Nanoparticle-Mediated CRISPR-Cas9 Delivery: A Precision Strike Against Treatment-Resistant Biofilms
The convergence of CRISPR-Cas9 gene-editing technology with advanced nanoparticle delivery systems represents a paradigm shift in combating biofilm-associated antimicrobial resistance.
Nanoparticle-Mediated CRISPR-Cas9 Delivery: A Precision Strike Against Treatment-Resistant Biofilms
Abstract
The convergence of CRISPR-Cas9 gene-editing technology with advanced nanoparticle delivery systems represents a paradigm shift in combating biofilm-associated antimicrobial resistance. This article provides a comprehensive analysis for researchers and drug development professionals, exploring the foundational science behind biofilm recalcitrance and the mechanistic synergy of CRISPR-nanoparticle hybrids. It details cutting-edge methodological approaches, including the design of lipid-based, polymeric, and metallic nanocarriers for efficient CRISPR component delivery. The content further addresses critical troubleshooting for optimization—tackling delivery inefficiency, off-target effects, and nanotoxicity—and validates the strategy through comparative analysis with conventional therapies. By synthesizing recent advances and persistent challenges, this review outlines a roadmap for translating these innovative platforms into next-generation, precision antimicrobial therapies.
The Biofilm Challenge and the CRISPR-Nanoparticle Synergy
Biofilms represent a predominant mode of bacterial life, characterized by structured microbial communities encased in a self-produced matrix of Extracellular Polymeric Substances (EPS) [1]. This matrix, which can constitute up to 85% of the biofilm volume, is a complex mixture of exopolysaccharides, proteins, extracellular DNA (eDNA), and lipids that provides critical structural integrity and protection [2] [1]. The transition from free-floating planktonic cells to a biofilm lifestyle confers a survival advantage, allowing bacteria to tolerate antimicrobial agents at concentrations up to 1000 times higher than those required to eliminate their planktonic counterparts [2] [3] [4]. This remarkable resilience makes biofilm-associated infections particularly challenging in clinical settings, contributing significantly to the global antimicrobial resistance (AMR) crisis that causes an estimated 700,000 deaths annually [2] [4].
The architecture of a mature biofilm is not a random aggregation of cells but a highly organized, heterogeneous structure often described as a "fortress" [2] [5]. Advanced imaging techniques reveal a complex topography with microcolonies interspersed with water channels that facilitate nutrient distribution and waste removal [2]. This sophisticated organization creates diverse microenvironments with gradients of oxygen, nutrients, and pH, leading to metabolic heterogeneity among the embedded bacterial cells [2] [6]. Understanding this architectural complexity is fundamental to developing effective strategies, such as nanoparticle-delivered CRISPR-Cas9, to dismantle these microbial strongholds.
The Structural and Functional Organization of Biofilms
Stages of Biofilm Development
Biofilm formation is a dynamic, multi-stage process that transforms individual planktonic cells into a complex, coordinated community:
- Initial Attachment: Planktonic cells reversibly adhere to surfaces (both biotic and abiotic) through weak forces like van der Waals interactions and hydrophobic effects [5]. Surface proteins such as biofilm-associated protein (BAP), SasG, and fibronectin-binding proteins facilitate this initial contact [5].
- Irreversible Attachment: Cells anchor themselves more permanently by producing adhesins and beginning EPS secretion, transitioning from reversible to stable attachment [2] [5].
- Maturation I: Microcolonies form and develop into a three-dimensional structure. The EPS matrix matures, and water channels develop to circulate nutrients and signals [2] [5]. Quorum sensing (QS) mechanisms coordinate population-wide behavior through autoinducer molecules [5].
- Maturation II: The biofilm reaches its peak architectural complexity, with prominent water channels and specialized, metabolically heterogeneous subpopulations of bacteria, including dormant persister cells [2] [6].
- Dispersion: Controlled detachment of individual cells or clusters from the biofilm occurs, allowing bacteria to colonize new surfaces and begin the cycle anew [2] [5].
Composition and Role of the Extracellular Polymeric Substance (EPS)
The EPS matrix is the defining component of biofilm architecture and its primary defense mechanism. The composition and function of key EPS constituents are detailed below:
Table 1: Key Components of the Biofilm Extracellular Polymeric Substance (EPS) Matrix
| EPS Component | Primary Composition | Functional Role in Biofilm Resistance |
|---|---|---|
| Exopolysaccharides | Alginate, cellulose, poly-N-acetylglucosamine (PNAG) | Forms a viscous physical barrier that limits antibiotic penetration and provides mechanical stability [2] [5]. |
| Proteins | Adhesins, amyloids, extracellular enzymes | Strengthens structural integrity and facilitates adhesion to surfaces and other cells [2] [5]. |
| Extracellular DNA (eDNA) | DNA from lysed bacterial cells | Contributes to matrix stability, chelates cationic antimicrobial peptides (AMPs), and facilitates horizontal gene transfer [2] [5]. |
| Lipids & Other Polymers | Surfactants, phospholipids | Modifies surface properties, contributes to hydrophobicity, and can act as a nutrient source [6]. |
Mechanisms of Antimicrobial Resistance in Biofilms
The protective nature of biofilms arises from a confluence of physical, physiological, and genetic mechanisms that operate simultaneously to defeat antimicrobial challenges.
Physical and Physiological Barriers
The EPS matrix acts as a dual physical barrier, significantly slowing the diffusion of antimicrobial agents into the biofilm's deeper layers while simultaneously binding and neutralizing these molecules, preventing them from reaching their cellular targets [2] [4] [5]. This limited penetration is a cornerstone of biofilm-associated tolerance.
Within the mature biofilm, environmental gradients (e.g., of oxygen and nutrients) create heterogeneous microenvironments [2] [6]. Bacteria in the inner core often enter a slow-growing or dormant state due to nutrient limitation. Since most conventional antibiotics target active cellular processes like cell wall synthesis or protein production, these dormant cells exhibit dramatically increased tolerance [2] [4]. A subpopulation of these, known as persister cells, can survive high-dose antibiotic exposure despite being genetically identical to susceptible cells, often leading to infection recurrence [6].
Genetic and Adaptive Resistance Mechanisms
The close proximity of cells within the biofilm matrix drastically enhances the efficiency of Horizontal Gene Transfer (HGT) via conjugation, transformation, or transduction [2] [6]. This turns biofilms into "hotspots" for the dissemination of antibiotic resistance genes, such as those encoding for beta-lactamase enzymes or efflux pumps, accelerating the development of multidrug-resistant (MDR) pathogens [2] [6].
Furthermore, biofilm communities utilize a sophisticated cell-to-cell communication system called Quorum Sensing (QS). Bacteria release and detect signaling molecules known as autoinducers; when a critical threshold concentration is reached, population-wide changes in gene expression are triggered [5]. QS regulates key biofilm behaviors, including EPS production, virulence factor secretion, and metabolic coordination, making it a master regulator of biofilm maintenance and pathogenicity [7] [5].
Table 2: Primary Mechanisms of Biofilm-Associated Antimicrobial Resistance
| Resistance Mechanism | Description | Impact on Antibiotic Efficacy |
|---|---|---|
| Physical Diffusion Barrier | EPS matrix binds and reters diffusion of antimicrobials. | Reduces antibiotic concentration reaching inner cells; can require 10-1000x higher doses [2] [4]. |
| Metabolic Heterogeneity | Gradients create zones of slow/dormant bacterial growth. | Antibiotics targeting active processes (e.g., β-lactams) become ineffective against dormant cells [2] [6]. |
| Horizontal Gene Transfer | Facilitates plasmid-borne resistance gene exchange. | Rapidly spreads resistance determinants (e.g., bla, mecA, ndm-1) across the population [2] [6]. |
| Persister Cell Formation | A small subpopulation enters a dormant, tolerant state. | Survives high-dose antibiotic treatment, leading to chronic infection relapse [2] [6]. |
Experimental Protocols for Biofilm Analysis
Protocol: Confocal Laser Scanning Microscopy (CLSM) for 3D Biofilm Architecture
Purpose: To visualize and quantitatively analyze the three-dimensional structure, biovolume, and spatial organization of live biofilms.
Materials:
- Strain(s): Biofilm-forming bacteria (e.g., Pseudomonas aeruginosa, Staphylococcus aureus)
- Growth Medium: Appropriate broth (e.g., Tryptic Soy Broth, LB Broth)
- Substrate: Sterile glass-bottom culture dishes or specialized coverslips
- Vital Fluorescent Stains: SYTO 9 (for live cell nucleic acids), Propidium Iodide (for dead cell nucleic acids), ConA-TRITC (for polysaccharides)
- Imaging System: Confocal Laser Scanning Microscope with appropriate laser lines and filters
Procedure:
- Biofilm Growth: Inoculate bacteria in culture medium and incubate with glass substrate under static or flow conditions for desired time (e.g., 24-72 hours) to form mature biofilms.
- Staining Preparation: Prepare staining solution in buffer. A common live/dead stain uses a 1:1 mixture of SYTO 9 and Propidium Iodide.
- Staining Protocol: Gently rinse the biofilm to remove non-adherent cells. Apply the staining solution to completely cover the biofilm. Incubate in the dark at room temperature for 15-30 minutes.
- Image Acquisition: Gently rinse the stained biofilm to remove excess dye. Image immediately using CLSM. For SYTO 9, use an argon laser (excitation ~488 nm) and detect emission at 500-550 nm.
- 3D Reconstruction & Analysis: Collect Z-stack images at regular intervals (e.g., 1 µm steps) through the entire biofilm depth. Use image analysis software (e.g., ImageJ with BiofilmQ plugin) to calculate biovolume, thickness, surface area, and roughness coefficient.
Protocol: Microtiter Plate Assay for Anti-biofilm Compound Screening
Purpose: To quantitatively assess the efficacy of novel anti-biofilm agents (e.g., CRISPR-NP formulations) in inhibiting biofilm formation or eradicating pre-formed biofilms.
Materials:
- Strain(s): Biofilm-forming bacteria
- Equipment: 96-well flat-bottom polystyrene microtiter plate, plate reader (OD600)
- Reagents: Growth broth, PBS, Crystal Violet stain (0.1% w/v), acetic acid (33% v/v)
- Test Formulations: CRISPR-Cas9 nanoparticle complexes, control nanoparticles, free antibiotics
Procedure:
- Biofilm Formation Assay:
- Dilute an overnight bacterial culture in fresh medium to ~1x10^6 CFU/mL.
- Dispense 100 µL per well into the microtiter plate. Include medium-only wells as negative controls.
- Add 100 µL of serially diluted test formulations to treatment wells.
- Incubate statically for 24-48 hours at appropriate temperature.
Biofilm Eradication Assay:
- First, incubate the bacterial inoculum in wells for 24 hours to allow mature biofilms to form.
- Carefully aspirate the planktonic culture and gently wash wells with PBS.
- Add fresh medium containing the test formulations to the pre-formed biofilms.
- Incubate for an additional 24 hours.
Biofilm Quantification (Crystal Violet Staining):
- Aspirate contents of wells and wash gently with PBS to remove non-adherent cells.
- Air-dry the plate for 30-60 minutes.
- Add 125 µL of 0.1% Crystal Violet to each well, stain for 15 minutes.
- Wash plate thoroughly under running tap water to remove excess stain.
- Add 125 µL of 33% acetic acid to solubilize the stain bound to the biofilm.
- Measure the optical density at 600 nm (OD600) using the plate reader.
Data Analysis: Calculate the percentage of biofilm inhibition or eradication relative to untreated control wells. Perform statistical analysis on replicate wells (typically n=6-8).
Pathway Visualization: Biofilm Development and Disruption Strategies
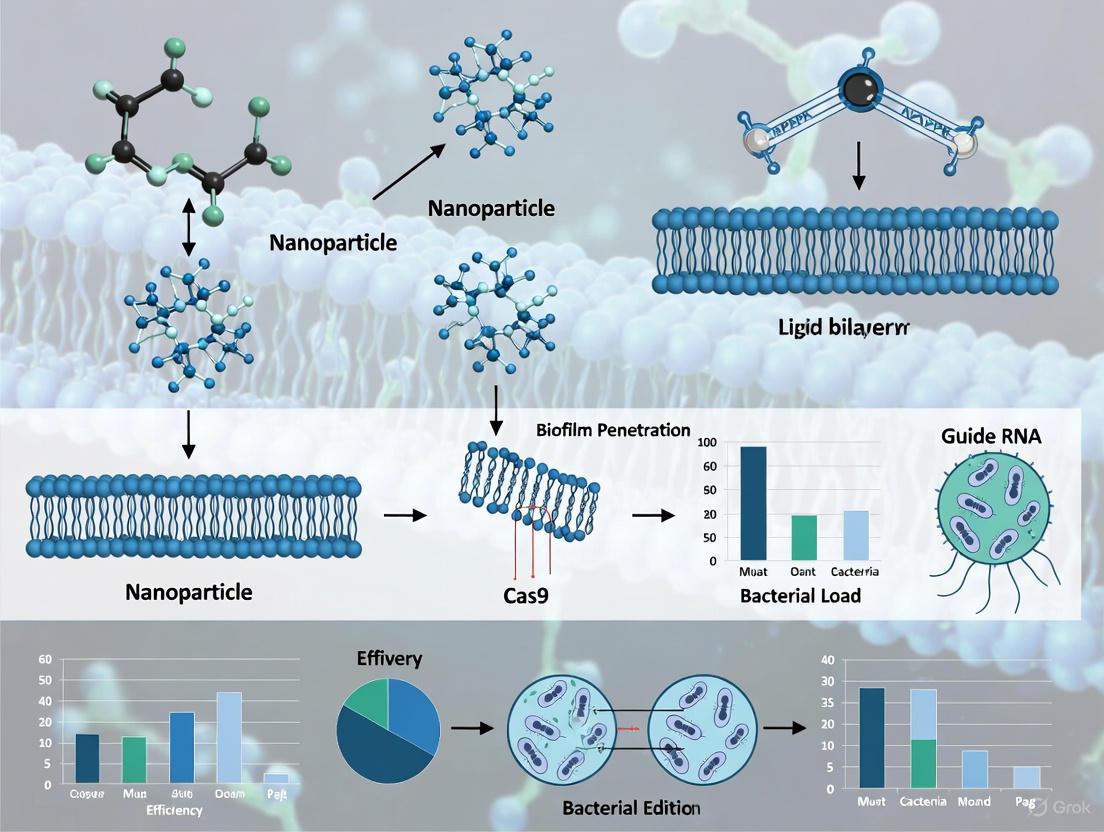
Diagram 1: Biofilm development cycle and NP-CRISPR disruption strategies. The diagram illustrates the staged process of biofilm formation and the key resistance mechanisms that emerge. It also maps how nanoparticle-delivered CRISPR-Cas9 strategies target these specific mechanisms for precise biofilm disruption.
The Scientist's Toolkit: Research Reagent Solutions
Table 3: Essential Research Reagents for Investigating NP-Delivered CRISPR-Cas9 Anti-biofilm Strategies
| Research Reagent / Material | Function & Application | Key Considerations |
|---|---|---|
| CRISPR-Cas9 Plasmid System | Expresses Cas9 nuclease and guide RNA (gRNA) for targeted gene editing. | Select promoters functional in target species (e.g., P. aeruginosa). gRNA must be designed against specific biofilm genes (e.g., pelA, pslD for EPS, lasI for QS) [2] [7]. |
| Lipid Nanoparticles (LNPs) | Biocompatible nanocarriers for encapsulating and delivering CRISPR payload. | Formulations with cationic lipids enhance complexation with nucleic acids. LNPs have demonstrated >90% reduction in P. aeruginosa biofilm biomass in vitro [2] [8]. |
| Gold Nanoparticles (AuNPs) | Inorganic nanocarriers for CRISPR component delivery. | Facile surface functionalization with thiolated biomolecules. AuNP-CRISPR hybrids show ~3.5x higher editing efficiency than non-carrier systems [2] [8]. |
| Quorum Sensing Inhibitors (QSIs) | Small molecules (e.g., AHL analogs) or natural compounds (e.g., curcumin) that disrupt bacterial communication. | Used as synergistic agents with CRISPR-NP therapy. Validate efficacy via reporter strain assays (e.g., lasB-gfp) [6] [5]. |
| EPS Degrading Enzymes | Enzymes such as Dispersin B (glycosidase) or DNase I to disrupt the biofilm matrix. | Pre-treatment with enzymes enhances NP penetration into biofilms. Use in combination therapies to weaken the EPS barrier [6]. |
| Metabolic Stains (e.g., CTC, XTT) | To assess bacterial metabolic activity and viability within biofilms post-treatment. | Differentiates between metabolic states; crucial for evaluating effects on dormant persister cells that standard CFU counts may miss [1]. |
| Anti-biofilm Peptides | Synthetic or natural antimicrobial peptides (AMPs) that disrupt membranes. | Co-delivery with CRISPR-NPs for a multi-mechanism attack. Select peptides with proven activity against target biofilm species [6]. |
Biofilms are structured communities of microbial cells enclosed in a self-produced extracellular polymeric substance (EPS) and adherent to biotic or abiotic surfaces [9]. This aggregated lifestyle represents the predominant mode of bacterial growth in nature and clinical settings, contributing significantly to the challenge of treating bacterial infections [10]. The transition from free-floating planktonic cells to surface-attached biofilms involves major physiological changes that confer enhanced tolerance to antimicrobial agents and host immune responses [10] [11].
The clinical impact of biofilm-associated infections is substantial, contributing to chronic infections that are notoriously difficult to eradicate [10]. Biofilms are implicated in numerous medical scenarios, including infections of indwelling medical devices (e.g., catheters, prosthetic joints), chronic wounds, cystic fibrosis lung infections, and infective endocarditis [10] [12]. The persistent nature of these infections results in significant morbidity, mortality, and healthcare costs, with an estimated nearly $300 billion spent annually globally on managing biofilm-associated wound infections alone [10]. Understanding the mechanisms underlying biofilm-mediated resistance is therefore crucial for developing effective therapeutic strategies.
Physical and Structural Barrier Mechanisms
The Extracellular Polymeric Substance Matrix as a Physical Barrier
The extracellular matrix is a defining characteristic of biofilms, constituting over 90% of the biofilm mass and serving as a primary defense mechanism [10] [12]. This complex matrix comprises various biopolymers, including polysaccharides, proteins, lipids, and extracellular DNA (eDNA), which collectively create a formidable physical and chemical barrier to antimicrobial penetration [10] [11].
Table 1: Major Components of Biofilm Extracellular Polymeric Substance (EPS) Matrix and Their Protective Functions
| EPS Component | Chemical Composition | Protective Function in Biofilms |
|---|---|---|
| Polysaccharides | Poly-N-acetylglucosamine, alginate, cellulose | Structural scaffolding, cation sequestration, barrier formation |
| Extracellular DNA (eDNA) | DNA from lysed cells | Structural integrity, cation chelation, antibiotic binding |
| Proteins | Adhesins, amyloids, enzymes | Structural stability, enzymatic degradation of antimicrobials |
| Lipids | Phospholipids, surfactants | Hydrophobic barriers, surface modification |
The matrix hinders antibiotic penetration through multiple mechanisms. Some antibiotics form complexes with matrix components or are degraded by matrix-associated enzymes, effectively reducing the concentration reaching bacterial cells [10]. Positively charged aminoglycosides, for instance, bind to negatively charged eDNA in the matrix, significantly slowing antibiotic penetration [10]. In chronic infections such as those in the cystic fibrosis lung, eDNA produced by Pseudomonas aeruginosa combines with host-derived DNA to form a physical shield that protects the biofilm from tobramycin and host immune cells [10]. Similarly, host neutrophil extracellular traps (NETs) can surround ocular P. aeruginosa biofilms, creating an additional barrier that limits antibiotic access while containing bacterial dissemination [10].
Biofilm Lifecycle and Structural Heterogeneity
Biofilm development follows a defined lifecycle comprising distinct stages: initial attachment, irreversible attachment, micro-colony formation, maturation, and dispersion [10] [9]. This progression creates a heterogeneous three-dimensional architecture characterized by microcolonies interspersed with water channels that facilitate nutrient distribution and waste removal [13] [9].
The structural heterogeneity of mature biofilms creates diverse microenvironments with gradients of nutrients, oxygen, pH, and metabolic waste products [13] [11]. This spatial organization significantly influences microbial physiology and contributes to variations in antimicrobial susceptibility within different biofilm regions [13]. Cells in the inner layers often experience nutrient and oxygen limitations, leading to reduced metabolic activity and growth rates that enhance antimicrobial tolerance [11] [9].
Diagram 1: Biofilm Development Lifecycle and Structural Features. The diagram illustrates the sequential stages of biofilm formation and key structural developments that contribute to antimicrobial resistance.
Physiological and Genetic Resistance Mechanisms
Metabolic Heterogeneity and Persister Cell Formation
Within biofilms, bacterial populations exhibit significant metabolic heterogeneity, with subpopulations of cells existing in various physiological states [13] [12]. Persister cells represent a small subset of metabolically dormant bacterial cells that exhibit exceptional tolerance to antimicrobial agents without undergoing genetic resistance mutations [12]. These phenotypic variants can survive high concentrations of antibiotics by reducing their metabolic activity and growth rates, effectively minimizing the corrupting action of bactericidal antibiotics that typically target active cellular processes [12].
The formation of persister cells is controlled by bacterial growth phases and environmental stress factors [12]. While persisters constitute only a small fraction of exponentially growing cells, their proportion increases significantly during stationary phase and in mature biofilms where nutrient limitations induce metabolic dormancy [12]. When antibiotic pressure is removed, these dormant persister cells can resuscitate and repopulate the biofilm, leading to recurrent infections and treatment failures [12].
The molecular mechanisms underlying persistence involve bacterial stress response pathways, particularly those activated by DNA damage [12]. Environmental stressors encountered during infection activate these pathways, upregulating DNA repair functions and facilitating survival under harsh conditions, including antibiotic exposure [12]. This "neither-grow-nor-die" state enables bacterial pathogens to withstand both antimicrobial treatment and host immune responses, contributing significantly to chronic and relapsing infections [12].
Enhanced Horizontal Gene Transfer and Resistance Gene Acquisition
The dense, structured environment of biofilms facilitates efficient exchange of genetic material between bacterial cells through horizontal gene transfer (HGT), accelerating the development and dissemination of antibiotic resistance [10] [11]. The close cell-to-cell contact within the biofilm matrix enhances conjugation efficiency, while the presence of extracellular DNA in the matrix provides a reservoir for natural transformation [10] [12].
Table 2: Mechanisms of Antibiotic Resistance in Biofilm Communities
| Resistance Mechanism | Process | Impact on Antibiotic Efficacy |
|---|---|---|
| Restricted Penetration | Physical barrier of EPS matrix limiting antibiotic diffusion | Reduced antibiotic concentration reaching interior cells |
| Metabolic Dormancy | Reduced growth rate and metabolic activity of persister cells | Decreased efficacy of bactericidal antibiotics |
| Horizontal Gene Transfer | Plasmid exchange and transformation within dense biofilm communities | Dissemination of resistance genes across population |
| Efflux Pump Overexpression | Upregulation of multidrug efflux systems | Active extrusion of antibiotics from bacterial cells |
| Enzymatic Inactivation | Production of antibiotic-modifying enzymes (e.g., β-lactamases) | Direct degradation or modification of antibiotic molecules |
Biofilms not only promote the acquisition of resistance genes but also provide a protective environment for the emergence and selection of resistant mutants [12]. Studies using E. coli biofilms have demonstrated elevated mutation rates in response to antibiotic pressure, with mutations occurring in genes such as sbmA (encoding an inner membrane peptide transporter) and fusA (encoding elongation factor G) following treatment with amikacin [12]. Similarly, in cystic fibrosis patients with chronic P. aeruginosa lung infections, repeated antibiotic exposure selects for high-persister (hip) mutants with enhanced tolerance phenotypes, demonstrating the direct correlation between persister formation and treatment failure [12].
Experimental Protocols for Studying Biofilm Resistance
Standardized Biofilm Cultivation and Analysis Workflow
Diagram 2: Standard Workflow for Biofilm Antimicrobial Susceptibility Testing. The protocol outlines key steps for evaluating anti-biofilm efficacy of novel therapeutic agents.
Protocol 4.1.1: Microtiter Plate Biofilm Formation Assay
Purpose: To establish reproducible in vitro biofilm models for evaluating antimicrobial susceptibility and resistance mechanisms.
Materials:
- Bacterial strains: Relevant clinical isolates or laboratory strains (e.g., P. aeruginosa, S. aureus)
- Growth media: Tryptic soy broth (TSB), Luria-Bertani (LB) broth, or specific media optimized for biofilm formation
- Surfaces: Polystyrene microtiter plates, glass coupons, or relevant biomedical materials
- Staining reagents: Crystal violet (0.1% w/v), safranin, or fluorescent nucleic acid stains (SYTO9)
- Equipment: Microplate reader, confocal laser scanning microscope (CLSM), scanning electron microscope (SEM)
Methodology:
- Inoculum Preparation: Grow bacterial cultures to mid-log phase (OD600 ≈ 0.5) and dilute to approximately 10^6 CFU/mL in appropriate growth medium.
- Surface Conditioning: For medical material testing, precondition surfaces with relevant biological fluids (e.g., plasma, serum) to mimic in vivo conditions [10].
- Biofilm Development: Add 200 μL bacterial suspension per well of 96-well plate. Incubate statically for 24-48 hours at optimal growth temperature (e.g., 37°C for human pathogens).
- Maturation Monitoring: Monitor biofilm development at 4-hour intervals using optical density measurements or microscopy to establish growth kinetics.
- Biofilm Quantification:
- Remove planktonic cells by gently washing wells with phosphate-buffered saline (PBS).
- Fix biofilms with 99% methanol for 15 minutes.
- Stain with 0.1% crystal violet for 20 minutes.
- Wash excess stain and solubilize bound stain with 33% acetic acid.
- Measure absorbance at 570-600 nm using microplate reader.
- Structural Analysis: For CLSM imaging, stain with LIVE/DEAD BacLight bacterial viability kit according to manufacturer's instructions and visualize using appropriate laser settings.
Quality Control: Include known strong and weak biofilm-forming strains as positive and negative controls. Perform technical replicates (n≥3) and biological replicates (n≥3) for statistical analysis.
Protocol for Evaluating CRISPR-Based Biofilm Disruption
Protocol 4.2.1: Nanoparticle-Mediated CRISPR Delivery Against Biofilms
Purpose: To assess efficacy of CRISPR-Cas9 systems delivered via nanoparticle carriers for targeted disruption of biofilm-related genes.
Materials:
- CRISPR Components: Cas9 nuclease (as plasmid, mRNA, or ribonucleoprotein), guide RNAs targeting biofilm-associated genes (e.g., pelA, pslD, alg8 for polysaccharide synthesis; lasR, rhlR for quorum sensing)
- Nanoparticle Carriers: Lipid nanoparticles (LNPs), gold nanoparticles, or polymeric nanoparticles optimized for bacterial delivery
- Biofilm Models: Established 24-48 hour biofilms of target pathogens in appropriate in vitro systems
- Assessment Tools: qPCR for gene expression, confocal microscopy for structural analysis, colony counting for viability assessment
Methodology:
- CRISPR-Nanoparticle Formulation:
- Complex CRISPR-Cas9 components (RNP preferred for immediate activity) with cationic lipid or polymer nanoparticles at optimal N:P ratios.
- Characterize nanoparticle size (target 50-200 nm), zeta potential, and encapsulation efficiency.
- Validate gene editing efficiency in planktonic cultures before biofilm application.
Biofilm Treatment:
- Establish mature biofilms (48-72 hours) in flow cell systems or on relevant substrates.
- Apply CRISPR-nanoparticle formulations at varying concentrations (e.g., 0.1-10 μg/mL CRISPR component).
- Include control treatments: naked CRISPR, nanoparticles alone, and scrambled gRNA complexes.
- For flow cells, maintain constant flow (0.2-0.5 mm/s) during treatment to mimic physiological conditions.
Efficacy Assessment:
- Biomass Quantification: Measure biofilm biomass pre- and post-treatment using crystal violet staining or SYTOX Green nucleic acid staining.
- Viability Analysis: Dissociate biofilms by sonication and plate serial dilutions for CFU enumeration.
- Structural Integrity: Assess biofilm architecture via CLSM and COMSTAT analysis.
- Gene Editing Confirmation: Extract biofilm DNA and perform targeted sequencing to verify specific gene disruption.
- Resistance Gene Elimination: Monitor reduction in antibiotic resistance gene prevalence (e.g., bla, mecA, ndm-1) via qPCR [13].
Optimization Notes:
- Lipid nanoparticle formulations have demonstrated >90% reduction in P. aeruginosa biofilm biomass in vitro when targeting essential biofilm genes [13].
- Gold nanoparticle carriers can enhance editing efficiency up to 3.5-fold compared to non-carrier systems [13].
- Co-delivery with conventional antibiotics may produce synergistic effects—test combinations with tobramycin, ciprofloxacin, or meropenem based on target pathogen.
The Scientist's Toolkit: Research Reagent Solutions
Table 3: Essential Research Reagents for Biofilm and CRISPR-Cas9 Studies
| Reagent/Category | Specific Examples | Research Application | Key Considerations |
|---|---|---|---|
| Biofilm Matrix Stains | Crystal violet, SYTO9, Calcofluor white, Congo red | Biofilm quantification and visualization | Differential staining of matrix components; compatibility with fixation methods |
| CRISPR-Cas9 Systems | SpCas9, SaCas9, AsCas12a; plasmid, mRNA, or RNP formats | Targeted gene disruption in biofilm-associated genes | RNP format reduces off-target effects; consider PAM requirements for target selection |
| Nanoparticle Delivery Systems | Cationic lipid nanoparticles (LNPs), gold nanoparticles, chitosan nanoparticles | Delivery of CRISPR components through biofilm matrix | Size (50-200 nm) and surface charge critical for penetration; bacterial toxicity screening required |
| Quorum Sensing Inhibitors | Furanones, ambuic acid, triclosan (research use) | Disruption of cell-to-cell signaling in biofilms | Specificity for pathogen QS systems; potential synergy with antimicrobials |
| Biofilm Dispersal Agents | D-amino acids, dispersin B, DNase I, glycoside hydrolases | Induction of biofilm dispersal for enhanced antimicrobial penetration | Enzyme stability in biofilm environment; potential immune activation in vivo |
| Metabolic Activity Probes | Resazurin, CTC, SYTOX Green, propidium iodide | Assessment of bacterial viability and metabolic status within biofilms | Distinction between bactericidal and bacteriostatic effects; penetration depth limitations |
Integration with Nanoparticle-Delivered CRISPR-Cas9 Therapeutics
The elucidated mechanisms of biofilm-mediated resistance directly inform the development of nanoparticle-delivered CRISPR-Cas9 strategies for biofilm eradication. The physical barrier function of the EPS matrix necessitates nanoparticle carriers capable of effective penetration and distribution throughout the biofilm architecture [13] [9]. Lipid nanoparticles (LNPs) and gold nanoparticles have demonstrated particular promise, achieving significant biofilm biomass reduction (>90% in P. aeruginosa models) and enhanced gene-editing efficiency (3.5-fold improvement compared to non-carrier systems) [13].
The metabolic heterogeneity and persister cell populations within biofilms highlight the importance of targeting essential genes that are required for both active and dormant cell survival [12]. CRISPR-Cas9 systems can be designed to target core cellular processes, resistance genes (e.g., bla, mecA, ndm-1), or biofilm-specific genes (e.g., quorum sensing regulators, matrix biosynthesis genes) to overcome phenotypic tolerance [13] [11]. The programmable specificity of CRISPR systems enables targeted elimination of pathogenic species while preserving commensal microbiota, addressing a significant limitation of broad-spectrum antibiotics [13] [14].
Advanced delivery strategies exploit the biofilm microenvironment for enhanced therapeutic efficacy. Nanoparticles can be engineered with enzyme-responsive coatings that degrade upon encounter with matrix components (e.g., DNase-functionalized particles for eDNA-rich matrices), facilitating deeper penetration [13] [9]. Similarly, quorum-sensing inhibitors can be co-delivered with CRISPR components to disrupt cell-cell communication and sensitize biofilms to conventional antibiotics [11] [9].
The integration of CRISPR-based antimicrobials with nanoparticle delivery systems represents a paradigm shift in addressing biofilm-mediated resistance, moving beyond growth inhibition to targeted genetic disruption of resistance mechanisms and biofilm integrity. As these technologies advance toward clinical application, understanding the fundamental resistance mechanisms outlined in this article will continue to guide the development of effective anti-biofilm strategies.
The Clustered Regularly Interspaced Short Palindromic Repeats (CRISPR) and CRISPR-associated (Cas) proteins constitute an adaptive immune system in prokaryotes that protects bacteria from foreign genetic elements such as viruses and plasmids [15]. First identified in E. coli in 1987 and later characterized as a bacterial defense mechanism, this system was repurposed into a revolutionary gene-editing tool following key discoveries by Emmanuelle Charpentier and Jennifer Doudna, who demonstrated that the system could be programmed for precise DNA cleavage [15]. This breakthrough earned them the 2020 Nobel Prize in Chemistry and opened unprecedented possibilities for precision genome modification [15].
The significance of CRISPR-Cas9 technology extends across multiple disciplines, including microbiology and therapeutic development. Within the context of combating biofilm-mediated antibiotic resistance, CRISPR-Cas9 offers a novel approach to target specific genetic elements that confer survival advantages to pathogenic bacteria [13] [11]. When integrated with nanoparticle-mediated delivery, this technology presents a promising strategy for overcoming the physical and biological barriers posed by biofilm matrices, potentially revolutionizing treatment approaches for persistent infections [13] [8].
Molecular Mechanisms of the CRISPR-Cas9 System
Core Components and Their Functions
The CRISPR-Cas9 system consists of two fundamental components that work in concert to achieve targeted DNA cleavage: the Cas9 nuclease and the guide RNA (gRNA) [13] [15].
Cas9 Nuclease: This enzyme acts as molecular scissors, creating double-strand breaks in DNA at precise locations specified by the gRNA [13]. The Cas9 protein contains multiple domains, including the HNH and RuvC nuclease domains, each responsible for cleaving one DNA strand [15].
Guide RNA (gRNA): This synthetic RNA molecule is a fusion of two natural RNA components: CRISPR RNA (crRNA) and trans-activating CRISPR RNA (tracrRNA) [15]. The gRNA includes a ~20 nucleotide sequence that is complementary to the target DNA site, directing Cas9 to this specific genomic locus through base-pairing [15].
Protospacer Adjacent Motif (PAM): This short (2-6 base pair) DNA sequence adjacent to the target site is essential for Cas9 recognition and binding [15]. The PAM sequence varies depending on the bacterial source of the Cas9 protein, with the most commonly used Streptococcus pyogenes Cas9 requiring a 5'-NGG-3' PAM [15].
The following diagram illustrates the relationship between these core components and the sequential process of DNA targeting and cleavage:
Functional Mechanism: From Target Recognition to DNA Cleavage
The CRISPR-Cas9 mechanism operates through a sequential process that ensures precise targeting of specific genetic sequences. Initially, the Cas9 nuclease forms a complex with the gRNA, creating a ribonucleoprotein complex that surveys the genome for potential target sites [15]. This surveillance is guided by the gRNA's complementary region, which base-pairs with matching DNA sequences. However, Cas9 only initiates binding when it recognizes a compatible PAM sequence immediately adjacent to the target site [15]. This PAM requirement serves as a safeguard mechanism, preventing unintended cleavage of the bacterial CRISPR locus itself, which lacks these adjacent motifs [15].
Once the Cas9-gRNA complex identifies a target sequence with the appropriate PAM, it undergoes a conformational change that activates its nuclease domains. The HNH domain cleaves the DNA strand complementary to the gRNA, while the RuvC domain cleaves the opposite strand, resulting in a precise double-strand break [15]. This break triggers the cell's natural DNA repair mechanisms—either non-homologous end joining (NHEJ) or homology-directed repair (HDR)—which can be harnessed to introduce specific genetic modifications, such as gene knockouts, insertions, or corrections [15].
Quantitative Performance Metrics of CRISPR-Cas9 Systems
The efficacy of CRISPR-Cas9 systems varies depending on delivery method, target organism, and experimental conditions. The table below summarizes key performance metrics from recent studies, particularly those relevant to antibacterial applications:
Table 1: Performance Metrics of CRISPR-Cas9 Systems in Antimicrobial Applications
| System Configuration | Target Organism/Application | Efficiency Metrics | Experimental Conditions |
|---|---|---|---|
| Liposomal Cas9 Formulations | Pseudomonas aeruginosa biofilm | >90% reduction in biofilm biomass [13] | In vitro culture systems [13] |
| Gold Nanoparticle Carriers | Bacterial gene editing | 3.5× enhancement in editing efficiency compared to non-carrier systems [13] | Laboratory strains [13] |
| CRISPR-Cas9 with Antibiotic Co-delivery | Biofilm-associated infections | Superior biofilm disruption via synergistic effects [13] | In vitro models [8] |
Research Reagent Solutions for CRISPR-Cas9 Experiments
Implementing CRISPR-Cas9 technology requires specific reagents and materials. The following table outlines essential components for establishing CRISPR-Cas9 workflows in a research setting, with particular emphasis on applications against bacterial biofilms:
Table 2: Essential Research Reagents for CRISPR-Cas9 Experiments
| Reagent/Material | Function/Purpose | Examples/Specifications |
|---|---|---|
| Cas9 Nuclease | Target DNA cleavage | Wild-type S. pyogenes Cas9, codon-optimized variants [15] |
| Guide RNA Components | Target recognition and Cas9 guidance | Synthetic crRNA:tracrRNA duplex or single-guide RNA (sgRNA) [15] |
| Nanoparticle Delivery Systems | Enhanced cellular delivery and stability | Liposomal nanoparticles, gold nanoparticles [13] |
| Antibiotic Resistance Genes | Selection of successfully transformed cells | Kanamycin, ampicillin, or other relevant resistance markers [11] |
| Bacterial Biofilm Models | Experimental testing of anti-biofilm efficacy | ESKAPE pathogen biofilms (P. aeruginosa, S. aureus) [9] |
| PAM-compatible Plasmids | Target sequence validation and screening | Vectors containing appropriate PAM sequences (5'-NGG-3' for SpCas9) [15] |
Application Notes: CRISPR-Cas9 for Biofilm Eradication
Targeting Strategic Genetic Elements in Biofilm-Forming Bacteria
CRISPR-Cas9 can be programmed to disrupt specific genetic targets that are crucial for biofilm formation and maintenance in pathogenic bacteria. The most promising targets include:
Antibiotic Resistance Genes: CRISPR-Cas9 can be designed to precisely cleave and disrupt genes conferring resistance to conventional antibiotics, such as beta-lactamases or vancomycin resistance genes, potentially resensitizing bacteria to existing treatments [13] [11].
Quorum Sensing Pathways: Bacterial cell-to-cell communication systems (quorum sensing) regulate biofilm formation and virulence factor production. Targeting quorum sensing genes (e.g., lasI, rhlI in P. aeruginosa) can disrupt biofilm development without directly killing bacteria, potentially reducing selective pressure for resistance [13].
Biofilm-Specific Regulatory Genes: Genes encoding master regulators of biofilm formation, such as those controlling production of extracellular polymeric substances (EPS), represent valuable targets for preventing biofilm maturation and stability [11].
The following experimental workflow outlines a standardized protocol for developing and testing CRISPR-Cas9 systems against bacterial biofilms:
Protocol: gRNA Design and Validation for Anti-Biofilm Applications
Objective: Design and validate guide RNAs targeting antibiotic resistance genes in ESKAPE pathogens.
Materials:
- Bacterial genomic DNA or synthetic target sequences
- gRNA design software (e.g., CRISPRscan, Benchling)
- In vitro transcription kit for gRNA production
- Purified Cas9 nuclease
- Target DNA plasmids containing resistance genes
Procedure:
- Target Selection: Identify 20-nucleotide sequences adjacent to PAM sites (5'-NGG-3') within your target gene (e.g., mecA in S. aureus or blaNDM-1 in K. pneumoniae).
- Specificity Screening: Use BLAST analysis to verify target uniqueness and minimize off-target effects.
- gRNA Synthesis: Transcribe gRNAs using T7 RNA polymerase-based in vitro transcription.
- In Vitro Cleavage Assay:
- Set up 20 μL reaction containing: 100 ng target plasmid, 50 nM Cas9 nuclease, 50 nM gRNA, and reaction buffer.
- Incubate at 37°C for 1 hour.
- Analyze cleavage efficiency by agarose gel electrophoresis.
- Validation: Successful cleavage is confirmed by appearance of expected DNA fragment sizes.
Troubleshooting Note: If cleavage efficiency is low, redesign gRNAs targeting different regions of the same gene, as chromatin accessibility and local DNA structure can impact efficacy.
Protocol: Nanoparticle-Mediated Delivery of CRISPR-Cas9 to Biofilms
Objective: Formulate CRISPR-Cas9 components in nanoparticle carriers and evaluate biofilm penetration and editing efficiency.
Materials:
- Cationic liposomes or gold nanoparticles
- Purified Cas9 protein or Cas9 expression plasmid
- Validated gRNA
- Biofilm-forming bacterial strains
- Confocal microscopy supplies for visualization
Procedure:
- Nanoparticle Formulation:
- For liposomal preparations: Mix cationic lipids with CRISPR components at optimal N:P ratio (typically 5:1 to 10:1).
- For gold nanoparticles: Conjugate thiol-modified gRNA to AuNPs, then complex with Cas9 protein.
- Characterize nanoparticle size (target: 50-200 nm) and zeta potential using dynamic light scattering.
Biofilm Treatment:
- Grow 24-48 hour mature biofilms in flow cells or 96-well plates.
- Apply nanoparticle formulations at predetermined concentrations.
- Include appropriate controls (untreated, empty nanoparticles, free CRISPR).
Penetration Assessment:
- Label nanoparticles with fluorescent dyes (e.g., Cy5 for gRNA, FITC for Cas9).
- Monitor biofilm penetration using confocal laser scanning microscopy at 2, 4, 6, and 24 hours post-treatment.
- Generate Z-stack images to visualize depth of penetration.
Efficacy Evaluation:
- Quantify biofilm biomass using crystal violet staining.
- Assess bacterial viability via colony-forming unit counts.
- Analyze target gene modification efficiency through sequencing.
Technical Note: Optimization of nanoparticle surface properties (e.g., PEGylation, targeting ligand conjugation) may enhance biofilm penetration and cellular uptake.
Concluding Remarks and Future Perspectives
The integration of CRISPR-Cas9 technology with advanced nanoparticle delivery systems represents a paradigm shift in our approach to combating biofilm-associated infections. By leveraging the fundamental mechanisms of bacterial immunity, researchers can now develop highly specific antimicrobial strategies that target the genetic underpinnings of antibiotic resistance and biofilm formation [13] [8] [11].
While significant progress has been made in demonstrating the efficacy of these systems in vitro, translation to clinical applications requires addressing several challenges. These include optimizing delivery efficiency to biofilm-embedded bacteria, minimizing potential off-target effects, and ensuring long-term safety [15]. Future research directions should focus on developing more sophisticated nanoparticle platforms that can navigate the complex biofilm microenvironment, creating Cas variants with enhanced specificity, and exploring combinatorial approaches that integrate CRISPR with conventional antibiotics for synergistic effects [13].
The protocols and application notes presented herein provide a foundation for researchers exploring CRISPR-Cas9 based approaches within the broader context of nanoparticle-mediated delivery for biofilm eradication. As this field continues to evolve, these fundamental principles will serve as a roadmap for developing next-generation antimicrobial therapies that address the pressing global challenge of antibiotic resistance.
The CRISPR-Cas9 system has emerged as a revolutionary tool for precision genome modification, offering targeted disruption of antibiotic resistance genes, quorum sensing pathways, and biofilm-regulating factors within bacterial populations [13]. However, the clinical application of CRISPR-based antibacterials faces significant challenges, particularly in achieving efficient delivery and stability within complex bacterial communities such as biofilms [13]. Biofilms, which are structured communities of microorganisms embedded in a self-produced extracellular polymeric substance (EPS), can exhibit up to 1000-fold greater tolerance to antibiotics compared to their planktonic counterparts [13]. This protective matrix limits the penetration of antimicrobial agents, enhances horizontal gene transfer, and enables bacterial survival in hostile environments, making conventional therapies largely ineffective [13].
The core delivery problem encompasses multiple barriers: the negatively charged EPS matrix repels negatively charged genetic material, extracellular nucleases degrade CRISPR components before cellular uptake, and the varied metabolic states of bacterial cells (including persister cells) further reduce editing efficiency [13] [16]. Overcoming these hurdles requires innovative delivery strategies that can protect the CRISPR payload, facilitate penetration through the biofilm architecture, and ensure efficient intracellular delivery to bacterial cells. Nanoparticles present an innovative solution, serving as effective carriers for CRISPR-Cas9 components while exhibiting intrinsic antibacterial properties [13]. These nanocarriers can enhance CRISPR delivery by improving cellular uptake, increasing target specificity, and ensuring controlled release within biofilm environments [13].
Nanoparticle-Mediated Delivery Strategies
Various nanoparticle platforms have been engineered to address the distinct challenges of delivering CRISPR-Cas9 components through biofilm matrices and into bacterial cells. These systems can be broadly categorized based on their composition and properties, as outlined in the table below.
Table 1: Nanoparticle Platforms for CRISPR-Cas9 Delivery Against Biofilms
| Nanoparticle Type | Key Advantages | CRISPR Payload Format | Reported Efficacy | Limitations |
|---|---|---|---|---|
| Lipid-Based Nanoparticles | High biocompatibility, enhanced biofilm penetration [13] | Plasmid DNA, RNP [13] [17] | >90% reduction in P. aeruginosa biofilm biomass [13] | Potential endosomal degradation, variable efficiency across species [17] |
| Gold Nanoparticles | Easy surface functionalization, high delivery efficiency [13] [17] | RNP, DNA [17] | 3.5-fold increase in editing efficiency [13] | Potential toxicity at high concentrations [17] |
| Polymeric Nanoparticles | Controlled release, high biocompatibility, low cytotoxicity [17] [16] | Plasmid DNA, mRNA, RNP [17] [16] | Effective resensitization to antibiotics [16] | Relatively lower delivery efficiency [17] |
| Hybrid Systems | Synergistic effects, multi-functional capabilities [13] | Various formats with antibiotic co-delivery [13] | Superior biofilm disruption [13] | Complex fabrication and optimization requirements [13] |
The selection of appropriate CRISPR payload format is crucial for editing efficiency. The three primary formats include: (1) DNA plasmid encoding both Cas9 and gRNA; (2) mRNA for Cas9 translation with a separate gRNA; and (3) Ribonucleoprotein (RNP) complex of preassembled Cas9 protein and gRNA [17] [16]. RNP delivery offers the advantage of rapid activity with reduced off-target effects and no risk of genomic integration, making it particularly suitable for antimicrobial applications where permanent genetic modification is not required [17].
Experimental Protocols for Nanoparticle-Based CRISPR Delivery
Synthesis of CRISPR-Loaded Lipid Nanoparticles
Principle: Cationic lipids self-assemble with negatively charged CRISPR payloads through electrostatic interactions, forming nanoparticles that protect the cargo and facilitate fusion with bacterial membranes [13] [17].
Materials:
- CRISPR payload: RNP complex or plasmid DNA targeting specific antibiotic resistance genes (e.g., bla, mecA, ndm-1) [13]
- Cationic lipids: DOTAP, DOPE, or commercial transfection lipids
- Sterile PBS buffer (pH 7.4)
- Extrusion apparatus with 100-200 nm membranes
- Dialysis tubing (MWCO 100 kDa)
Procedure:
- Prepare lipid film: Dissolve cationic lipid and helper lipid in chloroform at 75:25 molar ratio. Evaporate solvent under nitrogen stream to form thin lipid film.
- Hydrate film: Hydrate lipid film with sterile PBS to a final lipid concentration of 10 mM. Vortex extensively until multilamellar vesicles form.
- Size reduction: Extrude lipid suspension through polycarbonate membranes (100 nm pore size, 11 cycles) to form unilamellar vesicles.
- CRISPR complexation: Mix CRISPR payload (RNP at 1:2 molar ratio of Cas9:gRNA) with preformed liposomes at nitrogen-to-phosphate (N/P) ratio of 10:1. Incubate for 30 minutes at room temperature.
- Purification: Remove unencapsulated payload by dialysis against PBS for 2 hours or size exclusion chromatography.
- Characterization: Determine particle size (target: 100-150 nm), zeta potential (target: +20 to +30 mV), and encapsulation efficiency using fluorescence-based assays [13].
Quality Control: Verify CRISPR activity using gel retardation assay and in vitro cleavage assay with target DNA plasmid before biofilm studies.
Biofilm Penetration and Gene Editing Assessment
Principle: This protocol evaluates the ability of CRISPR-loaded nanoparticles to penetrate established biofilms and achieve targeted gene editing, measured through reduction in antibiotic resistance and biofilm viability [13].
Materials:
- Biofilm model: Pseudomonas aeruginosa or Escherichia coli biofilm grown in flow cell system or 96-well plates [13] [18]
- Culture media: Tryptic soy broth or LB medium
- CRISPR-nanoparticles: Prepared as in Protocol 3.1, targeting specific resistance genes (e.g., blaNDM-1)
- SYTO 9/propidium iodide live/dead stain
- qPCR equipment and primers for target gene quantification
- Confocal laser scanning microscopy (CLSM) system
Procedure:
- Biofilm establishment: Grow biofilms for 48-72 hours in flow cells or 96-well plates with medium replenishment every 24 hours.
- Nanoparticle treatment: Apply CRISPR-nanoparticles at sub-MIC concentrations of corresponding antibiotic. Include appropriate controls:
- Untreated biofilm
- Empty nanoparticles
- Free CRISPR system
- Incubation: Treat biofilms for 4-24 hours at 37°C with gentle agitation if using static models.
- Penetration assessment: For CLSM visualization, label nanoparticles with fluorescent dye (e.g., Cy5) prior to application. Image biofilm z-stacks at 1-2 hour intervals to track penetration kinetics.
- Efficacy assessment:
- Viability assay: Treat with SYTO 9/PI and quantify live/dead ratio using image analysis software.
- Gene editing efficiency: Extract genomic DNA from biofilm cells and perform qPCR to quantify reduction in target resistance gene abundance.
- Phenotypic validation: Measure changes in antibiotic susceptibility by exposing treated biofilms to previously ineffective antibiotics and assessing viability.
- Biomass quantification: Measure total biofilm biomass using crystal violet staining or direct dry weight measurement [13].
Expected Outcomes: Effective formulations should demonstrate >70% reduction in target gene expression, >50% reduction in viable biofilm cells, and significant resensitization to antibiotics (4-256 fold reduction in MIC values) [13] [18].
Quantitative Analysis of Delivery Efficacy
The efficacy of nanoparticle-mediated CRISPR delivery against bacterial biofilms has been quantitatively assessed across multiple studies, with results varying based on the target organism, nanoparticle system, and specific genes being edited.
Table 2: Quantitative Efficacy of CRISPR-Nanoparticle Systems Against Biofilms
| Target Bacteria | Nanoparticle Platform | Target Gene | Editing Efficiency | Biofilm Reduction | Resensitization Effect |
|---|---|---|---|---|---|
| P. aeruginosa | Liposomal RNP [13] | Quorum sensing genes | Not specified | >90% biomass reduction [13] | Significant improvement in antibiotic susceptibility [13] |
| E. coli | Conjugative plasmid delivery [18] | β-lactamase (bla) | 4.7%-100% [18] | Not specified | Restoration of β-lactam antibiotic efficacy [18] |
| Mixed species | Gold nanoparticle-RNP [13] | Antibiotic resistance genes | 3.5× higher vs. non-carrier [13] | Significant disruption | Synergistic effect with co-delivered antibiotics [13] |
| S. aureus | Polymeric nanoparticles [16] | mecA | Not specified | Not specified | Re-sensitization to methicillin [16] |
The variation in editing efficiency (4.7% to 100%) reflects differences in delivery efficiency, target accessibility, and bacterial uptake mechanisms [18]. Higher efficiency is typically observed when targeting essential resistance genes on plasmids rather than chromosomal genes, and when using RNP formulations with efficient nanoparticle packaging [13] [18].
Visualization of Workflows and Mechanisms
CRISPR-Nanoparticle-Mediated Biofilm Disruption
Mechanism of CRISPR-Cas9 Gene Editing
The Scientist's Toolkit: Essential Research Reagents
Table 3: Essential Reagents for CRISPR-Nanoparticle Biofilm Research
| Reagent/Category | Specific Examples | Function/Application | Key Considerations |
|---|---|---|---|
| CRISPR Components | SpCas9 protein, sgRNA targeting resistance genes (e.g., blaNDM-1, mecA) [13] [18] | Precision targeting of antibiotic resistance genes | Design sgRNAs with minimal off-target potential; validate efficiency |
| Nanoparticle Materials | Cationic lipids (DOTAP, DC-Chol), PLGA, Gold nanoparticles [13] [17] [16] | CRISPR payload protection and delivery | Optimize N/P ratio for nucleic acid binding; control particle size <200nm |
| Biofilm Assay Reagents | SYTO 9/propidium iodide, crystal violet, Calgary biofilm device [13] | Biofilm growth assessment and viability testing | Standardize growth conditions; include appropriate controls |
| Analytical Tools | Dynamic light scattering, confocal microscopy, qPCR systems [13] | Nanoparticle characterization and efficacy assessment | Monitor nanoparticle stability in biological fluids |
| Bacterial Strains | Reference strains with known resistance mechanisms (e.g., PAO1, MG1655) [13] [18] | Model systems for testing | Include both planktonic and biofilm growth modes |
Nanoparticle-mediated delivery of CRISPR-Cas9 represents a promising strategy to overcome the fundamental challenge of delivering genome-editing machinery through protective biofilm matrices and into bacterial cells. The integration of nanotechnology with gene editing creates synergistic effects, where nanoparticles not only facilitate efficient CRISPR delivery but can also provide intrinsic antibacterial activity and enable co-delivery of conventional antibiotics [13]. Current research demonstrates that this approach can achieve substantial reduction in biofilm biomass (over 90% in optimized systems) and significantly restore antibiotic efficacy against previously resistant strains [13] [18].
Future developments in this field will likely focus on creating smarter nanoparticle systems with enhanced biofilm-targeting capabilities through surface functionalization with biofilm-penetrating peptides or antibodies specific to bacterial surface antigens [16]. Additionally, the development of stimuli-responsive nanoparticles that release their CRISPR payload in response to unique biofilm microenvironment cues (such as acidic pH, specific enzymes, or low oxygen tension) could further improve specificity and reduce off-target effects [13]. As these delivery systems evolve, nanoparticle-based CRISPR therapies hold immense potential to transform the treatment of persistent biofilm-associated infections and address the growing crisis of antibiotic resistance [13] [18].
Nanoparticles as Intrinsic Anti-biofilm Agents and Advanced Delivery Vectors
Within the strategic framework of developing CRISPR-Cas9 delivery systems for biofilm eradication, nanoparticles (NPs) serve a dual therapeutic function: as intrinsic anti-biofilm agents and as advanced delivery vectors for genetic machinery. Biofilms, which are structured communities of microorganisms encapsulated in an extracellular polymeric substance (EPS), can exhibit up to 1000-fold greater tolerance to antibiotics compared to their planktonic counterparts [13]. This formidable resistance arises from the EPS matrix acting as a physical barrier, reduced metabolic activity of embedded cells, and enhanced horizontal gene transfer [13] [9]. Nanoparticles counter these mechanisms through their unique physicochemical properties, including their small size, high surface-area-to-volume ratio, and the ability to be engineered with specific surface functionalities [3] [19]. When leveraged to deliver CRISPR-Cas9 components, nanoparticles facilitate precision targeting of bacterial resistance genes, offering a synergistic and next-generation approach to combating biofilm-associated infections [13] [11].
Table 1: Major Classes of Nanoparticles Used as Intrinsic Anti-biofilm Agents
| Nanoparticle Class | Key Materials | Primary Anti-biofilm Mechanisms | Notable Efficacy Findings |
|---|---|---|---|
| Metal & Metal Oxide NPs | Silver (Ag), Gold (Au), Zinc Oxide | ROS generation, EPS degradation, membrane disruption [3] [20] | Green-synthesized AgNPs inhibited biofilm formation in enterococcal pathogens by >60% at 18 µg/mL [21] |
| Polymeric NPs | Chitosan, PLGA, Polyester | Electrostatic interaction with EPS, controlled release of antimicrobials [19] [22] | Chitosan NPs used to enhance drug absorption and for targeted delivery [22] |
| Lipid-Based NPs | Liposomes, Solid Lipid Nanoparticles (SLNs) | Fusion with bacterial membranes, efficient encapsulation of cargo [19] | Liposomal formulations reported to reduce P. aeruginosa biofilm biomass by over 90% in vitro [13] |
| Hybrid & Composite NPs | Metal-Polymer conjugates, Lipid-Polymer hybrids | Multi-mechanistic action combining physical disruption and enhanced drug delivery [3] | CRISPR-gold nanoparticle hybrids showed 3.5x increase in gene-editing efficiency [13] |
Anti-biofilm Mechanisms of Intrinsic Nanoparticle Activity
Reactive Oxygen Species (ROS) Generation and Physical Disruption
Metal nanoparticles, particularly silver nanoparticles (AgNPs), exert significant intrinsic antibiofilm activity primarily through the generation of reactive oxygen species (ROS) [3] [20]. The subsequent oxidative stress damages bacterial cell membranes, proteins, and DNA, leading to cell death [20] [21]. AgNPs also physically interact with the biofilm matrix, disrupting the intermolecular forces that maintain the integrity of the extracellular polymeric substance (EPS) and thereby enhancing permeability [21]. The release of silver ions (Ag+) at the nanoparticle-bacteria interface further augments this antibacterial effect [20]. Studies have demonstrated that the surface chemistry and size of NPs are critical for this activity; for instance, ginger-based AgNPs with an average size of 20.2 nm showed superior antibiofilm effects compared to larger, chemically synthesized AgNPs [21].
Quorum Sensing Inhibition and EPS Degradation
Beyond direct killing, nanoparticles can disrupt the social behavior of bacterial communities by inhibiting quorum sensing (QS) [3]. QS is a cell-density-dependent communication system that regulates biofilm formation, virulence factor production, and antibiotic resistance. By interfering with QS signaling molecules, nanoparticles can prevent biofilm maturation and render bacterial cells more vulnerable to antimicrobial agents [3] [21]. Furthermore, certain engineered nanoparticles can actively degrade essential components of the biofilm matrix, such as polysaccharides and extracellular DNA (eDNA), compromising the structural scaffold that protects the embedded cells [3].
Nanoparticles as Delivery Vectors for CRISPR-Cas9
The efficacy of the CRISPR-Cas9 system in combating biofilm-associated antibiotic resistance hinges on its precise delivery into bacterial cells [13] [11]. Nanoparticles are ideally suited to address the critical challenges of protecting the CRISPR machinery from degradation and facilitating its uptake into target bacteria. Lipid-based nanoparticles, for example, can encapsulate the Cas9 nuclease and guide RNA (gRNA) complexes, shielding them from enzymatic degradation in the extracellular environment [13]. Upon reaching the biofilm, these nanocarriers fuse with bacterial membranes, enabling the intracellular release of the CRISPR components. This delivery strategy has demonstrated remarkable success, with liposomal Cas9 formulations reducing Pseudomonas aeruginosa biofilm biomass by over 90% in vitro [13].
Similarly, gold nanoparticles (AuNPs) can be functionalized with CRISPR-Cas9 components through surface chemistry modifications, creating stable complexes that efficiently enter bacterial cells [13]. The "CRISPR-gold" platform has been shown to enhance gene-editing efficiency by 3.5-fold compared to non-carrier delivery systems [13]. This synergy between nanoparticles and CRISPR-Cas9 creates a powerful combinatorial attack: nanoparticles disrupt the biofilm's physical integrity and simultaneously deliver genetic tools to precisely target and disrupt antibiotic resistance genes, quorum-sensing pathways, or biofilm-regulating factors [13] [11] [23].
Experimental Protocols for Nanoparticle Synthesis and Evaluation
Protocol 1: Green Synthesis and Characterization of Silver Nanoparticles (AgNPs)
Principle: This protocol utilizes plant-derived phytochemicals as reducing and capping agents to synthesize biocompatible AgNPs with potent intrinsic antibiofilm activity [21].
Materials:
- Silver nitrate (AgNO₃) solution (2 mM)
- Plant extract (e.g., Cinnamon or Ginger)
- Centrifugal filter devices (e.g., 10 kDa MWCO)
- UV-Vis Spectrophotometer
- Transmission Electron Microscope (TEM)
- Dynamic Light Scattering (DLS) / Zeta Potential Analyzer
- FT-IR Spectrometer
Procedure:
- Extract Preparation: Finely powder 10 g of dried plant material (e.g., ginger rhizome). Boil in 100 mL deionized water for 10 minutes and filter through a 0.2 µm membrane.
- Reduction Reaction: Add 0.0197 g of the extract to 20 mL of boiling 2 mM AgNO₃ solution under constant stirring.
- Synthesis Monitoring: Maintain the reaction at 80°C for 10-60 minutes. Observe the color change (to yellowish-brown for ginger, dark reddish-brown for cinnamon) indicating NP formation [21].
- Purification: Centrifuge the cooled NP suspension at 20,000 × g for 30 minutes. Wash the pellet with deionized water and re-suspend via sonication.
- Characterization:
- UV-Vis Spectroscopy: Confirm synthesis by detecting the Surface Plasmon Resonance peak between 400-450 nm [21].
- DLS & Zeta Potential: Measure hydrodynamic diameter, polydispersity index (PDI), and surface charge.
- TEM: Determine the size, morphology, and size distribution of the AgNPs.
- FT-IR: Identify the functional groups from the plant extract responsible for capping and stabilizing the NPs.
Protocol 2: Assessing Anti-biofilm Efficacy In Vitro
Principle: This protocol quantifies the ability of nanoparticles to prevent biofilm formation and disrupt pre-formed biofilms using microtiter plate assays and molecular techniques [20] [21].
Materials:
- 96-well flat-bottom polystyrene microtiter plates
- Test bacterial strains (e.g., P. aeruginosa, S. aureus)
- Tryptic Soy Broth (TSB) or other appropriate growth media
- Crystal Violet (CV) stain (0.1% w/v)
- Acetic acid (33% v/v)
- Microplate reader
- Real-time PCR system
Procedure: A. Biofilm Formation Inhibition Assay:
- Prepare serial dilutions of the nanoparticles in growth media to achieve sub-inhibitory concentrations (e.g., 1/2x, 1/4x, 1/8x MIC).
- Inoculate wells with 100 µL of bacterial suspension (∼10⁶ CFU/mL) and 100 µL of NP solution. Include media-only (sterility control) and bacteria-only (growth control) wells.
- Incubate statically for 24-48 hours at 37°C.
- Carefully remove planktonic cells by washing wells twice with phosphate-buffered saline (PBS).
- Fix the adherent biofilm with 150 µL of 99% methanol for 15 minutes. Air dry.
- Stain with 150 µL of 0.1% CV for 20 minutes. Wash thoroughly to remove unbound dye.
- Elute the bound CV with 150 µL of 33% acetic acid.
- Measure the absorbance of the eluent at 570-595 nm. Calculate % biofilm inhibition relative to the untreated control [21].
B. Disruption of Pre-formed Biofilms:
- Allow biofilms to form in microtiter plates for 24 hours as described above.
- Gently wash the mature biofilms with PBS and add fresh media containing NPs.
- Incubate for an additional 24 hours.
- Quantify the remaining biofilm using the CV staining method described above.
C. Molecular Analysis of Biofilm Genes:
- Extract total RNA from NP-treated and untreated biofilms.
- Synthesize cDNA and perform real-time PCR using primers for key biofilm-related genes (e.g., algD, pelA, pslD in P. aeruginosa; icaA in S. aureus) [20].
- Normalize gene expression levels to a housekeeping gene and calculate fold-changes using the 2^–ΔΔCt method.
Table 2: Quantitative Anti-biofilm Efficacy of Selected Nanoparticles
| Nanoparticle Type | Target Bacteria | Key Metric | Result | Experimental Context |
|---|---|---|---|---|
| Ginger AgNPs [21] | Biofilm-forming Enterococci | Reduction in pre-formed biofilm | 60.86% reduction (to 39.14% of control) | Concentration: 18 µg/mL |
| Liposomal Cas9 [13] | Pseudomonas aeruginosa | Reduction in biofilm biomass | >90% reduction | In vitro |
| CRISPR-Gold Hybrid [13] | Model Bacteria | Gene-editing efficiency | 3.5-fold increase | Compared to non-carrier delivery |
| Cinnamon AgNPs [21] | Biofilm-forming Enterococci | Minimum Inhibitory Concentration (MIC) | Mean MIC: 725.7 µg/mL | Broth microdilution |
The Scientist's Toolkit: Essential Research Reagents and Materials
Table 3: Key Research Reagent Solutions for Nanoparticle Anti-biofilm Studies
| Reagent / Material | Function / Application | Example Specification / Notes |
|---|---|---|
| Silver Nitrate (AgNO₃) | Precursor salt for the synthesis of Silver Nanoparticles (AgNPs) | Typically used as a 1-2 mM aqueous solution for green synthesis [21] |
| C-Phycocyanin (C-Pc) | Stabilizing and capping agent for AgNPs; improves biocompatibility | Functional groups (amino, carboxyl) provide binding sites for silver atoms [20] |
| Polyethyleneimine (PEI) | Cationic polymer for forming polyplexes with nucleic acids (e.g., gRNA) | Aids in cellular uptake and endosomal escape; can be used to functionalize nanoparticles [14] |
| Citrate Reduction Reagents | Classical chemical method for synthesizing Gold Nanoparticles (AuNPs) | Trisodium citrate acts as both reducing and stabilizing agent [13] |
| CRISPR-Cas9 System | Core gene-editing machinery | Requires both Cas9 protein and guide RNA (gRNA) targeting specific bacterial resistance genes [13] [11] |
| Crystal Violet (0.1%) | Dye for staining and quantifying bacterial biofilm biomass in microtiter plates [21] | Bound dye is solubilized with acetic acid for absorbance measurement |
| Dynamic Light Scattering (DLS) Instrument | Characterizing nanoparticle hydrodynamic size, distribution (PDI), and zeta potential | Critical for quality control of synthesized NPs [20] [21] |
Engineering the Delivery Platform: Nanoparticle Designs and CRISPR Cargo Strategies
The escalating crisis of antimicrobial resistance, driven significantly by biofilm-associated infections, necessitates the development of next-generation therapeutic strategies. Biofilms, structured communities of microorganisms embedded in an extracellular polymeric substance (EPS), exhibit up to 1000-fold greater tolerance to antibiotics compared to their planktonic counterparts [13]. The CRISPR-Cas9 gene-editing system has emerged as a revolutionary tool for precision targeting of bacterial vulnerabilities, capable of disrupting antibiotic resistance genes, quorum sensing pathways, and biofilm-regulating factors [13] [8]. However, the clinical translation of CRISPR-Cas9 is critically dependent on safe and efficient delivery systems that can navigate the complex biofilm matrix and facilitate intracellular delivery.
Nanocarriers present an innovative solution to this challenge, serving as versatile vectors for CRISPR-Cas9 components while often exhibiting intrinsic biofilm-disrupting properties [13] [24]. These nanoscale systems enhance CRISPR delivery by protecting genetic payloads from degradation, improving cellular uptake, increasing target specificity, and ensuring controlled release within the biofilm microenvironment [13] [25]. The synergy between CRISPR-Cas9 and nanotechnology has demonstrated remarkable efficacy; for instance, liposomal CRISPR-Cas9 formulations have been shown to reduce Pseudomonas aeruginosa biofilm biomass by over 90% in vitro, while gold nanoparticle carriers can enhance gene-editing efficiency up to 3.5-fold compared to non-carrier systems [13] [8]. This application note delineates the primary classes of nanocarriers—lipid-based, polymeric, metallic, and hybrid systems—detailing their compositions, mechanisms, and experimental protocols for application in CRISPR-Cas9 delivery against resilient biofilms.
Classes of Nanocarriers: Composition and Characteristics
Table 1: Comparative Analysis of Nanocarrier Classes for CRISPR-Cas9 Delivery
| Nanocarrier Class | Key Components | CRISPR Format | Encapsulation Efficiency | Key Advantages | Primary Limitations |
|---|---|---|---|---|---|
| Lipid-Based NPs | Ionizable lipids, phospholipids, cholesterol, PEG-lipids [26] | mRNA/gRNA, RNP, pDNA [26] | High for nucleic acids (>85%) [26] | Low immunogenicity, clinical validation, endosomal escape [24] [26] | Cytotoxicity at high doses, complex formulation for RNP [24] [26] |
| Polymeric NPs | PLGA, chitosan, polyplexes, poly ε-caprolactone (PCL) [24] [25] | pDNA, RNP, mRNA/gRNA [25] | Moderate to High (varies with polymer) [25] | Controlled release, high stability, functionalizable surface [24] [25] | Potential cytotoxicity, batch-to-batch variability [24] |
| Metallic NPs | Gold, Silver [13] [27] | RNP, pDNA [13] [24] | Varies with surface functionalization [24] | Tunable optoelectronic properties, intrinsic antibacterial activity, surface plasmon resonance [13] [27] | Toxicity concerns, potential for oxidative stress [27] |
| Hybrid Systems | Combinations of above (e.g., lipid-polymer, metal-polymer) [13] | All formats [13] | Can be optimized for specific cargo | Synergistic properties, enhanced targeting, multi-functionality [13] | Increased complexity in manufacturing and characterization [13] |
Lipid-Based Nanoparticles (LNPs)
Lipid Nanoparticles represent the most clinically advanced non-viral delivery platform for nucleic acids, gaining prominence during the COVID-19 mRNA vaccine development [26]. Their core structure comprises four key components: ionizable lipids which are cationic at low pH and facilitate endosomal escape; phospholipids which support bilayer formation; cholesterol that enhances stability; and PEG-lipids which reduce protein adsorption and extend circulation half-life [26]. The ionizable lipids are particularly crucial for CRISPR delivery, as their positive charge enables complexation with negatively charged nucleic acids or proteins, and their phase transition in the acidic endosomal environment promotes disruption of the endosomal membrane and payload release into the cytoplasm [26].
LNPs can encapsulate various CRISPR-Cas9 formats, including plasmid DNA (pDNA) encoding Cas9 and guide RNA, Cas9 mRNA combined with guide RNA, and preassembled Cas9 ribonucleoprotein (RNP) complexes [26]. The RNP format offers the most rapid onset of gene editing as it bypasses transcription and translation steps, though its encapsulation presents technical challenges [24] [26]. Recent advances include Selective Organ Targeting (SORT) LNPs, where the addition of supplemental molecules enables tissue-specific delivery to lungs, spleen, or other organs—a critical capability for targeting biofilms in specific anatomical locations [26].
Polymeric Nanoparticles
Polymeric nanoparticles offer exceptional versatility for CRISPR-Cas9 delivery through tunable chemical properties and controlled release kinetics. These systems can be fabricated from natural polymers like chitosan, which exhibits mucoadhesive properties beneficial for penetrating biofilm matrices, or synthetic polymers such as PLGA (poly(lactic-co-glycolic acid)) and PCL (poly ε-caprolactone) that provide predictable degradation profiles [24] [25]. The encapsulation process typically involves self-assembly, nano-precipitation, or double-emulsion methods, with the choice depending on the CRISPR payload format and the desired release kinetics [25].
Polymeric systems excel in protecting CRISPR components from degradation by nucleases and the harsh biofilm microenvironment [25]. Functionalization with targeting ligands (e.g., peptides, antibodies) can further enhance their specificity for bacterial surfaces or biofilm components. Studies have demonstrated that antibiotic-loaded polymeric nanoparticles can overcome conventional antibiotic resistance mechanisms by enhancing intracellular delivery and bypassing efflux pumps [25], a principle that extends to CRISPR payload delivery. The modular nature of polymeric nanoparticles facilitates co-delivery of CRISPR components with antibiotics or biofilm-disrupting agents, creating synergistic anti-biofilm strategies [13] [25].
Metallic Nanoparticles
Metallic nanoparticles, particularly gold and silver, offer unique advantages for CRISPR delivery and intrinsic antibacterial activity. Gold nanoparticles (AuNPs) can be precisely engineered in size and shape, and their surface functionalization with thiol chemistry allows stable conjugation with CRISPR components [13] [24]. Studies have demonstrated that CRISPR-gold nanoparticle hybrids can enhance editing efficiency up to 3.5-fold compared to non-carrier systems while promoting synergistic action with antibiotics [13]. The high surface-area-to-volume ratio enables high payload capacity, and their tunable optoelectronic properties allow for potential light-controlled activation or thermal disruption of biofilms.
Silver nanoparticles (AgNPs) exhibit potent intrinsic antimicrobial activity through multiple mechanisms, including membrane disruption, reactive oxygen species generation, and interference with microbial DNA and proteins [27]. When combined with CRISPR systems, this intrinsic activity can provide a dual-action therapeutic approach. However, potential cytotoxicity to mammalian cells remains a concern for metallic nanoparticles, necessitating careful dosage control and surface modification to improve biocompatibility [27].
Hybrid Nanocarriers
Hybrid nanocarriers integrate multiple material classes to overcome individual limitations and create synergistic functionalities. Examples include lipid-polymer hybrids that combine the biocompatibility of lipids with the structural stability of polymers, metal-organic frameworks with high porosity for payload loading, and cell membrane-coated nanoparticles that leverage natural targeting mechanisms [13]. These systems can be engineered to sequentially release multiple payloads—for instance, initial release of biofilm-disrupting agents to penetrate the EPS matrix, followed by targeted delivery of CRISPR components to the exposed bacterial cells [13].
Hybrid platforms enable sophisticated targeting strategies through surface functionalization with antibodies, lectins, or aptamers that recognize specific bacterial surface markers or biofilm components [13]. They can also incorporate environment-responsive elements (e.g., pH-sensitive linkers, enzyme-cleavable coatings) that trigger payload release specifically in the biofilm microenvironment, characterized by acidic pH and elevated enzyme concentrations [13] [25]. The co-delivery capacity of hybrid systems is particularly valuable for biofilm eradication, allowing simultaneous targeting of multiple resistance mechanisms or combining genetic and conventional antimicrobial approaches [13].
Experimental Protocols for Nanocarrier Evaluation
Protocol 1: Formulation and Characterization of CRISPR-Loaded Lipid Nanoparticles
Materials:
- Ionizable lipid (e.g., DLin-MC3-DMA)
- Helper lipids: DSPC, Cholesterol
- PEG-lipid (e.g., DMG-PEG2000)
- CRISPR payload (mRNA, pDNA, or RNP)
- Acidic buffer (e.g., citrate buffer, pH 4.0)
- Ethanol and PBS solutions
- Microfluidic device or tubing setup
Methodology:
- Lipid Solution Preparation: Dissolve ionizable lipid, DSPC, cholesterol, and PEG-lipid in ethanol at molar ratio 50:10:38.5:1.5 to achieve total lipid concentration of 10 mM [26].
- Aqueous Phase Preparation: Dilute CRISPR payload in citrate buffer (pH 4.0) at concentration of 0.2 mg/mL for mRNA or 0.5 mg/mL for RNP complexes [26].
- Nanoparticle Formation: Utilize microfluidic device with staggered herringbone mixer geometry. Simultaneously pump lipid solution and aqueous phase through device at 1:3 volumetric flow rate ratio (total flow rate 12 mL/min) to facilitate rapid mixing [26].
- Buffer Exchange and Purification: Dialyze resulting LNP formulation against PBS (pH 7.4) for 4 hours at 4°C using 100 kDa MWCO dialysis membrane to remove ethanol and adjust pH. Alternatively, use tangential flow filtration for larger batches.
- Characterization:
- Size and Zeta Potential: Determine hydrodynamic diameter and polydispersity index via dynamic light scattering. Measure zeta potential using electrophoretic light scattering. Optimal diameter range: 80-120 nm for biofilm penetration [26].
- Encapsulation Efficiency: Quantify using RiboGreen assay for RNA-based payloads or SYBR Gold for DNA. Add assay directly to formulation versus detergent-disrupted formulation to calculate percentage encapsulated [26].
- Morphology: Confirm spherical morphology and core-shell structure using cryo-transmission electron microscopy.
Protocol 2: Biofilm Penetration and Gene Editing Assessment
Materials:
- Static or flow-cell biofilm culture system
- Confocal laser scanning microscope
- SYTO9 and propidium iodide stains
- PCR reagents for amplification of target locus
- T7 endonuclease I or Surveyor assay kit
- Next-generation sequencing platform
Methodology:
- Biofilm Establishment:
- Grow 48-hour mature biofilm of target pathogen (e.g., P. aeruginosa PAO1) in flow-cell system or 96-well plate format [13].
- For in vitro testing, standardize biofilm biomass via crystal violet staining before experimental treatments.
Nanocarrier Treatment:
- Apply fluorescently labeled nanocarriers (e.g., DyLight 650) at sub-inhibitory concentrations to prevent immediate biofilm detachment.
- Incubate for predetermined intervals (1, 2, 4, 8, 24 hours) under conditions matching original biofilm growth.
Penetration Analysis:
- Stain biofilm with SYTO9 (10 µM) for 15 minutes to visualize live cells [13].
- Using confocal microscopy, acquire z-stack images at 1 µm intervals through entire biofilm depth.
- Quantify nanocarrier penetration ratio as fluorescence intensity at basal layers versus superficial layers using ImageJ software.
Gene Editing Efficiency Assessment:
- Extract genomic DNA from treated and control biofilms using mechanical disruption and standard extraction kits.
- Amplify target genomic region (e.g., lasI for quorum sensing inhibition) using PCR with barcoded primers.
- Detect insertion/deletion mutations using T7 endonuclease I mismatch cleavage assay or by next-generation sequencing of amplicons.
- Calculate gene editing efficiency as percentage of sequencing reads containing indels at target site [13].
Protocol 3: Anti-Biofilm Efficacy Assessment
Materials:
- Calgary biofilm device or similar platform
- Resazurin reduction assay reagents
- Scanning electron microscopy (SEM) fixation and processing materials
- Quantitative RT-PCR reagents for virulence gene expression
Methodology:
- Biofilm Viability Assessment:
- Treat established biofilms with CRISPR-loaded nanocarriers at optimized concentration and time.
- Include controls: untreated biofilm, empty nanocarrier, free CRISPR, and conventional antibiotics.
- Assess metabolic activity using resazurin reduction assay: incubate with 0.15 mM resazurin for 2 hours, measure fluorescence (λex=560 nm, λem=590 nm) [13].
- Determine biomass reduction via crystal violet staining: fix biofilm with methanol, stain with 0.1% crystal violet, solubilize in acetic acid, measure absorbance at 590 nm.
Structural Analysis:
- Process biofilms for SEM: fix with 2.5% glutaraldehyde, dehydrate through ethanol series, critical point dry, sputter-coat with gold/palladium [13].
- Image using SEM at 5-15 kV to visualize structural integrity and EPS matrix disruption.
Virulence Gene Expression:
- Extract RNA from treated and control biofilms using RNA-protective reagents and mechanical disruption.
- Perform cDNA synthesis and quantitative PCR for key virulence genes (e.g., lasI, rhlI in P. aeruginosa).
- Normalize expression to housekeeping gene (e.g., rpoD) and calculate fold-change using 2^−ΔΔCt method [13].
The Scientist's Toolkit: Essential Research Reagents
Table 2: Key Research Reagent Solutions for Nanocarrier Development
| Reagent Category | Specific Examples | Research Function | Supplier Examples |
|---|---|---|---|
| CRISPR Components | Cas9 mRNA, sgRNA, RNP complexes [26] | Genome editing payload | GenScript, Integrated DNA Technologies |
| Lipid Formulations | Ionizable lipids (DLin-MC3-DMA), DSPC, Cholesterol, DMG-PEG2000 [26] | LNP structure and function | Avanti Polar Lipids, Sigma-Aldrich |
| Polymeric Materials | PLGA, PCL, Chitosan, PEI [24] [25] | Polymer nanoparticle synthesis | Sigma-Aldrich, Lactel Absorbable Polymers |
| Characterization Kits | RiboGreen Assay, DYNAMIC Light Scattering Standards | Encapsulation efficiency and size analysis | Thermo Fisher Scientific, Malvern Panalytical |
| Biofilm Assays | Calgary Biofilm Device, Resazurin, Crystal Violet | Anti-biofilm efficacy assessment | MBEC Biofilm Products, Sigma-Aldrich |
Workflow and Mechanisms of Action
Nanocarrier Mechanisms for Biofilm Eradication
The diagram illustrates the integrated workflow for utilizing nanocarriers to deliver CRISPR-Cas9 components against bacterial biofilms. The process initiates with the selection of appropriate nanocarrier type (lipid-based, polymeric, metallic, or hybrid systems) and CRISPR format (plasmid DNA, mRNA/gRNA, or RNP complexes). These nanocarriers employ multiple mechanisms including enhanced penetration through the biofilm matrix, specific targeting of bacterial cells, controlled release of payload in response to biofilm microenvironment cues, and precise gene editing of bacterial virulence or resistance determinants. The convergence of these mechanisms ultimately leads to the primary therapeutic outcome of biofilm eradication and restoration of antibiotic susceptibility.
The integration of CRISPR-Cas9 technology with advanced nanocarrier systems represents a paradigm shift in the approach to combat biofilm-mediated antimicrobial resistance. Each class of nanocarrier—lipid-based, polymeric, metallic, and hybrid systems—offers distinct advantages and can be selected based on the specific requirements of the target biofilm and CRISPR payload format. Lipid nanoparticles provide clinical relevance and efficient nucleic acid delivery, polymeric systems offer controlled release and functionalization versatility, metallic nanoparticles contribute unique physicochemical and intrinsic antibacterial properties, while hybrid systems create multifunctional platforms with synergistic capabilities. The experimental protocols outlined herein provide a standardized framework for developing and evaluating these nanocarrier systems, with a focus on quantitative assessment of biofilm penetration, gene editing efficiency, and therapeutic outcomes. As this field advances, the convergence of nanocarrier technology with CRISPR-based antimicrobials holds exceptional promise for addressing the global challenge of treatment-resistant biofilm infections through precision targeting of the genetic mechanisms underlying bacterial persistence and resistance.
The therapeutic application of the CRISPR-Cas9 system for precision eradication of bacterial biofilms hinges on the efficient delivery of gene-editing components into target cells. The CRISPR-Cas9 machinery can be delivered in three primary formats: plasmid DNA (pDNA), messenger RNA (mRNA), or as a preassembled ribonucleoprotein (RNP) complex [28]. The selection of cargo format significantly impacts critical parameters including editing efficiency, kinetics, specificity, and therapeutic safety profile. For biofilm research, where overcoming physical and biological barriers is paramount, nanoparticle formulations are engineered to protect these cargoes and facilitate their delivery to the resilient bacterial communities embedded in extracellular polymeric substances [13]. Each format presents distinct advantages and challenges, making the choice dependent on the specific experimental or therapeutic objectives, target cell type, and delivery modality.
Comparative Analysis of CRISPR Cargo Formats
The three primary cargo formats undergo different intracellular processing pathways before forming the active Cas9-gRNA complex that performs gene editing. Plasmid DNA must first enter the nucleus to be transcribed into mRNA, which is then exported to the cytoplasm for translation into Cas9 protein. The mRNA format bypasses the transcription step, directly undergoing translation in the cytoplasm. The RNP format is functionally immediate, as the precomplexed Cas9 protein and gRNA can directly enter the nucleus and perform editing [29] [30]. These divergent pathways result in significantly different onset kinetics and duration of editing activity.
Table 1: Comparative Characteristics of CRISPR-Cas9 Cargo Formats
| Parameter | Plasmid DNA (pDNA) | mRNA | Ribonucleoprotein (RNP) |
|---|---|---|---|
| Cargo Composition | DNA plasmid encoding Cas9 and gRNA [28] | mRNA encoding Cas9 + separate gRNA [28] | Precomplexed Cas9 protein and gRNA [28] |
| Onset of Activity | Slow (requires transcription and translation) [30] | Moderate (requires translation only) [30] | Immediate (active complex) [30] |
| Duration of Expression | Prolonged (days) [29] | Transient (hours) [30] | Very short (hours) [29] |
| Risk of Genomic Integration | Higher (risk of insertional mutagenesis) [30] | None [30] | None [30] |
| Off-Target Editing Risk | Higher (due to persistent expression) [30] | Moderate [29] | Lower (transient activity) [28] [30] |
| Immunogenicity | Moderate (bacterial backbone elements) [30] | Moderate (can trigger innate immunity) [29] | Lower [28] |
| Manufacturing Complexity | Low (straightforward bacterial production) [30] | High (cell-free, technically complex) [30] | Highest (protein purification) [30] |
| Cargo Size | Large (4-7 kB for Cas9 + gRNA) [29] | Moderate | Large (~160 kDa for Cas9 protein) [29] |
| Example Biofilm Application | - | - | Liposomal Cas9 RNP reduced P. aeruginosa biofilm by >90% in vitro [13] |
Cargo-Specific Experimental Protocols for Biofilm Research
Protocol for Lipid Nanoparticle (LNP) Mediated RNP Delivery Against Biofilms
The delivery of CRISPR-Cas9 as an RNP complex via lipid nanoparticles (LNPs) represents a highly promising strategy for biofilm eradication due to its high editing efficiency and transient activity, which minimizes off-target effects [13] [30]. The following protocol details the formulation of LNPs loaded with RNP and their application to a bacterial biofilm model, adapted from recent studies showing over 90% reduction in Pseudomonas aeruginosa biofilm biomass using this approach [13].
Research Reagent Solutions:
- Cas9 Nuclease: High-purity, recombinant S. pyogenes Cas9 protein.
- sgRNA: Synthetic single-guide RNA targeting specific biofilm-related genes (e.g., quorum-sensing or antibiotic resistance genes).
- Ionizable Lipid: A proprietary or commercially available ionizable lipid (e.g., DLin-MC3-DMA) for nanoparticle self-assembly and endosomal escape.
- Helper Lipids: A mixture of phospholipids (e.g., DOPE), cholesterol, and lipid-PEG to stabilize the LNP structure.
- Biofilm Growth Medium: Suitable rich medium (e.g., LB for E. coli, TSB for S. aureus) for cultivating robust biofilms.
Procedure:
- RNP Complex Formation: Reconstitute the Cas9 protein and sgRNA in nuclease-free buffer. Incubate the Cas9 protein with the sgRNA at a molar ratio of 1:1.2 for 10-15 minutes at room temperature to form the active RNP complex.
- LNP Formulation via Microfluidics: Prepare an organic phase containing the ionizable lipid, helper phospholipid, cholesterol, and lipid-PEG in ethanol. Prepare an aqueous phase containing the preformed RNP complex in a citrate buffer (pH 4.0). Use a microfluidic device to mix the organic and aqueous phases at a controlled flow rate (typically 1:3 ratio) to instantaneously form LNPs encapsulating the RNP.
- LNP Purification and Characterization: Dialyze the raw LNP formulation against a PBS buffer (pH 7.4) to remove residual ethanol. Concentrate the LNPs using centrifugal filter units. Characterize the final formulation for particle size (targeting 80-120 nm), polydispersity index (PDI), zeta potential, and RNP encapsulation efficiency using dynamic light scattering (DLS) and fluorescence-based assays.
- Biofilm Treatment and Analysis: Grow a mature biofilm (for 24-48 hours) of the target bacterium (e.g., P. aeruginosa) in a 96-well plate or on a relevant surface. Treat the established biofilm with the RNP-LNP formulation for a specified period (e.g., 4-24 hours). Assess the outcome through:
- Biomass Quantification: Use crystal violet staining to measure total biofilm biomass.
- Viability Assessment: Perform colony-forming unit (CFU) counts to determine bacterial survival.
- Editing Efficiency: Use PCR and sequencing of the target locus to confirm gene disruption.
Diagram 1: Experimental workflow for LNP-mediated RNP delivery against bacterial biofilms, from formulation to phenotypic outcome.
Protocol for RNP Delivery via Electroporation (Ex Vivo)
For ex vivo applications, such as engineering immune cells or editing bacterial cultures prior to biofilm formation, electroporation is a highly efficient method for RNP delivery [30]. This protocol is adapted from methods used in the first FDA-approved CRISPR-based therapy, Casgevy [30].
Research Reagent Solutions:
- Electroporation Buffer: A low-conductivity buffer suitable for the target cell type.
- Recovery Medium: Pre-warmed, rich culture medium.
Procedure:
- Cell Preparation: Harvest and wash the target cells (e.g., bacterial cells or eukaryotic cells in suspension). Resuspend the cell pellet at a high density (e.g., 10^8 cells/mL) in ice-cold electroporation buffer.
- RNP Complex Formation: Pre-complex Cas9 protein and sgRNA as described in Section 3.1.
- Electroporation: Mix the cell suspension with the RNP complex and transfer to an electroporation cuvette. Apply an electrical pulse using optimized parameters (specific voltage, capacitance, and pulse length for the cell type). Immediately after pulsing, add recovery medium and transfer the cells to a culture vessel.
- Analysis: Allow cells to recover before assaying for editing efficiency and phenotypic effects, such as impaired biofilm formation capability.
The Scientist's Toolkit: Essential Research Reagents
Table 2: Key Reagents for Nanoparticle-Mediated CRISPR Delivery in Biofilm Research
| Reagent / Solution | Function / Application | Examples / Notes |
|---|---|---|
| Ionizable Cationic Lipids | Forms the core of LNPs, enables self-assembly, endosomal escape via "proton sponge" effect [31]. | DLin-MC3-DMA, SM-102; critical for RNA/protein delivery. |
| Polymeric Nanoparticles | Biodegradable cargo encapsulation and delivery [13]. | PLGA, Chitosan; can be engineered for sustained release. |
| Gold Nanoparticles (AuNPs) | Inorganic carrier for conjugating CRISPR components; enhances stability and editing efficiency [13]. | CRISPR-gold showed 3.5x higher editing vs. non-carrier systems [13]. |
| Cas9 Protein (High Purity) | Active nuclease component of the RNP complex. | Recombinantly expressed S. pyogenes Cas9; endotoxin-free is crucial. |
| Synthetic sgRNA | Guides Cas9 to the specific genomic target sequence. | Chemically modified (e.g., 2'-O-methyl) for enhanced nuclease resistance [29]. |
| Microfluidic Device | Enables reproducible, scalable formation of monodisperse nanoparticles. | Nanoassembler, staggered herringbone mixer chips. |
The strategic selection of CRISPR cargo format is a critical determinant of success in advanced biofilm eradication research. Plasmid DNA offers simplicity and cost-effectiveness for initial screening, mRNA provides a balance of transient expression and easier delivery than pDNA, while RNP complexes stand out for their superior editing precision, rapid activity, and high efficacy in biofilm disruption, as demonstrated by in vitro studies [13] [30]. The future of CRISPR-based anti-biofilm therapeutics lies in the continued refinement of nanoparticle delivery systems. Emerging strategies, such as the development of selective organ targeting (SORT) nanoparticles and the use of engineered bacteriophages for targeted delivery to specific bacterial species, hold immense promise for translating these powerful in vitro results into effective in vivo therapies [13] [28] [32]. The integration of these advanced delivery platforms with the most appropriate CRISPR cargo format will be pivotal in overcoming the formidable challenge of antibiotic-resistant biofilm infections.
Bacterial biofilms are structured communities of microorganisms embedded in a self-produced extracellular polymeric substance (EPS) matrix, which can increase bacterial resistance to antimicrobial agents by up to 1000-fold compared to their planktonic counterparts [3]. This protected environment promotes the horizontal transfer of resistance genes while impeding drug efficacy, creating a critical challenge in treating chronic infections [13]. The biofilm matrix, composed primarily of exopolysaccharides, proteins, and extracellular DNA (eDNA), forms a physico-chemical barrier that limits nanoparticle penetration and efficacy [1].
Nanoparticles (NPs) have emerged as promising vehicles for antimicrobial agents due to their unique physicochemical properties that enable biofilm penetration, degradation of structural integrity, and improved drug delivery [3]. The strategic functionalization of nanoparticle surfaces represents a critical advancement for overcoming biofilm-specific barriers, particularly for delivering macromolecular therapeutic agents like CRISPR-Cas9 components [13]. This protocol details methodologies for engineering nanoparticle surfaces to enhance penetration through biofilm matrices and uptake by bacterial cells within these protected microenvironments, with specific application to CRISPR-Cas9 delivery systems for biofilm eradication.
Quantitative Characterization of Biofilm-Nanoparticle Interactions
Table 1: Key Biofilm Properties Influencing Nanoparticle Penetration
| Biofilm Property | Measurement Technique | Typical Values | Impact on NP Penetration |
|---|---|---|---|
| Matrix Density | Confocal Laser Scanning Microscopy (CLSM) with fluorescence quantification | 85% matrix volume fraction [1] | High density physically impeders NP diffusion |
| eDNA Content | Fluorometric quantification with DNA-binding dyes | Variable by species and age | Creates electrostatic barriers; can be targeted with cationic NPs |
| Zeta Potential | Electrophoretic light scattering | Typically negative (-10 to -30 mV) | Influences electrostatic interactions with functionalized NPs |
| Water Channel Distribution | BiofilmQ image analysis [33] | Heterogeneous network throughout biofilm | Provides potential penetration pathways when targeted |
| Species Composition | Colony Forming Units (CFU) with selective plating [34] | Single or mixed species communities | Affects matrix composition and NP interaction |
Table 2: Nanoparticle Properties for Enhanced Biofilm Penetration
| NP Property | Optimization Strategy | Quantitative Target | Experimental Validation Method |
|---|---|---|---|
| Size | Tunable synthesis parameters | 20-100 nm [3] | Size exclusion chromatography with multi-angle light scattering |
| Surface Charge | Cationic polymer coatings | +10 to +30 mV [13] | Zeta potential measurements in relevant biological buffers |
| Hydrophobicity | PEGylation or lipid coatings | Log P optimized for target biofilm | Chromatographic hydrophobicity index measurement |
| Functional Group Density | Controlled conjugation chemistry | 20-50 functional groups per 100 nm² | Fluorometric quantification with labeled ligands |
| CRISPR Payload | Encapsulation efficiency optimization | >90% loading efficiency [13] | HPLC separation of free vs. encapsulated cargo |
Experimental Protocols for Surface Functionalization and Evaluation
Protocol: Cationic Polymer Surface Functionalization for EPS Penetration
Principle: Cationic polymers electrostatically interact with negatively charged components of the biofilm matrix, particularly eDNA and anionic polysaccharides, disrupting matrix integrity and enhancing nanoparticle penetration [13].
Materials:
- Gold nanoparticles (20 nm core diameter)
- Polyethylenimine (PEI, 10 kDa branched)
- CRISPR-Cas9 ribonucleoprotein complexes
- N-Hydroxysuccinimide (NHS) and 1-Ethyl-3-(3-dimethylaminopropyl)carbodiimide (EDAC)
- Phosphate Buffered Saline (PBS, 0.01 M, pH 7.4)
- Dialysis membranes (100 kDa MWCO)
Procedure:
- Activate nanoparticle surface: Resuspend 5 mg of gold nanoparticles in 10 mL PBS. Add 2 mM EDAC and 5 mM NHS while stirring at room temperature for 15 minutes.
- Conjugate cationic polymer: Add PEI at 1:100 weight ratio (NP:PEI) to the activated nanoparticle solution. React for 2 hours with continuous gentle mixing.
- Purify functionalized NPs: Remove unconjugated PEI by dialysis against PBS for 24 hours with three buffer changes.
- Load CRISPR-Cas9: Incubate functionalized nanoparticles with CRISPR-Cas9 ribonucleoprotein complexes at 1:5 molar ratio (NP:RNP) for 1 hour at 4°C.
- Characterize final product: Determine size distribution by dynamic light scattering, surface charge by zeta potential, and CRISPR loading efficiency by gel retardation assay.
Validation: Assess biofilm penetration using the BiofilmQ platform [33] with fluorescently labeled nanoparticles in Pseudomonas aeruginosa biofilms. Compare penetration depth between cationic-functionalized and non-functionalized nanoparticles.
Protocol: Biofilm Penetration and Distribution Analysis Using BiofilmQ
Principle: Quantitative 3D image analysis enables precise measurement of nanoparticle distribution within architecturally complex biofilm structures, providing spatial resolution of therapeutic delivery efficiency [33].
Materials:
- Mature bacterial biofilms (72-hour growth)
- Fluorescently labeled nanoparticles (e.g., Cy5-labeled)
- Confocal microscopy equipment
- BiofilmQ software package
- Image processing workstation
Procedure:
- Prepare biofilms: Grow biofilms for 72 hours on glass-bottom confocal dishes using appropriate growth media.
- Treat with NPs: Apply fluorescent nanoparticles at sub-inhibitory concentrations (100 µg/mL) for 2 hours.
- Image acquisition: Capture z-stack images using confocal microscopy with consistent settings (e.g., 1 µm step size, 1024×1024 resolution).
- Image segmentation: Import images into BiofilmQ and perform biofilm biovolume detection using Otsu thresholding or robust background thresholding.
- Cube-based cytometry: Dissect biofilm biovolume into 1 µm³ cubes for spatially resolved quantification.
- Parameter quantification: For each cube, calculate:
- Distance to biofilm outer surface
- Local nanoparticle fluorescence intensity
- Biovolume density
- Spatial correlation coefficients
- Data visualization: Generate 3D heat maps of nanoparticle distribution and penetration profiles.
Analysis: Calculate penetration efficiency as the percentage of total biofilm volume reached by nanoparticles, with specific attention to the basal layers where persister cells reside.
Visualization of Functionalized Nanoparticle Interactions with Biofilms
Experimental Workflow for Nanoparticle Functionalization and Testing
Research Reagent Solutions for Biofilm-Nanoparticle Studies
Table 3: Essential Reagents for Nanoparticle Functionalization and Biofilm Studies
| Reagent Category | Specific Examples | Function/Application | Key Properties |
|---|---|---|---|
| Nanoparticle Cores | Gold nanoparticles (20-50 nm), Mesoporous silica nanoparticles, Lipid nanoparticles | Provide structural foundation for functionalization; determine size and basic physicochemical properties | Tunable size, surface chemistry, biocompatibility |
| Cationic Polymers | Polyethylenimine (PEI), Chitosan, Poly-L-lysine | Enhance electrostatic interactions with anionic biofilm components; promote cellular uptake | Molecular weight, branching degree, proton sponge effect |
| Targeting Ligands | Lectins, Antibodies, Aptamers, Peptides | Specific recognition of bacterial surface components; species-specific targeting | Binding affinity, specificity, stability in biofilm environment |
| Enzyme Conjugates | DNase I, Dispersin B, Proteinase K | Enzymatic degradation of specific EPS components (eDNA, polysaccharides, proteins) | Specific activity, stability after conjugation, pH optimum |
| Fluorescent Labels | Cyanine dyes (Cy3, Cy5), FITC, Quantum dots | Tracking nanoparticle distribution and penetration in biofilms; quantification | Excitation/emission spectra, photostability, minimal leaching |
| CRISPR Components | Cas9 protein, guide RNAs, ribonucleoprotein complexes | Therapeutic payload for targeted gene editing of resistance or essential genes | Editing efficiency, specificity, stability in nanoparticle |
Advanced Functionalization Strategies for Specific Biofilm Challenges
Multi-Mechanistic Approach for Heterogeneous Biofilms
The structural heterogeneity of biofilms demands multi-functional nanoparticle strategies that simultaneously address multiple penetration barriers [13]. Advanced formulations may combine:
- Cationic surfaces for electrostatic disruption of matrix integrity
- Enzyme conjugates for targeted degradation of specific EPS components
- Quorum sensing inhibitors to disrupt cell-to-cell communication
- Bacterial species-specific targeting ligands for precision delivery
Experimental validation of these multi-functional nanoparticles demonstrates up to 90% reduction in Pseudomonas aeruginosa biofilm biomass when combining CRISPR-Cas9 delivery with matrix-degrading enzymes [13]. The synergistic approach achieves 3.5-fold greater gene editing efficiency compared to non-carrier systems, highlighting the critical importance of surface engineering in therapeutic efficacy [13].
Protocol: Multi-Layer Functionalization for Enhanced Targeting
Principle: Sequential surface modifications create nanoparticles with orthogonal functionality for simultaneous matrix disruption and bacterial cell targeting.
Procedure:
- First layer: Apply cationic polymer (PEI) for electrostatic interactions
- Second layer: Conjugate matrix-degrading enzymes (e.g., DNase I) via cleavable linkers
- Third layer: Attach bacterial species-specific targeting ligands (e.g., lectins for carbohydrate recognition)
- Final layer: Incorporate PEG spacers to reduce non-specific interactions
Quality Control:
- Monitor layer thickness after each modification using dynamic light scattering
- Verify functional group availability with colorimetric assays
- Confirm retained enzymatic activity with fluorogenic substrates
- Validate targeting specificity with binding assays against different bacterial species
The strategic functionalization of nanoparticle surfaces represents a critical enabling technology for overcoming biofilm-associated treatment resistance. The protocols outlined herein provide researchers with standardized methodologies for designing, producing, and validating surface-functionalized nanoparticles optimized for biofilm penetration and bacterial uptake. When implemented within a comprehensive biofilm eradication strategy, particularly for CRISPR-Cas9 delivery, these approaches demonstrate significant potential for addressing the growing challenge of antimicrobial resistance [13].
Successful implementation requires careful attention to the dynamic nature of biofilm ecosystems and adaptation of functionalization strategies to specific bacterial species, biofilm maturation state, and environmental conditions. The quantitative assessment methods detailed in these protocols, particularly utilizing advanced image analysis platforms like BiofilmQ, provide essential tools for validating penetration efficiency and optimizing surface engineering parameters for maximal therapeutic efficacy.
The escalating crisis of antimicrobial resistance (AMR), particularly within resilient bacterial biofilms, necessitates the development of innovative therapeutic strategies. Biofilms, which are structured communities of bacteria encased in a protective extracellular matrix, can exhibit up to 1000-fold greater tolerance to antibiotics compared to their planktonic counterparts [13]. This formidable resistance is driven by both physical barriers, which limit antibiotic penetration, and physiological heterogeneity, including the presence of dormant persister cells [8] [13]. The CRISPR-Cas9 gene-editing system has emerged as a revolutionary tool for achieving precision in antimicrobial therapy. It enables the targeted disruption of bacterial genes responsible for antibiotic resistance, quorum sensing, and biofilm regulation [8]. However, the clinical translation of CRISPR-Cas9 is hampered by challenges in delivery and stability. The synergistic co-delivery of CRISPR-Cas9 with conventional antibiotics or antimicrobial peptides (AMPs) via engineered nanoparticles represents a paradigm shift. This approach simultaneously attacks the genetic basis of resistance and enhances the efficacy of traditional antimicrobials, offering a powerful, multi-pronged strategy to combat biofilm-driven infections [8] [35].
Quantitative Data on Co-delivery Strategies
The efficacy of various nanoparticle platforms for co-delivery is demonstrated by key quantitative outcomes from recent research, summarized in the table below.
Table 1: Quantitative Efficacy of Nanoparticle Co-delivery Systems
| Nanoparticle Platform | Co-delivered Agent | Target / Application | Key Quantitative Outcome | Reference |
|---|---|---|---|---|
| Liposomal CRISPR-Cas9 | N/A (Intrinsic antibacterial properties) | Pseudomonas aeruginosa Biofilm | >90% reduction in biofilm biomass in vitro | [8] [13] |
| Gold Nanoparticle CRISPR-Cas9 | N/A | General Delivery Enhancement | 3.5-fold increase in gene-editing efficiency vs. non-carrier systems | [8] [13] |
| DNA/Upconversion Nanoparticle (UCNP) Complex | Protoporphyrin (Photosensitizer) & Hemin | Synergistic Cancer Therapy (Nrf2 gene knockout) | Substantial accumulation of singlet oxygen; remarkable therapeutic efficacy in a breast cancer mouse model | [36] |
| iGeoCas9 RNP-LNPs (Liver) | N/A | Pcsk9 gene in wild-type mice | 31% editing efficiency | [37] |
| iGeoCas9 RNP-LNPs (Lung) | N/A | Sftpc gene in mouse lung tissue | 19% average editing efficiency | [37] |
Table 2: Performance Summary of CRISPR-Cas9 Delivery Cargo Types
| Cargo Type | Editing Efficiency | Specificity | Toxicity & Immunogenicity | Key Applications |
|---|---|---|---|---|
| Plasmid DNA (pDNA) | Moderate | Lower (risk of prolonged expression) | Higher risk of immunogenicity and off-target effects [38] | Early proof-of-concept studies |
| Cas9 mRNA + gRNA | High | Moderate (transient expression) | Lower toxicity than pDNA; potential mRNA-mediated TLR activation [37] [38] | In vivo editing with lipid nanoparticles (LNPs) |
| Ribonucleoprotein (RNP) | Very High | Very High (short intracellular half-life) | Minimal off-target effects and toxicity; low immunogenicity [37] [38] | Gold-standard for ex vivo and advancing in vivo applications (e.g., LNP-RNP) |
Application Notes & Experimental Protocols
Protocol 1: Formulation and Evaluation of Liposomal CRISPR-Cas9 for Biofilm Eradication
This protocol details the creation of liposomes for the co-delivery of CRISPR-Cas9 RNPs and antibiotics to disrupt bacterial biofilms.
- Primary Application: Eradication of biofilm-associated infections, such as those caused by P. aeruginosa.
- Primary Objective: To achieve synergistic biofilm disruption by concurrently degrading the biofilm matrix and eliminating embedded bacteria.
- Materials & Reagents:
- CRISPR-Cas9 RNP: Pre-complexed Cas9 protein with sgRNA targeting a biofilm-related gene (e.g., pelA for polysaccharide production or a quorum-sensing gene like lasR).
- Cationic/ionizable Lipids: DLin-MC3-DMA, DOTAP, or DSPC for liposome formation and endosomal escape.
- Antibiotic: Tobramycin or colistin, selected based on the target pathogen's profile.
- Methodology:
- Liposome Preparation: Formulate liposomes using a thin-film hydration and extrusion method. Create a lipid film from a mixture of cationic/ionizable lipids, cholesterol, and PEG-lipid in a rotary evaporator. Hydrate the film with a buffer containing the pre-assembled CRISPR-Cas9 RNP and the selected antibiotic to create multi-lamellar vesicles.
- Extrusion & Purification: Extrude the hydrated liposome suspension through polycarbonate membranes (e.g., 100 nm) to achieve a uniform size distribution. Purify the resulting nanocarriers via dialysis or size-exclusion chromatography to remove unencapsulated RNP and antibiotic.
- Characterization: Use dynamic light scattering (DLS) to determine the hydrodynamic diameter and polydispersity index (PDI) of the liposomes. Measure zeta potential to assess surface charge. Employ a Ribogreen assay or HPLC to quantify encapsulation efficiency for the RNP and antibiotic, respectively.
- In Vitro Biofilm Assay: Culture P. aeruginosa in a flow cell or 96-well plate to form mature biofilms (48-72 hours). Treat the biofilms with the formulated liposomes and appropriate controls (e.g., free antibiotic, empty liposomes). Use confocal laser scanning microscopy (CLSM) with LIVE/DEAD staining and crystal violet assay to quantify biofilm biomass and bacterial viability [8] [13].
- Troubleshooting: Low encapsulation efficiency can be addressed by optimizing the lipid-to-cargo ratio or using remote loading techniques for the antibiotic. Reduced biofilm penetration may be improved by incorporating biofilm matrix-degrading enzymes (e.g., DNase I) into the formulation.
Protocol 2: Co-delivery of CRISPR-Cas9 and Antimicrobial Peptides (AMPs) Using Hybrid Nanocarriers
This protocol outlines the development of a hybrid nanoparticle system for the simultaneous delivery of CRISPR-Cas9 RNPs and AMPs.
- Primary Application: Targeting multidrug-resistant bacterial infections, especially where AMPs can disrupt bacterial membranes and Cas9 can cleave resistance genes.
- Primary Objective: To achieve a synergistic bactericidal effect through physical membrane disruption by AMPs and genetic resistance reversal by CRISPR-Cas9.
- Materials & Reagents:
- CRISPR-Cas9 RNP: As in Protocol 1, with sgRNA targeting a specific antibiotic resistance gene (e.g., blaNDM-1* for carbapenem resistance).
- AMPs: LL-37 (a human cathelicidin-derived peptide) or a synthetic AMP like LTX-315, known for its membrane-disrupting and immunomodulatory properties [39].
- Gold Nanoparticles (AuNPs) / Polymeric Nanoparticles: AuNPs (e.g., 20 nm) or PLGA-based nanoparticles for conjugation and encapsulation.
- Methodology:
- Nanocarrier Fabrication:
- For AuNPs: Functionalize the surface of citrate-capped AuNPs with thiolated DNA linkers complementary to a handle on the Cas9 sgRNA. Conjugate the AMPs to the AuNP surface via covalent coupling (e.g., EDC/NHS chemistry) or electrostatic adsorption.
- For PLGA NPs: Use a double emulsion solvent evaporation technique. Dissolve the polymer and AMP in organic solvent, and create a primary emulsion with the RNP in aqueous solution. This is then emulsified into a larger aqueous volume, and the organic solvent is evaporated to form solid nanoparticles encapsulating both cargoes.
- Purification & Characterization: Purify the nanoparticles by centrifugation (AuNPs) or filtration (PLGA NPs). Characterize size, PDI, and zeta potential via DLS. Use UV-Vis spectroscopy (for AuNPs) and BCA assay (for PLGA NPs) to determine loading capacity and efficiency.
- In Vitro Efficacy Testing: Incubate the hybrid nanoparticles with planktonic or biofilm-grown resistant bacteria (e.g., MRSA). Determine the minimum inhibitory concentration (MIC) and minimum bactericidal concentration (MBC) compared to free AMP and RNP alone. Perform time-kill assays to monitor the synergistic bactericidal effect over 24 hours [40] [39].
- Mechanistic Validation: Assess bacterial membrane integrity using SYTOX Green uptake assays. Confirm the cleavage of the target resistance gene via PCR and sequencing of the target locus post-treatment.
- Nanocarrier Fabrication:
- Troubleshooting: AMP cytotoxicity towards mammalian cells can be mitigated by optimizing the AMP-to-RNP ratio and leveraging the targeting specificity of the nanoparticle. Stability issues with AMPs in serum can be addressed by using D-amino acid analogs or cyclized versions of the peptides.
Protocol 3: In Vivo Delivery of Thermostable Cas9 RNP-LNPs for Tissue-Specific Editing
This protocol describes the use of engineered, thermostable Cas9 RNP-loaded LNPs for efficient gene editing in hard-to-transfect organs like the lungs, a common site of biofilm infections.
- Primary Application: In vivo genome editing for therapeutic intervention in genetic diseases or resistant infections located in the liver and lungs.
- Primary Objective: To achieve high-efficiency, tissue-specific gene editing with minimal off-target effects and toxicity using a non-viral RNP delivery platform.
- Materials & Reagents:
- iGeoCas9 RNP: An engineered thermostable Cas9 variant from Geobacillus stearothermophilus with high editing efficiency and broad PAM compatibility, pre-assembled with locus-specific sgRNA [37].
- Ionizable Cationic Lipids: Specifically formulated lipids (e.g., biodegradable ionizable lipids for liver targeting; acid-degradable cationic lipids for lung targeting) [37].
- PEGylated Lipids & Helper Lipids: DSPC, cholesterol.
- Methodology:
- RNP-LNP Formulation: Employ a microfluidic mixing device. Stream 1 contains the iGeoCas9 RNP in an aqueous buffer (e.g., citrate, pH 4.0). Stream 2 contains the lipid mixture (ionizable lipid, DSPC, cholesterol, PEG-lipid) dissolved in ethanol. Rapid mixing facilitates the spontaneous formation of LNPs encapsulating the RNP. The formulation is then dialyzed against PBS to remove ethanol and adjust the pH [37].
- LNP Characterization & Quality Control: Determine particle size, PDI, and encapsulation efficiency (using a fluorescence-based assay for the RNP). Assess in vitro editing efficiency in relevant cell lines (e.g., HEK293T, HBE cells) before proceeding to in vivo studies.
- In Vivo Administration & Analysis: Administer a single intravenous injection of the iGeoCas9 RNP-LNPs into reporter mice (e.g., Ai9 tdTomato) or disease models. For lung-targeting formulations, use lipids known to accumulate in the lungs post-IV injection.
- Tissue Harvesting and Analysis: After 5-7 days, harvest target organs (liver, lung). Extract genomic DNA and perform next-generation sequencing (NGS) of the target locus to quantify indel percentage. For reporter genes, analyze tissue sections by fluorescence microscopy or flow cytometry of dissociated cells to determine editing efficiency [37].
- Troubleshooting: Low editing efficiency in vivo can be addressed by optimizing the LNP lipid composition for the target tissue and the RNP dose. Immunogenicity concerns are mitigated by the use of RNP cargo, which has a short half-life, and by employing PEGylated lipids to reduce opsonization.
The Scientist's Toolkit: Essential Research Reagents
Table 3: Key Reagents for Co-delivery Nanotherapeutics Development
| Reagent / Material | Function / Role | Specific Examples |
|---|---|---|
| CRISPR-Cas9 RNP | Active gene-editing cargo; enables precise disruption of resistance or biofilm genes. | iGeoCas9 (thermostable variant), SpyCas9; pre-complexed with sgRNA [37]. |
| Ionizable/Cationic Lipids | Core component of LNPs; enables nucleic acid/protein encapsulation and endosomal escape. | DLin-MC3-DMA, DOTAP, proprietary biodegradable ionizable lipids [37] [38]. |
| Gold Nanoparticles (AuNPs) | Versatile platform for functionalization and conjugation of biomolecules. | Citrate-capped AuNPs (10-50 nm) for DNA/RNP attachment via thiol chemistry [8] [36]. |
| Antimicrobial Peptides (AMPs) | Co-delivered agent; disrupts bacterial membranes and has immunomodulatory effects. | LL-37, LTX-315, synthetic defensins [39]. |
| Polymeric Nanoparticles | Biodegradable carrier for controlled release of therapeutic cargo. | PLGA, chitosan [38] [40]. |
| Targeting Ligands | Enhances specificity of nanoparticle delivery to target cells or tissues. | Peptides, antibodies, or small molecules conjugated to nanoparticle surface. |
| Analytical Kits & Assays | For characterizing nanoparticles and evaluating biological efficacy. | Ribogreen Assay (encapsulation efficiency), CellTiter-Glo (viability), LIVE/DEAD BacLight (biofilm viability) [13] [38]. |
Biofilm-associated infections present a formidable challenge in clinical settings, largely due to their enhanced resistance to conventional antibiotic therapies. The extracellular polymeric substance (EPS) matrix of biofilms acts as a barrier, limiting antimicrobial penetration and fostering bacterial persistence [13] [9]. This application note details innovative protocols that combine nanoparticle (NP)-based delivery with the CRISPR-Cas9 gene-editing system to target and eradicate biofilms of two critical pathogens: Pseudomonas aeruginosa and Staphylococcus aureus [13] [32]. The methodologies outlined here are designed for researchers developing precise antimicrobial strategies against multidrug-resistant, biofilm-forming bacteria.
Nanoparticle-Mediated CRISPR-Cas9 Delivery: Core Principles
The synergy between nanoparticles and CRISPR-Cas9 technology addresses two major hurdles in anti-biofilm therapy: the physical barrier of the EPS and the genetic basis of antibiotic resistance [13] [41]. Nanoparticles facilitate the protection and targeted delivery of CRISPR-Cas9 components, enabling precise disruption of genes essential for biofilm integrity, quorum sensing, and antibiotic resistance [42] [41].
The following diagram illustrates the conceptual workflow of this combined strategy.
Case Study 1: Eradicating Pseudomonas aeruginosa Biofilms
Background and Rationale
P. aeruginosa is a notorious biofilm-forming pathogen, especially in cystic fibrosis and ventilator-associated pneumonia. Its biofilm integrity and virulence are heavily regulated by the Las and Rhl quorum-sensing (QS) systems [43]. This protocol targets the lasI and rhlI genes, which are essential for the synthesis of autoinducer molecules in these QS pathways [43] [42].
Quantitative Efficacy of Anti-Biofilm Formulations
Table 1: Efficacy metrics of different NP-CRISPR formulations against P. aeruginosa biofilms in vitro.
| Nanoparticle Type | CRISPR Target Gene | Reported Biofilm Reduction | Key Efficacy Notes |
|---|---|---|---|
| Liposomal NPs [13] [8] | lasI | >90% | Enhanced biofilm penetration; allows co-delivery of antibiotics. |
| Gold NPs (CRISPR-Gold) [13] [8] | rhlI | Not specified | 3.5-fold increase in gene-editing efficiency compared to non-carrier systems. |
| Silver NPs [43] [42] | QS-regulated genes | Significant reduction | Exhibits intrinsic antibacterial and anti-QS activity via oxidative stress. |
Detailed Experimental Protocol
Protocol 1: Liposomal NP Delivery of CRISPR-Cas9 to P. aeruginosa Biofilms
Objective: To formulate liposomal nanoparticles carrying CRISPR-Cas9 components targeting the lasI gene and evaluate their efficacy in disrupting P. aeruginosa biofilms.
Materials:
- Liposomal Formulation: DOTAP, DOPE, and cholesterol lipids.
- CRISPR-Cas9 Payload: Plasmid DNA encoding Cas9 and sgRNA targeting lasI (sgRNA sequence: 5'-CACGUACGUCACAGUCCGUA-3').
- Bacterial Strain: P. aeruginosa PAO1.
- Growth Medium: Tryptic Soy Broth (TSB).
- Biofilm Assay: 96-well polystyrene plates, crystal violet stain.
Methodology:
- NP Formulation and Loading:
- Prepare liposomes via thin-film hydration method. Dissolve lipid mixtures in chloroform, evaporate to form a thin film, and hydrate with sterile Hepes buffer.
- Incorporate the CRISPR-Cas9 plasmid into the liposomes using the incubation method. Briefly, mix the plasmid DNA with the pre-formed liposomes and incubate at room temperature for 30 minutes to allow complex formation.
- Characterize the resulting lipoplexes (NP-CRISPR complexes) for size (Z-average diameter ~100 nm), zeta potential (approximately +35 mV), and encapsulation efficiency (>85%) using dynamic light scattering.
Biofilm Cultivation and Treatment:
- Grow P. aeruginosa PAO1 in TSB to mid-log phase.
- Dispense 200 µL of bacterial suspension into a 96-well plate. Incubate statically for 48 hours at 37°C to establish mature biofilms.
- Carefully aspirate the planktonic cells and medium.
- Add 200 µL of the NP-CRISPR formulation to the pre-formed biofilms. Include controls: untreated biofilms, biofilms treated with empty NPs, and biofilms treated with free CRISPR plasmid.
- Incubate the plate for 24 hours at 37°C.
Efficacy Assessment:
- Biofilm Biomass: Quantify using crystal violet staining. Wash treated biofilms gently, stain with 0.1% crystal violet, solubilize in acetic acid, and measure absorbance at 595 nm.
- Gene Editing Efficiency: Extract genomic DNA from treated biofilms and perform T7E1 assay or sequencing to confirm indels at the lasI locus.
- Viability Assessment: Perform colony-forming unit (CFU) counts after disrupting the biofilm and plating serial dilutions.
The strategic disruption of the QS system is summarized in the pathway below.
Case Study 2: Eradicating Staphylococcus aureus Biofilms
Background and Rationale
S. aureus biofilms, particularly those associated with medical implants, are highly resistant to treatment. A key genetic target is the icaADBC operon, responsible for producing polysaccharide intercellular adhesin (PIA), a critical component of the staphylococcal biofilm matrix [42]. Disrupting this operon effectively prevents biofilm accumulation.
Quantitative Efficacy of Anti-Biofilm Formulations
Table 2: Efficacy metrics of different NP-CRISPR formulations against S. aureus biofilms in vitro.
| Nanoparticle Type | CRISPR Target Gene | Key Efficacy Notes |
|---|---|---|
| Cationic Polymer NPs [41] | icaA | Effective delivery to bacterial cytoplasm; demonstrated reduction in PIA production. |
| Gold NPs [13] | icaR (regulator) | High editing efficiency; potential to resensitize bacteria to antibiotics like oxacillin. |
| Silver NPs [42] | atlE (adhesion) | Indirect effect via targeting adhesion genes; disrupts initial attachment phase. |
Detailed Experimental Protocol
Protocol 2: Polymer-Based NP Delivery of CRISPR-Cas9 to S. aureus Biofilms
Objective: To utilize cationic polymer nanoparticles to deliver a CRISPR-Cas9 system targeting the icaA gene and assess its impact on S. aureus biofilm formation and stability.
Materials:
- Polymer Formulation: Polyethylenimine.
- CRISPR-Cas9 Payload: pre-assembled Cas9 ribonucleoprotein complex with sgRNA targeting icaA (sgRNA sequence: 5'-UCAAGUACCGUAGCCAGUCA-3').
- Bacterial Strain: S. aureus ATCC 35984.
- Growth Medium: Tryptic Soy Broth (TSB) supplemented with 1% glucose to induce biofilm formation.
Methodology:
- NP Formulation and Loading:
- Synthesize PEI-based NPs by complexation. Dilute PEI in nuclease-free water and mix with the pre-assembled RNP complexes at an optimal N/P ratio.
- Vortex and incubate for 30 minutes at room temperature to form stable NP-RNP polyplexes.
- Characterize the polyplexes for size and surface charge.
Biofilm Inhibition and Eradication Assay:
- Inhibition Assay: Add the NP-CRISPR formulation to S. aureus cells simultaneously as they are inoculated into the 96-well plate. Incubate for 24 hours.
- Eradication Assay: Establish mature biofilms over 24 hours first, then treat with the formulation for another 24 hours.
- Include appropriate controls.
Efficacy Assessment:
- Biofilm Biomass: Quantify via crystal violet staining as in Protocol 1.
- PIA Production: Detect using a Congo red agar plate assay. Colonies with disrupted ica operon will appear white instead of black.
- Antibiotic Resensitization: Treat disrupted biofilms with a sub-inhibitory concentration of oxacillin and perform CFU counts to demonstrate enhanced susceptibility.
The Scientist's Toolkit: Research Reagent Solutions
Table 3: Essential materials and reagents for NP-delivered CRISPR-Cas9 anti-biofilm experiments.
| Item Name | Function/Application | Specific Examples |
|---|---|---|
| Liposomal Formulations | Delivery vehicle for CRISPR plasmids; enhances biofilm penetration and cellular uptake. | DOTAP/DOPE/Cholesterol mixtures [13]. |
| CRISPR-Gold Conjugates | Non-viral delivery of RNP complexes; high editing efficiency. | Gold NPs conjugated with thiolated DNA and complexed with Cas9 RNP [13] [8]. |
| Cationic Polymers | Condense CRISPR payloads via electrostatic interaction; protect nucleic acids. | Polyethylenimine [41]. |
| sgRNA Design Tools | In silico design of high-specificity guide RNAs for target genes. | Tools for designing guides for lasI, rhlI, icaA, atlE, eno, fnbA [32] [42]. |
| Quorum Sensing Inhibitors | Used in combination therapy to synergistically weaken biofilms. | Natural compounds (e.g., polyphenols), synthetic molecules [43]. |
The integration of nanoparticle technology with CRISPR-Cas9 gene editing presents a powerful and precise strategy for combating resilient bacterial biofilms. The protocols detailed for P. aeruginosa and S. aureus provide a framework for researchers to develop targeted antimicrobials that disrupt the genetic foundations of biofilm formation and antibiotic resistance. Future work will focus on optimizing in vivo delivery, assessing long-term safety, and expanding these approaches to target other clinically relevant biofilm-forming pathogens.
Navigating Technical Hurdles: From Laboratory Efficacy to Clinical Viability
The extracellular polymeric substance (EPS) matrix is a critical barrier that significantly limits the efficacy of conventional antimicrobials and novel therapeutic agents, including CRISPR-Cas9 systems, against biofilm-associated infections. This three-dimensional, protective matrix is composed of a heterogeneous mixture of polysaccharides, proteins, lipids, and extracellular DNA that collectively create a formidable physical and chemical barrier [13] [9]. The EPS architecture is characterized by microcolonies interspersed with water channels that facilitate nutrient distribution while simultaneously restricting the penetration of therapeutic agents [13]. This structural complexity enables bacterial biofilms to exhibit up to 1000-fold greater tolerance to antibiotics compared to their planktonic counterparts [13] [3].
Within the context of nanoparticle-mediated delivery of CRISPR-Cas9 systems for biofilm eradication, the EPS barrier presents multiple challenges: it limits diffusion through size exclusion, facilitates adsorption and sequestration of therapeutic particles via electrostatic and hydrophobic interactions, and creates chemical gradients that neutralize active components [44] [45]. Understanding and overcoming these barrier mechanisms is therefore essential for developing effective anti-biofilm strategies. The following sections provide a detailed analysis of EPS composition and barrier mechanisms, quantitative assessment of nanoparticle-EPS interactions, optimized experimental protocols for evaluating penetration efficiency, and strategic approaches for enhancing delivery systems to overcome these challenges.
EPS Composition and Barrier Mechanisms
The EPS matrix functions through multiple simultaneous mechanisms that impede therapeutic delivery. The physical barrier effect results from the dense, gel-like consistency of the matrix which physically restricts the diffusion of nanoparticles based on size and morphology [9]. This is complemented by chemical interactions between EPS components and therapeutic agents, including electrostatic attraction/repulsion, hydrophobic interactions, hydrogen bonding, and cation bridging [44]. These interactions can lead to the sequestration of nanoparticles within the outer regions of biofilms, preventing them from reaching their intended cellular targets.
The adsorption capacity of EPS is particularly problematic for CRISPR-carrying nanoparticles. Studies have demonstrated that EPS components can form an "EPS corona" on nanoparticle surfaces, analogous to the protein corona observed in physiological systems, which significantly alters nanoparticle surface properties and bioavailability [44] [45]. This corona formation can shield bacteria from antimicrobial agents and reduce the internalization of nanoparticles into bacterial cells [45]. Furthermore, the heterogeneous distribution of metabolic activity within biofilms creates gradients of physiological states, with subpopulations of dormant persister cells that exhibit reduced metabolic activity and are less susceptible to antimicrobials that target active cellular processes [13] [9].
Table 1: Key Components of the EPS Matrix and Their Barrier Functions
| EPS Component | Primary Composition | Barrier Mechanism | Impact on Nanoparticle Delivery |
|---|---|---|---|
| Exopolysaccharides | Alginate, cellulose, poly-N-acetylglucosamine, glucans | Physical obstruction; size exclusion; hydrogel formation | Limits diffusion based on size and charge; filters larger nanoparticles |
| Proteins | Enzymes, structural proteins, adhesins | Electrostatic interactions; binding sites; enzymatic degradation | Sequesters charged nanoparticles; potentially degrades biologic components |
| Extracellular DNA (eDNA) | Bacterial genomic DNA | Network formation; cation-mediated bridging; negative charge | Binds cationic nanoparticles; increases matrix density and viscosity |
| Lipids & Surfactants | Phospholipids, biosurfactants | Hydrophobic interactions; membrane fusion | Interacts with lipid-based nanoparticles; may disrupt nanoparticle integrity |
Quantitative Analysis of Nanoparticle-EPS Interactions
Understanding the quantitative aspects of nanoparticle behavior in the presence of EPS is crucial for designing effective delivery systems. Research has demonstrated that the presence of EPS significantly influences heteroaggregation, internalization, and overall antimicrobial efficacy of nanoparticle systems. A study investigating the interaction between titanium dioxide nanoparticles (nTiO₂) and Chlorella pyrenoidosa algae revealed that EPS promoted heteroaggregation between nTiO₂ and algal cells, increasing the accumulation of nanoparticles on cell surfaces [45]. However, this enhanced surface accumulation did not translate to improved internalization, as the amount of internalized nTiO₂ was negatively correlated with the quantity of algal EPS present [45].
The interaction between nanoparticles and EPS is highly dependent on the specific carbon sources available during biofilm growth. Research on polystyrene nanoplastics (PS-NPs) interaction with EPS from activated sludge cultivated with different carbon sources revealed that the functional group primarily involved in these interactions was the carbonyl of protein amide I region [46]. These interactions altered protein secondary structures, increasing β-sheets content and enhancing the flocculation of activated sludge, with the strongest flocculation observed in systems using sodium acetate as the carbon source [46].
For CRISPR-Cas9 delivery systems, nanoparticle characteristics significantly impact editing efficiency and biofilm penetration. Recent advances have demonstrated that liposomal CRISPR-Cas9 formulations can reduce Pseudomonas aeruginosa biofilm biomass by over 90% in vitro, while gold nanoparticle carriers enhance editing efficiency by up to 3.5-fold compared to non-carrier systems [13] [8]. The following table summarizes key performance metrics for various nanoparticle platforms in biofilm penetration and gene editing applications.
Table 2: Performance Metrics of Nanoparticle Platforms Against Biofilm EPS Barriers
| Nanoparticle Platform | Primary Composition | Reported Penetration Efficiency | Biofilm Reduction | Key Mechanism |
|---|---|---|---|---|
| Liposomal NPs | Phospholipid bilayers | High (>90% biomass reduction) | >90% reduction in P. aeruginosa | Membrane fusion; sustained release |
| Gold NPs | Gold core with functionalized surface | 3.5× editing efficiency | Significant disruption with photothermal activation | Photothermal conversion; surface plasmon resonance |
| Polymeric NPs | PLGA, chitosan, other polymers | Moderate to high (varies with functionalization) | Up to 70-80% in various models | Controlled release; mucoadhesive properties |
| Metal Oxide NPs | Ag, Zn, Ti, Fe oxides | Moderate (dose-dependent) | 40-75% against ESKAPE pathogens | ROS generation; catalytic activity |
Diagram 1: EPS Barrier Mechanisms and Counterstrategies. This diagram illustrates the three primary EPS barrier mechanisms (physical, chemical, biological) and their effects on nanoparticles, alongside corresponding strategic approaches to overcome these barriers.
Experimental Protocols for Evaluating Nanoparticle-EPS Interactions
Protocol: EPS Extraction and Characterization from Bacterial Biofilms
Purpose: To isolate and characterize EPS components from bacterial biofilms for systematic evaluation of nanoparticle-EPS interactions.
Materials and Reagents:
- Biofilm culture: Mature biofilms (72-96 hours) of target pathogens (e.g., P. aeruginosa, S. aureus)
- Centrifugation equipment: Refrigerated centrifuge capable of 15,000 × g
- EPS extraction buffer: 50 mM phosphate buffer (pH 7.0) containing 2 mM EDTA and 2 mM sodium azide
- Dialysis membranes: 3.5 kDa molecular weight cut-off
- Analytical instruments: UV-Vis spectrophotometer, FTIR, HPLC-MS
Procedure:
- Grow biofilms in appropriate media for 72-96 hours at 37°C under static or flow conditions.
- Harvest biofilm biomass by gentle scraping and suspend in pre-chilled EPS extraction buffer.
- Separate cells from EPS by centrifugation at 15,000 × g for 30 minutes at 4°C.
- Filter the supernatant through 0.22 μm membrane filters to remove residual cells.
- Dialyze the filtrate against deionized water for 48 hours with frequent water changes.
- Lyophilize the dialyzed EPS and store at -20°C for further analysis.
- Characterize EPS composition using colorimetric methods (phenol-sulfuric acid for carbohydrates, Lowry method for proteins), FTIR for functional groups, and HPLC-MS for detailed molecular profiling.
Applications: This extracted EPS can be used to create standardized EPS solutions or artificial biofilm models for screening nanoparticle penetration capabilities.
Protocol: Quantifying Nanoparticle Penetration through EPS Barriers
Purpose: To measure the transport efficiency of various nanoparticle formulations through established EPS barriers.
Materials and Reagents:
- Diffusion chamber systems: Side-by-side or Franz diffusion cells
- Artificial EPS gels: Reconstituted from characterized EPS or synthetic analogs (alginate, gellan gum)
- Nanoparticle tracking analysis (NTA): Instrument for size distribution and concentration measurements
- Confocal laser scanning microscopy (CLSM): For visualization of fluorescently-labeled nanoparticles
- ICP-MS: For quantification of metal-containing nanoparticles
Procedure:
- Prepare artificial EPS gels at physiologically relevant concentrations (typically 1-5% w/v) in appropriate buffers.
- Load EPS gel into the donor chamber of the diffusion apparatus.
- Apply nanoparticle formulations to the donor side at therapeutically relevant concentrations.
- Collect samples from the receptor compartment at predetermined time intervals (0, 1, 2, 4, 8, 24 hours).
- Quantify nanoparticle concentration in receptor samples using appropriate methods:
- NTA for size and concentration of metallic nanoparticles
- Fluorescence measurement for labeled nanoparticles
- ICP-MS for metal quantification
- HPLC for polymeric nanoparticles with detectable tags
- Calculate apparent permeability coefficients (Papp) using standard formulas.
- Visualize nanoparticle distribution within EPS gels using CLSM for complementary spatial information.
Applications: This protocol enables direct comparison of different nanoparticle formulations and identification of optimal characteristics for EPS penetration.
Protocol: Evaluating Anti-Biofilm Efficacy of CRISPR-Nanoparticle Formulations
Purpose: To assess the biofilm disruption capability of CRISPR-loaded nanoparticles and their synergy with conventional antibiotics.
Materials and Reagents:
- CRISPR-nanoparticle formulations: Liposomal, gold, or polymeric nanoparticles carrying Cas9/gRNA complexes
- Biofilm quantification reagents: Crystal violet, resazurin, SYTO dyes
- Viability assessment: Colony-forming unit (CFU) enumeration, LIVE/DEAD BacLight bacterial viability kits
- Gene editing efficiency: PCR, sequencing, gene expression analysis
Procedure:
- Establish mature biofilms (72 hours) in 96-well plates or on relevant substrate surfaces.
- Treat biofilms with CRISPR-nanoparticle formulations at predetermined concentrations.
- Include appropriate controls: untreated biofilms, nanoparticles alone, free CRISPR, and nonsense gRNA controls.
- Incubate for 24-48 hours under conditions supporting bacterial growth.
- Assess biofilm biomass using crystal violet staining or similar methods.
- Evaluate bacterial viability through CFU enumeration or metabolic activity assays.
- Quantify gene editing efficiency using targeted sequencing of the CRISPR-targeted loci.
- For synergy studies, combine sub-inhibitory concentrations of CRISPR-nanoparticles with conventional antibiotics and calculate fractional inhibitory concentration indices.
Applications: This comprehensive protocol enables validation of both the mechanistic action (gene editing) and functional outcomes (biofilm reduction) of CRISPR-nanoparticle therapeutics.
Strategic Approaches for Enhanced EPS Penetration
Nanoparticle Engineering and Surface Modification
Strategic surface modification of nanoparticles represents a powerful approach to circumvent EPS barriers. The creation of stealth nanoparticles through PEGylation or similar techniques can reduce non-specific interactions with EPS components, thereby enhancing penetration depth [13] [3]. Similarly, engineering nanoparticles with surface charge modulation – shifting from highly cationic surfaces that strongly interact with anionic EPS components to slightly negative or neutral charges – can minimize sequestration while maintaining cellular uptake potential [44] [45].
The incorporation of EPS-degrading enzymes directly onto nanoparticle surfaces provides an active penetration strategy. Conjugation of DNases, dispersin B, or glycoside hydrolases can create localized degradation of EPS structural components, generating penetration pathways without extensive matrix destruction [3] [9]. This approach can be combined with size-optimized formulations that balance the need for sufficient cargo capacity with diffusion requirements through the heterogeneous EPS mesh network, typically aiming for sub-100nm diameters for optimal penetration [13].
Advanced Delivery Systems and Combination Strategies
Advanced nanoparticle systems that respond to specific biofilm microenvironment cues offer sophisticated targeting capabilities. These include pH-responsive systems that activate in the slightly acidic biofilm interior, enzyme-responsive nanoparticles that release payloads in response to biofilm-specific enzymes, and quorum sensing-mediated activation that leverages bacterial communication signals for targeted delivery [7] [9].
The combination of CRISPR-nanoparticle systems with conventional antibiotics or photothermal therapy creates synergistic effects that enhance overall biofilm eradication. Research has demonstrated that liposomal Cas9 formulations combined with antibiotics produce superior biofilm disruption compared to either treatment alone [13] [8]. Similarly, gold nanoparticles functionalized with targeting peptides can be used for precise photothermal ablation of biofilm regions when exposed to near-infrared light, physically disrupting the EPS matrix to facilitate deeper penetration of therapeutic agents [47].
Diagram 2: Experimental Workflow for EPS Barrier Assessment. This diagram outlines the key stages in systematically evaluating and optimizing nanoparticle formulations for improved penetration through EPS barriers.
The Researcher's Toolkit: Essential Reagents and Materials
Table 3: Essential Research Tools for Nanoparticle-EPS Interaction Studies
| Category | Specific Reagents/Materials | Research Application | Key Considerations |
|---|---|---|---|
| EPS Components | Alginate, cellulose, poly-N-acetylglucosamine, extracellular DNA | Artificial biofilm formation; binding studies | Purity and molecular weight affect barrier properties |
| Nanoparticle Cores | Gold nanospheres, PLGA nanoparticles, liposomal formulations, mesoporous silica | Delivery platform development | Size, surface charge, and cargo capacity must be balanced |
| Surface Modifiers | PEG derivatives, cell-penetrating peptides, targeting ligands (e.g., bacteriophage tail proteins) | Enhanced penetration and targeting | Density of modification critical for function |
| Analytical Tools | Nanoparticle tracking analysis, quartz crystal microbalance, isothermal titration calorimetry | Quantifying NP-EPS interactions | Multiple complementary methods recommended |
| Visualization Agents | SYTO/Propidium iodide stains, fluorescent nanodiamonds, quantum dots | Penetration and distribution mapping | Photostability and size matching with therapeutic NPs |
Overcoming EPS barriers represents a critical challenge in advancing nanoparticle-mediated CRISPR-Cas9 delivery for biofilm eradication. The complex, multi-component nature of the EPS matrix requires sophisticated, multi-faceted approaches that address both physical and chemical barrier mechanisms. The integration of advanced material design with biological targeting strategies offers promising avenues for enhanced penetration and specificity.
Future developments in this field will likely focus on intelligent nanoparticle systems that dynamically respond to the biofilm microenvironment, combination therapies that simultaneously disrupt EPS structure and deliver precision genetic interventions, and personalized approaches that account for the unique EPS composition of clinical biofilm isolates. The continued refinement of experimental protocols and standardization of EPS models will accelerate the translation of these innovative strategies from laboratory research to clinical applications, ultimately addressing the significant challenge of biofilm-associated antimicrobial resistance.
The Clustered Regularly Interspaced Short Palindromic Repeats (CRISPR)/Cas9 system has revolutionized genetic engineering, offering unprecedented capability for precise genome manipulation. However, its therapeutic application, particularly in the context of nanoparticle-mediated delivery for biofilm eradication, faces a significant hurdle: off-target effects. These occur when the Cas9 nuclease cleaves DNA at unintended genomic sites with sequences similar to the intended target, potentially leading to adverse consequences including genotoxicity and oncogenesis [48] [49]. The challenge is compounded in biofilm environments, where efficient delivery is paramount. This Application Note details the sources of off-target activity and provides a structured framework of strategies to minimize these effects, ensuring the safety and efficacy of CRISPR-Cas9-based antimicrobial therapies.
Understanding the Mechanisms of Off-Target Effects
Off-target editing stems primarily from the tolerance of the Cas9-sgRNA complex for mismatches between the guide RNA and genomic DNA. Biochemical and structural studies reveal that this tolerance is influenced by several key factors:
- Mismatch Position and Type: Mismatches, especially in the PAM-distal region of the target site, are more readily tolerated than those closer to the Protospacer Adjacent Motif (PAM). The position and specific nucleotide combination of the mismatch significantly impact the likelihood of off-target cleavage [49].
- sgRNA Secondary Structure: The formation of secondary structures within the sgRNA itself can alter its binding affinity and specificity for the target DNA [49].
- Cellular Environment and Energetics: Factors such as local ion concentrations, chromatin accessibility, and the overall energetics of the RNA-DNA hybrid formation within the complex nuclear microenvironment influence off-target binding and cleavage events [48] [49].
- Enzyme Concentration: High intracellular concentrations of Cas9 protein can exacerbate off-target effects by increasing the probability of binding to lower-affinity, off-target sites [49].
Diagram: Mechanism of CRISPR-Cas9 Off-Target Effects. The diagram illustrates how the Cas9-sgRNA ribonucleoprotein (RNP) complex can lead to both on-target and off-target cleavage. Off-target effects are primarily driven by tolerated mismatches between the sgRNA and genomic DNA, a process influenced by multiple biochemical and cellular factors.
Strategic Framework for Minimizing Off-Target Effects
A multi-layered approach is required to ensure the precision of CRISPR-Cas9. The following strategies can be systematically implemented to significantly reduce off-target activity.
In Silico sgRNA Design and Prediction
The first line of defense is computational prediction and careful sgRNA selection.
- Principle: Utilize bioinformatic tools to nominate sgRNAs with high predicted on-target efficiency and low potential for off-target binding.
- Tools and Implementation: Several scoring-based algorithms are available. Cutting Frequency Determination (CFD) score is based on an experimentally validated dataset, while CCTop considers the distances of mismatches to the PAM for its predictions [48]. Tools like Cas-OFFinder allow for exhaustive searches with high tolerance for user-defined parameters, including sgRNA length, PAM type, and the number of mismatches or bulges [48].
- Application Note: For targeting bacterial biofilm resistance genes, screen candidate sgRNAs against the entire bacterial genome to identify sequences with minimal homology to non-target regions, especially other essential genes or regulatory elements.
Selection of High-Fidelity Cas9 Variants
Wild-type Cas9 can be replaced with engineered variants that exhibit enhanced specificity.
- Principle: These "high-fidelity" mutants, such as eSpCas9(1.1) and SpCas9-HF1, are engineered through structure-guided mutagenesis to weaken non-specific interactions between Cas9 and the DNA backbone, thereby enforcing stricter reliance on correct sgRNA-DNA pairing [49] [50].
- Protocol: When cloning your CRISPR construct, simply replace the gene for wild-type SpCas9 with the gene for a high-fidelity variant. Transfection and delivery protocols remain identical.
- Consideration for Nanoparticle Delivery: The protein size of these variants is similar to wild-type Cas9, posing no additional burden on nanoparticle packaging capacity [51].
RNP Delivery via Advanced Nanoparticles
The form of CRISPR-Cas9 delivery is a critical determinant of specificity.
- Principle: Direct delivery of the preassembled Cas9 protein and sgRNA complex, known as a Ribonucleoprotein (RNP), minimizes the time the nuclease is active in the cell, reducing the window for off-target events compared to plasmid DNA delivery, which leads to prolonged Cas9 expression [52] [50].
- Nanoparticle Protocol:
- Complex Formation: In vitro, pre-complex purified Cas9 protein with synthesized sgRNA at a optimal molar ratio (e.g., 1:2) to form the RNP.
- Nanoparticle Encapsulation: Encapsulate the RNP complex into your chosen nanoparticle system. Lipid nanoparticles (LNPs) and gold nanoparticles (AuNPs) have demonstrated high efficiency.
- Validation: Use gel electrophoresis or other biophysical methods to confirm successful RNP encapsulation and stability.
- Efficacy Data: Liposomal Cas9 RNP formulations have been shown to reduce Pseudomonas aeruginosa biofilm biomass by over 90% in vitro, while gold nanoparticle carriers can enhance editing efficiency up to 3.5-fold compared to non-carrier systems [2] [8].
Exploiting Natural Diversity: Cas9 Orthologs
The natural diversity of Cas9 proteins from different bacterial species offers a rich resource of enzymes with varying PAM requirements.
- Principle: Using Cas9 orthologs with longer or more complex PAM sequences (e.g., from S. thermophilus or G. stearothermophilus) drastically reduces the number of potential off-target sites in the genome, as the PAM becomes a more stringent recognition signal [53].
- Protocol:
- Selection: Bioinformatically identify an ortholog whose PAM sequence is present adjacent to your target site but is statistically rare in the rest of the genome.
- Cloning and Expression: Clone the ortholog's cas9 gene and its cognate tracrRNA sequence into your delivery system.
- Delivery: Co-deliver the ortholog Cas9 and its customized sgRNA as an RNP via nanoparticles for optimal activity.
- Advantage: A catalogue of 79 Cas9 orthologs revealed extraordinary diversity, with PAM requirements spanning T-, A-, C-, and G-rich sequences of varying lengths, providing a broad toolkit for precise targeting [53].
Experimental Detection and Validation of Off-Target Effects
Rigorous experimental validation is non-negotiable for therapeutic applications. The table below summarizes key quantitative detection methods.
Table 1: Methods for Experimental Detection of CRISPR-Cas9 Off-Target Effects
| Method | Principle | Key Advantages | Key Limitations | Suitable for Biofilm Models? |
|---|---|---|---|---|
| GUIDE-seq [48] | Integrates double-stranded oligodeoxynucleotides (dsODNs) into DSBs, followed by enrichment and sequencing. | Highly sensitive; cost-effective; low false positive rate. | Limited by transfection efficiency of dsODNs. | Moderate (requires efficient delivery into bacterial cells). |
| CIRCLE-seq [48] | Circularizes sheared genomic DNA, incubates with Cas9 RNP, and sequences linearized fragments. | Ultra-sensitive; works on purified DNA; does not require a reference genome. | In vitro method; may not reflect cellular chromatin context. | Yes (can be applied to purified bacterial DNA). |
| Digenome-seq [48] | Digests purified genomic DNA with Cas9 RNP in vitro, followed by whole-genome sequencing (WGS). | Highly sensitive; identifies cleavage sites without bias. | Expensive; requires high sequencing coverage and a reference genome. | Yes (can be applied to purified bacterial DNA). |
| qEva-CRISPR [54] | A ligation-based, quantitative method using multiplex ligation-based probe amplification (MLPA). | Detects all mutation types (indels, point mutations); multiplex capability; works in difficult genomic regions. | Requires prior knowledge of potential off-target sites for probe design. | Yes (if off-target sites are predicted). |
Diagram: Experimental Workflow for Off-Target Assessment. The flowchart outlines two primary pathways for detecting off-target effects: in vitro methods using purified DNA for unbiased discovery, and cell-based or in vivo methods that provide contextually relevant biological data.
The Scientist's Toolkit: Essential Reagents for Precision CRISPR-Cas9
Table 2: Key Research Reagent Solutions for Minimizing Off-Target Effects
| Reagent / Material | Function | Example & Notes |
|---|---|---|
| High-Fidelity Cas9 Variants | Engineered nuclease with stricter sgRNA-DNA pairing requirement. | eSpCas9(1.1), SpCas9-HF1. Use interchangeably with wild-type Cas9 in expression systems. |
| Cas9 Orthologs | Nuclease with divergent PAM requirement to reduce genomic target space. | S. thermophilus Cas9 (SthCas9), G. stearothermophilus Cas9 (GeoCas9). Require matching tracrRNA. |
| Lipid Nanoparticles (LNPs) | Non-viral vector for efficient RNP delivery; reduces off-target window. | Cationic/ionizable lipids (e.g., DOTAP). Can be functionalized for targeted delivery to biofilm cells [51] [52]. |
| Gold Nanoparticles (AuNPs) | Inorganic non-viral vector for RNP delivery. | Can enhance editing efficiency; surface can be modified with targeting ligands (e.g., peptides for bacterial attachment) [2] [51]. |
| Synthetic sgRNA | High-purity guide RNA for RNP assembly. | Chemically modified sgRNAs (e.g., 2'-O-methyl analogs) can improve stability and reduce immune responses in therapeutic contexts. |
| dsODN Tag (for GUIDE-seq) | Molecular tag for labeling and sequencing double-strand breaks in cells. | A short, double-stranded oligodeoxynucleotide that is integrated into DSBs. Essential reagent for the GUIDE-seq protocol [48]. |
Concluding Remarks
The successful and safe application of CRISPR-Cas9 in advanced therapies like nanoparticle-mediated biofilm eradication hinges on a rigorous, multi-faceted strategy to ensure precision. There is no single solution; rather, a combination of intelligent sgRNA design, the use of high-fidelity enzymes or orthologs, and transient RNP delivery via advanced nanoparticles forms the most robust foundation for minimizing off-target effects. This must be followed by comprehensive, experimentally validated off-target profiling using sensitive, unbiased methods. By systematically implementing the strategies and protocols outlined in this Application Note, researchers can significantly de-risk their therapeutic development pipeline and move closer to realizing the full clinical potential of CRISPR-Cas9 technology.
The convergence of nanoparticle (NP) technology with the CRISPR-Cas9 gene-editing system presents a transformative approach for combating biofilm-driven antibiotic-resistant infections. While this synergy enhances the delivery and efficacy of CRISPR-based antibacterials, the nanoscale properties that make NPs effective—high surface area to volume ratio and unique physicochemical characteristics—also necessitate a rigorous evaluation of their biocompatibility and long-term safety profiles [55]. The field of nanotoxicology is dedicated to this task, studying the potential toxicity of nanomaterials to ensure their safe application in medical and environmental contexts [55]. For research aimed at clinical translation, a systematic protocol for assessing nanotoxicity is not merely supplementary but foundational to developing safe and effective therapeutic platforms.
Key Nanotoxicity Assessment Methods
A comprehensive nanotoxicity assessment employs a combination of in vitro, in vivo, and in silico methods to evaluate biological interactions and toxic potential. The table below summarizes the key methods and their applications.
Table 1: Key Methods for Assessing Nanotoxicity
| Method Category | Specific Assay/Technique | Measured Endpoint | Application & Relevance |
|---|---|---|---|
| In Vitro | MTT Assay | Cell viability, metabolic activity | Initial screening for cytotoxicity in relevant cell lines (e.g., epithelial cells). |
| LDH Release Assay | Membrane integrity, cytotoxicity | Measures cell death and membrane damage caused by nanoparticle interactions. | |
| Comet Assay | DNA damage (genotoxicity) | Detects DNA strand breaks at the single-cell level. | |
| Micronucleus Assay | Chromosomal alterations | Assesses clastogenic and aneugenic effects leading to chromosomal damage. | |
| In Vivo | Rodent Studies (e.g., inhalation, injection) | Bioaccumulation, organ-specific toxicity (liver, kidneys, brain), long-term effects | Provides data on systemic toxicity in a whole organism; mimics real-world exposure routes. |
| Computational (In Silico) | Quantitative Structure-Activity Relationship (QSAR) | Toxicity prediction based on physicochemical properties | Uses descriptors like size, surface charge, and aggregation state to model and predict toxic potential, reducing animal testing. |
| Surface Characterization | Scanning Electron Microscopy (SEM) | Size, shape, surface morphology | Critical for characterizing the nanomaterial's physical state before testing. |
| Atomic Force Microscopy (AFM) | Surface roughness, stiffness, adhesion forces | Studies nanoparticle interactions with biological membranes under ambient or liquid conditions. | |
| X-ray Photoelectron Spectroscopy (XPS) | Elemental composition, oxidation states, surface chemistry | Analyzes surface coatings and functional groups that influence biological interactions. |
Experimental Protocols for Nanotoxicity Assessment
This section provides detailed, step-by-step protocols for critical nanotoxicity assays, adapted for evaluating nanoparticles used in CRISPR-Cas9 delivery.
Protocol for MTT Cytotoxicity Assay
Principle: Metabolically active cells reduce the yellow tetrazolium salt MTT (3-(4,5-dimethylthiazol-2-yl)-2,5-diphenyltetrazolium bromide) to purple formazan crystals. The amount of formazan produced is proportional to the number of viable cells.
Materials:
- Cell line relevant to exposure route (e.g., A549 for lung epithelium, Caco-2 for intestine)
- Nanoparticle suspension in appropriate medium (sterile)
- MTT reagent (e.g., 5 mg/mL in PBS)
- Cell culture medium and supplements
- Dimethyl sulfoxide (DMSO) or other solubilization buffer
- 96-well cell culture plate
- Multi-well plate spectrophotometer
Procedure:
- Cell Seeding: Seed cells in a 96-well plate at a density of (1 \times 10^4) cells per well in 100 µL of complete medium. Incubate for 24 hours (37°C, 5% CO₂) to allow cell attachment.
- Nanoparticle Exposure: Prepare a dilution series of the nanoparticle suspension. Remove the culture medium from the cells and replace it with 100 µL of medium containing nanoparticles. Include a negative control (medium only) and a positive control (e.g., a known cytotoxic agent). Use at least triplicates for each concentration.
- Incubation: Incubate the plate for the desired exposure period (e.g., 24 hours).
- MTT Incubation: Carefully remove the nanoparticle-containing medium. Add 110 µL of fresh medium containing 10 µL of MTT stock solution (5 mg/mL) to each well. Incubate for 2-4 hours.
- Solubilization: Carefully remove the MTT-containing medium. Add 100 µL of DMSO to each well to dissolve the formed formazan crystals. Gently shake the plate for 10-15 minutes.
- Absorbance Measurement: Measure the absorbance of each well at a wavelength of 570 nm, using a reference wavelength of 630-690 nm to correct for background.
- Data Analysis: Calculate the percentage of cell viability relative to the untreated control: (\text{% Viability} = (\text{Abs}{\text{sample}} / \text{Abs}{\text{control}}) \times 100).
Protocol for Alkaline Comet Assay for Genotoxicity
Principle: This sensitive technique detects DNA strand breaks at the level of a single cell. Under electrophoresis, damaged DNA migrates from the nucleus, forming a "comet tail," while intact DNA remains in the "head."
Materials:
- Trevigen CometAssay kit or equivalent components
- Normal melting point agarose (NMPA) and Low melting point agarose (LMPA)
- Lysis solution (e.g., 2.5 M NaCl, 100 mM EDTA, 10 mM Tris, 1% Triton X-100, pH 10)
- Alkaline electrophoresis solution (300 mM NaOH, 1 mM EDTA, pH >13)
- Neutralization buffer (0.4 M Tris, pH 7.5)
- Fluorescent DNA stain (e.g., SYBR Gold, Ethidium Bromide)
- Fully frosted microscope slides
- Electrophoresis tank and power supply
- Fluorescence microscope with image analysis software
Procedure:
- Slide Preparation: Coat slides with a layer of 1% NMPA and allow to dry.
- Cell Embedding: Mix treated cells with 1% LMPA (at 37°C) at a ratio of 1:10 (v/v). Pipette 100 µL of this mixture onto the pre-coated slide and immediately place a coverslip on top. Place slides on a flat surface at 4°C for 10-15 minutes to solidify.
- Lysis: Gently remove the coverslip and immerse the slides in a pre-chilled, freshly prepared lysis solution. Incubate at 4°C in the dark for a minimum of 1 hour (or overnight).
- Unwinding and Electrophoresis:
- Remove slides from lysis solution and gently place them in an electrophoresis tank filled with freshly prepared alkaline electrophoresis solution (pH >13).
- Allow DNA to unwind for 20-40 minutes in the solution.
- Perform electrophoresis at a fixed voltage (e.g., 1 V/cm) for 20-30 minutes, adjusted based on the amperage (typically ~300 mA).
- Neutralization and Staining:
- Carefully remove slides from the tank and neutralize by immersing in neutralization buffer for 5 minutes. Repeat this step three times.
- Dehydrate slides by immersing in 70% ethanol for 5 minutes and allow to air-dry.
- Stain DNA with an appropriate fluorescent dye and visualize using a fluorescence microscope.
- Analysis: Analyze at least 50-100 randomly selected cells per sample using image analysis software (e.g., OpenComet). The percentage of DNA in the tail is the primary metric for DNA damage.
Visualizing the Nanotoxicity Assessment Workflow
The following diagram illustrates the integrated workflow for assessing the safety of CRISPR-Cas9 nanoparticles, from material characterization to risk decision-making.
The Scientist's Toolkit: Essential Research Reagents & Materials
The table below catalogs key reagents and materials essential for conducting research on nanoparticle-mediated CRISPR-Cas9 delivery and its associated nanotoxicity assessments.
Table 2: Essential Research Reagents and Materials for NP-CRISPR Research
| Reagent/Material | Function/Application | Example & Notes |
|---|---|---|
| Cationic Lipids / Polymers | Formulation of lipid nanoparticles (LNPs); complex with negatively charged CRISPR components via electrostatic interactions. | Polyethyleneimine (PEI), Deoxycholic acid-modified PEI (PEI-DOCA) [56], ionizable lipids (e.g., DLin-MC3-DMA). Enable encapsulation and cellular uptake. |
| CRISPR-Cas9 Payload | The active gene-editing component. Can be delivered as plasmid DNA, mRNA, or Ribonucleoprotein (RNP). | Cas9 RNP is preferred for its rapid action and reduced off-target effects [56] [52]. Targeting biofilm genes (e.g., quorum sensing, antibiotic resistance genes) [2]. |
| Targeting Ligands | Enhances specificity of nanoparticles towards target cells or biofilms. | iRGD peptide [57], Hyaluronic Acid (HA) [57]. Surface modification improves tumor or biofilm targeting. |
| Fluorescent Dyes & Tags | Tracking nanoparticle uptake, biodistribution, and intracellular trafficking. | Conjugate with lipids or Cas9 protein. Used in conjunction with confocal laser scanning microscopy (CLSM) for visualization. |
| Standardized Assay Kits | Assessing cytotoxicity, genotoxicity, and other toxicological endpoints in vitro. | MTT, LDH, and Comet Assay kits provide standardized, reproducible protocols for nanotoxicity screening [58]. |
| Characterization Equipment | Determining the size, charge, and morphology of nanoparticles. Critical for quality control and understanding bio-interactions. | Dynamic Light Scattering (DLS) for size and zeta potential; SEM and AFM for high-resolution imaging [58]. |
For researchers developing nanoparticle-based CRISPR-Cas9 delivery systems against biofilms, a meticulous and multi-faceted approach to nanotoxicity is paramount. By integrating standardized in vitro and in vivo protocols with advanced computational and characterization tools, scientists can systematically unravel the complex interactions between nanomaterials and biological systems. This rigorous safety-by-design framework is not an obstacle but an essential enabler, ensuring that the immense therapeutic potential of this technology can be realized in a safe, effective, and clinically viable manner.
The escalating crisis of antibiotic-resistant biofilm-driven infections necessitates the development of next-generation antimicrobial strategies. The CRISPR-Cas9 gene-editing system has emerged as a revolutionary tool for the precise targeting of bacterial antibiotic resistance genes and biofilm-regulating factors [2]. However, the clinical translation of CRISPR-based antibacterials is critically limited by challenges in delivery efficiency and stability within bacterial populations [2] [8]. Nanoparticles (NPs) present an innovative solution, serving as effective carriers for CRISPR/Cas9 components while often exhibiting intrinsic antibacterial properties [2]. These hybrid systems can enhance cellular uptake, increase target specificity, and ensure controlled release within the challenging biofilm microenvironment [2]. Recent advances demonstrate that liposomal CRISPR-Cas9 formulations can reduce Pseudomonas aeruginosa biofilm biomass by over 90% in vitro, while gold nanoparticle carriers can enhance editing efficiency up to 3.5-fold compared to non-carrier systems [2]. The synergy of CRISPR and nanoparticle technologies holds immense potential for developing precision antimicrobial therapies; however, their clinical success is fundamentally dependent on overcoming scalability and manufacturing hurdles to achieve reproducible, high-quality formulations [2] [59].
Quantitative Analysis of CRISPR-Nanoparticle Platforms
The selection of an appropriate nanoparticle platform is critical for balancing editing efficiency, cargo capacity, scalability, and biocompatibility. Different nanoparticle systems offer distinct advantages and limitations for CRISPR delivery, influencing their suitability for industrial-scale manufacturing and therapeutic application against biofilms.
Table 1: Comparison of CRISPR-Nanoparticle Delivery Platforms for Biofilm Applications
| Platform | Typical Cargo Format | Key Advantages | Manufacturing & Scalability Considerations | Reported Efficacy Against Biofilms |
|---|---|---|---|---|
| Lipid Nanoparticles (LNPs) | RNP, mRNA, DNA [ [28] [59]] | High encapsulation efficiency; clinical validation; potential for organ-targeting [ [28]] | Scalable microfluidic mixing; chemically defined composition; requires strict control of PEG-lipid concentration [ [59]] | >300-fold enhancement in editing efficiency in vivo with optimized RNP-LNPs [ [59]] |
| Gold Nanoparticles (AuNPs) | RNP, DNA [ [2]] | Facile surface functionalization; high stability; enhanced editing efficiency [ [2]] | Reproducible synthesis; tunable size and surface chemistry; potential for conjugation with targeting ligands | 3.5-fold increase in gene-editing efficiency compared to non-carrier systems [ [2]] |
| Virus-Like Particles (VLPs) | RNP [ [28] [59]] | Transient delivery; no viral genome integration; intrinsic cell/tissue tropism [ [28]] | Complex manufacturing; cargo size limitations; challenges in large-scale production and stability [ [28]] | Effective precision correction in animal models; suitable for in vivo editing [ [59]] |
| Lipoplexes/Polyplexes | DNA, RNP [ [28]] | Simplicity of formulation; lower immunogenicity than viral vectors [ [28]] | Variable transfection efficiency; challenges with endosomal escape and nuclear access [ [28]] | Data specific to biofilm eradication is less established; primarily used for in vitro research |
Protocol: Reproducible Synthesis of CRISPR RNP-LNPs
This protocol details the optimized, reproducible synthesis of Lipid Nanoparticles (LNPs) encapsulating CRISPR ribonucleoproteins (RNPs) based on recent advancements in the field [59]. The use of RNPs is preferred over DNA or mRNA cargo due to their rapid onset and short duration of activity, minimizing off-target effects and immunological concerns [28] [59].
Materials and Reagents
Table 2: Essential Research Reagent Solutions for LNP Formulation
| Reagent/Solution | Function/Description | Critical Parameters |
|---|---|---|
| Ionizable Lipid (e.g., SM102) | Structural component; enables encapsulation and endosomal escape [ [59]] | pKa > 6; identified via screening for enhanced RNP delivery [ [59]] |
| DMG-PEG 2000 | Polyethylene glycol-lipid; confers stability and reduces opsonization [ [59]] | Concentration must be optimized for RNP stability and editing potency [ [59]] |
| Purified Base Editor or Prime Editor RNP | Active CRISPR editing complex [ [59]] | Complex pre-assembled with sgRNA; stabilized with 10% (w/v) sucrose [ [59]] |
| Aqueous Phase Buffer (e.g., Citrate Buffer, pH 4.0) | Hydrates the lipid film; creates acidic environment for lipid ionization | pH critical for initial solubility of ionizable lipids |
| Microfluidic Mixing Device | Enables precise, reproducible nanoprecipitation | Fixed total flow rate and flow rate ratio (FRR) determine LNP size and PDI |
Step-by-Step Procedure
- Lipid Solution Preparation: Dissolve the lipid mixture (ionizable lipid, phospholipid, cholesterol, and DMG-PEG 2000) in ethanol at a defined molar ratio. The optimal concentration of DMG-PEG 2000 must be determined empirically for each RNP type to balance stability and delivery efficiency [59].
- Aqueous Phase Preparation: Dilute the purified, pre-assembled RNP complex (e.g., ABE8e or PE2 complexed with sgRNA) into a citrate buffer (pH 4.0). The RNP should be refolded by heating and slow cooling to maximize stability prior to formulation [59].
- Microfluidic Mixing: Load the lipid and aqueous solutions into separate syringes on a microfluidic mixer. Use a fixed total flow rate and a flow rate ratio to initiate nanoprecipitation. The laminar flow within the device's channels ensures rapid and uniform mixing, leading to the self-assembly of LNPs with the RNP cargo encapsulated.
- Buffer Exchange and Purification: Dialyze or use tangential flow filtration (TFF) against a large volume of PBS (pH 7.4) to remove the ethanol and exchange the buffer. This step is critical for LNP stability and biocompatibility.
- Characterization and Quality Control: Determine the particle size, polydispersity index (PDI), and zeta potential using dynamic light scattering (DLS). Measure encapsulation efficiency using a Ribogreen assay. Verify that the process yields LNPs with a size of 70-100 nm and a PDI of <0.2, indicating a monodisperse population suitable for in vivo applications.
Protocol: Experimental Workflow for Anti-Biofilm Efficacy Testing
Validating the efficacy of CRISPR-NP formulations requires a standardized biofilm assay. The following protocol outlines the steps for testing formulations against established biofilm models, such as those formed by P. aeruginosa.
Materials and Reagents
- Bacterial Strain: e.g., Pseudomonas aeruginosa (PAO1 or clinical isolate).
- Growth Medium: Tryptic Soy Broth (TSB) or Lysogeny Broth (LB).
- 96-well Polystyrene Plate: For static biofilm cultivation.
- CRISPR-NP Formulation: Prepared as in Section 3, resuspended in PBS.
- Control Groups: Include untreated biofilm, naked RNP, and empty NPs.
- Staining Solution: 0.1% Crystal Violet (CV) solution or live/dead viability stains.
- Microplate Spectrophotometer.
Step-by-Step Procedure
- Biofilm Cultivation: Grow an overnight culture of the target bacterium. Dilute the culture 1:100 in fresh medium and aliquot 200 µL per well into a 96-well plate. Incubate statically for 24-48 hours at 37°C to allow biofilm formation.
- Treatment Application: Carefully remove the planktonic culture and wash the established biofilm gently with PBS. Add 200 µL of the CRISPR-NP formulation (at the desired concentration in medium) to the test wells. Include all relevant controls.
- Incubation and Exposure: Incubate the plate under static conditions for a defined period (e.g., 4-24 hours).
- Biofilm Biomass Quantification (Crystal Violet Assay):
- a. After treatment, remove the medium and wash the biofilm with PBS.
- b. Fix the biofilm with 200 µL of 99% methanol for 15 minutes, then discard.
- c. Air-dry the plate completely.
- d. Stain the biofilm with 200 µL of 0.1% crystal violet for 15 minutes.
- e. Wash the plate thoroughly with water to remove unbound dye.
- f. Elute the bound dye with 200 µL of 33% acetic acid.
- g. Measure the absorbance at 595 nm. A reduction in absorbance of >90% indicates highly effective biofilm disruption [2].
- Data Analysis: Calculate the percentage of biofilm reduction relative to the untreated control. Use statistical analysis (e.g., Student's t-test) to confirm significance.
The path to clinical translation of CRISPR-NP formulations for biofilm eradication hinges on overcoming manufacturing challenges. The protocols outlined herein for RNP-LNP synthesis and efficacy testing provide a foundation for reproducible production. Key to scalability is the adoption of chemically defined components and scalable processes like microfluidic mixing, which ensure batch-to-batch consistency [59]. Future efforts must focus on optimizing long-term storage stability, establishing comprehensive safety and toxicology profiles, and implementing rigorous quality-by-design (QbD) principles to navigate the regulatory pathway successfully. By addressing these scalability and manufacturing challenges, CRISPR-nanoparticle hybrids can transition from a powerful research tool to a transformative clinical therapy for resistant biofilm infections.
Regulatory and Ethical Considerations for Novel Genomic Antimicrobials
The emergence of nanoparticle-delivered CRISPR-Cas9 systems represents a paradigm shift in antimicrobial therapy, particularly for combating biofilm-associated infections. These advanced therapeutic products (ATPs), which combine gene-editing machinery with nanoscale delivery platforms, challenge existing regulatory frameworks and raise significant ethical considerations [2] [60]. The global antimicrobial resistance (AMR) crisis demands urgent innovation, with AMR projected to cause 10 million deaths annually by 2050 and create substantial economic burdens, including potential GDP reductions of 1.1%-3.8% and increased extreme poverty affecting 28.3 million people, primarily in low-income countries [61] [62]. This application note examines the current regulatory pathways and ethical imperatives for researchers developing these novel genomic antimicrobials, providing a structured framework for navigating the complex transition from laboratory research to clinical application.
Regulatory Landscape
Global Regulatory Classification and Pathways
Nanoparticle-delivered CRISPR-Cas9 antimicrobials occupy a complex regulatory space, typically classified as either advanced therapy medicinal products (ATMPs) or combination products depending on their primary mechanism of action. Regulatory agencies primarily categorize these products based on whether they function primarily through pharmacological, immunological, or metabolic means (medicinal products) or through physical/mechanical actions (medical devices) [60].
Table 1: Comparative Regulatory Frameworks for Genomic Antimicrobials
| Regulatory Aspect | European Union (EU) | United States (US) |
|---|---|---|
| Primary Legislation | Directive 2001/83/EC [60] | Federal Food, Drug, and Cosmetic Act [60] |
| Leading Authority | European Medicines Agency (EMA) [60] | Food and Drug Administration (FDA) [60] |
| Product Classification | Advanced Therapy Medicinal Products (ATMPs) [60] | Combination Products/Biologics [60] |
| Key Considerations | Quality, safety, efficacy; Nanospecific characterization [60] | Safety, effectiveness; Chemistry, manufacturing, controls (CMC) [60] |
The regulatory navigation for these products remains complex and often lags behind technological advancements, creating significant barriers to clinical application. Researchers must anticipate that regulators will require comprehensive data on quality, safety, and efficacy, with particular emphasis on the unique aspects of both the nanotechnology component and the gene-editing functionality [60].
Technical Characterization Requirements
Robust physicochemical and biological characterization forms the foundation of regulatory submissions for CRISPR-nanoparticle antimicrobials. Key parameters requiring thorough evaluation include:
Nanoparticle Characterization: Size distribution, surface charge (zeta potential), morphology, composition, stability, and drug loading/release profile [60] [19]. The high surface-to-volume ratio of nanomaterials exponentially increases their reactivity, necessitating careful evaluation of interactions with biological systems [60].
CRISPR Component Analysis: Guide RNA specificity, Cas enzyme activity, off-target editing potential, and delivery efficiency [2]. Recent advances have demonstrated that liposomal CRISPR-Cas9 formulations can reduce Pseudomonas aeruginosa biofilm biomass by over 90% in vitro, while gold nanoparticle carriers enhance editing efficiency up to 3.5-fold compared to non-carrier systems [2] [8].
Biological Performance: Biofilm penetration capability, bacterial uptake efficiency, resistance gene disruption efficacy, and resensitization to conventional antibiotics [2]. The combination of CRISPR-Cas9 with nanoparticles enables co-delivery with antibiotics, producing synergistic antibacterial effects and superior biofilm disruption [2].
Ethical Framework
Core Ethical Considerations
The development of CRISPR-based antimicrobials introduces several unique ethical dimensions that extend beyond conventional antibiotic development:
Environmental Impact and Gene Drive Potential: Unintended environmental release of CRISPR components could potentially propagate resistance genes through horizontal gene transfer [63]. The One Health framework emphasizes the interconnectedness of human, animal, and environmental health, highlighting the importance of containing gene-editing systems within target pathogens [63].
Equitable Access and Benefit Sharing: These advanced therapies risk becoming premium-priced treatments, potentially inaccessible in low-income countries where the AMR burden is most severe [61] [62]. Genuine partnerships for access to biodiversity and sharing of benefits accrued require a consideration of ethical practice and behavior [62].
Microbial Biodiversity and Bioprospecting Ethics: Research and development often requires access to microbial biodiversity, where the custodians of that biodiversity—and the traditional knowledge required to access it—must be recognized as key partners [62].
Table 2: Ethical Assessment Framework for Genomic Antimicrobial Development
| Ethical Dimension | Key Considerations | Risk Mitigation Strategies |
|---|---|---|
| Environmental Safety | Horizontal gene transfer, ecological impact [63] | Containment systems, kill switches, environmental risk assessments [63] |
| Social Justice | Equitable access, affordability [61] [62] | Tiered pricing, technology transfer, capacity building in LMICs [61] [62] |
| Benefit Sharing | Traditional knowledge, biodiversity use [62] | Ethical bioprospecting agreements, fair benefit sharing [62] |
| Antimicrobial Stewardship | Resistance development, appropriate use [61] | Diagnostic companions, use restriction protocols, stewardship programs [61] |
Community Engagement and Intersectionality
Responsive development of these technologies requires meaningful community engagement and consideration of intersectionality—how various forms of social stratification such as race, gender, and class interconnect to create unique modes of oppression and privilege in healthcare access [62]. The COVID-19 pandemic revealed significant disparities in how vulnerable communities experienced and accessed emerging health technologies, with Black, Indigenous, and People of Color (BIPOC) communities experiencing disproportionately severe outcomes due to long-standing systemic inequities [62]. Without major behavior change and equitable implementation strategies, these disparities are likely to persist with advanced AMR treatments [62].
Experimental Protocols
Regulatory-Grade Nanoparticle Characterization Protocol
Objective: To comprehensively characterize nanoparticle-CRISPR formulations for regulatory submission.
Materials:
- Dynamic Light Scattering (DLS) Instrument: For hydrodynamic diameter and size distribution [60]
- Zeta Potential Analyzer: For surface charge measurement [60]
- Transmission Electron Microscopy (TEM): For morphological analysis [60]
- UV-Vis Spectrophotometry: For concentration determination and purity assessment [60]
- HPLC System: For encapsulation efficiency and release kinetics [60]
Procedure:
- Size and Distribution Analysis: Dilute nanoparticle formulation in appropriate buffer (1:100 v/v) and measure hydrodynamic diameter via DLS. Perform triplicate measurements at 25°C [60].
- Surface Charge Determination: Measure zeta potential using electrophoretic light scattering. Report average of 5 measurements with standard deviation [60].
- Morphological Examination: Prepare TEM samples by negative staining with 1% uranyl acetate. Image at minimum 100 randomly selected particles [60].
- Encapsulation Efficiency: Separate free CRISPR components using size exclusion chromatography. Quantify encapsulated fraction via fluorescence or HPLC [60].
- Release Kinetics: Dialyze formulation against PBS (pH 7.4) at 37°C with gentle agitation. Sample at predetermined intervals (1, 2, 4, 8, 12, 24, 48h) and quantify released content [60].
Biofilm Eradication Assessment Protocol
Objective: To evaluate the efficacy of nanoparticle-delivered CRISPR-Cas9 against biofilm-forming pathogens.
Materials:
- CRISPR-Nanoparticle Formulation: Liposomal or gold nanoparticle-based Cas9-sgRNA complexes [2]
- Biofilm Reactor System: Flow cell or Calgary biofilm device [2]
- Confocal Laser Scanning Microscopy (CLSM): For biofilm structural analysis [2]
- Viability Stains: SYTO9/propidium iodide or resazurin [2]
- qPCR Equipment: For resistance gene expression analysis [2]
Procedure:
- Biofilm Formation: Grow standardized biofilms of target pathogen (e.g., P. aeruginosa, A. baumannii) for 48-72h under appropriate conditions [2].
- Treatment Application: Apply CRISPR-nanoparticle formulations at varying concentrations (0.1-100 μg/mL) to established biofilms. Include appropriate controls (untreated, nanoparticle-only, free CRISPR) [2].
- Viability Assessment: Post-treatment (24h), stain biofilms with viability markers and quantify live/dead cells via CLSM or fluorometry [2].
- Biomass Quantification: Measure total biofilm biomass using crystal violet staining or protein quantification [2].
- Gene Editing Confirmation: Extract genomic DNA from treated biofilms and assess target gene modification via sequencing or restriction fragment length polymorphism [2].
- Antibiotic Resensitization: Challenge treated biofilms with conventional antibiotics and determine MIC reduction [2].
Biofilm Efficacy Assessment Workflow
The Scientist's Toolkit
Table 3: Essential Research Reagents for CRISPR-Nanoparticle Antimicrobial Development
| Reagent/Material | Function | Specific Examples |
|---|---|---|
| Lipid Nanoparticles | CRISPR component delivery [2] [64] | POZ-lipid technology (non-immunogenic), PEGylated lipids, ionizable lipids [64] |
| Metallic Nanoparticles | Enhanced editing efficiency [2] | Gold nanoparticles (3.5x efficiency increase) [2] |
| Cas9 Enzymes | Target gene cleavage [2] [65] | S. pyogenes Cas9 (SpCas9), codon-optimized variants [65] |
| Guide RNA Constructs | Target specificity [2] [65] | sgRNA targeting antibiotic resistance genes (e.g., blaNDM-1, mecA) [2] [63] |
| Biofilm Reactors | In vitro biofilm models [2] | Flow cells, Calgary biofilm devices [2] |
| Characterization Instruments | Nanoparticle physicochemical analysis [60] | DLS, zeta potential analyzers, TEM [60] |
Environmental and Safety Assessment
The One Health approach recognizes that antimicrobial resistance impacts human, animal, and environmental health through interconnected pathways [63]. CRISPR-based antimicrobials require thorough environmental risk assessment as part of regulatory submissions:
Horizontal Gene Transfer Assessment: Evaluate potential for gene-editing components to transfer to environmental microorganisms using conjugation assays and genomic integration tests [63].
Ecological Impact Studies: Assess effects on beneficial microbiota and ecosystem function through microcosm studies and metabolic profiling [63].
Environmental Persistence: Determine degradation kinetics of nanoparticle components and CRISPR machinery under relevant environmental conditions [63].
Advanced genomic tools like whole-genome sequencing (WGS) and metagenomics provide powerful methods for tracking resistance genes and assessing ecological impacts across One Health domains [63].
One Health Approach to AMR
The development of nanoparticle-delivered CRISPR-Cas9 antimicrobials represents a cutting-edge approach to addressing the global AMR crisis. Navigating the regulatory landscape requires careful attention to product classification, comprehensive characterization, and thorough safety assessment. Ethical development demands consideration of environmental impact, equitable access, and community engagement. By integrating these regulatory and ethical frameworks during early research stages, scientists can accelerate the translation of these promising technologies into clinically effective treatments while maintaining public trust and ensuring responsible innovation.
Assessing Efficacy and Advantage: In Vitro, In Vivo, and Comparative Analyses
Within the burgeoning field of novel antimicrobial strategies, the combination of CRISPR-Cas9 gene-editing technology with nanoparticle-based delivery systems presents a promising approach for eradicating biofilm-associated infections. A critical component of this research is the accurate and standardized quantification of treatment efficacy. Assessing both the physical destruction of the biofilm structure and the resulting loss of bacterial viability is essential for validating new therapeutic platforms. This application note details established and emerging metrics for evaluating biofilm biomass and bacterial viability, providing a critical toolkit for researchers developing nanoparticle-delivered CRISPR-Cas9 anti-biofilm therapies.
Quantitative Metrics for Biofilm Biomass
Biofilm biomass encompasses the total accumulated material, including bacterial cells and the protective extracellular polymeric substance (EPS). The following table summarizes key quantitative methods for its assessment.
Table 1: Methods for Quantifying Biofilm Biomass
| Method | Principle | Output Metric | Key Advantages | Key Limitations |
|---|---|---|---|---|
| Crystal Violet (CV) Staining | Stains total biomass (cells and EPS) adhered to a surface [66] [34]. | Optical Density (OD) of dissolved stain [67]. | High-throughput, low-cost, simple protocol [34]. | Does not distinguish between live and dead cells [66] [34]. |
| Scanning Electron Microscopy (SEM) | High-resolution imaging of biofilm surface topography and ultrastructure [2] [67]. | Qualitative and semi-quantitative image analysis of biofilm surface area and structure [67]. | Provides detailed topographical and structural information [2]. | Requires extensive sample preparation; mostly qualitative [34]. |
| Confocal Laser Scanning Microscopy (CLSM) | Optical sectioning of live/dead stained biofilms to create 3D reconstructions [68] [67]. | Biovolume (µm³), thickness (µm), surface coverage (%) [68]. | Provides 3D structural data on intact biofilms; can couple structure with viability [68]. | Requires access to specialized, expensive equipment [34]. |
| Quartz Crystal Microbalance (QCM) | Measures mass change (including bound water) on a vibrating sensor surface [34]. | Frequency/ dissipation shift (Hz) correlated to mass (ng/cm²) [34]. | Label-free, real-time monitoring of biofilm formation and removal. | Measures wet mass, including hydrodynamically coupled water [34]. |
Quantitative Metrics for Bacterial Viability
Viability assays measure the metabolic activity or reproductive capacity of bacteria within a biofilm, which is the ultimate indicator of antimicrobial success.
Table 2: Methods for Quantifying Bacterial Viability
| Method | Principle | Output Metric | Key Advantages | Key Limitations |
|---|---|---|---|---|
| Colony Forming Unit (CFU) Enumeration | Culture and count of viable, cultivable bacteria from homogenized biofilms [34] [68] [67]. | CFU/mL or log10 CFU/mL [68] [67]. | Direct measure of cultivable bacteria; considered a gold standard [34]. | Time-consuming (24-72 hrs); misses viable but non-culturable (VBNC) cells [34]. |
| Resazurin / XTT Assay | Measures metabolic activity via reduction of a resazurin (blue) to resorufin (pink/fluorescent) [66]. | Fluorescence or Absorbance units. | High-throughput; measures metabolic activity. | Can overestimate viability if a small population is highly active [66]. |
| Flow Cytometry | Laser-based counting and characterization of individual cells stained with viability markers (e.g., PI) [34] [69]. | Percentage of live/dead cells; total cell count [69]. | Rapid, highly quantitative, and can analyze thousands of cells per second [34]. | Requires biofilm homogenization into single-cell suspension; expensive instrument [34]. |
| LIVE/DEAD Staining with CLSM | Uses membrane-integrity dyes (e.g., SYTO9 for live, PI for dead cells) and confocal microscopy [67]. | Percentage of live/dead cells; 3D spatial distribution of viability [67]. | Visually couples viability data with 3D spatial location in the biofilm [67]. | Semi-quantitative without advanced image analysis; can be dye penetration issues [34]. |
Experimental Protocols for Key Assays
This protocol is ideal for high-throughput screening of anti-biofilm treatments, such as the efficacy of different CRISPR-NP formulations.
- Biofilm Formation: Grow biofilms in a 96-well microtiter plate under optimal conditions for the target organism (e.g., 37°C for 24-48 hrs).
- Treatment: Aspirate the planktonic culture and treat the adhered biofilms with your CRISPR-NP complexes. Include appropriate controls (e.g., naked nanoparticles, free CRISPR, scramble gRNA).
- Fixing and Staining:
- Wash the wells gently with phosphate-buffered saline (PBS) to remove non-adherent cells.
- Fix the biofilms by adding 100-200 µL of methanol or 99% ethanol per well for 15 minutes.
- Aspirate the fixative and air-dry the plates.
- Stain each well with 0.1% (w/v) crystal violet solution (100-150 µL) for 15-20 minutes at room temperature.
- Destaining and Quantification:
- Wash the plates thoroughly under running tap water to remove unbound dye. Invert and tap to dry.
- Add 100-200 µL of 95% ethanol or 33% acetic acid to each well to solubilize the bound dye.
- Incubate for 10-15 minutes with gentle shaking.
- Transfer 100 µL of the solubilized dye to a new well or measure the optical density directly at 570 nm or 600 nm using a microplate reader.
This protocol provides a direct count of viable bacteria remaining after treatment.
- Biofilm Treatment: Grow and treat biofilms in a suitable vessel (e.g., 12-well plate, silicone tube model [67]).
- Biofilm Harvesting:
- After treatment, gently rinse the biofilm with PBS to remove the treatment solution.
- Add a known volume of sterile PBS or saline to the biofilm.
- Dislodge the biofilm by vigorous scraping with a sterile pipette tip or cell scraper. For more robust biofilms, sonicate in a water bath for 5-30 minutes followed by vortexing for 1-3 minutes to homogenize the sample [67].
- Serial Dilution and Plating:
- Perform a 10-fold serial dilution of the homogenized biofilm suspension in sterile saline or PBS.
- Plate 100 µL aliquots from appropriate dilutions (e.g., 10⁻¹ to 10⁻⁵) onto nutrient-rich agar plates (e.g., Tryptic Soy Agar).
- Spread the aliquot evenly across the agar surface using a sterile spreader.
- Incubation and Counting:
- Invert the plates and incubate at the organism's optimal temperature (e.g., 37°C) for 24-48 hours.
- Count the colonies on plates that contain between 30 and 300 colonies.
- Calculate the CFU per mL of the original biofilm suspension using the following formula:
CFU/mL = (Number of colonies counted × Dilution Factor) / Volume plated (mL) - Data is often presented as log10 CFU/mL for statistical analysis [68].
The Scientist's Toolkit: Research Reagent Solutions
Table 3: Essential Reagents and Materials for Biofilm Quantification
| Reagent / Material | Function | Example Application |
|---|---|---|
| Crystal Violet Solution | Total biomass staining. | Quantifying the reduction in biofilm matrix after NP-CRISPR treatment [66] [67]. |
| LIVE/DEAD BacLight Kit | Two-color fluorescence staining of bacterial viability based on membrane integrity. | Differentiating between bactericidal and biofilm-disrupting effects of treatment via CLSM [67]. |
| Resazurin Sodium Salt | Cell-permeant dye used to measure metabolic activity. | High-throughput screening of antimicrobial efficacy against biofilm cells [66]. |
| 96-well Microtiter Plates | Standard platform for biofilm growth and high-throughput assays. | CV staining, resazurin assays, and initial biofilm formation models [66] [34]. |
| Transwell Co-culture Systems | Allows spatial separation of test agents (e.g., MSCs) from biofilms while permitting molecular diffusion. | Studying the effect of secreted factors or indirect mechanisms of action [70]. |
| Silicone Tubing & Flow Cells | Creates dynamic, shear-stress biofilm models that mimic medical devices and in-vivo conditions. | Testing NP-CRISPR efficacy under more clinically relevant, flow-induced biofilm conditions [67]. |
Experimental Workflow for Evaluating NP-CRISPR Anti-biofilm Therapy
The following diagram illustrates the logical workflow for quantifying the success of a nanoparticle-delivered CRISPR-Cas9 anti-biofilm treatment, integrating the metrics and protocols described above.
The escalating global health crisis of antibiotic-resistant infections is driven significantly by bacterial biofilms. These structured microbial communities, encapsulated in a protective extracellular polymeric substance (EPS), can exhibit up to 1000-fold greater tolerance to antibiotics compared to their planktonic counterparts [13]. This recalcitrance makes biofilm-associated infections notoriously difficult to treat with conventional antimicrobials, necessitating the development of novel therapeutic strategies [8] [13].
The CRISPR-Cas9 gene-editing system has emerged as a revolutionary tool for precision targeting of bacterial virulence factors. By designing guide RNAs (gRNAs) specific to essential genes, this technology can disrupt antibiotic resistance genes, quorum-sensing pathways, and biofilm-regulating factors, thereby resensitizing bacteria to treatment [8] [13]. However, the clinical translation of CRISPR-based antimicrobials is hampered by significant delivery challenges, including poor cellular uptake, susceptibility to nuclease degradation, and limited stability within complex biofilm matrices [8] [71].
Lipid-based nanoparticles (LNPs), particularly liposomal formulations, present an innovative solution to these barriers. These nanoparticles serve as effective carriers for the Cas9 nuclease and its guide RNA, protecting the genetic payload and enhancing its delivery to bacterial cells within the biofilm [71] [72]. Recent advances demonstrate the powerful synergy of this hybrid approach, with liposomal Cas9 formulations reducing Pseudomonas aeruginosa biofilm biomass by over 90% in vitro [8] [13]. This application note details the protocols and key considerations for replicating these findings, providing a framework for in vitro validation of CRISPR-nanoparticle platforms for biofilm eradication.
The integration of CRISPR-Cas9 with nanoparticle delivery systems represents a paradigm shift in antimicrobial therapy. The quantitative outcomes of key experiments are summarized in the table below.
Table 1: Summary of Key Experimental Findings for CRISPR-Nanoparticle Biofilm Eradication
| CRISPR Component | Nanoparticle Carrier | Target Bacteria | Key Experimental Outcome | Efficiency Compared to Control |
|---|---|---|---|---|
| Cas9 + sgRNA (targeting biofilm genes) | Liposomal nanoparticles | Pseudomonas aeruginosa | >90% reduction in biofilm biomass [8] [13] | Significantly superior to non-carrier systems |
| Cas9 + sgRNA | Gold Nanoparticles | P. aeruginosa & other models | Up to 3.5-fold increase in gene-editing efficiency [8] [13] | Enhanced delivery and biofilm penetration |
| Cas9 mRNA + sgRNA | Ionizable Lipid Nanoparticles (1A14-iLNP) | HeLa-EGFP cells (model system) | ~70% EGFP knockout efficiency [72] | Demonstrates high potency of optimized LNPs |
These findings underscore the critical role of the nanoparticle carrier. Gold nanoparticles enhance editing efficiency by improving cellular uptake and target specificity, while liposomal formulations excel at disrupting the mature biofilm structure. The development of advanced ionizable lipids, such as the 1A14-iLNP with a spermine head group, further pushes the boundaries of delivery efficacy, achieving high levels of gene disruption in eukaryotic cells [72]. The synergy of this combined approach is illustrated below.
The Scientist's Toolkit: Essential Research Reagents
To replicate the described experiments, a specific set of reagents and materials is required. The following table catalogues the essential components for formulating liposomal Cas9 and conducting in vitro biofilm assays.
Table 2: Key Research Reagent Solutions for Liposomal Cas9 Biofilm Studies
| Reagent/Material | Function/Application | Specific Example / Rationale |
|---|---|---|
| Cationic/Ionizable Lipids | Forms core of LNP, complexes with nucleic acids, enables endosomal escape. | Spermine-head lipids (e.g., 1A14) show high efficacy for Cas9 mRNA delivery [72]. |
| Helper Lipids (DOPE, Cholesterol) | Stabilizes LNP structure, enhances membrane fusion and fluidity. | DOPE (1,2-dioleoyl-sn-glycero-3-phosphoethanolamine) is commonly used [72]. |
| PEGylated Lipids (DMG-PEG2000) | Provides "stealth" properties, improves nanoparticle stability and circulation time. | DMG-PEG2000 (1,2-dimyristoyl-rac-glycero-3-methoxy-polyethylene glycol-2000) [72]. |
| CRISPR-Cas9 Payload | Executes targeted gene editing. | Cas9 protein + sgRNA complexes (RNPs) for immediate activity; or Cas9 mRNA + sgRNA for sustained expression. |
| Biofilm Growth Media | Supports robust and reproducible biofilm formation in vitro. | Tryptic Soy Broth (TSB) supplemented with 1% glucose (TSG) is widely used for optimal growth [73]. |
| Resazurin Dye | Assesses metabolic activity and viability of biofilm cells post-treatment. | Used in Minimum Biofilm Inhibitory Concentration (MBIC) assays; concentration at 4-8 μg/mL is typical [73]. |
| Crystal Violet (CV) Stain | Quantifies total biofilm biomass (living and dead cells). | Standard protocol for staining adherent biomass in microtiter plates [74] [73]. |
Detailed Experimental Protocol
Liposomal Cas9 Formulation Preparation
This protocol outlines the preparation of liposomal nanoparticles for the co-delivery of Cas9 ribonucleoprotein (RNP).
Step 1: Lipid Mixture Preparation
- Combine cationic/ionizable lipids, helper lipids (DOPE, cholesterol), and PEG-lipid (e.g., DMG-PEG2000) in a molar ratio of 50:10:38.5:1.5 [72].
- Dissolve the lipid mixture in an organic solvent (e.g., ethanol) to create a homogeneous solution.
Step 2: Aqueous Phase Preparation
Step 3: Nanoparticle Formation
- Use microfluidics or rapid mixing techniques to combine the aqueous and lipid phases under controlled conditions.
- This process facilitates the self-assembly of lipids into nanoparticles encapsulating the Cas9 RNP payload.
Step 4: Buffer Exchange and Purification
- Dialyze the formed LNPs against phosphate-buffered saline (PBS) at pH 7.4 to remove organic solvent and unencapsulated components.
- Sterilize the final formulation by passing it through a 0.22 μm filter.
- Store the prepared liposomal Cas9 at 4°C for short-term use or at -80°C following lyophilization with cryoprotectants like sucrose for long-term stability [72].
In Vitro Biofilm Cultivation and Treatment
A standardized biofilm model is critical for consistent and interpretable results. The workflow below outlines the key stages from cultivation to analysis.
Step 1: Biofilm Cultivation
- Prepare an overnight culture of the target bacterium (e.g., P. aeruginosa PAO1) in a suitable broth like Tryptic Soy Broth (TSB).
- Dilute the culture to ~1x10^6 CFU/mL in TSB supplemented with 1% glucose (TSG) to promote robust biofilm formation [73].
- Dispense 200 μL of the bacterial suspension into each well of a sterile 96-well flat-bottom microtiter plate.
- Incubate the plate under static conditions at 37°C for 24-48 hours to allow for mature biofilm development.
Step 2: Biofilm Treatment
- After incubation, carefully aspirate the planktonic culture from each well.
- Gently wash the adherent biofilm once with 200 μL of PBS to remove loosely attached cells.
- Add the prepared liposomal Cas9 formulation to the test wells. Include critical controls:
- Untreated biofilm control (PBS only).
- Free Cas9 RNP control (without liposomes).
- Empty liposome control (without CRISPR payload).
- Incubate the treatment plate under static conditions at 37°C for 24-48 hours [8] [73].
Biofilm Reduction Analysis
Post-treatment, biofilm integrity and viability are assessed using multiple complementary methods.
Method 1: Biomass Quantification via Crystal Violet (CV) Staining
- Aspirate the treatment medium and wash the biofilm gently with PBS.
- Fix the biofilm by adding 190 μL of 0.01% aqueous crystal violet solution for 30 minutes at room temperature.
- Remove the stain and wash the wells thoroughly with sterile water to remove excess, unbound dye.
- Destain the bound CV by adding 200 μL of 96-99% ethanol and vigorously pipetting.
- Measure the optical density (OD) of the destained solution at 570 nm using a microplate reader [74] [73].
- Calculate the percentage reduction in biomass relative to the untreated control.
Method 2: Metabolic Activity Assessment via Resazurin Assay
- After treatment, wash the biofilm with PBS.
- Add 100 μL of resazurin solution (4-8 μg/mL in PBS) to each well.
- Incubate the plate in the dark at 25°C for 20-40 minutes (conditions optimized for Gram-negative bacteria) [73].
- Measure the relative fluorescence units (RFU) using a microplate reader (λEx 530 nm / λEm 590 nm).
- The reduction of blue, non-fluorescent resazurin to pink, highly fluorescent resorufin is directly proportional to the metabolic activity of the remaining biofilm cells.
Method 3: Confocal Microscopy Imaging
- Grow and treat biofilms on suitable surfaces for microscopy (e.g., glass-bottom dishes, plastic coupons).
- Stain with a live/dead bacterial viability kit (e.g., SYTO 9 and propidium iodide) according to the manufacturer's protocol.
- Image the biofilms using a Confocal Laser Scanning Microscope (CLSM).
- Analyze the 3D image Z-stacks to determine changes in biofilm thickness, biovolume, and the ratio of live-to-dead cells, providing visual confirmation of disruption [75].
Critical Data Interpretation and Troubleshooting
Successful validation requires careful interpretation of results and awareness of potential pitfalls.
Data Interpretation: A >90% reduction in CV-stained biomass coupled with a significant drop in metabolic activity in the resazurin assay strongly indicates successful biofilm eradication. CLSM should reveal structural collapse and a high proportion of dead cells. The control groups are essential to confirm that the observed effect is due to the targeted action of the liposomal Cas9 and not the liposomes alone or free RNP.
Common Challenges and Troubleshooting
- Low Editing Efficiency: If biofilm reduction is minimal, verify the activity and specificity of your sgRNA. Optimize the lipid-to-RNP ratio during formulation and ensure the LNP size is within the optimal range for biofilm penetration (~100-200 nm).
- Poor Biofilm Formation: Ensure the use of media supplements like glucose and verify incubation times. Some bacterial strains require extended incubation (e.g., 48 hours for some Enterococci) for robust biofilm development [73].
- High Background in Controls: Empty liposome controls should show minimal antibacterial activity. If they do, it may indicate intrinsic antibacterial properties of the lipids, necessitating a reformulation.
- Assay Variability: Always perform experiments with a sufficient number of biological and technical replicates (e.g., n=6 per group). Calculate assay quality metrics like Z'-factor (>0.5 is excellent) to ensure robustness [73].
The rise of antibiotic-resistant bacterial infections represents a critical global health challenge, with bacterial biofilms playing a pivotal role in treatment failure and bacterial persistence [13] [9]. Biofilms are structured communities of microorganisms embedded in a self-produced extracellular polymeric substance (EPS) matrix that can exhibit up to 1000-fold greater tolerance to antibiotics compared to their planktonic counterparts [13]. Against this challenge, the integration of CRISPR/Cas9 gene-editing technology with nanoparticle-based delivery systems has emerged as a promising therapeutic strategy for precision antimicrobial therapy [13] [8].
While in vitro studies demonstrate impressive results—including liposomal CRISPR-Cas9 formulations reducing Pseudomonas aeruginosa biofilm biomass by over 90% in vitro—these simplified systems cannot replicate the complex biological barriers present in living organisms [13] [35]. This Application Note provides researchers with comprehensive protocols for evaluating CRISPR-nanoparticle anti-biofilm therapeutics using in vivo models, which are essential for assessing true therapeutic efficacy, biodistribution, and safety prior to clinical translation.
Key In Vivo Models for Biofilm Infection Studies
The selection of an appropriate in vivo model is critical for generating clinically relevant data on the efficacy of CRISPR-nanoparticle therapeutics. The table below summarizes the primary animal models used in biofilm research.
Table 1: In Vivo Models for Evaluating Anti-Biofilm Therapeutics
| Model System | Biofilm-Related Applications | Key Advantages | Experimental Considerations |
|---|---|---|---|
| Galleria mellonella (Wax Moth Larvae) | - Initial virulence assessment- Preliminary efficacy screening- Immune response studies | - Low cost & high throughput- No ethical restrictions- Innate immune system similar to mammals | - Limited temperature range (25-37°C)- Short-term experiments only (≤2 weeks)- Smaller tissue volume for analysis |
| Murine Models (Mice/Rats) | - Chronic wound infections- Catheter-associated infections- Implant-related infections- Pneumonia models | - Well-characterized immune system- Extensive genetic tools available- Clinical relevance for many infection types | - Higher cost than invertebrate models- Requires ethical approval- Species-specific immune differences |
| Zebrafish Models | - Real-time visualization of infection- Host-pathogen interaction studies- Neutrophil and macrophage tracking | - Optical transparency for imaging- Genetic manipulability- High fecundity for large-scale studies | - Lower body temperature (28-33°C)- Limited immunological tools compared to mice |
The application of these models is demonstrated in recent research. For instance, the Galleria mellonella model was successfully employed to assess virulence attenuation in Acinetobacter baumannii following CRISPR/Cas9-mediated mutation of the smpB gene, with larval survival rates of 84% for the mutant compared to 72% for the wild-type strain [76]. Murine models offer more comprehensive assessment capabilities for localized biofilm infections on implants or in chronic wounds, allowing for evaluation of both biofilm eradication and host tissue response [13].
Quantitative Efficacy Endpoints for In Vivo Studies
Rigorous quantification of therapeutic outcomes is essential for validating CRISPR-nanoparticle efficacy. The following endpoints should be standardized across studies.
Table 2: Key Quantitative Endpoints for In Vivo Efficacy Assessment
| Endpoint Category | Specific Metrics | Methodology | Interpretation Guidelines |
|---|---|---|---|
| Bacterial Burden | - Colony-forming units (CFU)/g tissue- Bacterial load reduction (log10)- Biofilm metabolic activity | - Homogenization & plating- ATP-based bioluminescence assays- Scanning electron microscopy (SEM) | - ≥3-log reduction indicates bactericidal activity- Statistical power: n≥6/group for CFU |
| Host Response | - Inflammatory markers (IL-6, TNF-α, MPO)- Histopathological scoring- Immune cell infiltration | - ELISA/Luminex assays- H&E staining- Immunohistochemistry | - Correlate reduced inflammation with bacterial clearance- Score tissue architecture damage (0-4 scale) |
| Therapeutic Distribution | - Nanoparticle biodistribution- CRISPR editing efficiency in tissue- Target engagement verification | - Fluorescent labeling (DiR/DiD)- NGS of recovered bacteria- PCR-based resistance gene detection | - Track organ-specific accumulation- Measure indels at target loci- Confirm resistance gene disruption |
Recent advances in nanoparticle delivery systems have demonstrated significant promise for enhancing in vivo efficacy. Gold nanoparticle carriers have been shown to enhance CRISPR editing efficiency up to 3.5-fold compared to non-carrier systems, while liposomal formulations enable co-delivery of CRISPR components with antibiotics or antimicrobial peptides for synergistic effects [13] [8]. These delivery improvements directly impact the quantitative endpoints measured in animal models.
Experimental Protocol: Murine Chronic Wound Biofilm Model
Research Reagent Solutions
Table 3: Essential Research Reagents for In Vivo Biofilm Studies
| Reagent/Category | Specific Examples | Function/Application |
|---|---|---|
| Nanoparticle Formulations | - Liposomal CRISPR-Cas9- Gold nanoparticle-CRISPR conjugates- Polymeric nanoparticles with antibiotic co-loading | - Protect CRISPR components from degradation- Enhance biofilm penetration- Enable targeted delivery |
| Bacterial Strains & Culture | - ESKAPE pathogens (especially P. aeruginosa & A. baumannii)- Luciferase-tagged strains for bioluminescence imaging- Antibiotic-resistant clinical isolates | - Clinically relevant biofilm formation- Real-time infection monitoring- Testing resistance reversal via CRISPR |
| Animal Model Supplies | - Immunosuppressants (e.g., cyclophosphamide)- Anesthetics (e.g., isoflurane, ketamine/xylazine)- Analgesics (e.g., buprenorphine) | - Enable infection establishment- Humane procedure management- Post-procedural pain control |
| Analysis Kits & Reagents | - Bacterial genomic DNA isolation kits- CRISPR cleavage efficiency assays- Cytokine profiling arrays- Histology reagents (fixatives, stains) | - Molecular efficacy assessment- Host response characterization- Tissue morphology evaluation |
Step-by-Step Methodology
Week 1: Animal Preparation and Infection
- Day 1-3: Acclimate 8-10 week old C57BL/6 or BALB/c mice to facility conditions.
- Day 4: Induce immunosuppression with cyclophosphamide (150 mg/kg, IP) 2 days pre-infection to enhance susceptibility.
- Day 5: Anesthetize mice (isoflurane 2-3%), shave dorsal area, and create a 6mm full-thickness excisional wound using biopsy punch.
- Day 6: Inoculate wound with 1×10^7 CFU of methicillin-resistant Staphylococcus aureus (MRSA) or Pseudomonas aeruginosa in 20μL PBS. Cover with transparent semi-occlusive dressing.
Week 2: Biofilm Establishment and Treatment Initiation
- Day 7-10: Allow biofilm development (maturation typically occurs within 72-96 hours post-infection).
- Day 11: Randomize animals into treatment groups (n=8-10/group):
- Group 1: CRISPR-nanoparticle formulation (e.g., liposomal Cas9-sgRNA targeting bacterial resistance genes)
- Group 2: Empty nanoparticles (vehicle control)
- Group 3: Conventional antibiotic (e.g., vancomycin for MRSA)
- Group 4: Untreated infected control
- Administer first treatment via topical application (50μL of formulation) or systemic delivery (IV via tail vein), depending on nanoparticle design.
Week 3: Treatment Course and Monitoring
- Day 12-18: Continue treatment regimen based on formulation pharmacokinetics (typically daily for topical, every 2-3 days for systemic).
- Monitor animals daily for clinical signs: weight loss, activity level, wound appearance.
- Document wound healing progression through daily photography and planimetry measurements.
Week 4: Endpoint Analysis
- Day 19: Euthanize animals, collect wound tissue and surrounding skin.
- Divide tissue samples for multiple analyses:
- ½ tissue for bacterial quantification (homogenize and plate serial dilutions)
- ¼ tissue for histology (fix in 10% formalin for H&E and Gram staining)
- ¼ tissue for molecular analyses (snap freeze for CRISPR efficacy assessment and cytokine measurement)
In Vivo Biofilm Therapeutic Evaluation Workflow
Protocol: Galleria mellonella Virulence and Efficacy Screening
For initial high-throughput screening of CRISPR-nanoparticle anti-biofilm efficacy, the Galleria mellonella model provides a cost-effective alternative to mammalian systems.
Larval Preparation and Infection
- Select healthy larvae weighing 300-350 mg with creamy white coloration and no gray markings.
- Divide larvae randomly into experimental groups (n=15-20/group) including:
- Uninfected control (PBS injection)
- Infected untreated control
- CRISPR-nanoparticle treatment groups (varying formulations or targets)
- Conventional antibiotic control
- Disinfect larval prolegs with 70% ethanol before injection.
- Using a microsyringe with 26G needle, inject 10μL of bacterial suspension (5×10^5 CFU of A. baumannii or P. aeruginosa) into the hemocoel via the last left proleg.
- One hour post-infection, administer 10μL of CRISPR-nanoparticle formulation into the last right proleg.
Incubation and Monitoring
- Maintain injected larvae at 37°C in Petri dishes without food.
- Monitor survival every 12 hours for 5-7 days, scoring larvae as dead when unresponsive to touch.
- Record mortality rates and calculate Kaplan-Meier survival curves.
- At experiment endpoint, homogenize surviving larvae for bacterial quantification or extract hemolymph for immune response analyses.
Mechanism of Action and Analysis Verification
Understanding the mechanism of CRISPR-nanoparticle action against biofilms guides appropriate analytical methods throughout in vivo studies.
CRISPR-Nanoparticle Anti-Biofilm Mechanism of Action
Data Analysis and Interpretation Guidelines
Statistical Considerations
- Perform power analysis prior to experiments to determine appropriate group sizes (typically n≥6 for murine studies, n≥15 for Galleria).
- Employ ANOVA with post-hoc testing for multiple group comparisons.
- Utilize Kaplan-Meier analysis with log-rank test for survival data.
- Account for multiple comparisons using appropriate correction methods (e.g., Bonferroni, Tukey).
Success Criteria Definition
- High Efficacy: ≥3-log reduction in bacterial burden with significant improvement in host survival and histopathology scores.
- Moderate Efficacy: 1-3 log reduction in bacterial burden with measurable improvement in clinical outcomes.
- Synergistic Effects: Demonstrable enhancement of conventional antibiotic efficacy when combined with CRISPR-nanoparticle treatment.
The integration of in vivo models with appropriate analytical methods provides a critical pathway for translating promising CRISPR-nanoparticle anti-biofilm therapies from bench to bedside. These protocols establish standardized approaches for evaluating therapeutic efficacy within complex biological systems, accelerating the development of next-generation solutions for combating antibiotic-resistant biofilm infections.
Antimicrobial resistance (AMR) represents one of the most pressing global health threats of the 21st century, with biofilm-associated infections playing a pivotal role in bacterial persistence and treatment failure [13] [77]. The protective extracellular polymeric substance (EPS) matrix of biofilms limits antibiotic penetration, reduces metabolic activity of embedded cells, and enhances horizontal gene transfer, rendering conventional antibiotics increasingly ineffective [13]. This challenge has catalyzed the development of novel therapeutic strategies, with the integration of CRISPR/Cas9 gene-editing technology and nanoparticle-based delivery emerging as a promising approach for next-generation antimicrobial therapy [13] [11].
This Application Note provides a structured performance benchmarking analysis and detailed experimental protocols comparing innovative CRISPR-nanoparticle systems against conventional antibiotic therapies. The content is framed within a broader research thesis on nanoparticle delivery of CRISPR-Cas9 for biofilm eradication, targeting researchers, scientists, and drug development professionals working in antimicrobial discovery and therapeutic development.
Performance Benchmarking: Quantitative Analysis
The comparative efficacy of CRISPR-nanoparticle systems versus conventional antibiotics is quantified across multiple parameters in Table 1. Performance data demonstrate the potential of combinatorial approaches to overcome limitations associated with monotherapies.
Table 1: Performance Benchmarking of CRISPR-Nanoparticle Systems vs. Conventional Antibiotic Therapies
| Performance Parameter | Conventional Antibiotics | CRISPR-Nanoparticle Systems | Experimental Conditions |
|---|---|---|---|
| Biofilm Reduction | 10-60% biomass reduction [13] | >90% biomass reduction (liposomal Cas9) [13] [8] | In vitro P. aeruginosa biofilm [13] |
| Editing Efficiency | Not applicable | 3.5-fold increase (gold nanoparticle carriers) [13] [8] | Compared to non-carrier delivery systems [13] |
| Bacterial Resistance Development | Rapid selection of resistant mutants [78] | Targeted disruption of resistance genes (e.g., blaNDM, mecA, vanA) [79] | Laboratory and clinical isolates [79] |
| Target Specificity | Broad-spectrum activity affecting microbiome [78] | Precision targeting of resistance genes/pathogens [79] [78] | Species- and gene-specific gRNA design [79] |
| Penetration Efficiency | Limited by biofilm EPS matrix [13] | Enhanced via engineered nanoparticle properties [13] [11] | Biofilm penetration assays [13] |
| Minimum Inhibitory Concentration (MIC) | Increasing MIC values for resistant strains [11] | Resensitization to antibiotics (e.g., fosfomycin) [79] | MIC testing pre/post CRISPR treatment [79] |
The synergistic potential of combining CRISPR-nanoparticle systems with conventional antibiotics is quantified in Table 2. These combinatorial approaches leverage multiple mechanisms of action to enhance therapeutic outcomes.
Table 2: Synergistic Effects of CRISPR-Nanoparticle and Antibiotic Combinations
| Combination Therapy | Efficacy Outcome | Mechanistic Basis | Reference Pathogen |
|---|---|---|---|
| Liposomal CRISPR-Cas9 + Antibiotics | Superior biofilm disruption | CRISPR targets resistance genes; antibiotics kill sensitized cells [13] | Pseudomonas aeruginosa [13] |
| Gold NP-CRISPR + β-lactams | Enhanced bacterial killing | CRISPR disrupts β-lactamase genes (bla); restored antibiotic efficacy [13] [79] | MRSA, Enterobacteriaceae [79] |
| Phagemid CRISPR + Colistin | Restored colistin susceptibility | CRISPR targets mcr-1 resistance gene [79] | E. coli, K. pneumoniae [79] |
| Nanoparticle CRISPR + Fosfomycin | Resensitization achieved | CRISPR disrupts fosA3 resistance gene [79] | E. coli [79] |
Mechanism of Action: Comparative Pathways
The fundamental difference between conventional antibiotics and CRISPR-nanoparticle systems lies in their mechanisms of action. Conventional antibiotics typically target essential bacterial cellular processes, while CRISPR-nanoparticle systems precisely disrupt genetic determinants of resistance and virulence.
Experimental Protocols
Protocol 1: Liposomal CRISPR-Cas9 Formulation for Biofilm Eradication
This protocol describes the preparation of liposomal nanoparticles loaded with CRISPR-Cas9 components for enhanced biofilm penetration and targeted gene editing [13].
Materials and Reagents
- CRISPR-Cas9 plasmid DNA or ribonucleoprotein (RNP) complex
- Cationic lipid formulation (e.g., DOTAP, DOPE, cholesterol)
- Phosphate-buffered saline (PBS), pH 7.4
- Polycarbonate membranes (100 nm pore size)
- Extrusion device
- P. aeruginosa culture (or other target pathogen)
- Biofilm growth medium (e.g., LB, TSB)
- 96-well polystyrene plates for biofilm formation
- Crystal violet stain or SYTO-9 for biomass quantification
Step-by-Step Procedure
Liposome Preparation (Day 1):
- Prepare lipid film by dissolving cationic lipid mixture in chloroform (molar ratio: DOTAP:DOPE:cholesterol = 50:25:25)
- Remove organic solvent under nitrogen stream to form thin lipid film
- Hydrate lipid film with PBS containing CRISPR-Cas9 components (50 µg/mL final concentration)
- Subject the mixture to five freeze-thaw cycles (liquid nitrogen/37°C water bath)
- Extrude through polycarbonate membranes (100 nm pore size) 21 times
- Purify liposomes using size exclusion chromatography
Biofilm Formation (Day 1):
- Inoculate P. aeruginosa in biofilm growth medium and incubate overnight at 37°C with shaking
- Dilute overnight culture 1:100 in fresh medium
- Add 200 µL diluted culture to 96-well polystyrene plates
- Incubate statically for 24-48 hours at 37°C to establish mature biofilms
Treatment and Assessment (Day 3):
- Carefully remove planktonic cells and medium from established biofilms
- Add liposomal CRISPR-Cas9 formulations (50-100 µL/well)
- Incubate for 24 hours at 37°C
- Assess biofilm biomass using crystal violet staining or confocal microscopy
- Quantify gene editing efficiency via PCR and sequencing of target loci
Protocol 2: Gold Nanoparticle-Mediated CRISPR Delivery
This protocol outlines the synthesis of gold nanoparticle conjugates for CRISPR component delivery, achieving 3.5-fold higher editing efficiency compared to non-carrier systems [13].
Materials and Reagents
- Chloroauric acid (HAuCl₄)
- Trisodium citrate
- Thiol-modified CRISPR-Cas9 components
- Polyethylene glycol (PEG) spacer
- Bacterial culture of interest
- Luria-Bertani (LB) broth and agar
- Antibiotics for selection (if applicable)
- Gel electrophoresis equipment for verification
Step-by-Step Procedure
Gold Nanoparticle Synthesis (Day 1):
- Prepare 100 mL of 1 mM HAuCl₄ solution, bring to boil with stirring
- Rapidly add 10 mL of 38.8 mM trisodium citrate solution
- Continue heating and stirring until solution develops deep red color (≈20 minutes)
- Cool to room temperature while stirring
- Characterize nanoparticles using UV-Vis spectroscopy (peak ≈520 nm) and TEM
CRISPR Component Conjugation (Day 1):
- Thiol-functionalize Cas9 RNP complex or plasmid DNA using Traut's reagent
- Incubate functionalized CRISPR components with gold nanoparticles (molar ratio 50:1)
- Add PEG spacer (5 kDa) to stabilize conjugation
- Purify conjugates using centrifugation (15,000 × g, 30 minutes)
- Resuspend in appropriate buffer for bacterial treatment
Bacterial Transformation and Efficiency Assessment (Day 2):
- Grow target bacterial strain to mid-log phase (OD₆₀₀ ≈ 0.5-0.6)
- Incubate bacteria with gold nanoparticle-CRISPR conjugates (2 hours, 37°C)
- Plate on selective media if using CRISPR for plasmid curing
- Incubate overnight and count colonies to assess editing efficiency
- Verify gene editing through:
- Antibiotic susceptibility testing
- PCR amplification of target loci
- Sequencing of edited regions
Experimental Workflow for CRISPR-Nanoparticle Biofilm Studies
The comprehensive experimental workflow for evaluating CRISPR-nanoparticle systems against bacterial biofilms integrates nanoparticle formulation, biological assessment, and molecular validation steps.
The Scientist's Toolkit: Research Reagent Solutions
Table 3: Essential Research Reagents for CRISPR-Nanoparticle Anti-Biofilm Studies
| Reagent Category | Specific Examples | Function/Application | Key Considerations |
|---|---|---|---|
| CRISPR Components | Cas9 nuclease, guide RNA (gRNA), CRISPR plasmids [13] [79] | Precision targeting of antibiotic resistance genes (e.g., mecA, vanA, blaNDM) [79] | gRNA design specificity; off-target effect assessment [79] |
| Nanoparticle Systems | Liposomal formulations, gold nanoparticles, polymeric nanoparticles [13] | Enhanced delivery, cellular uptake, and biofilm penetration [13] | Size, surface charge, loading efficiency, stability [13] |
| Bacterial Strains | P. aeruginosa, MRSA, K. pneumoniae, E. coli [13] [79] | Biofilm formation models; antibiotic resistance profiling | Clinical vs. laboratory strains; growth conditions [11] |
| Biofilm Assessment Tools | Crystal violet, confocal microscopy, SYTO-9 staining [11] | Biofilm biomass quantification and structural analysis | Distinction between live/dead cells; 3D architecture [11] |
| Molecular Validation Kits | PCR reagents, sequencing kits, antibiotic susceptibility tests [79] | Verification of gene editing and resensitization outcomes | Sensitivity thresholds; quantitative analysis [79] |
The performance benchmarking data and protocols presented in this Application Note demonstrate the significant potential of CRISPR-nanoparticle systems to overcome limitations of conventional antibiotic therapies, particularly for biofilm-associated infections. The integration of precise genetic targeting with enhanced nanoparticle-mediated delivery represents a paradigm shift in antimicrobial strategy, moving from broad-spectrum activity to precision medicine approaches.
The quantitative data show that CRISPR-nanoparticle systems can achieve >90% biofilm biomass reduction and significantly increase gene-editing efficiency compared to conventional delivery methods. Furthermore, these systems enable resensitization to conventional antibiotics through targeted disruption of resistance genes, creating opportunities for combination therapies that may delay the emergence of resistance.
As research in this field advances, addressing challenges related to optimal delivery platforms, off-target effects, and long-term safety will be crucial for clinical translation. The experimental protocols provided herein offer researchers standardized methodologies for further investigating and optimizing these promising antimicrobial platforms.
Application Note: The Health and Economic Burden of Antimicrobial Resistance
Current Global Impact of AMR and Biofilm-Associated Infections
Antimicrobial resistance (AMR), particularly from biofilm-associated infections, presents a critical global health threat with severe economic consequences. Biofilms are structured communities of microorganisms embedded in a self-produced matrix that can exhibit up to 1,000-fold greater tolerance to antibiotics compared to their free-floating counterparts [13]. The protective extracellular matrix limits antibiotic penetration, enhances horizontal gene transfer, and enables bacterial survival in hostile environments, making conventional therapies largely ineffective [13].
The economic burden of AMR is substantial, with current estimates suggesting AMR could lead to $1-3 trillion in lost global GDP annually by 2050 [80]. In the United States alone, the Centers for Disease Control and Prevention reports over 2.8 million antibiotic-resistant infections annually, resulting in more than 35,000 deaths each year [80]. The growing prevalence of resistant infections threatens essential medical procedures including surgeries, cancer chemotherapy, and organ transplants, which become significantly riskier without effective antibiotics [13] [81].
Table 1: Global Burden of Antimicrobial Resistance (2019 Data)
| Metric | Value | Region/Pathogen Specifics |
|---|---|---|
| Total deaths associated with bacterial AMR | 4.71 million | Global estimate for 2021 [81] |
| Deaths directly attributable to AMR | 1.14 million | Global estimate for 2021 [81] |
| Annual AMR deaths in the United States | >35,000 | From 2.8 million infections [80] |
| UK AMR patient infections | 65,162 (2019) | Increased from 61,946 in 2018 [80] |
| Projected annual AMR deaths by 2050 | 1.91 million | Based on current trends [81] |
| Mortality from MRSA in the US | 19,832 deaths | From 119,247 infections [80] |
Nanoparticle-Delivered CRISPR-Cas as an Economic Solution
The integration of CRISPR-Cas technology with nanoparticle delivery systems represents a transformative approach that targets the root genetic mechanisms of antibiotic resistance while overcoming physical biofilm barriers. This combined strategy addresses both heritable genetic resistance (through precise gene editing) and phenotypic biofilm-mediated tolerance (through enhanced penetration) [13].
Liposomal CRISPR-Cas9 formulations have demonstrated remarkable efficacy, reducing Pseudomonas aeruginosa biofilm biomass by over 90% in vitro [13]. Similarly, gold nanoparticle carriers have enhanced editing efficiency by up to 3.5-fold compared to non-carrier systems [13]. These hybrid platforms enable co-delivery with antibiotics or antimicrobial peptides, producing synergistic antibacterial effects and superior biofilm disruption that could significantly reduce treatment duration and associated healthcare costs [13].
Quantitative Analysis of Therapeutic Potential
Efficacy Metrics of CRISPR-Nanoparticle Platforms
Recent advances in CRISPR-nanoparticle biofilms have yielded promising quantitative results that demonstrate significant potential for reducing morbidity in chronic infections. The therapeutic efficacy stems from two complementary mechanisms: precise genetic disruption of resistance determinants and enhanced physical penetration of biofilm matrices.
Table 2: Experimental Efficacy Metrics of CRISPR-Nanoparticle Anti-Biofilm Platforms
| Platform Type | Target Pathogen/Biofilm | Key Efficacy Metrics | Reference |
|---|---|---|---|
| Liposomal Cas9 formulations | Pseudomonas aeruginosa | >90% reduction in biofilm biomass in vitro | [13] |
| CRISPR-gold nanoparticle hybrids | Model bacterial systems | 3.5-fold increase in gene-editing efficiency | [13] |
| Elastin-like polypeptide AuNP | S. epidermidis biofilms | Targeted photothermal ablation demonstrated | [47] |
| Cas12a (Cpf1) systems | Bacterial biofilms | Collateral ssDNA cleavage enabling broader targeting | [82] |
Economic Projections of Novel Anti-Biofilm Therapies
While still in development, CRISPR-nanoparticle therapies offer potential for substantial cost savings through reduced hospitalization durations, decreased need for surgical interventions to remove biofilm-colonized medical devices, and lower rates of treatment failure. The ability to resensitize bacteria to conventional antibiotics could extend the lifespan of existing antimicrobials, delaying the need for more expensive last-line treatments and reducing selective pressure that drives resistance development [13] [80].
Experimental Protocols for CRISPR-Nanoparticle Biofilm Eradication
Protocol: Liposomal CRISPR-Cas9 Formulation and Biofilm Assessment
Objective: To prepare and evaluate liposomal nanoparticles encapsulating CRISPR-Cas9 components for efficacy against bacterial biofilms.
Materials:
- Cas9 ribonucleoprotein (RNP) complexes or encoding plasmid DNA
- Cationic lipid nanoparticles (LNPs)
- Guide RNAs targeting biofilm-related genes (e.g., quorum sensing, antibiotic resistance genes)
- Mature bacterial biofilms (e.g., P. aeruginosa 72-hour culture)
- Confocal laser scanning microscopy (CLSM) setup
- Crystal violet staining assay materials
- Viability PCR reagents
Methodology:
Liposomal Formulation Preparation:
- Hydrate lipid film containing DOTAP, cholesterol, and DSPE-PEG2000 in sterile PBS.
- Mix Cas9 RNP complexes with guide RNA targeting specific biofilm genes (e.g., lasI for quorum sensing disruption).
- Combine lipid hydration solution with CRISPR components using microfluidics device for uniform nanoparticle formation.
- Purify via size exclusion chromatography and characterize using dynamic light scattering (Z-average: 80-120 nm, PDI <0.2) [13].
Biofilm Cultivation and Treatment:
- Grow 72-hour mature biofilms in flow cells or 96-well plates.
- Treat biofilms with liposomal CRISPR formulations at sub-MIC antibiotic concentrations.
- Incubate for 24 hours at 37°C.
Efficacy Assessment:
- Quantify biofilm biomass reduction using crystal violet staining (measure at OD590nm).
- Assess bacterial viability within biofilms via colony-forming unit counts or viability PCR.
- Visualize architectural disruption using confocal laser scanning microscopy with LIVE/DEAD BacLight staining.
- Evaluate specific gene knockout efficiency through PCR and sequencing of target loci.
Expected Outcomes: >90% reduction in biofilm biomass and significant disruption of biofilm architecture with restoration of antibiotic susceptibility in previously resistant strains [13].
Protocol: Gold Nanoparticle-Mediated CRISPR Delivery with Photothermal Activation
Objective: To functionalize gold nanoparticles for targeted CRISPR delivery with optional photothermal biofilm disruption.
Materials:
- Gold nanoparticles (15-20 nm)
- Elastin-like polypeptide (ELP) targeting ligands
- CRISPR-Cas12a components (smaller size than Cas9)
- Near-infrared (NIR) laser system (808 nm)
- Bacterial strains with autolysin domains for targeting
- Inductively coupled plasma-mass spectrometry (ICP-MS)
Methodology:
Nanoparticle Functionalization:
- Conjugate ELP targeting domains to gold nanoparticle surface via thiol chemistry.
- Adsorb CRISPR-Cas12a RNP complexes onto functionalized AuNPs.
- Characterize conjugation efficiency using UV-Vis spectroscopy and TEM.
Targeted Biofilm Treatment:
- Incubate functionalized AuNP-CRISPR with mature biofilms for 4 hours.
- Apply NIR laser irradiation (808 nm, 1.5 W/cm², 5 minutes) for photothermal activation.
- Utilize targeting ligands specific to bacterial surface components (e.g., autolysin domains) for enhanced specificity [47].
Analysis:
- Quantify nanoparticle penetration using ICP-MS.
- Assess photothermal efficacy via thermal imaging during NIR exposure.
- Evaluate collateral ssDNA cleavage activity characteristic of Cas12a systems.
- Measure synergy between genetic disruption and thermal ablation.
Expected Outcomes: 3.5-fold enhancement in editing efficiency compared to non-carrier systems with combined genetic and physical biofilm disruption [13] [47].
Visualization of Mechanisms and Workflows
Mechanism of CRISPR-Nanoparticle Biofilm Penetration and Action
CRISPR-Nanoparticle Biofilm Penetration
Experimental Workflow for Anti-Biofilm Therapy Development
Anti-Biofilm Therapy Development Workflow
The Scientist's Toolkit: Key Research Reagent Solutions
Table 3: Essential Research Reagents for CRISPR-Nanoparticle Biofilm Studies
| Reagent Category | Specific Examples | Function/Application | Considerations |
|---|---|---|---|
| CRISPR Systems | Cas9, Cas12a (Cpf1), Cas13 | Gene editing, resistance disruption | Cas12a offers smaller size; Cas13 targets RNA [82] |
| Nanoparticles | Cationic liposomes, Gold nanoparticles (AuNPs), Polymeric NPs | Delivery vehicle, enhanced penetration | AuNPs enable photothermal therapy [13] [47] |
| Targeting Ligands | Elastin-like polypeptides (ELPs), Bacteriophage tail proteins | Biofilm-specific targeting | Enhances specificity, reduces off-target effects [47] |
| Guide RNAs | Targeting mecA, blaNDM-1, lasI, icaA | Specific resistance gene disruption | Biofilm-specific genes enhance efficacy [13] [82] |
| Assessment Tools | Confocal microscopy, Crystal violet, Viability PCR | Efficacy quantification | Multiple methods provide validation [13] |
| Delivery Enhancers | PEGylated lipids, Cell-penetrating peptides | Stability and cellular uptake | Improves pharmacokinetics [13] [50] |
Conclusion
The integration of nanoparticle delivery systems with CRISPR-Cas9 technology presents a formidable, dual-pronged strategy against biofilm-driven infections. This approach synergistically combines the physical biofilm-disrupting capabilities of nanoparticles with the genetic precision of CRISPR to target resistance genes, quorum sensing, and biofilm regulatory factors. While validated by impressive preclinical results—such as over 90% biofilm biomass reduction and significantly enhanced editing efficiency—the path to clinical application requires overcoming key challenges in delivery optimization, safety assurance, and manufacturing scalability. Future directions must focus on developing smart, stimuli-responsive nanocarriers, expanding the toolkit with novel Cas variants like Cas12 and Cas13, and advancing robust in vivo models to pave the way for clinical trials. This powerful combination holds the imminent potential to redefine the therapeutic landscape for some of the most persistent and costly infections in modern medicine.
References
- 1. Recent advances in nanotechnology for eradicating bacterial ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC8899562/]
- 2. integrating CRISPR/Cas9 and nanoparticles against biofilm ... [https://bmcmedicine.biomedcentral.com/articles/10.1186/s12916-025-04323-4]
- 3. Nanoparticles targeting biofilms: A new era in combating ... [https://www.sciencedirect.com/science/article/pii/S2590097825000370]
- 4. Nanomaterial-Based Strategies to Combat Antibiotic Resistance [https://pmc.ncbi.nlm.nih.gov/articles/PMC11852044/]
- 5. Biofilm and Antimicrobial Resistance: Mechanisms, ... [https://www.mdpi.com/2036-7481/16/8/183]
- 6. Biofilms and multidrug resistance: an emerging crisis ... [https://www.frontiersin.org/journals/bioengineering-and-biotechnology/articles/10.3389/fbioe.2025.1625356/full]
- 7. CRISPR–Cas systems as emerging tools for precision ... [https://www.sciencedirect.com/science/article/abs/pii/S0963996925021416]
- 8. Innovative approaches to combat antibiotic resistance [https://pubmed.ncbi.nlm.nih.gov/40830872/]
- 9. Biofilms: structure, resistance mechanism, emerging control ... [https://pubs.rsc.org/en/content/articlehtml/2025/pm/d5pm00094g]
- 10. Mechanisms of antimicrobial resistance in biofilms [https://www.nature.com/articles/s44259-024-00046-3]
- 11. Beyond antibiotics: CRISPR/Cas9 triumph over biofilm- ... [https://www.frontiersin.org/journals/cellular-and-infection-microbiology/articles/10.3389/fcimb.2024.1408569/full]
- 12. Bacterial Persister Cells and Development of Antibiotic ... - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC11335562/]
- 13. integrating CRISPR/Cas9 and nanoparticles against biofilm ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12366227/]
- 14. CRISPR-Cas9 system: A potent tool to fight antibiotic ... [https://www.sciencedirect.com/science/article/pii/S2950194624001511]
- 15. Harnessing bacterial immunity: CRISPR-Cas system as a ... [https://www.frontiersin.org/journals/cellular-and-infection-microbiology/articles/10.3389/fcimb.2025.1588446/full]
- 16. A CRISPR/Cas9 based polymeric nanoparticles to treat ... [https://www.sciencedirect.com/science/article/abs/pii/S1084952118301290]
- 17. Advances in CRISPR Delivery Methods - PubMed Central - NIH [https://pmc.ncbi.nlm.nih.gov/articles/PMC9835311/]
- 18. Unravelling the advances of CRISPR-Cas9 as a precise ... [https://www.sciencedirect.com/science/article/pii/S2213716525000360]
- 19. Advances in nanoparticles in targeted drug delivery–A review [https://www.sciencedirect.com/science/article/pii/S2666845925001163]
- 20. Antibacterial and antibiofilm activity of silver nanoparticles ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11544008/]
- 21. Antibiofilm activity of green synthesized silver ... [https://www.nature.com/articles/s41598-022-07831-y]
- 22. Nanoparticles in Drug Delivery: From History to Therapeutic ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC9781272/]
- 23. Addressing antimicrobial resistance with Cas9, Cas12, ... [https://www.sciencedirect.com/science/article/pii/S2405844025003937]
- 24. Nanocarriers: A novel strategy for the delivery of CRISPR ... [https://www.frontiersin.org/journals/chemistry/articles/10.3389/fchem.2022.957572/full]
- 25. Application of Polymeric Nanocarriers for Enhancing the ... [https://www.mdpi.com/2076-3417/11/22/10695]
- 26. Lipid Nanoparticles: A Breakthrough in CRISPR Delivery ... [https://www.genscript.com/lipid-nanoparticles-the-vanguard-of-crispr-delivery-systems.html]
- 27. Emerging technologies and innovative approaches to ... [https://www.sciencedirect.com/science/article/pii/S3050723525000033]
- 28. CRISPR Delivery Methods: Cargo, Vehicles, and Challenges [https://www.synthego.com/blog/delivery-crispr-cas9/]
- 29. Engineering the Delivery System for CRISPR-based ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC5801045/]
- 30. CRISPR This Way: Choosing Between Delivery System [https://en.vectorbuilder.com/resources/vector-academy/lessons/crispr-delivery-systems.html]
- 31. Nanoparticle based delivery of CRISPR/Cas9 genome editing ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC6398936/]
- 32. CRISPR-Cas mediated targeting of resistance genes for ... [https://www.sciencedirect.com/science/article/pii/S0141813025097375]
- 33. Quantitative image analysis of microbial communities with ... [https://www.nature.com/articles/s41564-020-00817-4]
- 34. Quantitative and Qualitative Assessment Methods for Biofilm ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC6133255/]
- 35. Innovative approaches to combat antibiotic resistance ... [https://www.springermedicine.com/antibiotic/innovative-approaches-to-combat-antibiotic-resistance-integratin/51360102]
- 36. A DNA/Upconversion Nanoparticle Complex Enables... | CoLab [https://colab.ws/articles/10.1002%2Fadma.202309534]
- 37. Lung and liver editing by lipid nanoparticle of a stable... delivery [https://www.nature.com/articles/s41587-024-02437-3?error=cookies_not_supported&code=6c7d99a5-2a3d-48d9-9619-ddcd880f4d48]
- 38. CRISPR/Cas9 Delivery Systems to Enhance Gene Editing ... [https://www.mdpi.com/1422-0067/26/9/4420]
- 39. Harnessing the Microbiome: CRISPR-Based Gene Editing ... [https://link.springer.com/article/10.1007/s12602-025-10573-8]
- 40. Antimicrobial nanoparticles: a new horizon to combat ... [https://www.frontiersin.org/journals/nanotechnology/articles/10.3389/fnano.2025.1611126/full]
- 41. Novel Strategy to Combat Antibiotic Resistance: A Sight ... [https://www.mdpi.com/1999-4923/13/3/352]
- 42. Targeting bacterial biofilm-related genes with nanoparticle ... [https://www.frontiersin.org/journals/microbiology/articles/10.3389/fmicb.2024.1387114/full]
- 43. Anti-QS Strategies Against Pseudomonas aeruginosa ... [https://www.mdpi.com/2076-2607/13/8/1838]
- 44. Interactions between extracellular polymeric substances and ... [https://pubs.rsc.org/en/content/articlehtml/2025/en/d5en00073d]
- 45. Influence of extracellular polymeric substance on the ... [https://www.sciencedirect.com/science/article/abs/pii/S004896972101514X]
- 46. Mechanisms of interaction between polystyrene ... [https://pubmed.ncbi.nlm.nih.gov/36581121/]
- 47. Treatment of S. epidermidis biofilms with targeted ... [https://www.sciencedirect.com/science/article/pii/S0021979725026062]
- 48. Off-target effects in CRISPR/Cas9 gene editing - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC10034092/]
- 49. Off-target interactions in the CRISPR-Cas9 Machinery [https://www.sciencedirect.com/science/article/pii/S2405580825002213]
- 50. CRISPR/Cas9 therapeutics: progress and prospects [https://www.nature.com/articles/s41392-023-01309-7]
- 51. Precisely Targeted Nanoparticles for CRISPR-Cas9 Delivery ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11990453/]
- 52. Nanoparticle Delivery of CRISPR/Cas9 for Genome Editing [https://www.frontiersin.org/journals/genetics/articles/10.3389/fgene.2021.673286/full]
- 53. A catalogue of biochemically diverse CRISPR-Cas9 ... [https://www.nature.com/articles/s41467-020-19344-1]
- 54. qEva-CRISPR: a method for quantitative evaluation of ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC6158505/]
- 55. sciencedirect.com/topics/pharmacology-toxicology-and-pharmaceutical... [https://www.sciencedirect.com/topics/pharmacology-toxicology-and-pharmaceutical-science/nanotoxicology]
- 56. A biodegradable lipid nanoparticle delivers a Cas9 ... [https://www.sciencedirect.com/science/article/abs/pii/S1742706124006226]
- 57. Nanotechnology-Based Delivery of CRISPR/Cas9 for ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12346122/]
- 58. How to Assess Nanotoxicity : Key Methods and Protocols [https://www.azonano.com/article.aspx?ArticleID=6855]
- 59. Safer and efficient base editing and prime editing via ... [https://www.nature.com/articles/s41551-024-01296-2]
- 60. Regulatory pathways and guidelines for nanotechnology ... [https://www.frontiersin.org/journals/medicine/articles/10.3389/fmed.2025.1544393/full]
- 61. Current economic and regulatory challenges in developing ... [https://www.nature.com/articles/s44259-025-00123-1]
- 62. Ethical bioprospecting and microbial assessments for ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11668235/]
- 63. Transforming antimicrobial resistance mitigation [https://link.springer.com/article/10.1007/s42452-025-07053-7]
- 64. Lipid Nanoparticle (LNP) News Brief: March 17-24, 2025 [https://www.precigenome.com/post/lipid-nanoparticle-lnp-drug-delivery-advances-march-17-24-2025?srsltid=AfmBOorb6uBJJJbb1NONsG8kJByy2iHAQI5_FYesi5cL4w-h08LX8ATh]
- 65. Microbial Genome Editing with CRISPR–Cas9 [https://www.mdpi.com/2311-5637/11/7/410]
- 66. Is Increased Biofilm Formation Associated with Decreased ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12566419/]
- 67. Investigation of shockwave treatment for disruption ... [https://www.nature.com/articles/s41598-025-19955-y]
- 68. Quantitative Insights and Visualization of Antimicrobial ... [https://www.mdpi.com/2227-9059/11/10/2640]
- 69. 2.10. Bacterial cell viability measurement [https://bio-protocol.org/exchange/minidetail?id=6120332&type=30]
- 70. Utility of a commercially available transwell system for ... [https://www.sciencedirect.com/science/article/abs/pii/S0167701225002416]
- 71. Lipid nanoparticles: The game-changer in CRISPR-Cas9 ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10823087/]
- 72. Development of ionizable lipid nanoparticles and a ... [https://www.sciencedirect.com/science/article/abs/pii/S0378517324000796]
- 73. Defining conditions for biofilm inhibition and eradication ... [https://bmcmicrobiol.biomedcentral.com/articles/10.1186/s12866-018-1321-6]
- 74. An overview of various methods for in vitro biofilm formation [https://pmc.ncbi.nlm.nih.gov/articles/PMC10533769/]
- 75. Optimization of an in vitro Pseudomonas aeruginosa ... [https://www.nature.com/articles/s41522-024-00483-y]
- 76. CRISPR/Cas9-targeted smpB mutation revealing roles in ... [https://journals.plos.org/plosone/article?id=10.1371/journal.pone.0329638]
- 77. Combating Antimicrobial Resistance: Innovative Strategies ... [https://www.mdpi.com/1424-8247/18/8/1119]
- 78. Targeted Antimicrobial Therapies: A Solution to ... [https://www.mdpi.com/2673-8430/4/3/26]
- 79. Reinvigorating AMR resilience: leveraging CRISPR–Cas ... [https://tropmedhealth.biomedcentral.com/articles/10.1186/s41182-025-00728-2]
- 80. CRISPR-Cas Systems in the Fight Against Antimicrobial ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11608035/]
- 81. Advanced Nanoparticles in Combating Antibiotic Resistance [https://www.mdpi.com/2624-845X/6/2/9]
- 82. integrating CRISPR/Cas9 and nanoparticles against biofilm ... [https://bmcmedicine.biomedcentral.com/articles/10.1186/s12916-025-04323-4/tables/2]