Eradicating the Persistent Threat: A Comprehensive Comparison of Modern Anti-Persister Cell Strategies
Persister cells, a dormant subpopulation of bacteria responsible for chronic infections and treatment relapse, represent a major challenge in antimicrobial therapy.
Eradicating the Persistent Threat: A Comprehensive Comparison of Modern Anti-Persister Cell Strategies
Abstract
Persister cells, a dormant subpopulation of bacteria responsible for chronic infections and treatment relapse, represent a major challenge in antimicrobial therapy. This article provides a systematic comparison of current and emerging persister cell elimination strategies for researchers and drug development professionals. It covers the foundational biology of persistence, details direct and indirect methodological approaches for eradication, analyzes troubleshooting and optimization for therapeutic development, and offers a critical validation of strategy efficacy across bacterial models. By synthesizing the latest research, this review aims to guide the selection and optimization of anti-persister therapies to combat recalcitrant infections.
Understanding the Enemy: The Biology of Bacterial Persistence and Its Clinical Impact
Persister cells represent a fascinating and clinically challenging survival strategy employed by bacterial and cancer cells. Unlike genetic resistance, which involves stable heritable mutations, persistence is a reversible, non-genetic phenotype that allows a small subpopulation of cells to withstand lethal doses of therapeutic agents [1] [2]. These dormant or slow-growing variants tolerate antibiotic or chemotherapeutic exposure not through specific resistance mechanisms, but primarily by arresting their metabolic activity, thereby rendering them insusceptible to drugs that target active cellular processes [2] [3]. First described in bacteria by Bigger in 1944 and later identified in cancer by Sharma et al. in 2010, persister cells across biological kingdoms share the remarkable ability to survive lethal treatments and regenerate the population once the stress is removed, causing relapse and chronic infections in bacterial contexts or cancer recurrence following therapy [1] [4].
The clinical significance of persister cells cannot be overstated. In bacteriology, they are implicated in recalcitrant chronic infections such as those occurring in cystic fibrosis patients, medical device-associated infections, and Lyme disease [2] [3]. Similarly, in oncology, drug-tolerant persister (DTP) cells act as clinically occult reservoirs that persist after treatment, seeding relapse long after the visible tumor has regressed [1]. Understanding the fundamental distinctions between phenotypic tolerance and genetic resistance is therefore crucial for developing more effective therapeutic strategies against both infectious diseases and cancer.
Table: Key Characteristics of Persister Cells Versus Genetic Resistance
| Feature | Persister Cells (Phenotypic Tolerance) | Genetic Resistance |
|---|---|---|
| Genetic Basis | No genetic mutations; reversible phenotype | Stable genetic mutations or acquired resistance genes |
| Population Frequency | Small subpopulation (typically 10⁻⁶ to 10⁻³) | Entire population |
| Mechanism | Dormancy, metabolic arrest, epigenetic adaptation | Target modification, drug inactivation, efflux pumps |
| Reversibility | Transient and reversible | Stable and heritable |
| Detection Methods | Time-kill assays, microfluidic single-cell analysis | MIC determination, genetic testing |
Defining the Persister Phenotype: Core Concepts and Mechanisms
Fundamental Distinctions from Genetic Resistance
The persister phenotype operates through mechanisms fundamentally distinct from genetic resistance. While genetically resistant cells proliferate continuously in the presence of antimicrobials or chemotherapeutic agents, persister cells survive through metabolic quiescence and can resume normal growth once the treatment pressure is removed [5]. This phenotypic tolerance affects only a small fraction of the population (typically 0.0001% to 0.1%) that exists in a transient, non-growing state, whereas genetic resistance confers protection to the entire population [5] [6]. At the single-cell level, both phenomena may appear similar with growth-restricted cells escaping the action of therapeutics, but their population dynamics and underlying mechanisms differ significantly [5].
The distinction becomes particularly evident when considering therapeutic implications. Antibiotics like β-lactams that target cell wall synthesis are ineffective against dormant bacterial persisters, just as chemotherapeutic agents that target rapidly dividing cells fail to eliminate quiescent cancer DTPs [1] [7]. However, unlike genetically resistant cells that exhibit specific mechanisms such as enzymatic drug inactivation or target site modification, persisters simply bypass vulnerable processes through metabolic arrest, making them tolerant to multiple unrelated drugs simultaneously – a phenomenon termed multidrug tolerance without cross-resistance [6].
Molecular Mechanisms of Persistence
The formation of persister cells is regulated by sophisticated molecular mechanisms that induce dormancy. In bacterial systems, key players include:
Toxin-Antitoxin (TA) Modules: These genetic elements produce a stable toxin and unstable antitoxin. Under stress conditions, the antitoxin degrades, allowing the toxin to inhibit essential cellular processes such as translation, replication, or ATP production, thereby inducing dormancy [8].
Stringent Response: Mediated by the alarmone (p)ppGpp, this global stress response redirects cellular resources away from growth and toward maintenance, promoting antibiotic tolerance [8].
Reduced ATP Production: Diminished cellular energy levels correlate strongly with antibiotic tolerance, as many antibiotics require active cellular processes or membrane potential for efficacy [8].
In cancer DTPs, parallel mechanisms include epigenetic reprogramming, translational remodeling, metabolic shifts, and therapy-induced mutagenesis [1]. Single-cell RNA sequencing has revealed that DTPs can coexist in multiple phenotypic states within the same tumor, exhibiting either mesenchymal-like or luminal-like transcriptional profiles in breast cancers, for instance [1]. This heterogeneity underscores the remarkable plasticity of the persister phenotype across biological systems.
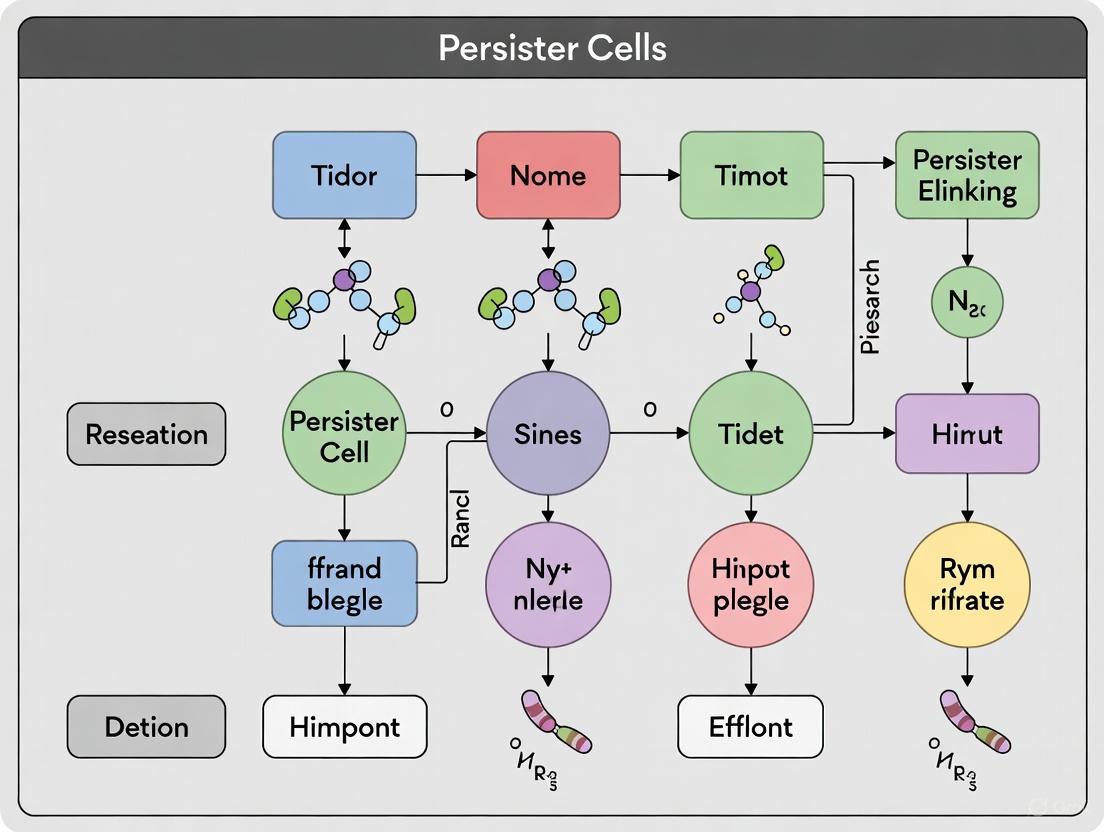
Diagram: Molecular Pathways to Persister Cell Formation. Multiple stress-responsive pathways converge to induce cellular dormancy, leading to multidrug tolerance.
Comparative Analysis: Persister Cells Versus Related Cell States
Bacterial Persisters Versus Other Dormant States
Persister cells occupy a specific niche within the spectrum of bacterial dormancy states, distinguished by their metabolic activity and revival capabilities. While often discussed alongside viable but non-culturable (VBNC) cells and spores, persisters maintain distinct characteristics. VBNC cells exist in a deeper state of dormancy with significantly reduced metabolic activity and cannot grow on standard culture media without a specific recovery process, whereas persister cells maintain higher metabolic activity and can grow on agar, albeit at reduced rates [9]. Unlike spores, which represent a specialized, highly resistant dormant structure formed in response to nutrient limitation in specific genera like Bacillus and Clostridium, persisters are not morphologically distinct from their normal counterparts and can form spontaneously in virtually all bacterial populations [2].
The relationship between persistence and antibiotic tolerance is particularly nuanced. Antibiotic tolerance describes a situation where the entire bacterial population survives bactericidal treatment due to uniformly restrictive growth conditions, while persistence specifically refers to the survival of a small subpopulation under conditions that are permissive for growth for the majority of cells [5]. This distinction was elegantly demonstrated in Salmonella strains, where histidine auxotrophy in restrictive conditions led to population-wide tolerance, masking the presence of persister subpopulations that became apparent only when growth-permissive conditions were restored [5].
Cancer DTPs Versus Other Resilient Cell Populations
In oncology, drug-tolerant persister (DTP) cells share several features with other resilient cell states but remain functionally distinct. DTPs resemble dormant disseminated tumor cells (DTCs) in their ability to survive therapy and seed relapse, but differ in that DTCs are typically Ki67-negative and survive in niche-dependent states, while DTPs are exclusively induced by standard-of-care therapy and display heterogeneous phenotypes including both quiescent and slow-cycling cells [1]. The relationship between DTPs and cancer stem cells (CSCs) is particularly complex, with evidence suggesting overlap in some contexts but distinction in others. For instance, in colorectal cancer patient-derived organoids, chemotherapy-induced DTPs resemble slow-cycling CSCs, mediated by MEX3A-dependent deactivation of the WNT pathway through YAP1 [1].
Similarly, the relationship with senescent cells remains ambiguous. While DTPs share features with senescent cells including reversible arrest and metabolic reprogramming, they often lack consistent senescence markers like γH2AX or p16INK4a [1]. This ambiguity highlights the importance of precisely defining DTPs based on their operational characteristics – specifically, their survival of otherwise lethal drug exposure – rather than presumed mechanistic similarities with other cell states.
Table: Comparative Analysis of Resilient Cell States Across Biological Systems
| Cell State | Defining Characteristics | Formation Triggers | Clinical Impact |
|---|---|---|---|
| Bacterial Persisters | Non-growing, multidrug tolerant, reversible | Stress, stochastic switching | Chronic/recurrent infections |
| VBNC Cells | Deeper dormancy, non-culturable | Severe environmental stress | Undetected reservoirs |
| Cancer DTPs | Therapy-surviving, reversible, heterogeneous | SOC therapy, epigenetic plasticity | Tumor relapse, minimal residual disease |
| Cancer Stem Cells | Tumor-initiating, self-renewing | Developmental programs | Tumor initiation, recurrence |
| Senescent Cells | Irreversible growth arrest, SASP | DNA damage, telomere shortening | Aging, tissue repair, paradoxically cancer |
Experimental Approaches for Persister Cell Research
Methodologies for Isolation and Quantification
Studying persister cells presents unique methodological challenges due to their low frequency and transient nature. The gold standard for quantifying bacterial persisters is the time-kill assay, which exposes a bacterial population to a lethal antibiotic concentration and monitors survival over time, typically revealing biphasic killing kinetics where the first phase represents rapid killing of normal cells and the second slower phase reveals persister survival [6] [7]. For more detailed mechanistic insights, microfluidic devices enable single-cell analysis of persistence dynamics, allowing researchers to track the pre- and post-antibiotic exposure history of individual cells [4]. One such approach utilizes a membrane-covered microchamber array (MCMA) that encloses E. coli cells in 0.8-µm deep microchambers, enabling visualization of over one million individual cells and revealing that many persisters were actually growing before antibiotic treatment [4].
In cancer research, analogous approaches include lineage tracing through DNA barcoding combined with single-cell RNA sequencing to follow the fates of individual cancer cells after treatment [1]. Patient-derived organoids (PDOs) and xenografts (PDXs) provide more physiologically relevant models for studying cancer DTPs, though these often lack immune components and other systemic influences [1]. For both bacterial and cancer persisters, critical experimental considerations include the growth phase of the population (with stationary phase cultures typically yielding higher persister frequencies), the specific therapeutic agent used (as persistence is often drug-specific), and the duration of exposure [6] [7].
Diagram: Experimental Workflow for Persister Cell Research. Multiple parallel approaches enable quantification and characterization of persister cells.
The Researcher's Toolkit: Essential Reagents and Methodologies
Table: Key Research Reagent Solutions for Persister Cell Studies
| Reagent/Method | Function | Application Examples |
|---|---|---|
| Microfluidic Devices (MCMA) | Single-cell confinement and imaging | Tracking E. coli persister histories pre/post antibiotic exposure [4] |
| DNA Barcoding | Lineage tracing at single-cell resolution | Mapping clonal fates of cancer cells after treatment [1] |
| Fluorescence Dilution (FD) | Monitoring growth status at single-cell level | Distinguishing growing vs. non-growing Salmonella in macrophages [5] |
| Patient-Derived Organoids (PDOs) | Physiologically relevant 3D culture models | Studying colorectal cancer DTPs and their resemblance to slow-cycling CSCs [1] |
| Membrane-Active Compounds | Disrupt membrane integrity to enhance antibiotic uptake | Anti-persister agents like XF-73, SA-558 against S. aureus [2] [3] |
| Metabolic Adjuvants | Reactivate persister metabolism | Mannitol, pyruvate to enhance aminoglycoside uptake [8] |
Quantitative Analysis of Persister Cell Dynamics
Survival Kinetics and Population Heterogeneity
Persister cell frequencies vary dramatically across species, growth conditions, and antibiotic classes. Comprehensive analysis of persistence across 36 bacterial species and 54 antibiotics revealed that the median percentage of surviving cells spans five orders of magnitude, from 7 × 10⁻⁴% in P. putida to 100% in E. faecium [7]. For species with substantial data points (≥20), the range was narrower but still varied from 0.01% in A. baumannii to approximately 5% in multidrug-resistant S. aureus (MRSA) [7]. This extensive variation underscores the context-dependent nature of persistence and cautions against overgeneralization from model systems.
The drug-specificity of persistence is particularly remarkable. Even antibiotics with nearly identical mechanisms of action, such as ciprofloxacin and nalidixic acid (both DNA gyrase inhibitors), can select for different persister subpopulations, suggesting that physiological changes beyond simple dormancy underlie persistence [6]. This contrasts with the multidrug tolerance often observed in laboratory E. coli mutants, highlighting the importance of studying persistence in diverse clinical and environmental isolates [6].
Mathematical Modeling of Persister Dynamics
Quantitative modeling of persister populations typically employs a two-state framework where cells switch stochastically between normal and persister states [6]. In this model, normal cells die at rate μ and switch to the persister state at rate α during antibiotic treatment, while persister cells do not die or grow but switch back to the normal state at rate β [6]. This mathematical formalism allows researchers to derive persister fractions that are independent of experimental idiosyncrasies, facilitating cross-study comparisons that are otherwise complicated by variations in antibiotic exposure times, growth states assessed, and methodology differences that have historically plagued the field [6].
Table: Bacterial Persistence Frequencies Across Species and Antibiotic Classes
| Bacterial Species | Antibiotic Class | Typical Persistence Frequency | Key Influencing Factors |
|---|---|---|---|
| Escherichia coli | β-lactams | 0.001% - 0.1% | Growth phase, medium richness |
| Staphylococcus aureus | Fluoroquinolones | 0.01% - 1% | Biofilm state, metabolic activity |
| Pseudomonas aeruginosa | Aminoglycosides | 0.1% - 5% | Quorum sensing, stress response |
| Mycobacterium tuberculosis | Multiple classes | 0.001% - 0.01% | Metabolic heterogeneity, granuloma environment |
| Salmonella enterica | β-lactams | 0.001% - 0.1% | Intracellular location, histidine availability |
The distinction between phenotypic tolerance in persister cells and genetic resistance has profound implications for therapeutic development. Traditional antibiotic discovery platforms that screen for compounds active against rapidly dividing bacteria have systematically overlooked anti-persister agents, creating a critical gap in our antimicrobial arsenal [2] [3]. Similarly, cancer drug development has historically prioritized agents that shrink bulk tumors rather than those that target the minimal residual disease maintained by DTPs [1]. Promising strategies emerging against bacterial persisters include membrane-active compounds that directly disrupt cell integrity independent of metabolic state, metabolite-antibiotic combinations that resuscitate persisters to render them susceptible, and prevention of persister formation through interference with quorum sensing or stress signaling pathways [2] [3] [8].
For cancer DTPs, analogous approaches include epigenetic modulators that prevent or reverse the adaptive reprogramming underlying drug tolerance, and therapeutic combinations that simultaneously target multiple co-existing DTP phenotypes [1]. In both fields, the field is moving toward more physiologically relevant model systems that better capture the complexity of host environments, and developing more sophisticated single-cell technologies to unravel the heterogeneity of persister populations. As research bridges these methodological gaps, targeting persister cells represents a promising frontier for overcoming therapeutic failure and preventing relapse across infectious disease and oncology.
Bacterial persisters are a subpopulation of cells that exhibit transient, non-heritable tolerance to high-dose antibiotic treatment without possessing genetic resistance mutations [2] [10]. These dormant cells were first identified by Joseph Bigger in 1944 during penicillin efficacy tests against Staphylococcus spp., where a small subset of cells survived despite being genetically susceptible to the antibiotic [11]. This phenomenon is now recognized as a major contributor to chronic and recurrent infections across clinical settings, including cystic fibrosis, medical device-associated infections, and urinary tract infections [2] [10]. Unlike resistant bacteria that possess stable genetic mutations enabling growth in antibiotic presence, persisters survive antibiotic exposure through a metabolically inactive or slow-growing state that prevents antibiotics from engaging their cellular targets [10]. When the antibiotic pressure is removed, these cells can resuscitate and repopulate, leading to infection relapse [12].
The study of persistence represents a particular challenge due to the transient nature of the phenotype and the low frequency of persister cells within bacterial populations, typically ranging from 0.001% to 1% [11]. This review systematically compares the primary molecular mechanisms driving persister formation, with particular focus on toxin-antitoxin (TA) modules and stochastic processes, while providing experimental methodologies for their investigation and contextualizing these findings within current drug development strategies aimed at eradicating persistent infections.
Classification and Characteristics of Persister Cells
Persister cells are broadly categorized based on their formation mechanisms and the growth phase in which they emerge. Understanding these classifications provides critical insights into the heterogeneous nature of bacterial persistence and informs targeted therapeutic strategies.
Table 1: Classification of Bacterial Persister Types
| Persister Type | Formation Trigger | Growth Phase | Key Characteristics | Experimental Model |
|---|---|---|---|---|
| Type I | Environmental stress cues (e.g., nutrient limitation) | Stationary phase | Preexisting non-growing cells; bet-hedging strategy | E. coli hipA7 mutants [11] |
| Type II | Stochastic fluctuations in gene expression | Throughout exponential phase | Slow-growing variants within actively dividing population | E. coli hipQ mutants [11] |
| Type III (Specialized) | Specific antibiotic-induced stress | Independent of growth phase | Antibiotic-specific persistence mechanisms; not necessarily slow-growing | Mycobacterium catalase-peroxidase low expressors [11] |
The "dormancy depth" hypothesis suggests these persister types exist along a spectrum of metabolic activity, with Type I persisters generally exhibiting the lowest metabolic rates and Type II maintaining some basal metabolism [10]. This continuum may extend to viable but non-culturable (VBNC) cells, which represent an even more profoundly dormant state that often requires specific resuscitation signals to regain culturability [10] [11]. The classification system provides researchers with a framework for designing experiments that account for this heterogeneity in persister populations.
Molecular Mechanisms of Persister Formation
Toxin-Antitoxin Systems as Central Regulators
Toxin-antitoxin systems represent one of the most extensively studied mechanisms of persister formation. These genetic modules consist of a stable toxin protein that disrupts essential cellular processes and an unstable antitoxin that neutralizes the toxin under normal conditions [13] [10]. Under stress conditions, proteases such as Lon and ClpP preferentially degrade the labile antitoxin, freeing the toxin to exert its effects [10] [14]. This system allows bacteria to rapidly transition to a dormant state in response to environmental challenges.
TA systems are currently classified into eight types based on the nature of the antitoxin and its mechanism of toxin neutralization [13] [10]. Type I and II systems are the most prevalent and best characterized in the context of persistence:
Type I TA systems: Feature protein toxins whose translation is inhibited by antisense RNAs. Examples include TisB/istR and Hok/Sok in E. coli, where the TisB and Hok toxins integrate into the bacterial membrane, dissipating the proton motive force and reducing ATP levels [10].
Type II TA systems: Consist of both protein toxins and antitoxins that form stable complexes. The HipA/HipB system was the first chromosomal TA module linked to persistence, with HipA phosphorylating glutamyl-tRNA synthetase (GltX), leading to accumulation of uncharged tRNA and activation of the stringent response [10]. Another well-characterized system, MazF/MazE, is co-transcribed with relA (which activates the stress sigma factor ϬS) in Gram-negative bacteria and with sigB in Gram-positive bacteria, directly linking TA activity to general stress response pathways [13].
Table 2: Major Toxin-Antitoxin Systems in Bacterial Persistence
| TA System | Type | Toxin Mechanism | Role in Persistence | Regulatory Connections |
|---|---|---|---|---|
| HipAB | II | HipA phosphorylates GltX, triggering stringent response | First chromosomal TA linked to persistence; hipA7 mutants increase persistence | Activates RelA, increasing (p)ppGpp [10] |
| MazEF | II | MazF is an endoribonuclease that cleaves mRNA | Nutrient starvation-induced persistence; among most widespread TA systems | Co-transcribed with relA (ϬS activation) and sigB (ϬB encoding) [13] |
| MqsRA | II | MqsR cleaves mRNA; MqsA regulates RpoS and CsgD | Biofilm-associated persistence; activates GhoT toxin | Represses rpoS and csgD, reducing biofilm formation [14] |
| TisB/istR | I | TisB disrupts membrane potential, reducing ATP | SOS response-induced persistence after DNA damage | Activated by DNA damage through LexA cleavage [10] |
| RelBE | II | RelE cleaves mRNA in ribosome-dependent manner | Nutritional stress-induced persistence | Activated by nutrient limitation [14] |
Beyond their role in persistence, TA systems function within broader physiological contexts, including phage inhibition through growth reduction, stabilization of genetic elements, and biofilm formation [14]. Recent evidence suggests TA systems may operate as part of an integrated nutrient-responsive cybernetic system (NRCS) that optimizes bacterial fitness by regulating population dynamics throughout the life cycle [13]. In this model, intracellular nutrient concentrations feedback to control growth, death, and growth/death arrest, with TA systems working in concert with alternative sigma factors ϬS and ϬB to efficiently transition between reproductive and survival states [13].
Stochastic Processes and Population Heterogeneity
Stochastic variation in gene expression represents a fundamental mechanism of persister formation independent of environmental cues. This phenomenon results from random fluctuations in cellular components that create distinct phenotypic states within genetically identical populations [11]. Type II persisters emerge spontaneously throughout all growth phases due to this natural heterogeneity, with varying subpopulations exhibiting differential expression of persistence-related genes.
Single-cell studies have revealed that stochastic expression of TA systems and other persistence-related genes creates a mixture of phenotypic states within bacterial populations [11]. This bet-hedging strategy ensures that a subpopulation is always prepared for sudden environmental challenges, enhancing overall population survival. Mathematical modeling of these stochastic processes has demonstrated biphasic killing curves in response to antibiotic treatment - an initial rapid decline of susceptible cells followed by a slower decline of the persistent subpopulation [10] [11].
Integrated Stress Response Pathways
Multiple signaling networks converge to regulate the entry into and exit from the persistent state:
Stringent Response: Nutrient limitation triggers RelA and SpoT to synthesize the alarmone (p)ppGpp, which dramatically reprograms cellular metabolism by downregulating energy-intensive processes and activating stress adaptation pathways [10]. (p)ppGpp directly influences persister formation through its effects on TA systems and cellular energetics.
SOS Response: DNA damage leads to LexA autocleavage, derepressing DNA repair genes and activating type I TA systems like TisB/istR that promote persistence [10] [11]. This pathway connects genotoxic stress to dormancy induction.
Quorum Sensing: Bacterial cell-cell communication via small signaling molecules influences persister formation density-dependently. In Pseudomonas aeruginosa, quorum sensing signals like phenazine pyocyanin and N-(3-oxododecanoyl)-L-homoserine lactone increase persister formation through oxidative stress and metabolic changes [2] [3].
The diagram below illustrates the integrated network of stress responses and TA systems regulating persister formation:
Experimental Approaches for Persister Research
Methodologies for Inducing and Quantifying Persisters
Research on persister cells requires specialized methodologies that account for their low abundance and transient phenotype. Standardized protocols have been developed to induce, isolate, and quantify persisters across different bacterial species and experimental conditions:
Antibiotic Killing Curves: The gold standard for persister quantification involves treating mid-log or stationary phase cultures with bactericidal antibiotics (e.g., fluoroquinolones, aminoglycosides) at 5-10× MIC and monitoring viability over time through plating and colony counting [10]. The characteristic biphasic killing curve demonstrates rapid killing of regular cells followed by a subpopulation that dies significantly slower.
Fluorescence-Activated Cell Sorting (FACS): Using fluorescent dyes that differentiate metabolic activity (e.g., CFSE, propidium iodide), researchers can isolate and quantify subpopulations with reduced metabolic activity that correlate with persistence [10].
Microfluidics and Single-Cell Analysis: Advanced platforms enable real-time observation of individual cells before, during, and after antibiotic exposure, allowing researchers to correlate persistence with specific pre-exposure states and track resuscitation dynamics [10] [1].
Table 3: Experimental Models and Their Applications in Persistence Research
| Experimental Model | Key Features | Applications | Limitations |
|---|---|---|---|
| In vitro planktonic cultures | Simplified system; controlled conditions; reproducible persister induction | Initial characterization of persister formation mechanisms; antibiotic screening | May not reflect host-environment complexity |
| Biofilm models | Reflects natural bacterial growth state; includes extracellular matrix | Studying matrix protection and niche-specific persistence; disinfectant testing | Technical challenges in complete recovery for quantification |
| Macrophage infection models | Intracellular environment; includes host-pathogen interactions | Studying immune evasion and antibiotic penetration issues | Difficult to separate bacteria from host cells for quantification |
| Animal infection models | Includes full immune system and in vivo pharmacokinetics | Studying persistence in realistic therapeutic contexts; assessing combination therapies | Ethical considerations; high cost; complex data interpretation |
The Researcher's Toolkit: Essential Reagents and Solutions
Investigating persister mechanisms requires specific reagents that target key pathways in dormancy formation. The following table details essential research tools for experimental studies:
Table 4: Essential Research Reagents for Persister Cell Studies
| Reagent Category | Specific Examples | Function/Mechanism | Application in Persistence Research |
|---|---|---|---|
| TA System Inducers | Mitomycin C (SOS inducer); serine hydroxamate (stringent response inducer) | Activates stress response pathways leading to TA system activation | Studying upstream triggers of persistence; validating TA system function |
| Protease Inhibitors | Lon protease inhibitor; ClpP inhibitors (e.g., ADEP4) | Blocks antitoxin degradation; stabilizes antitoxin levels | Testing TA activation mechanisms; combination therapies against persisters |
| Metabolic Probes | CFSE; CTC; resazurin; SYTOX Green | Labels cells based on metabolic activity or membrane integrity | Differentiating and isolating persisters from susceptible population |
| - Stringent Response Modulators: (p)ppGpp analogs; RelA inhibitors | Alarms nucleotide signaling; modulates stringent response | Investigating connection between nutrient stress and persistence | |
| Membrane-Active Compounds | CCCP; Nigericin; synthetic retinoids (CD437, CD1530) | Disrupts proton motive force and membrane integrity | Studying energy depletion-induced persistence; enhancing antibiotic uptake |
| ROS-Generating Agents | Methyl viologen; H₂O₂; MPDA/FeOOH-GOx@CaP nanoparticles | Induces oxidative stress; directly damages cellular components | Investigating oxidative stress role in persistence; developing anti-persister strategies |
Comparative Analysis of Persister Formation Mechanisms
The multiple pathways to persistence represent distinct but interconnected strategies that bacteria employ to survive adverse conditions. Each mechanism offers particular advantages under specific environmental contexts:
Toxin-antitoxin systems provide a rapid, post-translational response to stress that enables immediate metabolic downshift without requiring new gene expression [13] [14]. This makes TA systems particularly effective against sudden stressors like antibiotic exposure or phage infection. The regulatory connectivity of TA systems with global stress networks (stringent response, sigma factors) allows for coordinated population-level adaptation [13].
In contrast, stochastic persistence represents a bet-hedging strategy that prepares a subpopulation for unforeseen challenges, ensuring that some cells are always in a protected state regardless of environmental signals [11]. This mechanism is particularly advantageous in fluctuating environments where stress events are unpredictable.
From an evolutionary perspective, the coexistence of multiple persistence mechanisms within bacterial populations reflects the fitness advantage of phenotypic heterogeneity. While TA-mediated persistence requires energy expenditure for toxin and antitoxin production, and stochastic persistence carries the opportunity cost of reduced growth in the persistent subpopulation, both strategies enhance population survival under lethal stress, providing a selective advantage that maintains these traits across generations [13] [11].
The mechanistic understanding of persister formation has advanced significantly from the initial observation of antibiotic-surviving subpopulations to the current molecular-level characterization of TA systems, stochastic processes, and integrated stress responses. The evidence clearly demonstrates that bacterial persistence is not a singular phenomenon but rather a spectrum of dormant states enabled by multiple complementary mechanisms.
Future research directions should focus on elucidating the complex interactions between different persistence pathways and developing models that account for their synergistic effects. The application of single-cell technologies, advanced imaging, and multi-omics approaches will provide unprecedented resolution into the temporal dynamics of persister formation and resuscitation. From a therapeutic perspective, targeting key nodes in the persistence network - such as TA system activation, antitoxin degradation, or resuscitation signals - represents a promising approach for combating chronic and recurrent bacterial infections.
As our understanding of these dormant bacterial subpopulations continues to evolve, so too will strategies for their eradication, ultimately addressing a significant challenge in clinical management of bacterial diseases and industrial control of microbial contamination.
Bacterial persister cells represent a non-genetic, phenotypic variant of regular bacterial cells that exhibit a transient, high tolerance to antibiotic treatments by entering a dormant, metabolically inactive state [15] [2] [16]. Unlike resistant bacteria, which possess genetic mechanisms to grow in the presence of antibiotics, persisters do not grow during antibiotic exposure but can resume growth once the treatment ceases, leading to recurrent infections [17] [18]. This phenomenon is a significant contributor to the recalcitrance of chronic and biofilm-associated infections, posing a major challenge in clinical settings [15] [19]. It is estimated that over 65% of all microbial infections are associated with biofilms, which serve as reservoirs for these persistent cells [15] [20]. Their survival undermines conventional antibiotic therapies, which primarily target actively growing cells, making the development of specific anti-persister strategies a critical frontier in the fight against persistent infections [2] [3].
Molecular Mechanisms of Persister Formation and Survival
The formation and survival of persister cells are governed by a complex network of biochemical pathways that enable bacteria to survive lethal stress. Understanding these mechanisms is foundational to developing targeted elimination strategies.
Key Signaling Pathways in Persistence
The diagram below illustrates the core molecular pathways that regulate bacterial persistence.
Figure 1: Core molecular pathways regulating bacterial persistence. Environmental stressors trigger a stringent response, activating ppGpp, which induces toxin-antitoxin systems and ribosome hibernation, leading to cellular dormancy and antibiotic tolerance.
The formation of persister cells is primarily a stress response. Key pathways include:
- Toxin-Antitoxin (TA) Systems: These genetic modules encode a stable toxin that disrupts essential cellular processes (e.g., translation via mRNA cleavage) and a labile antitoxin that neutralizes the toxin [16] [17]. Under stress, proteases like Lon degrade the antitoxin, freeing the toxin to induce a dormant state. The HipA toxin, for instance, inhibits translation by phosphorylating elongation factor Tu, while MqsR acts as an mRNA interferase [17].
- The Stringent Response and (p)ppGpp: Nutrient limitation and other stresses trigger the accumulation of the alarmone (p)ppGpp [16]. This molecule acts as a central regulator of persistence by modulating RNA polymerase and promoting the transcription of stress response genes, including those in TA systems [17].
- Ribosome Hibernation: (p)ppGpp also stimulates the production of factors like Ribosome Modulation Factor (RMF) and RaiA, which inactivate ribosomes by forming 100S dimers or stabilizing inactive 70S complexes, thereby halting protein synthesis [16].
The Biofilm Environment as a Persister Niche
Biofilms are structured communities of bacteria encased in a self-produced extracellular polymeric substance (EPS) matrix. This environment is a hotspot for persister formation due to:
- Heterogeneous Microenvironments: Gradients of nutrients and oxygen within biofilms create zones of slow growth or metabolic arrest, naturally promoting dormancy [15] [19].
- Physical Protection: The EPS matrix, composed of polysaccharides, extracellular DNA, and proteins, acts as a physical barrier that impedes antibiotic penetration and protects bacteria from host immune responses [15] [19].
- Quorum Sensing (QS): Cell-to-cell communication via QS molecules can regulate persister formation. For example, in Pseudomonas aeruginosa, QS signals like phenazine pyocyanin can increase persister levels by inducing oxidative stress [2] [3].
Comparative Analysis of Persister Cell Elimination Strategies
A range of strategies has been developed to target the unique challenge of persister cells. The table below provides a high-level comparison of these approaches.
Table 1: Overview of Major Strategic Approaches to Combat Bacterial Persisters
| Strategic Approach | Core Principle | Key Advantages | Inherent Limitations |
|---|---|---|---|
| Direct Killing | Targets growth-independent structures like cell membranes or enables uncontrolled protein degradation [2] [3]. | Independent of bacterial metabolic state; effective against deep dormancy [2]. | Potential for off-target toxicity against host mammalian membranes [2] [3]. |
| Indirect Killing (Re-sensitization) | Prevents persister formation or wakes dormant cells, making them susceptible to conventional antibiotics [2] [3]. | Can leverage existing antibiotics; may reduce selection for resistance [2] [12]. | May not affect all persister sub-populations; efficacy depends on successful reactivation [3]. |
| Nanomaterial-Based | Uses nano-scale agents for physical disruption, targeted drug delivery, or generating lethal reactive oxygen species (ROS) [12]. | Enhanced biofilm penetration; multiple mechanisms of action; customizable functionality [12]. | Complex manufacturing; potential long-term toxicity and translational barriers require further study [12]. |
Direct Killing Strategies
Direct killing strategies aim to destroy persister cells by targeting essential, growth-independent cellular structures. The following table summarizes experimental data for selected direct-killing agents.
Table 2: Experimental Data for Selected Direct-Killing Anti-Persister Agents
| Agent / Compound | Proposed Mechanism of Action | Experimental Model | Reported Efficacy | Citation |
|---|---|---|---|---|
| XF-73 | Disrupts bacterial cell membrane; generates ROS upon light activation [2] [3]. | Staphylococcus aureus persisters (in vitro) [2]. | Effective against non-dividing and slow-growing cells [2]. | [2] [3] |
| ADEP4 | Activates ClpP protease, leading to uncontrolled ATP-independent protein degradation [2] [3]. | S. aureus and E. coli persisters (in vitro) [2]. | Renders cells unable to resuscitate; works synergistically with rifampicin to eradicate persisters [2]. | [2] [3] |
| Pyrazinamide (PZA) | Prodrug converted to pyrazinoic acid; disrupts membrane energetics and targets PanD protein [2] [18]. | Mycobacterium tuberculosis persisters (in vitro and in clinical use) [2] [18]. | Cornerstone of TB therapy due to unique activity against dormant bacilli [2] [18]. | [2] [3] [18] |
| Cationic Silver Nanoparticle Shelled Nanodroplets (C-AgND) | Interacts with negatively charged EPS; disrupts membranes and biofilms [2]. | S. aureus persisters within biofilms (in vitro) [2]. | Effective killing of persisters within biofilms [2]. | [2] [3] |
Experimental Protocol for Direct Killing Assay: A standard protocol for evaluating direct-killing agents involves:
- Persister Generation: A high-titer stationary-phase culture or biofilm of the target bacterium (e.g., S. aureus) is treated with a high concentration of a bactericidal antibiotic like ciprofloxacin (e.g., 10x MIC) for several hours to kill the actively growing population [17].
- Cell Washing and Confirmation: The surviving cells are washed to remove the first antibiotic and are plated on antibiotic-free media to confirm their persister status (viable but non-growing) [16].
- Treatment with Test Agent: The purified persister population is exposed to the candidate anti-persister compound (e.g., XF-73 at a range of concentrations) for a defined period.
- Viability Assessment: Serial dilutions are performed, and colonies are counted after plating to quantify the reduction in viable persister cells (CFU/mL) compared to an untreated persister control [2] [17].
Indirect Killing and Synergistic Strategies
This approach focuses on reversing the dormant state or preventing its establishment, thereby re-sensitizing persisters to conventional antibiotics.
Table 3: Experimental Data for Indirect and Synergistic Anti-Persister Strategies
| Strategy / Compound | Proposed Mechanism of Action | Experimental Model | Reported Efficacy / Synergy | Citation |
|---|---|---|---|---|
| Metabolic Reactivators (e.g., Mannitol, Serine) | Reactivates bacterial metabolism by stimulating central carbon metabolism or the electron transport chain [12]. | E. coli and S. aureus persisters (in vitro) [12]. | "Wake-and-kill"; re-sensitizes persisters to aminoglycoside antibiotics [12]. | [12] |
| Membrane Permeabilizers (e.g., MB6, PMBN) | Disrupts the integrity of the bacterial membrane, increasing uptake of co-administered antibiotics [2] [3]. | MRSA persisters (in vitro) [2]. | Cotreatment with gentamicin showed strong anti-persister activity [2]. | [2] [3] |
| H₂S Scavengers / CSE Inhibitors | Inhibits bacterial hydrogen sulfide (H₂S) biogenesis, which protects under stress [2] [3]. | S. aureus, P. aeruginosa, E. coli persisters (in vitro) [2]. | Reduces persister formation and potentiates killing by gentamicin [2]. | [2] [3] |
| Quorum Sensing Inhibitors (e.g., Brominated Furanones) | Inhibits cell-cell communication systems that regulate multicellular behaviors like biofilm and persister formation [2]. | P. aeruginosa (in vitro) [2]. | Reduces persister formation without affecting growth [2]. | [2] [3] |
Experimental Protocol for Synergy Assay (Checkboard):
- Persister Preparation: Persister cells are generated and purified as described in the direct-killing protocol.
- Checkerboard Setup: A range of concentrations of the conventional antibiotic (e.g., gentamicin, from 0 to 8x MIC) is combined with a range of concentrations of the sensitizing agent (e.g., a membrane permeabilizer like MB6) in a 96-well microtiter plate.
- Inoculation and Incubation: The purified persister suspension is added to each well.
- Analysis: After incubation, viability is assessed. The Fractional Inhibitory Concentration (FIC) index is calculated to determine if the interaction is synergistic (FIC ≤ 0.5) [2].
Emerging Nanomaterial-Based Strategies
Nanotechnology offers innovative tools to combat persisters, leveraging unique physicochemical properties for targeted action.
Table 4: Emerging Nanoagents for Targeting Bacterial Persisters
| Nanoagent | Composition | Mechanism of Action | Infection Model | Citation |
|---|---|---|---|---|
| Caff-AuNPs | Caffeine-functionalized Gold Nanoparticles | Disrupts mature biofilms and eradicates embedded dormant cells [12]. | In vitro, planktonic and biofilm-associated persisters [12]. | [12] |
| AuNC@CPP | Gold Nanoclusters with Cell-Penetrating Peptide | Induces membrane hyperpolarization by disrupting the proton gradient [12]. | Chronic suppurative otitis media (in vitro) [12]. | [12] |
| PS+(triEG-alt-octyl)PDA | Cationic Polymer on Polydopamine Nanoparticles | Photothermal-triggered release reactivates persisters via the electron transport chain and then disrupts membranes [12]. | In vitro, biofilm-associated persisters [12]. | [12] |
| MPDA/FeOOH-GOx@CaP | ROS-generating Hydrogel Microspheres | Glucose oxidase produces H₂O₂, converted to lethal hydroxyl radicals via Fenton-like reactions in the acidic biofilm microenvironment [12]. | Prosthetic joint infection model (in vitro) [12]. | [12] |
The Scientist's Toolkit: Key Reagents and Experimental Models
This section details essential reagents, compounds, and models used in persister research, providing a resource for designing experiments.
Table 5: Key Research Reagent Solutions for Persister Cell Studies
| Reagent / Material | Function in Research | Specific Examples & Notes |
|---|---|---|
| Membrane-Targeting Compounds | Directly lyse persister cells by disrupting cell envelope integrity, independent of metabolism [2] [3]. | XF-73, SA-558, synthetic retinoids (CD437, CD1530), thymol conjugates (TPP-Thy3) [2] [3]. |
| Metabolic Modulators | Reactivate dormant persisters ("wake") or inhibit their formation, re-sensitizing them to antibiotics [2] [12]. | Reactivators: Mannitol, serine. Inhibitors: Nitric oxide (NO), Cystathionine γ-lyase (CSE) inhibitors, medium-chain fatty acids (e.g., lauric acid) [2] [3] [12]. |
| Synergistic Sensitizers | Used in combination with conventional antibiotics to enhance their uptake or efficacy against persisters [2] [3]. | Membrane permeabilizers (PMBN, SPR741), H₂S scavengers [2] [3]. |
| Engineered Nanomaterials | Act as delivery vehicles for antimicrobials or possess intrinsic anti-persister activity (e.g., ROS generation, physical disruption) [12]. | Gold nanoparticles (Caff-AuNPs, AuNC@CPP), ROS-generating microspheres (MPDA/FeOOH-GOx@CaP), polymer nanocomposites [12]. |
| Bacterial Strains & Models | Provide relevant experimental systems for studying persistence and testing interventions. | Laboratory Strains: E. coli K-12, P. aeruginosa PAO1, S. aureus USA300 [15] [17]. Clinical Isolates: High-persister (hip) mutants from cystic fibrosis (CF) patients [15] [20]. Biofilm Models: Static (microtiter plate), flow-cell systems, in vivo catheter models [19]. |
The following diagram outlines a generalized workflow for screening and evaluating potential anti-persister therapeutic agents.
Figure 2: Anti-persister therapeutic development workflow. The process progresses from simple in vitro screens to complex in vivo models, with parallel mechanism-of-action studies.
The eradication of bacterial persister cells is paramount for successfully treating chronic and biofilm-associated infections. While conventional antibiotics remain ineffective, research has yielded a diversified arsenal of strategies, from direct membrane-lysing agents and metabolic re-sensitizers to sophisticated nanotechnology-based solutions. The experimental data compiled in this guide demonstrates that no single strategy is a universal solution; each possesses distinct advantages and limitations. Future progress will likely depend on combination therapies that simultaneously target multiple vulnerabilities—for instance, using a nanomaterial to disrupt the biofilm and deliver a metabolic activator alongside a conventional antibiotic. Furthermore, bridging the gap between promising in vitro results and clinical success requires standardized models and a deeper understanding of persister physiology in host environments. The continued development and comparison of these innovative strategies, as outlined here, provide a clear path toward overcoming one of the most stubborn challenges in modern antimicrobial therapy.
Bacterial persistence represents a significant challenge in clinical medicine, contributing to chronic and relapsing infections. Persisters are a subpopulation of genetically susceptible cells that exhibit transient, high-level tolerance to antibiotic treatment without acquiring heritable resistance mutations [18] [10]. This phenomenon was first identified by Joseph Bigger in 1944 when he observed that penicillin failed to eradicate all Staphylococcus cells, leaving a small fraction of survivors he termed "persisters" [18] [11]. The classification of persisters into distinct types provides a crucial framework for understanding their formation mechanisms, metabolic diversity, and implications for treatment strategies. This review systematically compares Type I, II, and III persister cells, examining their characteristic features, molecular drivers, and the experimental approaches essential for their study and eradication.
Classification and Comparative Analysis of Persister Types
Persister cells are broadly categorized based on their formation mechanisms, triggers, and metabolic states. The established classification system recognizes three primary types, each with distinct characteristics and physiological profiles.
Table 1: Comparative Characteristics of Persister Cell Types
| Feature | Type I (Triggered) | Type II (Stochastic) | Type III (Specialized) |
|---|---|---|---|
| Formation Trigger | Environmental stress (e.g., starvation, stationary phase) [11] | Spontaneous, stochastic errors during replication [11] | Antibiotic-specific stress signals or spontaneous mechanisms [11] |
| Growth State Before Antibiotic Exposure | Non-growing or growth-arrested [11] | Slow-growing [11] | Often actively growing [21] [11] |
| Primary Metabolic State | Dormant, low metabolic activity | Reduced but continuous metabolism | Variable, can be metabolically active |
| Key Regulatory Factors | Toxin-Antitoxin (TA) modules, (p)ppGpp [11] | TA modules, (p)ppGpp, stochastic gene expression [22] [11] | Antibiotic-specific mechanisms (e.g., low enzyme levels for prodrug activation) [11] |
| Persistence in Biofilms | Common | Common | Yes, can be induced by stress signals [8] |
Table 2: Elimination Strategies and Vulnerabilities by Persister Type
| Strategy | Mechanism of Action | Effectiveness Against Persister Type |
|---|---|---|
| Direct Membrane Attack | Disrupts cell membrane integrity, causes lysis [2] [3] | Effective against all types (growth-independent) |
| Metabolite Reprogramming ("Wake and Kill") | Reactivates metabolism to sensitize cells to antibiotics [8] | Most effective against Type I and II |
| Inhibition of Persister Formation | Targets pathways like (p)ppGpp accumulation or H₂S biogenesis [2] [3] | Prevents formation of Type I and II |
| Synergy with Antibiotics | Membrane permeabilizers increase antibiotic uptake [2] [3] | Enhances killing of all types, particularly Type III |
The following diagram illustrates the core signaling pathways and regulatory networks that drive the formation and maintenance of the different persister types, integrating triggers like stress, stochastic events, and antibiotic-specific actions.
Molecular Mechanisms and Metabolic Underpinnings
The formation and survival of persister cells are governed by complex molecular networks that regulate bacterial metabolism and stress responses.
Core Regulatory Systems
Several interconnected systems are central to persister formation across types. The Stringent Response, mediated by the alarmone (p)ppGpp, acts as a master regulator during nutrient limitation. (p)ppGpp accumulates and drastically reprograms cellular metabolism, shutting down energy-intensive processes like ribosome synthesis and promoting a dormant state [22] [10] [8]. This response is crucial for the formation of Type I persisters and also plays a role in Type II persistence.
Toxin-Antitoxin (TA) systems are another key component. These genetic modules consist of a stable toxin that can disrupt essential cellular processes (e.g., protein translation, DNA replication) and a labile antitoxin that neutralizes the toxin. Under stress, proteases degrade the antitoxin, allowing the toxin to induce dormancy [10] [11]. For example, in E. coli, the HipA toxin phosphorylates a glutamyl-tRNA synthetase, inhibiting translation and triggering persistence via the stringent response [10]. The TisB toxin can form pores in the inner membrane, dissipating the proton motive force (PMF) and reducing ATP levels, leading to a dormant state [10].
Metabolic Basis of Tolerance and Reactivation
A defining feature of Type I and II persisters is a reduction in metabolic activity, which underlies their antibiotic tolerance. Conventional antibiotics primarily target active processes like cell wall synthesis, DNA replication, and protein synthesis. In dormant persisters, these targets are largely inactive, rendering the drugs ineffective [2] [3] [8].
This metabolic dormancy exists on a continuum. Studies using ¹³C-isotopolog profiling on stationary-phase Staphylococcus aureus challenged with daptomycin have revealed that persisters maintain a baseline level of metabolic activity, with active glycolysis, TCA cycle, and amino acid anabolism [23]. This residual metabolism is critical for maintaining cell integrity and the potential for "resuscitation."
The "Wake and Kill" strategy exploits this metabolic plasticity. Research shows that certain metabolites can reprogram persister metabolism, reversing tolerance. For instance, mannitol and fructose can restore the PMF, facilitating the uptake of aminoglycoside antibiotics and leading to effective killing [8]. Similarly, exogenous pyruvate promotes the uptake of gentamicin in Vibrio alginolyticus [8]. This approach is particularly promising for eradicating Type I and II persisters.
Advanced Research Methodologies and Tools
Studying persisters is challenging due to their low abundance and transient phenotype. Advanced methodologies are required for their isolation, characterization, and analysis.
Experimental Workflows
A standard protocol for studying persister recovery involves several key stages. The process begins with obtaining a pure bacterial culture and exposing it to a high concentration of a bactericidal antibiotic for a defined period. This is followed by the removal of the antibiotic, typically through washing or dilution. The subsequent recovery phase is monitored using spectrophotometry (OD₆₀₀) to track population regrowth and flow cytometry to analyze the physiological states of individual cells during resuscitation [24]. This single-cell approach is vital given the heterogeneity of persister populations.
Microfluidic devices, such as the Membrane-Covered Microchamber Array (MCMA), have revolutionized single-cell analysis. These devices allow researchers to trap and observe over one million individual cells, tracking their lineage and morphological changes before, during, and after antibiotic exposure [21]. This technology was instrumental in demonstrating that many persisters from exponential growth phases are actually growing cells before treatment, a hallmark of Type II and III persistence [21].
The Scientist's Toolkit
Table 3: Key Research Reagent Solutions and Experimental Tools
| Reagent/Tool | Function/Application | Relevance to Persister Research |
|---|---|---|
| Microfluidic Devices (e.g., MCMA) | Single-cell confinement and long-term imaging [21] | Visualizing lineage histories and heterogeneous responses of Types I, II, and III persisters. |
| Fluorescent Reporter Proteins (e.g., GFP, mCherry) | Tagging and visualizing specific proteins or promoter activities. | Monitoring stress response pathways (e.g., RpoS) and metabolic activity in real-time. |
| Flow Cytometry | Multi-parameter analysis of single cells in a liquid suspension. | Quantifying physiological states (e.g., membrane potential, respiratory activity) in a recovering persister population [24]. |
| Carbon-13 (¹³C) Labeled Metabolites | Tracing metabolic flux through biochemical pathways. | Profiling the active metabolism in persister cells (e.g., in S. aureus) [23]. |
| Lethal-dose Antibiotics (e.g., Amp, CPFX) | Selective killing of non-persister cells. | Isolating and enriching the persister subpopulation from a larger culture for downstream analysis [21]. |
The following diagram outlines a generalized experimental workflow for isolating and analyzing persister cells, from initial culture to single-cell resolution.
The distinct characteristics of Type I, II, and III persisters necessitate tailored therapeutic approaches. A one-size-fits-all strategy is unlikely to succeed. For instance, Type I persisters, being deeply dormant, may be best targeted by direct-killing agents like membrane-disrupting compounds (e.g., synthetic cation transporters, antimicrobial peptides) or compounds that induce uncontrolled protein degradation (e.g., ADEP4) [2] [3]. In contrast, Type II and III persisters, which may retain some metabolic activity, could be vulnerable to "Wake and Kill" strategies that use metabolite adjuvants to re-sensitize them to conventional antibiotics [8].
Combination therapies that simultaneously target multiple persister types and active populations are the most promising path forward. For example, pairing an antibiotic with a membrane-permeabilizing agent can enhance drug uptake and kill a broader range of persisters [2] [3]. Furthermore, understanding the specific triggers and molecular pathways of each persister type opens the door to inhibitors that prevent their formation in the first place, such as quorum sensing inhibitors or molecules that reduce (p)ppGpp accumulation [2] [3].
In conclusion, the classification of persisters into Types I, II, and III provides an essential framework for understanding their metabolic diversity and complex biology. This refined understanding is pivotal for guiding the development of novel diagnostic tools and therapeutic regimens. Future research focusing on the precise metabolic vulnerabilities of each persister type, especially within the complex environment of biofilms and host tissues, will be critical for winning the battle against persistent bacterial infections.
The Anti-Persister Arsenal: From Direct Killing to Synergistic Approaches
Persister cells, which are dormant, non-dividing phenotypic variants found within bacterial populations and tumors, represent a major therapeutic challenge. Their low metabolic activity allows them to tolerate conventional treatments that target rapidly dividing cells or active growth processes. Direct killing strategies have emerged as a promising approach to eradicate these persistent cells by targeting fundamental, growth-state-independent cellular structures and processes. Unlike conventional antibiotics or chemotherapies, these strategies aim to disrupt essential cellular integrity or cause irreversible damage regardless of the target cell's metabolic state.
The most prominent direct killing approaches focus on two key areas: compromising the structural integrity of the cell membrane and disrupting essential cellular processes that remain active even in dormant cells. These strategies are particularly valuable because they do not require the target cells to be in an active growth phase, bypassing the primary mechanism of persister tolerance. This article provides a comprehensive comparison of these direct killing methodologies, examining their mechanisms, experimental validation, and relative performance across different persister cell models.
Membrane-Targeting Strategies
Mechanisms of Membrane Disruption
The cell membrane serves as a fundamental barrier maintaining cellular integrity, making it an attractive target for direct killing approaches. Membrane-targeting agents exert their effects through several distinct mechanisms that compromise membrane function and structure:
Electrostatic Interaction and Disruption: Many membrane-targeting compounds exploit differences in membrane composition between target and host cells. Bacterial membranes contain abundant negatively charged phospholipids like phosphatidylglycerol (PG) and cardiolipin in their outer leaflets, while cancer cells expose phosphatidylserine (PS) and other anionic molecules externally. Cationic antimicrobial peptides (AMPs) and synthetic membrane-targeting agents selectively interact with these negatively charged membranes through electrostatic attraction, leading to membrane disruption [25]. This interaction can cause depolarization, increased permeability, and eventual cell lysis.
Physical Membrane Perturbation: Beyond electrostatic interactions, many membrane-targeting agents incorporate hydrophobic regions that penetrate the lipid bilayer's interior. This penetration can lead to the formation of pores, membrane thinning, or complete dissolution of membrane integrity. The resulting loss of membrane potential and leakage of cellular contents proves rapidly lethal to both bacterial and cancer persister cells [25] [3].
Reactive Oxygen Species (ROS) Generation: Some membrane-targeting approaches, including certain photosensitizers used in nanodynamic therapies, generate lethal levels of reactive oxygen species upon activation. These ROS oxidize membrane lipids and proteins, amplifying the initial membrane damage and leading to comprehensive cellular destruction [26].
Key Membrane-Targeting Agents and Their Efficacy
Table 1: Comparison of Membrane-Targeting Agents Against Persister Cells
| Agent Category | Specific Examples | Primary Target | Reported Efficacy | Key Limitations |
|---|---|---|---|---|
| Cationic Peptides & Mimetics | 2D-24, AM-0016, IMT-P8 | Bacterial membrane integrity | Effective against S. aureus and E. coli persisters [2] | Potential toxicity to mammalian cells |
| Small Molecule Membrane Disruptors | XF-70, XF-73, SA-558 | Bacterial membrane potential | Kills non-dividing S. aureus cells; SA-558 disrupts homeostasis [2] [3] | Limited spectrum for some compounds |
| Nanoparticle Systems | Hb-Naf@RBCM NPs, C-AgND | Multiple membrane components | Effective against S. aureus persisters in biofilms [2] [3] | Complex manufacturing and characterization |
| Anticancer Peptides | Various cationic peptides | Exposed PS on cancer cells | Induces cytoplasmic leakage and ROS in cancer cells [25] | Selectivity challenges based on membrane charge differences |
| Nanodynamic Therapy | Photosensitizer-loaded CNPs | General membrane integrity | ROS generation under external energy source [26] | Requires external activation energy |
The diversity of membrane-targeting approaches reflects the adaptability of this strategy across different persister cell types. For bacterial persisters, synthetic compounds like XF-70 and XF-73 have demonstrated particular efficacy against Staphylococcus aureus by disrupting membrane integrity even in slow-growing and non-dividing cells [2] [3]. Similarly, SA-558 functions as a synthetic cation transporter that disrupts bacterial homeostasis, ultimately leading to autolysis of persister cells [3].
In anticancer applications, membrane-targeting strategies leverage the differential composition of cancer cell membranes, particularly the external exposure of phosphatidylserine, which is typically confined to the inner leaflet in healthy cells [25]. This fundamental difference in membrane architecture enables selective targeting of cancer persisters while minimizing damage to normal cells.
Advanced nanoparticle systems represent a convergence of these approaches, combining membrane-targeting capabilities with enhanced delivery mechanisms. For instance, red blood cell membrane-coated nanoparticles (Hb-Naf@RBCM NPs) incorporating naftifine and oxygenated hemoglobin have demonstrated effective killing of S. aureus persisters, including those embedded in biofilms [2]. Similarly, cationic silver nanoparticle-shelled nanodroplets (C-AgND) interact with negatively charged components of the extracellular polymeric substance, enabling effective penetration and killing of persisters within biofilms [3].
Diagram 1: Mechanisms of membrane-targeting agents showing common pathways to cell disruption. The diagram illustrates how cationic agents exploit differences in membrane composition between bacterial and cancer cells, leading to various disruptive mechanisms and ultimately cell lysis.
Targeting Essential Cellular Processes
Disruption of Critical Enzymes and Protein Homeostasis
While membrane targeting represents a physical approach to persister eradication, complementary strategies focus on disrupting essential cellular processes that remain vulnerable even in dormant cells. These approaches target fundamental biochemical pathways and protein homeostasis mechanisms that persister cells must maintain to survive and eventually resuscitate:
Protein Degradation Pathway Activation: Certain direct killing agents hijack or activate cellular proteolytic machinery to cause uncontrolled protein degradation. ADEP4, a semi-synthetic acyldepsipeptide, represents a promising example that binds to the ClpP protease and induces conformational changes. This activation enables ATP-independent protein degradation, resulting in the breakdown of hundreds of intracellular proteins, including metabolic enzymes essential for persister wake-up and recovery [2] [3]. The destruction of these essential components renders persister cells incapable of resuming growth even after favorable conditions return.
Enzyme Targeting in Metabolic Pathways: Pyrazinamide, a frontline tuberculosis therapeutic, demonstrates effective targeting of Mycobacterium tuberculosis persisters through a multi-faceted mechanism. Its active form, pyrazinoic acid, disrupts membrane energetics while also binding to PanD, an enzyme essential for coenzyme A biosynthesis. This binding triggers degradation of PanD by the ClpC1-ClpP complex, effectively disrupting multiple cellular processes simultaneously [3]. The multi-target nature of this approach reduces the likelihood of resistance development.
Interference with Death Pathway Signaling: Recent cancer research has revealed a paradoxical mechanism where surviving persister cells hijack enzymes typically associated with cell death to facilitate their regrowth. In models of melanoma, lung, and breast cancers, persister cells that survive initial treatment display chronic, low-level activation of DNA fragmentation factor B (DFFB), an enzyme normally involved in DNA fragmentation during apoptosis. At sublethal levels, this DFFB activation interferes with growth-suppressing signals like interferon signaling, enabling persister cell regrowth. Notably, removing DFFB keeps cancer persister cells dormant and prevents regrowth during drug treatment, identifying this non-essential enzyme in normal cells as a promising target for combination therapies [27].
Energy and Metabolic Pathway Disruption
Beyond direct enzyme targeting, disruption of cellular energy management and metabolic pathways presents another viable strategy for persister elimination:
Membrane Energetics Disruption: Several effective persister control agents operate by compromising bacterial membrane energetics and proton motive force (PMF). Compounds like pinaverium bromide (PB) disrupt PMF and generate reactive oxygen species, effectively undermining the delicate energy balance that persister cells maintain despite their dormant state [3]. Similarly, nitric oxide (NO) acts as a metabolic disruptor, interfering with energy production pathways essential for persister maintenance and eventual resuscitation [2].
Metabolic Cofactor Depletion: The targeted degradation of metabolic cofactors and essential small molecules represents another effective strategy. As demonstrated in the pyrazinamide/PanD mechanism, disrupting the biosynthesis of coenzyme A through PanD degradation effectively starves persister cells of essential metabolic cofactors, preventing their recovery and eventual proliferation [3].
Table 2: Agents Targeting Essential Cellular Processes in Persister Cells
| Agent Category | Specific Examples | Cellular Target | Mechanism of Action | Therapeutic Applications |
|---|---|---|---|---|
| Protease Activators | ADEP4 | ClpP protease | Causes conformational change enabling ATP-independent protein degradation [2] [3] | Broad-spectrum antibacterial |
| Metabolic Disruptors | Pyrazinamide/Pyrazinoic acid | Membrane energetics & PanD enzyme | Disrupts membrane potential and triggers PanD degradation [3] | Mycobacterium tuberculosis persisters |
| Death Pathway Exploiters | DFFB inhibition | DNA fragmentation factor B | Blocks sublethal death signaling that promotes regrowth [27] | Melanoma, lung, and breast cancer persisters |
| Energy Pathway Disruptors | Pinaverium bromide (PB) | Proton motive force (PMF) | Disrupts PMF and generates ROS [3] | Bacterial persister control |
| Metabolic Modulators | Nitric oxide (NO) | Multiple metabolic enzymes | Acts as metabolic disruptor [2] | Reduces persister formation |
The strategic targeting of essential cellular processes offers the advantage of exploiting vulnerabilities that persister cells cannot easily circumvent through dormancy alone. Unlike conventional treatments that require active cellular processes, these approaches recognize that dormant cells must still maintain basic homeostasis and preserve the machinery necessary for eventual resuscitation.
Diagram 2: Strategies for targeting essential cellular processes in persister cells, showing three primary approaches and their outcomes.
Experimental Protocols and Methodologies
Standardized Assays for Evaluating Direct Killing Efficacy
Robust experimental protocols are essential for accurately assessing the efficacy of direct killing strategies against persister cells. The following methodologies represent standardized approaches used across the field:
Persister Cell Isolation and Enrichment:
- High-Dose Antibiotic Selection: Bacterial persisters are typically isolated by treating mid-log phase cultures with high concentrations of bactericidal antibiotics (e.g., 10-100× MIC of fluoroquinolones or aminoglycosides) for 3-6 hours, followed by extensive washing to remove the antibiotics and dead cells [2] [3]. This approach enriches for the non-growing, tolerant persister subpopulation.
- Drug Selection in Cancer Models: Cancer persister cells are often generated by exposing sensitive cell lines to targeted therapies (e.g., EGFR inhibitors for NSCLC, BRAF inhibitors for melanoma) at clinically relevant concentrations for 7-14 days. The surviving population, typically representing 0.1-5% of the original culture, is characterized as drug-tolerant persisters [1].
- Fluorescence-Activated Cell Sorting (FACS): For more precise isolation, dye-based staining (e.g., membrane potential-sensitive dyes, efflux pump substrates) can be employed to distinguish and sort persister subpopulations based on their reduced metabolic activity [1].
Membrane Integrity and Viability Assessment:
- Membrane Permeability Assays: SYTOX Green and propidium iodide uptake are standard methods for evaluating membrane integrity. These fluorescent dyes are excluded from viable cells but penetrate and bind nucleic acids in membrane-compromised cells, providing quantitative assessment of membrane disruption [2] [25].
- CFU Enumeration: The gold standard for assessing bacterial persister killing involves determining colony-forming units (CFU) before and after treatment. True persister eradication is demonstrated by a ≥3-log reduction in viable counts after direct killing treatment [3].
- ATP Content Measurement: Cellular ATP levels, measured via luciferase-based assays, provide a sensitive indicator of metabolic activity and cell viability following treatment with membrane-targeting agents [1].
Time-Kill Kinetics Analysis: Comprehensive time-kill assays are essential for distinguishing between bactericidal/cytotoxic activity and true persister eradication. These experiments typically monitor viability over 24-72 hours, with effective direct killing agents demonstrating rapid, concentration-dependent reduction in viable counts without regrowth upon drug removal [2] [3].
Advanced Mechanistic Studies
Understanding the specific mechanisms of action for direct killing agents requires specialized experimental approaches:
- Membrane Depolarization Measurements: The fluorescent dye 3,3'-diethyloxacarbocyanine iodide (DiOC₂(3)) is commonly used to monitor changes in membrane potential following treatment with membrane-targeting agents. Flow cytometric analysis of stained cells provides quantitative assessment of membrane depolarization [25].
- Reactive Oxygen Species Detection: Intracellular ROS generation can be quantified using fluorescent probes such as 2',7'-dichlorodihydrofluorescein diacetate (H₂DCFDA) or dihydroethidium (DHE). Increased fluorescence following treatment indicates ROS production, which often contributes to the lethal effects of membrane-targeting agents [26].
- Protein Degradation Monitoring: For agents like ADEP4 that activate proteolytic systems, western blot analysis of specific protein substrates (e.g., FabD, PanB) over time provides direct evidence of uncontrolled protein degradation [3].
- Electron Microscopy: Transmission and scanning electron microscopy offer visual evidence of membrane damage, including blebbing, pore formation, and complete membrane disintegration following treatment with membrane-targeting agents [25].
Comparative Performance Analysis
Efficacy Across Persister Cell Types
Table 3: Comparative Performance of Direct Killing Strategies Against Different Persister Cell Types
| Strategy Category | Bacterial Persisters | Cancer DTP Cells | Biofilm-Embedded Persisters | Key Advantages | Primary Limitations |
|---|---|---|---|---|---|
| Membrane-Targeting Agents | Highly effective against Gram-positive pathogens; variable against Gram-negative [2] [3] | Moderate efficacy, dependent on membrane charge differences [25] | Good penetration and efficacy against biofilm populations [2] | Rapid killing; independence from metabolic state | Potential toxicity to host cells; variable spectrum |
| Protease Activators | Broad-spectrum activity against Gram-positive bacteria [3] | Limited direct evidence in cancer models | Reduced activity in biofilm environments | Novel mechanism; low resistance potential | Pharmacokinetic challenges; limited spectrum |
| Metabolic Disruptors | Species-specific (e.g., pyrazinamide for Mtb) [3] | Emerging evidence for cancer metabolic dependencies [1] | Variable efficacy based on biofilm metabolism | High selectivity for specific pathogens | Narrow spectrum; context-dependent efficacy |
| Nanoparticle Systems | Enhanced targeting and penetration [2] [3] | Promising for targeted delivery to cancer DTPs [28] [29] | Superior penetration and retention in biofilms [2] | Multifunctional platforms; enhanced targeting | Complex manufacturing; potential immunogenicity |
| Signaling Interference | Limited application in bacterial systems | Highly specific for cancer DTP pathways [27] | Not typically applied | High specificity for persistence mechanisms | Limited to specific cancer types with defined pathways |
The comparative analysis reveals that membrane-targeting strategies generally offer broader applicability across different persister cell types, while approaches targeting essential cellular processes tend to demonstrate more specific, context-dependent efficacy. For bacterial persisters, direct membrane disruption consistently shows robust activity, particularly against Gram-positive pathogens, with agents like XF-73 and SA-558 demonstrating potent killing against Staphylococcus aureus persisters [2] [3].
In anticancer applications, the recently discovered DFFB mechanism represents a paradigm shift in persister targeting, focusing not on direct killing but on preventing the regrowth of survived persister cells [27]. This approach highlights the importance of understanding the unique biology of cancer persisters, which may leverage sublethal activation of typically lethal pathways to facilitate their survival and recurrence.
Nanoparticle-based delivery systems enhance both membrane-targeting and essential process-disrupting strategies by improving drug delivery to persistent cell populations. Cancer cell membrane-coated nanoparticles (CCM-NPs), for instance, leverage homologous targeting to selectively accumulate in tumor tissues, while also preserving immune evasion proteins that prolong circulation time [28]. Similarly, red blood cell membrane-coated nanoparticles (RBCM) demonstrate extended circulation and enhanced tumor accumulation, improving the delivery of encapsulated therapeutic agents to persister cell populations [29].
Resistance Development and Safety Profiles
A critical consideration in evaluating direct killing strategies is their potential for resistance development and associated safety profiles:
Resistance Development: Membrane-targeting agents generally demonstrate lower resistance potential compared to conventional antibiotics, as the target (cell membrane) cannot be easily modified through single genetic mutations. However, bacteria can develop resistance through membrane composition alterations, efflux pump upregulation, and membrane repair mechanisms [25]. Strategies targeting essential cellular processes like ADEP4-activated protein degradation show particularly low resistance frequencies in laboratory studies, making them attractive for persistent infection treatment [3].
Selectivity and Toxicity: The primary challenge for membrane-targeting approaches is achieving selective toxicity against target versus host cells. Strategies leveraging differences in membrane composition (e.g., negative charge in bacterial vs. mammalian membranes) enable selective targeting, though complete specificity remains challenging [25]. Agents targeting non-essential host proteins, like DFFB in cancer persisters, offer improved safety profiles, as normal cells tolerate inhibition of these targets [27].
Therapeutic Index: The combination of membrane-targeting agents with conventional antibiotics often demonstrates synergistic effects, allowing lower concentrations of both agents to be used while maintaining efficacy. This combination approach can significantly improve the therapeutic index by reducing dose-related toxicity while enhancing persister eradication [2] [3].
The Scientist's Toolkit: Essential Research Reagents
Table 4: Key Research Reagents for Studying Direct Killing Approaches
| Reagent Category | Specific Examples | Primary Research Application | Key Considerations |
|---|---|---|---|
| Membrane Integrity Indicators | SYTOX Green, Propidium Iodide, DiOC₂(3) | Quantitative assessment of membrane disruption and depolarization [2] [25] | Distinguish primary vs. secondary membrane damage; optimize loading conditions |
| Viability Assay Systems | CFU enumeration, ATP-based assays (CellTiter-Glo), resazurin reduction | Standardized assessment of persister killing and metabolic activity [3] [1] | CFU remains gold standard; metabolic assays may not distinguish static vs. cidal effects |
| ROS Detection Probes | H₂DCFDA, DHE, MitoSOX Red | Quantification of reactive oxygen species generation [26] | Consider compartment-specific ROS; use with appropriate antioxidants controls |
| Persister Isolation Tools | Antibiotic selection (ciprofloxacin, gentamicin), FACS sorting | Generation of enriched persister populations for mechanistic studies [2] [1] | Validate persistence phenotype (reversibility, non-genetic basis) |
| Model System Reagents | 3D tumor spheroids, biofilm reactors, patient-derived organoids | Physiologically relevant models for evaluating penetration and efficacy [28] [1] | Balance physiological relevance with experimental tractability |
| Membrane-Coated Nanoparticles | CCM-NPs, RBCM-NPs, macrophage membrane NPs | Advanced delivery systems for targeted persister eradication [28] [29] | Standardize membrane extraction and characterization protocols |
This toolkit enables researchers to comprehensively evaluate both the efficacy and mechanisms of direct killing strategies. The selection of appropriate reagents and model systems is critical for generating physiologically relevant data that can effectively guide therapeutic development.
Direct killing strategies targeting cell membranes and essential cellular processes represent a promising frontier in the battle against persister cells. The comparative analysis presented herein demonstrates that membrane-targeting approaches offer broad applicability and rapid killing across diverse persister types, while strategies targeting essential cellular processes provide greater specificity and novel mechanisms of action. The convergence of these approaches through advanced nanoparticle delivery systems further enhances their potential by improving targeting and reducing off-site toxicity.
Future directions in this field will likely focus on combinatorial approaches that leverage the strengths of both strategies while mitigating their individual limitations. The development of resistance-resistant therapies that simultaneously target membrane integrity and essential processes represents a particularly promising avenue. Furthermore, improved understanding of persister cell biology, including their unique metabolic states and signaling pathways, will continue to reveal new vulnerabilities for targeted eradication.
As research progresses, standardized experimental protocols and rigorous comparative assessments will be essential for translating these direct killing strategies from laboratory concepts to clinical realities. The tools and frameworks presented in this comparison provide a foundation for such systematic evaluation, ultimately contributing to more effective therapies against persistent bacterial infections and cancer recurrence.
Persister cells, characterized by their metabolic dormancy and enhanced tolerance to conventional antibiotics, represent a significant challenge in eradicating persistent infections. Membrane-targeting agents have emerged as a promising therapeutic strategy to combat these recalcitrant bacterial populations. Unlike traditional antibiotics that act on specific intracellular targets, these agents primarily disrupt the structural and functional integrity of microbial membranes, a mechanism against which bacteria develop resistance less readily [30] [31]. This review provides a comparative analysis of three principal classes of membrane-targeting agents—cationic peptides, synthetic transporters, and nanoparticles—evaluating their mechanisms, efficacy, and practical application in persister cell elimination strategies.
The fundamental rationale for targeting bacterial membranes lies in the pronounced electrostatic differences between microbial and mammalian cell membranes. Bacterial membranes are rich in anionic phospholipids such as phosphatidylglycerol (POPG) and cardiolipin (CL), conferring a net negative charge that attracts cationic agents [30] [31]. In contrast, mammalian cell membranes predominantly consist of zwitterionic phospholipids like phosphatidylcholine and sphingomyelin, and contain cholesterol, which stabilizes the bilayer and reduces susceptibility to cationic membrane disruptors [30]. This charge selectivity enables membrane-targeting agents to preferentially interact with and disrupt bacterial membranes while minimizing damage to host cells, making them particularly valuable for eliminating persister cells that resist conventional therapies [31].
Comparative Mechanisms of Membrane-Targeting Agents
Cationic Antimicrobial Peptides (AMPs)
Cationic Antimicrobial Peptides represent a class of innate immune defense molecules that exhibit potent activity against persister cells through membrane-disruptive actions. Their mechanism is primarily governed by two structural features: a net positive charge (typically +2 to +9) and an amphipathic structure, which enables them to interact with and disrupt bacterial membranes [31] [32]. The mechanistic actions of AMPs can be categorized into several models:
- Barrel-Stave Pore Model: Peptides insert perpendicularly into the membrane bilayer, forming transmembrane pores where the hydrophobic regions face the lipid core and hydrophilic regions line the pore interior, causing rapid ion efflux and loss of membrane integrity [31] [33].
- Toroidal Pore Model: Peptides induce lipid monolayers to bend continuously, forming pores lined by both peptide molecules and lipid head groups, leading to membrane disruption [31] [33].
- Carpet Model: Peptides cover the membrane surface in a "carpet-like" manner, causing membrane disintegration through detergent-like effects once a threshold concentration is reached [31] [33].
- Detergent-like Model: Peptides directly dissolve the membrane structure through extensive hydrophobic interactions, resulting in micellization and complete membrane breakdown [33].
Beyond these membrane-disruptive mechanisms, certain AMPs such as nisin exhibit "dual-mechanism synergistic sterilization," where the N-terminal ring specifically binds to the pyrophosphate group of Lipid II (inhibiting cell wall synthesis), while the C-terminal inserts into the membrane to form pores [33]. Similarly, indolicidin, a tryptophan-rich bovine-derived AMP, can embed itself within the minor groove of DNA, inhibiting topoisomerase-mediated supercoiling relaxation, while PR-39 degrades proteins associated with DNA replication [33].
Synthetic Transmembrane Ion Transporters
Synthetic transmembrane ion transporters represent an emerging class of artificial molecules designed to disrupt cellular ion homeostasis by facilitating the transport of ions across lipid bilayers [34]. These compounds offer a fundamentally different approach compared to AMPs, as they typically do not cause gross membrane disruption but instead induce selective ion dysregulation that can trigger apoptosis or disrupt vital cellular processes in persister cells.
These synthetic transporters function through two primary mechanisms:
- Ion Carrier Mechanism: Mobile transporters that bind specific ions, shuttle them across the lipid bilayer, and release them on the other side, effectively dissipiating crucial ion gradients [34].
- Ion Channel Formation: Rigid molecules that assemble into transmembrane pores, creating selective pathways for specific ions to flow down their concentration gradients [34].
The strategic advantage of synthetic transporters lies in their programmable nature; their structures can be rationally designed to transport specific ions (e.g., H+, Cl-, Na+, K+) with precise selectivity, enabling targeted disruption of pH gradients or ionic balances essential for bacterial survival [34]. This ion selectivity is particularly relevant for eradicating persister cells, as these dormant populations often maintain membrane potential and proton motive force despite their metabolic inactivity, making them vulnerable to precise ion homeostasis disruption.
Membrane-Targeting Nanoparticles
Nanoparticles represent a versatile platform for membrane targeting, functioning both as direct antibacterial agents and as delivery vehicles for enhancing the efficacy of other membrane-disruptive compounds [30] [35]. Their mechanisms of action encompass:
- Direct Membrane Interaction: Cationic nanoparticles, particularly those with surface functionalization, electrostatically bind to anionic bacterial membranes, causing structural disruption, increased permeability, and eventual cell lysis [30] [35].
- Reactive Oxygen Species (ROS) Generation: Metallic and metal oxide nanoparticles (e.g., silver, zinc oxide, titanium dioxide) can produce ROS upon appropriate stimulation, leading to oxidative damage to membrane lipids and proteins [35].
- Photodynamic Therapy (PDT): Photosensitizer-loaded nanoparticles generate cytotoxic ROS upon light irradiation, causing lipid peroxidation and membrane damage, particularly effective against biofilms containing persister cells [36].
- Drug Delivery Vehicles: Nanoparticles can be engineered to co-deliver multiple therapeutic agents (e.g., AMPs with conventional antibiotics), overcoming efflux pump-mediated resistance and enhancing penetration into bacterial sanctuaries [30] [35].
A significant advantage of nanoparticles is their ability to be functionalized with targeting moieties (e.g., antibodies, peptides, sugars) that enhance their specificity for bacterial membranes over host cells, thereby improving therapeutic indices and reducing off-target effects [35] [37]. Additionally, their multi-mechanistic approach simultaneously targets multiple cellular processes, making it difficult for bacteria to develop resistance—a crucial advantage when dealing with persister populations [35].
Table 1: Comparative Mechanisms of Membrane-Targeting Agents
| Agent Class | Primary Mechanism | Molecular Targets | Resistance Potential | Selectivity Basis |
|---|---|---|---|---|
| Cationic AMPs | Membrane disruption via pore formation or carpet model | Anionic phospholipids (PG, CL), Lipid II | Low | Charge difference (bacterial vs. mammalian membranes) |
| Synthetic Transporters | Ion gradient dissipation, disruption of cellular homeostasis | Specific ions (H+, Cl-, Na+, K+) | Very Low | Molecular recognition of target ions |
| Nanoparticles | Direct membrane disruption, ROS generation, drug delivery | Membrane integrity, multiple cellular components | Low | Size, surface charge, functionalization with targeting ligands |
Experimental Data and Performance Comparison
Quantitative Efficacy Against Resistant Pathogens
Numerous studies have demonstrated the potent activity of membrane-targeting agents against drug-resistant bacterial strains, including those with persister phenotypes. The following table summarizes key efficacy data from recent investigations:
Table 2: Quantitative Efficacy of Membrane-Targeting Agents Against Resistant Pathogens
| Agent Class | Specific Agent | Target Pathogen | MIC Value | Efficacy Against Persisters | Key Findings |
|---|---|---|---|---|---|
| Cationic AMPs | Murepavadin | Multidrug-resistant Pseudomonas aeruginosa | Not specified | High (Phase III clinical trials) | Dual mechanism: biofilm disruption and rapid bactericidal activity [33] |
| Cationic AMPs | Melittin (nanoparticle-combined) | Solid tumor-associated bacteria | Not specified | Enhanced efficacy | Controlled release and reduced hemolytic toxicity in early clinical trials [33] |
| Cationic AMPs | LL-37-Derived Peptide | Melanoma-associated microbes | Not specified | Effective | Completed Phase I/II Clinical Trial in 2024 [33] |
| Nanoparticles | Cationic polymeric NPs | Multidrug-resistant Gram-negative bacteria | Not specified | Disrupts membrane potential | Overcomes efflux pump-mediated resistance [30] |
| Nanoparticles | Silver NPs | ESKAPE pathogens | Variable by formulation | Effective via ROS generation | Broad-spectrum activity, enhances antibiotic penetration [35] |
| Photodynamic NPs | ICG-loaded NPs conjugated to S. typhimurium | Solid tumors (cancer cells) | N/A | High (14-fold tumor accumulation) | Significant tumor removal with no regression [38] |
Comparative Performance in Biofilm Eradication
Biofilms represent a protected niche for persister cells, making their eradication particularly challenging. Membrane-targeting agents have demonstrated variable efficacy against biofilms:
Cationic AMPs: Show superior biofilm penetration compared to conventional antibiotics. For instance, NP213 (Novexatin), a water-soluble cyclic antimicrobial peptide, has shown significant efficacy against onychomycosis fungi due to its exceptional nail penetration capability, completing Phase II clinical trials [33]. Omiganan, a synthetic analog, has demonstrated superior safety and efficacy in patients with human tumor virus-induced genital lesions in Phase II trials [33].
Nanoparticles: Exhibit enhanced biofilm penetration due to their nanoscale size and surface properties. Cationic nanoparticles particularly accumulate in biofilm matrices, disrupting the extracellular polymeric substance and reaching embedded persister cells [35]. Photosensitizer-encapsulated nanoparticles for photodynamic therapy have shown remarkable efficacy against biofilms, as the generated ROS can diffuse through the biofilm matrix, damaging bacterial membranes throughout the structure [36].
Synthetic Transporters: Their small molecular size enables deep biofilm penetration, and their ion transport mechanisms remain effective against metabolically dormant persisters within biofilms, as maintenance of ion gradients is essential even in dormant cells [34].
Experimental Protocols for Evaluating Membrane-Targeting Agents
Membrane Permeabilization and Depolarization Assays
Protocol 1: Membrane Depolarization using DiSC₃(5) Fluorescent Probe
- Principle: The cyanine dye DiSC₃(5) accumulates in polarized bacterial membranes, resulting in fluorescence quenching. Membrane depolarization causes dye release and fluorescence increase.
- Procedure:
- Grow bacterial cells to mid-log phase in appropriate medium.
- Harvest cells by centrifugation (5000 × g, 10 min) and wash twice with buffer (5 mM HEPES, 5 mM glucose, pH 7.3).
- Resuspend cells to OD₆₀₀ ≈ 0.05 in the same buffer containing 100 mM KCl.
- Add DiSC₃(5) to a final concentration of 0.4 µM and incubate for 30-60 minutes until fluorescence stabilizes (indicating dye uptake and quenching).
- Add test membrane-targeting agent at desired concentrations while continuously monitoring fluorescence (λex = 622 nm, λem = 670 nm).
- Include positive control (gramicidin, 1 µM) and negative control (buffer only).
- Calculate percentage depolarization relative to positive control [31].
Protocol 2: SYTOX Green Uptake Assay for Membrane Permeabilization
- Principle: SYTOX Green is a DNA-binding dye that is impermeant to intact membranes but enters cells with compromised membranes, exhibiting strong fluorescence enhancement upon DNA binding.
- Procedure:
- Prepare bacterial suspension as described in Protocol 1.
- Add SYTOX Green to a final concentration of 1 µM.
- Incubate for 10 minutes in the dark.
- Add test compound and monitor fluorescence increase (λex = 504 nm, λem = 523 nm) over time.
- Include positive control (70% methanol) to determine maximum fluorescence.
- Express results as percentage permeabilization relative to positive control [31].
Minimum Inhibitory Concentration (MIC) and Minimum Bactericidal Concentration (MBC) Determinations
Protocol 3: Broth Microdilution for MIC/MBC Against Planktonic and Persister Cells
- Procedure for Planktonic Cells:
- Prepare two-fold serial dilutions of test agents in appropriate broth medium in 96-well plates.
- Inoculate wells with ~5 × 10⁵ CFU/mL of mid-log phase bacteria.
- Incubate at appropriate temperature for 16-20 hours.
- Determine MIC as the lowest concentration showing no visible growth.
- For MBC, spot aliquots from clear wells onto agar plates and determine the lowest concentration yielding <0.1% survival [35].
- Procedure for Persister Cells:
- Generate persister cells by treating stationary-phase cultures with high concentrations of bactericidal antibiotics (e.g., 50× MIC of ciprofloxacin for 3-4 hours).
- Wash cells extensively to remove antibiotics.
- Confirm persister formation by verifying >99% killing with maintained viability in small subpopulation.
- Expose persister cells to membrane-targeting agents using the microdilution method above.
- Extend incubation time to 24-48 hours to account for slow killing of dormant cells [35].
Time-Kill Kinetics Assay
Protocol 4: Time-Dependent Killing of Persister Populations
- Procedure:
- Prepare persister cells as described in Protocol 3.
- Expose persister population to test agents at concentrations 1×, 4×, and 10× MIC in appropriate buffer or medium.
- Remove aliquots at predetermined time points (0, 1, 2, 4, 6, 8, 24 hours).
- Perform serial dilutions and plate for viable counts.
- Include untreated control and conventional antibiotic control (e.g., ampicillin or ciprofloxacin) to demonstrate persister phenotype.
- Plot log CFU/mL versus time to determine killing kinetics [35] [31].
Visualization of Mechanisms and Experimental Approaches
Mechanism of Action of Membrane-Targeting Agents
Diagram 1: Mechanisms of Membrane-Targeting Agents in Persister Cell Elimination
Experimental Workflow for Evaluating Membrane-Targeting Agents
Diagram 2: Experimental Workflow for Evaluating Membrane-Targeting Agents
The Scientist's Toolkit: Essential Research Reagents and Materials
Table 3: Essential Reagents for Membrane-Targeting Agent Research
| Category | Specific Reagents | Application/Function | Key Considerations |
|---|---|---|---|
| Membrane Integrity Probes | SYTOX Green, Propidium Iodide, FM4-64 | Assess membrane permeabilization and damage | SYTOX Green is impermeant to intact membranes; fluorescence increases upon DNA binding in compromised cells [31] |
| Membrane Potential Probes | DiSC₃(5), JC-1, Oxonol VI | Measure membrane depolarization | DiSC₃(5) accumulates in polarized membranes; fluorescence increases upon depolarization [31] |
| Bacterial Strain Panels | ESKAPE pathogens (Enterococcus faecium, Staphylococcus aureus, Klebsiella pneumoniae, etc.), Isogenic efflux pump mutants | Efficacy assessment across resistant strains | Include both Gram-positive and Gram-negative species with varying membrane compositions [35] |
| Persister Cell Generation | High-concentration ciprofloxacin, ampicillin, tobramycin | Generate homogeneous persister populations | Verify persistence by survival after antibiotic exposure with maintained regrowth potential [35] |
| Lipid Model Systems | POPG, POPE, CL, LPS vesicles | Mechanism studies in simplified systems | Mimic bacterial membrane composition for biophysical studies [31] |
| Cell Culture Models | Mammalian cell lines (HEK293, HeLa), red blood cells | Cytotoxicity and selectivity assessment | Determine selective toxicity against bacterial vs. mammalian membranes [30] |
| Nanoparticle Synthesis | PLGA, chitosan, gold nanoparticles, cationic polymers | Carrier development and direct therapeutic agents | Surface charge, size, and functionalization critical for membrane interaction [35] |
Membrane-targeting agents represent a promising arsenal in the battle against persister cells and antibiotic-resistant infections. Cationic peptides offer broad-spectrum activity with multiple mechanistic approaches to membrane disruption; synthetic transporters provide precise targeting of ion homeostasis with minimal resistance development; and nanoparticles present versatile platforms that can be engineered for enhanced delivery, targeting, and multi-mechanistic action. The strategic selection among these classes depends on the specific clinical or research context, considering factors such as the target pathogen spectrum, penetration requirements (e.g., biofilm versus planktonic cells), and toxicity tolerances.
Future directions in this field will likely focus on hybrid approaches that combine the advantages of multiple classes—such as nanoparticle-encapsulated AMPs with enhanced stability and targeting capabilities, or synthetic transporters conjugated to penetration-enhancing moieties. Additionally, advances in computational design and high-throughput screening will accelerate the development of next-generation membrane-targeting agents with optimized selectivity and efficacy against the most recalcitrant persister cell populations. As these technologies mature, membrane-targeting strategies are poised to become increasingly central in overcoming the challenge of persistent bacterial infections.
Bacterial persister cells, characterized by their dormant, non-growing state, pose a significant challenge in treating chronic and recurrent infections. Unlike antibiotic-resistant bacteria, persisters survive antibiotic treatment through phenotypic tolerance rather than genetic mutation. This guide objectively compares two fundamental strategic approaches for persister cell elimination: disrupting essential proteolytic systems and exploiting vulnerabilities in cellular energy metabolism. Both strategies represent promising avenues for targeting the unique physiological state of persister cells, which are typically recalcitrant to conventional antibiotics that require active cellular processes for their efficacy. The following sections provide a detailed comparison of these approaches, supported by experimental data and methodological protocols to facilitate research and development in this critical area.
Strategic Comparison: Core Mechanisms and Applications
The table below compares the fundamental characteristics, mechanisms, and research status of protease-targeting versus energy metabolism-disrupting strategies.
| Strategic Approach | Core Mechanism of Action | Key Molecular Targets | Representative Agents | Primary Advantages | Major Limitations |
|---|---|---|---|---|---|
| Protease Disruption | Induces uncontrolled protein degradation or disrupts essential protein homeostasis [3] [2]. | ClpP protease, ClpC1-ClpP complex [3] [18] [2]. | ADEP4, Pyrazinamide (active form) [3] [18] [2]. | Functions independently of bacterial metabolic state; effective against dormant cells [3] [2]. | Potential for off-target toxicity if host proteases are affected; resistance may develop [18]. |
| Energy Metabolism Disruption | Depletes cellular energy (ATP) or disrupts the proton motive force (PMF), crippling cellular maintenance [39] [40]. | Membrane energetics, ATP synthases, pH homeostasis machinery [39] [40]. | Pyrazinoic acid, Uncoupling agents [3] [40]. | Exploits a fundamental aspect of cell viability; can bypass specific resistance mechanisms [40]. | May require specific cellular conditions for maximum efficacy; potential for host toxicity [40]. |
Quantitative Performance Data
The following table summarizes experimental findings from key studies, providing a comparative view of the efficacy of different strategies and compounds.
| Compound/Strategy | Experimental Model | Key Performance Metric | Reported Outcome | Notes / Mechanism |
|---|---|---|---|---|
| ADEP4 + Rifampicin | S. aureus persisters [3] [2] | Sterilization time | Achieved complete eradication | ADEP4 activates ClpP protease, causing uncontrolled protein degradation [3] [2]. |
| Pyrazinamide (PZA) | M. tuberculosis persisters [3] [18] [2] | Therapy shortening, relapse reduction | Cornerstone of TB therapy | Active form (pyrazinoic acid) disrupts membrane energy and targets PanD for degradation by ClpC1-ClpP [3] [2]. |
| Uncoupling Agents | E. coli [40] | Inhibition of protein degradation | >90% inhibition | Collapses proton motive force, depletes ATP, and blocks energy-dependent proteolysis [40]. |
| Intracellular pH Reduction | E. coli persisters [39] | Correlation with survival | Pre-existing lower pH linked to persistence | Persisters exhibit lower intracellular pH before antibiotic exposure, linked to TnaA activity [39]. |
Essential Research Reagents and Tools
This table catalogs key reagents and their applications for studying proteases and energy metabolism in persister cells.
| Reagent / Tool Name | Primary Function in Research | Experimental Utility |
|---|---|---|
| ADEP4 (Acyldepsipeptide 4) | ClpP protease activator [3] [2] | Induces ATP-independent protein degradation in persister cells. |
| Pyrazinamide (PZA) | Prodrug converted to pyrazinoic acid [3] [18] [2] | Studies anti-persister activity against M. tuberculosis via dual mechanisms. |
| pHluorin (plasmid-encoded) | Intracellular pH reporter (fluorescent) [39] | Measures single-cell intracellular pH dynamics via fluorescence. |
| Microfluidic Mother Machine | Single-cell bacterial culturing and imaging [39] | Tracks individual cell fate and pH dynamics under controlled conditions. |
| Sodium Arsenate | Phosphorylation inhibitor [40] | Depletes ATP levels to study energy dependency of protein degradation. |
| TnaA Knockout Strain | Genetic model lacking tryptophanase [39] | Investigates link between indole signaling, pH homeostasis, and persistence. |
Experimental Protocols for Key Assays
Protocol for Assessing Energy-Dependent Protein Degradation
This classic protocol establishes the requirement for metabolic energy in intracellular protein breakdown [40].
- Cell Preparation and Labeling: Grow E. coli cells in minimal medium. Induce the synthesis of aberrant proteins by substituting arginine with the analog L-[14C]-canavanine during the growth phase.
- Energy Depletion: Wash cells to remove canavanine and resuspend in fresh medium. Deplete endogenous energy reserves by adding specific inhibitors:
- For aerobic cultures: Add sodium azide (NaN3) or potassium cyanide (KCN) to inhibit respiratory chain.
- For broader inhibition: Use sodium arsenate to inhibit all forms of phosphorylation, or add uncoupling agents like 2,4-dinitrophenol.
- Control Setup: Include parallel cultures with oxidizable substrates (e.g., glucose, D-lactate) to restore energy.
- Measurement: Incubate and periodically sample the culture. Measure the release of acid-soluble [14C]-radioactivity from the pre-labeled proteins into the supernatant as a direct metric of protein degradation. Correlate degradation rates with intracellular ATP levels measured via a parallel luciferase assay.
Protocol for Single-Cell Intracellular pH Measurement in Persisters
This modern protocol uses microfluidics and fluorescence to link pH heterogeneity to persistence at the single-cell level [39].
- Strain Engineering: Transform E. coli with a plasmid encoding a ratiometric, pH-sensitive fluorescent protein like pHluorin. A second fluorophore (e.g., mCherry) can be used for normalization.
- Microfluidics and Imaging: Load the bacterial culture into a microfluidic "mother machine" device. This platform traps individual cells in microscopic channels, allowing for continuous medium perfusion and long-term, time-lapse microscopy.
- Antibiotic Treatment & Tracking: Perfuse the device with a high concentration of ampicillin (e.g., 100x MIC) for several hours. Acquire fluorescence images of the trapped cells over time, both during treatment and after antibiotic removal in fresh medium.
- Data Analysis: Calculate the intracellular pH for each cell from the pHluorin/mCherry fluorescence ratio. Classify cell fates as: Susceptible (lyse during treatment), Persister (survive and regrow after removal), or VBNC (remain intact but do not divide). Compare the pre-treatment intracellular pH distributions across these subpopulations.
Strategic Pathways for Persister Elimination
The following diagram illustrates the core logical relationships and mechanisms of the two main strategies discussed.
The strategic disruption of intracellular proteases and energy metabolism represents a promising frontier in the battle against bacterial persister cells. Protease-targeting agents like ADEP4 offer the distinct advantage of operating independently of the bacterial growth state, directly attacking the dormant persisters. Conversely, strategies that sabotage energy sources or pH homeostasis exploit fundamental vulnerabilities, preventing these cells from powering the protective mechanisms that underlie tolerance. While both approaches face challenges, particularly regarding potential toxicity and the complexity of bacterial metabolism, the experimental data and methodologies outlined in this guide provide a robust foundation for ongoing research and development. The future of anti-persister therapies likely lies in intelligent combination strategies that simultaneously target multiple vulnerabilities, ultimately aiming to eradicate chronic and recurrent infections that have long evaded conventional antibiotic treatments.
Bacterial persisters are a subpopulation of growth-arrested, dormant cells that are genetically identical to their susceptible parents but exhibit extreme tolerance to conventional antibiotics [3] [18]. Unlike resistant bacteria, persisters do not grow in the presence of antibiotics but can resume growth once the antibiotic pressure is removed, leading to recurrent and chronic infections [18] [11]. The clinical significance of persisters is profound, as they are implicated in recalcitrant diseases such as chronic lung infections in cystic fibrosis patients, medical device-associated infections, and Lyme disease [3] [2].
The fundamental challenge in eradicating persisters lies in their dormant state. Most conventional antibiotics target active cellular processes like cell wall synthesis, DNA replication, and protein synthesis, which are largely inactive in dormant persister cells [3]. This physiological state renders these antibiotics ineffective. Indirect strategies offer a promising alternative by either preventing cells from entering this dormant state or by forcing dormant cells to wake up and become susceptible again to conventional antibiotics [3]. This guide provides a comparative analysis of these two indirect approaches, detailing their mechanisms, key compounds, experimental protocols, and applications for research and drug development.
Strategy Comparison: Prevention vs. Wake-up
The table below summarizes the core principles, molecular targets, and advantages of the two main indirect persister control strategies.
Table 1: Comparison of Indirect Persister Control Strategies
| Strategy | Core Principle | Key Molecular Targets/Pathways | Primary Advantage |
|---|---|---|---|
| Preventing Persister Formation | Intercepting signaling or metabolic cascades that initiate dormancy [3] | (p)ppGpp alarmone, H2S biogenesis, Quorum Sensing (QS) regulators (e.g., MvfR) [3] [2] | Prevents the establishment of a tolerant population before it occurs |
| Forcing Persister Wake-up | Reversing dormancy to re-sensitize cells to conventional antibiotics [3] [41] | Membrane pore complexes (e.g., HokB), Proton Motive Force (PMF), and drug efflux pumps [41] [42] [43] | Eradicates existing persister cells that are already tolerant |
Preventing Persister Formation
This proactive strategy aims to reduce the initial size of the persister subpopulation within a bacterial culture by targeting the physiological pathways that lead to dormancy.
Key Mechanisms and Experimental Evidence
Several cellular systems have been identified as key regulators of persistence formation, and their inhibition effectively reduces persister numbers.
- Targeting the Stringent Response: The stringent response is a global stress response in bacteria mediated by the alarmone (p)ppGpp. In Enterococcus faecalis, the pheromone cCf10 has been shown to inhibit persister formation by reducing (p)ppGpp accumulation, thereby maintaining the cells in a metabolically active state [3] [2].
- Inhibiting Hydrogen Sulfide (H2S) Biogenesis: H2S acts as a protectant under stress conditions. Bacterial cystathionine γ-lyase (bCSE) is a primary generator of H2S in Staphylococcus aureus and Pseudomonas aeruginosa. CSE inhibitors reduce biofilm formation and persister cell numbers and potentiate antibiotic efficacy against both planktonic and biofilm populations [3] [2]. Synthetic H2S scavengers have also been shown to sensitize S. aureus, P. aeruginosa, E. coli, and MRSA persisters to gentamicin [3].
- Disrupting Quorum Sensing (QS): QS is a cell-cell communication system that can influence persistence. In P. aeruginosa, the QS signals phenazine pyocyanin and N-(3-oxododecanoyl)-L-homoserine lactone increase persister formation. Compounds with a benzamide-benzimidazole backbone bind to the QS regulator MvfR and inhibit its regulon, thereby reducing persister formation without affecting bacterial growth [3] [2]. Similarly, brominated furanones, which are QS inhibitors, reduce persister formation in P. aeruginosa [3].
Table 2: Compounds that Prevent Persister Formation
| Compound | Target/Pathway | Experimental Bacterium | Key Experimental Finding | Reference |
|---|---|---|---|---|
| cCf10 (pheromone) | (p)ppGpp alarmone | Enterococcus faecalis | Reduces (p)ppGpp accumulation, inhibiting persister formation | [3] [2] |
| CSE Inhibitors | H2S biogenesis | S. aureus, P. aeruginosa | Reduces biofilm and persister cell numbers; potentiates antibiotics | [3] [2] |
| H2S Scavengers | H2S neutralization | S. aureus, P. aeruginosa, E. coli, MRSA | Sensitizes persisters to gentamicin | [3] [2] |
| Benzamide-benzimidazole compounds | Quorum Sensing (MvfR) | P. aeruginosa | Binds to MvfR, reducing persister formation without affecting growth | [3] [2] |
| Brominated furanones | Quorum Sensing | P. aeruginosa | Reduces persister formation | [3] [2] |
| Nitric Oxide (NO) | Metabolic disruption | E. coli | Acts as a metabolic disruptor to prevent persister formation | [3] [2] |
Experimental Protocol: Evaluating Anti-Formation Compounds
The following protocol is adapted from methods used to assess the efficacy of compounds like CSE inhibitors and QS inhibitors [3] [2].
Bacterial Culture and Compound Treatment:
- Grow the target bacterium (e.g., P. aeruginosa or S. aureus) to mid-exponential phase in an appropriate liquid medium.
- Divide the culture into two flasks: one serving as an untreated control and the other supplemented with the test compound (e.g., a CSE inhibitor at its sub-inhibitory concentration).
- Continue incubation to allow the culture to enter stationary phase, where type I persisters are typically enriched.
Persister Isolation and Enumeration:
- Take samples from both control and treated cultures.
- Expose these samples to a high concentration of a bactericidal antibiotic (e.g., ampicillin at 10x MIC or ciprofloxacin at 10x MIC) for a period sufficient to kill all non-persister cells (e.g., 3-5 hours).
- Wash the cells to remove the antibiotic and serially dilute the samples.
- Plate the dilutions onto fresh, antibiotic-free agar plates.
- Incubate the plates for 24-48 hours and count the resulting colonies, which represent the persister cells that survived the antibiotic challenge.
Data Analysis:
- Compare the number of colony-forming units (CFU) from the treated culture to the control culture.
- A significant reduction in CFU counts in the treated sample indicates that the test compound successfully reduced the formation of persister cells.
Forcing Persister Wake-up
This strategy targets the dormant persister cells after they have formed, either by reactivating their metabolism to make them vulnerable to conventional antibiotics or by exploiting their physiological weaknesses.
Key Mechanisms and Experimental Evidence
Mechanism 1: Stimulating Awakening via Membrane Pores Research on the E. coli HokB peptide has provided a clear mechanistic insight into persister wake-up. HokB forms pores in the bacterial membrane, leading to energy depletion and dormancy. Awakening is triggered when the linked HokB peptides (dimers) break apart (monomerization), which degrades the pore. This allows the cell to re-establish its membrane potential and resume metabolic activity by consuming available nutrients [42] [43]. This process is a potential target for molecules that can artificially induce awakening.
Mechanism 2: Leveraging Reduced Drug Efflux in Dormancy A key physiological change in dormant persisters is a reduction in proton motive force (PMF), which powers energy-dependent efflux pumps [41]. This weakness can be exploited. Minocycline, an amphiphilic tetracycline, is a substrate for efflux pumps in normal E. coli cells, making it ineffective against them. However, in persisters with impaired efflux, minocycline accumulates intracellularly. When these persisters wake up, the accumulated drug effectively kills them by binding to the ribosome. This principle was validated by demonstrating that minocycline killed 70.8 ± 5.9% of E. coli HM22 persisters at 100 µg/mL, while it was ineffective against normal cells [41]. Eravacycline, a tetracycline with higher ribosomal binding affinity, showed even greater efficacy, achieving a 3-log reduction in persisters under the same conditions [41].
Table 3: Compounds and Methods for Forcing Persister Wake-up and Killing
| Compound/Method | Target/Mechanism | Experimental Bacterium | Key Experimental Finding | Reference |
|---|---|---|---|---|
| Minocycline | Ribosome (exploiting reduced efflux) | E. coli HM22 | Killed 70.8 ± 5.9% of persisters at 100 µg/mL during wake-up. | [41] |
| Eravacycline | Ribosome (exploiting reduced efflux) | E. coli HM22 | 3-log (99.9%) killing of persisters at 100 µg/mL. | [41] |
| Sugar Metabolites (e.g., glucose, mannitol) | Proton Motive Force (PMF) generation | E. coli | Potentiates aminoglycoside uptake and killing during metabolic wake-up. | [41] |
Experimental Protocol: Testing Wake-up and Killing
The following protocol is based on studies that demonstrated the efficacy of minocycline and eravacycline against E. coli persisters by leveraging reduced efflux [41].
Persister Cell Isolation:
- Grow a high-persistence strain like E. coli HM22 (carrying the hipA7 allele) to stationary phase.
- Treat the culture with a high concentration of ampicillin (e.g., 100 µg/mL) for several hours to kill all actively growing cells.
- Centrifuge the culture, wash the pellet with sterile PBS or saline to remove the antibiotic, and resuspend the cells in fresh medium or PBS. This cell suspension is enriched for persisters.
Treatment with Wake-up/Killing Agent:
- Divide the persister suspension into aliquots.
- Treat these aliquots with different concentrations of the test antibiotic (e.g., minocycline or eravacycline at 10-100 µg/mL). Include an untreated control (only PBS).
- Incubate the mixtures for a set period (e.g., 3-24 hours) to allow for wake-up and killing.
Viability Assessment:
- After incubation, wash the cells to remove the test antibiotic.
- Serially dilute and plate the samples onto antibiotic-free LB agar plates.
- Incubate the plates for 24-48 hours and count the CFUs.
Data Analysis:
- Compare the CFU counts from the treated samples to the untreated control.
- The percentage of killing or the log-reduction in viability is calculated to determine the efficacy of the compound against persisters.
Research Toolkit: Essential Reagents and Models
Table 4: Key Research Reagent Solutions for Persister Studies
| Reagent / Material | Function / Application | Example Use Case |
|---|---|---|
| High-Persistence Bacterial Strains | Models for generating high yields of persister cells for screening and mechanistic studies. | E. coli HM22 (hipA7 mutant) for studying Type I persistence [41]. |
| CSE Inhibitors | Tool compounds to investigate the role of H2S in persister formation and biofilm maintenance. | Testing synergy between CSE inhibitors and gentamicin against S. aureus biofilms [3] [2]. |
| Synthetic H2S Scavengers | Chemically neutralize H2S to study its protective effects and validate it as a target. | Sensitizing MRSA persisters to aminoglycosides [3]. |
| Membrane-Permeabilizing Agents | Increase uptake of conventional antibiotics into persister cells by disrupting membrane integrity. | Using PMBN or SPR741 to potentiate rifampin activity against A. baumannii persisters [2]. |
| Defined Wake-up Media | Provides specific metabolites to stimulate energy generation and resuscitation of dormant cells. | Using pyruvate or glucose to generate PMF and potentiate aminoglycoside killing [41]. |
Visualizing the Pathways and Workflows
Preventing Persister Formation
Figure 1: Pathway for preventing persister formation. Environmental stressors activate key pathways like quorum sensing, the stringent response, and H2S biogenesis, leading to dormancy. Specific inhibitors (red, blue, green arrows) can block these pathways to prevent persister formation.
Forcing Wake-up via Reduced Efflux
Figure 2: Mechanism of wake-up via reduced efflux. In persisters with low PMF, efflux pumps are inactive. Amphiphilic antibiotics like minocycline diffuse in and accumulate. Upon wake-up, the high intracellular drug concentration leads to death.
Experimental Workflow for Wake-up Strategies
Figure 3: Workflow for testing wake-up strategies. The standard protocol involves generating a persister-rich population, treating it with the experimental compound, and quantifying the loss of viability after a recovery period.
Bacterial persisters are a subpopulation of growth-arrested, dormant cells that exhibit exceptional tolerance to conventional antibiotic treatments without acquiring genetic resistance [18]. Unlike resistant bacteria, which possess genetic mechanisms to counteract antibiotics, persisters survive antibiotic assault through a phenotypic state of metabolic quiescence, enabling them to evade antibiotics that target active cellular processes [3] [2]. This dormant nature allows persister cells to resume growth once antibiotic pressure diminishes, leading to recurrent infections, chronic conditions, and treatment failures [44] [18]. The clinical significance of persisters is profound, as they underlie recalcitrant infections in cystic fibrosis patients, medical device-associated infections, Lyme disease, and tuberculosis [3] [45] [2].
The emergence of persister cells represents a critical challenge in clinical management of bacterial infections, particularly as these cells provide a reservoir for the development of full antibiotic resistance over time [3] [2]. Conventional antibiotics discovered based on bacterial growth inhibition—including those targeting cell wall synthesis, DNA replication, and protein synthesis—prove largely ineffective against dormant persisters due to their low metabolic activity [3] [2]. This therapeutic gap has stimulated intensive research into anti-persister adjuvants that can potentiate conventional antibiotics by either directly targeting persister cells or disrupting their dormant state, thereby making them susceptible to traditional antimicrobial agents [45] [2].
Mechanisms of Persister Formation and Survival
Molecular Pathways to Persistence
Bacterial persistence is regulated through multiple interconnected biological pathways that enable subpopulations of cells to enter a dormant state. Toxin-antitoxin (TA) systems represent a fundamental mechanism, where bacterial toxins such as HipA from the HipAB system inhibit critical cellular processes including translation and replication [18]. The stringent response, mediated by the alarmone (p)ppGpp, serves as another key pathway that redirects cellular resources during stress conditions, facilitating entry into dormancy [18]. Additionally, quorum sensing mechanisms allow bacterial populations to coordinate persistence in response to cell density, with signals like phenazine pyocyanin in Pseudomonas aeruginosa demonstrated to increase persister formation through induction of oxidative stress and metabolic alterations [3] [2].
The metabolic state of persister cells is characterized by dramatic reduction in metabolic activity and suppression of reactive oxygen species (ROS) accumulation, which protects them from ROS-mediated antibiotic lethality [46]. Recent research has revealed that both genetic persistence mutations (e.g., hipA7 and metG2 in Escherichia coli) and environmentally induced tolerance share this common feature of ROS suppression [46]. This understanding is crucial for designing effective combination therapies, as it suggests that ROS-independent killing strategies may prove more effective against persistent cells than approaches relying on oxidative damage.
Visualizing Persister Dynamics and Therapeutic Targeting
The following diagram illustrates the transition between normal and persister bacterial cells, along with the primary strategies for combating persistence:
Comparative Analysis of Anti-Persister Adjuvant Strategies
Direct Killing Approaches
Direct killing strategies target growth-independent cellular structures, primarily the bacterial membrane, to eradicate persister cells without requiring metabolic activity [3] [2]. Membrane-targeting agents disrupt the structural integrity of bacterial membranes, causing cell lysis through physical damage rather than biochemical inhibition. Notable examples include synthetic compounds such as 2D-24 and AM-0016, which have demonstrated efficacy against non-dividing cells of Staphylococcus aureus [3] [2]. Similarly, XF-70 and XF-73 exert anti-persister activity by disrupting cell membranes, with XF-73 generating lethal reactive oxygen species upon light activation [3] [2]. SA-558, a synthetic cation transporter, disrupts bacterial homeostasis leading to autolysis, while thymol triphenylphosphine conjugates (TPP-Thy3) and tea tree essential components represent natural product-derived membrane disruptors [3] [2].
Beyond membrane targeting, alternative direct killing approaches exploit intracellular targets that remain accessible in dormant cells. Pyrazinamide, a frontline tuberculosis drug, serves as a prototypical example—its active form, pyrazinoic acid, disrupts membrane energetics and triggers degradation of PanD, an enzyme essential for coenzyme A biosynthesis [3] [2]. Another innovative approach utilizes ADEP4, a semi-synthetic acyldepsipeptide that activates the ClpP protease, causing uncontrolled protein degradation in dormant cells [3] [2]. This mechanism is particularly effective as it bypasses the need for ATP-dependent protein degradation, which is compromised in metabolically inactive persisters. The direct lysis strategy offers the significant advantage of independence from bacterial metabolic state, though challenges remain regarding potential off-target toxicity against mammalian membranes [3] [2].
Resensitization and Synergistic Approaches
Resensitization strategies aim to reverse the dormant state of persister cells or potentiate conventional antibiotics through synergistic combinations. Metabolic stimulation represents one approach, where persister cells are induced to exit dormancy, thereby restoring their susceptibility to conventional antibiotics [45] [2]. Alternatively, membrane permeabilizing agents enhance antibiotic uptake by compromising the barrier function of bacterial membranes. For instance, polymyxin B nonapeptide (PMBN) and its derivative SPR741 have shown promise in sensitizing Gram-negative persisters to antibiotics by increasing membrane permeability [2]. Similarly, synthetic retinoids CD437 and CD1530 embed in the MRSA lipid bilayer, disrupting membrane integrity and increasing antibiotic uptake [2].
The following table summarizes the efficacy of selected anti-persister adjuvant strategies based on experimental findings:
Table 1: Comparative Efficacy of Anti-Persister Adjuvant Strategies
| Adjuvant Class | Specific Agent | Target Pathogen | Efficacy Outcome | Proposed Mechanism |
|---|---|---|---|---|
| Antimicrobial Peptide | Novel 20-aa peptide + AgNPs | P. aeruginosa PAO1 | 94.3% reduction in persisters [44] | Membrane disruption coupled with ROS generation |
| Antibiotic Combination | Aminoglycoside + Polymyxin | E. coli (including hipA7 and metG2 mutants) | Rapid sterilization at clinical concentrations [46] | Synergistic membrane disruption, ROS-independent |
| Membrane Disruptor | XF-73 | S. aureus | Effective against non-dividing cells [3] [2] | Membrane damage with light-activated ROS generation |
| Protease Activator | ADEP4 | S. aureus | Eradication of persisters [3] [2] | Activation of ClpP protease, protein degradation |
| Metabolic Inhibitor | CSE Inhibitors | S. aureus, P. aeruginosa | Reduced persister formation [3] [2] | Inhibition of H₂S biogenesis |
Prevention of Persister Formation
An alternative to eradicating established persisters involves preventing their formation through interference with the underlying regulatory mechanisms. Quorum sensing inhibitors represent a promising approach, as bacterial cell-cell communication significantly influences persistence development [3] [2]. Compounds sharing a benzamide-benzimidazole backbone bind to the QS regulator MvfR in P. aeruginosa and inhibit its regulon, thereby reducing persister formation without affecting bacterial growth [2]. Similarly, brominated furanones have demonstrated efficacy in reducing persister formation in P. aeruginosa by disrupting quorum sensing pathways [2].
Inhibition of bacterial stress response pathways provides another preventive strategy. The pheromone cCf10 inhibits Enterococcus faecalis persister formation by reducing (p)ppGpp alarmone accumulation and maintaining metabolically active states [2]. Additionally, targeting hydrogen sulfide (H₂S) biogenesis has emerged as a viable approach, as H₂S protects bacteria under stress conditions by scavenging free radicals and enhancing antioxidant enzyme activity [2]. CSE inhibitors, which target the primary generator of H₂S in S. aureus and P. aeruginosa, reduce biofilm formation and persister cell numbers while potentiating antibiotic efficacy against both pathogens [2]. Complementary approaches include nitric oxide (NO) that acts as a metabolic disruptor, pinaverium bromide (PB) that disrupts proton motive force and generates ROS, and medium-chain saturated fatty acids such as undecanoic acid and lauric acid that reduce persister formation through less characterized mechanisms [2].
Experimental Models and Assessment Methodologies
In Vitro Models for Evaluating Anti-Persister Strategies
Robust experimental models are essential for evaluating the efficacy of anti-persister combination therapies. Laboratory automation systems using robotic liquid-handling platforms can simulate hospital epidemiological dynamics, including continuous patient admission and discharge, treatment regimens, and transmission events [47]. This approach permits massively parallel experimental evolution over extended periods (up to 40 days) while enabling researchers to monitor resistance evolution and spread under controlled conditions that approximate clinical settings [47]. In such systems, individual patients are represented by wells in microtiter plates containing bacterial growth medium, with infection status, treatment administration, and transmission events precisely controlled through automated liquid transfers [47].
Persister isolation protocols typically involve exposure to high concentrations of bactericidal antibiotics to eliminate actively growing cells while retaining the dormant persister subpopulation. For instance, colistin at 50 times the minimal inhibitory concentration (MIC) has been used to induce metabolic dormancy in P. aeruginosa PAO1 [44]. Similarly, ciprofloxacin at 20× MIC effectively eliminates growing cells while allowing persisters to survive [46]. Following antibiotic exposure, persistence is quantified by determining the proportion of surviving cells through viable counting assays. The metabolic state of persister cells can be further characterized through assessment of ROS accumulation, DNA damage, and global metabolic activity using fluorescent probes and biochemical assays [46].
Experimental Workflow for Combination Therapy Assessment
The following diagram outlines a standardized experimental workflow for evaluating antibiotic-adjuvant combinations against bacterial persisters:
Quantitative Assessment of Combination Therapy Efficacy
Research findings consistently demonstrate the superior efficacy of combination therapies over monotherapies against bacterial persisters. A systematic evaluation of combination approaches reveals distinct levels of effectiveness across different adjuvant classes:
Table 2: Experimental Efficacy of Combination Therapies Against Bacterial Persisters
| Antibiotic Class | Adjuvant | Pathogen | Reduction in Persisters | Key Findings |
|---|---|---|---|---|
| Gentamicin | Membrane-active compounds (bithionol, nTZDpa) | MRSA | Significant killing [2] | Disrupted membrane integrity enhances antibiotic uptake |
| Gentamicin | Synthetic H₂S scavengers | S. aureus, P. aeruginosa, E. coli, MRSA | Increased sensitivity [2] | Scavengers potentiate antibiotic activity against persisters |
| Conventional antibiotics | Silver nanoparticles (AgNPs) | P. aeruginosa | Enhanced eradication [44] | ROS generation and intracellular interference |
| Aminoglycosides | Polymyxin derivatives | E. coli (including persister mutants) | Rapid sterilization [46] | Synergistic membrane disruption, ROS-independent |
| Various antibiotics | Antimicrobial peptide + AgNPs | P. aeruginosa PAO1 | 94.3% ± 2.1% [44] | Strong synergy (FICI = 0.25) with low host cytotoxicity |
Research Reagent Solutions for Persister Studies
Table 3: Essential Research Reagents for Anti-Persister Investigations
| Reagent Category | Specific Examples | Research Application | Key Considerations |
|---|---|---|---|
| Persister-Inducing Agents | Colistin (50× MIC), Ciprofloxacin (20× MIC) | Generate persister populations for experimental studies [44] [46] | Concentration optimization required for different bacterial strains |
| Membrane-Targeting Adjuvants | Polymyxin B nonapeptide, Synthetic retinoids (CD437, CD1530) | Increase membrane permeability to enhance antibiotic penetration [2] | Potential cytotoxicity requiring careful concentration determination |
| Antimicrobial Peptides | Novel 20-aa peptide (RRFFKKAAHVGKHVGKAARR) | Direct anti-persister activity and synergy with conventional antibiotics [44] | Sequence optimization for target pathogens; stability considerations |
| Nanoparticle Systems | Silver nanoparticles (AgNPs), Cationic silver nanoparticle shelled nanodroplets | Enhance antibiotic efficacy through membrane disruption and ROS generation [3] [44] | Size, shape, and surface charge characterization critical for reproducibility |
| Metabolic Modulators | Nitric oxide (NO), Pinaverium bromide (PB) | Disrupt persister dormancy to resensitize to conventional antibiotics [2] | Concentration-dependent effects on bacterial metabolism and resuscitation |
| Quorum Sensing Inhibitors | Benzamide-benzimidazole compounds, Brominated furanones | Prevent persister formation by interfering with bacterial communication [2] | Specificity for target pathogen QS systems required for efficacy |
Combination therapies incorporating conventional antibiotics with anti-persister adjuvants represent a promising strategy to address the significant clinical challenge posed by bacterial persistence. The experimental evidence summarized in this review demonstrates that approaches targeting bacterial membranes, interfering with persistence mechanisms, or resensitizing dormant cells to antibiotics can significantly enhance eradication of persistent bacterial populations. The superior performance of combination therapy over monotherapy strategies, including cycling or mixing of antibiotics, has been established in both in vitro models and preclinical studies [47] [46].
Future directions in anti-persister research will likely focus on optimizing adjuvant combinations for specific pathogen-persister populations, developing novel delivery systems to enhance local concentrations at infection sites, and identifying biomarkers to guide personalized combination therapy approaches. Additionally, the continued elucidation of molecular mechanisms governing persister formation and survival will reveal new targets for therapeutic intervention. As combination therapies progress through development pipelines, standardized assessment methodologies and robust experimental models will be crucial for translating promising research findings into clinically effective treatments that address the persistent challenge of bacterial persistence in human medicine.
Navigating the Pipeline: Challenges and Rational Design in Anti-Persister Development
Dormant cells, known as persisters in bacterial populations and drug-tolerant persister (DTP) cells or dormant disseminated tumor cells (DTCs) in cancer, represent a significant therapeutic challenge across biological domains. These non-proliferative, metabolically quiescent cell states exhibit remarkable tolerance to conventional antimicrobial and anticancer therapies that primarily target actively dividing cells [2] [48] [1]. The dormant nature of these cells creates a formidable physiological barrier to drug penetration and action, enabling survival during treatment and subsequent recurrence once therapy is withdrawn.
The clinical implications of dormant cells are profound. In bacteriology, persister cells contribute to chronic and relapsing infections in conditions such as cystic fibrosis, medical device-associated infections, and Lyme disease [2] [3]. Similarly, in oncology, DTP cells serve as reservoirs for minimal residual disease (MRD) that evade initial cancer therapies, ultimately driving tumor relapse and metastatic progression, sometimes years or decades after initial treatment [48] [1] [49]. Understanding and overcoming the unique physiological barriers that protect these dormant populations represents a critical frontier in therapeutic development for both infectious diseases and oncology.
Comparative Analysis of Dormant Cell Characteristics
Defining Features Across Biological Systems
Despite originating from different biological kingdoms, bacterial persisters and cancer DTP cells share remarkable similarities in their fundamental characteristics. Both populations exhibit reduced metabolic activity, reversible growth arrest, and enhanced survival mechanisms that distinguish them from their proliferating counterparts [2] [1] [50]. This dormancy enables tolerance to therapeutic agents that target essential cellular processes in actively dividing cells, such as cell wall synthesis, DNA replication, and protein synthesis in bacteria, or rapidly proliferating pathways in cancer cells.
The table below summarizes the core characteristics of dormant cells across these biological systems:
Table 1: Fundamental Characteristics of Dormant Cells
| Characteristic | Bacterial Persisters | Cancer DTP Cells |
|---|---|---|
| Proliferation Status | Growth-arrested, non-dividing [2] | Quiescent, slow-cycling or non-proliferative [48] [1] |
| Metabolic Activity | Low metabolic activities, dormant [2] [3] | Reduced metabolic rate, altered energy consumption [48] |
| Genetic Basis | No genetic mutations (phenotypic variant) [2] | Non-genetic adaptations, epigenetic reprogramming [1] [50] |
| Reversibility | Capable of returning to normal growth [2] | Reversible drug sensitivity [50] [48] |
| Therapeutic Impact | Antibiotic tolerance, infection recurrence [2] [3] | Therapy resistance, tumor relapse [48] [1] |
Molecular Mechanisms Governing Dormancy
The entry and maintenance of dormancy are regulated by sophisticated molecular programs. In bacterial systems, persistence is controlled through mechanisms including toxin-antitoxin (TA) modules, (p)ppGpp-mediated stringent response, reactive oxygen species (ROS)-induced stress responses, and quorum sensing (QS) systems [8]. These pathways collectively drive the metabolic shutdown that characterizes the persistent state.
In cancer, DTP cells are regulated by distinct signaling pathways including p38 MAPK activation, ERK downregulation, and altered epigenetic states [48] [51]. The balance between p38 and ERK signaling has been identified as a critical regulator, with a p38High/ERKLow signature characterizing dormant cancer populations [48]. Additional pathways such as PERK-mediated stress response and hypoxia-inducible factors (HIFs) further contribute to dormancy maintenance and drug resistance [49].
Figure 1: Molecular Pathways Governing Dormancy. This diagram illustrates the key regulatory mechanisms that drive bacterial persistence and cancer DTP cell formation, highlighting both shared features and system-specific pathways.
Experimental Models and Methodologies for Dormancy Research
Established Models for Dormant Cell Investigation
Research into dormant cells employs sophisticated experimental models that recapitulate key aspects of dormancy in controlled settings. In cancer research, 3D hydrogel-based models have proven particularly valuable for studying dormancy-associated drug resistance. Kondapaneni et al. developed a biomimetic hyaluronic acid (HA) hydrogel that effectively induces dormancy in brain metastatic breast cancer (BMBC) spheroids, while suspension culture promotes proliferation, enabling direct comparison of dormant versus proliferative states [51]. This model system allows investigators to assess therapeutic responses in both dormancy contexts, providing critical insights into dormancy-specific resistance mechanisms.
In bacterial systems, biofilm models and nutrient-limited cultures are widely employed to study persistence. Biofilms represent structured microbial communities embedded in an extracellular matrix that creates spatial heterogeneity in metabolic activity and replicative status [12] [8]. The nutrient gradients within biofilms naturally generate subpopulations of dormant cells that exhibit heightened antibiotic tolerance, making these models clinically relevant for studying chronic infections.
Identification and Validation Methodologies
Accurately identifying and characterizing dormant cells requires specialized methodologies. The table below summarizes key experimental approaches used across biological systems:
Table 2: Experimental Methods for Dormant Cell Identification and Analysis
| Method Category | Specific Techniques | Application and Interpretation |
|---|---|---|
| Proliferation Markers | Ki67/M30 staining [48], EdU assay [51] | Ki67 and M30 double-negative population indicates dormant state [48] |
| Nucleotide/Dye Labeling | BrdU/EdU/3H-T incorporation [48], CSFE, PKH26, DiD dyes [48] | Label-retaining cells indicate slow-cycling populations |
| Reporter Systems | H2B-GFP reporter [48], FUCCI reporter [48], CDKN2A promoter reporter [48] | Fluorescence-based identification of cell cycle status |
| Metabolic Sensors | Seahorse extracellular flux analysis [8] | Direct measurement of metabolic activity and energy pathway utilization |
| Pathway Activation | Phosphorylated-ERK/p38 staining [51] | p38High/ERKLow ratio indicates dormancy signaling |
These methodologies enable researchers to not only identify dormant cells but also characterize their physiological state, including metabolic activity, signaling pathway activation, and responsiveness to therapeutic challenges. The combination of these approaches provides a comprehensive toolkit for dissecting the complex biology of dormant cells across experimental systems.
Strategic Comparison of Persister Cell Elimination Approaches
Direct Killing Strategies
Direct killing approaches target essential cellular structures that remain accessible even in dormant cells, bypassing the need for metabolic activity. These strategies are particularly valuable because they address dormant cells in their persistent state without requiring reactivation.
Table 3: Direct Killing Strategies for Dormant Cells
| Therapeutic Approach | Mechanism of Action | Experimental Evidence | Limitations |
|---|---|---|---|
| Membrane-Targeting Agents (e.g., XF-70, XF-73, SA-558) [2] | Disrupt cell membrane integrity, induce lysis, generate ROS [2] | Effective against non-dividing S. aureus; XF-73 generates ROS upon light activation [2] | Potential off-target toxicity to mammalian membranes [2] |
| Nanoparticle Systems (e.g., Caff-AuNPs, AuNC@ATP) [12] | Enhance bacterial membrane permeability, disrupt outer membrane protein folding [12] | Caff-AuNPs disrupt biofilms; AuNC@ATP achieves 7-log reduction in persisters [12] | Optimization needed for complex infectious niches [12] |
| Protease Activation (e.g., ADEP4) [2] | Activates ClpP protease, causes ATP-independent protein degradation [2] | Breakdown of >400 intracellular proteins, including metabolic enzymes essential for wake-up [2] | Limited research on therapeutic window |
| Metabolic Disruption (e.g., Pyrazinamide) [2] | Disrupts membrane energetics, triggers PanD degradation [2] | Effective against M. tuberculosis persisters [2] | Species-specific mechanisms may limit broad application |
Reactivation and Sensitization Strategies
The "wake-and-kill" approach aims to reverse dormancy, forcing dormant cells to re-enter an active metabolic state where they become vulnerable to conventional therapeutics. This strategy leverages the inherent biological capacity of dormant cells to eventually resume proliferation under favorable conditions.
Table 4: Reactivation and Sensitization Strategies
| Therapeutic Approach | Mechanism of Action | Experimental Evidence | Limitations |
|---|---|---|---|
| Metabolic Reactivation (e.g., metabolites) [8] | Restores proton motive force, enhances antibiotic uptake [8] | Mannitol enhances aminoglycoside sensitivity in P. aeruginosa biofilms [8] | Maintaining effective local concentrations in complex niches [8] |
| Cationic Polymers (e.g., PS+(triEG-alt-octyl)) [12] | Activates electron transport chain, disrupts bacterial membranes [12] | Light-triggered release from PDA nanoparticles clears persistent biofilms [12] | Optimization of delivery efficiency required |
| Membrane Permeabilizers (e.g., MB6, synthetic retinoids) [2] | Disrupts membrane integrity, increases antibiotic uptake [2] | Combined treatment with gentamicin shows strong anti-persister activity against MRSA [2] | Specificity for bacterial versus mammalian membranes |
| p38 MAPK Inhibition (Cancer) [51] | Reactivates dormant cancer cells, enhances therapeutic sensitivity [51] | Reversal of HA hydrogel-induced dormancy in BMBC spheroids [51] | Risk of promoting undesirable proliferation |
Figure 2: Strategic Approaches to Dormant Cell Elimination. This workflow illustrates the two primary strategic paradigms for targeting dormant cells: direct killing approaches and reactivation strategies that enable subsequent targeting with conventional therapies.
Prevention of Dormancy Formation
An alternative to eliminating established dormant cells involves preventing entry into dormancy altogether. This proactive approach targets the molecular triggers and signaling pathways that initiate the dormancy program, potentially reducing the formation of persistent populations before they can establish therapeutic tolerance.
In bacterial systems, quorum sensing inhibitors such as brominated furanones and benzamide-benzimidazole compounds have demonstrated efficacy in reducing persister formation in P. aeruginosa by interfering with cell-cell communication systems that regulate multicellular behaviors [2]. Similarly, H2S biogenesis inhibitors and synthetic H2S scavengers reduce persister formation and potentiate antibiotic effects against S. aureus, P. aeruginosa, E. coli, and MRSA persisters [2] [3].
In cancer, targeting pre-DTP states and dormancy-priming signals represents an emerging frontier. Research has identified that a subset of tumor cells exhibits bivalent chromatin configurations prior to treatment, predisposing them to acquire a DTP phenotype upon therapeutic challenge [1]. Similarly, oncofetal-like reprogramming and retinoid X receptor dysfunction appear to act as gatekeepers for the lineage plasticity that characterizes some DTP states [1]. Therapeutic intervention targeting these priming mechanisms may prevent the initial transition into dormancy.
The Scientist's Toolkit: Essential Research Reagents and Materials
Advancing research into dormant cells requires specialized reagents and experimental tools. The following table summarizes key research solutions used in the field:
Table 5: Essential Research Reagents for Dormancy Studies
| Reagent Category | Specific Examples | Research Application |
|---|---|---|
| Dormancy Induction Systems | Hyaluronic acid (HA) hydrogel [51], Biofilm models [12] | Induces and maintains dormant state in 3D culture systems |
| Cell Cycle Tracking | EdU/BrdU assay kits [48], CSFE/PKH26 dyes [48], FUCCI reporters [48] | Identifies slow-cycling or quiescent populations |
| Viability Indicators | Ki67 antibodies [48] [51], TUNEL assay kits [48], Phospho-histone H3 antibodies [48] | Distinguishes proliferating, apoptotic, and quiescent cells |
| Pathway Reporters | p38/ERK activity reporters [48] [51], H2B-GFP cell cycle reporters [48] | Monitors dormancy-associated signaling pathway activation |
| Metabolic Probes | Seahorse assay reagents [8], ROS-sensitive dyes [2] | Measures metabolic activity and oxidative stress |
| Membrane Integrity Assays | Propidium iodide, SYTOX green, LDH release assays [2] [12] | Evaluates membrane disruption strategies |
These research tools enable the identification, characterization, and therapeutic targeting of dormant cells across experimental systems. The continued refinement of these reagents, particularly those enabling real-time monitoring of dormancy states in complex physiological environments, will accelerate progress in overcoming the challenge of drug penetration into dormant cells.
The challenge of drug penetration into dormant cells represents a fundamental therapeutic barrier across infectious disease and oncology. While bacterial persisters and cancer DTP cells originate from different biological systems, they share remarkable similarities in their physiological state and therapeutic evasion strategies. The comparative analysis presented in this guide reveals both convergent approaches and context-specific strategies that are advancing the field.
Future progress will likely depend on advanced model systems that better recapitulate the complex physiological environments in which dormant cells reside, including immune component integration and organ-specific microenvironments [1]. Additionally, the application of single-cell technologies and artificial intelligence to dissect the heterogeneity within dormant populations promises to reveal new vulnerabilities [49] [52]. The development of novel delivery systems, particularly nanomaterial-based approaches that enhance penetration into protective niches and biofilms, represents another promising frontier [12].
Ultimately, overcoming the physiological barriers presented by dormant cells will require integrated strategies that combine direct killing approaches, reactivation mechanisms, and prevention of dormancy establishment. The continuing translation of these comparative insights from bench to bedside holds significant promise for addressing one of the most persistent challenges in therapeutic development.
Chemoinformatics has emerged as a critical discipline in modern drug discovery, providing computational frameworks to manage chemical data and extract meaningful knowledge for decision-making. This field represents a convergence of older disciplines including computational chemistry, chemometrics, QSAR, and chemical information science, unified by the specialized requirement to work with and interpret chemical structures [53]. In contemporary pharmaceutical research, cheminformatics addresses fundamental challenges in the drug discovery pipeline, particularly the optimization of both lead identification and lead optimization processes through high-throughput techniques [53]. The primary applications include compound selection, virtual library generation, virtual high-throughput screening (HTS), HTS data mining, and in silico prediction of ADMET (absorption, distribution, metabolism, excretion, and toxicity) properties [53].
The evolution of drug discovery has been marked by sequential bottlenecks. While high-throughput screening enabled the testing of hundreds of thousands of compounds per drug target annually, and combinatorial chemistry addressed the demand for novel compounds, these approaches alone proved insufficient [53]. Initial emphasis on chemical diversity in compound libraries gradually shifted toward more sophisticated considerations of drug-likeness and lead-likeness, reflecting the understanding that mere structural variety does not guarantee therapeutic potential [53]. This refinement process has positioned cheminformatics as an indispensable tool for multi-parametric optimization, where ADMET properties are considered concurrently with potency and selectivity rather than sequentially [53].
Comparative Analysis of Chemoinformatic Clustering Methods
Clustering algorithms play a vital role in diversity-related tasks in modern chemoinformatics, with extensive applications throughout pharmaceutical industry drug discovery programs [54]. These methods enable the systematic organization of chemical compounds into groups based on structural or property similarity, facilitating efficient compound selection, library design, and SAR (structure-activity relationship) analysis.
Fundamental Clustering Approaches
Table 1: Comparison of Key Chemical Clustering Methods
| Clustering Method | Underlying Principle | Optimal Use Cases | Performance Notes |
|---|---|---|---|
| Ward's Method | Hierarchical agglomerative; minimizes variance within clusters | General-purpose chemical clustering | Generally superior performance with fingerprints; requires significant computation [54] [55] |
| Jarvis-Patrick | Shared nearest neighbors based on similarity threshold | Large dataset clustering | Proven effectiveness but parameter-dependent [55] |
| Butina Algorithm | Density-based; requires similarity threshold | Diverse compound selection within scaffolds | Used in commercial clustered libraries [56] |
| CAST | Statistical mechanics model; probability-based | Specialized applications | Variable performance depending on dataset characteristics [55] |
| Scatter Search | Population-based metaheuristic optimization | Complex chemical spaces | Novel approach with promising results [55] |
The performance of these grouping strategies depends on various factors including molecular representation, mathematical method, algorithmic technique, and statistical distribution of data [54]. No single method universally outperforms others across all datasets and applications, necessitating careful selection based on specific research requirements.
Structural Representation for Clustering
The effectiveness of clustering methods is intrinsically linked to how chemical structures are represented and compared:
- Fingerprint-Based Similarity: Uses fragment substructures encoded in binary fingerprints with similarity typically calculated using the Tanimoto coefficient. This approach offers computational efficiency and has demonstrated reasonable performance in practice [55].
- Graph-Based Similarity: Employs maximum common subgraph (MCS) isomorphism algorithms to identify the largest substructure common to two molecules. While computationally intensive, methods like RASCAL now enable viable graph-based similarity searching of large chemical databases [55].
- Descriptor-Based Approaches: Utilizes real molecular descriptors selected by machine learning techniques, which can model pharmacological activities with few descriptor families while avoiding problems associated with non-relevant features [54].
Recent comparative studies indicate that three of five proposed cluster algorithms showed superior performance over most classical algorithms, performing similarly (or slightly superior) to Ward's algorithm, and comparably to potent QSAR and machine learning classifiers in some cases [54].
Experimental Protocol for Method Comparison
To objectively evaluate clustering methods in practice, researchers can implement the following protocol:
- Dataset Selection: Curate eight or more well-established and validated drug datasets from medicinal chemistry literature [54].
- Molecular Representation: Generate both fingerprint-based and graph-based representations for all compounds. For fingerprint approaches, use extended-connectivity fingerprints (ECFPs); for graph-based methods, implement the RASCAL algorithm [55].
- Descriptor Selection: Apply machine learning techniques to select real molecular descriptors consistent with the neighborhood principle [54].
- Clustering Execution: Implement multiple clustering methods (Ward, Jarvis-Patrick, Butina, CAST, Scatter Search) using standardized parameters.
- Validation Metrics: Compare calculated clusterings with reference clusterings using normalized mutual information and variation of information metrics [55].
- Practical Assessment: Evaluate method performance on specific therapeutic classes (tetracyclines, dihydropyridines, angiotensin antagonists) to assess "series grouping" effectiveness as perceived by medicinal chemists [55].
Key Physicochemical Properties in Drug Design
Physicochemical properties form the foundation of a drug's interaction with biological systems, directly influencing absorption, distribution, metabolism, excretion, and toxicity (ADMET) profiles [57]. Optimization of these parameters is essential for developing successful therapeutic agents.
Critical Property Descriptors
Table 2: Essential Physicochemical Properties in Drug Design
| Property | Definition | Optimal Range | Biological Impact |
|---|---|---|---|
| Lipophilicity (Log P) | Partition coefficient between octanol and water | 1-5 [57] | Membrane permeability, solubility, metabolic stability |
| Molecular Weight | Mass of molecule | <500 Da preferred [58] | Absorption, distribution, BBB penetration |
| Hydrogen Bonding | Count of H-bond donors/acceptors | Donors ≤5, Acceptors ≤10 [58] | Solubility, permeability, target binding |
| Polar Surface Area | Surface area of polar atoms | <140 Ų | Cellular permeability, especially BBB |
| Ionization (pKa) | pH at which molecule is 50% ionized | Dependent on target environment | Solubility, membrane permeability, protein binding |
| Rotatable Bonds | Number of rotatable bonds | ≤10 [58] | Oral bioavailability, conformational flexibility |
Analysis of oral drugs approved from 2000-2022 demonstrates that while these ranges provide useful guidance, successful drugs can exist outside these parameters, particularly larger molecules (MW >500 Da) when lipophilicity, hydrogen bonding, and flexibility are carefully controlled [58].
Property Measurement Methodologies
Reliable experimental determination of physicochemical properties requires standardized protocols:
Lipophilicity Measurement:
- Shake-flask method: Compound partitioned between n-octanol and aqueous buffer
- Chromatographic methods: Reverse-phase HPLC to derive log P values
- Potentiometric methods: For ionizable compounds to determine log D at physiological pH
Solubility Assessment:
- Kinetic solubility: From DMSO stock solutions in biologically relevant media
- Thermodynamic solubility: Equilibrium solubility of solid material
- The experimental determination should use standardized buffers simulating gastrointestinal fluids (FaSSIF/FeSSIF) for biologically relevant data [59].
Permeability Evaluation:
- PAMPA (Parallel Artificial Membrane Permeability Assay): High-throughput assessment of transcellular passive diffusion
- Caco-2 cell models: More complex system incorporating some active transport mechanisms
- MDCK models: Faster alternative with similar predictive capability for passive diffusion
Integration of Clustering and Property Optimization
The true power of cheminformatics emerges when structural clustering and physicochemical optimization are integrated into a cohesive drug design strategy.
Workflow for Library Design and Compound Selection
The following diagram illustrates the integrated approach for designing optimized compound libraries:
Diagram 1: Integrated Library Design Workflow
Structure-Property Relationships (SPR)
Understanding the connections between chemical structure and physicochemical properties enables rational design:
- Functional Group Effects: Specific moieties directly influence properties; hydroxyl groups increase solubility, ester groups improve lipophilicity and permeability [57].
- Molecular Size and Shape: Smaller molecules (MW <500 Da) generally show better oral bioavailability, while shape affects interactions with receptors, enzymes, and transporters [57].
- Stereochemistry Considerations: Spatial arrangement significantly impacts pharmacokinetic and pharmacodynamic properties, as demonstrated by enantioselective activity of ibuprofen and thalidomide [57].
Quantitative Structure-Property Relationship (QSPR) models utilize mathematical relationships between molecular descriptors and properties to predict compound behavior, guiding lead optimization [57].
Research Toolkit for Chemoinformatic Studies
Essential Computational Tools and Reagents
Table 3: Research Reagent Solutions for Chemoinformatic Studies
| Tool/Reagent | Type | Function | Application Context |
|---|---|---|---|
| Bemis-Murcko Scaffolding | Algorithm | Decomposes molecules into core frameworks | Library diversity analysis [56] |
| Morgan Fingerprints | Structural Representation | Circular topological fingerprints | Similarity searching and clustering [56] |
| RDKit | Open-Source Toolkit | Cheminformatics functionality | Property calculation, descriptor generation [56] |
| RASCAL | Graph Algorithm | Rapid maximum common subgraph identification | Graph-based similarity searching [55] |
| Butina Clustering | Algorithm | Density-based clustering | Diverse compound selection [56] |
| UMAP | Dimensionality Reduction | Visualization of high-dimensional data | Chemical space visualization [56] |
Experimental Implementation Framework
For researchers implementing these approaches, the following structured protocol provides a roadmap:
- Compound Curation: Apply substructure filters to exclude undesirable compounds (PAINS, REOS, reactive molecules) [56].
- Physicochemical Filtering: Implement rules-based filters (Lipinski, Veber) to ensure drug-like properties [57] [58].
- Scaffold Analysis: Apply Bemis-Murcko decomposition to identify core frameworks and assess scaffold diversity [56].
- Descriptor Calculation: Compute key physicochemical descriptors (log P, molecular weight, HBD, HBA, TPSA) using tools like RDKit [56].
- Clustering Implementation: Execute multiple clustering algorithms (Butina for general diversity, Ward's for hierarchical grouping) [54] [56].
- Visualization: Employ dimensionality reduction techniques (PCA, UMAP) with hexagonal bin plotting to visualize chemical space coverage [56].
- Validation: Assess cluster quality using internal (silhouette index) and external (biological activity segregation) metrics.
The strategic integration of chemoinformatic clustering with physicochemical property optimization represents a powerful paradigm in modern drug discovery. As the field advances, the shift from empirical, diversity-focused screening toward targeted, hypothesis-driven approaches continues to gain momentum [60]. The comparative analysis presented herein provides researchers with a framework for selecting appropriate methodologies based on specific research objectives, whether exploring broad chemical space or optimizing focused compound series.
Future directions point toward more sophisticated multi-parameter optimization, where machine learning-enhanced clustering integrates seamlessly with predictive ADMET modeling [53] [58]. Furthermore, emerging technologies such as DNA-encoded libraries are increasingly incorporating rational design principles, including fragment-based strategies and targeted library designs for specific protein families [60]. As physicochemical profiling techniques continue to advance and clustering algorithms become more refined, the drug discovery community is positioned to navigate beyond traditional property spaces, opening new opportunities for addressing challenging therapeutic targets.
The eradication of persister cells, a dormant subpopulation of bacteria capable of surviving antibiotic treatment, represents a critical frontier in the fight against recurrent infections. While numerous innovative strategies have emerged to target these resilient cells, their therapeutic potential is often limited by a significant challenge: off-target toxicity on host cells. The very mechanisms that enable these agents to disrupt dormant bacterial cells—such as membrane disruption or reactive oxygen species (ROS) generation—can also damage mammalian cells, posing substantial safety concerns that hinder clinical translation [2] [3]. This review systematically compares current persister cell elimination strategies, with a focused analysis on their respective toxicity profiles and the methodologies employed to mitigate collateral damage to host tissues.
The fundamental biological differences between bacterial and mammalian cells create both opportunities and challenges for selective toxicity. Although bacterial cell membranes differ in composition from mammalian membranes, many membrane-targeting agents lack sufficient selectivity, leading to undesirable cytotoxicity [2]. Similarly, approaches that generate reactive oxygen species can oxidize essential cellular components in both bacterial and host cells, creating a narrow therapeutic window. Understanding these limitations has driven the development of more sophisticated strategies that leverage bacterial-specific pathways, physical targeting mechanisms, and precision delivery systems to enhance selectivity while minimizing host damage.
Comparative Analysis of Persister Elimination Strategies and Toxicity Profiles
Table 1: Comprehensive Comparison of Persister Cell Elimination Strategies and Associated Toxicity Risks
| Strategy Class | Representative Agents | Mechanism of Action | Efficacy Against Persisters | Reported Toxicity Concerns | Toxicity Mitigation Approaches |
|---|---|---|---|---|---|
| Direct Membrane Disruption | XF-73, SA-558, TPP-Thy3, Cationic Silver Nanodroplets (C-AgND) | Physical membrane damage, pore formation, ion leakage | High efficacy against non-dividing cells; 4-7 log reduction in persister counts [2] [3] | High potential for mammalian membrane disruption; hemolytic activity; general cytotoxicity [2] | Structural optimization for selective targeting of bacterial membranes; nanoparticle encapsulation; localized delivery |
| Metabolic Reactivation | PS+(triEG-alt-octyl)PDA NPs, FAlsBm, Synthetic Retinoids + Gentamicin | Reactivation of electron transport chain, metabolic stimulation | Reverses dormancy, restoring antibiotic susceptibility; 3-5 log reduction in combination [12] | Lower direct toxicity but risk of excessive inflammation from bacterial debris; potential for metabolic interference in host cells | Controlled release systems; combination with rapid-kill antibiotics; targeting bacterial-specific metabolic pathways |
| Reactive Oxygen Species Generation | MPDA/FeOOH-GOx@CaP hydrogel, Photocatalytic XF-73 | ROS generation via Fenton reactions or photoactivation | Potent against biofilm-embedded persisters; effective in prosthetic joint infection models [2] [12] | Oxidative damage to host tissues; inflammation; potential DNA damage | Microenvironment-responsive activation (pH, enzymes); physical confinement to infection sites |
| Intracellular Target Exploitation | ADEP4, Pyrazinamide, CSE Inhibitors | Activation of ClpP protease; disruption of membrane energetics; inhibition of H₂S biogenesis | Target-specific; effective against mycobacterial persisters; breaks protein homeostasis [2] [3] | Off-target protease activation; disruption of host cell processes; narrow spectrum | Prodrug approaches; bacterial-specific target selection; pathway-specific inhibition |
Experimental Protocols for Assessing Efficacy and Toxicity
Standardized Persister Killing Assay with Parallel Cytotoxicity Assessment
Objective: To simultaneously evaluate anti-persister efficacy and host cell toxicity of candidate compounds under physiologically relevant conditions.
Methodology:
- Persister Cell Preparation: Generate bacterial persisters by exposing mid-log phase cultures (e.g., Staphylococcus aureus, Pseudomonas aeruginosa) to high concentrations of ciprofloxacin (5× MIC) for 3-5 hours, followed by antibiotic washout. Confirm persistence status via viability counts on nutrient agar [21].
- Co-culture Establishment: Seed human epithelial cells (e.g., HEK-293 or A549) in 96-well plates at 2×10⁴ cells/well and allow adherence for 24 hours. Add prepared persister cells at multiplicity of infection (MOI) of 10:1 (bacteria:host cells).
- Compound Treatment: Apply test compounds at serial dilutions (typically 0.5-100 µM) to co-cultures, including appropriate controls (untreated, vehicle-only, and maximal killing control with high-dose gentamicin).
- Dual-End Point Assessment: After 24-hour incubation:
- Bacterial Viability: Lyse host cells with 0.1% Triton X-100, serially dilute, and plate on nutrient agar for colony forming unit (CFU) enumeration.
- Host Cell Viability: Assess using MTT assay (measure absorbance at 570 nm) and lactate dehydrogenase (LDH) release assay (measure absorbance at 490 nm) in parallel wells.
- Therapeutic Index Calculation: Determine IC₅₀ (host cell toxicity) and EC₅₀ (persister killing) values from dose-response curves. Therapeutic Index = IC₅₀/EC₅₀ [2].
Membrane Selectivity Profiling Assay
Objective: To quantitatively evaluate the selectivity of membrane-active agents for bacterial versus mammalian membranes.
Methodology:
- Bacterial Membrane Permeabilization: Assess using SYTOX Green uptake assay. Treat persister cells (10⁸ CFU/mL) with test compounds, add SYTOX Green (1 µM), and monitor fluorescence intensity (excitation/emission: 504/523 nm) over 60 minutes.
- Mammalian Membrane Integrity: Seed human red blood cells (RBCs) at 2% hematocrit in PBS. Treat with test compounds for 1 hour at 37°C, centrifuge, and measure hemoglobin release at 540 nm. Calculate percentage hemolysis relative to Triton X-100 (100% lysis) and PBS (0% lysis) controls.
- Selectivity Index Calculation: Determine EC₅₀ for bacterial membrane permeabilization and HC₅₀ (concentration causing 5% hemolysis). Selectivity Index = HC₅₀/EC₅₀. Agents with SI >10 are considered promising for further development [2].
Visualizing Strategic Approaches and Experimental Workflows
Diagram 1: Strategic Framework for Mitigating Off-Target Toxicity in Persister Cell Elimination
Diagram 2: Integrated Experimental Workflow for Simultaneous Efficacy and Toxicity Assessment
The Scientist's Toolkit: Essential Research Reagents and Materials
Table 2: Key Research Reagents for Investigating Anti-Persister Agents and Toxicity
| Reagent Category | Specific Examples | Research Application | Functional Purpose |
|---|---|---|---|
| Membrane Integrity Indicators | SYTOX Green, Propidium Iodide, N-Phenyl-1-naphthylamine (NPN) | Differentiating bacterial vs. mammalian membrane disruption | Fluorescent dyes that penetrate compromised membranes; quantify permeabilization kinetics and selectivity [2] |
| Viability and Cytotoxicity Assays | MTT, XTT, AlamarBlue, LDH Release Assay, ATP Luminescence | Parallel assessment of antibacterial activity and host cell damage | Metabolic activity indicators and membrane integrity markers for dual-endpoint therapeutic index calculation |
| Nanoparticle Delivery Systems | Polydopamine NPs, Gold Nanoclusters, Lipid Nanoparticles, Hydrogel Microspheres | Targeted delivery and toxicity reduction | Enhance compound penetration at infection sites while minimizing systemic exposure; enable controlled release [12] |
| Bacterial-Specific Pathway Reporters | (p)ppGpp biosensors, H₂S detection probes, Quorum Sensing Inhibitors | Selective targeting of persistence mechanisms | Monitor and manipulate bacterial stress responses without affecting host cell pathways [2] [3] |
| Reactive Oxygen Species Detection | H₂DCFDA, Dihydroethidium, Amplex Red | Quantifying oxidative stress in bacteria and host cells | Measure ROS generation and distinguish between antibacterial efficacy and collateral host damage |
| 3D Co-culture Models | Transwell systems, Organ-on-a-chip, Biofilm-epithelial co-cultures | Physiologically relevant toxicity screening | Mimic host-pathogen interfaces to better predict in vivo toxicity while evaluating anti-persister efficacy [61] |
The strategic comparison of persister cell elimination approaches reveals an evolving paradigm in antimicrobial development—one that increasingly prioritizes selective toxicity alongside efficacy metrics. While membrane-disrupting agents demonstrate potent anti-persister activity, their therapeutic potential remains constrained by significant host cell toxicity concerns. In contrast, metabolic reactivation strategies and bacterial-specific pathway interventions offer more favorable safety profiles, though often with trade-offs in spectrum of activity or potential for resistance development.
The most promising approaches emerging from current research integrate multiple mitigation strategies, such as nanoparticle-based delivery of targeted agents that exploit bacterial-specific physiological differences. The continued refinement of these strategies, guided by robust assessment protocols that simultaneously evaluate efficacy and toxicity, will be essential for translating anti-persister compounds from laboratory discoveries to clinically viable therapeutics. Future advances will likely depend on even more sophisticated targeting mechanisms, including antibody-drug conjugates specific to bacterial surface markers and smart delivery systems activated exclusively in the infection microenvironment, ultimately achieving the critical goal of eradicating persistent infections while sparing host cells from collateral damage.
The challenge of delivering therapeutic agents efficiently and safely to their intended site of action remains a significant hurdle in modern medicine. This is particularly acute in the treatment of conditions involving persistent bacterial infections and complex diseases like cancer, where conventional drug formulations often fail due to poor bioavailability, systemic toxicity, and the inability to overcome biological barriers [62] [63]. Advanced formulation strategies, particularly those leveraging nanotechnology, are revolutionizing therapeutic approaches by enabling precise targeting, controlled release, and enhanced stability of active pharmaceutical ingredients (APIs) [64] [65].
The "translational gap" in nanomedicine highlights a critical challenge: while thousands of nanomedicines show promise in preclinical studies, only an estimated 50-80 have achieved global clinical approval by 2025. This represents a conversion rate of less than 0.1% of research output reaching patients, underscoring the need for more robust and clinically viable formulation strategies [62]. This guide provides a comparative analysis of advanced drug delivery platforms, focusing on their performance in enhancing therapeutic efficacy, with special consideration for applications in challenging scenarios such as persister cell elimination.
Comparative Analysis of Advanced Delivery Platforms
Performance Metrics of Nanotechnology-Based Formulations
Nanocarriers significantly enhance drug performance by modulating release kinetics, improving the solubility and bioavailability of poorly soluble APIs, and reducing systemic side effects [64]. The table below summarizes the key characteristics and experimental efficacies of major nanocarrier types.
Table 1: Comparison of Advanced Nanocarrier Platforms for Drug Delivery
| Nanocarrier Type | Key Composition | Size Range | Encapsulation Efficiency | Experimental Efficacy Findings |
|---|---|---|---|---|
| Liposomes | Phospholipids, cholesterol | 50-200 nm | Variable (hydrophilic/hydrophobic) | Doxil (pegylated liposomal doxorubicin): Prolonged circulation, reduced cardiotoxicity in ovarian/breast cancer [62]. |
| Polymeric Nanoparticles | PLGA, Chitosan, Silk Fibroin | 20-200 nm | CUR: 37%, 5-FU: 82% in silk fibroin particles [64] | CUR/5-FU-loaded SFPs: Induced G2/M cell cycle arrest in breast cancer cells; enhanced tumor necrosis with magnetic guidance in vivo [64]. |
| Lipid Nanoparticles (LNPs) | Ionizable lipids, phospholipids, PEG-lipids | 75-90 nm | 95-100% for mRNA [64] | Successful mRNA delivery in COVID-19 vaccines; robust mRNA expression in liver after intramuscular injection in mice [62] [65]. |
| Inorganic Nanoparticles | Mesoporous Silica, Silver, Gold | 20-50 nm (MSNs) | ~27 mg/g CBD for carbon supports [64] | MSN@NH2-CLB: Higher cytotoxicity vs. free chlorambucil in A549 lung cancer cells [64]. C-AgND: Effective against S. aureus persisters in biofilms [2] [3]. |
| Albumin Nanoparticles | Bovine Serum Albumin (BSA) | ~200 nm | N/A | CLA-BSA NPs: Significant anticancer activity vs. A549 cells; minimal toxicity to healthy fibroblasts; notable antibacterial effects [64]. |
| Hyaluronic Acid Nanoparticles | Hyaluronic acid, Phosphatidylcholine | 179-209 nm | N/A | LicpHA Rutin: Significant reduction in endothelial cell death and inflammation caused by epirubicin [64]. |
Advanced Formulation Technologies Beyond Nanocarriers
Beyond nanoparticle design, integrating nanocarriers into secondary delivery systems is crucial for clinical application, addressing challenges related to administration route, stability, and patient compliance [62].
Table 2: Secondary Formulation Platforms for Clinical Translation
| Formulation Platform | Description | Key Advantages | Clinical Applications |
|---|---|---|---|
| Sterile Injectables | Liquid formulations for IV/SC administration | Immediate systemic or localized delivery; high bioavailability | Emergency medicine, biologics delivery (e.g., subcutaenous injectors for high-viscosity biologics) [62] [65]. |
| Implantable Systems | Polymeric implants, microspheres, medication-eluting stents | Sustained release over months; reduced dosing frequency; improved compliance | Chronic conditions (e.g., schizophrenia, diabetes), ophthalmology [66] [65]. |
| Inhalation Systems | Dry powder inhalers, nebulizers | Large lung surface area for rapid absorption; non-invasive | Respiratory diseases (asthma, COPD); systemic delivery of biologics and vaccines [65]. |
| Transdermal Patches & Microneedles | Skin-penetrating systems with dissolvable/biodegradable materials | Painless delivery; avoidance of first-pass metabolism; controlled release | Vaccine delivery, chronic disease treatment (e.g., hormone replacement, pain management) [65]. |
Experimental Protocols for Formulation Development and Evaluation
Synthesis and Characterization of Nanocarriers
Protocol 1: Microfluidics-Assisted Desolvation for Silk Fibroin Particles (SFPs)
- Objective: To produce uniform, stable protein-based nanoparticles for co-delivery of therapeutic agents [64].
- Materials: Silk fibroin solution, desolvating agent (e.g., ethanol), swirl mixer microfluidic device, curcumin (CUR), 5-fluorouracil (5-FU).
- Methodology:
- Synthesis: Introduce silk fibroin solution and desolvating agent into a microfluidic swirl mixer. Controlled mixing induces protein self-assembly into particles.
- Drug Loading: Incubate pre-formed SFPs with drug solutions (CUR or 5-FU) for encapsulation via absorption or diffusion.
- Purification: Remove unencapsulated drug and solvent via centrifugation or ultrafiltration.
- Characterization:
- Size and Zeta Potential: Determine via Dynamic Light Scattering (DLS). SFPs were <200 nm with uniform distribution [64].
- Encapsulation Efficiency (EE): Calculate using EE% = (Amount of drug loaded / Total drug input) × 100. Reported EE was 37% for CUR and 82% for 5-FU [64].
- Stability: Monitor particle size and aggregation over 30 days at storage conditions.
Protocol 2: Preparation and Functionalization of Mesoporous Silica Nanoparticles (MSNs)
- Objective: To create inorganic nanocarriers for enhanced drug loading and targeted delivery [64].
- Materials: Tetraethyl orthosilicate (TEOS), template agent (e.g., CTAB), chlorambucil (CLB), aminosilane coupling agent.
- Methodology:
- Synthesis: Hydrolyze and condense TEOS in the presence of a surfactant template to form mesoporous structures. Remove the template via extraction or calcination.
- Functionalization: React MSNs with an aminosilane coupling agent (e.g., APTES) to create amine-terminated surfaces (MSN@NH₂).
- Drug Loading: Incubate MSN@NH₂ with CLB solution for covalent conjugation or physical adsorption.
- Characterization:
- FTIR and Elemental Analysis: Confirm surface functionalization [64].
- TEM/N₂ Physisorption: Analyze particle size (20-50 nm) and pore volume/surface area [64].
- In Vitro Cytotoxicity: Evaluate against human lung adenocarcinoma (A549) and colon carcinoma (CT26WT) cells. MSN@NH2-CLB showed significantly higher cytotoxicity and selectivity than free CLB [64].
Efficacy and Safety Assessment Models
Protocol 3: In Vivo Evaluation of Anti-inflammatory Activity using Cotton Pellet Granuloma Model
- Objective: To compare the efficacy of encapsulated vs. free drug in a subacute inflammation model [64].
- Materials: Rats, diclofenac (DCF), diclofenac encapsulated in chitosan-coated lipid microvesicles (DCF-m), cotton pellets.
- Methodology:
- Induction: Implant sterilized cotton pellets subcutaneously in rats.
- Grouping & Dosing: Divide rats (n=5 per group) into: negative control, granuloma control, free DCF-treated, and DCF-m-treated. Administer formulations daily.
- Analysis:
- Gravimetric: Excision and weigh granuloma tissue to determine mass.
- Biochemical: Measure serum inflammatory markers (e.g., cytokines) and antioxidant enzyme activities.
- Outcome: DCF-m exhibited superior anti-inflammatory effects and greater enhancement of antioxidant enzyme activity compared to free DCF [64].
Protocol 4: In Vitro Assessment of Anti-Persister Activity
- Objective: To evaluate the efficacy of formulations against bacterial persister cells [2] [3].
- Materials: Cationic silver nanoparticle-shelled nanodroplets (C-AgND), S. aureus persister cells (pre-formed by antibiotic exposure), gentamicin, culture media.
- Methodology:
- Persister Formation: Treat a stationary-phase bacterial culture with a high dose of a cidal antibiotic (e.g., ciprofloxacin). Wash away the antibiotic after a few hours; surviving cells are enriched persisters.
- Treatment: Incubate persister cells with:
- Test formulation (e.g., C-AgND)
- Conventional antibiotic (e.g., gentamicin) as control
- Combination of both
- Viability Assessment: Plate treated samples on nutrient agar after serial dilution. Count Colony Forming Units (CFUs) after incubation.
- Outcome: C-AgND alone, or in combination with gentamicin, causes a significant reduction in persister CFUs compared to antibiotic alone [2] [3].
Visualization of Pathways and Workflows
Nanoparticle Design and Biological Interaction Workflow
The development of effective nanocarriers involves a multi-stage process from design to biological interaction, crucial for overcoming translational challenges.
Diagram 1: Integrated Workflow for Nanomedicine Development from Design to Clinical Application. This flowchart outlines the critical stages in developing viable nanomedicines, highlighting the integration of core particle design with surface engineering, final dosage form selection, and the essential considerations of in vivo performance and scalable manufacturing (Chemistry, Manufacturing, and Controls) [62] [67].
Mechanisms of Persister Cell Control Strategies
Bacterial persister cells, characterized by their dormant state, require unique strategies for eradication that differ from conventional antibiotics.
Diagram 2: Strategic Approaches for Controlling Bacterial Persister Cells. This diagram categorizes the primary mechanisms for combating tolerant bacterial persisters, highlighting both direct methods that target growth-independent structures like the cell membrane and indirect strategies that prevent formation or enable synergistic killing with conventional antibiotics [2] [3].
The Scientist's Toolkit: Essential Research Reagents and Materials
Table 3: Key Reagents and Materials for Advanced Formulation Research
| Reagent/Material | Function/Application | Specific Examples |
|---|---|---|
| Ionizable Lipids | Key component of LNPs for nucleic acid delivery; enables endosomal escape [62] [65]. | Proprietary lipids used in COVID-19 mRNA vaccines [62]. |
| Poly(D,L-lactic-co-glycolic acid) (PLGA) | Biodegradable polymer for controlled-release nanoparticles and implants [62]. | Used in microspheres and implants for sustained drug release over weeks to months [65]. |
| Hyaluronic Acid (HA) | Natural biopolymer for surface functionalization; enhances targeting and biocompatibility [64]. | Coating material in LicpHA nanoparticles for vasculoprotective effects [64]. |
| PEGylated Lipids/Polymers | Surface "stealth" coating to reduce opsonization and extend circulation half-life [62]. | Critical component in Doxil and mRNA LNPs; potential for anti-PEG immunity with repeated dosing [62]. |
| Targeting Ligands | Surface functionalization for active targeting to specific cells or tissues [63]. | Antibodies, peptides, folate, etc., grafted onto nanocarrier surfaces [63]. |
| Mesoporous Silica | Inorganic scaffold with high surface area for high drug loading [64]. | MSNs functionalized with chlorambucil (MSN@NH2-CLB) for cancer therapy [64]. |
| Cationic Silver Nanoparticles | Antimicrobial agent effective against persister cells and biofilms [2] [3]. | Shell component in C-AgND nanodroplets for targeting S. aureus persisters [2] [3]. |
| Process Analytical Technology (PAT) | Tools for real-time monitoring and control of manufacturing processes [67]. | Ensures consistent Critical Quality Attributes (CQAs) during scale-up [62] [67]. |
The comparative analysis presented in this guide demonstrates that nanotechnology and advanced formulations significantly enhance therapeutic efficacy by improving targeting, controlling release, and stabilizing drug compounds. However, successfully bridging the translational gap requires an integrated approach that moves beyond nanoparticle design alone to encompass the development of robust final dosage forms, scalable manufacturing processes, and a deeper understanding of nanomaterial-immune system interactions [62] [67].
Future directions point toward increased personalization and intelligence in formulation design. The integration of Artificial Intelligence (AI) and Machine Learning (ML) is accelerating formulation development by predicting optimal compositions and performance, thereby navigating high-dimensional design spaces more efficiently than traditional trial-and-error approaches [68] [69]. Furthermore, the exploration of non-PEG stealth alternatives, the development of multifunctional nanocarriers for combination therapy and theranostics, and the application of these advanced systems to overcome persistent challenges—such as bacterial persistence—will define the next generation of therapeutic delivery [62] [65]. This evolution promises a more targeted, effective, and patient-centric paradigm for treating a wide range of complex diseases.
Bench to Bedside: Efficacy Analysis and Future Therapeutic Directions
Bacterial persisters are dormant, non-growing phenotypic variants that exhibit tolerance to conventional antibiotics, contributing significantly to chronic and recurrent infections [3] [18]. Unlike antibiotic-resistant bacteria, persisters do not possess genetic resistance mutations but survive antibiotic treatment through metabolic dormancy, which renders antibiotics that target active cellular processes ineffective [18]. This phenomenon is a major clinical challenge in infections such as cystic fibrosis, tuberculosis, and device-associated infections [3]. The development of strategies to eradicate persister cells has therefore become a critical focus in antimicrobial research. This review provides a comparative analysis of contemporary anti-persister agents, evaluating their efficacy spectra across bacterial species, their mechanisms of action, and their inherent limitations, to inform future research and therapeutic development.
Comparative Efficacy of Anti-Persister Strategies
Anti-persister strategies can be broadly categorized into direct killing, indirect killing via metabolic reactivation, and suppression of persister formation [3] [12]. The efficacy of these strategies varies considerably based on their mechanism of action and the target bacterial species. The table below provides a comparative overview of major anti-persister strategies and their documented efficacy.
Table 1: Comparative Efficacy of Major Anti-Persister Strategies
| Strategy Category | Example Agents | Mechanism of Action | Reported Efficacy | Key Limitations |
|---|---|---|---|---|
| Direct Killing (Membrane Targeting) | Compound 171, 161, 173, 175 [70] | Membrane penetration & disruption; Target binding during wake-up [70] | • E. coli HM22: 85.2% - 95.5% killing [70]• P. aeruginosa & UPEC: Active against persisters & biofilms [70] | Off-target mammalian cell toxicity [3] |
| XF-70, XF-73 [3] | Membrane disruption; ROS generation [3] | Effective against non-dividing S. aureus [3] | Potential host cytotoxicity [3] | |
| SA-558 [3] | Synthetic cation transporter; disrupts homeostasis [3] | Induces autolysis in persisters [3] | - | |
| Direct Killing (Other Targets) | ADEP4 [3] | Activates ClpP protease; causes ATP-independent protein degradation [3] | Kills S. aureus persisters by degrading essential proteins [3] | - |
| Pyrazinamide (active form) [3] | Disrupts membrane energetics; binds PanD triggering degradation [3] | Active against M. tuberculosis persisters [3] | Species-specific activation | |
| Indirect Killing (Metabolic Reactivation) | KL1 [71] | Host-directed; reduces macrophage ROS/RNS, resuscitating bacterial metabolism [71] | • 10-fold enhanced killing of intracellular S. aureus with antibiotics [71]• Active in murine infection models [71] | Specific to intracellular persisters; host-directed effects |
| PS+(triEG-alt-octyl)PDA NPs [12] | Activates electron transport chain to "wake up" persisters, then disrupts membrane [12] | Effective clearance of persistent biofilms [12] | Requires light irradiation for polymer release | |
| Nanomaterial-Based | Caff-AuNPs [12] | Disrupts mature biofilms and kills embedded dormant cells [12] | Active against planktonic and biofilm-associated Gram+/Gram- persisters [12] | - |
| AuNC@ATP [12] | Enhances membrane permeability; disrupts outer membrane protein folding [12] | 7-log reduction in persister populations [12] | - | |
| Synergistic Combinations | MB6, CD437, CD1530 + Gentamicin [3] | Membrane disruption increases antibiotic uptake [3] | Strong anti-persister activity against MRSA [3] | Multi-component regimen |
| KL1 + Rifampicin/Moxifloxacin [71] | Reactivates metabolism, sensitizing cells to antibiotics [71] | Enhanced killing of intracellular MRSA [71] | - |
Experimental Protocols for Evaluating Anti-Persister Agents
High-Throughput Screening for Intracellular Persister Sensitizers
This protocol, used to discover the host-directed adjuvant KL1, identifies compounds that alter the metabolic state of intracellular persisters to sensitize them to antibiotics [71].
- Bacterial Strain and Reporter: Utilize a bioluminescent MRSA strain (e.g., JE2-lux). The Lux system requires ATP and reducing co-factors, providing a reliable proxy for bacterial metabolic activity [71].
- Macrophage Infection: Infect bone marrow-derived macrophages (BMDMs) with the reporter strain. Following infection, treat with gentamicin-containing media to eliminate extracellular bacteria [71].
- Compound Screening: Dispense infected macrophages into 384-well plates. Add the library of test compounds (e.g., drug-like compounds, kinase inhibitor analogs) alongside controls (e.g., rifampicin for metabolic suppression, vancomycin as a non-penetrating control) [71].
- Dual-Parameter Measurement: After a 4-hour incubation, measure:
- Bacterial Metabolic Activity: Via bioluminescence output.
- Host Cell Viability: Using a cell viability assay to rule out cytotoxicity [71].
- Hit Validation: Candidates that significantly increase bioluminescence without cytotoxicity are selected. Their adjuvant activity is validated by co-administering with antibiotics (e.g., rifampicin, moxifloxacin) and quantifying the reduction in intracellular bacterial viability compared to antibiotic treatment alone [71].
Guided Screening Based on Physicochemical Properties
This rational design approach identifies persister-active compounds based on molecular properties favoring penetration into dormant cells [70].
- Lead Compound Selection: Choose reference antibiotics with proven persister-killing activity (e.g., eravacycline, minocycline, rifamycin SV) [70].
- Descriptor Identification: Extract key structural and physicochemical parameters from the reference compounds. Relevant descriptors include:
- Chemoinformatic Clustering: Apply a clustering algorithm (e.g., k-means within the ChemMine platform) to a specialized antimicrobial library (e.g., Asinex SL#013 Gram Negative Antibacterial Library) using the selected descriptors. Focus on the cluster that contains the most effective lead compound (e.g., eravacycline) [70].
- Experimental Validation: Procure compounds from the target cluster and test their efficacy against isolated persister cells (e.g., of E. coli HM22 with a high-persistence allele) at a standard concentration (e.g., 100 µg/mL). Quantify persister killing by measuring the reduction in viable cell counts after treatment [70].
Signaling Pathways and Workflows in Persister Control
The following diagrams illustrate the core mechanisms of action for different anti-persister strategies and the experimental workflow for high-throughput screening.
Anti-Persister Agent Mechanisms
High-Throughput Screening Workflow
The Scientist's Toolkit: Research Reagent Solutions
The following table details key reagents, compounds, and materials essential for research in persister cell control, as featured in the cited studies.
Table 2: Essential Research Reagents for Anti-Persister Studies
| Reagent / Material | Function / Application | Specific Example(s) |
|---|---|---|
| High-Persistence Bacterial Strains | Model strains for generating high persister fractions in vitro. | E. coli HM22 (hipA7 allele) [70] |
| Bioluminescent Reporter Strains | Real-time probing of intracellular bacterial metabolic activity and energy status. | JE2-lux MRSA strain [71] |
| Specialized Compound Libraries | Source for screening potential anti-persister leads with known antibacterial properties. | Asinex SL#013 Gram Negative Antibacterial Library [70] |
| Reference Anti-Persister Antibiotics | Positive controls for persister killing; basis for rational drug design. | Eravacycline, Minocycline, Rifamycin SV [70] |
| Membrane-Active Compounds | Used in synergy studies to disrupt membrane integrity and potentiate antibiotics. | MB6, synthetic retinoids (CD437, CD1530) [3] |
| Host-Directed Adjuvants | Compounds that alter the host environment to sensitize intracellular persisters. | KL1 [71] |
| Cationic Polymers / Nanoparticles | Directly target and disrupt bacterial membranes; can be activated by external stimuli. | PS+(triEG-alt-octyl)PDA nanoparticles [12] |
| Functionalized Nanoclusters | Engineered nanomaterials for targeted disruption of persister membranes or proteins. | AuNC@ATP, AuNC@CPP [12] |
| Protease Activators | Induce uncontrolled protein degradation in dormant cells. | ADEP4 [3] |
| Metabolic Modulators | Reactivate bacterial metabolism to reverse dormancy. | Serine-based nanodelivery system (FAlsBm) [12] |
In Vitro and In Vivo Model Systems for Validating Anti-Persister Activity
Bacterial persisters are a subpopulation of growth-arrested, metabolically dormant cells that exhibit remarkable tolerance to conventional antibiotics despite being genetically susceptible [18] [2]. These phenotypic variants play a significant role in chronic and recurrent infections by surviving antibiotic treatment and repopulating bacterial communities once therapy ceases [18] [12]. The clinical importance of persisters is well-established in numerous persistent infections, including tuberculosis, cystic fibrosis-related pulmonary infections, recurrent urinary tract infections, and medical device-associated biofilm infections [18] [72]. The eradication of persister cells represents a critical challenge in clinical medicine and necessitates specialized model systems for evaluating potential therapeutic interventions.
A fundamental characteristic distinguishing persister cells from antibiotic-resistant bacteria is the transient, non-heritable nature of their tolerance. While antibiotic resistance arises through genetic mutations and is perpetuated in subsequent generations, persistence represents a phenotypic survival strategy that is reversed once environmental conditions become favorable [18] [73]. This biological distinction necessitates specialized experimental approaches for studying persister cells, as conventional antimicrobial susceptibility tests designed for growing bacteria fail to accurately assess anti-persister activity [73]. This guide systematically compares the available in vitro and in vivo model systems for validating anti-persister compounds, providing researchers with methodological frameworks and analytical tools for assessing novel therapeutic strategies.
Fundamental Differences Between In Vitro and In Vivo Approaches
The selection between in vitro and in vivo models represents a fundamental decision in anti-persister drug development, with each approach offering distinct advantages and limitations. In vitro models involve testing in controlled laboratory environments outside living organisms, typically using bacterial cultures in plates, flasks, or specialized biofilm systems [74]. These systems excel in isolating specific biological processes, enabling high-throughput screening, and providing detailed mechanistic insights under defined conditions. Conversely, in vivo models involve testing within whole living organisms, most commonly animals, allowing researchers to study complex host-pathogen interactions and therapeutic efficacy in physiologically relevant contexts [74].
Table 1: Core Differences Between In Vitro and In Vivo Model Systems
| Aspect | In Vitro Models | In Vivo Models |
|---|---|---|
| Definition | Testing in controlled lab environment outside living organisms [74] | Testing within a whole, living organism [74] |
| Complexity | Simplified systems focusing on specific components | Whole-organism response with integrated physiological systems |
| Cost | Lower due to simplified setup [74] | High due to animal maintenance, ethical oversight, and monitoring [74] |
| Time to Results | Quicker, enabling high-throughput screening [74] | Longer duration due to complex experimental timelines [74] |
| Physiological Relevance | Limited to specific cells/tissues, lacking full organism context [74] | Highly accurate for whole-body response prediction [74] |
| Ethical Considerations | Lower, no live animals involved [74] | Significant, especially with animal testing requirements [74] |
| Primary Applications | Early-stage drug screening, mechanistic studies, toxicity assessment [74] | Drug efficacy validation, toxicity profiling, disease modeling [74] |
The complementary strengths of both approaches have led to the widespread recognition that integrated strategies, utilizing in vitro models for initial screening and in vivo systems for validation, often provide the most robust path for therapeutic development [74]. Emerging technologies such as organ-on-chip systems and advanced computational models are further bridging the gap between these traditional approaches, offering enhanced physiological relevance while maintaining some practical advantages of in vitro systems [74] [75].
In Vitro Model Systems for Anti-Persister Screening
In vitro models provide essential platforms for initial anti-persister compound screening and mechanistic studies. These systems range from simple planktonic persistence models to more complex biofilm setups that better mimic infection environments.
Planktonic Persister Models
Planktonic persister models typically involve generating non-growing bacterial populations through various induction methods followed by compound exposure. These systems offer reproducibility and are well-suited for high-throughput screening campaigns.
Key Methodological Approaches:
- Starvation-Induced Persistence: Stationary-phase cultures transferred to carbon-free minimal media before antibiotic exposure maintain the persister phenotype effectively. This approach enabled generation of high concentrations of Staphylococcus aureus persisters tolerant to 50× MIC ciprofloxacin, facilitating screening for biocidal antibiotics [73].
- Chemical Induction: Compounds like cyanide m-chlorophenylhydrazone (CCCP), which uncouples the proton motive force, or brief rifampicin exposure can induce high persister fractions. CCCP pretreatment generated Pseudomonas aeruginosa persisters that showed marked tolerance to ciprofloxacin (20× MIC) but remained susceptible to Lacticaseibacillus rhamnosus culture filtrate supernatants [72].
- Antibiotic Selection: High-dose antibiotic exposure (e.g., tobramycin at 128× MIC) eliminates susceptible cells, leaving persister populations. These antibiotic-selected persisters can then be used to test novel anti-persister compounds [72].
Table 2: Standardized Protocol for Planktonic Persister Formation and Assessment
| Step | Procedure | Key Parameters | Quality Controls |
|---|---|---|---|
| Culture Preparation | Grow bacteria to stationary phase (typically 24-48 hours) | Growth medium, temperature, aeration | Measure optical density and verify growth phase |
| Persistence Induction | Transfer to nutrient-depleted medium or add inducing agent | Medium composition, inducer concentration, exposure duration | Confirm growth arrest via optical density monitoring |
| Persister Enrichment | Treat with high-dose bactericidal antibiotic (e.g., 50× MIC ciprofloxacin) | Antibiotic concentration, exposure time (typically 24h) | Verify biphasic killing curve; assess CFU pre/post treatment |
| Compound Screening | Expose persister-enriched population to test compounds | Compound concentration, solvent controls, exposure conditions | Include viability controls and reference antibiotics |
| Viability Assessment | Serial dilution and plating for CFU enumeration | Dilution factors, plating medium, incubation conditions | Determine limit of detection; confirm persister phenotype by re-testing antibiotic susceptibility |
Biofilm Persister Models
Biofilm models are particularly relevant for persister studies as biofilms naturally contain subpopulations of persister cells protected by the extracellular matrix. These models provide enhanced clinical relevance for studying chronic infections.
Advanced Biofilm Model Systems:
- Semi-Solid Biofilm Models: The Modified Crone's Model (MCM) embeds bacteria in soft-tissue-like agar-based matrices, better recapitulating the structural and physiological characteristics of tissue-associated biofilms compared to liquid cultures. This model has demonstrated different antimicrobial susceptibility rankings than traditional assays, significantly affecting potency evaluation [75].
- Minimum Biofilm Eradication Concentration (MBEC) Assay: Conventional MBEC assays utilize biofilms grown on pegs or other surfaces followed by exposure to antimicrobial agents. While widely used, these liquid-culture systems poorly reflect the structural characteristics of in vivo biofilms [75].
- Biofilm Persister Isolation: Pre-formed biofilms can be treated with high doses of antibiotics like ciprofloxacin (128× MIC) to eliminate susceptible cells, leaving biofilm-derived persisters for compound testing. LRM-CFS (cell-free supernatants from Lacticaseibacillus rhamnosus) demonstrated effectiveness against such biofilm-derived persisters of P. aeruginosa [72].
Specialized In Vitro Conditions
The culture conditions during anti-persister assessment significantly impact results. Research indicates that maintaining starvation conditions during antibiotic exposure is crucial for preserving the persister phenotype throughout the assay duration. Transferring stationary-phase cultures to carbon-free minimal medium before antimicrobial testing helps maintain cells in the antibiotic-tolerant non-dividing state, preventing resuscitation during extended exposure periods [73]. Furthermore, using artificial sputum medium (ASM) to mimic the cystic fibrosis lung environment provides more clinically relevant conditions for evaluating anti-persister activity against pathogens like P. aeruginosa [72].
In Vivo Model Systems for Anti-Persister Validation
In vivo models provide essential physiological context for evaluating anti-persister compounds, incorporating host immune responses, pharmacokinetic parameters, and tissue-specific microenvironments that cannot be replicated in vitro.
Murine Infection Models
Murine models represent the most widely used in vivo systems for assessing anti-persister therapeutic efficacy, offering well-characterized immune systems and genetic manipulability.
Established Murine Models for Persister Studies:
- Subcutaneous Abscess Model: This localized infection model enables direct evaluation of bacterial burden reduction in a contained environment. Penfluridol demonstrated significant efficacy in reducing MRSA loads in a mouse subcutaneous abscess model, highlighting its potential against persister-related infections [76].
- Skin Wound Infection Model: S. aureus persisters play significant roles in chronic wound infections. Murine skin wound models infected with MRSA have been used to validate anti-persister compounds like penfluridol, which showed considerable therapeutic efficacy in promoting wound healing and reducing bacterial counts [76].
- Acute Peritonitis Model: Systemic infection models like acute peritonitis allow assessment of both antimicrobial efficacy and survival benefits. Compounds with anti-persister activity have shown improved outcomes in such models compared to conventional antibiotics alone [76].
- Prosthetic Joint Infection Model: Nanomaterial-based approaches like ROS-generating hydrogel microspheres (MPDA/FeOOH-GOx@CaP) have demonstrated efficacy against S. aureus and S. epidermidis persisters in prosthetic joint infection models, addressing a key clinical scenario where persisters cause relapse [12].
Alternative Infection Models
- Caenorhabditis elegans MRSA Infection Model: The C. elegans model has been utilized for high-throughput screening of synthetic molecules against MRSA persister cells, leading to identification of synthetic retinoids with potent anti-persister activities [70].
- Rabbit Endocarditis Model: Earlier studies demonstrated a clear relationship between Streptococcus sanguis tolerance and treatment efficacy in rabbit endocarditis models, with tolerant bacteria surviving better than non-tolerant strains after extended antibiotic treatment [18].
Table 3: Standardized Protocols for In Vivo Persister Infection Models
| Model Type | Induction Method | Treatment Protocol | Endpoint Assessment |
|---|---|---|---|
| Subcutaneous Abscess | Bacterial injection (e.g., 10^7 CFU MRSA) into flank [76] | Compound administration (IP, oral, or topical) starting 2h post-infection [76] | Abscess size measurement, bacterial load enumeration in homogenized tissue [76] |
| Skin Wound Infection | Excisional or burn wound creation followed by bacterial inoculation [76] | Topical application or systemic administration for 3-7 days [76] | Wound healing rate, bacterial counts in tissue, histopathological analysis [76] |
| Acute Peritonitis | Intraperitoneal bacterial injection with or without mucin [76] | Single or multiple doses post-infection (typically within 1h) [76] | Survival monitoring, bacterial load in organs (liver, spleen, blood) [76] |
| Prosthetic Joint Infection | Surgical implantation of colonized catheter or material [12] | Local delivery via hydrogel microspheres or systemic administration [12] | Bacterial counts on explanted hardware, surrounding tissue histology [12] |
Experimental Protocols for Anti-Persister Assessment
Standardized methodologies are essential for generating reproducible and comparable data on anti-persister activity across different research platforms.
High-Throughput Screening Protocol for Anti-Persister Compounds
A optimized protocol for identifying compounds with activity against Staphylococcus aureus persister cells involves several key steps [73]:
Bacterial Culture Preparation:
- Grow S. aureus overnight in tryptic soy broth (TSB) at 37°C with shaking (180 rpm)
- Dilute 1:1000 in fresh TSB and incubate overnight again to ensure uniform stationary-phase culture
Persister Cell Enrichment:
- Transfer stationary-phase culture to carbon-free minimal medium (modified M9)
- Add ciprofloxacin at 50× MIC concentration
- Incubate for 24 hours at 37°C with shaking
- Wash cells to remove antibiotic before compound screening
Compound Screening:
- Resuspend persister-enriched population in carbon-free minimal medium
- Distribute into 96-well plates containing test compounds
- Incubate for 24 hours at 37°C
- Include controls (untreated persisters, conventional antibiotics, solvent controls)
Viability Assessment:
- Serially dilute samples in physiological saline
- Plate on tryptic soy agar (TSA)
- Incubate plates at 37°C for 24-48 hours
- Enumerate colony forming units (CFU)
- Calculate log reduction compared to untreated persister control
This protocol's key innovation involves maintaining starvation conditions during antibiotic exposure to prevent persister resuscitation, thereby enabling identification of compounds truly effective against the dormant population [73].
Assessment of Anti-Biofilm and Anti-Persister Activity
A comprehensive protocol for evaluating compound effects on biofilms and biofilm-associated persisters includes [72] [76]:
Biofilm Formation:
- Grow biofilms for 24-48 hours on appropriate surfaces (peg lids, tissue culture plates)
- Use suitable growth media optimized for biofilm formation of target pathogen
Biofilm Persister Enrichment:
- Treat mature biofilms with high concentrations of ciprofloxacin (128× MIC) for 24 hours
- Gently wash to remove antibiotic and non-adherent cells
Compound Testing:
- Expose biofilm-associated persisters to test compounds for 24 hours
- For biofilm inhibition studies, add compounds during biofilm development
- Include appropriate controls (untreated biofilms, conventional antibiotics)
Viability Assessment:
- Disrupt biofilms by sonication or scraping
- Serially dilute and plate for CFU enumeration
- Calculate percentage reduction in viable counts
This approach was successfully used to demonstrate the anti-persister activity of Lacticaseibacillus rhamnosus culture filtrate supernatants against P. aeruginosa biofilm persisters, with 1:4 dilution achieving near-complete eradication [72].
The Scientist's Toolkit: Essential Research Reagents and Materials
Table 4: Key Research Reagent Solutions for Anti-Persister Studies
| Reagent Category | Specific Examples | Research Applications | Key Considerations |
|---|---|---|---|
| Persistence Inducers | CCCP, rifampicin, high-dose tobramycin [72] [73] | Generate homogenous persister populations for screening | Concentration optimization required; mechanism varies by inducer |
| Culture Media | Artificial sputum medium (ASM), modified M9 minimal medium, TSB [72] [73] | Mimic infection environments or maintain persistence | Composition significantly affects persister formation and maintenance |
| Reference Anti-Persister Compounds | Pyrazinamide, ADEP4, penfluridol, cis-2-decenoic acid [18] [2] [76] | Positive controls for assay validation | Mechanism of action varies (membrane disruption, protease activation) |
| Nanomaterial Systems | Caffeine-functionalized AuNPs, ROS-generating hydrogels, cationic polymers [12] | Novel delivery and killing mechanisms | Size, charge, and functionalization critical for penetration and efficacy |
| Viability Assessment Tools | ATP assays, resazurin reduction, propidium iodide, CFU enumeration [73] | Measure metabolic activity and membrane integrity | Multiple methods recommended as no single assay captures all persisters |
| Biofilm Model Systems | Modified Crone's Model, MBEC assays, tissue-embedded models [75] | Evaluate anti-persister activity in structured communities | Model selection significantly influences susceptibility results |
Integrated Model Selection Framework
Choosing appropriate model systems for anti-persister therapeutic development requires careful consideration of research objectives, pathogen characteristics, and practical constraints.
This integrated framework emphasizes a sequential approach where promising compounds identified in high-throughput in vitro screens progress through increasingly complex biofilm models before final validation in physiologically relevant in vivo systems. This strategy maximizes resource efficiency while ensuring clinical relevance of therapeutic candidates.
The comprehensive eradication of bacterial persisters represents a critical frontier in combating chronic and recurrent infections. This comparison of in vitro and in vivo model systems demonstrates that effective therapeutic development requires strategic integration of both approaches, leveraging the throughput and mechanistic insights of in vitro systems with the physiological relevance of in vivo models. The ongoing refinement of biofilm models that better mimic infection environments, combined with advanced nanomaterial delivery systems and compound screening approaches tailored to dormant bacteria, promises to accelerate the development of effective anti-persister therapies. As our understanding of persister biology deepens, continued innovation in model system development will be essential for translating basic research findings into clinical interventions that address the significant challenge of persistent bacterial infections.
The ESKAPE pathogens—Enterococcus faecium, Staphylococcus aureus, Klebsiella pneumoniae, Acinetobacter baumannii, Pseudomonas aeruginosa, and Enterobacter spp.—represent a critical group of multidrug-resistant organisms responsible for the majority of nosocomial infections worldwide [77] [78]. These pathogens possess the alarming ability to "escape" the biocidal action of conventional antimicrobial agents, compounded by their capacity to form persistent, difficult-to-treat infections [77]. The World Health Organization has classified multiple ESKAPE pathogens as critical or high priority targets for new antibiotic development, highlighting their significant threat to global public health [77].
A fundamental challenge in treating ESKAPE infections involves bacterial persister cells—dormant, non-growing phenotypic variants that exhibit exceptional tolerance to conventional antibiotics without genetic resistance mechanisms [3] [18]. These metabolically quiescent cells can survive antibiotic exposure and regenerate infections once treatment ceases, contributing significantly to chronic and relapsing infections [18]. Persisters are particularly problematic in biofilm-associated infections, where they serve as reservoirs for recurrent disease and potential development of genetic resistance [77] [18]. This scientific review comprehensively evaluates the cross-species efficacy of emerging persister elimination strategies against ESKAPE pathogens, providing comparative analysis of therapeutic approaches and their underlying mechanisms of action.
Comparative Analysis of Anti-Persister Strategies Across ESKAPE Pathogens
Current research has yielded multiple strategic approaches for combating persister cells, each with distinct mechanisms and limitations. The table below summarizes the primary strategies, their functional basis, and evidence of efficacy across ESKAPE pathogens.
Table 1: Anti-Persister Strategies and Their Cross-Species Efficacy
| Strategy | Mechanism of Action | Key Agents/Compounds | Efficacy Against ESKAPE Pathogens | Limitations |
|---|---|---|---|---|
| Direct Membrane Targeting | Disrupts cell membrane integrity, causes lysis independent of metabolic state | XF-70, XF-73, SA-558, TPP-Thy3, C-AgND nanoparticles [3] | Effective against S. aureus persisters including MRSA; C-AgND effective against S. aureus biofilms [3] | Potential off-target toxicity to mammalian membranes [3] |
| Protein Degradation Activation | Activates uncontrolled proteolysis of essential cellular proteins | ADEP4 (activates ClpP protease) [3] | Eradicates S. aureus persisters by degrading metabolic enzymes needed for resuscitation [3] | Limited spectrum testing across ESKAPE pathogens |
| Metabolic Disruption | Alters bacterial metabolism to prevent dormancy entry or force resuscitation | Pyrazinamide (disrupts membrane energetics), nitric oxide [3] | Pyrazinamide specifically effective against M. tuberculosis; evidence for NO across multiple species [3] | Species-specific efficacy variations; mechanisms not fully elucidated |
| Persister Formation Inhibition | Targets signaling pathways that induce dormancy | CSE inhibitors, H2S scavengers, QS inhibitors (brominated furanones) [3] | CSE inhibitors reduce persisters in S. aureus and P. aeruginosa; QS inhibitors effective against P. aeruginosa [3] | Limited efficacy against established persister populations |
| Synergistic Antibiotic Combinations | Increases membrane permeability to enhance antibiotic uptake | MB6 + gentamicin; bithionol/nTZDpa + gentamicin [3] | Effectively kills MRSA persisters; broader efficacy across Gram-positive ESKAPE pathogens [3] | Requires precise dosing optimization; potential increased toxicity |
The comparative efficacy data reveals significant variation in how different anti-persister strategies perform across the ESKAPE pathogen spectrum. Direct membrane targeting approaches demonstrate particular promise against Gram-positive ESKAPE pathogens like S. aureus, with compounds such as XF-73 showing efficacy against non-dividing and slow-growing cells through membrane disruption and ROS generation [3]. Conversely, strategies targeting persister formation through quorum sensing inhibition appear particularly relevant for P. aeruginosa, where QS signals like phenazine pyocyanin directly increase persister formation [3]. The species-specific efficacy patterns underscore the importance of pathogen-directed therapeutic development rather than universal approaches.
Experimental Models and Methodologies for Evaluating Anti-Persister Agents
Laboratory Evolution and Resistance Assessment
Robust evaluation of anti-persister therapeutics requires standardized experimental approaches that model the development of resistance and tolerance. Recent research has employed adaptive laboratory evolution (ALE) to assess the potential for resistance development against novel therapeutic candidates [79]. In these experiments, multiple bacterial populations (typically 10 parallel lines per strain) are exposed to gradually increasing concentrations of antimicrobial agents over approximately 120 generations (60 days), with regular monitoring of minimum inhibitory concentration (MIC) changes [79]. This methodology allows researchers to quantify the evolutionary trajectory of resistance and identify mutations that confer reduced susceptibility.
Complementing ALE, frequency-of-resistance (FoR) analysis enables detection of first-step resistance mutations by exposing large bacterial populations (approximately 10^10 cells) to antimicrobial agents at multiple concentrations for 48 hours [79]. This approach identifies spontaneous mutants with significantly decreased antibiotic sensitivity (typically ≥4-fold MIC increase) and provides quantitative data on mutation frequencies under selective pressure [79]. For persister-specific studies, these conventional resistance assessments are often coupled with tolerance quantification through time-kill assays that measure survival rates after prolonged antibiotic exposure, distinguishing between genetically resistant mutants and phenotypically tolerant persister cells.
Persister-Specific Screening Protocols
Specific experimental protocols have been developed to isolate and evaluate persister cell populations. The standardized approach involves several key steps:
Persister Induction: Stationary phase cultures (typically 24-48 hours growth) or biofilm-grown cells are used as enriched sources of persisters [18]. Additional induction methods include nutrient limitation, acid stress, or subinhibitory antibiotic exposure.
Population Fractionation: High-level antibiotic treatment (typically with bactericidal antibiotics like fluoroquinolones or aminoglycosides at 10-100× MIC) for several hours eliminates growing cells while preserving persisters [18]. The surviving population is then washed to remove antibiotics.
Viability Assessment: Resuscitation of persister cells is quantified through CFU counting after antibiotic removal or using fluorescent viability stains coupled with flow cytometry [18].
Therapeutic Screening: Anti-persister compounds are applied to the purified persister population, and viability is monitored over time to assess killing efficacy [3].
This methodological framework enables standardized comparison of anti-persister strategies across different laboratories and pathogen systems, facilitating the identification of promising therapeutic candidates with genuine persister-eradicating activity.
Signaling Pathways in Persister Formation and Elimination
The molecular mechanisms governing persister formation and elimination involve complex regulatory networks that differ across bacterial species. The following diagram illustrates key pathways and their intersections with therapeutic intervention points.
Figure 1: Molecular Pathways in Persister Formation and Therapeutic Intervention Points
The diagram illustrates how environmental stressors activate key bacterial signaling pathways including toxin-antitoxin (TA) modules, stringent response, quorum sensing, and H2S signaling, collectively driving metabolic arrest and persister formation [3] [18]. Critical intervention points show where anti-persister strategies disrupt this network: quorum sensing inhibitors block cell-cell communication; H2S scavengers disrupt stress signaling; metabolic disruptors like nitric oxide prevent dormancy entry; and membrane-targeting agents directly kill persisters independent of their metabolic state [3].
Research Reagent Solutions for Persister Studies
Table 2: Essential Research Reagents for Persister Cell Investigations
| Reagent Category | Specific Examples | Research Applications | Key Considerations |
|---|---|---|---|
| Anti-Persister Compounds | XF-73, SA-558, ADEP4, Pyrazinamide, Brominated furanones [3] | Direct persister killing assays; synergy studies with conventional antibiotics | Stability in assay buffers; cytotoxicity profiling required |
| Metabolic Probes | Fluorescent viability stains (SYTO9/propidium iodide), ROS detection dyes, CTC viability stain | Persister metabolism quantification; resuscitation monitoring; membrane integrity assessment | Optimization of staining protocols for dormant cells; background signal challenges |
| Genetic Tools | CRISPR-interference systems; transposon mutant libraries; reporter gene fusions | Identification of persister-related genes; pathway analysis; promoter activity monitoring | Delivery efficiency into dormant cells; promoter selection for persistence genes |
| Cell Culture Media | Mueller-Hinton broth; specific minimal media for nutrient limitation; artificial sputum medium | Persister induction under controlled conditions; biofilm models; in vitro infection models | Media composition effects on persistence frequency; reproducibility concerns |
| Membrane-Targeting Agents | Cationic silver nanoparticles (C-AgND); thymol triphenylphosphine conjugates (TPP-Thy3) [3] | Biofilm penetration studies; membrane integrity assays; combination therapy screening | Nanoparticle characterization; solubility in aqueous systems; aggregation potential |
The selection of appropriate research reagents is critical for robust investigation of persister cell biology and therapeutic screening. Recent advances have yielded specialized compounds like cationic silver nanoparticle-shelled nanodroplets (C-AgND) that interact with negatively charged extracellular polymeric substances, enabling improved penetration and efficacy against biofilm-embedded persisters [3]. Similarly, synthetic cation transporters like SA-558 disrupt bacterial homeostasis leading to autolysis, providing novel mechanisms for direct persister targeting independent of metabolic activity [3]. These specialized reagents complement standard antimicrobial susceptibility testing materials, enabling comprehensive evaluation of anti-persister strategies across diverse experimental conditions.
The evolving challenge of persister cells in ESKAPE pathogens demands innovative approaches that move beyond conventional antibiotic discovery. The most promising strategies leverage combination therapies that simultaneously target multiple persistence mechanisms, such as membrane-active compounds that potentiate conventional antibiotics or approaches that disrupt dormancy pathways while maintaining susceptibility to killing agents [3]. Future research priorities should include expanded investigation of species-specific persistence mechanisms, development of standardized persister quantification methods, and exploration of anti-virulence approaches that disrupt persistence without direct killing pressure. As our understanding of persister biology deepens, the integration of computational approaches, including machine learning and evolutionary prediction models, will be essential for designing next-generation therapeutics that preempt resistance and tolerance development across the full spectrum of high-priority bacterial pathogens.
The escalating global threat of antimicrobial resistance (AMR), projected to cause 10 million deaths annually by 2050, has necessitated innovative therapeutic strategies beyond traditional antibiotic development [80]. Compounding this challenge is the phenomenon of bacterial persistence, where dormant, non-growing bacterial cells tolerate conventional antibiotic treatments and lead to chronic, relapsing infections [2] [3]. Drug repurposing—identifying new antibacterial applications for existing non-antibiotic drugs—has emerged as a rapid, cost-effective approach to address this crisis, as these compounds already have established human safety profiles [80]. Concurrently, artificial intelligence (AI) has revolutionized early-stage drug discovery, compressing traditional development timelines from years to months and enabling the systematic identification of non-antibiotic drugs with previously unrecognized antibacterial properties [81]. This guide provides a comparative analysis of leading AI-driven platforms and their applications in discovering and optimizing non-antibiotic drugs for eradicating bacterial persisters, offering researchers a comprehensive resource for navigating this rapidly evolving frontier.
AI-Driven Drug Discovery Platforms: Comparative Landscape and Performance Metrics
AI has transitioned from a theoretical promise to a tangible force in drug discovery, with multiple platforms now delivering clinical-stage candidates. These systems leverage machine learning (ML), generative models, and large-scale biological data analysis to accelerate target identification, compound design, and therapeutic repurposing.
Table 1: Leading AI-Driven Drug Discovery Platforms and Their Applications in Anti-Persister Therapeutics
| Platform/Company | Core AI Technology | Key Applications in Anti-Persister Drug Discovery | Reported Performance Metrics | Clinical-Stage Candidates |
|---|---|---|---|---|
| Exscientia | Generative AI + Automated Design-Make-Test-Analyze Cycles | De novo drug design, antibiotic adjuvants, lead optimization | ~70% faster design cycles; 10x fewer compounds synthesized than industry norms; clinical candidate with only 136 compounds [81] | DSP-1181 (first AI-designed drug in Phase I); EXS-21546; GTAEXS-617 [81] |
| Insilico Medicine | Generative Adversarial Networks (GANs) + Reinforcement Learning | Target discovery, small molecule generation, prediction of drug repurposing candidates | Target-to-hit in 46 days; 18 months from target discovery to Phase I trials [81] | Idiopathic pulmonary fibrosis drug (Phase I) [81] |
| Recursion | Phenotypic Screening + Computer Vision | High-content cellular imaging, mechanism of action identification | Maps biological relationships across millions of cellular images; identifies novel drug-pathway interactions [81] | Multiple oncology and neurology candidates (Phase I/II) [81] |
| BenevolentAI | Knowledge Graphs + ML | Target identification, biomarker discovery, patient stratification | Analyzes scientific literature, clinical trials, omics data to generate testable hypotheses [81] | Ben-2293 (atopic dermatitis, Phase II) [81] |
| Schrödinger | Physics-Based Computational Platform + ML | Molecular simulations, binding affinity prediction, ADMET optimization | Combines first-principles physics with ML for accurate property prediction [81] | Multiple partnered programs in oncology and immunology [81] |
The integration of AI across the drug discovery pipeline represents a paradigm shift from traditional, labor-intensive approaches. Exscientia's "Centaur Chemist" model, which combines algorithmic creativity with human expertise, exemplifies how AI can compress the design-make-test-learn cycle [81]. Their platform uses deep learning models trained on vast chemical libraries and experimental data to propose novel molecular structures satisfying precise target product profiles, including potency, selectivity, and ADMET (absorption, distribution, metabolism, excretion, and toxicity) properties [81]. This approach is particularly valuable for identifying non-antibiotic drugs with anti-persister activity, as AI systems can detect subtle structure-activity relationships that might escape conventional screening methods.
Table 2: AI Model Types and Their Specific Applications in Non-Antibiotic Drug Repurposing
| AI Model Category | Specific Techniques | Applications in Non-Antibiotic Repurposing | Advantages | Limitations |
|---|---|---|---|---|
| Machine Learning (ML) | Random Forest, Support Vector Machines, XGBoost | Quantitative Structure-Activity Relationship (QSAR) modeling, ADMET prediction, toxicity screening | Handles diverse feature types; works with small datasets; interpretable models | Requires feature engineering; performance plateaus with data complexity [82] |
| Deep Learning (DL) | Deep Neural Networks (DNNs), Convolutional Neural Networks (CNNs), Recurrent Neural Networks (RNNs) | Molecular property prediction, chemical representation learning, high-content image analysis | Automatic feature extraction; scales with data size; handles raw molecular structures | Data hungry; computationally intensive; "black box" interpretability challenges [83] [82] |
| Generative Models | Variational Autoencoders (VAEs), Generative Adversarial Networks (GANs), Transformer Networks | De novo molecular design, scaffold hopping, multi-parameter optimization | Explores novel chemical space; generates structures with desired properties | Synthetic feasibility challenges; potential for unrealistic structures [81] |
| Hybrid Models | Physics-Informed Neural Networks, Structure-Based + Ligand-Based Approaches | Binding affinity prediction, molecular docking, free energy calculations | Leverages physical principles with data-driven insights; improved generalization | Implementation complexity; computational cost [83] |
Experimental Approaches for Validating Anti-Persister Activity
Standardized Persister Cell Assays and Methodologies
Research on bacterial persisters requires specialized experimental protocols that account for their dormant, non-growing state. Standardized methods have been developed to isolate, quantify, and evaluate potential anti-persister compounds:
Persister Isolation Protocol: Bacterial cultures are typically treated with high concentrations of bactericidal antibiotics (e.g., 10-100× MIC of fluoroquinolones or aminoglycosides) for 3-5 hours to eliminate actively growing cells. Surviving persister cells are collected by centrifugation, washed, and resuspended in fresh medium [2] [3]. For biofilm persisters, established biofilms are treated with antibiotics before harvesting persistent cells.
Minimum Inhibitory Concentration (MIC) Determinations: While conventional MIC assays measure growth inhibition against planktonic cells, they provide limited value for persister cells. Modified MIC assays using high-density stationary-phase cultures (10^8-10^9 CFU/mL) can provide preliminary evidence of anti-persister activity [80].
Time-Kill Kinetics Assays: The gold standard for evaluating anti-persister compounds involves time-dependent killing assays against isolated persister populations. Compounds are tested at various concentrations (typically 1-10× MIC), and viability counts are performed over 24-72 hours. A effective anti-persister agent should achieve ≥3-log reduction in CFU/mL within 24 hours against stationary-phase cultures or biofilm-derived persisters [2] [3].
Fractional Inhibitory Concentration (FIC) Index Testing: For combination therapies, checkerboard assays determine synergistic interactions. FIC indices are calculated as (MIC of drug A in combination/MIC of drug A alone) + (MIC of drug B in combination/MIC of drug B alone). Synergy is defined as FIC ≤0.5, additivity as 0.5-1.0, indifference as 1.0-4.0, and antagonism as >4.0 [80].
Mechanism-Specific Methodologies for Anti-Persister Compounds
Different classes of non-antibiotic drugs exert antibacterial effects through distinct mechanisms, requiring specialized assays:
Membrane Disruption Assays: For compounds suspected of targeting bacterial membranes (e.g., antipsychotics, statins):
- Membrane Permeabilization: Use fluorescent dyes like propidium iodide or SYTOX Green that penetrate only compromised membranes.
- Membrane Depolarization: Employ potential-sensitive dyes like DiOC₂(3) or JC-1 to measure changes in membrane potential.
- ATP Release Measurements: Quantify extracellular ATP as an indicator of membrane integrity loss [80] [3].
Efflux Pump Inhibition Assays:
- Ethidium Bromide Accumulation Assay: Measure intracellular accumulation of ethidium bromide in the presence and absence of potential efflux pump inhibitors.
- Real-time Fluorometry: Monitor fluorescence of efflux pump substrates (e.g., Hoechst 33342) over time.
- RT-qPCR of Efflux Pump Genes: Assess transcriptional regulation of major efflux pump genes after exposure to non-antibiotic drugs [80].
Biofilm Disruption Assays:
- Crystal Violet Staining: Quantify total biofilm biomass after treatment.
- Confocal Microscopy with Live/Dead Staining: Visualize biofilm architecture and viability using BacLight LIVE/DEAD kit.
- Quorum Sensing Inhibition: Reporter strains (e.g., Chromobacterium violaceum for acyl-homoserine lactone signaling) assess interference with bacterial communication [2] [3].
AI-Driven Discovery Workflow for Anti-Persister Therapeutics
Non-Antibiotic Drug Classes with Documented Anti-Persister Activity
Quantitative Analysis of Anti-Persister Efficacy Across Drug Classes
Emerging evidence indicates that diverse classes of non-antibiotic drugs exhibit intrinsic antibacterial activity or can potentiate conventional antibiotics against persister cells. The table below summarizes experimental data for promising candidates:
Table 3: Anti-Persister Activity of Non-Antibiotic Drug Classes with Experimental Validation
| Drug Class | Specific Examples | Reported Antibacterial MICs | Synergy with Antibiotics (FIC Index) | Proposed Mechanism of Action | Key Experimental Evidence |
|---|---|---|---|---|---|
| Antipsychotics | Thioridazine | 64-128 µg/mL (S. aureus) | Clarithromycin: FIC not calculated [80] | Efflux pump inhibition, membrane disruption | Reversed resistance to isoniazid and rifampicin in M. tuberculosis; enhanced oxacillin efficacy against S. aureus [80] |
| Chlorpromazine | 2-64 µg/mL (various species) | Erythromycin: FIC ≤0.5 (B. pseudomallei) [80] | AcrAB-TolC efflux inhibition, membrane intercalation | Reduced norfloxacin MIC (4→1 µg/mL) in S. aureus; synergy with erythromycin confirmed [80] | |
| Antidepressants (SSRIs) | Sertraline | 3 µM (C. albicans) | Fluconazole: FIC <0.5 [80] | Efflux pump inhibition | Synergy with fluconazole against C. albicans persisters [80] |
| Paroxetine | 64 µg/mL (S. aureus) | Enhanced aminoglycoside efficacy (FIC not calculated) [80] | Efflux pump inhibition | MIC 64 µg/mL; enhanced aminoglycoside efficacy against S. aureus persisters [80] | |
| Calcium Channel Blockers | Verapamil | >100 µg/mL | Bedaquiline: FIC 0.06 (M. tuberculosis) [80] | Efflux inhibition, membrane energetics disruption | Bedaquiline MIC reduced from 0.5→0.025 µM (20×); synergy with clofazimine (MIC 1.0→0.25 µM) [80] |
| Statins | Simvastatin | 15.6-32 µg/mL (S. aureus, P. aeruginosa) | Tetracycline: FIC <0.5; Levofloxacin: FIC 0.31 [80] | Efflux pump inhibition + membrane disruption | MIC 15.6-31.25 µg/mL; synergistic with tetracycline (FIC <0.5) [80] |
| Atorvastatin | 64 µg/mL (T. rubrum) | Terbinafine: FIC 0.45 [80] | Efflux inhibition | MIC 64 µg/mL; synergy with terbinafine against T. rubrum [80] | |
| NSAIDs | Ibuprofen, Diclofenac | 64-512 µg/mL | Gentamicin/Ciprofloxacin: FIC <0.5 [80] | Proposed efflux pump inhibition | MICs 64-512 µg/mL; synergy with gentamicin/ciprofloxacin (FIC <0.5) [80] |
Mechanisms of Action Against Bacterial Persisters
Non-antibiotic drugs target persister cells through diverse mechanisms that circumvent their metabolic dormancy:
Mechanisms of Anti-Persister Action for Non-Antibiotic Drug Classes
Membrane-Targeting Mechanisms: Many non-antibiotic drugs, particularly antipsychotics and statins, disrupt bacterial membrane integrity through physicochemical interactions. These compounds often contain amphipathic structures that intercalate into lipid bilayers, causing depolarization, increased permeability, and eventual cell lysis [80] [3]. This mechanism is particularly effective against persisters as it does not require metabolic activity.
Efflux Pump Inhibition: Several drug classes, including antidepressants and calcium channel blockers, inhibit bacterial efflux pumps that export antibiotics [80]. By blocking these multidrug resistance transporters, these compounds increase intracellular antibiotic concentrations, restoring efficacy against otherwise tolerant persister populations.
Biofilm Disruption and Quorum Sensing Interference: Non-antibiotic drugs can interfere with bacterial communication systems (quorum sensing) and extracellular polymeric substance (EPS) production, critical for biofilm formation and maintenance [2] [3]. By disrupting these community behaviors, these compounds sensitize biofilm-associated persisters to conventional antibiotics.
Metabolic Modulation: Some repurposed drugs can alter bacterial metabolic states, either by preventing entry into dormancy or stimulating resuscitation from persistence [2] [3]. This metabolic rewiring renders persisters susceptible to conventional antibiotics that require metabolic activity for efficacy.
The Scientist's Toolkit: Essential Reagents and Methodologies
Table 4: Essential Research Reagents for Anti-Persister Drug Discovery
| Reagent Category | Specific Examples | Application in Persister Research | Key Function | Considerations for Use |
|---|---|---|---|---|
| Bacterial Strains | MRSA USA300, Pseudomonas aeruginosa PAO1, E. coli K-12, Mycobacterium tuberculosis H37Rv | Validation of anti-persister activity across clinically relevant pathogens | Provide genetically defined backgrounds for reproducible assays | Include both reference strains and clinical isolates; verify persistence frequency |
| Viability Stains | Propidium iodide, SYTOX Green, BacLight LIVE/DEAD kit | Membrane integrity assessment, viability counting in persister populations | Differentiate live/dead cells in non-growing populations | Combine with culture methods for validation; optimize staining conditions |
| Efflux Pump Reporters | Ethidium bromide, Hoechst 33342, Rhodamine 6G | Efflux pump inhibition assays | Substrates for major efflux systems; fluorescence indicates inhibition | Use with efflux-deficient mutants as controls; measure kinetics |
| Biofilm Matrix Dyes | Crystal violet, Congo red, Calcofluor white | Biofilm biomass quantification, matrix characterization | Stain extracellular polymeric substances | Normalize to protein content; combine with microscopy |
| Metabolic Probes | Resazurin, Alamar Blue, CTC (5-cyano-2,3-ditolyl tetrazolium chloride) | Metabolic activity measurements in dormant cells | Indicators of metabolic activity in non-growing cells | May not detect deeply dormant persisters; use with viability stains |
| Antibiotic Controls | Ciprofloxacin, Tobramycin, Ampicillin, Vancomycin | Persister isolation, combination therapy assays | Positive controls for persistence induction and killing | Use at appropriate concentrations (typically 10-100× MIC) |
| Cell Line Models | Mammalian cell lines (HEK293, HepG2) | Cytotoxicity screening for repurposed drugs | Assess eukaryotic cell toxicity of non-antibiotic drugs | Include primary cells when possible; test therapeutic indices |
Comparative Analysis of Platform Performance and Experimental Validation
The integration of AI-driven discovery with rigorous experimental validation has yielded significant advances in identifying non-antibiotic drugs with anti-persister activity. When evaluating platforms and approaches, researchers should consider several critical factors:
Data Quality and Context Awareness: The performance of AI models is heavily dependent on the quality, volume, and contextual richness of training data. Eric Ma of Moderna emphasizes that "statistical discipline in statistical systems" is essential, as historical assay data often contains undocumented variations in protocols, operators, and measurement techniques that can compromise model performance [84]. Platforms that implement rigorous data curation and metadata tracking generally produce more reproducible results.
Validation Comprehensiveness: AI-generated hypotheses require thorough experimental validation across multiple dimensions. The most successful platforms employ orthogonal validation methods, combining traditional MIC determinations with time-kill kinetics, mechanism-of-action studies, and synergy testing [80] [2]. Researchers should prioritize platforms that provide transparent validation data across these parameters.
Clinical Translation Potential: While computational efficiency and preclinical validation are important, ultimate success depends on clinical translation. Platforms that incorporate ADMET prediction, toxicity screening, and pharmacological modeling early in the discovery process demonstrate higher downstream success rates [81] [82].
The field of AI-driven drug repurposing for persister eradication continues to evolve rapidly, with emerging opportunities in personalized combination therapies, nanoparticle-based delivery of repurposed drugs, and multi-omics integration for mechanism elucidation. As AI platforms mature and validation methodologies become more standardized, the systematic identification of non-antibiotic solutions for persistent bacterial infections represents a promising frontier in addressing the global AMR crisis.
The emergence of drug-tolerant persister cells represents a critical barrier to effective treatment in both infectious diseases and oncology. These transiently dormant, non-proliferating cell subpopulations survive initial therapy, potentially leading to disease recurrence and treatment failure [2] [18]. In bacteria, persisters are growth-arrested phenotypic variants with low metabolic activities that enable tolerance to high doses of conventional antibiotics [2]. Similarly, in cancer, drug-tolerant persisters (DTPs) constitute a rare subpopulation that survives standard-of-care therapies through reversible, non-genetic adaptations rather than stable genetic resistance [85] [1]. This biological parallel between microbial and cancer persisters has created a convergent therapeutic challenge: conventional therapies primarily target rapidly dividing cells, leaving dormant persister populations largely intact.
The clinical significance of persister cells is profound. In infectious diseases, they underlie the recalcitrant nature of chronic infections including cystic fibrosis-related lung infections, medical device-associated infections, and Lyme disease [2] [18]. In oncology, DTPs act as clinically occult reservoirs that survive initial treatment, seeding relapse long after visible tumor regression [1]. These persistent cells provide a reservoir for the development of fully resistant strains or clones over time, compounding therapeutic challenges [2] [85]. Assessing the therapeutic potential of leading candidates requires understanding these shared biological features while recognizing the distinct clinical contexts in which they operate.
Comparative Analysis of Leading Anti-Persister Strategies
The therapeutic landscape for targeting persister cells encompasses diverse approaches, each with distinct mechanisms of action, advantages, and limitations. The leading strategies can be broadly categorized into direct killing approaches, persistence disruption, and reactivation-enabling mechanisms.
Table 1: Comparative Analysis of Leading Anti-Persister Therapeutic Candidates
| Therapeutic Strategy | Representative Candidates | Mechanism of Action | Efficacy Evidence | Development Stage |
|---|---|---|---|---|
| Membrane-Targeting Agents | XF-73, SA-558, Cationic Silver Nanoparticles (C-AgND) | Disrupts cell membrane integrity, induces lysis, generates ROS | 7-log reduction in bacterial load; effective against biofilm-embedded persisters [2] [12] | Preclinical development |
| Protease Activation | ADEP4 | Activates ClpP protease, causes uncontrolled protein degradation | Eradicates persistent S. aureus in chronic infection models [2] [45] | Preclinical development |
| Metabolic Reactivation | PS+(triEG-alt-octyl)PDA nanoparticles, FAlsBm | "Wake-and-kill" strategy reactivates dormant cells for antibiotic susceptibility | Effective clearance of persistent bacterial biofilms [12] | Preclinical development |
| Nanoparticle-Based Delivery | Caff-AuNPs, AuNC@ATP, Hb-Naf@RBCM NPs | Enhanced penetration, targeted delivery, controlled release, multimodal action | Potent against planktonic and biofilm-associated persisters [2] [12] | Preclinical development |
| Host-Directed Therapies | Not specified | Targets host pathways supporting persister survival, modulates immune response | Limited but promising in cancer DTP models [85] [86] | Early research |
Bacterial vs. Cancer Persister Therapeutic Approaches
While sharing conceptual parallels, therapeutic strategies for bacterial and cancer persisters differ significantly in their molecular targets and implementation. Bacterial persister control heavily emphasizes direct physical disruption of cellular structures or reactivation of metabolic processes. In contrast, cancer DTP targeting often focuses on epigenetic modulation, signaling pathway interference, and immune-mediated eradication [85] [86]. This distinction reflects fundamental biological differences: bacterial persisters primarily exploit physical dormancy, while cancer DTPs utilize complex regulatory networks and microenvironmental interactions to survive treatment.
The translational maturity of anti-persister strategies also varies substantially between fields. Bacterial persister control benefits from several advanced preclinical candidates with robust in vivo efficacy data, particularly for membrane-targeting compounds and nanoparticle-based delivery systems [2] [12]. For cancer DTPs, therapeutic development remains more exploratory, with fewer candidates approaching clinical evaluation despite extensive mechanistic understanding [1] [86]. This disparity highlights both the relative complexity of mammalian systems and the more recent recognition of DTPs in oncology compared to microbiology.
Experimental Models and Assessment Methodologies
Standardized Persister Isolation and Characterization Protocols
Robust assessment of anti-persister therapeutic candidates requires standardized methodologies for persister isolation and characterization. For bacterial persisters, the biphasic killing curve represents a hallmark validation method, where antibiotic treatment causes initial rapid killing followed by a plateau phase representing persister survival [85] [18]. This methodology typically involves: (1) exposing stationary-phase cultures or biofilms to high concentrations of bactericidal antibiotics; (2) monitoring viability over extended time periods (24-72 hours); (3) quantifying persistent survivors through colony-forming unit counts; and (4) confirming regained drug sensitivity upon regrowth [18].
In cancer DTP research, established protocols involve: (1) continuous exposure of cancer cell lines to lethal drug concentrations; (2) maintenance of drug pressure with periodic renewal to avoid experimental bias; (3) demonstration of biphasic population dynamics similar to bacterial models; and (4) confirmation of recovered drug sensitivity upon drug withdrawal [85] [52]. A critical validation step across both fields involves comparing drug sensitivity of persisters versus parental cells, though DTPs are notably fragile and require careful handling with gentle processing and optimized plating densities [85].
Advanced Model Systems for Clinical Translation
The predictive value of anti-persister therapeutic assessment depends heavily on model system complexity. Simple in vitro systems, while valuable for initial screening, frequently fail to recapitulate the physiological conditions that support persister formation and maintenance in clinical settings.
Table 2: Advanced Model Systems for Anti-Persister Therapeutic Evaluation
| Model System | Key Features | Applications | Limitations |
|---|---|---|---|
| Biofilm Models | Structured microbial communities encased in protective matrix; mimic chronic infection environments | Testing antibiotic penetration, evaluating matrix-degrading agents, assessing combination therapies [12] [45] | Limited host factors; variable standardization |
| Patient-Derived Organoids (PDOs) | 3D cultures retaining patient-specific tumor architecture and heterogeneity | Studying cancer DTP mechanisms, assessing tumor-specific therapeutic responses [1] | Technically challenging; limited microenvironment components |
| In Vivo Persistence Models | Chronic infection models (e.g., prosthetic joint infection, catheter models); immunocompromised mouse models for cancer DTPs | Evaluating pharmacokinetics/pharmacodynamics, assessing host toxicity, modeling persister resuscitation [45] | High cost; variable persister levels; limited human immune components |
| Virtual Patient Cohorts | Computer-generated simulations mimicking clinical patient characteristics; uses AI/ML, digital twins, Monte Carlo simulations | Predicting drug effects without human trials; optimizing dosing regimens; modeling rare scenarios [87] | Computational nature may yield erroneous outcomes; requires substantial expertise/resources |
Critical Signaling Pathways and Molecular Mechanisms
Understanding the molecular networks governing persister formation and survival is essential for targeted therapeutic development. The following diagram illustrates key signaling pathways and mechanisms shared between bacterial and cancer persister cells:
The diagram illustrates how both bacterial and cancer persisters initiate stress response programs upon therapeutic challenge, though the specific molecular implementations differ. Bacterial persisters prominently activate the stringent response mediated by the alarmone (p)ppGpp, which coordinates metabolic downregulation through toxin-antitoxin (TA) systems and reduces membrane potential [18] [11]. Cancer DTPs, conversely, undergo extensive epigenetic reprogramming that enables cell state plasticity and metabolic rewiring toward oxidative phosphorylation and fatty acid β-oxidation [85] [86]. Both persister types implement antioxidant defenses, with bacterial persisters often employing hydrogen sulfide (H₂S)-mediated protection, while cancer DTPs upregulate endogenous ROS scavenging systems [2] [85].
These shared pathway architectures reveal therapeutic vulnerabilities. Bacterial persister control strategies can target membrane integrity, protease systems, or H₂S biogenesis [2]. For cancer DTPs, vulnerabilities include epigenetic regulators, metabolic dependencies, and immune surveillance escape mechanisms [1] [86]. The convergence on dormancy and stress adaptation mechanisms across evolutionary kingdoms suggests potential for cross-disciplinary therapeutic insights.
The Scientist's Toolkit: Essential Research Reagents
Advancing anti-persister therapeutic development requires specialized research tools and reagents. The following table catalogs essential materials for experimental investigation in this field:
Table 3: Essential Research Reagents for Persister Cell Investigations
| Reagent Category | Specific Examples | Research Applications | Key Functions |
|---|---|---|---|
| Persistence-Inducing Compounds | Ciprofloxacin, Ofloxacin, Tobramycin, Cisplatin, EGFR inhibitors | Generating persister populations in vitro | Creating therapy-induced dormant cells for experimental study [85] [18] |
| Membrane Integrity Probes | Propidium iodide, SYTOX Green, FM4-64 | Assessing membrane damage in persister cells | Evaluating mechanism of membrane-targeting anti-persister agents [2] [12] |
| Metabolic Activity Assays | AlamarBlue, Resazurin, MTI, ATP luminescence assays | Quantifying persister metabolic state | Measuring dormancy depth and reactivation kinetics [18] |
| ROS Detection Reagents | H2DCFDA, MitoSOX, CellROX | Measuring reactive oxygen species in persisters | Evaluating oxidative stress mechanisms in persister survival and killing [2] [12] |
| Epigenetic Modulators | HDAC inhibitors, DNMT inhibitors, BET bromodomain inhibitors | Investigating cancer DTP epigenetic regulation | Probing chromatin-mediated persistence mechanisms and therapeutic targeting [1] [86] |
| Selective Culture Media | Antibiotic-containing media, Drug-supplemented culture systems | Maintaining selective pressure during persister studies | Enriching and maintaining persister populations during experimental procedures [85] [18] |
Clinical Translation Challenges and Future Directions
The path from preclinical candidate to clinically effective anti-persister therapy faces several formidable challenges. Pharmacokinetic optimization presents particular difficulties, as effective eradication often requires sustained drug exposure at infection or tumor sites to target slowly resuscitating persister populations [45]. For direct-killing anti-persister agents, balancing efficacy and toxicity remains challenging, especially for membrane-targeting compounds that may affect host membranes [2]. Additionally, the heterogeneous nature of persister populations necessitates combination approaches rather than monotherapies, creating regulatory and development complexities [1] [45].
Promising translational approaches include adaptive dosing regimens informed by mathematical modeling of persister resuscitation dynamics [52] [86]. Nanoparticle-based delivery systems offer enhanced penetration into biofilms and tumor sanctuaries while enabling targeted delivery and reduced off-target effects [12]. Emerging diagnostic capabilities for minimal residual disease monitoring in cancer may enable better timing of anti-persister therapies [1] [86]. Furthermore, host-directed therapies that modulate the immune system or microenvironment to target persisters represent an innovative approach with potential application across infectious disease and oncology [85] [86].
The continued development of robust predictive models, including more physiologically relevant in vitro systems and virtual patient cohorts, will accelerate clinical translation [87]. As understanding of persister biology deepens, therapeutic strategies will increasingly focus on manipulating persistence pathways rather than simply killing dormant cells, potentially leading to more effective and durable treatments for recurrent and persistent diseases across clinical domains.
Conclusion
The fight against bacterial persistence requires a paradigm shift from traditional antibiotic discovery toward multi-pronged therapeutic strategies. This analysis demonstrates that no single approach offers a universal solution; instead, the future lies in intelligently combining direct killing agents, persistence-disrupting compounds, and conventional antibiotics. Success will depend on leveraging rational, property-based drug design informed by a deep understanding of persister physiology, alongside robust model systems for validation. Future research must prioritize overcoming penetration barriers and toxicity concerns to translate these promising strategies from the laboratory into clinical tools capable of eradicating the root cause of chronic and relapsing infections.
References
- 1. Drug-tolerant persister cells in cancer: bridging the gaps ... [https://www.nature.com/articles/s41467-025-66376-6]
- 2. Mini review: Persister cell control strategies [https://www.frontiersin.org/journals/pharmacology/articles/10.3389/fphar.2025.1706115/full]
- 3. Mini review: Persister cell control strategies - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC12568461/]
- 4. Observation of persister cell histories reveals diverse ... [https://elifesciences.org/articles/79517]
- 5. Antibiotic tolerance and persistence have distinct fitness ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC9704765/]
- 6. Quantitative analysis of persister fractions suggests different ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC3682893/]
- 7. A Quantitative Survey of Bacterial Persistence in the Presence ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC7460088/]
- 8. Metabolite-driven reprogramming of bacterial persisters [https://www.sciencedirect.com/science/article/abs/pii/S1368764625001256]
- 9. Persister Cells and Differences From Other Cell Types [https://estechlab.com/persister-cells-and-differences-from-other-cell-types-2/]
- 10. Molecular mechanism and application of emerging ... [https://bmcmicrobiol.biomedcentral.com/articles/10.1186/s12866-024-03628-3]
- 11. From Dormancy to Eradication: Strategies for Controlling ... [https://www.mdpi.com/2304-8158/14/6/1075]
- 12. Antibacterial nanoagents: an emerging arsenal against ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12537890/]
- 13. Toxin–antitoxins and sigma factors may optimize the fitness of ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12440627/]
- 14. Conformational change as a mechanism for toxin activation in ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11575165/]
- 15. Bacterial Persister Cells and Development of Antibiotic ... [https://www.frontierspartnerships.org/journals/british-journal-of-biomedical-science/articles/10.3389/bjbs.2024.12958/full]
- 16. Persister cells: formation, resuscitation and combative ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC8590677/]
- 17. Bacterial Persister Cell Formation and Dormancy - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC3837759/]
- 18. Bacterial persisters: molecular mechanisms and ... - Nature [https://www.nature.com/articles/s41392-024-01866-5]
- 19. The Role of Bacterial Biofilms in Antimicrobial Resistance [https://asm.org/articles/2023/march/the-role-of-bacterial-biofilms-in-antimicrobial-re]
- 20. Bacterial Persister Cells and Development of Antibiotic ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11335562/]
- 21. Observation of persister cell histories reveals diverse ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12074638/]
- 22. Integrative biology of persister cell formation - PubMed Central [https://pmc.ncbi.nlm.nih.gov/articles/PMC9470271/]
- 23. Metabolic aspects of bacterial persisters - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC4205924/]
- 24. Protocol for assessing single-cell persister recovery ... [https://www.sciencedirect.com/science/article/pii/S2666166724001497]
- 25. Therapeutic approaches to addressing drug resistance by ... [https://www.sciencedirect.com/science/article/abs/pii/S1359644625002399]
- 26. Nanodynamic therapy for cancer: mechanistic innovations ... [https://translational-medicine.biomedcentral.com/articles/10.1186/s12967-025-07277-6]
- 27. Cancer cells hijack cell death enzyme to regrow after ... [https://www.news-medical.net/news/20251119/Cancer-cells-hijack-cell-death-enzyme-to-regrow-after-treatment.aspx]
- 28. Cancer Cell Membrane-Coated NPs as a Biomimetic ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12566714/]
- 29. Advances in the multifunctionality of cell membrane ... [https://www.frontiersin.org/journals/immunology/articles/10.3389/fimmu.2025.1657722/full]
- 30. Antimicrobial Peptides and Cationic Nanoparticles [https://pmc.ncbi.nlm.nih.gov/articles/PMC9181033/]
- 31. Membrane Active Antimicrobial Peptides: Translating ... [https://www.frontiersin.org/journals/neuroscience/articles/10.3389/fnins.2017.00073/full]
- 32. Therapeutic peptides and their delivery using lipid-based ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12306875/]
- 33. Antimicrobial peptide biological activity, delivery systems and ... [https://translational-medicine.biomedcentral.com/articles/10.1186/s12967-025-06321-9]
- 34. Artificial transmembrane ion transporters as potential ... [https://www.sciencedirect.com/science/article/pii/S2451929421005349]
- 35. Nanoparticle-mediated approaches to combat antibiotic ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12584957/]
- 36. Recent strategies for developing membrane-targeting ... [https://www.sciencedirect.com/science/article/abs/pii/S0010854525000967]
- 37. Advances in nanoparticles in targeted drug delivery–A review [https://www.sciencedirect.com/science/article/pii/S2666845925001163]
- 38. Bacterial nanotechnology as a paradigm in targeted cancer ... [https://www.nature.com/articles/s41378-024-00743-z]
- 39. Persister Escherichia coli Cells Have a Lower Intracellular pH ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC8406257/]
- 40. Influence of protease inhibitors and energy metabolism on ... [https://www.sciencedirect.com/science/article/pii/0006291X73911583]
- 41. Persister control by leveraging dormancy associated reduction ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC8716142/]
- 42. Waking Up Sleeping Bacteria to Fight Infections [https://www.infectioncontroltoday.com/view/waking-sleeping-bacteria-fight-infections]
- 43. Waking up sleeping bacteria to fight infections [https://www.sciencedaily.com/releases/2019/07/190718112516.htm]
- 44. Synergistic effect of A novel antimicrobial peptide and silver ... [https://amb-express.springeropen.com/articles/10.1186/s13568-025-01979-2]
- 45. Fighting bacterial persistence: Current and emerging anti- ... [https://www.sciencedirect.com/science/article/abs/pii/S1368764618300232]
- 46. Antibiotic-persistent bacterial cells exhibiting low-level ROS ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12345145/]
- 47. Comparing treatment strategies to reduce antibiotic resistance ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC8020770/]
- 48. Cellular Dormancy in Cancer: Mechanisms and Potential ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10372609/]
- 49. Towards understanding cancer dormancy over strategic ... [https://molecular-cancer.biomedcentral.com/articles/10.1186/s12943-025-02250-9]
- 50. Characteristics and molecular mechanism of drug-tolerant ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10360399/]
- 51. An in vitro hydrogel-based model to study dormancy ... [https://www.nature.com/articles/s44385-025-00043-9]
- 52. Inheritable cell-states shape drug-persister correlations and ... [https://journals.plos.org/ploscompbiol/article?id=10.1371/journal.pcbi.1013446]
- 53. Chemoinformatics and Drug Discovery - PMC - PubMed Central [https://pmc.ncbi.nlm.nih.gov/articles/PMC6146447/]
- 54. Comparison of combinatorial clustering methods on ... [https://pubmed.ncbi.nlm.nih.gov/22098113/]
- 55. Comparison of chemical clustering methods using graph [https://www.sciencedirect.com/science/article/pii/S1093326302001882]
- 56. Chemoinformatic Clustered Compound Library [https://lifechemicals.com/screening-libraries/chemoinformatic-clustered-compound-library]
- 57. Physicochemical properties | Medicinal Chemistry Class ... [https://fiveable.me/medicinal-chemistry/unit-4/physicochemical-properties/study-guide/Ez7tCKt21HKLA2y0]
- 58. An analysis of the physicochemical properties of oral drugs ... [https://pubmed.ncbi.nlm.nih.gov/39309358/]
- 59. Using Physicochemical Measurements to Influence Better ... [https://www.sciencedirect.com/science/article/pii/S247255522206806X]
- 60. Rational Design Strategies in DNA-Encoded Libraries for ... [https://pubmed.ncbi.nlm.nih.gov/40708441/]
- 61. A guide to drug discovery [https://www.nature.com/collections/hkgvrspwtn]
- 62. Bridging the Gap: The Role of Advanced Formulation ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12579833/]
- 63. Nanomaterials in Drug Delivery: Strengths and Opportunities ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11173789/]
- 64. Advances in Nanotechnology-Based Drug Delivery Systems [https://pmc.ncbi.nlm.nih.gov/articles/PMC12389492/]
- 65. Drug Delivery Technologies Impacting 2025 and Beyond [https://www.pharmaadvancement.com/pharma-trends/drug-delivery-technologies-impacting-2025-and-beyond/]
- 66. Technological Advancements in Drug Formulation and ... [https://pubmed.ncbi.nlm.nih.gov/41163270/]
- 67. the transformative potential of nanotechnology in medicine [https://www.frontiersin.org/journals/drug-delivery/articles/10.3389/fddev.2025.1556426/full]
- 68. Revolutionizing drug formulation development [https://www.sciencedirect.com/science/article/abs/pii/S0169409X23004234?via%3Dihub]
- 69. Artificial intelligence for drug delivery: Yesterday, today and ... [https://www.sciencedirect.com/science/article/pii/S2211383525006227]
- 70. A rational approach to discovering new persister control ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12406675/]
- 71. A host-directed adjuvant sensitizes intracellular bacterial ... [https://www.nature.com/articles/s41564-025-02124-2]
- 72. Anti-Persisters Activity of Lacticaseibacillus rhamnosus ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11241021/]
- 73. A high-throughput assay identifies molecules with ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11316564/]
- 74. In Vivo vs. In Vitro Models: Key Differences and ... [https://liveonbiolabs.com/in-vivo-vs-in-vitro-models/]
- 75. A Semi-Solid In Vitro Biofilm Model for Evaluating ... [https://www.sciencedirect.com/science/article/pii/S2590207525000760]
- 76. Antimicrobial, Antibiofilm, and Anti-persister Activities of ... [https://www.frontiersin.org/journals/microbiology/articles/10.3389/fmicb.2021.727692/full]
- 77. Emerging Strategies to Combat ESKAPE Pathogens in the Era ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC6452778/]
- 78. Coping with the ESKAPE pathogens: Evolving strategies ... [https://www.sciencedirect.com/science/article/abs/pii/S0882401022005769]
- 79. ESKAPE pathogens rapidly develop resistance against ... [https://www.nature.com/articles/s41564-024-01891-8]
- 80. Repurposing Non-Antibiotic Drugs as Novel Antibacterial ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12563741/]
- 81. Leading AI-Driven Drug Discovery Platforms [https://www.sciencedirect.com/science/article/abs/pii/S0031699725075118]
- 82. Artificial intelligence in drug discovery and development - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC7577280/]
- 83. AI-driven drug discovery using a context-aware hybrid ... [https://www.nature.com/articles/s41598-025-19593-4]
- 84. Making science run at the speed of thought: the reality of AI ... [https://www.drugtargetreview.com/article/190632/making-science-run-at-the-speed-of-thought-the-reality-of-ai-in-drug-discovery-part-1/]
- 85. Cancer drug-tolerant persister cells: from biological questions ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12622869/]
- 86. Drug-induced tolerant persisters in tumor - Molecular Cancer [https://molecular-cancer.biomedcentral.com/articles/10.1186/s12943-025-02323-9]
- 87. Virtual Patients in Clinical Trials for Drug Development [https://pmc.ncbi.nlm.nih.gov/articles/PMC12228009/]