Next-Generation Pathogen Detection: Advanced Strategies for Maximizing Assay Sensitivity
This article provides a comprehensive guide for researchers and drug development professionals seeking to enhance the sensitivity of pathogen detection assays.
Next-Generation Pathogen Detection: Advanced Strategies for Maximizing Assay Sensitivity
Abstract
This article provides a comprehensive guide for researchers and drug development professionals seeking to enhance the sensitivity of pathogen detection assays. Covering foundational principles to real-world application, it explores cutting-edge CRISPR methodologies, synthetic biology, and liquid biopsy advancements. The content delivers actionable strategies for troubleshooting common pitfalls, optimizing assay performance, and conducting rigorous clinical validation. By integrating the latest research and comparative analyses, this resource aims to bridge the gap between laboratory innovation and clinically viable, high-sensitivity diagnostic tools.
The Science of Signal and Noise: Core Principles of High-Sensitivity Detection
In the field of molecular diagnostics, a significant sensitivity gap exists between detection methods for nucleic acid biomarkers and those for protein biomarkers. While techniques like PCR can detect nucleic acids at attomolar to femtomolar concentrations, conventional protein detection methods like the enzyme-linked immunosorbent assay (ELISA) typically achieve detection limits only in the nanomolar to picomolar range [1]. Bridging this gap is critical for advancing in vitro diagnostics, particularly for infectious diseases where sensitive pathogen detection can dramatically improve early intervention and treatment outcomes [2] [3]. This technical resource center provides methodologies and troubleshooting guides to help researchers implement advanced techniques that enhance detection sensitivity for both classes of biomarkers.
Sensitivity Comparison of Detection Methods
The table below summarizes the typical sensitivity ranges for various biomarker detection techniques, highlighting the performance gap between conventional and advanced methods.
| Detection Method | Biomarker Type | Typical Limit of Detection | Key Applications |
|---|---|---|---|
| Conventional ELISA [1] | Protein | Nanomolar to Picomolar | General protein biomarker detection |
| Digital PCR [4] | Nucleic Acid | Single Molecule (e.g., 0.1% VAF) | Rare mutation detection, liquid biopsy |
| BEAMing [4] | Nucleic Acid | 0.01% Variant Allele Frequency | Ultra-rare variant quantification |
| Immuno-PCR [5] | Protein | Femtomolar (e.g., 2 fM BSA) | High-sensitivity protein detection |
| NATA-ELISA [1] | Protein | Femtomolar | Early disease diagnosis |
| ActCRISPR-TB [3] | Nucleic Acid | 5 copies/μL | Sensitive pathogen DNA detection |
Enhanced Experimental Protocols
Protocol 1: Nucleic Acid-Templated Target Amplification (NATA)-ELISA
This protocol enhances traditional ELISA sensitivity by several hundred-fold through in-situ amplification of the protein biomarker itself, inspired by viral replication mechanisms [1].
- Step 1: Capture Antigen. Coat wells with a capture antibody specific to your target protein biomarker. Incubate with the sample to allow antigen binding.
- Step 2: Bind DNA-Labelled Antibody. Incubate with a biotinylated detection antibody. Subsequently, add a complex of streptavidin and a single-stranded DNA (ssDNA) template. This ssDNA encodes the target biomarker (for direct amplification) or a universal reporter protein like Streptococcal protein G with an Avi-tag (for surrogate amplification).
- Step 3: Cell-Free Protein Synthesis. Add a cell-free protein synthesis system to the well. This system will use the tethered DNA template to synthesize new copies of the protein.
- Step 4: Detect Synthesized Protein. The newly synthesized proteins will bind to adjacent, unoccupied capture antibodies on the surface. Detect these bound proteins using a conventional ELISA detection system (e.g., an HRP-streptavidin conjugate for an Avi-tagged surrogate).
Troubleshooting:
- High Background Signal: Ensure thorough washing between steps, particularly after adding the DNA-labelled antibody complex. Optimize the concentration of the cell-free synthesis components.
- Low Signal Amplification: Check the activity of the cell-free protein synthesis system. Verify the integrity and functionality of the DNA template conjugated to the detection antibody.
Protocol 2: One-Pot Asymmetric CRISPR Assay (ActCRISPR)
This protocol describes a sensitive, one-pot nucleic acid detection method, optimized for pathogen DNA, that favors trans-cleavage to improve signal [3].
- Step 1: Assemble Reaction. In a single tube, combine the sample DNA with recombinase polymerase amplification (RPA) reagents (500 nM primers, 16.8 nM Mg²⁺) and CRISPR reagents (40 nM Cas12a ribonucleoprotein (RNP) pre-complexed with multiple guide RNAs favoring trans-cleavage, and 600 nM ssDNA reporter).
- Step 2: Isothermal Amplification & Detection. Incubate the reaction at 37-40 °C for 45-60 minutes. The RPA will isothermally amplify the target pathogen DNA. The Cas12a RNP will bind the amplicon and exhibit collateral trans-cleavage of the reporter, generating a fluorescent or lateral flow signal.
- Step 3: Read Results. Measure fluorescence in real-time or at the endpoint. For lateral flow, dip the strip into the reaction mixture and read the visual bands.
Troubleshooting:
- Attenuated or Delayed Signal: This may be due to excessive cis-cleavage (degradation of the amplicon). Titrate the ratios of the multiple gRNAs to further favor trans-cleavage activity. gRNAs targeting non-canonical PAM sites often exhibit this desirable asymmetric activity [3].
- Low Amplification Efficiency: Optimize the concentration of Mg²⁺ and primers in the RPA reaction. Ensure the reaction temperature is maintained consistently within 36-40 °C.
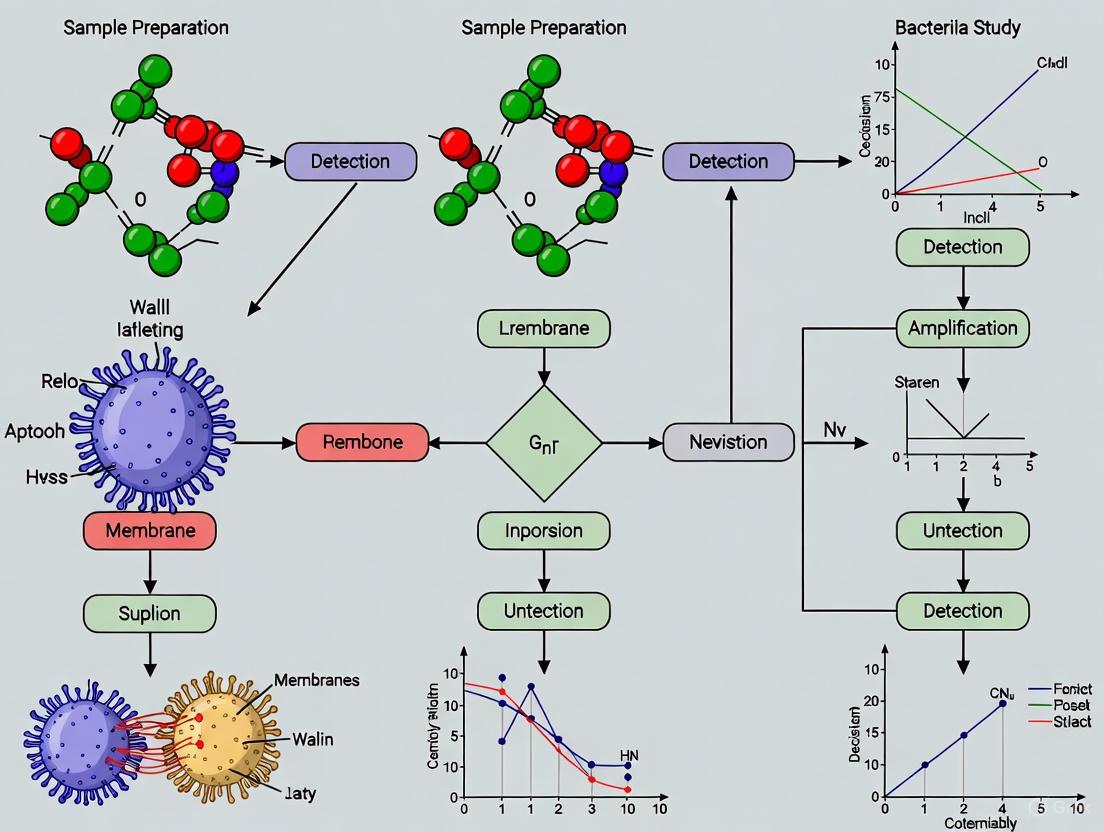
Experimental Workflow Visualization
The following diagrams illustrate the core workflows for the advanced protocols described above.
NATA-ELISA Workflow
One-Pot ActCRISPR Workflow
Researcher's Toolkit: Essential Reagents
The table below lists key reagents required for implementing the advanced sensitivity-bridging techniques discussed.
| Reagent / Material | Function / Description | Example Application |
|---|---|---|
| Cell-Free Protein Synthesis System [1] | An in vitro system for protein production without living cells, enabling target amplification in NATA-ELISA. | NATA-ELISA |
| DNA-Encoded Antibodies [1] | Detection antibodies conjugated to a DNA template that serves as a blueprint for the target protein or a surrogate. | NATA-ELISA, Immuno-PCR |
| Cas12a Ribonucleoprotein (RNP) [3] | A CRISPR-associated complex that binds specific DNA sequences and cleaves a reporter molecule upon activation. | ActCRISPR Assay |
| Trans-Cleavage Favouring gRNAs [3] | Guide RNAs designed to minimize cis-cleavage of the amplicon while maintaining high trans-cleavage activity for signal generation. | ActCRISPR Assay |
| Recombinase Polymerase Amplification (RPA) Kit [3] | An isothermal nucleic acid amplification kit used for rapid target DNA amplification at constant temperature. | ActCRISPR Assay |
| Single-Stranded DNA (ssDNA) Reporter [3] | A short ssDNA molecule labeled with a fluorophore/quencher pair; cleavage by Cas12a generates a fluorescent signal. | ActCRISPR Assay |
Frequently Asked Questions (FAQs)
Q1: Why is there a inherent sensitivity gap between nucleic acid and protein detection methods? The gap primarily exists because of the availability of enzymatic amplification techniques like PCR for nucleic acids, which can exponentially copy a single target molecule. Until recently, no equivalent method existed for proteins, leaving immunoassays like ELISA to rely on signal amplification from a single enzyme molecule [4] [1].
Q2: What are the main advantages of one-pot CRISPR assays over traditional PCR-based methods for nucleic acid detection? One-pot CRISPR assays, like ActCRISPR, integrate target amplification and detection into a single tube. This simplifies the workflow, reduces contamination risk, and can be faster, making it highly suitable for point-of-care or resource-limited settings [3].
Q3: My NATA-ELISA experiment shows high background. What could be the cause? High background in NATA-ELISA is often due to non-specific binding of the DNA-antibody conjugate or uncontrolled protein synthesis. Ensure stringent washing conditions after each binding step and titrate the components of the cell-free expression system to minimize off-target activity [1].
Q4: Can these advanced protein detection methods be multiplexed to detect several biomarkers at once? Yes, methods like NATA-ELISA and Immuno-PCR are inherently suited for multiplexing. By using DNA tags with unique sequences for different antibodies, you can detect multiple targets simultaneously in a single well using a universal detection system, such as a surrogate protein or different PCR amplicons [5] [1].
Q5: How does the use of multiple gRNAs in a CRISPR assay improve sensitivity? Using multiple gRNAs that target different sites on the same amplicon can enhance the overall trans-cleavage activity and signal strength. However, the gRNA combination must be carefully optimized to ensure they do not have strong cis-cleavage activity that would degrade the amplicon and reduce sensitivity [3].
CRISPR-Cas systems have revolutionized biological research and diagnostic applications. Among these, the Class 2 Type V and Type VI systems—featuring the effector proteins Cas12a and Cas13, respectively—exhibit a unique trans-cleavage activity that has been particularly transformative for nucleic acid detection. This activity, triggered upon recognition of a specific target sequence, enables these enzymes to cleave surrounding non-target nucleic acids indiscriminately, providing a powerful signal amplification mechanism. Within the context of improving sensitivity in pathogen detection assays, understanding the distinct properties, troubleshooting common experimental issues, and optimizing the use of Cas12a and Cas13 is paramount for researchers and drug development professionals. This technical support center provides a detailed guide to navigating these powerful systems.
Core System Fundamentals: Cas12a vs. Cas13
What are the fundamental operational differences between Cas12a and Cas13?
Cas12a and Cas13 are both RNA-guided effector proteins from Class 2 CRISPR-Cas systems but target different nucleic acids and possess distinct mechanisms. The table below summarizes their key characteristics, which are crucial for selecting the appropriate system for your application.
Table 1: Fundamental Comparison of Cas12a and Cas13
| Feature | Cas12a (Type V-A) | Cas13 (Type VI) |
|---|---|---|
| Primary Target | Double-stranded DNA (dsDNA) [6] [7] | Single-stranded RNA (ssRNA) [8] [9] |
| Trans-cleavage Substrate | Single-stranded DNA (ssDNA) [10] [7] | Single-stranded RNA (ssRNA) [8] [9] |
| PAM Requirement | Yes (e.g., 5'-TTTV-3') [6] [7] | No PAM; instead, has protospacer flanking site (PFS) preferences [10] |
| Guide RNA | Single crRNA (no tracrRNA needed) [6] [7] | Single crRNA [8] |
| Native Function | Bacterial adaptive immunity against DNA viruses and plasmids [6] | Bacterial adaptive immunity against RNA viruses [8] |
| Key Diagnostic Application | DNA detection (e.g., HPV, SARS-CoV-2 DNA) [10] | RNA detection (e.g., SARS-CoV-2 RNA) [9] [10] |
The following diagram illustrates the core mechanism and trans-cleavage activity for each system.
Frequently Asked Questions (FAQs)
FAQ 1: My Cas12a-based detection assay has low sensitivity. What could be wrong?
Low sensitivity often stems from suboptimal Protospacer Adjacent Motif (PAM) recognition, inefficient crRNA design, or inadequate signal amplification. The PAM sequence (typically 5'-TTTV-3' for Cas12a) is absolutely required for initial target DNA recognition and unwinding [6] [7]. If your target DNA lacks a compatible PAM, Cas12a will not bind. Furthermore, ensure your crRNA spacer sequence is specific and has minimal potential for off-target binding. For detecting low-abundance targets, always couple the CRISPR reaction with a pre-amplification step like Recombinase Polymerase Amplification (RPA) or Loop-Mediated Isothermal Amplification (LAMP) [10]. The "HOLMES" and "DETECTR" platforms are examples of Cas12a assays that use pre-amplification to achieve attomolar (aM) sensitivity [9] [10].
FAQ 2: Why is my Cas13 assay producing high background (false positive) signals?
High background in Cas13 assays is frequently caused by reagent contamination or non-specific activation of the Cas13 protein. Cas13's trans-cleavage activity is powerfully activated upon binding its specific RNA target, but it can sometimes be triggered non-specifically. To troubleshoot:
- Meticulous Lab Practice: Use dedicated pre- and post-amplification workspaces and UV irradiation to degrade contaminating nucleic acids.
- Optimize crRNA: Ensure your crRNA does not have significant homology to non-target sequences present in the reaction. A single mismatch may not always prevent activation, but double mismatches, especially at positions 3-5, can significantly reduce it [11].
- Check Reporter Integrity: Degraded or improperly quenched fluorescent reporters can lead to high background. Aliquot and store reporters properly.
FAQ 3: Can I use Cas12a and Cas13 in a single reaction for multiplexed detection?
Yes, the distinct nucleic acid targets (DNA for Cas12a, RNA for Cas13) and trans-cleavage substrates (ssDNA reporter for Cas12a, ssRNA reporter for Cas13) allow for multiplexing in a single pot [10]. This enables the simultaneous detection of a DNA virus and an RNA virus, for example. The key is to use two different reporters—for instance, one ssDNA reporter labeled with a HEX fluorophore and one ssRNA reporter labeled with a FAM fluorophore. Each will be cleaved exclusively by the activated Cas12a or Cas13 system, respectively, allowing for independent signal detection on different channels.
FAQ 4: How does RNA secondary structure affect my Cas13 assay, and how can I mitigate it?
RNA structure can significantly inhibit Cas13 activity by blocking access of the Cas13-crRNA complex to the target protospacer [12]. Structured regions compete with the crRNA for base pairing. A recent study quantitatively explained this through a kinetic strand displacement model, where Cas13 must displace the occluding structure to bind, which can reduce activity by an order of magnitude or more [12]. To mitigate this:
- crRNA Design: Use computational tools to predict secondary structure in your target RNA and design crRNAs that target regions with minimal predicted structure.
- Use Multiple crRNAs: Employing a pool of crRNAs targeting different regions of the same RNA increases the probability that at least one will access an unstructured site, enhancing overall sensitivity [11].
- Assay Conditions: Incubating the reaction at a higher temperature (e.g., 50-55°C for LwaCas13a) can help melt secondary structures, though this must be balanced with enzyme stability.
Troubleshooting Guides
Troubleshooting Low Signal in Cas12a/Cas13 Detection Assays
Table 2: Troubleshooting Low Signal in Trans-cleavage Assays
| Problem | Potential Causes | Solutions |
|---|---|---|
| No or Weak Signal | 1. Target concentration below limit of detection.2. Inefficient or failed pre-amplification.3. Suboptimal Mg²⁺ concentration.4. Incorrect PAM (for Cas12a) or problematic PFS (for Cas13).5. crRNA designed against a highly structured region (Cas13). | 1. Include a pre-amplification step (RPA/LAMP/PCR). Validate amplification separately.2. Titrate Mg²⁺, as it is a critical cofactor for both amplification and Cas activity.3. Verify the target sequence contains a valid PAM (e.g., TTTV) [7]. For Cas13, avoid a G base immediately following the protospacer [10].4. Re-design crRNA to target a different, more accessible site. |
| Inconsistent Signal Between Replicates | 1. Pipetting errors with viscous samples or reagents.2. Inefficient mixing of reaction components.3. Fluctuations in isothermal amplification temperature. | 1. Use master mixes for critical reagents to minimize pipetting variability.2. Centrifuge tubes briefly before incubation and vortex thoroughly.3. Use a calibrated heat block or water bath. |
| Signal is Delayed | 1. Low reaction temperature.2. Suboptimal crRNA:target ratio.3. Partially inactive protein or nucleasedamaged reporters. | 1. Ensure the reaction is performed at the optimal temperature for the Cas ortholog (e.g., 37-42°C for LbCas12a).2. Titrate the crRNA concentration.3. Use fresh, high-quality reagents. |
Troubleshooting Specificity Issues: False Positives and Off-Target Effects
Table 3: Troubleshooting Specificity Issues
| Problem | Potential Causes | Solutions |
|---|---|---|
| False Positive (No target control is positive) | 1. Amplicon or nucleic acid contamination.2. Non-specific activation of Cas protein.3. Impure oligonucleotide synthesis. | 1. Implement strict physical separation of pre- and post-amplification areas. Use uracil-DNA glycosylase (UDG) treatment to carryover contamination.2. Include an appropriate negative control crRNA (targeting a non-existent sequence).3. Purify crRNAs and oligos via HPLC or PAGE. |
| Inability to Discriminate Single-Nucleotide Variants (SNPs) | 1. crRNA tolerance to single mismatches.2. Over-amplification leading to high target concentration that saturates the system. | 1. Intentionally design crRNAs with a mismatch at the SNP site or utilize an "occluded" Cas13 design that enhances mismatch discrimination [12].2. Reduce the number of amplification cycles or time and titrate the amplified product volume added to the CRISPR reaction. |
Experimental Protocols
Detailed Protocol: SHERLOCK-like Assay for SARS-CoV-2 RNA Detection using Cas13
This protocol is adapted from the SHERLOCK (Specific High-sensitivity Enzymatic Reporter unLOCKing) platform, which is designed for highly sensitive and specific RNA detection [9] [10].
Principle: Target RNA is first converted to DNA and isothermally amplified. The amplicon is then transcribed back to RNA, which is detected by the Cas13-crRNA complex. Activation of Cas13 upon target binding leads to trans-cleavage of an RNA reporter, generating a fluorescent signal.
Workflow:
Materials & Reagents:
- Purified LwaCas13a or LbuCas13a protein
- Target-specific crRNA: Designed against a conserved region of the SARS-CoV-2 genome (e.g., N-gene or E-gene).
- RT-RPA Kit: For combined reverse transcription and isothermal amplification.
- T7 RNA Polymerase: For in vitro transcription.
- Fluorescent RNA Reporter: A short ssRNA oligonucleotide labeled with a 5' fluorophore (e.g., FAM) and a 3' quencher (e.g., Iowa Black FQ).
- Nuclease-free water and tubes.
Step-by-Step Procedure:
- Sample Preparation & Amplification:
- In a first reaction tube, set up a 50 µL RT-RPA reaction according to the manufacturer's instructions, using primers designed to amplify a ~100-200 bp region of the SARS-CoV-2 genome. Include a T7 promoter sequence in the forward primer.
- Incubate the RT-RPA reaction at 42°C for 20-30 minutes.
Cas13 Detection Reaction Setup:
- Prepare a master mix for the detection reaction on ice. For a single 20 µL reaction:
- 1 µL Cas13 protein (100-200 nM)
- 1 µL crRNA (100-200 nM)
- 1 µL RNA Reporter (100-200 nM)
- 11.5 µL Nuclease-free water
- 0.5 µL Ribonuclease Inhibitor (optional)
- Aliquot 15 µL of the master mix into a new tube or plate.
- Prepare a master mix for the detection reaction on ice. For a single 20 µL reaction:
Reaction Initiation & Readout:
- Add 5 µL of the completed RT-RPA reaction (or a 1:10 dilution thereof) to the 15 µL detection master mix.
- Mix thoroughly by pipetting and briefly centrifuge.
- Immediately transfer to a real-time PCR instrument or fluorescent plate reader.
- Incubate at 37°C and measure fluorescence every 30 seconds for 10-30 minutes.
- A sharp increase in fluorescence over time indicates a positive detection.
The Scientist's Toolkit: Essential Reagents for CRISPR Detection
Table 4: Key Research Reagent Solutions
| Reagent / Material | Function / Explanation |
|---|---|
| Cas12a/Cas13 Effector Protein | The core enzyme that, upon target recognition, performs cis- and trans-cleavage. Common orthologs include LbCas12a and AacCas12b; LwaCas13a and LbuCas13a [9] [13]. |
| crRNA (CRISPR RNA) | A short RNA molecule consisting of a direct repeat (scaffold) that binds the Cas protein and a spacer sequence that guides it to the target nucleic acid. It requires only a single RNA for both Cas12a and Cas13 [6] [8]. |
| Fluorescent Reporter | A quenched oligonucleotide (ssDNA for Cas12a, ssRNA for Cas13) that, when cleaved during trans-cleavage, produces a fluorescent signal. This is the primary detection readout [9] [10]. |
| Isothermal Amplification Kits (RPA/LAMP) | Enzymatic kits for amplifying nucleic acids at a constant temperature, enabling simple instrumentation and coupling with CRISPR detection in one-pot or two-step assays [10]. |
| Microfluidic Chamber Array | A device containing millions of femtoliter-sized chambers used in digital detection methods (e.g., SATORI) to achieve single-molecule sensitivity without target pre-amplification, reducing errors and time [11]. |
| Uracil-DNA Glycosylase (UDG) | An enzyme used in pre-amplification steps to prevent carryover contamination by degrading uracil-containing DNA amplicons from previous reactions. |
| Ribonuclease Inhibitor | A protein added to Cas13 reactions to protect the crRNA, target RNA, and RNA reporter from degradation by environmental RNases. |
Troubleshooting Guide: Common Issues in One-Pot Assay Development
FAQ 1: Why does my one-pot CRISPR assay show delayed or attenuated signal compared to my two-step assay?
Problem: The integrated one-pot assay exhibits slower signal generation and reduced overall signal intensity, limiting detection sensitivity.
Root Cause: This is primarily due to competitive cis-cleavage activity of the Cas protein on the RPA amplicon. In a one-pot reaction, the Cas complex (e.g., Cas12a) binds to the target sequence and can cleave both the amplicon itself (cis-cleavage, which degrades the target) and the fluorescent reporter (trans-cleavage, which generates signal). Excessive cis-cleavage depletes the amplicon before significant amplification can occur, undermining the assay's efficiency [14] [3].
Solutions:
- Utilize guide RNAs (gRNAs) with asymmetric cleavage activity: Select or design gRNAs that favor trans-cleavage over cis-cleavage. These are often gRNAs targeting sequences with non-canonical Protospacer Adjacent Motifs (PAMs). For example, in a tuberculosis assay (ActCRISPR-TB), gRNA-5 demonstrated superior kinetics because its trans-cleavage activity was preserved while its cis-cleavage activity was weakened [14] [3].
- Employ a multi-guide RNA strategy: Combine multiple gRNAs that favor trans-cleavage and target distinct sites on the amplicon. A combination of gRNA-2, -3, and -5 in the ActCRISPR-TB assay achieved a limit of detection (LoD) of 5 copies/μL, which was 20 times more sensitive than using a canonical gRNA (gRNA-0) alone [14] [3].
- Implement thermal regulation: Use Cas proteins with different temperature optima to temporally separate the amplification and detection phases. The TRACE assay uses Cas12b. An initial lower temperature (37°C) favors RPA amplification, while a subsequent temperature shift (to 60°C) maximizes Cas12b detection activity, preventing amplicon degradation during the critical amplification phase [15].
- Use a single-stranded RNA (ssRNA) blocker: To further prevent early Cas activity, an ssRNA complementary to the gRNA spacer region can be added. This blocker binds the gRNA during the amplification phase, inhibiting Cas RNP complex formation and cis-cleavage. It dissociates upon a temperature increase, restoring full Cas activity for detection [15].
FAQ 2: My one-pot assay has high background noise. How can I improve the signal-to-noise ratio?
Problem: The assay produces significant signal even in no-template control samples, leading to potential false positives and difficulty in interpreting weak positive results.
Root Cause: High background can stem from several factors, including non-specific amplification, premature trans-cleavage activity triggered by non-target molecules, or suboptimal reagent concentrations.
Solutions:
- Optimize guide RNA specificity: Carefully design gRNAs to ensure high target specificity and avoid off-target binding. Use bioinformatics tools to check for unique sequences within the target genome and minimize homology with non-target sequences [14] [16].
- Fine-tune Mg²⁺ concentration: Increasing Mg²⁺ concentration can reduce assay signal and background. Systematically titrate Mg²⁺ to find the level that minimizes background without compromising the true positive signal [14] [3].
- Adjust reporter concentration: While a 600 nM reporter concentration was selected in the ActCRISPR-TB assay to minimize background and cost, testing different concentrations can help optimize the signal-to-noise ratio for your specific setup [14] [3].
- Validate gRNAs for primer overlap: Ensure your gRNA sequences do not overlap with the RPA primer sequences, as this can cause template-independent signal generation and high background, as was observed with gRNA-6 in the ActCRISPR-TB study [14] [3].
FAQ 3: How can I adapt my one-pot assay for point-of-care use with lateral flow readout?
Problem: The assay needs to be simplified for use in resource-limited settings without fluorescent readers.
Solution: The core optimized one-pot chemistry is often directly compatible with lateral flow assay (LFA) formats. The ActCRISPR-TB assay demonstrated that transitioning from a fluorescent readout to an LFA format resulted in no loss of analytical or diagnostic sensitivity. This allows for visual detection of results using self-collected samples like tongue swabs, making it suitable for decentralized testing [14] [3]. The TRACE assay was also designed to meet ASSURED criteria (Affordable, Sensitive, Specific, User-friendly, Rapid and robust, Equipment-free, and Deliverable), which is a key benchmark for point-of-care tests [15].
Experimental Protocols: Key Methodologies
Protocol 1: Identifying gRNAs with Favorable Asymmetric Cleavage Activity
This protocol is based on the development of the ActCRISPR-TB assay [14] [3].
- Tile the Target Amplicon: Identify a series of candidate gRNA sequences that tile across your target amplicon sequence (e.g., within the IS6110 element for TB).
- Include Non-Canonical PAMs: deliberately include candidates that bind to sequences with non-canonical PAM sites (not TTTV for Cas12a).
- Analyze Secondary Structures: Use software to predict secondary structures of candidate gRNAs and select those with stable configurations.
- Test Cis- and Trans-Cleavage Activities:
- Incubate each Cas RNP (with its unique gRNA) with a dsDNA substrate (the target).
- Use gel electrophoresis or a similar method to monitor the depletion of the dsDNA substrate over time. This measures cis-cleavage activity.
- In a parallel reaction, include a quenched ssDNA reporter. Monitor the fluorescence increase over time to measure trans-cleavage activity.
- Normalize and Compare: Normalize the cis- and trans-cleavage activities of each gRNA to a canonical gRNA (e.g., gRNA-0). Select gRNAs that exhibit low normalized cis-cleavage activity but high normalized trans-cleavage activity (e.g., gRNA-4, gRNA-5).
- Validate in One-Pot Format: Test the top-performing gRNAs individually in a one-pot RPA-CRISPR reaction to confirm improved reaction kinetics.
Protocol 2: Implementing a Thermally Regulated Asynchronous (TRACE) Assay
This protocol is adapted from the TRACE assay for MPXV detection [15].
- Reaction Setup: Prepare a one-pot master mix containing:
- RPA reagents (primers, enzymes).
- Cas12b protein and its specific gRNA.
- A single-stranded RNA (ssRNA) blocker complementary to the gRNA spacer.
- A fluorescent or lateral-flow-compatible poly-T ssDNA reporter.
- The template DNA.
- Thermal Cycling:
- Stage 1 - Amplification: Incubate the reaction at 37°C for 10 minutes. During this phase, RPA amplification proceeds efficiently. The ssRNA blocker binds to the gRNA, significantly inhibiting Cas12b cis-cleavage activity and preventing amplicon degradation.
- Stage 2 - Detection: Immediately transfer the reaction to 60°C for 30 minutes. The higher temperature causes the ssRNA blocker to dissociate from the gRNA, activating the Cas12b RNP complex. The amplified target is now detected via trans-cleavage of the reporter.
- Readout: Measure fluorescence at the endpoint of Stage 2 or apply the reaction to a lateral flow strip for visual interpretation.
The Scientist's Toolkit: Essential Reagents for Optimization
The following table summarizes key reagents and their optimized roles based on the cited research.
Table 1: Key Research Reagent Solutions for One-Pot Assay Optimization
| Reagent / Tool | Function & Rationale | Example from Literature |
|---|---|---|
| Non-Canonical gRNAs | Guide RNAs targeting sequences with suboptimal PAMs to reduce cis-cleavage of the amplicon while preserving trans-cleavage for signal generation. | gRNA-5 for IS6110 target, which showed optimal asymmetric activity [14] [3]. |
| Multi-gRNA Cocktails | Using multiple gRNAs targeting different sites on the same amplicon to enhance signal and lower the limit of detection. | A combination of gRNA-2, gRNA-3, and gRNA-5 improved LoD to 5 copies/μL [14] [3]. |
| ssRNA Blockers | Short RNA strands that temporarily inhibit Cas RNP activity during the amplification phase by binding to the gRNA, preventing amplicon degradation. | ssRNA 1-S14 used in the TRACE assay to block Cas12b during the 37°C RPA phase [15]. |
| Cas12b Protein | A Cas protein with a higher temperature optimum (up to 60°C), enabling thermal separation of RPA (37°C) and CRISPR detection (60°C). | Used in the TRACE assay for MPXV to achieve an LoD of 2.5 copies/test [15]. |
| Magnesium (Mg²⁺) | A critical co-factor whose concentration must be optimized; increases can reduce assay signal and background. | An optimal concentration of 16.8 nM was used in the ActCRISPR-TB assay [14] [3]. |
Visualizing Workflows and Strategies
Diagram 1: Core Challenge in One-Pot Assays - Competitive Cleavage
Diagram 2: Multi-gRNA Strategy for Enhanced Sensitivity
Diagram 3: Thermally Programmed Workflow (TRACE Assay)
In the field of molecular diagnostics, particularly in sensitive pathogen detection, two metrics are fundamental for evaluating assay performance: the Limit of Detection (LoD) and Variant Allele Frequency (VAF). The LoD defines the lowest quantity of an analyte that can be reliably distinguished from its absence, while the VAF measures the proportion of sequencing reads that carry a specific mutation. Understanding and optimizing these parameters is crucial for developing assays that can detect low-abundance pathogens and their genetic variations, which is a core focus of research aimed at improving diagnostic sensitivity for diseases like tuberculosis. This guide provides a technical framework for troubleshooting common issues related to these key metrics.
Limit of Detection (LoD): Core Concepts and Definitions
What is the Limit of Detection (LoD) and how is it statistically defined?
The Limit of Detection (LoD) is the lowest concentration or quantity of an analyte that can be reliably distinguished from a blank sample (one containing no analyte) with a stated confidence level [17] [18]. It is not a fixed value but a statistical concept that balances the risks of false positives and false negatives [17].
- Key Statistical Definitions:
- Limit of Blank (LoB): The highest apparent analyte concentration expected to be found when replicates of a blank sample are tested. It is calculated as
LoB = mean_blank + 1.645(SD_blank), which establishes a threshold where no more than 5% of blank measurements will exceed it (false positive rate of 5%) [19]. - Limit of Detection (LoD): The lowest analyte concentration that can be reliably distinguished from the LoB. It is calculated using both the LoB and a low-concentration sample:
LoD = LoB + 1.645(SD_low concentration sample)[19]. This formula ensures that a sample at the LoD will be incorrectly classified as a blank less than 5% of the time (false negative rate of 5%) [17] [19].
- Limit of Blank (LoB): The highest apparent analyte concentration expected to be found when replicates of a blank sample are tested. It is calculated as
The following diagram illustrates the statistical relationship and calculation basis for LoB and LoD.
What is the difference between LoD and Limit of Quantitation (LoQ)?
The Limit of Quantitation (LoQ) is the lowest concentration at which an analyte can not only be reliably detected but also measured with acceptable precision and accuracy [18] [19]. While the LoD is about confirming the presence of an analyte, the LoQ is about reliably measuring its amount. The LoQ is always at a concentration equal to or higher than the LoD [19].
Table: Key Differences between LoB, LoD, and LoQ
| Parameter | Definition | Sample Type Used | Primary Goal |
|---|---|---|---|
| Limit of Blank (LoB) | Highest apparent concentration expected from a blank sample. | Sample containing no analyte. | Establish the threshold for false positives. |
| Limit of Detection (LoD) | Lowest concentration reliably distinguished from the LoB. | Blank sample and sample with low analyte concentration. | Define the lowest concentration for reliable detection. |
| Limit of Quantitation (LoQ) | Lowest concentration measured with acceptable precision and accuracy. | Sample with analyte concentration at or above the LoD. | Define the lowest concentration for reliable measurement. |
Variant Allele Frequency (VAF): A Guide for Molecular Pathology
What is Variant Allele Frequency (VAF) and how is it calculated?
In molecular pathology, the Variant Allele Frequency (VAF), also known as variant allele fraction, is the proportion of sequencing reads that carry a specific mutation or variant at a particular genomic location [20]. It is calculated as:
VAF = (Number of mutated sequencing reads) / (Total number of sequencing reads at that locus) [20]
For example, if 6 out of 50 sequencing reads at a specific genomic position show a mutation, the VAF is 12% [20].
How is VAF used to interpret genetic variants?
The VAF is a critical metric for inferring the origin and biological significance of a genetic variant, especially in the context of cancer and liquid biopsies.
- Germline Variants: Heterozygous germline variants are expected to have a VAF of approximately 50%, while homozygous variants have a VAF close to 100% [20].
- Somatic Variants and Mosaicism: VAFs less than 50% but above the assay's detection limit can indicate mosaicism (where a mutation occurs after fertilization and is not present in all cells) or a somatic mutation in a mixed cell population [20].
- Liquid Biopsies and Tumor Heterogeneity: In liquid biopsies, cell-free tumor DNA (ctDNA) is a small fraction of the total cell-free DNA. Consequently, VAFs for tumor-derived variants can be very low (e.g., down to 0.1%), reflecting the tumor's genetic heterogeneity and burden [20]. At these low levels, distinguishing true variants from sequencing errors becomes a major challenge, directly related to the assay's LoD [20].
The diagram below shows how VAF helps infer the origin of a genetic variant.
Troubleshooting Common Experimental Issues
FAQ: Our assay's LoD is higher than desired. What are the main factors that influence LoD and how can we improve it?
A high LoD is often driven by excessive background noise or suboptimal signal generation. Key factors and improvement strategies include:
- Factor 1: Assay Chemistry and Design. The fundamental biochemical reactions can be optimized to favor signal detection.
- Solution: In CRISPR-based assays, using guide RNAs (gRNAs) that favor trans-cleavage activity (which generates the detectable signal) over cis-cleavage activity (which degrades the target amplicon) can significantly improve LoD. One study achieved a 20-fold lower LoD (5 copies/μL) by selecting such gRNAs [3].
- Factor 2: Signal-to-Noise Ratio. A low signal relative to background noise obscures detection.
- Solution: In chromatography, the LoD is often defined as a signal-to-noise ratio (S/N) of 3:1 [17]. Ensure your detection instrument is optimally configured and consider methods to reduce background noise, such as optimizing wash steps or using different reporters.
- Factor 3: Sample Matrix Effects. The sample itself can interfere with the assay.
- Solution: Use a sample for LoD determination that is commutable with real patient specimens to account for matrix effects [19]. Proper sample preparation and purification are critical.
- Factor 4: Reagent Quality and Concentration. Suboptimal reagent conditions can limit reaction efficiency.
- Solution: Systematically optimize concentrations of key reagents like primers, magnesium, and enzymes. For example, in the ActCRISPR-TB assay, optimizing primer and RNP concentrations was a key step in maximizing signal and kinetics [3].
FAQ: We are detecting low VAF variants, but are concerned they might be artifacts. How can we validate them?
Distinguishing true low-VAF variants from technical artifacts is a major challenge in next-generation sequencing (NGS).
- Strategy 1: Establish a VAF Cutoff. Set a conservative VAF threshold based on your assay's validated performance. One study of medical exome sequencing found that all clinically relevant single-nucleotide variants had a VAF between 0.33 and 0.63, while 82% of technical artifacts had a VAF below 0.33. Implementing a cutoff of 0.30 for manual review reduced curation time by 20% without missing real variants [21].
- Strategy 2: Use Ultrasensitive NGS Methods. Standard NGS has a high error rate (~0.5% per base), making it unreliable for VAFs below 1% [22]. Employ specialized methods that generate consensus sequences from multiple reads of the original DNA molecule. These include:
- Strategy 3: Independent Validation. Confirm findings using an orthogonal method with a different detection chemistry (e.g., digital PCR) to rule out method-specific artifacts.
FAQ: How do LoD and VAF relate to each other in the context of pathogen detection?
LoD and VAF are interconnected concepts when detecting low levels of pathogen DNA, especially in a background of host DNA.
- The Relationship: The LoD of your assay defines the minimum number of pathogen DNA molecules required for a positive detection. The VAF in this context is the proportion of all DNA molecules (host + pathogen) that are derived from the pathogen. A positive detection requires that the pathogen DNA concentration is above the assay's LoD, which typically means the VAF must be above a certain threshold.
- Practical Implication: In a sample with a high amount of host DNA, the VAF of a pathogen sequence will be very low. To detect it, your assay must have a sufficiently sensitive LoD to find the absolute number of pathogen molecules within that large pool. For example, a CRISPR-TB assay with an LoD of 5 copies/μL was able to detect Mycobacterium tuberculosis in patient samples where the pathogen DNA was present at a very low frequency [3].
Essential Research Reagent Solutions
The following table lists key reagents and their functions in developing sensitive detection assays, as exemplified by the search results.
Table: Key Reagents for Sensitive Pathogen Detection Assays
| Reagent / Material | Function in the Assay | Example from Literature |
|---|---|---|
| Cas12a Ribonucleoprotein (RNP) | CRISPR-associated protein complex that binds target DNA and cleaves a reporter molecule upon recognition. | Core component of the ActCRISPR-TB assay for specific Mtb DNA detection [3]. |
| Asymmetric gRNAs | Guide RNAs engineered to favor trans-cleavage activity over cis-cleavage, improving signal amplification and LoD. | Use of gRNA-5 in ActCRISPR-TB to reduce amplicon degradation and enhance kinetics [3]. |
| Multi-gRNA Cocktails | Using multiple distinct gRNAs targeting the same amplicon to increase signal intensity and improve LoD. | Combining gRNA-2, -3, and -5 in ActCRISPR-TB to achieve an LoD of 5 copies/μL [3]. |
| Recombinase Polymerase Amplification (RPA) Reagents | Enzymes and buffers for isothermal nucleic acid amplification, enabling rapid target pre-amplification. | Used for target amplification in the one-pot ActCRISPR-TB assay [3]. |
| Hybrid Capture Probes | Target-specific oligonucleotide probes used to enrich pathogen DNA from a complex sample prior to NGS. | Used in the RP-MT-Capture NGS assay to enrich over 300 respiratory pathogen targets, improving sensitivity [23]. |
| ssDNA Fluorescent Reporter | A single-stranded DNA molecule coupled to a fluorophore/quencher pair; cleavage by Cas12a generates a fluorescent signal. | Reporter molecule used for real-time detection in the CRISPR-based assay [3]. |
Detailed Experimental Protocol: Estimating LoD for a Chromatographic Method
The following protocol, based on established guidelines, provides a robust method for determining the LoD [17] [19].
Preparation:
- Obtain a test sample with a low concentration of the analyte, close to the expected LoD. Ideally, this should be in a real sample matrix.
- Prepare a blank sample (containing no analyte).
Analysis:
- Analyze a minimum of 10 (ideally 20 for verification, 60 for establishment) replicate portions of the blank sample, following the complete analytical procedure.
- Analyze a minimum of 10 (ideally 20 for verification, 60 for establishment) replicate portions of the low-concentration test sample.
Data Conversion:
- Convert the raw instrument signals (e.g., peak height, area) to concentration values using a calibration curve.
Calculation:
- For the blank measurements, calculate the mean (
mean_blank) and standard deviation (SD_blank). - Calculate the Limit of Blank (LoB) as:
LoB = mean_blank + 1.645(SD_blank). - For the low-concentration sample measurements, calculate the standard deviation (
SD_low). - Calculate the Limit of Detection (LoD) as:
LoD = LoB + 1.645(SD_low).
- For the blank measurements, calculate the mean (
Verification (as per EP17 guidelines):
- Analyze several samples with a concentration at the calculated LoD. If more than 5% of the results fall below the LoB, the LoD estimate is too low and should be re-estimated at a slightly higher concentration [19].
Cutting-Edge Workflows: From CRISPR Engineering to Synthetic Biology
Technical Support Center: Troubleshooting Guides and FAQs
Frequently Asked Questions (FAQs)
FAQ 1: What is the primary advantage of using a multi-guide RNA strategy in Cas12a assays? Using multiple guide RNAs (gRNAs) that target distinct sites on the same pathogen's DNA significantly enhances the signal and sensitivity of the assay. This approach increases the chances of Cas12a activation and amplifies the trans-cleavage activity, leading to a stronger detection signal, which is crucial for identifying low-abundance pathogens [3].
FAQ 2: My one-pot Cas12a assay has low sensitivity. Could my gRNA design be the issue? Yes. Traditional gRNAs with strong cis-cleavage activity (cutting the target amplicon) can compete with the trans-cleavage activity (cutting the reporter) that generates your signal. Using gRNAs engineered to have asymmetric cleavage activity—favoring trans-cleavage over cis-cleavage—can prevent amplicon degradation, allowing for greater target accumulation and a stronger signal in one-pot assays [3].
FAQ 3: How do I select gRNAs for a multi-guide RNA assay? Not all gRNA combinations are effective. It is essential to tile the target sequence and empirically test the cis- and trans-cleavage activities of individual gRNA candidates [3]. The table below summarizes performance data for different gRNAs targeting the M. tuberculosis IS6110 element, which can serve as a reference for selection criteria.
Table: Performance Characteristics of Example gRNAs for Cas12a Assays
| gRNA Name | PAM Type | Relative Cis-Cleavage Activity | Relative Trans-Cleavage Activity | Suitability for One-Pot Assays |
|---|---|---|---|---|
| gRNA-0 | Canonical (TTTV) | Very Strong | Very Strong (100%) | Low (high amplicon degradation) |
| gRNA-2 | Non-canonical | Strong | Very Strong (comparable to gRNA-0) | Moderate |
| gRNA-5 | Non-canonical | Weaker than gRNA-0 | Very Strong (comparable to gRNA-0) | High |
| gRNA-4 | Non-canonical | Weak | Moderate (42% of gRNA-0) | High |
| gRNA-1 | Non-canonical | Weak | Low (12% of gRNA-0) | Low |
Source: Adapted from Nature Communications (2025) 16:8257 [3].
FAQ 4: Why are the relative ratios of gRNAs important in a multi-guide setup? The ratio of gRNAs in the reaction mixture is critical because gRNAs with strong cis-cleavage activity can dominate and degrade the amplicon if present in high concentrations, thereby reducing sensitivity. For example, a mixture favoring the asymmetric gRNA-5 over the strong cis-cleaving gRNA-2 (e.g., a 30:10 ratio) enhanced assay kinetics, while a ratio favoring gRNA-2 (10:30) markedly attenuated the signal [3].
Troubleshooting Common Experimental Issues
Table: Troubleshooting Guide for Multi-guide RNA Cas12a Assays
| Problem | Potential Cause | Recommended Solution |
|---|---|---|
| High background noise or false positives | Non-specific activation of Cas12a; gRNA sequence overlap with primers. | Check all gRNA sequences for homology with primer sequences. Exclude gRNAs with any overlap (e.g., >10 nt) with primers [3]. |
| Low signal or false negatives in one-pot assay | Competitive cis-cleavage of amplicon depletes the target; suboptimal reaction conditions. | Use gRNAs with asymmetric cleavage activity (high trans-, low cis-). Systematically optimize Mg2+ concentration, primer concentration, and RNP complex concentration [3]. |
| Poor limit of detection (LoD) | Insufficient signal amplification from a single gRNA. | Implement a multi-gRNA strategy. A combination of gRNA-2, -3, and -5 was shown to achieve a LoD of 5 copies/μL, a 20-fold improvement over a single canonical gRNA [3]. |
| Inconsistent results between replicates | Unstable crRNA components; suboptimal reassembly kinetics in split systems. | For advanced designs using split crRNA technology, optimize fragment lengths, hybridization stability, and sequence complementarity to improve reassembly efficiency [24]. |
Experimental Protocol: Establishing a Multi-guide RNA Cas12a Assay
The following protocol is adapted from the "ActCRISPR-TB" assay for sensitive detection of Mycobacterium tuberculosis [3].
1. gRNA Design and Selection
- Target Identification: Identify a unique, multi-copy sequence element specific to the target pathogen (e.g., IS6110 for Mtb).
- gRNA Tiling: Tile the target sequence to design several gRNA candidates, including those with non-canonical Protospacer Adjacent Motifs (PAMs).
- In vitro Screening: Express and purify each gRNA candidate. Test them individually in a cleavage assay to quantify their:
- Cis-cleavage activity: Measure the depletion of a dsDNA substrate.
- Trans-cleavage activity: Measure the cleavage of a fluorescent ssDNA reporter.
- Selection: Prioritize gRNAs that exhibit high trans-cleavage activity but low cis-cleavage activity (asymmetric cleavage).
2. Assay Optimization and Validation
- Reaction Setup: Develop a one-pot reaction that integrates recombinase polymerase amplification (RPA) and CRISPR detection in a single tube.
- Parameter Optimization:
- Primer Concentration: Test a range (e.g., 100-500 nM).
- Mg2+ Concentration: A critical co-factor; test a range (e.g., 12-20 nM).
- RNP Concentration: Test Cas12a-gRNA complex concentrations (e.g., 20-60 nM).
- Multi-guide Formulation: Combine the top-performing asymmetric gRNAs (e.g., gRNA-5, gRNA-2, gRNA-3) at optimized ratios. Keep the total gRNA concentration constant while varying individual ratios.
- Performance Assessment:
- Limit of Detection (LoD): Determine the lowest copy number of target DNA that can be reliably detected.
- Specificity: Test against a panel of non-target pathogens to confirm specificity.
- Kinetics: Establish the time-to-signal for positive samples.
Visualizing the Multi-guide RNA Cas12a Workflow
The diagram below illustrates the streamlined workflow for a one-pot assay using multiple gRNAs.
The Scientist's Toolkit: Essential Research Reagents
Table: Key Reagents for Multi-guide RNA Cas12a Pathogen Detection
| Reagent / Tool | Function / Description | Example & Notes |
|---|---|---|
| Asymmetric gRNAs | Guide RNAs engineered for high trans-cleavage and low cis-cleavage activity to maximize signal in one-pot assays. | gRNA-5, gRNA-4 from the IS6110 target [3]. |
| Cas12a Nuclease | The effector enzyme that, upon guided recognition of target DNA, cleaves the target and exhibits collateral trans-cleavage. | Can be sourced from various suppliers; LbCas12a and AsCas12a are common variants. |
| Isothermal Amplification Mix | Enables nucleic acid amplification at a constant temperature to boost target copy number before detection. | Recombinase Polymerase Amplification (RPA) or LAMP kits [3] [25]. |
| Fluorescent Reporter | A single-stranded DNA oligonucleotide labeled with a fluorophore and quencher; cleavage generates a fluorescent signal. | Often an ssDNA oligo labeled with FAM (fluorophore) and BHQ (quencher) [25]. |
| gRNA Design Tools | Computational tools to design gRNA sequences with high on-target and low off-target potential. | Synthego CRISPR Design Tool, Benchling CRISPR Design Tool [26]. |
| Split Technology Components | For advanced assays: Split crRNA or activator fragments that reassemble only in the presence of the target, enhancing specificity. | Truncated crRNA (tcrRNA) and complementary activator strands [24]. |
A significant challenge in molecular diagnostics, particularly for diseases like Tuberculosis (TB), is achieving clinically relevant sensitivity with streamlined, point-of-care compatible assays. Conventional CRISPR assays often lack the requisite sensitivity for direct clinical utility, primarily due to complex workflows and competitive reactions that limit target accumulation [3] [14]. This case study examines the development of ActCRISPR-TB, an asymmetric cis/trans CRISPR cleavage assay that achieves a remarkable sensitivity of 5 copies/μL within 60 minutes [3]. We will explore the technical foundations of this assay, provide detailed experimental protocols, and establish a technical support framework to assist researchers in implementing and troubleshooting this advanced diagnostic platform.
Core Technology: Principles of the Asymmetric Cis/Trans Cleavage Assay
The Fundamental Problem: Competitive Cis-Cleavage in One-Pot Assays
Traditional one-pot CRISPR assays combine target amplification (e.g., via Recombinase Polymerase Amplification - RPA) and detection in a single reaction vessel. However, they face a critical limitation: the Cas enzyme's cis-cleavage activity (cutting of the target amplicon) competes with the amplification process, reducing overall amplification efficiency and limiting sensitivity [3] [27]. This competition between amplicon production and degradation creates a fundamental sensitivity barrier in one-pot formats.
The ActCRISPR-TB Solution: Engineering Trans-Cleavage Preference
ActCRISPR-TB addresses this limitation through a novel guide RNA (gRNA) engineering strategy that favors trans-cleavage (collateral cleavage of reporter molecules) over cis-cleavage [3]. The key innovation involves using multiple gRNAs targeting sequences with non-consensus protospacer-adjacent motifs (PAMs) that demonstrate asymmetric cleavage activity—maintaining robust trans-cleavage for signal generation while minimizing cis-cleavage that degrades the amplicon target [3]. This balance allows for greater accumulation of amplification products while maintaining strong signal output.
Figure 1: ActCRISPR-TB Workflow Logic - The core innovation utilizes gRNAs with non-canonical PAM binding sites to reduce cis-cleavage (amplicon degradation) while maintaining strong trans-cleavage activity for signal generation, creating a positive feedback loop that enhances sensitivity.
Experimental Protocols & Methodologies
gRNA Screening and Characterization Protocol
Objective: Identify gRNA candidates with favorable trans- versus cis-cleavage activity ratios.
Procedure:
- Tile the target sequence: Design gRNAs tiling the IS6110 amplicon sequence, focusing on sites with non-canonical PAM sequences [3].
- Analyze secondary structures: Use computational tools (e.g., NUPACK) to evaluate gRNA secondary structure stability [3].
- Measure cleavage activities:
- Calculate normalized activity ratios: Rank gRNAs based on their trans-/cis-cleavage activity ratios [3].
- Exclude non-specific binders: Eliminate gRNAs with sequence overlap to RPA primers to prevent template-independent signal [3].
Critical Note: gRNA-6 was excluded from final development due to a 10-nucleotide sequence overlap with the RPA forward primer, which generated template-independent signal [3].
Optimized One-Pot ActCRISPR-TB Reaction Setup
Reaction Components:
- Primers: 500 nM each (IS6110-targeting RPA primers)
- Magnesium acetate: 16.8 nM
- RNP complex: 40 nM (Cas12a with gRNA-2, -3, and -5 mixture)
- ssDNA reporter: 600 nM (FQ-labeled or biotin/FAM-labeled for lateral flow)
- Template DNA: 5 μL in 50 μL total reaction volume
- RPA basic kit components (as per manufacturer's instructions)
Thermal Conditions:
- Amplification & Detection: 36-40°C for 45-60 minutes [3]
- Reaction Vessel: Single tube with no intermediate steps
gRNA Combination Optimization: The optimal multi-guide RNA combination was determined to be gRNA-2, gRNA-3, and gRNA-5 at specific ratios that maximize signal while minimizing competitive cis-cleavage [3].
Clinical Sample Processing Protocol
Sample Types Validated:
- Respiratory specimens (sputum)
- Pediatric stool samples
- Adult cerebral spinal fluid
- Tongue swabs [3] [28]
DNA Extraction Method:
- Process clinical samples using standard DNA extraction kits
- Elute DNA in nuclease-free water or TE buffer
- Use 5 μL of extracted DNA as template for the ActCRISPR-TB reaction
Readout Methods:
- Real-time fluorescence: Monitor every minute for 60 minutes
- Endpoint detection: Lateral flow strip readout after 45-60 minutes [3]
Performance Data & Validation
Analytical Sensitivity and Specificity
Table 1: Analytical Performance of ActCRISPR-TB Across Sample Types
| Parameter | Performance | Experimental Conditions |
|---|---|---|
| Limit of Detection | 5 copies/μL | Synthetic targets [3] |
| Time to Positive | 15 minutes for high bacterial load samples | Clinical sputum samples [3] |
| Assay Specificity | 100% for MTB complex species | Testing against non-tuberculous mycobacteria [3] |
| Optimal Read Time | 45 minutes | Balances speed and sensitivity [3] |
Clinical Validation Performance
Table 2: Clinical Performance of ActCRISPR-TB in 603 Clinical Samples
| Sample Type | Sensitivity | Specificity | Comparative Performance |
|---|---|---|---|
| Adult Respiratory | 93% | Not specified | Comparable to reference molecular diagnostics [3] |
| Pediatric Stool | 83% | Not specified | Superior to sputum-based references [3] |
| Adult CSF | 93% | Not specified | Detected 64% of clinically diagnosed TB meningitis [3] |
| Tongue Swabs | 74% | 100% | Superior to most sensitive reference test (56%) [3] [28] |
Technical Support Center: Troubleshooting Guides & FAQs
Research Reagent Solutions
Table 3: Essential Research Reagents for ActCRISPR-TB Implementation
| Reagent | Function | Optimization Notes |
|---|---|---|
| Cas12a Protein | CRISPR effector enzyme; performs target recognition and cleavage | Use purified LbCas12a; concentration optimized at 40 nM [3] |
| gRNA-2, -3, -5组合 | Guide RNAs targeting IS6110 element; determine cleavage specificity | Critical ratio optimization required; total gRNA concentration 40 nM [3] |
| IS6110 RPA Primers | Amplify target sequence isothermally | 500 nM each primer; asymmetric design may enhance performance [3] |
| ssDNA Reporter | Signal generation via trans-cleavage | 600 nM FQ-labeled or lateral flow-compatible (biotin/FAM) [3] |
| Magnesium Acetate | Cofactor for enzymatic reactions | Critical concentration: 16.8 nM; excess reduces signal [3] |
Frequently Asked Questions & Troubleshooting
Q1: Our ActCRISPR-TB assay shows high background signal even without template. What could be causing this?
A: Background signal typically results from:
- gRNA-primer overlap: Check for sequence complementarity between your gRNA and RPA primers (as encountered with gRNA-6) [3].
- Contaminated reagents: Prepare fresh aliquots of all reagents, particularly the RPA master mix.
- Suboptimal magnesium concentration: Titrate magnesium acetate between 15-20 nM; excess magnesium increases background [3].
- RNP complex precipitation: Ensure Cas12a-gRNA complexes are properly formed and not aggregated.
Q2: We're not achieving the published 5 copies/μL sensitivity. What optimization steps should we take?
A: Sensitivity issues commonly stem from:
- Suboptimal gRNA ratios: Systematically test gRNA-2, -3, and -5 combinations at different ratios while maintaining total gRNA at 40 nM [3].
- Reaction temperature: Ensure consistent temperature between 36-40°C throughout the reaction [3].
- Template quality: Verify DNA extraction efficiency and avoid inhibitors.
- Reaction time extension: Increase incubation time to 60 minutes for very low target concentrations [3].
Q3: How does ActCRISPR-TB maintain sensitivity while using non-canonical PAM sites that typically reduce Cas12a activity?
A: The key innovation is the discovery that trans- and cis-cleavage activities are functionally independent [3]. While non-canonical PAMs typically reduce both activities, specific gRNAs (particularly gRNA-5) demonstrate disproportionate preservation of trans-cleavage while minimizing cis-cleavage. This asymmetric activity profile reduces amplicon degradation while maintaining signal generation capacity [3].
Q4: Can ActCRISPR-TB be adapted for detection of other pathogens?
A: Yes, the core principle of engineering gRNAs that favor trans- versus cis-cleavage is broadly applicable. The researchers note potential for expansion to other pathogens, including emerging threats like COVID-19 and monkeypox [28]. Successful adaptation requires:
- Identification of suitable multi-copy target sequences
- Systematic gRNA tiling and characterization
- Optimization of the guide RNA combinations for the new target
Q5: What are the limitations of using tongue swabs instead of sputum for TB detection?
A: While tongue swabs offer significant practical advantages for screening, particularly in resource-limited settings, they present certain challenges:
- Lower bacterial load: M. tuberculosis DNA levels are typically lower on tongue swabs [28].
- Sampling variability: DNA recovery fluctuates with sampling technique, disease burden, and even daily activities affecting "respiratory material transfer to and depletion from the oral cavity" [28].
- Reduced sensitivity: The assay detected 74% of TB cases versus 93% with respiratory samples [3] [28].
Figure 2: ActCRISPR-TB Troubleshooting Decision Tree - A systematic approach to resolving common experimental challenges when implementing the assay.
ActCRISPR-TB represents a significant advancement in CRISPR diagnostics by fundamentally addressing the cis-/trans-cleavage competition that has limited one-pot assay sensitivity. Through strategic gRNA engineering that creates an asymmetric cleavage profile favoring trans-cleavage, the assay achieves detection limits as low as 5 copies/μL while maintaining a streamlined, single-reaction format [3]. This approach, validated across diverse clinical specimens, demonstrates that careful balancing of the competing reactions in one-pot assays can overcome traditional sensitivity barriers. The technical framework established by ActCRISPR-TB provides a blueprint for developing next-generation molecular diagnostics that combine high sensitivity with practical implementation requirements, particularly valuable for resource-limited settings where TB burden is highest.
Conventional enzyme-linked immunosorbent assays (ELISA) face a significant sensitivity gap compared to nucleic acid-based tests, typically detecting biomarkers in the pico- to nanomolar range while molecular techniques like PCR achieve atto- to femtomolar sensitivity [2] [29]. This limitation is particularly critical for pathogen detection where early diagnosis requires identifying low-abundance proteins. Cell-free synthetic biology has emerged as a transformative approach to bridge this sensitivity gap by integrating programmable nucleic acid and protein synthesis systems into traditional immunoassay workflows [2] [1].
Novel platforms such as expression immunoassays and CRISPR-linked immunoassays (CLISA) leverage cell-free protein synthesis (CFPS) to create highly sensitive and modular diagnostic systems [2]. These approaches enable signal amplification through synthetic biology mechanisms, potentially enhancing detection sensitivity by hundreds-fold while maintaining the specificity and accessibility of traditional ELISA [1]. This technical support center provides comprehensive guidance for researchers implementing these advanced protein detection methodologies within pathogen detection assays.
★ Key Concepts and FAQs
What are expression immunoassays and how do they enhance detection sensitivity? Expression immunoassays integrate cell-free protein synthesis directly into immunoassay workflows. In these systems, detection antibodies are labeled with DNA sequences encoding reporter proteins or the target biomarkers themselves [1]. When these antibody-DNA conjugates bind to their targets, the associated DNA serves as a template for in situ protein synthesis using CFPS systems, effectively amplifying the detection signal through continuous production of reporter molecules rather than relying on a finite number of enzyme labels [2] [1].
How does CLISA differ from traditional ELISA? CLISA (CRISPR-linked immunoassay) incorporates CRISPR-based nucleic acid detection systems into immunoassay formats. While traditional ELISA uses enzyme-conjugated antibodies for colorimetric detection, CLISA leverages the programmability and amplification capabilities of CRISPR systems to detect DNA tags attached to detection antibodies [2]. This approach combines the specificity of antibody-antigen interactions with the powerful signal amplification of CRISPR systems, potentially achieving detection sensitivities comparable to nucleic acid tests [2].
What are the primary advantages of integrating cell-free systems with immunoassays?
- Enhanced Sensitivity: Cell-free systems enable signal amplification through continuous protein synthesis or nucleic acid amplification, potentially improving detection limits by hundreds-fold [1]
- Modularity: DNA-programmable systems allow rapid adaptation to detect different biomarkers by simply changing the DNA template [2] [1]
- Flexibility: CFPS operates without cell viability constraints, enabling optimization of reaction conditions specific to each assay [30]
- Accessibility: Lyophilized cell-free systems can be distributed and used in resource-limited settings with minimal equipment [31]
Troubleshooting Guides
Common Expression Immunoassay Issues
Table 1: Troubleshooting Low Detection Sensitivity
| Problem | Possible Causes | Solutions |
|---|---|---|
| High background signal | Non-specific binding of detection antibody-DNA conjugates | Optimize blocking conditions using BSA, casein, or synthetic polymers like PEG; Implement nonfouling surface modifications [29] |
| Weak or no signal | Inefficient cell-free protein synthesis; Suboptimal DNA template design | Verify DNA template purity and sequence; Ensure proper T7 promoter and terminator sequences; Add RNase inhibitor to reactions [32] [33] |
| Inconsistent results between replicates | Variable washing efficiency; Unequal reagent distribution | Implement microfluidic systems for consistent mixing and washing; Use automated liquid handling systems where available [29] |
| Reduced protein yield in CFPS | Resource depletion in cell-free reactions; Suboptimal conditions | Utilize multiple feeding steps with smaller volumes of feed buffer (e.g., every 45 minutes); Add mild detergents (up to 0.05% Triton-X-100) to improve yields [32] |
Table 2: Addressing Cell-Free Protein Synthesis Problems
| Problem | Possible Causes | Solutions |
|---|---|---|
| No protein synthesis | Inactive kit components; Missing T7 RNA polymerase | Minimize freeze-thaw cycles of cell extract; Confirm addition of T7 RNA polymerase to reactions [32] [33] |
| Low protein yield | RNase contamination; Suboptimal DNA template design | Add RNase inhibitor; Verify DNA template contains proper UTR stem loop to stabilize mRNA; Optimize template amount (typically 250 ng for 50 μL reaction) [33] |
| Truncated protein products | Premature termination; Ribosome stalling at rare codons | Reduce incubation temperature to 25-30°C; Check for internal initiation sites; Consider codon optimization for eukaryotic proteins [32] [33] |
| Inactive synthesized proteins | Improper folding; Lack of essential cofactors | Add molecular chaperones to reactions; Include required cofactors in protein synthesis reaction; Extend incubation time at lower temperatures (16°C for up to 24 hours) [32] |
DNA Template Design and Preparation
How should I design DNA templates for expression immunoassays? Effective DNA template design is crucial for successful expression immunoassays. Ensure your template includes:
- Strong promoter sequences (typically T7) for efficient transcription [33]
- Optimal 5' untranslated regions (UTRs) to enhance translational efficiency [33]
- Stem-loop structures or T7 terminators to stabilize mRNA [33]
- Coding sequence for your reporter protein (fluorescent protein, enzyme, etc.)
- Avoidance of complex secondary structures near the translation initiation site [33]
What are the common DNA template preparation mistakes?
- Using DNA purified from agarose gels, which often contains translation inhibitors [32] [33]
- Residual ethanol, salts, or SDS from plasmid preparation protocols [32]
- RNase contamination from commercial mini-prep kits [33]
- Insufficient DNA concentration quantification due to RNA contamination [33]
Always repurify DNA using commercial cleanup kits and verify concentration and purity by both UV spectrophotometry (260/280 ratio ~1.8) and agarose gel electrophoresis [33].
Experimental Protocols
Protocol 1: Nucleic Acid-Templated Target Amplification (NATA)-ELISA
This protocol enables hundreds-fold sensitivity enhancement for protein detection by integrating target amplification into standard ELISA workflows [1].
Materials Required:
- Capture and detection antibodies specific to your target biomarker
- DNA template encoding your target biomarker or a universal surrogate protein (e.g., Streptococcal protein G with Avi-tag)
- Coupling reagents for antibody-DNA conjugation
- Cell-free protein synthesis system (E. coli extract-based or PURExpress)
- Standard ELISA plates and detection reagents
Procedure:
- Surface Preparation: Coat ELISA plates with capture antibodies using orientation strategies (Protein A/G, biotin-streptavidin) to enhance binding efficiency [29]
- Sample Incubation: Add samples containing target biomarker and incubate to allow antigen capture
- Detection Antibody Binding: Add DNA-conjugated detection antibodies and incubate
- Cell-Free Protein Synthesis: Add CFPS reaction mixture containing:
- Cell extract (E. coli, wheat germ, or rabbit reticulocyte-based)
- Energy regeneration system (ATP, GTP)
- Amino acids mixture
- RNA polymerase (typically T7)
- Nucleotides
- Signal Development: Incubate to allow synthesis of reporter proteins (2-4 hours at 30-37°C)
- Detection: Quantify synthesized reporters using appropriate methods (colorimetric, fluorescent, or luminescent)
Key Optimization Tips:
- Implement multiple feeding steps during CFPS to improve protein yields [32]
- Include RNase inhibitor to protect DNA templates and mRNA transcripts [33]
- For low-abundance targets, extend CFPS incubation time and reduce temperature to 25°C [32]
Protocol 2: CLISA Implementation
This protocol outlines CRISPR-enhanced immunoassay development for ultra-sensitive detection.
Materials Required:
- Antibody-DNA conjugates (detection antibodies linked to specific DNA sequences)
- CRISPR-Cas system (Cas12a, Cas13, or Cas9)
- Reporter nucleic acids (fluorescently quenched DNA or RNA probes)
- Cell-free transcription-translation system
- Standard immunoassay components
Procedure:
- Traditional Immunoassay Steps: Complete capture and detection antibody binding as in standard ELISA
- CRISPR Activation: Release or activate DNA templates bound via detection antibodies
- Nucleic Acid Amplification: Amplify activated DNA templates using PCR or isothermal amplification
- CRISPR Detection: Incubate amplified products with appropriate CRISPR system and reporter probes
- Signal Measurement: Detect cleavage of reporter probes via fluorescence or colorimetric changes
The Scientist's Toolkit
Table 3: Essential Research Reagent Solutions
| Reagent | Function | Application Notes |
|---|---|---|
| E. coli-based CFPS systems | Provides transcription/translation machinery for protein synthesis | Cost-effective; high protein yields; suitable for most reporter proteins [34] [35] |
| PURExpress In Vitro Protein Synthesis Kit | Reconstituted purified components for CFPS | Eliminates background E. coli activities; defined system for standardized results [34] |
| T7 RNA Polymerase | Drives transcription from T7 promoters | Essential for systems utilizing T7 promoters; typically used at 1-1.5 μL per 50 μL reaction [32] |
| RNase Inhibitor | Protects RNA components from degradation | Critical when using DNA prepared from commercial mini-prep kits [33] |
| MembraneMax Reagent | Enables membrane protein expression in CFPS | Essential for expressing membrane-bound targets; forms lipid bilayers for proper protein folding [32] |
| PURExpress Disulfide Bond Enhancer | Promotes proper disulfide bond formation | Improves activity of proteins requiring disulfide bonds; add 2 μL of each enhancer per 50 μL reaction [33] |
Workflow Visualization
Expression Immunoassay Workflow - This diagram illustrates the key steps in implementing expression immunoassays, highlighting the integration of traditional immunoassay steps with synthetic biology enhancement for superior sensitivity.
Advanced Applications and Future Directions
The integration of cell-free synthetic biology with immunoassays continues to evolve with emerging applications in pathogen detection. Recent developments include:
Multiplexed Detection Platforms: Leveraging cell-free systems to detect multiple pathogens simultaneously by encoding distinct reporter proteins for different targets [1]. This approach enables comprehensive pathogen screening from single samples.
Point-of-Care Adaptation: Utilizing lyophilized, shelf-stable cell-free systems that can be deployed in resource-limited settings [31] [36]. These systems maintain functionality for months at room temperature and can be activated by just adding water.
CRISPR-Enhanced Specificity: Combining the specificity of CRISPR systems with antibody-based detection to create dual-validation platforms that reduce false positives in pathogen identification [2].
As these technologies mature, researchers can expect increasingly sophisticated tools for sensitive protein detection that bridge the gap between immunoassays and molecular diagnostics, ultimately enhancing early pathogen detection capabilities in both clinical and field settings.
Technical Support Center
Core Mechanism and Principle FAQs
Q1: What is the fundamental principle that enables amplification-free CRISPR detection?
Amplification-free CRISPR diagnostics rely on the trans-cleavage activity of certain Cas proteins. Upon recognizing and binding to its specific target nucleic acid, the Cas protein becomes activated and unleishes non-specific, "collateral" cleavage of surrounding reporter molecules [37] [38]. For example, Cas12a targets DNA and trans-cleaves single-stranded DNA (ssDNA) reporters, while Cas13a targets RNA and trans-cleaves single-stranded RNA (ssRNA) reporters [37] [25]. This cleavage of reporter molecules generates a detectable signal (fluorescent, electrochemical, etc.), allowing for direct pathogen detection without the need for pre-amplification of the target sequence.
Q2: How do "cascade" systems enhance sensitivity without target amplification?
Cascade CRISPR systems improve sensitivity by linking the activities of multiple Cas proteins in a sequential manner, creating a signal amplification effect. One documented system for microRNA detection uses Cas13a and Cas12f in tandem [37] [39]. In this setup, the target miRNA first activates Cas13a. The trans-cleavage activity of Cas13a then produces a product that serves as the activator for a second Cas protein (e.g., Cas12f). This subsequent Cas protein then cleaves its own reporter, leading to a cascading signal boost. This multi-enzyme circuit can achieve femtomolar (fM) sensitivity and single-base resolution without any pre-amplification step [39].
Q3: What is the working principle behind digital droplet CRISPR platforms?
Digital droplet platforms work by partitioning a reaction mixture into thousands of nanoliter- or picoliter-sized reactors [37]. This micro-confinement effect significantly increases the local concentration of the target molecule within positive droplets. Platforms like SATORI (CRISPR-based amplification-free digital RNA detection) combine Cas13 detection with microchamber-array technologies [37]. Each droplet is analyzed individually, allowing for absolute quantification of the target nucleic acid at concentrations as low as 5 fM in just a few minutes, all without amplification [37].
Troubleshooting Common Experimental Issues
Q4: What should I do if my amplification-free assay shows no signal or a weak signal?
- Check Target Concentration: Verify that the target concentration meets or exceeds the limit of detection (LOD) for your specific Cas protein. The activation concentration can be around 100 pM for Cas12 and ~50 pM for Cas13 [37]. If your target is too dilute, consider alternative concentration methods or switching to a more sensitive platform like a digital droplet system.
- Optimize the Reporter System: The design of the reporter molecule is critical. Research indicates that using a stem-loop reporter (e.g., a 7nt stem-loop for Cas12a) can outperform traditional linear reporters, potentially offering a 10-fold increase in sensitivity [40]. Ensure the fluorophore and quencher pair on your reporter are compatible and that the reporter is present at an optimal concentration.
- Select the Right Cas Variant: Not all Cas enzymes are created equal. For Cas12a-based systems, the LbCas12a-Ultra variant has been identified as one of the most sensitive orthologs and can significantly boost detection capability [40].
- Verify crRNA Design: Ensure your crRNA is correctly designed and has stable secondary structures. Using multiple gRNAs targeting different sites on the same target amplicon has been shown to enhance signal production and improve overall assay sensitivity [3].
Q5: How can I address issues with specificity, such as false-positive signals?
- Refine crRNA Specificity: Meticulously design crRNAs to ensure high specificity for the target sequence. Use bioinformatic tools to check for potential off-target binding sites. The location of mismatches is important; those in the seed sequence (8–10 bases at the 3' end of the gRNA) are more likely to inhibit cleavage [41].
- Include Rigorous Controls: Always run negative controls (samples without the target) to identify any background signal or non-specific trans-cleavage activity. Use cells transfected with irrelevant plasmids or mock-transfected cells as negative controls to distinguish background from specific cleavage [42].
- Optimize Reaction Conditions: Parameters like Mg²⁺ concentration can influence signal specificity. Excessive Mg²⁺ has been shown to reduce assay signal and may contribute to background noise [3]. Follow optimization data to use concentrations that minimize background.
Q6: What are the common challenges when adapting an amplification-free assay to a lateral flow format?
- Signal Strength: The signal from the trans-cleavage reaction must be strong enough to be visible on a lateral flow strip. This often requires further optimization of the Cas protein, reporter (e.g., switching from fluorescent to biotin/FAM labels), and reaction time to ensure sufficient reporter cleavage occurs [38] [40].
- Sample Compatibility: Complex biological samples (e.g., plant extracts, serum) can contain inhibitors that interfere with the Cas protein's enzymatic activity. One study noted a 63% performance drop in Cas14-based assays under high humidity in field conditions, highlighting the sensitivity of these systems to non-ideal environments [38]. Sample purification or dilution may be necessary.
Experimental Protocol Summaries
Protocol 1: Cascade CRISPR/cas for miRNA Detection [39]
This protocol outlines a method for detecting microRNA with fM sensitivity without amplification.
- Reaction Setup: Prepare a master mix containing both Cas13a and Cas12f ribonucleoproteins (RNPs), their respective reporters, and the designed crRNA.
- Activation: Introduce the sample containing the target miRNA. The miRNA binds to and activates the Cas13a-crRNA complex.
- Signal Cascade: Activated Cas13a trans-cleaves a specific RNA substrate. The products of this cleavage act as a DNA activator for the Cas12f system.
- Signal Output: Activated Cas12f then trans-cleaves an ssDNA reporter labeled with a fluorophore-quencher pair, generating a fluorescent signal.
Protocol 2: Digital Droplet CRISPR (SATORI) for RNA Detection [37]
This protocol describes a platform for absolute quantification of target RNA at low concentrations.
- Droplet Generation: The CRISPR reaction mixture—containing Cas13 RNP, target RNA, and fluorescent RNA reporter—is partitioned into a vast array of picoliter-sized microchambers using microfluidic technology.
- Incubation: The array is incubated at a constant temperature (e.g., 37°C) for a short period (e.g., 5 minutes).
- Signal Detection: Each microchamber is imaged using a fluorescence microscope. Chambers containing the target RNA will show high fluorescence due to Cas13 activation and reporter cleavage.
- Quantification: The number of positive chambers is counted, and the target concentration is calculated using Poisson statistics, enabling absolute quantitation down to 5 fM.
Performance Data and Comparisons
Table 1: Comparison of Amplification-Free CRISPR Platforms
| Platform / Principle | Cas Protein Used | Reported Targets | Limit of Detection (LOD) | Approximate Assay Time |
|---|---|---|---|---|
| Microvolume / Digital Droplet | Cas13a | SARS-CoV-2, miRNA, 16S rRNA | 5 - 10 aM [37] | 5 - 60 min [37] |
| Microvolume / Digital Droplet | Cas12a | ASFV, EBV, HBV | 29 aM [37] | 60 min [37] |
| Cascade CRISPR (casCRISPR) | Cas13a & Cas12f | miRNA-17 | 1.33 fM [39] | 100 min [37] |
| Electrochemical Biosensor | Cas12a | Dengue virus, HIV-1 | 105 – 1010 aM [37] | 30 - 60 min [37] |
| Stem-loop Reporter + LbCas12a-Ultra | LbCas12a-Ultra | Phytoplasma | Not Specified (10x improvement) [40] | Not Specified |
Table 2: Key Cas Proteins for Amplification-Free Diagnostics
| Characteristic | Cas12a | Cas13a | Cas14 (Cas12f) |
|---|---|---|---|
| Target | DNA/RNA [25] | RNA [25] | ssDNA/dsDNA/RNA [25] |
| PAM Requirement | TTTV, etc. [25] | None [25] | None [25] |
| Trans-cleavage Substrate | ssDNA [37] [25] | ssRNA [37] [25] | ssDNA [25] |
| Reported Sensitivity | High [25] | High [25] | Very High [25] |
| Best Use Case | DNA virus detection [25] | RNA virus detection [25] | SNP detection, short targets [25] |
Essential Visual Workflows
Research Reagent Solutions
Table 3: Essential Reagents for Amplification-Free CRISPR Assays
| Reagent / Material | Function / Description | Examples / Notes |
|---|---|---|
| Cas Protein Variants | The engineered nuclease that provides detection specificity and trans-cleavage activity. | LbCas12a-Ultra: High-sensitivity variant for DNA targets [40]. Cas13a: For direct RNA target detection [37]. Cas12f (Cas14): Small size, useful for cascade systems and sensitive to SNPs [25] [39]. |
| Stem-Loop Reporters | A modified reporter structure that enhances signal upon cleavage compared to linear reporters. | A 7-nucleotide stem-loop reporter for Cas12a was shown to significantly outperform linear reporters, boosting sensitivity [40]. |
| Multiple crRNAs | Several guide RNAs designed to target different regions of the same amplicon. | Using a combination of 2-3 crRNAs (e.g., gRNA-2, -3, -5) can enhance signal and improve the limit of detection by favoring trans- over cis-cleavage [3]. |
| Microfluidic Chip / Droplet Generator | Hardware for partitioning reactions into thousands of micro-compartments for digital detection. | Essential for platforms like SATORI, enabling single-molecule sensitivity by increasing local target concentration [37]. |
| Lateral Flow Strips | A simple, instrument-free platform for visualizing detection results. | Used with reporters labeled with biotin and FAM, allowing for visual readout of results in field settings [38] [40]. |
FAQ: Liquid Biopsy Sensitivity and Limit of Detection
Q: What does a "0.15% VAF Limit of Detection" mean in practical terms for my research?
A: A 0.15% Variant Allele Frequency (VAF) Limit of Detection (LOD) means an assay can reliably detect a mutant DNA fragment present in a background of wild-type DNA at a frequency of just 0.15%. In practical research terms, this represents an approximately 2-5x improvement in sensitivity over many first-generation liquid biopsy assays. This enhanced sensitivity is crucial for detecting clinically actionable alterations in patients with low-shedding tumors, where the fraction of circulating tumor DNA (ctDNA) in the total cell-free DNA (cfDNA) is very small. The majority (91%) of additional clinically actionable variants detected at this sensitivity level are found below 0.5% VAF, where other assays typically fail [43] [44].
Q: My research involves tumors known for low ctDNA shedding. How can the latest technologies address this?
A: Advanced liquid biopsy technologies like the Northstar Select assay, which employs single-molecule next-generation sequencing (smNGS) with Quantitative Counting Templates (QCT), are specifically designed for this challenge. This platform achieves a 95% Limit of Detection (LOD95) of 0.15% VAF for single nucleotide variants (SNVs) and insertions/deletions (indels) by accurately counting individual DNA molecules. This technological approach has demonstrated the ability to detect alterations in 87% of central nervous system cancer cases, a tumor type historically difficult for plasma liquid biopsy due to low shedding rates [45] [44].
Q: What is the risk of false positives at this high sensitivity level, and how is it mitigated?
A: The risk of false positives is managed through several technical approaches. First, the use of Unique Molecular Identifiers (UMIs) helps distinguish true biological signals from PCR amplification errors and sequencing artifacts. Second, orthogonal validation using digital droplet PCR (ddPCR) has confirmed 98% concordance with NGS results, demonstrating that additional variants found are true positives. Furthermore, matched buffy coat testing can identify and filter out variants derived from clonal hematopoiesis (CH), a common source of false positives in liquid biopsy. One study confirmed that CH variants were identified at similar rates in both high-sensitivity and comparator assays, indicating the superior detection was not due to CH [46] [44].
Q: How does sensitivity affect the detection of different variant types beyond SNVs?
A: Sensitivity varies significantly across different variant classes. The most advanced assays now demonstrate comprehensive sensitivity across multiple variant types, though with different performance characteristics for each. The following table summarizes the LOD for different variant classes from a leading-edge assay:
Table: Limit of Detection Across Variant Classes
| Variant Class | 95% Limit of Detection (LOD95) | Key Improvement |
|---|---|---|
| SNVs/Indels | 0.15% VAF | 2-5x more sensitive than earlier assays |
| Gene Fusions | 0.30% VAF | Addresses a key challenge in liquid biopsy |
| Copy Number Variations (CNVs) | 2.11 copies (amplifications)1.80 copies (losses) | 5x better for CNVs; particularly improved for detecting losses |
This multi-variant sensitivity is critical as CNVs and fusions represent important actionable targets in cancer therapy. The ability to detect copy number losses has been a particular weakness in earlier liquid biopsy approaches [43] [47] [44].
Troubleshooting Common Experimental Challenges
Problem: Inconsistent detection of low-frequency variants across replicates.
Solution: This issue often relates to insufficient input material or suboptimal library preparation.
- Verify Input DNA Quantity: Ensure adequate cfDNA input. Achieving 20,000× coverage after deduplication requires a minimum input of 60 ng DNA, which corresponds to approximately 18,000 haploid genome equivalents. The absolute number of mutant DNA fragments in your sample must be sufficient for detection [46].
- Implement UMI Best Practices: Use Unique Molecular Identifiers (UMIs) during library preparation to account for duplicate reads and PCR artifacts. Under optimal sequencing conditions, expect a UMI deduplication yield of approximately 10%. This means a depth of coverage of 20,000× before deduplication will result in approximately 2,000× after deduplication [46].
- Adjust Variant Calling Parameters: For ctDNA analysis, consider lowering the minimum supporting read threshold to n=3 (from the typical n=5 used for tissue DNA) while maintaining high specificity thresholds. This adjustment accounts for the lower VAF in ctDNA while the lack of cytosine deamination in liquid biopsy DNA helps minimize false positives from this common source of artifacts [46].
Problem: Difficulty detecting Copy Number Variations (CNVs) in liquid biopsy samples.
Solution: CNV detection in ctDNA is particularly challenging due to biological and technical factors.
- Employ Advanced Counting Technologies: Utilize single-molecule counting methods like smNGS with QCT technology, which can differentiate focal "driver" amplifications from broad chromosomal aneuploidies that lack specific therapeutic targets. This differentiation is crucial for appropriate clinical interpretation [44].
- Validate with Orthogonal Methods: Confirm CNV calls using digital droplet PCR (ddPCR), which provides absolute quantification and can validate findings from NGS approaches. In validation studies, orthogonal testing with ddPCR demonstrated 98% concordance with the primary NGS results [44].
- Leverage Specialized Bioinformatics: Implement bioinformatics pipelines specifically designed for CNV detection in ctDNA that account for sample-specific factors like tumor fraction and sequencing depth. Some assays have demonstrated detection of 109% more CNVs than comparator tests, with particular improvement in detecting copy number losses [43] [44].
Problem: High "null report" rate in samples from patients with advanced cancers.
Solution: A null report (no pathogenic or actionable results) often indicates sensitivity limitations rather than true absence of alterations.
- Adopt Higher Sensitivity Assays: Implement assays with lower limits of detection (0.15% VAF vs. standard 0.5% VAF). In head-to-head comparisons, this approach resulted in 45% fewer null reports by identifying pathogenic variants present at low frequencies that were missed by other tests [43].
- Optimize Blood Collection and Processing: Standardize pre-analytical variables including blood collection tubes, processing time, and plasma separation protocols to preserve ctDNA yield and quality. The quantity of cfDNA in cancer patients is highly variable and influenced by tumor type, stage, and volume, making consistent processing critical [46].
- Evaluate Tumor Shedding Characteristics: Understand that different tumor types shed ctDNA at different rates. For example, lung cancers can have low cfDNA levels (5.23 ± 6.4 ng/mL), while liver cancers often show much higher levels (46.0 ± 35.6 ng/mL). Consider tumor type when interpreting results [46].
Experimental Protocols for Validation
Protocol: Analytical Validation of Limit of Detection for Low-Frequency Variants
This protocol outlines the procedure for establishing the limit of detection for SNVs/indels down to 0.15% VAF, as demonstrated in recent validation studies [43] [47].
Table: Key Research Reagent Solutions for LOD Validation
| Reagent/Material | Function in Experiment | Implementation Notes |
|---|---|---|
| Reference Standard DNA | Provides known variants at specific VAFs for precision measurement | Use commercially available reference standards with validated variant frequencies |
| Digital Droplet PCR (ddPCR) | Orthogonal validation method for NGS findings | Provides absolute quantification independent of NGS; target >98% concordance |
| Single-Molecule NGS (smNGS) with QCT | Enables precise molecular counting for rare variants | Core technology for achieving 0.15% VAF sensitivity |
| UMI Adapters | Tags individual DNA molecules to track amplification | Critical for distinguishing true variants from PCR/sequencing errors |
| Buffy Coat DNA | Control for clonal hematopoiesis variants | Isolate from same blood draw to identify germline or hematopoietic mutations |
Procedure:
- Sample Preparation: Serially dilute reference standard DNA containing known variants to create samples with VAFs ranging from 1.0% to 0.01%.
- Library Preparation: Use smNGS with QCT technology and UMI incorporation. The QCT technology enables precise counting of individual DNA molecules, which is fundamental to the enhanced sensitivity.
- Sequencing: Sequence to an appropriate depth. Commercial assays achieving 0.15% LOD typically achieve raw coverage of ~15,000×, yielding ~2,000× effective coverage after deduplication.
- Variant Calling: Process data through a bioinformatics pipeline optimized for low-VAF variant detection. Include steps for UMI deduplication and filtering of sequencing errors.
- Orthogonal Validation: Confirm a subset of variants, particularly those at the lowest VAFs (0.1-0.2%), using ddPCR. In validation studies, this approach demonstrated 98% concordance between the primary NGS method and ddPCR.
- Data Analysis: Calculate the LOD95 by determining the lowest VAF at which 95% of expected variants are detected across replicates.
Protocol: Head-to-Head Performance Comparison of Liquid Biopsy Assays
This protocol describes the methodology for comparing the performance of different liquid biopsy assays, as used in a recent prospective study of 182 patients [43] [44].
Procedure:
- Sample Collection: Collect plasma samples from patients with advanced solid tumors. The referenced study included over 17 solid tumor types from both community oncology clinics and large hospitals.
- Parallel Testing: Split each sample and test using the novel high-sensitivity assay and multiple commercially available comparator assays. The referenced study compared against six assays from four CLIA/CAP laboratories with panel sizes ranging between 73 and 523 genes.
- Data Analysis: Compare the number and type of pathogenic variants detected across assays. Key metrics include:
- Number of additional pathogenic SNVs/indels detected (51% more in referenced study)
- Number of additional CNVs detected (109% more in referenced study)
- Reduction in null reports (45% fewer in referenced study)
- Concordance for variants detected by multiple assays
- Orthogonal Confirmation: Use ddPCR to validate additional variants found only by the higher-sensitivity assay to confirm they represent true positives rather than false positives.
- VAF Distribution Analysis: Categorize additionally detected variants by their VAF. In the referenced study, 91% of additional clinically actionable SNVs/indels were detected below 0.5% VAF.
Technical Diagrams
Diagram: Enhanced Liquid Biopsy Workflow
This workflow illustrates the integrated process for high-sensitivity liquid biopsy analysis, highlighting key technological innovations that enable detection down to 0.15% VAF. The critical sensitivity-enhancing components include single-molecule counting with QCT technology for precision molecular quantification and UMI incorporation during library preparation to distinguish true biological variants from technical artifacts. Orthogonal validation with digital droplet PCR provides confirmation of low-frequency variants detected by the primary NGS method.
Advanced Sensitivity Enhancement Techniques
Leveraging CRISPR Technology for Pathogen Detection
While not directly applied to the 0.15% VAF ctDNA detection, CRISPR-based detection systems represent complementary sensitivity enhancement approaches in molecular diagnostics, particularly for pathogen detection:
- Asymmetric cis/trans Cleavage Assays: Advanced CRISPR assays like ActCRISPR-TB use guide RNAs that favor trans-cleavage versus cis-cleavage activity, enhancing signal production for low-abundance targets. This approach has achieved detection sensitivity of 5 copies/μL in tuberculosis detection [3].
- Multi-guide RNA Strategies: Employing multiple gRNAs targeting distinct sites on the same amplicon can increase signal intensity. One study found that adding specific gRNAs to an optimized assay differentially increased kinetics and sensitivity [3].
- One-Pot Assay Formats: Integrated "one-pot" assays that combine target amplification and detection in a single tube simplify workflows and reduce contamination risk. These assays must be carefully optimized to balance amplicon production and cleavage for maximum sensitivity [3].
Computational and Simulation Approaches
Advanced simulation tools like GENOMICON-Seq enable researchers to model sequencing workflows and optimize parameters for low-frequency variant detection:
- Ground Truth Mutation Insertion: These tools allow insertion of known mutations at specific frequencies before simulating entire sequencing workflows, enabling precise assessment of detection limits [48].
- Technical Noise Modeling: By modeling PCR errors, probe-capture enrichment biases, and sequencing errors, these tools help researchers distinguish true biological signals from technical artifacts [48].
- Pipeline Optimization: Simulations enable benchmarking of variant callers and optimization of data analysis pipelines for low-VAF detection without costly wet-lab trial and error [48].
From Problem to Performance: A Practical Guide to Assay Optimization
Frequently Asked Questions
Q1: What are the primary causes of a weak or absent signal in my detection assay? A weak signal can stem from several sources, including degraded or low-affinity reagents (especially antibodies), insufficient incubation times or incorrect temperatures that reduce binding efficiency, and the use of an incompatible or old standard [49] [50]. The sample itself may also contain very low levels of the target analyte [50].
Q2: How can I reduce high background noise in my assay? High background is frequently caused by inadequate washing or insufficient blocking [49] [50]. To solve this, increase the number and duration of washes, add a low-concentration detergent like Tween-20 to your wash buffer, and optimize your blocking solution (e.g., BSA, milk, or casein) [49] [51] [50]. Also, ensure your detection antibody concentrations are not too high [50].
Q3: My results are inconsistent between runs. How can I improve reproducibility? Poor reproducibility often results from variable reagent preparation, inconsistent sample handling, or deviations in protocol execution [49] [52]. To ensure consistency, standardize all pipetting, incubation, and wash steps using strict Standard Operating Procedures (SOPs), use the same lot of reagents across experiments when possible, and always prepare fresh calibration curves for each run [49] [52] [50].
Q4: What does it mean if I have a good standard curve but my samples are reading too high or too low? If your standard curve is good but samples are off, it typically indicates an issue with the sample matrix. Samples may contain analyte concentrations outside the assay's dynamic range or matrix components that interfere with detection [53]. Dilute your samples and run them again to see if the readings fall within the standard curve [51] [50].
Troubleshooting Guide
The table below summarizes common symptoms, their potential causes, and recommended solutions.
| Symptom | Potential Causes | Recommended Solutions |
|---|---|---|
| Weak Signal [49] [51] [50] | • Low-affinity or degraded antibodies• Insufficient incubation time/temperature• Incorrect plate coating | • Titrate and use high-affinity reagents [52]• Increase antibody concentration or incubation time [50] [53]• Optimize coating concentration; verify plate binding capacity [49] [50] |
| High Background [49] [51] [50] | • Inadequate washing or blocking• Non-specific antibody binding• Too high antibody concentration | • Increase wash stringency and volume; add detergent [49] [51] [53]• Optimize blocking buffer and incubation time [49] [50]• Titrate down antibody concentrations [50] |
| Poor Reproducibility [49] [52] [50] | • Inconsistent reagent preparation or storage• Variable pipetting or protocol steps• Equipment miscalibration | • Use large reagent batches; document lot numbers [52]• Implement strict SOPs; train personnel [49] [52]• Calibrate pipettes and plate readers regularly [49] |
| Narrow Dynamic Range [49] | • Assay cannot measure low and high analyte concentrations | • Adjust dilution series• Use higher-sensitivity detection (e.g., chemiluminescence) [49] |
| Edge Effects [49] [50] | • Evaporation from outer wells due to temperature gradients | • Pre-equilibrate plates to room temperature• Use plate seals; avoid stacking plates [50]• Use a humidified chamber during incubation [49] |
Experimental Protocols for Optimization
1. Protocol for Evaluating Matrix Interference via Spike-and-Recovery This experiment is critical for validating an assay for use with a new sample type (e.g., plasma, serum) to ensure the sample matrix does not interfere with the detection of the analyte [49].
- Materials:
- Test sample matrix (e.g., pooled plasma)
- High-purity analyte standard
- Assay buffer
- Standard assay reagents
- Method:
- Prepare a sample of the matrix that is known to be free of the analyte (or use a baseline sample).
- Spike this matrix with a known, moderate concentration of the purified analyte standard.
- Prepare the same concentration of the analyte standard in your standard assay buffer.
- Run both the spiked matrix sample and the standard-in-buffer sample in your assay.
- Calculate the percent recovery:
(Measured concentration in spiked matrix / Measured concentration in buffer) x 100%.
- Interpretation: A recovery of 80-120% is generally acceptable. Recovery outside this range indicates significant matrix interference. To resolve this, you may need to dilute your samples or use a matched matrix for your standards [49] [50].
2. Protocol for Determining Minimum Required Dilution (MRD) The MRD is the lowest dilution factor for a sample that reliably reduces matrix interference to an acceptable level while maintaining the analyte within the assay's detection range [52].
- Materials:
- Blank sample matrix (without analyte)
- Assay diluent
- Method:
- Prepare a series of dilutions (e.g., 1:2, 1:4, 1:8, 1:16) of the blank matrix in your assay diluent.
- Run these diluted blank samples in your assay.
- The MRD is the dilution at which the signal from the blank matrix approximates the background signal of your assay diluent alone (or falls within an acceptable pre-defined range, e.g., within 20% of the diluent background).
- Interpretation: All experimental samples should be diluted at least to the MRD before analysis to minimize false positives or signal suppression caused by the matrix [52].
Experimental Workflow for Pathogen Detection Assay Development
The following diagram illustrates a logical workflow for developing and optimizing a pathogen detection assay, integrating key steps to mitigate common failures.
The Scientist's Toolkit: Research Reagent Solutions
The table below lists essential materials and their critical functions in developing robust pathogen detection assays.
| Reagent/Material | Function | Considerations for Optimization |
|---|---|---|
| High-Affinity Antibodies [52] | Specifically captures and/or detects the target pathogen or antigen. | Use monoclonal antibodies for consistency. Titrate to find the optimal concentration that maximizes signal and minimizes background [52]. |
| Blocking Agents (e.g., BSA, Casein, Milk) [49] [52] | Coats unused protein-binding sites on the solid phase (e.g., microplate) to prevent non-specific binding of detection reagents. | Different blockers may work better for different assays. If background is high, switch or optimize the blocking buffer [49] [50]. |
| Wash Buffer with Detergent (e.g., Tween-20) [49] [51] | Removes unbound reagents and sample components during wash steps, critical for reducing background. | A typical concentration is 0.05% Tween-20. Increase wash stringency (volume, frequency, soak time) for high background [49]. |
| Calibration Standards [49] [52] | A series of known analyte concentrations used to generate a standard curve for quantifying unknown samples. | Prepare fresh for each run from a certified stock. Use a matrix that matches the sample to control for matrix effects [49] [52]. |
| Signal Detection System (e.g., HRP/TMB, Chemiluminescent) [49] [52] | Generates a measurable signal proportional to the amount of bound target. | Chemiluminescence often offers higher sensitivity than colorimetric (TMB) detection. Protect light-sensitive substrates [49] [53]. |
Frequently Asked Questions (FAQs)
FAQ 1: Why is antibody orientation so critical for maximizing biomarker capture efficiency? Proper antibody orientation ensures that the antigen-binding sites (Fab regions) are fully exposed and accessible to the target biomarker in solution. Traditional passive adsorption methods often lead to random antibody orientation, where a significant proportion of antibodies are immobilized in a way that blocks their binding sites. This reduces the functional capacity of the capture surface. Controlled orientation, typically by selectively attaching to the antibody's Fc region, can significantly enhance the number of available binding sites, leading to a higher capture efficiency of target biomarkers and a substantial improvement in assay sensitivity [54] [55].
FAQ 2: What are the primary surface engineering strategies to prevent non-specific binding in solid-phase assays? The key strategy involves using effective blocking agents and nonfouling surface coatings. Blocking agents like bovine serum albumin (BSA), skim milk, or casein are used to occupy any uncovered surfaces on the solid support after antibody coating. For more robust performance, synthetic polymers such as polyethylene glycol (PEG) can be grafted onto surfaces to create a hydrophilic, nonfouling layer that physically repels non-specific protein adsorption. Other materials like dextran, chitosan, and hyaluronic acid have also been successfully used to create surfaces that minimize background noise, thereby enhancing the signal-to-noise ratio [54].
FAQ 3: How does improving biomarker capture efficiency bridge the sensitivity gap between protein and nucleic acid detection? Nucleic acid tests (e.g., PCR) benefit from intrinsic enzymatic amplification, allowing for ultra-sensitive detection. Proteins lack such direct amplification methods. Enhancing capture efficiency directly increases the number of target biomarker molecules immobilized on the detection surface. When combined with powerful signal amplification techniques, this approach can push the detection limits of immunoassays like ELISA toward the atto- to femtomolar range, which is comparable to nucleic acid tests. This enables more accurate detection of low-abundance protein biomarkers for early disease diagnosis [54].
FAQ 4: What is the impact of mixing and washing efficiency on assay performance? In conventional assays, biomarker-antibody binding relies on passive diffusion, which can be slow and inefficient, especially for low-concentration targets. Inefficient washing can leave unbound reagents behind, increasing background signal and reducing specificity. Implementing convective mixing, often through microfluidic systems, enhances the interaction between target biomarkers and immobilized capture antibodies, reducing incubation times and improving the consistency of binding. Automated, efficient washing is crucial for removing unbound materials and minimizing false positives [54].
Troubleshooting Guides
Issue 1: Low Signal Intensity or Poor Sensitivity
| Potential Cause | Investigation & Verification | Solution |
|---|---|---|
| Random Antibody Orientation | Compare assay performance using a randomly immobilized antibody vs. one oriented via Protein G or a biotin-streptavidin system. | Implement an antibody orientation strategy (e.g., Protein A/G, Fc-specific biotinylation) to maximize binding site availability [54] [56]. |
| Inefficient Surface Blocking | Test different blocking agents (e.g., BSA, casein, commercial protein blockers) and assess background signal in negative controls. | Optimize the type and concentration of the blocking agent. Incorporate synthetic polymer coatings like PEG to create a nonfouling surface [54]. |
| Low Capture Antibody Activity | Verify antibody functionality in an alternative assay (e.g., Western blot). Check storage conditions and avoid repeated freeze-thaw cycles. | Aliquot antibodies for single use. Use a covalent crosslinking method for more stable antibody immobilization [54] [57]. |
Issue 2: High Background Signal
| Potential Cause | Investigation & Verification | Solution |
|---|---|---|
| Non-specific Protein Adsorption | Run a no-primary-antibody control. If background is high, non-specific binding is likely. | Improve blocking conditions; increase blocking time or try a different blocking agent. Introduce a nonfouling polymer coating to the surface [54] [58]. |
| Over-concentration of Antibodies | Perform a titration series for both capture and detection antibodies. | Determine the optimal dilution for both primary and secondary antibodies to minimize non-specific interactions while retaining specific signal [58] [57]. |
| Inadequate Washing | Inspect the assay protocol for the number, volume, and duration of wash steps. | Increase the number of washes; include a mild detergent (e.g., 0.05% Tween-20) in the wash buffer; ensure thorough aspiration between washes [54] [59]. |
Issue 3: Inconsistent Results Between Experiments
| Potential Cause | Investigation & Verification | Solution |
|---|---|---|
| Variable Antibody Immobilization | Assess the reproducibility of the coating process by testing different batches of coated plates with a standard sample. | Switch from passive adsorption to a consistent, oriented immobilization method (e.g., using a biotin-streptavidin system or covalent crosslinking) [54] [56]. |
| Suboptimal Mixing During Incubation | Check if the assay platform provides consistent and uniform mixing. | If using a microplate, employ a plate shaker during incubation steps. For superior performance, consider transitioning to a microfluidic system that provides controlled fluidics [54]. |
| Unstable Surface Coating | Test the shelf-life of pre-coated plates or surfaces. | Use fresh coatings for each experiment. For longer-term storage, ensure coated plates are sealed, desiccated, and stored at recommended temperatures [57]. |
Experimental Protocols & Data
Protocol 1: Oriented Antibody Immobilization Using the Biotin-Streptavidin System
This protocol details a highly effective method for achieving uniform antibody orientation on a solid surface, enhancing capture efficiency and assay reproducibility [54].
Biotinylation of Capture Antibody:
- Prepare the capture antibody in a bicarbonate buffer (pH ~8.4), which is optimal for the reaction.
- Incubate the antibody with a 20-fold molar excess of NHS-PEG4-Biotin for 30 minutes at room temperature.
- Remove unreacted biotin using a desalting column or dialysis against PBS.
Surface Coating with Streptavidin:
- Coat the solid surface (e.g., microplate well, magnetic bead) with a 10 µg/mL solution of streptavidin in PBS for 1 hour at 37°C or overnight at 4°C.
- Wash the surface three times with PBS to remove unbound streptavidin.
Blocking:
- Incubate the surface with a suitable blocking buffer (e.g., 1% BSA in PBS) for at least 1 hour at room temperature to prevent non-specific binding.
Immobilization of Biotinylated Antibody:
- Add the biotinylated capture antibody to the streptavidin-coated surface and incubate for 1 hour at room temperature.
- Wash thoroughly with PBS containing 0.05% Tween-20 (PBST) to remove any unbound antibody. The surface is now ready for the assay.
Protocol 2: Enhancing Signal with Functionalized Nanoparticles
This protocol leverages the signal amplification properties of chromium-doped zinc gallate nanoparticles (ZGO-NPs) for ultra-sensitive detection [60].
Functionalization of ZGO-NPs:
- Synthesize ZGO-NPs via a hydrothermal method (e.g., 12 hours at 120°C) for optimal luminescent properties.
- PEGylate the nanoparticles using biotin-PEG-NHS to create a stable, functional surface.
- Conjugate the detection antibody to the PEGylated ZGO-NPs via streptavidin-biotin binding or direct covalent linkage to create the ZGO-AbD complex.
Integration into Immunoassay:
- Perform the standard steps of a sandwich ELISA until the detection step.
- Instead of an enzyme-linked secondary antibody, incubate with the ZGO-AbD conjugate.
- After washing, expose the particles to a low concentration of hydrogen peroxide (H₂O₂).
- Measure the amplified persistent luminescence signal after UV excitation. The signal intensity is correlated with the target antigen concentration.
Quantitative Impact of Optimization Strategies
Table 1: Comparison of Strategies to Enhance Biomarker Capture and Detection
| Strategy | Key Parameter Improved | Demonstrated Improvement | Reference |
|---|---|---|---|
| Antibody Oriented-Immobilization (vs. Random) | Antigen Capture Efficiency | ~14-fold increase at 0.5 h incubation | [56] |
| Use of ZGO2-NPs with H₂O₂ (vs. conventional ELISA) | Limit of Detection (LoD) | LoD of 56 fg mL⁻¹ (vs. typical pg-ng mL⁻¹ range) | [60] |
| PEG-grafted Copolymer Surface | Non-specific Binding Reduction | Significant enhancement in signal-to-noise ratio | [54] |
| Protein G-expressing Cell Coating | Antibody-coating Capacity | Enhanced capacity via uniform Fc-specific binding | [54] |
The Scientist's Toolkit
Table 2: Key Research Reagent Solutions for Surface Engineering
| Reagent | Function & Mechanism |
|---|---|
| Protein A / Protein G | Bacterial proteins that bind the Fc region of antibodies, enabling oriented immobilization on surfaces when pre-immobilized. |
| Biotin-Streptavidin System | Exploits the strong non-covalent interaction between biotin and streptavidin. Biotinylated antibodies are uniformly captured on streptavidin-coated surfaces. |
| PEG (Polyethylene Glycol) | A synthetic polymer grafted onto surfaces to create a nonfouling, hydrophilic brush layer that minimizes non-specific protein adsorption. |
| Chromium-doped Zinc Gallate NPs (ZGO-NPs) | Persistent luminescence nanoparticles whose signal is amplified in the presence of H₂O₂, used as a label for ultra-sensitive detection. |
| Chitosan / Dextran | Natural polysaccharides used as coating materials to enhance protein immobilization while reducing non-specific binding. |
| Magnetic Beads | Serve as mobile solid phases that improve washing efficiency and reaction kinetics due to their high surface-area-to-volume ratio. |
Workflow and Pathway Diagrams
Antibody Immobilization Impact
Optimized Assay Workflow
This technical support guide addresses a critical challenge in developing sensitive pathogen detection assays: the fine-tuning of key reaction components. Achieving maximal sensitivity and specificity requires a careful balance between primer concentration, magnesium ion (Mg²⁺) levels, and the composition of Ribonucleoprotein (RNP) complexes. Optimal primer concentration ensures efficient and specific target amplification. Magnesium ions act as an essential cofactor for both polymerase and CRISPR-Cas enzyme activities. Finally, properly assembled RNP complexes are the core machinery for precise target recognition and signal generation. This document provides detailed troubleshooting guides and FAQs to help researchers navigate this complex optimization landscape.
Key Reagents and Their Functions
The following table outlines the essential reagents used in advanced pathogen detection assays, particularly those combining isothermal amplification with CRISPR-based detection.
Table 1: Research Reagent Solutions for Pathogen Detection Assays
| Reagent | Function | Key Considerations |
|---|---|---|
| Primers | Initiate specific amplification of the target nucleic acid sequence. | Optimal length (15-30 nt); GC content (40-60%); concentration typically 0.1-1.0 µM to avoid non-specific products [61] [62]. |
| Mg²⁺ (MgCl₂) | Essential cofactor for DNA polymerases and Cas enzymes; stabilizes nucleic acid duplexes [61]. | Concentration is critical; typically optimized between 0.5-5.0 mM. Affects enzyme activity, specificity, and signal strength [3] [61]. |
| RNP Complex | The core detection unit: a complex of Cas protein (e.g., Cas12a) and guide RNA (crRNA or pegRNA). | Guides specific target recognition and activates trans-cleavage activity. Efficiency can be enhanced by protein engineering and guide RNA modifications [63] [3]. |
| Cas12a Protein | RNA-guided nuclease that, upon target binding, cleaves the target (cis-cleavage) and non-specifically cleaves ssDNA reporters (trans-cleavage) [64]. | Requires a TTTV Protospacer Adjacent Motif (PAM) sequence for target recognition. Its activity is highly dependent on Mg²⁺ concentration [25] [64]. |
| crRNA/pegRNA | Guide RNA that directs the Cas protein to the specific target DNA sequence [63] [64]. | Can be engineered (e.g., "La-accessible pegRNA" with polyU tail) to enhance stability and interaction with Cas proteins, boosting editing or detection efficiency [63]. |
| dNTPs | The building blocks (A, T, C, G) for DNA synthesis during amplification. | Usually used at concentrations of 20-200 µM each. Imbalances can reduce amplification efficiency and fidelity [61]. |
| Isothermal Amplification Mix | Contains enzymes (recombinase, polymerase) and proteins to amplify DNA at a constant temperature (37-42°C) [64]. | Enables rapid target pre-amplification without complex thermal cyclers, making it suitable for point-of-care use [65] [64]. |
| Fluorescent ssDNA Reporter | A single-stranded DNA molecule labeled with a fluorophore and quencher. | When cleaved non-specifically by activated Cas12a, the fluorophore is separated from the quencher, generating a detectable fluorescent signal [25] [64]. |
Optimization Parameters and Experimental Protocols
Successful assay development requires systematic optimization. The following table summarizes target ranges and effects of key parameters, while the subsequent protocol provides a method for their balanced optimization.
Table 2: Quantitative Optimization Parameters for Key Reaction Components
| Parameter | Typical Optimal Range | Effect of Low Concentration | Effect of High Concentration |
|---|---|---|---|
| Primer Concentration | 0.1 - 1.0 µM [61] [62] | Low amplification yield [62]. | Non-specific amplification, primer-dimer formation, increased background [61] [62]. |
| Mg²⁺ Concentration | 0.5 - 5.0 mM [61] [62] | Reduced enzyme activity, low signal [61]. | Non-specific amplification, increased background noise [61]. |
| RNP Complex Concentration | ~40 nM (e.g., Cas12a RNP) [3] | Slow reaction kinetics, low signal. | Increased cost without benefit, potential increase in non-specific signal. |
| dNTP Concentration | 20 - 200 µM (each) [61] | Reduced amplification efficiency. | Potential introduction of errors (reduced fidelity), mispriming [62]. |
Experimental Protocol: Balanced Optimization of a One-Pot RPA-CRISPR/Cas12a Assay
This protocol is adapted from recent research on developing highly sensitive pathogen detection assays and general molecular biology optimization principles [3] [64].
Objective: To determine the optimal concentrations of primers, Mg²⁺, and RNP complexes in a one-pot reaction for maximum sensitivity and specificity.
Materials:
- Target DNA template (e.g., synthetic pathogen DNA fragment).
- RPA dry pellet or kit (e.g., from TwistDx or comparable supplier).
- Cas12a protein (commercially available, e.g., from IDT or New England Biolabs).
- In vitro transcribed crRNA targeting the pathogen sequence of interest.
- Fluorescent ssDNA reporter (e.g., FAM-TTATTATT-BHQ1).
- Nuclease-free water.
- Microcentrifuge tubes or 96-well PCR plates.
- Real-time PCR instrument or fluorometer for kinetic reading.
Method:
- Primer Titration:
- Prepare a master RPA mix according to the manufacturer's instructions, using a fixed, intermediate concentration of Mg²⁺ (e.g., 16.8 mM stock, as used in optimized protocols [3]).
- Set up a series of reactions where the primer concentration varies (e.g., 0.1, 0.2, 0.5, 1.0 µM).
- Keep the concentration of the RNP complex and Mg²⁺ constant in this initial test.
- Run the reactions and monitor fluorescence in real-time. Select the primer concentration that yields the lowest time to positive signal (fastest kinetics) and the highest fluorescence endpoint without increasing background noise.
Mg²⁺ Titration:
- Using the optimal primer concentration determined in Step 1, set up a new reaction series.
- Titrate the Mg²⁺ concentration across a range (e.g., 2 mM, 4 mM, 6 mM, 8 mM from a stock solution). Note that the final concentration in the RPA reaction is dictated by the magnesium acetate provided in the kit, which may need to be supplemented [3].
- Monitor the reactions. Identify the Mg²⁺ concentration that provides the strongest specific signal with minimal background. Note that excessive Mg²⁺ can reduce the signal [3].
RNP Complex Titration:
- Using the optimized primer and Mg²⁺ conditions, perform a final titration of the RNP complex.
- Test a range of RNP concentrations (e.g., 20 nM, 40 nM, 60 nM, 80 nM). The RNP is formed by pre-incubating the Cas12a protein with crRNA at a fixed molar ratio for 10-20 minutes at room temperature before adding to the reaction [63] [3].
- The optimal RNP concentration should provide a rapid signal onset and a high signal-to-noise ratio. Using multiple gRNAs targeting different sites on the same amplicon can further enhance sensitivity [3].
Validation:
- Validate the fully optimized assay conditions using samples with known target concentrations (including negative controls) to confirm sensitivity and specificity.
Troubleshooting FAQs
FAQ 1: My assay shows high background fluorescence (false positive). What could be the cause and how can I fix it?
- Potential Causes and Solutions:
- Cause: Excessive Mg²⁺ concentration. High Mg²⁺ can lead to non-specific enzymatic activity and destabilize the RNP complex, causing premature reporter cleavage [61] [62].
- Solution: Titrate Mg²⁺ downward in 1 mM increments. Use the lowest concentration that still supports robust amplification and Cas activity.
- Cause: Primer concentration is too high. This can cause primer-dimer formation and non-specific amplification, which may inadvertently activate the Cas enzyme [62].
- Solution: Reduce primer concentration to the lower end of the optimal range (e.g., 0.1-0.2 µM) and ensure primers are well-designed with no self-complementarity.
- Cause: RNP complex is degraded or assembled incorrectly.
- Solution: Ensure guide RNA is intact and free of degradation. Always pre-assemble the RNP complex on ice and use it immediately.
- Cause: Excessive Mg²⁺ concentration. High Mg²⁺ can lead to non-specific enzymatic activity and destabilize the RNP complex, causing premature reporter cleavage [61] [62].
FAQ 2: I am getting a weak or delayed signal (low sensitivity). How can I improve it?
- Potential Causes and Solutions:
- Cause: Suboptimal primer efficiency. Primers may not be binding or extending efficiently.
- Solution: Redesign primers following best practices (e.g., 18-24 bp length, Tm ~55-65°C, avoid secondary structures). Empirically test new primer sets [61].
- Cause: Insufficient Mg²⁺. Mg²⁺ is a cofactor for both the polymerase and Cas enzyme; low levels can cripple the entire reaction cascade [61].
- Solution: Titrate Mg²⁺ upward, but do not exceed 5-6 mM without careful validation due to the risk of increasing background.
- Cause: RNP complex concentration is too low or its activity is suboptimal.
- Cause: Suboptimal primer efficiency. Primers may not be binding or extending efficiently.
FAQ 3: How do I balance the conditions when moving from a two-step assay to a one-pot assay?
- Explanation: In a two-step assay, amplification and detection are separate, allowing for independent optimization. In a one-pot assay, these steps occur simultaneously in a single tube, creating competition for reagents and conditions.
- Solutions:
- Attenuate Cas Activity: Use guide RNAs with non-canonical Protospacer Adjacent Motifs (PAMs) that favor trans-cleavage activity (signal generation) over cis-cleavage activity (degradation of the amplicon). This allows the amplicon to accumulate and drive the signal [3].
- Fine-tune Concentrations: The optimal concentrations of primers, Mg²⁺, and RNP in a one-pot setup are often different from the two-step assay. A systematic titration of all components simultaneously, as described in the protocol above, is necessary.
- Use Favorably Balanced gRNAs: Select gRNAs that have been experimentally verified to have high trans-cleavage activity relative to their cis-cleavage activity to prevent the RNP from degrading the amplicon before it can be detected [3].
Workflow Visualization
The following diagram illustrates the logical decision process for optimizing a pathogen detection assay, integrating the key parameters discussed in this guide.
Assay Optimization Troubleshooting Workflow
Troubleshooting Guides
Why is my assay data inconsistent, and how can I pinpoint liquid handling as the source?
Inconsistent assay data, such as skewed concentration ratios or unknown sample concentrations, often stems from volumetric errors in liquid handling [66]. To systematically identify if the liquid handler is the source, follow these diagnostic steps:
Step 1: Verify Volumetric Performance Measure the accuracy and precision of the liquid handler using the following methodology [66]:
- Gravimetric Method: Weigh the mass of water dispensed. Convert mass to volume using the density of water. This method is not suitable for volumes under 5 µL due to evaporation [66].
- Photometric Method: Use absorbance or fluorescence measurements of a dye. This is more reliable for sub-microliter volumes and for positive displacement systems [66].
During verification, calculate these key performance indicators:
- Systematic Error (Accuracy):
(Mean Delivered Volume - Target Volume) / Target Volume x 100%[66] - Random Error (Precision): Expressed as the Coefficient of Variation (CV):
(Standard Deviation / Mean Measured Volume) x 100%[66]
Step 2: Investigate Common Mechanical and Protocol-Based Errors
- Tip Contamination: For systems with fixed tips, validate that washing protocols are effective and prevent carryover [67] [68]. For disposable tips, ensure vendor-approved tips are used to avoid issues related to poor fit, wetting properties, or residual plastic [67] [68].
- Sequential Dispensing Inaccuracy: If a large volume is aspirated and dispensed sequentially across a plate, verify that the first and last dispenses deliver the same volume. Ensure a "dry dispense" or non-contact dispensing to avoid tip contamination [67] [68].
- Inefficient Mixing in Serial Dilutions: In serial dilution protocols, ensure the liquid handler provides adequate mixing (e.g., via aspirate/dispense cycles or on-board shaking) to achieve homogeneity before the next transfer. Inefficient mixing leads to inaccurate concentrations across the dilution series [67] [68].
- Droplet Fall-Contamination: Check for droplets falling from tips as the robotic head moves. A "trailing air gap" after aspiration can minimize this [67] [68].
My pathogen detection assay is producing false positives/negatives. Could liquid handling be a factor?
Yes, inaccurate liquid delivery directly impacts assay sensitivity and specificity. Under-dispensing critical reagents like antibodies or enzymes in an immunoassay can lead to false negatives, as the signal fails to reach the detection threshold [67]. Over-dispensing can cause false positives by increasing background noise or non-specific binding [67] [68].
A study on the FilmArray GI Panel, a molecular diagnostic tool, highlighted that non-reproducible positive results for certain low-prevalence pathogens were a significant concern, emphasizing the need for diagnostic stewardship and reliable liquid handling to prevent false reporting [69].
Troubleshooting Steps:
- Calibrate for Liquid Properties: For viscous reagents (e.g., some buffers) or foaming liquids, use reverse-mode pipetting (aspirating extra volume and dispensing only the target volume) instead of the standard forward mode [67] [68].
- Check Software Parameters: Confirm that procedural variables like aspirate/dispense rates, liquid class settings, and tip immersion depth (recommended 2–3 mm below the liquid surface) are correctly defined in the method [67] [68].
- Validate Tip Performance: Use a standardized method to verify volume transfer across all channels and tips, especially when screening rare or expensive samples where errors can have major economic and scientific consequences [67] [68].
Frequently Asked Questions (FAQs)
What is the difference between accuracy and precision in liquid handling?
In the context of liquid handling, these terms have specific, quantifiable meanings [66]:
- Accuracy (Systematic Error): The difference between the mean volume delivered by the instrument and the target volume it was programmed to transfer. It measures correctness.
- Precision (Random Error): The variation in delivered volumes when the same operation is repeated under identical conditions. It is expressed as the Coefficient of Variation (CV) and measures reliability.
How often should I verify the volumetric performance of my automated liquid handler?
Verification should be performed [66]:
- During regular, scheduled intervals as part of a quality control program.
- After instrument installation and when developing new automated protocols.
- Whenever a critical parameter changes, such as the liquid type or target delivery volume.
When should I use gravimetric versus photometric methods for verification?
The choice depends on volume range and liquid type [66]:
- Gravimetric Methods: Best for volumes ≥ 5 µL. It is a direct measurement but is time-consuming and susceptible to evaporation at lower volumes.
- Photometric Methods (Absorbance/Fluorescence): Ideal for volumes < 5 µL. For air-displacement systems, use a dye with properties matched to your actual reagents. Positive displacement systems provide more consistent performance across different liquid types with fluorescent dyes.
What are the economic impacts of liquid handling errors?
Errors can have severe financial consequences [67] [68]:
- Over-dispensing: Wastes expensive and rare reagents. In high-throughput screening, a 20% over-delivery can cost hundreds of thousands of dollars annually in reagents alone and deplete compound libraries.
- Under-dispensing: Increases false negatives, which can cause a promising drug candidate or a true positive pathogen detection to be missed, potentially costing a company billions in future revenue.
Key Performance Data and Metrics
Quantitative Performance Metrics
Table 1: Key Formulas for Assessing Liquid Handler Performance [66]
| Metric | Formula | Interpretation |
|---|---|---|
| Systematic Error (Accuracy) | (Mean Delivered Volume - Target Volume) / Target Volume x 100% |
A value of 0% indicates perfect accuracy. A positive value means over-delivery; negative means under-delivery. |
| Random Error (Precision as CV) | (Standard Deviation / Mean Measured Volume) x 100% |
A lower CV % indicates higher precision and more reproducible liquid transfers. |
Pathogen Detection Reproducibility Data
Table 2: Reproducibility of Positive Results for Selected Pathogens on a Commercial PCR Panel (FilmArray GI Panel) [69]
| Pathogen | Reproducible Results | Non-Reproducible Results | Reproducibility Rate |
|---|---|---|---|
| Giardia lamblia | 57 | 0 | 100% |
| Cryptosporidium spp. | 61 | 2 | 97% |
| Rotavirus A | 76 | 1 | 99% |
| Adenovirus F40/41 | 38 | 16 | 70% |
| Yersinia enterocolitica | 36 | 14 | 72% |
| Vibrio cholerae | 3 | 5 | 37.5% |
Experimental Protocols
Protocol: Gravimetric Verification of Liquid Handler Performance
This protocol is suitable for verifying volumes of 5 µL and above [66].
1. Materials:
- High-precision analytical balance (capable of µg resolution)
- Purified water
- Weigh boat or microplate
- Data collection software or spreadsheet
2. Methodology:
- Place a weigh boat on the balance and tare.
- Program the liquid handler to dispense the target volume of water into the weigh boat.
- Record the mass dispensed. Tare the balance after each dispense if performing multiple transfers.
- Repeat for at least n=8 replicates per volume per channel to ensure statistical significance.
- Convert mass to volume using the density of water (0.9982 g/mL at 20 °C).
- Calculate the mean delivered volume, standard deviation, systematic error, and CV using the formulas in Table 1.
Protocol: Optimizing a Lateral Flow Assay (LFA) using Automated Liquid Handling
Automated liquid handlers can systematically optimize LFA parameters like antibody pair selection and reagent concentration [70].
1. Materials:
- Automated robotic liquid handling system with LFA-specific hardware/software
- LFA nitrocellulose strips
- Capture and detection antibodies
- Sample solutions containing the target pathogen (e.g., Plasmodium falciparum for malaria)
- Blocking buffers, running buffers
2. Workflow: The following diagram illustrates the automated optimization process for a Lateral Flow Assay.
3. Key Steps:
- Define Parameters: Input discrete (antibody pairs) and continuous (reagent concentration) variables into the liquid handler's software [70].
- Automated Setup: The liquid handler uses its deck and pipetting arms to prepare a matrix of different reagent combinations directly on LFA strips, minimizing hands-on time [70].
- Analysis: The developed strips are imaged. The system's high throughput and reproducibility enable the identification of the combination that provides the best sensitivity and specificity for the target pathogen [70].
The Scientist's Toolkit
Table 3: Essential Research Reagent Solutions for Sensitive Pathogen Detection Assays
| Item | Function in Pathogen Detection |
|---|---|
| High-Affinity Antibodies | Key reagents for immunoassays (e.g., LFAs, ELISAs); specificity and affinity directly impact assay sensitivity and reduce false positives [70]. |
| Precision Disposable Tips | Vendor-approved tips ensure proper fit, seal, and wettability, minimizing volume transfer errors that skew critical reagent concentrations [67] [68]. |
| Molecular Grade Water | Used for preparing standards, buffers, and reagents; its purity is essential to avoid nuclease contamination or interference in molecular assays like PCR. |
| Standardized Dyes for Verification | Fluorescent or absorbance-based dyes used in photometric verification of low-volume dispensing, ensuring the liquid handler performs accurately for the assay [66]. |
| Stable Control Panels | Well-characterized positive and negative control samples (e.g., inactivated pathogens) are crucial for validating assay reproducibility and day-to-day performance [69]. |
FAQs: Fundamental DoE Principles for Assay Development
Q1: What is Design of Experiments (DoE), and why is it better than our usual method for optimizing pathogen detection assays?
DoE is a structured, statistical method for planning, conducting, and analyzing controlled tests to determine the relationship between input variables (factors) and output variables (responses) [71]. Unlike the traditional "One-Factor-at-a-Time" (OFAT) approach, which changes one variable while holding others constant, DoE simultaneously investigates multiple factors and their interactions [72]. This is critical for complex biological assays where factors like temperature, primer concentration, and buffer pH can interact in non-obvious ways. Using DoE leads to more robust, reliable, and efficient assay development by saving time and resources while providing a deeper understanding of the entire system [71] [72].
Q2: What are the key terms I need to know to implement DoE in my research?
- Factors: The independent input variables you can control and change in your experiment (e.g., Mg²⁺ concentration, incubation temperature, primer concentration) [71] [72].
- Levels: The specific values or settings at which you test a factor (e.g., testing Mg²⁺ concentration at 16.8 nM and 20 nM) [71].
- Responses: The dependent output variables or results you measure (e.g., assay sensitivity (LOD), signal-to-noise ratio, time to positive result) [71] [72].
- Interactions: When the effect of one factor on the response depends on the level of another factor. For example, the optimal primer concentration might be different at varying temperatures. Detecting these interactions is a key advantage of DoE over OFAT [71].
Q3: Which common DoE designs are most suitable for developing a diagnostic assay?
The choice of design depends on your goal and the number of factors [71] [72].
| DoE Design | Primary Use | Key Advantage | Example Application in Assay Development |
|---|---|---|---|
| Full Factorial | Investigating a small number of factors (e.g., <5) | Uncovers all main effects and interactions between every factor [71]. | Optimizing a simple LAMP assay by testing all combinations of 3 factors (temperature, time, primer conc.) at 2 levels each. |
| Fractional Factorial | Screening a large number of factors to identify the most significant ones [72]. | Drastically reduces the number of experiments required while identifying vital factors [71]. | Identifying which of 7 potential factors (buffer, Mg²⁺, enzymes, etc.) most significantly impact CRISPR-Cas12a assay kinetics. |
| Response Surface Methodology (RSM) | Optimizing and refining the levels of critical factors after screening [72]. | Models the relationship to find the "sweet spot" or optimal combination that maximizes or minimizes a response [71]. | Fine-tuning the concentrations of gRNAs and Mg²⁺ in a one-pot RPA-CRISPR assay to achieve the lowest possible Limit of Detection (LOD) [73]. |
Troubleshooting Guide: Common DoE Implementation Challenges
Problem: The DoE results are unclear, or the model has poor predictive power.
- Potential Cause 1: Inadequate control of non-experimental variables.
- Potential Cause 2: The chosen range for a factor's levels was too narrow.
- Solution: Before the main DoE, conduct wide-ranging scouting experiments to ensure your selected levels (e.g., low and high values for temperature) will produce a measurable effect on the response [72].
- Potential Cause 3: The measured response is not sufficiently precise or accurate.
- Solution: Ensure your data collection methods are robust. Use calibrated instruments and replicate measurements to reduce noise. Automate data logging where possible to minimize human error [72].
Problem: The assay performance degrades when transferred to a different instrument or operator, despite DoE optimization.
- Potential Cause: The DoE model did not account for factors that cause process variation, leading to a non-robust method.
- Solution: Incorporate "noise factors" (factors that are hard to control in routine use, like different instrument models or ambient humidity) into your DoE design. Using RSM to find a robust "design space" where the response is insensitive to these minor variations can solve this [71] [72]. Validate the final model with confirmatory runs in the real-world environment [71].
Problem: My process has too many potential variables to test efficiently.
- Potential Cause: Attempting a full factorial design with too many factors.
Experimental Protocol: Applying DoE to a One-Pot Pathogen Detection Assay
This protocol outlines how DoE was applied to develop ActCRISPR-TB, a one-pot assay for detecting Mycobacterium tuberculosis, as referenced in the research [73]. The goal was to optimize the reaction conditions for maximum sensitivity (lowest LOD).
1. Define the Problem and Objective
- Objective: Optimize the reagent concentrations in a one-pot RPA-CRISPR reaction to achieve the highest sensitivity (lowest copy number/μL detection) for the IS6110 target in Mtb DNA [73].
2. Identify Factors and Responses
- Key Factors (Input Variables): Based on preliminary data, the critical factors were:
- Primer Concentration (nM)
- Mg²⁺ Concentration (nM)
- RNP Concentration (nM)
- Responses (Output Variables):
- Primary: Limit of Detection (LOD) in copies/μL.
- Secondary: Time to half-maximum signal (kinetics), Signal-to-Noise Ratio [73].
3. Select the Experimental Design
- A Response Surface Methodology (RSM) design, such as a Central Composite Design, is appropriate here. This design is ideal for optimizing a smaller number of critical factors (identified from prior screening) and modeling their complex interactions to find the optimal combination [71] [72].
4. Execute the Experiment and Analyze Data
- Prepare the reaction mixtures according to the combinations of factor levels specified by the RSM design.
- Run the assays with a standardized template (e.g., serial dilutions of Mtb DNA) and measure the fluorescence kinetics.
- Input the response data (LOD, kinetics) into statistical software (e.g., Minitab, JMP, Design-Expert). Perform ANOVA to identify which factors and interactions are statistically significant. The software will generate a predictive model and contour plots to visualize the optimal region [71] [72].
5. Interpret Results and Validate
- The model might reveal, for instance, that a specific ratio of gRNA-5 to gRNA-2 is critical for favoring trans-cleavage over cis-cleavage, thereby improving amplification efficiency and signal [73].
- The software will predict the optimal settings (e.g., 500 nM primers, 16.8 nM Mg²+, 40 nM RNP). To validate, perform confirmatory experiments at these predicted settings to ensure the assay consistently achieves the target LOD (e.g., 5 copies/μL) [73] [71].
Experimental Workflow Diagram
The Scientist's Toolkit: Research Reagent Solutions
Essential materials and reagents used in the development of advanced optical biosensors for pathogen detection, as discussed in the research [73].
| Item / Reagent | Function in Pathogen Detection | Application Example |
|---|---|---|
| CRISPR-Associated (Cas) Proteins | Molecular scissors that bind to and cleave nucleic acids upon recognizing a specific target sequence guided by gRNA [73]. | Cas12a protein is used in one-pot assays for its trans-cleavage activity, which cleaves a reporter molecule to generate a detectable signal upon target pathogen DNA binding [73]. |
| Guide RNA (gRNA) | A short RNA sequence that directs the Cas protein to a specific complementary DNA sequence of the target pathogen [73]. | Multiple gRNAs (e.g., gRNA-2, -5) can be used simultaneously to target different sites on a pathogen's genome, enhancing signal and assay sensitivity [73]. |
| Recombinase Polymerase Amplification (RPA) Kit | An isothermal nucleic acid amplification technique that rapidly copies target DNA at a constant temperature (e.g., 37-42°C), eliminating the need for a thermal cycler [73]. | Used for pre-amplifying trace amounts of pathogen DNA (e.g., from Mtb) in a sample to detectable levels within the one-pot assay [73]. |
| Fluorescent or Colorimetric Reporters | Single-stranded DNA molecules linked to a fluorophore/quencher pair (for fluorescence) or substrates for enzymatic color change (for colorimetry). Cleavage by Cas proteins produces a signal [73]. | In fluorescent CRISPR assays, trans-cleavage of a quenched ssDNA reporter releases a fluorescent signal. In colorimetric assays, enzymatic reactions or nanoparticles cause a visible color change [73]. |
| Metal Ions (e.g., Mg²⁺) | Acts as a cofactor for enzymatic reactions. Its concentration is critical for the efficiency of both RPA amplification and Cas protein cleavage activity [73]. | A key factor optimized using DoE; the concentration of Mg²⁺ was found to be crucial for balancing amplification and detection in the one-pot ActCRISPR-TB assay [73]. |
DoE Advantage Diagram
Bench to Bedside: Ensuring Clinical Validity and Comparative Advantage
This technical support center provides guidance for researchers and scientists working on the analytical validation of pathogen detection assays. The content is framed within the broader thesis of improving sensitivity in pathogen detection research, focusing on the critical parameters of the 95% Limit of Detection (LoD) and Clinical Specificity. The following FAQs and troubleshooting guides address specific experimental challenges and provide detailed methodologies to ensure your assays are robust, accurate, and fit for their intended clinical purpose.
Core Concepts: Understanding LoD and Specificity
What is the 95% Limit of Detection (LoD) and how is it statistically defined?
The Limit of Detection (LoD) is the lowest concentration of an analyte that can be reliably distinguished from a blank sample (containing no analyte) [19] [74]. The "95%" designation refers to the statistical confidence level, meaning the assay should detect the analyte at or above this concentration 95% of the time [19].
The calculation of LoD builds upon another parameter, the Limit of Blank (LoB). The LoB is the highest apparent analyte concentration expected to be found when replicates of a blank sample are tested [19] [74]. It is defined as: LoB = mean~blank~ + 1.645(SD~blank~) [19]
This formula establishes a one-sided 95% confidence interval, assuming a Gaussian distribution where 95% of blank sample measurements will fall below this value [19]. Once the LoB is established, the LoD can be determined using the following statistical definition: LoD = LoB + 1.645(SD~low concentration sample~) [19]
In this formula, the low concentration sample is one known to contain a small amount of the analyte. This calculation ensures that the LoD is a concentration that can be reliably distinguished from the LoB with 95% confidence [19].
How is Clinical Specificity defined and calculated in a validation study?
Clinical Specificity is the ability of an assay to correctly identify the absence of a target pathogen or condition. In a validation study, it is calculated as the percentage of true negative samples that are correctly identified as negative by the test [75].
A recent study evaluating next-generation sequencing assays for lower respiratory tract infections reported specificities of 84.85% and 75.00% for two different pathogen enrichment approaches [75]. The study emphasized that high specificity is crucial to prevent misdiagnosis and the overuse of antibiotics in cases of non-infectious diseases [75].
Experimental Protocols and Methodologies
Detailed Protocol: Establishing the 95% LoD for a Pathogen Detection Assay
This protocol outlines the key steps for determining the 95% LoD, a critical parameter for characterizing the sensitivity of your assay.
Step 1: Define the Analytical Target Profile (ATP)
Before beginning wet-lab work, define the ATP. This is a formal statement of the required assay performance, including the target LoD, intended use, and acceptable levels of imprecision and bias [76]. This aligns with a modern Analytical Procedure Lifecycle Management approach, which emphasizes building quality into the method from the design stage [76].
Step 2: Prepare Study Samples
- Blank Samples: Use a matrix that matches your clinical samples (e.g., serum, sputum) but is confirmed to be free of the target analyte [19] [74].
- Low Concentration Samples: Prepare samples with known, low concentrations of the target pathogen. The concentration should be near the expected LoD. For microbial targets, this can be expressed as Colony Forming Units per milliliter (CFU/mL) or genomic copies per microliter [77].
Step 3: Conduct Testing and Data Collection
- Test a sufficient number of replicates to ensure statistical reliability. Regulatory standards often recommend at least 60 replicate measurements each for the blank and the low-concentration sample for a robust initial establishment. For verification studies, a minimum of 20 replicates may be acceptable [19].
- Perform testing across different instruments, operators, and reagent lots to capture expected routine performance variation [19].
Step 4: Data Analysis and LoD Calculation
- Calculate the LoB using the results from the blank samples:
LoB = mean~blank~ + 1.645(SD~blank~)[19]. - Calculate the provisional LoD using the results from the low-concentration sample:
LoD = LoB + 1.645(SD~low concentration sample~)[19]. - Confirm the LoD: Test additional replicates at the calculated provisional LoD concentration. The LoD is confirmed if no more than 5% of these test results fall below the LoB [19].
Table 1: Key Characteristics of Analytical Limits
| Parameter | Sample Type | Definition | Key Statistical Formula |
|---|---|---|---|
| Limit of Blank (LoB) | Sample containing no analyte [19] | Highest apparent analyte concentration expected from a blank sample [19] | LoB = mean~blank~ + 1.645(SD~blank~) [19] |
| Limit of Detection (LoD) | Sample with low concentration of analyte [19] | Lowest analyte concentration reliably distinguished from the LoB [19] | LoD = LoB + 1.645(SD~low concentration sample~) [19] |
| Limit of Quantitation (LoQ) | Sample with low concentration of analyte [19] | Lowest concentration that can be quantified with acceptable precision and accuracy [19] | LoQ ≥ LoD (Typically defined by a precision goal, e.g., CV=20%) [19] |
Detailed Protocol: Determining Clinical Specificity
- Select a Panel of Samples: Obtain a well-characterized set of clinical samples that are known to be negative for the target pathogen. This panel should include samples that may contain other, similar pathogens or commensal flora to challenge the assay's specificity and check for cross-reactivity [78] [75].
- Run the Assay: Test all samples in the panel using your validated pathogen detection method.
- Calculate Specificity: Use the results to calculate specificity. > Specificity (%) = [Number of True Negatives / (Number of True Negatives + Number of False Positives)] × 100 [75]
Troubleshooting Guides and FAQs
FAQ: LoD and Specificity
Q1: Our assay's LoD is higher than required. What are the main strategies to improve it?
- Strategy 1: Enhance Signal Generation. Adopt novel enzymatic amplification strategies. For example, the Target-amplification-free Collateral-cleavage-enhancing CRISPR-CasΦ (TCC) method uses a dual-stem-loop DNA amplifier to enhance detection signals, achieving an LoD as low as 0.11 copies/μL for clinical pathogens [77].
- Strategy 2: Optimize Sample Preparation. Improve nucleic acid extraction efficiency to increase the absolute copy number of the target recovered from the sample [77]. Incomplete cell lysis during extraction is a common cause of suboptimal yield and should be addressed by strictly following incubation times and temperatures [79].
- Strategy 3: Combine with Pre-amplification. Integrate an isothermal amplification step, such as Enzymatic Recombinase Amplification (ERA), prior to detection. An ERA-CRISPR/Cas12a method for detecting Human Adenovirus Type 55 achieved a sensitivity of 2.5 copies/reaction [78].
Q2: We are observing a high rate of false positives, reducing our specificity. What should we investigate?
- Investigation 1: Check for Contamination. "Contamination can turn up at any point during sample handling" [79]. Always use sterile techniques, reagents, and work environments. Review your plate setup for potential cross-contamination during pipetting [80].
- Investigation 2: Assess Assay Specificity. Ensure your primers and probes are highly specific for the target pathogen. Test for cross-reactivity against a panel of other common pathogens found in the same sample type [78] [75]. Non-specific amplification can also be caused by incorrect annealing temperatures; optimize this using a temperature gradient [79] [80].
- Investigation 3: Re-evaluate the Threshold. In qPCR assays, an incorrect baseline setting can skew results and lead to misinterpretation [79].
Q3: How many replicates are sufficient for a rigorous LoD study? For a manufacturer to establish a robust LoD, it is recommended to use at least 60 replicate measurements for both the blank and the low-concentration sample. For a single laboratory verifying a manufacturer's claim, 20 replicates are often considered sufficient [19]. This larger sample size helps capture the expected performance variation across the population of instruments and reagent lots.
Troubleshooting Guide: Common Experimental Issues
Table 2: Troubleshooting Common Pathogen Detection Assay Problems
| Problem | Potential Causes | Solutions |
|---|---|---|
| High / Variable Ct values in qPCR | Low template concentration, template degradation, reagent degradation, poor pipetting technique, or partial inhibition [80]. | Check template quality and concentration [80]. Verify reagent storage and minimize freeze-thaw cycles of primers/probes [80]. Ensure proper pipetting calibration and technique [80]. |
| Non-Specific Amplification | Annealing temperature is too low [79] [80], primer-dimer formation, or contaminated reagents [80]. | Optimize annealing temperature via gradient PCR [79] [80]. Check for environmental contamination [80]. Use "Hot Start" PCR kits to reduce non-specific amplification [79]. |
| Inconsistent Replicate Results | Inconsistent pipetting, uneven mixing of reagents, or improper sealing of reaction plates leading to evaporation [80]. | Calibrate pipettes and ensure consistent pipetting technique [80]. Mix reagents thoroughly before aliquoting [80]. Ensure plates are evenly and properly sealed [80]. |
The Scientist's Toolkit: Essential Research Reagents & Materials
Table 3: Key Research Reagent Solutions for Advanced Pathogen Detection
| Reagent / Material | Function in Validation | Examples / Notes |
|---|---|---|
| CRISPR-Cas Systems (e.g., CasΦ, Cas12a) | Provides highly specific nucleic acid detection and signal amplification via collateral cleavage activity [77] [78]. | CasΦ is a compact Cas12 protein used in the TCC method for amplification-free detection [77]. |
| Isothermal Amplification Kits (e.g., ERA, RPA, LAMP) | Pre-amplifies target nucleic acids to enhance detection sensitivity before the CRISPR detection step [77] [78]. | An ERA kit was used to pre-amplify the Hexon gene of HAdV55 prior to CRISPR detection [78]. |
| Nucleic Acid Extraction Kits | Isolates and purifies pathogen DNA/RNA from complex clinical matrices (e.g., blood, sputum) [79]. | The choice of kit (DNA, RNA, or total nucleic acid) depends on the target pathogen and sample type [79]. |
| qPCR Master Mix | A pre-mixed solution containing enzymes, dNTPs, and buffer for efficient real-time PCR amplification [79]. | "Hot Start" master mixes are recommended to improve specificity by reducing primer-dimer formation [79]. |
| Fluorescent Reporters | Single-stranded DNA oligonucleotides linked to a fluorophore and quencher; cleavage by activated Cas enzymes produces a fluorescent signal for detection [77]. | The linker between the fluophore and quencher is cleaved by CasΦ's collateral activity in the TCC method [77]. |
Workflow and Relationship Diagrams
LoD Establishment Workflow
Relationship Between LoB, LoD, and LoQ
Accurate pathogen detection is critical for diagnosing infections, yet clinical specimens like respiratory samples, stool, and cerebrospinal fluid (CSF) present unique challenges due to their differing compositions and pathogen loads. Advanced molecular diagnostics, including CRISPR-based assays and next-generation sequencing, have significantly improved detection sensitivity and specificity across these diverse sample types. This technical support center provides troubleshooting guides and detailed protocols to help researchers optimize these assays, ensuring reliable performance in the context of a broader thesis on improving sensitivity in pathogen detection assays. The following sections address specific experimental issues, provide comparative performance data, and outline essential methodologies for working with complex clinical specimens.
Performance Data Comparison Across Specimen Types
Understanding the expected performance characteristics of advanced detection assays across different specimen matrices is crucial for experimental design and result interpretation. The table below summarizes clinical sensitivity data for two leading technologies—CRISPR-based assays and metagenomic next-generation sequencing (mNGS)—across respiratory, stool, and CSF specimens.
Table 1: Clinical Sensitivity of Advanced Pathogen Detection Assays by Specimen Type
| Specimen Type | Technology | Pathogen Target | Clinical Sensitivity | Key Performance Notes |
|---|---|---|---|---|
| Respiratory | ActCRISPR-TB Assay [3] | Mycobacterium tuberculosis | 93% (adult samples) | Detected 85% of Xpert-positive samples within 15 minutes |
| Stool | ActCRISPR-TB Assay [3] | Mycobacterium tuberculosis | 83% (pediatric samples) | Suitable for pediatric applications where sputum collection is difficult |
| Cerebral Spinal Fluid (CSF) | ActCRISPR-TB Assay [3] | Mycobacterium tuberculosis | 93% | Valuable for detecting tuberculous meningitis |
| CSF | Metagenomic NGS (mNGS) [81] | Multiple CNS infection pathogens | 77.1% (overall pathogen detection) | Significantly outperformed culture methods (6.36% sensitivity) |
| CSF | Nanopore Sequencing [82] | Bacterial meningitis pathogens | 50% (vs. culture) | Increased overall detection rate to 70.6% when combined with culture |
For CSF specimens specifically, multiplex PCR panels have demonstrated significant utility in clinical decision-making. A recent study of 144 pediatric patients with suspected central nervous system (CNS) infections found that CSF multiplex PCR identified pathogens in 24.3% of cases, leading to treatment modifications in 35.4% of patients, primarily through discontinuation of unnecessary antivirals or antibiotics [83].
Table 2: Pathogen Distribution in CSF Samples from Suspected CNS Infections (n=35 positive cases) [83]
| Pathogen Category | Specific Pathogens Detected | Number of Cases |
|---|---|---|
| Viral Agents | Enterovirus, HSV-1, HHV-6, HHV-7, HHV-8, VZV, CMV | 22 |
| Bacterial Agents | Streptococcus pneumoniae, Neisseria meningitidis, Haemophilus influenzae type b | 11 |
| Mixed Infections | Multiple pathogens detected simultaneously | 2 |
Experimental Protocols & Methodologies
ActCRISPR-TB Assay Protocol
The ActCRISPR-TB assay represents a significant advancement in rapid, sensitive pathogen detection suitable for multiple specimen types. Below is the detailed experimental protocol adapted from the published methodology [3]:
Specimen Preparation:
- Respiratory samples: Process sputum using standard N-acetyl-L-cysteine-NaOH decontamination and concentration methods.
- Stool samples: Homogenize 1-2 grams in 10 mL phosphate-buffered saline, then centrifuge at 3,000 × g for 10 minutes.
- CSF specimens: Centrifuge 1-3 mL at 10,000 × g for 10 minutes, then resuspend the pellet in 500 μL TE buffer.
DNA Extraction:
- Use commercial DNA extraction kits suitable for the specimen type (e.g., TIANamp Micro DNA Kit).
- Include appropriate positive and negative controls in each extraction batch.
- Elute DNA in 50-100 μL elution buffer suitable for downstream molecular applications.
One-Pot ActCRISPR-TB Reaction Setup:
- Prepare master mix containing:
- 500 nM forward and reverse IS6110-targeting primers
- 40 nM Cas12a ribonucleoprotein complex (RNP)
- Multiple gRNAs (gRNA-2, gRNA-3, gRNA-5 at optimized ratios)
- 600 nM ssDNA reporter (e.g., FAM-TTATT-BHQ1)
- 16.8 nM Mg2+ (critical concentration)
- RPA enzyme mix
- Add 5-10 μL of extracted DNA template to 20-25 μL master mix
- Incubate at 37-40°C for 45-60 minutes
- Monitor fluorescence in real-time or read endpoint signal
Optimization Notes:
- Maintain total gRNA concentration constant when adjusting ratios
- Temperature tolerance: 36-40°C without significant performance loss
- Reaction time: 15 minutes for preliminary positive identification, 45 minutes for maximum sensitivity
Metagenomic Next-Generation Sequencing for CSF
For comprehensive pathogen detection in CSF, mNGS offers an unbiased approach [81]:
CSF Processing and DNA Extraction:
- Collect 1.5-3 mL CSF via lumbar puncture
- Add 0.6 mL sample to tube with 250 μL, 0.5 mm glass beads
- Agitate vigorously at 2800-3200 rpm for 30 minutes
- Add 7.2 μL lysozyme for wall-breaking reaction
- Extract DNA using TIANamp Micro DNA Kit per manufacturer's instructions
- For RNA pathogens, extract using TIANamp Micro RNA Kit and synthesize cDNA
Library Preparation and Sequencing:
- Construct DNA libraries through enzymatic fragmentation (20 minutes at 37°C)
- Perform end repair, adapter ligation, and PCR amplification
- Use unique barcodes for individual patient samples
- Sequence on BGISEQ-50/MGISEQ-2000 platform
- Include negative controls in each sequencing run
Bioinformatic Analysis:
- Filter raw sequences to remove common background microorganisms and low-quality reads
- Subtract human sequences by mapping to hg38 reference genome
- Align remaining data to pathogen databases (RefSeq)
- Apply positive criteria: bacteria (≥3 reads), fungi/parasites (≥5 reads), viruses (≥10 reads)
Troubleshooting Guides & FAQs
Frequently Asked Questions
Q: Our ActCRISPR-TB assay shows high background signal in stool samples. How can we reduce this? A: High background in stool samples often results from inhibitor carryover or non-specific amplification. We recommend: (1) Increasing the dilution factor during DNA extraction; (2) Including a bead-beating step during sample processing to improve homogenization; (3) Optimizing the Mg2+ concentration in 0.5 nM increments around the recommended 16.8 nM; (4) Implementing a pre-amplification purification step using magnetic beads [3].
Q: What is the minimum CSF volume required for reliable mNGS detection? A: While optimal volume is 3-5 mL, reliable detection has been achieved with volumes as low as 1.5 mL, though with potentially reduced sensitivity. For volumes under 2 mL, consider: (1) Reducing the elution volume during DNA extraction to concentrate nucleic acids; (2) Adding carrier RNA during extraction to improve yields; (3) Increasing PCR cycle numbers during library preparation (though this may increase duplication rates) [81].
Q: How can we distinguish true pathogens from background contamination in mNGS of CSF? A: Contamination remains a significant challenge. Implement these strategies: (1) Always include negative control samples in the same extraction and sequencing batch; (2) Establish laboratory-specific background contamination databases; (3) Apply strict read threshold filters (bacteria: ≥3 reads, fungi/parasites: ≥5 reads, viruses: ≥10 reads); (4) Correlate findings with clinical presentation and conventional test results [81] [82].
Q: Our CRISPR assay sensitivity for respiratory samples falls below the published 93%. What factors should we investigate? A: Several factors can impact sensitivity: (1) Verify primer and gRNA sequences, as minor synthesis errors dramatically affect performance; (2) Check RPA reagent storage conditions and expiration dates; (3) Optimize the gRNA ratio—try different combinations of gRNA-2, gRNA-3, and gRNA-5; (4) Confirm adequate specimen decontamination for respiratory samples; (5) Validate against a reference method to ensure your comparison is appropriate [3].
Q: Can these advanced detection methods be implemented in resource-limited settings? A: Yes, with appropriate adaptations: (1) The ActCRISPR-TB assay has been successfully adapted to lateral flow format, eliminating the need for fluorescence readers; (2) For mNGS, portable nanopore sequencing platforms can provide results within 10 minutes after bioinformatic analysis; (3) Simplified "one-pot" reactions reduce equipment requirements; (4) Strategic partnerships can help establish sequencing capabilities in central reference laboratories [3] [82].
Signaling Pathways & Experimental Workflows
Diagram 1: Comparative Workflows for Advanced Pathogen Detection Technologies. This diagram illustrates the parallel pathways for CRISPR-based and metagenomic NGS detection methods, highlighting key decision points in the experimental process.
The Scientist's Toolkit: Research Reagent Solutions
Table 3: Essential Research Reagents for Advanced Pathogen Detection Assays
| Reagent/Material | Function | Specification Notes |
|---|---|---|
| TIANamp Micro DNA Kit | Nucleic acid extraction from limited-volume specimens | Optimized for low-biomass samples; suitable for CSF and other precious specimens [81] |
| Cas12a Protein | CRISPR-associated nuclease for target recognition and signal generation | Ensure high purity and nuclease-free status; verify activity with control targets [3] |
| Guide RNAs (gRNAs) | Target-specific recognition elements for Cas12a | Multiple gRNAs (gRNA-2, -3, -5) recommended for enhanced sensitivity; requires HPLC purification [3] |
| RPA Enzyme Mix | Isothermal amplification of target sequences | Enables "one-pot" reaction format; sensitive to Mg2+ concentration [3] |
| IS6110-targeting Primers | Specific amplification of M. tuberculosis complex | Critical for ActCRISPR-TB assay; validate specificity against non-target species [3] |
| BGISEQ-50/MGISEQ-2000 Platform | High-throughput sequencing for mNGS | Alternative: Nanopore sequencing for rapid turnaround [81] [82] |
| Pathogen Databases (RefSeq) | Reference for bioinformatic pathogen identification | Contains 4945 viral, 6350 bacterial, 1064 fungal, and 234 parasite genomes [81] |
| ssDNA Fluorescent Reporter | Signal generation in CRISPR assays | FAM-TTATT-BHQ1 commonly used; alternative quenchers available for optimization [3] |
Frequently Asked Questions
What does it mean for an assay to detect 51% more variants, and why is this significant? In a prospective head-to-head comparison study involving 182 patients, a comprehensive genomic profiling (CGP) assay demonstrated the ability to detect 51% more pathogenic single nucleotide variants (SNVs) and insertions/deletions (indels) compared to other on-market assays [84]. This enhanced sensitivity is particularly impactful because 91% of these additional clinically actionable variants were found below 0.5% variant allele frequency (VAF), a range where many conventional tests fail to reliably detect alterations [84]. This means significantly fewer patients receive null reports with no pathogenic findings, thereby increasing opportunities for matched targeted therapies.
Which specific assay demonstrated this superior performance, and what is its underlying technology? The assay is Northstar Select, a plasma-based, tumor-naive CGP assay that utilizes proprietary Quantitative Counting Template (QCT) technology, a form of single-molecule next-generation sequencing (smNGS) [84] [85]. This core technology allows for precise molecular counting, which minimizes errors during sample processing and bioinformatic analysis, leading to enhanced sensitivity across all variant classes, including SNVs, indels, copy number variants (CNVs), fusions, and microsatellite instability (MSI-H) [84].
How was this performance advantage validated to ensure the extra findings were not false positives? The superior sensitivity was confirmed through orthogonal testing with digital droplet PCR (ddPCR), which demonstrated 98% concordance with the Northstar Select results [85]. Furthermore, the study confirmed that the additional variants detected were not due to clonal hematopoiesis (CH), a common source of false positives in liquid biopsy. Matched buffy coat testing identified CH variants at similar rates in both Northstar Select and the comparator assays [84] [85].
What are the key wet and dry lab quality parameters that correlate with variant call accuracy? Research has shown a significant correlation between false-positive variant calls and specific quality parameters [86]. Key parameters from the wet lab process include ΔΔCq (for DNA degradation), pre-capture library metrics (peak size and DNA amount), and post-capture library concentration. In the dry lab process (bioinformatics), important metrics are total reads, mapping rates, duplication rates, mean depth, and depth coverage [86]. Among these, capture library concentration and mean depth were identified as strong independent predictors of somatic false-positive variants [86].
Table 1: Key Analytical Performance Metrics from the Head-to-Head Validation Study
| Performance Metric | Northstar Select Performance | Comparator Assays (Range) |
|---|---|---|
| Patients Analyzed | 182 (across >17 tumor types) | 182 (same patient cohort) |
| Additional Pathogenic SNV/Indels Detected | +51% [84] | Baseline |
| Additional Copy Number Variants (CNVs) Detected | +109% [84] | Baseline |
| Reduction in Null Reports (No Pathogenic Results) | 45% fewer [84] | Baseline |
| SNV/Indel Limit of Detection (LOD95) | 0.15% VAF [84] | Typically >0.2% VAF [84] |
| CNV Limit of Detection (LOD95) | 2.11 copies (amp), 1.80 copies (loss) [84] | 2.46-3.83 copies (amp), ≥20-30% TF (loss) [85] |
| Specificity | >99.9% for all variant classes [84] | Varies by assay |
Table 2: Correlated Quality Parameters for Minimizing False Positives in CGP [86]
| Process Area | Quality Parameter | Impact on Variant Calling |
|---|---|---|
| Wet Lab | ΔΔCq, Pre-capture library peak size & DNA amount, Capture library concentration | Inferior quality correlates with higher false-positive rates. |
| Dry Lab (Bioinformatics) | Total reads, Mapping rates, Duplication rates, Mean depth, Depth coverage | Inferior quality correlates with higher false-positive rates. |
Detailed Experimental Protocols
Protocol 1: Prospective Head-to-Head Clinical Validation
This protocol outlines the methodology used to compare the clinical performance of the investigational assay against established on-market tests [84].
- Patient Cohort & Sample Collection: Enroll 182 patients with advanced-stage solid tumors from multiple clinical sites. At the time a routine, on-market CGP liquid biopsy is ordered as standard of care, collect two blood samples from the same venipuncture.
- Sample Processing: One blood sample is processed using the clinician's chosen comparator assay (from a selection of commercially available tests). The paired sample is processed using the investigational assay (Northstar Select).
- Analysis: Perform genomic profiling according to each assay's established workflow. For the investigational assay, this involves:
- cfDNA Extraction: Isolate cell-free DNA from plasma.
- Library Preparation: Use the proprietary QCT technology for target enrichment and library construction.
- Sequencing: Perform next-generation sequencing.
- Bioinformatic Analysis: Utilize custom pipelines for variant calling, including SNVs/indels, CNVs, fusions, and MSI.
- Data Comparison: Compare the final reports from both assays for the number and type of pathogenic variants detected, the rate of null reports, and the VAF of additional variants found.
- Orthogonal Confirmation: For a subset of variants detected only by the investigational assay, use digital droplet PCR (ddPCR) on the same patient sample to confirm true positivity.
Protocol 2: Determining Limit of Detection (LOD)
This protocol describes the analytical validation to establish the lowest concentration of a variant that can be reliably detected [84].
- Sample Preparation: Create contrived reference samples with known variants (SNVs, indels, CNVs) at a range of concentrations. For SNV/indels, this involves dilutions spanning a VAF range (e.g., 0.06% to 0.35%).
- Replication and Testing: Analyze each dilution level in multiple replicates (e.g., 10-20 times) using the investigational assay.
- Data Analysis: Calculate the detection rate at each concentration level. The Limit of Detection (LOD95) is defined as the lowest concentration at which 95% of the replicates test positive.
- Orthogonal Confirmation: Confirm the LOD using an alternative method, such as digital droplet PCR, to verify the true variant allele frequency in the contrived samples.
The Scientist's Toolkit: Essential Research Reagents & Materials
Table 3: Key Reagent Solutions for Advanced CGP Assay Development
| Research Reagent / Material | Function in the Workflow |
|---|---|
| Quantitative Counting Template (QCT) Oligos | Proprietary templates that enable precise, single-molecule counting and minimize amplification bias, forming the core of the sensitive detection technology [84]. |
| Hybridization Capture Probes (84-gene panel) | Biotinylated oligonucleotides designed to enrich genomic regions of clinical interest from a broad gene list for sequencing [84]. |
| Magnetic Beads (Streptavidin-coated) | Used to capture and wash the probe-bound targets, enabling the purification of the enriched library before sequencing. |
| Custom Bioinformatic Pipelines | Specially designed algorithms for base calling, alignment, variant calling, and noise reduction, crucial for distinguishing low-VAF true positives from background noise [84]. |
| Digital Droplet PCR (ddPCR) Reagents | Used as an orthogonal method for independent confirmation of low-frequency variants detected by NGS, validating assay sensitivity [84] [85]. |
Experimental Workflow and Technology Diagram
CGP Assay Comparison Workflow
Sensitivity Enhancement Logic
Lateral Flow Assays (LFAs) have emerged as indispensable point-of-care diagnostic tools, aligning with the WHO ASSURED criteria (Affordable, Sensitive, Specific, User-friendly, Rapid and robust, Equipment-free, and Deliverable) [87]. Their significance is particularly pronounced in the context of pathogen detection, where rapid, on-site diagnosis can dramatically impact public health outcomes and epidemic containment [88]. The core challenge in adapting LFAs for sophisticated pathogen detection lies in enhancing their analytical sensitivity and specificity to match or approach the performance of laboratory-based methods, without compromising their point-of-care advantages [89]. This technical support center addresses the key experimental and performance-related issues researchers encounter in this pursuit, providing troubleshooting guidance and detailed methodologies to advance the field of high-sensitivity pathogen detection.
Frequently Asked Questions (FAQs): Enhancing LFA Performance
1. What are the primary strategies to improve the sensitivity of a pathogen LFA? Sensitivity enhancement is multi-faceted. Key strategies include:
- Advanced Labels: Replacing conventional colloidal gold with more potent signal generators such as magnetic nanozymes, upconversion nanoparticles, or fluorescent tags [89] [87].
- Assay Format Innovation: Employing novel formats, like a competitive assay with two test lines for small molecules, or using multivalent aptamers to improve binding affinity and kinetics for pathogens [90] [89].
- Pre-enrichment Techniques: Utilizing methods like test-zone pre-enrichment, where the sample is allowed to interact with the capture probe before the signaling unit is released, thereby increasing the effective analyte concentration at the test line [91].
- Signal Amplification: Integrating enzymatic amplification or nucleic acid amplification techniques like isothermal amplification or CRISPR/Cas systems [87] [92].
2. How does the choice between sandwich and competitive format affect my LFA design for pathogens? The format is dictated by the size and epitope availability of the target.
- Sandwich Format: Used for larger analytes (like many pathogen antigens) with multiple, distinct epitopes. It requires two different antibodies (or other capture molecules) that bind to the target simultaneously. A positive result shows a colored test line [93].
- Competitive Format: Used for small molecules (like toxins or antibiotics) with a single epitope. The analyte in the sample competes with a labeled analog for a limited number of antibody binding sites. In a common format, the absence of a test line indicates a positive result [90] [93]. For pathogens, the sandwich format is most common.
3. What are the critical components of an LFA strip and their functions? A standard LFA strip consists of overlapping modules on a backing card:
- Sample Pad: The point of sample application; it controls sample release and can be pre-treated with buffers or blockers to condition the sample [88] [93].
- Conjugate Pad: Contains the dried, labeled biorecognition element (e.g., antibody-conjugated nanoparticles). It must release the conjugate rapidly and uniformly upon contact with the liquid sample [88].
- Nitrocellulose Membrane: The heart of the assay, where the test and control lines are immobilized. Capillary flow and the critical immunoreaction occur here [93].
- Absorbent Pad: Acts as a sink, wicking the fluid through the strip and ensuring continuous flow [88].
4. My LFA shows weak test line intensity. What could be the cause? Weak signal intensity can stem from several factors, often related to reagent quality or strip assembly.
- Suboptimal Conjugation: The pH of the conjugation buffer may not be ideal, leading to inefficient binding of antibodies to nanoparticles and subsequent aggregation [93].
- Insufficient Capture Reagent: The concentration of the antibody immobilized on the test line may be too low to efficiently capture the labeled complex [93].
- Poor Release from Conjugate Pad: The conjugate pad material or its pre-treatment may not allow for complete and rapid release of the labeled detector [88].
- Incorrect Membrane Flow Rate: A membrane with too large a pore size may cause the sample to flow too quickly, reducing the interaction time between the analyte and the capture antibody [93].
Troubleshooting Guides
Problem: Low Sensitivity and High Limit of Detection
Potential Causes and Solutions:
Cause: Inefficient Signal Label.
- Solution: Transition from conventional colloidal gold to more sensitive labels. For example, utilize magnetic nanozymes (e.g., Fe₃O₄@MOF@PtPd), which offer both separation/enrichment capabilities and high catalytic activity for signal amplification [89].
- Protocol:
- Synthesize carboxyl-functionalized Fe₃O₄ nanoparticles via a solvothermal method.
- Grow a metal-organic framework (MOF) on the magnetic core.
- Deposit a bimetallic PtPd shell onto the MOF to create the nanozyme.
- Functionalize the nanozyme with vancomycin (for Gram-positive bacteria) or specific antibodies for targeted capture [89].
Cause: Slow Binding Kinetics of Probes.
- Solution: Implement multivalent aptamers (multi-Apts) instead of monovalent ones. Multivalency creates a synergistic effect, significantly improving binding affinity and reducing the required incubation time [89].
- Protocol (Construction of HCR-multi-Apt):
- Design two metastable, biotinylated hairpin DNAs (H1 and H2) and a biotinylated extended aptamer (Bio-exApt).
- Initiate a hybridization chain reaction (HCR) by adding a trigger DNA to H1 and H2, forming a multibranched DNA scaffold.
- Hybridize the Bio-exApt to the HCR scaffold to create the final HCR-multi-Apt with multiple aptamer units [89].
Cause: Low Analytic Concentration.
- Solution: Apply a test-zone pre-enrichment strategy. This method increases the local concentration of the analyte at the test line before the signaling unit arrives.
- Protocol (Test-zone Pre-enrichment):
- Assemble the LFA strip without the conjugate pad.
- Apply the sample directly to the sample pad. Allow it to flow and be captured by the immobilized antibody on the test line.
- After the sample has been enriched (e.g., 6-8 minutes for 50 µL), place the conjugate pad in its standard position.
- Apply running buffer to release the detector conjugate from the pad, which then flows to the test line and generates a signal [91].
Problem: Non-Specific Binding and High Background
Potential Causes and Solutions:
Cause: Inadequate Blocking.
- Solution: Systematically optimize the blocking agents and surfactants used in the sample and conjugate pads.
- Protocol: Pre-treat the sample pad with a solution containing blockers like BSA (1%), casein (0.1-0.5%), or gelatin (0.05-0.1%), and surfactants like Tween-20 (<0.05%) in a suitable buffer (e.g., carbonate or Tris). Dry the pad at 60-70°C for 1 hour before assembly [93].
Cause: Suboptimal Conjugation pH.
- Solution: Meticulously determine the ideal pH for conjugating your specific antibody to nanoparticles.
- Protocol:
- Prepare a series of colloidal gold solutions adjusted to different pH values.
- Add a fixed amount of antibody to each and incubate.
- Add 2M sodium chloride to each tube. Aggregation (color change from red to blue) indicates unstable conjugation.
- The highest pH value that does not cause aggregation is the optimum for conjugation [93].
Experimental Protocols for Key Methodologies
Protocol 1: Developing a Novel Quantitative LFA for Small Molecules
This protocol outlines the development of a quantitative, competitive LFA for vancomycin, featuring a two-test-line design for an extended dynamic range [90].
Conjugate Preparation:
- Couple vancomycin to Bovine Serum Albumin (BSA) using EDC chemistry.
- Purify the BSA-Van conjugate via dialysis.
- Biotinylate the BSA-Van conjugate using an NHS-LC-biotin kit.
Gold Nanoparticle (AuNP) Labelling:
- Adjust the pH of AuNP solutions to 8.4.
- Separately conjugate the anti-vancomycin IgG and the biotinylated BSA-Van to the AuNPs.
- Block excess sites with BSA.
Strip Assembly and Printing:
- Dispense two test lines onto the nitrocellulose membrane:
- Test Line 1 (Antibody Line): Anti-vancomycin IgG.
- Test Line 2 (Avidin Line): Avidin.
- The control line contains a species-specific secondary antibody.
- Assemble the strip with sample pad, conjugate pad (containing the dried AuNP conjugates), membrane, and absorbent pad.
- Dispense two test lines onto the nitrocellulose membrane:
Quantitative Readout:
- Acquire an image of the developed strip using a smartphone camera.
- Use an automated image analysis algorithm to quantify the signal ratio between the two test lines.
- Extrapolate the vancomycin concentration from a pre-established calibration curve [90].
Protocol 2: Ultra-Sensitive Pathogen Detection using Multivalent Aptamer and Nanozyme
This protocol describes a highly sensitive sandwich LFA for S. aureus, integrating a multivalent aptamer for capture and a magnetic nanozyme for detection [89].
Prepare the Capture Probe (HCR-multi-Apt):
- Synthesize the HCR-multi-Apt as described in the troubleshooting guide above.
Prepare the Detection Probe (Vancomycin-Modified Nanozyme):
- Synthesize the Fe₃O₄@MOF@PtPd nanozyme.
- Modify the nanozyme surface with vancomycin to enable specific binding to Gram-positive bacteria.
LFA Procedure:
- Immobilize the HCR-multi-Apt on the test line.
- Apply the sample. Pathogens are captured by the HCR-multi-Apt.
- The vancomycin-modified nanozyme is added and binds to the captured pathogens, forming a sandwich complex.
- The magnetic property of the nanozyme allows for external enrichment and separation, concentrating the signal at the test line.
- The peroxidase-like activity of the PtPd shell can be used for catalytic signal amplification [89].
Key Research Reagent Solutions
The following table details essential materials and their functions in LFA development for pathogen detection.
| Reagent / Material | Function and Importance in LFA Development |
|---|---|
| Nitrocellulose Membrane | The substrate for capillary flow and the platform where test/control lines are immobilized; pore size directly impacts flow rate and sensitivity [93]. |
| Gold Nanoparticles (AuNPs) | A classic colorimetric label; inert and easily conjugated to antibodies/aptamers via electrostatic interactions; size (20-80 nm) affects color and performance [93]. |
| Magnetic Nanozymes | Multifunctional labels (e.g., Fe₃O₄@MOF@PtPd) that provide separation (magnetism), enrichment, and high catalytic activity for signal amplification [89]. |
| Multivalent Aptamer | A synthetic DNA/RNA probe with multiple binding sites; significantly improves binding affinity and kinetics to pathogen targets compared to monovalent aptamers [89]. |
| Biotin-Streptavidin/Avidin | A high-affinity binding pair used to immobilize capture probes or, as in a novel vancomycin LFA, to create a second test line for quantitative analysis [90]. |
| Blocking Agents (BSA, Casein) | Proteins used to passivate the strip's components (pads, membrane), reducing non-specific binding and background noise [93]. |
| Surfactants (Tween-20) | Added to running buffers and pads to modulate flow characteristics and minimize hydrophobic interactions that cause non-specific binding [93]. |
LFA Workflow and Enhancement Strategies
The diagram below illustrates the core workflow of a standard Lateral Flow Assay and integrates key sensitivity-enhancement strategies discussed in this guide.
LFA Strip Assembly and Material Functions
This diagram provides a detailed view of the physical construction of an LFA strip and the specific function of each component.
This technical support center provides troubleshooting guides and FAQs to help researchers address common challenges in pathogen detection assays, framed within the broader thesis of improving assay sensitivity.
Frequently Asked Questions (FAQs) and Troubleshooting Guides
Sample Preparation and Quality Control
Q1: What are the common issues in sample preparation that affect pathogen detection sensitivity?
Incomplete cell lysis and contamination are major issues leading to suboptimal yields and inaccurate results [79] [94] [95].
- Solution for Incomplete Lysis: Ensure strict adherence to protocol instructions regarding incubation times and temperatures [79] [95].
- Solution for Contamination: Always use sterile techniques and reagents when handling samples [79] [94] [95].
Q2: How does sample quality impact detection accuracy?
High-quality samples are paramount for accurate pathogen detection. Contaminants present in the sample can interfere with the analysis and lead to erroneous interpretations [79] [94] [95]. Proper extraction kits tailored to your sample type (e.g., blood, tissue, environmental) are crucial as they significantly affect nucleic acid yield and purity [79] [94].
qPCR Optimization and Troubleshooting
Q3: What should I do if I detect no amplification in my qPCR assay?
When no signal appears, investigate several potential causes [79] [94]:
- Reagent Quality: Check reagent expiration dates and ensure proper storage conditions [79] [95].
- Primer Design: Verify primer specificity and efficiency; consider using software tools for optimal primer selection [79] [94].
- Instrument Calibration: Ensure your qPCR instrument is properly calibrated [79] [94].
Q4: How can I address non-specific amplification in qPCR?
Non-specific binding leads to false positives.
- Solution: Optimize annealing temperatures using gradient testing [79] [94] [95]. Using Hot Start PCR Kits can also minimize non-specific amplification by activating polymerases only at elevated temperatures [79] [94].
Q5: What factors influence my Ct (Cycle Threshold) values?
Ct values represent the point at which fluorescence exceeds background levels, with lower Ct values indicating higher initial template concentrations [79] [94]. Factors affecting Ct values include [79] [94] [95]:
- Template quality and quantity
- Primer efficiency
- Reaction mixture quality
Advanced Detection Methods
Q6: What are the limitations of culture-based methods, and what are the alternatives?
Culture-based methods, while considered a gold standard, are often slow, labor-intensive, and unsuitable for real-time decision-making [96]. Advanced molecular methods like qPCR and innovative CRISPR-based assays offer faster, more sensitive alternatives [96].
Q7: How can I improve pathogen detection rates from complex samples like abscess specimens?
Implementing optimized diagnostic protocols significantly enhances pathogen detection efficacy. A 2025 study demonstrated that a comprehensive protocol combining aerobic/anaerobic culture, gram-stain microscopy, acid-fast bacilli staining, and blood culture bottle enrichment achieved an 81.9% positivity rate—a 20.1 percentage point improvement over conventional methods [97].
Pathogen Distribution from 1,297 Abscess Specimens
The following data is adapted from a 2025 study analyzing optimized pathogen detection in abscess specimens [97].
Table 1: Overall Pathogen Distribution from 1,297 Clinical Abscess Specimens
| Pathogen Category | Percentage | Predominant Species (Composition) |
|---|---|---|
| Gram-negative bacteria | 50.6% | Escherichia coli (55.0%), Klebsiella pneumoniae (23.0%), Acinetobacter baumannii (4.0%) |
| Gram-positive cocci | 33.7% | Streptococcus spp. (45.0%), Staphylococcus aureus (19.0%), Enterococcus faecium (6.0%) |
| Anaerobic bacteria | 5.3% | Recovered through optimized protocols |
| Acid-fast bacilli | 1.1% | Detected via enhanced microscopy and culture |
Table 2: Anatomical Distribution of Pathogens in Abscess Specimens
| Anatomical Site | Cases | Predominant Pathogens |
|---|---|---|
| Perianal abscesses | 358 | E. coli (51.8%), K. pneumoniae (14.7%), Streptococcus spp. (15.7%) |
| Maxillofacial infections | 244 | Various pathogens (18.0% of total isolates) |
| Abdominal abscesses/peritonitis | ~221 | Various pathogens (17.0% of total isolates) |
| Hepatic abscesses | ~67 | Various pathogens (5.2% of total isolates) |
Impact of Protocol Optimization on Detection Rates
Table 3: Additional Pathogens Detected Through Enhanced Protocols (n=261)
| Detection Method | Additional Pathogens Identified | Percentage |
|---|---|---|
| Anaerobic Culture | 88 strains | 33.7% |
| Smear Microscopy | 84 cases (bacteria observed prior to culture) | 32.2% |
| Acid-Fast Staining | 18 strains | 6.9% |
| Enrichment Techniques | Brucella melitensis (4 isolates) and others | 1.5% |
Detailed Experimental Protocols
Optimized Diagnostic Protocol for Abscess Specimens
This protocol, validated on 1,297 specimens, significantly improves pathogen detection rates [97]:
Primary Aerobic Culture
- Inoculate pus specimens onto Sheep blood agar and China Blue agar plates
- Incubate at 35°C with 5% CO₂ for 24 hours
- Process culture-positive samples for identification and antimicrobial susceptibility testing
Extended and Specialized Culture for Negative Specimens
- Extend aerobic culture incubation to 72 hours
- Perform parallel anaerobic culture using GENbag anaerobic bags at 35°C for 72 hours
- Conduct Gram staining and acid-fast staining on all specimens
Enrichment Culture for Microscopy-Negative Specimens
- Aseptically inject 2-3 mL of pus specimen into blood culture bottles
- Load into automated blood culture system (e.g., FX2000) for continuous monitoring
- When positivity signaled: aseptically aspirate culture broth for Gram staining and microscopic examination
- Inoculate positive cultures onto aerobic, selective, and anaerobic blood agar plates
- Incubate for 5 days maximum
Bacterial Identification
- Perform Gram staining on all isolates
- Identify anaerobic isolates using VITEK Compact 2 with ANC cards or MALDI-TOF MS
- Identify aerobic isolates using standard identification systems
CRISPR-Based Pathogen Detection Protocol
CRISPR technology enables rapid, precise pathogen detection with applications in food safety and public health [96]:
Sample Processing and Nucleic Acid Extraction
- Extract target nucleic acids (DNA or RNA) from food or clinical matrices
- Use appropriate extraction kits based on sample type
Target Amplification
- Employ isothermal amplification techniques like Recombinase Polymerase Amplification (RPA)
- Amplify target pathogen sequences at constant temperature (no thermal cycler required)
CRISPR-Cas Detection
- Program Cas proteins (Cas12, Cas13) with specific crRNAs to recognize target sequences
- Upon target recognition, Cas proteins exhibit collateral cleavage activity
- This activity cleaves reporter molecules (fluorescent or colorimetric)
Result Visualization
- Detect fluorescence signals for laboratory settings
- Use lateral flow strips for point-of-care applications
- Results are typically available within hours
Experimental Workflow and Signaling Pathways
Optimized Abscess Specimen Processing Workflow
CRISPR-Based Pathogen Detection Mechanism
Research Reagent Solutions
Table 4: Essential Research Reagents for Pathogen Detection Assays
| Reagent / Material | Function | Application Notes |
|---|---|---|
| Nucleic Acid Extraction Kit | Isolates DNA/RNA from samples | Choose based on sample type: RNA Extraction Kit for blood, DNA Extraction Kit for tissue, general Nucleic Acid Extraction Kit for environmental samples [79] [94] |
| qPCR Master Mix | Contains enzymes, dNTPs, buffers for qPCR | Hot Start PCR Kits reduce non-specific amplification; optimize formulation for your assay [79] [95] |
| Blood Culture Bottles | Enriches low-abundance pathogens | Critical for detecting fastidious organisms; use with automated systems like FX2000 [97] |
| Selective Culture Media | Supports growth of specific pathogens | Examples: Sheep blood agar, China Blue agar; essential for primary cultivation [97] |
| CRISPR-Cas Reagents | Enables specific nucleic acid detection | Includes Cas proteins (Cas12, Cas13) and crRNAs; ideal for rapid, portable detection [96] |
| Staining Reagents | Visualizes microorganisms microscopically | Gram stain kits, acid-fast stain kits crucial for direct specimen examination [97] |
Conclusion
The relentless pursuit of higher sensitivity in pathogen detection is yielding transformative diagnostic tools. The integration of multi-guide RNA CRISPR assays, synthetic biology components, and ultra-sensitive liquid biopsy platforms is consistently pushing detection limits downward, enabling the identification of previously undetectable infections and low-frequency genomic alterations. Future progress hinges on the seamless merging of innovative biological mechanisms with robust, automated workflows to ensure these advanced assays are not only powerful in research settings but also reproducible, accessible, and clinically actionable. The continued evolution of these technologies promises to redefine the standards of early diagnosis, personalized treatment, and precision oncology, ultimately improving patient outcomes on a global scale.
References
- 1. Revisiting ELISA with in situ amplification of biomarkers to ... [https://www.sciencedirect.com/science/article/abs/pii/S0925400524015107]
- 2. Enhancing ELISA Sensitivity: From Surface Engineering to ... [https://pubmed.ncbi.nlm.nih.gov/40710084/]
- 3. Sensitive pathogen DNA detection by a multi-guide RNA ... [https://www.nature.com/articles/s41467-025-63094-x]
- 4. Analytical techniques for nucleic acid and protein detection ... [https://www.nature.com/articles/s12276-025-01453-w]
- 5. Nucleic Acids for Ultra-Sensitive Protein Detection - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC3574740/]
- 6. CRISPR-Cas12a: Functional overview and applications [https://pmc.ncbi.nlm.nih.gov/articles/PMC7090318/]
- 7. Cas12a [https://en.wikipedia.org/wiki/Cas12a]
- 8. Structures, mechanisms and applications of RNA ... - PMC - NIH [https://pmc.ncbi.nlm.nih.gov/articles/PMC11375968/]
- 9. Development and application of sensitive, specific, and rapid ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC8014745/]
- 10. CRISPR-Cas-based techniques for pathogen detection [https://pmc.ncbi.nlm.nih.gov/articles/PMC10403697/]
- 11. Amplification-free RNA detection with CRISPR–Cas13 [https://www.nature.com/articles/s42003-021-02001-8]
- 12. RNA structure modulates Cas13 activity and enables ... [https://www.nature.com/articles/s41587-025-02868-6]
- 13. Discovery of CRISPR-Cas12a clades using a large ... [https://www.nature.com/articles/s41467-025-63160-4]
- 14. Sensitive pathogen DNA detection by a multi-guide RNA ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12443966/]
- 15. Thermally programmed one-pot CRISPR assay for on-site ... [https://www.nature.com/articles/s41467-025-65193-1]
- 16. Rapid detection of Nipah virus using the one-pot RPA- ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10345719/]
- 17. The Limit | LCGC International of Detection [https://www.chromatographyonline.com/view/limit-detection]
- 18. - Wikipedia Detection limit [https://en.wikipedia.org/wiki/Detection_limit]
- 19. Blank, Limit and of Quantitation - PMC Limit of Detection Limit of [https://pmc.ncbi.nlm.nih.gov/articles/PMC2556583/]
- 20. Variant Allele Frequency [https://cegat.com/variant-allele-frequency/]
- 21. Establishing a Variant Allele Frequency Cutoff for Manual ... [https://www.sciencedirect.com/science/article/pii/S1525157824002502]
- 22. Next-Generation Sequencing Methodologies To Detect ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10843083/]
- 23. A novel targeted hybrid capture-NGS assay for sensitive ... [https://pubmed.ncbi.nlm.nih.gov/41247049/]
- 24. Transforming Molecular Diagnostics and Biosensing [https://pmc.ncbi.nlm.nih.gov/articles/PMC12467008/]
- 25. Advances in the application of CRISPR technology ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12620484/]
- 26. How To Design Guide RNA for CRISPR [https://www.synthego.com/guide/how-to-use-crispr/design-grna-crispr/]
- 27. A streamlined CRISPR-based test for tuberculosis detection ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12327463/]
- 28. CRISPR Mouth-Swab Test Could Transform Tuberculosis ... [https://www.genengnews.com/topics/infectious-diseases/crispr-mouth-swab-test-could-transform-tuberculosis-screening/]
- 29. Enhancing ELISA Sensitivity: From Surface Engineering to ... [https://www.mdpi.com/2079-6374/15/7/434]
- 30. Cell-Free Protein Synthesis Explained [https://eu.idtdna.com/pages/applications/cell-free-protein-synthesis]
- 31. At-home, Cell-free Synthetic Biology Education Modules for ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11577157/]
- 32. Cell-Free Expression Support—Troubleshooting [https://www.thermofisher.com/us/en/home/technical-resources/technical-reference-library/protein-expression-support-center/cell-free-expression-support/cell-free-expression-support-troubleshooting.html]
- 33. Troubleshooting Guide for NEBExpress™ Cell-free E. coli ... [https://www.neb.com/en-us/tools-and-resources/troubleshooting-guides/troubleshooting-guide-for-nebexpress-cell-free-e-coli-protein-synthesis-system-neb-e5360?srsltid=AfmBOopnDF7EUN11vZyUPECuzKN4ImISbsQsFPKURP4NjnkOPD_YtIRb]
- 34. Cell-Free Protein Expression [https://www.neb.com/en-us/applications/protein-expression/cell-free-protein-expression?srsltid=AfmBOoq0YsPzwWxSYORAmqja74qPTkIOX8ltTX86uAhQhfU6VylASufR]
- 35. A User's Guide to Cell-Free Protein Synthesis - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC6481089/]
- 36. Recent Advances in Developing Cell-Free Protein ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12385134/]
- 37. Recent Improvements in CRISPR-Based Amplification ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC8515055/]
- 38. CRISPR‐driven diagnostics: Molecular mechanisms, clinical ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12464570/]
- 39. Cascade CRISPR/cas enables amplification-free ... [https://pubs.rsc.org/en/content/articlelanding/2021/cc/d0cc06412b]
- 40. Amplification-free detection of plant pathogens by ... [https://www.frontiersin.org/journals/plant-science/articles/10.3389/fpls.2025.1544513/full]
- 41. CRISPR Guide [https://www.addgene.org/guides/crispr/]
- 42. CRISPR-Based Genome Editing Support—Troubleshooting [https://www.thermofisher.com/us/en/home/technical-resources/technical-reference-library/genome-editing-support-center/crispr-based-genome-editing-support/crispr-based-genome-editing-support-troubleshooting.html]
- 43. Validation of a liquid biopsy assay with increased ... [https://pubmed.ncbi.nlm.nih.gov/40980342/]
- 44. BillionToOne's Northstar Select® Demonstrates Superior ... [https://www.billiontoone.com/news-media/billiontoones-northstar-select-r-demonstrates-superior-sensitivity-in-prospective-head-to-head-validation-study-publication]
- 45. Exploring Northstar Select: A Liquid Biopsy Built for Clinical ... [https://www.northstaronc.com/insights/introducing-northstar-select-a-liquid-biopsy-built-for-clinical-action]
- 46. Real-World Technical Hurdles of ctDNA NGS Analysis [https://pmc.ncbi.nlm.nih.gov/articles/PMC12564474/]
- 47. Validation of a liquid biopsy assay with increased ... [https://www.sciencedirect.com/science/article/pii/S2950195425000384]
- 48. GENOMICON-Seq enables realistic simulation of amplicon ... [https://www.nature.com/articles/s41598-025-05267-8]
- 49. Common Problems in Assay Development and How to Solve ... [https://protocolsandsolutions.com/blogs/news/common-problems-in-assay-development-and-how-to-solve-them]
- 50. ELISA Guide; Part 4: Troubleshooting [https://www.jacksonimmuno.com/secondary-antibody-resource/immuno-techniques/elisa-guide-part-4-troubleshooting/]
- 51. Troubleshooting Guide: ELISA [https://www.rndsystems.com/resources/troubleshooting-guide-elisa-development]
- 52. Optimizing Ligand Binding Assay Conditions for Accurate ... [https://swordbio.com/blog/optimizing-ligand-binding-assay-conditions-for-accurate-and-reproducible-results/]
- 53. Troubleshooting a Faulty ELISA [https://bitesizebio.com/37935/troubleshooting-faulty-elisa/]
- 54. Enhancing ELISA Sensitivity: From Surface Engineering to ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12293621/]
- 55. The importance of antibody orientation for enhancing ... [https://pubs.rsc.org/en/content/articlehtml/2024/sd/d4sd00206g]
- 56. Revolutionizing the capture efficiency of ultrasensitive ... [https://pubmed.ncbi.nlm.nih.gov/39257162/]
- 57. Troubleshooting Guide: Immunohistochemistry [https://www.rndsystems.com/resources/technical/troubleshooting-guide-immunohistochemistry]
- 58. IHC Troubleshooting Guide [https://www.thermofisher.com/us/en/home/life-science/protein-biology/protein-biology-learning-center/protein-biology-resource-library/pierce-protein-methods/ihc-troubleshooting-guide.html]
- 59. ICC/IF Troubleshooting [https://www.antibodies.com/applications/immunofluorescence/immunofluorescence-troubleshooting]
- 60. Chromium‐Doped Zinc Gallate Nanoparticles for ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12499398/]
- 61. Optimizing PCR: Proven Tips and Troubleshooting Tricks [https://www.the-scientist.com/optimizing-pcr-proven-tips-and-troubleshooting-tricks-71660]
- 62. PCR Optimization: Factors Affecting Reaction Specificity ... [https://www.mybiosource.com/learn/pcr-optimization-factors-affecting-reaction-specificity-and-efficien/]
- 63. Optimized Ribonucleoprotein Complexes Enhance Prime ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12345536/]
- 64. Research progress on the application of RPA-CRISPR/ ... [https://www.frontiersin.org/journals/cellular-and-infection-microbiology/articles/10.3389/fcimb.2025.1640938/full]
- 65. Development of a highly sensitive, high-throughput and ... [https://www.sciencedirect.com/science/article/abs/pii/S0956566325001976]
- 66. Liquid Handling for Reproducible Science Post 1: Basics of ... [https://formulatrix.com/life-science-automation-blog/liquid-handling-for-reproducible-science-post-1-basics-of-accuracy-and-precision/]
- 67. Automated Liquid Handlers As Sources of Error [https://www.bioprocessintl.com/assays/automated-liquid-handlers-as-sources-of-error]
- 68. Automated Liquid Handlers as Sources of Error [https://www.aicompanies.com/education-training/knowledge-center/automated-liquid-handlers-as-sources-of-error/]
- 69. Reproducibility of positive results for rare pathogens on the ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC7286436/]
- 70. Automated liquid handling robot for rapid lateral flow assay ... [https://pubmed.ncbi.nlm.nih.gov/35091761/]
- 71. Using Design of Experiments (DoE) in Method Development [https://www.labmanager.com/using-design-of-experiments-doe-in-method-development-34251]
- 72. Best Practices For Implementing Design Of Experiments ... [https://enertherm-engineering.com/best-practices-for-implementing-design-of-experiments-doe-in-industrial-settings/]
- 73. Research Progress on Multiplexed Pathogen Detection ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12191064/]
- 74. Method Validation Essentials, Limit of Blank ... [https://www.biopharminternational.com/view/method-validation-essentials-limit-blank-limit-detection-and-limit-quantitation]
- 75. Clinical evaluation of two pathogen enrichment ... [https://pubmed.ncbi.nlm.nih.gov/40497682/]
- 76. Understanding the Lifecycle Approach for Analytical ... [https://www.chromatographyonline.com/view/understanding-lifecycle-approach-analytical-procedures]
- 77. Ultrasensitive detection of clinical pathogens through a ... [https://www.nature.com/articles/s41467-025-59219-x]
- 78. An ERA-CRISPR/Cas12a Method for Highly Sensitive ... [https://pubmed.ncbi.nlm.nih.gov/41226017/]
- 79. Troubleshooting qPCR: Common Issues and Solutions for ... [https://www.visiblegenetics.com/troubleshooting-qpcr-common-issues-and-solutions-for-accurate-pathogen-detection/]
- 80. PCR/qPCR Troubleshooting Quick Reference [https://biopathogenix.com/pcr-qpcr-troubleshooting-quick-reference/]
- 81. Diagnostic performance and clinical utility of metagenomic ... [https://www.frontiersin.org/journals/cellular-and-infection-microbiology/articles/10.3389/fcimb.2025.1612628/full]
- 82. Clinical performance of real-time nanopore metagenomic ... [https://pubmed.ncbi.nlm.nih.gov/39875797/]
- 83. Clinical Impact of Cerebrospinal Fluid Multiplex Polymerase ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12478634/]
- 84. Validation of a liquid biopsy assay with increased sensitivity ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12447423/]
- 85. BillionToOne's Northstar Select® Demonstrates Superior ... [https://www.northstaronc.com/news/billiontoones-northstar-select-r-demonstrates-superior-sensitivity-in-prospective-head-to-head-validation-study-publication]
- 86. Correlation between variant call accuracy and quality ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10884978/]
- 87. Lateral flow assay with green nanomaterials [https://www.sciencedirect.com/science/article/abs/pii/S0166526X23000648]
- 88. Lateral flow assays for viruses diagnosis - PubMed Central - NIH [https://pmc.ncbi.nlm.nih.gov/articles/PMC9252863/]
- 89. Rapid and ultra-sensitive lateral flow assay for pathogens ... [https://www.sciencedirect.com/science/article/abs/pii/S0956566324000472]
- 90. Development of a novel quantitative lateral flow assay for ... [https://www.nature.com/articles/s41598-025-09145-1]
- 91. Improvement in Detection Limit for Lateral Flow Assay of ... [https://www.nature.com/articles/s41598-020-66456-1]
- 92. Recent advances in rapid detection of Helicobacter pylori ... [https://pubmed.ncbi.nlm.nih.gov/39820420/]
- 93. Development and Troubleshooting in Lateral Flow ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC7994469/]
- 94. Common Issues and Solutions for Accurate Pathogen Detection [https://www.pfgd.org/troubleshooting-qpcr-common-issues-and-solutions-for-accurate-pathogen-detection/]
- 95. Common Issues and Solutions for Accurate Pathogen Detection [https://www.rtslifescience.com/troubleshooting-qpcr-common-issues-and-solutions-for-accurate-pathogen-detection/]
- 96. CRISPR revolution: Unleashing precision pathogen ... [https://www.sciencedirect.com/science/article/pii/S104620232500115X]
- 97. Optimization of pathogen detection in abscess specimens [https://pmc.ncbi.nlm.nih.gov/articles/PMC12261717/]