Substrate Control as an Anti-Persister Strategy: Disrupting Metabolic Dormancy to Combat Chronic Infections
This article explores the critical role of substrate availability in the formation and survival of bacterial persister cells, a major cause of chronic and relapsing infections.
Substrate Control as an Anti-Persister Strategy: Disrupting Metabolic Dormancy to Combat Chronic Infections
Abstract
This article explores the critical role of substrate availability in the formation and survival of bacterial persister cells, a major cause of chronic and relapsing infections. We synthesize foundational research and recent advances demonstrating that nutrient limitation is a key environmental trigger driving phenotypic switching to the dormant, antibiotic-tolerant persister state. The content details methodological approaches for quantifying substrate-dependent persister dynamics, including computational modeling and stable isotope tracing. It further examines practical strategies for optimizing substrate environments to prevent persister formation and enhance the efficacy of conventional antibiotics. By integrating foundational knowledge with application-focused and comparative analyses, this resource provides researchers and drug development professionals with a comprehensive framework for developing novel therapeutic interventions that target the metabolic vulnerabilities of persistent pathogens.
The Metabolic Basis of Bacterial Persistence: How Nutrient Cues Drive Dormancy
Fundamental Concepts: Persistence, Tolerance, and Resistance
What is the fundamental difference between a persister cell and a genetically resistant bacterium?
The core distinction lies in the heritability and mechanism of survival. Persister cells are a sub-population of genetically normal, drug-susceptible bacteria that survive antibiotic treatment by entering a transient, dormant state. Their offspring are fully susceptible once the antibiotic is removed. In contrast, genetically resistant bacteria possess inherited genetic mutations that allow them to grow in the presence of the antibiotic, and their offspring inherit this resistance [1] [2] [3].
The table below summarizes the key differentiating characteristics.
Table 1: Key Characteristics Differentiating Antibiotic Resistance, Tolerance, and Persistence
| Characteristic | Genetic Resistance | Tolerance (General) | Persistence (A Subset of Tolerance) |
|---|---|---|---|
| Definition | Inherited ability to grow in the presence of an antibiotic. | Ability to survive a transient exposure to a bactericidal antibiotic without growing. | A phenotypic variant within an isogenic population that survives antibiotic treatment by entering a dormant state. |
| Underlying Mechanism | Genetic mutations (e.g., drug target modification, efflux pumps, enzyme inactivation). | Slower overall death rate of the entire population, often linked to slow growth. | Non-growing or slow-growing dormancy of a small subpopulation. |
| Minimum Inhibitory Concentration (MIC) | Increased | Unchanged | Unchanged |
| Killing Kinetics | Can grow at antibiotic concentrations above the MIC of susceptible cells. | The entire population dies slower than a susceptible population. | Biphasic killing curve: rapid killing of most cells, followed by a subpopulation (persisters) that dies very slowly. |
| Heritability | Stable and heritable across generations. | Can be a heritable trait of the entire strain or a non-heritable, transient phenotype. | Transient and non-heritable; the progeny of persisters are as susceptible as the original population. |
| Percentage in Population | Can be 100% of the population. | 100% of the population exhibits the trait. | Typically a very small fraction (e.g., 0.001% - 1%) [4] [3]. |
What is the relationship between antibiotic tolerance and persister cells?
The terms are often used interchangeably but have a specific relationship. Tolerance describes the general phenomenon of surviving an antibiotic treatment without growing. Persistence is a specific form of tolerance that refers to the small, dormant subpopulation responsible for the biphasic killing pattern observed in an otherwise susceptible culture [3]. All persisters are tolerant, but not all tolerance is due to persistence (e.g., an entire population could be tolerant due to slow growth in stationary phase).
Core Molecular Mechanisms and Experimental Workflows
What are the primary molecular mechanisms driving persister cell formation?
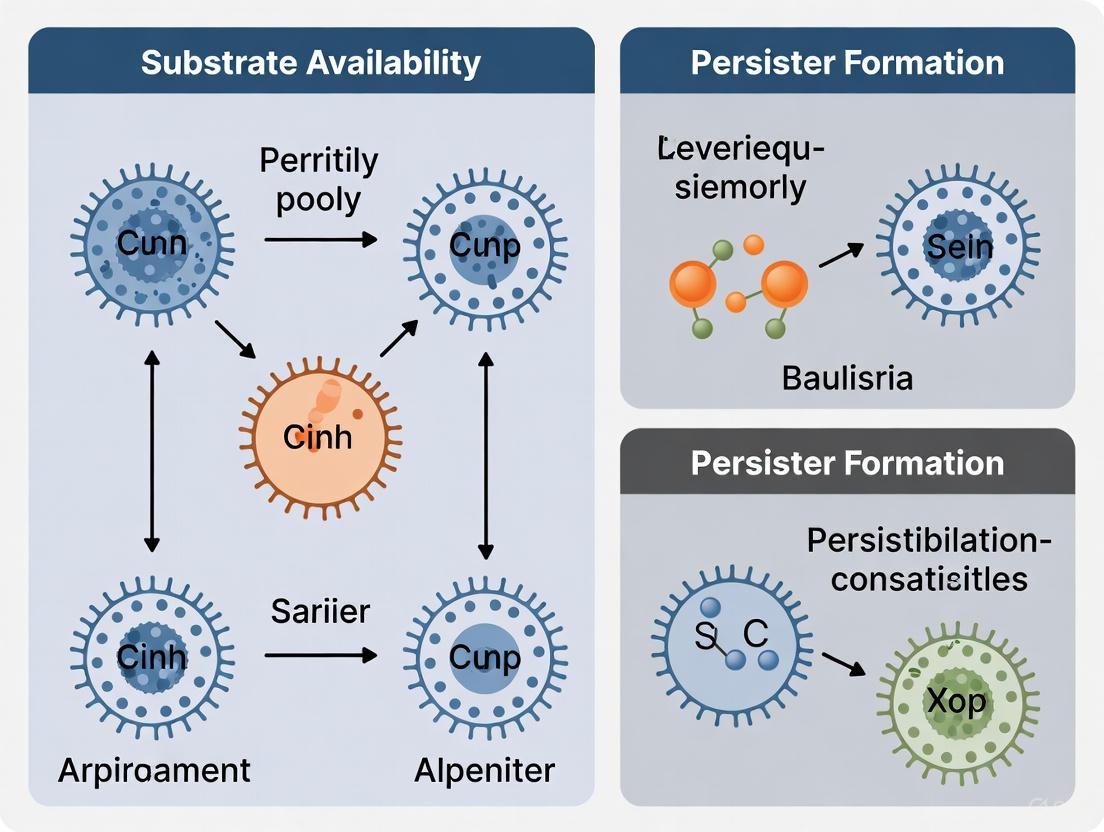
Persister formation is not governed by a single mechanism but by a network of interconnected biological processes that lead to cellular dormancy. The major pathways are illustrated below and detailed thereafter.
Diagram 1: Key pathways to persister formation.
A. Toxin-Antitoxin (TA) Modules
TA systems are genetic loci encoding a stable "toxin" and an unstable "antitoxin." Under stress, the antitoxin is degraded, allowing the toxin to act on targets such as translation or membrane potential, inducing growth arrest [2] [3]. For example, in E. coli, the HipA toxin phosphorylates a tRNA synthetase, leading to a halt in protein synthesis and promoting persistence [1] [3].
B. The Stringent Response and (p)ppGpp
Nutrient starvation triggers the stringent response, mediated by the alarmone (p)ppGpp. This signaling molecule acts as a global regulator that dramatically reprograms cellular metabolism, shutting down energy-intensive processes like ribosome synthesis and promoting a dormancy-like state [2].
C. Biofilms
Biofilms are structured communities of bacteria encased in a self-produced extracellular matrix. The biofilm environment creates gradients of nutrients and oxygen, leading to heterogeneous metabolic states. Bacteria in the inner, nutrient-poor regions of a biofilm often enter a dormant state, making biofilms a major reservoir for persister cells [5] [2]. It is estimated that over 65% of all infections are associated with biofilms [5].
D. The SOS Response
Antibiotics that cause DNA damage (e.g., fluoroquinolones) can induce the SOS response, a coordinated DNA repair system. This response can also lead to cell cycle arrest and promote the formation of persister cells [5] [2].
What is a standard experimental workflow for isolating and studying persister cells?
The most common method for quantifying persisters is the biphasic killing assay, which leverages their defining characteristic of antibiotic tolerance followed by regrowth upon drug removal. The workflow is as follows [6] [3].
Diagram 2: Workflow for a persister killing assay.
The Scientist's Toolkit: Key Reagents & Models
Table 2: Essential Research Reagents and Model Systems for Persister Studies
| Reagent / Model | Function / Rationale | Example Use-Case |
|---|---|---|
| High-Persister (Hip) Mutants | Genetically engineered or selected strains that produce a higher frequency of persisters, facilitating their study. | E. coli hipA7 mutants are widely used to study Type II (stochastic) persistence and to screen for anti-persister compounds [1] [7]. |
| Biphasic Killing Assay | The gold-standard method for detecting and quantifying persister cells based on their unique killing kinetics [6]. | Used to demonstrate the tolerance of a bacterial subpopulation to high doses of ciprofloxacin or ampicillin. |
| Stationary Phase Cultures | An enrichment method for Type I (triggered) persisters, which are more abundant in the stationary phase [4]. | Isolating persisters from an overnight culture without the need for genetic mutants. |
| In Vitro Biofilm Models | Systems (e.g., flow cells, microtiter plates) to study persisters in a clinically relevant, biofilm-associated context. | Testing the efficacy of antimicrobial agents against P. aeruginosa biofilms grown on a catheter-like substrate [5]. |
| Uropathogenic E. coli (UPEC) | A clinically relevant model for studying chronic and recurrent infections linked to persisters. | Evaluating drug penetration and killing of persisters within bladder cells or biofilms [7]. |
Troubleshooting Guide & FAQs
FAQ 1: During the killing assay, my entire population dies and I see no persister "tail." What could be wrong?
- Problem: Incorrect antibiotic choice or concentration.
- Solution: Ensure you are using a bactericidal antibiotic (e.g., fluoroquinolones, aminoglycosides, β-lactams) at a concentration significantly above the MIC (e.g., 10x to 100x MIC). Bacteriostatic antibiotics will not produce a biphasic killing curve. Verify the MIC for your specific strain and growth conditions [6].
- Problem: Cell density is too low.
- Solution: The persister fraction is very small. Start with a sufficiently dense culture (e.g., >10^8 CFU/mL) to ensure a detectable number of persisters remain after antibiotic treatment.
- Problem: Antibiotic degradation or instability.
- Solution: Prepare fresh antibiotic solutions and confirm stability under your experimental conditions (e.g., temperature, pH).
- Problem: Stochastic nature of persistence.
- Solution: This is a known challenge. Type II persisters form spontaneously, leading to inherent variability. Increase the number of biological replicates (e.g., n ≥ 5) to achieve statistical power. Use tightly controlled and consistent growth conditions (media, temperature, shaking speed, growth phase) for all experiments [4].
- Problem: Inconsistent preparation of "stationary phase" cultures.
- Solution: Precisely define the stationary phase by growth time and optical density (OD). Using cultures that are too old may enter the death phase and skew results.
FAQ 3: How can I distinguish between a true persister and a resistant mutant?
- Problem: Uncertainty in interpreting surviving colonies.
- Solution: Perform a re-challenge experiment. Isolate colonies that survive the initial antibiotic treatment. Re-grow them in fresh, drug-free medium, and then subject the new culture to the same antibiotic. A population derived from true persisters will show the same biphasic killing pattern as the original culture. A population derived from a resistant mutant will grow in the presence of the antibiotic or show a monophasic killing curve with a much higher MIC [3].
Connecting to Your Thesis: Optimizing Substrate Availability to Prevent Persister Formation
The research context of optimizing substrate availability is directly targeted at a core mechanism of persistence. The following diagram and table outline the logical framework and potential experimental approaches for this research.
Diagram 3: Substrate availability impacts persistence.
Table 3: Experimental Approaches to Link Substrate Availability and Persistence
| Research Question | Experimental Strategy | Expected Outcome & Interpretation |
|---|---|---|
| Does specific nutrient limitation (e.g., carbon, nitrogen) increase persister levels? | Grow cultures in defined media with and without specific nutrient limitations. Perform biphasic killing assays. | Expected: Limitation of a key nutrient increases the persister fraction. Interpretation: Specific substrate starvation induces a protective dormancy response. |
| Can supplementing a specific metabolite "awaken" persisters and re-sensitize them to antibiotics? | Isolate persisters via antibiotic treatment, then re-suspend them in fresh media containing the metabolite of interest plus a second antibiotic. | Expected: Metabolite supplementation (e.g., sugars, amino acids) enhances killing by the second antibiotic. Interpretation: The metabolite reactivates metabolism, corrupting antibiotic targets. This is the basis for "anti-persister" strategies [8]. |
| Does optimized substrate availability prevent the induction of high-persister (Hip) mutants? | Passage wild-type strains in nutrient-rich vs. nutrient-limited media under intermittent antibiotic pressure. Monitor the emergence of Hip mutants. | Expected: Hip mutants are selected for more readily in nutrient-limited environments. Interpretation: Substrate optimization reduces the selective advantage of the persister phenotype. |
Substrate Limitation as a Primary Trigger for Persister Formation
FAQs: Understanding the Core Concepts
Q1: What is the fundamental link between substrate limitation and persister cell formation? Substrate limitation, particularly the depletion of a primary carbon source, acts as an environmental stress signal that triggers a subset of bacterial cells to enter a dormant, persistent state. This state is characterized by drastically reduced metabolic activity and growth arrest, which allows these cells to survive exposure to bactericidal antibiotics that typically target active cellular processes. The transition is mediated by sophisticated stress response pathways within the cell [9] [10].
Q2: How does substrate limitation-induced persistence differ from antibiotic resistance? Unlike genetic antibiotic resistance, persistence is a reversible, phenotypic tolerance. Persister cells do not possess genetic mutations that make antibiotics ineffective. Instead, their dormant state makes them less vulnerable because antibiotics often corrupt active cellular functions like cell wall synthesis or protein translation. Once the stressful condition (e.g., substrate limitation) passes and growth resumes, the new population remains genetically susceptible to the same antibiotics [1] [11].
Q3: What are the key molecular mechanisms connecting nutrient stress to the persister state? The primary pathway involves:
- The Stringent Response: Upon substrate exhaustion, uncharged tRNAs accumulate, activating the RelA enzyme to produce the alarmone (p)ppGpp [11] [12] [9].
- Toxin-Antitoxin (TA) Systems: High levels of (p)ppGpp can stimulate Lon protease to degrade labile antitoxins, freeing toxins (often mRNA-degrading enzymes) that further inhibit growth and promote dormancy. Key systems include HipBA, MqsR/MqsA, and TisB/IstR-1 [11] [9].
- Ribosome Hibernation: (p)ppGpp also promotes the production of factors like RMF and HPF, which inactivate ribosomes, halting protein synthesis and cementing the dormant state [9].
Q4: In a biofilm, where are substrate-limited persisters most likely to form? In biofilms, substrate gradients are naturally established. Substrate concentration decreases from the biofilm-bulk fluid interface toward the substratum. Consequently, substrate-limited persisters are predominantly located in the inner depths of the biofilm, where nutrient access is most restricted, rather than at the well-nourished surface [13] [10].
Troubleshooting Guides: Common Experimental Challenges
Challenge 1: Inconsistent Persister Yields in Batch Cultures
Problem: Difficulty obtaining reproducible subpopulations of persister cells between experiments. Solution:
- Precisely Control Growth Phase: The proportion of persisters increases as a culture transitions from exponential to stationary phase. Use the culture's optical density (OD) and substrate concentration monitoring to standardize the harvesting point [11].
- Define Substrate Limitation: Instead of using vague "stationary phase" cultures, directly measure and define the trigger point. For example, in a glucose-limited experiment, confirm glucose exhaustion with a glucose assay kit. This provides a consistent and measurable trigger for persister formation [12].
- Standardize Inoculum Age: The age of the inoculum can significantly affect persister levels. Always use an inoculum of the same physiological age and growth history to improve reproducibility [11].
Challenge 2: Differentiating Between Slow Growth and True Dormancy
Problem: Determining if cells are genuine, non-growing persisters or merely slow-growers. Solution:
- Employ Fluorescent Reporter Systems: Use a stable fluorescent protein (e.g., GFP) under the control of a ribosomal promoter. Genuine persisters will exhibit dim or absent fluorescence due to halted ribosome activity and protein synthesis. These cells can be isolated and quantified using Fluorescence-Activated Cell Sorting (FACS) [11] [9].
- Conduct Kill Curve Assays: Treat the population with a high concentration of a bactericidal antibiotic. A biphasic killing curve—a rapid initial drop (death of susceptible cells) followed by a stable, flat plateau (indicating non-killing of persisters)—is a hallmark of a persister subpopulation [14].
Challenge 3: Accounting for Environmental Factors in Biofilm Persistence
Problem: Biofilm persister dynamics are complex and influenced by multiple, fluctuating factors. Solution:
- Utilize Computational Modeling: Implement Individual-Based Models (IBMs) to simulate biofilm growth and persister formation. These models can account for spatial heterogeneity in substrate concentration and help distinguish between different persister formation strategies (e.g., stochastic vs. substrate-dependent) [14] [13].
- Measure Local Microenvironments: If technically feasible, use microsensors to directly measure substrate (e.g., oxygen, glucose) gradients within the biofilm. This provides empirical data to correlate with observed persister locations [10].
The table below summarizes key quantitative findings from computational and experimental studies on substrate limitation and persistence.
Table 1: Quantitative Data on Substrate Limitation and Persister Dynamics
| Parameter | Experimental System | Key Finding | Citation |
|---|---|---|---|
| Biofilm Killing Time | Mathematical model of a 300μm biofilm | Time for 6-log reduction increased from 13 hours (8 mg/L substrate) to 66 hours (1 mg/L substrate). | [10] |
| Persister Location | Computational model (IBM) | Substrate-dependent persisters form primarily in the inner, nutrient-deprived regions of the biofilm. | [13] |
| Metabolic State | E. coli with ribosomal GFP promoter | Persister cells showed dim fluorescence, confirming downregulation of ribosomal activity and translation. | [9] |
| Switching Strategy Impact | Computational model comparing strategies | Substrate-dependent switching allowed high persister formation rates (a_max) without penalizing overall biofilm growth. | [13] [15] |
Key Experimental Protocols
Protocol 1: Inducing Persisters via Carbon Source Transition
This protocol is based on the discovery that carbon source transitions are a potent trigger for fluoroquinolone persister formation in E. coli [12].
- Grow cultures to mid-exponential phase in a rich medium containing a readily usable carbon source (e.g., 0.2% glucose).
- Trigger substrate limitation by harvesting cells via centrifugation and resuspending them in a minimal medium with a poor carbon source or by allowing them to naturally exhaust the primary carbon source. Monitor growth and carbon concentration to confirm the transition point.
- Incubate the substrate-limited culture for a defined period (e.g., 1-2 hours) to allow the persistence state to establish.
- Treat with antibiotic (e.g., a fluoroquinolone like ofloxacin) at a high concentration (e.g., 10x MIC) for a set duration.
- Quantify persisters by washing the antibiotic-treated culture to remove the drug, serially diluting it, and plating on fresh rich medium to count the Colony Forming Units (CFUs) of surviving cells that can regrow.
Protocol 2: Computational Modeling of Substrate-Dependent Persistence
This methodology uses agent-based modeling to study persister dynamics in biofilms [14] [13].
- Define the virtual environment: Create a 2D grid representing a surface, with a bulk liquid above it from which a growth-limiting substrate diffuses.
- Initialize bacterial agents: Place a small number of susceptible bacterial cells randomly on the surface.
- Set growth rules: Model bacterial growth using Monod kinetics, where the local growth rate of a cell is determined by the local substrate concentration.
- Implement phenotypic switching rules:
- Substrate-dependent switching: A susceptible cell switches to a persister state with a probability that increases as the local substrate concentration decreases. A persister cell switches back to susceptible when local substrate is abundant.
- Introduce antibiotic: Simulate the diffusion of an antibiotic into the biofilm and define differential killing rates for susceptible (high death rate) and persister (low or zero death rate) cells.
- Run simulations and analyze: Output data on biofilm size, persister number and location over time, and population recovery after antibiotic removal.
Signaling Pathway and Experimental Workflow Diagrams
Molecular Signaling Pathway from Substrate Limitation to Persistence
Experimental Workflow for Substrate-Limitation Studies
The Scientist's Toolkit: Research Reagent Solutions
Table 2: Essential Reagents and Tools for Studying Substrate-Limited Persistence
| Item | Function/Description | Application Example |
|---|---|---|
| Controlled Bioreactors | Systems for precise control and monitoring of growth parameters (pH, dissolved O₂, substrate feed). | Maintaining defined, steady-state substrate concentrations to study persistence triggers. |
| Microsensors (e.g., O₂, Glucose) | Needle-type sensors for measuring microscale gradients within biofilms. | Mapping substrate concentration profiles in a biofilm to correlate with persister locations. |
| Fluorescent Protein Reporters (e.g., GFP) | Genes encoding fluorescent proteins under control of specific promoters. | Constructing reporter strains where fluorescence intensity indicates ribosomal activity or growth rate (e.g., ribosomal promoter). |
| Fluorescence-Activated Cell Sorter (FACS) | Instrument that sorts cells based on fluorescence and other light-scattering properties. | Isolating subpopulations of dim/non-fluorescent cells (potential persisters) from a larger population for downstream analysis. |
| LON Protease Inhibitors | Chemical compounds that specifically inhibit the activity of LON protease. | Experimentally blocking the TA system activation pathway to confirm its role in substrate-limited persistence. |
| Computational Modeling Software (e.g., NetLogo) | Platforms for creating agent-based models to simulate complex biological systems. | Building in silico models of biofilms to test hypotheses about substrate-dependent persister formation and treatment strategies. |
Carbon Source Utilization and Metabolic Shutdown in Dormant Cells
Frequently Asked Questions (FAQs)
Q1: What is the fundamental metabolic characteristic of dormant cells, such as bacterial persisters or dormant cancer cells? Dormant cells are characterized by a profound metabolic slowdown and a transition into a non-replicating, quiescent state. They enter a low-energy, non-growing state that makes them tolerant to conventional antibiotics and therapies, which typically target actively metabolizing and dividing cells. This state is a survival strategy under stress. The metabolic shutdown involves a general reduction in anabolic processes, including protein synthesis and ATP consumption [16] [17].
Q2: How does carbon source availability influence the formation and awakening of dormant persister cells? Carbon source availability is a critical environmental cue. Nutrient limitation, including starvation for carbon, is a key trigger that induces cells to enter the dormant persister state [17]. Conversely, the presence of readily available carbon sources can stimulate awakening. The addition of sugars and glycolysis intermediates like mannitol, glucose, fructose, and pyruvate has been shown to rapidly resuscitate persister cells, making them susceptible again to traditional antibiotics [16].
Q3: Are there specific metabolic pathways that are upregulated in dormant cells? While overall metabolism is low, certain pathways are adaptively maintained or upregulated. In some dormant cancer cells, studies suggest a dependency on fatty acid oxidation (FAO) and mitochondrial oxidative phosphorylation (OXPHOS) to generate energy in a low-proliferation state [18]. This represents a shift away from the aerobic glycolysis (Warburg effect) often seen in proliferating cancer cells. In bacteria, stress response pathways linked to the production of alarmones like (p)ppGpp are involved in initiating persistence [19] [17].
Q4: What are the key signaling pathways that regulate the metabolic shift into dormancy? The balance between specific signaling pathways dictates the dormant state. A well-established regulator is the p38/ERK signaling balance. High activity of p38 mitogen-activated protein kinase (MAPK) in conjunction with low activity of extracellular signal-regulated kinase (ERK) promotes cell cycle arrest and the maintenance of dormancy in cancer cells [20] [21]. In bacteria, the DosR regulon and SigH factor are involved in coordinating the transcriptional response to stress and inducing a dormant state in Mycobacterium tuberculosis [19].
Troubleshooting Guide: Common Experimental Issues
Table 1: Troubleshooting Metabolic and Dormancy Assays
| Problem | Potential Cause | Solution |
|---|---|---|
| Low persister cell yield in a population. | Insufficient or inappropriate stressor (e.g., antibiotic concentration too high, killing all cells; stress duration too short). | Optimize the inducer: Titrate the concentration and duration of the antibiotic or other stressor (e.g., nutrient starvation) to achieve a sub-population of survivors [16]. |
| Inconsistent awakening of dormant cells upon carbon source addition. | Carbon source is not readily utilizable; cells are in a deeply dormant state. | Use a mix of glycolytic intermediates (e.g., pyruvate, glucose) to provide multiple entry points into metabolism. Confirm the carbon source is suitable for the specific strain or cell type being studied [16]. |
| High background proliferation in label-retention assays (e.g., CFSE, PKH26). | Dye concentration too low; chase period insufficient; proliferating cells not adequately distinguished. | Increase dye concentration during initial labeling and extend the "chase" period to dilute the label in proliferating cells. Use flow cytometry gates to strictly separate bright (dormant) from dim (proliferated) populations [21]. |
| Failure to eradicate persisters with a candidate anti-persister compound. | Compound requires active metabolism for uptake or activity; compound is ineffective. | Consider combination therapy: Pair the compound with a metabolic activator (e.g., a carbon source) to "wake up" persisters, or use a membrane-active compound that works independently of metabolism [16] [17]. |
Experimental Protocols for Key Dormancy Assays
Protocol 1: Generating and Isulating Bacterial Persister Cells via Antibiotic Selection
Principle: This method uses a high dose of a bactericidal antibiotic to kill the majority of the growing population, leaving behind tolerant persister cells.
Materials:
- Late-exponential or stationary phase bacterial culture (e.g., E. coli, S. aureus)
- Appropriate bactericidal antibiotic (e.g., Ciprofloxacin, Ampicillin)
- Phosphate Buffered Saline (PBS) or fresh medium
- Centrifuge
Procedure:
- Grow the bacterial culture to the desired phase (late-exponential phase often yields a higher persister frequency).
- Treat the culture with a high concentration of antibiotic (typically 10-100x the MIC) for a defined period (e.g., 3-5 hours).
- After incubation, pellet the cells by centrifugation.
- Wash the cell pellet twice with PBS or fresh medium to remove the antibiotic thoroughly.
- Resuspend the pellet in fresh medium. This surviving population is enriched for persister cells and can be used for downstream awakening or killing assays [16].
Protocol 2: Identifying Dormant Cancer Cells Using Label-Retention (CFSE Staining)
Principle: Proliferating cells dilute a fluorescent dye with each division, while dormant, non-dividing cells retain the label, allowing for their identification and isolation.
Materials:
- Cancer cell line of interest (in vitro or from a primary tumor)
- Carboxyfluorescein succinimidyl ester (CFSE) dye
- Cell culture medium and standard reagents
- Flow cytometer
Procedure:
- Harvest and wash the cells in PBS.
- Resuspend the cell pellet in pre-warmed PBS containing a low micromolar concentration of CFSE (e.g., 1-5 µM). Incubate for 15-20 minutes at 37°C.
- Quench the staining reaction by adding at least 5 volumes of complete culture medium and incubate for another 10 minutes.
- Wash the cells thoroughly to remove all free dye. This is the "pulse" step.
- Plate the labeled cells and culture for several days to weeks (the "chase" period). Allow proliferating cells to dilute the CFSE.
- Analyze the cells by flow cytometry. The population of cells that remains highly fluorescent (CFSE-high) represents the dormant, slow-cycling, or quiescent cells [21].
Research Reagent Solutions
Table 2: Essential Reagents for Dormancy and Metabolism Research
| Reagent / Material | Function / Application |
|---|---|
| CFSE, PKH26, DiD Lipophilic Dyes | Fluorescent cell labels for tracking cell division and identifying dormant, label-retaining cells in vitro and in vivo [21]. |
| Cis-2-decenoic acid | A fatty acid signaling molecule that can induce the awakening of bacterial persister cells (e.g., in P. aeruginosa), sensitizing them to antibiotics [16]. |
| Mitomycin C | A DNA-cross-linking agent that can kill dormant persister cells independently of their metabolic state, effective against both planktonic and biofilm-derived persisters [16]. |
| ADEP4 | An acyldepsipeptide that activates the ClpP protease, leading to uncontrolled protein degradation and death of dormant bacteria, even without metabolic activity [16] [17]. |
| Pyrazinamide (PZA) | A frontline anti-tuberculosis drug; its active form, pyrazinoic acid, disrupts membrane energetics and targets PanD, showing efficacy against dormant M. tuberculosis [17]. |
| 3D Spheroid Culture Systems | In vitro models that better recapitulate the tumor microenvironment, including gradients of nutrients and oxygen, which are useful for studying cancer cell dormancy and quiescence [22]. |
Signaling Pathway and Experimental Workflow Diagrams
Dormancy Induction Signaling Pathway
Dormancy Experiment Workflow
Linking Central Metabolism, the TCA Cycle, and Antibiotic Tolerance
Frequently Asked Questions (FAQs)
1. What is the fundamental link between bacterial metabolism and antibiotic tolerance? Antibiotic tolerance is strongly associated with a low metabolic state in bacteria. Most clinically used antibiotics are effective against metabolically active cells but fail to kill dormant or slow-growing bacteria. Reduced metabolism, particularly through the tricarboxylic acid (TCA) cycle, decreases cellular processes that antibiotics typically target, enabling survival during treatment [23] [24].
2. How does the TCA cycle directly influence antibiotic efficacy? The TCA cycle is a central hub of bacterial metabolism. Its activity is directly linked to cellular respiration and generation of proton motive force (PMF), which is required for the uptake of certain antibiotics like aminoglycosides. Retarded TCA cycle activity, for instance by metabolites like glyoxylate, decreases PMF and drug internalization, leading to tolerance [23].
3. What is the difference between antibiotic resistance and tolerance? Antibiotic resistance is the ability of bacteria to grow at high concentrations of an antibiotic, typically mediated by genetic mutations. Antibiotic tolerance refers to the ability of genetically susceptible bacteria to survive transient antibiotic exposure without growing, often through phenotypic changes like metabolic dormancy. They have unaltered Minimum Inhibitory Concentration (MIC) values but survive treatment that kills their non-tolerant counterparts [23] [1].
4. Why are biofilms hotspots for antibiotic tolerance? Biofilms create heterogeneous microenvironments. Nutrient gradients within the biofilm structure lead to zones of slow growth or metabolic dormancy, particularly in deeper layers. This, combined with physical barriers from the extracellular matrix, protects bacterial cells from antibiotic killing and promotes the formation of persister cells [25] [26].
5. Can modulating substrate availability prevent tolerance? Yes, research indicates that exogenous metabolites can reactivate bacterial metabolism and re-sensitize tolerant cells. For example, providing specific amino acids, TCA cycle intermediates, or nucleotides can stimulate metabolic activity, making bacteria susceptible again to antibiotic killing [23].
Troubleshooting Common Experimental Issues
Problem: Inconsistent Persister Cell Yields in Stationary Phase Cultures
- Potential Cause: Uncontrolled or undefined growth conditions leading to variable metabolic states.
- Solution: Standardize the growth conditions meticulously.
- Use a defined growth medium instead of complex broths like LB to ensure reproducible nutrient availability.
- Precisely control the incubation time for the stationary phase. The duration of nutrient starvation significantly impacts the proportion of type I (triggered) persisters.
- Monitor culture density (OD600) over time to establish a consistent harvest point [4] [24].
Problem: Failed Re-sensitization of Tolerant Cells with Metabolic Stimulants
- Potential Cause 1: The stimulant does not effectively reactivate the core metabolic pathways targeted by the antibiotic.
- Solution 1: Systematically test different classes of metabolites. Refer to Table 1 for metabolite selection and ensure they are used at physiological concentrations that do not independently inhibit growth [23].
- Potential Cause 2: The antibiotic's mechanism is not sufficiently dependent on bacterial metabolism.
- Solution 2: Characterize the metabolic dependence of your antibiotic. Use a control WDM antibiotic like mitomycin C to confirm that your tolerant population can be killed. Optimize your strategy based on the antibiotic class [27].
Problem: Poor Antibiotic Penetration in Biofilm Assays
- Potential Cause: The dense, charged extracellular polymeric substance (EPS) matrix of the biofilm is binding or hindering the diffusion of the antibiotic.
- Solution:
- For biofilms known to have a high eDNA content (e.g., P. aeruginosa), consider adding low, non-bacteriolytic concentrations of DNase I to the treatment medium to degrade the matrix and improve penetration.
- Validate penetration issues by comparing killing efficacy with and without matrix-disrupting agents [25] [26] [28].
Experimental Protocols & Data
Protocol 1: Evaluating the Role of Specific Metabolites in Re-sensitizing Tolerant Cells
Objective: To test if exogenous TCA cycle metabolites can reverse antibiotic tolerance.
- Induce Tolerance: Grow bacteria to stationary phase or under nutrient limitation (e.g., carbon source exhaustion) to generate a population with a high frequency of tolerant cells.
- Prepare Metabolites: Prepare sterile solutions of key metabolites (e.g., succinate, α-ketoglutarate, malate) in the appropriate buffer or minimal medium. Filter sterilize.
- Co-incubation: Incubate the tolerant cell population with a range of metabolite concentrations (e.g., 0.1-10 mM) in the presence of a bactericidal antibiotic. Include controls with metabolite alone and antibiotic alone.
- Viability Assessment: Perform time-kill assays. Take samples at 0, 2, 4, 6, and 24 hours, serially dilute, and plate for colony-forming unit (CFU) counts.
- Analysis: Compare the killing curves. A significant increase in killing rate in the presence of the metabolite indicates successful re-sensitization [23] [12].
Protocol 2: Assessing Metabolic Dependence of an Antibiotic
Objective: To classify an antibiotic as Strongly (SDM) or Weakly Dependent on Metabolism (WDM).
- Generate Metabolically Dormant Cells: Create a model tolerant population. This can be achieved by using a known ΔnhaA E. coli mutant, which has downregulated metabolism, or by harvesting cells from deep, nutrient-starved zones of a biofilm [27].
- Antibiotic Exposure: Treat the dormant population and a control, log-phase (metabolically active) population with the antibiotic of interest at a clinically relevant concentration (e.g., 10x MIC).
- Quantify Survival: After a set time (e.g., 6 hours), determine the survival rate via CFU counts.
- Classification: An antibiotic that kills dormant cells as effectively as active cells is classified as WDM (e.g., mitomycin C). An antibiotic that shows significantly reduced killing of dormant cells is classified as SDM (e.g., ampicillin) [27].
Quantitative Data on Metabolic Interventions
Table 1: Effect of Exogenous Metabolites on Antibiotic Tolerance
| Metabolite Class | Specific Example | Experimental Model | Effect on Tolerance | Proposed Mechanism |
|---|---|---|---|---|
| TCA Cycle Intermediates | Succinate, α-ketoglutarate | P. aeruginosa | Re-sensitization to tobramycin | Increased TCA cycle activity, elevated PMF, enhanced drug uptake [23] |
| TCA Cycle Modulator | Glyoxylate | P. aeruginosa | Induced tolerance to tobramycin | Retarded TCA cycle activity, decreased cellular respiration and PMF [23] |
| Amino Acids | Various | E. coli | Re-sensitization to fluoroquinolones | Activation of central metabolism, exit from dormancy [23] |
| Nucleotides | - | E. coli | Re-sensitization to fluoroquinolones | Activation of central metabolism, exit from dormancy [23] |
Table 2: Comparison of Antibiotics with Different Metabolic Dependencies
| Antibiotic | Metabolic Dependence | Efficacy Against Tolerant ΔnhaA E. coli | Clinical Relevance |
|---|---|---|---|
| Ampicillin | Strong (SDM) | Low ( >1000-fold reduced killing) | Beta-lactam; fails against dormant populations [27] |
| Ciprofloxacin | Strong (SDM) | Low | Fluoroquinolone; fails against dormant populations [27] |
| Gentamicin | Weak (WDM) | High | Aminoglycoside; retains activity, but uptake requires PMF* [27] [23] |
| Mitomycin C | Weak (WDM) | High | Cytotoxic; cross-links DNA independently of metabolism [27] |
| Halicin | Weak (WDM) | High | Novel antibiotic; mechanism distinct from metabolic state [27] |
*Note: Gentamicin is classified as WDM in the cited study but is known to require PMF for uptake, highlighting context-dependent efficacy.
Pathway and Workflow Visualizations
Metabolic Path to Antibiotic Tolerance
Strategies to Combat Tolerance
The Scientist's Toolkit: Research Reagent Solutions
Table 3: Essential Reagents for Investigating Metabolism and Tolerance
| Reagent / Material | Function in Experimentation | Example Use Case |
|---|---|---|
| Defined Minimal Media | Provides controlled nutrient availability to precisely manipulate metabolic states and avoid undefined components in complex broths. | Studying the effect of specific carbon sources on TCA cycle activity and tolerance induction [23]. |
| TCA Cycle Metabolites (e.g., Succinate, α-Ketoglutarate) | Used as exogenous supplements to test if reactivation of specific metabolic pathways can reverse antibiotic tolerance. | Re-sensitizing dormant P. aeruginosa to aminoglycoside antibiotics [23]. |
| Keio Collection Knockout Mutants (e.g., ΔnhaA E. coli) | Pre-made gene deletion mutants to study the role of specific genes in metabolic regulation and tolerance without needing to construct mutants. | Validating the role of the nhaA gene in metabolic suppression and SDM antibiotic tolerance [27]. |
| Weakly Metabolism-Dependent Antibiotics (e.g., Mitomycin C) | Serve as positive controls in experiments to confirm that a bacterial population is susceptible to killing when metabolic dormancy is bypassed. | Differentiating between general cell death failure and metabolism-specific tolerance [27]. |
| DNase I | An enzyme that degrades extracellular DNA (eDNA), a key component of the biofilm matrix for some species. | Improving antibiotic penetration in biofilm assays for species like P. aeruginosa [25] [26]. |
| ATP Assay Kits | Quantify intracellular ATP levels as a direct, quantitative measure of a bacterial cell's metabolic activity and energy status. | Correlating the metabolic state (high vs. low ATP) of populations with their level of antibiotic tolerance [27]. |
Understanding the Persister Continuum: Frequently Asked Questions
What is the "Persister Continuum" hypothesis? The Persister Continuum hypothesis proposes that bacterial persisters exist in a spectrum of dormancy depths, rather than as a single, uniform state. This continuum ranges from "shallow" persisters, which are slow-growing and can resuscitate quickly, to "deep" persisters, which are metabolically dormant and resemble viable but non-culturable (VBNC) cells [29] [1]. The depth of dormancy influences how long a cell takes to resuscitate and its tolerance level to antibiotics.
How does substrate availability influence a cell's position on this continuum? Substrate availability is a primary environmental trigger that determines a cell's metabolic state and thus its position on the persister continuum. Nutrient-rich conditions typically promote active growth, while nutrient limitation or starvation pushes cells into deeper dormancy states [1] [4]. Optimizing substrate availability in experimental cultures is therefore critical for controlling the depth of dormancy and preventing the formation of deeply persistent subpopulations that are extremely difficult to eradicate.
What are the key differences between Type I, II, and III persisters in the context of this continuum? Within the continuum, persisters are often categorized based on their formation mechanisms, which correlate with different dormancy depths [4]:
- Type I (Triggered): Form in response to environmental stress (e.g., nutrient starvation) and are often deeply dormant.
- Type II (Stochastic): Arise spontaneously during exponential growth due to random fluctuations and are typically shallow persisters.
- Type III (Specialized): Induced by specific antibiotic-induced stress signals and may not be deeply dormant prior to exposure.
Why is it critical to distinguish between shallow and deep persisters in experimental outcomes? Distinguishing between shallow and deep persisters is essential because they respond differently to treatments and have varying resuscitation times [1]. An experimental treatment might effectively eliminate shallow persisters but fail against deep persisters, leading to a false positive result. Understanding the composition of the persister population in your model is key to developing effective anti-persister therapies.
Troubleshooting Common Experimental Challenges
Problem: Inconsistent Persister Frequencies in Replicate Cultures
- Potential Cause: Stochastic formation of persisters and uncontrolled, minor fluctuations in the growth medium or substrate concentration.
- Solution:
- Standardize Inoculum: Always use cells from the same growth phase. The stationary phase is associated with a higher frequency of Type I persisters [4].
- Control Substrate: Use well-defined, fresh media for all experiments. Pre-condition cells in consistent nutrient environments to synchronize their metabolic states.
- Increase Biological Replicates: Due to the inherent stochasticity of persistence, a minimum of 3-5 biological replicates is recommended for reliable data.
Problem: Failure to Eradicate Persisters with Conventional Antibiotics
- Potential Cause: The persister population is dominated by deeply dormant cells that are not susceptible to antibiotics targeting active cellular processes.
- Solution:
- Profile Dormancy Depth: Use ATP assays or membrane potential dyes (e.g., DISC3(5)) to assess the metabolic activity of your persister population [7].
- Employ Anti-Persister Agents: Consider compounds that target dormant cells, such as membrane-disrupting agents [17] or compounds like ADEP4 which force uncontrolled protein degradation [17].
- Combine with Wake-Up Strategies: Use a "kick and kill" approach by first adding a metabolite like pyruvate or an appropriate carbon source to resuscitate shallow persisters, then applying a conventional antibiotic [7].
Problem: Inability to Resuscitate Surviving Cells After Antibiotic Treatment
- Potential Cause: The surviving cells may have entered a deep dormancy state, such as the VBNC state, from which they cannot be cultured on standard media [29].
- Solution:
- Extend Recovery Time: Allow for longer recovery periods in fresh, nutrient-rich media.
- Use of Resuscitation Promoters: Supplement recovery media with known resuscitation factors, such as sodium pyruvate or catalase, to counteract accumulated reactive oxygen species.
- Alternative Detection: Use viability staining (e.g., LIVE/DEAD BacLight) coupled with microscopy to confirm the presence of VBNC cells that are viable but not culturable [29].
Quantitative Data on Persister Survival
The table below summarizes key quantitative data on persister survival under different antibiotic treatments, which is essential for benchmarking your experimental results.
Table 1: Quantifying Persister Survival Under Antibiotic Exposure
| Bacterial Strain | Antibiotic & Concentration | Treatment Duration | Survival Frequency | Key Experimental Context |
|---|---|---|---|---|
| E. coli MG1655 (WT) [30] | Ampicillin (200 µg/mL, 12.5x MIC) | 3-5 hours | Multiphasic decay curve | Cells from exponential phase; most persisters were growing before treatment. |
| E. coli MG1655 (WT) [30] | Ciprofloxacin (1 µg/mL, 32x MIC) | 3-5 hours | Multiphasic decay curve | Cells from exponential phase; all identified persisters were growing before treatment. |
| E. coli HM22 (high-persistence) [7] | Eravacycline (100 µg/mL) | Not Specified | 99.9% killing | Treatment during "wake-up" phase; effective due to compound accumulation in persisters. |
| Mycobacterium tuberculosis [29] | Various | Standard treatment | Up to 1% of population | Persisters are primary cause of refractory tuberculosis, found in granulomas. |
Essential Experimental Protocols
Protocol 1: Isolation and Enumeration of Persisters via Antibiotic Killing Curves
This is a foundational method for quantifying persisters in a population [29] [30].
Key Research Reagent Solutions:
- Antibiotic Stock Solutions: Prepare high-concentration stocks (e.g., 10-100 mg/mL) of bactericidal antibiotics like ampicillin or ciprofloxacin in appropriate solvents. Filter sterilize and store at -20°C.
- Phosphate-Buffered Saline (PBS) or M9 Minimal Salts: For washing and diluting cells to remove nutrients and stop growth during antibiotic exposure.
- Neutralizing Agent: Sodium polyanethol sulfonate (SPS) or specific β-lactamase can be added to the plating media to neutralize antibiotic carryover during viability plating.
Methodology:
- Grow culture to the desired growth phase (exponential or stationary).
- Treat with a lethal dose of antibiotic (typically 10-100x MIC). Maintain a control without antibiotic.
- Incubate under optimal growth conditions with aeration for 3-24 hours.
- At designated time points, remove aliquots, wash twice with PBS to remove the antibiotic, and perform serial dilutions.
- Plate dilutions on fresh, antibiotic-free agar plates.
- Incubate plates and count colony-forming units (CFUs) after 24-48 hours.
- Plot the killing curve as log(CFU/mL) versus time. A biphasic curve, with an initial rapid kill followed by a slower second phase, indicates the presence of persisters.
Protocol 2: Single-Cell Analysis of Persister Dormancy Depth Using a Microfluidic Device
This advanced protocol allows for tracking the pre-history and fate of individual persister cells [30].
Key Research Reagent Solutions:
- Microfluidic Device: Such as a Membrane-Covered Microchamber Array (MCMA). The membrane allows for rapid medium exchange while trapping cells for imaging.
- Time-Lapse Microscopy Setup: An inverted microscope with a high-precision stage, camera, and environmental chamber (to maintain 37°C and CO₂).
- Fluorescent Stains: Membrane potential-sensitive dyes (e.g., DISC3(5)) or fluorescent protein reporters for stress genes (e.g., rpoS) can be used to correlate physiology with persistence.
Methodology:
- Load cells into the microchambers of the device.
- Perfuse with fresh growth medium and monitor single-cell growth and division to establish pre-treatment histories.
- Switch perfusion to medium containing a lethal antibiotic (e.g., 200 µg/mL ampicillin).
- Image continuously throughout the antibiotic treatment period (e.g., 5-10 hours).
- Switch back to fresh, antibiotic-free medium to monitor for resuscitation and regrowth.
- Analyze lineage data to correlate pre-antibiotic growth status (growing vs. non-growing) with survival outcomes, identifying different persister phenotypes.
Visualizing Key Concepts and Workflows
Diagram 1: The Persister Continuum and Fates
This diagram illustrates the metabolic states of cells along the persister continuum and their potential fates following antibiotic treatment and subsequent removal.
Diagram 2: Experimental Workflow for Profiling the Continuum
This diagram outlines a comprehensive experimental strategy to profile a bacterial population across the persister continuum, from culture to data analysis.
Quantifying and Modeling Substrate-Dependent Persister Dynamics
Stable Isotope Tracing (13C-Glucose/Acetate) to Map Metabolic Flux
Frequently Asked Questions (FAQs)
Q1: Why is stable isotope tracing particularly useful for studying metabolic perturbations that lead to bacterial persister formation? Stable isotope tracing allows for the direct measurement of metabolic flux, which is the dynamic flow of metabolites through metabolic pathways. In the context of persister formation—a state of metabolic dormancy and antibiotic tolerance—this technique can identify specific bottlenecks or rerouting in central carbon metabolism that occur as cells enter dormancy. Unlike static "snapshot" measurements (e.g., metabolite concentrations), flux analysis can reveal whether a change in metabolite level is due to increased production or decreased consumption, providing mechanistic insight into the metabolic state of pre-persisters and persisters that is crucial for designing strategies to optimize substrate availability and prevent persistence [31] [32].
Q2: What is the critical difference between metabolic steady state and isotopic steady state, and why does it matter for my persister study? These are two distinct concepts that are both critical for experimental design and data interpretation.
- Metabolic Steady State: This means that intracellular metabolite levels and metabolic fluxes are constant over time [31]. In practice, many systems are studied at a pseudo-steady state, where changes are minimal during the experiment.
- Isotopic Steady State: This is achieved when the enrichment of the heavy isotope (e.g., 13C) in a metabolite pool no longer changes over time [31]. For studies on persister formation, it is crucial to first establish that your system is at a metabolic (pseudo-)steady state before introducing the isotope tracer. This ensures that any measured labeling patterns reflect the fluxes of the metabolic state you intend to study. The time to reach isotopic steady state varies; glycolytic intermediates may reach it in minutes, while TCA cycle intermediates can take hours [31].
Q3: My mass spectrometry data shows labeling in metabolites, but the patterns are difficult to interpret. What is the most common oversight when processing this raw data? The most common oversight is a failure to properly correct the raw mass isotopologue distribution (MID) data for the presence of naturally occurring heavy isotopes [31] [33]. Elements like carbon, oxygen, and nitrogen have heavy but stable isotopes (e.g., 13C, 18O, 15N) that occur at low natural abundance. These atoms contribute to the mass signal, making it seem like your tracer has labeled a metabolite when it has not. This must be corrected computationally using algorithms in tools like PolyMID-Correct, IsoCor, or AccuCor to obtain the true MID resulting only from your administered tracer [33].
Q4: How can I use 13C-acetate to probe specific metabolic functions relevant to bacterial energy metabolism and persistence? 13C-acetate is a powerful tracer for studying the tricarboxylic acid (TCA) cycle and lipid synthesis. Upon uptake, acetate is converted to acetyl-CoA, which directly enters the TCA cycle. The labeling pattern from 13C-acetate (e.g., [1,2-13C]acetate or [U-13C]acetate) in TCA intermediates like citrate and α-ketoglutarate provides a direct readout of TCA cycle activity [34] [35]. Since persister cells often exhibit downregulated TCA cycle and energy metabolism, a reduction in 13C-incorporation from acetate into these intermediates is a key indicator of a shift toward metabolic dormancy. Furthermore, 13C-acetate is efficiently incorporated into fatty acids, allowing you to monitor the flux into membrane lipid biosynthesis, which may be altered in dormant cells [36].
Troubleshooting Guides
Poor or Unpredictable Isotopic Enrichment
This problem manifests as low or inconsistent incorporation of the 13C label into your target metabolites.
Table: Troubleshooting Poor Isotopic Enrichment
| Problem | Potential Cause | Solution |
|---|---|---|
| Low label incorporation in all downstream metabolites | Tracer concentration is too low; cells are using unlabeled carbon sources. | - Determine the minimum tracer concentration required to achieve >90% enrichment in the initial metabolic node (e.g., Glucose 6-P for [U-13C]glucose) [37].- Use defined media and ensure the tracer is the principal carbon source for the pathway under investigation. |
| Enrichment is highly variable between replicates | System is not at a metabolic steady state; cell growth is inconsistent. | - Use controlled bioreactors (e.g., chemostats) or ensure cells are harvested during mid-exponential growth phase for pseudo-steady state [31] [37].- Monitor growth rate (OD600) and key extracellular rates (e.g., glucose consumption, lactate production) to confirm steady-state conditions. |
| Specific metabolites fail to label | Presence of large, unlabeled intracellular or extracellular pools diluting the tracer. | - For amino acids, this is a common issue due to exchange with media pools. Use dialyzed serum and label-free media formulations where possible [31].- Allow sufficient time for the label to reach isotopic steady state in the target pathway. |
Inconsistent or Noisy Flux Results
This issue arises when technical or biological variability leads to flux estimates with large confidence intervals.
Table: Troubleshooting Inconsistent Flux Results
| Problem | Potential Cause | Solution |
|---|---|---|
| High measurement error in Mass Isotopologue Distributions (MIDs) | Inadequate analytical sensitivity; ion suppression in MS; poor chromatographic separation. | - Use chemical derivatization (e.g., for GC-MS) to improve sensitivity and separation [31].- Optimize LC-MS methods (e.g., HILIC for polar metabolites) to reduce ion suppression [34] [36].- Use multiple reaction monitoring (MRM) or parallel reaction monitoring (PRM) on triple-quadrupole or Q-Exactive instruments for higher sensitivity of target metabolites [34]. |
| Model fails to fit the data | Underdetermined system; metabolic network model is incorrect or incomplete. | - Use complementary tracers (e.g., [1,2-13C]glucose and [U-13C]glutamine) to provide more labeling constraints for the model [34] [37].- Incorporate external flux measurements (nutrient uptake, secretion rates, growth rate) as additional constraints to reduce the solution space [37]. |
| Large confidence intervals for estimated fluxes | The chosen tracer does not provide good resolution for the pathway of interest. | - For the Pentose Phosphate Pathway (PPP), [1,2-13C]glucose provides better flux resolution than [U-13C]glucose because it generates distinct labeling patterns for glycolysis vs. PPP-derived lactate [34].- Select a tracer (or combination) based on a simulation of the expected labeling patterns for your hypothesized flux changes. |
Key Pathway Diagrams and Workflows
13C-Glucose Tracing Workflow
13C-Glucose and Acetate Metabolic Pathways
Research Reagent Solutions
Table: Essential Reagents and Tools for Stable Isotope Tracing Experiments
| Item | Function/Description | Key Considerations |
|---|---|---|
| 13C-Labeled Tracers ([U-13C]Glucose, [1,2-13C]Glucose, 13C-Acetate) | The core reagents used to trace carbon atoms through metabolic pathways. | - Purity and isotopic enrichment (>99%) are critical [33].- Select tracer based on pathway: [U-13C]glucose for general tracing; [1,2-13C]glucose for resolving PPP vs. glycolysis [34]. |
| Defined Culture Media | To control the availability of nutrients and ensure the tracer is the principal carbon source. | - Must be free of unlabeled compounds that could dilute the tracer (e.g., use dialyzed serum) [31] [37].- Allows for precise calculation of extracellular fluxes. |
| Mass Spectrometer | The primary instrument for measuring mass isotopologue distributions (MIDs). | - LC-MS (HILIC/RP) or GC-MS are standard [34] [36].- High-resolution instruments (Orbitrap, TOF) are preferred for untargeted work; triple-quadrupole for sensitive targeted assays [34] [36]. |
| Metabolite Extraction Solvents (e.g., Methanol, Acetonitrile) | To rapidly quench metabolism and extract intracellular metabolites from bacterial cells. | - Use cold (-20°C to -40°C) solvent for rapid quenching to preserve in vivo metabolic state [34].- Protocol should be optimized for bacterial cell wall lysis. |
| Data Correction Software (e.g., PolyMID-Correct, IsoCor) | Computationally removes the effect of naturally occurring heavy isotopes from raw MID data. | Essential for accurate data interpretation. Correction requires the exact chemical formula of the measured metabolite (or its derivative) [31] [33]. |
| Flux Analysis Software (e.g., INCA, Metran) | Integrated software platforms for performing 13C-Metabolic Flux Analysis (13C-MFA). | - Uses corrected MIDs and extracellular fluxes to calculate intracellular reaction rates [37].- Requires a defined metabolic network model of your organism. |
Agent-Based and Mathematical Models of Nutrient Gradients in Biofilms
This technical support center addresses the critical challenge of nutrient gradient control in biofilm research, a fundamental aspect for investigators aiming to optimize substrate availability to prevent persister cell formation. Bacterial persisters—dormant, transiently antibiotic-tolerant phenotypic variants—are a primary cause of chronic and relapsing infections [1] [4]. Their formation and survival are intrinsically linked to the heterogeneous microenvironment within biofilms, which is largely governed by the interplay between bacterial metabolism and the diffusion of nutrients and substrates [38] [39].
Agent-Based Models (ABMs) and other mathematical frameworks are indispensable tools for unraveling this complexity. These models treat each bacterial cell as an individual agent with defined properties and rules, allowing researchers to observe how large-scale community structures, such as nutrient gradients and sub-populations of persister cells, emerge from individual cellular behaviors [40] [41]. This technical resource provides troubleshooting guides, standardized protocols, and key reagent information to support the application of these models in your research, with the ultimate goal of designing interventions that disrupt the conditions leading to persistence.
The Scientist's Toolkit: Research Reagent Solutions
The table below catalogs essential computational and biological components frequently used in the development and validation of biofilm models concerning nutrient gradients and persistence.
Table 1: Key Research Reagents and Computational Tools in Biofilm Modeling
| Item Name | Type | Primary Function in Research | Relevance to Nutrient Gradients & Persistence |
|---|---|---|---|
| iDynoMiCS [40] | Software Platform | An open-source agent-based modeling framework for simulating microbial systems. | Used to explore mechanisms like detachment and the role of cell aggregates in biofilm structure under nutrient limitation [40]. |
| NetLogo [14] | Software Platform | A programmable modeling environment for simulating natural and social phenomena, widely used for ABMs. | Enables the development of custom ABMs to test periodic antibiotic dosing regimens and their effect on persisters in structured biofilms [14]. |
| Spherocylindrical Particles [38] | Computational Cell Representation | A 3D geometric model (cylinder with hemispherical ends) used in Individual-based Models (IbM) to represent bacterial cells. | Allows for more realistic modeling of structural features in biofilms, coupling cell growth to local nutrient concentration [38]. |
| Monod Equation [38] [14] | Mathematical Kinetic Model | Describes the dependence of microbial growth rate on the local concentration of a limiting nutrient. | A fundamental equation implemented in ABMs to simulate how nutrient gradients lead to heterogeneous growth and dormancy within a biofilm [38] [14]. |
| Tet Operon Reporter [39] | Fluorescent Reporter System | A two-color plasmid (e.g., PR-GFP, PA-mCherry) reporting the expression and intracellular accumulation of tetracycline resistance genes. | Used in microfluidic studies to correlate spatial nutrient gradients with heterogeneous gene expression of antibiotic resistance mechanisms [39]. |
| Microfluidic Biofilm Trap [39] | Experimental Device | Creates confined, diffusion-limited environments for growing spatially extended microcolonies with defined nutrient gradients. | Provides experimental validation for models by allowing real-time observation of colony dynamics in response to controlled nutrient and antibiotic gradients [39]. |
Core Concepts & Signaling Pathways
Understanding the mechanistic link between nutrient availability and cellular dormancy is key. The following diagram synthesizes the primary signaling pathways that integrate environmental nutrient status with the regulatory networks leading to persister cell formation, as explored in both experimental and modeling studies.
Figure 1: Integrated Signaling Pathways in Nutrient-Linked Persister Formation. This diagram illustrates how nutrient limitation acts as a key environmental stressor, triggering intracellular signaling cascades that can lead to growth arrest and the formation of phenotypically heterogeneous persister cells.
Experimental Protocols & Methodologies
Protocol: Implementing a 3D Individual-Based Model (IbM) for Biofilm Nutrient Gradients
This protocol outlines the steps for constructing a three-dimensional Individual-based Model to simulate the emergence of nutrient gradients and their effect on bacterial subpopulations, based on established methodologies [38] [42].
1. Model Initialization and Computational Domain Setup
- Define a three-dimensional computational space with a flat, impermeable substrate at the bottom (z=0).
- Set initial conditions by placing a small number of bacterial agents (e.g., 27 cells) randomly on the substrate surface to mimic initial adhesion [14].
- Overlay the domain with an aqueous solution representing the bulk liquid, which contains a defined initial concentration of the growth-limiting nutrient (e.g., carbon source) and oxygen [38] [42].
2. Agent (Bacterial Cell) Properties and Rules
- Represent each bacterial cell as a spherocylinder (a cylinder with hemispherical ends) with defined initial dimensions (e.g., aspect ratio L₀* = 2.6 for Pseudomonas putida) [38].
- Program agent growth using the Monod Kinetic Model. The growth rate of each cell is calculated as:
dmi/dt = mi * μmax * [C/(C + Ks)]wheremiis cell mass,μmaxis the maximal specific growth rate,Cis the local nutrient concentration, andKsis the half-saturation constant [14] [42]. - Implement cell division: when an agent's mass doubles, it divides into two daughter cells of equal or slightly randomized mass (e.g., 40%-60% split) [14].
3. Nutrient Diffusion and Consumption Dynamics
- Simulate the spatial and temporal distribution of nutrients by solving the reaction-diffusion equation:
∂C/∂t = Dₙ * ∇²C - ΣμᵢwhereDₙis the nutrient's diffusion coefficient,∇²is the Laplacian operator (modeling diffusion), andΣμᵢis the sum of nutrient uptake by all cells in a given volume [38]. - Calculate individual nutrient uptake
μᵢfor each cell also via a Monod-type function relative to its local environment [38].
4. Implementation of Dormancy and Persistence Logic
- Introduce rules for transitions to a dormant state based on testable hypotheses. Common implementations include:
- Nutrient-Dependent: A cell switches to a dormant state if the local nutrient concentration
Cfalls below a critical threshold (e.g.,C < C_crit) [42]. - Stochastic: Each active cell has a low, fixed probability per time step of switching to a persister state, independent of the environment [42].
- Time-Dependent: Cells that have been growth-arrested due to local conditions for a prolonged duration transition to dormancy [42].
- Nutrient-Dependent: A cell switches to a dormant state if the local nutrient concentration
5. Simulation Execution and Data Collection
- Run the simulation with a finite difference numerical scheme, using a time step sufficiently small to ensure stability.
- At defined intervals, collect quantitative data on: biofilm biovolume and thickness, spatial distribution of nutrient concentrations, and the number and location of dormant vs. active cells.
Protocol: Experimental Validation Using Microfluidic Cultivation
This protocol describes the use of a microfluidic device to cultivate biofilms with controlled nutrient gradients, enabling direct observation and validation of model predictions [39].
1. Device Fabrication and Preparation
- Fabricate a microfluidic device featuring one or more cultivation traps (e.g., 170 μm deep, 100 μm wide) connected to nutrient supply channels using standard soft lithography techniques with Polydimethylsiloxane (PDMS) [39].
- Bond the PDMS device to a glass coverslip to create sealed channels. Sterilize the device before use, typically by autoclaving or flushing with ethanol.
2. Bacterial Strain and Inoculation
- Use a relevant bacterial strain (e.g., E. coli). For studies on resistance dynamics, employ a strain carrying a fluorescent reporter system for a gene of interest (e.g., TetA-mCherry for tetracycline resistance) [39].
- Dilute an overnight culture to a low optical density and inject it into the device's main channel, allowing cells to settle into the traps by gravity or flow.
3. Establishing Steady-State Nutrient Gradients
- Continuously perfuse the supply channels with fresh growth medium at a controlled, low flow rate. This creates a diffusion-limited environment where nutrients are consumed as they penetrate the trap, generating a stable gradient from the open edge to the interior [39].
- Allow the colony to grow for 24-48 hours until it fills the trap and reaches a steady state, characterized by a clear boundary between fast-growing cells near the nutrient source and slow-growing or dormant cells in the interior.
4. Real-Time Monitoring and Perturbation
- Place the device on a temperature-controlled stage of an inverted fluorescence/phase-contrast microscope.
- Monitor cell growth, morphology, and fluorescence reporter expression in real time using time-lapse microscopy.
- To test model predictions or treatment efficacy, rapidly switch the inlet tubing to medium containing an antimicrobial agent or a different nutrient composition. The device design allows for swift changes in the bulk condition [39].
5. Image and Data Analysis
- Use Particle Image Velocimetry (PIV) algorithms on time-lapse images to quantify cellular displacement and calculate local growth rates throughout the colony [39].
- Quantify fluorescence intensity to map the spatial expression patterns of resistance or stress genes in response to the nutrient gradient and any applied perturbations.
Troubleshooting Guides and FAQs
Q1: Our ABM simulations consistently predict uniform, homogenous biofilms without the expected nutrient gradients and stratified dormant regions. What could be wrong?
- Check Nutrient Consumption Parameters: The most common cause is an imbalance between nutrient diffusion and consumption. Verify that your maximum nutrient uptake rate (
μ_maxorq_max) is sufficiently high relative to the diffusion coefficient (Dₙ). If uptake is too slow, nutrients will not be depleted in the biofilm interior. Consult literature for realistic parameter values [38]. - Verify Diffusion Coefficient: Ensure the diffusion coefficient used for the biofilm interior is significantly lower than that in the bulk liquid to account for the hindrance caused by the extracellular polymeric matrix [38].
- Increase Biofilm Size: The gradients may not have space to develop if the simulation domain or time is too small. Allow the biofilm to grow thicker, as stratification is more apparent in larger colonies [38].
Q2: When we apply an antibiotic in our model, it clears the biofilm too effectively and does not match experimental observations of persister survival. How can we improve the model?
- Implement Persister-Specific Killing Rates: Model susceptible and persister cells as having different death rates upon antibiotic exposure. Persister death rates should be several orders of magnitude lower [14].
- Review Persister Induction Logic: The rules for forming persisters might be insufficient. Ensure you are modeling the correct type (e.g., type I vs. type II) and that the switching rates (to and from persistence) are calibrated to experimental data [1] [42]. Incorporating both stochastic and nutrient-dependent switching can enhance realism [14] [42].
- Confirm Antibiotic Diffusion/Penetration: If the antibiotic does not fully penetrate the biofilm, it will not reach all cells. Model antibiotic diffusion and potential binding/degradation to create sanctuaries where persisters can survive [40].
Q3: In our microfluidic experiments, we do not observe a clear nutrient gradient or distinct growth zones in the trap. What are potential causes?
- Check for Flow Rate Issues: If the flow rate is too high, it can flush away the gradient and create a well-mixed environment. Conversely, if it's too low, waste products may accumulate and confound results. Optimize the flow rate to be low enough to be diffusion-limited but high enough to prevent waste accumulation [39].
- Verify Trap Geometry and Cell Density: The trap might be too shallow or wide to establish a strong gradient. Ensure the cell density is high enough to consume nutrients significantly as they diffuse inward [39].
- Confirm Nutrient Concentration: The initial nutrient concentration in the medium might be too high, preventing depletion. Consider using a more minimal or nutrient-limited medium.
Q4: What are the key quantitative parameters we need to extract from the literature to parameterize a realistic ABM of nutrient gradients? The following table summarizes critical parameters and their typical roles in model behavior.
Table 2: Key Quantitative Parameters for ABM of Biofilm Nutrient Gradients
| Parameter | Symbol | Description | Impact on Model | Exemplary Source |
|---|---|---|---|---|
| Max. Specific Growth Rate | μ_max |
Maximum rate of cell mass increase. | Controls speed of biofilm development and nutrient consumption. | Monod Kinetics [14] |
| Half-Saturation Constant | K_s |
Nutrient conc. at half μ_max. |
Determines sensitivity of growth to low nutrient levels. | Monod Kinetics [14] |
| Nutrient Diffusion Coefficient | D_n |
Measure of nutrient mobility in biofilm. | Lower values lead to steeper gradients and larger dormant zones. | [38] |
| Max. Nutrient Uptake Rate | q_max |
Maximum rate of nutrient consumption per cell. | High rates promote faster nutrient depletion and stratification. | [38] [42] |
| Critical Nutrient Threshold | C_crit |
Nutrient level below which dormancy is triggered. | Directly sets the location and size of the dormant region. | Hypothesis-driven [42] |
| Stochastic Persister Switch Rate | P_switch |
Probability of a cell becoming a persister per unit time. | Governs the baseline level of persistence in active regions. | [14] [42] |
Advanced Analysis: Optimizing Anti-Persister Strategies
The ultimate goal of modeling is to inform effective strategies. A key application is optimizing treatment schedules. The following diagram outlines the workflow for using an ABM to design and test a periodic antibiotic dosing regimen aimed at eradicating persisters by exploiting their "reawakening" phase.
Figure 2: Workflow for ABM-Guided Optimization of Periodic Dosing. This logic flow depicts how agent-based models can be iteratively used to design treatment schedules that capitalize on the dynamic nature of persister cells, potentially reducing the total antibiotic dose required for eradication [14].
Research demonstrates that this approach can be highly effective. One ABM study found that by carefully tuning the timing of periodic antibiotic doses to align with the dynamics of persister resuscitation, the total dose required for effective treatment could be reduced by nearly 77% compared to continuous treatment, without compromising efficacy [14]. This highlights the powerful predictive potential of integrating realistic nutrient-gradient and persistence models into therapeutic planning.
Measuring Environment-Dependent Switching Rates Between Cell States
Frequently Asked Questions (FAQs)
FAQ 1: What is the fundamental difference between bacterial persister cells and antibiotic-resistant bacteria? Persister cells are phenotypic variants of genetically drug-susceptible bacteria that survive antibiotic exposure by entering a transient, dormant state. They are characterized by tolerance, not resistance. Unlike resistant bacteria, which have a higher minimum inhibitory concentration (MIC), persisters do not grow in the presence of the drug but remain susceptible to it once the antibiotic is removed and they resume growth [5] [1]. This tolerance is often linked to slowed metabolism, a state which can be influenced by environmental factors like substrate availability [5].
FAQ 2: How do environmental stresses like substrate limitation trigger the formation of persister cells? Substrate limitation and other environmental stresses (e.g., nutrient starvation, acidic pH) activate key bacterial stress response pathways. A central mechanism is the stringent response, where nutrient scarcity leads to the accumulation of (p)ppGpp. This alarmone triggers a dramatic slowdown of cellular metabolism and growth, facilitating the transition to a dormant, persister state. This state protects bacteria because most antibiotics target active cellular processes [5] [1].
FAQ 3: What are the main types of persisters, and how do they relate to my experiments? Persisters exist on a continuum, but two primary categories are often described [1]:
- Type I Persisters: Form in response to a specific external environmental trigger, such as entering the stationary phase due to nutrient exhaustion. They are typically pre-formed before antibiotic exposure.
- Type II Persisters: Form spontaneously during balanced growth without an external trigger. These are often slow-growing or non-growing cells within an otherwise active population. Your experimental setup (e.g., batch culture growth phase, continuous culture parameters) will influence which type you predominantly study.
FAQ 4: Why is measuring cell state switching rates to and from the persister state critical for my research? Quantifying switching rates is essential for:
- Understanding Persistence Dynamics: It moves research from a static snapshot (persister frequency) to a dynamic understanding of how quickly cells enter and exit the dormant state.
- Predicting Treatment Outcomes: The rate of switching back to an active state can determine the likelihood of infection relapse after antibiotic therapy is stopped.
- Identifying Therapeutic Targets: Interventions aimed at reducing the rate of entry into persistence or increasing the rate of exit could make infections more susceptible to conventional antibiotics.
Troubleshooting Guides
Low Persister Cell Yields in Stationary Phase Cultures
Problem: The proportion of persister cells isolated from stationary-phase cultures is consistently lower than expected, making downstream analysis difficult.
Possible Causes and Solutions:
- Cause 1: Inconsistent Culture Conditions.
- Solution: Standardize the growth medium, temperature, and shaking speed. Precisely define the "stationary phase" by optical density (OD) and duration to ensure reproducibility between experiments.
- Cause 2: Ineffective Antibiotic Selection.
- Solution: Verify the concentration and stability of the bactericidal antibiotic used for selection. Use a concentration that is 10x the MIC and confirm its activity. Ensure exposure time is sufficient to kill all growing cells but not so long as to start killing persisters.
- Cause 3: Suboptimal Growth Phase Harvesting.
- Solution: The proportion of persisters increases from mid-log to a peak in the stationary phase [5]. Perform a time-course experiment to determine the optimal harvesting point for your specific bacterial strain.
High Variability in Switching Rate Measurements
Problem: Measurements of the rate at which cells switch to or from the persister state show high variability between technical and biological replicates.
Possible Causes and Solutions:
- Cause 1: Inadequate Control of the Pre-conditioning Environment.
- Solution: Fluctuations in substrate availability (carbon, nitrogen sources) prior to the assay are a major source of noise. Use chemostat cultures to maintain a perfectly stable and defined growth environment before inducing the switching signal.
- Cause 2: Carryover of Metabolic Byproducts.
- Solution: When isolating persisters via antibiotic treatment and centrifugation, ensure thorough washing with fresh, pre-warmed medium to remove any residual antibiotics or waste products that could influence the outgrowth phase.
- Cause 3: Low Temporal Resolution for Outgrowth.
- Solution: When measuring the switching from persistent to active state (outgrowth), sample frequently. A low resolution will miss rapid changes in the population dynamics. Use high-throughput methods like plate readers or flow cytometry for continuous monitoring.
Difficulty in Distinguishing Between Slow-Growing and Truly Dormant Cells
Problem: It is challenging to confirm whether surviving cells are genuine, non-growing persisters or merely slow-growing variants.
Possible Causes and Solutions:
- Cause 1: Reliance on Single Time-Point Assays.
- Solution: Employ time-kill curve assays. Genuine persisters will show a biphasic killing pattern, with an initial rapid drop (killing of active cells) followed by a flat plateau where the number of surviving cells remains constant over time [1].
- Cause 2: Lack of Direct Metabolic Activity Measurement.
- Solution: Supplement colony-forming unit (CFU) counts with direct measures of metabolic activity. Use fluorescent dyes that stain metabolically active cells (e.g., GFP under a growth-promoter) in combination with viability stains. True persisters will be viable but non-fluorescent.
Key Experimental Protocols & Data Presentation
Protocol: Isolation and Quantification of Persisters from Biofilms
Biofilms are a major reservoir of persister cells and are highly relevant to chronic infections [5].
Detailed Methodology:
- Biofilm Growth: Grow a biofilm in a suitable system (e.g., Calgary Biofilm Device, flow cell) using your chosen growth medium for 24-48 hours.
- Harvesting: Gently scrape or sonicate (at a low, standardized power to disaggregate without killing) the biofilm into a suspension.
- Antibiotic Selection:
- Dissociate the biofilm cluster via gentle vortexing or pipetting.
- Treat the suspension with a high concentration of a bactericidal antibiotic (e.g., 100x MIC of ciprofloxacin for E. coli) for a defined period (e.g., 5 hours) to kill all planktonic and actively growing cells.
- Include a control sample without antibiotic treatment to determine the total initial cell count.
- Washing and Plating:
- After antibiotic exposure, pellet the cells by centrifugation.
- Wash the pellet twice with phosphate-buffered saline (PBS) or fresh medium to remove the antibiotic completely.
- Resuspend the final pellet and perform serial dilutions for spot-plating on drug-free agar plates.
- Enumeration: Count the colonies that appear after incubation. These are the persister cells that survived antibiotic treatment. The persister frequency is calculated as (CFU/mL after antibiotic treatment) / (CFU/mL before antibiotic treatment).
Protocol: High-Throughput Single-Cell Density Measurement for State Transition Profiling
This advanced protocol allows for the rapid tracking of physiological changes in cells, which can be correlated with state switching [43].
Detailed Methodology:
- Sample Preparation: Prepare a single-cell suspension of your bacterial culture in an appropriate isotonic buffer.
- Fluorescent Staining for Volume Measurement: Suspend the cells in a fluorescent dye that cannot be absorbed by the cells (e.g., a membrane-impermeant dye). This creates a background fluorescence from which the cell volume can be derived.
- Mass and Density Measurement:
- Flow the cell suspension through a specialized microfluidic device called a suspended microchannel resonator (SMR).
- As each cell passes through a microcantilever, its buoyant mass is measured with high precision based on the shift in the cantilever's vibration frequency.
- The cell's volume is simultaneously determined by the dip in fluorescent signal as it passes a microscope point.
- Data Analysis: The density of each cell is calculated in real-time from its mass and volume. By measuring up to 30,000 cells per hour, you can build a high-resolution profile of population heterogeneity and track density shifts associated with state transitions, such as the drop in density observed when T-cells become activated [43].
Table 1: Summary of Key Quantitative Findings from Cited Research
| Finding / Metric | Value / Result | Experimental Context | Research Significance |
|---|---|---|---|
| Throughput of Density Measurement [43] | Up to 30,000 cells/hour | SMR combined with fluorescent volume measurement | Enables high-resolution, dynamic profiling of cell state transitions at the single-cell level. |
| Density Change in T-cell Activation [43] | Drop from ~1.08 g/mL to ~1.06 g/mL | Human T-cells transitioning from quiescent to active state | Suggests increased water uptake during activation; density serves as a rapid, functional biomarker. |
| Biofilm-Associated Infections [5] | >65% of all infections | Clinical analysis of chronic infections | Highlights the critical importance of understanding and targeting persisters within biofilms. |
| Large Text Contrast Ratio (WCAG) [44] [45] | At least 4.5:1 | Web accessibility guidelines for visualizations | A minimum standard for ensuring diagrams and charts are readable for all users, crucial for publication. |
| Other Text Contrast Ratio (WCAG) [44] [45] | At least 7:0:1 | Web accessibility guidelines for visualizations | A minimum standard for ensuring diagrams and charts are readable for all users, crucial for publication. |
The Scientist's Toolkit: Research Reagent Solutions
Table 2: Essential Materials for Studying Cell State Switching and Persistence
| Item | Function / Application | Example / Note |
|---|---|---|
| Suspended Microchannel Resonator (SMR) | Measures buoyant mass and, when combined with fluorescence, density of single cells. Ideal for tracking physiological state changes [43]. | Commercial systems or custom-built setups as used in Manalis lab. |
| Bactericidal Antibiotics | Used for selective killing of growing cells to isolate and enumerate the non-growing persister subpopulation [5] [1]. | Aminoglycosides (e.g., amikacin), Fluoroquinolones (e.g., ciprofloxacin). |
| Microfluidic Biofilm Reactors | Provides a controlled environment for growing biofilms under defined shear stress and nutrient conditions, key for studying environment-dependent persistence [5]. | Calgary Biofilm Device, flow cells. |
| Flow Cytometer | Enables high-throughput analysis and sorting of cells based on size, granularity, and fluorescence (e.g., using viability dyes, GFP-reporters) [46]. | Can be used for analyzing heterogeneity and isolating subpopulations. |
| Fluorescent Viability/Activity Dyes | To distinguish between live/dead cells and to gauge metabolic activity, helping to differentiate dormant persisters from active cells. | Propidium Iodide (dead stain), GFP under a growth-promoter (active stain). |
| Chemostat/Chemostat Cultures | Maintains microbial cells in a constant, nutrient-limited growth state for prolonged periods. Essential for precisely controlling substrate availability [1]. | Allows study of persistence under stable, defined environmental conditions. |
Signaling Pathways and Experimental Workflows
Cell State Switching to Persister
Nuclei Prep for scRNA-seq
Experimental Platforms for Controlling Substrate Availability In Vitro
FAQs on Substrate Availability and Bacterial Persistence
Q1: Why is controlling substrate availability critical in persister cell research?
Substrate availability, particularly nutrients, is a primary environmental trigger for the formation of persister cells—dormant, antibiotic-tolerant bacterial subpopulations responsible for chronic and relapsing infections [4]. When substrates become limited, it induces a stress response that can push a subpopulation of bacteria into a dormant, persistent state [1] [11]. This state is characterized by low metabolic activity, allowing them to survive antibiotic treatments that typically target active cellular processes [4]. Therefore, precise control over substrate in in vitro models is essential for studying the conditions that lead to persistence and for screening potential anti-persister compounds.
Q2: What are the main types of persisters formed in response to substrate levels?
Persisters are broadly classified based on their formation mechanisms, which are heavily influenced by growth phase and substrate availability:
- Type I (Triggered Persisters): These form during the transition into the stationary phase, largely triggered by the depletion of a substrate or other environmental stresses [1] [4]. They are a pre-existing subpopulation of non-growing cells.
- Type II (Stochastic Persisters): These are generated spontaneously at a low rate throughout the exponential growth phase, even in nutrient-rich conditions, and are characterized by slow growth [1] [4].
- Type III (Specialized Persisters): This class exhibits persistence mechanisms specific to particular antibiotics and can be induced by stress signals, not necessarily relying on slow growth alone [4].
Q3: What key molecular mechanisms link low substrate availability to persistence?
The primary molecular link is the stringent response. Upon substrate limitation, bacteria produce the alarmone (p)ppGpp, which orchestrates a massive reprogramming of cellular metabolism [11]. This response promotes dormancy and has been shown to activate key persistence pathways, most notably Toxin-Antitoxin (TA) systems [11] [4]. Activated TA toxins (e.g., MqsR, TisB) can halt essential processes like translation and reduce ATP levels, driving cells into a protective, dormant state [11].
Q4: How can in vitro models dynamically control substrate to mimic in vivo conditions?
Computational models, such as agent-based models, are valuable tools for simulating complex in vivo environments. These models can incorporate substrate diffusion gradients and simulate how local substrate availability affects bacterial behavior, including persister formation [14]. For example, an agent-based model can simulate the growth of a biofilm where cells at the core, with limited substrate access, develop higher persistence levels than those at the nutrient-rich surface [14]. This allows researchers to test and optimize periodic antibiotic dosing regimens designed to exploit the "reawakening" of persisters when substrates become available, potentially reducing the total antibiotic dose required by up to 77% [14].
Troubleshooting Guides for Substrate-Linked Experimental Issues
Table 1: Troubleshooting Persistence Assays
| Problem | Potential Cause | Suggested Solution |
|---|---|---|
| High & Variable Persister Levels Between Replicates | Inconsistent substrate concentration or growth phase at time of antibiotic challenge. | Standardize inoculum age and ensure cultures are grown to the precise optical density (OD) for the target phase (e.g., mid-exponential vs. stationary) [11]. |
| Low Persister Frequency in Stationary Phase | Substrate not fully depleted, preventing entry into deep dormancy. | Confirm culture has entered true stationary phase by monitoring OD over time. Use a defined medium to ensure a single substrate is limiting [4]. |
| Inability to Eradicate Persisters in a Biofilm Model | Substrate gradients creating sanctuaries of deep persisters in the biofilm core. | Combine antibiotics with molecules that disrupt the biofilm matrix or use periodic dosing to kill cells as they resuscitate due to nutrient fluctuations [14]. |
Quantitative Data on Substrate and Treatment Efficacy
Table 2: Impact of Optimized Treatment on Bacterial Survival
The following table summarizes key quantitative findings from an agent-based modeling study that tuned periodic antibiotic dosing to biofilm substrate dynamics [14].
| Treatment Strategy | Total Antibiotic Dose | Bacterial Survival | Key Conditioning Factor |
|---|---|---|---|
| Conventional Continuous Dosing | 100% (Baseline) | High (Baseline) | N/A |
| Untuned Periodic Dosing | Variable | Moderate Reduction | Ineffective against all persister subpopulations. |
| Optimized Periodic Dosing | Reduced by nearly 77% | Significantly Lower | Aligned with biofilm persister switching dynamics [14]. |
Experimental Protocols for Key Methodologies
Protocol: Agent-Based Modeling of Biofilm Growth and Treatment
This protocol is adapted from a computational study that tested periodic dosing regimens [14].
1. Model Initialization:
- Surface: Initialize a defined two-dimensional surface.
- Inoculation: Randomly place a set number of susceptible bacterial cells (e.g., 27) on the surface to mimic initial adhesion [14].
2. Biofilm Growth Dynamics:
- Substrate Diffusion: Model the diffusion of a growth-limiting substrate from the bulk liquid above the biofilm.
- Cell Growth: Simulate growth of individual cells (agents) using Monod kinetics, where the growth rate is a function of local substrate concentration [14].
dm_i/dt = m_i * μ_max * (C_S / (C_S + K_S))- where
m_iis cell mass,μ_maxis max growth rate,C_Sis local substrate concentration, andK_Sis half-saturation constant [14].
- Cell Division: A cell divides upon reaching a threshold mass, splitting into two daughter cells with a random 40-60% mass distribution [14].
3. Incorporation of Persister Dynamics:
- State Switching: Program cells to stochastically switch between susceptible and persister states.
- Switching Triggers: Define switching rates to be dependent on both local substrate availability and the presence of antibiotics, creating a more realistic model [14].
4. Simulating Antibiotic Treatment:
- Diffusion: Model the diffusion of the antibiotic from the bulk liquid.
- Killing Kinetics: Implement different kill rates for susceptible and persister cells upon exposure.
- Testing Regimens: Run simulations to compare the efficacy of continuous vs. periodic antibiotic dosing schedules, measuring total dose required and final biofilm eradication [14].
Signaling Pathways and Workflow Diagrams
The Scientist's Toolkit: Research Reagent Solutions
Table 3: Essential Materials for Substrate-Linked Persistence Research
| Item | Function in Research | Specific Example / Note |
|---|---|---|
| Defined Minimal Medium | Allows precise control and limitation of a single substrate (e.g., carbon, nitrogen source) to trigger starvation-induced persistence. | M9 or MOPS medium with a defined carbon source like glucose [4]. |
| Continuous Culture System (Chemostat) | Maintains bacterial cultures in a constant, nutrient-limited state at a defined growth rate for studying steady-state persistence. | Useful for studying Type II stochastic persisters under controlled substrate availability. |
| Agent-Based Modeling Software | Computationally simulates the effects of substrate gradients and cellular heterogeneity on persister formation and treatment outcomes. | NetLogo platform, as used in published studies [14]. |
| ATP Assay Kit | Quantifies cellular ATP levels, a key metric for metabolic activity and dormancy depth in persister cells [47]. | Confirms low metabolic state in isolated persisters. |
| Lon Protease Inhibitor | Investigates the role of TA systems; Lon degrades antitoxins, freeing toxins to induce dormancy [11]. | Tool for validating TA system mechanism in persistence. |
Correlating Metabolic Activity with Antibiotic Killing Curves
Fundamental Concepts FAQ
What is the relationship between bacterial metabolic activity and antibiotic killing curves? Antibiotic killing curves typically show biphasic kinetics, characterized by an initial rapid killing phase of the majority population, followed by a much slower second phase. This second phase represents the survival of a subpopulation of phenotypically tolerant cells known as persisters [29] [1]. The core relationship is that a reduction in cellular metabolic activity is a key mechanism enabling this tolerance. Persisters are often dormant or slow-growing, which shields them from antibiotics that target active cellular processes like cell wall synthesis, transcription, and translation [48] [1] [49]. The metabolic state of the bacteria is a stronger predictor of antibiotic efficacy than the drug concentration alone [49].
How do "antibiotic persistence" and "antibiotic resistance" differ in the context of metabolism? It is crucial to distinguish these concepts, as their underlying mechanisms and clinical implications differ significantly. The table below summarizes the key differences:
| Feature | Antibiotic Persistence | Antibiotic Resistance |
|---|---|---|
| Genetic Basis | Non-heritable, phenotypic variation [29] [48] | Heritable, via genetic mutations or acquisition of resistance genes [29] |
| Population Impact | Small subpopulation of cells [29] [48] | Entire population [29] |
| Measurement | Biphasic killing curve; MDK99 (Minimum Duration for Killing 99%) [29] | Increased MIC (Minimum Inhibitory Concentration) [29] [50] |
| Metabolic State | Associated with dormancy or reduced metabolic activity [1] [49] | Can occur in actively metabolizing cells [29] |
| Post-Treatment | Population regrows and remains susceptible to the same antibiotic [48] | Population remains resistant upon regrowth [29] |
Why is substrate availability critical for research on preventing persister formation? Substrate availability, particularly carbon sources, directly controls bacterial growth and metabolic flux. Transitions between carbon sources have been shown to stimulate persister formation [12]. Optimizing substrate availability in experimental models ensures a more uniform metabolic state, preventing the stochastic emergence of dormant cells. Furthermore, research shows that supplementing with specific metabolites can "re-sensitize" persisters by re-awakening their metabolism, making them vulnerable to antibiotic killing again. This forms the basis of the "wake-and-kill" therapeutic strategy [49].
Experimental Protocols & Data Analysis
Protocol: Generating and Analyzing an Antibiotic Killing Curve
This protocol is used to assess the tolerance of a bacterial population to a bactericidal antibiotic and quantify the persister fraction.
Materials:
- Late-exponential or early-stationary phase bacterial culture (e.g., E. coli, P. aeruginosa)
- Appropriate liquid growth medium (e.g., Lysogeny Broth (LB), Mueller Hinton Broth)
- Sterile antibiotic stock solution (e.g., Ofloxacin, Ampicillin)
- Phosphate Buffered Saline (PBS) for serial dilution
- Agar plates for colony counting
Method:
- Inoculum Preparation: Grow bacteria to the late-exponential/early-stationary phase (e.g., dilute an overnight culture 1:1000 in fresh medium and grow for 5 hours) [51].
- Antibiotic Challenge: Add a high concentration of a bactericidal antibiotic (e.g., 5 µg/mL ofloxacin) to the culture. The concentration should far exceed the MIC for the strain [51].
- Time-point Sampling: Immediately before adding antibiotic (t=0) and at regular intervals after (e.g., 1, 2, 4, 6, 8, and 24 hours), aseptically remove a sample aliquot.
- Viable Count: Serially dilute each sample in PBS and plate onto antibiotic-free agar plates. Incubate plates for 16-24 hours and count the resulting colonies (CFU/mL).
- Data Plotting: Plot the log10(CFU/mL) versus time to generate the killing curve.
Troubleshooting: Inconsistent Biphasic Curve
- Problem: Lack of a clear biphasic pattern.
- Solution: Ensure the culture is in the correct growth phase. Persister levels are often higher in stationary phase cultures. Verify the antibiotic concentration is sufficiently bactericidal and that the stock solution is potent.
Protocol: Modulating Metabolism to Eradicate Persisters
This protocol tests the effect of metabolic inhibitors as adjuvants to reduce the persister fraction [51].
Materials:
- Bacterial culture prepared as above
- Antibiotic stock (e.g., Ofloxacin)
- Metabolic inhibitor stocks (e.g., Thioridazine (TDZ), Chloramphenicol, Rifampicin, Arsenate)
- Sterile DMSO (if needed for solvent-soluble compounds)
Method:
- Treatment Conditions:
- Viable Count: After a total incubation of 20-24 hours with the antibiotic, sample and determine the CFU/mL as in the previous protocol.
- Data Analysis: Compare the final survival fraction (CFU/mL at end / CFU/mL at start) across different treatment conditions.
Expected Results & Data Presentation: Metabolic inhibitors like Chloramphenicol (translation inhibitor) often exhibit antagonism with antibiotics, increasing persister survival. In contrast, proton motive force (PMF) disruptors like Thioridazine can show strong synergy [51]. The table below quantifies this effect:
Table: Synergy Scores of Metabolic Inhibitors with Ofloxacin against E. coli [51]
| Metabolic Inhibitor (Function) | Pre-treatment Synergy | Co-treatment Synergy | Post-treatment Synergy | Interpretation |
|---|---|---|---|---|
| Thioridazine (PMF disruptor) | High Positive | High Positive | Low | Strong synergy when added before/with antibiotic |
| Chloramphenicol (Translation inhibitor) | Negative | Negative | Negative | Antagonism |
| Rifampicin (Transcription inhibitor) | Negative | Negative | Negative | Antagonism |
| Arsenate (ATP production inhibitor) | Negative | Negative | Negative | Antagonism |
Synergy scores are calculated using models like HSA, Bliss, ZIP, or Loewe. A positive score indicates synergy, zero indicates additivity, and a negative score indicates antagonism [51].
Metabolic Pathways to Persistence
The following diagram illustrates the key metabolic pathways that lead to the formation of persister cells, connecting external stresses to dormancy and antibiotic tolerance.
Fig. 1: Metabolic Pathways to Antibiotic Tolerance. External stresses activate the stringent response and toxin-antitoxin modules, leading to a shutdown of metabolism and dormancy, which confers tolerance [48] [1] [12].
The Scientist's Toolkit
Table: Essential Research Reagents for Metabolic Persistence Studies
| Reagent/Category | Function in Research | Key Examples |
|---|---|---|
| Metabolic Inhibitors | Probe the role of specific metabolic pathways in persistence [51]. | Thioridazine (PMF disruptor), Chloramphenicol (translation), Rifampicin (transcription), Arsenate (ATP production), Carbon source variants (e.g., Glucose, Glycerol) [12]. |
| Bactericidal Antibiotics | Induce persister formation in killing curve assays [29] [51]. | Fluoroquinolones (e.g., Ofloxacin, Ciprofloxacin), β-lactams (e.g., Ampicillin), Aminoglycosides. |
| Exogenous Metabolites | "Wake-and-kill" strategy; re-sensitize persisters by restoring metabolism [49]. | Sugars (e.g., Mannitol, Pyruvate), Amino acids, Nucleotide precursors. |
| Standard Laboratory Strains | Model organisms for genetic and mechanistic studies. | Escherichia coli, Pseudomonas aeruginosa, Staphylococcus aureus. |
| Specialized Growth Media | Control nutrient availability and induce metabolic stresses. | Defined minimal media, Media for carbon source switching [12]. |
Workflow for a "Wake-and-Kill" Experiment
The "wake-and-kill" strategy is a promising therapeutic approach to eradicate persisters. The diagram below outlines a generalized experimental workflow to test this strategy.
Fig. 2: "Wake-and-Kill" Experimental Workflow. This workflow tests the hypothesis that awakening persisters with metabolites re-sensitizes them to antibiotic killing [49].
Strategies for Substrate Modulation to Prevent and Eradicate Persisters
Overcoming Physiologic Heterogeneity in Biofilm Microenvironments
Frequently Asked Questions (FAQs)
What are the primary causes of physiologic heterogeneity in biofilms? Physiologic heterogeneity in biofilms arises primarily from two interconnected mechanisms. First, chemical and nutrient gradients form due to bacterial metabolic activity and limited solute diffusion within the biofilm matrix. This creates microenvironments with varying concentrations of oxygen, nutrients, and waste products [52] [53]. Second, even in identical local conditions, stochastic gene expression can lead to phenotypic variation between genetically identical, adjacent cells [54]. These factors together generate a spectrum of physiological states, including metabolically active, slow-growing, and dormant cells.
Why do standard antimicrobial protocols often fail against biofilms? Standard protocols typically target metabolically active cells and are ineffective against the dormant or slow-growing subpopulations known as persister cells that are sheltered within the biofilm [1]. The biofilm's extracellular polymeric substance (EPS) matrix acts as a diffusion barrier, reducing antimicrobial penetration and creating concentration gradients [55] [56]. Furthermore, the heterogeneous metabolism means that antibiotics requiring active cellular processes fail to kill dormant persisters, leading to treatment failure and infection relapse [1] [7].
How does substrate availability directly influence persister cell formation? Substrate limitation is a key environmental stressor that induces a dormant, non-growing state. Nutrient starvation, especially for carbon sources, triggers cellular stress responses (e.g., the stringent response) that shut down energy-intensive processes like translation and replication [1] [54]. This metabolic quiescence is a hallmark of persister cells, allowing them to tolerate antibiotics. Gradients of electron acceptors like oxygen are particularly influential; oxygen-rich zones near the biofilm surface support aerobic respiration, while anoxic zones in the interior force cells into fermentative or other anaerobic metabolisms, drastically altering their physiology and antibiotic susceptibility [52] [53].
Troubleshooting Common Experimental Challenges
Challenge 1: Inconsistent Persister Cell Yields
| Symptom | Possible Cause | Solution |
|---|---|---|
| Low persister counts after antibiotic challenge | Biofilms grown under overly rich nutrient conditions, minimizing starvation-induced dormancy. | Standardize biofilm growth in nutrient-limited media (e.g., minimal media with low carbon) or transition to stationary phase before experimentation [1]. |
| High variability in persister numbers between replicates | Fluctuations in the local microenvironment (e.g., temperature, gas exchange) during static biofilm growth. | Use flow-cell or bioreactor systems to maintain a consistent and controllable environment throughout biofilm development [57] [56]. |
| Failure to observe a biphasic killing curve | Antibiotic concentration is too low or killing time is insufficient. | Confirm the Minimum Inhibitory Concentration (MIC) and apply a concentration 10-100x MIC. Extend treatment time to ensure complete killing of planktonic and susceptible biofilm cells [1] [56]. |
Challenge 2: Difficulty in Characterizing Microenvironmental Gradients
| Symptom | Possible Cause | Solution |
|---|---|---|
| Inability to verify gradient formation | Reliance on bulk measurements that average conditions across the entire biofilm. | Incorporate microsensor technology (e.g., O₂, pH, specific ions) for direct, spatially-resolved measurement of gradients [52] [53]. |
| Lack of spatial resolution in metabolic activity data | Using destructive, whole-biofilm assays like crystal violet or CFU counts. | Implement fluorescence-based techniques with reporter constructs for metabolic genes or stains for viability (e.g., CTC for respiratory activity) combined with confocal laser scanning microscopy (CLSM) [52] [54]. |
Key Experimental Protocols & Data
Protocol: Isolation and Quantification of Biofilm-Associated Persister Cells
This protocol is designed to isolate the tolerant persister subpopulation from a mature biofilm after antibiotic treatment [1] [56].
- Biofilm Growth: Grow a mature biofilm (typically 24-72 hours) using a standardized model like the Calgary Biofilm Device (peg lid) or a flow-cell system.
- Antibiotic Challenge: Expose the biofilm to a high concentration of a bactericidal antibiotic (e.g., 100x MIC of ciprofloxacin or ampicillin) for a defined period (e.g., 3-5 hours) to kill planktonic and susceptible biofilm cells.
- Washing and Dispersal: Carefully wash the biofilm twice with sterile saline or buffer to remove the antibiotic and any dead cells. Physically disrupt the biofilm (e.g., by sonication or vortexing with beads) to release the viable, protected cells into suspension.
- Persister Quantification: Serially dilute the cell suspension and spot-plate onto fresh, antibiotic-free agar plates. Count the Colony Forming Units (CFUs) after 24-48 hours of incubation. These colonies represent persister cells that survived the antibiotic challenge and regained proliferative capacity.
Quantitative Data on Biofilm Antimicrobial Tolerance
The table below summarizes the dramatically increased tolerance observed in biofilms and persister cells compared to their planktonic counterparts.
Table 1: Comparative Antimicrobial Susceptibility of Planktonic vs. Biofilm Cells
| Bacterial Species | Antimicrobial Agent | Planktonic MIC (µg/mL) | Biofilm Tolerance Level (e.g., MBIC/MIC ratio) | Key Tolerant Mechanism | Reference |
|---|---|---|---|---|---|
| Pseudomonas aeruginosa | Tobramycin | 1 | Up to 1000-fold increase in survival | Quorum-sensing dependent tolerance, matrix barrier | [52] |
| Escherichia coli | Ampicillin | 10 | Biphasic killing with a persistent subpopulation | Metabolic dormancy, stochastic expression of toxin-antitoxin modules | [1] [56] |
| Staphylococcus aureus | Ciprofloxacin | 0.5 | High persister frequency post-treatment | Reduced membrane potential, low metabolic activity | [1] [7] |
Abbreviations: MIC: Minimum Inhibitory Concentration; MBIC: Minimum Biofilm Inhibitory Concentration.
The Scientist's Toolkit: Key Research Reagent Solutions
Table 2: Essential Reagents for Biofilm and Persister Cell Research
| Reagent / Material | Function / Application | Key Consideration |
|---|---|---|
| Crystal Violet Stain | Colorimetric quantification of total adhered biofilm biomass. | Does not distinguish between live/dead cells or cells/matrix [57]. |
| CTC (5-Cyano-2,3-Ditolyl Tetrazolium Chloride) | Fluorescent stain used to detect metabolically active/respiring cells within biofilms via CLSM. | Signal is dependent on electron transport activity; dormant cells may not be stained [52]. |
| LIVE/DEAD BacLight Viability Kit | Dual staining (SYTO9/PI) to differentiate intact (live) and damaged (dead) cell membranes. | Can overestimate viability in biofilms as persisters have intact membranes but are non-growing [57]. |
| Microsensors (e.g., O₂, pH) | Direct measurement of chemical gradients within biofilms at micron-scale resolution. | Requires specialized equipment and calibration; can be invasive [52] [53]. |
| DNase I | Enzyme that degrades extracellular DNA (eDNA) in the biofilm matrix. | Used to study matrix integrity and its role in antimicrobial penetration and tolerance [55]. |
| Eravacycline | A fluorocycline antibiotic identified as a potent anti-persister compound. | Effective due to its ability to penetrate dormant cells via energy-independent diffusion and bind strongly to its target [7]. |
Conceptual Diagrams and Workflows
Biofilm Heterogeneity and Persister Formation
Experimental Workflow for Anti-Persister Compound Screening
Optimizing Carbon Source Selection to Maintain Metabolic Activity
Frequently Asked Questions (FAQs)
Why is carbon source selection critical in persister cell research? The choice of carbon source directly influences the metabolic state of bacteria. Research shows that persister cells, which are dormant variants that tolerate antibiotics, undergo a major metabolic shutdown. However, the extent of this shutdown depends on the available carbon source. Using a suboptimal carbon source can inadvertently increase persister formation by deepening metabolic dormancy, making it crucial to select one that maintains baseline metabolic activity for studies aimed at preventing or eradicating persisters [58] [59].
What are the key metabolic differences in persister cells? Persister cells exhibit significantly reduced metabolic activity compared to normal cells. Key findings from isotopic tracing studies include [58] [59]:
- Reduced and Delayed Metabolism: Peripheral pathways, including parts of the central carbon metabolic pathway, the pentose phosphate pathway, and the tricarboxylic acid (TCA) cycle, show delayed labeling dynamics.
- Slowed Protein Synthesis: There is a generalized reduction in the labeling of proteinogenic amino acids.
- Carbon Source Dependence: The metabolic shutdown is far more pronounced when persister cells utilize acetate compared to glucose.
Which carbon source is better for maintaining metabolic activity in E. coli cultures? For maintaining metabolic activity and potentially reducing the depth of persistence, glucose is superior to acetate. Under acetate conditions, persister cells exhibit a "more substantial metabolic shutdown," with markedly reduced labeling across nearly all pathway intermediates and amino acids. This is likely due to the ATP demand required to activate acetate for entry into central metabolism, which is problematic in the energy-depleted persister state [59].
Troubleshooting Guide
Problem: High Persister Cell Formation in Batch Cultures
| Symptom | Potential Cause | Recommended Solution |
|---|---|---|
| High proportion of cells surviving antibiotic treatment during mid-log phase. | Use of a poor carbon source (e.g., acetate) that promotes metabolic dormancy. | Switch the primary carbon source from acetate to glucose [59]. |
| Inconsistent persister counts between experimental replicates. | Depletion of the carbon source, leading to starvation and heterogeneity in metabolic states. | Monitor culture growth and ensure carbon source is not depleted; use a sufficient concentration (e.g., 2 g/L) [59]. |
| Low metabolic activity in control cells, compliculating data interpretation. | Carbon source is not efficiently utilized by the bacterial strain, leading to a pre-existing dormant subpopulation. | Validate the strain's ability to consume the carbon source and confirm it supports robust growth in non-stressed conditions. |
Problem: Poor Data Interpretation from Metabolic Flux Studies
| Symptom | Potential Cause | Recommended Solution |
|---|---|---|
| Low signal-to-noise ratio in isotopic labeling data. | Insufficient incorporation of the stable isotope label due to low metabolic activity. | Use U-13C-glucose instead of 2-13C-sodium acetate for a stronger labeling signal in persister populations [59]. |
| High variability in metabolite labeling patterns. | Inadequate washing steps post-induction, leaving residual carbon sources that dilute the label. | Increase the number of wash steps (e.g., three times) in carbon source-free medium after persister induction and before labeling [59]. |
Featured Experimental Protocol
The following is a detailed methodology for investigating metabolic states in persister cells using stable isotope labeling, adapted from a key study [59].
Objective: To trace the functional metabolic pathways in E. coli persister cells and compare them to normal cells using 13C-labeled carbon sources.
Materials:
- Bacterial Strain: Escherichia coli BW25113 [59].
- Culture Medium: M9 minimal medium [59].
- Carbon Sources:
- 2 g/L 1,2–13C2 glucose (CLM-504-PK, Cambridge Isotope Laboratories, Inc.)
- 2 g/L 2–13C sodium acetate (CLM-381-PK, Cambridge Isotope Laboratories, Inc.) [59].
- Persister Inducing Agent: 100 μg/mL Carbonyl cyanide m-chlorophenyl hydrazone (CCCP) [59].
- Key Equipment: Centrifuge, Liquid Nitrogen, Lyophilizer, LC-MS/MS System, GC-MS System [59].
Procedure:
- Culture and Induction:
- Grow an overnight culture of E. coli in M9 medium with 2 g/L glucose.
- Sub-culture into fresh medium to an OD600 of 0.05 and incubate at 37°C with shaking at 200 rpm.
- When the sub-culture reaches OD600 of 0.5, immediately expose the cells to 100 μg/mL of CCCP for 15 minutes to induce persister formation [59].
- Cell Harvesting and Washing:
- Collect cells by centrifugation at 13,000 rpm for 3 minutes at room temperature.
- Wash the cell pellet three times in M9 medium without a carbon source to remove CCCP and residual nutrients [59].
- Stable Isotope Labeling:
- Concentrate the control and induced persister cells to an OD600 of 5 in 10 mL of M9 medium.
- Initiate the tracer experiment by adding either 2 g/L 13C-glucose or 2 g/L 13C-acetate.
- Incubate at 37°C with shaking and collect samples at specific timepoints (e.g., 0, 20 seconds, 5 minutes, 30 minutes, 2 hours) [59].
- Metabolic Quenching and Extraction:
- At each timepoint, rapidly cool samples using liquid nitrogen to halt all metabolic activity within seconds.
- Centrifuge the quenched samples at 4°C and 5,000 × g for 3 minutes. Store the cell pellets at -80°C [59].
- For metabolite analysis:
- Lyophilize the cell pellet.
- Add 0.5 mL of an 80:20 methanol-water extraction solution and incubate at -20°C for 1 hour.
- Centrifuge at 10,000 × g for 10 minutes at 0°C.
- Filter the supernatant through a 0.2 µm filter for LC-MS analysis [59].
- For proteinogenic amino acid analysis:
- Hydrolyze the remaining cell pellet with 1.5 mL of 6 N HCl at 100°C for 18 hours.
- Analyze the hydrolyzed amino acids using the TBDMS method via GC-MS [59].
Experimental Workflow and Metabolic Pathways
Persister Cell Metabolic Analysis Workflow
Central Carbon Metabolism in Persisters
The Scientist's Toolkit: Research Reagent Solutions
| Reagent / Material | Function in the Experiment |
|---|---|
| CCCP (Carbonyl cyanide m-chlorophenyl hydrazone) | A protonophore that disrupts the membrane potential, reversibly inducing a persister-like dormant state without using antibiotics, allowing for clean metabolic analysis [59]. |
| 1,2–13C2 Glucose | A stable isotope-labeled tracer used to map functional flux through central carbon metabolism, glycolysis, and the pentose phosphate pathway [59]. |
| 2–13C Sodium Acetate | A stable isotope-labeled tracer used to investigate metabolic flux through the TCA cycle, especially revealing the profound metabolic shutdown in persisters on this carbon source [59]. |
| M9 Minimal Medium | A defined chemical medium that allows precise control over the carbon source presented to the bacteria, essential for reproducible metabolic studies [59]. |
| Methanol-Water (80:20) | A standard quenching and extraction solution used to rapidly halt metabolism and extract intracellular metabolites for LC-MS analysis [59]. |
Bacterial persisters are a subpopulation of growth-arrested, metabolically inactive cells that exhibit extreme tolerance to conventional antibiotics. Unlike resistant bacteria, persister cells do not possess genetic mutations; their survival is a reversible phenotypic state. This dormancy allows them to survive antibiotic treatment and subsequently regrow, causing relapsing and chronic infections that pose a significant challenge in clinical settings and pharmaceutical development [1] [17]. The formation of persister cells is closely linked to environmental conditions, with substrate availability (nutrients) being a critical trigger. Research demonstrates that nutrient limitation and starvation conditions significantly increase the persister cell fraction within bacterial populations [5] [60] [4]. This technical resource center provides established methodologies and troubleshooting guides for researchers investigating how strategic manipulation of substrate availability can prevent persister formation and synergistically enhance antibiotic efficacy.
FAQs: Core Concepts for Researchers
Q1: What is the fundamental relationship between substrate availability and bacterial persistence?
Substrate limitation is a primary environmental trigger for bacterial persistence. As nutrients become scarce, a subpopulation of bacteria transitions into a dormant, slow-growing or non-growing state. This state is characterized by reduced metabolic activity, which decreases the efficacy of most antibiotics that target active cellular processes. The proportion of persister cells typically increases as a bacterial culture moves from the exponential growth phase into the stationary phase, where substrate depletion occurs [5] [60]. Mathematical models have quantified this relationship, showing that the persister population begins to increase significantly as substrate concentration decreases in a batch culture [60].
Q2: How can controlling substrate availability synergize with antibiotic treatments?
Substrate control can synergize with antibiotics through several mechanistic pathways:
- Preventing Persistence Induction: Maintaining adequate substrate levels can prevent the large-scale shift of bacterial cells into the dormant persister state, thereby keeping a larger portion of the population susceptible to antibiotics [60] [4].
- "Reawakening" Persisters: The controlled re-introduction of nutrients or specific metabolites can induce persister cells to exit dormancy and resume metabolic activity. Once these cells "wake up," they regain susceptibility to conventional antibiotics [14] [61]. Computational models suggest that periodic dosing regimens timed to these awakening events can reduce the total antibiotic dose required for eradication by up to 77% [14].
- Exploiting Physiological Weaknesses: Dormancy, while protective, alters cell physiology in ways that can be targeted. For instance, persister cells have reduced membrane potential and proton motive force, which inactivates energy-dependent efflux pumps. This allows certain amphiphilic antibiotics that penetrate cells via passive diffusion to accumulate to higher levels in persisters than in normal cells, leading to effective killing upon wake-up [61] [7].
Q3: What are the key parameters to model in substrate-antibiotic synergy experiments?
When developing mathematical or computational models to simulate and optimize these synergistic approaches, researchers should incorporate the following key parameters, derived from established agent-based and kinetic models [14] [60]:
- Substrate Concentration (
C_S): The local concentration of the limiting nutrient (e.g., glucose). - Switching Rates (
a,b): The rates at which normal cells switch to the persister state (a) and persister cells revert to the normal state (b). These rates should be modeled as dependent on substrate concentration and/or antibiotic presence. - Antibiotic Concentration (
C_A): The concentration of the antibiotic over time, especially for periodic dosing regimens. - Killing Rates (
k_n,k_p): The specific death rates of normal cells (k_n) and persister cells (k_p) when exposed to the antibiotic. - Growth Rates (
μ_n,μ_p): The specific growth rates of normal (μ_n) and persister (μ_p) subpopulations, typically modeled using Monod kinetics relative toC_S.
Table 1: Key Parameters for Modeling Substrate-Persistence Dynamics
| Parameter | Description | Typical Units | Model Dependency |
|---|---|---|---|
C_S |
Local substrate concentration | g/L or mM | Independent variable |
a |
Switching rate (Normal → Persister) | h⁻¹ | Function of C_S and C_A |
b |
Switching rate (Persister → Normal) | h⁻¹ | Function of C_S and C_A |
C_A |
Local antibiotic concentration | μg/mL or μM | Independent variable (treatment regimen) |
k_n |
Killing rate of normal cells | h⁻¹ | Function of C_A |
k_p |
Killing rate of persister cells | h⁻¹ | Function of C_A (often much lower than k_n) |
μ_n, μ_p |
Growth rates of normal and persister cells | h⁻¹ | Function of C_S (Monod kinetics) |
Q4: Which bacterial signaling pathways are most critical in substrate-induced persistence?
The transition to a persistent state in response to substrate limitation is governed by sophisticated cellular signaling pathways.
- The Stringent Response: This is a primary global response to nutrient starvation. It involves the rapid synthesis of the alarmone (p)ppGpp, which dramatically reprogrammes cellular metabolism, shuts down energy-intensive processes like ribosome synthesis, and promotes dormancy [1] [4].
- Toxin-Antitoxin (TA) Modules: These are genetic switches where a stable toxin protein can inhibit essential cellular processes (e.g., translation) and a labile antitoxin counteracts it. Stress conditions like nutrient starvation can lead to antitoxin degradation, freeing the toxin to induce growth arrest. The HipAB and other TA systems are frequently linked to persister formation [14] [1] [61].
- The SOS Response: This pathway is activated in response to DNA damage, which can be a secondary consequence of metabolic stress or antibiotic action. The SOS response can upregulate DNA repair functions and has been linked to increased persister formation, particularly in biofilm-associated populations [5] [1].
The following diagram illustrates the interplay between these pathways in response to substrate limitation:
Diagram 1: Signaling Pathways in Substrate-Induced Persistence
Troubleshooting Guides for Common Experimental Challenges
Inconsistent Persister Cell Yields
Problem: The fraction of persister cells obtained in stationary-phase cultures or after substrate depletion is highly variable between experimental replicates.
Potential Causes and Solutions:
- Cause 1: Inconsistent Substrate Depletion.
- Solution: Standardize inoculum preparation and growth medium volume-to-flask ratio to ensure reproducible aeration and growth kinetics. Use spectrophotometers to initiate experiments at a precise optical density (OD) and confirm substrate depletion with assays (e.g., glucose test strips) at the time of harvesting [60] [4].
- Cause 2: Unaccounted for Carbon Sources.
- Solution: Use defined minimal media instead of complex, nutrient-rich media like LB. Complex media can contain multiple carbon sources, leading to diauxic shifts and unpredictable persistence dynamics. This provides greater experimental control over the limiting substrate [60].
- Cause 3: Stochastic Nature of Persistence.
Failed Synergy in Antibiotic Killing Assays
Problem: The planned substrate control intervention does not yield the expected enhancement in antibiotic killing of the bacterial population.
Potential Causes and Solutions:
- Cause 1: Substrate Re-introduction Timing is Incorrect.
- Solution: The "reawakening" process is temporally sensitive. Use data from your model to time the antibiotic pulse to coincide with the expected resurgence of metabolic activity in persisters, not before. Monitor wake-up kinetically by measuring ATP levels or a fluorescent metabolic dye (e.g., AlamarBlue) in parallel control experiments [14] [61].
- Cause 2: The Antibiotic Requires Active Transport.
- Solution: Avoid antibiotics that rely on active, energy-dependent uptake mechanisms (e.g., aminoglycosides like tobramycin in the absence of potentiation), as these will not effectively enter dormant cells. Prioritize antibiotics that can penetrate cells via passive diffusion and are less affected by reduced membrane potential. Computational clustering has identified properties for ideal anti-persister agents, including positive charge, amphiphilicity, and energy-independent uptake [61] [7].
- Cause 3: Biofilm Confounding the Treatment.
- Solution: Biofilms present an additional physical and physiological barrier. If working with biofilms, consider combining your approach with agents that disrupt the extracellular polymeric substance (EPS) or use experimental setups that allow for precise control and measurement of substrate gradients within the biofilm structure [5] [14].
Discrepancies Between Model Predictions and Experimental Data
Problem: Results from in vitro experiments do not align with the outputs of your computational model of substrate-persister dynamics.
Potential Causes and Solutions:
- Cause 1: Over-simplified Switching Rates.
- Solution: Many basic models use constant switching rates. Refine your model by implementing substrate-dependent switching rates where the transition from normal to persister state (
a) increases as substrate concentration (C_S) falls below a threshold. Similarly, the reversion rate (b) can be modeled to increase upon substrate re-addition [60].
- Solution: Many basic models use constant switching rates. Refine your model by implementing substrate-dependent switching rates where the transition from normal to persister state (
- Cause 2: Ignoring Population Spatial Heterogeneity.
- Solution: In biofilms or microcolonies, nutrient gradients create heterogeneous microenvironments. Agent-based models (ABM) that incorporate spatial structure and local diffusion of substrates can more accurately simulate the non-uniform distribution of persister cells observed in structured populations, as opposed to simple deterministic models [14].
- Cause 3: Inaccurate Initial Parameter Estimation.
- Solution: Systematically calibrate your model parameters using dedicated experiments. For example, obtain killing curves for your specific strain and antibiotic at multiple time points during batch culture growth to accurately fit the parameters for
k_n,k_p, and the switching ratesaandb[60].
- Solution: Systematically calibrate your model parameters using dedicated experiments. For example, obtain killing curves for your specific strain and antibiotic at multiple time points during batch culture growth to accurately fit the parameters for
The Scientist's Toolkit: Key Reagents and Materials
Table 2: Essential Research Reagents for Substrate-Persister Studies
| Reagent / Material | Function / Application | Key Considerations |
|---|---|---|
| Defined Minimal Media | Provides precise control over the type and concentration of the growth-limiting substrate (e.g., glucose, nitrogen). | Essential for reproducible induction of substrate-limited persistence; avoids confounding effects of complex media [60]. |
| High-Persister (Hip) Mutant Strains | Model strains (e.g., E. coli HM22 with hipA7) that yield a higher baseline persister fraction. |
Useful for boosting signal-to-noise ratio in mechanistic studies and initial drug screening [61] [7]. |
| Metabolic Activity Dyes | Fluorescent probes (e.g., AlamarBlue, CTC, SYTOX stains) to distinguish and quantify live, dead, and dormant cells via flow cytometry or microscopy. | Critical for experimentally validating the metabolic state of the population before, during, and after treatment [61]. |
| ATP Assay Kits | Luciferase-based kits to measure cellular ATP levels, a direct indicator of metabolic activity. | Provides a quantitative measure of the "dormancy depth" of a population and the success of "reawakening" [47]. |
| Agent-Based Modeling Software | Platforms (e.g., NetLogo) to build spatially explicit models of biofilm growth and persister formation under substrate gradients. | Allows for simulation of complex, heterogeneous systems that are difficult to capture with ordinary differential equations [14]. |
This protocol provides a standardized method for investigating the synergy between substrate re-addition and antibiotic efficacy against bacterial persisters.
Objective: To determine if and when the controlled re-introduction of a limiting substrate can re-sensitize a population with a high persister fraction to a conventional antibiotic.
Workflow Summary:
Diagram 2: Substrate Re-introduction Experimental Workflow
Step-by-Step Methodology:
- Culture and Persistence Induction: Grow your bacterial strain (e.g., E. coli MG1655 or a Hip mutant) in a defined minimal medium with a single, limiting carbon source (e.g., 0.1% glucose) to mid-exponential phase. Transfer the culture to a fresh medium and allow it to grow into the stationary phase (e.g., for 24 hours) to induce persistence via substrate depletion. Confirm substrate depletion if possible [60] [4].
- Persister Isolation: Treat the stationary-phase culture with a high concentration of a bactericidal antibiotic (e.g., ampicillin at 100 µg/mL for 3-6 hours, depending on the strain) to kill the metabolically active population. The surviving cells will be highly enriched for persisters.
- Cell Washing: Centrifuge the antibiotic-treated culture, carefully discard the supernatant containing the antibiotic, and wash the cell pellet twice with sterile phosphate-buffered saline (PBS) or a similar non-nutritive buffer to remove all traces of the antibiotic and any residual substrates.
- Experimental Treatment Arms: Resuspend the washed persister cells in fresh buffer and divide them into equal aliquots for the following treatment arms:
- Control (Buffer + Antibiotic): Add only the antibiotic being tested.
- Test (Substrate + Antibiotic): Add the limiting substrate (e.g., 0.2% glucose) and the antibiotic.
- Wake-up Control (Substrate Only): Add only the substrate to monitor the natural regrowth of persisters in the absence of antibiotic.
- Incubation and Sampling: Incubate all treatment arms under optimal growth conditions. Sample at predetermined time points (e.g., 0, 1, 2, 4, 6 hours). Immediately serially dilute and plate samples onto fresh, rich agar plates for Colony Forming Unit (CFU) enumeration.
- Data Analysis: Calculate the log-reduction in CFU/mL for each arm compared to the T=0 count. A significantly greater log-reduction in the "Test" arm (Substrate + Antibiotic) compared to the "Control" arm (Buffer + Antibiotic) demonstrates successful re-sensitization. The "Wake-up Control" should show stable or increasing CFUs, confirming viability [14] [61].
Frequently Asked Questions (FAQs)
Q1: What is the key principle behind using intermittent dosing to eradicate bacterial persisters? Intermittent or pulse dosing alternates between periods of high antibiotic concentration ("on" periods) and periods of low or no antibiotic concentration ("off" periods). This approach is designed to target persister cells when they resuscitate and become metabolically active again during the antibiotic-free window, making them susceptible to killing in the next "on" pulse [62] [63].
Q2: My pulse dosing regimen isn't eradicating the bacterial population. What could be wrong? Failed eradication is often linked to an incorrect ratio of antibiotic "on" and "off" durations. The efficacy of pulse dosing critically depends on this ratio rather than the individual durations of each phase. An inappropriate ratio may kill normal cells but fail to effectively target resuscitating persisters [62]. Other common issues include non-compliance with the treatment schedule and insufficient contact time of the antibiotic during the "on" period [64].
Q3: How do I determine the optimal "on" and "off" times for a pulse dosing regimen?
The systematic design involves estimating parameters for bacterial switching between normal and persister states, and net growth/decline rates under antibiotic-present ("on") and antibiotic-absent ("off") conditions. Simple formulas have been derived to calculate critical and optimal values for the ton/toff ratio based on these parameters, which can be estimated from a minimal set of standard experimental data [62].
Q4: Besides pulse dosing, what other strategies can combat persister cells? Multiple strategies exist, often categorized as follows:
- Direct Killing: Using agents that target growth-independent structures, such as cell membranes (e.g., synthetic cation transporters, antimicrobial peptides) or causing uncontrolled protein degradation (e.g., ADEP4) [17].
- Indirect Killing: Preventing persister formation (e.g., using inhibitors of H₂S biogenesis or quorum sensing) or using synergists that increase membrane permeability to allow conventional antibiotics to enter persister cells [17] [63].
Troubleshooting Guides
Problem: Rapid Re-growth of Bacteria Between Treatment Pulses
Potential Causes and Solutions:
- Cause 1: Inadequate "Off" Duration
- Solution: The "off" period may be too long, allowing normal cells to proliferate excessively. Use mathematical modeling to shorten the
toffperiod while maintaining the optimalton/toffratio to ensure persisters have time to resuscitate without the population expanding [62].
- Solution: The "off" period may be too long, allowing normal cells to proliferate excessively. Use mathematical modeling to shorten the
- Cause 2: Incomplete Treatment During "On" Pulse
- Solution: Ensure the antibiotic concentration during the "on" pulse is consistently at the required bactericidal level. Verify stock concentrations and avoid improper dilution. In liquid cultures, ensure thorough mixing [64].
- Cause 3: Refuge for Persisters
- Solution: Biofilms can shield persisters. Consider combining pulse dosing with anti-biofilm agents or membrane-active compounds that disrupt the extracellular matrix and facilitate antibiotic penetration [17].
Problem: Failure to Reduce Bacterial Load Below Baseline After Multiple Pulses
Potential Causes and Solutions:
- Cause 1: Sub-optimal
ton/toffRatio- Solution: This is a primary failure mode. Re-estimate the model parameters (
a,b,Kn,Kp) for both "on" and "off" conditions from your experimental system. Re-calculate the optimal ratio; it may differ from initial theoretical predictions [62].
- Solution: This is a primary failure mode. Re-estimate the model parameters (
- Cause 2: Failure to Air Purge (in specific systems like water lines)
- Solution: In systems where this applies, an air purge before introducing the antibiotic prevents dilution. A purge after treatment helps remove residual chemicals and discourages regrowth. While more relevant to equipment disinfection, the principle of ensuring full agent contact and removing residual moisture can be informative [64].
Experimental Protocols
Protocol 1: In Vitro Evaluation of a Pulse Dosing Regimen
This protocol is adapted from methods used to validate systematic pulse dosing design [62].
1. Materials and Reagents
- Bacterial Strain: Escherichia coli WT or other pathogen of interest.
- Culture Media: Luria-Bertani (LB) broth and LB agar plates.
- Antibiotic Stock Solution: e.g., Ampicillin at 100 μg/mL.
- Washing Buffer: Phosphate Buffered Saline (PBS), sterile.
- Equipment: Shaker incubator, spectrophotometer, centrifuge, serial dilution equipment, colony counter.
2. Methodology
- Day 1: Culture Preparation
- Inoculate an overnight culture of bacteria in LB broth. Incubate at 37°C with shaking (e.g., 250 rpm) for a standardized period (e.g., 24 hours).
- Day 2: Initiate Pulse Dosing
- First "On" Pulse: Sub-culture the overnight culture into fresh LB broth. Expose the culture to the predetermined antibiotic concentration (e.g., 100 μg/mL Ampicillin) for the duration
ton. - Washing: After
ton, pellet the cells by centrifugation. Carefully remove the supernatant containing the antibiotic and wash the cell pellet with sterile PBS to remove residual antibiotic. - First "Off" Pulse: Re-suspend the washed cells in fresh, pre-warmed LB broth. Incubate for the duration
toffto allow persister cells to resuscitate. - Sampling: Sample the culture at the end of each "on" and "off" period for Colony Forming Unit (CFU) enumeration.
- First "On" Pulse: Sub-culture the overnight culture into fresh LB broth. Expose the culture to the predetermined antibiotic concentration (e.g., 100 μg/mL Ampicillin) for the duration
- CFU Enumeration
- Perform serial dilutions of the sampled culture in PBS.
- Spot diluted samples onto LB agar plates.
- Incubate plates at 37°C for 16-24 hours.
- Count colonies and calculate the CFU/mL for each time point.
- Subsequent Pulses
- Repeat the cycle of "on" pulse (with antibiotic, washing) and "off" pulse (fresh media) for the desired number of cycles, sampling at each key time point.
3. Data Analysis
- Plot the log(CFU/mL) over time to visualize the population decline.
- Compare the experimental results with the predictions from the mathematical model to validate the chosen
ton/toffratio.
Protocol 2: Parameter Estimation for the Two-State Persister Model
This protocol outlines how to gather data to fit the mathematical model used for designing pulse doses [62].
1. Experimental Phases
- Constant Antibiotic Exposure (Control): Expose a bacterial culture to a constant, high concentration of the antibiotic. Sample frequently over 24-48 hours for CFU enumeration. This data helps estimate the kill rates (
kn,kp) and switching rates (a,b) under the "on" condition. - Antibiotic-Free Growth (Control): Grow a bacterial culture in the absence of antibiotic, sampling frequently to monitor growth. This data helps estimate the natural growth rates (
μn,μp) and switching rates under the "off" condition.
2. Model Fitting
- Use the differential equations for the two-state model to fit the obtained CFU data from both control experiments.
dn/dt = Kn*n(t) + b*p(t)dp/dt = a*n(t) + Kp*p(t)
- Employ software like Mathematica or MATLAB for parameter estimation, deriving values for
{a, b, Kn, Kp}for both "on" and "off" conditions.
Data Presentation
Table 1: Example Anti-Persister Compounds and Their Mechanisms
This table summarizes strategies beyond pulse dosing, as identified in recent literature [17].
| Compound/Strategy | Class / Type | Proposed Mechanism of Action | Target Pathogens (Examples) |
|---|---|---|---|
| ADEP4 | Acyldepsipeptide | Activates ClpP protease, causing uncontrolled protein degradation | S. aureus, E. faecalis |
| Pyrazinamide | Prodrug | Active form (pyrazinoic acid) disrupts membrane energetics and targets PanD | Mycobacterium tuberculosis |
| SA-558 | Synthetic cation transporter | Disrupts bacterial membrane homeostasis, leading to autolysis | S. aureus |
| CSE Inhibitors | Enzyme inhibitor | Inhibits bacterial cystathionine γ-lyase (bCSE), reducing H₂S-mediated protection | S. aureus, P. aeruginosa |
| Brominated Furanones | Quorum Sensing Inhibitor | Inhibits quorum sensing, reducing persister formation | P. aeruginosa |
| MB6, CD437 | Membrane-active compounds | Disrupts membrane integrity, potentiating uptake of antibiotics like gentamicin | MRSA |
Table 2: Key Parameters for the Two-State Persister Model
This table defines the variables used in the mathematical model for designing intermittent regimens [62].
| Parameter | Description | Typical Units |
|---|---|---|
n(t) |
Number of normal, susceptible cells at time ( t ) | CFU/mL |
p(t) |
Number of persister cells at time ( t ) | CFU/mL |
a |
Switching rate from normal to persister state | h⁻¹ |
b |
Switching rate from persister to normal state | h⁻¹ |
μn, μp |
Growth rate of normal or persister cells, respectively | h⁻¹ |
kn, kp |
Kill rate of normal or persister cells by antibiotic, respectively | h⁻¹ |
Kn |
Net decline/growth rate of normal cells (( μn - kn - a )) | h⁻¹ |
Kp |
Net decline/growth rate of persister cells (( μp - kp - b )) | h⁻¹ |
Visualizations
Conceptual Workflow for Designing a Pulse Dosing Regimen
Relationship Between Substrate Availability, Dormancy, and Treatment Strategy
The Scientist's Toolkit: Research Reagent Solutions
Table 3: Essential Materials for Pulse Dosing and Persister Research
| Item | Function / Application | Example(s) / Notes |
|---|---|---|
| Two-State Mathematical Model | Used for simulating bacterial population dynamics and predicting optimal ton/toff ratios for pulse dosing. Implementable in MATLAB or Mathematica [62]. |
Equations (1) and (2) from [62]. |
| Membrane-Active Compounds | Used to disrupt the cell membrane of persisters, facilitating the entry of conventional antibiotics (synergy strategy) [17]. | Synthetic retinoids (CD437), MB6, bithionol. |
| Quorum Sensing Inhibitors | Used to investigate and inhibit cell-cell signaling that influences persister cell formation [17]. | Brominated furanones, benzamide-benzimidazole compounds. |
| Protease Activators | Used to force uncontrolled protein degradation in dormant cells, leading to death (direct killing strategy) [17]. | ADEP4 (activates ClpP protease). |
| H₂S Biogenesis Inhibitors / Scavengers | Used to reduce levels of hydrogen sulfide (H₂S), a molecule that protects bacteria under stress, thereby sensitizing persisters [17]. | CSE inhibitors, synthetic H₂S scavengers. |
| PBS Buffer | Used for washing bacterial cells to remove antibiotics between "on" and "off" pulses in in vitro protocols [62]. | Essential for clean transitions in pulse dosing cycles. |
Challenges in Translating In Vitro Findings to In Vivo Models
Frequently Asked Questions (FAQs)
FAQ 1: What is the core reason for the poor translatability of many in vitro persister studies to in vivo models? The primary reason is that most in vitro studies are conducted in the "test tube" under ideal, controlled laboratory conditions that do not simulate the complex environmental stresses found in a host [65]. In vitro conditions often fail to replicate key aspects of persistent infections, such as nutrient limitation, immune system pressures, and biofilm microenvironments, leading to an oversimplified understanding of persister formation mechanisms [65] [1].
FAQ 2: How does substrate availability specifically influence persister cell formation? Substrate availability is a major environmental trigger for phenotypic tolerance [65]. Limited nutrient availability causes bacteria to enter a slow-growing or non-growing dormant state, which directly reduces the efficacy of bactericidal antibiotics that target active cellular processes [1] [17] [3]. This growth arrest is a key mechanism underlying the persister phenotype.
FAQ 3: What are the main physiological differences between in vitro- and in vivo-generated persisters? In vivo, bacteria face a multitude of simultaneous stresses. For instance, in cystic fibrosis lungs, Pseudomonas aeruginosa encounters oxidative stress, nutrient starvation, and immune factors, leading to the selection of high-persister (hip) mutants with complex genetic adaptations (e.g., in mucA, mexT, lasR) [66]. These multifaceted stress responses are difficult to recapitulate in standard in vitro culture.
FAQ 4: Why are biofilms critical in the context of in vivo persistence and translation? Over 65% of infections are biofilm-associated [66]. Biofilms are a specific form of persistent infection where bacteria are encased in an extracellular polymeric substance (EPS), creating physical and chemical gradients that lead to heterogeneous microenvironments. This heterogeneity drives the formation of persister cells that are highly concentrated within biofilms, making them notoriously difficult to eradicate with conventional antibiotics [1] [66].
FAQ 5: What strategies can make in vitro models more predictive of in vivo outcomes? Strategies include:
- Inhibiting Persister Formation: Using compounds that target pathways like H2S biogenesis or quorum sensing to prevent entry into dormancy [17].
- Advanced Culturing: Employing bioreactors or microfluidics that mimic dynamic nutrient conditions and shear stresses [67].
- Incorporating Host Factors: Adding components like serum, immune cells, or using media based on host metabolomes to better simulate the in vivo environment.
Troubleshooting Guides
Problem 1: In Vitro Models Fail to Replicate In Vivo Persister Levels
Symptoms:
- Persister fraction in your animal model is significantly higher than in your in vitro culture.
- Different persister subpopulations are observed in vivo compared to in vitro.
| Possible Cause | Diagnostic Steps | Solution |
|---|---|---|
| Oversimplified nutrient environment [65] | Compare growth phase (log vs. stationary) and medium composition to host site (e.g., amino acid availability in urine). | Transition to more physiologically relevant media or use conditioned media from host cell cultures. |
| Lack of host-induced stress factors [1] [66] | Check for absence of immune components (e.g., neutrophils, reactive oxygen species) and other host defenses in your model. | Incorporate sub-inhibitory concentrations of host defense peptides or oxidative stress-inducing agents. |
| Missing biofilm-inducing conditions [66] | Assess culture method; planktonic cultures will not mimic biofilm-associated persistence. | Adopt biofilm culture models (e.g., flow cells, peg lids) to enrich for biofilm-derived persisters. |
Experimental Workflow for Model Validation:
Problem 2: Anti-Persister Compounds Effective In Vitro but Not In Vivo
Symptoms:
- Compound shows high efficacy against in vitro persisters but fails in an animal infection model.
- Compound toxicity is observed in vivo but not in cell-based assays.
| Possible Cause | Diagnostic Steps | Solution |
|---|---|---|
| Compound inability to penetrate biofilms [66] | Perform biofilm killing assays; measure compound concentration within biofilm matrix. | Use compounds that disrupt EPS (e.g., DNase, alginate lyase) in combination with antimicrobials. |
| Inactivation by host factors or serum binding [17] | Perform MIC/persister killing assays in presence of serum or host fluid. | Modify compound chemistry for improved stability or explore formulation in drug delivery vehicles. |
| Insufficient targeting of dormant cell physiology [17] | Verify compound's mechanism of action is independent of bacterial metabolism (e.g., membrane disruption). | Shift strategy to direct-killing agents (e.g., membrane-targeting compounds, protonophores). |
Experimental Protocol: Evaluating Compound Penetration and Efficacy
- Grow Biofilms: Form 24-48 hour mature biofilms of the target pathogen in a flow cell or on peg lids [66].
- Treat with Compound: Expose biofilms to the anti-persister compound at the desired concentration for a set time.
- Assess Viability:
- Viable Counts: Dislodge biofilm cells, homogenize, and plate on agar to count CFUs after compound exposure and removal.
- Viability Staining: Use live/dead staining (e.g., SYTO9/propidium iodide) and confocal microscopy to visualize killing within the biofilm structure.
- Measure Compound Penetration: Use fluorescently labeled derivatives of the compound or mass spectrometry to quantify its distribution and concentration within the biofilm layers.
Problem 3: Inability to Induce or Recover Persisters from Complex Models
Symptoms:
- Low or inconsistent yields of persister cells from complex co-culture or biofilm systems.
- Inability to reliably resuscitate persisters after treatment for downstream analysis.
| Possible Cause | Diagnostic Steps | Solution |
|---|---|---|
| Inefficient isolation from host debris/biofilm [3] | Check recovery rates by spiking known quantities of bacteria into the complex matrix and enumerating. | Optimize physical disaggregation (e.g., gentle sonication, vortexing with beads) and differential centrifugation protocols. |
| Overgrowth by non-persisters during recovery [1] | Monitor culture density closely during the recovery phase after antibiotic removal. | Use dilution techniques or microfluidics to separate and individually culture recovered cells, preventing overgrowth. |
| Cells entering a deeper VBNC state [3] | Perform viability PCR or use vital dyes that stain metabolically active cells versus those in VBNC state. | Supplement recovery media with specific resuscitation factors like pyruvate, glutamate, or catalase [3]. |
The Scientist's Toolkit: Key Reagents & Materials
Table: Essential Research Reagents for Studying Persisters and Substrate Availability
| Reagent/Material | Function/Brief Explanation | Key Considerations |
|---|---|---|
| Physiological Media (e.g., Artificial Sputum Medium, Urine-based Medium) | Mimics the nutrient and ion composition of specific host infection sites, providing more relevant substrate conditions [66]. | Composition can vary between donors; may require customization for specific research questions. |
| Microfluidic Chambers | Allows for precise control of dynamic nutrient gradients and fluid shear forces, mimicking host microenvironments and enabling single-cell analysis [68]. | Requires specialized equipment and expertise; can be low-throughput. |
| Membrane-Targeting Compounds (e.g., XF-70, SA-558, thymol conjugates) | Directly disrupts bacterial membranes, a growth-independent target, making them effective against dormant persisters [17]. | Potential for host cell cytotoxicity requires careful evaluation of selectivity index. |
| Reactivation Inducers (e.g., Pyruvate, Glutamate, Specific Sugars) | Provides a metabolic "jump-start" to help persister cells exit dormancy and resume growth, facilitating their detection and study [3]. | The specific effector required may depend on the bacterial species and the nature of the dormancy. |
| Quorum Sensing Inhibitors (e.g., brominated furanones, benzamide-benzimidazole compounds) | Blocks cell-to-cell communication, which can reduce persister formation in response to population density in pathogens like P. aeruginosa [17]. | Efficacy can be species- and strain-specific. |
| ClpP Activators (e.g., ADEP4) | Activates the ClpP protease, leading to uncontrolled protein degradation in a non-growth-dependent manner, effectively killing persisters [17]. | Resistance can develop rapidly if used as a monotherapy. |
Signaling Pathways in Persister Formation and Wake-Up
The formation and resuscitation of persister cells are governed by interconnected signaling networks that respond to environmental stresses like substrate limitation.
Evaluating Efficacy: Comparative Analysis of Anti-Persister Strategies
Substrate Control vs. Membrane-Targeting Agents and Prodrugs
Troubleshooting Guides & FAQs
Common Experimental Challenges and Solutions
FAQ: Why are my prodrugs failing to activate specifically in bacterial cultures despite using protease-sensitive linkers?
- Potential Cause: The chosen substrate sequence (linker) may not be efficiently recognized or cleaved by the bacterial proteases present in your experimental model. The specificity of bacterial proteases can vary significantly between species and even strains.
- Solution: Employ a directed evolution approach to engineer highly efficient and specific substrate sequences. Utilize a bacterial display platform, such as an E. coli system with an autotransporter (e.g., AIDA-I), to screen combinatorial peptide libraries. High-throughput sorting via Flow Cytometry (FACS) can isolate clones with superior cleavage efficiency based on the loss of a surface reporter tag [69].
- Prevention: Prior to full-scale prodrug synthesis, characterize the cleavage kinetics (kcat/KM) of candidate substrate sequences against the purified target protease to confirm efficiency and specificity [69].
FAQ: My membrane-targeting agent shows good in vitro efficacy but high cytotoxicity in host cells. How can I improve its selectivity?
- Potential Cause: The agent likely interacts non-specifically with both bacterial and mammalian cell membranes. The composition of bacterial membranes is rich in negatively charged phospholipids like phosphatidylglycerol (PG) and cardiolipin on their outer leaflets, while mammalian cells typically neutralize this charge on their outer surface [70].
- Solution: Redesign the agent to exploit these electrostatic differences. Incorporate cationic groups (e.g., in antimicrobial peptides or peptidomimetics) that are preferentially attracted to the net negative charge of bacterial membranes. Adjust the hydrophobicity of the agent to optimize insertion into the bacterial lipid bilayer without disrupting mammalian membranes [70].
- Prevention: Perform comparative assays using liposomes that mimic bacterial (rich in PG) versus mammalian (rich in phosphatidylcholine and cholesterol) membrane composition to pre-screen for selectivity during the development phase [70].
FAQ: How can I effectively target and eradicate dormant bacterial persisters that are tolerant to conventional antibiotics?
- Potential Cause: Persister cells have drastically reduced metabolic activity, making them insensitive to antibiotics that target active cellular processes like cell wall synthesis or protein production [1] [24].
- Solution: Consider one of two strategic approaches:
- "Re-awakening" Strategy: Use a compound to force persisters back into an active metabolic state, thereby re-sensitizing them to conventional antibiotics. For example, the host-directed adjuvant KL1 has been shown to increase intracellular bacterial metabolic activity and sensitize S. aureus and Salmonella persisters to rifampicin and moxifloxacin [71].
- Direct Killing with Non-Traditional Agents: Utilize agents that physically disrupt membranes or generate destructive radicals, independent of bacterial metabolism. Cationic polymers or reactive oxygen species (ROS)-generating nanomaterials (e.g., hydrogel microspheres with Fenton-like catalysts) can directly lyse cells or damage cellular components [72] [70].
FAQ: My antibiotic prodrug is successfully cleaved, but the active drug is immediately effluxed by the bacteria. What can I do?
- Potential Cause: The bacterium may be overexpressing efflux pumps that recognize the active drug moiety once it is released intracellularly.
- Solution: Implement a combination therapy. Co-administer the prodrug with an efflux pump inhibitor. Alternatively, design a double prodrug where the second moiety is an efflux pump inhibitor that is released concurrently with the primary active drug [73] [74].
FAQ: How can I validate that my substrate control strategy is effectively reducing persister formation in my infection model?
- Potential Cause & Solution: The link between substrate availability and persistence is complex. A key validated mechanism involves nutrient stress. Carbon source transitions or exhaustion can trigger the stringent response and toxin-antitoxin (TA) modules, leading to dormancy [12].
- Experimental Validation:
- Measure Persister Frequency: Use a standardized antibiotic kill curve assay (e.g., exposure to high concentrations of ciprofloxacin or ofloxacin) followed by plating for Colony Forming Units (CFUs) on rich media to quantify tolerant cells [24] [71].
- Manipulate Nutrient Availability: Conduct the kill assay under conditions of nutrient sufficiency versus starvation and compare persister frequencies [12].
- Monitor Metabolic Activity: Use a metabolic reporter strain (e.g., S. aureus JE2-lux, where bioluminescence correlates with ATP levels) to confirm that your substrate control strategy maintains bacterial metabolic activity and prevents the descent into dormancy [71].
Experimental Protocols
Protocol 1: High-Throughput Screening of Protease Substrates Using Bacterial Display
This protocol is adapted from methodologies used to engineer high-efficiency matriptase substrates and is applicable for discovering substrates for bacterial proteases [69].
1. Principle: A library of potential substrate sequences is displayed on the surface of E. coli between two reporter domains. Protease cleavage releases one reporter, allowing fluorescence-activated cell sorting (FACS) to isolate clones with high cleavage efficiency.
2. Materials:
- Library Vector: pPALU_CRS or similar, containing an autotransporter (e.g., AIDA-I), a surface expression reporter (e.g., Albumin-Binding Domain, ABD), and a cleavage reporter (e.g., HER2-binding affibody, ZHER2) [69].
- E. coli display strain (e.g., MC1061 or similar).
- Purified target protease.
- Detection Reagents: Fluorescently labeled albumin (e.g., HSA-Alexa647) to bind ABD, and biotinylated HER2/Streptavidin-R-Phycoerythrin (SAPE) to bind ZHER2.
- Flow cytometer with cell sorting capability.
3. Procedure:
- Step 1: Library Transformation. Clone your designed peptide substrate library into the display vector and transform into the E. coli display strain. Ensure library diversity exceeds 10^7 transformants [69].
- Step 2: Induction and Display. Induce expression of the display construct according to your system's specifications (e.g., with L-arabinose). Grow cells under conditions that promote surface localization.
- Step 3: Protease Cleavage. Harvest bacterial cells and incubate with your purified target protease. Include a no-protease control.
- Step 4: Fluorescent Labeling. Wash cells to stop the reaction. Label with HSA-Alexa647 and HER2-biotin/SAPE.
- Step 5: FACS Analysis and Sorting. Analyze cells by flow cytometry. The population of interest displays high HSA-Alexa647 signal (confirming surface expression) but low SAPE signal (indicating successful cleavage). Gate and sort this population for enrichment.
- Step 6: Iteration and Validation. Regrow the sorted population and repeat steps 2-5 for 2-3 rounds to enrich the best substrates. Finally, isolate single clones, sequence the substrate region, and characterize cleavage kinetics using soluble peptides.
The workflow for this protocol is as follows:
Protocol 2: Evaluating Anti-Persister Efficacy of Membrane-Targeting Agents
This protocol outlines methods to test the ability of membrane-targeting agents to kill dormant persister cells.
1. Principle: Persisters are generated by exposing a stationary-phase culture to a high concentration of a bactericidal antibiotic. The surviving, non-growing cells are then challenged with the membrane-targeting agent to assess direct killing efficacy [72] [24].
2. Materials:
- Test bacterium (e.g., Staphylococcus aureus or Escherichia coli).
- Bactericidal antibiotic (e.g., Ofloxacin or Ciprofloxacin).
- Test membrane-targeting agent (e.g., antimicrobial peptide, cationic polymer, or nanoagent).
- Phosphate Buffered Saline (PBS) or minimal medium.
- Equipment for CFU counting.
3. Procedure:
- Step 1: Generate Persister Cells.
- Grow the bacterial culture to stationary phase (e.g., 24-48 hours).
- Treat the culture with a high concentration of a bactericidal antibiotic (e.g., 10x MIC of ofloxacin) for 3-5 hours. This kills the majority of the population but enriches for tolerant persisters.
- Wash the cells 2-3 times with PBS or minimal medium to remove the antibiotic.
- Step 2: Treat with Membrane-Targeting Agent.
- Resuspend the persister-enriched pellet in a fresh medium.
- Divide the suspension into aliquots and treat with:
- A: No agent (Vehicle control)
- B: Your membrane-targeting agent at desired concentrations.
- C: A known anti-persister agent as a positive control (e.g., high-dose colistin if applicable).
- Incubate for a set time (e.g., 2-4 hours).
- Step 3: Quantify Viability.
- Serially dilute the samples and plate on rich agar plates.
- Incubate plates until colonies appear (this may take longer for resuscitating persisters).
- Count CFUs to determine the log-reduction in viable persisters compared to the vehicle control.
Table 1: Efficacy of Selected Anti-Persister Agents and Strategies
| Agent / Strategy | Target / Mechanism | Model System | Efficacy / Key Metric | Citation |
|---|---|---|---|---|
| Caff-AuNPs (Caffeine-functionalized Gold Nanoparticles) | Direct membrane disruption | Planktonic & biofilm-associated persisters (in vitro) | Potent bactericidal activity against Gram-positive and Gram-negative persisters | [72] |
| AuNC@ATP (ATP-functionalized Gold Nanoclusters) | Enhances membrane permeability, disrupts outer membrane proteins | Planktonic persisters (in vitro) | ~7-log reduction in persister counts at 2.2 μM | [72] |
| MPDA/FeOOH-GOx@CaP (ROS-generating hydrogel) | Fenton-like reaction generating hydroxyl radicals | Prosthetic joint infection model (S. aureus & S. epidermidis) | Effective eradication of persisters in an acidic infection microenvironment | [72] |
| PS+(triEG-alt-octyl) Polymer | Reactivates persisters via electron transport chain, then lyses cells | Biofilm-associated persisters (in vitro) | "Wake-and-kill" strategy; effective biofilm clearance | [72] |
| KL1 (Host-directed adjuvant) | Suppresses host ROS, increases bacterial metabolism | Intracellular S. aureus, Salmonella, M. tuberculosis (in macrophages & murine models) | Up to 10-fold enhanced killing when combined with rifampicin/moxifloxacin | [71] |
| Engineered Matriptase Substrate | Protease-activated prodrug linker | In vitro prodrug activation assay | >40-fold improvement in kcat/KM over previous substrates | [69] |
Table 2: Key Characteristics of Bacterial Persister Cells
| Characteristic | Description | Experimental Implication |
|---|---|---|
| Metabolic State | Non-growing or slow-growing (dormant), metabolically heterogeneous. | Standard antibiotics that target active processes (cell wall, protein synthesis) are ineffective [1] [24]. |
| Formation Trigger | Stress responses (e.g., nutrient starvation, antibiotic exposure, ROS). | Models should incorporate stress conditions (stationary phase, carbon source transition) to generate meaningful persister populations [24] [12]. |
| Tolerance vs. Resistance | Tolerance is a non-heritable, phenotypic survival. Post-stress population remains genetically susceptible. | Distinguish via Minimum Inhibitory Concentration (MIC) tests (unchanged) vs. kill curve assays (survival) [1] [24]. |
| Link to Biofilms | Biofilms are a major reservoir for persister cells, contributing to chronic infections and relapse. | Anti-persister strategies must be evaluated in biofilm models for clinical relevance [1] [72]. |
The molecular pathways controlling entry into and exit from the persister state are complex. The following diagram summarizes key mechanisms based on current research, highlighting points where substrate control and therapeutic intervention can be applied.
The Scientist's Toolkit: Key Research Reagent Solutions
Table 3: Essential Materials for Research on Persisters and Targeted Therapies
| Category | Reagent / Tool | Function in Research | Example & Notes |
|---|---|---|---|
| Bacterial Display | AIDA-I Autotransporter Vector (e.g., pPALU_CRS) | Display of peptide/protein libraries on the E. coli surface for high-throughput screening of protease substrates or binders [69]. | Contains surface expression (ABD) and cleavage (ZHER2) reporter domains [69]. |
| Persister Generation | Bactericidal Antibiotics (e.g., Ofloxacin, Ciprofloxacin) | Used in kill curves to eliminate growing cells and enrich for a population of antibiotic-tolerant persisters for downstream assays [24] [71]. | Typically used at 10-100x MIC for 3-5 hours on stationary phase cultures. |
| Metabolic Reporter | Bioluminescent Reporter Strains (e.g., JE2-lux) | Real-time, non-destructive probing of intracellular bacterial metabolic activity and energy status, useful for screening resuscitating compounds [71]. | Lux output correlates with cellular ATP, NAD(P)H, and FMNH2 levels [71]. |
| Membrane Targeting | Cationic Antimicrobial Peptides (AMPs) / Polymers | Investigate mechanisms of membrane disruption independent of bacterial metabolism; potential anti-persister agents [72] [70]. | Selectivity is based on attraction to negatively charged bacterial membranes. |
| Host-Directed Therapy | KL1-like Small Molecules | As adjuvants to modulate the host environment, reduce ROS/RNS, and re-sensitize intracellular persisters to conventional antibiotics [71]. | A research tool for validating the "re-awakening" strategy in intracellular infection models. |
| Prodrug Linkers | Engineered Peptide Substrates | Serve as cleavable linkers in antibody-prodrugs or targeted delivery systems, activated by specific bacterial proteases [69] [73]. | Optimized via directed evolution for high kcat/KM values and specificity [69]. |
Benchmarking Against Known Anti-Persister Compounds (e.g., Pyrazinamide)
Why is Pyrazinamide (PZA) the benchmark for anti-persister drug development? Pyrazinamide (PZA) is a cornerstone of tuberculosis therapy and serves as a critical benchmark in anti-persister research due to its unique, sterilizing activity against non-replicating, dormant bacterial persisters [75] [76]. Unlike conventional antibiotics that target growing cells, PZA is a prodrug that is converted to its active form, pyrazinoic acid (POA), which acts against a phenotypically resistant subpopulation of bacteria largely responsible for prolonged therapy and relapse [75] [1] [17]. Its inclusion in the first-line TB regimen shortens treatment duration from 9-12 months to 6 months, providing a clinical proof-of-concept for the critical importance of eradicating persister cells [75]. For researchers optimizing substrate availability to prevent persister formation, PZA represents a model for how a drug can target the metabolic downshift and environmental stress tolerance inherent to the persister state.
Frequently Asked Questions (FAQs)
Q1: What is the primary mechanism of action of Pyrazinamide against persister cells? PZA's action is complex and multifaceted, primarily targeting cellular energy and essential metabolic processes in non-growing cells [75]. The accepted model involves:
- Prodrug Conversion: PZA passively diffuses into the mycobacterial cell, where it is converted to its active form, pyrazinoic acid (POA), by the bacterial enzyme pyrazinamidase (PncA) [75] [76].
- Acid-Facilitated Accumulation: POA is effluxed from the cell. In an acidic environment (pH ~5.5), a proportion of POA becomes protonated (HPOA), which readily diffuses back into the cell. A deficient efflux mechanism in M. tuberculosis causes POA to accumulate intracellularly [75].
- Multiple Target Inhibition: Accumulated POA disrupts membrane energetics by collapsing the proton motive force (PMF) and causes cytoplasmic acidification [75]. Key enzymatic targets have been identified:
- PanD (Aspartate Decarboxylase): POA competitively inhibits PanD, an enzyme essential for coenzyme A biosynthesis. This binding triggers degradation of PanD, disrupting a vital metabolic pathway [17] [76].
- RpsA (Ribosomal Protein S1): POA can interfere with trans-translation, a stress-response system [75].
- Membrane Energy: POA disrupts the membrane potential and energy metabolism, particularly affecting non-replicating persisters with low metabolic activity [75] [17].
Q2: How do the mechanisms of persister formation relate to PZA's efficacy and the role of substrate availability? Persister formation is a bet-hedging strategy where a subpopulation of bacteria enters a slow- or non-growing state, often triggered by environmental stresses like nutrient limitation (substrate depletion), acidity, or antibiotic attack [1] [60] [77]. This dormancy makes them tolerant to most antibiotics. PZA is uniquely effective because its activity is enhanced under the same conditions that induce persistence, such as acidic pH and low metabolic energy [75]. Research shows that nutrient starvation leads to a drop in cellular energy (ATP) and activates stress responses like the stringent response, which can induce the persister state [77]. PZA exploits this by further disrupting the already compromised membrane energy of dormant cells [75]. Therefore, optimizing substrate availability to maintain bacterial populations in a replicating state can reduce the formation of persisters that PZA is designed to eliminate.
Q3: What are the primary genetic causes of resistance to Pyrazinamide? Resistance to PZA is most commonly caused by mutations that prevent the activation of the prodrug [75].
- pncA Mutations: Over 70-99% of PZA-resistant clinical isolates have loss-of-function mutations in the pncA gene, which encodes the pyrazinamidase enzyme. These mutations prevent the conversion of PZA to active POA [75] [78].
- panD Mutations: Mutations in the panD gene, encoding the target enzyme aspartate decarboxylase, are a significant mechanism of resistance. These mutations typically reduce the binding affinity or residence time of POA, allowing the bacterium to bypass the drug's inhibition [75] [76].
- rpsA Mutations: Mutations in the rpsA gene, involved in trans-translation, are associated with some cases of PZA resistance, though this is less common than pncA-mediated resistance [75].
Q4: What are the key considerations for designing in vitro assays to benchmark new compounds against PZA? Benchmarking requires replicating the specific conditions under which PZA is active [75].
- Culture pH: PZA is only active in vitro under acidic conditions (pH 5.0-5.8). Standard culture media at neutral pH (7.0) will not show PZA activity, leading to false negatives [75].
- Bacterial Growth Phase: PZA is more active against old, stationary-phase cultures where a higher proportion of persister cells exist, compared to young, actively growing cultures [75].
- Compound Exposure Time: Due to its slow, cumulative bactericidal effect, assays must allow for sufficient drug exposure time (several days) to accurately assess killing kinetics [76].
- Resistance Monitoring: Include control strains with known pncA or panD mutations to confirm that the activity of a new compound is not confounded by common PZA resistance mechanisms.
Experimental Protocols & Methodologies
Protocol for In Vitro Pyrazinamide Susceptibility Testing
This protocol is adapted for assessing the activity of PZA and benchmark compounds against M. tuberculosis persisters under acidic conditions [75].
Principle: To measure the minimum inhibitory concentration (MIC) and bactericidal activity of a test compound against M. tuberculosis in an acidic environment that mimics the intracellular niche of persisters.
Materials:
- Middlebrook 7H9 broth or 7H10 agar, adjusted to pH 5.5 with sterile HCl or phosphate buffer.
- Pyrazinamide stock solution (sterile).
- Test compound stock solutions (sterile).
- Mid-log phase M. tuberculosis culture (e.g., H37Rv strain).
- Sterile 0.9% saline with 0.05% Tween 80.
- Cell culture incubator set to 37°C with 5-10% CO₂.
Procedure:
- Inoculum Preparation: Dilute a mid-log phase M. tuberculosis culture to a concentration of approximately 10⁷ CFU/mL in saline-Tween.
- Drug Dilution: Prepare two-fold serial dilutions of PZA and the test compound in Middlebrook 7H9 broth at pH 5.5 in a 96-well plate or tissue culture tubes. Include a drug-free growth control and a sterile control.
- Inoculation and Incubation: Inoculate each well/tube with the prepared bacterial inoculum (final cell density ~10⁵-10⁶ CFU/mL). Seal the plate/tubes to prevent evaporation and incubate at 37°C for 7-14 days.
- MIC Determination: The MIC is defined as the lowest concentration of drug that inhibits >90% of visible growth compared to the drug-free control.
- Minimum Bactericidal Concentration (MBC) Determination: Subculture broth from clear wells (showing no growth) onto Middlebrook 7H10 agar at neutral pH. The MBC is the lowest drug concentration that results in a ≥99.9% reduction in the initial bacterial inoculum, indicating killing of persisters that can resume growth.
Protocol for Isolating and Characterizing Persister Cells
Principle: To isolate a highly enriched population of persister cells from a bacterial culture using high-dose antibiotic exposure, which kills regular cells but leaves dormant persisters intact [1] [77].
Materials:
- Mid-log and stationary-phase bacterial cultures.
- High-concentration antibiotic (e.g., Ciprofloxacin at 10x MIC or Amikacin).
- Phosphate-Buffered Saline (PBS), pH 7.4.
- Centrifuge and sterile tubes.
- Middlebrook 7H9 broth and agar plates.
Procedure:
- Antibiotic Selection: Expose a stationary-phase bacterial culture (where persister frequency is highest) to a high concentration of a bactericidal antibiotic (e.g., ciprofloxacin) for a defined period (e.g., 4-6 hours).
- Washing: Pellet the cells by centrifugation, discard the supernatant containing the antibiotic, and wash the pellet twice with sterile PBS to remove all traces of the antibiotic.
- Persister Enumeration: Resuspend the final pellet in fresh media. Perform serial dilutions and spot them on drug-free agar plates to determine the number of Colony Forming Units (CFUs) that survived the antibiotic exposure—these are the persister cells.
- Downstream Application: This enriched persister population can now be used in benchmarking assays against PZA and novel anti-persister compounds to assess their killing efficacy.
The Scientist's Toolkit: Key Reagents & Materials
Table 1: Essential Research Reagents for Anti-Persister Compound Benchmarking
| Reagent/Material | Function in Experiment | Key Considerations |
|---|---|---|
| Pyrazinamide (PZA) | Benchmark compound; positive control for anti-persister activity. | Ensure solubility and prepare fresh stock solutions. Verify activity at acidic pH. |
| Middlebrook Media (7H9/7H10) | Culture medium for growing M. tuberculosis. | Must be acidified to pH 5.5 for PZA activity testing. |
| Ciprofloxacin/Ami kacin | Tool for selecting and enriching persister populations from bacterial cultures. | Use at high concentrations (5-10x MIC) to kill all non-persister cells. |
| pncA & panD Mutant Strains | Control strains to validate the mechanism of action and distinguish between specific and non-specific killing. | Essential for confirming that a new compound's activity is not dependent on the PZA activation pathway. |
| ATP Assay Kit | To measure cellular energy levels in bacterial populations after drug treatment. | Useful for investigating if a new compound, like PZA, disrupts membrane energy. |
Data Presentation & Analysis
Table 2: Benchmarking a Novel Compound "X" Against Pyrazinamide
| Parameter | Pyrazinamide (Benchmark) | Novel Compound X | Interpretation & Implications |
|---|---|---|---|
| MIC at pH 7.0 | >1,600 µg/mL (Inactive) | 800 µg/mL | Compound X may have some activity against growing cells, unlike PZA. |
| MIC at pH 5.5 | 50 µg/mL | 25 µg/mL | Compound X shows superior potency under acidic, persister-inducing conditions. |
| MBC against Persisters | 100 µg/mL (99.9% killing) | 50 µg/mL (99.9% killing) | Compound X is more bactericidal against the dormant population. |
| Activity against pncA Mutant | No activity (Resistant) | Retains activity | Compound X does not require PZase for activation; different mechanism. |
| Cytotoxicity (CC₅₀) | >1,000 µg/mL (in mammalian cells) | 200 µg/mL | Compound X has a lower therapeutic window; potential toxicity concern. |
Signaling Pathways & Workflow Visualization
PZA Mechanism of Action and Resistance Pathways
PZA Mechanism and Resistance Pathways: This diagram illustrates the activation of pyrazinamide (PZA) into pyrazinoic acid (POA) by the PncA enzyme, its accumulation under acidic conditions, and its multi-target mechanism of action leading to bacterial cell death. Major resistance pathways via pncA and panD mutations are also shown.
Experimental Workflow for Anti-Persister Compound Screening
Anti-Persister Compound Screening Workflow: This diagram outlines the key steps for screening new compounds against PZA, starting with persister cell enrichment, followed by drug treatment under physiologically relevant acidic conditions, and culminating in multiple analytical endpoints to assess compound potency, efficacy, and mechanism.
Validation in Multi-Species Biofilms and Chronic Infection Models
Frequently Asked Questions (FAQs)
FAQ 1: What defines a multi-species biofilm in the context of a chronic infection, and why is its validation critical? A multi-species biofilm is an aggregate consisting of different microorganisms interwoven or in close proximity, allowing for potential interspecies interactions [79]. Validating their presence and structure is critical because traditional diagnostic methods that homogenize tissue samples lose all spatial organization information, which is key to understanding community-level antibiotic tolerance and pathogenicity [79]. It is this complex spatial organization, often disrupted by sample processing, that necessitates specific validation techniques.
FAQ 2: How can we accurately distinguish between mixed-species biofilms and mere co-location of mono-species aggregates in a clinical sample? Accurate distinction requires in situ visualization techniques that preserve the spatial structure of the sample. While culturing and bulk DNA sequencing can identify which species are present, they cannot show how they are organized [79]. Confocal Laser Scanning Microscopy (CLSM) combined with peptide nucleic acid fluorescence in situ hybridization (PNA-FISH) using species-specific fluorescent probes allows for direct visualization of different species within the same biofilm aggregate, confirming a true mixed-species biofilm rather than separate, co-located colonies [79].
FAQ 3: What are the major technical challenges in quantifying persister cells within multi-species biofilms, and how can they be overcome? A major challenge is that traditional persister isolation methods rely on prolonged antibiotic exposure, which can itself induce a stress response and alter the persister population, creating a bias [80]. Furthermore, it is difficult to differentiate between persister types (e.g., Type I vs. Type II) from a complex biofilm. A novel protocol that uses a combination of alkaline and enzymatic lysis (e.g., lysozyme) to rapidly kill normally growing cells, leaving persisters intact, can overcome this. This method is faster, less inductive, and can be adapted to selectively isolate different persister types from both exponential and stationary phase cultures [80].
FAQ 4: How does optimizing substrate availability influence persister cell formation in biofilms? Substrate availability directly impacts bacterial metabolic state. Nutrient scarcity, such as carbon or amino acid starvation, is a key environmental trigger that pushes a subpopulation of cells into a dormant, persistent state [66] [26]. These slow-growing or non-growing persisters are highly tolerant to antibiotics that target active cellular processes. Therefore, optimizing substrate availability to prevent nutrient deprivation can theoretically reduce the formation of metabolically dormant persister cells, making the biofilm more susceptible to conventional antibiotics [66].
Troubleshooting Guides
Problem 1: Inconsistent or Low Yield of Persister Cells from Biofilm Samples
Potential Cause: The method for isolating persisters is inducing stress, thereby altering the very subpopulation you wish to study. Traditional antibiotic-based methods require long incubation times (≥3 hours), which can stably activate stress responses [80].
Solution: Implement a rapid, antibiotic-free lysis protocol.
- Harvest the biofilm: Gently wash the biofilm to remove non-adherent planktonic cells.
- Apply lysis solution: Add a commercial osmotic lysis solution (e.g., from a miniprep kit) to the biofilm pellet. Vortex and incubate at room temperature for 10 minutes.
- Enzymatic digestion: Add a lysozyme solution (e.g., 45 mg in 1 mL TE buffer) to degrade the cell wall. Incubate at 37°C with shaking for 15 minutes.
- Recover persisters: Centrifuge the mixture, wash the pellet to remove the lysis mix, and resuspend in fresh medium. The surviving cells are the persister population [80]. Validation: Use Time-Lapse Microscopy to confirm that the isolated cells are in a dormant state but can resume growth after the stress is removed [80].
Problem 2: Failure to Visually Confirm Mixed-Species Biofilms in Infected Tissue
Potential Cause: Reliance on bulk analysis methods like homogenization and sequencing, which destroy the spatial architecture of the sample [79].
Solution: Adopt an in situ visualization workflow that preserves spatial information.
- Tissue Fixation: Immediately fix tissue biopsies in formalin and embed them in paraffin (FFPE).
- Sectioning: Cut thin sections (e.g., 5 µm) of the FFPE tissue block.
- Fluorescent In Situ Hybridization (FISH): Hybridize the tissue sections with species-specific PNA probes, each tagged with a different fluorescent dye.
- Imaging and Analysis: Image the stained sections using Confocal Laser Scanning Microscopy (CLSM). The presence of multiple colors within a single, cohesive aggregate confirms a mixed-species biofilm [79]. Note: This method is considered the gold standard for validating the organization of multi-species biofilms in chronic infections [79].
Problem 3: High Background in PNA-FISH Staining of Clinical Specimens
Potential Cause: Non-specific binding of probes to host tissue or debris, or autofluorescence of the sample.
Solution:
- Optimize Probe Stringency: Increase the hybridization temperature or formamide concentration in the buffer to enhance specificity.
- Include Controls: Always use a nonsense probe as a negative control and a universal bacterial probe (e.g., targeting 16S rRNA) as a positive control.
- DNase Treatment: Treat samples with DNase to confirm that the signal is from RNA and not from trapped DNA.
- Image Processing: Use spectral unmixing tools in your microscopy software to separate specific fluorescence signals from background autofluorescence.
Table 1: Persister Cell Types and Characteristics
| Persister Type | Formation Trigger | Metabolic/Growth State | Key Characteristics |
|---|---|---|---|
| Type I [1] [4] | Entry into stationary phase; environmental stress [1]. | Non-growing cells [1]. | Preexist in population; generated in response to environmental triggers [4]. |
| Type II [1] [4] | Stochastic, spontaneous process during exponential growth [1]. | Slow-growing cells [1]. | Generated continuously; independent of external triggers [4]. |
| Type III (Specialized) [4] | Specific antibiotic pressure or stress signals [4]. | Not necessarily slow-growing prior to antibiotic exposure [4]. | Exhibit persistence mechanisms tailored to particular antibiotics [4]. |
Table 2: Comparison of Methods for Analyzing Multi-Species Biofilms
| Method | Principle | Key Advantage | Key Limitation |
|---|---|---|---|
| Culture-Based [79] | Growth on selective agar media. | Low cost; identifies viable pathogens. | Drastically underestimates diversity (e.g., 10% vs 64% with molecular methods); loses spatial data [79]. |
| Bulk DNA Sequencing [79] | DNA extraction & sequencing from homogenized samples. | Provides comprehensive species list and relative abundance. | Complete loss of spatial organization and structural context [79]. |
| PNA-FISH/CLSM [79] | Fluorescent probes target species-specific rRNA in situ. | Visual confirmation of mixed-species aggregates and spatial organization [79]. | Small imaging area may miss sparse aggregates; requires a priori knowledge for probes [79]. |
Detailed Experimental Protocols
Protocol 1: Rapid Isolation of Persister Cells from Biofilms Using a Lytic Method
This protocol bypasses the use of antibiotics, allowing for faster and less biased isolation of persister cells [80].
Key Research Reagent Solutions:
- Lysis Solution: Commercially available alkaline lysis solution (e.g., from a plasmid miniprep kit).
- Enzymatic Lysis Solution: Lysozyme from chicken egg white, dissolved in TE buffer at 45 mg/mL.
- TE Buffer: 10 mM Tris-Cl, 1 mM EDTA, pH 8.0.
Methodology:
- Biofilm Harvesting: Grow biofilms in a suitable medium. Gently wash the biofilm (e.g., in a flask or on coupons) with sterile saline to remove loosely attached cells. Physically scrape the biofilm into a suspension using a sterile cell scraper and suspend in a known volume of saline.
- Primary Lysis: Transfer 1 mL of the biofilm suspension to a 15 mL tube. Add 200 µL of the alkaline lysis solution. Vortex vigorously for 10 seconds and incubate at room temperature for 10 minutes.
- Secondary Enzymatic Lysis: Add 200 µL of the freshly prepared lysozyme solution to the mixture. Invert the tube gently to mix. Incubate at 37°C with shaking at 200 rpm for 15 minutes.
- Persister Recovery: Centrifuge the lysate at high speed (e.g., 10,000 x g for 5 min) to pellet the surviving persister cells. Carefully discard the supernatant and wash the pellet twice with sterile buffer or medium to remove all traces of the lysis mix. Resuspend the final pellet in a suitable medium for downstream applications (e.g., culturing, molecular analysis).
- Enumeration: Serially dilute the resuspended persister cells and plate on non-selective agar plates to determine the colony-forming units (cfu) and calculate the persister frequency [80].
Differentiating Type I and Type II Persisters: To selectively isolate only Type I persisters, increase the volume of both the alkaline and enzymatic lysis solutions to 500 µL each. The harsher conditions will kill both normally growing cells and the more vulnerable Type II persisters [80].
Protocol 2: In Situ Visualization of Mixed-Species Biofilms via PNA-FISH
This protocol is designed for validating the presence and spatial organization of multiple bacterial species within a biofilm, such as one formed on an implant or in infected tissue [79].
Key Research Reagent Solutions:
- PNA Probes: Commercially synthesized species-specific PNA probes with different fluorescent labels (e.g., FITC for S. aureus, Cy3 for P. aeruginosa).
- Fixative: 10% Neutral Buffered Formalin.
- Hybridization Buffer: According to the PNA probe manufacturer's instructions.
- Mounting Medium: Antifade mounting medium containing DAPI to stain all DNA (highlighting host cell nuclei and bacterial cells).
Methodology:
- Sample Fixation and Preparation:
- For tissue: Immediately immerse the biopsy in 10% formalin for 24 hours, then process and embed in paraffin (FFPE). Cut 4-5 µm thick sections and mount on glass slides.
- For biofilms on devices: Fix the entire device or a representative section in formalin. If possible, embed and section, or perform whole-mount staining.
- Deparaffinization and Permeabilization: For FFPE sections, deparaffinize with xylene and rehydrate through a graded ethanol series. Treat the samples with a permeabilization agent (e.g., proteinase K) to facilitate probe entry.
- Hybridization: Apply the hybridization buffer containing the mixture of fluorescently labeled PNA probes to the sample. Place the sample in a humidified chamber and incubate at the optimal temperature (e.g., 55°C) for 90 minutes.
- Washing: Wash the slides in a pre-warmed wash buffer to remove unbound probes and reduce background.
- Mounting and Imaging: Apply a coverslip using an antifade mounting medium containing DAPI. Visualize the stained samples using a Confocal Laser Scanning Microscope. Use sequential scanning settings to avoid bleed-through between channels [79].
Interpretation of Results: Co-localization of different colored fluorescent signals (e.g., red and green merging to yellow) within the same three-dimensional aggregate structure provides visual confirmation of a mixed-species biofilm.
Signaling Pathways and Experimental Workflows
Diagram 1: Biofilm Development and Persister Formation
Diagram 2: Workflow for Multi-Species Biofilm Validation
The Scientist's Toolkit: Research Reagent Solutions
Table 3: Essential Reagents for Biofilm and Persister Research
| Item | Function/Brief Explanation | Example Application |
|---|---|---|
| Lysozyme | An enzyme that degrades the peptidoglycan layer of bacterial cell walls. | Used in the rapid lytic protocol to kill non-persister cells by lysing their cell walls [80]. |
| PNA (Peptide Nucleic Acid) Probes | Synthetic DNA mimics with a peptide backbone that bind tightly and specifically to rRNA sequences. | Used in FISH (PNA-FISH) for high-specificity in situ identification of bacterial species within a biofilm sample without bulk processing [79]. |
| Alkaline Lysis Solution | A solution containing SDS and NaOH that disrupts cell membranes and denatures proteins. | The primary agent in the antibiotic-free persister isolation protocol to rapidly kill vulnerable cells [80]. |
| Extracellular DNA (eDNA) | A key component of the biofilm matrix, contributing to structure and cation-mediated cross-linking. | Target for disruption using DNase to weaken the biofilm matrix and enhance antibiotic penetration [81] [26]. |
| Diguanylate Cyclase (DGC) Inhibitors | Enzymes that synthesize the secondary messenger c-di-GMP, a key promoter of the biofilm lifestyle. | Potential therapeutic target; inhibiting DGCs can reduce biofilm formation and stability [26]. |
| Quorum Sensing Inhibitors | Molecules that interfere with bacterial cell-to-cell communication systems (Quorum Sensing). | Used in research to prevent coordinated biofilm behaviors and maturation without directly killing bacteria [81]. |
Frequently Asked Questions (FAQs)
Q1: Why do I observe high variability in persister resuscitation times in my experiments? The resuscitation of bacterial persisters is not a stochastic (random) process but occurs exponentially [82]. The rate of resuscitation is initially slow but accelerates over time, governed by factors such as the antibiotic concentration during the previous treatment phase and the cells' efflux capacity during resuscitation [82]. Variability is therefore expected and is influenced by these treatment parameters and the resulting cellular damage.
Q2: What does it mean if I observe unusual cell morphologies, like filamentation or structural defects, after antibiotic treatment? The appearance of damaged progeny, such as cells with triangular structural defects or filamentation, is a common phenomenon known as persister partitioning [82] [83]. After resuscitating from antibiotic-induced damage, a single persister cell can divide unevenly, producing one healthy daughter cell and one defective or non-viable one [82]. The specific type of damage is often determined by the antibiotic's mechanism of action [83].
Q3: My persister counts are low and unpredictable. How can I consistently generate persisters for my assays? Persister formation is linked to stress responses and dormancy. You can enhance persister formation by:
- Using stationary-phase cultures or biofilms, where persister fractions can be up to 1,000-fold higher than in exponential phase [1] [11].
- Applying external stresses that trigger the stringent response. For example, using a strain with a temperature-sensitive valyl-tRNA synthetase allele (
valSts) at a semi-permissive temperature can induce amino acid starvation and raise (p)ppGpp levels, boosting persister formation stochastically [84].
Q4: How do microbial communities affect persister resuscitation, which I might observe in co-culture experiments? In a polymicrobial environment, ecological interactions significantly impact pathogen clearance and resuscitation [83]. Competitive interactions from other species can suppress the resuscitation of a pathogen's persister subpopulation, especially when the persister pool is small and susceptible to stochastic extinction [83]. The presence of protective species, however, could have the opposite effect.
Troubleshooting Guides
Background: Resuscitation is a transient, single-cell event that is difficult to capture. The classical model suggests persisters resuscitate stochastically, but recent evidence shows the process is exponential and dependent on previous treatment conditions [82].
Investigation and Resolution:
- Step 1: Verify Antibiotic Removal. Ensure the antibiotic is thoroughly washed out after treatment, as residual drug will delay or prevent resuscitation.
- Step 2: Quantify Treatment Intensity. Note that the key parameters controlling resuscitation map to the antibiotic concentration during treatment and efflux capacity during resuscitation [82]. Reproducibility requires tight control over these factors.
- Step 3: Implement Appropriate Imaging. Use time-lapse microscopy to track individual cells after antibiotic removal. Image at intervals of 30 minutes or less to accurately capture the first division event [82].
- Step 4: Model Your Data Dynamically. Fit your resuscitation time data to both stochastic ((Pt = e^{-kt})) and exponential ((Pt = e^{α/β(e^{βt} - 1)})) models. The exponential model is often a better fit for ampicillin-treated E. coli and Salmonella enterica persisters [82].
Problem: High Relapse Rates in Infection Models After Antibiotic Therapy
Background: Relapse occurs when a pathogen population is not fully eradicated, often due to the presence of antibiotic-tolerant persister cells that resuscitate after treatment ends [1].
Investigation and Resolution:
- Step 1: Assess Persister Burden Pre- and Post-Treatment. Use standard persister assays (e.g., antibiotic exposure followed by plating on drug-free media) to quantify the size of the surviving persister population before and after your treatment regimen [1] [11].
- Step 2: Check for Partitioning-Derived Damage. Be aware that even after resuscitation, the persister-derived population may not be healthy. Look for signs of persister partitioning, where damaged persisters produce a mixed population of healthy and defective daughter cells, which can exhibit a reduced growth rate overall [82] [83].
- Step 3: Consider the Community Context. If using a complex infection model (e.g., polymicrobial), remember that microbe-microbe interactions can either inhibit or promote the resuscitation of your target pathogen's persisters, thereby influencing relapse [83]. Use controlled co-culture experiments to deconvolute these effects.
- Step 4: Evaluate Anti-Persister Compounds. Consider adjunct therapies that target persister cells. Research is ongoing into compounds that disrupt persister mechanisms (e.g., TA systems, (p)ppGpp synthesis) or kill dormant cells [1].
Key Experimental Data
Summary of key parameters from single-cell tracking of bacterial persister resuscitation after ampicillin treatment [82].
| Parameter | Description | Experimental Value |
|---|---|---|
| Resuscitation Time ((t_R)) | Time to first cell division after antibiotic removal | Variable; follows exponential dynamics |
| Doubling Time ((δ)) | Growth rate of persister progeny after resuscitation | Consistent; uncorrelated with (t_R) |
| Resuscitation Rate ((k)) | Rate constant for transition from dormant to dividing state | Increases exponentially with time |
| Key Model Parameters | Empirical parameters from exponential model ((P_t = e^{α/β(e^{βt} - 1)})) | α and β map to antibiotic concentration and efflux capacity |
Table 2: Research Reagent Solutions
Essential materials and tools for studying persister formation and resuscitation. [82] [1] [11]
| Research Reagent | Function / Application |
|---|---|
| Time-lapse Microscopy System | Tracks resuscitation dynamics and cell division of individual persister cells. |
| Fluorescent Reporter Genes (e.g., GFP, mCherry) | Labels cells for automated image processing and to report on promoter activity or stress responses. |
| RpoS-mCherry Fusion | Serves as a fluorescent reporter for (p)ppGpp levels and the stringent response. |
| QUEEN-7µ | Genetically encoded sensor for monitoring intracellular ATP concentrations in single cells. |
TA Module Reporters (e.g., relB promoter-YFP) |
Reports on the activation of specific Toxin-Antitoxin systems linked to persistence. |
Strains with Inducible Persistence (e.g., valSts mutant) |
Provides a controlled system to induce high levels of persister formation via amino acid starvation. |
Detailed Experimental Protocols
This protocol is adapted from methods used to demonstrate exponential resuscitation dynamics in E. coli [82].
Principle: To monitor and quantify the transition of individual, antibiotic-tolerant persister cells from a dormant state to active growth after the removal of stress.
Workflow:
Procedure:
- Culture Preparation and Antibiotic Treatment:
- Grow bacterial culture to the desired phase (e.g., stationary phase for high persister numbers).
- Treat the culture with a lethal concentration of antibiotic (e.g., ampicillin) for a defined period (e.g., 3 hours) to kill the majority of the population.
- Wash and Concentrate:
- Centrifuge the antibiotic-treated culture and carefully remove the supernatant.
- Wash the cell pellet 2-3 times with fresh, pre-warmed, antibiotic-free medium to thoroughly remove the antibiotic.
- Re-suspend the cells in a small volume of fresh medium.
- Microscopy Setup:
- Embed the washed cell suspension in a thin layer of low-melt agarose on a microscopy slide to immobilize cells for tracking.
- Ensure the slide is maintained at the appropriate temperature (e.g., 37°C) in an environmental control chamber.
- Time-Lapse Imaging:
- Program the microscope to capture images of multiple fields of view at regular intervals (e.g., every 30 minutes) over 12-24 hours.
- Use phase contrast and/or fluorescence (if using reporter strains) to monitor cell growth and division.
- Data Analysis:
- Use image analysis software to track lineages of individual cells.
- For each persister, record the resuscitation time ((tR))
- Calculate the doubling time ((δ)) of the progeny from the microcolony growth.
- Plot the fraction of persisters yet to resuscitate ((Pt)) over time and fit the data to exponential and stochastic models.
Protocol 2: Standard Persister Assay and CFU Enumeration
A core method for isolating and quantifying persister cells from a population [11].
Principle: To determine the fraction of a bacterial population that survives a high concentration of a bactericidal antibiotic without genetic resistance.
Procedure:
- Sample Preparation: Grow cultures to the desired optical density (OD). It is critical to note that older inocula (stationary phase) have more persister cells [11].
- Antibiotic Exposure: Add a lethal dose of antibiotic to the culture. Common practice is to use 10-100x the MIC. Include a control culture without antibiotic.
- Incubation: Incubate the culture under normal growth conditions for a defined period (e.g., 3-5 hours).
- Viable Count (Plating):
- At specific time points, take aliquots from the antibiotic-treated and control cultures.
- Serially dilute the samples in buffer or medium to neutralize the antibiotic.
- Spot or spread the dilutions onto antibiotic-free agar plates.
- Calculation:
- After incubation (typically 24-48 hours), count the colony-forming units (CFUs).
- The persister fraction is calculated as (CFU/mL after antibiotic treatment) / (CFU/mL before antibiotic treatment).
Signaling Pathways and Mechanisms
The following diagram integrates key mechanisms influencing persister resuscitation and the subsequent phenomenon of damage partitioning, as revealed by recent studies [82] [83] [1].
Cost-Benefit Analysis for Pre-Clinical Therapeutic Development
Frequently Asked Questions (FAQs)
Q1: What are bacterial persisters and why are they a significant problem in pre-clinical therapeutic development? Bacterial persisters are a subpopulation of genetically drug-susceptible bacteria that are in a transient, non-growing, or slow-growing state. This dormancy allows them to survive exposure to high concentrations of antibiotics and other environmental stresses. After the stress is removed, they can regrow, leading to relapse of infections. Persisters are a primary cause of chronic and recurrent infections, treatment failures, and are major contributors to the difficulty in eradicating biofilm-associated infections. Their presence significantly complicates pre-clinical development as they are not killed by conventional antibiotics, which typically target active cellular processes, necessitating specialized assays and therapeutic strategies [1].
Q2: How does optimizing substrate availability help prevent persister formation? The formation and survival of persister cells are highly dependent on environmental conditions, with nutrient availability being a key factor. Substrate limitation (e.g., carbon, nitrogen, or oxygen starvation) is a known trigger that pushes a larger fraction of the bacterial population into the persistent state. Therefore, ensuring optimal substrate availability during in vitro experiments and in model systems can help minimize the induction of persistence. This is crucial for obtaining reproducible results in pre-clinical studies, as high and variable persister levels can lead to inconsistent efficacy data for new drug candidates. Optimizing growth conditions to prevent starvation-induced persistence is a fundamental step in streamlining the assessment of a therapy's true potential [14] [1].
Q3: What are the key parameters for a cost-benefit analysis when deciding to outsource pre-clinical work to a CRO? A cost-benefit analysis for outsourcing pre-clinical work should extend beyond simple per-study cost comparisons. Key parameters to consider include:
- Internal Resource Allocation: The cost of diverting your scientific team from core R&D activities to manage complex pre-clinical studies.
- Specialized Expertise and Technology Access: The value of accessing the CRO's specialized knowledge, particularly in areas like toxicology testing or complex models (e.g., PDX, organoids), and their advanced technological platforms without major capital investment [85] [86].
- Timeline Acceleration: The financial benefit of faster study initiation and completion due to the CRO's established protocols and capacity, which can ultimately lead to an earlier IND submission [87].
- Risk Mitigation: The value of the CRO's experience in navigating regulatory requirements, which reduces the risk of costly study repeats or regulatory delays [85] [86].
Q4: What are the emerging trends in pre-clinical models that can improve the predictive power of my research on persistent infections? The field is rapidly moving towards more human-relevant models that can better mimic the in vivo conditions where persisters thrive. Two key trends are:
- Patient-Derived Organoids (PDOs): These 3D micro-tissues derived from patient cells closely mimic the human tissue and tumor microenvironments. They provide better translational relevance for studying bacterial persistence in host-like conditions and for predicting drug responses [86].
- Advanced Translational Models: There is an 11-fold increase in research using organoids and organ-on-a-chip technologies. These models aim to replicate human organ functions more accurately, improving the predictive power of pre-clinical testing for identifying compounds that can eradicate persistent infections [88]. Adopting these models, though sometimes more costly initially, can provide a better return on investment by reducing late-stage failures attributed to inaccurate pre-clinical data [88].
Troubleshooting Guides
Guide 1: Addressing High Variability in Persister Cell Counts in Biofilm Assays
Problem: Inconsistent numbers of persister cells recovered from replicate biofilm treatments with antibiotics.
Solution:
- Step 1: Standardize Growth Conditions. Ensure complete consistency in inoculum age, medium composition, and substrate concentrations (e.g., carbon source). Even slight variations in nutrient availability can significantly alter the baseline level of persister cells [14] [1].
- Step 2: Control Biofilm Maturity. Precisely define and control the biofilm growth time and environmental conditions (temperature, shaking). The architecture and persister distribution within a biofilm are highly dependent on its developmental stage and the local microenvironment [14].
- Step 3: Validate Antibiotic Killing Kinetics. Perform a time-kill curve assay to confirm the antibiotic is fully effective against planktonic cells and to establish the minimum treatment time required to eliminate all non-persisters before counting survivors.
- Step 4: Optimize Homogenization. For biofilm dispersal, use a consistent and validated method (e.g., vortexing with beads, sonication) and confirm its efficiency by quantifying the number of cells released. Incomplete dispersal will lead to inaccurate colony-forming unit (CFU) counts.
Guide 2: Troubleshooting a Failed Cost-Benefit Analysis for a New Anti-Persister Compound
Problem: The initial cost-benefit analysis for developing a novel anti-persister compound is unfavorable, showing high costs and uncertain returns.
Solution:
- Step 1: Re-evaluate the Target Product Profile (TPP). Refine the TPP to focus on a specific, high-unmet-need indication where persisters are a recognized problem (e.g., cystic fibrosis, chronic urinary tract infections, biofilm-related device infections). This can justify a higher price point and improve the market potential [89] [90].
- Step 2: Explore Partnership Models. Consider mitigating costs and risks through partnerships. This includes:
- CRO Alliances: Partner with a CRO that offers integrated services from pre-clinical to commercial strategy. This can provide cost efficiencies and expert guidance [87].
- Strategic Collaborations: Form research alliances with academic institutes or larger biopharma companies to share the R&D burden and access complementary resources [90].
- Step 3: Incorporate Real-World Evidence (RWE). Plan for the early collection of RWE to demonstrate the compound's value in treating persistent infections, which is increasingly important for market access and reimbursement, especially for novel therapies [87] [90].
- Step 4: Leverage AI and Computational Tools. Integrate AI-driven approaches in the early discovery phase to reduce pre-clinical timelines and costs. AI can be used for compound screening and designing molecules with better penetration into persister cells, improving the probability of success [88] [7].
Data Presentation: Pre-Clinical CRO Market and Service Costs
The global pre-clinical CRO market is experiencing significant growth, driven by the increasing complexity and cost of internal drug development. The following tables summarize key market and service segment data relevant for a cost-benefit analysis.
Table 1: Global Preclinical CRO Market Forecast (2024-2034)
| Metric | Value in 2024 | Projected Value in 2033/2034 | CAGR | Key Drivers |
|---|---|---|---|---|
| Market Size | USD 6.4 billion [85] | USD 11.3 billion (2033) [85] | 6.5% [85] | Rising R&D costs, chronic disease burden, need for specialized expertise [85] [86] |
| USD 6.25 billion [86] | USD 14.34 billion (2034) [86] | 8.73% [86] | ||
| Regional Share (2024) | North America: 47.5% [85] | - | - | High R&D investment, regulatory complexity, presence of major players [85] |
| Fastest Growing Region | Asia Pacific [85] [86] | - | 11.4% (India, 2024-2033) [85] | Cost-effective R&D, regulatory support, expanding biopharma sector [85] [86] |
Table 2: Preclinical CRO Market Segmentation and Key Service Areas
| Segment | Category | Market Share / Note | Relevance to Persister Research |
|---|---|---|---|
| By Service | Toxicology Testing | Largest segment (51.6% in 2024) [85] | Essential for safety profiling of new anti-persister compounds. |
| Bioanalysis and DMPK Studies | Fastest growing segment [86] | Critical for understanding drug metabolism & pharmacokinetics of persister-active drugs. | |
| By End Use | Biopharmaceutical Companies | Largest end-user (81% in 2024) [85] | Primary clientele for CROs developing anti-persister therapies. |
| By Model Type | Patient-Derived Organoid (PDO) | Largest share in model type segment [86] | Emerging, human-relevant model for studying persistent infections. |
Experimental Protocols
Protocol 1: Agent-Based Modeling of Substrate Availability and Persister Dynamics
This protocol outlines the development of a computational model to simulate how substrate availability influences persister formation and the efficacy of periodic antibiotic treatment, as described in [14].
Methodology:
- Model Framework: Implement an agent-based model (ABM) in a platform like NetLogo. Each bacterial cell is represented as an independent "agent" [14].
- Biofilm Growth Initialization:
- Start the simulation by randomly placing a small number of susceptible bacterial cells on a surface.
- Program cell growth to follow Monod kinetics, where the growth rate of a cell is dependent on the local concentration of a growth-limiting substrate (CS):
dmi/dt = mi * μmax * (CS / (CS + KS)), wheremiis cell mass,μmaxis maximal growth rate, andKSis the half-saturation constant [14].
- Incorporating Persister Dynamics:
- Define rules for phenotypic switching between susceptible and persister states. The switching rates should be dependent on both local substrate concentration and the presence of antibiotics to mimic realistic triggers [14].
- Simulating Antibiotic Treatment:
- Introduce an antibiotic into the simulated environment, allowing it to diffuse from the bulk fluid.
- Program susceptible cells to be killed at a high rate and persister cells at a much slower rate upon antibiotic exposure.
- Testing Periodic Dosing:
- Run simulations with various periodic dosing regimens (e.g., different on/off durations of antibiotic application).
- The output to analyze is the total antibiotic dose required to eradicate the biofilm. The goal is to identify a regimen that minimizes this dose by allowing persisters to "wake up" during off-periods, making them susceptible again [14].
Protocol 2: High-Throughput Screening for Anti-Persister Compounds Using a Rational Chemoinformatic Approach
This protocol details a rational method for discovering new persister control agents, moving away from conventional growth-inhibition screens [7].
Methodology:
- Compound Library Selection: Begin with a focused library of compounds with known antimicrobial activity (e.g., the Asinex SL#013 Gram-Negative Antibacterial Library) [7].
- Rational Lead Identification via Clustering:
- Define Key Molecular Descriptors: Extract physicochemical properties from known persister-killing antibiotics (e.g., eravacycline, minocycline). Key descriptors include
LogP(octanol-water partition coefficient), halogen content, number of hydroxyl groups, and molecular globularity [7]. - Perform k-means Clustering: Use a chemoinformatics platform (e.g., ChemMine) to cluster the compound library based on the selected descriptors. Focus subsequent testing on the cluster that contains the known effective leads [7].
- Define Key Molecular Descriptors: Extract physicochemical properties from known persister-killing antibiotics (e.g., eravacycline, minocycline). Key descriptors include
- Experimental Validation:
- Persister Preparation: Generate a high-persistence bacterial population. This can be done using a strain with a
hipA7allele or by treating a wild-type strain with a high concentration of a bactericidal antibiotic (e.g., a fluoroquinolone) and harvesting the surviving cells after a defined period [7]. - Compound Treatment: Treat the purified persister cells with candidate compounds identified from the clustering step (e.g., at 100 µg/mL) for a set duration.
- Viability Assessment: Remove the drug by washing and plate the cells to determine the number of surviving colony-forming units (CFUs). Compare this to an untreated persister control to calculate the log-killing efficacy [7].
- Persister Preparation: Generate a high-persistence bacterial population. This can be done using a strain with a
Signaling Pathways and Experimental Workflows
The following diagram illustrates the core workflow for conducting a cost-benefit analysis of a pre-clinical project, integrating both experimental and strategic considerations.
Diagram Title: Pre-Clinical Project Analysis Workflow
This diagram outlines the logical relationship between substrate availability, the formation of bacterial persisters, and the potential therapeutic strategies to combat them, which is central to the thesis context.
Diagram Title: From Substrate Stress to Infection Relapse
The Scientist's Toolkit: Research Reagent Solutions
Table 3: Essential Reagents and Materials for Anti-Persister Research
| Item | Function / Application | Key Consideration |
|---|---|---|
High-Persistence Bacterial Strains (e.g., E. coli HM22 with hipA7 allele) |
Provides a model system with a genetically high level of persister cells for consistent screening and mechanistic studies [7]. | Ensure genetic stability and use appropriate selective markers. |
| Bactericidal Antibiotics (e.g., Ciprofloxacin, Amikacin) | Used for "persister purification" by killing the actively growing population, leaving behind the tolerant persister subpopulation for experiments [1] [7]. | Confirm MIC/MBC for your strain; use at high multiples of MIC for selection. |
| Specialized Growth Media Components | To precisely control substrate availability (carbon, nitrogen) for studying nutrient-starvation-induced persistence [14]. | Use defined media for precise control over nutrient composition. |
| Iminosugar Scaffold Compound Library | A focused library for rational screening of compounds with potential activity against persister cells, as used in [7]. | Ideal for proof-of-concept screens based on chemoinformatic clustering. |
| Cell Membrane Potential Sensitive Dyes (e.g., DiOC₂(3)) | To measure membrane potential, a key physiological property that is often reduced in persister cells and affects drug penetration [7]. | Use with flow cytometry or fluorescence microscopy for quantification. |
| Patient-Derived Organoid (PDO) Kits | Provides a more human-relevant, 3D model system for studying persister infections in a tissue-like environment [88] [86]. | Requires specialized cell culture skills and optimized infection protocols. |
Conclusion
The strategic manipulation of substrate availability presents a powerful, non-traditional approach to combat bacterial persistence. Evidence confirms that nutrient limitation is a dominant environmental signal inducing metabolic dormancy and antibiotic tolerance. By leveraging tools like metabolic flux analysis and computational modeling, researchers can design interventions that maintain bacterial populations in a metabolically active, antibiotic-susceptible state. When optimized and combined with conventional antibiotics, these substrate-control strategies can significantly reduce persister burdens and improve treatment outcomes for chronic infections. Future research must focus on translating these principles into clinically viable therapies, exploring in vivo nutrient dynamics, and developing combination regimens that simultaneously target metabolic pathways and other persistence mechanisms. This paradigm shift from direct bacterial killing to microenvironmental control holds immense promise for overcoming one of the most challenging obstacles in modern antimicrobial therapy.
References
- 1. Bacterial persisters: molecular mechanisms and ... [https://www.nature.com/articles/s41392-024-01866-5]
- 2. Recent Advances in Bacterial Persistence Mechanisms - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC10531727/]
- 3. Molecular mechanism and application of emerging ... [https://bmcmicrobiol.biomedcentral.com/articles/10.1186/s12866-024-03628-3]
- 4. From Dormancy to Eradication: Strategies for Controlling ... [https://www.mdpi.com/2304-8158/14/6/1075]
- 5. Bacterial Persister Cells and Development of Antibiotic Resistance in Chronic Infections: An Update - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC11335562/]
- 6. Studying Bacterial Persistence: Established Methods and ... [https://pubmed.ncbi.nlm.nih.gov/34590248/]
- 7. A rational approach to discovering new persister control ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12406675/]
- 8. Unraveling persistent bacteria: Formation, niches, and ... [https://www.sciencedirect.com/science/article/abs/pii/S0944501325001454]
- 9. Persister cells: formation, resuscitation and combative ... [https://link.springer.com/article/10.1007/s00203-021-02585-z]
- 10. Modeling Antibiotic Tolerance in Biofilms by Accounting for ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC310152/]
- 11. Bacterial Persister Cell Formation and Dormancy - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC3837759/]
- 12. Metabolic Control of Persister Formation in Escherichia coli [https://www.sciencedirect.com/science/article/pii/S1097276513002839]
- 13. How do environment-dependent switching rates between ... [https://www.nature.com/articles/s41522-018-0049-2]
- 14. Optimization of periodic treatment strategies for bacterial ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11003776/]
- 15. How do environment-dependent switching rates between ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC5854711/]
- 16. Strategies for combating persister cell and biofilm infections [https://pmc.ncbi.nlm.nih.gov/articles/PMC5609227/]
- 17. Mini review: Persister cell control strategies [https://www.frontiersin.org/journals/pharmacology/articles/10.3389/fphar.2025.1706115/full]
- 18. Cancer dormancy and metabolism: From molecular ... [https://www.sciencedirect.com/science/article/abs/pii/S030438352500669X]
- 19. Dormancy: There and Back Again - PMC - PubMed Central [https://pmc.ncbi.nlm.nih.gov/articles/PMC9534470/]
- 20. Metabolic Features of Tumor Dormancy - PubMed Central - NIH [https://pmc.ncbi.nlm.nih.gov/articles/PMC8833651/]
- 21. Cellular Dormancy in Cancer: Mechanisms and Potential ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10372609/]
- 22. Recent insights into the effects of metabolism on breast ... [https://www.nature.com/articles/s41416-022-01869-5]
- 23. Combating Antibiotic Tolerance Through Activating Bacterial ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC7642520/]
- 24. Persister cells: formation, resuscitation and combative ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC8590677/]
- 25. Strategies for combating antibiotic resistance in bacterial ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10846525/]
- 26. Mechanisms of antimicrobial resistance in biofilms [https://www.nature.com/articles/s44259-024-00046-3]
- 27. Modulating the evolutionary trajectory of tolerance using ... [https://www.nature.com/articles/s41467-022-30272-0]
- 28. The Role of Bacterial Biofilms in Antimicrobial Resistance [https://asm.org/articles/2023/march/the-role-of-bacterial-biofilms-in-antimicrobial-re]
- 29. Combatting persister cells: The daunting task in post- ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10250163/]
- 30. Observation of persister cell histories reveals diverse ... [https://elifesciences.org/articles/79517]
- 31. A roadmap for interpreting 13C metabolite labeling patterns ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC4552607/]
- 32. Tracing metabolic flux in vivo: basic model structures of ... [https://www.nature.com/articles/s12276-022-00814-z]
- 33. Correcting for Naturally Occurring Mass Isotopologue ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC8151723/]
- 34. Measurement of metabolic fluxes using stable isotope tracers ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC5794022/]
- 35. Tracing metabolic flux through time and space with isotope ... [https://www.sciencedirect.com/science/article/pii/S0958166919301132]
- 36. Metabolomics in drug research and development: The recent ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10465962/]
- 37. A guide to 13C metabolic flux analysis for the cancer biologist [https://www.nature.com/articles/s12276-018-0060-y]
- 38. Computer simulation study of nutrient-driven bacterial biofilm ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11285826/]
- 39. Nutrient Gradients Mediate Complex Colony-Level ... [https://www.frontiersin.org/journals/microbiology/articles/10.3389/fmicb.2022.740259/full]
- 40. Agent Based Models of Polymicrobial Biofilms and the ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC7922883/]
- 41. Agent-based Modeling of Microbial Communities - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC10129392/]
- 42. Mathematical modeling of dormant cell formation in ... [https://www.frontiersin.org/journals/microbiology/articles/10.3389/fmicb.2015.00534/full]
- 43. New technique rapidly tracks cell state changes through ... [https://www.news-medical.net/news/20250521/New-technique-rapidly-tracks-cell-state-changes-through-density-measurements.aspx]
- 44. Text has enhanced contrast | ACT Rule | WAI [https://www.w3.org/WAI/standards-guidelines/act/rules/09o5cg/]
- 45. Text color must provide high contrast with its background [https://docs.acquia.com/web-governance/text-color-must-provide-high-contrast-its-background]
- 46. Protocol for flow cytometry-assisted single-nucleus RNA ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10909897/]
- 47. Isolation and characterization of persisters of the ... [https://www.sciencedirect.com/science/article/pii/S2589004224012276]
- 48. Antibiotic Persistence as a Metabolic Adaptation [https://pmc.ncbi.nlm.nih.gov/articles/PMC5874710/]
- 49. Metabolite-driven reprogramming of bacterial persisters [https://www.sciencedirect.com/science/article/abs/pii/S1368764625001256]
- 50. Antimicrobial Susceptibility Testing - StatPearls - NCBI - NIH [https://www.ncbi.nlm.nih.gov/books/NBK539714/]
- 51. Unveiling the critical roles of cellular metabolism ... [https://www.nature.com/articles/s44259-024-00034-7]
- 52. Physiological heterogeneity in biofilms [https://www.nature.com/articles/nrmicro1838]
- 53. Gradients and consequences of heterogeneity in biofilms [https://pmc.ncbi.nlm.nih.gov/articles/PMC9590228/]
- 54. Dissecting cell heterogeneities in bacterial biofilms and ... [https://www.sciencedirect.com/science/article/abs/pii/S1369527424000262]
- 55. Biofilms: structure, resistance mechanism, emerging control ... [https://pubs.rsc.org/en/content/articlehtml/2025/pm/d5pm00094g]
- 56. Biofilm antimicrobial susceptibility through an experimental ... [https://www.nature.com/articles/s41522-022-00346-4]
- 57. Biofilms Exposed: Innovative Imaging and Therapeutic ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12466655/]
- 58. Differential carbon source utilization drives metabolic state ... [https://pubmed.ncbi.nlm.nih.gov/40969939/]
- 59. Differential carbon source utilization drives metabolic state ... [https://www.frontiersin.org/journals/pharmacology/articles/10.3389/fphar.2025.1634627/full]
- 60. Relating switching rates between normal and persister ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC5658594/]
- 61. Persister control by leveraging dormancy associated reduction ... [https://journals.plos.org/plospathogens/article?id=10.1371/journal.ppat.1010144]
- 62. Systematic design of pulse dosing to eradicate persister ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC9882918/]
- 63. Fighting bacterial persistence: Current and emerging anti- ... [https://www.sciencedirect.com/science/article/abs/pii/S1368764618300232]
- 64. DUWL- Troubleshooting Dental Water Quality Problems [https://www.myads.org/topics-duwl--troubleshooting-dental-water-quality-problems]
- 65. In Vitro Studies of Persister Cells - PMC - PubMed Central [https://pmc.ncbi.nlm.nih.gov/articles/PMC7667008/]
- 66. Bacterial Persister Cells and Development of Antibiotic ... [https://www.frontierspartnerships.org/journals/british-journal-of-biomedical-science/articles/10.3389/bjbs.2024.12958/full]
- 67. Predicting Metabolic Adaptation Under Dynamic Substrate ... [https://www.frontiersin.org/journals/molecular-biosciences/articles/10.3389/fmolb.2022.863470/full]
- 68. Molecular Mechanisms Underlying Bacterial Persisters [https://www.sciencedirect.com/science/article/pii/S0092867414002979]
- 69. Engineering high-efficiency matriptase substrates using E. ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12272249/]
- 70. Therapeutic approaches to addressing drug resistance by ... [https://www.sciencedirect.com/science/article/abs/pii/S1359644625002399]
- 71. A host-directed adjuvant sensitizes intracellular bacterial ... [https://www.nature.com/articles/s41564-025-02124-2]
- 72. Antibacterial nanoagents: an emerging arsenal against ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12537890/]
- 73. Antibacterial Prodrugs to Overcome Bacterial Resistance [https://pmc.ncbi.nlm.nih.gov/articles/PMC7180472/]
- 74. Antibacterial Prodrugs to Overcome Bacterial Antimicrobial ... [https://www.mdpi.com/1424-8247/17/6/718]
- 75. of Mechanisms Action and Resistance - PMC Pyrazinamide [https://pmc.ncbi.nlm.nih.gov/articles/PMC4268777/]
- 76. The molecular basis of pyrazinamide activity... | Nature Communications [https://www.nature.com/articles/s41467-019-14238-3?error=cookies_not_supported&code=2f7c4a55-533f-4e04-8c0a-02ddf5642935]
- 77. Metabolic aspects of bacterial persisters [https://www.frontiersin.org/journals/cellular-and-infection-microbiology/articles/10.3389/fcimb.2014.00148/full]
- 78. sciencedirect.com/topics/medicine-and-dentistry/ pyrazinamide [https://www.sciencedirect.com/topics/medicine-and-dentistry/pyrazinamide]
- 79. Do Mixed-Species Biofilms Dominate in Chronic Infections? [https://www.frontiersin.org/journals/cellular-and-infection-microbiology/articles/10.3389/fcimb.2020.00396/full]
- 80. Novel Protocol for Persister Cells Isolation - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC3931647/]
- 81. Strategies to prevent, curb and eliminate biofilm formation ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC9534288/]
- 82. Resuscitation dynamics reveal persister partitioning after ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10090945/]
- 83. An ecological and stochastic perspective on persisters ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11697298/]
- 84. Birth and Resuscitation of (p)ppGpp Induced Antibiotic ... [https://www.nature.com/articles/s41598-019-42403-7]
- 85. Preclinical CRO Trends and Forecast Report 2025 [https://finance.yahoo.com/news/preclinical-cro-trends-forecast-report-114900451.html]
- 86. Preclinical CRO Market Size at USD 6.8 Billion in 2025, [https://www.globenewswire.com/news-release/2025/07/16/3116561/0/en/Preclinical-CRO-Market-Size-at-USD-6-8-Billion-in-2025-Forecasted-to-Grow-at-8-73-CAGR-Through-2034.html]
- 87. 2025 Biotech Economics: CROs, Advanced Therapies & ... [https://www.precisionformedicine.com/blog/2025-biotech-economics-cros-advanced-therapies-trends-in-funding]
- 88. Biopharma Trends 2025 [https://www.bcg.com/publications/2025/biopharma-trends]
- 89. Trends Shaping Biopharma in 2025 [https://www.deloitte.com/us/en/Industries/life-sciences-health-care/blogs/health-care/trends-shaping-biopharma.html]
- 90. Pharmaceutical industry trends 2025, outlook and strategies [https://www.zs.com/insights/pharmaceutical-trends-2025-outlook-ai-supplychain-and-beyond]