolutionized the identification of genetic determinants underlying bacterial persistence. This high-throughput functional genomics approach enables researchers to systematically assess the fitness contribution of nearly every gene in a bacterial genome under specific conditions, such as those that induce antibiotic persistence. Tn-seq combines saturated transposon mutagenesis with high-throughput sequencing to quantitatively measure how the loss of each gene affects bacterial survival and growth, making it particularly valuable for studying rare subpopulations like persister cells that survive antibiotic treatment [42] [43].
The application of Tn-seq to persistence research has uncovered complex genetic networks that bacteria employ to enter and maintain a transient, non-growing state that confers tolerance to bactericidal antibiotics. Unlike conventional resistance mechanisms that involve genetic mutations, persistence represents a phenotypic switch that enables a small fraction of bacterial populations to survive antibiotic exposure, often leading to chronic and recalcitrant infections. Understanding the genetic architecture of persistence through Tn-seq provides critical insights for developing novel therapeutic strategies that target both growing populations and these persistent subpopulations [43] [44].
Fundamental Principles of Tn-seq Methodology
Core Technological Framework
Tn-seq methodology relies on the creation of a comprehensive transposon mutant library where individual mutants carry random insertions throughout the bacterial genome. The core principle involves tracking the abundance of each mutant before and after exposure to selective conditions—such as antibiotic treatment—through high-throughput sequencing of transposon-genome junctions. Genes that become conditionally essential under the selective pressure will show significant depletion of corresponding mutants in the final population, identifying them as genetic determinants of persistence [42] [45].
The methodology encompasses several technically similar approaches, including Tn-seq proper, Transposon-Directed Insertion Site Sequencing (TraDIS), High-Throughput Insertion Tracking by Deep Sequencing (HITS), and INSeq, which primarily differ in their library preparation and amplification strategies for identifying transposon insertion sites [43]. These methods all enable the simultaneous assessment of thousands of mutants in a single experiment, providing unprecedented scale and resolution for functional genetic studies in microorganisms [43] [45].
Experimental Workflow and Design
The standard Tn-seq workflow begins with the construction of a saturated mariner transposon insertion library, typically containing between 50,000-200,000 unique mutants to ensure comprehensive coverage of the genome. The Mariner transposon system is particularly valued for its minimal insertion bias and broad host range [42] [43]. Following library construction, the mutant pool is subjected to the condition of interest—such as antibiotic exposure for persistence studies—with an aliquot preserved as a reference control (often denoted as Time0, t0, or input population). Genomic DNA is extracted from both pre-selection and post-selection populations, and transposon insertion sites are amplified and sequenced en masse [42] [45].
Bioinformatic analysis pipelines, including specialized software tools like TRANSIT, Con-ARTIST, and TRADIS, then map the sequencing reads to the reference genome and quantify the abundance of insertions at each position [43] [46]. Statistical models account for various sources of noise and bias, with recent approaches employing Zero-Inflated Negative Binomial (ZINB) regression to handle the excess of zero-count sites (representing absent insertions) that characterize TnSeq data [46]. The resulting fitness values for each gene reveal which genetic disruptions impair survival under the test conditions, pinpointing molecular pathways essential for persistence.
Table: Key Steps in Standard Tn-seq Experimental Workflow
| Step | Description | Key Considerations |
|---|---|---|
| Library Construction | Create saturated transposon mutant library using Mariner transposon | Aim for 50,000-200,000 mutants; ensure wide genomic coverage |
| Selection | Expose library to selective condition (e.g., antibiotics) with control aliquot | Maintain population diversity; avoid bottlenecks |
| DNA Preparation | Extract genomic DNA and prepare sequencing libraries | Amplify transposon-genome junctions specifically |
| Sequencing | High-throughput sequencing of insertion sites | Sufficient depth to detect rare mutants |
| Data Analysis | Map reads, quantify insertion abundances, calculate fitness defects | Use specialized software (TRANSIT, TRADIS); apply statistical models (ZINB) |
Figure 1: Tn-seq Experimental Workflow. This diagram illustrates the key steps in a standard Tn-seq experiment, from library construction through bioinformatic analysis.
Comparative Analysis of Persistence Mechanisms Across Bacterial Species
Tn-seq studies have revealed both conserved and species-specific genetic pathways underlying antibiotic persistence across diverse bacterial pathogens. The following comparative analysis synthesizes findings from recent investigations that employed Tn-seq to dissect persistence mechanisms in various microorganisms.
Persistence Mechanisms in Mycobacterial Species
Mycobacterial pathogens present a compelling case for Tn-seq applications due to their remarkable ability to establish persistent infections that require prolonged, multi-drug antibiotic regimens. In Mycobacterium abscessus (Mabs), one of the most antibiotic-resistant bacterial pathogens, Tn-seq screens identified an unexpected role for reactive oxygen species (ROS) detoxification systems in maintaining both spontaneous and starvation-induced persister cells [44]. The catalase-peroxidase enzyme KatG was found to be essential for persister survival, with endogenous ROS generation following antibiotic exposure contributing to bacterial killing. Under hypoxic conditions, however, KatG became dispensable, suggesting oxygen-dependent mechanisms of antibiotic lethality that persister cells must counteract [44].
Similarly, a multi-strain Tn-seq analysis of Mycobacterium intracellulare clinical isolates identified 131 shared essential or growth-defect genes under hypoxic conditions that represent core persistence mechanisms in this pathogen. These included genes involved in gluconeogenesis and the type VII secretion system, which showed increased requirement in clinical strains compared to type strains [47]. The study demonstrated that clinical MAC-PD strains exhibited more rapid adaptation to hypoxic growth, with genetic requirements confirmed in a mouse lung infection model, highlighting the importance of using clinically relevant strains and conditions to identify persistence mechanisms [47].
Enterococcal Persistence Mechanisms
In vancomycin-resistant Enterococcus faecium, a leading cause of hospital-acquired bloodstream infections, Tn-seq revealed that metabolic adaptations are critical for growth in human serum—an environment that bacteria encounter during systemic infections. Genes involved in de novo nucleotide biosynthesis (pyrK2, pyrF, purD, purH) and carbohydrate uptake (manY2, encoding a phosphotransferase system subunit) were identified as essential for persistence in serum [48]. Mutants in these genes not only showed impaired growth in human serum but also exhibited significantly attenuated virulence in a zebrafish infection model, confirming the importance of these metabolic pathways to in vivo persistence and pathogenesis [48].
Cross-Species Commonalities and Variations
When comparing persistence mechanisms across bacterial species, certain patterns emerge. Metabolic adaptation appears to be a universal requirement for persistence, though the specific pathways involved vary between organisms. For instance, while nucleotide biosynthesis is critical for E. faecium persistence in serum [48], ROS detoxification assumes greater importance in M. abscessus [44]. Similarly, stress response systems consistently contribute to persistence across species, but the specific components differ—from the hypoxia adaptation systems in mycobacteria to the purine biosynthesis pathways in Enterococcus [44] [47] [48].
Table: Comparative Genetic Determinants of Persistence Across Bacterial Species
| Bacterial Species | Key Genetic Determinants | Experimental Conditions | Biological Process |
|---|---|---|---|
| Mycobacterium abscessus | katG (catalase-peroxidase), ROS detoxification genes | Spontaneous & starvation-induced persistence to TIG/LZD, RIF/INH/EMB | Reactive oxygen species detoxification |
| Mycobacterium intracellulare | pckA (phosphoenolpyruvate carboxykinase), eccC5 (T7SS), mycP5 (serine protease) | Hypoxic growth & mouse lung infection | Gluconeogenesis, type VII secretion |
| Enterococcus faecium | pyrK2, pyrF, purD, purH (nucleotide biosynthesis), manY2 (carbohydrate transport) | Growth in human serum & zebrafish infection model | Purine biosynthesis, carbohydrate metabolism |
Figure 2: Conserved Pathways in Bacterial Persistence. This diagram illustrates key molecular pathways identified through Tn-seq studies that contribute to persister formation across bacterial species.
Advanced Tn-seq Applications and Methodological Innovations
Statistical Advances in Tn-seq Analysis
The analysis of Tn-seq data presents unique statistical challenges due to the nature of insertion count data, which typically contains an excess of zero counts (sites with no insertions) and over-dispersed count distributions. Traditional approaches like ANOVA are inadequate for such data, as they assume normally distributed residuals, leading to increased risk of Type I and Type II errors [46]. To address these limitations, Zero-Inflated Negative Binomial (ZINB) regression has been introduced as a specialized statistical framework for Tn-seq data analysis [46].
The ZINB model incorporates two components: a Negative Binomial distribution that models the magnitude of insertion counts at sites with insertions, and a zero-inflation component that accounts for the excess of sites without insertions. This dual approach enables separate modeling of condition-dependent effects on both insertion density (through the zero-inflation parameter) and the magnitudes of insertion counts (through the Negative Binomial parameters) [46]. In practical applications to Mycobacterium tuberculosis Tn-seq data, ZINB regression has demonstrated superior sensitivity compared to pairwise resampling methods, identifying a superset of varying genes and enabling analysis across multiple (≥3) conditions simultaneously [46].
Specialized Tn-seq Methodological Variants
The basic Tn-seq framework has spawned numerous innovative variants that extend its application to diverse biological questions. Droplet TnSeq (dTnSeq) enables the analysis of mutant libraries at single-cell resolution, while randomly barcoded TnSeq incorporates unique molecular identifiers to track individual mutants more accurately through complex experiments [43]. SorTnSeq and loxTnSeq introduce additional manipulation steps that allow for dynamic monitoring of mutant abundances under changing conditions [43].
For persistence research specifically, TRADISort and density-TRADISort have been developed to select mutants based on physical properties such as motility, capsule formation, or efflux activity, enabling direct linkage of these phenotypes to genetic requirements [43]. These methodological innovations significantly expand the range of biological questions that can be addressed with Tn-seq approaches, particularly for understanding the multifactorial phenomenon of bacterial persistence.
The Scientist's Toolkit: Essential Research Reagents and Materials
Successful Tn-seq experiments require specialized reagents and materials optimized for creating and analyzing comprehensive transposon mutant libraries. The following toolkit outlines essential components for implementing Tn-seq in persistence research.
Table: Essential Research Reagents for Tn-seq Experiments
| Reagent Category | Specific Examples | Function & Importance |
|---|---|---|
| Transposon Systems | Mariner-based transposons (Himar1), Tn5 | Efficient random insertion; Mariner preferred for minimal bias and broad host range [42] [43] |
| Library Construction | High-efficiency electrocompetent cells, Transposase enzyme | Generation of saturated mutant library with comprehensive genomic coverage |
| Selection Media | Antibiotics for selection, Defined nutrient conditions | Application of selective pressure to identify conditionally essential genes |
| Sequencing Reagents | Illumina-compatible adapters, Polymerases for amplification | Preparation of high-quality libraries for sequencing transposon-genome junctions |
| Bioinformatic Tools | TRANSIT, TRADIS, Con-ARTIST | Statistical analysis of insertion data and fitness calculation [43] [46] |
Tn-seq has established itself as an indispensable methodology for systematically unraveling the genetic basis of bacterial persistence across diverse microbial pathogens. By enabling genome-wide assessment of gene fitness contributions under antibiotic pressure, this approach has revealed both conserved and species-specific mechanisms that enable bacterial subpopulations to survive lethal treatments. The continuing evolution of Tn-seq technologies—including advanced statistical methods like ZINB regression and specialized variants such as dTnSeq—promises to further enhance our understanding of persistence mechanisms.
The consistent identification of metabolic pathways, stress response systems, and detoxification mechanisms across multiple bacterial species suggests potential targets for novel anti-persister therapies. As Tn-seq applications expand to include more clinical isolates and relevant host-mimicking conditions, the resulting insights will increasingly translate into improved strategies for combating persistent bacterial infections that pose significant challenges in clinical settings.
Bacterial persisters are non-growing or slow-growing phenotypic variants that are genetically identical to the susceptible population but can survive antibiotic treatment and lead to treatment failure and chronic infections [1]. The study of intracellular persistence within macrophages is particularly crucial for understanding chronic infections caused by Salmonella enterica serovar Typhimurium (S. Typhimurium) and Mycobacterium tuberculosis (M. tuberculosis), as these pathogens have evolved sophisticated mechanisms to survive within host phagocytic cells [49] [50]. In vivo infection models provide indispensable platforms for investigating host-pathogen interactions, immune responses, and therapeutic efficacy under physiologically relevant conditions. This guide compares the established in vivo models for studying intramacrophage persistence of these two important bacterial pathogens, providing researchers with experimental data, methodologies, and practical resources to advance this critical area of infectious disease research.
Salmonella Infection Models and Persistence Mechanisms
Established Mouse Models for Salmonella Infection
Mouse models for Salmonella infection can be broadly categorized into systemic infection and colitis models, each with distinct applications for studying persistence.
Table 1: Comparison of Salmonella Mouse Infection Models
| Model Type | Infection Route | Mouse Strain | Pretreatment | Primary Disease Manifestation | Key Applications | Persistence Insights |
|---|---|---|---|---|---|---|
| Systemic Infection | Intragastric or Intraperitoneal | C57BL/6, BALB/c | None | Systemic dissemination, typhoid-like disease | Studying systemic dissemination, virulence factors | Historically used to model aspects of extraintestinal disease [51] |
| Streptomycin-Pretreated Colitis | Intragastric | C57BL/6, BALB/c | Streptomycin (20mg) 24h prior to infection | Inflammatory colitis in cecum and colon | Investigating inflammatory diarrhea, host-pathogen interactions in gut | Enables study of NTS-associated colitis; mimics human gastroenteritis [51] |
| Genetically Resistant | Intragastric | Resistant lines (e.g., Nramp1+) | None | Controlled extraintestinal infection | Probing host resistance mechanisms | Models how susceptible humans control infection [51] |
The streptomycin-pretreated murine colitis model is particularly valuable for studying non-typhoidal Salmonella (NTS) persistence. In this model, administration of streptomycin 24 hours prior to S. Typhimurium inoculation inhibits microbiota-associated intestinal colonization resistance, prompting a neutrophilic inflammatory response in the cecum and colon that mimics human inflammatory diarrhea [51]. This model has revealed that in susceptible mice (e.g., C57BL/6), significant S. Typhimurium dissemination from the gut to systemic sites occurs despite intestinal inflammation.
Molecular Mechanisms of Salmonella Intramacrophage Persistence
Salmonella employs sophisticated molecular strategies to establish and maintain intramacrophage persistence, primarily through toxin-antitoxin (TA) modules and metabolic adjustments.
Toxin-Antitoxin Systems: Salmonella possesses at least 14 putative class II TA modules that contribute to intramacrophage persister formation [49]. Among these, the GNAT family acetyltransferase toxin TacT (also called T8) promotes persister formation by acetylating aminoacyl-tRNA molecules, thereby blocking translation and inducing growth arrest [49]. This mechanism represents a novel strategy for bacterial persistence where tRNA acetylation inhibits protein synthesis without leading to cell death.
Another recently characterized TA system, ResTAResA (STM145441-STM145442), functions as an RNA cleavage-induced energy storage system. Structural analyses reveal that ResT toxin expression enhances persistence and increases intracellular ATP levels, particularly in the presence of aminoglycosides [52]. RNA-seq demonstrated that ResT-modulated gene expression provides a potential mechanism for ATP accumulation during persister formation, highlighting the connection between TA systems and bacterial energetics in persistence.
The following diagram illustrates the molecular mechanisms of Salmonella intramacrophage persistence:
Mycobacterium tuberculosis Infection Models and Persistence
Established Mouse Models for Tuberculosis Research
Multiple mouse models have been developed to study M. tuberculosis infection, each offering unique advantages for investigating different aspects of tuberculosis pathogenesis and persistence.
Table 2: Comparison of M. tuberculosis Mouse Infection Models
| Model Type | Infection Route | Mouse Strain | Inoculum Size | Disease Characteristics | Key Applications | Persistence Insights |
|---|---|---|---|---|---|---|
| Low-Dose Aerosol (LDA) | Aerosol | BALB/c, C57BL/6, C3HeB/FeJ | 30-100 CFU/lung | Chronic infection, organized granulomas | Vaccine testing, drug efficacy against chronic infection | Models latent infection with metabolic downshift [53] [50] |
| High-Dose Aerosol (HDA) | Aerosol | BALB/c, C57BL/6 | 3,000-10,000 CFU/lung | Rapidly progressive disease, high bacterial loads | Drug screening, bactericidal activity | Represents bacterial burden in human cavities [53] |
| Intravenous | Intravenous (tail vein) | BALB/c, C57BL/6 | High dose (e.g., 10^6 CFU) | Disseminated disease | Studying extrapulmonary TB, immune responses | Shows slower bactericidal killing with drug regimens [53] |
| C3HeB/FeJ (Kramnik) | Aerosol | C3HeB/FeJ | Low or high dose | Necrotic, hypoxic granulomas, human-like pathology | Studying caseous necrosis, drug penetration | Models persisters in necrotic lesions [50] [54] |
The C3HeB/FeJ mouse strain has emerged as a particularly valuable model because it develops necrotic, hypoxic granulomas that closely resemble human TB pathology, including caseous necrosis [54]. This model provides a more physiologically relevant environment for studying drug-tolerant persister populations that reside within these structured lesions.
Comparative studies have demonstrated that treatment outcomes for drug regimens are generally similar across different infection models, though the intravenous model shows slower bactericidal killing kinetics and higher relapse rates than aerosol infection models [53]. These findings underscore the importance of model selection when evaluating new therapeutic interventions.
Molecular Basis of M. tuberculosis Intramacrophage Persistence
M. tuberculosis employs multiple sophisticated strategies to establish and maintain persistence within the hostile macrophage environment, with metabolic downshift being a central theme.
Metabolic Downregulation and ATP Depletion: Single-cell analysis has revealed that M. tuberculosis persisters are stochastically generated low-ATP cells [55]. This low-energy state renders them tolerant to multiple antibiotics. Researchers using a FRET-based ATP biosensor (ATeam1.03YEMK) demonstrated that cell-to-cell variation in the expression of energy-generating enzymes like acetate kinase AckA drives persister formation [55]. Quenching this noise by overexpressing ackA dramatically decreases persisters, confirming that stochastic variation in energy metabolism contributes significantly to persistence.
High Persister (hip) Mutants: Selection experiments have identified M. tuberculosis mutants with dramatically increased persister frequencies. These hip mutants carry mutations in genes involved in lipid biosynthesis, carbon metabolism, toxin-antitoxin systems, and transcriptional regulators [56]. Transcriptome analysis of these mutants reveals high similarity in gene expression patterns despite different mutations, suggesting convergence on common persistence pathways. Importantly, clinical hip isolates exhibit greater ex vivo survival than low persister isolates, indicating their potential role in treatment failure and chronic infection [56].
Toxin-Antitoxin Systems: M. tuberculosis possesses approximately 80 TA modules, indicating an extremely high level of redundancy in mechanisms governing dormancy [56]. Ectopic overexpression of individual RelE homologues (Rv1246c, Rv2866, Rv3358) increases drug tolerance in a drug and isoform-specific manner, suggesting multiple persister subpopulations [56].
The following diagram illustrates M. tuberculosis intramacrophage persistence pathways:
Comparative Analysis of Persistence Mechanisms
Shared and Distinct Persistence Strategies
While both Salmonella and M. tuberculosis establish intramacrophage persistence, their strategies reflect adaptation to different host environments and disease manifestations.
Table 3: Comparative Analysis of Persistence Mechanisms
| Feature | Salmonella enterica serovar Typhimurium | Mycobacterium tuberculosis |
|---|---|---|
| Primary Disease | Gastroenteritis, invasive disease in immunocompromised | Pulmonary TB, disseminated disease |
| Intracellular Niche | Phagosome, Salmonella-containing vacuole | Phagosome, modified phagolysosome |
| Key Persistence Mechanisms | TA modules (TacT, ResTAResA), metabolic arrest | Metabolic downshift, TA modules, lipid bodies |
| TA Modules | 14+ putative class II TA modules [49] | ~80 TA modules [56] |
| Energy State in Persisters | Increased ATP under aminoglycoside stress [52] | Low ATP [55] |
| Stochastic Formation | Demonstrated in intracellular populations [49] | Driven by noise in energy metabolism [55] |
| hip Mutants | RelB mutation increases persisters >1000-fold [56] | Identified in clinical and in vitro selections [56] |
| Metabolic Adaptations | Not well characterized in persisters | Lipid accumulation, carbon source utilization shifts [56] |
Both pathogens extensively utilize toxin-antitoxin systems to induce dormancy, though M. tuberculosis possesses a significantly larger arsenal of these modules. Interestingly, they appear to employ different energy management strategies—Salmonella can increase ATP under certain stress conditions while M. tuberculosis persisters consistently demonstrate low ATP levels.
Experimental Workflow for Studying Intramacrophage Persistence
The following diagram illustrates a generalized experimental workflow for studying intramacrophage persistence in both pathogens:
The Scientist's Toolkit: Essential Research Reagents and Models
Table 4: Essential Research Resources for Intramacrophage Persistence Studies
| Category | Specific Reagents/Models | Application/Function | Examples from Literature |
|---|---|---|---|
| Mouse Strains | C57BL/6, BALB/c | Standard TB-resistant models for systemic infection | [51] [53] |
| C3HeB/FeJ (Kramnik model) | TB-susceptible strain with human-like pathology | [54] | |
| Bacterial Strains | S. Typhimurium 14028s | Wild-type strain for persistence studies | [52] |
| M. tuberculosis Erdman, H37Rv | Standard virulent strains for infection models | [53] [56] | |
| M. tuberculosis mc26020 (H37Rv ΔpanCD ΔleuCD) | Auxotrophic strain for BSL-2 studies | [56] | |
| Antibiotics for Model Setup | Streptomycin sulfate | Disrupt microbiota for Salmonella colitis model | [51] |
| Rifampicin, Isoniazid, Pyrazinamide | Standard TB drugs for treatment studies | [53] [34] | |
| Analytical Tools | λ Red recombination system | Gene deletion in Salmonella | [52] |
| ATeam1.03YEMK ATP biosensor | Single-cell ATP measurement in M. tuberculosis | [55] | |
| Flow cytometry with cytokine staining | Immune cell profiling from infected tissues | [51] [54] | |
| Specialized Reagents | IVE-TB antigen panels | T-cell recognition studies in murine models | [54] |
| ResTA complex structural analysis | TA system structure-function studies | [52] |
The comparative analysis of in vivo infection models for studying intramacrophage persistence in Salmonella and M. tuberculosis reveals both shared and pathogen-specific strategies for surviving within the hostile macrophage environment. While both pathogens utilize toxin-antitoxin systems and metabolic adjustments to establish persistence, they differ in their energy management strategies and specific molecular mechanisms. The selection of appropriate animal models—whether the streptomycin-pretreated colitis model for Salmonella or the C3HeB/FeJ mouse for M. tuberculosis—is critical for investigating relevant aspects of persistence in physiologically meaningful contexts. As research advances, the integration of these models with single-cell technologies and structural biology approaches will continue to unravel the complex mechanisms of bacterial persistence, potentially identifying new therapeutic targets for combating chronic and recurrent bacterial infections.
Metabolomic and Proteomic Profiling of Dormant Bacterial Subpopulations
Bacterial dormant subpopulations, including persister cells and viable but non-culturable (VBNC) cells, represent a significant challenge in treating persistent infections and contribute to antibiotic treatment failure worldwide [1] [57]. These phenotypic variants survive antibiotic exposure through mechanisms that include metabolic dormancy, reduced cellular energy, and altered proteomic profiles, while remaining genetically identical to their susceptible counterparts [4] [1] [5]. Understanding the molecular basis of bacterial persistence is critical for developing more effective treatments for chronic and recurrent infections.
This guide provides a comprehensive comparison of the mechanisms underlying persister formation across bacterial species, with a specific focus on insights gained from metabolomic and proteomic profiling. We objectively present experimental data and methodologies that reveal how bacterial pathogens rewire their metabolic networks and protein expression to survive antibiotic stress, offering researchers a resource for comparing persistence mechanisms across experimental models and bacterial species.
Comparative Mechanisms of Persister Formation Across Bacterial Species
Defining Bacterial Persister Subpopulations
Bacterial persisters are non-growing or slow-growing cells that tolerate high concentrations of antibiotics and can resume growth once the stress is removed [1] [57]. These cells are genetically identical to antibiotic-sensitive cells in the population but exhibit phenotypic heterogeneity that allows survival during treatment [5]. Several distinct subpopulations have been characterized:
- Type I Persisters: Form in response to environmental cues during stationary phase, demonstrate deep dormancy [1]
- Type II Persisters: Spontaneously generated during exponential growth, exhibit slow metabolism and shallow persistence [1]
- Viable But Non-Culturable (VBNC) Cells: Maintain viability and metabolic activity but cannot be cultured on routine media [58]
The table below compares key characteristics of these dormant bacterial subpopulations:
Table 1: Characteristics of Bacterial Dormant Subpopulations
| Characteristic | Persister Cells | VBNC Cells |
|---|---|---|
| Culturability | Can be cultured after antibiotic removal | Cannot be cultured on routine media, require specific resuscitation conditions [58] |
| Metabolic State | Reduced metabolic activity, but not always dormant [57] [59] | Metabolically active but at reduced capacity [58] |
| Antibiotic Tolerance | Transient tolerance to high antibiotic concentrations [1] | Tolerant to multiple stressors including antibiotics [58] |
| Formation Triggers | Antibiotic exposure, nutrient limitation, stress responses [4] [1] | Low temperature, salinity, oxidative stress, nutrient starvation [58] |
| Resuscitation | Stochastic awakening or in response to environmental signals [5] | Requires specific environmental stimuli (e.g., temperature upshift, nutrient addition) [58] |
Molecular Mechanisms of Persistence
Multiple molecular pathways contribute to persister formation across bacterial species, with considerable variation in their importance depending on the bacterial strain, growth phase, and specific stressor:
Toxin-Antitoxin (TA) Systems: Overproduction of toxins such as HipA, MqsR, and TisB induces dormancy by disrupting essential cellular processes including translation, DNA replication, and ATP synthesis [4] [57]. For example, HipA phosphorylates glutamyl-tRNA synthetase, inhibiting translation and leading to growth arrest [57].
(p)ppGpp Signaling: The alarmone guanosine tetraphosphate/pentaphosphate accumulates during nutrient limitation and stress responses, inhibiting RNA polymerase and GTP biosynthesis to arrest growth [57].
Energy Metabolism Reprogramming: Stationary-phase persisters in E. coli maintain active oxidative phosphorylation through Crp/cAMP regulation of the TCA cycle and electron transport chain, demonstrating that energy metabolism remains crucial for persistence despite reduced anabolism [60] [59].
Oxidative Stress Management: In Vibrio parahaemolyticus, lactate dehydrogenase (LldD) plays a critical role in VBNC state regulation by converting lactate to pyruvate, with deletion of the lldD gene accelerating VBNC formation [58].
Experimental Approaches for Profiling Dormant Subpopulations
Proteomic Profiling Methodologies
Proteomic analyses have revealed distinct protein expression patterns in dormant subpopulations, with advanced separation techniques enabling characterization of these rare cell states:
Subpopulation Isolation via Fluorescence-Activated Cell Sorting (FACS): Researchers have used FACS to isolate metabolically inactive E. coli persisters based on diminished fluorescence from a GFP reporter downstream of a ribosomal promoter [4]. Similarly, VBNC subpopulations of V. parahaemolyticus have been separated based on metabolic activity and cell shape [58].
LC-MS/MS Proteomic Workflow: For Mycobacterium tuberculosis dormant cells, liquid chromatography-tandem mass spectrometry identified 1,379 proteins preserved after 5 months of dormancy, with 468 showing statistically significant differences compared to actively growing cells [61]. Sample preparation typically includes protein extraction, digestion, peptide purification, and LC-MS/MS analysis with database searching.
Two-Dimensional Gel Electrophoresis: Earlier studies used 2D electrophoresis to separate and visualize protein expression differences, though this approach has limitations in proteome coverage and quantitative accuracy compared to LC-MS methods [61].
The table below summarizes key proteomic findings across bacterial species:
Table 2: Comparative Proteomic Profiles of Dormant Bacterial Subpopulations
| Bacterial Species | Key Proteomic Findings in Dormant State | Experimental Method | Reference |
|---|---|---|---|
| Vibrio parahaemolyticus (VBNC) | Two distinct subpopulations (P1/P2) with different resuscitation potentials; Lactate dehydrogenase (LldD) significantly upregulated | FACS separation, LC-MS/MS | [58] |
| Mycobacterium tuberculosis (Dormant) | 1,379 proteins preserved after 5 months dormancy; 468 significantly different from growing cells; pH-dependent regulatory system PhoP proteins identified | LC-MS/MS | [61] |
| Escherichia coli (Persisters) | Crp/cAMP complex redirects metabolism from anabolism to oxidative phosphorylation; TCA cycle and electron transport chain proteins maintained | LC-MS/MS, mutant analysis | [60] [59] |
| Staphylococcus aureus (Antibiotic Stress) | Minimal proteome changes under sub-MIC antibiotics despite significant metabolomic perturbations; altered translation and oxidative stress management proteins | LC-MS/MS | [62] |
Metabolomic Profiling Methodologies
Metabolomic approaches provide complementary insights into the biochemical activities of dormant cells, revealing how metabolic pathways are rewired under stress conditions:
Sample Preparation for Intracellular Metabolomics: Bacterial cultures are rapidly filtered, quenched, and metabolites extracted using methanol/acetonitrile/water mixtures. Careful handling is required to preserve labile metabolites and prevent stress responses during processing [62].
¹H NMR Spectroscopy: Untargeted ¹H NMR profiling identifies and quantifies metabolites in both intracellular and extracellular compartments. This approach revealed that E. coli, K. pneumoniae, E. faecium, and S. aureus exhibit distinct metabolome profiles under sub-inhibitory antibiotic concentrations despite minimal proteome changes in Gram-negative species [62].
Integrated Multi-Omics Analysis: Combining metabolomic data with proteomic and genomic validation provides a comprehensive view of metabolic rewiring. In E. coli persisters, this approach demonstrated that Crp/cAMP maintains active energy metabolism while downregulating anabolic pathways [60] [59].
Diagram 1: Experimental workflow for multi-omics analysis of dormant bacterial subpopulations, showing parallel proteomic and metabolomic pathways that converge for data integration.
Metabolic Pathways in Bacterial Persistence
Energy Metabolism and Redox Balance
Contrary to the historical view of persisters as completely dormant cells, recent metabolomic and proteomic evidence demonstrates that specific metabolic pathways remain active or are reprogrammed to support survival:
Lactate-Pyruvate Interconversion: In V. parahaemolyticus VBNC cells, lactate dehydrogenase (LldD) was significantly upregulated, and deletion of the lldD gene accelerated VBNC entry. Adding lactate to VBNC cells aided resuscitation and extended the resuscitation window, indicating a crucial role in maintaining redox balance [58].
TCA Cycle and Electron Transport Chain: E. coli persisters in stationary phase maintain active oxidative phosphorylation through Crp/cAMP-mediated regulation. Disruption of the Crp/cAMP complex reduced persister levels, demonstrating the importance of energy metabolism for survival [60] [59].
Stringent Response and (p)ppGpp Signaling: Nutrient limitation triggers (p)ppGpp accumulation, which inhibits GTP biosynthesis and translation while promoting persistence through toxin-antitoxin system activation [57].
Metabolic Heterogeneity Across Species
Different bacterial species employ distinct metabolic strategies for persistence, as revealed by comparative metabolomic studies:
Trimethylamine Metabolism: Under sub-inhibitory antibiotic concentrations, E. coli, K. pneumoniae, E. faecium, and S. aureus all showed alterations in trimethylamine metabolism, suggesting a conserved role in antibiotic stress survival [62].
Amino Acid and Nucleotide Metabolism: M. tuberculosis dormant cells maintain specific biosynthetic pathways, including salvaged pathways for mycothiol and UMP biosynthesis, supporting long-term survival under nutrient limitation [61].
Cell Wall Precursor Metabolism: In S. aureus exposed to vancomycin, suppression of D-alanine metabolism was observed, corresponding to altered cell wall biosynthesis in response to antibiotic pressure [62].
Diagram 2: Signaling pathways and metabolic reprogramming in dormant bacterial subpopulation formation, showing how environmental stressors trigger molecular responses that lead to metabolic changes and persistence.
The Scientist's Toolkit: Essential Research Reagents and Methodologies
This section provides a comparative overview of key reagents, methodologies, and experimental approaches used in persister research, enabling researchers to select appropriate tools for their specific bacterial system and research questions.
Table 3: Research Reagent Solutions for Dormancy Studies
| Reagent/Method | Function/Application | Examples in Literature |
|---|---|---|
| Fluorescence-Activated Cell Sorting (FACS) | Isolation of metabolically inactive subpopulations based on fluorescence markers | Separation of E. coli persisters using ribosomal promoter-GFP fusions [4]; Isolation of V. parahaemolyticus VBNC subpopulations [58] |
| Lactate Dehydrogenase Inhibitors/Activators | Modulation of lactate-pyruvate conversion to study redox balance in persistence | lldD gene deletion in V. parahaemolyticus accelerated VBNC formation; lactate addition extended resuscitation window [58] |
| cAMP Analogs/Crp Modulators | Investigation of Crp/cAMP-mediated metabolic regulation in persistence | Δcrp and ΔcyaA E. coli mutants showed reduced persister levels and altered energy metabolism [60] [59] |
| Toxin-Antitoxin System Modulators | Induction of dormancy through targeted toxin overexpression or antitoxin degradation | HipA overexpression increased E. coli persistence 10,000-fold; MqsR toxin cleaves most cellular transcripts inducing dormancy [4] [57] |
| LC-MS/MS Platforms | Comprehensive proteomic and metabolomic profiling of dormant subpopulations | Identification of 1,379 proteins in 5-month dormant M. tuberculosis [61]; Crp/cAMP proteomic network in E. coli [59] |
| ¹H NMR Spectroscopy | Untargeted metabolomic profiling of intracellular and extracellular metabolites | Revealed trimethylamine metabolism alterations across multiple species under antibiotic stress [62] |
Metabolomic and proteomic profiling has revolutionized our understanding of dormant bacterial subpopulations, revealing complex and heterogeneous mechanisms that extend beyond simple cellular dormancy. The comparative data presented in this guide demonstrates both conserved and species-specific adaptations in persister cells and VBNC states, highlighting the importance of metabolic rewiring rather than complete metabolic shutdown in many cases.
Key findings across studies indicate that energy metabolism maintenance, redox balance through lactate-pyruvate conversion, and stress signaling through (p)ppGpp and TA systems represent crucial nodes in persistence networks. These insights provide promising targets for developing anti-persister therapies that could address the significant clinical challenge of recurrent and persistent infections. Future research directions should focus on single-cell multi-omics approaches to better resolve the heterogeneity within persister subpopulations and temporal studies tracking metabolic transitions into and out of persistence states.
Bacterial persisters—dormant, metabolically inactive phenotypic variants present within genetically susceptible populations—represent a critical frontier in the challenge of eradicating persistent infections. These cells survive high-dose bactericidal antibiotic exposure without possessing heritable resistance mutations, then resume proliferation after antibiotic withdrawal, leading to recurrent infections and treatment failures [63] [1]. Evaluating compounds for anti-persister activity requires specialized models that mirror the unique physiological state of these cells, which conventional susceptibility testing fails to address. This guide provides a systematic comparison of experimental models for assessing anti-persister drug efficacy, from fundamental in vitro systems to clinically representative in vivo models, equipping researchers with the methodological framework necessary for translating promising compounds into effective therapies.
Persister Biology and Therapeutic Challenges
Defining Persistence, Tolerance, and Resistance
Understanding the distinction between antibiotic persistence, tolerance, and resistance is fundamental to designing appropriate evaluation strategies:
- Antibiotic Persistence: A phenomenon where a small subpopulation of genetically susceptible cells survives antibiotic treatment due to transient non-growing states, exhibiting a biphasic killing curve. Upon antibiotic removal, the surviving persisters regrow a population with identical susceptibility as the parent strain [63] [64].
- Antibiotic Tolerance: The ability of an entire bacterial population to survive transient antibiotic exposure due to slowed killing kinetics, without an increase in minimum inhibitory concentration (MIC) [63].
- Antibiotic Resistance: Genetically heritable ability to grow at elevated antibiotic concentrations, demonstrated by an increased MIC [64].
Table 1: Key Characteristics Differentiating Bacterial Survival Strategies
| Characteristic | Antibiotic Resistance | Antibiotic Tolerance | Antibiotic Persistence |
|---|---|---|---|
| MIC Change | Increased | Unchanged | Unchanged |
| Population Affected | Entire population | Entire population | Small subpopulation (typically <1%) |
| Heritability | Genetic mutation | Can be genetic or phenotypic | Non-heritable, phenotypic |
| Killing Kinetics | Monophasic | Monophasic, slowed | Biphasic ("killing curve with a tail") |
| Growth State | Growing | Slow-growing or non-growing | Dormant or slow-growing |
Molecular Mechanisms of Persister Formation
Persister formation involves multiple interconnected biological pathways that induce metabolic dormancy. Key mechanisms include:
- Toxin-Antitoxin (TA) Systems: Under stress conditions, stable toxins are released from unstable antitoxins, disrupting essential cellular processes. Type II TA systems like HipAB in E. coli phosphorylate glutamyl-tRNA synthetase, activating the stringent response via (p)ppGpp accumulation [64].
- Stringent Response: Nutrient limitation triggers (p)ppGpp alarmone synthesis, which dramatically reprograms cellular metabolism toward dormancy by downregulating energy-intensive processes like ribosome synthesis [1] [64].
- Biofilm-Associated Tolerance: The structured, matrix-encased communities in biofilms create heterogeneous microenvironments with nutrient and oxygen gradients that induce dormancy in subpopulations. Biofilms can contain up to 1000-fold more persisters than planktonic cultures [65] [2].
- Other Regulatory Systems: Quorum sensing, SOS response to DNA damage, and oxidative stress responses also contribute to persister formation through diverse signaling pathways that ultimately converge on growth arrest [1] [64].
Figure 1: Molecular Pathways of Persister Formation. Multiple environmental stresses converge on key bacterial stress response systems, ultimately leading to metabolic dormancy and the persister state.
Experimental Models for Anti-Persister Drug Evaluation
In Vitro Persister Models
In vitro systems provide controlled, reproducible platforms for initial compound screening and mechanism studies.
Planktonic Persister Models
These models generate persisters from liquid cultures without biofilm formation:
- Stationary Phase Persisters: inoculating from prolonged cultures (typically 24-48 hours) where nutrient depletion naturally induces dormancy in a subpopulation [63] [64].
- Antibiotic-Induced Persisters: pre-treating exponential-phase cultures with bacteriostatic antibiotics to enrich for persisters before testing experimental compounds [63].
- Chemical-Induced Persisters: using metabolic inhibitors like carbonyl cyanide m-chlorophenyl hydrazone (CCCP) to disrupt proton motive force and induce dormancy [20].
Table 2: Comparison of Planktonic Persister Models
| Model Type | Protocol Summary | Key Applications | Advantages | Limitations |
|---|---|---|---|---|
| Stationary Phase | Culture bacteria for 16-48h, harvest cells, treat with test compound | Initial drug screening, mechanism studies | Simple, high yield, reproducible | Heterogeneous population with mixed metabolic states |
| Antibiotic-Induced | Pre-treat exponential culture with bacteriostatic antibiotic (e.g., rifampicin), wash, then test compound | Studying persister awakening, combination therapies | Synchronized population, defined induction | Potential carryover effects, complex protocol |
| Chemical-Induced | Treat exponential culture with metabolic inhibitor (e.g., CCCP), wash, then test compound | Studying energy-dependent mechanisms | Highly controlled induction, rapid | Non-physiological induction, toxicity concerns |
Biofilm Persister Models
Biofilm models better mimic clinical persistent infections, as biofilms naturally contain elevated persister levels:
- Static Biofilm Models: Growing biofilms on polystyrene plates or coverslips, then treating with test compounds [66] [2].
- Flow-Cell Biofilm Models: Culturing biofilms under continuous nutrient flow to establish mature, structured communities with characteristic antibiotic tolerance profiles [65].
- Alginate Bead Encapsulation: Embedding bacteria in seaweed alginate beads to mimic the extracellular polymeric substance matrix of in vivo biofilms, particularly relevant for Pseudomonas aeruginosa cystic fibrosis infections [67].
Standardized Biofilm Susceptibility Testing Protocol [66]:
- Inoculate 6-well polystyrene plates with bacterial suspension (10^5 CFU/mL) in appropriate medium.
- Incubate statically at 37°C for 7 hours to allow biofilm formation.
- Carefully remove planktonic phase and replace with fresh medium containing test compounds.
- Incubate for additional 15-24 hours under appropriate conditions.
- Quantify viable biofilm bacteria by sonication followed by serial dilution and plating.
- Include appropriate controls: untreated biofilm, vehicle control, and planktonic culture reference.
In Vivo Persister Models
In vivo models provide critical assessment of anti-persister efficacy in the context of host immunity and tissue environments.
Murine Lung Infection Model
This model specifically addresses Pseudomonas aeruginosa persistence in cystic fibrosis-like conditions [67]:
Optimized Protocol:
- Embed P. aeruginosa in seaweed alginate beads to mimic biofilm conditions.
- Intratracheally instill 5×10^5 CFU/mouse into BALB/c mice.
- Allow infection to establish for 24 hours.
- Administer tobramycin (120 mg/kg) via nasal droplets to simulate inhalation therapy.
- Monitor bacterial load in lungs over time, typically demonstrating initial 2-log reduction followed by persister survival plateau.
- Compare survival levels between strains and treatments to assess persistence.
Key Validation: This model demonstrated positive correlation between in vitro persister survival and in vivo antibiotic tolerance, validating classical persistence assays as predictive of clinical outcomes [67].
Other In Vivo Models
- Subcutaneous Biofilm Model: Implanting biofilm-colonized catheters or chambers subcutaneously to study device-related infections [67].
- Urinary Tract Infection Model: Infecting mouse bladder with uropathogenic E. coli to study recurrent UTIs associated with persisters [63] [64].
- Mycobacterium tuberculosis Models: Using various mouse and guinea pig models to evaluate drugs like pyrazinamide that specifically target persister cells [1].
Table 3: Comparison of In Vivo Persister Models
| Model System | Infection Method | Treatment Administration | Key Readouts | Clinical Relevance |
|---|---|---|---|---|
| Murine Lung Model | Intratracheal instillation of bacteria in alginate beads | Nasal droplets, inhalation | Lung bacterial load, survival | Cystic fibrosis, ventilator-associated pneumonia |
| Subcutaneous Biofilm | Implantation of colonized catheter | Systemic, localized | Catheter bacterial counts, local inflammation | Medical device infections |
| Urinary Tract Model | Transurethral instillation | Systemic, intravesical | Bladder/kidney bacterial load, recurrence rates | Recurrent UTIs |
| M. tuberculosis Models | Aerosol, intravenous | Oral, systemic | Organ bacterial load, relapse rates | Tuberculosis therapy |
Anti-Persister Therapeutic Strategies
Direct Killing Approaches
Direct killing strategies target growth-independent cellular structures and processes:
- Membrane-Targeting Compounds: Synthetic cation transporters (SA-558), porphyrin derivatives (XF-70, XF-73), and antimicrobial peptides disrupt membrane integrity, causing leakage and death regardless of metabolic state [34].
- Protease Activation: ADEP4 activates ClpP protease, causing uncontrolled protein degradation in dormant cells [34].
- Energy Disruption: Pyrazinoic acid (active form of pyrazinamide) disrupts membrane energetics in M. tuberculosis persisters [34].
Indirect Killing Approaches
Indirect approaches target persister viability by altering their metabolic state:
- Metabolite-Mediated Reprogramming: Exogenous metabolites (mannitol, pyruvate) can reactivate central metabolism and proton motive force, sensitizing persisters to conventional antibiotics [20].
- Wake-and-Kill Strategies: Compounds that induce resuscitation from dormancy followed by conventional antibiotic treatment [20] [34].
- Prevention of Persister Formation: Quorum sensing inhibitors, H2S biosynthesis inhibitors, and nitric oxide donors can reduce de novo persister formation [34].
Figure 2: Anti-Persister Compound Mechanisms of Action. Therapeutic strategies either directly kill persisters through growth-independent mechanisms or sensitize them to conventional antibiotics by altering their metabolic state.
The Scientist's Toolkit: Essential Research Reagents
Table 4: Key Reagents for Persister Research
| Reagent/Category | Specific Examples | Research Application | Key Considerations |
|---|---|---|---|
| Bacterial Strains | E. coli hipA7 mutant, P. aeruginosa PA14, S. aureus HG001, M. tuberculosis H37Rv | Mechanism studies, compound screening | Select strains with documented persistence phenotypes; consider clinical isolates for translational studies |
| Persister-Inducing Agents | CCCP, rifampicin, ampicillin, nutrient limitation media | Generating persister populations for testing | Optimize concentration and exposure time to maximize yield while maintaining viability |
| Biofilm Matrix Materials | Seaweed alginate, polystyrene plates, flow cells | Creating biofilm-associated persister models | Alginate beads better mimic cystic fibrosis mucus than plastic substrates |
| Detection Reagents | Live/dead staining (SYTO9/propidium iodide), ATP assays, ROS probes | Assessing viability and metabolic state | Combine multiple methods as no single assay fully captures persister physiology |
| Anti-Persister Compounds | ADEP4, pyrazinamide, mannitol, XF-73, SA-558 | Positive controls for assay validation | Include compounds with different mechanisms of action |
| Conventional Antibiotics | Tobramycin, ciprofloxacin, ofloxacin, ampicillin | Combination studies and persister enrichment | Select based on bacterial species and target pathway |
Evaluating anti-persister drug efficacy requires specialized approaches that account for the unique biological characteristics of these dormant bacterial subpopulations. A tiered testing strategy—progressing from simple in vitro planktonic models through biofilm systems to clinically relevant animal models—provides the most comprehensive assessment of therapeutic potential. The correlation between in vitro persistence levels and in vivo treatment outcomes [67] validates this systematic approach while highlighting the necessity of incorporating host environment factors in later development stages. As research advances, standardization of persister-specific efficacy metrics and increased implementation of biofilm and host-mimicking models will accelerate the development of therapies capable of addressing the significant clinical challenge posed by persistent bacterial infections.
Overcoming Therapeutic Roadblocks: Challenges and Emerging Anti-Persister Strategies
Bacterial persisters are a subpopulation of cells that are genetically identical to their antibiotic-susceptible kin but can survive lethal antibiotic treatment by entering a transient, dormant state. Unlike resistant bacteria, persisters do not possess heritable genetic resistance mutations and exhibit normal Minimum Inhibitory Concentrations (MICs); their survival is instead attributed to phenotypic tolerance [1] [64]. When antibiotic pressure is removed, these cells can resume growth, leading to relapsing and chronic infections that are notoriously difficult to treat [1]. The presence of persister cells is a major contributor to treatment failure in infections such as tuberculosis, recurrent urinary tract infections, and biofilm-associated infections on medical devices [1] [14]. Current standard clinical diagnostics, which rely on determining MICs and genetic resistance markers, are fundamentally blind to this phenotypic tolerance. This critical diagnostic gap undermines effective treatment and contributes to the global antimicrobial resistance (AMR) crisis. As the World Health Organization (WHO) has recently highlighted, there are persistent and critical gaps in diagnostics, particularly for detecting non-resisting bacterial survival strategies [68]. This guide provides a comparative analysis of persister mechanisms and the experimental methodologies essential for developing diagnostics that can close this gap.
Comparative Analysis of Persister Formation Across Bacterial Species
The molecular mechanisms driving persister formation are diverse and can vary significantly between bacterial species and even within a population. Understanding these differences is crucial for developing broad-spectrum detection strategies. The table below summarizes key persistence mechanisms and their prevalence across major pathogenic species, as evidenced by current research.
Table 1: Comparison of Persister Formation Mechanisms in Major Pathogenic Bacteria
| Bacterial Species | Key Persistence Mechanisms | Inducing Antibiotics | Reported Persister Frequency | Key Genetic Elements Identified |
|---|---|---|---|---|
| Staphylococcus aureus | Biofilm formation, potential TA systems, reduced metabolism [69] [1] | Gentamicin [69] | Forms persisters with Gentamicin [69] | mazF (2.44% of clinical isolates) [69] |
| Pseudomonas aeruginosa | Biofilm formation, stringent response, low metabolic activity [1] [14] | Ciprofloxacin, Gentamicin [69] | No persister formation observed in one study [69] | mazF (28.13% of clinical isolates) [69] |
| Salmonella spp. | Intracellular survival, SOS response, TA systems [1] [64] | Ciprofloxacin [69] | Forms persisters with Ciprofloxacin [69] | hipA (28.57% of clinical isolates) [69] |
| Escherichia coli | Type I & II TA modules (e.g., hipA, mazF), (p)ppGpp, Lon protease, SOS response [1] [14] [64] |
Ampicillin, Ciprofloxacin [70] [5] | Varies with strain, growth phase, and assay conditions [70] | hipA, mazF, relE, tisB, hokB [64] [5] |
| Mycobacterium tuberculosis | Stringent response, redox homeostasis, toxin-antitoxin systems [1] | Isoniazid, Rifampicin [1] | Primary driver of lengthy TB therapy [1] | hipA, Rel (p)ppGpp synthetase [1] |
Key Insights from Comparative Data
- Mechanistic Heterogeneity: No single, universal mechanism explains persister formation. While Toxin-Antitoxin (TA) modules are prominent in E. coli, their role in S. aureus is less clear, and P. aeruginosa relies more heavily on biofilm formation and stringent response [69] [14] [64].
- Strain and Context Dependence: The formation of persisters and the efficacy of specific mechanisms are highly dependent on the bacterial strain, growth phase, and environmental context (e.g., biofilm vs. planktonic) [70]. This is evidenced by the varying prevalence of persistence genes like
mazFin clinical isolates of P. aeruginosa and S. aureus [69]. - Antibiotic-Specific Killing: The ability to form persisters is not absolute but can depend on the class of antibiotic used. For example, S. aureus showed persister formation with gentamicin but not with ciprofloxacin in a specific study, while the opposite was true for Salmonella sp. [69]. This suggests that future diagnostics may need to account for the treatment context.
Standardized Experimental Protocols for Persister Research
Robust and reproducible experimental protocols are the bedrock of persister research. The following section details key methodologies used to quantify and study persisters, with a focus on standardizing conditions to avoid common pitfalls.
Time-Kill Assay for Persister Quantification
The time-kill assay is the gold-standard method for quantifying persister cells based on their characteristic biphasic killing curve [69] [64].
Detailed Protocol:
- Culture Preparation: Grow bacterial cultures to the desired growth phase (e.g., mid-exponential or stationary phase). Note that the inoculum size and growth medium (LB vs. defined M9) can dramatically affect results and must be carefully controlled [70].
- Antibiotic Exposure: Expose the culture to a high concentration of a bactericidal antibiotic (typically 10-100x the MIC). Examples from studies include:
- Viable Cell Count: At predetermined time points (e.g., 1, 3, 5, 7, and 20 hours), remove aliquots from the culture [69].
- Wash Steps: Centrifuge the aliquot, discard the supernatant containing the antibiotic, and resuspend the pellet in sterile saline (0.85%) to remove the antibiotic. This step is critical to prevent carryover during plating [69].
- Serial Dilution & Plating: Perform serial dilutions in sterile diluent and spot-plate or spread-plate onto fresh, antibiotic-free Mueller-Hinton (MH) agar plates [69] [70].
- Incubation and Enumeration: Incubate plates at 37°C for 24-48 hours. Count the resulting colonies (CFUs) using automated colony counters or manual counts.
- Data Analysis: Plot the log(_{10}) of CFU/mL versus time. The persister population is identified as the subpopulation that survives after the initial rapid killing phase, resulting in a biphasic curve [64].
Single-Cell Persister Recovery Analysis
Understanding the resuscitation dynamics of persisters is as important as detecting their initial formation.
Detailed Protocol (Adapted from Wilmaerts et al.) [71]:
- Persister Isolation: First, generate and isolate persister cells using a time-kill assay as described above, followed by washing and resuspension in fresh media.
- Recovery Monitoring: Distribute the resuspended persisters into a 96-well plate. Use a microplate spectrophotometer to monitor optical density (OD) at 600 nm for each well continuously over 24-48 hours.
- Single-Cell Physiology: To correlate recovery kinetics with physiological states, sample cells from recovering cultures at different OD time points and analyze using flow cytometry with viability stains (e.g., propidium iodide) and metabolic activity probes (e.g., CFDA-AM) [71].
- Data Analysis: Determine the lag time (time until growth resumption) and growth rate for each well. Flow cytometry data will reveal the heterogeneity in metabolic activity within the recovering persister population.
Diagram: Experimental Workflow for Persister Analysis
Molecular Mechanisms and Signaling Pathways of Persistence
Persister formation is governed by a network of interconnected biochemical pathways that sense stress and induce a dormant, tolerant state. The following diagram and table detail the core molecular players.
Diagram: Core Molecular Pathways of Bacterial Persister Formation
Table 2: Key Molecular Mechanisms and Effectors in Bacterial Persistence
| Mechanism/Pathway | Key Effector Molecules | Molecular Function in Persistence | Bacterial Species Where Found |
|---|---|---|---|
| Toxin-Antitoxin (TA) Modules | HipA (toxin), MazF (toxin), RelE (toxin) | Toxins inhibit essential processes (translation, replication); Lon protease degrades antitoxins under stress [69] [14] [64]. | E. coli, Salmonella, P. aeruginosa, M. tuberculosis [69] [1] |
| Stringent Response | (p)ppGpp ("alarmone") | Triggers global transcriptional reprogramming, downregulating energy-intensive processes and promoting dormancy [1] [14]. | Nearly all bacteria, including E. coli, M. tuberculosis, S. aureus [1] [14] |
| Biofilm Formation | Extracellular Polymeric Substance (EPS) matrix | Provides physical barrier to antibiotics and immune cells; creates nutrient gradients that induce dormancy [14] [64]. | P. aeruginosa, S. aureus, E. coli [1] [14] |
| SOS Response | RecA, LexA | DNA damage repair system induced by fluoroquinolones; can lead to cell cycle arrest and increased persistence [64] [5]. | E. coli, Salmonella, other Gram-negatives [64] |
| Membrane Potential & ATP | HokB (toxin), ATP pools | Toxins like HokB can collapse membrane potential, reducing ATP production and aminoglycoside uptake [64] [5]. | E. coli, B. subtilis [64] [5] |
The Scientist's Toolkit: Essential Reagents and Solutions
The following table catalogs critical reagents and their applications for studying bacterial persisters, forming a core toolkit for researchers in the field.
Table 3: Essential Research Reagent Solutions for Persister Studies
| Reagent / Material | Function in Persister Research | Examples & Key Details |
|---|---|---|
| Bactericidal Antibiotics | To apply lethal selective pressure for isolating and quantifying persisters via time-kill assays. | Ciprofloxacin (0.1 mg/mL) [69]; Gentamicin (0.1-0.4 mg/mL) [69]; Ampicillin (100x MIC) [70]. |
| Defined Culture Media | To provide a reproducible and consistent growth environment, minimizing batch-to-batch variability. | M9 minimal medium (superior reproducibility vs. nutrient-rich LB medium) [70]. |
| Metabolic Activity Probes | To assess the metabolic state of cells at the single-cell level, distinguishing dormant persisters. | Flow cytometry with stains like CFDA-AM (measures esterase activity) [71]. |
| Viability Stains | To differentiate between live and dead cells, especially in combination with metabolic probes. | Propidium Iodide (PI) stains dead cells with compromised membranes [71]. |
| Molecular Biology Kits | To detect and quantify the genetic elements associated with persistence mechanisms. | PCR kits for detecting TA genes (hipA, mazF, relE) in clinical isolates [69]. |
| Lon Protease Assays | To study the role of protein degradation in activating TA modules. | Activity assays to monitor Lon-mediated degradation of antitoxins [14] [64]. |
| (p)ppGpp Detection Kits | To quantify the "alarmone" levels, a central regulator of the stringent response. | HPLC or enzymatic assays for intracellular (p)ppGpp measurement [1] [14]. |
The fight against antimicrobial resistance is incomplete without addressing the challenge of bacterial persistence. As this guide has detailed, persisters are a heterogeneous population arising from multiple, species-specific mechanisms that render them invisible to standard MIC-based diagnostics. The experimental data and protocols summarized here provide a foundation for researchers to consistently study this phenotype. The current diagnostic landscape, as analyzed by the WHO, suffers from a critical lack of tools suitable for detecting these tolerant cells, particularly in low-resource settings [68]. Closing this gap requires a concerted effort to innovate diagnostics that move beyond genetic resistance and capture phenotypic tolerance. Promising avenues include developing assays that probe cellular metabolic activity, detect specific persistence-related biomarkers, or utilize phage-based technologies to identify dormant cells [72]. Investing in such next-generation diagnostics is not merely an academic exercise; it is a critical public health imperative to improve the treatment of chronic and relapsing infections and to curb the escalation of AMR.
The global health landscape faces a mounting threat from antimicrobial resistance (AMR), which the World Health Organization (AMR) associates with nearly 5 million deaths annually [73]. The development of new antibacterial agents is failing to keep pace with this growing crisis. According to the WHO's latest analysis, the antibacterial pipeline faces a dual crisis of scarcity and lack of innovation [68] [73]. The number of antibacterial agents in clinical development has decreased from 97 in 2023 to 90 in 2025 [68] [73]. Among these 90 agents, only 15 qualify as innovative, and merely 5 are effective against at least one of the WHO's "critical" priority pathogens—the most dangerous category of drug-resistant bacteria [68] [73] [74]. This innovation gap becomes particularly problematic when confronting bacterial persistence, a phenotypic adaptation where susceptible bacterial cells survive antibiotic treatment by entering a dormant state, only to resume growth after treatment cessation, leading to chronic and relapsing infections [1] [14] [64].
Quantitative Analysis of the Global Antibacterial Pipeline
The clinical pipeline for antibacterial agents has contracted since 2023, with traditional antibiotics constituting just over half of the candidates in development [68] [73]. The preclinical pipeline shows more activity, with 232 programs across 148 groups worldwide, though this ecosystem is considered fragile as 90% of companies involved are small firms with fewer than 50 employees [68] [73].
Table 1: Clinical Pipeline for Antibacterial Agents (2025 WHO Data)
| Pipeline Category | Number of Agents | Key Characteristics and Gaps |
|---|---|---|
| Total Clinical Pipeline | 90 | Down from 97 in 2023 [73] |
| Traditional Antibacterial Agents | 50 | Direct-acting small molecules [68] [73] |
| Non-Traditional Agents | 40 | Bacteriophages, antibodies, microbiome-modulating agents [68] [73] |
| Innovative Agents | 15 | Absence of known cross-resistance, new targets/classes/modes of action [68] [73] |
| Agents Targeting Critical Priority Pathogens | 5 | Target carbapenem-resistant A. baumannii, Enterobacterales, or rifampicin-resistant TB [73] |
Table 2: Analysis of Innovation Gaps in the Antibacterial Pipeline
| Pipeline Deficiency | Impact on Public Health |
|---|---|
| Lack of pediatric formulations and oral outpatient treatments | Limits treatment options for vulnerable populations and in community settings [68] [73] |
| Insufficient solutions for escalating resistance | Highlights need for combination strategies with non-traditional agents [68] |
| Focus on Gram-negative bacteria | While innovation is urgently needed here, balance across pathogen types is important [68] |
| Market failures and R&D ecosystem fragility | Disproportionate reliance on small companies threatens pipeline sustainability [68] [73] |
Bacterial Persistence: A Formidable Challenge to Antibacterial Efficacy
Defining Persisters and Their Clinical Significance
Bacterial persisters are a subpopulation of genetically susceptible, quiescent cells that can survive exposure to high concentrations of antibiotics and other environmental stresses [1] [65]. After the stress is removed, these cells can regrow and remain susceptible to the same stress [1]. This phenomenon differs fundamentally from antibiotic resistance, which involves heritable genetic changes that enable bacteria to grow in the presence of antibiotics [14] [64]. In contrast, persistence is a transient, non-heritable phenotypic adaptation where cells survive without growing during antibiotic exposure [14] [4]. Persisters are now recognized as a primary cause of chronic and relapsing infections such as tuberculosis, recurrent urinary tract infections, and biofilm-associated infections in cystic fibrosis patients [1] [65] [14].
Comparative Mechanisms of Persister Formation Across Bacterial Species
Research across multiple bacterial pathogens has revealed conserved mechanisms that drive persister formation. The table below synthesizes key findings from experimental studies on major pathogenic species.
Table 3: Comparison of Persister Formation Mechanisms Across Bacterial Species
| Bacterial Species | Key Molecular Mechanisms | Experimental Evidence | Clinical/Model Association |
|---|---|---|---|
| Escherichia coli | Toxin-antitoxin systems (HipBA, MqsRA, TisB/IstR-1); (p)ppGpp; SOS response [14] [4] [64] | Deletion of mqsR and tisAB-istR reduces persistence; HipA7 mutant increases persistence 1000-fold [4] [64] | Selected in patients with recurrent urinary tract infections [64] |
| Mycobacterium tuberculosis | Stringent response; metabolic reprogramming; DosR regulon [1] | Analysis of persister genes in non-replicating populations [1] | Crucial role in chronic tuberculosis requiring lengthy treatment [1] |
| Pseudomonas aeruginosa | Biofilm-mediated tolerance; toxin-antitoxin modules; SOS response [1] [65] [14] | Late CF isolates show 100-fold higher persistence than early isolates; high-persister mutants in CF patients [65] [14] | Major concern in cystic fibrosis and immunocompromised patients [14] |
| Staphylococcus aureus | Biofilm formation; metabolic dormancy [1] [14] | First described by Bigger in 1944; stationary phase cells show high tolerance [14] [4] | Associated with chronic infections like endocarditis [1] |
Experimental Methodologies for Investigating Persistence Mechanisms
Standardized Persister Isolation and Quantification Protocols
A critical methodology for persister research involves the antibiotic kill curve assay, which generates the characteristic biphasic killing curve where susceptible cells die rapidly, leaving a subpopulation of persisters that die slowly [14] [64]. The standard protocol involves:
- Culture Preparation: Grow bacterial cultures to desired growth phase (exponential, stationary, or biofilm) [4]
- Antibiotic Exposure: Expose to bactericidal antibiotics at 10-100× MIC for defined periods [64]
- Viable Counting: Remove samples at time intervals, wash to remove antibiotics, serially dilute, and plate on antibiotic-free media [4] [64]
- Data Analysis: Plot killing curves (log CFU/mL vs. time); persister levels are quantified as the surviving fraction after 24 hours of antibiotic exposure [64]
For more precise isolation of persister cells, fluorescence-activated cell sorting (FACS) can be employed using fluorescent reporters under control of ribosomal promoters to isolate metabolically inactive cells with diminished fluorescence [4].
Advanced Techniques for Mechanistic Studies
Recent technological advances have enabled more detailed investigation of persister mechanisms:
- Single-cell analysis techniques including microfluidics, high-throughput sequencing, and microscopy reveal heterogeneity within persister populations [14]
- Transcriptomic and proteomic approaches compare gene expression and protein profiles between persisters and normal cells [1] [4]
- Metabolic flux analysis examines the reduced metabolic activity characteristic of persistent cells [64]
Diagram Title: Experimental Workflow for Persister Quantification
The Scientist's Toolkit: Essential Reagents for Persistence Research
Table 4: Key Research Reagent Solutions for Persister Studies
| Reagent/Category | Specific Examples | Research Application | Experimental Function |
|---|---|---|---|
| Bactericidal Antibiotics | Ampicillin, Ofloxacin, Ciprofloxacin | Persister induction and killing assays [4] [64] | Select for and quantify persister populations via biphasic killing curves |
| Fluorescent Reporters | GFP under ribosomal promoters | FACS isolation of persisters [4] | Identify and isolate metabolically inactive cells based on diminished fluorescence |
| Molecular Biology Tools | Deletion mutants (e.g., ΔmqsR, ΔtisB), overexpression plasmids | Mechanistic studies [4] [64] | Determine gene function in persister formation via genetic manipulation |
| Metabolic Probes | ATP assays, membrane potential dyes | Metabolic state characterization [4] [64] | Measure metabolic activity and energy status of persister cells |
| Biofilm Culturing Systems | Flow cells, microtiter plates, catheter segments | Biofilm persister studies [65] [14] | Model biofilm-associated persistence in environmentally relevant conditions |
Integrated Signaling Pathways in Bacterial Persistence
The molecular mechanisms governing persister formation involve interconnected cellular signaling systems that respond to environmental stress. The diagram below illustrates the key pathways and their interactions.
Diagram Title: Signaling Pathways in Persister Formation
The molecular mechanisms illustrated above represent promising targets for novel anti-persister therapies. The HipBA toxin-antitoxin system was the first persistence module identified in E. coli, where HipA phosphorylates glutamyl-tRNA synthetase (GltX), leading to accumulation of uncharged tRNA and activation of the stringent response via (p)ppGpp production [64]. The MqsRA system promotes persistence through MqsR toxin cleavage of cellular mRNAs, effectively dampening translation and metabolic activity [4]. The TisB/IstR-1 type I system generates a small toxin peptide that inserts into the membrane, dissipating the proton motive force and reducing ATP levels [4] [64]. These mechanisms collectively drive cells into a dormant state that protects essential cellular processes from antibiotic targeting.
The scarcity of innovative antibacterial agents in the development pipeline represents a critical vulnerability in our defense against drug-resistant infections. With only 15 innovative agents in clinical development and just 5 targeting critical priority pathogens, the pipeline remains insufficient to address the growing AMR threat [68] [73]. This innovation gap is particularly problematic for addressing bacterial persistence, which requires therapeutic approaches fundamentally different from those needed for genetic resistance. Overcoming the persister problem will require dedicated investment in R&D targeting the molecular mechanisms of dormancy and phenotypic tolerance, with emphasis on combination strategies incorporating non-traditional agents [68] [74]. The WHO urges developers to publish data on antibacterial activity to foster collaboration, attract investment, and accelerate the innovation needed to stay ahead of bacterial evolution [68]. Without substantial increases in research investment and a coordinated global effort, drug-resistant infections—including those driven by bacterial persisters—will continue to threaten modern medicine and global public health.
Bacterial biofilms, which are structured communities of microorganisms encased in a self-produced extracellular polymeric substance (EPS), represent a significant challenge in clinical and industrial settings [75]. Biofilm-associated infections account for 65-80% of all human microbial infections, leading to serious mortality and morbidity due to their elevated tolerance to antimicrobial agents and host immune responses [76]. This tolerance is distinct from genetic resistance; it is a phenotypic state enabled by the biofilm's physical and physiological properties [28]. The biofilm matrix functions as a protective barrier, shielding resident cells and creating heterogeneous microenvironments that support metabolically dormant persister cells [1] [76]. These non-growing or slow-growing bacterial subsets can survive antibiotic exposure and repopulate biofilms after treatment ceases, contributing significantly to chronic and relapsing infections [1].
Understanding the mechanisms of biofilm-associated tolerance is crucial for developing effective therapeutic strategies. This guide provides a comparative analysis of two promising approaches: dispersal agents that trigger biofilm breakdown and matrix-targeting compounds that disrupt structural integrity. We objectively evaluate their performance, mechanisms, and experimental support to inform research and development decisions for professionals addressing the persistent challenge of biofilm-associated infections.
Biofilm Composition and Tolerance Mechanisms
The Extracellular Polymeric Substance (EPS) Matrix
The EPS matrix is a complex, dynamic assemblage of biopolymers that constitutes the structural scaffold of biofilms, making up over 90% of their dry mass [28]. This matrix is primarily composed of exopolysaccharides, extracellular proteins, lipids, and extracellular DNA (eDNA) [76]. The composition varies significantly between species and environmental conditions, but common exopolysaccharides include partially de-N-acetylated poly-β-(1,6)-N-acetyl-D-glucosamine (dPNAG), alginate, Pel, Psl, and cellulose [76]. The matrix traps nutrients, facilitates cell-cell communication, and provides mechanical stability, but its most clinically relevant function is protection [77] [75].
Mechanisms of Biofilm-Associated Tolerance
Biofilms confer tolerance through interconnected physical, physiological, and genetic mechanisms:
- Physical Barrier Function: The anionic nature of matrix components (e.g., eDNA, certain polysaccharides) can bind cationic antibiotics, such as aminoglycosides, retarding their diffusion and preventing lethal concentrations from reaching interior cells [75] [28].
- Metabolic Heterogeneity: Gradients of nutrients and oxygen within the biofilm create zones of slow growth or metabolic dormancy. As most antibiotics target active cellular processes, these dormant cells exhibit extreme tolerance [76] [28].
- Persister Cell Formation: A small subpopulation of cells enters a dormant, non-dividing state that is highly tolerant to antimicrobials. These persister cells can survive treatment and regrow once the stress is removed, causing relapse [1] [76].
- Enhanced Mutation and Gene Exchange: The structured, high-density environment of biofilms facilitates more efficient horizontal gene transfer, accelerating the development of genuine, heritable antibiotic resistance [28].
The following diagram illustrates the key signaling pathway that regulates the transition between planktonic and biofilm lifestyles, a central switch controlling tolerance.
Figure 1: Cyclic di-GMP (c-di-GMP) Signaling Pathway in Biofilm Regulation. This secondary messenger system is a central switch controlling the transition between planktonic and biofilm lifestyles. High intracellular c-di-GMP, promoted by diguanylate cyclases (DGCs), upregulates EPS production and represses motility, encouraging biofilm formation. Conversely, phosphodiesterases (PDEs) degrade c-di-GMP, and low levels promote dispersal and a return to motile, planktonic behavior [75] [28].
Comparative Analysis of Anti-Biofilm Agents
Matrix-Targeting Enzymes
Enzymes that degrade specific components of the EPS matrix are highly effective dispersal agents. They act extracellularly, making resistance development less likely, and can expose embedded cells to antimicrobials [76].
Table 1: Comparative Performance of Major Biofilm-Dispersing Enzymes
| Enzyme Class | Key Molecular Targets | Representative Experimental Results | Notable Advantages |
|---|---|---|---|
| Glycoside Hydrolases | dPNAG, Alginate, Cellulose, Psl, Pel [76] | Dispersase (glycoside hydrolase) reduced P. aeruginosa biofilm biomass by >80% in vitro; combined with tobramycin, reduced bacterial load by ~4 log CFU in a murine model [76]. | High specificity; effective against pre-existing biofilms; synergy with antibiotics demonstrated in vivo. |
| Proteases | Matrix proteins, Adhesins [76] | Serine protease dispersed >70% of S. aureus biofilm; potentiated action of gentamicin, leading to complete eradication in an in vitro model [76]. | Targets proteinaceous scaffold and adhesion factors; broad-spectrum potential. |
| Deoxyribonucleases (DNases) | Extracellular DNA (eDNA) [76] | DNase I treatment reduced biofilm integrity of multiple species; enhanced susceptibility to vancomycin in S. epidermidis biofilms [76]. | Disrupts anionic matrix component that binds antibiotics; effective against early-stage biofilms. |
Small Molecule Dispersal Agents and Matrix Inhibitors
Small molecules can interfere with biofilm formation and maintenance by targeting regulatory systems, signal molecules, or EPS synthesis.
Table 2: Small Molecule Agents Targeting Biofilm Formation and Tolerance
| Agent Category | Molecular Target/Mechanism | Representative Experimental Results | Research Context |
|---|---|---|---|
| Quorum Sensing Inhibitors | AHL/LuxS systems, Quorum Sensing (QS) receptors [77] | A furanone compound (C-30) inhibited QS in P. aeruginosa, enhancing biofilm susceptibility to tobramycin by >100-fold in vitro [77]. | Disrupts cell-to-cell communication coordinating virulence and biofilm maturation. |
| c-di-GMP Pathway Inhibitors | Diguanylate Cyclases, Phosphodiesterases [77] [78] | Loss-of-function mutations in phosphodiesterase bmo in P. fluorescens led to high c-di-GMP, increased biofilm, and reduced motility [78]. | Targeting this pathway can force a switch from biofilm to planktonic lifestyle. |
| EPS Synthesis Inhibitors | Glucosyltransferases (Gtfs), Adhesins [77] | Myricetin and tt-farnesol inhibited GtfB in S. mutans, reducing exopolysaccharide synthesis and cariogenic biofilm assembly in vitro and in rodent models [77]. | Prevents initial biofilm formation and structural development. |
| Adhesin Blockers | FimH adhesin (in Uropathogenic E. coli) [77] | C-mannosides reduced bladder colonization of uropathogenic E. coli by 2-4 logs in a mouse UTI model [77]. | Prevents initial attachment, a critical first step in biofilm formation. |
| Natural Polyphenols | Bacterial membranes, Glucosyltransferases [79] | 17% cranberry juice (containing proanthocyanidins) inhibited growth and biofilm formation of multiple oral taxa (Veillonella parvula, Granulicatella adiacens) in an ex vivo shed oral biofilm model [79]. | Multi-target action; potential for reducing biofilm virulence without inducing resistance. |
Detailed Experimental Protocols for Key Assays
In Vitro Biofilm Dispersal Enzyme Assay
This protocol is adapted from studies evaluating glycoside hydrolases and proteases for disrupting pre-established biofilms [76].
- Biofilm Cultivation: Grow biofilms in flow cells or static microtiter plates. For Pseudomonas aeruginosa or Staphylococcus aureus, use a suitable medium like TSB or LB and incubate for 24-48 hours at 37°C to form mature biofilms.
- Enzyme Treatment: Gently wash the established biofilms with saline to remove non-adherent cells. Add the test enzyme (e.g., Dispersase, DNase I, Serine Protease) at a predetermined concentration (typically 0.1-100 µg/mL) in an appropriate buffer. Include a buffer-only negative control and a known biocide (e.g., 1% sodium hypochlorite) as a positive control.
- Incubation and Quantification: Incubate for 1-4 hours at 37°C. Quantify dispersal by:
- Crystal Violet (CV) Staining: Fix and stain remaining biofilm with 0.1% CV, elute with acetic acid, and measure absorbance at 595 nm to determine residual biomass.
- Viable Cell Counts: Treat the biofilm with enzyme, then vortex the substrate vigorously to dislodge remaining cells. Serially dilute the suspension and plate on agar to enumerate CFUs of dispersed and residual adherent cells.
- Microscopy: Use confocal laser scanning microscopy (CLSM) with live/dead staining (e.g., SYTO9/propidium iodide) to visualize biofilm architecture and cell viability pre- and post-treatment.
Bead Model for Experimental Evolution of Biofilms
This protocol, derived from the EvolvingSTEM project, is used to study biofilm adaptation and select for dispersal-enhanced mutants [78].
- Setup: Inoculate Pseudomonas fluorescens SBW25 into test tubes containing a sterile polystyrene bead and liquid growth medium.
- Evolutionary Cycling: Daily, aseptically transfer the biofilm-covered bead to a new tube containing fresh medium and a new sterile bead. This daily cycle selects for mutants proficient at dispersal from the old biofilm, travel through the liquid, and colonization of the new bead.
- Mutant Isolation and Analysis: After several cycles (e.g., 5-10 days), plate the biofilm community to isolate individual colonies with altered morphology (e.g., wrinkly, fuzzy). Sequence the genomes of these mutants to identify mutations in known biofilm regulators (e.g., wsp, yfiBNR, morA) or novel genes (e.g., bmo, a phosphodiesterase) [78].
The workflow for this experimental evolution model is outlined below.
Figure 2: Bead Model Workflow for Biofilm Evolution. This diagram illustrates the serial transfer protocol used to experimentally evolve biofilm-forming bacteria. The daily cycle of dispersal and re-colonization applies strong selective pressure for mutations that enhance fitness within the biofilm lifecycle, revealing key genetic pathways involved in adaptation [78].
The Scientist's Toolkit: Essential Research Reagents
Table 3: Key Reagents for Anti-Biofilm Research
| Reagent / Material | Primary Function in Research | Specific Application Examples |
|---|---|---|
| Polystyrene Beads/Plates | Provides a standardized, inert surface for in vitro biofilm formation. | High-throughput screening of anti-biofilm compounds in microtiter plates; experimental evolution studies in bead models [78]. |
| Flow Cell Systems | Enables real-time, microscopic observation of biofilm development under constant nutrient flow. | Studying biofilm architecture via CLSM; monitoring dispersal events in real-time [28]. |
| Recombinant Glycoside Hydrolases (e.g., Dispersin B) | Degrades specific exopolysaccharides (e.g., dPNAG) in the biofilm matrix. | Used as a positive control in dispersal assays; component of combination therapy studies with antibiotics [76]. |
| DNase I | Degrades extracellular DNA (eDNA), a key structural component of many biofilms. | Disrupting early-stage biofilms; studying the role of eDNA in matrix integrity and antibiotic binding [76]. |
| c-di-GMP Pathway Modulators | Small molecule inhibitors/activators of DGCs or PDEs to manipulate intracellular c-di-GMP. | Probing the role of c-di-GMP in the biofilm life cycle; forcing dispersal by artificially lowering c-di-GMP levels [77] [78]. |
| Live/Dead Bacterial Viability Kits (e.g., BacLight) | Fluorescent staining to distinguish live from dead cells in a biofilm. | Quantifying bactericidal effects of antimicrobials alone or in combination with dispersal agents via microscopy or flow cytometry [76]. |
The comparative data presented in this guide underscores that no single agent is a magic bullet for eradicating biofilms. Matrix-targeting enzymes like glycoside hydrolases and DNases offer high specificity and potency against pre-formed biofilms, while small molecules like QS inhibitors and c-di-GMP modulators provide a proactive approach to prevent biofilm maturation and virulence. The most promising strategy emerging from current research is combination therapy, where a dispersal agent is used to break down the biofilm's physical defenses and release dormant cells, followed by a conventional antibiotic to kill the now-vulnerable planktonic population [77] [76].
Future development must focus on translating in vitro success into clinical efficacy. This will require advanced in vivo models that accurately reflect the polymicrobial and host-factor-rich environments of chronic infections. Furthermore, overcoming the metabolic stability and delivery challenges of small-molecule inhibitors will be critical. As our understanding of the complex biology of persister cells and biofilm regulation deepens, particularly across different bacterial species, it will illuminate new targets and refine existing strategies, paving the way for a new generation of anti-biofilm therapeutics that can effectively combat chronic, recalcitrant infections.
Bacterial persisters represent a formidable challenge in the treatment of infectious diseases. These phenotypic variants are genetically susceptible to antibiotics but exist in a transient, dormant state that confers tolerance to conventional antimicrobial treatments [1]. Unlike antibiotic resistance, which involves genetic mutations that reduce drug efficacy, persistence operates through physiological dormancy, enabling bacterial survival during antibiotic exposure and subsequent regrowth once treatment ceases, leading to chronic and relapsing infections [1] [20]. The metabolic dormancy of persister cells renders them recalcitrant to most conventional antibiotics that target active cellular processes like cell wall synthesis, DNA replication, and protein translation [34].
The emerging strategy of using metabolites to "wake" persister cells from their dormant state represents a paradigm shift in combating persistent infections. This approach, often termed the "wake and kill" strategy, leverages our growing understanding of bacterial metabolism to reactivate persister cells, thereby sensitizing them to conventional antibiotics [20]. By exploiting the fundamental metabolic requirements of bacterial cells, researchers have identified specific metabolites that can reprogram persister metabolism, reverse antibiotic tolerance, and enhance killing efficacy. This comprehensive review examines the current state of metabolite-based approaches for eradicating bacterial persisters, comparing mechanisms, efficacy, and experimental methodologies across diverse bacterial species and antibiotic classes.
Comparative Analysis of Metabolic Stimulation Approaches
Central Metabolic Pathways as Therapeutic Targets
The metabolic state of bacterial cells profoundly influences their susceptibility to antibiotics. Research has demonstrated that bactericidal antibiotic efficacy correlates strongly with cellular metabolic activity, making metabolic reactivation a promising strategy for targeting dormant persisters [20]. The table below summarizes key metabolic pathways and their roles in persister cell resuscitation and antibiotic sensitization.
Table 1: Key Metabolic Pathways in Persister Cell Resuscitation and Antibiotic Sensitization
| Metabolic Pathway | Role in Persister Metabolism | Effect on Antibiotic Efficacy | Key Metabolites |
|---|---|---|---|
| Pyruvate Cycle (P Cycle) | Inactivated in antibiotic-resistant cells; reactivation increases NADH production and proton motive force [80] | Significantly enhances aminoglycoside uptake and killing [80] | Glucose, Alanine, Fructose, Pyruvate [80] |
| Tricarboxylic Acid (TCA) Cycle | Exhibits delayed labeling dynamics in persisters; peripheral pathways particularly affected [81] | Reactivation restores energy metabolism and antibiotic susceptibility [81] | Acetate, Succinate, Fumarate [81] |
| Electron Transport Chain | Reduced activity in persisters decreases proton motive force [82] | Increased activity enhances aminoglycoside uptake via proton motive force [80] [82] | Glucose, Amino Acids [82] |
| Stringent Response | Regulated by (p)ppGpp; maintains dormancy through toxin-antitoxin systems [20] | Reversal resensitizes cells to multiple antibiotic classes [20] | Nutrient metabolites [20] |
Metabolite-Specific Mechanisms and Efficacy Profiles
Different classes of metabolites exhibit distinct mechanisms for reactivating persister cells and sensitizing them to antibiotics. The efficacy of these metabolites varies depending on the bacterial species, antibiotic class, and environmental conditions. The following table provides a comparative analysis of metabolite classes and their specific effects on persister cells.
Table 2: Comparative Efficacy of Metabolite Classes Against Bacterial Persisters
| Metabolite Class | Specific Metabolites | Target Antibiotics | Bacterial Species | Proposed Mechanism | Efficacy (Fold Reduction in Survival) |
|---|---|---|---|---|---|
| Sugars | Glucose, Fructose, D-ribose [80] [82] | Aminoglycosides, Fluoroquinolones [80] [82] | S. aureus, E. coli, E. tarda [80] [82] | Activates P cycle, increases PMF and NADH [80] | 100-10,000× in vitro [80] |
| Amino Acids | Alanine, Glutamine, Arginine, Leucine, Lysine, Threonine, Glycine [80] | Aminoglycosides, β-lactams, Tetracyclines [80] | S. aureus, E. coli, V. alginolyticus [80] | Stimulates biosynthetic processes, enhances TCA cycle flux [80] [82] | Varies by species; up to 100× for S. aureus [82] |
| Nucleotides/Nucleobases | Adenosine, Guanosine, UMP [80] | Tetracyclines, Aminoglycosides [80] | E. coli, S. aureus [80] | Reverses stringent response, reactivates transcription [80] | Enhanced killing observed but not quantified [80] |
| Fatty Acids | Undecanoic acid, Lauric acid, N-tridecanoic acid [34] | Multiple classes [34] | S. aureus, P. aeruginosa, E. coli [34] | Disrupts membrane potential, reduces persister formation [34] | Significant reduction in persister formation [34] |
| Organic Acids | Fumarate, Pyruvate [80] | Aminoglycosides, Cephalosporins [80] | P. aeruginosa, E. coli [80] | Donates electrons to ETC, stimulates ROS production [80] [82] | Reverts resistant phenotype to sensitive [80] |
Experimental Approaches and Methodologies
Standardized Workflows for Metabolic Stimulation Studies
Research on metabolite-mediated persister sensitization employs carefully controlled experimental workflows to generate reproducible results. The following diagram illustrates a generalized protocol for evaluating metabolite-antibiotic combinations against bacterial persisters:
Diagram 1: Experimental workflow for evaluating metabolite-antibiotic combinations against bacterial persisters, showing core protocol and mechanistic analysis phases.
The Scientist's Toolkit: Essential Research Reagents
Implementing metabolite-based persister eradication strategies requires specific reagents and methodologies. The following table details essential research tools and their applications in this emerging field.
Table 3: Essential Research Reagents for Metabolite-Based Persister Studies
| Reagent Category | Specific Examples | Research Application | Key Function |
|---|---|---|---|
| Metabolic Inducers | 13C-labeled glucose, 13C-acetate, Alanine, Fructose, Fumarate [81] [80] | Isotopic tracing, Metabolic flux analysis [81] | Reprogram persister metabolism, enhance PMF [80] |
| Antibiotic Classes | Aminoglycosides, Fluoroquinolones, β-lactams [80] [82] | Efficacy assessment post-metabolic stimulation [82] | Target reactivated cellular processes [82] |
| Biosensors & Reporters | JE2-lux bioluminescent strain, ATP measurement assays, ROS-sensitive dyes [83] [82] | Real-time metabolic activity monitoring [83] | Quantitate bacterial metabolic state and response [83] |
| Analytical Platforms | LC-MS, GC-MS [81] | Metabolome profiling, 13C-labeling quantification [81] | Measure metabolite levels and metabolic fluxes [81] |
| Persister Induction Agents | CCCP, Rifampicin pretreatment, Nutrient starvation [81] [84] | Generate high-persistence populations [81] | Create experimental persister models [81] |
Molecular Mechanisms of Metabolic Reactivation
The process of metabolite-mediated persister sensitization involves complex interactions between metabolic pathways, stress responses, and antibiotic killing mechanisms. The following diagram illustrates the key signaling pathways and their interrelationships in this process:
Diagram 2: Signaling pathways in metabolite-mediated persister sensitization, showing how different metabolite classes activate metabolic processes that enhance antibiotic efficacy.
Species-Specific Variations in Metabolic Responses
Different bacterial species exhibit variations in their metabolic responses to stimulation, influenced by their unique physiological adaptations and environmental niches. The table below compares metabolic reactivation strategies across clinically relevant bacterial species.
Table 4: Species-Specific Metabolic Reactivation Profiles
| Bacterial Species | Most Effective Metabolites | Preferred Antibiotic Combinations | Species-Specific Mechanisms |
|---|---|---|---|
| Staphylococcus aureus | Glucose + Amino Acids, D-ribose [82] | Delafloxacin, Moxifloxacin, Aminoglycosides [82] | Nutrient stimulation increases DNA synthesis and ROS generation during FQ treatment [82] |
| Escherichia coli | Glucose, Alanine, Fructose [81] [80] | Aminoglycosides, β-lactams [80] | Redox state and membrane potential normalization via P cycle activation [80] |
| Pseudomonas aeruginosa | Fumarate, NADH, Nitrate [80] | Cefoperazone-sulbactam, Aminoglycosides [80] | Nitric oxide biosynthesis restoration; P cycle activation [80] |
| Mycobacterium tuberculosis | Pyruvate, Glucose [20] | Pyrazinamide, Rifampicin [20] | Membrane energetics disruption; Coenzyme A biosynthesis interference [20] |
| Vibrio alginolyticus | Glucose, Alanine [80] | Gentamicin, Tetracycline [80] | cAMP/CRP complex-dependent normalization of Na+-NQR system [80] |
The strategic use of metabolites to reverse antibiotic tolerance in bacterial persisters represents a promising approach to addressing the persistent infection crisis. The comparative analysis presented in this review demonstrates that metabolic stimulation, particularly through central carbon metabolism activators like glucose, alanine, and TCA cycle intermediates, can significantly enhance the efficacy of conventional antibiotics against dormant bacterial subpopulations across multiple species. The "wake and kill" strategy capitalizes on the fundamental relationship between bacterial metabolic state and antibiotic susceptibility, offering a pathway to overcome the limitations of current antimicrobial therapies.
While substantial progress has been made in understanding the mechanisms underlying metabolite-mediated persister sensitization, significant challenges remain in translating these findings into clinical applications. Future research directions should focus on optimizing metabolite delivery to infection sites, identifying species-specific metabolic vulnerabilities, and developing combination therapies that minimize resistance development. As our understanding of persister metabolism continues to evolve, metabolite-based adjuvant therapies hold immense potential for transforming the treatment of persistent bacterial infections and addressing the global antimicrobial resistance crisis.
The global health crisis of antimicrobial resistance (AMR) demands innovative therapeutic strategies. A significant challenge in treating bacterial infections is the presence of bacterial persisters—metabolically dormant, non-growing or slow-growing cells that survive antibiotic exposure without genetic resistance and contribute to chronic and relapsing infections [1] [14] [5]. While traditional antibiotics are effective against actively growing cells, they often fail to eradicate this persistent subpopulation. This guide compares the performance of therapeutic strategies that combine traditional antibiotics with non-traditional antimicrobials to target persisters, framing the discussion within the broader thesis of comparing persister formation mechanisms across bacterial species.
Comparative Analysis of Therapeutic Strategies
The table below summarizes the key combination therapy approaches, their mechanisms of action, and their performance against persister cells and biofilms.
Table 1: Comparison of Combination Therapy Strategies Targeting Bacterial Persisters
| Combination Strategy | Traditional Component | Non-Traditional Component | Proposed Mechanism of Action | Efficacy Against Persisters | Key Experimental Findings |
|---|---|---|---|---|---|
| Antibiotic + Anti-biofilm Agents | Standard-of-care antibiotics (e.g., Carbapenems) | Monoclonal antibodies, Phytochemicals [85] [86] | Disrupts extracellular polymeric substance (EPS) matrix, enhancing antibiotic penetration [14] | High for biofilm-associated persisters | Disruption of physical shelter and nutrient gradients that maintain persistence [14] |
| Antibiotic + Efflux Pump Inhibitors (EPIs) | Fluoroquinolones, Aminoglycosides | Peptide Nucleic Acids, specific phytochemicals [85] [86] | Reduces intracellular antibiotic concentration by blocking efflux pumps [85] [5] | Moderate | Can reverse one mechanism of transient tolerance; efficacy may vary with specific pump [5] |
| Collateral Sensitivity-Based Cycling | Antibiotic A | Antibiotic B | Exploits evolutionary trade-off where resistance to Drug A increases sensitivity to Drug B [87] | High potential to delay resistance | In S. aureus, alternating neomycin and ciprofloxacin significantly slowed resistance emergence [87] |
| Antibiotic + Metabolic Stimulators | Aminoglycosides | Carbon sources (e.g., Mannitol) | Awakens dormant persisters by stimulating metabolism, making them susceptible to antibiotics [5] | High in specific conditions | Effective in lab models; must be carefully timed with antibiotic administration [5] |
| Antibiotic + Phage Therapy | Last-resort antibiotics (e.g., Colistin) | Bacteriophages [85] [87] | Phages lyse persister cells by targeting cell wall structures, some rely on efflux pumps [87] | High for specific pathogens | Phage U136B relies on TolC efflux pump, selecting for its loss and re-sensitizing bacteria to antibiotics [87] |
Experimental Protocols for Evaluating Combination Therapies
Biphasic Killing Curve Assay
This is the gold-standard method for quantifying and isolating persister cells [1] [88].
- Culture Preparation: Grow a bacterial culture to the desired growth phase (mid-exponential or stationary).
- Antibiotic Exposure: Expose the culture to a lethal concentration of a single antibiotic or a combination. The concentration should be several times the minimum inhibitory concentration (MIC).
- Viable Count Monitoring: At regular time intervals (e.g., 0, 2, 4, 8, 24 hours), take aliquots from the culture.
- Washing and Dilution: Wash the aliquots to remove the antibiotic, then perform serial dilutions.
- Plating and Incubation: Plate the dilutions on antibiotic-free agar plates and incubate to allow viable cells to form colonies.
- Data Analysis: Plot the log of colony-forming units (CFU) per milliliter over time. A biphasic killing curve, characterized by an initial rapid decline in viability (killing of normal cells) followed by a plateau (survival of persisters), confirms persister presence [88]. The combination therapy's efficacy is measured by a continued decline in the plateau phase, indicating persister killing.
Checkerboard Synergy Assay
This protocol tests for synergistic interactions between two antimicrobial agents.
- Microtiter Plate Setup: Prepare a two-dimensional dilution series of the traditional antibiotic (e.g., along the rows) and the non-traditional agent (e.g., along the columns) in a 96-well microtiter plate containing growth medium.
- Inoculation: Inoculate each well with a standardized bacterial suspension.
- Incubation and Reading: Incubate the plate and measure bacterial growth using an optical density reader.
- Fractional Inhibitory Concentration (FIC) Calculation:
- FIC of Drug A = (MIC of Drug A in combination) / (MIC of Drug A alone)
- FIC of Drug B = (MIC of Drug B in combination) / (MIC of Drug B alone)
- ΣFIC = FIC of Drug A + FIC of Drug B
- Interpretation: ΣFIC ≤ 0.5 indicates synergy; >0.5 to 4 indicates indifference; and >4 indicates antagonism [87].
Visualizing Key Mechanisms and Workflows
Mechanisms of Persister Formation and Targeting
The following diagram illustrates the core mechanisms of bacterial persister formation and the corresponding targets for combination therapies.
Experimental Workflow for Combination Therapy
This diagram outlines a standardized experimental workflow for evaluating the efficacy of combination therapies against bacterial persisters.
The Scientist's Toolkit: Research Reagent Solutions
The table below details essential reagents and tools for researching persister cells and evaluating combination therapies.
Table 2: Key Research Reagents and Tools for Persister and Combination Therapy Studies
| Reagent/Tool | Function in Research | Specific Application Example |
|---|---|---|
| iChip / Microfluidics Device | Cultivation of unculturable bacteria in their natural environment [85] | Discovery of novel antimicrobials (e.g., Teixobactin) from previously inaccessible species [85] |
| ATP Assay Kits | Quantifying cellular ATP levels as a direct indicator of metabolic activity and dormancy [5] | Differentiating metabolically active cells from dormant persisters in a population after treatment |
| Reporter Strains (e.g., hipA7 E. coli) | Bacterial strains with mutations that lead to high persistence frequency for controlled studies [1] | Serving as a model system to screen for anti-persister compounds and combination therapies |
| Live/Dead Staining Kits (e.g., with SYTO9/PI) | Fluorescent differentiation between live and dead cells in a population using microscopy or flow cytometry | Visualizing and quantifying the proportion of surviving persister cells after antibiotic treatment |
| Patient-Derived Organoids (PDOs) | 3D ex vivo models that mimic the architecture and physiology of human organs and their microbiomes [89] [88] | Studying host-pathogen interactions and therapy efficacy in a more clinically relevant context than 2D cultures |
| Specific Toxin-Antitoxin System Mutants | Genetically engineered strains with deletions or knockouts of specific TA system components (e.g., hipBA, mqsRA) [14] [5] | Elucidating the precise role of individual TA modules in persister formation and awakening |
Combination therapies that synergize traditional antibiotics with non-traditional antimicrobials represent a promising frontier in the battle against persistent bacterial infections. The strategies outlined here—ranging from mechanistically direct approaches like biofilm disruption to evolutionarily informed ones like collateral sensitivity cycling—offer diverse tools to overcome the challenge of bacterial persistence. The experimental frameworks and tools provided will enable researchers to objectively compare the performance of these strategies. Advancing this field requires a deep understanding of the heterogeneous mechanisms of persister formation across species, which in turn will guide the rational design of more effective, relapse-preventing combination regimens.
Cross-Species Analysis: Validating Conserved and Unique Persistence Mechanisms
Bacterial persistence represents a formidable challenge in clinical settings, underlying recurrent infections and treatment failures. This phenomenon is defined by the presence of a small, genetically drug-susceptible subpopulation of bacteria that enters a transient, non-growing or slow-growing state to survive antibiotic exposure and other stresses [1]. Unlike stable antibiotic resistance, persistence is a reversible, phenotypic state where surviving cells can regrow once the stress is removed, exhibiting the same antibiotic susceptibility as the parent population [14] [1]. Toxin-Antitoxin (TA) modules have emerged as pivotal molecular systems governing this phenotypic switch. These ubiquitous genetic loci consist of a stable toxin that inhibits essential cellular processes and a labile antitoxin that neutralizes the toxin's activity [12] [90]. Under normal conditions, the antitoxin counteracts the toxin; however, during stress, accelerated antitoxin degradation or altered expression can lead to toxin activation, inducing growth arrest and facilitating persistence [12] [91]. This review systematically compares two paradigm systems—Escherichia coli and Staphylococcus aureus—in their utilization of specific TA modules, notably HipBA and MazEF, to elucidate the conserved and divergent strategies underlying bacterial persistence.
TA modules are classified into eight types (I-VIII) based on the nature and mode of action of the antitoxin [12]. Type I and II systems are the most extensively studied. Type I antitoxins are small RNAs that inhibit toxin translation by binding to the toxin's mRNA, whereas Type II antitoxins are proteins that form tight complexes with the toxin to neutralize its activity [14] [12]. The HipBA and MazEF systems discussed herein are both Type II TA modules.
These systems function as sophisticated stress response networks. When bacteria encounter unfavorable conditions, such as nutrient starvation or antibiotic insult, cellular proteases like Lon are activated, leading to the preferential degradation of the more labile antitoxin [14] [91]. This liberates the stable toxin to act on its intracellular target, which can include translation machinery, DNA replication, or cell wall synthesis, ultimately causing growth arrest and enabling the cell to survive the lethal stress [12] [90].
Table 1: Key Type II Toxin-Antitoxin Modules in E. coli and S. aureus
| TA Module | Toxin Function | Antitoxin Type | Primary Regulatory Role |
|---|---|---|---|
| HipBA (E. coli) | Kinase that phosphorylates EF-Tu, inhibiting translation [91] [18] | Protein (HipB) [14] | Post-segregational killing, persistence [91] |
| MazEF (E. coli) | Ribonuclease that cleaves mRNA [12] [91] | Protein (MazE) [12] | Stress-induced stasis, persistence [12] |
| RelBE (E. coli) | Ribonuclease that cleaves mRNA in a translation-dependent manner [18] | Protein (RelB) [18] | Stringent response, persistence [18] |
| TA Modules (S. aureus) | Varies (e.g., ribonucleases) [92] | Protein [92] | Biofilm formation, virulence, persistence [92] |
Comparative Analysis of TA Module-Mediated Persistence
Escherichia coli: A Model for HipBA and MazEF Function
E. coli has served as the primary model organism for elucidating the fundamental mechanisms of TA module operation and their link to persistence. The HipBA system is historically significant, as the hipA7 mutant was the first genetic element identified to confer a high-persistence (Hip) phenotype [1] [91]. This mutant, containing two amino acid substitutions (G22S and D291S), leads to a substantial increase in persister frequency without altering the minimum inhibitory concentration (MIC) of antibiotics, perfectly characterizing the persistence phenotype [14] [91]. The HipA toxin functions by phosphoryrating elongation factor Tu (EF-Tu), thereby disrupting translation and leading to growth arrest [18].
The MazEF system is another well-characterized module in E. coli. The MazF toxin is an endoribonuclease that cleaves cellular mRNAs at specific sequences, leading to a rapid halt in protein synthesis [12] [91]. This system is intricately linked to the stringent response. Stress-induced signals, such as the accumulation of guanosine tetraphosphate (ppGpp), can trigger MazF activation, promoting a dormant state [14]. Furthermore, the complex autoregulation of TA modules like MazEF and RelBE through conditional cooperativity—where the toxin acts as a co-repressor or de-repressor of its own operon depending on the toxin-to-antitoxin ratio—adds a layer of sophisticated control that prevents inadvertent toxin activation while allowing rapid response to stress [18].
Staphylococcus aureus: Distinctive Persistence and TA Module Roles
In contrast to E. coli, S. aureus employs persistence strategies that are notably influenced by its role as a major human pathogen. While TA modules are present and functional in S. aureus, their direct implication in antibiotic persistence appears to be more complex and potentially less pronounced than in E. coli [92]. Evidence suggests that the absence of certain TA modules in S. aureus does not consistently affect persister levels, indicating redundancy or the involvement of alternative mechanisms [14] [92].
S. aureus exhibits a strong propensity to form Small Colony Variants (SCVs), which are a specific type of persister with an altered, slow-growing morphology [92]. SCVs are frequently associated with chronic and recurrent infections, such as bovine mastitis and human device-related infections, due to their ability to persist within host cells and evade antibiotic therapy [92]. Recent research has highlighted the critical role of energy metabolism in S. aureus persisters. Studies isolating pure populations of S. aureus persisters induced by vancomycin or enrofloxacin have shown that maintaining cellular ATP levels and balanced reactive oxygen species (ROS) production are key to their survival [93]. This suggests that metabolic regulation, potentially alongside TA systems, is a cornerstone of persistence in this pathogen.
Table 2: Comparative Features of Persistence in E. coli and S. aureus
| Feature | Escherichia coli | Staphylococcus aureus |
|---|---|---|
| Model TA System | HipBA, MazEF [91] [18] | Multiple, but less characterized [14] [92] |
| Key Persistence Mechanism | Toxin-mediated growth arrest (translation inhibition) [91] [18] | Metabolic remodeling, SCV formation, and potential TA involvement [92] [93] |
| Link to Biofilm | Well-established; biofilm shelters persisters [14] | Strongly associated; biofilm is a key persistence niche [92] |
| Role of Stringent Response | Strong link via ppGpp and (p)ppGpp signaling [14] | Implied, but less explicitly documented than in E. coli |
| Metabolic State of Persisters | Reduced but active energy metabolism; TCA cycle and ETC critical [60] | Active energy management; ATP maintenance crucial [93] |
| Single-Cell Observations | Heterogeneous; persisters can be derived from growing cells [94] | Formation of distinct SCV morphologies [92] |
Essential Experimental Methodologies for Persister Research
Persister Isolation and Enrichment Protocols
A foundational challenge in persistence research is the isolation of a pure persister population for downstream analysis. A validated protocol for S. aureus involves treating a stationary-phase culture with a high concentration of antibiotic (e.g., 10x MIC) for a defined period (e.g., 24 hours) to kill the susceptible population. The surviving cells, enriched for persisters, are then collected by centrifugation and washed to remove the antibiotic [93]. For E. coli, a similar approach is used, often employing drugs like ampicillin or ciprofloxacin. The use of microfluidic devices, such as the membrane-covered microchamber array (MCMA), has revolutionized the field by allowing for long-term, single-cell observation and tracking of persister formation and resuscitation dynamics [94].
Assessing Persister Frequency: Killing Curve Assays
The gold standard for quantifying persisters is the time-kill curve assay. In this experiment, a bacterial culture is exposed to a lethal dose of a bactericidal antibiotic. Samples are taken at regular intervals, serially diluted, and plated on antibiotic-free medium to enumerate viable colony-forming units (CFU) over time. A biphasic killing curve, characterized by an initial rapid decline in CFU followed by a much slower decline, is the hallmark of a population containing persisters. The surviving fraction after 24 hours is typically reported as the persister frequency [14] [94].
Molecular Characterization: Proteomics and Metabolomics
Advanced omics technologies are critical for dissecting the molecular state of persisters. Proteomic profiling via mass spectrometry can identify protein abundance changes between normal and persister cells. For instance, studies on S. aureus have revealed distinct protein profiles in vancomycin-induced versus enrofloxacin-induced persisters, pointing to different underlying survival mechanisms [93]. Metabolomic analysis provides a snapshot of the metabolic network activity. Research on E. coli has shown that the global regulator Crp/cAMP redirects persister metabolism away from anabolism towards oxidative phosphorylation, underscoring the importance of the TCA cycle and electron transport chain for persister survival [60].
Visualization of Pathways and Workflows
HipBA TA Module Regulation and Induction of Persistence
Experimental Workflow for Persister Isolation and Characterization
The Scientist's Toolkit: Key Research Reagents and Solutions
Table 3: Essential Reagents for Persistence Research
| Reagent / Solution | Function in Research | Specific Application Example |
|---|---|---|
| Microfluidic Devices (MCMA) | Enables long-term, single-cell imaging and tracking of persister dynamics in a controlled environment [94]. | Observing E. coli persister cell histories and resuscitation after ampicillin treatment [94]. |
| Lon Protease Inhibitor | Inhibits the protease responsible for antitoxin degradation; used to test the dependency of persistence on specific TA systems [14]. | Validating the role of Lon in HipB degradation and HipA-mediated persistence in E. coli [14]. |
| BacTiter-Glo Assay Kit | Measures intracellular ATP levels as a indicator of metabolic activity and cell viability in persister populations [92] [93]. | Quantifying ATP in S. aureus persisters to confirm active energy maintenance despite dormancy [93]. |
| TRIzol LS Reagent | For RNA isolation from bacterial samples, preserving RNA integrity for transcriptional analysis [92]. | Extracting RNA from S. aureus persisters for RT-qPCR to quantify gene expression (e.g., TA module genes) [92]. |
| cAMP / Crp Modulators | Chemicals that alter intracellular cAMP levels or disrupt Crp function; used to study metabolic rewiring in persisters [60]. | Investigating the role of the Crp/cAMP regulon in directing E. coli persister metabolism towards oxidative phosphorylation [60]. |
The comparative analysis of E. coli and S. aureus reveals a fascinating dichotomy in the implementation of TA module-mediated persistence. E. coli serves as a paradigm where specific, well-characterized TA systems like HipBA and MazEF play a direct and demonstrable role in generating growth-arrested persister cells through mechanisms like translation inhibition. In contrast, S. aureus appears to employ a more multifaceted strategy where classical TA modules may work in concert with other adaptations, such as the SCV phenotype and sophisticated metabolic reprogramming, to achieve persistence.
This mechanistic divergence has profound implications for therapeutic development. Targeting a single, central TA system might be a viable strategy against pathogens like E. coli. However, for pathogens like S. aureus, effective anti-persister therapies will likely require a multi-pronged approach that disrupts metabolic hubs, such as the TCA cycle or ATP synthase, in addition to targeting TA modules. Future research should focus on further elucidating the interconnected networks of stress response, TA system activation, and metabolic control across different bacterial species to identify the most vulnerable nodes for eradicating persistent infections.
Pseudomonas aeruginosa establishes recalcitrant chronic infections in the lungs of cystic fibrosis (CF) patients, serving as a primary driver of morbidity and mortality. The remarkable resilience of this pathogen is attributed to its ability to form biofilms and undergo genetic adaptation leading to the emergence of high-persister (hip) mutants [95] [96]. These adaptations create a perfect storm for therapeutic failure. While planktonic P. aeruginosa may show susceptibility to antibiotics in standard laboratory tests, the same drugs often fail to eradicate the infection in the CF lung [95] [97]. This clinical paradox has focused research on understanding the unique biology of biofilms and persister cells—dormant, phenotypic variants that exhibit extreme antibiotic tolerance without genetic resistance [95] [98]. This review objectively compares the mechanisms of persister formation and biofilm adaptation in P. aeruginosa, framing these processes within the broader context of bacterial persistence research. We synthesize key experimental data and methodologies to provide a resource for researchers and drug development professionals tackling this persistent challenge.
Comparative Mechanisms of Biofilm and Persister-Mediated Tolerance
The survival of P. aeruginosa in the CF lung is facilitated by a multi-layered strategy of tolerance and resistance, primarily orchestrated through biofilm formation and the presence of persister cells. Understanding the distinction and interplay between these mechanisms is crucial.
Biofilm-Specific Tolerance Mechanisms
The biofilm mode of growth protects bacteria through a combination of physical, physiological, and genetic factors [97] [99]. The extracellular polymeric substance (EPS) matrix, comprising exopolysaccharides (Pel, Psl, alginate), proteins, extracellular DNA (eDNA), and lipids, creates a physical barrier that can retard antibiotic diffusion and sequester certain drug classes [97] [100]. For instance, cationic aminoglycosides like tobramycin interact with anionic eDNA, while neutral antibiotics like ciprofloxacin penetrate more readily [97] [96].
Within the biofilm, gradients of nutrients and oxygen generate metabolic heterogeneity [98] [97]. This results in subpopulations of metabolically inactive or dormant cells, particularly in the deeper layers of the biofilm, which are inherently more tolerant to antibiotics that target active cellular processes [98]. This dormant state is further reinforced by activation of core molecular pathways, including the stringent response (mediated by (p)ppGpp), the SOS response to DNA damage, and the activity of Toxin-Antitoxin (TA) systems [98]. These systems collectively shut down metabolism and growth, promoting survival under stress.
High-Persister (hip) Mutants
Persisters are dormant phenotypic variants that exist within a larger, susceptible population. They are not mutants in the traditional sense, but the frequency at which cells enter this persistent state can be increased by mutations, creating high-persister (hip) mutants [95]. These mutants stably produce elevated levels of drug-tolerant cells and have been isolated from CF patients after long-term infection and antibiotic pressure [95]. A critical study found that late isolates from a majority of CF patients (10 out of 15 tested) were hip mutants, and this increased persister formation was their primary survival mechanism, often without a concomitant increase in conventional antibiotic resistance [95]. The selection of hip mutants during chemotherapy appears to be a key culprit in the recalcitrance of chronic CF infections [95].
Table 1: Key Characteristics of Biofilm vs. Persister-Mediated Tolerance
| Feature | Biofilm-Mediated Tolerance | Persister-Mediated Tolerance (hip mutants) |
|---|---|---|
| Nature | Population-level, structured community | Subpopulation of dormant, phenotypic variants |
| Primary Cause | Physical barrier, metabolic heterogeneity, matrix | Increased frequency of entry into dormant state due to mutation |
| Genetic Basis | Biofilm-specific gene expression (e.g., brlR, ndvB) | Mutations in global regulators or persistence genes (e.g., mutS, hipA homologs) |
| Reversibility | Dispersal returns cells to planktonic state | Phenotype is temporary for a cell, but frequency is heritable |
| Impact on MIC | No change in MIC of dispersed cells | No change in MIC [95] |
| Clinical Evidence | Observed in microcolonies in CF lungs [96] | Late CF isolates form more persisters than early isolates [95] |
Quantitative Data and Experimental Evidence
Comparative Analysis of hip Mutants
Direct evidence from longitudinal studies of CF isolates confirms the in vivo selection of hip mutants. One seminal study compared a clonal pair of early and late isolates from a single CF patient, demonstrating a dramatic increase in persister levels over time [95].
Table 2: Experimental Data from a Clonal Pair of P. aeruginosa CF Isolates [95]
| Parameter | Early Isolate (AMT0023-30) | Late Isolate (AMT0023-34) | Notes |
|---|---|---|---|
| Patient Age at Isolation | 0.5 years | 8.0 years (96 months) | - |
| Persister Level | Baseline (Reference) | ~100-fold increase | Across exponential, stationary, and biofilm populations |
| Mutational Status | Wild-type | Hypermutator (mutS mutation) and mexZ mutation | - |
| MIC (Ofloxacin) | 1 µg/mL | 8 µg/mL | Moderate increase due to MexXY-OprM pump overexpression |
| MIC (Tobramycin) | 1.0 µg/mL | 32.0 µg/mL | - |
| MIC (Carbenicillin) | 64 µg/mL | 128 µg/mL | - |
| Impact of mexXY Knockout | - | Restored ofloxacin and tobramycin MIC to parental level; did not affect high persister levels | Confirming hip phenotype is independent of efflux pump mutation |
Evolution of Resistance from Persister Cells
Persister cells not only survive antibiotic treatment but can also serve as a reservoir for the emergence of resistant mutants. Experimental evolution studies tracking P. aeruginosa PA14 under lethal meropenem pressure have illuminated this pathway [101].
Table 3: Evolutionary Pathway to High-Level Resistance from Persister Cells [101]
| Serial Passage Stage | Observed Mutations | Antibiotic Resistance Profile | Population Survival |
|---|---|---|---|
| Initial Passages | Various low-level resistance mutations | Low-level meropenem resistance | Increasing |
| Intermediate Passages | Mutations in the oprD porin gene | Increased meropenem resistance (4–32-fold MIC increase) | High |
| Later Passages | Mutations in mexR (derepressing MexAB-OprM efflux pump) | High-level meropenem resistance and collateral resistance to ciprofloxacin | Very High |
The Scientist's Toolkit: Key Research Reagents and Solutions
Advancing research in this field relies on a standardized set of tools and assays. The table below details essential materials and their applications based on cited experimental approaches.
Table 4: Essential Research Reagents and Experimental Solutions
| Reagent / Solution | Primary Function in Research | Exemplary Use Case |
|---|---|---|
| Cation-Adjusted Mueller-Hinton Broth (CAMHB) | Standardized medium for antimicrobial susceptibility testing (MIC determination) | CLSI-standard broth microdilution assays [101] |
| Luria-Bertani (LB) Medium | General-purpose medium for routine bacterial culture and maintenance | Growing overnight cultures for killing assays and experimental evolution [95] [101] |
| Synthetic Cystic Fibrosis Sputum Medium (SCFM2) | In vitro simulation of the CF lung environment for more clinically relevant biofilm studies | Assessing biofilm control efficacy of phages or antibiotics under CF-like conditions [102] |
| Crystal Violet Stain | Quantitative and qualitative assessment of biofilm biomass | Tissue Culture Plate (TCP) method for biofilm quantification [103] |
| Glacial Acetic Acid | Solubilizes crystal violet stain bound to biofilm for spectrophotometric reading | Modified Tissue Culture Plate (MTCP) method, enhancing accuracy [103] |
| DNase I | Degrades extracellular DNA (eDNA), a key component of the biofilm matrix | Studying matrix contribution to tolerance; can increase antibiotic penetration [96] |
| Clodronate Liposomes | Depletes monocytes/macrophages in vivo | Elucidating the role of specific immune cells in host response to biofilm infections [104] |
| Anti-Ly6G Antibodies | Depletes neutrophils in vivo | Investigating the critical protective role of neutrophils in murine infection models [104] |
Detailed Experimental Protocols for Key Assays
Protocol for Identification of High-Persister (hip) Mutants
Objective: To isolate and characterize P. aeruginosa variants that produce elevated levels of antibiotic-tolerant persister cells [95].
Methodology:
- Culture and Inoculum Preparation: Grow the bacterial strain of interest to mid-exponential phase in a suitable broth like Mueller-Hinton Broth (MHB).
- Antibiotic Killing Assay: Expose the culture to a high concentration of a bactericidal antibiotic (e.g., 50x MIC of a fluoroquinolone like ofloxacin). Ensure the concentration is sufficient to kill all planktonic, non-persister cells.
- Viability Counting: At designated time points (e.g., 0, 4, 8, 24 hours), remove aliquots, wash to remove the antibiotic, serially dilute, and plate on non-selective agar. Incubate plates and count Colony Forming Units (CFUs). The surviving population after prolonged exposure represents the persister fraction.
- Selection of hip Mutants: Subject a mutagenized population to periodic, high-dose antibiotic treatments. The surviving populations are regrown and the killing assay is repeated. Isolates that consistently show a significantly higher fraction of surviving cells compared to the wild-type parent strain are classified as hip mutants.
- Characterization: Confirm the hip phenotype by performing killing assays on exponential phase, stationary phase, and biofilm populations of the candidate mutant. Determine MICs to verify that tolerance is not due to conventional resistance.
Protocol for In Vitro Experimental Evolution of Resistance
Objective: To track the emergence of antibiotic resistance mutations in bacterial populations derived from persister cells under lethal antibiotic pressure [101].
Methodology:
- Initial Persister Isolation: Grow a wild-type strain (e.g., PA14) to mid-exponential phase. Treat with a lethal dose of antibiotic (e.g., 8 µg/mL meropenem) for a set period (e.g., 6 hours).
- Processing Survivors: Centrifuge the culture in a protective medium like 0.3 M sucrose to remove dead cell debris. Resuspend the surviving persister cells in fresh medium and allow them to recover and regrow.
- Serial Passage and Selection: Plate an aliquot of the revived culture on agar containing the antibiotic at various concentrations to determine the rate of resistant mutants. Use the remaining culture to initiate the next round of lethal antibiotic treatment. Repeat this process for multiple passages.
- Monitoring and Analysis: After each passage, track population survival (CFU counts) and the MIC of the antibiotic. Once the population evolves to survive the initial lethal dose, whole-genome sequence the evolved populations or individual resistant clones to identify accumulated mutations (e.g., in oprD or mexR).
Protocol for Modified Tissue Culture Plate (MTCP) Biofilm Assay
Objective: To quantitatively measure the biofilm-forming capacity of bacterial clinical isolates with enhanced sensitivity [103].
Methodology:
- Biofilm Formation: Inoculate a standardized bacterial suspension into the wells of a sterile, flat-bottomed tissue culture plate containing growth medium. Incubate statically for a specified time (e.g., 24-48 hours) to allow biofilm adhesion and growth.
- Biofilm Staining: Carefully remove the planktonic cells and rinse the wells with phosphate-buffered saline (PBS) to remove non-adherent bacteria. Fix the adherent biofilm with an appropriate fixative and then stain with a 0.1% crystal violet solution.
- Solubilization and Quantification: After rinsing off excess stain, treat the wells with 33% glacial acetic acid (e.g., 160 µL for 15 minutes) to solubilize the crystal violet bound to the biofilm.
- Spectrophotometric Reading: Transfer the solubilized dye to a new plate and measure the Optical Density (OD) at 570 nm using a microtiter plate reader. The OD value is proportional to the biofilm biomass. Classify isolates as non-, weak, moderate, or strong biofilm producers based on calculated cut-off OD values.
Visualizing Key Concepts and Pathways
Biofilm Heterogeneity and Persister Formation Pathways
The following diagram synthesizes the key environmental stresses within a P. aeruginosa biofilm and the major molecular pathways they activate, leading to the generation of persister cells.
Experimental Workflow for hip Mutant Selection and Analysis
This diagram outlines a standard experimental workflow for selecting and characterizing high-persister (hip) mutants from a bacterial population, as derived from the cited methodologies.
Tuberculosis (TB) treatment is notoriously prolonged and complex, primarily due to the remarkable ability of Mycobacterium tuberculosis (M. tuberculosis) to enter a non-replicating, drug-tolerant state. This phenotypic heterogeneity, rather than classic genetic resistance, underpins the need for multi-drug regimens lasting at least six months. A small subpopulation of bacterial cells, known as persisters, can survive antibiotic exposure by becoming metabolically dormant or shifting their metabolic state, thus escaping the lethal action of drugs that typically corrupt active cellular processes [55] [1]. Understanding the metabolic adaptations of M. tuberculosis is therefore critical for improving therapeutic strategies.
Among the first-line TB drugs, Pyrazinamide (PZA) holds a unique position due to its exceptional ability to target these non-replicating persister cells, thereby playing a crucial role in shortening therapy duration [105]. This guide provides a comparative analysis of the metabolic shifts associated with M. tuberculosis persister formation and the specific action of PZA. It synthesizes current experimental data and protocols to offer a resource for researchers and drug development professionals working to overcome the challenge of bacterial persistence in chronic infections.
Metabolic Basis ofM. tuberculosisPersister Formation
Persister cells are characterized by their transient, non-heritable tolerance to antibiotics. They are not mutants; instead, they represent a phenotypic variant of the wild-type population that enters a dormant or slow-growing state [1] [4]. In M. tuberculosis, this state is strongly linked to a low-energy cellular profile, which is achieved through distinct metabolic remodeling.
The Low-Energy Persister State
A seminal study demonstrated a direct causal link between low intracellular ATP levels and antibiotic tolerance in M. tuberculosis. Using a FRET-based ATP biosensor (ATeam1.03YEMK), researchers showed that:
- Sorted low-ATP cells exhibited significantly greater survival after 72 hours of treatment with rifampicin or streptomycin compared to high-ATP cells from the same culture [55].
- Artificially lowering ATP levels with a short, high-dose pretreatment of bedaquiline (an ATP synthase inhibitor) increased the population's tolerance to subsequent challenges with rifampicin/streptomycin or isoniazid [55].
- The formation of these low-ATP persisters is driven by stochastic noise (natural variation) in the expression of energy-generating enzymes. For instance, when grown on acetate, cell-to-cell variation in acetate kinase (AckA) mRNA levels was observed. Quenching this noise by overexpressing ackA dramatically reduced persister formation, identifying it as a key "persister gene" under these conditions [55].
Metabolic Remodeling in Biofilm-Derived Persisters
An in vitro biofilm model of M. tuberculosis persister-like bacilli (PLB) has provided deep insights into specific metabolic rewiring. Isotopic metabolomics profiling revealed a critical trehalose-catalytic shift in these cells [106].
- In replicating cells, trehalose is primarily used for the biosynthesis of cell surface glycolipids (trehalose monomycolate - TMM and trehalose dimycolate - TDM).
- In PLB, trehalose metabolism is redirected. The enzyme TreS converts trehalose to maltose, which is subsequently funneled into central carbon metabolism (CCM), including glycolysis and the pentose phosphate pathway [106].
- This shift away from cell wall synthesis and towards CCM helps maintain baseline levels of ATP and antioxidants (e.g., glutathione), enabling survival during antibiotic-induced stress. A TreS deficiency (ΔtreS) significantly impaired the formation of drug-tolerant persisters [106].
The following diagram illustrates the stark metabolic contrast between actively replicating M. tuberculosis and persister cells.
Comparison of Persister Formation Mechanisms:M. tuberculosisvs.E. coli
While a low-energy state is a common theme in bacterial persistence, the mechanisms and their consistency across species vary, as shown in the table below.
Table 1: Comparison of Persister Formation Mechanisms in M. tuberculosis and E. coli
| Aspect | M. tuberculosis | E. coli |
|---|---|---|
| Primary Metabolic Driver | Noise in energy metabolism (e.g., AckA); Trehalose-catalytic shift to sustain CCM [55] [106] | Toxin-Antitoxin (TA) systems inducing dormancy (e.g., MqsR, TisB) [4] |
| Energy State of Persisters | Demonstrably low ATP; direct correlation between low ATP and survival [55] | Low ATP; toxins like TisB reduce proton motive force and ATP [4] |
| Phenotypic Consistency | Drug-specific mechanisms suggested by studies in other bacteria [107] | Lack of correlation in persister fractions across different antibiotics, even with similar modes of action [107] |
| Key Experimental Evidence | FRET-based ATP biosensing; metabolomics of biofilm persisters [55] [106] | Mutant studies (e.g., hipA7); deletion of multiple TA loci reduces persisters [4] [107] |
Pyrazinamide: The Anti-Persister Drug
Unique Characteristics and Mechanism of Action
Pyrazinamide is a cornerstone of modern TB therapy because it uniquely targets persister populations that other drugs miss.
- Prodrug Activation: PZA is a prodrug that requires conversion to its active form, pyrazinoic acid (POA), by the bacterial enzyme pyrazinamidase (PZase) encoded by the pncA gene [105].
- Multi-Target Action: Unlike most antibiotics, PZA does not have a single primary target. Evidence suggests it disrupts multiple cellular processes essential for persister survival, including:
Its ability to kill non-replicating persisters is what allows TB therapy to be shortened from 9-12 months to 6 months [105] [108].
Resistance Mechanisms and Susceptibility Testing
Resistance to PZA primarily arises from mutations that disrupt its activation.
- pncA Mutations: The most common mechanism involves mutations in the pncA gene, which impair PZase activity and prevent conversion of PZA to POA [105].
- Alternative Resistance Mechanisms: Mutations in the drug target ribosomal protein S1 (rpsA) and the pantothenate/coenzyme A biosynthesis gene panD have also been identified in some PZA-resistant strains, suggesting a complex resistance landscape [105] [108].
A significant challenge in the clinic has been the unreliable nature of phenotypic PZA susceptibility testing, which traditionally requires acidic conditions (pH ~5.5) that are suboptimal for M. tuberculosis growth and can lead to high rates of false resistance [108] [109]. A novel approach using broth microdilution at a neutral pH of 6.8 in a defined culture medium has been developed to overcome this limitation. This method reliably determines the Minimum Inhibitory Concentration (MIC) of PZA, with values for clinical isolates ranging from ≤12.5 to 100 μg/mL [108] [109]. The workflow of this improved assay is detailed below.
Comparative Experimental Data and Protocols
This section consolidates key quantitative findings and methodologies from recent research to facilitate direct comparison and experimental replication.
Key Experimental Findings on Persister Metabolism and PZA
Table 2: Summary of Key Experimental Data on M. tuberculosis Persisters and PZA
| Experimental Focus | Key Finding | Quantitative Data / Range | Significance |
|---|---|---|---|
| ATP Level & Persistence [55] | Low-ATP cells are multidrug tolerant. | Sorted low-ATP cells showed significant survival at 72h vs. elimination of high-ATP cells. | Establishes a direct causal link between low energy and the persister phenotype. |
| ackA Overexpression [55] | Quenching metabolic noise reduces persisters. | Overexpression sharply decreased persister formation. | Identifies a specific metabolic gene as a key node in persister formation. |
| PZA MIC at Neutral pH [108] [109] | Reliable MIC testing in defined medium at pH 6.8. | MICs for clinical isolates ranged from ≤12.5 to 100 μg/mL. | Provides a more accurate and reliable method for PZA susceptibility testing. |
| Trehalose Metabolic Shift [106] | TreS-mediated shift fuels central metabolism in PLB. | ΔtreS mutant had ~2 log₁₀ reduction in persister formation. | Identifies a critical adaptive metabolic pathway for survival under stress. |
Detailed Experimental Protocol: Broth Microdilution for PZA MIC
The following is a detailed protocol based on the novel neutral pH method [108] [109]:
- Strain Preparation: Use fresh M. tuberculosis cultures (from 7H10 or 7H11 agar plates) no older than 4 weeks.
- Inoculum Standardization:
- Suspend growth in PZA DST buffer (containing 5.0 mL/L glycerol and 0.025% Tween 80).
- Adjust the suspension turbidity to match a 0.5 McFarland standard.
- Perform a 1:50 dilution in the same buffer to achieve a final inoculum density of ~1.0–5.0 × 10⁵ CFU/mL.
- Plate Inoculation:
- Use a dry-format 96-well PZA DST plate with PZA concentrations typically ranging from 12.5 to 800 μg/mL, plus a no-drug control.
- Inoculate each well with 200 μL of the diluted bacterial suspension.
- Incubation and Reading:
- Seal plates with sterile sealing foils and incubate at 37°C for up to 14 days.
- The MIC is determined as the lowest concentration of PZA that prevents visible growth. Incorporating a fluorescence-based growth indicator can enhance reading accuracy by overcoming issues with turbidity and clumping.
The Scientist's Toolkit: Key Research Reagents and Materials
Table 3: Essential Research Reagents for Studying M. tuberculosis Persisters and PZA Action
| Reagent / Material | Function / Application | Example Use Case |
|---|---|---|
| ATeam1.03YEMK Biosensor | FRET-based measurement of intracellular ATP levels in single cells. | Quantifying ATP heterogeneity and sorting low-ATP persister populations [55]. |
| Defined Culture Medium (pH 6.8) | Supports M. tuberculosis growth for PZA MIC testing at neutral pH. | Reliable phenotypic determination of PZA susceptibility, overcoming false resistance [108]. |
| Bedaquiline | Inhibits F1Fo ATP synthase, reducing bacterial ATP levels. | Experimental induction of a low-energy state to study its link to antibiotic tolerance [55]. |
| Dry-Format PZA DST Plate | Pre-made microdilution plate with PZA concentration gradient at neutral pH. | Standardized high-throughput PZA susceptibility testing [108] [109]. |
| ΔtreS Mutant Strain | Trehalose synthase-deficient M. tuberculosis. | Investigating the role of the trehalose-catalytic shift in persister formation and drug tolerance [106]. |
The battle against tuberculosis is fundamentally a battle against the remarkable resilience and metabolic plasticity of M. tuberculosis. The evidence is clear: stochastic formation of low-energy persister cells through metabolic noise and reprogramming is a key contributor to treatment difficulty. The trehalose-catalytic shift represents a sophisticated adaptive mechanism that maintains vitality in a dormant state.
Pyrazinamide stands as a model anti-persister drug, and its unique role highlights the importance of targeting bacterial metabolism for improved therapeutic outcomes. The development of more reliable susceptibility testing methods, such as broth microdilution at neutral pH, is a significant step forward for both clinical management and antimicrobial research.
Future research should focus on exploiting these vulnerabilities. Combining PZA with other drugs that disrupt the trehalose shift or other persister-specific metabolic pathways represents a promising avenue for novel adjunctive therapies. Furthermore, the differences in persister formation mechanisms across bacterial species suggest that while the dormant phenotype is universal, the specific paths to dormancy are varied. This underscores the need for pathogen-specific persistence research to develop truly effective treatments for chronic and biofilm-associated infections.
Salmonella enterica serovar Typhimurium employs sophisticated intracellular survival strategies to establish persistent infections, posing significant challenges for antimicrobial therapy. Recent research has identified the sulfur transferase complex—encoded by yheM, yheL, yheN, trmU, and yhhP—as a critical metabolic hub coordinating bacterial persistence within macrophages. This complex regulates tRNA thiolation and bacterial metabolism, influencing reactive nitrogen species (RNS) accumulation, (p)ppGpp-mediated stringent response, and energy generation. Disruption of this complex paradoxically increases antibiotic persistence through metabolic reprogramming. This review comprehensively compares the molecular mechanisms through which the sulfur transferase complex governs intramacrophage survival and persistence, providing a framework for developing novel anti-persister therapeutic strategies.
Bacterial persisters represent a transient, phenotypically variant subpopulation capable of surviving lethal antibiotic exposure without genetic resistance mutations. These dormant or slow-growing cells contribute significantly to chronic and recurrent infections, as they withstand antimicrobial therapy and subsequently resuscitate when treatment ceases [1]. For intracellular pathogens like Salmonella, macrophages serve as crucial sanctuaries for persister formation, where bacteria encounter diverse stress conditions including nutrient limitation, acidic pH, and antimicrobial peptides [110] [111].
The sulfur transferase complex has recently emerged as a key regulator of bacterial persistence, functioning at the intersection of metabolic adaptation and stress response. This complex facilitates the 2-thiolation of 5-methylaminomethyl-2-thiouridine (mnm⁵s²U³⁴) at the wobble position of specific tRNAs, fine-tuning translation efficiency under stress conditions [110] [111]. This review systematically compares the mechanisms through which this complex influences Salmonella intramacrophage survival and persistence, integrating recent experimental findings to provide a comprehensive resource for researchers and drug development professionals.
The Sulfur Transferase Complex: Structure, Function, and Genetic Determinants
Genetic Components and Molecular Architecture
The sulfur transferase complex in Salmonella Typhimurium comprises five core genes (yheM, yheL, yheN, trmU, and yhhP) that function coordinately in tRNA modification. Structural and functional analyses indicate these genes encode enzymes responsible for the biosynthesis and transfer of sulfur groups to specific tRNA targets, particularly those for glutamate, glutamine, and lysine [110] [111]. This modification optimizes translational accuracy and efficiency, especially for stress-responsive proteins.
Functional Role in Cellular Physiology
The complex catalyzes the 2-thiolation of 5-methylaminomethyl-2-thiouridine (mnm⁵s²U³⁴) at the wobble position (U34) of specific tRNAs. This modification enhances translational fidelity under stress conditions by stabilizing codon-anticodon interactions and preventing frameshift errors [110]. The absence of this modification triggers pleiotropic effects including metabolic reprogramming, altered stress response, and reduced translational accuracy during macrophage infection.
Table 1: Genetic Components of the Sulfur Transferase Complex in Salmonella
| Gene | Function | Phenotype of Deletion Mutant |
|---|---|---|
| yheM | Sulfur transfer component | Increased intramacrophage persistence, elevated RNS, reduced ATP |
| yheN | Sulfur transfer component | Enhanced persister formation, increased non-replicating cells |
| trmU | tRNA modification enzyme | Elevated (p)ppGpp levels, antibiotic tolerance |
| yheL | Complex stabilization | Impaired tRNA thiolation, metabolic reprogramming |
| yhhP | Sulfur mobilization | Increased persister frequency in stationary phase |
Experimental Approaches for Studying Persistence Mechanisms
High-Throughput Genetic Screening
Tn-seq Screening Protocol: Researchers employed a saturated transposon mutant library of Salmonella Typhimurium to identify genes involved in persister formation within macrophages [110] [111]. The experimental workflow involved:
- Infection of mouse macrophage RAW 264.7 cells with the transposon library (5×10⁷ CFU)
- Elimination of extracellular bacteria with gentamicin treatment (2 hours post-infection)
- Treatment with cefotaxime (β-lactam antibiotic) for 24 hours to eliminate replicating intracellular bacteria
- Recovery of surviving persister cells and genomic DNA extraction
- High-throughput sequencing to map transposon insertion sites and quantify relative abundance
This approach identified 157 genes involved in persister formation, with 88 classified as negative determinants and 105 as positive determinants of persistence [110]. The sulfur transferase complex genes (yheM, yheN, trmU) emerged as significant negative persistence determinants, whose disruption enhanced bacterial survival during antibiotic treatment.
Single-Cell Persistence Assays
Fluorescence-Based Replication Tracking: Intracellular replication dynamics were quantified using carboxyfluorescein diacetate succinimidyl ester (CFSE)-labeled bacteria analyzed by flow cytometry [110] [111]. CFSE fluorescence intensity decreases proportionally with cell division, enabling discrimination between replicating and non-replicating subpopulations. This method revealed that deletion of sulfur transferase genes significantly increased the proportion of non-replicating Salmonella within macrophages, correlating with enhanced antibiotic persistence.
LIVE/DEAD Staining with FACS: Membrane integrity and viability of persistent subpopulations were assessed using the BacLight viability kit containing SYTO 9 (green fluorescent, membrane-permeant) and propidium iodide (red fluorescent, membrane-impermeant) [112]. Fluorescence-activated cell sorting (FACS) enabled isolation and quantification of viable but non-culturable subpopulations, providing insights into dormancy states.
Comparative Analysis of Persistence Mechanisms
Sulfur Transferase-Mediated Persistence Pathways
The sulfur transferase complex governs persistence through distinct mechanisms across bacterial growth phases:
Exponential Phase Mechanism: Disruption of the complex increases intracellular reactive nitrogen species (RNS), which inhibits bacterial respiration and ATP generation. This metabolic downshift promotes a dormant state resistant to antibiotics targeting active cellular processes [110] [111].
Stationary Phase Mechanism: In absence of functional sulfur transferase, RelA-mediated (p)ppGpp synthesis increases, activating the stringent response. This global stress adaptation pathway redirects cellular resources toward maintenance and survival, enhancing multi-drug tolerance [110].
Table 2: Quantitative Effects of Sulfur Transferase Complex Disruption on Salmonella Physiology
| Parameter | Wild-Type Strain | ΔyheM Mutant | Experimental Conditions |
|---|---|---|---|
| Intracellular survival with cefotaxime | Baseline | 3-5 fold increase | RAW 264.7 macrophages, 24h treatment [110] |
| Non-replicating cells | 15-20% | 40-50% | CFSE labeling, 24h post-infection [110] |
| ATP levels | Normal | 60-70% reduction | Exponential phase, in vitro [110] |
| (p)ppGpp levels | Baseline | 2-3 fold increase | Stationary phase, in vitro [110] |
| Reactive Nitrogen Species | Baseline | 2.5-3.5 fold increase | Exponential phase, in vitro [110] |
Alternative Persistence Mechanisms in Salmonella
While the sulfur transferase complex represents a significant pathway, recent research highlights additional mechanisms contributing to Salmonella persistence:
Nutrient Limitation-Induced Resilience: Severe nutrient starvation restricts bacterial replication rates, dramatically reducing antibiotic efficacy independently of specific persistence pathways. In mouse infection models, nutrient access controlling replication rate dominated antibiotic survival, with a 165-fold effect size compared to 3-fold for osmolarity and 1.5-fold for H₂O₂ [113].
Toxin-Antitoxin Systems: Modules such as tisB, ecnB, shpAB, and phD-doc have been implicated in persistence, though their quantitative impact appears limited under physiological conditions [113].
Stress-Induced Dormancy: Microenvironmental stresses including acidic pH, oxidative stress, and antimicrobial peptides induce dormancy programs, though their individual contributions to persistence are modest compared to nutrient limitation [113].
Signaling Pathways and Molecular Mechanisms
The molecular mechanisms through which the sulfur transferase complex influences persistence involve interconnected signaling networks:
Figure 1: Molecular Mechanisms of Sulfur Transferase-Mediated Persistence. The complex regulates persistence through distinct pathways in exponential (RNS respiration inhibition) and stationary ((p)ppGpp stringent response) phases.
The Scientist's Toolkit: Essential Research Reagents and Methodologies
Table 3: Key Research Reagents for Studying Bacterial Persistence
| Reagent/Method | Application | Key Features | Experimental Use |
|---|---|---|---|
| Tn-seq Mutant Library | Genome-wide persistence gene identification | Saturated transposon insertion mutants | High-throughput screening in host cells [110] [111] |
| CFSE Labeling | Single-cell replication tracking | Fluorescence dilution with division | Flow cytometry analysis of non-replicating populations [110] |
| BacLight LIVE/DEAD Kit | Membrane integrity assessment | SYTO9/PI differential staining | FACS isolation of viable but dormant cells [112] |
| Cefotaxime | β-lactam antibiotic | Effective against intracellular bacteria | Selection of intramacrophage persisters [110] [111] |
| ATP Assay Kit | Metabolic activity quantification | Luminescence-based detection | Measurement of bacterial energy status [110] |
| Mouse Macrophage RAW 264.7 | Intracellular infection model | Murine leukemic monocyte-macrophage | Standardized persister formation assays [110] [111] |
Discussion and Therapeutic Implications
The sulfur transferase complex represents a metabolic control point that balances bacterial replication and persistence within the hostile macrophage environment. Its disruption creates a physiological state characterized by reduced energy generation, slowed replication, and enhanced stress tolerance—ideal conditions for antibiotic persistence. This mechanistic understanding provides valuable insights for countering persistent Salmonella infections.
From a therapeutic perspective, targeting the sulfur transferase complex presents a paradoxical challenge: while its disruption increases persistence, its complete inhibition might lock bacteria in a persistent state. Alternative approaches could focus on modulating the downstream consequences of sulfur transferase dysfunction, such as RNS accumulation or (p)ppGpp signaling. Combining conventional antibiotics with inhibitors of the stringent response or RNS detoxification pathways may provide more effective eradication of persistent populations.
Future research should explore the conservation of these mechanisms across bacterial species and investigate potential host-directed therapies that manipulate the macrophage microenvironment to disrupt these bacterial adaptation pathways. The experimental approaches outlined here provide a robust framework for such investigations, enabling systematic comparison of persistence mechanisms across pathogen species and identification of broad-spectrum therapeutic targets.
Bacterial persisters, a subpopulation of cells characterized by transient, non-heritable antibiotic tolerance, present a significant challenge in treating chronic and recurrent infections. Unlike resistant bacteria, persisters do not grow in the presence of antibiotics but can resume growth once the antibiotic pressure is removed, leading to relapsing infections [1]. Their formation is strongly associated with treatment failure in biofilm-associated infections, tuberculosis, and recurrent urinary tract infections [114] [1]. The molecular mechanisms underlying persister formation are complex and multifaceted, extending beyond traditional genetic mutations to include sophisticated physiological adaptations. This review systematically compares three emerging mechanisms of bacterial persistence—the SOS response, epigenetic regulation, and RNA degradation—evaluating their unique molecular pathways, experimental evidence, and implications for therapeutic development. By examining these mechanisms across key bacterial pathogens, we aim to provide researchers and drug development professionals with a comprehensive framework for understanding and targeting bacterial persistence.
Table 1: Comparative analysis of emerging persister formation mechanisms
| Mechanism | Key Molecular Components | Primary Inducing Signals | Core Physiological Effect | Representative Pathogens |
|---|---|---|---|---|
| SOS Response | LexA repressor, RecA co-protease, error-prone DNA polymerases (Pol II, IV, V) | DNA damage (fluoroquinolones, UV), reactive oxygen species | DNA repair activation, cell division arrest, mutagenesis, induction of toxin-antitoxin systems | Escherichia coli, Pseudomonas aeruginosa, Staphylococcus aureus, Mycobacterium tuberculosis [114] |
| Epigenetic Regulation | DNA methyltransferases, nucleoid-associated proteins, non-coding RNAs | Antibiotic exposure, environmental stress | Heritable changes in gene expression without DNA sequence alteration, transcriptional reprogramming | E. coli, S. aureus, M. tuberculosis [115] [116] |
| RNA Degradation | mRNA endonucleases (RelE, MazF, MqsR), Lon protease, toxin-antitoxin systems | Nutrient starvation, antibiotic stress, SOS response activation | Global translation shutdown via mRNA cleavage, metabolic dormancy | E. coli, P. aeruginosa, M. tuberculosis [117] |
The SOS Response: An Inducible DNA Damage Survival Pathway
Molecular Mechanism and Regulation
The SOS response represents a well-characterized inducible pathway for bacterial persistence that activates upon DNA damage. This complex regulatory network is primarily controlled by two key proteins: LexA, a transcriptional repressor, and RecA, a co-protease [114] [118]. Under normal growth conditions, LexA dimers bind to specific operator sequences (SOS boxes) in the promoter regions of more than 50 genes comprising the SOS regulon [118]. When DNA damage occurs through exposure to fluoroquinolones, UV radiation, or other DNA-damaging agents, single-stranded DNA (ssDNA) gaps form at stalled replication forks. RecA binds to this ssDNA, forming nucleoprotein filaments (RecA) that stimulate the self-cleavage of LexA at an Ala84-Gly85 bond [118]. LexA inactivation leads to derepression of SOS genes in a temporally regulated manner: early genes include excision repair components (uvrA, *uvrB), followed by recombination repair genes (recA, recN, ruvAB), and finally error-prone translesion DNA polymerases (umuDC, dinB, polB) that allow replication past DNA lesions but with reduced fidelity [114] [118].
The timing and amplitude of SOS induction are precisely regulated based on the extent of DNA damage. Genes with SOS boxes closely matching the consensus sequence (TACTG(TA)5CAGTA) are derepressed first and most strongly, while those with divergent sequences require more persistent DNA damage for activation [118]. This graduated response enables bacteria to prioritize high-fidelity repair mechanisms initially, resorting to error-prone repair only when damage is extensive. Additional regulation occurs through proteolytic degradation of LexA fragments by ClpXP and Lon proteases, ensuring complete removal of the repressor during sustained stress [118].
Experimental Evidence and Methodologies
Table 2: Key experimental approaches for studying SOS-mediated persistence
| Experimental Approach | Protocol Summary | Key Measurements | Supporting Evidence |
|---|---|---|---|
| Genetic Knockouts | Construction of recA, recB, lexA, and SOS gene mutants in target pathogens | Persister counts after ciprofloxacin exposure; survival kinetics | recA and recB mutants show 35-103-fold persister reduction [119] |
| SOS-Inducible Reporter Systems | Fusion of SOS-regulated promoters (e.g., sulA, recN) to fluorescent proteins | Single-cell fluorescence quantification after DNA damage | Correlation between SOS induction strength and persistence frequency [119] |
| SOS Inhibition Studies | Treatment with SOS inhibitors (suramin, p-coumaric acid) combined with antibiotics | MIC changes, mutation frequency reduction, persister eradication | Suramin inhibits RecA-mediated LexA cleavage and prevents persistence [120] |
| Toxin-Antitoxin Analysis | Deletion of SOS-regulated TA systems (e.g., tisB/istR) | Persister levels after SOS induction with fluoroquinolones | TisB toxin expression required for SOS-induced persistence [114] |
Seminal research by Dörr et al. demonstrated that the SOS response actively induces persistence to fluoroquinolones in E. coli, challenging the prevailing view that persisters are exclusively pre-existing [119]. Using a combination of genetic mutants and carefully controlled persistence assays, they showed that recA, recB, and non-cleavable lexA3 mutants exhibited 35-103-fold reductions in persister levels after ciprofloxacin exposure, while maintaining normal persistence to antibiotics like ampicillin that do not target DNA [119]. This established that SOS induction is specifically required for persistence to DNA-damaging agents rather than being a general persistence mechanism.
The experimental workflow for these studies typically involves exposing exponentially growing bacterial cultures to ciprofloxacin (typically at 5-10× MIC) for varying durations, with aliquots removed at timed intervals, washed to remove antibiotic, and plated on drug-free media to quantify surviving colony-forming units (CFUs) [119]. The biphasic killing curves generated—with an initial rapid decline followed by a persistent plateau—provide the key evidence for persister cell presence. To specifically assess SOS induction during persistence development, researchers often employ fluorescent reporter constructs where SOS-responsive promoters (e.g., sulA, recN) drive expression of GFP or other fluorescent proteins, enabling single-cell analysis of SOS induction dynamics in persister populations using flow cytometry or microscopy [119].
Pathogen-Specific Variations
The core SOS response mechanism is conserved across bacterial species, but its regulation and connection to persistence display pathogen-specific adaptations. In E. coli, the SOS system directly controls the tisB/istR toxin-antitoxin module, where TisB toxin expression disrupts membrane potential and induces dormancy [114]. Pseudomonas aeruginosa integrates SOS signaling with biofilm formation pathways, with SOS-induced persisters being particularly abundant in mature biofilms [114]. In Staphylococcus aureus, SOS activation promotes the emergence of small colony variants (SCVs)—slow-growing, quasi-dormant cells with heightened antibiotic tolerance [114]. Mycobacterium tuberculosis employs SOS-mediated mutagenesis through error-prone DNA polymerases to adapt to antibiotic pressure, contributing to treatment recalcitrance [114]. These variations highlight the importance of studying SOS-mediated persistence in specific pathogenic contexts for therapeutic development.
Epigenetic Regulation: Heritable Changes Without DNA Sequence Alteration
Molecular Mechanisms of Bacterial Epigenetics
Epigenetic mechanisms in bacteria mediate heritable phenotypic changes without altering the underlying DNA sequence, primarily through DNA modification and non-coding RNA regulation. While eukaryotes employ complex chromatin remodeling systems, bacterial epigenetics revolves around three principal mechanisms: DNA methylation, DNA phosphorothioation, and regulation by non-coding RNAs [116]. DNA methylation represents the most extensively characterized epigenetic modification in bacteria, with three major forms: N6-methyladenosine (m6A), 5-methylcytosine (m5C), and N4-methylcytosine (m4C) [116]. These modifications are catalyzed by specific DNA methyltransferases (MTases), which transfer methyl groups from S-adenosylmethionine to specific DNA residues. The m6A and m5C modifications occur in most bacterial species, while m4C is restricted to bacteria and archaea [116].
DNA methyltransferases are frequently associated with restriction-modification (R-M) systems, which serve as defense mechanisms against foreign DNA. However, "orphan" methyltransferases lacking cognate restriction enzymes increasingly appear to function as genuine epigenetic regulators that modulate gene expression in response to environmental cues [116]. For instance, in Helicobacter pylori, phase variation controlled by DNA methylation regulates expression of virulence factors and outer membrane proteins, potentially influencing antibiotic tolerance [116]. DNA phosphorothioation represents another epigenetic-like modification where a non-bridging oxygen atom in the DNA sugar-phosphate backbone is replaced by sulfur. This modification, governed by the dndABCDE gene cluster, contributes to antioxidant defense, cellular redox homeostasis, and antibiotic resistance [116].
Non-coding RNAs (ncRNAs) constitute a second major epigenetic regulatory layer in bacteria. These small RNA molecules act as post-transcriptional regulators that allow rapid adaptation to environmental stresses, including antibiotic exposure. ncRNAs can modulate mRNA stability, translation efficiency, and protein activity, enabling bacteria to fine-tune gene expression without genetic mutations [116]. Under antibiotic stress, ncRNA networks can reconfigure bacterial physiology toward dormancy by repressing metabolic enzymes, ribosome assembly factors, and other growth-related processes [115].
Experimental Approaches and Evidence
Investigating epigenetic persistence mechanisms requires specialized methodologies that capture transient, reversible phenotypic states. Key approaches include:
Single-molecule real-time (SMRT) sequencing: This technology directly detects DNA methylation patterns across the bacterial genome by monitoring DNA polymerase kinetics during replication. SMRT sequencing enables comprehensive mapping of m6A and m4C methylation at single-base resolution, allowing researchers to correlate methylation status with gene expression changes in persistent cells [115].
Methyltransferase knockout studies: Genetic deletion of specific DNA methyltransferases followed by phenotypic characterization can identify epigenetic persistence pathways. For example, deletion of the dam methyltransferase in E. coli alters replication timing and gene expression, potentially influencing persistence frequency [116].
ncRNA profiling and manipulation: High-throughput RNA sequencing under antibiotic stress identifies ncRNAs differentially expressed in persister cells. Functional validation involves ncRNA overexpression or deletion followed by persistence quantification using standard antibiotic killing assays [116].
Epigenetic inhibitor studies: Compounds that disrupt DNA methylation or ncRNA function can reverse persistence when combined with conventional antibiotics. While clinical applications remain exploratory, these pharmacological approaches provide mechanistic insights and potential therapeutic avenues [116].
Emerging evidence suggests that epigenetic regulation creates heterogeneous bacterial populations where distinct physiological states—including persistence—coexist genetically identical cells. This epigenetic heterogeneity may explain why some cells enter persistence while their genetically identical counterparts succumb to antibiotic treatment [115].
RNA Degradation Systems: Global Translation Shutdown via Targeted mRNA Cleavage
Molecular Mechanisms of Persistence Through RNA Degradation
RNA degradation represents a rapid and effective mechanism for inducing bacterial dormancy through targeted cleavage of essential mRNAs, resulting in global translation inhibition. This process is primarily mediated by chromosomally-encoded toxin-antitoxin (TA) systems that produce mRNA endonucleases (mRNases) [117]. In E. coli, ten known type II TA loci encode mRNases that cleave cellular mRNAs at specific sequences or ribosomal sites, effectively halting protein synthesis [117]. These include RelE, YoeB, HigB, YhaV, YafO, YafQ, MazF, ChpB, MqsR, and HicA, which collectively provide a redundant network for persistence induction under diverse stress conditions [117].
Under normal growth conditions, these mRNases are neutralized by their cognate protein antitoxins, which form stable complexes with the toxins and suppress their enzymatic activity. The antitoxins are metabolically unstable and susceptible to degradation by cellular proteases, particularly Lon protease [117]. Under stress conditions such as nutrient starvation or antibiotic exposure, increased Lon protease activity tips the balance toward free toxin, enabling mRNase activation. For example, amino acid starvation triggers Lon-mediated degradation of the RelB antitoxin, freeing RelE to cleave mRNAs positioned at the ribosomal A-site [117]. Similarly, SOS response activation can induce expression of certain TA systems, creating a direct link between DNA damage and translation shutdown [114].
The molecular targets and cleavage specificities vary among mRNases. RelE-family toxins (RelE, YoeB, HigB, YhaV, YafO, YafQ) cleave mRNA positioned at the ribosomal A-site between the second and third nucleotides of the codon, while MazF-like toxins (MazF, ChpB, MqsR, HicA) cleave RNA at specific sequences independent of ribosomes [117]. This diversity enables fine-tuned response to different environmental insults, with specific mRNases activated under particular stress conditions.
Experimental Validation and Methodologies
Key evidence supporting RNA degradation in persistence comes from systematic genetic and biochemical studies:
TA system deletion analysis: Successive deletion of the ten mRNase-encoding TA loci in E. coli progressively reduced persister levels, demonstrating their cumulative contribution to persistence [117]. Individual deletions produced varying effects depending on the inducing condition, indicating functional specialization among different TA systems.
Controlled toxin expression: Artificial induction of mRNase expression from inducible promoters rapidly generates high persister fractions (up to 4,000-fold increase), while subsequent induction of the cognate antitoxin rescues cells from dormancy, confirming the cause-effect relationship [117].
Lon protease manipulation: Deletion of lon dramatically reduces persister formation, while Lon overexpression increases persistence in a mRNase-dependent manner, establishing the central role of proteolytic antitoxin degradation in persistence induction [117].
Single-cell persistence tracking: Fluorescent transcriptional fusions to TA operons demonstrate heterogeneous expression patterns, with a small fraction of cells spontaneously activating TA systems even in unstressed conditions, contributing to pre-existing persister subpopulations [117].
The standard experimental workflow involves growing bacterial cultures to mid-exponential phase, treating with lethal antibiotic concentrations (typically 10-100× MIC), removing samples at timed intervals, washing to remove antibiotics, and plating on drug-free media to enumerate surviving CFUs. To specifically assess TA system involvement, researchers compare persistence levels in wild-type and TA deletion strains, often using fluoroquinolones (which indirectly induce TA systems via SOS) and aminoglycosides (which require active transport for efficacy) to probe different persistence mechanisms.
Integrated Signaling Pathways in Persister Formation
The three mechanisms discussed do not operate in isolation but rather form an interconnected network that coordinates bacterial persistence in response to diverse environmental stresses. The relationships between these pathways can be visualized through the following regulatory network:
Integrated Pathways in Bacterial Persistence
This integrated network reveals how different environmental stressors activate specific persistence mechanisms that converge on metabolic dormancy. The SOS response initiates upon DNA damage, inducing toxin-antitoxin systems that contribute to RNA degradation while simultaneously promoting epigenetic changes through error-prone replication. Epigenetic regulation establishes heritable persistence states that can be further reinforced through ncRNA-mediated control of TA systems. RNA degradation directly implements metabolic shutdown by halting protein synthesis, the final common pathway for multiple persistence-inducing signals.
Research Toolkit: Essential Reagents and Methodologies
Table 3: Key research reagents and solutions for studying persister mechanisms
| Reagent Category | Specific Examples | Research Applications | Experimental Considerations |
|---|---|---|---|
| SOS Reporters | sulA-gfp, recN-gfp transcriptional fusions | Real-time monitoring of SOS induction at single-cell level | Requires flow cytometry or microscopy for quantification; may miss low-level induction |
| TA System Tools | Controlled expression vectors for toxins/antitoxins; TA deletion mutants | Functional dissection of specific TA roles in persistence | Toxin expression often lethal; requires tightly regulated inducible systems |
| Epigenetic Modifiers | DNA methyltransferase inhibitors; SMRT sequencing kits | Mapping methylation patterns; probing epigenetic contributions | Bacterial epigenetics less characterized than eukaryotic; interpretation challenges |
| SOS Inhibitors | Suramin, p-coumaric acid, lexazin | Blocking SOS-induced persistence and resistance evolution | Often affect multiple cellular processes; require careful control experiments |
| Lon Protease Modulators | Lon protease mutants; proteasome inhibitors | Testing TA activation via antitoxin degradation | Lon has multiple cellular targets beyond antitoxins; pleiotropic effects possible |
| Metabolic Activators | Sugars, amino acids, electron carriers | Reversing persistence via metabolic resuscitation | Concentration-dependent effects; pathogen-specific responses |
This research toolkit enables systematic dissection of persistence mechanisms across bacterial species. SOS reporters provide dynamic, single-cell resolution data on DNA damage response activation, while TA system tools allow direct manipulation of the RNA degradation pathway. Epigenetic modifiers represent emerging technologies for investigating heritable persistence states that cannot be explained by genetic mutations. Inhibitors and modulators of these pathways serve both mechanistic probes and potential therapeutic starting points.
When employing these reagents, researchers should consider several methodological aspects. For persistence assays themselves, critical parameters include the initial bacterial growth phase (exponential vs. stationary), antibiotic concentrations (typically 5-100× MIC), and the timing of survival quantification (biphasic killing curves typically emerge after 3-5 hours of antibiotic exposure) [1] [119]. For mechanistic studies, combination approaches—such as measuring SOS activation in TA system mutants—can reveal pathway interactions. Additionally, species-specific differences necessitate optimization; for example, M. tuberculosis persistence studies require extended timeframes due to slow growth, while E. coli enables rapid experimental turnaround.
The comparative analysis of SOS response, epigenetic regulation, and RNA degradation mechanisms reveals both shared and distinctive pathways to bacterial persistence. The SOS response represents an inducible mechanism activated by specific antibiotic classes that damage DNA, while RNA degradation through TA systems provides a rapid translation shutdown strategy effective against multiple antibiotic classes. Epigenetic regulation offers a heritable yet reversible persistence mechanism that may explain population heterogeneity without genetic mutation.
From a therapeutic perspective, each mechanism presents unique targeting opportunities. SOS inhibition (e.g., with suramin or p-coumaric acid) may prevent persistence to fluoroquinolones and reduce resistance evolution [120]. TA system manipulation could resensitize persistent cells to conventional antibiotics, while epigenetic modulators might reverse persistence programs in bacterial subpopulations. The integrated pathway analysis suggests that combination approaches targeting multiple persistence mechanisms simultaneously may prove most effective, particularly for recalcitrant biofilm infections where multiple persistence pathways likely operate in parallel.
Future research directions should include comprehensive mapping of epigenetic persistence markers across clinical isolates, development of more specific SOS and TA system inhibitors, and clinical evaluation of anti-persister adjuvants that target these mechanisms. As these emerging mechanisms become better characterized, they offer promising avenues for extending the useful life of existing antibiotics and addressing the growing challenge of persistent bacterial infections.
Conclusion
The comparative analysis of bacterial persister formation reveals a complex interplay of conserved pathways, such as TA systems and the stringent response, with species-specific adaptations that enable survival across diverse host environments. This synthesis underscores that overcoming the challenge of persistent infections requires a multi-faceted approach: developing diagnostics that detect dormant cells, innovating beyond traditional antibiotic discovery to target persister-specific physiology, and designing combination therapies that disrupt protective niches like biofilms. Future research must prioritize translating single-cell mechanistic insights into clinically effective strategies that can eradicate the recalcitrant persister subpopulations responsible for chronic infections and treatment relapse, thereby addressing a critical frontier in the global fight against antimicrobial resistance.
References
- 1. Bacterial persisters: molecular mechanisms and ... [https://www.nature.com/articles/s41392-024-01866-5]
- 2. Bacterial Persister Cells and Development of Antibiotic ... [https://www.frontierspartnerships.org/journals/british-journal-of-biomedical-science/articles/10.3389/bjbs.2024.12958/full]
- 3. Phenotypic Resistance to Antibiotics - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC4790337/]
- 4. Bacterial Persister Cell Formation and Dormancy - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC3837759/]
- 5. General Mechanisms Leading to Persister Formation and ... [https://www.sciencedirect.com/science/article/abs/pii/S0168952519300538]
- 6. Exploring antibiotic-induced persister formation and bacterial ... [https://bmcinfectdis.biomedcentral.com/articles/10.1186/s12879-024-09906-9]
- 7. Phenotypic and genotypic characterization of antibiotic- ... [https://www.frontiersin.org/journals/microbiology/articles/10.3389/fmicb.2025.1649307/full]
- 8. Combatting persister cells: The daunting task in post- ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10250163/]
- 9. Persister Cell - an overview | ScienceDirect Topics [https://www.sciencedirect.com/topics/neuroscience/persister-cell]
- 10. Bacterial Persistence: A Model of Survival in Changing ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC1449587/]
- 11. A Shift in Perspective: A Role for the Type I Toxin TisB ... [https://www.frontiersin.org/journals/microbiology/articles/10.3389/fmicb.2022.871699/full]
- 12. Bacterial toxin-antitoxin modules: classification, functions, and ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC8610362/]
- 13. Cross-Regulations between Bacterial Toxin–Antitoxin ... [https://www.sciencedirect.com/science/article/abs/pii/S0966842X20301438]
- 14. Recent Advances in Bacterial Persistence Mechanisms - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC10531727/]
- 15. Molecular mechanism and application of emerging ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11568608/]
- 16. Characterization of toxin-antitoxin systems from public ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC9424990/]
- 17. A minimal model for gene expression dynamics of bacterial ... [https://www.nature.com/articles/s41598-021-98570-z]
- 18. A General Model for Toxin-Antitoxin Module Dynamics Can ... [https://journals.plos.org/ploscompbiol/article?id=10.1371/journal.pcbi.1003190]
- 19. A toxin-antitoxin module as a target for antimicrobial ... [https://pubmed.ncbi.nlm.nih.gov/19800365/]
- 20. Metabolite-driven reprogramming of bacterial persisters [https://www.sciencedirect.com/science/article/abs/pii/S1368764625001256]
- 21. (p)ppGpp and Its Role in Bacterial Persistence [https://pmc.ncbi.nlm.nih.gov/articles/PMC7508602/]
- 22. Recent advances in the understanding, detection and ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12333241/]
- 23. Studies on the Regulation of (p)ppGpp Metabolism and Its ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC7593582/]
- 24. (p)ppGpp imposes graded transcriptional changes to ... [https://www.nature.com/articles/s41522-025-00795-7]
- 25. Possible Roles for Basal Levels of (p)ppGpp: Growth ... [https://www.frontiersin.org/journals/microbiology/articles/10.3389/fmicb.2020.592718/full]
- 26. Persisters of Bacterial Biofilms [https://www.intechopen.com/chapters/1211701]
- 27. Biofilms: structure, resistance mechanism, emerging control ... [https://pubs.rsc.org/en/content/articlehtml/2025/pm/d5pm00094g]
- 28. Mechanisms of antimicrobial resistance in biofilms [https://www.nature.com/articles/s44259-024-00046-3]
- 29. biofilms, quorum sensing, formation and prevention [https://pmc.ncbi.nlm.nih.gov/articles/PMC7086079/]
- 30. Comparative Analysis of Biofilm Formation and Antibiotic ... [https://pubmed.ncbi.nlm.nih.gov/40868035/]
- 31. Formation, architecture, and persistence of oral biofilms [https://www.frontiersin.org/journals/microbiology/articles/10.3389/fmicb.2025.1602962/full]
- 32. New Strategies to Kill Metabolically-Dormant Cells Directly ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10295454/]
- 33. Biofilm, resistance, and quorum sensing: The triple threat in ... [https://www.sciencedirect.com/science/article/pii/S2950194625003462]
- 34. Mini review: Persister cell control strategies [https://www.frontiersin.org/journals/pharmacology/articles/10.3389/fphar.2025.1706115/full]
- 35. Empowering single-cell analysis with emerging active ... [https://www.sciencedirect.com/science/article/abs/pii/S0142961225005368]
- 36. How single-cell immunology is benefiting from microfluidic ... [https://www.nature.com/articles/s41378-020-0140-8]
- 37. Microfluidic Biochips for Single‐Cell Isolation and ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11267386/]
- 38. Microfluidics applications for high-throughput single cell ... [https://jnanobiotechnology.biomedcentral.com/articles/10.1186/s12951-021-01045-6]
- 39. In vivo molecular and single cell imaging - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC9252890/]
- 40. Performance comparison of high throughput single-cell ... [https://www.sciencedirect.com/science/article/pii/S2405844024132161]
- 41. Comparative benchmarking of single-cell clustering ... [https://genomebiology.biomedcentral.com/articles/10.1186/s13059-025-03719-y]
- 42. Genome-wide fitness and genetic interactions determined by Tn - seq ... [https://pubmed.ncbi.nlm.nih.gov/21053251/]
- 43. Shedding light on bacteria–host interactions with the aid of ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11237515/]
- 44. Reactive Oxygen Detoxification Contributes to Mycobacterium... [https://elifesciences.org/reviewed-preprints/104944v1]
- 45. - Tn : seq - high parallel sequencing for fitness and throughput ... genetic [https://www.nature.com/articles/nmeth.1377?error=cookies_not_supported&code=322a304b-a223-495e-9011-1b66b2f8f8a8]
- 46. Statistical analysis of variability in TnSeq data across ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC6873424/]
- 47. Functional genomics reveals strain-specific genetic ... [https://elifesciences.org/reviewed-preprints/99426]
- 48. RNA-seq and Tn - seq reveal fitness determinants of... [https://bmcgenomics.biomedcentral.com/articles/10.1186/s12864-017-4299-9]
- 49. A Salmonella Toxin Promotes Persister Formation through ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC4942678/]
- 50. Model systems to study Mycobacterium tuberculosis ... [https://www.frontiersin.org/journals/cellular-and-infection-microbiology/articles/10.3389/fcimb.2025.1572547/full]
- 51. Murine models of Salmonella infection - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC10372748/]
- 52. Structural and functional analyses of STM14_5441- ... [https://www.sciencedirect.com/science/article/abs/pii/S136876462500010X]
- 53. Comparative Studies Evaluating Mouse Models Used for ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC3067068/]
- 54. In-vivo expressed Mycobacterium tuberculosis antigens ... [https://www.nature.com/articles/s41541-021-00343-2]
- 55. Noise in a Metabolic Pathway Leads to Persister Formation ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC9602276/]
- 56. High Persister Mutants in Mycobacterium tuberculosis [https://journals.plos.org/plosone/article?id=10.1371/journal.pone.0155127]
- 57. Are Bacterial Persisters Dormant Cells Only? [https://www.frontiersin.org/journals/microbiology/articles/10.3389/fmicb.2021.708580/full]
- 58. Bacterial dormancy: A subpopulation of viable but non ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC7837498/]
- 59. Unraveling CRP/cAMP-mediated metabolic regulation in ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12237405/]
- 60. Unraveling CRP/cAMP-mediated metabolic regulation in ... [https://elifesciences.org/articles/99735]
- 61. Shotgun proteomic profiling of dormant, 'non-culturable ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC9362914/]
- 62. Proteomic and metabolomic responses of priority bacterial ... [https://www.nature.com/articles/s44259-025-00147-7]
- 63. In Vitro Studies of Persister Cells - PMC - PubMed Central [https://pmc.ncbi.nlm.nih.gov/articles/PMC7667008/]
- 64. Molecular mechanism and application of emerging ... [https://bmcmicrobiol.biomedcentral.com/articles/10.1186/s12866-024-03628-3]
- 65. Bacterial Persister Cells and Development of Antibiotic ... - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC11335562/]
- 66. Comparison of the In vitro Activity of Five Antimicrobial ... [https://www.frontiersin.org/journals/microbiology/articles/10.3389/fmicb.2016.01187/full]
- 67. In Vitro Persistence Level Reflects In Vivo Antibiotic ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10269860/]
- 68. WHO releases new reports on new tests and treatments in ... [https://www.who.int/news/item/02-10-2025-who-releases-new-reports-on-new-tests-and-treatments-in-development-for-bacterial-infections]
- 69. Exploring antibiotic-induced persister formation and ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11409487/]
- 70. Prophages and Growth Dynamics Confound Experimental ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC5727415/]
- 71. Protocol for assessing single-cell persister recovery ... [https://www.sciencedirect.com/science/article/pii/S2666166724001497]
- 72. Targeting bacterial persistence with bacteriophages [https://www.sciencedirect.com/science/article/abs/pii/S0042682225002624]
- 73. Reports identify weakness in global pipeline for new ... [https://www.cidrap.umn.edu/antimicrobial-stewardship/reports-identify-weakness-global-pipeline-new-antibiotics-diagnostics]
- 74. Antimicrobial resistance: Not enough antibacterials in the ... [https://www.soci.org/news/2025/10/antimicrobial-resistance-not-enough-antibacterials-in-the-pipeline-says-who]
- 75. Biofilm tolerance, resistance and infections increasing ... [http://microbialcell.com/researcharticles/2023a-yang-microbial-cell/]
- 76. Strategy to combat biofilms: a focus on biofilm dispersal ... [https://www.nature.com/articles/s41522-023-00427-y]
- 77. Targeting Biofilms Therapy: Current Research Strategies and ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC7465149/]
- 78. Student-led experimental evolution reveals novel biofilm ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12157681/]
- 79. Ex vivo oral biofilm model for rapid screening of ... [https://www.nature.com/articles/s41598-025-87382-0]
- 80. Metabolic state-driven nutrient-based approach to combat ... [https://www.nature.com/articles/s44259-025-00092-5]
- 81. Differential carbon source utilization drives metabolic state ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12440864/]
- 82. Metabolites augment oxidative stress to sensitize antibiotic ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11633220/]
- 83. A host-directed adjuvant sensitizes intracellular bacterial ... [https://www.nature.com/articles/s41564-025-02124-2]
- 84. Bacterial persistence is an active σS stress response to ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC5043093/]
- 85. Emerging Non-Traditional Approaches to Combat Antibiotic ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC9510247/]
- 86. Non-traditional Antibacterial Therapeutic Options and ... [https://www.sciencedirect.com/science/article/pii/S1931312819302938]
- 87. Drug combinations targeting antibiotic resistance [https://www.nature.com/articles/s44259-024-00047-2]
- 88. Cancer drug-tolerant persister cells: from biological questions ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12622869/]
- 89. Drug-tolerant persister cells in cancer: bridging the gaps ... [https://www.nature.com/articles/s41467-025-66376-6]
- 90. Bacterial toxin-antitoxin modules: classification, functions, ... [https://www.sciencedirect.com/science/article/pii/S2666517421000286]
- 91. Clarifying the Link between Toxin–Antitoxin Modules and ... [https://www.sciencedirect.com/science/article/abs/pii/S0022283619301500]
- 92. Nutritional Stress Leads to Persistence and ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11944742/]
- 93. Isolation and characterization of persisters of the ... [https://www.sciencedirect.com/science/article/pii/S2589004224012276]
- 94. Observation of persister cell histories reveals diverse ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12074638/]
- 95. Emergence of Pseudomonas aeruginosa Strains ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC2981199/]
- 96. Pseudomonas aeruginosa biofilms in disease - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC3977026/]
- 97. Mechanisms of antibiotic resistance in Pseudomonas ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10189392/]
- 98. Tolerance and Persistence of Pseudomonas aeruginosa in ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC7481396/]
- 99. Tolerance and Resistance of Pseudomonas aeruginosa ... [https://www.frontiersin.org/journals/microbiology/articles/10.3389/fmicb.2019.00913/full]
- 100. Pseudomonas aeruginosa Biofilms: Host Response and ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC5894500/]
- 101. Evolution of Resistant Mutants in Pseudomonas aeruginosa ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12299539/]
- 102. Directed evolution of phages in biofilms enhances ... [https://www.nature.com/articles/s41467-025-65014-5]
- 103. Comparative Study of Biofilm Formation in Pseudomonas ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC4079995/]
- 104. A novel mouse model for septic arthritis induced by ... [https://www.nature.com/articles/s41598-019-53434-5]
- 105. Mechanisms of Pyrazinamide Action and Resistance - PubMed [https://pubmed.ncbi.nlm.nih.gov/26104205/]
- 106. Transient drug-tolerance and permanent drug-resistance ... [https://www.nature.com/articles/s41467-019-10975-7]
- 107. Quantitative analysis of persister fractions suggests different ... [https://bmcmicrobiol.biomedcentral.com/articles/10.1186/1471-2180-13-25]
- 108. Determining the minimum inhibitory concentrations of ... [https://www.frontiersin.org/journals/microbiology/articles/10.3389/fmicb.2025.1688772/full]
- 109. Determining the minimum inhibitory concentrations of ... [https://pubmed.ncbi.nlm.nih.gov/41195388/]
- 110. Disruption of sulfur transferase complex increases bacterial ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12077765/]
- 111. Disruption of sulfur transferase complex increases bacterial ... [https://journals.plos.org/plospathogens/article?id=10.1371/journal.ppat.1013136]
- 112. Pseudomonas aeruginosa displays a dormancy phenotype ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC6147739/]
- 113. Limited impact of Salmonella stress and persisters on ... [https://www.nature.com/articles/s41586-024-08506-6]
- 114. The DNA Damage Inducible SOS Response Is a Key ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC7417476/]
- 115. Epigenetic Memories: The Hidden Drivers of Bacterial ... [https://www.sciencedirect.com/science/article/pii/S0966842X2030322X]
- 116. Antimicrobial resistance and mechanisms of epigenetic ... [https://www.frontiersin.org/journals/cellular-and-infection-microbiology/articles/10.3389/fcimb.2023.1199646/full]
- 117. Bacterial persistence by RNA endonucleases - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC3156201/]
- 118. The SOS system: A complex and tightly regulated response to ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC6590174/]
- 119. SOS Response Induces Persistence to Fluoroquinolones in ... [https://journals.plos.org/plosgenetics/article?id=10.1371/journal.pgen.1000760]
- 120. The central role of the SOS DNA repair system in ... [https://www.sciencedirect.com/science/article/abs/pii/S0024320520313151]