Selective Inhibition Agents: Precision Tools for Target Microbe Isolation and Antimicrobial Development
This article provides a comprehensive resource for researchers and drug development professionals on the use of selective inhibition agents for the precise isolation of target microbes.
Selective Inhibition Agents: Precision Tools for Target Microbe Isolation and Antimicrobial Development
Abstract
This article provides a comprehensive resource for researchers and drug development professionals on the use of selective inhibition agents for the precise isolation of target microbes. It covers the foundational principles of selective action, from target-specific antibiotics to novel microbial metabolites, and details the methodological pipeline from screening to validation. The content addresses key challenges in the field, including economic barriers and resistance co-selection, and offers comparative analyses of agent efficacy. By synthesizing current research and emerging strategies, this review aims to equip scientists with the knowledge to advance precision microbiology and combat the escalating crisis of antimicrobial resistance.
The Principles and Promise of Selective Inhibition: From Broad-Spectrum to Precision Antimicrobials
In antimicrobial research and therapeutic development, "selective inhibition" describes strategies designed to target a specific biological process, virulence factor, or a narrow range of microbial species, while minimizing impact on non-targets. This approach contrasts with broader-spectrum strategies that exert a wider, less discriminatory effect.
The following table outlines the core characteristics of these two strategies:
| Feature | Narrow-Spectrum / Selective Strategy | Broad-Spectrum Strategy |
|---|---|---|
| Primary Goal | Disable a specific function (e.g., virulence, biofilm formation) or target a specific pathogen [1] [2]. | Kill or inhibit a wide range of bacteria, typically both Gram-positive and Gram-negative [3]. |
| Mechanism of Action | Targets virulence factors (e.g., Type III Secretion Systems), biofilm matrix components, or specific enzymatic pathways [1] [2]. | Often targets essential, conserved cellular structures like the cell wall or ribosomes [3]. |
| Spectrum of Activity | Limited and precise [4]. | Wide range [3]. |
| Impact on Microbiota | Minimal disruption, as commensals are largely spared. | Significant disruption, which can lead to dysbiosis. |
| Pressure for Resistance | Theoretically lower, as it does not directly threaten bacterial survival [1]. | Higher, due to direct lethal pressure on a broad range of bacteria [1]. |
| Ideal Use Case | Targeted anti-virulence therapy, biofilm disruption, and isolating specific microbes. | Empiric therapy for severe infections when the pathogen is unknown [4] [3]. |
Experimental Protocols for Studying Selective Inhibition
Protocol: Assessing Selective Inhibition of a Bacterial Virulence System
This protocol is adapted from studies on inhibiting the Type III Secretion System (T3SS) in Yersinia enterocolitica [1].
- Objective: To evaluate the effect of a candidate compound (e.g., Cinnamtannin B1) on the expression and secretion of virulence factors without affecting bacterial growth.
- Materials:
- Bacterial strain: e.g., Yersinia enterocolitica KT0004 (for phospholipase activity assay) [1].
- Candidate inhibitor compound.
- Culture media: TYE medium (for flagellar T3SS), Ysp medium (high salt, for Ysa T3SS), Yop medium (37°C, low calcium, for Ysc T3SS) [1].
- Centrifuge and cold trichloroacetic acid (for protein precipitation).
- SDS-PAGE equipment and Western blot reagents for specific effector proteins (e.g., YopH, YopO).
- Method:
- Culture and Treatment: Grow bacteria in the appropriate secretion media in the presence or absence of the inhibitor compound.
- Separate Fractions: Centrifuge cultures to separate the bacterial cell pellet from the culture supernatant (which contains secreted proteins).
- Precipitate Secreted Proteins: Treat the supernatant with cold trichloroacetic acid to precipitate secreted proteins [1].
- Analysis:
- Analyze both cell pellets and precipitated supernatant proteins via SDS-PAGE.
- Perform Western blotting to quantify specific effector proteins (e.g., YopH, YopO) in both fractions.
- Compare band intensity between treated and untreated samples to determine inhibition of secretion.
- Viability Control: Perform viable cell counts (CFU/mL) or measure culture optical density (Abs600) to ensure the compound does not affect bacterial growth [1].
Protocol: Evaluating Inhibition of Biofilm Amyloid Matrix
This protocol is based on research investigating the inhibition of curli fibers in E. coli biofilms [2].
- Objective: To determine if a compound selectively inhibits the production of functional amyloid fibers (curli) in a biofilm.
- Materials:
- Bacterial strain: e.g., E. coli W3110 (produces curli as primary ECM).
- Candidate inhibitor (e.g., Bacillaene).
- Salt-free LB agar.
- Amyloid-binding dyes: Congo Red (CR) and Thioflavine S (TS).
- Macrocolony biofilm setup.
- Method:
- Macrocolony Assay: Inoculate the bacterium on CR-containing agar in the presence of the inhibitor, or set up a pairwise interaction with a putative inhibitor-producing strain (e.g., Bacillus subtilis) [2].
- Visual Assessment: After incubation, observe macrocolony morphology and red staining (from CR) as a direct readout for curli production. Inhibition is indicated by loss of typical morphology and lack of CR staining [2].
- Microscopic Validation:
- Prepare cross-sections of the biofilm.
- Stain with the fluorescent dye Thioflavine S (TS).
- Visualize under a fluorescence microscope. A dense network of TS-stained fibers around cells indicates normal curli production, while a lack of fluorescence or a dispersed, unstructured appearance indicates successful inhibition [2].
The Scientist's Toolkit: Key Research Reagents
| Reagent / Material | Function in Selective Inhibition Research |
|---|---|
| Cinnamtannin B1 | A natural compound used to selectively inhibit the expression and secretion of specific effector proteins (YopH, YopO) in the Ysc T3SS of Yersinia enterocolitica without broad bactericidal activity [1]. |
| Bacillaene | A microbial metabolite that acts as a bifunctional inhibitor, exhibiting antibiotic activity at high concentrations and selectively inhibiting the assembly of curli amyloid fibers in E. coli biofilms at lower concentrations [2]. |
| Specialized Culture Media (Yop, Ysp) | Defined media that create specific environmental conditions (e.g., 37°C, low calcium) to induce the expression and function of target systems like the T3SS, enabling the study of their selective inhibition [1]. |
| Amyloid-Binding Dyes (Congo Red, Thioflavine S) | Vital tools for visualizing and quantifying the extracellular amyloid matrix of biofilms. A reduction in dye binding is a key indicator of successful anti-curli inhibition [2]. |
| PF-06446846 (PF846) | A drug-like compound that selectively inhibits eukaryotic translation termination by stalling the ribosome, demonstrating the application of selective inhibition in modulating host cell processes [5]. |
Troubleshooting FAQs
Q1: My candidate compound shows excellent selective inhibition in vitro, but it is ineffective in a cell culture infection model. What could be the reason?
A: This is a common translational challenge. Consider the following:
- Cellular Toxicity: Test the compound on the host cell line alone to rule out general cytotoxicity.
- Serum Binding: The compound may bind to serum proteins in the culture medium, reducing its effective concentration.
- Poor Cellular Uptake: The compound might not efficiently enter the host cells where the pathogen resides. Review the compound's chemical properties (e.g., logP, molecular weight) to predict permeability.
- Metabolic Instability: Host or bacterial enzymes may be degrading or modifying the compound. Investigate the compound's stability in conditioned media or cell lysates.
A: If bacterial viability is unaffected, the issue likely lies in the induction or detection of the T3SS.
- Confirm T3SS Induction: Double-check that the culture conditions (temperature, calcium concentration, pH) are correct for strong induction of the T3SS in your specific bacterial strain [1].
- Positive Control: Include a known T3SS inhibitor (if available) or a mutant strain deficient in T3SS to confirm that your assay conditions can detect a reduction in secretion.
- Secretion Efficiency: Ensure the centrifugation speed and time are sufficient to completely clear the bacterial cells from the supernatant. Contamination of the supernatant with lysed cells will give false positive signals.
- Detection Sensitivity: Optimize the concentration of trichloroacetic acid for protein precipitation and consider using Western blotting instead of Coomassie-stained gels for higher sensitivity and specificity for your target effectors [1].
Q3: When testing a compound for selective biofilm inhibition, I see a reduction in matrix but also a reduction in bacterial growth. How can I determine if the anti-biofilm activity is selective?
A: To dissect these effects, perform a dose-response experiment.
- Dose-Response Curves: Test a range of concentrations of your compound.
- Dual-Readout Assay: At each concentration, measure both bacterial growth (e.g., OD600 or CFU/mL) and a biofilm-specific metric (e.g., crystal violet staining for total biomass, CR/TS staining for curli).
- Determine Minimum Inhibitory Concentrations (MICs): Identify the minimum biofilm inhibitory concentration (MBIC) and the minimum growth inhibitory concentration (MGIC). A compound with selective anti-biofilm activity will have an MBIC that is significantly lower than its MGIC [2]. This indicates that the matrix is disrupted at concentrations that do not affect planktonic growth.
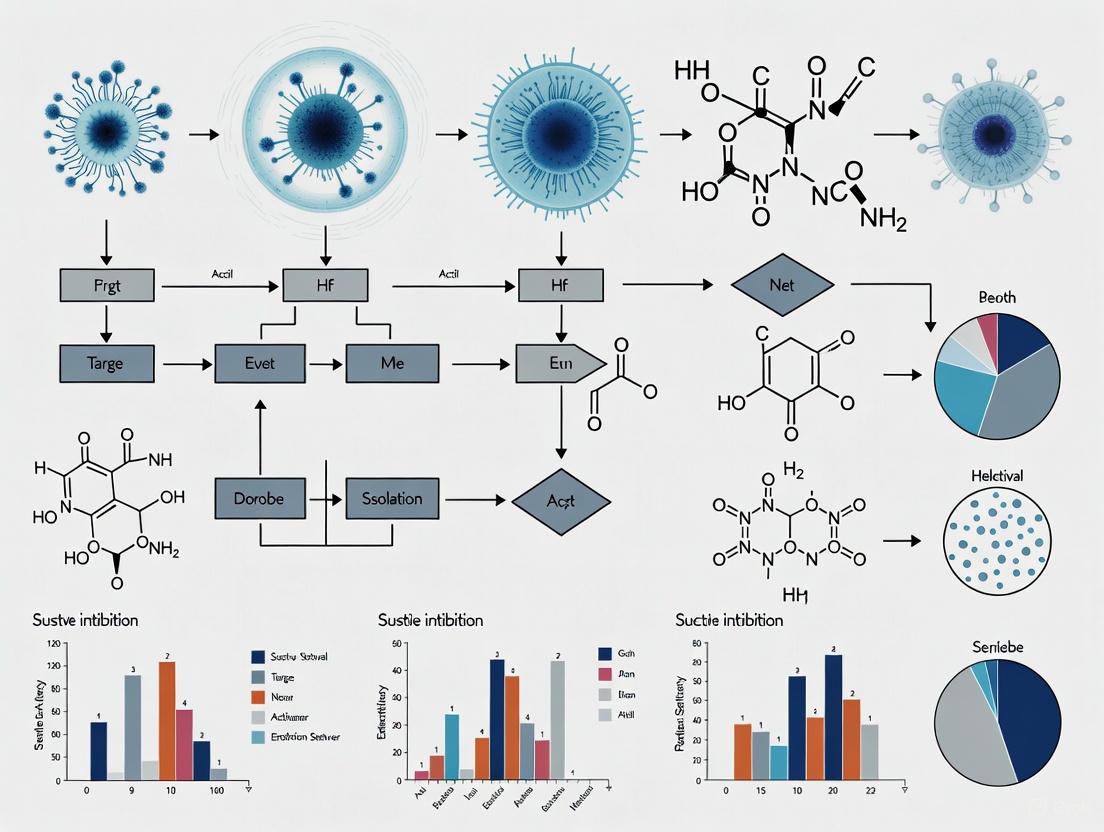
Visualizing the Strategic Concepts
The following diagram illustrates the core strategic differences between narrow-spectrum and broad-spectrum inhibition approaches.
The escalating global antimicrobial resistance (AMR) crisis underscores the urgent need for antibiotics with novel mechanisms of action. Inhibitors targeting bacterial enoyl-acyl carrier protein (ACP) reductases, particularly FabI, represent a promising class of antibacterial agents. These enzymes catalyze an essential, rate-limiting step in the bacterial fatty acid synthesis (FAS-II) pathway, which is fundamentally distinct from the mammalian FAS-I system. This structural and mechanistic divergence enables the development of inhibitors that selectively disrupt bacterial cell membrane integrity without harming host cells, making FabI a valuable target for selective inhibition and target microbe isolation research [6] [7].
Troubleshooting Guide: Common Experimental Challenges in FabI Research
1. Issue: Lack of Inhibitory Activity in Whole-Cell Assays Despite Strong Enzymatic Inhibition
- Potential Cause: Poor cellular penetration of the compound, often due to molecular properties incompatible with bacterial membrane transporters [8].
- Solution: Evaluate the compound against a panel of Gram-positive and Gram-negative strains. Gram-negative bacteria possess an outer membrane that can significantly limit uptake. Consider synthesizing analogs guided by rules for accumulation in Gram-negative bacteria (e.g., as applied in the development of fabimycin from Debio-1452) [8].
2. Issue: Inconsistent Minimum Inhibitory Concentration (MIC) Values
- Potential Cause: Inoculum size effect or improper culture medium preparation.
- Solution: Standardize the bacterial inoculum to ensure it is within the range of 1-5 x 10^5 CFU/mL for broth microdilution methods. Use freshly prepared Mueller-Hinton broth according to CLSI guidelines, as variations in cation concentration can affect results [6] [9].
3. Issue: Inability to Confirm FabI as the Primary Cellular Target
- Potential Cause: Off-target effects or the presence of alternative enoyl reductase isozymes (e.g., FabK, FabV) that compensate for FabI inhibition [7].
- Solution: Perform genetic knockout studies. For instance, in P. aeruginosa, which expresses FabV, a FabV knock-out can restore sensitivity to FabI inhibitors like triclosan [8]. Additionally, establish a correlation between the inhibitor's Ki (enzyme inhibition constant) and its MIC value; a strong linear correlation suggests FabI is the primary target [7].
4. Issue: High Compound Toxicity in Eukaryotic Cell Lines
- Potential Cause: Lack of selective toxicity, potentially due to inhibition of mitochondrial function, as mammalian mitochondria share a prokaryotic ancestry [10].
- Solution: Conduct cytotoxicity assays on mammalian cell lines (e.g., HEK-293, HepG2) early in the development pipeline. Counter-screen against mammalian fatty acid synthase (FAS-I) to confirm selectivity for the bacterial FAS-II pathway [7] [10].
5. Issue: Rapid Development of Bacterial Resistance
- Potential Cause: Single-point mutations in the fabI gene that alter the inhibitor's binding site [7].
- Solution: Combine FabI inhibitors with other antibiotics having different mechanisms of action. This approach reduces the selective pressure for resistant mutants. Monitor for mutations in the FabI catalytic triad (Tyrosine, Lysine, Serine) through serial passage experiments [11] [7].
Frequently Asked Questions (FAQs)
Q1: What makes FabI an attractive target for selective antimicrobial therapy? FabI is a key enzyme in the bacterial FAS-II pathway, which is essential for producing the lipids needed for bacterial cell membranes and, in Gram-negative bacteria, lipopolysaccharides. This pathway is absent in humans, who use the structurally different FAS-I system. Furthermore, FabI catalysis is a rate-determining step, meaning its inhibition severely disrupts the entire pathway, leading to bacterial cell death [6] [7].
Q2: Are there bacterial species inherently resistant to FabI inhibitors, and why? Yes, some species possess alternative enoyl-ACP reductase isozymes. For example, Streptococcus and Enterococcus express FabK, which is structurally and mechanistically distinct from FabI and resistant to typical FabI inhibitors like triclosan. Pseudomonas aeruginosa expresses FabV alongside FabI, contributing to its intrinsic resistance to many FabI inhibitors [8] [7].
Q3: How can I validate the binding mode of a novel FabI inhibitor? The most definitive method is X-ray crystallography of a ternary complex involving the target FabI enzyme, the NAD+ or NADH cofactor, and your inhibitor. This reveals atomic-level interactions, such as π-stacking with the nicotinamide ring of NAD+, hydrogen bonding with the catalytic tyrosine (e.g., Y159 in N. gonorrhoeae), and van der Waals contacts [12] [7]. Molecular dynamics simulations (e.g., 100 ns MD runs followed by MM-GBSA calculations) can further estimate binding stability and energies [6].
Q4: What are the critical steps for assessing the in vivo efficacy of a FabI inhibitor? After confirming in vitro potency and pharmacokinetic properties, use a relevant animal infection model. For instance, a murine vaginal gonorrhea model demonstrated the in vivo efficacy of Debio 1453 against multidrug-resistant Neisseria gonorrhoeae [12] [13]. Key steps include infecting the animal, treating with the compound, and monitoring bacterial load reduction over time compared to controls.
Q5: What are the best practices for performing an enzymatic FabI inhibition assay? Use a spectrophotometric assay that monitors the decrease in absorbance of NADH at 340 nm. The reaction mixture typically contains Tris buffer (pH 8.0), NADH, the FabI enzyme, and a substrate like crotonoyl-CoA. Initiate the reaction with the substrate, and measure the initial velocity of NADH oxidation. Pre-incubate the enzyme with the inhibitor to detect time-dependent inhibition. Calculate IC₅₀ values from dose-response curves [8] [7].
Experimental Protocols & Data Presentation
Protocol 1: Determination of Minimum Inhibitory Concentration (MIC)
The broth microdilution method is the standard for determining MIC [6].
- Preparation: Prepare Mueller-Hinton broth in 96-well plates. For fastidious organisms, supplement with lysed horse blood or other growth factors.
- Compound Dilution: Serially dilute the test compound in a logarithmic or two-fold manner across the plate.
- Inoculation: Standardize the bacterial suspension to 0.5 McFarland standard, then dilute to achieve a final inoculum of ~5 × 10⁵ CFU/mL in each well.
- Incubation & Reading: Incubate the plate at 35±2°C for 16-20 hours. The MIC is the lowest concentration of the compound that completely inhibits visible growth.
Protocol 2: Molecular Docking and Dynamics Simulation for FabI Inhibitors
This protocol is used to understand the binding mode and stability of inhibitors [6].
- Protein Preparation: Obtain the 3D structure of FabI (e.g., from PDB). Remove water molecules, add hydrogen atoms, and assign protonation states.
- Ligand Preparation: Draw the 3D structure of your inhibitor and minimize its energy using molecular mechanics.
- Docking: Perform molecular docking into the FabI active site (e.g., using MOE, AutoDock Vina) to generate potential binding poses.
- Simulation: Subject the best docking pose to molecular dynamics simulation (e.g., 100 ns using GROMACS/AMBER) in a solvated system to assess complex stability.
- Energy Calculation: Use MM-GBSA or MM-PBSA methods to calculate the binding free energy.
Quantitative Data on Promising FabI Inhibitors
The following table summarizes experimental data for key FabI inhibitors from recent literature, providing a benchmark for researchers.
Table 1: Comparative Activity of Selected FabI Inhibitors
| Compound Name / ID | Chemical Class | Target Enzyme | MIC Range (μg/mL) | Key Bacterial Strains | Key Findings |
|---|---|---|---|---|---|
| RK10 [6] | Diphenylmethane | saFabI | 1.32 - 47.64 | S. aureus, B. subtilis, E. coli | Broad-spectrum activity; superior to lead MN02. |
| Debio 1453 [12] [13] | Pyrido-enamide | NgFabI | 0.008 - 0.125 | Multidrug-resistant N. gonorrhoeae | Sub-nanomolar enzyme inhibitor (IC₅₀ 0.6 nM); efficacious in vivo. |
| Compound 1 [7] | Benzimidazole | FtuFabI | N/A | F. tularensis | Novel binding mode distinct from triclosan; IC₅₀ 0.3 μM. |
| Nilofabicin (CG400549) [8] | 2-Pyridone | SaFabI | N/A | MRSA | Completed Phase 2 clinical trials for skin infections. |
| Fabimyrin [8] | Pyrido-enamide | FabI | N/A | Broad-spectrum (Gram-negative) | Derivative of Debio-1452 engineered for Gram-negative accumulation. |
| Triclosan [6] [7] | Diphenyl ether | FabI | 0.13 - 64.00 | S. aureus, E. coli | Prototypical FabI inhibitor; widely studied but clinical use limited. |
Table 2: Reagent Solutions for Key FabI Experimental Workflows
| Research Reagent | Function / Application | Key Details / Considerations |
|---|---|---|
| Recombinant FabI Enzyme | In vitro enzymatic inhibition assays. | Can be expressed in E. coli with an N-terminal His-tag for purification via nickel-chelated chromatography [7]. |
| NADH / NAD+ | Essential cofactor for FabI enzymatic activity. | Used in spectrophotometric assays; NADH oxidation monitored at 340 nm [7]. |
| Crotonoyl-CoA | Model substrate for FabI enzymatic assays. | The enoyl substrate that is reduced in the FabI-catalyzed reaction [7]. |
| Triclosan | Control compound for FabI inhibition studies. | A well-characterized, reversible FabI inhibitor; useful for validating new assay systems [6] [7]. |
| Mueller-Hinton Broth | Standard medium for antimicrobial susceptibility testing (MIC). | Must be prepared consistently to avoid cation concentration variations that affect results [6] [9]. |
Visualizing Mechanisms and Workflows
The following diagrams illustrate the core concepts and experimental processes discussed in this guide.
FabI Inhibition Mechanism
FabI Inhibitor Development Workflow
The modern antibiotic development pipeline is in a state of crisis, characterized by a critical void in novel drug discovery and an accelerating global spread of antimicrobial resistance (AMR). This section addresses the most frequent high-level questions from researchers entering the field.
FAQ 1: Why is there so little investment in developing new antibiotics, despite a clear clinical need? The primary barrier is economic. Antibiotics are victim of a unique market failure where the financial return on investment (ROI) is fundamentally misaligned with their societal value.
- Short Treatment Duration: Unlike medications for chronic conditions (e.g., hypertension, diabetes), antibiotics are typically prescribed for short courses (days or weeks), severely limiting revenue potential compared to drugs taken for life [14].
- High Development Cost, Low Revenue: The mean cost to develop a systemic anti-infective is estimated at $1.3 billion, matching other drug classes. However, a new antibiotic typically generates only $15-50 million in annual US sales, far less than the estimated $300 million per year needed for sustainability [15].
- Stewardship vs. Sales: Effective new antibiotics are deliberately held in reserve and used as a last resort to slow resistance. This necessary "stewardship" practice directly conflicts with traditional pharmaceutical sales models that rely on volume [15].
FAQ 2: What is the "discovery void," and how long has it lasted? The "discovery void" or "innovation gap" refers to the period since the last truly novel antibiotic class was discovered. Analysis shows there have been no successful discoveries of novel antibacterial classes since 1987. The few new classes approved since 2000 (e.g., oxazolidinones, lipopeptides) were first discovered or patented decades earlier [14] [16]. The pipeline is now dominated by analogues of existing classes, which offers only a temporary solution due to cross-resistance [14].
Table 1: Global Burden of Antimicrobial Resistance (AMR)
| Metric | Statistic | Source & Context |
|---|---|---|
| Global deaths associated with AMR (2021) | 4.71 million annually | [14] |
| Projected AMR-associated deaths by 2050 | 10 million annually | [14] |
| Laboratory-confirmed infections resistant to antibiotics (2023) | 1 in 6 (global average) | WHO GLASS report (2025) [17] [18] |
| Resistant infections in S.-E. Asia & E. Mediterranean | 1 in 3 | WHO GLASS report (2025) [18] |
| E. coli resistant to 1st-line antibiotics (3rd-gen cephalosporins) | >40% | [17] |
| K. pneumoniae resistant to 1st-line antibiotics (3rd-gen cephalosporins) | >55% | [17] |
Technical Troubleshooting: Selective Inhibition & Isolation
This section provides practical guidance for common experimental challenges in developing selective inhibition agents, particularly for isolating and targeting Gram-negative pathogens.
FAQ 3: My candidate inhibitor shows great in vitro binding but fails to kill or inhibit Gram-negative bacteria in culture. What are the most likely causes? This is a classic problem in antibacterial discovery. The most probable causes relate to the formidable barriers presented by the Gram-negative bacterial cell.
- Cause A: Impermeable Outer Membrane. The lipopolysaccharide (LPS)-rich outer membrane of Gram-negative bacteria is a highly effective permeability barrier, blocking many hydrophobic and large compounds.
- Troubleshooting: Perform an accumulation assay. Compare intracellular concentration of your compound in a standard Gram-negative strain (e.g., E. coli) versus a strain with defined permeability mutations (e.g., lpxC mutants with impaired LPS biosynthesis). A significant increase in accumulation in the mutant strain confirms a permeability issue [16].
- Cause B: Efflux Pumps. Bacteria express multi-drug efflux pumps (e.g., AcrAB-TolC in E. coli) that actively export a wide range of compounds out of the cell.
- Troubleshooting: Repeat the MIC assay in the presence of a sub-inhibitory concentration of an efflux pump inhibitor (e.g., Phe-Arg β-naphthylamide, PABN). A significant drop (e.g., 4-fold or greater) in the MIC of your compound in the presence of the inhibitor indicates it is an efflux pump substrate [16].
FAQ 4: How can I selectively inhibit a specific bacterial target, like a biofilm matrix component, without broadly killing the organism? This approach, known as "anti-virulence" or "anti-biofilm" strategy, aims to disarm the pathogen without imposing strong selective pressure for resistance. A prime example is the inhibition of curli amyloid fibers in E. coli biofilms.
- Background: Curli fibers are a primary ECM component in many E. coli biofilms. Their synthesis involves a highly regulated pathway, offering multiple targets for selective inhibition [2].
- Experimental Protocol: Screening for Curli Inhibitors using Macrocolony Biofilms
- Strain and Media: Use E. coli K-12 strain W3110, which produces curli as its primary ECM. Use salt-free LB agar, optimal for curli production, supplemented with the amyloid-binding dye Congo Red (CR) at 20-40 µg/mL.
- Test Compound Application: Spot your candidate compound (e.g., purified metabolite, synthetic molecule) at a sub-inhibitory concentration (determined by prior MIC assay) onto the agar near the intended inoculation point.
- Inoculation and Growth: Inoculate the center of the plate with E. coli and incubate statically at 28-30°C for 3-5 days to allow macrocolony biofilm development.
- Analysis of Inhibition:
- Positive Result (Inhibition): A zone of altered morphology and lack of red CR staining around the compound spot indicates successful inhibition of curli production.
- Negative Result (No Inhibition): The biofilm will display a characteristic wrinkled, concentric ring morphology with intense, uniform red staining.
- Control: Always include a solvent-only control spot [2].
Diagram 1: Screening workflow for curli inhibitors.
Advanced Methodologies & Reagent Solutions
For researchers moving from screening to mechanistic studies, this section details specific protocols and essential reagents.
Experimental Protocol: Verifying Direct Inhibition of Curli Fiber Assembly In Vitro This protocol follows up on a positive result from the macrocolony screen to determine if the compound directly blocks the polymerization of the core curli subunits (CsgA and CsgB) [2].
- Purify Curli Subunits: Express and purify recombinant CsgA and/or CsgB protein from E. coli using His-tag affinity chromatography.
- Prepare Reaction Mixtures:
- Test: Purified CsgA (e.g., 5 µM) + candidate inhibitor at various concentrations.
- Positive Control: Purified CsgA alone.
- Negative Control: Buffer only.
- Induce Polymerization: Incubate all reaction mixtures at 37°C for 16-24 hours to allow for amyloid fiber formation.
- Quantify Amyloid Formation:
- Thioflavin T (ThT) Assay: Add ThT dye to each reaction. ThT fluorescence (excitation ~440 nm, emission ~485 nm) increases upon binding to amyloid fibrils. A significant reduction in fluorescence in the test sample compared to the positive control indicates direct inhibition of fiber assembly.
- Transmission Electron Microscopy (TEM): Visualize aliquots from each reaction with TEM. The positive control should show abundant fibrils, while the effective test sample will show few or no fibrils.
Table 2: Research Reagent Solutions for Selective Inhibition Studies
| Reagent / Material | Function / Application in Research | Key Consideration |
|---|---|---|
| Congo Red (CR) | Amyloid dye for visual detection of curli fibers in bacterial colonies or on filters. | CR binding is a qualitative, not quantitative, measure of curli production [2]. |
| Thioflavin T (ThT) / Thioflavin S (TS) | Fluorescent dyes used to quantify (ThT in vitro) or visualize (TS in situ) amyloid fibrils. | ThT fluorescence is directly proportional to amyloid content in solution [2]. |
| Bacillaene | A microbial metabolite serving as a proof-of-concept bifunctional inhibitor;它具有 bacteriostatic and anti-curli activity. | Demonstrates the potential for compounds that combine antibiotic and anti-virulence properties [2]. |
| Phe-Arg β-naphthylamide (PABN) | An efflux pump inhibitor used to troubleshoot compound accumulation in Gram-negative bacteria. | Can be toxic at high concentrations; use sub-inhibitory levels in checkerboard MIC assays [16]. |
| Salt-Free LB Agar | Culture medium optimized to induce robust curli production in E. coli for screening purposes. | Standard LB contains salt (NaCl), which can suppress curli expression [2]. |
Diagram 2: Curli biogenesis pathway and inhibition point.
Path Forward & Incentive Structures
FAQ 5: What innovative economic models are being proposed to fix the broken antibiotic market? Recognizing that traditional market forces are insufficient, global health bodies and industry alliances are proposing "pull" incentives to reward successful innovation.
- Lump-Sum Market Entry Rewards: Governments or a consortium of payers would offer a substantial, one-time monetary prize (e.g., $1-3 billion) to a company that successfully develops and licenses a priority antibiotic. This de-links the company's revenue from the volume of drug sold, allowing for responsible stewardship while ensuring a positive ROI [15].
- Subscription Models: Similar to Netflix, a government health system could pay an annual subscription fee to a company for access to a new antibiotic, regardless of how much is used in a given year. This model is already being piloted in the UK and Sweden [14] [15].
- Transferable Exclusivity Vouchers: A company that develops a priority antibiotic could receive a voucher granting an additional year of market exclusivity for any other drug in its portfolio, which could be worth billions. This voucher could also be sold to another company [15].
The quest for novel selective agents is pivotal in microbiology for isolating and studying specific microbes, a cornerstone of drug development and microbiological research. The human gut, a complex ecosystem teeming with microorganisms, produces a diverse array of metabolites that play crucial roles in microbial interference and communication. These gut-derived metabolites, including short-chain fatty acids (SCFAs), bile acids, polyamines, and tryptophan derivatives, function as natural selective agents by modulating the microbial environment [19] [20]. They inhibit the growth of competing species, shape community structure, and maintain ecological balance, offering a rich repository of compounds for targeted microbial isolation and inhibition. Understanding the mechanisms of these endogenous metabolites provides a framework for developing sophisticated strategies to isolate target microbes, manipulating microbial communities to favor or suppress specific members, and discovering new therapeutic avenues. This technical support document synthesizes current knowledge on these microbial interactions, providing troubleshooting guidance and practical methodologies for researchers in the field.
Troubleshooting Guides and FAQs
Frequently Asked Questions (FAQs)
FAQ 1: What are the primary classes of gut-derived metabolites that can act as selective agents? The gut microbiota produces several key classes of metabolites with demonstrated selective, inhibitory potential [19] [20]:
- Short-Chain Fatty Acids (SCFAs): Acetate, propionate, and butyrate, produced from dietary fiber fermentation.
- Bile Acids: Primary bile acids (e.g., cholic acid) metabolized by gut bacteria into secondary bile acids (e.g., deoxycholic acid, lithocholic acid).
- Tryptophan Derivatives: Metabolites like indole-3-propionic acid and other indole derivatives produced from dietary tryptophan.
- Polyamines: Spermidine, spermine, and putrescine, derived from dietary protein and microbial synthesis.
FAQ 2: How do microbial metabolites achieve selective inhibition? Selective inhibition is achieved through multiple mechanisms [19] [20]:
- Receptor-Mediated Signaling: Metabolites bind to specific receptors on host or microbial cells (e.g., GPR41, GPR43, FXR, AhR), triggering signaling cascades that alter the microenvironment and make it less hospitable for certain microbes.
- Epigenetic Modulation: Metabolites like butyrate inhibit histone deacetylases (HDAC), influencing host gene expression related to inflammation and immune cell differentiation, which indirectly shapes the microbial community.
- Metabolic Interference: Some metabolites can disrupt essential metabolic pathways in susceptible microbes or alter local pH.
- Membrane Integrity: Certain metabolites, particularly secondary bile acids, can damage bacterial cell membranes.
FAQ 3: Why is my targeted inhibition of a pathogen using a metabolite not working? Several factors could be at play:
- Insufficient Concentration: The metabolite concentration may be below the effective inhibitory threshold. Troubleshooting:
- Perform a dose-response curve to determine the Minimum Inhibitory Concentration (MIC).
- Ensure stability of the metabolite in your culture medium; some compounds may degrade.
- Microbial Resistance: The target pathogen may possess efflux pumps, degrading enzymes, or genetic mutations that confer resistance. Troubleshooting:
- Check for known resistance mechanisms in the literature.
- Consider using a combination of metabolites to overcome resistance.
- Incorrect Environmental Conditions: Factors like pH, oxygen levels, and the presence of other nutrients can affect metabolite activity. Troubleshooting:
- Mimic the natural gut environment as closely as possible (e.g., anaerobic conditions, appropriate pH).
- Review the growth requirements of both the target microbe and the producer microbes.
FAQ 4: How can I model complex gut microbiome interactions in vitro? To accurately study these interactions, complex models are required:
- Co-culture Systems: Culturing the target microbe with one or more producer strains.
- Simulated Gut Reactors: Using sophisticated bioreactors that simulate the human gut's physiological conditions, including pH gradients, nutrient delivery, and microbial retention times.
- Microbial Interaction Networking: Analyze your data to map out potential stimulatory and inhibitory relationships between the species in your consortium.
Troubleshooting Common Experimental Issues
Problem: Inconsistent Metabolite Production in a Microbial Co-culture
- Potential Cause 1: Variability in the growth of the metabolite-producing strain.
- Solution: Standardize the inoculum preparation and growth conditions. Use spectrophotometry to ensure consistent starting optical density (OD). Monitor the growth of the producer strain separately to confirm its viability and metabolic activity.
- Potential Cause 2: Depletion of the necessary dietary precursor (e.g., fiber for SCFAs, tryptophan for indoles).
- Solution: Supplement the culture medium with an excess of the required precursor. Take regular samples to measure precursor concentration over time.
- Potential Cause 3: Metabolite degradation by other members of the microbial community.
- Solution: Profile the metabolite concentration throughout the experiment using techniques like Liquid Chromatography-Mass Spectrometry (LC-MS). This will help identify if the metabolite is being produced but then rapidly consumed or broken down.
Problem: Failure to Transmit a Phenotype via Fecal Microbiota Transplant (FMT) in a Gnotobiotic Mouse Model
- Potential Cause 1: Incomplete or unsuccessful microbial engraftment in the recipient.
- Solution: Verify engraftment by 16S rRNA sequencing of fecal samples from donors and recipients pre- and post-FMT. Ensure recipients are properly germ-free before the procedure.
- Potential Cause 2: Host factors (e.g., genotype, diet, age) are overriding the microbial influence.
- Solution: Tightly control the host environment, including using inbred mouse strains and providing a standardized diet. The study by [21] successfully used C57BL/6NTac mice and controlled conditions to demonstrate transmission of locomotion behavior.
- Potential Cause 3: The phenotype is dependent on a specific microbial consortium that is not being transferred intact.
- Solution: Consider using a defined microbial community (synthetic consortium) instead of a complex fecal slurry to reduce variability and identify key effector strains, as the enrichment of Lactobacillus was key to transmitting the behavior in the aforementioned study [21].
Quantitative Data on Key Microbial Metabolites
Table 1: Key Immunomodulatory Gut Microbial Metabolites and Their Functions [19] [20].
| Metabolite Class | Examples | Primary Microbial Producers | Key Receptors/Pathways | Immunomodulatory Role & Selective Potential |
|---|---|---|---|---|
| Short-Chain Fatty Acids (SCFAs) | Acetate, Propionate, Butyrate | Bacteroides, Bifidobacterium, Faecalibacterium prausnitzii, Clostridium clusters | GPR41, GPR43, GPR109A, HDAC inhibition | Promote Treg differentiation; inhibit HDAC; modulate cytokine production; can suppress specific pathogens by lowering pH. |
| Secondary Bile Acids (BAs) | Deoxycholic Acid (DCA), Lithocholic Acid (LCA) | Bacteroides, Clostridium, Eubacterium, Lactobacillus | FXR, TGR5 (GPBAR1) | Regulate Th17/Treg balance; DCA can negatively impact CD8+ T cell function [19]; exhibit direct antimicrobial activity against susceptible bacteria. |
| Tryptophan Derivatives | Indole-3-propionic acid (IPA), Indole, Indolealdehyde | Clostridium sporogenes, Bifidobacterium, Lactobacillus | Aryl Hydrocarbon Receptor (AhR) | Enhance mucosal defense via IL-22; regulate Th17/Treg balance; induce apoptosis in Th1/Th17 cells [19]. |
| Polyamines | Spermidine, Spermine, Putrescine | Wide range, including Bifidobacterium, Bacteroides | Influences autophagy, mitochondrial function | Essential for T cell differentiation; promote Treg and suppress Th17 responses [19]. |
Table 2: Concentration Ranges and Experimental Considerations for Microbial Metabolites.
| Metabolite | Typical Colonic Concentration | Reported Experimental Doses (In Vitro/Vivo) | Stability & Handling |
|---|---|---|---|
| Butyrate | 20-70 mM [20] | 0.1 - 5 mM (cell culture) [19] | Sodium salt is stable. Store at room temperature. Soluble in water. |
| Propionate | 20-70 mM [20] | 0.1 - 5 mM (cell culture) [19] | Sodium salt is stable. Store at room temperature. Soluble in water. |
| Deoxycholic Acid (DCA) | Varies with diet | 50 - 500 µM (cell culture) [19] | Light-sensitive. Store at -20°C. Soluble in DMSO or ethanol. |
| Indole-3-propionic acid | µM range | 10 - 100 µM (cell culture) [20] | Store at -20°C. Soluble in DMSO. |
Detailed Experimental Protocols
Protocol: Assessing Selective Inhibition Using Microbial Metabolites in Vitro
Objective: To determine the minimum inhibitory concentration (MIC) of a gut microbial metabolite (e.g., a secondary bile acid) against a target bacterial pathogen.
Materials:
- Test Compound: e.g., Deoxycholic acid (DCA) sodium salt.
- Target Microbe: e.g., Clostridium difficile or other pathogen of interest.
- Growth Medium: Appropriate broth medium (e.g., BHI, YCFA).
- Equipment: Anaerobic chamber, 96-well flat-bottom plates, multichannel pipettes, spectrophotometer (plate reader).
Methodology:
- Preparation of Metabolite Stock Solution: Prepare a high-concentration stock solution of DCA in sterile water or DMSO. Filter sterilize (0.2 µm filter). If using DMSO, ensure the final concentration in the assay is ≤1% (v/v).
- Broth Microdilution in 96-well Plate:
- Dispense 100 µL of growth medium into all wells of a 96-well plate.
- Add 100 µL of the metabolite stock solution to the first well (e.g., well A1). Mix thoroughly. This is the first serial two-fold dilution.
- Serially dilute the metabolite across the plate by transferring 100 µL from well to well, resulting in a dilution series (e.g., from 1000 µM to ~2 µM). Discard 100 µL from the last well.
- Prepare a growth control well (medium + inoculum, no metabolite) and a sterility control well (medium only).
- Inoculation:
- Prepare a standardized inoculum of the target microbe in log-phase growth (e.g., 0.5 McFarland standard, ~1-5 x 10^8 CFU/mL).
- Dilute the inoculum in fresh medium to achieve a final concentration of ~5 x 10^5 CFU/mL in each well.
- Add 100 µL of the diluted inoculum to all test and growth control wells. Add 100 µL of sterile medium to the sterility control well. The final volume in each well is 200 µL.
- Incubation and Measurement:
- Seal the plate with a breathable membrane or lid and incubate under appropriate conditions (temperature, anaerobic) for 16-24 hours.
- Measure the optical density (OD) at 600 nm using a plate reader.
- Data Analysis:
- The MIC is defined as the lowest concentration of the metabolite that completely inhibits visible growth (OD ~= OD of sterility control).
Protocol: Phenotype Transfer via Fecal Microbiota Transplantation (FMT)
Objective: To transfer a microbiome-driven phenotype (e.g., reduced locomotion) to germ-free recipient mice, as described in [21].
Materials:
- Donor Mice: Mice exhibiting the desired phenotype (e.g., low activity).
- Recipient Mice: Age-matched, male germ-free mice (e.g., C57BL/6NTac strain).
- Equipment: Anaerobic workstation, homogenizer, cages with autoclaved bedding and food, behavioral tracking system (e.g., open field, automated cage system).
Methodology:
- Donor Fecal Sample Collection: Fresh fecal pellets are collected from donor mice directly into pre-reduced, sterile phosphate-buffered saline (PBS) within an anaerobic chamber to preserve obligate anaerobes.
- Inoculum Preparation: Fecal material is homogenized in PBS (e.g., 1 pellet per 1 mL). The slurry is filtered through a sterile mesh to remove large particles. The inoculum should be prepared fresh and used immediately.
- Recipient Inoculation: Germ-free recipient mice are orally gavaged with a defined volume (e.g., 200 µL) of the fecal slurry. Control recipients receive slurry from control donors (e.g., high-activity or random selection).
- Phenotype Monitoring:
- House recipients in sterile, flexible film isolators or positive pressure ventilated cages to maintain sterility post-inoculation.
- Allow for stable microbial engraftment (typically 2-3 weeks).
- Assess the target phenotype (e.g., distance traveled, total activity) using standardized behavioral assays. The study in [21] measured "distance traveled" after 24 hours in an automated cage system at 5-6 weeks of age.
- Confirmation of Engraftment: Collect fecal samples from recipients pre- and post-FMT. Perform 16S rRNA gene sequencing to confirm that the donor microbial community has successfully colonized the recipients.
Signaling Pathway and Experimental Workflow Diagrams
Diagram: Immunomodulatory Mechanisms of SCFAs
Diagram: Workflow for One-Sided Host-Microbiome Selection
The Scientist's Toolkit: Research Reagent Solutions
Table 3: Essential Research Reagents for Studying Microbial Metabolites.
| Reagent / Material | Function / Application | Example & Notes |
|---|---|---|
| Germ-Free Mice | In vivo model to study causality of microbiome and metabolite effects without confounding microbial influences. | C57BL/6NTac strain used in phenotype transfer studies [21]. |
| Anaerobic Chamber | Provides an oxygen-free environment for handling obligate anaerobic gut bacteria and preparing fecal inocula to maintain microbial viability. | Essential for culturing many SCFA-producing bacteria like Faecalibacterium prausnitzii. |
| Targeted Mass Spectrometry | Quantifying specific metabolite concentrations in complex samples like fecal content, serum, or culture media. | LC-MS/MS for precise measurement of SCFAs, bile acids, and tryptophan metabolites. |
| 16S rRNA Gene Sequencing | Profiling microbial community composition to assess engraftment after FMT or changes due to metabolite treatment. | Standard method for confirming microbiome changes in animal models [21]. |
| G-Protein Coupled Receptor Assays | Mechanistic studies to validate direct binding and activation of host pathways by metabolites. | Cell-based assays for GPR41, GPR43, TGR5, etc. |
| Engineered Probiotics | Tool for delivering specific metabolites in situ. Bacteria engineered to overproduce a metabolite of interest. | e.g., Lactobacillus engineered to produce indole derivatives [20]. |
| Photoimmuno-Antimicrobial Conjugates | A novel targeted antimicrobial strategy using antibody-IR700 conjugates and near-infrared light to selectively eliminate pathogens [22]. | Effective against bacterial, fungal, and viral pathogens, including drug-resistant strains, without disrupting commensals. |
A Practical Pipeline: Screening, Cultivation, and Application of Selective Agents
The relentless emergence of antimicrobial resistance (AMR) presents a formidable global challenge, making the discovery of novel antimicrobial agents more critical than ever [23]. Screening methodologies form the backbone of this discovery process, providing crucial insights into the effectiveness and mechanisms of action of potential antimicrobial compounds [23]. These assays have evolved from simple, traditional techniques to sophisticated, high-throughput technologies.
Traditional agar-based methods, such as disk-diffusion and well-diffusion, are valued for their simplicity and low cost, providing a preliminary assessment of antimicrobial activity [23] [24]. In contrast, modern techniques like flow cytometry and bioluminescence assays offer higher sensitivity, reproducibility, and deeper insights into the impact of antimicrobials on cellular integrity and specific cellular functions [23]. The choice of screening method is pivotal, as it must align with the research goals, whether for initial broad screening or detailed mechanistic studies, to efficiently identify promising antimicrobial candidates in the fight against infectious diseases [23].
This technical support center is designed within the context of research on selective inhibition agents for target microbe isolation. It provides detailed troubleshooting guides, FAQs, and protocols to address the specific experimental challenges faced by researchers and drug development professionals utilizing these technologies.
Key Methodologies and Comparative Analysis
The following table summarizes the core principles, advantages, and limitations of the primary antimicrobial screening methodologies in use today.
| Methodology | Core Principle | Key Advantages | Primary Limitations |
|---|---|---|---|
| Agar Diffusion (Disk/Well) [23] [24] | Measurement of microbial growth inhibition zones around a compound source on agar. | Simple, low-cost, ability to test many compounds/microbes. | Qualitative/semi-quantitative, cannot distinguish bactericidal vs. bacteriostatic effects. |
| Broth Dilution [23] | Determination of Minimum Inhibitory Concentration (MIC) via compound serial dilution in liquid media. | Provides quantitative MIC data. | Time-consuming, labor-intensive. |
| Time-Kill Kinetics [23] | Evaluation of the rate and extent of microbial killing over time. | Distinguishes bactericidal from bacteriostatic activity. | Complex protocol, requires multiple time-point sampling. |
| Flow Cytometry [23] | Multi-parameter analysis of single cells using light scattering and fluorescence. | Rapid, provides insights into mechanism of action on cellular integrity. | Higher cost, complex data analysis, requires expertise. |
| Bioluminescence [23] [25] [26] | Quantification of microbial viability or specific enzyme activity via light emission. | Highly sensitive, rapid, amenable to high-throughput screening (HTS). | Sensitivity to interfering compounds, requires specialized reagents. |
Advanced and Emerging Screening Technologies
Beyond the common methods, the field is rapidly advancing with technologies that offer greater depth of information or screening efficiency.
- Bioluminescence Inhibition Assays: These assays utilize bioluminescent proteins, such as aequorin or NanoLuc luciferase, as both recognition and signal-generating elements [25] [26] [27]. The core principle is that the binding of an inhibitory compound to the photoprotein can cause a dose-dependent decrease in bioluminescence, which can be quantified to detect the inhibitor [25]. This provides a rapid, sensitive, and cost-effective method for screening compounds that target specific microbial pathways [25].
- AI-Enhanced Screening: Artificial Intelligence (AI) and Machine Learning (ML) are now being deployed to accelerate antimicrobial discovery. These technologies can process large datasets to predict interactions between active compounds and microbial targets, and to design novel antimicrobial peptides (AMPs) with desired properties, significantly streamlining the initial discovery pipeline [28].
- Impedance Analysis & Bioautography: Other advanced techniques include impedance analysis, which measures electrical changes in media to monitor microbial growth, and bioautography, which couples thin-layer chromatography (TLC) with a biological activity assay to locate active compounds in a complex mixture [23].
Troubleshooting Guides
Flow Cytometry Troubleshooting
Flow cytometry is a powerful tool for assessing antimicrobial mechanisms, but it can be prone to specific technical issues.
| Problem | Possible Causes | Recommendations |
|---|---|---|
| Weak or No Signal | • Low target expression.• Inadequate fixation/permeabilization.• Dim fluorochrome paired with low-density target.• Incorrect laser/PMT settings. | • Optimize treatment for target induction.• Follow standardized fixation/permeabilization protocols (e.g., ice-cold methanol added drop-wise while vortexing) [29].• Use brightest fluorochrome (e.g., PE) for lowest density targets [29].• Verify instrument settings match fluorochrome specs. |
| High Background/Non-specific Staining | • Fc receptor binding on immune cells.• Too much antibody.• Presence of dead cells.• High autofluorescence. | • Block with BSA, Fc receptor blockers, or normal serum [30] [29].• Titrate antibodies to optimal concentration.• Use viability dye to gate out dead cells.• Use red-shifted fluorochromes (e.g., APC) or brighter dyes in autofluorescent channels [29]. |
| Poor Cell Cycle Resolution | • High flow rate on cytometer.• Insufficient staining with DNA dye. | • Run samples at the lowest flow rate setting [29].• Resuspend cell pellet directly in PI/RNase solution and incubate sufficiently [29]. |
Bioluminescence Assay Troubleshooting
Bioluminescence assays are highly sensitive but can be affected by reagent stability and environmental factors.
| Problem | Possible Causes | Recommendations |
|---|---|---|
| Low Signal Intensity | • Luciferase enzyme inhibition or degradation.• Substrate depletion or instability.• Incorrect cation cofactors (e.g., Mg²⁺, Ca²⁺). | • Ensure purified enzyme is active and stored correctly.• Use fresh, recommended substrates (e.g., D-luciferin, coelenterazine) [27].• Include necessary cofactors in reaction buffer (e.g., ATP/Mg²⁺ for firefly luciferase) [27]. |
| High Background Luminescence | • Contamination with luciferase-expressing microbes.• Auto-luminescence of test compounds.• Substrate contamination. | • Use aseptic technique.• Run control wells with compound alone (no enzyme) to check for interference.• Use high-purity substrates. |
| Inconsistent Results | • Inconsistent reagent dispensing.• Temperature fluctuations during reading.• Tandem dye degradation. | • Use automated dispensers for reagents.• Allow plate to equilibrate to instrument temperature.• Include tandem stabilizer in staining and storage buffers [30]. |
Frequently Asked Questions (FAQs)
Q1: When should I use agar diffusion versus broth dilution methods? A1: Use agar diffusion for initial, low-cost qualitative screening of a large number of compounds or microbial isolates to quickly identify those with inhibitory activity [23] [24]. Opt for broth dilution when you need a quantitative result, specifically the Minimum Inhibitory Concentration (MIC), which is crucial for determining the potency of a promising compound [23].
Q2: How can flow cytometry provide information on the mechanism of antimicrobial action? A2: Flow cytometry can distinguish between different mechanisms of action by using fluorescent probes. For example, probes that assess membrane integrity (e.g., propidium iodide), metabolic activity, or mitochondrial membrane potential can be used simultaneously. The resulting multi-parameter data can indicate whether a compound is causing membrane disruption, metabolic shutdown, or apoptosis, providing a deeper understanding than growth inhibition alone [23].
Q3: What are the key advantages of bioluminescence-based screening assays? A3: The primary advantages are sensitivity, speed, and adaptability to high-throughput screening (HTS). These assays often have a wide dynamic range with very low background, allowing for the detection of subtle changes in viability or specific enzymatic activity [23] [26]. Reactions are typically rapid, and the format is easily miniaturized for automated screening of large compound libraries [25].
Q4: My flow cytometry data shows high background in the negative control. What steps should I take? A4: High background is often caused by non-specific antibody binding. First, ensure you are blocking your cells with an appropriate reagent like BSA, normal serum, or a commercial Fc receptor block, especially for immune cells [30] [29]. Second, titrate your antibodies to use the optimal concentration. Third, incorporate a viability dye to gate out dead cells, which often bind antibodies non-specifically. Finally, perform additional wash steps to remove unbound antibody [29].
Q5: Can AI truly accelerate the discovery of new antimicrobials? A5: Yes, AI and machine learning are proving to be transformative. They can rapidly analyze vast chemical and genomic datasets to predict new antimicrobial peptides, optimize existing compound structures, and identify potential targets [28]. This computational pre-screening narrows down the candidate pool, making the subsequent experimental validation in the lab far more efficient and targeted [28].
Essential Experimental Protocols
Principle: To evaluate the antimicrobial activity of a compound by measuring the zone of growth inhibition around a disk impregnated with the test substance.
Materials:
- Mueller-Hinton Agar (MHA) plates (or other appropriate media)
- Sterile filter paper discs (6 mm diameter)
- Standardized microbial inoculum (e.g., 0.5 McFarland standard)
- Test antimicrobial compound and appropriate controls (e.g., solvent, known antibiotic)
Procedure:
- Prepare a standardized bacterial suspension (e.g., equivalent to 0.5 McFarland standard, ~1.5 x 10⁸ CFU/mL).
- Evenly swab the entire surface of the MHA plate with the bacterial inoculum.
- Aseptically place the sterile paper discs onto the inoculated agar surface.
- Apply a defined volume (typically 10-20 µL) of the test compound onto separate discs. Include positive and negative control discs.
- Allow the discs to dry and then incubate the plates at the appropriate temperature (e.g., 37°C for most human pathogens) for 16-24 hours.
- Measure the diameter of the zones of inhibition (including the disc) in millimeters.
Principle: To detect specific surface markers on cells while minimizing non-specific antibody binding through a optimized blocking step.
Materials:
- Cells of interest (e.g., mammalian immune cells)
- FACS buffer (e.g., PBS with 1-2% FBS)
- Blocking solution (e.g., containing rat serum, mouse serum, and tandem stabilizer) [30]
- Fluorescently-conjugated antibodies
- V-bottom 96-well plates
- Centrifuge and flow cytometer
Procedure:
- Prepare Cells: Dispense cells into a V-bottom 96-well plate. Centrifuge at 300 × g for 5 minutes and remove supernatant.
- Block: Resuspend the cell pellet in 20 µL of blocking solution. Incubate for 15 minutes at room temperature in the dark [30].
- Stain: Prepare a surface staining master mix in FACS buffer containing the fluorescent antibodies and Brilliant Stain Buffer (if using polymer dyes). Add 100 µL of this mix directly to the cells without washing away the blocking solution. Mix by pipetting.
- Incubate: Incubate for 1 hour at room temperature in the dark.
- Wash: Add 120 µL of FACS buffer, centrifuge, and discard supernatant. Repeat this wash step with 200 µL of FACS buffer.
- Resuspend and Acquire: Resuspend the final cell pellet in FACS buffer and acquire data on a flow cytometer.
Principle: To detect inhibitors of a specific bioluminescent protein (e.g., aequorin) by measuring a dose-dependent decrease in light emission.
Materials:
- Purified bioluminescent protein (e.g., Aequorin)
- Required cofactors (e.g., Ca²⁺ for aequorin) and substrate (e.g., coelenterazine)
- Test compounds in a concentration series
- White, opaque multi-well plates
- Luminometer
Procedure:
- Reconstitute Protein: Activate purified aequorin by incubating with coelenterazine to form the functional holo-protein.
- Dispense Reagents: In a white 96-well plate, mix a fixed concentration of the test compound with a constant amount of the functional aequorin.
- Initiate Reaction: Trigger the bioluminescence reaction by injecting a solution containing calcium ions.
- Measure Luminescence: Immediately measure the peak luminescence or integrated light output over a short period (seconds) using a luminometer.
- Analyze Data: Plot the relative light units (RLU) against the compound concentration. A decrease in RLU compared to the no-inhibitor control indicates inhibition.
Workflow Visualization
Agar Diffusion Assay Workflow
Bioluminescence Inhibition Assay Workflow
Research Reagent Solutions
This table details key reagents essential for successfully conducting the featured modern screening methodologies.
| Reagent / Material | Primary Function | Application Notes |
|---|---|---|
| Brilliant Stain Buffer [30] | Prevents dye-dye interactions between conjugated antibodies in polychromatic flow cytometry. | Critical for panels using SIRIGEN "Brilliant" or "Super Bright" polymer dyes to ensure accurate signal detection [30]. |
| Fc Receptor Blocking Reagent [30] [29] | Reduces non-specific antibody binding to Fc receptors on immune cells (e.g., monocytes). | Significantly lowers background staining in flow cytometry. Can be normal serum or commercial blocking reagents. |
| Tandem Stabilizer [30] | Prevents the breakdown of tandem fluorophores, which can cause erroneous signal detection. | Should be included in staining buffers and sample storage buffers for flow cytometry to maintain signal integrity. |
| Coelenterazine [25] [27] | Substrate for coelenterazine-dependent bioluminescent systems (e.g., Aequorin, Gaussia, NanoLuc). | Light-sensitive and can be unstable; requires proper storage and handling. Different analogs offer varying emission properties and permeability. |
| D-Luciferin [27] | Substrate for D-luciferin-dependent luciferases (e.g., Firefly, Click Beetle). | Requires ATP and Mg²⁺ as cofactors. Used in assays for viability, metabolism, and reporter gene expression. |
| Viability Dye (e.g., PI, 7-AAD) [29] | Distinguishes live from dead cells based on membrane integrity. | Essential for gating out dead cells in flow cytometry to reduce non-specific background and improve data quality. |
| Aminoluciferin (AML) Conjugates [26] | Acts as a dark substrate for luciferase; light is emitted upon cleavage. | Used in protease activity assays (e.g., DUB-Glo). Conjugation to full-length proteins (e.g., Ub-AML) increases specificity versus short peptide substrates. |
Technical Support Center
Troubleshooting Guides
Problem: Poor or No Growth of Target Fastidious Anaerobe
| Possible Cause | Recommended Solution |
|---|---|
| Oxygen Exposure | Use specialized anaerobic transport systems (e.g., Anaerobic Transport Medium) for specimen collection; never use swabs, opt for tissue biopsies or aspirates [31]. |
| Improper Storage of Media | Store dehydrated media in a cool, dry environment; heat and moisture can degrade nutrients. Store prepared plates in conditions that maintain product quality [32]. |
| Suboptimal Growth Conditions | Ensure the use of a rich, specialized base medium like Fastidious Anaerobe Agar (FAA). Provide appropriate temperature and atmospheric conditions for the specific anaerobe [33] [34]. |
| Incorrect Incubation Parameters | For anaerobic growth, use an anaerobic indicator and validate incubator temperatures routinely. Incubate plates in stacks of four or less to ensure rapid, even warming [35]. |
Problem: Contaminated Cultures or Overgrowth of Competing Flora
| Possible Cause | Recommended Solution |
|---|---|
| Faulty Media Sterilization | Follow stated sterilization directions precisely; use autoclaves, not microwaves, to prevent nutrient destruction or toxin development [32]. |
| Use of Expired Media | Never use expired collection media or agars; components like reducing agents and selective agents degrade, leading to false results [31]. |
| Leaking Specimen Container | Ensure transport containers (e.g., Lukens traps) are securely closed with sterile transport caps, not tubing, to prevent leaks and contamination [31]. |
| Insufficient Selective Agents | Confirm that selective additives (e.g., antibiotics) are added correctly—after sterilization if heat-labile—and at the proper concentration [32] [36]. |
Frequently Asked Questions (FAQs)
Q1: What is the recommended medium and method for culturing a broad spectrum of anaerobic bacteria from fecal samples? A1: Fastidious Anaerobe Agar (FAA-HB) is highly recommended. A 2025 study demonstrated that FAA-HB exhibited excellent culture performance for thirty-six anaerobic species from fecal samples, with most EUCAST candidate-species showing confluent growth within 16-20 hours. It also performed well for antimicrobial susceptibility testing (AST) [33] [34].
Q2: Why is my target microbe growing poorly on selective media but well on non-selective media? A2: This is expected behavior. Selective media contain inhibitors (like crystal violet, bile salts, or antibiotics) that create a stressful environment to suppress competing flora. While they allow the target to grow, it will not be as luxuriantly as on a nutrient-rich, non-selective medium. There is no requirement for a specific percent recovery on selective versus non-selective agar [35].
Q3: How should I handle and transport samples for anaerobic culture? A3: Proper handling is critical.
- Collection: Use aspirates or tissue biopsies; swabs are not appropriate [31].
- Transport: Place the specimen in an Anaerobic Transport Medium (ATM), which is designed to exclude oxygen [31].
- Transport Conditions: Keep specimens at room temperature during transport; oxygen diffuses more easily into cold liquid medium. Deliver to the lab within 3 hours [31].
Q4: What are some best practices for preparing culture media to ensure optimal growth? A4:
- Storage: Protect dehydrated media from extreme temperatures and moisture, which can destroy nutrients [32].
- Preparation: Use trained staff and the correct labware (e.g., a flask of appropriate size) for accurate measuring and mixing [32].
- Sterilization: Follow manufacturer directions for autoclaving to avoid damaging heat-sensitive components [32].
- Additives: Add supplements like antibiotics after sterilization if they are heat-labile [32].
Experimental Protocol: Evaluating Culture Media Performance for Fastidious Anaerobes
Objective: To assess the growth promotion properties of a selective or enriched medium (e.g., Fastidious Anaerobe Agar) for specific fastidious anaerobic bacteria.
Methodology:
- Inoculum Preparation: Use a standardized inoculum to deliver 10-100 Colony Forming Units (CFU) per plate [35]. Confirm the viable count of the inoculum by parallel plating on a non-selective agar like Tryptic Soy Agar (TSA) [35].
- Plating: Inoculate the test batch of the selective/enriched medium and a previous, approved batch of the same medium for comparison. Use the spread plate or pour plate method.
- Incubation:
- Analysis: After incubation, count the colonies on each plate. The growth on the new batch of media should be "comparable" to the previous batch. The USP states that the strict "factor of two" rule does not necessarily apply to selective media [35].
Workflow and Conceptual Diagrams
The Scientist's Toolkit: Research Reagent Solutions
| Item | Function/Benefit |
|---|---|
| Fastidious Anaerobe Agar (FAA-HB) | A highly effective solid medium supporting the rapid growth (16-20 hours) of a wide spectrum of anaerobic bacteria from clinical and environmental samples [33] [34]. |
| Anaerobic Transport Medium (ATM) | A specialized collection medium designed to exclude oxygen and preserve the viability of fastidious anaerobic bacteria during specimen transport from clinic to lab [31]. |
| Selective Media (e.g., MacConkey Agar) | Contains inhibitors (e.g., crystal violet, bile salts) that suppress the growth of Gram-positive bacteria, thereby selecting for specific Gram-negative organisms [36]. |
| Differential Media (e.g., Blood Agar) | Allows differentiation of microorganisms based on their biochemical reactions, such as hemolysis patterns on blood agar or color changes on EMB agar from fermentation [36]. |
| EZ-Accu Shot / EZ-CFU | Commercially prepared, standardized microbial inoculants that deliver a precise CFU range (e.g., 10-100 CFU), saving hands-on time and improving Growth Promotion Test reproducibility [35]. |
This technical support center addresses key challenges in developing antibiotics that selectively target pathogens while preserving the beneficial gut microbiome. This approach is critical for treating infections without causing dysbiosis—an imbalance in gut microbiota linked to secondary infections and other long-term health issues [37]. Below, you will find troubleshooting guides, FAQs, and detailed protocols to support your research on selective inhibition agents.
FAQs and Troubleshooting Guides
FAQ 1: What are pathogen-selective antibiotics and why are they important?
Answer: Pathogen-selective antibiotics are designed to target and kill specific pathogenic bacteria without harming commensal (beneficial) gut bacteria. Traditional broad-spectrum antibiotics disrupt the gut microbiome, leading to dysbiosis. This can result in secondary infections like Clostridioides difficile, inflammatory bowel disease (IBD), and other long-term health problems [37]. Selective antibiotics aim to maximize treatment efficacy while minimizing these collateral detrimental effects on the host's microbiome.
FAQ 2: My bacterial cultures are being contaminated by fast-growing organisms likeE. coliafter sample collection. How can I prevent this?
Answer: The overgrowth of organisms like E. coli is a classic sign of inadequate sample preservation. To prevent this bias:
- Preserve Immediately: Do not delay sample stabilization. Even short delays can allow fast-growing species to bloom and consume others, severely skewing the microbial community data [38].
- Use Chemical Preservatives: Relying on freezing alone can be insufficient, as freeze-thaw cycles lyse cells (especially Gram-negative ones) and reactivate degradative enzymes upon thawing. Use room-temperature chemical preservatives (e.g., DNA/RNA Shield) that instantly inactivate nucleases and stop all biological activity at the point of collection [38].
- Avoid Freeze-Thaw Cycles: If you must freeze samples, ensure it is at -80°C and avoid repeated thawing, as damage is cumulative and selectively affects more fragile microbes [38].
FAQ 3: I am working with a Gram-negative pathogen. Why is my experimental compound failing to lyse the cells for analysis?
Answer: Gram-negative bacteria can be difficult to lyse due to their complex cell envelope.
- Modify the Growth Medium: Bacteria grown in rich media (high glucose) are particularly resistant to lysis. Try reducing the glucose concentration in your culture medium [39].
- Use Enhancing Agents: For efficient lysis of Gram-negative bacteria, add lysozyme to your lysis reagent. For some over-expressed proteins, this may not be needed, but it is generally recommended [39].
- Pre-treatment: Freezing the bacterial cells before extraction can also make them more susceptible to lysis [39].
Experimental Protocols & Data
Protocol 1: In Vitro Assessment of Selective Antibacterial Activity
This protocol outlines how to evaluate a compound's ability to selectively target a pathogen while sparing commensal bacteria.
- 1. Culturing: Grow your target pathogen (e.g., a multidrug-resistant Gram-negative strain) and selected commensal bacteria (e.g., Bacteroides thetaiotaomicron) in appropriate media and conditions [40].
- 2. Compound Exposure: Treat the cultures with your experimental compound at a range of concentrations. Include controls (vehicle-only) for both pathogen and commensals.
- 3. Viability Assessment: After a set incubation period, determine the Minimum Inhibitory Concentration (MIC) for both the pathogen and the commensal strains. Use methods like broth microdilution or plating for colony-forming unit (CFU) counts [40].
- 4. Selectivity Calculation: A selective compound will show a significantly lower MIC against the pathogen compared to the commensal strains. The selectivity index can be calculated as (MICcommensal / MICpathogen).
Protocol 2: Evaluating Microbiome Sparing in a Mouse Model
This in vivo protocol tests the impact of an antibiotic on the gut microbiome.
- 1. Animal Grouping: House mice in controlled conditions and divide them into groups: one treated with your selective antibiotic, one with a broad-spectrum antibiotic (positive control), and one with a vehicle (negative control) [40].
- 2. Dosing: Administer the compounds to the mice orally or via injection for a set duration.
- 3. Fecal Sample Collection: Collect fecal samples at baseline, during treatment, and post-treatment. Crucially, preserve samples immediately in a stabilizing solution like DNA/RNA Shield to prevent microbial community shifts after collection [38].
- 4. Microbiome Analysis: Extract genomic DNA from the preserved samples and perform 16S rRNA gene sequencing or shotgun metagenomics to analyze the composition and diversity of the gut microbiota [40].
- 5. Pathogen Challenge (Optional): To demonstrate functional protection, challenge the mice with a pathogen like Clostridioides difficile after the antibiotic course and monitor for infection [40].
Quantitative Data on Microbiota-Sparing Antibacterial Agents
The table below summarizes key experimental data for emerging selective antibacterial agents, demonstrating their potential to spare the gut microbiome.
Table 1: Overview of Microbiota-Sparing Antibacterial Agents [37]
| Antibacterial Agent | Target / Mechanism of Action | Selectivity Towards Pathogen | Gut Microbiota Sparing Property | Clinical Status |
|---|---|---|---|---|
| Lolamicin | Lipoprotein transport system (LolCDE) | >130 multidrug-resistant clinical Gram-negative isolates [40] | Spared gut microbiome in mice; prevented secondary C. difficile infection [40] | Preclinical |
| Hygromycin A | Pathogen-specific BmpD transporter | Borrelia burgdorferi | Caused only mild microbiota changes, promoted beneficial bacteria [37] | Phase 1 |
| Ridinilazole | Binds DNA minor groove; interferes with cell division | Clostridium difficile | Minimal disruption, preserved key microbiota for bile acid metabolism [37] | Phase 3 |
| Cadazolid | pH-dependent cellular uptake | Clostridium difficile | Spared Gram-negative anaerobes like Bacteroides thetaiotaomicron [37] | Discontinued after Phase 3 |
| Ribaxamase | β-Lactamase enzyme degrades antibiotics in GI tract | N/A (protects microbiome from antibiotics) | Safeguarded gut microbiota from ceftriaxone-induced damage [37] | Phase 1b/2a |
Mechanisms and Targets for Selective Antibiotics
The table below lists validated and emerging bacterial targets for developing novel antibacterial agents.
Table 2: Promising Targets for Novel Antibacterial Agents [41]
| Target Category | Specific Target | Rationale for Selectivity |
|---|---|---|
| Cell Wall & Membrane | Lipoprotein Transport (LolCDE) | Essential for viability of Gram-negative bacteria; low sequence homology in commensals like Bacteroides allows for selective targeting [40]. |
| Cell Wall & Membrane | Peptidoglycan Biosynthesis | Preferred target as mammalian cells lack a peptidoglycan wall structure [41]. |
| Protein Synthesis | Methionyl-tRNA synthetase (MetRS) | Differences in bacterial vs. human enzyme structures can be exploited for selective inhibition [37]. |
| DNA Replication | DNA Polymerase IIIC | A bacterial-specific enzyme, making it an ideal target for selective antibiotics [37]. |
| Metabolic Pathways | Dihydrofolate Reductase (DHFR) | Can be targeted with adjuvants (e.g., thymine) to create pathogen-selective inhibition [37]. |
Visualization of Workflows and Pathways
Lolamicin Selective Inhibition Mechanism
Microbiome-Sparing Drug Development Workflow
The Scientist's Toolkit: Research Reagent Solutions
Table 3: Essential Materials for Selective Agent and Microbiome Research
| Item | Function in Research | Key Considerations |
|---|---|---|
| DNA/RNA Shield or similar | Chemical preservative that instantly stabilizes nucleic acids in samples (e.g., feces) at room temperature. | Inactivates nucleases and prevents microbial growth; crucial for preserving an accurate snapshot of the microbiome at collection [38]. |
| Glycerol (15-20% v/v) | Cryoprotectant for long-term storage of bacterial and fungal strains at -80°C. | Glycerol stocks are considered good indefinitely if freeze-thaw cycles are avoided [39]. |
| Selective Antibacterial Agents (e.g., Lolamicin) | Tool compounds for validating selective inhibition in vitro and in vivo. | Key for proof-of-concept studies demonstrating microbiome sparing [40]. |
| Lysozyme | Enzyme used to break down the peptidoglycan layer of bacterial cell walls, aiding in lysis. | Essential for efficient extraction from Gram-positive bacteria; often improves lysis of Gram-negative strains as well [39]. |
| B-PER Reagent or similar | Bacterial Protein Extraction Reagent for lysing bacterial cells to isolate proteins or nucleic acids. | More efficient for Gram-negative bacteria but can be used for some Gram-positives, especially with lysozyme addition [39]. |
This technical support guide provides troubleshooting and methodological support for researchers using metagenomics to identify Biosynthetic Gene Clusters (BGCs), particularly within the context of developing selective inhibition agents for target microbe isolation. The content addresses common computational and experimental challenges in profiling microbial communities for bioactive compound discovery.
Frequently Asked Questions (FAQs)
Q1: What is the advantage of a taxonomy-guided approach for BGC identification over direct read-mapping methods?
A taxonomy-guided approach, as implemented in tools like TaxiBGC, first identifies the microbial species present in a metagenome before predicting BGCs. This method significantly improves predictive performance. In benchmarks, this approach achieved a mean positive predictive value (PPV) score of 0.80, compared to 0.41 for methods that directly map sequencing reads onto BGC genes. The F1 score, a measure of overall accuracy, was also higher (0.56 vs. 0.49) [42]. This strategy reduces false positives and allows researchers to trace BGCs back to their likely taxonomic origins.
Q2: My metagenomic assembly is not reconstructing BGCs effectively. What strategies can improve this?
Poor BGC reconstruction often stems from suboptimal assembly. The choice of assembler and parameters is critical:
- Assembler Selection: For single-sample projects,
metaSPAdesproduces contigs of superior fidelity, albeit at greater computational cost. For multiple samples,MEGAHIToffers faster co-assembly [43]. - Parameter Optimization: K-mer length exerts a determinant effect on assembly. Use tools like
KmerGenieto infer the optimal k-mer value for your dataset [43]. - Performance Metrics: A key indicator of successful assembly is the N50 value and the read-mapping rate. One study reported that an optimized assembly pipeline tripled the N50 value and achieved a read-mapping rate of 55.8%, a four-fold enhancement over conventional methods [43].
Q3: How can I isolate rare Actinomycetes from complex environmental samples for BGC discovery?
Isolating rare Actinomycetes requires selective techniques to suppress fast-growing bacteria:
- Sample Pretreatment: Subject environmental samples (e.g., soil, cave sediments) to harsh chemical, heat, or drought conditions. Actinomycete spores are highly resistant, allowing them to germinate under conditions that suppress other bacteria [44].
- Selective Media: Use culture media that mimic the oligotrophic and extreme conditions of the source environment (e.g., low-nutrient cave environments) to select for desired microbial traits [44].
- Validation: A study applying these methods successfully cultured 55 Actinomycete-like isolates from a Fijian cave, 19 of which were confirmed Actinomycetes (13 Streptomyces and 6 rare Actinomycetes) [44].
Q4: What is the most efficient method for the functional profiling of a metagenome?
A tiered search strategy, as implemented in HUMAnN2, provides fast and accurate functional profiling.
- Workflow: It first identifies known species, then aligns reads to their pangenomes (a fast nucleotide-level search), and finally performs a translated search on unclassified reads [45].
- Performance: This approach is 3x faster and produces more accurate gene family profiles (89% accuracy) compared to pure translated search strategies (67% accuracy) [45]. It also provides species-resolved functional contributions, which is invaluable for target microbe isolation research.
Troubleshooting Guides
Issue 1: Low Confirmation Rate of Predicted BGCs
Problem: In-silico predicted BGCs are not being confirmed by read-mapping, leading to potential false positives.
Solution:
- Confirm Mapping Thresholds: The final step of a pipeline like TaxiBGC requires mapping sequencing reads to the predicted BGC genes using a predetermined pair of minimum BGC gene presence and BGC coverage thresholds [42]. Re-calibrate these thresholds for your specific dataset if the confirmation rate is low.
- Inspect Read Quality: Re-visit your pre-processing steps. Ensure that adaptor sequences and low-quality bases have been adequately trimmed. Use a tool like
FastQCto visualize read quality, aiming for at least 85% of bases with a Phred score ≥ Q30 [43]. - Check for Host Contamination: In host-associated samples, residual host DNA can drastically reduce microbial signal. Use
Bowtie2orKraken2to align reads to a host reference genome and remove them. One study noted that removing host reads increased detection sensitivity for a pathogen from 50% to 90% [43].
Issue 2: Inability to Determine the Produced Secondary Metabolite
Problem: You have identified a BGC but cannot infer the secondary metabolite (SM) it produces.
Solution:
- Leverage Annotated Databases: Use tools that link BGCs to experimentally characterized SMs. The TaxiBGC reference database, for instance, contains a predefined collection of 390 unique species with their experimentally characterized BGCs and known SMs [42]. This allows for direct inference of the SM product.
- Conduct Advanced Annotation: Perform functional annotation of your assembled contigs or Metagenome-Assembled Genomes (MAGs) using specialized databases. The
antiSMASHtool can detect multiple BGC types (e.g., terpenes, bacteriocins). Additionally,KEGGpathway analysis can identify key biosynthetic pathways like terpenoid and polyketide biosynthesis [46].
Issue 3: Difficulty in Isolating Target Microbes from a Complex Sample
Problem: The microbe of interest is being outcompeted or is not growing under standard laboratory culture conditions.
Solution:
- Employ Selective Media: Incorporate inhibiting agents (e.g., antibiotics) into your culture media to eliminate undesirable bacteria from the microbiota and select for the desired target [9].
- Mimic the Natural Environment: Develop culture media based on a better knowledge of the bacterium's natural environment and nutritional needs. This is particularly crucial for isolating fastidious bacteria that are difficult to culture [9].
- Use Metagenomic Insights: Let the metagenomic data guide your isolation strategy. The taxonomic and functional profile can reveal the metabolic capabilities of your target microbe, allowing you to design a more specific medium. For example, if functional profiling shows an enrichment for certain nutrient transporters, you can tailor your media accordingly [46].
Experimental Protocols & Data Presentation
Protocol 1: Shotgun Metagenomic Sequencing for BGC Prediction from Environmental Samples
This protocol is adapted from a study investigating microbial diversity in hospital and pharmaceutical waste [46].
1. Sample Collection and DNA Extraction:
- Soil/Sludge: Aseptically collect samples (e.g., 5g) and store at -20°C. For DNA extraction, suspend the sample in an extraction buffer (e.g., CTAB, Tris-HCl, EDTA, NaCl), incubate with Proteinase K and SDS, and extract DNA using phenol-chloroform-isoamyl alcohol precipitation [46].
- Wastewater: Filter water through a 0.22 μm membrane. Place the filter in an extraction buffer and follow a similar incubation and extraction procedure as for soil [46].
2. Library Preparation and Sequencing:
- Use the extracted metagenomic DNA to construct a whole-genome shotgun library.
- Sequence the library using a high-throughput platform like Illumina HiSeq [46].
3. Bioinformatic Analysis:
- Pre-processing: Perform quality control with
FastQCandTrimmomatic[43]. - Assembly: Assemble quality-filtered reads into contigs using
MEGAHITormetaSPAdes[43]. - BGC Prediction: Analyze the assembled contigs with the
antiSMASHtool to detect BGCs, such as those encoding terpenes, bacteriocins, and non-ribosomal peptide synthetases (NRPS) [46].
Protocol 2: Selective Isolation of Bioactive Actinomycetes
This protocol is derived from the successful isolation of bioactive bacteria from a Fijian cave [44].
1. Sample Pretreatment:
- To suppress fast-growing bacteria and fungi, subject soil or sediment samples to pretreatments such as exposure to harsh chemicals, mild heat, or desiccation. Actinomycete spores are resistant to these conditions.
2. Selective Culturing:
- Plate the pretreated, diluted samples on selective media designed to mimic the oligotrophic source environment (e.g., low-nutrient cave conditions).
- Incubate cultures for several days to weeks to allow for the slow growth of Actinomycetes.
3. Screening for Bioactivity:
- Purify isolates with Actinomycete-like morphology (e.g., filamentous, forming spores).
- Screen for antibacterial activity using a simple cross-streak test against pathogenic bacterial strains. In the referenced study, 34 out of 55 isolates (62%) showed antibacterial properties [44].
4. Genetic Identification:
- Identify promising isolates by sequencing partial 16S rRNA genes and comparing them to curated databases like EzBioCloud or SILVA [44].
Research Reagent Solutions
Table 1: Essential Computational Tools for Metagenomic BGC Identification
| Tool Name | Function | Key Feature |
|---|---|---|
| TaxiBGC [42] | Predicts experimentally characterized BGCs from metagenomes. | Taxonomy-guided approach that first pinpoints the microbial species. |
| antiSMASH [46] | Detects biosynthetic gene clusters in assembled sequences. | Identifies a wide range of BGC types (e.g., NRPS, PKS, bacteriocins). |
| HUMAnN2 [45] | Functional profiling of metagenomes and metatranscriptomes. | Uses tiered search for fast, species-resolved functional abundance data. |
| MetaPhlAn [42] | Taxonomic profiling of metagenomes. | Provides species-level identification using clade-specific marker genes. |
| MEGAHIT [43] | De novo metagenomic assembler. | Efficient for assembling large, complex datasets from multiple samples. |
Table 2: Key Laboratory Reagents and Materials for Target Microbe Isolation
| Reagent/Material | Function | Application Note |
|---|---|---|
| Selective Media [9] | Selects for growth of target microbes while inhibiting others. | Incorporate specific carbon sources or antibiotics based on metagenomic insights. |
| CTAB Buffer [46] | Used in DNA extraction to lyse cells and separate DNA from proteins. | Critical for efficient DNA extraction from complex environmental samples like soil. |
| Proteinase K & SDS [46] | Enzymatic and detergent-based lysis for DNA release. | Used in the metagenomic DNA extraction protocol for robust cell disruption. |
| Phenol-Chloroform-Isoamyl Alcohol [46] | Organic solvent mixture for purifying DNA from aqueous extracts. | Essential for removing contaminants and proteins during DNA extraction. |
Workflow and Pathway Diagrams
BGC Identification Workflow
Selective Inhibition in Microbial Isolation
Navigating Challenges: Resistance, Co-Selection, and Optimization Strategies
Frequently Asked Questions (FAQs)
What is the fundamental difference between co-selection and cross-resistance? Co-selection and cross-resistance describe two distinct mechanisms through which exposure to one antimicrobial agent can lead to resistance against another.
- Co-selection occurs when resistance to multiple agents is selected for simultaneously. This primarily happens through three processes: co-resistance (where resistance genes for multiple agents are located close together on the same genetic element, like a plasmid), cross-resistance (where a single resistance mechanism, such as an efflux pump, provides protection against multiple structurally different agents), and co-regulation (where the expression of multiple separate resistance mechanisms is triggered by the presence of one agent) [47].
- Cross-resistance is specifically a situation where one mechanism, such as the overexpression of a multidrug efflux pump, confers reduced susceptibility to multiple antimicrobial classes simultaneously [48] [49].
Which biocides are most commonly associated with co-selection for antibiotic resistance? Laboratory and genomic studies have identified several biocide classes of concern:
- Quaternary Ammonium Compounds (QACs), such as benzalkonium chloride, are frequently cited. The
qacE∆1gene, which provides low-level resistance to QACs, is commonly found co-located with antibiotic resistance genes (ARGs) on plasmids [50]. - Triclosan, a bisphenol, has a specific enzyme target (enoyl-acyl carrier protein reductase, FabI) in fatty acid synthesis. Mutations in the
fabIgene or its homologs can lead to reduced susceptibility to both triclosan and certain antibiotics [48] [49]. - Chlorhexidine, a biguanide, has been linked to resistance mechanisms that can also affect antibiotic susceptibility, often involving efflux pumps [51] [49].
What are the critical methodological challenges in studying biocide resistance? Research in this field faces several significant hurdles [52]:
- Lack of Standardized Breakpoints: Unlike antibiotics, there are no internationally agreed-upon concentration values (breakpoints) to define whether a bacterium is "resistant" or "susceptible" to a specific biocide.
- Complex Mode of Action: Most biocides target multiple cellular sites simultaneously, making it difficult to pinpoint specific resistance mechanisms.
- Variable In-Use Concentrations: Biocides are typically used at concentrations that are multiples of their minimum lethal concentration, making it challenging to replicate real-world conditions in lab tests for "resistance."
- Distinguishing Tolerance from Resistance: It is methodologically difficult to differentiate between a temporary, adaptive tolerance and genuine, heritable resistance.
Troubleshooting Common Experimental Issues
Problem: Inconsistent Minimum Inhibitory Concentration (MIC) results for biocides across replicate experiments.
| Potential Cause | Diagnostic Steps | Solution |
|---|---|---|
| Sub-lethal biocide exposure leading to adaptive, non-heritable tolerance [52]. | - Test for stability of resistance by passaging cells in biocide-free medium.- Use quantitative real-time PCR to check for upregulation of efflux pump genes (e.g., qacA, qacB). |
- Standardize pre-culture conditions and inoculum preparation.- Ensure precise, lethal biocide concentrations as per manufacturer/scientific guidelines. |
| Biofilm formation during the assay, conferring inherent reduced susceptibility [53]. | - Perform crystal violet staining or microscopy to check for biofilm.- Compare MIC in planktonic vs. biofilm-grown cells. | - Use specific anti-biofilm reagents or surfactants in the protocol where appropriate.- Ensure vigorous shaking during liquid culture assays. |
| Carryover of organic matter from growth media inactivating the biocide [51]. | - Review protocol for proper cleaning and neutralization steps.- Confirm the biocide's compatibility with the test media components. | - Include appropriate controls for biocide activity in the test medium.- Follow standardized suspension tests (e.g., European Standards EN 1276, EN 1650). |
Problem: Suspected horizontal gene transfer of resistance genes during an experiment.
| Potential Cause | Diagnostic Steps | Solution |
|---|---|---|
| Co-selection from a biocide or metal promoting the transfer of a plasmid carrying both Biocide/Metal Resistance Genes (BMRGs) and ARGs [47] [50]. | - Perform plasmid conjugation assays with and without sub-inhibitory biocide pressure.- Use PCR and sequencing to screen for common co-occurring genes (e.g., qacE∆1 with β-lactamase genes). |
- Maintain strict aseptic technique to prevent cross-contamination.- Consider using strains lacking mobile genetic elements for specific controls. |
| Biocide-induced cell disruption releasing intact DNA into the environment, facilitating natural transformation [53]. | - Quantify extracellular DNA (eDNA) in the culture supernatant after biocide exposure. | - Include DNase in the experimental medium to degrade free DNA where applicable to the research question. |
Key Experimental Protocols
Protocol for Detecting Efflux Pump-Mediated Cross-Resistance
Principle: This method identifies if reduced susceptibility to a biocide is due to active efflux and determines if the same pump confers cross-resistance to antibiotics [49].
Materials:
- Bacterial test strain and appropriate control strains.
- Biocides and antibiotics of interest (e.g., a QAC and a fluoroquinolone).
- Efflux pump inhibitor (e.g., Carbonyl Cyanide m-Chlorophenylhydrazone (CCCP), Phe-Arg β-naphthylamide (PAβN)).
- Mueller-Hinton Broth (MHB) or other suitable medium.
- 96-well microtiter plates.
- Spectrophotometer.
Procedure:
- Prepare MIC plates: In a 96-well plate, create two-fold serial dilutions of the biocide and the antibiotic in MHB, with and without a sub-inhibitory concentration of the efflux pump inhibitor.
- Inoculate: Standardize the bacterial inoculum to ~5 × 10^5 CFU/mL and add to each well.
- Incubate: Incubate the plates at the optimal growth temperature for 16-20 hours.
- Analyze: Determine the MIC as the lowest concentration that completely inhibits visible growth.
- Interpretation: A ≥4-fold decrease in the MIC of the biocide or antibiotic in the presence of the efflux pump inhibitor is indicative of efflux pump involvement. If the same inhibitor affects MICs for both a biocide and an antibiotic, it suggests cross-resistance via a common efflux mechanism [49].
Protocol for Genomic Co-occurrence Analysis of Resistance Genes
Principle: This bioinformatics workflow identifies whether genes for biocide/metal resistance and antibiotic resistance are physically linked on the same chromosome or plasmid, indicating a high risk for co-selection [50].
Materials:
- Fully sequenced bacterial genome or plasmid (FASTA format).
- Curated databases of resistance genes (e.g., BacMet for BMRGs, Resqu or CARD for ARGs).
- Bioinformatics software (e.g., USEARCH, BLAST+, R for statistical analysis).
Procedure:
- Data Collection: Obtain the complete genome sequence of the bacterial isolate(s) of interest.
- Similarity Searching: Use a sequence similarity tool (e.g.,
ublastin USEARCH) to search the genome against the BacMet and ARG databases. Apply stringent thresholds (e.g., ≥90% sequence identity and query coverage) [50]. - Co-occurrence Analysis: Identify all genomic locations (chromosome or plasmid) that contain both one or more BMRGs and one or more ARGs.
- Mobile Genetic Element Screening: Screen these co-location sites for markers of mobile genetic elements (MGEs), such as integrase genes (
intI) or transposases, which indicate a high potential for horizontal transfer. - Statistical Evaluation: Use logistic regression or Fisher's exact tests to determine if the co-occurrence of BMRGs and ARGs is statistically significant and if it is linked to conjugative plasmids [50].
Research Reagent Solutions
| Reagent / Material | Function in Experiment | Key Considerations |
|---|---|---|
| Efflux Pump Inhibitors (e.g., CCCP, PAβN) | To chemically inhibit the activity of multidrug efflux pumps, confirming their role in observed resistance. | Cytotoxicity can affect bacterial growth; optimal sub-inhibitory concentration must be determined empirically [49]. |
| Standardized Biocide Solutions | To provide consistent and reproducible selective pressure in susceptibility and selection experiments. | Purity and formulation can impact activity; prepare fresh stock solutions or verify stability [52]. |
| Metal Salts (e.g., CuSO₄, ZnCl₂) | Used to investigate co-selection between heavy metals and antibiotics, a major concern in agricultural settings. | Bioavailability is key; environmental factors like pH and organic matter can influence results [48] [47]. |
| Integron & Transposase PCR Primers | To detect genetic platforms that facilitate the capture and spread of resistance gene cassettes. | Targets should include intI1 (Class 1 integron integrase) and common transposase genes [50]. |
| Biofilm Detection Kits (e.g., Crystal Violet) | To quantify biofilm formation, a phenotype conferring high-level, multi-agent tolerance. | Methods must differentiate between planktonic and surface-attached cells [53]. |
Visualizing Co-selection Mechanisms and Experimental Workflows
Co-selection Mechanisms
Efflux Pump Investigation Workflow
Biofilm & Gene Transfer
The discovery and development of novel antimicrobials have slowed to a critical level, creating a dangerous innovation gap in our ability to combat drug-resistant infections. This crisis stems from a confluence of scientific challenges and, more fundamentally, from severe market failures that have rendered antibiotic research and development (R&D) economically non-viable for most pharmaceutical companies. Despite the growing threat of antimicrobial resistance (AMR), which causes millions of deaths annually and could result in 10 million deaths per year by 2050, the pipeline for new antibiotics remains insufficient [54] [55]. The situation is exacerbated by the exit of major pharmaceutical companies from antibiotic R&D, with at least 18 major firms leaving the field since the 1990s [14]. This technical support article examines the current incentive models designed to address these market failures and provides researchers with a framework for navigating the evolving landscape of antimicrobial R&D funding.
Understanding the Market Failure
Antibiotics face unique market challenges that distinguish them from other drug classes and create what economists term "market failure." Understanding these fundamental issues is crucial for researchers seeking to align their projects with feasible development pathways.
The Economic Challenge
The conventional pharmaceutical business model, which links revenue to sales volume, is fundamentally misaligned with appropriate antibiotic use. Key economic barriers include:
- Limited Usage Requirements: To preserve efficacy, new antibiotics must be used sparingly and reserved for the most resistant infections, deliberately limiting sales volume [56].
- Short Treatment Duration: Unlike medications for chronic conditions, antibiotics are typically prescribed for short periods (days to weeks), further reducing revenue potential [57].
- Price and Reimbursement Pressures: Healthcare systems typically encourage use of the cheapest available antibiotic, creating downward price pressure even for novel agents [57].
- Development Costs and Risks: The mean cost for developing systemic anti-infectives is approximately $1.3 billion, matching the average for all drug classes, despite better Phase 1 to approval success rates (25% vs. 14% average) [15].
The "Brain Drain" and Infrastructure Loss
The economic challenges have led to a significant loss of specialized expertise and research infrastructure:
- An estimated 3,000 AMR researchers remain active globally—a critically small number to address the escalating threat [15].
- Most antibiotic research has shifted to small biotech companies and academics, with antibiotic INDs filed by large companies declining from over 75% in the 1980s to under 20% in the 2010s [15].
- The collapse of several biotech companies even after achieving regulatory approval for new antibiotics (e.g., Achaogen's bankruptcy following plazomicin approval) demonstrates the severity of the commercialization challenge [15].
Current Incentive Models: A Technical Analysis
Incentive models for antibiotic R&D are broadly categorized as "push" or "pull" mechanisms. Push incentives reduce upfront R&D costs, while pull mechanisms reward successful development. The table below summarizes the major incentive types, their mechanisms, and examples.
Table 1: Classification of Antibiotic R&D Incentive Models
| Incentive Type | Mechanism | Examples | Key Characteristics |
|---|---|---|---|
| Push Mechanisms | Reduce early R&D costs through direct funding | CARB-X, IMI AMR Accelerator, GARDP, REPAIR | Targets basic science through clinical development; primarily benefits academics and SMEs |
| Pull Mechanisms | Reward successful development through market guarantees | UK subscription model, Market Entry Rewards (MERs) | Delinks payment from volume sold; aims to attract large pharmaceutical companies |
| Hybrid Models | Combine push and pull elements | Antibiotic Susceptibility Bonus (ASB) | Provides upfront support with conditional future payments based on performance |
| Regulatory Incentives | Accelerate development or extend market exclusivity | Transferable Exclusivity Extensions | Grants extended exclusivity that can be applied to other products |
Push Funding Mechanisms
Push funding mechanisms provide critical support for early-stage research, covering costs from basic science through preclinical development and early clinical trials. These programs are essential for academics and small companies who lack the capital to advance promising compounds independently.
Table 2: Major Global Push Funding Initiatives
| Initiative | Funding Scope | Focus Areas | Recent Funding |
|---|---|---|---|
| CARB-X | Preclinical research | Gram-negative bacteria, diagnostics | $500M (2016-2021) [55] |
| IMI AMR Accelerator | Phase II trials | TB, Gram-negative bacteria | Nearly €500M [55] |
| GARDP | Clinical research | Unmet R&D gaps, equitable access | $270M (2017-2023) [55] |
| AMR Action Fund | Late-stage clinical | Phase II and III trials | $1B (2020-2030) [58] |
Pull Incentive Models
Pull incentives have gained significant political momentum in recent years as mechanisms to address the commercial viability of new antibiotics. These models are increasingly being implemented at national levels:
- Subscription Models (UK): The UK's innovative model pays pharmaceutical companies an annual fee for access to antibiotics, negotiated based on AMR-specific health technology assessment and delinked from volume supplied [55].
- Market Entry Rewards (MERs): Proposed as large, upfront payments upon antibiotic approval (e.g., $1.6 billion in the 2016 UK AMR Review), these aim to provide sufficient return on investment independent of sales volume [56].
- Transferable Exclusivity Extensions: These grant extended market exclusivity that can be applied to other, more profitable products in a company's portfolio, creating cross-subsidization [59].
- Antibiotic Susceptibility Bonus (ASB): A innovative staged bonus component of an MER that rewards developers when resistance to their drug remains low over time, directly aligning stewardship with financial return [56].
Table 3: National Pull Incentive Implementations in Europe
| Country | Program | Mechanism | Target Pathogens |
|---|---|---|---|
| Sweden | Annual revenue guarantee | Minimum guaranteed annual revenue in exchange for supply | WHO Priority Pathogens [55] |
| Germany | Health Insurance Law | Automatic exception of 'reserve' antibiotics from reference pricing | WHO Priority Pathogens [55] |
| France | Antibiotic exception | Price guarantee for antibiotics with 'minor' added benefit | All antibiotics, including non-inferiority trials [55] |
Experimental Protocols for Aligning Research with Incentive Priorities
To maximize the likelihood of securing funding and advancing through the development pipeline, researchers should design projects that explicitly address the priorities of major incentive programs.
Protocol: Developing a Target Product Profile (TPP) for Priority Pathogens
Objective: Create a comprehensive TPP that aligns with WHO Bacterial Priority Pathogens List (BPPL) and funder requirements.
Methodology:
- Pathogen Selection: Identify target pathogens from the WHO BPPL 2024, prioritizing critical pathogens (Acinetobacter baumannii, Pseudomonas aeruginosa, Enterobacterales) [14].
- Resistance Mechanism Mapping: Characterize resistance mechanisms for the selected pathogen using whole-genome sequencing of clinical isolates.
- Spectrum Definition: Precisely define the spectrum of activity, prioritizing narrow-spectrum agents to support stewardship goals.
- Innovation Criteria Assessment: Evaluate compounds against WHO innovation criteria (novel chemical class, new target, novel mechanism of action, no cross-resistance) [14].
- Development Pathway Planning: Outline a development pathway that addresses the challenges of clinical trials for resistant infections, including potential for streamlined approval pathways.
Technical Considerations:
- Focus on compounds with activity against carbapenem-resistant and extended-spectrum β-lactamase (ESBL)-producing pathogens
- Incorporate resistance propensity studies early in development
- Include plans for rapid diagnostics to enable targeted therapy
Protocol: Designing a Compound Development Package for CARB-X Applications
Objective: Prepare a comprehensive compound package that meets the scientific and technical requirements for CARB-X and similar push funding mechanisms.
Methodology:
- Hit Validation:
- Confirm chemical structure and purity (>95%) using NMR and LC-MS
- Determine minimum inhibitory concentrations (MICs) against ESKAPE pathogens using CLSI standards
- Assess cytotoxicity against mammalian cell lines (HEK293, HepG2)
Lead Optimization:
- Perform structure-activity relationship (SAR) studies
- Evaluate pharmacokinetic properties (absorption, distribution, metabolism, excretion)
- Assess potential for resistance development through serial passage experiments
In Vivo Efficacy:
- Conduct studies in relevant animal models (e.g., neutropenic murine thigh infection model)
- Establish pharmacokinetic/pharmacodynamic (PK/PD) relationships
- Determine dose fractionation for efficacy optimization
Technical Considerations:
- Prioritize compounds with novel mechanisms of action or new chemical classes
- Demonstrate activity against multidrug-resistant Gram-negative pathogens
- Include plans for overcoming permeability and efflux challenges in Gram-negative bacteria
The Scientist's Toolkit: Research Reagent Solutions
Table 4: Essential Research Materials for Antimicrobial Development
| Reagent/Material | Function | Application Notes |
|---|---|---|
| Checkerboard Assay Systems | Synergy testing | Essential for combination therapy approaches; required by many funders |
| Galleria mellonella Model | Early in vivo efficacy | Low-cost alternative to mammalian models for initial efficacy screening |
| Membrane Permeability Assays | Compound optimization | Critical for Gram-negative compounds; assess outer membrane penetration |
| Efflux Pump Inhibition Assays | Resistance mechanism analysis | Identify compounds affected by major efflux systems (e.g., AcrAB-TolC) |
| Whole Genome Sequencing Kits | Resistance mechanism identification | Characterize resistant mutants from serial passage experiments |
Troubleshooting Guide: Common Experimental Challenges
FAQ: Our promising compound shows excellent in vitro activity but poor in vivo efficacy. What could explain this discrepancy?
Answer: This common challenge typically stems from several potential issues:
- Pharmacokinetic Limitations: The compound may have poor bioavailability, rapid clearance, or extensive protein binding. Conduct comprehensive PK studies to identify the specific issue.
- Tissue Penetration Problems: The compound may not reach the infection site at effective concentrations. Use microdialysis or other tissue penetration studies to evaluate distribution.
- Host Factor Effects: Serum components or immune factors may inhibit compound activity. Compare activity in serum vs. broth media.
- Experimental Model Issues: The infection model may not adequately reflect human disease. Validate the model with standard comparators.
FAQ: How can we demonstrate "innovation" for funding applications when most new antibiotics are derivatives of existing classes?
Answer: Focus on these key areas:
- Novel Targets: Identify and validate new bacterial targets using genetic approaches (e.g., CRISPRi, essential gene studies).
- Mechanism of Action: Use techniques like transcriptomics or morphological profiling to demonstrate distinct mechanisms even within known classes.
- Resistance Profile: Show absence of cross-resistance with existing antibiotics through testing against resistant clinical isolates.
- Chemical Structure: Emphasize structural novelty through computational chemistry and molecular modeling.
Visualization: The Antimicrobial R&D Incentive Pipeline
The following diagram illustrates the antibiotic development pipeline and the primary incentive mechanisms that support each stage:
Antibiotic R&D Pipeline and Incentive Flow
Future Directions and Research Opportunities
The landscape of antibiotic incentives continues to evolve, with several promising developments that researchers should monitor:
- Integrated Pull-Push Models: New models like the Antibiotic Susceptibility Bonus (ASB) that combine upfront funding with long-term stewardship incentives represent the next generation of incentives [56].
- Global Coordination Efforts: The 2024 UN High-level Meeting on AMR resulted in commitments to reduce AMR-associated deaths by 10% by 2030 and calls for catalytic funding of $100 million to support national action plans [14].
- Novel Therapeutic Approaches: Beyond traditional small molecules, incentives are increasingly supporting non-traditional approaches including monoclonal antibodies, bacteriophages, and microbiome modulators [15] [60].
- Diagnostic-Linked Reimbursement: There is growing interest in models that link antibiotic reimbursement to companion diagnostics that ensure appropriate use.
Researchers who strategically align their programs with these evolving incentive structures and clearly articulate how their work addresses both innovation and stewardship priorities will be best positioned to secure funding and contribute to rebuilding the antimicrobial pipeline.
Optimizing Agent Delivery and Biofilm Penetration
Troubleshooting Guides
FAQ 1: Why is my anti-biofilm agent failing to penetrate the biofilm matrix?
Issue: The extracellular polymeric substance (EPS) matrix of biofilms acts as a formidable barrier, physically preventing therapeutic agents from reaching their target microbial cells. [61] [62]
Solutions:
- Utilize Nanoparticle (NP) Carriers: Engineered nanoparticles can significantly enhance penetration. Their small size and customizable surface properties allow them to diffuse through the EPS matrix more effectively than conventional therapeutics. [62] [63]
- Employ Matrix-Degrading Enzymes: Use enzymes such as DNases, dispersin B, or other polysaccharidases in combination with your primary agent. These enzymes disrupt key components of the EPS, weakening the matrix structure and facilitating deeper penetration. [61] [64]
- Leverage Physical Methods: Techniques like ultrasound can create cavitation bubbles that physically disrupt the biofilm's integrity, making it more permeable to agents. [61]
FAQ 2: How can I improve the selectivity of my anti-biofilm agent to avoid harming beneficial microbiota or host cells?
Issue: Non-selective agents can cause off-target effects, which is a significant concern for both environmental applications and therapeutic use. [65]
Solutions:
- Target Microbial-Specific Pathways: Design agents that interfere with targets absent in host cells, such as quorum-sensing (QS) signaling systems or unique bacterial enzyme pathways. [64] [2] For instance, the metabolite bacillaene selectively inhibits the assembly of curli amyloid fibers in E. coli biofilms without affecting all bacterial functions. [2]
- Functionalize Nanoparticles: Attach specific ligands, antibodies, or peptides to the surface of nanoparticles. These functional groups can bind to receptors unique to the target microbe, ensuring highly specific delivery. [64] [62]
- Employ a Dual-Function Strategy: Some natural metabolites, like bacillaene, exhibit concentration-dependent selectivity. At lower concentrations, they may inhibit specific biofilm components (e.g., curli fibers), while exhibiting broader antibiotic activity at higher concentrations. Optimizing delivery concentration can enhance selectivity. [2]
FAQ 3: My agent is effective in vitro but loses efficacy in a more complex, multi-species biofilm model. What could be the reason?
Issue: Multi-species biofilms possess increased heterogeneity and synergistic interactions that can enhance overall community resistance, rendering agents developed against single-species biofilms ineffective. [61]
Solutions:
- Adopt a Multi-Targeted Approach: Instead of a single-mechanism agent, use a combination therapy. This could include a QS inhibitor to disrupt communication, an EPS-degrading enzyme, and a conventional antibiotic delivered via a nanocarrier. [64] [63]
- Incorrate Advanced Gene-Targeting Tools: For genetically defined resistance mechanisms, consider the CRISPR/Cas9 system delivered via nanoparticles. This allows for the precise disruption of antibiotic resistance genes within the mixed population. [63]
- Validate in Complex Models: Begin testing agents in more relevant, complex biofilm models earlier in the development pipeline. This helps identify and address efficacy issues related to microbial diversity before moving to advanced stages. [61]
FAQ 4: How can I overcome biofilm-associated metabolic dormancy that leads to antibiotic tolerance?
Issue: Biofilms contain subpopulations of metabolically dormant or slow-growing "persister" cells that are highly tolerant to antibiotics that target active cellular processes. [61] [63]
Solutions:
- Use Pro-Active Compounds: Agents that induce a metabolic wake-up call in dormant cells can re-sensitize them to conventional antibiotics.
- Combine with EPS-Penetrating Systems: Deliver antimicrobial agents using nanoparticle systems that can penetrate the biofilm and reach these dormant cells, even in nutrient-poor zones. [62] [63]
- Target the EPS Matrix Directly: Strategies that dismantle the physical protective barrier, such as enzymatic degradation or chelating agents, can expose persister cells to the host immune system or higher concentrations of antimicrobials. [61] [64]
Experimental Protocols
Protocol 1: Assessing Biofilm Penetration of Nanoparticle Carriers
Objective: To quantitatively evaluate the depth and distribution of nanoparticles within a mature biofilm.
Materials:
- Fluorescently labeled nanoparticles (e.g., metal, polymeric, or lipid-based) [62]
- Mature biofilm (e.g., of Pseudomonas aeruginosa or Staphylococcus aureus) [61]
- Confocal Laser Scanning Microscopy (CLSM) system [63]
- Image analysis software (e.g., ImageJ, COMSTAT)
Methodology:
- Biofilm Growth: Grow a mature biofilm on a suitable substrate (e.g., a glass-bottom dish) for 48-72 hours under optimal conditions. [61]
- NP Treatment: Incubate the biofilm with the fluorescently labeled nanoparticle suspension for a predetermined time (e.g., 2-4 hours).
- Washing and Fixation: Gently wash the biofilm with a buffer (e.g., PBS) to remove non-adherent nanoparticles. Fix the biofilm with a suitable agent (e.g., paraformaldehyde) if necessary.
- CLSM Imaging: Use CLSM to capture Z-stack images of the biofilm from the top to the bottom surface.
- Image Analysis: Analyze the Z-stack images to determine the fluorescence intensity profile across the biofilm depth. This profile indicates the penetration efficiency of the nanoparticles.
Protocol 2: Evaluating Selective Inhibition of Target Biofilm Matrix Components
Objective: To test the selective inhibition of a specific biofilm matrix component, such as curli amyloid fibers, using a bifunctional inhibitor.
Materials:
- Target microbe (e.g., E. coli strain producing curli fibers) [2]
- Test compound (e.g., bacillaene) [2]
- Congo Red (CR) dye or Thioflavine S (TS) dye [2]
- Salt-free LB agar plates [2]
- Macrocolony biofilm setup
Methodology:
- Macrocolony Setup: Inoculate the target microbe and the inhibitor-producing microbe (e.g., Bacillus subtilis) as neighboring colonies on CR-containing salt-free LB agar plates. [2]
- Incubation: Incubate the plates under conditions conducive to biofilm formation (e.g., at 28-30°C for several days).
- Visual Assessment: Observe the macrocolony biofilm of the target microbe for changes in morphology and a loss of CR staining (which indicates inhibition of curli fiber production) in the zone of interaction with the inhibitor-producing colony. [2]
- Validation with Fluorescent Dyes: For higher resolution, grow biofilms on membranes, section them, and stain with the fluorescent amyloid dye TS. Analyze using fluorescence microscopy to confirm the absence or disruption of curli fibers. [2]
Table 1: Efficacy of Selected Anti-Biofilm Nano-Agents
| Nanoparticle Type | Target Biofilm / Bacterium | Key Mechanism | Reported Efficacy | Citation |
|---|---|---|---|---|
| Liposomal Cas9 Formulation | Pseudomonas aeruginosa | Delivery of CRISPR/Cas9 to disrupt resistance genes | >90% reduction in biofilm biomass in vitro | [63] |
| Gold Nanoparticle-CRISPR | Model Bacterial Systems | Enhanced delivery of gene-editing machinery | 3.5x increase in gene-editing efficiency | [63] |
| Metal & Metal Oxide NPs | Various Biofilm-Forming Pathogens | ROS generation, EPS degradation, direct membrane disruption | Effective in controlling biofilm-forming pathogens (specific efficacy varies by NP) | [62] |
Table 2: Selective Inhibition Agents and Their Targets
| Agent | Primary Target | Mechanism of Action | Selectivity Evidence | Citation |
|---|---|---|---|---|
| Bacillaene | E. coli Curli Amyloid Fibers | Directly impedes assembly of CsgA/CsgB amyloid subunits | Inhibits curli without affecting exopolysaccharide (pEtN-cellulose) production in isogenic mutants | [2] |
| Synthetic Quorum Sensing Inhibitors (e.g., Furanones) | Quorum Sensing Pathways | Interferes with bacterial cell-to-cell communication | Disrupts biofilm maturation without broad-spectrum bactericidal activity | [64] |
| CRISPR/Cas9 with specific gRNA | Antibiotic Resistance Genes (e.g., bla, mecA) | Precise cleavage of genetic sequences conferring resistance | High specificity for the targeted DNA sequence, resensitizing bacteria to antibiotics | [63] |
Pathway and Workflow Visualizations
Biofilm Agent Troubleshooting Flow
E. coli Curli Assembly & Inhibition
The Scientist's Toolkit: Research Reagent Solutions
Table 3: Essential Reagents for Selective Biofilm Inhibition Research
| Reagent / Material | Function in Research | Key Consideration |
|---|---|---|
| Metal/Metal Oxide Nanoparticles (e.g., Ag, ZnO) [62] | Intrinsic anti-biofilm agents; drug delivery carriers. Penetrate EPS and generate ROS. [62] | Size, surface charge, and coating are critical for penetration efficiency and biocompatibility. [62] |
| Functionalized NPs (Ligand-coated) [64] [62] | Enhance targeting specificity to desired microbial species within a mixed community. | Choice of ligand (antibody, peptide, aptamer) determines selectivity and binding affinity. |
| Quorum Sensing Inhibitors (Synthetic furanones, peptide-based) [64] | Disrupt bacterial cell-cell communication, preventing biofilm maturation and virulence. | Specificity for the QS system of the target pathogen must be validated to avoid off-target effects. |
| Matrix Degrading Enzymes (DNases, Dispersin B, amylases) [61] [64] | Weaken the EPS matrix by degrading eDNA, polysaccharides, or proteins, enabling agent penetration. | Enzyme stability and activity in the specific biofilm environment are key for efficacy. |
| CRISPR/Cas9 System with gRNA [63] | For precise genetic disruption of antibiotic resistance or virulence genes within the biofilm. | Requires an efficient delivery system (e.g., NPs) to reach intracellular targets in biofilm cells. [63] |
| Bifunctional Microbial Metabolites (e.g., Bacillaene) [2] | Naturally optimized compounds that can selectively inhibit specific biofilm matrix components. | Effective concentration window for selective vs. broad-spectrum activity must be determined. [2] |
Mitigating Damage to Beneficial Microbiota During Target Pathogen Elimination
Strategic Approaches for Microbiota Conservation
What are the primary strategic approaches to minimize collateral damage to commensal microbiota during antimicrobial therapy?
The core strategies involve moving away from broad-spectrum agents toward highly targeted interventions. These can be categorized as follows:
- Pathogen-Selective Antibiotics: These compounds are designed to inhibit targets unique to the pathogen or to have high affinity for pathogen-specific isoforms of essential targets. An example is Debio 1452, a FabI inhibitor highly selective for Staphylococcus aureus that demonstrated minimal disturbance to the gut microbiome in mouse studies [66].
- Targeted Physical Elimination: Technologies like the Photoimmuno-Antimicrobial Strategy (PIAS) use antibody-probe conjugates that bind to specific pathogens. Subsequent near-infrared light activation generates mechanical stress that eliminates the target pathogen while sparing non-targeted commensals, as shown with S. aureus, Candia albicans, and SARS-CoV-2 [22].
- PK-PD Driven Selective Uptake: This approach designs antibiotics to be preferentially absorbed by pathogens. Strategies include exploiting pathogen-specific transporter systems (e.g., Hygromycin A), pH-dependent cellular uptake (e.g., Cadazolid), or adjuvant-driven selectivity [37].
- Enzyme-Mediated Antibiotic Degradation: This method protects the gut microbiome by inactivating residual antibiotics in the gastrointestinal tract. Ribaxamase, for example, is an oral enzyme that degrades certain beta-lactam antibiotics in the gut, safeguarding the microbiota [37].
- Microbiome Restoration and Engineering: After necessary broad-spectrum treatment, the microbiome can be restored through Fecal Microbiota Transplantation (FMT) or modulated with probiotics, prebiotics, or synthetic microbial communities to re-establish colonization resistance [67] [68].
Comparative Efficacy of Antimicrobial Strategies
What quantitative data compares the impact of broad-spectrum versus targeted antimicrobials on gut microbiota?
The following table summarizes experimental data from key studies, highlighting the superior microbiota-sparing properties of targeted approaches.
Table 1: Quantitative Comparison of Antimicrobial Impacts on Gut Microbiota
| Antimicrobial Strategy | Target Pathogen | Impact on Commensal Abundance | Recovery Time Post-Treatment | Key Experimental Findings |
|---|---|---|---|---|
| Debio 1452 (Pathogen-Selective) [66] | Staphylococcus aureus | Minimal disturbance; only one taxon (S24-7) reduced | 2 days | Gut bacterial abundance and composition were indistinguishable from untreated mice 2 days after cessation. |
| Broad-Spectrum Antibiotics (e.g., Clindamycin) [66] | Wide Range | 100 to 4,000-fold decrease in bacterial abundance | 7-20+ days | Bacterial abundance took 7 days to recover; gut composition remained different from the control group after 20 days. |
| PIAS (Photoimmuno-Conjugate) [22] | S. aureus, C. albicans | No apparent effect on non-target S. epidermidis | Not Applicable (No damage incurred) | Selectively eliminated target pathogen MRSA within mixed samples containing non-target S. epidermidis. |
| Ridinilazole (PK-PD Driven) [37] | Clostridioides difficile | Minimal disruption; affected only a limited number of microbial families | Not Specified | Phase 3 candidate that preserves key gut microbiota involved in bile acid metabolism. |
Detailed Experimental Protocols
Protocol 1: Evaluating Microbiota Impact of a Selective Antibiotic in a Mouse Model
This protocol is adapted from studies on pathogen-selective antibiotics like Debio 1452 [66].
1. Reagents and Materials:
- Test antibiotic (e.g., Debio 1452) and broad-spectrum comparators (e.g., clindamycin, amoxicillin)
- Six-week-old female C57-BL6 mice
- DNA extraction kit (e.g., QIAamp fast DNA stool minikit)
- SYBR Green PCR master mix and real-time PCR system
- Primers for 16S rRNA gene and a host control gene (e.g., TNF-α)
- NEXTflex 16S V1-V3 amplicon-seq kit or similar
- Illumina MiSeq platform or other NGS system
2. Experimental Procedure:
- Animal Dosing: Administer antibiotics once daily via oral gavage for 10 days. The control group should receive the drug carrier only (e.g., 1% Pluronic F-127). Use dose levels converted from human doses to body surface area.
- Sample Collection: Collect stool samples from each mouse via abdominal massage at defined intervals: before treatment, daily during treatment, and on multiple days post-cessation (e.g., days 12, 17, 23, 30, 37). Store samples at -80°C.
- DNA Extraction: Extract total DNA from standardized stool weights using a commercial kit. Include a heating step (70°C for 10 min) and homogenize using a bead-beating system to ensure efficient lysis.
- 16S rRNA Gene Abundance (qPCR):
- Perform real-time PCR with 16S rRNA gene-specific primers on diluted DNA samples.
- Use a serial dilution of a pre-treatment DNA pool to determine the optimal dilution for analysis.
- Calculate the relative abundance of 16S rRNA genes for each sample. Also, quantify a host gene (e.g., TNF-α) to monitor DNA extraction efficiency across samples.
- Microbial Composition (16S Sequencing):
- Generate amplicon libraries targeting the V1-V3 hypervariable regions of the 16S rRNA gene.
- Clean the PCR products, normalize by concentration, and sequence using an Illumina MiSeq platform with paired-end reads.
- Data Analysis:
- Abundance: Plot the qPCR data (log2 scale) to visualize changes in total bacterial load over time.
- Composition: Process sequencing reads to assign taxonomies. Use dimensionality reduction (e.g., PCoA) and statistical tests to compare microbial community structures between treatment groups over time.
Protocol 2: Assessing Targeted Pathogen Killing via Photoimmuno-Antimicrobial Strategy (PIAS)
This protocol is based on the PIAS methodology for targeted pathogen elimination [22].
1. Reagents and Materials:
- Pathogen-specific monoclonal antibody (e.g., against S. aureus peptidoglycan)
- IRDye700DX (IR700) NIR photosensitizer
- Conjugation kit or buffer for antibody-probe conjugation
- Target pathogen (e.g., MRSA) and non-target commensal control (e.g., S. epidermidis)
- NIR light source (LED releasing light at 670-710 nm)
- Colony counting supplies (agar plates) or flow cytometer
2. Experimental Procedure:
- Conjugate Preparation: Conjugate the pathogen-specific mAb with the IR700 probe according to the manufacturer's instructions. A non-specific antibody-IR700 conjugate (e.g., anti-HER2) should be prepared as a control.
- Pathogen Preparation: Culture the target pathogen and non-target control to the desired growth phase (e.g., stationary phase). Wash and resuspend in an appropriate buffer.
- Conjugate Binding: Incubate the pathogen suspension with the specific or control conjugate for a defined period. Use fluorescence microscopy, SEM, or flow cytometry to confirm target-selective binding.
- NIR Illumination: Expose the conjugate-treated pathogens to NIR light at a specific dose (e.g., 5 J/cm² for 1 minute). Include controls: no conjugate + NIR, conjugate + no NIR.
- Viability Assessment:
- Colony Counting: Serially dilute the treated and control suspensions and plate on agar. Incubate and count colony-forming units (CFU) to determine the percentage of killing.
- Specificity Test: Perform the same assay on a mixed culture of target and non-target pathogens to demonstrate selective elimination.
- Data Analysis: Calculate the log-reduction in CFU/mL for the target pathogen under different conditions. Statistical analysis should confirm that killing is significant and specific to the combination of target pathogen, specific conjugate, and NIR light.
Research Reagent Solutions
Table 2: Key Reagents for Developing Microbiota-Sparing Antimicrobials
| Reagent / Technology | Function / Mechanism | Application in Research | Key Feature |
|---|---|---|---|
| Debio 1452 (AFN-1252) [66] | Staphylococcal FabI inhibitor; inhibits fatty acid synthesis | Validating pathogen-selective principle; anti-staphylococcal therapy | High selectivity for staphylococcal FabI due to unique active-site methionine interaction |
| IRDye700DX (IR700) [22] | Photosensitizer probe; generates photo-induced mechanical stress | Core component of PIAS for targeted elimination of bacteria, fungi, viruses | Conjugated to antibodies for target specificity; activated by safe NIR light |
| Hygromycin A [37] | Aminoglycoside antibiotic; exploits BmpD transporter | Selective targeting of Borrelia burgdorferi | Pathogen-specific uptake via a unique transporter system, sparing most gut microbiota |
| Ridinilazole [37] | Bis-benzimidazole; binds DNA minor groove, interferes with cell division | Targeting Clostridioides difficile infection | Selective cellular accumulation due to absence of efflux pumps in C. diff |
| Ribaxamase [37] | Beta-lactamase enzyme; degrades residual beta-lactam antibiotics | Orally administered to protect gut microbiome during IV beta-lactam therapy | Prevents dysbiosis by inactivating antibiotics that diffuse into the GI tract |
| Panobacumab (AR-101) [37] | Monoclonal antibody; targets P. aeruginosa serotype O11 LPS | Immunotherapy for Pseudomonas infections | Precision targeting of a specific pathogen serotype, safeguarding commensals |
Efficacy and Impact: Validating and Comparing Selective Inhibition Strategies
Minimum Inhibitory Concentration (MIC) Assay
FAQ & Troubleshooting Guide
Q1: What does a high MIC value indicate about my test compound? A1: A high MIC value indicates that a higher concentration of the antimicrobial agent is required to inhibit visible bacterial growth. This suggests that the test organism has lower susceptibility or is resistant to the compound. Drugs with lower MIC scores are considered more effective antimicrobial agents [69].
Q2: My MIC results are inconsistent between replicate experiments. What could be the cause? A2: Inconsistent MIC results often stem from improper preparation of the inoculum or antibiotic stock solutions. Ensure that the bacterial inoculum is standardized to approximately 5 × 10^5 CFU/mL and that stock solutions are prepared with the correct solvents and diluents, as these factors significantly impact MIC reliability [70].
Q3: Which method should I choose for MIC determination: broth microdilution or agar dilution? A3: The choice depends on your organism and antibiotic. Broth microdilution is recommended by EUCAST for most cases, while agar dilution is preferred for specific antibiotics like fosfomycin and mecillinam. For fastidious organisms like H. influenzae, broth dilution with HTM medium is required [70].
Detailed Methodology: Broth Microdilution
Principle: The broth microdilution method determines the lowest concentration of an antimicrobial agent that prevents visible growth of a microorganism in a liquid medium after overnight incubation [70].
Step-by-Step Protocol:
- Prepare antibiotic stock solutions: Dissolve antibiotics in appropriate solvents (water, alcohol, or phosphate buffer per Table 2 specifications) [70].
- Prepare serial dilutions: Create two-fold serial dilutions of the antibiotic in Mueller-Hinton Broth (MHB) in a 96-well microtiter plate [70] [71].
- Standardize inoculum: Adjust the test organism to a 0.5 McFarland standard in saline, then dilute to achieve a final concentration of approximately 5 × 10^5 CFU/mL in each well [70].
- Inoculate plates: Add 20 μL of standardized inoculum to each well containing 100 μL of double-strength nutrient broth and antibiotic dilutions [71].
- Include controls: Incorporate growth control (medium + organism), sterility control (medium only), and reference strain control wells [70].
- Incubate: Incubate plates at 35±2°C for 16-20 hours [70].
- Read results: The MIC is the lowest antibiotic concentration that completely inhibits visible growth, indicated by absence of turbidity [69].
MIC Interpretive Criteria Table
Table 1: MIC Interpretive Criteria for Selected Organism-Antibiotic Combinations
| Organism | Antibiotic | Susceptible (μg/mL) | Intermediate (μg/mL) | Resistant (μg/mL) | Test Method |
|---|---|---|---|---|---|
| S. aureus (ATCC 29213) | Plumbagin | ≤0.5 | 1 | ≥2 | Broth microdilution [71] |
| E. coli (ATCC 25922) | Plumbagin | ≤1 | 2 | ≥4 | Broth microdilution [71] |
| P. aeruginosa (ATCC 27853) | Plumbagin | ≤4 | 8 | ≥16 | Broth microdilution [71] |
| S. aureus | Ciprofloxacin | ≤1 | 2 | ≥4 | Broth microdilution [71] |
| E. coli | Ciprofloxacin | ≤0.25 | 0.5 | ≥1 | Broth microdilution [71] |
MIC Determination Workflow
Research Reagent Solutions
Table 2: Essential Reagents for MIC Determination
| Reagent/Material | Function/Purpose | Example Specifications |
|---|---|---|
| Mueller-Hinton Broth (MHB) | Standardized growth medium for most organisms | Cation-adjusted for consistent results [70] |
| Dimethyl Sulfoxide (DMSO) | Solvent for water-insoluble compounds | Sterile, cell culture grade [71] |
| 0.5 McFarland Standard | Inoculum density reference | ~1.5 × 10^8 CFU/mL [70] |
| 96-well Microtiter Plates | Platform for broth microdilution | Sterile, U-bottom or flat-bottom [71] |
| MTT (3-(4,5-dimethylthiazol-2-yl)-2,5-diphenyltetrazolium bromide) | Viability indicator for endpoint determination | 1.25 mg/mL solution [71] |
| Quality Control Strains | Verification of test performance | E. coli ATCC 25922, S. aureus ATCC 29213 [70] |
Time-Kill Kinetics Assay
FAQ & Troubleshooting Guide
Q1: How do I determine if my antimicrobial agent is bactericidal or bacteriostatic? A1: An agent is considered bactericidal if it reduces the initial inoculum by ≥3 log10 CFU/mL (99.9% killing) at a specified time. Bacteriostatic activity maintains the inoculum within 3 log10 CFU/mL of the initial concentration. Time-kill kinetics assays provide this dynamic information beyond what MIC values can show [71].
Q2: My time-kill assay shows regrowth after initial killing. What does this indicate? A2: Regrowth often indicates the presence of a resistant subpopulation, antibiotic degradation during incubation, or insufficient drug concentration. Consider testing higher concentrations or combination therapies to suppress resistance development [72].
Q3: What are the advantages of using both MPN and CFU plating in time-kill assays? A3: Using Most Probable Number (MPN) in a 96-well plate and Colony Forming Unit (CFU) plating simultaneously provides complementary data. MPN detects viable cells at lower concentrations while CFU provides quantitative counts, together offering a comprehensive view of bacterial burden over time [72].
Detailed Methodology: Time-Kill Kinetics
Principle: Time-kill assays provide longitudinal data reflecting the dynamics of the antibiotic effect over time against planktonic cultures, quantifying the concentration-effect relationship and determining whether an antimicrobial is bactericidal or bacteriostatic [72].
Step-by-Step Protocol:
- Prepare inoculum: Dilute an overnight bacterial culture in saline to 0.5 McFarland turbidity, then further dilute 1:50 in appropriate growth medium (e.g., LB broth) [73].
- Set up treatment conditions: Dispense cultures into tubes or flasks containing antimicrobial agents at desired concentrations (e.g., 0.5×, 1×, 2×, and 4× MIC) [71].
- Establish time points: Designate sampling intervals (e.g., 0, 2, 4, 6, 8, 12, 24 hours) with separate culture vessels for each time point to avoid cross-contamination [72].
- Sample and quantify: At each time point, remove 100 μL aliquots, perform serial dilutions in phosphate-buffered saline (pH 7.2), and plate on appropriate agar plates [73].
- Incubate and enumerate: Incubate plates for 18-24 hours at 37°C, then count colonies to determine CFU/mL [73].
- Analyze data: Plot log10 CFU/mL versus time to generate killing curves and determine bactericidal/bacteriostatic activity [71].
Time-Kill Kinetic Parameters Table
Table 3: Key Parameters for Time-Kill Kinetic Analysis
| Parameter | Definition | Interpretation | Calculation Method |
|---|---|---|---|
| Bactericidal Activity | ≥3 log10 CFU/mL reduction from initial inoculum | Indicates killing activity | Compare minimum log reduction to baseline |
| Bacteriostatic Activity | <3 log10 CFU/mL reduction from initial inoculum | Inhibits growth without killing | Maintains inoculum within 3 log10 |
| Rate of Killing | Slope of the killing curve | Speed of antimicrobial action | Δlog10 CFU/mL/unit time |
| Post-Antibiotic Effect | Persistent suppression after removal | Continued activity after brief exposure | Measure regrowth delay after drug removal |
| MBC | Minimum Bactericidal Concentration | Lowest concentration killing 99.9% | Derived from time-kill data |
Time-Kill Assay Workflow
Biofilm Disruption Assays
FAQ & Troubleshooting Guide
Q1: Why are biofilm-forming bacteria significantly more resistant to antibiotics than planktonic cells? A1: Biofilms demonstrate up to 1000-fold increased antibiotic resistance due to multiple factors: (1) limited antibiotic penetration through the extracellular matrix, (2) altered metabolic states of embedded cells, (3) presence of persistent cells, and (4) induction of biofilm-specific resistance mechanisms [74].
Q2: The crystal violet assay shows increased biomass after anti-biofilm treatment. Is this possible? A2: Yes, when using polysaccharide-degrading agents like depolymerases, crystal violet staining may show apparent increased biomass because degradation products can bind more dye molecules. Always complement crystal violet with colony counting or viability staining for accurate interpretation [75].
Q3: What is the difference between MBIC and MBEC? A3: Minimum Biofilm Inhibitory Concentration (MBIC) is the lowest concentration that prevents biofilm formation, while Minimum Biofilm Eradication Concentration (MBEC) is the lowest concentration that eradicates a pre-formed biofilm. MBEC values are typically much higher than MBIC values [74].
Detailed Methodology: Biofilm Disruption Assessment
Principle: Biofilm disruption assays evaluate the ability of antimicrobial agents to prevent biofilm formation or eradicate pre-existing biofilms, typically using microtiter-based methods with multiple readout systems to assess different aspects of biofilm viability and structure [75].
Step-by-Step Protocol for Biofilm Inhibition:
- Grow biofilms: Inoculate 96-well plates with test organisms and incubate for 24-72 hours to allow biofilm formation [75].
- Treat biofilms: Add antimicrobial agents at various concentrations to pre-formed biofilms [74].
- Incubate: Incubate for additional 24 hours to assess disruption activity [75].
- Assess by multiple methods:
- Colony counting: Remove planktonic cells, resuspend biofilm cells by scraping/sonication, plate serial dilutions, and count CFU [75].
- Viability staining: Use LIVE/DEAD BacLight Bacterial Viability Kit to distinguish live/dead cells within biofilms [75].
- Crystal violet staining: Fix biofilms with methanol, stain with 0.1% crystal violet, destain with ethanol, and measure absorbance at 570-600nm [75].
- Calculate disruption: Compare treated samples to untreated controls to determine percentage inhibition or eradication [74].
Biofilm Assay Comparison Table
Table 4: Comparison of Biofilm Assessment Methods
| Method | Principle | Measures | Advantages | Limitations |
|---|---|---|---|---|
| Crystal Violet Staining | Dye binding to biomass | Total biofilm biomass (cells + matrix) | Simple, high-throughput | Does not distinguish live/dead cells [75] |
| Colony Counting | Viable cell enumeration | Biofilm-associated viable cells | Direct measure of viability | Labor-intensive, underestimates aggregates [75] |
| LIVE/DEAD Staining | Membrane integrity | Ratio of live to dead cells | Distinguishes viability states | May not detect metabolically inactive cells [75] |
| MPN Assay | Statistical viability | Most probable number of viable cells | Detects low numbers of viable cells | Less precise than direct counting [72] |
Research Reagent Solutions for Biofilm Studies
Table 5: Essential Reagents for Biofilm Disruption Assays
| Reagent/Material | Function/Purpose | Application Notes |
|---|---|---|
| Crystal Violet Solution (0.1%) | Total biofilm biomass staining | Use after methanol fixation; destain with ethanol [75] |
| LIVE/DEAD BacLight Bacterial Viability Kit | Differentiation of live/dead cells | Uses SYTO9 and propidium iodide fluorescence [75] |
| 96-well Flat-bottom Polystyrene Plates | Substrate for biofilm growth | Surface properties significantly affect attachment [75] |
| Phage-derived Depolymerases | Matrix degradation agents | Target specific exopolysaccharides (e.g., KP34p57 for K. pneumoniae) [75] |
| MTT Solution (1.25 mg/mL) | Metabolic activity indicator | Measures cellular reduction of tetrazolium dye [71] |
Biofilm Disruption Assessment Workflow
FAQs: Disinfectant Efficacy and Biofilm Challenges
Q1: Why are biofilms significantly more resistant to disinfectants than planktonic cells? Biofilms are up to 1000 times more resistant to antimicrobial agents than their planktonic counterparts [76]. This increased resistance is not due to a single mechanism but a combination of factors:
- Physical Barrier: The extracellular polymeric substance (EPS) matrix, composed of polysaccharides, proteins, and extracellular DNA, acts as a physical barrier, restricting the penetration of antimicrobial agents [61] [77].
- Metabolic Heterogeneity: Biofilms contain subpopulations of dormant or slow-growing bacteria. Many disinfectants and antibiotics target actively growing cells, making these dormant cells less susceptible [77].
- Adaptive Responses: The biofilm microenvironment can induce physiological changes in bacteria, enhancing their tolerance [61].
Q2: What are the key limitations of conventional disinfectants like sodium hypochlorite against biofilms? While sodium hypochlorite (SH) is a common biocide, it faces specific challenges:
- Formation of Harmful By-products: Its use can lead to the formation of organochlorinated carcinogenic compounds [78].
- Reduced Efficacy on Sessile Cells: Although it may have fast antimicrobial action on planktonic cells, its effectiveness is considerably diminished against mature, biofilm-embedded cells [78].
Q3: What defines a "selective" or "alternative" anti-biofilm agent? These are agents that often target specific biofilm-related functions or use novel mechanisms of action, rather than relying on broad-spectrum cytotoxicity. Examples include:
- Quorum Sensing Inhibitors (QSI): These compounds interfere with bacterial cell-to-cell communication, disrupting biofilm maturation and virulence without directly killing the bacteria, potentially reducing selective pressure for resistance [79] [76].
- Nanomaterial-based Formulations: Nano-delivery systems can be designed to penetrate the EPS matrix and deliver antimicrobials directly to bacterial cells within the biofilm, enhancing efficacy and reducing required doses [77].
- Physical Disruption Agents: Techniques like ultrasound use acoustic cavitation to generate localized shockwaves that physically disrupt the biofilm structure and enhance the efficacy of co-applied antimicrobials [80].
Q4: What are the ESKAPE pathogens and why are they a particular concern in biofilm research? The ESKAPE pathogens are a group of bacteria renowned for their ability to "escape" the action of conventional antibiotics. They are:
- Enterococcus faecium
- Staphylococcus aureus
- Klebsiella pneumoniae
- Acinetobacter baumannii
- Pseudomonas aeruginosa
- Enterobacter species [61]
These pathogens are a major cause of healthcare-associated infections, and their ability to form biofilms on medical devices and tissues creates a critical challenge in clinical settings [61].
Troubleshooting Common Experimental Issues
Problem: Inconsistent Biofilm Formation in Assays
- Potential Cause 1: Surface Properties. Rough surfaces have been shown to promote better initial microbial adhesion and propagation compared to smooth surfaces [61].
- Solution: Standardize the material and surface roughness (e.g., for coupon assays) across all experiments. Ensure proper cleaning protocols to avoid residual contaminants that may influence attachment.
- Potential Cause 2: Growth Medium and Conditions. Biofilm formation is influenced by nutrient availability, temperature, and flow conditions [61] [81].
- Solution: Use a standardized, well-defined growth medium. Control for temperature and, if using flow cells, ensure consistent hydrodynamic conditions. Allow the biofilm to mature for a consistent time period.
Problem: High Variability in Disinfectant Efficacy Data
- Potential Cause: Inadequate Neutralization of Disinfectant. After the treatment phase, residual disinfectant carried over into the viability assay can continue to kill cells, leading to overestimation of its efficacy.
- Solution: Include a disinfectant neutralization step immediately after the contact time. Validate the neutralization method to confirm it effectively stops the disinfectant's action without being toxic to the bacteria itself [82].
Problem: Poor Penetration of Anti-biofilm Agents
- Potential Cause: The Dense EPS Matrix. The EPS can hinder the diffusion of chemical agents, preventing them from reaching cells in the deeper layers of the biofilm [77] [76].
- Solution:
- Consider Combination Therapy: Use an EPS-degrading enzyme (e.g., DNase, dispersin B) in conjunction with the disinfectant to weaken the matrix [61].
- Utilize Nanocarriers: Employ nanoparticle-based delivery systems designed to penetrate the biofilm matrix and release their payload internally [77].
- Apply Physical Methods: Pre-treat the biofilm with low-frequency ultrasound to disrupt its physical integrity and enhance agent penetration [80].
Experimental Protocols & Data
Protocol: Microtiter Plate Biofilm Assay for Disinfectant Screening
This is a standard method for quantifying biofilm formation and assessing the efficacy of anti-biofilm agents in a high-throughput format [79].
- Inoculation: Dilute an overnight culture of the test microorganism (e.g., Staphylococcus aureus) in a fresh, appropriate broth to a standardized optical density.
- Biofilm Formation: Aliquot the cell suspension into the wells of a sterile 96-well flat-bottom microtiter plate. Include control wells with broth alone for background subtraction. Incubate the plate under static conditions at a suitable temperature for 24-48 hours to allow biofilm formation.
- Treatment: Gently remove the planktonic cells and growth medium by inverting and tapping the plate. Wash the adhered biofilms twice with a phosphate-buffered saline (PBS) to remove loosely attached cells. Add serial dilutions of the test disinfectants to the wells. Include a positive control (e.g., a known biocide) and a negative control (PBS only). Incubate for a specified contact time.
- Disinfectant Neutralization: After contact time, remove the disinfectant and add a validated neutralizer to stop the action.
- Biofilm Quantification (Crystal Violet Staining):
- Remove the neutralizer and air-dry the biofilm.
- Stain the biofilm with 0.1% crystal violet solution for 15-20 minutes.
- Wash the plate thoroughly under running tap water to remove unbound dye.
- Destain the bound dye by adding 200 µL of 30% acetic acid or 95% ethanol per well.
- Transfer 125 µL of the destained solution to a new microtiter plate and measure the absorbance at 570-600 nm.
- Data Analysis: The absorbance is proportional to the amount of biofilm biomass. Calculate the percentage of biofilm inhibition relative to the untreated control.
Protocol: Assessing Efficacy on Planktonic vs. Sessile Cells
A direct comparison requires parallel tests on the same bacterial strain in its two states.
- Planktonic Susceptibility Test: Use a standard broth microdilution method to determine the Minimum Inhibitory Concentration (MIC) of the disinfectant against free-floating cells [79].
- Sessile (Biofilm) Susceptibility Test: Grow biofilms as described above. After disinfectant treatment and neutralization, instead of staining, disrupt the biofilm by sonication or vigorous scraping/vortexing with beads. Serially dilute the resulting suspension and plate on agar to enumerate the colony-forming units (CFU) to determine the log reduction in viable cells [78].
Quantitative Efficacy Data
The following table summarizes data from a study comparing chlorine-based biocides against Escherichia coli.
Table 1: Comparative Efficacy of Chlorine-Based Biocides Against E. coli [78]
| Biocide | Key Planktonic Findings | Biofilm Reduction (log CFU·cm⁻²) | Stability Notes |
|---|---|---|---|
| Sodium Hypochlorite (SH) | Fastest antimicrobial action | Data not specified | Standard stability |
| Neutral Electrolyzed Oxidizing Water (NEOW) | Highest antimicrobial effects, highest ROS formation | 3.26 | Longest decay time (70 days at 5°C) |
| Chlorine Dioxide (CD) | -- | 3.20 | Equivalent to NaDCC |
| Sodium Dichloroisocyanurate (NaDCC) | Highest antimicrobial rate | -- | Equivalent to CD |
Research Reagent Solutions
Table 2: Essential Reagents for Anti-Biofilm Research
| Reagent / Material | Function in Experimentation |
|---|---|
| Crystal Violet (0.1%) | A simple stain used to quantify total biofilm biomass in microtiter plate assays [79]. |
| 96-well Flat-bottom Polystyrene Plates | The standard platform for growing biofilms in a high-throughput manner for screening assays [79]. |
| Neutralizing Buffers (e.g., containing Lecithin, Polysorbate) | Critical for inactivating disinfectants after the contact time to prevent carry-over effects during viability counting [82]. |
| Extracellular Polymeric Substance (EPS) Degrading Enzymes (e.g., DNase, Proteases) | Used to chemically disrupt the biofilm matrix, studying its role in resistance or enhancing biocide penetration [61]. |
| Lipid-based Nanoparticles | Nano-delivery systems that can encapsulate antimicrobials to improve their penetration and retention within biofilms [77]. |
Visualization of Concepts and Workflows
Biofilm Development and Disruption Strategies
Diagram 1: Biofilm lifecycle and disruption.
Mechanism of Nanomaterial Action
Diagram 2: Nanomaterial mechanism of action.
FAQs and Troubleshooting Guide
Q1: How can I improve the reproducibility of microbiome assembly in my model system? A: Achieving high reproducibility, especially in synthetic community (SynCom) experiments, requires strict standardization. A multi-laboratory study demonstrated that consistent results can be achieved by using a common, detailed protocol, centralized reagents, and standardized analysis. Key steps include:
- Standardized Protocols: All participating laboratories should follow identical, detailed written protocols and annotated videos.
- Centralized Reagents: Critical components like the synthetic microbial community inoculum and seeds should be prepared centrally and distributed to all labs to minimize batch effects.
- Uniform Analysis: Sending all samples to a single laboratory for sequencing and metabolomic analysis minimizes technical variation introduced by different analytical platforms [83].
Q2: What are the primary sources of contamination in low-biomass microbiome experiments, and how can I control for them? A: Low-biomass samples are exceptionally vulnerable to contamination, which can lead to misleading results. Key sources and controls include:
- Sources: Contamination can originate from human operators, sampling equipment, laboratory reagents, kits, and cross-contamination between samples during processing [84].
- Controls: It is essential to include multiple negative controls, such as empty collection vessels, swabs of the sampling environment, and aliquots of preservation solutions. These controls must be processed alongside your samples to identify contaminating DNA [84].
- Prevention: Use single-use, DNA-free collection materials where possible. Decontaminate equipment with ethanol followed by a nucleic acid-degrading solution (e.g., bleach). Use personal protective equipment (PPE) like gloves, masks, and clean suits to limit human-derived contamination [84].
Q3: My computational model of microbial dynamics does not forecast future states accurately. How can I improve inference? A: Accurate inference of microbial dynamical systems requires high-quality temporal data and sophisticated modeling approaches.
- Data Requirements: Models require data with high temporal resolution, especially around perturbation events, to capture informative transient behaviors. Measurements of total bacterial concentration (e.g., via qPCR) are also formally necessary for accurate inference of generalized Lotka-Volterra (gLV) models [85].
- Model Selection: Consider using advanced Bayesian inference tools like MDSINE2, which explicitly models measurement noise and stochastic effects in dynamics. A key innovation is the learning of "interaction modules"—groups of taxa with similar interaction patterns—which reduces model complexity and increases interpretability and forecasting accuracy [85].
Q4: How significant is the order of microbial introduction (priority effects) in shaping the final community? A: Priority effects can be a decisive stochastic factor in community assembly. The arrival order of species can create alternative stable community states by enabling early colonizers to pre-empt ecological niches or modify the environment to facilitate later species. The impact of priority effects is often amplified by high niche overlap and phylogenetic relatedness among species. These effects are best studied through controlled experiments that manipulate species arrival history [86].
Q5: Why is it challenging to study microbiome dynamics at the strain level, and what tools can help? A: Observational data alone often lacks the resolution to distinguish strains. Short-read sequencing technologies struggle with repetitive genomic regions, and marker gene evolution is often too slow to resolve strain-level differences. To overcome this:
- Experimental Models: Use gnotobiotic systems (e.g., mice colonized with defined synthetic communities) to mechanistically study the function and impact of specific strains.
- Computational Models: Strain-specific genome-scale metabolic models (GEMs) built from pan-genome data can provide insights into subspecies-level metabolic interactions [86].
Experimental Protocols for Key Methodologies
This protocol outlines a standardized method for studying microbiome assembly in a fabricated ecosystem (EcoFAB).
- Objective: To investigate the reproducible assembly of a synthetic microbial community (SynCom) in the rhizosphere of the model grass Brachypodium distachyon.
- Materials:
- EcoFAB 2.0 devices.
- Sterile growth medium.
- Surface-sterilized Brachypodium distachyon seeds.
- Defined SynCom (e.g., 16- or 17-member community from a public biobank).
- Methodology:
- Device Assembly: Aseptically assemble the EcoFAB 2.0 devices with growth medium.
- Plant Preparation: Dehusk and surface-sterilize seeds. Stratify at 4°C for 3 days, then germinate on agar plates for 3 days.
- Transfer: Transfer seedlings to the EcoFAB device and grow for 4 days.
- Inoculation: Test device sterility, then inoculate the SynCom into the medium (e.g., final density of 1 × 10^5 bacterial cells per plant).
- Growth and Monitoring: Grow plants for 22 days post-inoculation, with periodic water refills and root imaging.
- Sampling: At harvest, collect root and media samples for 16S rRNA amplicon sequencing, metabolomic analysis (LC-MS/MS), and measure plant biomass.
- Troubleshooting Tip: Less than 1% of sterility tests should show microbial growth. If contamination is higher, re-evaluate your aseptic technique during device assembly and inoculation [83].
This protocol describes the workflow for using the MDSINE2 software to learn dynamical systems models from longitudinal microbiome data.
- Objective: To infer a predictive, ecosystems-scale model of microbial interactions and dynamics from timeseries abundance data.
- Materials:
- Timeseries measurements of bacterial relative abundances (e.g., 16S rRNA or shotgun metagenomic count data).
- Timeseries measurements of total bacterial concentrations (from qPCR).
- Associated sample metadata (e.g., timepoints, perturbation status).
- MDSINE2 open-source software package.
- Methodology:
- Data Preparation: Format your timeseries data, total biomass data, and metadata according to MDSINE2 requirements.
- Model Inference: Run MDSINE2 to learn the model from your data. The software will:
- Model measurement noise and stochastic dynamics.
- Automatically infer "interaction modules" of taxa with similar interaction patterns.
- Quantify all parameters and their uncertainties (Bayes factors).
- Model Interpretation: Use the built-in tools to:
- Visualize predicted versus actual taxa trajectories.
- Analyze the topology of the inferred microbial interaction network.
- Quantify the "keystoneness" (ecological importance) of taxa or modules.
- Assess the stability of the microbial ecosystem.
- Troubleshooting Tip: For accurate model inference, ensure your experimental design includes intentional perturbations (e.g., diet change, antibiotics) and is sampled at a high temporal frequency, especially around these perturbations, to capture informative transient dynamics [85].
Data Presentation
Table 1: Quantitative Benchmarks from Reproducibility and Modeling Studies
| Metric | Value / Result | Context / Model System |
|---|---|---|
| Inter-laboratory Variability | Consistent plant phenotype and microbiome assembly across 5 labs | Reproducibility of SynCom experiments in EcoFAB 2.0 devices [83]. |
| Dominant Colonizer Abundance | 98 ± 0.03% average relative abundance of Paraburkholderia sp. | Root microbiome in SynCom17 inoculation treatment [83]. |
| Forecasting Performance (RMSE) | Significantly lower error vs. gLV-L2 and gLV-net methods | MDSINE2 model forecasting on high-temporal-resolution murine data [85]. |
| Strain-Level Colonization | Single strain typically dominates each bacterial species in the gut | Observation from human gut microbiome studies (oligocolonization) [86]. |
Table 2: Research Reagent Solutions for Microbiome Impact Assessment
| Research Reagent / Tool | Function in Experiment |
|---|---|
| Synthetic Microbial Communities (SynComs) | Defined, low-complexity communities that bridge the gap between natural microbiomes and single-strain studies, enabling mechanistic insights into community assembly [83] [86]. |
| EcoFAB 2.0 Device | A standardized, sterile "fabricated ecosystem" that provides a controlled habitat for highly reproducible study of plant-microbe interactions [83]. |
| MDSINE2 Software | A Bayesian computational tool that infers compact, interpretable dynamical systems models from microbiome timeseries data, including interaction modules and stability metrics [85]. |
| Gnotobiotic Mouse Models | Germ-free animals that can be colonized with defined microbial communities, providing an in vivo system to study host-microbe interactions under controlled conditions [85] [86]. |
| DNA Decontamination Solutions | Reagents like sodium hypochlorite (bleach) or commercial DNA removal solutions used to eliminate contaminating DNA from sampling equipment and surfaces in low-biomass studies [84]. |
Workflow and Pathway Visualizations
Microbiome Assessment Workflow
Microbial Dynamics Modeling
Scientific Background and Definitions
What are bifunctional metabolites in the context of antimicrobial research? Bifunctional metabolites are natural or synthetic compounds that exhibit two distinct mechanisms of action: traditional antimicrobial activity (inhibiting growth or killing planktonic cells) and specific anti-biofilm activity (disrupting or preventing biofilm formation through non-microbicidal mechanisms). These compounds are particularly valuable for selective isolation of target microbes because they can disarm virulence mechanisms without necessarily killing the bacteria, thereby reducing selective pressure for resistance development.
How do anti-biofilm activities differ from traditional antibiotic activities? Traditional antibiotics primarily target essential bacterial processes such as cell wall synthesis, protein production, or DNA replication, exerting strong selective pressure that drives resistance development. In contrast, anti-biofilm activities specifically target the biofilm lifecycle without necessarily killing bacteria, including:
- Inhibition of adhesion to surfaces during initial attachment phase
- Interference with quorum sensing (QS) communication systems
- Disruption of extracellular polymeric substance (EPS) production and matrix stability
- Induction of biofilm dispersal from mature structures
- Prevention of virulence factor secretion through systems like Type III Secretion Systems (T3SS)
This distinction is crucial because biofilms demonstrate 10-1,000 times greater tolerance to conventional antibiotics compared to their planktonic counterparts, necessitating alternative strategies [87] [74] [88].
Why are bifunctional metabolites particularly valuable for selective inhibition strategies? Bifunctional metabolites enable researchers to suppress unwanted microbes through multiple mechanisms simultaneously while preserving delicate microbial communities. This approach aligns with the "anti-virulence" strategy that seeks to disarm pathogens without killing them, thereby minimizing selective pressure for resistance development. By targeting biofilm-specific pathways like quorum sensing and EPS production, these compounds can convert pathogenic bacteria into non-pathogenic commensals, allowing the host immune system to clear infections naturally without driving resistance evolution [1] [88].
Troubleshooting Guides
FAQ: Experimental Design and Validation
How should I determine whether a metabolite's activity is truly bifunctional rather than merely antibacterial? To confirm genuine bifunctional activity, you must demonstrate anti-biofilm effects at concentrations below the minimum inhibitory concentration (MIC) for planktonic cells. Follow this experimental validation framework:
- Step 1: Precisely determine MIC and sub-MIC values using standardized broth microdilution methods
- Step 2: Conduct biofilm inhibition assays at concentrations 1/2, 1/4, and 1/8 of the established MIC
- Step 3: Verify reduced biofilm formation via crystal violet staining or confocal microscopy while confirming maintained bacterial viability through ATP assays or colony counting
- Step 4: Specifically quantify biomarkers of biofilm activity (e.g., extracellular DNA, polysaccharides, or quorum sensing molecules) to confirm matrix disruption independent of killing
True bifunctional activity is confirmed when biofilm suppression exceeds 50% at concentrations where planktonic growth reduction is less than 20% [87] [74] [89].
What are the common pitfalls in distinguishing bactericidal from anti-biofilm effects, and how can I avoid them? The most frequent errors include:
- Using overly high concentrations that kill cells rather than specifically disrupt biofilms
- Inadequate controls for viability and metabolic activity within biofilm structures
- Failure to assess multiple timepoints throughout biofilm development
- Overreliance on single assessment methods rather than complementary techniques
Implementation strategy: Always include a known anti-biofilm agent (such as quercetin or tannic acid) as a positive control and verify results with at least two independent assessment methods (e.g., crystal violet staining combined with microscopy) [87] [89].
My biofilm quantification results show high variability between replicates. What could be causing this? High variability typically stems from these technical issues:
- Inconsistent biofilm maturation times between experimental runs
- Temperature fluctuations during the static incubation period
- Variations in surface preparation for biofilm attachment
- Improper washing techniques that either remove too many cells or leave behind non-adherent cells
Standardization protocol: Precisely control incubation temperature (±0.5°C), use validated surface materials (such as specific polystyrene brands), implement standardized washing procedures (volume, flow rate, and duration), and ensure consistent inoculum preparation through optical density verification coupled with colony counting [89] [88].
FAQ: Technical Challenges and Solutions
Why do my biofilm inhibition results not correlate well with anti-virulence gene expression data? This common discrepancy arises from several methodological factors:
- Temporal disconnect between biofilm formation (physical process) and gene expression (rapidly changing)
- Spatial heterogeneity within biofilms where different zones exhibit distinct transcriptional profiles
- Technical limitations of RNA extraction from biofilm matrices leading to biased representation
Resolution approach: Implement time-course experiments with synchronized sampling for both physical measurements and transcriptomics, utilize laser capture microdissection to sample specific biofilm regions, and validate with multiple gene targets across different functional categories (adhesion, quorum sensing, matrix production) [90] [74].
How can I effectively screen for bifunctional activity in natural product extracts with complex compositions? For complex natural extracts, employ this tiered screening strategy:
- Primary screening: Rapid assessment of biofilm inhibition at fixed sub-MIC concentrations using high-throughput methods like microtiter plate assays
- Secondary confirmation: Dose-response evaluation with simultaneous measurement of planktonic growth and biofilm formation
- Mechanistic investigation: Target-specific assays for quorum sensing inhibition, adhesion interference, or EPS disruption
- Bioassay-guided fractionation: Isolation of active components with tracking of both antibacterial and anti-biofilm activities through purification steps
This approach successfully identified bioactive components in Morus leaf extracts, where quercetin and kaempferol glycosides correlated with antibiofilm activity independent of direct antibacterial effects [89].
Experimental Protocols and Methodologies
Standardized Biofilm Inhibition Assay
Purpose: To quantitatively measure a compound's ability to prevent biofilm formation at sub-inhibitory concentrations.
Materials:
- Sterile 96-well flat-bottom polystyrene plates
- Trypticase Soy Broth (TSB) supplemented with 0.5% glucose
- Crystal violet staining solution (0.1% w/v)
- Acetic acid (30% v/v) for dye solubilization
- Microplate reader capable of measuring OD570nm and OD600nm
Procedure:
- Prepare test compound dilutions in TSB+0.5% glucose across the plate, ensuring concentrations range from 1/2 to 1/16 of predetermined MIC
- Inoculate wells with bacterial suspension standardized to 1×10^6 CFU/mL
- Incubate stationary for 24-48 hours at appropriate growth temperature (typically 37°C)
- Carefully aspirate planktonic cells and gently wash wells with phosphate buffered saline (PBS)
- Air-dry plates and stain with crystal violet for 15 minutes
- Wash excess stain and solubilize bound dye with acetic acid
- Measure OD570nm for biofilm quantification and OD600nm from separate wells for parallel growth assessment
Calculation: % Biofilm Inhibition = [1 - (OD570 sample / OD570 untreated control)] × 100 % Growth Inhibition = [1 - (OD600 sample / OD600 untreated control)] × 100
True anti-biofilm activity is indicated when % Biofilm Inhibition > % Growth Inhibition, particularly at lower concentrations [89].
Quorum Sensing Inhibition Bioassay
Purpose: To specifically assess interference with bacterial cell-to-cell communication systems.
Materials:
- Reporter strains responsive to acyl-homoserine lactone (AHL) signals
- Appropriate growth medium with necessary antibiotics for selection
- Positive control autoinducer compounds
- Microplate fluorometer or luminometer for quantification
Procedure:
- Culture reporter strains to mid-log phase in appropriate selective medium
- Mix bacterial suspension with sub-MIC concentrations of test compounds
- Add known concentrations of relevant autoinducer molecules
- Incubate with shaking for specific duration (typically 4-6 hours)
- Measure fluorescence/ luminescence output indicating quorum sensing activation
- Compare signal reduction relative to untreated controls with autoinducers
Interpretation: Significant reduction in reporter signal without corresponding growth inhibition indicates specific quorum quenching activity, a key anti-biofilm mechanism of many bifunctional metabolites [87] [74].
Data Presentation and Analysis
Quantitative Comparison of Selected Bifunctional Metabolites
Table 1: Efficacy Parameters of Characterized Bifunctional Metabolites
| Metabolite | Source | Anti-biofilm MIC (μg/mL) | Planktonic MIC (μg/mL) | Primary Anti-biofilm Mechanism | Key Target Organisms |
|---|---|---|---|---|---|
| Quercetin | Morus nigra, onions | 32-64 | 128-256 | Quorum sensing inhibition, EPS disruption | P. aeruginosa, E. faecalis |
| Cinnamtannin B1 | Lindera obtusiloba | 25-50 | >200 | Selective T3SS inhibition, YopH/YopO suppression | Y. enterocolitica |
| Apigenin | Chamomile, parsley | 64-128 | 256-512 | Adhesion interference, QS suppression | S. aureus, Escherichia coli |
| Gallic acid | Gallnuts, tea leaves | 128-256 | 512->1024 | EPS reduction, matrix integrity disruption | Mixed species biofilms |
| Morus nigra extract | Mulberry leaves | 125* | 500* | Multi-target: QS, adhesion, matrix synthesis | E. faecalis biofilms |
*Values represent extract concentration in μg/mL [87] [89] [1]
Research Reagent Solutions for Bifunctional Metabolite Studies
Table 2: Essential Research Materials and Their Applications
| Reagent/Category | Specific Examples | Research Function | Technical Notes |
|---|---|---|---|
| Biofilm Assessment Dyes | Crystal violet, SYTO stains, Concanavalin A-FITC | Matrix quantification, viability staining, EPS visualization | Combine multiple stains for matrix composition analysis |
| Quorum Sensing Reporters | AHL-responsive E. coli, P. aeruginosa lasB-gfp | Specific detection of QS interference | Validate with known QS inhibitors as controls |
| Natural Product Standards | Quercetin, rutin, cinnamtannin B1, apigenin | Reference compounds for activity comparison | Source from reputable suppliers with HPLC verification |
| Surface Materials | Polystyrene, silicone, titanium coupons | Assessment of biofilm formation on clinically relevant surfaces | Standardize surface pretreatment protocols |
| Matrix Disruption Enzymes | DNase I, dispersin B, proteinase K | Positive controls for specific disruption mechanisms | Use to differentiate mechanical vs. enzymatic disruption |
Visualization of Concepts and Workflows
Selective Inhibition of Virulence Pathways
Experimental Workflow for Bifunctional Assessment
Conclusion
Selective inhibition represents a paradigm shift in microbial control, moving from indiscriminate eradication to precision targeting. This approach, exemplified by agents like the staphylococcus-selective Debio 1452 and the anti-curli metabolite bacillaene, offers a dual benefit: effectively controlling target pathogens while minimizing collateral damage to the microbiome and reducing selection pressure for broad resistance. The successful application of this strategy hinges on a multidisciplinary pipeline that integrates foundational knowledge of microbial interactions, robust methodological screening, careful troubleshooting of economic and resistance challenges, and rigorous comparative validation. Future progress depends on incentivizing antibiotic R&D, exploring underutilized sources like human gut-derived microbes, and developing combination therapies that integrate selective agents with diagnostics. By advancing these precision tools, researchers can forge a more sustainable path in the fight against antimicrobial resistance, ultimately protecting the efficacy of our current antibiotics and supporting the viability of modern medicine.
References
- 1. Selective Inhibition of Yersinia enterocolitica Type III ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12473489/]
- 2. Selective inhibition of the amyloid matrix of Escherichia coli ... [https://www.nature.com/articles/s41522-023-00449-6]
- 3. Broad vs Narrow Spectrum Drugs: Videos & Practice Problems [https://www.pearson.com/channels/microbiology/learn/jason/28-antimicrobial-drugs/broad-vs-narrow-spectrum-drugs]
- 4. Modelling the implementation of narrow versus broader ... [https://www.nature.com/articles/s41598-024-66193-9]
- 5. Selective inhibition of human translation termination by a ... [https://www.nature.com/articles/s41467-020-18765-2]
- 6. Molecular Modelling Study and Antibacterial Evaluation of ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10095751/]
- 7. Structural and enzymatic analyses reveal the binding mode ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC3386789/]
- 8. Investigating the structure-activity-relationship of diaryl ... [https://www.sciencedirect.com/science/article/abs/pii/S0223523425005471]
- 9. Bacterial culture through selective and non- ... [https://www.sciencedirect.com/science/article/pii/S2052297519301192]
- 10. Selective toxicity of antibacterial agents—still a valid ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC7851017/]
- 11. An overview of the antimicrobial resistance mechanisms ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC6604941/]
- 12. The bactericidal FabI inhibitor Debio 1453 clears antibiotic ... [https://www.nature.com/articles/s41467-025-63508-w]
- 13. The bactericidal FabI inhibitor Debio 1453 clears antibiotic- ... [https://pubmed.ncbi.nlm.nih.gov/40968127/]
- 14. Current economic and regulatory challenges in developing antibiotics for Gram-negative bacteria | npj Antimicrobials and Resistance [https://www.nature.com/articles/s44259-025-00123-1]
- 15. Antibiotics re-booted—time to kick back against drug ... [https://www.nature.com/articles/s44259-025-00096-1]
- 16. Challenges of Antibacterial Discovery - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC3021209/]
- 17. WHO warns of widespread resistance to common ... [https://www.paho.org/en/news/13-10-2025-who-warns-widespread-resistance-common-antibiotics-worldwide]
- 18. Sharp global rise in antibiotic-resistant infections in hospitals, WHO finds | World Health Organization | The Guardian [https://www.theguardian.com/world/2025/oct/13/sharp-global-rise-in-antibiotic-resistant-infections-in-hospitals-who-finds]
- 19. Communication between gut microbiota-derived metabolites ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12568434/]
- 20. Immunomodulatory role of gut microbial metabolites [https://www.frontiersin.org/journals/microbiology/articles/10.3389/fmicb.2025.1675065/full]
- 21. Selection and transmission of the gut microbiome alone ... [https://www.nature.com/articles/s41467-025-65368-w]
- 22. Antimicrobial strategy for targeted elimination of different ... [https://www.nature.com/articles/s42003-022-03586-4]
- 23. Methods for screening and evaluation of antimicrobial activity [https://pmc.ncbi.nlm.nih.gov/articles/PMC11097785/]
- 24. Current Screening Methodologies in Drug Discovery for ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC6117650/]
- 25. BIOLUMINESCENCE INHIBITION ASSAY FOR THE ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC4127403/]
- 26. Bioluminescence Assay Platform for Selective and ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC3465522/]
- 27. A Comprehensive Exploration of Bioluminescence Systems ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10861286/]
- 28. Harnessing AI for enhanced screening of antimicrobial ... [https://www.sciencedirect.com/science/article/abs/pii/S0924224425000238]
- 29. Flow Cytometry Troubleshooting Guide [https://www.cellsignal.com/learn-and-support/troubleshooting/flow-cytometry-troubleshooting-guide?srsltid=AfmBOorEc9lZ9sCcUarINOziwy5WBZnxh_C8TqWive2QV4oaAIaPWSl1]
- 30. Optimization of the Blocking and Signal Preservation ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12462741/]
- 31. Specimen Collection Practices for Microbiologic Culture [https://health.ucdavis.edu/blog/lab-best-practice/specimen-collection-practices-for-microbiologic-culture/2020/07]
- 32. Five Tips for Culture Media Preparation Success [https://www.thermofisher.com/blog/food/five-tips-for-culture-media-preparation-success/]
- 33. Culture performance of Fastidious Anaerobe Agar for ... [https://www.sciencedirect.com/science/article/pii/S1075996425000356]
- 34. Culture performance of Fastidious Anaerobe Agar for ... [https://pubmed.ncbi.nlm.nih.gov/40398807/]
- 35. 9 Tips for Growth Promotion Testing on Selective Media [https://blog.microbiologics.com/9-tips-for-growth-promotion-testing-on-selective-media/]
- 36. 6.3C: Selective and Differential Media [https://bio.libretexts.org/Bookshelves/Microbiology/Microbiology_(Boundless)/06%3A_Culturing_Microorganisms/6.03%3A_Culturing_Bacteria/6.3C%3A_Selective_and_Differential_Media]
- 37. How to spare gut microbiota from antibiotic effects? PK-PD ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12459201/]
- 38. How to Master the Microbiome: Sample Collection [https://www.zymoresearch.de/blogs/blog/how-to-master-the-microbiome-sample-collection]
- 39. Microbiological Analysis Support—Troubleshooting [https://www.thermofisher.com/us/en/home/technical-resources/technical-reference-library/cell-analysis-support-center/microbiological-analysis-support/microbiological-analysis-support-troubleshooting.html]
- 40. A Gram-negative-selective antibiotic that spares the gut ... [https://www.nature.com/articles/s41586-024-07502-0]
- 41. Potential next generation targets for antibacterial agent's ... [https://www.sciencedirect.com/science/article/abs/pii/S0223523425009535]
- 42. TaxiBGC: a Taxonomy-Guided Approach for Profiling ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC9765181/]
- 43. Metagenomic Sequencing Data: Step-by-Step Guide From ... [https://www.cd-genomics.com/resource-how-analyze-metagenomic-sequencing-data.html]
- 44. Isolation, antibacterial screening, and identification of ... [https://www.frontiersin.org/journals/microbiology/articles/10.3389/fmicb.2022.1012867/full]
- 45. Species-level functional profiling of metagenomes and ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC6235447/]
- 46. Secondary metabolite biosynthetic gene clusters and ... [https://www.nature.com/articles/s41598-025-03467-w]
- 47. Co-selection for antibiotic resistance by environmental ... [https://www.nature.com/articles/s44259-024-00026-7]
- 48. Co-Selection of Resistance to Antibiotics, Biocides and Heavy ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC4790313/]
- 49. Overview Perspective of Bacterial Strategies of Resistance ... [https://brieflands.com/journals/archcid/articles/65744]
- 50. Co-occurrence of resistance genes to antibiotics, biocides and ... [https://bmcgenomics.biomedcentral.com/articles/10.1186/s12864-015-2153-5]
- 51. Biocidal Resistance in Clinically Relevant Microbial Species [https://pmc.ncbi.nlm.nih.gov/articles/PMC8156472/]
- 52. Reviewing the complexities of bacterial biocide ... [https://www.nature.com/articles/s44259-025-00108-0]
- 53. Biocides as drivers of antibiotic resistance: A critical review ... [https://www.sciencedirect.com/science/article/pii/S2666498425000353]
- 54. Antibiotic resistance: The challenges and some emerging ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC9459344/]
- 55. Challenges and opportunities for incentivising antibiotic ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10403717/]
- 56. Industry incentives and antibiotic resistance [https://www.nature.com/articles/s41429-020-0300-y]
- 57. A systematic review and critical assessment of incentive strategies for discovery and development of novel antibiotics | The Journal of Antibiotics [https://www.nature.com/articles/ja201598]
- 58. Towards the sustainable discovery and development of new antibiotics | Nature Reviews Chemistry [https://www.nature.com/articles/s41570-021-00313-1]
- 59. Incentivising innovation in antibiotic drug discovery and development: progress, challenges and next steps | The Journal of Antibiotics [https://www.nature.com/articles/ja2017124]
- 60. Addressing the global challenge of bacterial drug resistance [https://www.frontiersin.org/journals/microbiology/articles/10.3389/fmicb.2025.1517772/full]
- 61. Biofilms: structure, resistance mechanism, emerging control ... [https://pubs.rsc.org/en/content/articlehtml/2025/pm/d5pm00094g]
- 62. Nanoparticles Targeting Biofilms: A New Era in Combating ... [https://www.sciencedirect.com/science/article/pii/S2590097825000370]
- 63. integrating CRISPR/Cas9 and nanoparticles against biofilm ... [https://bmcmedicine.biomedcentral.com/articles/10.1186/s12916-025-04323-4]
- 64. Strategies for biofilm inhibition: the role of synthetic drug [https://pubmed.ncbi.nlm.nih.gov/41269277/]
- 65. A guide to picking the most selective kinase inhibitor tool ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC3417414/]
- 66. A Pathogen-Selective Antibiotic Minimizes Disturbance to ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC4914625/]
- 67. Engineering the Microbiome to Prevent Adverse Events [https://pmc.ncbi.nlm.nih.gov/articles/PMC9015100/]
- 68. Microbiota-mediated protection against antibiotic-resistant ... [https://www.nature.com/articles/s41435-021-00129-5]
- 69. 13.5A: Minimal Inhibitory Concentration (MIC) [https://bio.libretexts.org/Bookshelves/Microbiology/Microbiology_(Boundless)/13%3A_Antimicrobial_Drugs/13.05%3A_Measuring_Drug_Susceptibility/13.5A%3A_Minimal_Inhibitory_Concentration_(MIC)]
- 70. The Minimum Inhibitory Concentration of Antibiotics [https://pmc.ncbi.nlm.nih.gov/articles/PMC7913839/]
- 71. Resistance Modulation Action, Time-Kill Kinetics Assay, ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC6899278/]
- 72. Protocol to quantify bacterial burden in time-kill assays ... [https://www.sciencedirect.com/science/article/pii/S2666166725000498]
- 73. Time-kill kinetics assay. [https://bio-protocol.org/exchange/minidetail?id=4874664&type=30]
- 74. Strategies for combating bacterial biofilms: A focus on anti ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC5955472/]
- 75. Advantages and limitations of microtiter biofilm assays in ... [https://www.nature.com/articles/s41598-020-77198-5]
- 76. Bacterial Biofilm Inhibition: A Focused Review on Recent ... [https://www.frontiersin.org/journals/microbiology/articles/10.3389/fmicb.2021.676458/full]
- 77. Nanomaterial-enabled anti- biofilm strategies: new opportunities for... [https://pubs.rsc.org/en/content/articlehtml/2025/nr/d4nr04774e]
- 78. stability and Comparative of efficacy chlorine-based... selected [https://pubmed.ncbi.nlm.nih.gov/29195980/]
- 79. Integrative experimental and computational dataset for ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12446609/]
- 80. Frontiers | Ultrasonic strategies for mitigating microbial adhesion and... [https://www.frontiersin.org/journals/microbiology/articles/10.3389/fmicb.2025.1558035/full]
- 81. A review of research advances on disinfection strategies ... [https://www.sciencedirect.com/science/article/pii/S0043135424001751]
- 82. Comparison of the Efficiency of Selected Disinfectants ... [https://www.mdpi.com/2076-2607/11/6/1593/review_report]
- 83. Breaking the reproducibility barrier with standardized ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12416739/]
- 84. Guidelines for preventing and reporting contamination in ... [https://www.nature.com/articles/s41564-025-02035-2]
- 85. Learning ecosystem-scale dynamics from microbiome data ... [https://www.nature.com/articles/s41564-025-02112-6]
- 86. Experimental systems are essential for strengthening ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12363228/]
- 87. Potential Use of Selected Natural Compounds with Anti- ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11765509/]
- 88. Strategies for combating bacterial biofilm infections [https://www.nature.com/articles/ijos201465]
- 89. Comparative metabolite profiling of four polyphenol rich ... [https://www.nature.com/articles/s41598-022-24382-4]
- 90. Strategies for combating antibiotic resistance in bacterial ... [https://www.frontiersin.org/journals/cellular-and-infection-microbiology/articles/10.3389/fcimb.2024.1352273/full]