Persister Cell Resuscitation: Mechanisms, Methods, and Therapeutic Implications
This article provides a comprehensive analysis of bacterial persister cell resuscitation, a critical process underlying chronic and relapsing infections.
Persister Cell Resuscitation: Mechanisms, Methods, and Therapeutic Implications
Abstract
This article provides a comprehensive analysis of bacterial persister cell resuscitation, a critical process underlying chronic and relapsing infections. Tailored for researchers, scientists, and drug development professionals, it synthesizes foundational knowledge on the triggers and molecular mechanisms that awaken dormant persisters. The content delves into cutting-edge single-cell and omics methodologies for studying resuscitation, addresses common challenges in experimental workflows, and offers a comparative evaluation of current models and validation techniques. By integrating these four core intents, this review aims to equip the scientific community with the insights needed to develop novel anti-persister strategies and overcome the clinical challenge of treatment-recalcitrant infections.
The Awakening Switch: Core Principles and Molecular Triggers of Persister Resuscitation
Troubleshooting Guides and FAQs
FAQ 1: How can I definitively confirm that the cells I am studying are in the VBNC state and not simply dead?
Answer: Confirming the VBNC state requires a multi-parameter approach, as no single assay is sufficient. You must demonstrate three key criteria simultaneously:
- Loss of Culturability: The cells must not form colonies on routine laboratory media that normally support their growth. This is confirmed when the colony-forming unit (CFU) count drops to zero.
- Maintenance of Viability: The cells must show signs of life through measures of metabolic activity or membrane integrity.
- Capacity for Resuscitation: The cells must be able to return to a culturable state when provided with specific, non-standard conditions (e.g., incubation in a resuscitation medium, passage through a host model) [1].
Troubleshooting Tip: A common error is misinterpreting a low CFU count for the VBNC state. Always combine plate counts with a direct viability method, such as live/dead staining. If all cells stain as "dead" (membrane-compromised), they are likely not VBNC. True VBNC cells will have intact membranes and often exhibit low-level metabolic activity [2] [3].
FAQ 2: My persister cell assays show high variability. What could be the cause?
Answer: Persister cell levels are highly sensitive to growth phase and environmental conditions.
- Growth Phase: The physiological state of the culture (exponential vs. stationary phase) dramatically influences persister frequency. Standardize the optical density and growth conditions precisely for all experiments.
- Antibiotic Killing Kinetics: Ensure you are performing a time-kill curve assay. A hallmark of persistence is a biphasic killing pattern, where the population is rapidly killed initially, followed by a plateau where the killing rate drastically decreases. This plateau represents the persister subpopulation [4] [5].
- Antibiotic Concentration and Type: Use a bactericidal antibiotic at a concentration significantly above the MIC (e.g., 5-100x MIC). Be aware that different antibiotics (e.g., ceftazidime vs. ciprofloxacin) can select for different persister subpopulations based on their mechanism of action [4].
FAQ 3: What is the most reliable method to distinguish between a persister cell and a VBNC cell in my sample?
Answer: The definitive test is the resuscitation assay following antibiotic removal.
- For Persisters: Wash the antibiotic away and resuspend the cells in fresh nutrient broth. Persister cells will typically resume growth and form colonies on solid media within hours to a day.
- For VBNC Cells: After washing, you will not see growth on standard media immediately. Instead, you must apply a specific resuscitation stimulus (e.g., incubation in a nutrient-poor medium, temperature shift, or addition of specific nutrients) and wait for a longer period (e.g., 24 hours) before culturable cells reappear [2] [1].
The following table summarizes the core differences to guide your experimental design.
| Feature | Persister Cells | VBNC Cells |
|---|---|---|
| Culturability | Retained on standard media [1] | Lost on standard media (CFU=0) [1] |
| Induction | Stochastic or by specific stresses (e.g., antibiotics) [6] [4] | Moderate, long-term stresses (e.g., starvation, temperature) [1] |
| Resuscitation | Rapid upon stress removal [1] | Requires specific resuscitation conditions [1] |
| Key Diagnostic | Biphasic killing in time-kill curves [4] | Resuscitation from a non-culturable state [2] |
Table 1: Experimental Evidence of Antibiotic-Induced Persister and VBNC States
This table summarizes quantitative data from key studies demonstrating how different antibiotics induce dormancy in bacterial populations.
| Bacterial Species | Stress Condition | Cell Survival Fraction (Log CFU/mL) | Phenotype Observed | Citation |
|---|---|---|---|---|
| Pseudomonas aeruginosa (PAO1) | Ceftazidime (5x MIC, 24h) | ~9.0 | High persister cell count | [4] |
| Pseudomonas aeruginosa (PAO1) | Ciprofloxacin (5x MIC, 24h) | ~6.0 | Lower persister cell count | [4] |
| Vibrio vulnificus & E. coli | Ampicillin → Resuscitation | Increased count after 24h resuscitation | Presence of VBNC cells in persister isolation experiments | [2] |
| E. coli | Ofloxacin (60x MIC, 5-7h) | Surviving subpopulation | Drug-induced persisters from metabolically active cells | [7] |
Table 2: Key Methodologies for Differentiating Bacterial States
This table compares the primary techniques used to assess the viability and physiological state of bacterial cells.
| Method | What It Measures | Application to Persisters/VBNC | Key Advantage | Key Limitation |
|---|---|---|---|---|
| Plate Count (Culture) | Culturability | Gold standard for detecting persisters; confirms non-culturability of VBNC cells [3] | Simple, inexpensive | Cannot detect VBNC cells [3] |
| Live/Dead Staining (e.g., BacLight) | Membrane Integrity | Identifies viable (membrane-intact) cells within a non-culturable population [2] [3] | Distinguishes live from dead cells | Does not confirm resuscitability |
| Redox Sensor Green (RSG) | Metabolic/Redox Activity | Detects low-level metabolic activity in dormant cells [4] | Probes metabolic state, not just membranes | Signal may be low or heterogeneous |
| Microfluidics & Single-Cell Imaging | Single-cell growth and division | Tracks history and fate of individual persister cells [7] | Unprecedented resolution of cell heterogeneity | Technically complex and specialized |
Experimental Protocols
Protocol 1: Isolation and Quantification of Persister Cells
Principle: Persisters are isolated by exposing a bacterial population to a high concentration of a bactericidal antibiotic, which kills the majority of the population. The surviving, antibiotic-tolerant cells are persisters [4] [5].
Method:
- Culture Preparation: Grow the bacterial strain of interest to the mid-exponential growth phase (e.g., OD610 ~0.2-0.3) in a suitable broth.
- Antibiotic Exposure: Treat the culture with a bactericidal antibiotic at a high multiple of the MIC (e.g., 5-100x MIC). Incubate for a defined period (typically 4-6 hours) under standard growth conditions with aeration.
- Wash and Removal: After incubation, wash the cells at least twice with phosphate-buffered saline (PBS) or saline solution to remove the antibiotic thoroughly.
- Viability Assessment: Resuspend the cell pellet in fresh medium. Perform serial dilutions and plate on non-selective agar plates to determine the number of surviving culturable cells (CFU/mL). This quantifies the persister population [2] [4].
Principle: VBNC cells are induced by prolonged exposure to a sub-lethal environmental stress. Their viability is confirmed by metabolic assays, and resuscitation is triggered by removing the stress and providing specific stimulating conditions [2] [1].
Method: A. Induction:
- Stress Application: Take a log-phase culture, wash to remove nutrients, and resuspend in a minimal, non-growth-supporting medium (e.g., 1/2 artificial seawater for vibrios, 0.85% NaCl for E. coli).
- Incubation: Incubate the culture under inducing conditions (e.g., 4°C for several days or weeks). Monitor culturability daily by plating.
- Confirmation: The VBNC state is achieved when the CFU count drops below the detection limit (<10 CFU/mL) while viability is maintained, as confirmed by live/dead staining [2].
B. Resuscitation:
- Stimulus: Once the VBNC state is confirmed, transfer the cells to a resuscitation medium. This could be a nutrient-rich broth diluted with the induction medium or a specific medium supplemented with host factors (e.g., serum).
- Incubation: Incubate under permissive conditions (e.g., a higher temperature like 20-37°C) for up to 24-48 hours.
- Confirmation: After resuscitation, plate the cells on standard agar to confirm the return of culturability. A significant increase in CFU count compared to the non-resuscitated control confirms successful resuscitation [2].
Signaling Pathways and Molecular Mechanisms
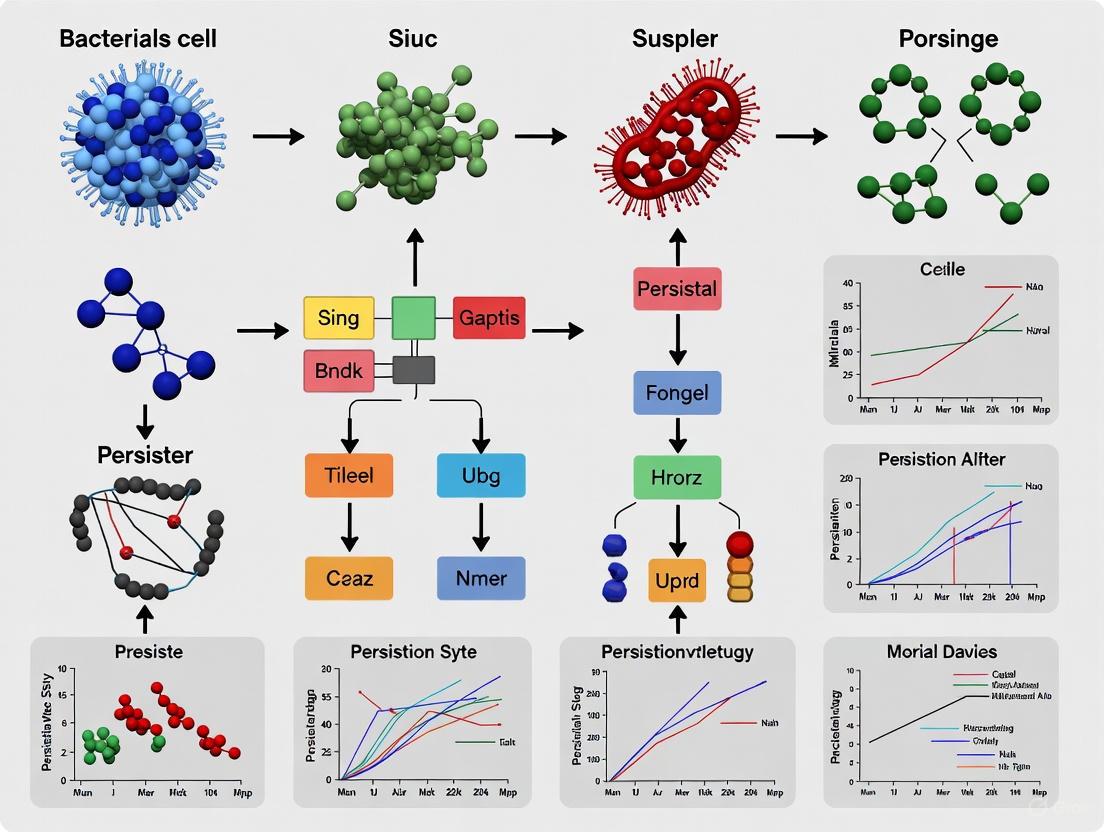
The formation of persister and VBNC cells is regulated by interconnected molecular pathways that respond to environmental stress. The diagram below illustrates the key mechanisms.
Diagram 1: Molecular Pathways Leading to Bacterial Dormancy. This diagram illustrates how environmental stress triggers core cellular responses—the Stringent Response, Toxin-Antitoxin (TA) System activation, and the SOS Response—that converge to induce a dormant state. The depth of this dormancy may influence whether a cell enters a readily revivable Persister state or requires specific signals to resuscitate from the VBNC state [6] [5] [2].
The Scientist's Toolkit: Research Reagent Solutions
Table 3: Essential Reagents for Studying Dormant Bacteria
This table lists key reagents and their applications in experiments focused on persister and VBNC cells.
| Reagent / Material | Function / Application | Specific Example |
|---|---|---|
| BacLight Live/Dead Viability Kit | Differentiates cells with intact (live) vs. compromised (dead) membranes using SYTO 9 and propidium iodide stains [2] [3]. | Confirming viability of non-culturable populations. |
| Redox Sensor Green (RSG) | Fluorescent dye used to detect metabolic and redox activity in cells, helping identify dormant but metabolically active persisters [4]. | Flow cytometry or microscopy to probe metabolic state. |
| Propidium Monoazide (PMA) | DNA-binding dye that penetrates only membrane-compromised cells; used with qPCR to selectively amplify DNA from viable cells (PMA-qPCR) [1]. | Quantifying viable pathogens in a sample without culture. |
| Ruthenium-based Oxygen Sensor (RTDP) | Oxygen-quenching fluorophore used in metabolic monitoring to detect oxygen consumption by viable bacteria in microfluidic devices [8]. | Real-time monitoring of bacterial growth and drug efficacy. |
| Toxin-Antitoxin Mutant Strains | Genetically modified strains (e.g., ΔhipA, Δ10TA) used to elucidate the functional role of specific TA modules in persistence [6] [4]. | Mechanistic studies on persister formation. |
| Microfluidic Devices | Platforms for single-cell analysis and long-term imaging, allowing tracking of individual cell fates before, during, and after antibiotic treatment [7]. | Studying heterogeneity and resuscitation of persisters. |
Frequently Asked Questions (FAQs)
Q1: Why do my persister cells fail to resuscitate after antibiotic removal and transfer to fresh media? The most common cause is the failure to completely remove the antibiotic or other stressors during washing steps. Even trace amounts can prevent resuscitation. Ensure thorough washing, for example, via membrane filtration and resuspension in fresh, pre-warmed medium at least three times [9]. Furthermore, the history of the pre-culture significantly impacts resuscitation potential; cells from long-term stationary phase cultures may have entered a deeper dormant state or a Viable But Non-Culturable (VBNC) state, which has different resuscitation requirements [9].
Q2: My persister cell counts are highly variable between replicate experiments. How can I improve consistency? Persister formation is inherently heterogeneous, but consistency can be improved by strictly standardizing pre-culture conditions. The length of the stationary phase, precise optical density at the time of antibiotic treatment, and the specific growth medium all dramatically influence persister levels [9] [10]. For example, extended stationary phase incubation increases the proportion of VBNC cells, which do not resuscitate on standard media, leading to variable colony-forming unit (CFU) counts [9].
Q3: Are persister cells truly dormant, or can they be metabolically active before resuscitating? The classical view is that persisters are dormant. However, recent single-cell studies reveal a more complex picture. When sampled from exponential phase, a significant fraction of cells that survive antibiotic treatment were actually growing before drug exposure [10]. The metabolic state of persisters is a continuum, ranging from deep dormancy to slow metabolism, and this state can change with environmental conditions [11].
Q4: What is the difference between a persister cell and a VBNC cell, and how can I distinguish them in my assays? Both are non-growing, antibiotic-tolerant phenotypes. The key distinguishing feature is that persisters can resuscitate in standard culture media after antibiotic removal, whereas VBNC cells cannot under the same conditions [9]. Persistence is often considered a transitional state that can lead to the VBNC state. In your assays, use methods that can differentiate them, such as flow cytometry with a fluorescent protein dilution method to monitor cell division, or parallel plating on standard media versus media supplemented with resuscitation factors like catalase [9].
Troubleshooting Guides
| Symptom | Possible Cause | Recommended Solution |
|---|---|---|
| No colony growth on plates after washing and plating. | Incomplete antibiotic removal. | Increase number of washing steps; use membrane filtration for more effective antibiotic removal; validate wash efficacy with a bioassay or HPLC. |
| Cells have entered a VBNC state. | Supplement resuscitation media with antioxidants (e.g., catalase) or use spent media from growing cultures [9]. | |
| Insufficient nutrient availability in the resuscitation media. | Use rich, fresh media (e.g., LB); ensure proper aeration for aerobic organisms. | |
| Colonies appear only after extended, unpredictable delays. | Stochastic resuscitation model assumed, but dynamics may be different. | Note that recent evidence suggests resuscitation can be exponential and accelerated over time, not purely stochastic. Ensure adequate incubation time and monitor plates for up to a week [12]. |
Issue: Inconsistent Persister Levels in Pre-Cultures
| Symptom | Possible Cause | Recommended Solution |
|---|---|---|
| High variability in persister counts between biological replicates. | Inconsistent pre-culture growth history. | Standardize inoculum size, growth time, and shaking speed. Use cultures grown to the same optical density (OD) from a fresh, overnight pre-culture. |
| Biofilm formation in culture flasks. | Use baffled flasks to improve aeration and minimize biofilm; sub-culture from the well-mixed suspension. | |
| A sudden drop in persister frequency. | Contamination. | Check for contamination by streaking on selective media and checking colony morphology. |
| Genetic drift in strain. | Re-streak from a frozen, master stock culture stored at -80°C. |
Table 1: Key Resuscitation Parameters from Single-Cell Studies
| Parameter | Value / Observation | Experimental Context | Source |
|---|---|---|---|
| Resuscitation Initiation | Within 1 hour post-antibiotic removal. | E. coli persisters after ampicillin treatment in fresh LB broth. | [9] |
| Doubling Time Post-Resuscitation | ~23-24 minutes. | First divisions of resuscitating E. coli persisters. This matches the doubling time of normal, untreated cells. | [9] |
| Resuscitation Dynamics Model | Exponential, not stochastic. The resuscitation rate accelerates over time. | E. coli and Salmonella enterica persisters after ampicillin treatment. | [12] |
| Impact of Treatment Duration | Longer antibiotic exposure increases cellular damage in persister progeny. | Treatment with β-lactams and quinolones leads to damaged resuscitated cells. | [12] |
| Key Controlling Parameter | Antibiotic concentration during treatment; efflux activity during resuscitation. | Efflux was identified as a critical factor for successful resuscitation after ampicillin treatment. | [12] |
Table 2: Impact of Pre-Culture Conditions on Persister States and Resuscitation
| Pre-Culture Condition | Effect on Persister Population | Implication for Resuscitation | |
|---|---|---|---|
| Short-term Stationary Phase | Higher proportion of "shallow" persisters with a greater likelihood of resuscitation. | More reliable and synchronous resuscitation in fresh media. | |
| Long-term Stationary Phase | Increased sub-population of VBNC cells and "deep" persisters. | Lower and more variable CFU counts after antibiotic treatment; may require specific resuscitation signals. | [11] [9] |
| Exponential Phase | Persisters can originate from both growing and non-growing sub-populations. | Resuscitation dynamics are highly heterogeneous, with some cells showing L-form-like growth or filamentation. | [10] |
Detailed Experimental Protocols
Adapted from BMC Microbiology [9]
Objective: To monitor persister resuscitation at the single-cell level and simultaneously quantify persister, VBNC, and dead cell subpopulations.
Key Reagents:
- Strain: E. coli with a chromosomally integrated, IPTG-inducible fluorescent protein (e.g., mCherry).
- Antibiotics: Ampicillin (or other β-lactam).
- Media: LB broth and LB agar plates.
- Equipment: Flow cytometer with cell-sorting capability, microcentrifuge, membrane filtration unit.
Methodology:
- Pre-culture and Fluorescence Induction: Grow the reporter strain overnight in LB with IPTG to induce strong fluorescent protein expression.
- Antibiotic Treatment: Dilute the pre-culture in fresh media (with IPTG) and grow to mid-exponential phase. Treat with a lethal dose of ampicillin (e.g., 200 µg/mL) for 3 hours to lyse all antibiotic-sensitive cells.
- Washing and Resuspension: Pellet the cells, wash thoroughly 3x with fresh LB (no IPTG, no antibiotic) to remove all traces of IPTG and the drug. Resuspend in fresh, pre-warmed LB.
- Flow Cytometry Analysis: Analyze the cells immediately using a flow cytometer. Monitor forward scatter (FSC) and fluorescence over time.
- Resuscitating Persisters: Cells that show a decrease in fluorescence over time due to dilution of the pre-formed fluorescent protein as they divide.
- VBNC Cells: Cells that retain high, constant fluorescence because they are not dividing.
- Validation: Plate samples on LB agar at various time points to correlate fluorescence dilution with CFU counts.
Adapted from MSB [12]
Objective: To track the resuscitation dynamics and cell fates of individual persister cells.
Key Reagents:
- Strain: E. coli constitutively expressing a fluorescent protein (e.g., GFP).
- Antibiotics: Ampicillin, Ciprofloxacin.
- Media: LB broth.
- Equipment: Time-lapse fluorescence microscope, agarose pads, microfluidic device (e.g., membrane-covered microchamber array).
Methodology:
- Persister Generation: Grow culture to stationary phase. Add to fresh media and treat with a high dose of ampicillin for 3+ hours until >99% of cells are killed.
- Cell Immobilization: Wash cells thoroughly to remove antibiotics. Concentrate and immobilize them on an agarose pad or load into a microfluidic device.
- Time-Lapse Imaging: Place the sample on a temperature-controlled stage and acquire images every 30 minutes for 12-24 hours.
- Data Analysis:
- Resuscitation Time (tʀ): Record the time of the first cell division for each persister.
- Doubling Time (δ): Calculate the doubling time of the persister progeny.
- Cell Fate Tracking: Observe for morphological changes (e.g., filamentation, L-form-like growth) and the phenomenon of "persister partitioning," where a damaged mother cell divides to produce one healthy and one defective daughter cell [12].
Signaling Pathways and Experimental Workflows
The Scientist's Toolkit: Research Reagent Solutions
Table 3: Essential Reagents and Materials for Persister Resuscitation Studies
| Item | Function / Application | Specific Examples & Notes |
|---|---|---|
| Fluorescent Reporter Strains | Enabling single-cell tracking and monitoring of cell division via protein dilution. | E. coli with IPTG-inducible mCherry [9]; E. coli constitutively expressing GFP [12]. |
| Microfluidic Devices | For long-term, single-cell time-lapse microscopy under controlled conditions. | Membrane-covered microchamber array (MCMA) [10]; other commercial or custom-made cell-trapping devices. |
| β-Lactam Antibiotics | For persister generation and enrichment, as they lyse growing but not dormant cells. | Ampicillin (common, requires thorough washing) [9] [12]. Piperacillin (less stable, may require less washing). |
| Metabolic Inhibitors | To manipulate cellular energy levels and study the role of metabolism in persistence. | Arsenate (uncouples oxidative phosphorylation) [9]. Carbonyl cyanide m-chlorophenyl hydrazone (CCCP) (protonophore). |
| Efflux Pump Inhibitors | To investigate the role of efflux in the resuscitation process. | Phe-Arg β-naphthylamide (PAβN); Carbonyl cyanide-m-chlorophenylhydrazone (CCCP) [12]. |
| Antioxidants / Catalase | As supplements to resuscitation media to aid recovery of cells under oxidative stress, potentially reviving VBNC cells. | Used in media for VBNC resuscitation studies [9]. |
Troubleshooting Guide: Frequently Asked Questions
FAQ 1: How can I confirm that my bacterial population has entered a persistent state?
A successful persistence model should show a clear subpopulation that survives a high dose of a conventional antibiotic (e.g., bactericidal concentration 10-100x MIC) while remaining genetically identical to the parent strain. Key indicators include:
- Growth Arrest: A significant reduction in growth rate, observable via optical density or colony-forming unit (CFU) counts.
- Metabolic Downshift: Measurable reduction in ATP levels, membrane potential, or anabolic activity [13] [14].
- Tolerance, Not Resistance: Upon re-culturing in fresh media, the surviving cells should regain sensitivity to the same antibiotic [11].
FAQ 2: What are the primary metabolic characteristics of persister cells I should measure?
Your experimental focus should be on central carbon and energy metabolism. The table below summarizes key quantitative findings from metabolic studies on E. coli persisters.
Table 1: Key Metabolic Features of Bacterial Persister Cells
| Metabolic Parameter | Observation in Persister Cells | Experimental Method | Citation |
|---|---|---|---|
| Global Metabolic Rate | Substantially reduced compared to normal cells. | Stable Isotope Labeling (13C-Glucose, 13C-Acetate) with LC-MS/GC-MS | [13] [14] |
| Central Carbon Pathway Flux | Delayed labeling dynamics in glycolysis, PPP, and TCA cycle. | 13C-Glucose tracing | [13] [14] |
| Protein Synthesis Rate | Generalized, uniform slowdown. | Proteinogenic amino acid profiling via 13C labeling | [13] [14] |
| Energy Charge | Lower ATP levels and diminished proton motive force. | ATP assays, membrane potential-sensitive dyes | [15] [16] |
FAQ 3: My resuscitating agent isn't sensitizing persisters to antibiotics. What could be wrong?
This is a common hurdle. Consider the following:
- Verify Metabolic Activation: Ensure your agent truly increases metabolic activity. Use a bioluminescent reporter (e.g., JE2-lux strain) or measure ATP levels to confirm a shift from dormancy before adding antibiotics [15].
- Check Antibiotic Penetration: For intracellular persister models, confirm your antibiotic can penetrate the host cell membrane. Use rifampicin as a positive control, as it penetrates mammalian cells, unlike vancomycin [15].
- Timing and Dosage: The adjuvant may need to be administered before or concurrently with the antibiotic. Perform a time-kill curve assay to optimize the sequence and concentration [15].
FAQ 4: Why are my isolated ribosomes from nutrient-starved cells not binding tRNA/mRNA?
This is an expected characteristic of hibernating ribosomes. Under prolonged glucose depletion, ribosomes enter a protected, inactive state.
- Confirmed Phenomenon: Cryo-EM structures reveal that ribosomes from glucose-depleted yeast are intact but devoid of tRNA and mRNA [17].
- Structural Change: A conformational change in the ribosomal RNA helix H69 can occur, which physically blocks the tRNA binding site in the peptidyl transferase center and disrupts inter-subunit bridge B2a, preventing translation initiation [17].
- Experimental Validation: Perform polysome profiling. Hibernating ribosomes will appear as an accumulation of 80S monosomes and a loss of polysome fractions [17].
Experimental Protocols for Key Assays
Protocol 1: Inducing and Isating Persister Cells via Chemical Treatment
This protocol is adapted for generating E. coli persisters using the protonophore CCCP [14].
- Principle: CCCP dissipates the proton motive force, depleting ATP and inducing a dormant, persister-like state reversibly.
- Materials:
- Bacterial Strain: E. coli BW25113
- Culture Medium: M9 minimal medium supplemented with 2 g/L glucose.
- Inducing Agent: Carbonyl cyanide m-chlorophenyl hydrazone (CCCP) stock solution (e.g., 10 mg/mL in DMSO).
- Centrifuge, microcentrifuge tubes, shaking incubator.
- Procedure:
- Grow an overnight culture of E. coli in M9 medium at 37°C with shaking (200 rpm).
- Sub-culture into fresh M9 medium to an OD600 of 0.05.
- Incubate until the culture reaches mid-exponential phase (OD600 ≈ 0.5).
- Add CCCP to a final concentration of 100 µg/mL.
- Incubate for 15 minutes at 37°C with shaking.
- Collect cells by centrifugation (13,000 rpm, 3 min, room temperature).
- Wash the cell pellet three times with M9 medium (no carbon source) to remove CCCP completely.
- The resulting cell pellet is enriched for persisters and can be used immediately in downstream assays (e.g., metabolic tracing, antibiotic killing) [14].
Protocol 2: High-Throughput Screening for Metabolic Resuscitation Adjuvants
This protocol outlines a cell-based screen to identify host-directed compounds that resuscitate intracellular S. aureus persisters [15].
- Principle: A bioluminescent reporter strain (JE2-lux) whose light output depends on cellular energy (ATP, NAD(P)H) is used to probe intracellular bacterial metabolic activity.
- Materials:
- Bacterial Strain: Bioluminescent MRSA strain JE2-lux.
- Host Cells: Bone marrow-derived macrophages (BMDMs) or relevant mammalian cell line.
- Assay Plates: 384-well plates, tissue culture-treated.
- Detection Instrument: Plate reader capable of measuring bioluminescence and a fluorescence/absorbance-based cell viability dye.
- Compound Library: A collection of drug-like molecules.
- Procedure:
- Infect macrophages with the JE2-lux strain at a suitable MOI (e.g., 10:1).
- Treat with gentamicin (typically 50 µg/mL) for 1-2 hours to kill extracellular bacteria.
- Wash cells to remove gentamicin and dispense infected macrophages into 384-well plates.
- Add compounds from the library to respective wells. Include controls: DMSO (vehicle), rifampicin (metabolic inhibition control).
- Incubate for 4 hours.
- Measure bioluminescence (bacterial metabolic activity) and a cell viability signal (host cytotoxicity) using the plate reader.
- Hit Selection: Primary hits are compounds that increase bioluminescence >1.5-fold over the vehicle control without reducing host cell viability [15].
- Secondary Screening: Confirm hits in a time-kill assay with a relevant antibiotic (e.g., rifampicin, moxifloxacin) to demonstrate enhanced killing of intracellular persisters.
Key Signaling Pathways and Experimental Workflows
Diagram 1: Host-Directed Metabolic Resuscitation Pathway
Diagram 2: Experimental Workflow for Persister Metabolic Analysis
The Scientist's Toolkit: Research Reagent Solutions
Table 2: Essential Reagents for Studying Persister Metabolism and Ribosome Biology
| Reagent / Material | Function / Application | Key Detail / Example |
|---|---|---|
| CCCP (Carbonyl cyanide m-chlorophenyl hydrazone) | Chemical inducer of bacterial persistence by dissipating the proton motive force and depleting ATP. | Used at 100 µg/mL for 15 min to induce E. coli persisters reversibly [14]. |
| Stable Isotope Tracers (13C-Glucose, 13C-Acetate) | To measure metabolic flux in central carbon pathways (glycolysis, TCA cycle) in persister cells. | Tracer incorporation into metabolic intermediates and proteinogenic amino acids is measured via LC-MS/GC-MS [13] [14]. |
| Bioluminescent Reporter Strain (e.g., JE2-lux) | Real-time, non-invasive probing of intracellular bacterial metabolic activity and energy status. | Lux activity requires ATP and reducing equivalents (NAD(P)H, FMNH2), coupling light output to metabolism [15]. |
| KL1 (Host-Directed Compound) | A lead compound that resuscitates intracellular persisters by modulating the host immune response. | Suppresses host macrophage ROS/RNS production, alleviating a key inducer of bacterial metabolic shutdown [15]. |
| Ribosome Hibernation Analysis | Polysome profiling to assess the translational status of ribosomes (active polysomes vs. inactive monosomes). | Accumulation of 80S monosomes and loss of polysomes indicate translation shutdown and ribosome hibernation [17]. |
| Cryo-Electron Microscopy (Cryo-EM) | High-resolution structural analysis of ribosomal conformational states during hibernation. | Can reveal changes like H69 rRNA rotation that prevent tRNA binding and disrupt translation initiation [17]. |
Troubleshooting Guides and FAQs
FAQ 1: Why is my persister cell enrichment not working, and how can I improve it?
Issue: Low yield of persister cells after enrichment protocols.
Answer: A low yield of persisters is often due to incomplete metabolic arrest or unintended resuscitation during handling. The key is to ensure full dormancy and avoid introducing nutrients.
- Confirm Stressor Efficacy: Verify that the concentration of your inducer (e.g., rifampicin, CCCP) is sufficient and the treatment duration is appropriate. For E. coli and P. aeruginosa, pretreatment with rifampicin (inhibits transcription), tetracycline (inhibits translation), or CCCP (uncouples oxidative phosphorylation) can convert nearly all exponential-phase cells into persisters, increasing persistence by up to 10,000-fold [18]. Always include a positive control.
- Minimize Resuscitation During Washing: Persister cells can resuscitate immediately upon exposure to fresh nutrients [18]. During the washing steps after antibiotic treatment, use a minimal buffer or spent medium instead of fresh, nutrient-rich medium to prevent accidental reactivation.
- Validate Dormancy: Use a metabolic dye like Redox Sensor Green to confirm low metabolic activity in the enriched population via flow cytometry [18].
FAQ 2: How can I distinguish between (p)ppGpp-mediated persistence and Toxin-Antitoxin (TA) system-mediated persistence?
Issue: Uncertainty in identifying the primary molecular pathway responsible for persister formation in my experimental system.
Answer: While historically linked, current evidence suggests (p)ppGpp plays a more central and general role, while the involvement of specific TA modules under physiological conditions is less clear.
- Genetic Knockouts: Generate deletion mutants for key synthetases. A ΔrelA ΔspoT double mutant in E. coli is completely devoid of (p)ppGpp and should show a sharp decrease in persister formation upon amino acid starvation [19] [20]. In contrast, deletion of up to 10 or 12 type II TA systems in E. coli and Salmonella enterica has been shown to have no significant effect on persistence [18].
- Single-Cell Reporter Assays: Use fluorescent reporters to correlate persistence events with molecular activity. An RpoS-mCherry fusion can serve as a proxy for (p)ppGpp activity [19]. However, note that one study found no direct correlation between single-cell (p)ppGpp levels and antibiotic tolerance, suggesting the transcriptional response may be more critical than the alarmone level itself [19].
- Key Differentiator: The model that polyphosphate activates Lon protease to degrade antitoxins in a (p)ppGpp-dependent manner has been retracted and disputed by subsequent studies [18]. Therefore, a lack of persistence in a (p)ppGpp-deficient mutant, but persistence in a TA module deletion mutant, strongly implicates the stringent response.
FAQ 3: My bacterial cultures are not resuscitating consistently. What factors can affect Rpf efficiency?
Issue: Inconsistent or low resuscitation rates of dormant cells using Recombinant Rpf proteins.
Answer: Rpf efficacy is highly dependent on the physiological state of the dormant cells and the enzymatic activity of the Rpf protein.
- Confirm Rpf Activity and Concentration: Rpf is active at picomolar concentrations [21]. Use a positive control, such as dormant Micrococcus luteus, to verify the activity of your Rpf stock. Ensure your Rpf is properly stored and not degraded.
- Match Rpf to the Bacterial Species: The structure of peptidoglycan varies between Gram-positive and Gram-negative species, affecting which bonds Rpf can cleave [21]. The Rpf from M. luteus is most effective against other high G+C Gram-positive bacteria like mycobacteria. For other species, you may need an Rpf analogue (e.g., YeaZ in some Gram-negative bacteria) [21].
- Consider the Dormancy State: The "depth" of dormancy affects resuscitation. Cells in a deeper dormant state (e.g., VBNC) may require a longer exposure to Rpf or a combination of multiple resuscitation factors [11] [21]. Ensure other resuscitation conditions (temperature, minimal medium) are optimal.
Table 1: Key Molecular Initiators in Bacterial Persistence and Resuscitation
| Initiator | Full Name | Primary Role | Key Experimental Findings |
|---|---|---|---|
| (p)ppGpp | Guanosine pentaphosphate / tetraphosphate ("Magic Spot") | Central alarmone of the Stringent Response; induces a multidrug-tolerant, dormant state [18] [20]. | - A 16-fold increase in ppGpp levels upon valyl-tRNA synthetase inhibition led to a >1000-fold increase in persister formation [19]. - (p)ppGpp accumulation reprograms transcription, inhibits DNA primase and GTPases, and reduces ribosome synthesis [18] [20]. |
| Rpf | Resuscitation-Promoting Factor | Bacterial cytokine with peptidoglycan hydrolase activity; reactivates cells from dormancy [22] [21]. | - Picomolar concentrations of Rpf can increase the viable count of dormant M. luteus by >100-fold [21]. - In M. tuberculosis, the five Rpf genes (rpfA-E) are differentially expressed under various stresses (acid, hypoxia, nutrient starvation) to facilitate reactivation [22]. |
| cAMP | Cyclic Adenosine Monophosphate | Secondary messenger; core regulator of catabolite repression and some stress responses. | Information from the provided search results was insufficient to populate this cell with specific findings related to persistence. Further research is required. |
Table 2: Common Methods for Persister Enrichment and Their Validation
| Method | Mechanism of Action | Reported Increase in Persistence | Key Validation Metrics |
|---|---|---|---|
| Rifampicin/Tetracycline/CCCP Pre-treatment | Stops transcription, translation, or ATP production, forcing cells into a dormant state [18]. | Up to 10,000-fold in E. coli and P. aeruginosa [18]. | Multi-drug tolerance, dormancy via metabolic dyes, immediate resuscitation with nutrients, no change in MIC [18]. |
| Amino Acid Starvation (e.g., valSts) | Induces (p)ppGpp synthesis via RelA in response to uncharged tRNA [19]. | 3 to 4 orders of magnitude in E. coli [19]. | RelA-dependence, stochastic persister formation, RpoS reporter induction [19]. |
| Toxin Overexpression (e.g., MqsR) | Induces growth arrest by cleaving mRNA or other essential cellular targets [18]. | Up to 14,000-fold for E. coli [18]. | Dependence on toxin catalytic activity, growth arrest, and antibiotic tolerance. |
Experimental Protocols
Protocol 1: Inducing and Quantifying (p)ppGpp-Dependent Persisters via Amino Acid Starvation
This protocol uses a temperature-sensitive valyl-tRNA synthetase mutant (valSts) to trigger (p)ppGpp accumulation and persister formation in a controlled manner [19].
Key Materials:
- Bacterial Strain: E. coli MG1655 with valSts mutation (e.g., strain SEM3147).
- Antibiotics: Ampicillin sodium salt (or other cell-wall active antibiotic for killing).
- Equipment: Water bath or incubator for precise temperature control, plate reader or colony counter.
Methodology:
- Growth and Induction: Grow the valSts strain overnight at a fully permissive temperature (e.g., 30°C). Dilute the culture in fresh, pre-warmed medium and grow to mid-exponential phase at 30°C. Shift the culture to a semi-permissive temperature (e.g., 36.6°C) to partially inactivate ValS and induce amino acid starvation. Incubate for 60-90 minutes.
- Antibiotic Challenge: Take a sample of the induced culture and challenge it with a high concentration of ampicillin (e.g., 100 µg/mL, >10x MIC) for a defined period (e.g., 3-5 hours) to kill non-persister cells.
- Quantification of Persisters: After antibiotic treatment, wash the cells 2-3 times in sterile PBS or minimal buffer to remove the antibiotic. Serially dilute and spot the cells onto LB agar plates. Incubate the plates at the permissive temperature (30°C) for 24-48 hours to allow surviving persisters to resuscitate and form colonies. Count the Colony Forming Units (CFU) to determine the number of persisters.
- Control Strains: Always include control strains in parallel: the wild-type MG1655 and a ΔrelAvalSts double mutant. The latter should show a significant reduction in persister formation, confirming RelA/(p)ppGpp dependence [19].
Protocol 2: Assessing Persister Cell Recovery Kinetics
This protocol outlines steps to study the resuscitation of persister cells after antibiotic removal at the single-cell level [23].
Key Materials:
- Bacterial Culture: A purified population of persister cells.
- Equipment: Spectrophotometer for bulk growth measurement, Flow cytometer with capability for metabolic staining (e.g., Redox Sensor Green).
- Reagents: Appropriate culture medium, metabolic dyes.
Methodology:
- Sample Preparation: Obtain persister cells using a time-kill assay with a high concentration of a bactericidal antibiotic. Ensure >99.9% killing of the initial population. Thoroughly wash the cells to remove the antibiotic.
- Bulk Recovery Kinetics: Resuspend the persister cells in fresh, pre-warmed medium. Immediately transfer the suspension to a cuvette and place it in a spectrophotometer. Monitor the optical density (OD600) continuously with shaking. The lag time before resumption of growth is a key parameter of persister recovery.
- Single-Cell Physiological States: In parallel, take samples at regular time points (e.g., every 30-60 minutes) during the recovery phase. Stain these samples with a metabolic dye like Redox Sensor Green and analyze them via flow cytometry. This allows you to track the heterogeneity in metabolic activity as the population transitions from dormancy to active growth [23].
Signaling Pathway and Experimental Workflow Diagrams
Diagram 1: Pathway from Stress to Persistence and Resuscitation
Diagram 2: Experimental Workflow for Persister Analysis
The Scientist's Toolkit: Key Research Reagents
Table 3: Essential Reagents for Studying Molecular Initiators of Persistence
| Reagent / Tool | Function / Target | Example Use Case | Key Considerations |
|---|---|---|---|
| valSts E. coli Strain | Temperature-sensitive valyl-tRNA synthetase; induces (p)ppGpp synthesis at restrictive temperatures [19]. | Controlled, RelA-dependent induction of persister cells via amino acid starvation. | Requires precise temperature control. A ΔrelAvalSts double mutant is a critical control. |
| RpoS-mCherry Reporter | Fluorescent reporter for (p)ppGpp activity and the general stress response [19]. | Monitoring stringent response activation at the single-cell level in relation to persistence events. | Correlation with (p)ppGpp levels may not be perfect; it reports on the downstream transcriptional response. |
| Recombinant Rpf Protein | Peptidoglycan hydrolase that cleaves bonds in the cell wall to stimulate resuscitation [22] [21]. | Reactivating dormant (including VBNC) cells in culture to study resuscitation mechanisms. | Activity is species-specific due to peptidoglycan structural variation. Use picomolar concentrations. |
| QUEEN-7µ ATP Sensor | Genetically encoded fluorescent biosensor for intracellular ATP concentration [19]. | Correlating ATP levels with persister formation and resuscitation at single-cell resolution. | Allows monitoring of metabolic state without disrupting cells. |
| Metabolic Dyes (e.g., Redox Sensor Green) | Fluorescent dyes that report on metabolic (redox) activity. | Differentiating and isolating dormant (low metabolism) cells from active cells via flow cytometry [18]. | Useful for validating enrichment protocols and analyzing population heterogeneity during recovery. |
| Membrane-Active Compounds (e.g., CD437, CD1530) | Disrupts membrane integrity and proton motive force (PMF) [24]. | Used in combination with conventional antibiotics to sensitize persister cells by enhancing drug uptake. | Shows synergistic killing when combined with aminoglycosides against MRSA persisters [24]. |
Advanced Workflows: Single-Cell and Omics Techniques for Monitoring Resuscitation Dynamics
Frequently Asked Questions (FAQs)
FAQ 1: What is the key advantage of using flow cytometry over CFU counting for studying bacterial persister resuscitation?
Flow cytometry provides single-cell resolution, allowing you to detect heterogeneous subpopulations and transient physiological states that are invisible to conventional Colony Forming Unit (CFU) counts. While CFU counts only detect cells capable of replication on a plate, flow cytometry can identify viable but non-culturable (VBNC) cells and dormant subpopulations through metabolic markers and membrane integrity assays. This high-resolution is critical, as studies have shown that cells can regain metabolic activity and resuscitate even when conventional culture methods indicate complete inactivation [25] [26].
FAQ 2: How can I distinguish between true resuscitation and non-specific staining during a persister recovery time-course?
To reliably distinguish resuscitation, employ a multi-parameter staining panel. Combine a membrane integrity dye (like PI) with a marker for metabolic activity (like CFDA or a redox-sensitive dye). A resuscitating cell will transition from PI-positive/CFDA-low to PI-negative/CFDA-high. Always include controls: an unstained sample to set autofluorescence baselines, a killed population (e.g., disinfectant-treated) as a dead cell control, and a healthy, growing culture as a live cell control. The use of a metabolic activity dye was key in a study on Mycobacterium bovis BCG to confirm the sublethal effect of a disinfectant and subsequent resuscitation [26].
FAQ 3: My flow cytometry data shows a high background in the negative cell populations. What could be the cause and how can I resolve it?
High background in negative populations is often caused by non-specific antibody binding or the presence of dead cells. You can address this by:
- Blocking Fc Receptors: Use Bovine Serum Albumin, Fc receptor blocking reagents, or normal serum from the same host as your antibodies prior to staining [27].
- Gating Out Dead Cells: Use a viability dye such as Propidium Iodide (PI) or 7-AAD to identify and gate out dead cells during live cell surface staining. For fixed cells, use fixable viability dyes [27].
- Optimizing Washes: Perform additional wash steps between antibody incubations to remove unbound antibody [27].
FAQ 4: What are the critical steps in sample preparation to ensure accurate tracking of persister cell recovery?
The key is to preserve the physiological state of the cells at the moment of sampling.
- Gentle Handling: Avoid bubbles, vigorous vortexing, and excessive centrifugation to prevent mechanical stress and cell damage [28].
- Rapid Fixation (if required): If you need to pause an experiment for batch analysis, add fixative immediately after sampling. Cross-linking fixatives like 4% formaldehyde are recommended to inhibit enzymatic activity and preserve cell structures [27].
- Consistent Timing: For time-course experiments, process each sample at the same interval after collection to ensure comparability.
Troubleshooting Guides
Problem: Weak or No Fluorescence Signal
| Possible Cause | Recommendation |
|---|---|
| Inadequate fixation/permeabilization | For intracellular targets, ensure you use the appropriate fixation and permeabilization method. For cytosolic antigens, mild detergents like saponin may suffice, while nuclear antigens may require harsher detergents like Triton X-100 [27] [28]. |
| Suboptimal antibody concentration | Titrate your antibodies to determine the optimal concentration. Over-dilution can lead to weak signals, while over-concentration can cause high background [27]. |
| Instrument laser/PMT settings | Verify that the flow cytometer's laser wavelength and photomultiplier tube (PMT) settings are correctly configured for the fluorochromes you are using [27]. |
| Low expression of the target | Pair a low-density target with the brightest possible fluorochrome (e.g., PE) to maximize detection sensitivity [27]. |
Problem: Unclear Separation Between Live, Dead, and Resuscitating Populations
| Possible Cause | Recommendation |
|---|---|
| Reliance on a single dye | Use a multi-parametric viability stain. The LIVE/DEAD BacLight bacterial viability kit, for example, uses SYTO9 and PI to differentiate cells with intact membranes (green), damaged membranes (red), and those with intermediate states [25]. |
| Incorrect gating strategy | Use a forward scatter (FSC) vs. side scatter (SSC) plot to gate on your primary bacterial population. Then, use fluorescence plots from single-stained controls to set the boundaries for positive and negative populations accurately. |
| Cell aggregation | Pass your cell suspension through a narrow-gauge needle or filter it through a cell strainer before running it on the cytometer to ensure a single-cell suspension and avoid doublet artifacts. |
The Scientist's Toolkit: Essential Research Reagents
The following table details key reagents used in flow cytometry protocols for studying bacterial persistence and resuscitation.
| Item | Function/Application in Persister Research |
|---|---|
| Propidium Iodide (PI) | A membrane-impermeant DNA dye that only enters cells with compromised membranes, labeling dead cells. It is a standard for assessing membrane integrity [25] [27]. |
| SYTO9 | A cell-permeant green fluorescent nucleic acid stain that labels all cells in a population. Used in combination with PI for viability assessment [25]. |
| Fixable Viability Dyes | Amine-reactive dyes that covalently bind to proteins in dead cells before fixation. They allow for the exclusion of dead cells during subsequent intracellular staining procedures [27] [28]. |
| Fc Receptor Blocking Buffer | Used to block Fc receptors on immune cells (e.g., in PBMCs co-cultured with bacteria) to prevent non-specific antibody binding and reduce background signal [27]. |
| Paraformaldehyde (PFA) | A cross-linking fixative used to preserve cell structure and immobilize intracellular components at a specific time point, crucial for time-course experiments [27] [28]. |
| Permeabilization Detergents | Agents like Saponin (mild) or Triton X-100 (harsh) are used to permeabilize cell membranes after fixation, allowing antibodies to access intracellular targets for staining [27] [28]. |
Experimental Workflow & Data Analysis
This protocol is adapted from methodologies used to assess persister recovery and is ideal for tracking resuscitation in real-time [23].
- Persister Generation: Treat a mid-logarithmic phase bacterial culture with a high concentration of a bactericidal antibiotic (e.g., a fluoroquinolone or aminoglycoside) for a defined period (e.g., 3-5 hours).
- Wash-Out: Pellet the cells by centrifugation and wash twice with fresh, pre-warmed medium to remove the antibiotic thoroughly.
- Resuscitation and Staining: Resuspend the cell pellet in fresh medium to initiate resuscitation. At regular intervals (e.g., 0, 30, 60, 120, 240 minutes), withdraw aliquots and immediately incubate them with your chosen fluorescent dye panel (e.g., SYTO9 and PI).
- Flow Cytometry Analysis: Analyze the stained samples on a flow cytometer. For each time point, collect at least 10,000 events. Use FSC vs. SSC to gate on the bacterial population.
- Data Interpretation: Plot the fluorescence data over time. A successful resuscitation will show a population shift from a primarily PI-positive state (dead) to a SYTO9-positive/PI-negative state (live) as cells repair their membranes and resume activity.
Visualizing the Experimental Workflow
The following diagram illustrates the logical flow of a typical experiment for tracking persister cell resuscitation.
This diagram maps the physiological transitions of a bacterial cell during the resuscitation process, as determined by flow cytometry parameters.
Frequently Asked Questions (FAQs)
Q1: Our 13C-labeling data from persister cell cultures shows very low enrichment, making flux estimation unreliable. What could be the cause? Low isotopic enrichment is a common challenge when working with dormant cells. Potential causes and solutions include:
- Low Metabolic Activity: Persister cells exhibit drastically reduced metabolic rates. Ensure you are using a sufficiently high density of persister cells (e.g., OD600 of 5 as used in successful protocols) to obtain measurable signals [14].
- Insufficient Labeling Time: The metabolic slowdown means label incorporation is delayed. Extend the labeling time course and include early time points (e.g., 20 seconds, 5 minutes) to capture slow labeling dynamics, not just endpoint measurements [14].
- Tracer Choice: If using acetate as a carbon source, be aware that persister cells show a more substantial metabolic shutdown compared to glucose. Substrate inhibition and high ATP demands for acetate activation can further reduce metabolic activity. Using 13C-glucose may yield better results [14].
Q2: How can we differentiate metabolic fluxes between different species in a mixed microbial community? Traditional 13C-MFA using amino acid labeling patterns cannot distinguish between species in a community. A promising solution is a peptide-based 13C-MFA method. This approach leverages high-throughput proteomics to:
- Identify the origin of a peptide, linking it to a specific species in the community.
- Use the peptide's labeling pattern to infer intracellular fluxes for that specific organism, as the peptide labeling is derived from its constituent amino acids [29]. This method allows for the simultaneous quantification of species-specific metabolic fluxes and metabolite exchange within a community.
Q3: What software tools are available for 13C Metabolic Flux Analysis, and which is best for beginners? Several software tools are available, ranging from those requiring expert knowledge to more user-friendly options.
| Software Tool | Key Features | Best For | Citation |
|---|---|---|---|
| INCA / Metran | User-friendly; preferred for quantitative flux maps in mammalian and microbial cells. | Cancer biologists and researchers without extensive coding/math backgrounds. | [30] |
| BiGGR | An R/Bioconductor package; integrates with gene expression data and metabolic databases. | R users who want to combine flux analysis with other 'omics' data. | [31] [32] |
| WUflux | An open-source solution for steady-state flux calculations. | Researchers needing a free, dedicated platform for flux calculations. | [33] |
Q4: The fluxes in our persister cell cultures do not seem to be at a metabolic steady state. Can we still perform 13C-MFA? Yes. Standard 13C-MFA often assumes both metabolic and isotopic steady state. However, persister cell resuscitation is a dynamic process. In such cases, Isotopically Non-Stationary 13C-MFA (INST-MFA) is the appropriate method. INST-MFA does not require the system to be at an isotopic steady state and uses early time-point labeling data to estimate fluxes, making it ideal for studying dynamic processes like resuscitation [34].
Troubleshooting Guides
Issue: Inconsistent or Implausible Flux Results
| Problem | Potential Cause | Solution |
|---|---|---|
| Poor Flux Resolution | Limited labeling data for upper metabolism (PPP, glycolysis). | Incorporate labeling measurements of glycogen and RNA. The glucose and ribose moieties provide direct information on G6P and R5P pools, greatly improving flux observability in pentose phosphate and glycolytic pathways [35]. |
| High Uncertainty in Flux Estimates | The flux solution is underdetermined; many flux distributions fit the data equally well. | Use ensemble modeling (e.g., via BiGGR) to sample the space of possible flux solutions. This quantifies uncertainty and provides confidence intervals for each estimated flux [32]. |
| Violation of Steady-State Assumption | The cell culture is not in a metabolic steady state during the labeling experiment. | * Ensure constant growth and nutrient conditions before starting the tracer experiment.* If studying a dynamic process like resuscitation, switch to INST-MFA [34]. |
Issue: Challenges in Sample Preparation and Measurement
| Problem | Potential Cause | Solution |
|---|---|---|
| Low Abundance of Metabolites | Rapid quenching and efficient extraction are critical, especially for low-concentration intracellular metabolites. | * Rapid Quenching: Use a cold methanol-water solution and liquid nitrogen to stop metabolic activity within seconds [14].* Efficient Extraction: Use an 80:20 methanol-water extraction solution at -20°C [14]. |
| Difficulty Measuring PPP Intermediates | Low concentrations of metabolites like erythrose-4-phosphate (E4P) make direct measurement hard. | Rely on proteinogenic amino acids as proxies. For example, phenylalanine labeling provides information on E4P and PEP pools. For mammalian cells that don't synthesize phenylalanine, use labeling of lower glycolytic intermediates like 3PG [35] [30]. |
Experimental Protocols
Detailed Methodology: 13C-Labeling of Bacterial Persister Cells
This protocol is adapted from studies investigating the metabolic state of E. coli persister cells induced by CCCP [14].
1. Persister Cell Induction and Preparation
- Culture: Grow E. coli BW25113 in M9 minimal medium with 2 g/L glucose.
- Induction: At mid-exponential phase (OD600 ~0.5), expose cells to 100 µg/mL of CCCP for 15 minutes at 37°C with shaking.
- Washing: Collect cells by centrifugation and wash three times with M9 medium without a carbon source to remove CCCP and residual metabolites.
2. Tracer Experiment
- Resuspension: Concentrate control and persister cells to a high density (OD600 of 5) in 10 mL of M9 medium.
- Labeling: Initiate the experiment by adding 2 g/L of a 13C-labeled tracer (e.g., 1,2-13C2 glucose or 2-13C sodium acetate).
- Time Course: Incubate at 37°C and collect samples at specific timepoints (e.g., 0, 20 s, 5 min, 30 min, 2 h) to capture labeling dynamics.
- Quenching: For each timepoint, immediately cool samples in liquid nitrogen to stop metabolic activity.
3. Sample Processing for LC-MS/MS Analysis
- Metabolite Extraction:
- Lyophilize the quenched cell pellet.
- Add 0.5 mL of 80:20 methanol-water extraction solution and incubate at -20°C for 1 hour.
- Centrifuge at 10,000 × g for 10 min at 0°C.
- Filter the supernatant through a 0.2 µm filter for LC-MS analysis of free metabolites.
- Proteinogenic Amino Acid Analysis:
- Hydrolyze the remaining cell pellet with 6 N HCl at 100°C for 18 hours.
- Derivatize the hydrolyzed amino acids using the TBDMS method for GC-MS analysis [14].
The Scientist's Toolkit: Research Reagent Solutions
Essential materials and software for conducting 13C-MFA in persister cell studies.
| Category | Item / Reagent | Function / Explanation |
|---|---|---|
| Chemical Inducers | Carbonyl cyanide m-chlorophenyl hydrazone (CCCP) | A protonophore used to induce a reversible state of persistence by disrupting the membrane potential and ATP synthesis, without permanent damage [14]. |
| Isotopic Tracers | 1,2-13C2 Glucose; 2-13C Sodium Acetate | Essential substrates for tracing carbon fate. Glucose is a core substrate; acetate can reveal distinct metabolic shutdowns in persisters [14]. |
| Mass Spectrometry | LC-MS (Q-Exactive system) & GC-MS | Used to measure the 13C-labeling patterns of free metabolic intermediates (via LC-MS) and proteinogenic amino acids (via GC-MS after derivatization) [14]. |
| Analytical Columns | Agilent InfinityLab Poroshell 120 HILIC-Z | A hydrophilic interaction liquid chromatography (HILIC) column effective for separating polar metabolites for LC-MS analysis [14]. |
| Flux Analysis Software | INCA, Metran, WUflux, BiGGR | Software tools that use labeling data and external rates to compute quantitative intracellular flux maps [34] [33] [30]. |
Data Inputs and External Rate Calculations for 13C-MFA
Successful flux analysis requires precise measurement of external rates, which constrain the possible intracellular flux distributions [30].
| Parameter | Measurement Method | Calculation Formula | Application Notes |
|---|---|---|---|
| Growth Rate (μ) | Tracking cell number (Nx) over time. | μ = (ln Nx,t2 - ln Nx,t1) / ΔtDoubling time: t_d = ln(2) / μ | For persister resuscitation, monitor the lag phase and the onset of growth. |
| Nutrient Uptake / Product Secretion Rates (r_i) | Measuring metabolite concentration (Ci) in the media over time. | For growing cells:r_i = 1000 · μ · V · ΔCi / ΔNxUnits: nmol/10^6 cells/h | Correct glutamine uptake rates for spontaneous degradation in the media [30]. |
Data Analysis Pathway for 13C-MFA
Transcriptomic and Proteomic Profiling of Awakening Persisters
Bacterial persister cells represent a transient, non-growing (or slow-growing) subpopulation within an isogenic culture that exhibits remarkable tolerance to high concentrations of bactericidal antibiotics. These cells are not genetically resistant but rather exist in a phenotypic state of dormancy that enables survival during antibiotic exposure. Upon removal of the antibiotic stress, a subpopulation of these persister cells can resuscitate and resume normal growth, leading to relapse of infections. This resuscitation process represents a critical phase in the persister life cycle and understanding the molecular mechanisms underlying awakening is fundamental to developing novel therapeutic strategies against chronic and recurrent bacterial infections. The following technical support guide addresses key methodological considerations and frequent challenges encountered when investigating the transcriptomic and proteomic profiles of persister cells during this crucial awakening phase, providing a structured troubleshooting framework for researchers in the field.
Troubleshooting Guide: Common Experimental Challenges
Table 1: Troubleshooting Guide for Persister Resuscitation Studies
| Problem Area | Specific Challenge | Potential Causes | Recommended Solutions |
|---|---|---|---|
| Persister Isolation | Low persister yields after antibiotic treatment | Incorrect antibiotic concentration or exposure time; Insufficient initial population heterogeneity | - Determine Minimum Inhibitory Concentration (MIC) first; Use 10-100x MIC [36].- Use stationary-phase cultures or stress pre-treatment (e.g., CSP pheromone in S. mutans) to induce persistence [36]. |
| Contamination with viable non-persisters | Incomplete killing of non-persister cells | - Include viability staining (e.g., propidium iodide) with colony counts [6].- Validate with time-kill curves extending beyond 24 hours [11]. | |
| Transcriptomic Profiling | Low RNA yield/quality from persisters | Extremely low transcriptional activity in deep persisters; RNA degradation | - Use single-cell RNA-seq techniques (e.g., PETRI-seq) designed for low-biomass samples [37].- Implement rigorous RNA integrity assessment (RIN > 7.0) [36]. |
| High background noise in data | Residual ribosomal RNA dominates limited transcript pool | - Employ Cas9-driven ribosomal RNA depletion in protocol [37].- Apply downsampling bioinformatic normalization to equalize mRNA counts per cell [37]. | |
| Proteomic Analysis | Insufficient protein material for LC-MS/MS | Low protein synthesis in dormant persisters | - Use pulsed-SILAC labeling to identify de novo protein synthesis during recovery [38] [39].- Scale up persister cell isolation volumes to milligram quantities. |
| Resuscitation Triggering | Inconsistent awakening kinetics between replicates | Stochastic nature of resuscitation; Inadequate trigger consistency | - Standardize resuscitation media (e.g., using L-glutamic acid for V. splendidus) [40] [41].- Monitor single-cell resuscitation dynamically using microscopy [40]. |
Frequently Asked Questions (FAQs)
Q1: What defines a "persister cell" in the context of resuscitation studies, and how does it differ from antibiotic-resistant cells or VBNC cells?
Persisters are genetically drug-susceptible phenotypic variants that survive antibiotic exposure by entering a transient, non-growing state. Unlike resistant cells, persisters do not have a higher Minimum Inhibitory Concentration (MIC) and the phenotype is not heritable. Upon antibiotic removal, a subpopulation can resuscitate. In contrast, Viable But Non-Culturable (VBNC) cells typically require specific, complex resuscitation signals and may represent a deeper state of dormancy, though the boundaries between these states can be fluid [11] [42].
Q2: My transcriptomic data shows persisters have very low overall mRNA content. How can I be sure that the transcriptional signals I detect are biologically relevant and not just noise?
This low mRNA content is a genuine characteristic of the dormant state. To ensure robustness:
- Technical Replication: Perform multiple independent persister isolations and sequencing runs to distinguish consistent signals from stochastic noise [37].
- Spike-in Controls: Use external RNA controls to normalize for technical variation.
- Validation: Confirm key findings via orthogonal methods, such as transcriptional fusions to validate promoter activity or qRT-PCR on selected genes [37].
- Statistical Rigor: Apply stringent false discovery rate corrections in differential expression analysis.
Q3: What are the key proteomic changes I should focus on when studying the initial hours of persister resuscitation?
Proteomic studies indicate that the early resuscitation phase involves a coordinated upregulation of specific functional protein categories. Key changes to monitor include:
- Metabolic Reactivation: Proteins involved in central carbon metabolism (e.g., amino acid metabolism like arginine, L-glutamic acid utilization) [40] [41].
- Cellular Repair: Proteins for cell envelope and peptidoglycan biosynthesis [40] [41].
- Stress Detoxification: Antioxidant proteins like alkyl hydroperoxide reductase (AhpF) [38] [39].
- Ribosome Assembly: While ribosomes may be downregulated initially, factors for ribosome preservation and resuscitation are critical [40] [6].
Q4: Are persister cells truly metabolically dormant, or is there activity I should account for in my experimental design?
Emerging evidence challenges the traditional view of complete metabolic inactivity. While persisters are non-growing, they can maintain a basal level of metabolism and can even actively respond to their environment. Studies show that persister cells can:
- Undergo new RNA synthesis during antibiotic exposure, indicating active transcription [42].
- Synthesize specific proteins in response to stress, such as those involved in protection against ampicillin-induced damage [38]. This residual metabolic activity means researchers should consider the potential for active gene regulation during the persistence phase itself, not just during resuscitation.
Detailed Experimental Protocols for Transcriptomic and Proteomic Profiling
This protocol is designed for isolating stress-induced persisters for subsequent transcriptomic analysis, using the CSP pheromone system in S. mutans as a model for triggered persistence.
Culture Preparation:
- Grow the bacterial strain (e.g., S. mutans UA159) overnight in an appropriate rich medium (e.g., THYE).
- Dilute the overnight culture 1:100 in 200 mL of fresh pre-warmed medium.
- Induce persistence by adding the trigger (e.g., 50 ng/mL CSP pheromone). Incubate for 2 hours at 37°C with 5% CO₂.
Antibiotic Selection:
- Treat the culture with a lethal dose of a bactericidal antibiotic (e.g., 20 µg/mL ofloxacin, 10x MIC) for 22 hours to kill all non-persister cells.
- Critical: Determine the MIC for your strain and antibiotic beforehand. Use concentrations significantly above the MIC (10-100x).
Persister Collection and Washing:
- Centrifuge the antibiotic-treated culture to pellet cells.
- Wash the pellet thoroughly with sterile phosphate-buffered saline (PBS) at least twice to completely remove the antibiotic.
- Resuspend the final pellet (containing the persister population) in a suitable buffer for RNA extraction.
RNA Extraction and Quality Control:
- Use a commercial kit designed for bacterial RNA extraction (e.g., RiboPure-Bacteria Kit).
- Treat the extracted RNA with DNase (e.g., RQ1 DNase) to remove genomic DNA contamination.
- Assess RNA quality using an instrument such as an Agilent Bioanalyzer. Proceed only with samples having an RNA Integrity Number (RIN) of 7.0 or higher.
Library Preparation and Sequencing:
- Use a ribosomal RNA depletion kit (e.g., Illumina Stranded Total RNA Prep Ligation with Ribo-Zero Plus) to enrich for mRNA.
- Prepare sequencing libraries and sequence on an appropriate platform (e.g., Illumina MiSeq for 75 bp paired-end reads).
This protocol outlines the steps for a label-free quantitative proteomics approach to characterize the proteome of persister cells during the recovery phase.
Generation and Isolation of Persisters:
- Generate a high-persister strain or use wild-type strains under persistence-inducing conditions (e.g., stationary phase, toxin overexpression).
- Treat the culture with a high concentration of antibiotic (e.g., ampicillin) for a defined period to eliminate growing cells.
- Wash the surviving persisters with PBS to remove the antibiotic.
Initiation of Resuscitation and Sample Collection:
- Resuspend the persister pellet in fresh, pre-warmed recovery medium.
- Incubate under optimal growth conditions to allow resuscitation.
- Collect samples at critical time points during recovery (e.g., T=0h, T=1h, T=3h) by centrifugation. Snap-freeze cell pellets in liquid nitrogen and store at -80°C.
Protein Extraction and Digestion:
- Lyse the frozen cell pellets using a strong denaturant (e.g., urea or SDS) in combination with physical disruption (e.g., bead beating or sonication).
- Reduce and alkylate cysteine residues.
- Digest the protein extract into peptides using a sequence-grade protease, typically trypsin.
LC-MS/MS Analysis and Data Processing:
- Analyze the digested peptides by Liquid Chromatography tandem Mass Spectrometry (LC-MS/MS).
- Acquire data in a data-dependent acquisition (DDA) mode.
- Identify and quantify proteins by searching the MS/MS spectra against a protein database for the organism using specialized software (e.g., MaxQuant).
- Perform statistical analysis to identify proteins with significantly altered abundance across the different recovery time points.
The following diagrams illustrate the core experimental workflow for profiling awakening persisters and the key molecular pathways active during their resuscitation.
Diagram 1: Experimental workflow for profiling awakening persisters.
Diagram 2: Key pathways activated during persister resuscitation.
The Scientist's Toolkit: Key Research Reagents & Materials
Table 2: Essential Research Reagents for Persister Resuscitation Studies
| Reagent / Material | Specific Example(s) | Function / Application in Research |
|---|---|---|
| Induction Compounds | CSP Pheromone (for S. mutans) [36], L-Glutamic Acid (for V. splendidus) [40] [41] | Used to trigger or induce the formation of persister cells in a population prior to antibiotic selection. |
| Bactericidal Antibiotics | Ofloxacin [36], Ampicillin [37] [38], Ciprofloxacin [37] | Applied at high concentrations (10-100x MIC) to selectively kill non-persister cells, thereby isolating the tolerant persister subpopulation. |
| RNA Stabilization & Extraction Kits | RNAwiz, RiboPure-Bacteria Purification Kit [36] | Critical for preserving the often low-abundance and labile RNA transcriptome of persister cells immediately upon lysis. |
| rRNA Depletion Kits | Illumina Stranded Total RNA Prep with Ribo-Zero Plus [36] | Used during RNA-seq library preparation to remove abundant ribosomal RNA, thereby enriching for mRNA and improving sequencing depth of the transcriptome. |
| Proteomic Buffers & Enzymes | Urea/SDS Lysis Buffers, Trypsin [38] [39] | For the efficient extraction, denaturation, and digestion of proteins from persister cells into peptides suitable for LC-MS/MS analysis. |
| Stable Isotope Labels (SILAC) | Heavy Isotope-labeled Amino Acids (Lysine, Arginine) [38] [39] | Enables pulsed-SILAC proteomics to track and quantify de novo protein synthesis during the resuscitation process, distinguishing it from pre-existing proteins. |
Standardized Protocols for Enriching, Isolating, and Resuscitating Persisters In Vitro
FAQs and Troubleshooting Guide
FAQ 1: Why is my persister enrichment low after antibiotic treatment? A low persister yield often stems from an incorrectly determined Minimal Inhibitory Concentration (MIC) or an insufficient antibiotic treatment duration. The persister fraction only becomes apparent after the majority of susceptible cells have been killed.
- Solution:
- Confirm the MIC: Re-conduct a susceptibility test to ensure the antibiotic concentration is appropriate. A common practice is to use a concentration of at least 10 times the MIC to eliminate all non-persister cells [43].
- Perform a Time-Kill Assay: Establish a biphasic killing curve. The persister plateau is reached when the number of viable cells stabilizes over time despite continued antibiotic exposure. The duration to reach this plateau must be determined for each strain and antibiotic combination [43] [11].
FAQ 2: How can I distinguish between persisters and viable but non-culturable (VBNC) cells during resuscitation? This is a common challenge as both cell types appear alive with standard viability stains but do not immediately form colonies. The key difference is that persisters can resuscitate in standard culture media upon antibiotic removal, while VBNC cells typically cannot [9].
- Solution: Use a protein dilution method with flow cytometry.
- Induce expression of a stable fluorescent protein (e.g., mCherry) in your culture.
- Treat the cells with ampicillin, which lyses growing cells but leaves non-growing persisters and VBNC cells intact and fluorescent.
- After washing away the antibiotic, monitor the culture in fresh media without the inducer.
- Persisters will dilute the fluorescent protein as they divide, showing a decrease in fluorescence. VBNC cells will retain high fluorescence as they do not divide [9].
FAQ 3: My persister cells are not resuscitating consistently. What could be the cause? Inconsistent resuscitation can be due to the metabolic state of the persisters or the composition of the recovery medium.
- Solution:
- Optimize the Carbon Source: Research shows that persister cells have a reduced metabolic state, and their ability to resuscitate is highly dependent on the available carbon source. For example, E. coli persisters resuscitate more readily on glucose than on acetate [44] [13].
- Standardize Pre-culture Conditions: The length of the stationary phase in the pre-culture can affect the physiological state of persisters. Ensure consistent and documented pre-culture conditions [9].
- Confirm Recovery Time: Flow-cytometry data indicates that ampicillin persisters of E. coli can begin resuscitation within 1 hour after transfer to fresh media, with a doubling time similar to normal cells (~23 minutes) [9].
FAQ 4: Are there non-antibiotic-based methods to isolate persisters? Yes, traditional methods rely on antibiotics, which can themselves induce a stress response. Alternative protocols can reduce this potential bias.
- Solution: A lytic protocol using a combination of alkaline and enzymatic lysis (e.g., a commercial miniprep lysis solution and lysozyme) can rapidly kill normally growing cells based on their physiological state, leaving persister cells intact. This method is faster (under 45 minutes) and allows for the differentiation between Type I (stationary phase) and Type II (spontaneously generated during growth) persisters [45].
Key Experimental Protocols
Protocol 1: Determining the Minimum Inhibitory Concentration (MIC) and Time-Kill Curve
This is a foundational protocol for any persister study, as detailed in [43].
Method:
- Susceptibility Test (MIC):
- Prepare a two-fold dilution series of the antibiotic in a 96-well plate.
- Inoculate each well with a standardized bacterial inoculum (approx. 5x10^5 CFU/mL).
- Incubate for 16-20 hours.
- The MIC is the lowest antibiotic concentration that completely inhibits growth, determined by measuring OD595 and comparing it to a positive control [43].
- Time-Kill Assay:
- Expose a bacterial culture to a lethal dose of antibiotic (e.g., 10x MIC).
- Take 1 mL aliquots at regular time intervals (e.g., 0, 2, 4, 6, 24 hours).
- Serially dilute each aliquot and plate on non-selective agar to determine Colony Forming Units (CFU).
- Plot log(CFU/mL) over time. The point where the curve stabilizes indicates the "persister plateau" [43] [11].
Protocol 2: Isolating and Resuscitating Persisters for Downstream Analysis
This protocol combines established antibiotic treatment with monitoring techniques.
Method:
- Persister Isolation:
- Treat a mid-exponential or stationary-phase culture with a lethal antibiotic concentration (e.g., 100 µg/mL ampicillin for E. coli) for a duration determined from the time-kill curve (e.g., 3 hours) [43] [9].
- Centrifuge the sample to sediment the cells and wash the pellet twice with fresh medium or phosphate-buffered saline to remove the antibiotic thoroughly.
- Resuscitation and Monitoring:
- Resuspend the pellet in fresh, pre-warmed culture medium.
- To monitor resuscitation, you can:
- Measure CFU: Plate samples at regular intervals to track the recovery of cultivable cells.
- Use Flow Cytometry: Employ the protein-dilution method described in FAQ 2 to track the division of individual persister cells in real-time [9].
The workflow for isolating and monitoring persister cells is summarized below.
The Scientist's Toolkit: Research Reagent Solutions
Table 1: Essential reagents and their functions in persister cell research.
| Reagent / Material | Function in Persister Research | Key Considerations |
|---|---|---|
| Amikacin / Ofloxacin | Antibiotics used for persister enrichment via time-kill assays. | Mode of action is important. Amikacin (aminoglycoside) is often used for E. coli. Determine the specific MIC for your strain [43]. |
| Carbon Sources (e.g., 13C-Glucose, 13C-Acetate) | To study the metabolic state of persisters and their substrate preferences during resuscitation using isotopic tracing [44] [13]. | Persister metabolism is carbon-source-dependent. Glucose often supports better resuscitation than acetate [44]. |
| Carbonyl Cyanide m-chlorophenyl hydrazone (CCCP) | A chemical inducer of persister formation. It dissipates the proton motive force, leading to dormancy [44] [13]. | Useful for generating a synchronized persister population without using antibiotics, reducing potential stress-response biases [44]. |
| Lysozyme & Alkaline Lysis Solution | Key components of non-antibiotic persister isolation protocols. They selectively lyse metabolically active cells [45]. | This method is faster than antibiotic-based isolation and can help differentiate between Type I and Type II persisters [45]. |
| Fluorescent Proteins (e.g., mCherry) | Expressed in cells to monitor cell division and resuscitation at the single-cell level via flow cytometry or microscopy [9]. | The dilution of the fluorescent signal upon cell division allows visual confirmation of persister awakening and distinguishes them from VBNC cells [9]. |
| Sodium Arsenate | A metabolic inhibitor used to induce ATP depletion and a dormant, persister-like state [9]. | Useful as an experimental control for studying the link between low metabolic activity and antibiotic tolerance [9]. |
The following diagram illustrates the flow cytometry-based method for tracking persister cell division and distinguishing them from VBNC cells.
Overcoming Experimental Hurdles: A Guide to Optimizing Resuscitation Studies
Frequently Asked Questions (FAQs)
FAQ 1: Why do my viability counts disagree? I get different results from plate counts, flow cytometry, and molecular methods. This is a classic indicator of VBNC state interference. The table below summarizes what each method detects, explaining the discrepancies.
| Method | Target of Detection | Detects VBNC Cells? | Common Discrepancy Source |
|---|---|---|---|
| Culture-Based Plate Counts | Ability to replicate and form colonies on standard media. | No | The core definition of the VBNC state is the inability to grow on routine media, leading to significant underestimation of viable cells [46]. |
| Flow Cytometry | Membrane integrity and/or enzymatic activity via fluorescent dyes. | Yes, but can overestimate | Can overestimate VBNC counts in complex matrices due to interference; may not distinguish between viable and recently dead cells with intact membranes [47] [48]. |
| Viability PCR (v-PCR) | Amplifiable DNA from cells with intact membranes (using PMA/EMA dyes). | Yes | Requires rigorous optimization of dye concentration and incubation conditions for each specific sample matrix to prevent false positives/negatives [49] [47]. |
| Droplet Digital PCR (ddPCR) | Absolute quantification of target genes from viable cells (when combined with PMA). | Yes | Provides direct, absolute quantification without a standard curve, reducing variability and offering high precision for viable cell counts [49] [50]. |
FAQ 2: My antimicrobial efficacy tests show no colonies, but the infection recurs. Could VBNC cells be the cause? Yes. A sub-population of bacteria can enter the VBNC state upon exposure to sub-lethal doses of antimicrobials, including antibiotics and disinfectants like chlorine [46] [51]. While these cells are non-culturable at the time of testing, they remain viable and can resuscitate when the stressor is removed, leading to recurrent contamination or infection. This is a major blind spot in tests that rely solely on culture-based quantification.
FAQ 3: How can I definitively confirm the presence of VBNC cells in my sample and not just dead cells? Confirmation requires a multi-method approach, as no single technique is perfect. A robust protocol involves:
- Demonstrating Non-culturability: Confirm the absence of growth on standard culture media.
- Demonstrating Viability: Use culture-independent methods (e.g., PMA-ddPCR, flow cytometry with live/dead stains) to show that a significant population of cells maintains membrane integrity and metabolic activity [49] [52].
- Inducing Resuscitation: Attempt to revert the cells to a culturable state by removing the stressor and providing favorable conditions (e.g., nutrient upshift, temperature adjustment, or adding resuscitation supplements like catalase) [53]. An increase in CFU counts following resuscitation is definitive proof of the VBNC state.
Troubleshooting Guides
Issue 1: Optimizing Viability PCR (v-PCR) for Accurate VBNC Detection
Problem: High background signal from free DNA or dead cells, leading to overestimation of viable cells.
Solution: Optimize the protocol for using nucleic acid intercalating dyes like Propidium Monoazide (PMA) or PMAxx.
Step 1: Dye Selection and Concentration
- PMA/PMAxx: These dyes penetrate only cells with compromised membranes, crosslink to DNA upon photoactivation, and inhibit PCR amplification. PMAxx is an improved formulation with better efficacy [47] [48].
- Optimization is critical. Test a range of final concentrations (e.g., from 5 μM to 100 μM) to find the ideal level that fully suppresses DNA amplification from a heat-killed control sample without inhibiting signal from live cells [49] [50].
Step 2: Incubation and Photoactivation
- Incubate the dye with the sample in the dark for 20-30 minutes [49] [50].
- Perform photoactivation using a dedicated PMA-Lite device or a 650W+ halogen light source for 15 minutes on ice to prevent DNA degradation. Tubes should be placed horizontally and positioned close to the light source (~20 cm) for even exposure [50].
Step 3: Validate with Controls
- Always run three controls:
- Live Control: Untreated, culturable cells. Should show high DNA amplification.
- Dead Control: Heat- or chlorine-killed cells. Should show >99% inhibition of DNA amplification after PMA treatment.
- VBNC-Induced Sample: Your test sample.
- Always run three controls:
The following workflow outlines the optimized v-PCR protocol for VBNC cell detection:
Issue 2: Detecting VBNC Cells in Complex Sample Matrices
Problem: Standardized VBNC detection methods fail or give unreliable results in complex samples like fecal matter, soil, or process wash water (PWW) due to organic matter and particulates [47].
Solution: Use a combined dye approach and consider switching to digital PCR.
- EMA/PMAxx Combination: For complex matrices like food industry PWW, a protocol using 10 μM EMA and 75 μM PMAxx, incubated at 40°C for 40 minutes followed by a 15-minute light exposure, has been validated to effectively suppress DNA from dead cells [47] [48].
- Transition to ddPCR: Droplet Digital PCR (ddPCR) is highly recommended for complex samples. It partitions the sample into thousands of individual reactions, reducing the impact of inhibitors that are common in complex matrices. Furthermore, it provides absolute quantification without a standard curve, as demonstrated for quantifying HiAlc K. pneumoniae in mouse fecal samples [49] [50].
Problem: VBNC cells resuscitate during experiments, causing unexpected contamination and confounding results.
Solution: Understand resuscitation triggers and use chemical inhibitors.
- Identify and Control Triggers: Resuscitation can be induced by temperature upshifts, nutrient availability (e.g., yeast extract, amino acids), and the removal of stressors [52] [53]. Carefully control these environmental factors.
- Use of Chemical Inhibitors: Studies have shown that certain antibiotics can inhibit the resuscitation process without necessarily killing the VBNC cells. For example, ciprofloxacin has been shown to inhibit the recovery of VBNC-state K. pneumoniae while the cells maintained the potential for future resuscitation after the antibiotic was removed [49] [50]. This can be a valuable tool to "freeze" the VBNC population during specific experimental windows.
Research Reagent Solutions
The following table lists key reagents essential for researching VBNC cells and their functions.
| Reagent | Function in VBNC Research | Example Application |
|---|---|---|
| PMA / PMAxx | Viability dye; penetrates dead cells with compromised membranes, binding DNA and inhibiting its amplification in PCR. | Differentiating viable/VBNC cells from dead cells in qPCR/ddPCR assays [49] [47] [48]. |
| Ethidium Monoazide (EMA) | Viability dye; an alternative to PMA that uses efflux pumps to enter cells. Often used in combination with PMAxx in complex matrices. | Used with PMAxx (10μM EMA + 75μM PMAxx) to detect Listeria monocytogenes VBNC cells in process wash water [47] [48]. |
| Catalase | Enzyme that decomposes hydrogen peroxide (H₂O₂), a reactive oxygen species (ROS). | Resuscitation of VBNC lactic acid bacteria (e.g., L. brevis) from beer by supplementing culture media with 1000 IU/mL to counteract oxidative stress [53]. |
| Sodium Pyruvate | Chemical that acts as an H₂O₂ scavenger. | Used in culture media to recover L. rhamnosus GG cells that entered the VBNC state after high-pressure processing [53]. |
| Ferrioxamine E | A siderophore that provides the essential micronutrient iron (III) to bacteria. | Improves recovery and growth of stressed Salmonella and other pathogens from environmental samples and food, aiding in resuscitation [54]. |
| Ciprofloxacin | A broad-spectrum antibiotic. | Can be used at specific concentrations (e.g., 3-18 µg/mL) to inhibit the resuscitation of VBNC K. pneumoniae without eliminating the dormant population [49] [50]. |
## Frequently Asked Questions (FAQs)
FAQ 1: How does the pre-culture growth phase influence the type and resuscitation efficiency of persister cells?
The pre-culture growth phase fundamentally determines whether persisters originate from growth-arrested or actively growing cell subpopulations, which in turn affects their resuscitation dynamics.
- Exponential Phase Pre-culture: When cells are sampled from exponentially growing populations, most persisters that survive antibiotic treatment were actually growing actively before drug exposure [10]. These persisters exhibit heterogeneous survival modes, including continuous growth with L-form-like morphologies, responsive growth arrest, or post-exposure filamentation [10].
- Stationary Phase Pre-culture: Incubating cells under stationary phase conditions increases both the frequency and survival probability of non-growing persisters [10]. For example, with ampicillin treatment, most persisters giving rise to proliferating progeny were derived from the non-growing cell fraction after stationary phase pre-culture [10].
FAQ 2: What is the functional metabolic state of persister cells, and how do carbon sources affect their resuscitation?
Persister cells exhibit a generalized metabolic slowdown, but their metabolic state is not uniformly dormant; it adapts flexibly to the available carbon sources, which directly impacts resuscitation potential [14] [44] [13].
- Reduced Metabolic Activity: Compared to normal cells, persisters show delayed labeling dynamics in central metabolic pathways like the pentose phosphate pathway and the TCA cycle [14] [44].
- Carbon Source Dependence: The degree of metabolic shutdown is highly dependent on the carbon source.
- With glucose, persisters show generalized but reduced labeling in proteinogenic amino acids, indicating a uniform slowdown in protein synthesis [14] [44].
- With acetate, persisters undergo a more substantial metabolic shutdown, with markedly reduced labeling across nearly all pathway intermediates and amino acids. This is likely due to the high ATP cost of activating acetate for central metabolism [14] [44]. This suggests that resuscitating persisters might be more efficient when provided with readily utilizable carbon sources like glucose.
FAQ 3: Are all persister cells completely dormant, and why is this distinction important for resuscitation studies?
No, the classical view of persisters as uniformly dormant is an oversimplification. A continuum of metabolic states exists, which is crucial for designing resuscitation protocols [10] [55] [56].
- Metabolic Heterogeneity: Persisters can be broadly categorized, with Type I being non-growing (metabolically stagnant) and often induced by external stresses, and Type II being slow-growing (slow-metabolizing) and generated spontaneously without external triggers [55].
- Hierarchy of Persistence: A hierarchy exists where some persisters have "deep" persistence (strong persistence ability) while others have "shallow" persistence (weak persistence ability) [55]. This continuum means that resuscitation conditions that wake "shallow" persisters may not be effective for "deep" persisters.
FAQ 4: How do antibiotic classes interact with pre-culture conditions to determine the origin of persisters?
The antibiotic mechanism of action is a critical factor that interacts with pre-culture history. For instance, when treated with ciprofloxacin (a fluoroquinolone), all identified persisters were growing before treatment, even when samples were derived from post-stationary phase culture [10]. In contrast, ampicillin (a β-lactam) treatment resulted in persisters from both growing and non-growing fractions, depending on the pre-culture stage [10]. This highlights the need to consider both the antibiotic stressor and the cell's history.
## Troubleshooting Guides
Potential Cause 1: Inappropriate or Inhibitory Carbon Source The chosen carbon source in the resuscitation medium may not effectively support the reactivation of central metabolism in persister cells.
- Solution: Switch to a more favorable carbon source or include multiple options.
- Recommended Action: Use glucose (e.g., 2 g/L) as the primary carbon source instead of more metabolically demanding substrates like acetate [14] [44]. Glucose supports a more active, though still reduced, metabolic state in persisters, facilitating a smoother transition back to growth.
- Experimental Support: Data from stable isotope labeling shows that persister cells incorporate 13C from glucose into proteinogenic amino acids, confirming their capacity to utilize it, albeit at a reduced rate compared to normal cells [14] [44].
Potential Cause 2: Failure to Account for Pre-culture History The resuscitation conditions are not optimized for the specific type of persister (e.g., from exponential vs. stationary phase) being studied.
- Solution: Tailor resuscitation conditions based on the origin of the persisters.
- Recommended Action:
- For persisters generated from exponential phase cultures, expect heterogeneity. Monitor for various resuscitation modes such as filamentation or L-form-like growth [10].
- For persisters generated from stationary phase cultures, ensure the resuscitation medium is nutrient-rich to exit the deep dormancy state effectively [10].
- Recommended Action:
Potential Cause: Overlooking Small Population Stochasticity and Cell-Cell Interactions When the resuscitating persister population is very small, its dynamics become less predictable and are influenced by random fluctuations and ecological factors [57].
- Solution:
- Increase Replicates: Conduct a higher number of technical and biological replicates to account for inherent noise in small population behaviors [57].
- Standardize Inoculum Size: Precisely control the initial number of persister cells used in resuscitation assays to minimize variability stemming from population size effects [57].
The table below consolidates key quantitative findings on how carbon sources and pre-culture stages impact persister cell physiology and recovery.
Table 1: Impact of Culture Conditions on Persister Cell Metabolism and Survival
| Factor | Condition | Key Observational or Quantitative Findings | Experimental Context |
|---|---|---|---|
| Carbon Source | Glucose | Reduced but uniform labeling in proteinogenic amino acids; delayed labeling in central pathway, PPP, and TCA cycle intermediates [14] [44]. | E. coli BW25113 persisters induced by CCCP; 13C-tracing with LC-MS/GC-MS [14] [44]. |
| Carbon Source | Acetate | More substantial metabolic shutdown; markedly reduced labeling across nearly all pathway intermediates and amino acids [14] [44]. | E. coli BW25113 persisters induced by CCCP; 13C-tracing with LC-MS/GC-MS [14] [44]. |
| Pre-culture Stage | Exponential Phase | Most persisters to ampicillin or ciprofloxacin were growing before antibiotic treatment [10]. | Wildtype E. coli MG1655; single-cell observation in a microfluidic device [10]. |
| Pre-culture Stage | Stationary Phase | Increased frequency and survival probability of non-growing persisters to ampicillin [10]. | Wildtype E. coli MG1655; single-cell observation in a microfluidic device [10]. |
| Antibiotic Type | Ciprofloxacin | All identified persisters were growing before treatment, regardless of pre-culture phase [10]. | Wildtype E. coli MG1655; single-cell observation in a microfluidic device [10]. |
## Detailed Experimental Protocols
Protocol 1: Investigating Carbon Source Utilization in Persister Cells via Stable Isotope Tracing
This protocol is adapted from foundational metabolic tracing studies to analyze the functional metabolic state of persisters [14] [44] [13].
Persister Induction:
- Grow E. coli BW25113 in M9 minimal medium with 2 g/L unlabeled glucose to an OD600 of 0.5 [14] [44].
- Expose the culture to 100 μg/mL of the protonophore CCCP for 15 minutes at 37°C with shaking to induce persister formation [14] [44].
- Collect cells by centrifugation (3 min, 13,000 rpm) and wash three times with M9 medium without a carbon source to remove CCCP and metabolic byproducts [14] [44].
13C-Labeling and Sampling:
- Resuspend the pelleted control and persister cells to an OD600 of 5 in 10 mL of M9 medium [14] [44].
- Immediately initiate labeling by adding 2 g/L of either 1,2-13C2 glucose or 2-13C sodium acetate [14] [44].
- Incubate at 37°C with shaking and collect samples at critical timepoints (e.g., 0, 20 s, 5 min, 30 min, 2 h). At each timepoint, rapidly quench metabolic activity by cooling samples in liquid nitrogen [14] [44].
Metabolite and Proteinogenic Amino Acid Analysis:
- Metabolite Extraction: Lyophilize the cell pellets. Add 0.5 mL of 80:20 methanol-water extraction solution, incubate at -20°C for 1 hour, centrifuge, and filter the supernatant for LC-MS analysis of free metabolites [14] [44].
- Proteinogenic Amino Acid Analysis: Hydrolyze the remaining cell pellets with 6N HCl at 100°C for 18 hours. Derivatize the hydrolyzed amino acids using the TBDMS method and analyze via GC-MS [14] [44].
Data Interpretation:
Protocol 2: Single-City Analysis of Persister Resuscitation Dynamics Based on Pre-culture History
This protocol leverages microfluidic devices to track the resuscitation of individual persister cells with known histories [10].
Cell Preparation and Loading:
Antibiotic Treatment and Tracking:
Resuscitation Monitoring:
- After removing the antibiotic by switching the flow to fresh medium, continue time-lapse imaging to monitor the fate of surviving cells.
- Categorize the resuscitation dynamics of persisters based on their pre-treatment state (growing vs. non-growing) and their post-antibiotic behavior (e.g., immediate division, filamentation, L-form switching) [10].
## Experimental Workflow and Pathway Diagrams
## The Scientist's Toolkit: Research Reagent Solutions
Table 2: Essential Reagents and Materials for Persister Resuscitation Studies
| Reagent / Material | Function in Research | Key Considerations |
|---|---|---|
| 13C-Labeled Substrates (e.g., 1,2-13C2 Glucose, 2-13C Acetate) | To trace functional metabolic activity and carbon flux in persister cells during resuscitation via LC-MS/GC-MS [14] [44]. | Purity and isotope position are critical. Use concentrations around 2 g/L in M9 minimal medium to ensure the label is the primary carbon source [14] [44]. |
| Membrane-Covered Microchamber Array (MCMA) | A microfluidic device for single-cell, long-term tracking of bacterial growth and resuscitation under controlled medium conditions [10]. | Enables observation of over a million individual cells, allowing for the identification of rare persister events and their heterogeneous behaviors [10]. |
| Chemical Persister Inducers (e.g., CCCP) | To generate a synchronized population of persister cells for downstream metabolic or resuscitation assays without using antibiotics [14] [44]. | CCCP is a protonophore that disrupts the membrane potential. A typical protocol uses 100 µg/mL for 15 minutes. Requires thorough washing post-induction [14] [44]. |
| Catalase | An enzyme used in resuscitation media to decompose hydrogen peroxide, relieving oxidative stress that can maintain bacteria in a VBNC state [53]. | Effective for resuscitating certain lactic acid bacteria (e.g., Lactobacillus brevis) from the VBNC state. Typical supplementation is 1000 IU/mL in recovery agar [53]. |
| Propidium Monoazide (PMA) | A DNA-binding dye used in viability PCR (e.g., PMA-qPCR, PMA-ddPCR) to distinguish between viable cells (with intact membranes) and dead cells/damaged cells [58]. | Penetrates only compromised membranes, allowing selective quantification of viable cells. Optimal concentration and incubation time in the dark must be determined (e.g., 5-200 µM, 5-30 min) [58]. |
Frequently Asked Questions (FAQs)
FAQ 1: What makes metabolically sensitive persister cells more prone to lysis during experimental handling? Persister cells achieve antibiotic tolerance by entering a dormant state with drastically reduced metabolic activity. This dormancy involves downregulation of biosynthesis genes and energy production, rendering their cellular processes, including cell wall maintenance, vulnerable to sudden environmental shifts. When transferred from a stress condition (e.g., an antibiotic-containing medium) to a nutrient-rich resuscitation medium, rapid osmotic changes or abrupt restart of metabolic processes can overwhelm the fragile, inactive cell wall repair systems, leading to cell lysis [6] [11].
FAQ 2: How does the choice of resuscitation medium influence persister cell recovery and lysis? The nutrient composition of the resuscitation medium is critical. Evidence indicates that persister cells resuscitate primarily when presented with specific carbon sources, rather than spontaneously. For instance, in E. coli, L-alanine was shown to be a highly effective nutrient for initiating resuscitation, whereas other amino acids like asparagine were not [59]. Using an overly rich, non-specific medium (like undiluted Lysogeny Broth) can cause osmotic shock and inconsistent waking times, increasing the risk of lysis for a subpopulation of cells. A defined medium with a key nutrient is often preferable for controlled recovery [59].
FAQ 3: What are the best practices for physically handling persister cell pellets to prevent lysis? After centrifugation, the persister cell pellet is particularly fragile. It is essential to avoid vigorous vortexing and to resuspend the pellet gently, using a pipette with a wide-bore tip to minimize shear stress. Furthermore, pellets should never be allowed to dry out. Always carefully aspirate the supernatant and proceed with immediate, gentle resuspension in an isotonic buffer or the intended resuscitation medium that is matched for osmolarity [23].
Troubleshooting Guide
| Problem | Possible Cause | Recommended Solution |
|---|---|---|
| Low post-resuscitation viability | Osmotic shock from direct transfer to rich medium [59] | Gradually transition cells by resuspending in a balanced salt solution or a diluted (e.g., 0.1x) nutrient medium before moving to full-strength medium [60]. |
| High variability in recovery rates | Spontaneous, stochastic waking leading to asynchronous resuscitation [11] [59] | Use a waking agent like L-alanine for E. coli to synchronize the resuscitation initiation; employ single-cell techniques (microfluidics, microscopy) to monitor subpopulations [59]. |
| Cell lysis upon resuspension | Mechanical shear stress from harsh pipetting or vortexing [23] | Resuspend the cell pellet gently by pipetting up and down with a wide-bore pipette tip; avoid vortexing. |
| Failure to resuscitate any cells | (1) Persister population was not adequately enriched, or (2) Resuscitation medium lacks an essential nutrient [59] | (1) Validate persister isolation protocol with a kill curve using a bactericidal antibiotic. (2) Systematically test different carbon sources and nutrients in a minimal medium to identify the one required for waking. |
| Contamination of cultures | Improper sterile technique during the multi-step handling process. | Ensure all solutions are filter-sterilized or autoclaved; work in a laminar flow hood using aseptic technique. |
The following diagram illustrates the experimentally determined pathway through which E. coli persister cells sense nutrients and initiate resuscitation, a process critical to preventing lysis by ensuring a coordinated recovery.
Experimental Workflow for Gentle Persister Handling
The workflow below outlines a protocol designed to maximize the recovery of metabolically sensitive persister cells while minimizing stress and lysis.
The table below summarizes data from a key study investigating the effect of different nutrients on the resuscitation of E. coli persister cells, providing a quantitative basis for medium selection [59].
| Nutrient/Condition | Concentration | Resuscitation Frequency after 6 hours (%) | Key Finding |
|---|---|---|---|
| L-alanine (Ala) | 5X | 18 ± 1 | Highly effective waking signal; activates specific membrane sensor pathway. |
| Asparagine (Asn) | 5X | 2 ± 2 | Poor waking signal; highlights nutrient specificity in resuscitation. |
| No Carbon Source | N/A | 0 | Confirms waking is nutrient-triggered, not spontaneous. |
| Rich Medium (LB) | 1X | High (data not quantified) | Can lead to rapid but potentially asynchronous and stressful recovery. |
The Scientist's Toolkit: Research Reagent Solutions
| Reagent/Material | Function in Persister Protocols | Technical Notes |
|---|---|---|
| Lysogeny Broth (LB), Miller's Formula | Standard rich medium for routine bacterial culture and growing pre-cultures for persister induction [61] [62] [60]. | Contains 10 g/L Tryptone, 5 g/L Yeast Extract, 10 g/L NaCl. High salt content can be osmotically stressful for sensitive cells [60]. |
| M9 Minimal Salts | Base for creating defined resuscitation media, allowing precise control over nutrient composition [59]. | Prevents uncontrolled metabolic bursts; essential for testing the effect of specific carbon sources. |
| L-Alanine | A key amino acid for synchronously resuscitating E. coli persister cells by serving as a specific waking signal [59]. | Prepare as a filter-sterilized stock solution and add to M9 medium. Effectiveness is concentration-dependent. |
| Rifampicin | Antibiotic used to inhibit transcription and enrich for a high percentage of persister cells in a culture prior to experiments [59]. | Pretreatment stops transcription in non-persisters, making persisters the dominant population for study. |
| Carbonyl Cyanide m-Chlorophenyl Hydrazone (CCCP) | Protonophore that depletes cellular ATP, inducing a persister-like dormant state for experimental studies [59]. | An alternative method to generate persisters by halting energy production. |
| Phosphate Buffered Saline (PBS) | Isotonic buffer for washing cell pellets and making gentle dilutions without causing osmotic shock. | Crucial for resuspending fragile persister pellets after antibiotic removal and centrifugation. |
Frequently Asked Questions (FAQs)
Q1: What is a typical resuscitation rate for bacterial persister cells, and what should I consider "low"? Resuscitation rates for persister cells are inherently low. A study on Lactobacillus persisters observed that only around 0.5–1% of persister cells resuscitated when fresh media was added [63]. In the same study, persister cells themselves constituted a very small subpopulation (0.0001–1%) of the original bacterial culture [63]. A "low" rate should be evaluated against these benchmarks. If your observed resuscitation is significantly below this range, it could indicate an issue with the persister induction method, resuscitation conditions, or detection sensitivity.
Q2: My persister cells are not waking up. What are the most critical factors to check in my media composition? The choice of carbon source in your resuscitation media is a critical factor. Research on E. coli persisters demonstrates that their metabolic state and capacity to resuscitate are highly dependent on the available carbon source [44] [13]. Persisters exhibit reduced and delayed metabolic activity across central pathways like the Tricarboxylic Acid (TCA) cycle and pentose phosphate pathway. Furthermore, while persisters can utilize glucose, they may experience a more substantial metabolic shutdown when acetate is the sole carbon source due to the high ATP cost of activating it for metabolism [44]. Always ensure your media is fresh and that you have verified the pH and osmolarity are appropriate for your bacterial strain.
Q3: How long should I wait to see persister cell resuscitation? Resuscitation is not instantaneous and can occur over hours. Single-cell analysis of Lactobacillus persisters showed that resuscitation could be observed at specific time points such as 0, 8, and 15 hours after the introduction of fresh media [63]. For E. coli persisters induced by CCCP, metabolic labeling experiments tracked resuscitation over a period of 2 hours [44]. The timeline can vary based on the bacterial species, the method of persister induction, and the richness of the resuscitation media. Monitoring over a time course, rather than at a single endpoint, is recommended.
Q4: What is the difference between a persister cell and a resistant bacterium? Persister cells are tolerant, not resistant. This is a crucial distinction. Persister cells are genetically identical to the susceptible population but have entered a dormant, non-growing or slow-growing state that allows them to survive antibiotic treatment [11]. Once the antibiotic stress is removed and they resuscitate, their offspring are fully susceptible to the same drug. In contrast, resistant bacteria have acquired genetic mutations or mechanisms that allow them to grow in the presence of the antibiotic indefinitely [11].
Troubleshooting Guides
| Problem Area | Specific Issue to Investigate | Suggested Action |
|---|---|---|
| Persister Cell Quality | Incomplete removal of antibiotics before resuscitation. | Ensure adequate washing (e.g., 3x with fresh medium) after induction and before plating/incubating in recovery media [44]. |
| Induction method kills cells instead of inducing dormancy. | Validate the kill curve to ensure a biphasic pattern with a persistent subpopulation and confirm cell viability post-induction [63]. | |
| Resuscitation Media | Carbon source is unsuitable for resuscitating dormant cells. | Switch from a poor carbon source (e.g., acetate) to a more readily utilized one like glucose [44] [13]. |
| Media lacks essential nutrients or cofactors. | Use a rich, complete medium (e.g., MRS for Lactobacilli, LB for E. coli) for the best chance of recovery. | |
| Environmental Conditions | Incubation temperature is sub-optimal. | Verify the optimal growth temperature for your specific bacterial strain and ensure the incubator is correctly calibrated. |
| Resuscitation timeline is too short. | Extend the observation period and perform single-cell monitoring over a time course (e.g., 0, 8, 15, 24 hours) to catch heterogeneous resuscitation [63]. | |
| Detection Method | Assay is not sensitive enough to detect small resuscitating populations. | Use sensitive detection methods like single-cell analysis on agarose pads or counting CFUs from large volume concentrations [63]. |
| Media Component | Importance for Resuscitation | Optimization Strategy |
|---|---|---|
| Carbon Source | Drives the metabolic state and energy production required to exit dormancy [44] [13]. | Test multiple sources: Glucose is often preferred over acetate, as persisters show markedly reduced metabolic activity on acetate [44]. |
| Nitrogen & Amino Acids | Required for protein synthesis during the switch back to active growth. | Use complex media containing peptides and amino acids (e.g., tryptone, yeast extract) to provide building blocks. |
| Salts & Buffers | Maintains osmotic balance and stable pH, preventing additional stress. | Use a well-balanced salts medium (e.g., M9) supplemented with a buffer to maintain pH stability during extended incubation. |
| Vitamin & Cofactors | Essential cofactors for central metabolic enzymes. | Ensure your medium or rich supplements provide a full range of vitamins and cofactors. |
Data Presentation
The following table summarizes key quantitative findings from recent persister cell studies.
| Bacterial Species | Induction Method | Resuscitation Media | Key Quantitative Findings | Citation |
|---|---|---|---|---|
| Lactobacillus plantarum | Ampicillin (400 µg/ml, 30 h) | Fresh MRS Broth | • Persister population: 0.0001-1% of total population• Resuscitation rate: ~0.5-1% of persister cells | [63] |
| Escherichia coli | CCCP (100 µg/ml, 15 min) | M9 with 13C-Glucose or 13C-Acetate | • Substantial metabolic shutdown in persisters vs. normal cells• Markedly reduced labeling from acetate vs. glucose in persisters | [44] [13] |
Experimental Protocols
This protocol is adapted from methods used to generate and study Lactobacillus persisters [63].
Key Materials:
- Bacterial Strain: e.g., L. plantarum
- Growth Medium: MRS Broth and Agar
- Induction Antibiotic: Ampicillin stock solution (e.g., 10 mg/mL)
- Equipment: Centrifuge, microscope, agarose gel pads.
Methodology:
- Culture Preparation: Grow L. plantarum overnight in MRS broth at 37°C. Dilute the culture 1:50 in fresh MRS broth and incubate until the exponential growth phase is reached (OD600 ~0.6).
- Persister Induction: Treat the exponential-phase culture with a high concentration of ampicillin (e.g., 400 µg/mL). Incubate for a duration determined to result in a stable persister population (e.g., 30 hours), as validated by a kill curve assay showing a plateau in cell death.
- Washing: Collect the cells by centrifugation. Wash the cell pellet 2-3 times with 0.85% NaCl or fresh MRS broth to remove all traces of the antibiotic thoroughly.
- Resuscitation & Detection:
- Viable Count: Serially dilute the washed cell suspension and spot it onto MRS agar plates. Incubate and count Colony Forming Units (CFUs) after 24-48 hours.
- Single-Cell Microscopy: Place 5 µL of the washed persister cell suspension onto a 1.2% agarose/MRS gel pad. Cover with a coverslip and observe under a microscope at 37°C. Monitor and record resuscitation events at 0, 8, and 15-hour time points [63].
Protocol 2: Investigating Persister Metabolism via Stable Isotope Labeling
This protocol outlines the use of stable isotopes to probe the metabolic state of persister cells during resuscitation, as applied to E. coli [44] [13].
Key Materials:
- Bacterial Strain: e.g., E. coli BW25113
- Culture Medium: M9 minimal medium
- Persister Inducer: Carbonyl cyanide m-chlorophenyl hydrazone (CCCP)
- Tracers: 1,2-13C2 Glucose or 2-13C Sodium Acetate
- Equipment: LC-MS or GC-MS, centrifuge, liquid nitrogen.
Methodology:
- Persister Induction: Grow E. coli in M9 medium with 2 g/L glucose to mid-exponential phase (OD600 ~0.5). Expose the culture to CCCP (100 µg/mL) for 15 minutes with shaking. Centrifuge and wash the cells 3x with carbon-free M9 medium.
- Tracer Experiment: Resuspend the control and CCCP-induced persister cells in M9 medium at a high density (OD600 ~5). Immediately add the 13C-labeled carbon source (2 g/L 13C-glucose or 13C-acetate).
- Sampling and Quenching: At specific time points (e.g., 0, 20 sec, 5 min, 30 min, 2 h), withdraw samples and rapidly quench metabolism by submerging them in liquid nitrogen.
- Metabolite Analysis:
- Lyophilize the quenched cell pellets.
- Extract metabolites using an 80:20 methanol-water solution.
- Analyze the incorporation of the 13C label into metabolic intermediates (e.g., from TCA cycle, pentose phosphate pathway) using Liquid Chromatography-Mass Spectrometry (LC-MS) [44].
- For proteinogenic amino acids, hydrolyze the pellet with HCl and analyze via GC-MS using the TBDMS method [44].
Visualization
Metabolic State of Persister Cells
The Scientist's Toolkit
Key Research Reagent Solutions
| Reagent / Material | Function in Persister Resuscitation Studies |
|---|---|
| Beta-lactam Antibiotics (Ampicillin, Amoxicillin) | Used to induce the persister state in susceptible bacteria like Lactobacillus by targeting cell wall synthesis, leading to a dormant, tolerant subpopulation [63]. |
| CCCP (Carbonyl cyanide m-chlorophenyl hydrazone) | A chemical inducer of persistence that disrupts the proton motive force and ATP synthesis, allowing for the generation of a synchronized persister population for metabolic studies [44] [13]. |
| Stable Isotope Tracers (13C-Glucose, 13C-Acetate) | Essential for probing the functional metabolic state of persister cells. Their incorporation into metabolites and proteinogenic amino acids reveals pathway activity and carbon source preferences during resuscitation [44] [13]. |
| Agarose Gel Pads | Provide a solid support for single-cell microscopy, allowing for the direct, real-time observation of heterogeneous persister cell resuscitation over time [63]. |
| M9 Minimal Medium | A defined salts medium used to control the exact nutritional environment, particularly the carbon source, during tracer experiments and resuscitation assays [44]. |
Benchmarking Models and Metrics: Validating Resuscitation in Clinical and Ecological Contexts
FAQ 1: What defines a bacterial persister cell, and how is it different from antibiotic-resistant cells? Persisters are a subpopulation of genetically drug-susceptible bacteria that survive antibiotic treatment by entering a transient, dormant, and non-growing (or slow-growing) state. They are phenotypically tolerant, not genetically resistant. After the antibiotic stress is removed, they can resuscitate and resume normal growth, remaining susceptible to the same antibiotic. In contrast, resistant cells have genetic mutations that allow them to grow in the presence of the antibiotic [11] [64].
FAQ 2: What are the key molecular mechanisms known to trigger persister formation and resuscitation? The stringent response and the subsequent accumulation of the bacterial alarmone (p)ppGpp is a central regulator of persistence. High levels of ppGpp lead to a shutdown of cellular processes and growth [65] [64]. Key effector mechanisms include:
- Ribosome Dimerization: ppGpp induces proteins like RMF and Hpf, which convert active 70S ribosomes into inactive 100S ribosomes, inducing dormancy. Resuscitation involves the GTPase HflX, which dissociates these 100S ribosomes back to active 70S subunits [64].
- Toxin-Antitoxin (TA) Modules: These systems can act as effectors of ppGpp-induced persistence, where toxins disrupt essential cellular processes like translation [11] [65].
- Trans-translation and Protein Degradation: These systems help manage stalled translation and protein quality control during stress and recovery [11].
- Efflux Pumps: Active efflux during the resuscitation phase has been identified as a key parameter for persisters to recover after antibiotic treatment [12].
FAQ 3: My persister assays show inconsistent resuscitation rates. What factors can affect this? Resuscitation is not a purely stochastic (random) process but can be influenced by several factors [12]:
- Antibiotic Concentration During Treatment: Higher drug concentrations can cause more cellular damage, potentially delaying or altering the resuscitation dynamics [12].
- Efflux Pump Activity: The ability of cells to actively export residual antibiotics or toxins is critical for initiating regrowth [12].
- Cellular Damage: Many persisters resuscitate with structural and transcriptional damage from the antibiotic treatment, which can lead to heterogeneous resuscitation times and cell fates [12].
- Nutrient Availability: The presence of specific nutrients, such as alanine or glucose, can act as resuscitation signals by triggering chemotaxis pathways and lowering cAMP levels, which promotes ribosome reactivation [64].
FAQ 4: What is "persister partitioning," and why is it significant? Persister partitioning is a phenomenon observed during the first cell division of a damaged persister cell. The mother cell unevenly distributes cellular damage, generating one healthy daughter cell and one defective or non-viable daughter cell. This is considered a potential survival strategy for the population, as it allows a subpopulation to resume normal growth without the burden of damage [12]. This has been observed in E. coli, Salmonella enterica, Klebsiella pneumoniae, and Pseudomonas aeruginosa [12].
| Symptom | Possible Cause | Recommended Solution |
|---|---|---|
| No growth after sub-culturing | Viable but non-culturable (VBNC) state induced | Extend post-wash recovery time in rich media; consider adding known resuscitation signals (e.g., alanine, pyruvate) [66] [64]. |
| Insufficient washing of antibiotics | Increase wash volume and number of cycles; verify wash efficiency with a bioassay or HPLC. | |
| Antibiotic carryover inhibiting growth | Include efflux pump substrates (e.g., in energy-rich media) during recovery; use a neutralization agent in the recovery medium if available [12]. | |
| Low and inconsistent resuscitation | High antibiotic concentration during induction causing deep dormancy | Standardize persister induction protocol (e.g., use stationary-phase cultures, define MIC and treatment time precisely); use a lower, defined antibiotic concentration for induction [12] [11]. |
| Suboptimal recovery conditions | Use a nutrient-rich recovery medium (e.g., SOC, LB); ensure adequate aeration during outgrowth; recover at the optimal temperature for the bacterial species [67] [68]. |
| Symptom | Possible Cause | Recommended Solution |
|---|---|---|
| High scatter in resuscitation timing data | Heterogeneous persister population with varying damage | Use single-cell tracking techniques (e.g., microfluidics, time-lapse microscopy) to monitor individual cell resuscitation and partition sub-populations [12]. |
| Inconsistent initial persister population | Standardize the pre-culture growth conditions (media, temperature, shaking speed, exact growth phase) to minimize batch-to-batch variation in persister levels [66]. | |
| Clumping of cells during recovery | Use dispersing agents in media (e.g., low-concentration agarose); use flasks with baffles for better aeration and to prevent clumping [66]. |
Data derived from single-cell tracking of E. coli and Salmonella enterica after ampicillin treatment [12].
| Parameter | Description | Experimental Finding |
|---|---|---|
| Resuscitation Time (tR) | Time from antibiotic removal to first cell division. | Highly variable between individual cells, following an exponential model rather than a stochastic one [12]. |
| Doubling Time (δ) | Generation time of persister progeny after resuscitation. | Consistent and uncorrelated with tR, indicating normal growth once resuscitation is initiated [12]. |
| Exponential Rate Constant (β) | Parameter describing the acceleration of the resuscitation rate over time. | Increased with higher ampicillin concentration during treatment, indicating deeper dormancy [12]. |
Table 2: Observed Persister Partitioning Across Bacterial Species
Summary of the "persister partitioning" phenomenon where damaged persisters produce one healthy and one defective daughter cell [12].
| Bacterial Species | Antibiotic Class Used for Induction | Observation of Partitioning |
|---|---|---|
| Escherichia coli | β-lactam (Ampicillin) | Yes |
| Salmonella enterica | β-lactam (Ampicillin) | Yes |
| Klebsiella pneumoniae | Information missing from source | Yes |
| Pseudomonas aeruginosa | Information missing from source | Yes |
| E. coli UTI isolate | Information missing from source | Yes |
| In situ clinical UTI sample | Information missing from source | Yes |
This protocol is adapted from single-cell studies investigating the resuscitation dynamics of E. coli and Salmonella persisters after ampicillin treatment [12].
Principle: Track the resuscitation of individual persister cells after antibiotic treatment using time-lapse microscopy to quantify resuscitation times and observe cell fates like partitioning.
Materials:
- Bacterial strains (e.g., E. coli MG1655 expressing a fluorescent protein for visualization).
- LB broth and LB agar.
- Antibiotic stock solution (e.g., ampicillin, 100 mg/mL).
- Phosphate Buffered Saline (PBS) or fresh LB for washing.
- Agarose pads (1.5% in PBS or LB).
- Microscope slides and coverslips.
- Time-lapse fluorescence microscope with an environmental chamber (set to 37°C).
Procedure:
- Persister Induction:
- Grow a stationary-phase culture of the bacterial strain (e.g., incubate LB culture for ~16-24 hours).
- Add a high concentration of ampicillin (e.g., 100 µg/mL) to the culture. The exact concentration and treatment time should be determined empirically to kill >99% of the population.
- Incubate for 3-5 hours with shaking.
Washing and Preparation:
- Pellet the cells by centrifugation.
- Wash the cell pellet thoroughly 2-3 times with sterile PBS or fresh LB to remove all traces of the antibiotic.
- Resuspend the final pellet in a small volume of fresh LB.
Microscopy Setup:
- Prepare an agarose pad on a microscope slide.
- Spot a small volume (e.g., 2-5 µL) of the washed cell suspension onto the agarose pad and gently cover with a coverslip.
- Seal the edges with valap or another sealant to prevent drying.
Image Acquisition:
- Place the slide on the microscope stage pre-warmed to 37°C.
- Program the microscope to capture images of multiple fields of view at regular intervals (e.g., every 30 minutes) for 12-24 hours.
Data Analysis:
- Resuscitation Time (tR): Manually or computationally analyze the time-lapse images to determine the frame in which each initially non-growing cell undergoes its first division.
- Doubling Time (δ): Track the number of cells in each microcolony over time and calculate the doubling time post-resuscitation.
- Persistence Partitioning: Visually inspect the first and subsequent divisions for evidence of aberrant morphologies (e.g., filamentation, blebbing) in one of the two daughter cells.
This diagram illustrates the central role of the stringent response and ribosome inactivation in the formation and awakening of persister cells [64].
This diagram details how specific nutrients like alanine and glucose can trigger distinct signaling pathways to wake persister cells [64].
The Scientist's Toolkit: Key Reagents and Materials
Table 3: Essential Research Reagents for Persister Studies
| Reagent / Material | Function in Persister Research | Example / Note |
|---|---|---|
| Stationary-Phase Cultures | A standard method for generating a high subpopulation of Type I persisters. | Culture grown for 16-24 hours in rich medium (e.g., LB) [12] [11]. |
| Carbonyl Cyanide m-Chlorophenylhydrazone (CCCP) | An protonophore used to induce energy depletion and persister formation. | Used at sub-inhibitory concentrations to study the link between metabolism and persistence [11]. |
| SOC Medium | A nutrient-rich recovery medium used after antibiotic treatment and washing. | Supports efficient recovery and resuscitation of stressed bacterial cells [67] [68]. |
| Microfluidics Chips / Agarose Pads | Enable single-cell imaging and tracking of persister resuscitation over time. | Allows for monitoring of heterogeneous resuscitation dynamics and cell division events [12]. |
| Fluorescent Reporter Strains | Visualize and track persister cells and their progeny during microscopy. | Common reporters: GFP, mCherry. Can be fused to promoters of stress-responsive genes [12]. |
| Anti-persister Compounds | Molecules used to target and kill dormant persister cells. | Examples: Substituted indoles [64], Pyrazinamide (for M. tuberculosis) [11]. |
Frequently Asked Questions (FAQs)
Q1: What are the fundamental differences between the three main persister model systems? The three common model systems—chemical induction, antibiotic treatment, and biofilm-derived—generate persisters through different physiological routes, which impacts their dormancy depth and resuscitation dynamics.
- Chemical Induction: Uses metabolic inhibitors to rapidly induce a dormant state by depleting cellular energy (ATP). This method is efficient and reproducible but may produce persisters with uniform, shallow dormancy.
- Antibiotic-Treated: Relies on exposing a population to a lethal dose of antibiotics, which selectively kills growing cells and enriches for pre-existing, tolerant persisters. This method is highly relevant for studying treatment failure but can yield a heterogeneous mix of persister types.
- Biofilm-Derived: Harvests persisters from mature biofilms, where nutrient gradients and stress signaling naturally generate these cells. This model is most clinically relevant for chronic infections but is more complex and time-consuming to establish.
Q2: During the resuscitation phase, my persister cells are not regrowing. What could be the issue? A lack of resuscitation can stem from several factors related to cell viability and culture conditions.
- Verify True Persister Status: Ensure the non-growing cells are true persisters and not viable but non-culturable (VBNC) cells. True persisters should resuscitate in fresh, nutrient-rich media without antibiotics. Techniques like flow cytometry with fluorescent protein dilution can help distinguish them from VBNC cells [9].
- Check for Carryover Antibiotics: In antibiotic-treated models, incomplete washing can leave trace antibiotics in the resuscitation medium, preventing growth. Ensure thorough washing, potentially using a higher volume or multiple cycles.
- Confirm Media Richness: Resuscitation requires fresh, nutrient-rich media (e.g., LB broth for E. coli) to provide the signals to exit dormancy. The doubling time of resuscitating persisters should match that of normal cells in the same media [9].
Q3: Why is there high variability in persister counts in my antibiotic-treated models? Variability in persister counts is a common challenge, often influenced by pre-culture conditions and treatment specifics.
- Standardize Pre-culture Conditions: The length of the stationary phase in the overnight pre-culture significantly impacts persister levels. Long-term pre-cultures can accumulate more VBNC cells, which do not resuscitate, leading to inaccurate counts [9]. Consistently use pre-cultures of the same age and growth phase.
- Control Treatment Time and Concentration: Adhere strictly to defined antibiotic treatment times and concentrations. The method of persister formation (e.g., ampicillin treatment lyses growing cells) should be appropriate for your bacterial strain and research question [9].
Q4: How does the choice of model system affect the study of resuscitation mechanisms? The model system directly influences the observed resuscitation dynamics and underlying mechanisms.
- Antibiotic-Treated Models: Recent single-cell studies show that resuscitation after ampicillin treatment is not stochastic but follows an exponential model, where the resuscitation rate accelerates over time. This process is influenced by treatment antibiotic concentration and efflux pump activity during recovery [12].
- Biofilm vs. Planktonic Models: Persisters derived from biofilms may have different metabolic histories and damage levels compared to those from planktonic cultures. Biofilm structures can also physically trap cells and influence nutrient access during resuscitation.
Troubleshooting Guides
Issue 1: Low Persister Yield in Antibiotic-Treated Models
Potential Causes and Solutions:
- Cause: Inconsistent pre-culture growth phase.
- Solution: Always inoculate pre-cultures from a single colony and grow to a standardized optical density (OD) for the mid-exponential phase, or for a precise duration for the stationary phase. Use biological replicates.
- Cause: Incorrect antibiotic concentration or treatment duration.
- Solution: Perform a kill curve assay to establish the appropriate antibiotic concentration (typically 10-100x MIC) and treatment time that results in a biphasic killing pattern, confirming persister survival [9].
- Cause: Strain-specific low persistence.
- Solution: Use a strain with a known high-persistence (Hip) mutation (e.g., hipA7 in E. coli) as a positive control [69].
Issue 2: Contamination with Non-Persister Cells in Biofilm Models
Potential Causes and Solutions:
- Cause: Incomplete removal of planktonic cells before harvesting biofilm.
- Solution: Gently but thoroughly wash the biofilm multiple times with a buffer like PBS or saline before dislodging the biofilm-associated cells for antibiotic treatment.
- Cause: Ineffective antibiotic treatment to kill non-persisters within the biofilm.
- Solution: Use a higher antibiotic concentration or longer treatment duration than for planktonic cultures, as biofilm matrices can hinder antibiotic penetration. Validate the killing efficiency by plating and counting CFUs after treatment.
Potential Causes and Solutions:
- Cause: Heterogeneity in cellular damage from antibiotic treatment.
- Solution: Be aware that persisters are not a uniform population. After treatment, some persister cells partition damage unevenly during division, producing one healthy daughter cell and one defective one. This "persister partitioning" can lead to variable growth outcomes [12].
- Cause: Limitations in the detection method.
- Solution: Employ high-resolution single-cell tracking techniques (e.g., microfluidics with time-lapse microscopy) to monitor individual cell lineages before, during, and after antibiotic exposure. This allows for direct observation of heterogeneous resuscitation behaviors, such as continuous growth, filamentation, or L-form like division [10].
Table 1: Key Characteristics of Bacterial Persister Model Systems
| Characteristic | Chemical Induction | Antibiotic-Treated (Planktonic) | Biofilm-Derived |
|---|---|---|---|
| Induction Method | Metabolic inhibitors (e.g., Arsenate, CCCP) [70] | Lethal dose of antibiotics (e.g., Amp, Cip) [9] | Natural formation within biofilms [71] |
| Key Mechanism | ATP depletion, forced dormancy [70] | Selection of pre-existing dormant variants [11] | Nutrient gradient, stress response [71] |
| Typical Frequency | Can be increased to ~80% [70] | ~0.01% - 1% in exponential phase [71] [70] | Up to 1% or higher [71] |
| Resuscitation Onset | Rapid upon inducer removal | Within 1 hour in fresh media [9] | Varies, can be slower |
| Heterogeneity | Lower, more uniform | High, diverse subpopulations [10] | High, influenced by biofilm location |
| Clinical Relevance | Moderate (mimics energy depletion) | High (directly models treatment failure) | Very High (associated with chronic infections) [71] |
Table 2: Persister Resuscitation Dynamics from Single-Cell Studies
| Parameter | Findings | Experimental System |
|---|---|---|
| Resuscitation Time | Most persisters resuscitate within 1 hour of antibiotic removal [9]. | Flow cytometry of E. coli after ampicillin treatment |
| Doubling Time Post-Resuscitation | ~23.3 minutes, matching normal growth of untreated cells [9]. | Flow cytometry of E. coli |
| Resuscitation Dynamics Model | Exponential model (rate accelerates), not stochastic [12]. | Single-cell tracking of E. coli and Salmonella after ampicillin treatment |
| Key Controlling Parameters | Antibiotic concentration during treatment; efflux activity during resuscitation [12]. | Single-cell tracking and modeling |
| Cell Fate Post-Treatment | Heterogeneous: healthy growth, damage, or failure; includes "persister partitioning" [12]. | Single-cell tracking of multiple bacterial species |
Experimental Protocols
Protocol 1: Generating and Isulating Antibiotic-Treated Persisters from Planktonic Culture
This is a standard protocol for enriching persister cells [9].
- Grow pre-culture: Inoculate bacteria from a single colony into liquid medium (e.g., LB broth) and incubate overnight (~16 hours) at 37°C with shaking.
- Dilute culture: Dilute the overnight culture 1:100 into fresh medium and grow to the desired growth phase (e.g., mid-exponential phase, OD600 ~0.2-0.3).
- Administer antibiotic: Add a lethal dose of antibiotic (e.g., 100μg/mL ampicillin for E. coli, at 10-100x MIC). Incubate for a predetermined time (e.g., 3-5 hours).
- Remove antibiotic: Centrifuge the culture and carefully discard the supernatant. Wash the cell pellet 2-3 times with phosphate-buffered saline (PBS) or fresh medium to remove all traces of the antibiotic.
- Resuspend and quantify: Resuspend the washed cell pellet in fresh medium. Determine the persister titer by plating serial dilutions on antibiotic-free agar plates for CFU counting. This population is now enriched for persisters and can be used for resuscitation studies.
Protocol 2: Monitoring Resuscitation via Flow Cytometry and Protein Dilution
This protocol allows for tracking the resuscitation of persisters at the single-cell level [9].
- Generate fluorescent pre-culture: Grow an overnight culture of a strain harboring an inducible fluorescent protein (e.g., mCherry) in the presence of an inducer (e.g., IPTG).
- Treat with antibiotic: As in Protocol 1, dilute and grow the culture, then treat with ampicillin in the continued presence of the inducer to maintain fluorescence in all cells.
- Wash and resuspend: After treatment, wash the cells thoroughly to remove both the antibiotic and the inducer.
- Analyze via flow cytometry: Transfer the cells to fresh, inducer-free medium and monitor immediately using a flow cytometer. As persister cells resuscitate and divide, they will dilute the pre-existing mCherry protein, leading to a decrease in fluorescence intensity in the daughter cells. The number of cells with high fluorescence (non-dividing) and low fluorescence (dividing) can be quantified over time.
Signaling Pathways and Experimental Workflows
The Scientist's Toolkit: Research Reagent Solutions
Table 3: Essential Reagents for Persister Cell Research
| Reagent / Tool | Function / Application | Specific Examples |
|---|---|---|
| Metabolic Inhibitors | Chemically induce dormancy and increase persister frequency. | Arsenate (inhibits ATP synthesis), Carbonyl cyanide m-chlorophenyl hydrazone (CCCP, protonophore uncoupler) [70] |
| Beta-Lactam Antibiotics | Select for persisters by lysing growing, cell wall-synthesizing cells. | Ampicillin, Penicillin [9] |
| Fluoroquinolone Antibiotics | Select for persisters by targeting DNA gyrase in growing cells. | Ciprofloxacin, Ofloxacin [10] |
| Microfluidic Devices | Enable high-resolution, single-cell time-lapse imaging of persister formation and resuscitation. | Membrane-covered microchamber array (MCMA) [10] |
| Fluorescent Protein Systems | Track cell division and resuscitation via protein dilution; report on gene expression. | IPTG-inducible mCherry [9], GFP [10] |
| Flow Cytometry | Quantify and isolate subpopulations of cells based on physiology and fluorescence; monitor resuscitation. | Distinguishing persisters from VBNC cells [9] |
| ATP-Level Assays | Quantify cellular energy status, a key correlate of dormancy in persister cells. | Luciferase-based assays [70] |
Correlating In Vitro Findings with In Vivo Infection Models and Clinical Outcomes
Frequently Asked Questions (FAQs) & Troubleshooting Guides
FAQ 1: What are the fundamental differences between antibiotic resistance, tolerance, and persistence?
Answer: It is crucial to distinguish between these three phenomena when studying recalcitrant infections.
- Antibiotic Resistance: This is a heritable genetic trait in a bacterial population that allows it to grow in the presence of an antibiotic. It is typically measured by an increase in the Minimum Inhibitory Concentration (MIC) [72] [73].
- Antibiotic Tolerance: This describes the ability of the entire bacterial population to survive transient exposure to a bactericidal antibiotic. It is characterized by a slower rate of killing and is often associated with slow growth or metabolic inactivity, but is not necessarily heritable [72] [11].
- Antibiotic Persistence: This refers to a phenomenon where a small sub-population of genetically identical, antibiotic-susceptible bacteria enters a transient, non-growing or slow-growing state. This dormant state allows them to survive antibiotic treatment that kills their kin. Upon antibiotic removal, these "persister cells" can resuscitate and re-establish a susceptible population, leading to chronic or relapsing infections [72] [11] [71].
FAQ 2: Why do my in vitro persister assays not correlate with outcomes in my animal infection model?
Answer: This is a common challenge. Discrepancies often arise because standard in vitro conditions fail to replicate the complex host environment.
- Problem: In vitro models often use rich media and optimal growth conditions, which may not induce the same depth of dormancy as the nutrient-limited, immune-challenged environment in a host [72]. Furthermore, in vitro tests might not account for host factors like immune responses and spatial structures like biofilms.
- Solution:
- Refine Your In Vitro Model: Use media that more closely mimics the in vivo environment (e.g., nutrient starvation, acidic pH) to induce a more clinically relevant persister state [72] [11].
- Incorporate Host-Mimicking Conditions: Consider using models that include host-mimicking stressors or even ex vivo host samples.
- Verify with Multiple Detection Methods: Relying solely on Colony Forming Unit (CFU) counts can be misleading. Supplement with other techniques like fluorescence-activated cell sorting (FACS) with viability stains or nanomotion microscopy to better detect metabolically heterogeneous populations [73].
FAQ 3: How can I effectively target and eradicate bacterial persisters?
Answer: Eradicating persisters requires strategies that either kill the dormant cells or force them back into an active, antibiotic-susceptible state.
- Direct Killing Strategies:
- Membrane-Targeting Agents: Compounds like antimicrobial peptides (e.g., LL-37) or polymyxins can disrupt cell membranes and kill persisters even in a dormant state [73].
- Metabolic Wake-Up Strategies: Metabolites like mannitol or fructose can "wake up" persister cells, restarting their metabolism and making them susceptible to conventional antibiotics. This approach, known as UROPOT, is under clinical investigation [73].
- Inhibiting Dormancy Entry:
FAQ 4: What are the key molecular mechanisms governing persister cell formation?
Answer: Persister formation is a multifactorial process controlled by several interconnected biological pathways rather than a single dedicated mechanism [72] [11].
- (p)ppGpp/Stringent Response: This is a central global regulator. Under nutrient stress, accumulation of (p)ppGpp signaling molecules triggers a dramatic shutdown of ribosome and protein synthesis, promoting growth arrest and tolerance [73] [11].
- Toxin-Antitoxin (TA) Systems: These genetic modules are heavily implicated. Under stress, labile antitoxins are degraded, freeing stable toxins that can disrupt essential cellular processes like translation and replication, leading to growth arrest. The HipAB system is one of the most studied TA modules linked to persistence [73] [11].
- SOS Response: DNA damage can activate the SOS response, which involves the RecA/LexA pathway. This can induce the expression of toxins like TisB, which forms membrane pores and reduces proton motive force, leading to a dormant state [73] [71].
- Bacterial Envelope Stress: Research has identified a novel inducible stress response mechanism in the bacterial outer membrane, which involves the formation of a supramolecular complex that protects against envelope stress and may contribute to survival [74].
The following diagram illustrates the interplay between these key pathways in the formation of a persister cell.
Table 1: Key Metrics for Detecting and Characterizing Bacterial Persisters
| Detection Method | Key Principle | Quantifiable Output | Key Advantages | Noted Limitations |
|---|---|---|---|---|
| CFU Counting | Counting colonies after antibiotic exposure & plating. | Persister frequency = (CFU post-treatment / CFU pre-treatment) | Simple, widely available, gold standard. | Can overestimate efficacy for some antibiotics (e.g., fluoroquinolones); labor-intensive [73]. |
| Single-Cell RNA Sequencing (scRNA-seq) | Profiling transcriptome of individual cells. | Gene expression heterogeneity, identification of dormancy signatures. | Reveals metabolic diversity within a population. | Technically complex, expensive, does not distinguish viability [73]. |
| Nanomotion Microscopy | Detecting nanoscale vibrations of living cells. | Frequency and amplitude of oscillations as a proxy for metabolic activity. | Real-time, label-free monitoring of metabolic activity and resuscitation [73]. | Requires specialized equipment, data interpretation can be complex. |
Table 2: Efficacy of Anti-Persister Strategies and Compounds
| Therapeutic Strategy | Example Compound / Approach | Proposed Mechanism of Action | Reported Efficacy (In Vitro/Ex Vivo) | Clinical Development Stage |
|---|---|---|---|---|
| Metabolic Wake-up | Mannitol (UROPOT approach) | Increases proton motive force, enhancing uptake of aminoglycoside antibiotics. | Re-sensitizes E. coli and S. aureus persisters to killing by aminoglycosides [73]. | Clinical trials ongoing. |
| Membrane Targeting | Antimicrobial Peptide LL-37 | Disrupts bacterial cell membrane integrity. | Kills S. aureus persisters effectively [73]. | Pre-clinical research. |
| Inhibit Dormancy Entry | Tetrazole Ketone (e.g., NVS-100) | Inhibits (p)ppGpp synthesis, blocking the stringent response. | Reduces persister formation in P. aeruginosa and E. coli [73]. | Pre-clinical research. |
| Protein Aggregation Disruption | Bortezomib / DnaK/ClpB Inhibitors | Inhibits proteostasis systems, preventing recovery from protein aggregation during dormancy. | Induces permanent dormancy or death in resuscitating persisters [73]. | Early pre-clinical research. |
Experimental Protocols
Protocol 1: Induction and Isolation of Stationary-Phase Persisters
Principle: When a bacterial culture enters the stationary phase due to nutrient depletion, a significant subpopulation enters a non-growing state, enriching for persister cells [72] [71].
Methodology:
- Culture Preparation: Inoculate your bacterial strain of interest (e.g., E. coli, P. aeruginosa) into a suitable liquid medium (e.g., LB). Incubate with shaking at the appropriate temperature (e.g., 37°C).
- Growth Monitoring: Monitor the culture's optical density at 600 nm (OD600) until it reaches the stationary phase (typically after 16-24 hours, when the OD600 plateaus).
- Antibiotic Challenge:
- Take a 1 mL sample of the stationary-phase culture and perform serial dilutions in sterile saline or phosphate-buffered saline (PBS) to determine the pre-treatment CFU/mL by plating on antibiotic-free agar plates.
- To the main culture, add a high concentration of a bactericidal antibiotic (e.g., 100x MIC of ciprofloxacin or ampicillin).
- Incubate the culture with the antibiotic for a defined period (e.g., 3-5 hours).
- Persister Isolation:
- After incubation, pellet the cells by centrifugation (e.g., 5,000 x g for 5-10 minutes).
- Wash the cell pellet twice with sterile PBS to remove the antibiotic thoroughly.
- Resuspend the final pellet in fresh medium or PBS.
- Perform serial dilutions and plate on antibiotic-free agar to determine the post-treatment CFU/mL, which represents the persister population.
Troubleshooting: Ensure complete removal of the antibiotic through multiple washes to avoid carryover effects during the subsequent outgrowth or viability assessment.
Protocol 2: Anti-Persister Efficacy Assay Using Metabolic Wake-up Compounds
Principle: This assay tests the ability of a compound to re-sensitize bacterial persisters to a conventional antibiotic by perturbing their metabolic dormancy [73].
Methodology:
- Persister Preparation: Generate a persister-enriched population using Protocol 1 or a similar method.
- Treatment Setup: Prepare the following treatment groups in a 96-well plate or culture tubes:
- Group A: Persisters + Fresh Medium (Control for regrowth)
- Group B: Persisters + Antibiotic (e.g., Gentamicin)
- Group C: Persisters + "Wake-up" Compound (e.g., Mannitol)
- Group D: Persisters + "Wake-up" Compound + Antibiotic
- Incubation and Assessment:
- Incubate all groups for a specified period (e.g., 4-6 hours).
- After incubation, wash the cells to remove compounds/antibiotics if necessary.
- Serially dilute and plate each group on antibiotic-free agar to determine the viable CFU/mL for each condition.
- Data Analysis: Compare the CFU/mL from Group D (combination) to Group B (antibiotic alone). A significant reduction in CFU/mL in Group D indicates a synergistic effect where the "wake-up" compound has restored the antibiotic's efficacy against persisters.
The Scientist's Toolkit: Research Reagent Solutions
Table 3: Essential Reagents and Materials for Persister Cell Research
| Reagent / Material | Function in Research | Specific Examples & Notes |
|---|---|---|
| Bactericidal Antibiotics | To kill growing cells and select for the tolerant persister subpopulation. | Ciprofloxacin (DNA gyrase inhibitor), Ampicillin (cell wall synthesis inhibitor), Gentamicin (protein synthesis) [72]. |
| Viability Stains | To distinguish live/dead cells and assess membrane integrity via fluorescence. | Propidium Iodide (PI), SYTO 9 (used in LIVE/DEAD kits). Can be analyzed by fluorescence microscopy or flow cytometry. |
| Stress Inducers | To mimic host conditions and induce persister formation in vitro. | Carbon/Nitrogen starvation media, weak organic acids (to lower pH), Hydrogen Peroxide (oxidative stress) [11]. |
| Metabolic Modulators | "Wake-up" compounds to reverse persistence; inhibitors of persistence pathways. | Mannitol, Fructose, Pyruvate (to stimulate metabolism). Tetrazole ketones to inhibit (p)ppGpp synthesis [73]. |
| Biofilm Culturing Equipment | To grow surface-associated communities which are highly enriched in persisters. | Calgary biofilm device (peg lids), flow cells for continuous culture, polyvinyl chloride (PVC) or polystyrene plates [71]. |
Answer: Bacterial persisters are dormant, phenotypic variants within a genetically susceptible population that survive antibiotic treatment without genetic resistance. They are characterized by metabolic inactivity or slow growth, which protects them from conventional antibiotics that target active cellular processes. The critical problem emerges when antibiotic pressure is removed – persister cells can resuscitate and resume normal growth, leading to recurrent infections and treatment failure. This resuscitation phenomenon underlies many chronic and relapsing infections, including those associated with biofilms, urinary tract infections, and tuberculosis [11] [16].
Answer: Targeting resuscitation represents a strategic shift from conventional antibiotic approaches. Rather than killing all persisters immediately (which is challenging due to their dormancy), blocking resuscitation prevents population regrowth and eventual relapse. Scientifically, this approach exploits the transitional metabolic reactivation phase when persisters are vulnerable. During resuscitation, cells remain susceptible to compounds that disrupt critical wake-up processes before they achieve full metabolic recovery. Evidence indicates resuscitation is not entirely stochastic but can follow exponential dynamics influenced by prior antibiotic exposure and efflux pump activity [12]. Effective resuscitation blockade therefore interrupts specific molecular pathways essential for the dormant-to-active transition.
Troubleshooting Common Experimental Challenges
Why do my persister counts show high variability between replicates?
Answer: High variability in persister counts typically stems from several methodological issues:
- Inconsistent persister induction: Ensure standardized stressor conditions (antibiotic concentration, duration, physiological state of starter culture). For E. coli, stationary phase cultures typically yield ~1% persisters, while mid-log phase may yield only ~0.01% [64].
- Incomplete antibiotic removal: Residual antibiotics can inhibit resuscitation, falsely reducing counts. Implement thorough washing protocols with verification plates to confirm no carryover effect.
- Variable resuscitation conditions: Maintain precise temperature, nutrient composition, and removal of metabolic byproducts during recovery. Even slight pH variations can significantly impact resuscitation kinetics [75].
- Sampling timing: Persister resuscitation occurs asynchronously. Sample at multiple time points to capture the entire resuscitation curve rather than single endpoints [12].
Answer: This critical distinction requires experimental designs that exclude residual culturable cells:
- Serial dilution method: Dilute bacterial suspensions to extinction before resuscitation to ensure any growth originates from single, previously non-culturable cells [76].
- Antibiotic pretreatment: Add antibiotics like ampicillin to resuscitation media to inhibit any remaining culturable cells without affecting truly dormant persisters [76].
- H₂O₂ scavenger inclusion: Incorporate catalase or sodium pyruvate into media to eliminate hydrogen peroxide-sensitive culturable cells that might be misclassified as persisters [76].
- Single-cell tracking: Use microfluidic devices or time-lapse microscopy to directly observe resuscitation events from individual non-growing cells, providing the most definitive evidence [12].
Answer: False negatives (failing to detect effective compounds) can occur due to:
- Suboptimal compound timing: Administer test compounds both during and after antibiotic treatment, as some agents only work during specific resuscitation phases.
- Insufficient compound exposure: Some anti-persister compounds require prolonged contact due to slow penetration into dormant cells [77].
- Inappropriate viability markers: Rely on multiple viability assays (CFU, membrane integrity, metabolic activity) as compounds may inhibit resuscitation without immediate killing.
- Resuscitation window miss: Recognize that persistence ability decays over time – cells may lose resuscitability if tested too late after persister formation [76].
Frequently Asked Questions (FAQs)
Answer: Current research indicates several crucial pathways regulate resuscitation:
- Ribosome Reactivation: The ppGpp-mediated ribosome dimerization persister (PRDP) model highlights inactivation of 70S ribosomes to 100S dimers during persistence, with HflX GTPase-mediated redisassembly critical for resuscitation [64].
- Carbon Source Utilization: Metabolic tracing studies show persisters differentially utilize carbon sources during resuscitation, with glucose and acetate supporting distinct metabolic reactivation patterns [44] [13].
- Efflux Pump Activity: Evidence indicates efflux capability during resuscitation significantly influences resuscitation success and timing [12].
- Chemotaxis Systems: Alanine and glucose resuscitation pathways involve methyl-accepting chemotaxis proteins (Tar and Trg) and phosphotransferase systems that stimulate ribosome rescue [64].
The following diagram illustrates the core molecular pathway of ribosome-mediated resuscitation:
Answer: Implement these specific experimental approaches:
- Time-course monitoring: Track resuscitation kinetics in treated vs. untreated populations. True resuscitation blockers will show delayed or absent regrowth despite maintained viability [12].
- Metabolic state assessment: Compare metabolic activity (using 13C-labeled substrates) in compound-treated persisters during recovery. True resuscitation blockers will prevent metabolic reactivation patterns seen in controls [44].
- Membrane integrity testing: Use membrane-impermeant dyes to confirm cells remain intact despite blocked division, indicating cytostatic rather than cytotoxic effects.
- Wash-out experiments: Remove compounds after various intervals and assess whether resuscitation capacity returns, distinguishing reversible inhibition from killing.
Answer: A robust assay requires appropriate controls:
- Positive controls (known resuscitation blockers): Compounds like eravacycline, minocycline, or rifamycin SV have demonstrated persister-killing activity during wake-up phases [77].
- Negative controls (resuscitation permitters): Untreated persisters in fresh nutrient media should show characteristic exponential resuscitation dynamics [12].
- Viability controls: Include samples to confirm persisters remain viable despite resuscitation blockade (e.g., using different resuscitation triggers).
- Compound vehicle controls: Account for any effects of solvents or carriers used in compound preparation.
Quantitative Data on Anti-Persister Compound Efficacy
Table 1: Efficacy of Validated Anti-Persister Compounds
| Compound Class | Example Compounds | Target Pathway | Efficacy Against E. coli Persisters | Efficacy Against Other Species | Key Findings |
|---|---|---|---|---|---|
| Tetracycline derivatives | Eravacycline, Minocycline | Ribosome protection during wake-up | 99.9% killing at 100 µg/mL [77] | Active against P. aeruginosa and UPEC [77] | Accumulates in persisters; effective during resuscitation |
| Membrane-targeting compounds | XF-70, XF-73 | Cell membrane integrity | Not reported | Effective against S. aureus persisters [16] | Disrupts membrane potential; generates ROS |
| Synthetic cation transporters | SA-558 | Ion homeostasis | Not reported | Effective against S. aureus [16] | Causes autolysis in dormant cells |
| Metabolic disruptors | Pyrazinamide | Membrane energetics & PanD degradation | Not reported | Specific against M. tuberculosis [16] | Disrupts membrane energetics in acidic environment |
| Iminosugar derivatives | Compound 171, 161 | Unknown (structural similarity to eravacycline) | 85.2-95.5% killing at 100 µg/mL [77] | Under investigation | Identified through rational clustering approach |
| Bacterial Species | Induction Condition | Resuscitation Pattern | Key Influencing Factors | Partitioning Observed? |
|---|---|---|---|---|
| E. coli | Ampicillin treatment | Exponential acceleration [12] | Antibiotic concentration during treatment; efflux during resuscitation | Yes - damaged and healthy daughters [12] |
| Salmonella enterica | Ampicillin treatment | Exponential acceleration [12] | Antibiotic concentration during treatment; efflux during resuscitation | Yes - damaged and healthy daughters [12] |
| Klebsiella pneumoniae | β-lactam antibiotics | Not specified | Cellular damage from antibiotic treatment | Yes - damaged and healthy daughters [12] |
| Pseudomonas aeruginosa | Quinolone antibiotics | Not specified | Cellular damage from antibiotic treatment | Yes - damaged and healthy daughters [12] |
| Uropathogenic E. coli | Urinary tract infection context | Not specified | Environmental conditions (pH, nutrients) | Yes - observed in clinical isolates [12] |
Experimental Protocols for Key Assays
Purpose: Generate consistent persister populations and evaluate compound efficacy during resuscitation.
Materials:
- Bacterial strains (e.g., E. coli BW25113 or UPEC clinical isolates)
- Antibiotics for persister induction (e.g., ampicillin, ofloxacin)
- Test compounds for resuscitation blockade
- M9 minimal medium with defined carbon sources (glucose or acetate)
- LB broth for recovery media
- Plate counting materials or automated cell counter
Procedure:
- Persister induction: Grow bacteria to mid-log phase (OD600 ~0.5) in appropriate medium. Add 5-10× MIC of antibiotic (e.g., 100 µg/mL ampicillin for E. coli) and incubate for 3-5 hours until killing plateau is observed [12].
- Antibiotic removal: Wash cells 3× with fresh medium by centrifugation (5,000 × g, 5 min) to completely remove antibiotics. Verify removal by plating supernatant.
- Compound treatment: Resuspend persisters in fresh medium with test compounds at desired concentrations. Include positive and negative controls.
- Resuscitation monitoring: Incubate under optimal growth conditions. Sample at 0, 2, 4, 6, 8, 24, and 48 hours for:
- Viable counts (CFU/mL) on non-selective media
- Metabolic activity assays (e.g., AlamarBlue, ATP measurements)
- Morphological assessment (microscopy)
- Data analysis: Plot resuscitation curves and calculate resuscitation parameters:
- Lag time until first division
- Resuscitation rate (slope of exponential phase)
- Final recovery percentage
Troubleshooting notes:
- For slow-growing species, extend sampling to 72-96 hours.
- Include osmoprotectants in media for species prone to osmotic stress.
- For stringent anaerobes, maintain anaerobic conditions throughout.
Purpose: Visualize and quantify resuscitation dynamics at single-cell level.
Materials:
- Agarose pads or microfluidic device
- Time-lapse microscopy system with environmental chamber
- GFP-expressing bacterial strains (optional, for automated tracking)
- Image analysis software (e.g., ImageJ, CellProfiler)
Procedure:
- Sample preparation: After persister induction and washing, concentrate cells 10× and apply to agarose pads containing test compounds or vehicle control [12].
- Image acquisition: Program microscope to capture images every 15-30 minutes for 24-48 hours at appropriate magnification (60×-100×).
- Cell tracking: Manually or automatically track individual cells from dormancy through first division and subsequent divisions.
- Parameter quantification: For each resuscitating cell, measure:
- Resuscitation time (tR): time from start to first division
- Doubling time (δ): time between subsequent divisions
- Partitioning outcome: fate of daughter cells (growth, death, dormancy)
- Data analysis: Compare distributions of resuscitation parameters between treatment conditions using appropriate statistical tests.
The following diagram illustrates the experimental workflow for single-cell resuscitation analysis:
The Scientist's Toolkit: Essential Research Reagents
| Reagent Category | Specific Examples | Function in Resuscitation Studies | Considerations for Use |
|---|---|---|---|
| Persister-inducing antibiotics | Ampicillin, Ofloxacin, Colistin, Meropenem | Generate persister populations through bactericidal treatment | Concentration and duration must be optimized for each strain; monitor for complete killing of non-persisters [12] [75] |
| Metabolic labeling substrates | 13C-glucose, 13C-acetate | Trace metabolic reactivation during resuscitation | Use defined media; quench metabolism rapidly for accurate snapshots [44] [13] |
| Resuscitation blockers (positive controls) | Eravacycline, Minocycline, Rifamycin SV | Benchmark compounds for assessing resuscitation blockade | Effective during wake-up phase; accumulate in persister cells [77] |
| Efflux pump inhibitors | CCCP, PAβN | Probe role of efflux in resuscitation | Can induce persistence themselves at subinhibitory concentrations [44] |
| Ribosome-targeting probes | Antibodies against RMF, HPF, RaiA | Monitor ribosome state transitions during resuscitation | Requires fixation or lysis, not compatible with live tracking |
| Membrane integrity stains | PI, SYTOX Green | Distinguish live vs. dead cells during resuscitation | May not detect metabolically inactive but viable persisters |
| Culture media for resuscitation | LB, M9 with varied carbon sources, Artificial urine medium | Support recovery under controlled conditions | Carbon source significantly influences resuscitation success [75] [44] |
| Reactive oxygen detection | H2DCFDA, CellROX | Measure oxidative stress during recovery | Can itself generate ROS under light exposure |
Conclusion
The resuscitation of bacterial persister cells from a dormant state is not a singular event but a finely regulated process initiated by environmental and metabolic cues. A deep understanding of this process, enabled by advanced single-cell and omics technologies, is paramount for combating chronic infections. Future research must focus on bridging the gap between in vitro models and in vivo infection environments, identifying universal molecular targets across diverse pathogens to prevent resuscitation, and developing combination therapies that either lock persisters in a permanent dormant state or sensitize them to conventional antibiotics during wake-up. Success in this arena holds the key to significantly shortening treatment courses and reducing the global burden of relapsing bacterial diseases.
References
- 1. Viable but nonculturable (VBNC) state, an underestimated ... [https://www.sciencedirect.com/science/article/abs/pii/S0966842X23001476]
- 2. Viable but Nonculturable and Persister Cells Coexist ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC4598401/]
- 3. Recent Methods for the Viability Assessment of Bacterial ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC9500772/]
- 4. Pseudomonas aeruginosa persister cell formation upon ... [https://www.nature.com/articles/s41598-022-20323-3]
- 5. Tolerance and Persistence of Pseudomonas aeruginosa in ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC7481396/]
- 6. Persister cells: formation, resuscitation and combative ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC8590677/]
- 7. Single-cell imaging and characterization of Escherichia coli ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC6584399/]
- 8. Fast and Inexpensive Detection of Bacterial Viability and ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC5134538/]
- 9. Flow-cytometry analysis reveals persister resuscitation ... [https://bmcmicrobiol.biomedcentral.com/articles/10.1186/s12866-020-01888-3]
- 10. Observation of persister cell histories reveals diverse ... [https://elifesciences.org/articles/79517]
- 11. Bacterial persisters: molecular mechanisms and ... [https://www.nature.com/articles/s41392-024-01866-5]
- 12. Resuscitation dynamics reveal persister partitioning after ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10090945/]
- 13. Differential carbon source utilization drives metabolic state ... [https://pubmed.ncbi.nlm.nih.gov/40969939/]
- 14. Differential carbon source utilization drives metabolic state ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12440864/]
- 15. A host-directed adjuvant sensitizes intracellular bacterial ... [https://www.nature.com/articles/s41564-025-02124-2]
- 16. Mini review: Persister cell control strategies [https://www.frontiersin.org/journals/pharmacology/articles/10.3389/fphar.2025.1706115/full]
- 17. Ribosomes hibernate on mitochondria during cellular stress [https://pmc.ncbi.nlm.nih.gov/articles/PMC11461667/]
- 18. Forming and waking dormant cells: The ppGpp ribosome ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC7798447/]
- 19. Birth and Resuscitation of (p)ppGpp Induced Antibiotic ... [https://www.nature.com/articles/s41598-019-42403-7]
- 20. (p)ppGpp and Its Role in Bacterial Persistence [https://pmc.ncbi.nlm.nih.gov/articles/PMC7508602/]
- 21. Resuscitation Promotion Factor: A Pronounced Bacterial ... [https://www.mdpi.com/2076-2607/12/8/1528]
- 22. Exploring the multifaceted roles of resuscitation-promoting ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11978375/]
- 23. Protocol for assessing single-cell persister recovery ... [https://www.sciencedirect.com/science/article/pii/S2666166724001497]
- 24. Mini review: Persister cell control strategies - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC12568461/]
- 25. Flow cytometry study of Escherichia coli treated with ... [https://www.frontiersin.org/journals/microbiology/articles/10.3389/fmicb.2025.1592471/full]
- 26. Flow Cytometry Coupled with Resuscitation Assays As a ... [https://www.mdpi.com/2076-2607/12/6/1068]
- 27. Flow Cytometry Troubleshooting Guide [https://www.cellsignal.com/learn-and-support/troubleshooting/flow-cytometry-troubleshooting-guide?srsltid=AfmBOooofW-rW981w20rvIO9EkymYKMmaLEGyjP3elJliW281yFCZL-d]
- 28. Flow Cytometry Protocol | Abcam [https://www.abcam.com/en-us/technical-resources/protocols/flow-cytometry-for-intracellular-and-extracellular-targets]
- 29. A Peptide-Based Method for 13 C Metabolic Flux Analysis in ... [https://journals.plos.org/ploscompbiol/article?id=10.1371/journal.pcbi.1003827]
- 30. A guide to 13C metabolic flux analysis for the cancer biologist [https://pmc.ncbi.nlm.nih.gov/articles/PMC5938039/]
- 31. Using bioconductor package BiGGR for metabolic flux ... [https://pubmed.ncbi.nlm.nih.gov/25806817/]
- 32. Using Bioconductor Package BiGGR for Metabolic Flux ... [https://journals.plos.org/plosone/article?id=10.1371/journal.pone.0119016]
- 33. 13C-Fingerprinting and Metabolic Flux Analysis of ... [https://pubmed.ncbi.nlm.nih.gov/30788795/]
- 34. 13C metabolic flux analysis - PubMed Central - NIH [https://pmc.ncbi.nlm.nih.gov/articles/PMC9493264/]
- 35. 13C metabolic flux analysis of microbial and mammalian ... [https://www.sciencedirect.com/science/article/abs/pii/S1096717616300519]
- 36. Transcriptome Analysis of Streptococcus mutans Quorum ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10606796/]
- 37. Identification and genetic dissection of convergent persister ... [https://www.nature.com/articles/s41586-024-08124-2]
- 38. High-Throughput Proteomics Identifies Proteins With ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC6414554/]
- 39. High-Throughput Proteomics Identifies Proteins With ... [https://www.frontiersin.org/journals/microbiology/articles/10.3389/fmicb.2019.00378/full]
- 40. Proteomic analysis of the initial wake up of vibrio ... [https://pubmed.ncbi.nlm.nih.gov/36918451/]
- 41. Proteomic analysis of the initial wake up of vibrio ... [https://link.springer.com/article/10.1007/s11274-023-03559-7]
- 42. Antibiotic persisters are metabolically active, non-growing ... [https://www.sciencedirect.com/science/article/pii/S0924857924003029]
- 43. Protocol for assessing single-cell persister recovery ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11015153/]
- 44. Differential carbon source utilization drives metabolic state ... [https://www.frontiersin.org/journals/pharmacology/articles/10.3389/fphar.2025.1634627/full]
- 45. Novel Protocol for Persister Cells Isolation - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC3931647/]
- 46. How to Evaluate Non-Growing Cells—Current Strategies ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC7912045/]
- 47. Detection and Quantification Methods for Viable but Non ... [https://www.frontiersin.org/journals/microbiology/articles/10.3389/fmicb.2020.00673/full]
- 48. Detection and Quantification Methods for Viable but Non- ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC7214806/]
- 49. Absolute quantification of VBNC state formation and ... [https://pubmed.ncbi.nlm.nih.gov/41122686/]
- 50. Absolute quantification of VBNC state formation and ... [https://www.frontiersin.org/journals/cellular-and-infection-microbiology/articles/10.3389/fcimb.2025.1627943/full]
- 51. Regulatory formation of VBNC state antibiotic-resistant ... [https://www.sciencedirect.com/science/article/abs/pii/S0304389425029607]
- 52. Bacterial dormancy: A subpopulation of viable but non ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC7837498/]
- 53. Probiotic Viability Reconsidered: Integrating VBNC ... [https://www.mdpi.com/2076-2607/13/11/2479]
- 54. Viable but Nonculturable (VBNC) Bacteria [https://www.sigmaaldrich.com/US/en/technical-documents/technical-article/microbiological-testing/microbial-culture-media-preparation/viable-but-nonculturable-bacteria?srsltid=AfmBOoqATKGC3rqEvXyME2eGdTotzV9Noo80DhYSbMzha9Ubmc0GdHB5]
- 55. : molecular mechanisms and therapeutic... Bacterial persisters [https://www.nature.com/articles/s41392-024-01866-5?error=cookies_not_supported&code=4bbdd9bc-caa6-4305-9e89-2929af9a7100]
- 56. Slow and steady wins the race: an examination of bacterial persistence [https://www.aimspress.com/microbiology/article/1345/fulltext.html]
- 57. An ecological and stochastic perspective on persisters ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11697298/]
- 58. Absolute quantification of VBNC state formation and ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12535994/]
- 59. Persister Cells Resuscitate Using Membrane Sensors that ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC6957856/]
- 60. ProtocolsRecipesLysogenyBroth < Lab < TWiki [https://barricklab.org/twiki/bin/view/Lab/ProtocolsRecipesLysogenyBroth]
- 61. Lysogeny Broth (LB) [https://www.protocols.io/view/Lysogeny-Broth-LB-fcrbiv6]
- 62. Lysogeny broth (LB) Medium Preparation and Recipe [https://www.novoprolabs.com/tools/buffer-preparations-and-recipes/lysogeny-broth-lb-medium]
- 63. Lactobacillus Persisters Formation and Resuscitation - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC11091699/]
- 64. Combatting Persister Cells With Substituted Indoles [https://www.frontiersin.org/journals/microbiology/articles/10.3389/fmicb.2020.01565/full]
- 65. Molecular Mechanisms Underlying Bacterial Persisters [https://www.sciencedirect.com/science/article/pii/S0092867414002979]
- 66. How to culture bacteria - INTEGRA Biosciences [https://www.integra-biosciences.com/united-states/en/blog/article/how-culture-bacteria]
- 67. Protocols Inoculating a Liquid Bacterial Culture [https://www.addgene.org/protocols/inoculate-bacterial-culture/]
- 68. Enhance Bacterial Growth: Strategies for Efficient Cultures [https://en.vectorbuilder.com/resources/vector-academy/troubleshooting/bacterial-culture-troubleshoot.html]
- 69. Persister cells: formation, resuscitation and combative therapies | Archives of Microbiology [https://link.springer.com/article/10.1007/s00203-021-02585-z]
- 70. Strategies for combating persister cell and biofilm infections [https://pmc.ncbi.nlm.nih.gov/articles/PMC5609227/]
- 71. Bacterial Persister Cells and Development of Antibiotic ... - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC11335562/]
- 72. In Vitro Studies of Persister Cells - PMC - PubMed Central [https://pmc.ncbi.nlm.nih.gov/articles/PMC7667008/]
- 73. 综述:细菌顽固性机制的理解、检测与治疗靶向研究新进展 [https://www.ebiotrade.com/newsf/2025-8/20250809034856198.htm]
- 74. 昌增益 [https://www.bio.pku.edu.cn/homes/Index/news_cont_jl/17/30.html]
- 75. Anti-persister efficacy of colistin and meropenem against ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10710840/]
- 76. Wake Up! Resuscitation of Viable but Nonculturable Bacteria [https://pmc.ncbi.nlm.nih.gov/articles/PMC9818539/]
- 77. A rational approach to discovering new persister control ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12406675/]