The Biofilm Barrier: Decoding Matrix Composition and Its Role in Antibiotic Treatment Failure
Biofilms, structured communities of microbes encased in a self-produced extracellular matrix, represent a primary driver of antibiotic treatment failure in chronic infections.
The Biofilm Barrier: Decoding Matrix Composition and Its Role in Antibiotic Treatment Failure
Abstract
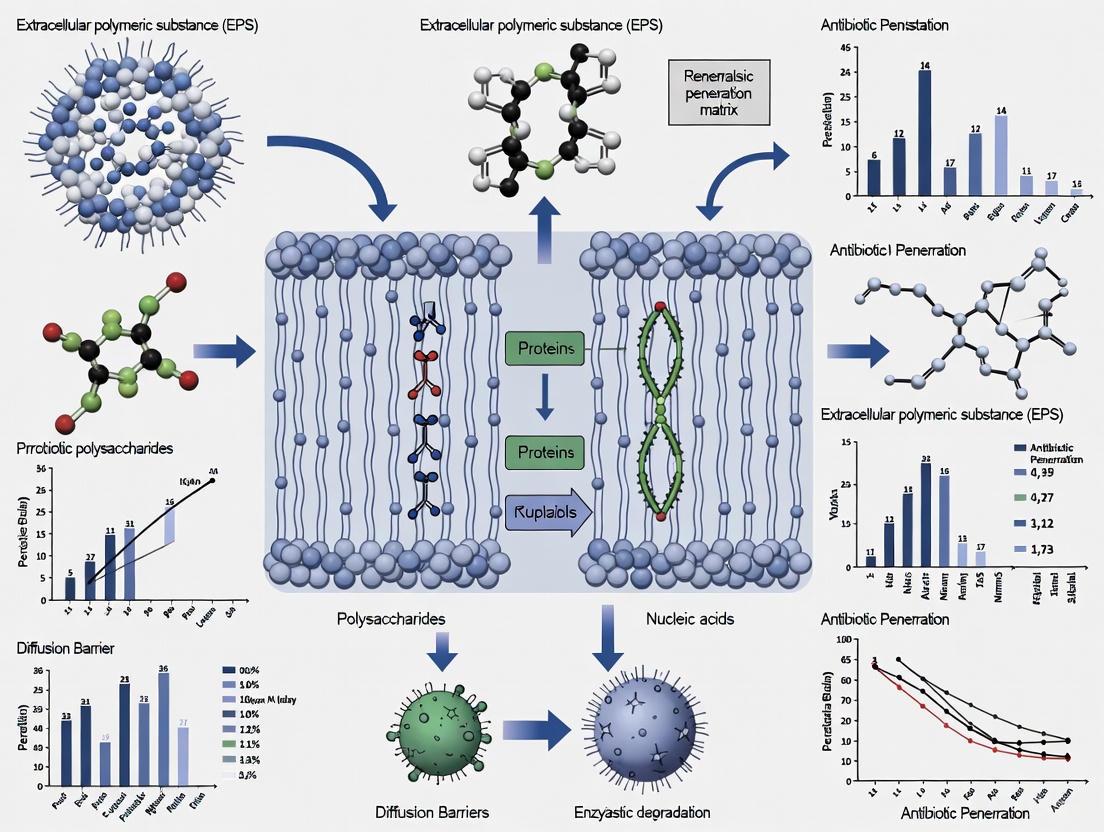
Biofilms, structured communities of microbes encased in a self-produced extracellular matrix, represent a primary driver of antibiotic treatment failure in chronic infections. This article provides a comprehensive analysis for researchers and drug development professionals on the intricate relationship between biofilm matrix composition and impaired antibiotic penetration. We first deconstruct the foundational architecture of the biofilm matrix, detailing its key components—exopolysaccharides, proteins, eDNA, and lipids—and their collective role in creating a physical and functional barrier. The review then transitions to methodological approaches for studying antibiotic diffusion and efficacy, followed by an critical examination of the multifaceted resistance mechanisms, including hindered diffusion, enzymatic inactivation, and metabolic heterogeneity. Finally, we evaluate and compare emerging therapeutic strategies, from matrix-degrading enzymes and nanoparticle-based delivery systems to quorum-sensing inhibitors and combinatorial therapies, offering a validated perspective on the future of anti-biofilm drug development.
Deconstructing the Fortress: An Architectural Guide to the Biofilm Matrix
Core Components of the Extracellular Polymeric Substance (EPS)
The extracellular polymeric substance (EPS) is a complex, self-produced matrix that encompasses microbial cells within a biofilm, serving as the primary architectural and functional component of this aggregated community [1] [2]. This organic polymer matrix of microbial origin is critical for establishing and maintaining the biofilm structure, conferring stability, cohesion, and viscoelasticity to the entire system [1]. The EPS matrix represents a key element in the biofilm's defensive strategy, creating a protected microenvironment that significantly contributes to intrinsic resistance against antimicrobial agents [2]. This review provides an in-depth technical examination of EPS core components, their physicochemical properties, and their collective role in hindering antibiotic penetration, all within the context of advancing biofilm matrix composition and antibiotic resistance research.
Core Biochemical Composition of EPS
EPS are organic polymers comprised of a diverse array of biopolymers that interact to form a protective hydrogel matrix. The composition is highly dynamic, varying based on microbial species, environmental conditions, and growth phase [2] [3].
Table 1: Primary Constituents of Microbial EPS
| Component | Relative Abundance | Key Functional Groups | Major Functional Roles |
|---|---|---|---|
| Polysaccharides | Often dominant (variable) | Hydroxyl, Carboxyl, Uronic acids | Structural integrity, hydration, adhesion [3] [4] |
| Proteins | 15%-75% (can be dominant) | Amino, Carboxyl, Sulfhydryl | Structural support, enzymatic activity, adhesion [5] [3] |
| Extracellular DNA (eDNA) | 1%-10% (variable) | Phosphate (negative charge) | Polymer entanglement, cation exchange, genetic info [1] [2] |
| Lipids | Variable (often minor) | Alkyl chains | Hydrophobicity, surface attachment [1] [3] |
| Humic-like Substances | Variable in environmental biofilms | Phenolic, Quinoid | Redox activity, metal binding [6] |
Polysaccharides
Exopolysaccharides form the sugar-based backbone of many EPS matrices, consisting of monosaccharides (e.g., glucose, galactose, mannose) and non-carbohydrate substituents including acetate, pyruvate, and succinate [3]. These polymers can be linear or branched and are frequently anionic due to the presence of uronic acids (e.g., glucuronic acid) or ketal-linked pyruvates, contributing to their cation-exchange capacity and gel-forming properties [3] [4]. Notable examples include alginate in Pseudomonas aeruginosa, poly-N-acetylglucosamine (PNAG) in Staphylococcus epidermidis, and cellulose in Acetobacter xylinum [2] [3].
Proteins
The proteinaceous component of EPS includes structural proteins and extracellular enzymes (exoenzymes) [3]. Structural proteins often contain repetitive sequences and facilitate surface adhesion and cell-to-cell interactions [2]. Exoenzymes such as proteases, glycosidases, and phosphatases remain active within the matrix, performing critical functions in nutrient acquisition by breaking down complex organic molecules into assimilable subunits [5] [3]. These enzymes also contribute to biofilm remodeling and detachment [1].
Extracellular DNA (eDNA)
eDNA is released into the matrix through cell lysis and active secretion [2]. It functions as a structural cross-linking agent, particularly in biofilms of species like Staphylococcus aureus and Pseudomonas aeruginosa [2]. The negatively charged phosphate groups of eDNA engage in electrostatic interactions with other EPS components and cationic antimicrobials, such as aminoglycosides, effectively trapping them and reducing their penetration [2].
Other Components
Lipids, though typically a minor component, can increase matrix hydrophobicity, influencing surface attachment and resistance to hydrophobic antibiotics [1] [3]. Humic-like substances, prevalent in environmental biofilms, contribute to the matrix's electron-transfer capabilities and can bind various contaminants [6].
Quantitative Analysis of EPS Composition
The relative proportions of EPS constituents vary significantly across microbial species and environmental conditions. Technical quantification is essential for understanding structure-function relationships.
Table 2: Quantitative EPS Composition from Selected Systems
| Biological System / Condition | Proteins (%) | Polysaccharides (%) | eDNA/Lipids/Other | Protein/Polysaccharide Ratio | Source |
|---|---|---|---|---|---|
| General Microbial EPS | 15-75 | 15-75 | 1-10% eDNA, variable lipids | Highly variable (0.2-5.0) | [5] [3] [7] |
| Anammox Granular Biofilm | ~60-75 (of total organic matter) | ~25-40 (of total organic matter) | Not specified | ~1.5 - 3.0 | [6] |
| Fusarium culmorum (Pathogen) | Variable | High total sugar, rich in mannose | Phenolic components | Variable, strain-dependent | [4] |
| E. coli (Lab Culture) | ~10% (by dry weight) | ~30% (by dry weight) | Not specified | ~0.33 | [8] |
Factors Influencing Composition
EPS composition is not static but responds dynamically to environmental cues. Stress conditions such as nutrient limitation, presence of toxins (e.g., antibiotics, heavy metals), and osmotic stress can trigger significant shifts in EPS production and composition [5] [4]. For instance, the protein/polysaccharide ratio can indicate the physiological state of the biofilm, with a decrease potentially signaling preferential polysaccharide production [1].
Functional Properties and Role in Antibiotic Resistance
The EPS matrix acts as a multifaceted barrier against antimicrobial agents, employing several mechanisms that collectively contribute to the remarkable tolerance of biofilms to antibiotic treatments [2] [9].
Physical Barrier and Retarded Diffusion
The dense, highly hydrated network of EPS creates a physical diffusion barrier that significantly slows the penetration of antimicrobial molecules into the deeper layers of the biofilm [2] [9]. This retarded diffusion is influenced by factors such as biofilm thickness, matrix porosity, and the physicochemical properties of the antibiotic itself [9]. Positively charged aminoglycosides, for example, are particularly susceptible to binding with negatively charged polymers like eDNA and alginate within the matrix, leading to their sequestration before reaching cellular targets [2].
Chemical Interactions and Sequestration
EPS components provide abundant functional groups (e.g., carboxyl, hydroxyl, amine, phosphoryl) that serve as binding sites for antibiotics [5]. The primary mechanisms of antibiotic adsorption onto EPS include electrostatic interactions, hydrogen bonding, hydrophobic interactions, and surface complexation [5]. Proteins in EPS often exhibit a higher binding strength and capacity for antibiotics like tetracycline and sulfamethazine compared to humic-like organics, playing a predominant role in this sequestration process [5].
Physiological and Metabolic Heterogeneity
As antibiotics penetrate the biofilm, they encounter gradients of nutrients, oxygen, and waste products, leading to zones of varying metabolic activity [9]. Cells in the deep, nutrient-depleted layers of the biofilm often enter a slow-growing or dormant state, making them less susceptible to antibiotics that target active cellular processes [9]. These conditions promote the formation of persister cells—dormant variants that exhibit high tolerance to antibiotics and can repopulate the biofilm after treatment cessation [9].
Analytical Methods for EPS Characterization
A combination of destructive and non-destructive analytical techniques is employed to elucidate the composition, structure, and function of EPS.
Fourier Transform Infrared (FT-IR) Spectroscopy
FT-IR spectroscopy is a powerful, non-destructive technique that provides information about the chemical content and relative proportions of different EPS constituents based on their functional groups' absorption of infrared radiation [1].
- Experimental Protocol: Biofilm samples can be analyzed in situ under hydrated conditions using Attenuated Total Reflection (ATR) mode, which probes approximately the first 2 µm of the surface layer. Alternatively, dried mature biofilms can be analyzed to reduce the confounding effect of water [1].
- Spectral Interpretation: Key spectral windows include:
- 2800–3000 cm⁻¹: C-H stretching vibrations, primarily from lipids.
- 1500–1800 cm⁻¹: Amide I (C=O) and Amide II (N-H) bands from proteins.
- 900–1250 cm⁻¹: C-O, C-O-C stretching, and P=O stretching from polysaccharides and nucleic acids [1].
- Data Analysis: Monitoring the evolution of band intensity ratios (e.g., Amide II/Polysaccharide) over time can reveal shifts in biofilm composition, such as preferential polysaccharide production (ratio decrease) or protein accumulation (ratio increase) [1].
EPS Extraction and Quantitative Analysis
To determine the absolute abundance of EPS components, physical and/or chemical extraction methods are required, followed by quantitative assays.
- Extraction Protocol: A common method involves low-speed centrifugation (e.g., 3000 × g for 10 min) to separate cells from the bulk liquid. The harvested cells are washed and resuspended in a suitable buffer (e.g., ultrapure water or NaCl). EPS are then separated from the cells via sonication (e.g., 2.7 W/cm², 40 Hz, 10 min at 4°C) followed by high-speed centrifugation (e.g., 10,600 × g for 20 min) [8]. The supernatant containing the EPS is filtered (0.45 µm) to remove any remaining cells.
- Quantification of Components:
- Proteins: Commonly measured using the Lowry or Bradford assays, with bovine serum albumin as a standard.
- Polysaccharides: Often quantified by the phenol-sulfuric acid method, with glucose or other relevant sugars as standards.
- eDNA: Can be quantified using fluorescent dyes like PicoGreen after purification [6].
- Advanced Qualitative Techniques:
- Three-Dimensional Excitation-Emission Matrix (3D-EEM) Fluorescence Spectroscopy: Identifies and characterizes fluorescent organic compounds like specific protein motifs (tryptophan/tyrosine) and humic-like substances [6].
- Size Exclusion Chromatography (SEC): Provides information about the apparent molecular weight distribution of EPS polymers [6].
- Hydrophobicity Measurement: Determined by contact angle measurement or hydrophobic interaction chromatography [6].
The Scientist's Toolkit: Key Research Reagents and Methods
Table 3: Essential Reagents and Methods for EPS Research
| Reagent / Method | Function in EPS Research | Key Considerations |
|---|---|---|
| Cation Exchange Resin | Extracts EPS from microbial aggregates by disrupting ionic bonds. | Minimizes cell lysis compared to chemical methods [6]. |
| Sonication Bath | Physically shears EPS from cell surfaces during extraction. | Power and duration must be optimized to avoid cell disruption [8]. |
| ATR/FT-IR Spectroscopy | Provides in-situ, non-destructive analysis of biofilm chemical composition. | Germanium crystals are common Internal Reflection Elements (IRE) [1]. |
| Fluorescence Spectrophotometer | Used for 3D-EEM to characterize protein and humic components. | Can identify specific fluorophores based on excitation/emission pairs [6]. |
| Hydrolytic Enzymes (e.g., Proteases, DNases, Amylases) | Selectively degrades specific EPS components to study their functional role. | Used to test biofilm destabilization and component involvement in integrity [1]. |
| Propidium Iodide | Fluorescent dye used to assess cell membrane permeability and viability. | Can be used to correlate EPS removal with increased cell permeability [8]. |
The extracellular polymeric substance is a sophisticated biological construct whose core components—polysaccharides, proteins, eDNA, and lipids—operate in concert to form a dynamic and protective matrix. The quantitative and qualitative characterization of these components reveals a system engineered for resilience, directly contributing to the challenge of treating biofilm-associated infections through mechanisms of physical blockage, chemical interaction, and induction of microbial physiological heterogeneity. A deep understanding of EPS composition and function, enabled by the detailed methodologies outlined herein, is paramount for the future development of targeted therapeutic strategies aimed at disrupting this critical barrier and overcoming antibiotic resistance in biofilms.
Spatial Organization and the 3D Structural Scaffold
The spatial organization and three-dimensional structural scaffold of biofilms represent a fundamental pillar of microbial life, underpinning the remarkable resilience of these communities to antimicrobial agents. Within the context of biofilm matrix composition and antibiotic penetration resistance research, understanding this sophisticated architecture is paramount. The extracellular polymeric substance (EPS) matrix forms a complex, heterogeneous scaffold that not only provides structural integrity but also creates formidable physical and chemical barriers to antibiotic penetration [10]. This organized ecosystem, characterized by gradients of nutrients, oxygen, and metabolic activity, enables microbial populations to survive concentrations of antimicrobials that would readily eliminate their planktonic counterparts [11]. The 3D organization of biofilms thus presents a critical challenge in clinical and industrial settings, driving the urgent need for advanced analytical techniques to decipher its intricacies and overcome the therapeutic failures associated with biofilm-mediated resistance.
Matrix Composition: The Building Blocks of the Biofilm Scaffold
The biofilm scaffold is an amalgamation of microbial cells and self-produced extracellular substances, creating a heterogeneous structure with significant architectural complexity. Biofilms are primarily composed of microbial cells (10-25%) embedded within an EPS matrix (75-90%) that is predominantly water (up to 97%) [10]. This EPS forms a protective scaffold that holds the biofilm together through various intermolecular forces, including van der Waals interactions, electrostatic forces, and hydrogen bonding [10].
Table 1: Key Components of the Biofilm Extracellular Polymeric Substance Matrix
| Component | Percentage | Primary Functions | Representative Examples |
|---|---|---|---|
| Polysaccharides | 1-2% | Structural backbone, adhesion, cohesion, protection | Pel, Psl, alginate in Pseudomonas aeruginosa; cellulose, glucans [10] |
| Proteins | <1-2% | Matrix stabilization, enzymatic activity, surface colonization | Cell surface adhesins, proteases, glycosyl hydrolases, disulfide-isomerases [10] |
| Extracellular DNA (eDNA) | <1-2% | Structural cohesion, horizontal gene transfer, antibiotic chelation | DNA from lysed cells, contributes to antimicrobial resistance [11] [10] |
| Lipids | Variable | Hydrophobicity, barrier functions | Influence biofilm hydrophobicity and permeability [11] |
| Inorganic Ions | Variable | Matrix cross-linking, mineralization | Calcium, magnesium facilitate component cross-linking [11] |
The compositional profile of the EPS is not static but dynamically adapts to environmental conditions. For instance, in Pseudomonas aeruginosa, three exopolysaccharides—Pel, Psl, and alginate—play distinct yet complementary roles in maintaining biofilm architecture and conferring resistance properties [10]. Similarly, extracellular proteins contribute to structural integrity through interactions with polysaccharides and nucleic acids, while some specialized proteins facilitate matrix degradation and dispersal when environmental conditions favor biofilm dissemination [10].
Methodologies for Spatial Analysis of Biofilm Architecture
Advanced Imaging and Computational Analysis
Deciphering the spatial organization of biofilms requires sophisticated imaging technologies coupled with powerful computational tools. Confocal laser scanning microscopy (CLSM) has proven invaluable for visualizing the 3D architecture of biofilms without disrupting their native structure, revealing multiple layers with distinct ecological niches occupied by different bacterial species [11]. This spatial heterogeneity creates microenvironments with varying nutrient gradients, oxygen levels, and metabolic activities that fundamentally influence biofilm function and pathogenicity [11].
For comprehensive quantitative analysis, BiofilmQ software provides an advanced image cytometry platform specifically designed for 3D microbial communities [12]. This tool enables automated high-throughput quantification of numerous biofilm-internal and whole-biofilm properties, including:
- Structural parameters: Volume, mean thickness, surface area, roughness coefficient, and surface-to-volume ratio
- Spatially resolved properties: Gradient analyses of fluorescent reporters, distance to biofilm outer surface or substratum
- Correlation metrics: Species cluster sizes and separation distances in multispecies biofilms using 3D correlation functions [12]
The software employs cube-based image cytometry, dissecting the biofilm biovolume into a cubical grid with user-defined dimensions, enabling 3D spatially resolved quantification even in images where single-cell segmentation is not possible [12]. For higher resolution images, users can import custom-segmented biofilm images, including those generated by convolutional neural networks like U-Net, which offer improved segmentation accuracy for specific biofilm morphologies [12].
Accessible Staining and Visualization Techniques
While advanced microscopy offers unparalleled resolution, practical constraints often necessitate simpler methodologies for routine biofilm analysis. The dual-staining protocol using Maneval's stain and Congo red provides a cost-effective alternative for visualizing and differentiating microbial biofilms with basic laboratory equipment [13]. This method effectively distinguishes bacterial cells (magenta-red) from the biofilm matrix (blue) in a single stain, with the complete process requiring only 30-45 minutes [13].
Table 2: Experimental Protocols for Biofilm Spatial Analysis
| Method | Key Applications | Technical Requirements | Output Parameters |
|---|---|---|---|
| BiofilmQ Software Analysis | High-throughput 3D quantification of biofilm architecture | Fluorescence images, standard computer | 49+ structural, textural, and fluorescence properties; population analysis; temporal tracking [12] |
| Dual Staining with Maneval's Stain | Differentiation of bacterial cells vs. matrix; capsule visualization | Light microscope, basic stains | Color differentiation: blue matrix vs. magenta-red cells; identification of halo formation indicating capsules [13] |
| Microtiter Plate Biofilm Assay | Semiquantitative assessment of adherent biomass | 96-well plates, crystal violet, plate reader | Optical density measurements of stained biofilms; high-throughput capability [14] |
| Colony-Based Biofilm System | Monitoring cell death in antimicrobial treatments | Agar plates, viability stains | Viability counts; antimicrobial efficacy assessment [14] |
The technical workflow for the dual-staining method begins with biofilm growth on glass slides submerged in diluted culture broth for 3 days at 37°C, followed by gentle rinsing, fixation with 4% formaldehyde, and sequential staining with Congo red and Maneval's stain [13]. This approach allows researchers to identify distinct stages of biofilm development—from early cobweb-like structures through intermediate clustered stages to mature honeycomb-like architectures with well-defined channels [13].
The Scientist's Toolkit: Essential Research Reagents and Materials
Table 3: Research Reagent Solutions for Biofilm Spatial Analysis
| Reagent/Material | Function/Application | Examples/Specifications |
|---|---|---|
| BiofilmQ Software | 3D image cytometry and analysis of microbial communities | Quantitative analysis of spatially resolved structural parameters; available at https://drescherlab.org/data/biofilmQ [12] |
| Maneval's Stain | Differential staining of bacterial cells and matrix | Composition: 0.05 g fuchsin, 3.0 g ferric chloride, 5 mL acetic acid, 3.9 mL phenol, 95 mL distilled water [13] |
| Congo Red Stain | Polysaccharide matrix staining | 1% solution in distilled water; interacts with hydrophobic regions of polysaccharides through hydrogen bonds [13] |
| Crystal Violet | Biomass staining for microtiter plate assays | 0.1% solution in water; stains adherent cells for semiquantitative assessment [14] |
| 96-Well Microtiter Plates | High-throughput biofilm cultivation | Non-tissue culture treated plates (e.g., Becton Dickinson #353911) for static biofilm assays [14] |
| Solvents for Dye Elution | Solubilization of stained biofilms for quantification | 30% acetic acid, 95% ethanol, or 100% DMSO; choice is organism-dependent [14] |
Architectural Dynamics and Functional Consequences
The spatial organization of biofilms is not merely structural but fundamentally functional, creating heterogeneous microenvironments that drive microbial behavior and therapeutic resistance. The 3D architecture typically features water channels separating microcolonies, enabling nutrient circulation and waste removal [10]. This organization often follows a stratification pattern where early colonizers such as Streptococcus spp. consume oxygen, creating anaerobic niches that support pathogenic obligate anaerobes implicated in periodontal disease [11].
The following diagram illustrates the key stages in the development of this complex spatial architecture:
This developmental process culminates in a mature biofilm that may acquire "mushroom" or "tower" shaped structures where microorganisms arrange themselves according to aero-tolerance and metabolic rates [10]. The resulting spatial heterogeneity creates diffusion barriers that significantly impede antibiotic penetration, while the varied metabolic states of cells in different regions reduce antimicrobial susceptibility [11] [10]. Additionally, the EPS components can directly bind and neutralize certain antimicrobial compounds, further enhancing the protective function of the biofilm scaffold [10].
The spatial organization and 3D structural scaffold of biofilms represent a sophisticated adaptation that continues to challenge conventional antimicrobial strategies. As research progresses, the integration of advanced imaging technologies with computational analytics like BiofilmQ promises to unravel the complex architecture-function relationships that underpin biofilm resilience [12]. Emerging therapeutic approaches are increasingly targeting the structural integrity of biofilms through enzymatic matrix degradation, quorum sensing inhibition, and disruption of spatial organization mechanisms [10] [15]. The continuing refinement of accessible methodologies, such as the dual-staining technique using Maneval's stain, will enable broader screening capabilities across diverse laboratory settings [13]. Ultimately, overcoming the barrier presented by biofilm spatial organization will require multidisciplinary approaches that bridge microscopy, materials science, microbiology, and computational analytics to develop effective interventions against these recalcitrant microbial communities.
In the ongoing battle against antimicrobial resistance (AMR), bacterial biofilms represent a formidable challenge, contributing significantly to persistent infections and treatment failures. A biofilm is a complex, surface-associated microbial community encased in a self-produced matrix of extracellular polymeric substances (EPS) [16]. This structured consortium is not merely a collection of cells but a dynamic, organized ecosystem that demonstrates a distinct lifecycle. Comprehending this lifecycle—from initial attachment to final dispersion—is paramount for developing effective interventions against biofilm-associated infections, particularly those involving multidrug-resistant ESKAPE pathogens (Enterococcus faecium, Staphylococcus aureus, Klebsiella pneumoniae, Acinetobacter baumannii, Pseudomonas aeruginosa, and Enterobacter species) [16]. This review delineates the biofilm lifecycle within the critical context of matrix composition and its role in impeding antibiotic penetration, providing a technical guide for researchers and drug development professionals.
The Biofilm Lifecycle: A Stage-by-Stage Analysis
The formation of a biofilm is a multifaceted process involving physical, chemical, and biological elements. It typically unfolds in several sequential, yet overlapping, stages [16] [2].
Initial Reversible Attachment
The lifecycle commences with the adhesion of free-living (planktonic) microorganisms to a conditioned surface [16] [2]. This initial attachment is mediated by weak, reversible interactions such as van der Waals forces and electrostatic interactions [16]. The nature of the surface plays a critical role; for instance, rough surfaces tend to promote better microbial adhesion compared to smooth ones [16]. Bacteria may employ structures like pili for a more passive attachment or engage active mechanisms requiring prolonged surface contact [16]. Notably, traditional models of single-cell attachment are now complemented by understanding that seeding often begins with clumps of cells or aggregates that detach from existing biofilms, which are inherently more resilient to stress [2].
Irreversible Attachment and Microcolony Formation
Following initial attachment, the connection to the surface becomes permanent. The reversibly attached cells utilize environmental nutrients to grow, divide, and begin secreting the sticky, three-dimensional EPS matrix, primarily composed of polysaccharides, proteins, lipids, and extracellular DNA (eDNA) [16] [2]. This matrix facilitates irreversible attachment and anchors the cells together [16]. A key molecular regulator in this transition is the secondary messenger cyclic diguanylate monophosphate (c-di-GMP). High intracellular levels of c-di-GMP, controlled by the balance of diguanylate cyclases (DGCs) and phosphodiesterases (PDEs), promote a sessile lifestyle by reducing motility and encouraging matrix production [2]. This stage leads to the formation of distinct microcolonies [16] [2].
Maturation
During maturation, microcolonies expand and develop into a mature biofilm with a complex, heterogeneous architecture [16] [2]. The EPS matrix can constitute over 90% of the biofilm's biomass, creating a structured environment with gradients of oxygen, nutrients, and pH [2]. These gradients generate diverse microniches, leading to metabolic heterogeneity among the embedded cells [2]. The biofilm community engages in sophisticated coordination through quorum sensing (QS), a cell-to-cell communication system where bacteria detect population density via signaling molecules like acyl-homoserine lactones (AHLs) in Gram-negative bacteria [2] [11]. QS regulates collective behaviors, including virulence expression and further matrix synthesis [11]. The resulting structure, often characterized by mushroom-shaped towers or other architectures depending on the species and environment, is highly resistant to external threats [2].
Dispersion
The final stage of the lifecycle is dispersion, where cells actively detach from the biofilm to colonize new substrates [2]. This complex process can be initiated in response to environmental cues such as nutrient starvation or the presence of antimicrobials [2]. Mechanisms of dispersal include:
- Seeding (Central Hollowing): An active process where large quantities of cells or micro-colonies are promptly released, forming hollow cavities within the biofilm [2].
- Erosion and Sloughing: Passive processes where smaller fragments erode over time or substantial fragments detach abruptly due to external forces like shear flow [2]. Dispersal is a critical event for bacterial survival and propagation, completing the lifecycle and allowing it to begin anew in a different location.
Table 1: Key Stages of the Biofilm Lifecycle and Their Characteristics
| Lifecycle Stage | Key Processes | Physiological Regulators | Structural Outcomes |
|---|---|---|---|
| Initial Attachment | Reversible adhesion via weak forces (van der Waals, electrostatic) | Surface properties (roughness, hydrophobicity) | Formation of a preconditioned layer; presence of pioneer cells or aggregates [16] [2] |
| Irreversible Attachment | EPS secretion, transition from planktonic to sessile growth | Increased intracellular c-di-GMP levels [2] | Stable anchorage to surface; formation of a protective matrix [16] |
| Maturation | Microcolony development, 3D architectural formation, metabolic heterogeneity | Quorum Sensing (e.g., AHLs, AI-2) [11] | Complex, heterogeneous structures (e.g., mushroom-shaped); established nutrient/gradient niches [2] |
| Dispersion | Active (seeding) or passive (erosion, sloughing) detachment | Environmental stress (e.g., nutrient depletion) [2] | Release of planktonic cells or aggregates for new colonization; hollowing of biofilm structure [2] |
Quantitative Analysis of Biofilm Composition and Dynamics
Understanding the temporal evolution of biofilm matrix components is crucial for targeting its structural integrity. Advanced techniques like solid-state nuclear magnetic resonance (ssNMR) enable non-destructive, quantitative tracking of compositional changes.
A time-resolved ssNMR study of Bacillus subtilis biofilms over a 5-day period revealed distinct phases of development and degradation [17]. The mature biofilm, established within 48 hours, underwent significant degradation in the subsequent 72 hours. The steepest decline in proteins preceded that of exopolysaccharides, likely reflecting their distinct spatial distribution and functional roles within the matrix [17]. Furthermore, different sugar units within the exopolysaccharides displayed clustered temporal patterns, suggesting the presence of distinct polysaccharide types with varying stability or turnover rates [17]. A sharp rise in aliphatic carbon signals on day 4 was also noted, probably corresponding to a surge in biosurfactant production, potentially linked to the dispersal phase [17].
Table 2: Time-Resolved Compositional Changes in Bacillus subtilis Biofilm Matrix (ssNMR Data) [17]
| Time Point | Key Compositional and Dynamic Events | Interpretation and Functional Implication |
|---|---|---|
| Day 1-2 | Establishment of mature biofilm structure; distinct dynamic regimes (90% mobile, 10% rigid phases) | Initial matrix assembly creates a heterogeneous environment with components of varying molecular mobility [17] |
| Day 3-5 | Initiation of degradation phase; steepest decline of proteins precedes exopolysaccharide loss | Proteins may be more accessible to degradation or located in vulnerable regions of the matrix, impacting structural stability [17] |
| Throughout | Clustered temporal patterns of exopolysaccharide sugar units | Suggests presence of structurally and functionally distinct polysaccharide types within the EPS [17] |
| Day 4 | Sharp increase in aliphatic carbon signals | Likely reflects increased production of biosurfactants, molecules often associated with biofilm dispersal [17] |
Mechanisms of Biofilm-Associated Antibiotic Resistance
The biofilm matrix and the altered physiology of its resident cells create multiple, synergistic barriers to antibiotic efficacy, contributing to profound tolerance and resistance [16] [2].
- Physical Barrier and Charge-Based Sequestration: The dense EPS matrix acts as a diffusion barrier, physically impeding the penetration of antimicrobial agents [2]. Some antibiotics are rendered ineffective by forming complexes with matrix components or being broken down by enzymes within the matrix [2]. Positively charged antibiotics, such as aminoglycosides, can bind to negatively charged biopolymers like eDNA in the matrix, significantly slowing their penetration and reducing the effective concentration that reaches the cells [2].
- Metabolic Heterogeneity and Persister Cells: The spatial heterogeneity of biofilms results in gradients of nutrient availability, oxygen, and waste products [2]. This creates zones of slow bacterial growth or metabolic dormancy. Since many conventional antibiotics target active cellular processes (e.g., cell wall synthesis, protein production), these dormant or slow-growing cells are inherently tolerant [2] [18]. A subpopulation of these, known as persister cells, can survive high doses of antibiotics without genetic mutation and repopulate the biofilm once treatment ceases [18].
- Horizontal Gene Transfer (HGT): The dense, structured environment of a biofilm, facilitated by components like eDNA, provides an ideal platform for the efficient exchange of genetic material between cells through conjugation, transformation, and transduction [18]. This makes biofilms hotspots for the dissemination of antibiotic resistance genes, accelerating the development of multidrug-resistant strains [18].
Advanced Methodologies for Biofilm Research
Image Cytometry with BiofilmQ
For the quantification and visualization of biofilm-internal properties in three-dimensional space and time, BiofilmQ serves as a comprehensive image cytometry software tool [12]. It is designed for automated, high-throughput analysis of 3D fluorescence images from a wide variety of microbial communities [12].
Protocol: 3D Image Analysis Using BiofilmQ
- Image Acquisition & Segmentation: Acquire 3D fluorescence images (e.g., via CLSM). BiofilmQ requires identification of the biofilm's biovolume. This can be achieved using:
- Automatic segmentation (e.g., Otsu, Ridler-Calvard algorithms).
- Semi-manual thresholding with visual feedback.
- Import of pre-segmented images from other tools (e.g., U-Net convolutional neural networks) [12].
- Image Cytometry: If single-cell segmentation is not feasible, BiofilmQ dissects the biofilm biovolume into a cubical grid. Each cube is treated as a pseudo-object for analysis [12].
- Parameter Quantification: For each cube (or custom-segmented object), BiofilmQ calculates numerous cytometric properties (e.g., fluorescence intensity, distance to biofilm surface, local biomass density). It also computes hundreds of global parameters for the whole biofilm (e.g., volume, mean thickness, surface area, roughness) [12].
- Data Analysis and Gating: Analogous to flow cytometry, apply gates/filters to the cube-based data to analyze specific subpopulations (e.g., cells in the core vs. shell of the biofilm) [12] [19].
- Data Visualization: Use the visualization tab to create publication-quality figures, including histograms, 2D/4D scatter plots, kymographs, and 3D heatmaps [19].
Quantitative Measurement of Biofilm Activity
Planar O₂ Optodes provide a non-destructive method for quantifying biological activity and spatial heterogeneity in biofilms. This technique is particularly useful in studying biofouling in membrane filtration systems but is applicable to other substrates [20].
Protocol: Measuring O₂ Consumption Rates with Planar Optodes
- Setup Integration: Integrate a planar O₂ optode—a transparent foil coated with an O₂-sensitive luminescent dye—into the experimental system (e.g., a membrane fouling simulator or flow cell) [20].
- Image Acquisition: Use a luminescence lifetime imaging system to capture high-resolution, two-dimensional maps of O₂ distribution across the optode surface over time [20].
- Rate Calculation: Quantify the O₂ consumption rate by monitoring the temporal decline of O₂ concentration in the system after briefly stopping the flow, or by analyzing the steady-state O₂ gradients that form within the biofilm [20].
- Data Correlation: Correlate the spatial maps of O₂ concentration and consumption rates with concurrent measurements, such as pressure drop increases and flow distribution images, to link biofilm activity directly to its functional impact [20].
Experimental Design for CLSM Time-Lapse Imaging
When designing CLSM time-lapse experiments to study early biofilm formation or antimicrobial treatment effects, careful consideration of variability is key [21].
Protocol: Optimizing CLSM Experimental Design
- Pilot Study: Conduct initial pilot experiments to quantify the inherent variability in the system. Key factors include bacterial growth phase (lag vs. exponential) and the efficacy of the antimicrobial treatment being studied [21].
- Determine Variance Components: Analyze pilot data to determine the variability arising from:
- Independent experiments (biological replicates).
- Different fields of view (FOV) within one experiment.
- Temporal resolution (frame capture rate) [21].
- Power Analysis: Use the variance components from the pilot study in an experimental design assessment tool (e.g., a custom spreadsheet) to predict the statistical power of different experimental designs [21].
- Final Design: Choose a design that balances statistical confidence with practical constraints, specifying:
- The number of independent experiments.
- The number of FOVs per experiment.
- The optimal frame capture rate per hour to avoid phototoxicity and data overload while capturing critical dynamics [21].
The Scientist's Toolkit: Key Research Reagents and Materials
Table 3: Essential Research Reagents and Materials for Biofilm Studies
| Reagent/Material | Primary Function/Application | Key Characteristics and Considerations |
|---|---|---|
| BiofilmQ Software [12] | 3D image cytometry, analysis, and visualization of biofilm internal properties and global parameters. | Handles images from micro- to macro-colonies; requires prior biofilm biovolume segmentation; includes batch processing and data gating. |
| Planar O₂ Optodes [20] | Non-destructive, spatially resolved measurement of O₂ concentration and consumption rates as a proxy for metabolic activity. | Provides both structural and quantitative activity data; can be correlated with other imaging techniques like MRI. |
| Confocal Laser Scanning Microscope (CLSM) [21] | Non-invasive, real-time 3D imaging of hydrated, intact biofilms. | Enables visualization of spatial organization, gene expression localization (with reporters), and biocide action over time. |
| Solid-State NMR (ssNMR) [17] | Non-destructive, quantitative in-situ characterization of biofilm composition and molecular dynamics. | Provides detailed information on abundance and mobility of specific matrix components (e.g., proteins, polysaccharides) over time. |
| 13C-labeled Glycerol [17] | Isotopic labeling of carbon sources for tracking metabolic incorporation into biofilm components via ssNMR. | Allows for precise quantitative analysis of the temporal production and degradation of specific matrix molecules. |
| Membrane Fouling Simulator (MFS) [20] | Laboratory-scale system for controlled studies of biofilm formation (biofouling) under conditions mimicking industrial settings. | Allows for simultaneous monitoring of operational parameters (e.g., pressure drop) and biofilm activity (e.g., via optodes). |
The dynamic biofilm lifecycle, from attachment to dispersion, is a highly regulated process that culminates in a resilient, structured community. This resilience is fundamentally rooted in the biofilm's EPS matrix, which acts as a primary barrier to antibiotic penetration and fosters an environment conducive to physiological tolerance and genetic resistance. Tackling the challenge of biofilm-associated infections, particularly in the context of multidrug resistance, requires a multifaceted approach. Promising strategies include enzymatic matrix disruption (e.g., Dispersin B, DNase I), quorum sensing inhibition, phage-antibiotic synergistic therapies, and nanoparticle-mediated drug delivery [18]. Overcoming this challenge demands a deep understanding of biofilm biology, supported by advanced quantitative techniques like those detailed in this review, to inform the development of next-generation anti-biofilm therapeutics.
The escalating global health crisis of antimicrobial resistance (AMR) is profoundly driven by the ability of bacterial pathogens to form biofilms. These complex, matrix-encased communities are a hallmark of chronic and recurrent infections, providing resident bacteria with formidable protection against antibiotics and host immune defenses [2] [16]. The ESKAPE pathogens—an acronym for Enterococcus faecium, Staphylococcus aureus, Klebsiella pneumoniae, Acinetobacter baumannii, Pseudomonas aeruginosa, and Enterobacter species—exemplify this challenge, as they represent the leading causes of nosocomial infections that effectively "escape" the action of conventional antimicrobial therapies [22] [23]. The extracellular polymeric substance (EPS) matrix is the central architectural component of biofilms, acting as a physical and functional barrier that limits antibiotic penetration, inactivates antimicrobial molecules, and fosters a heterogeneous microbial physiology conducive to tolerance [2] [24]. Among the ESKAPE pathogens, P. aeruginosa has emerged as a paradigmatic model organism for biofilm research due to its extensively studied and versatile matrix machinery, sophisticated regulatory networks, and its role as a primary agent in chronic lung infections, particularly in cystic fibrosis patients, and in wounds and medical device-related infections [24] [23]. This whitepaper delineates the key matrix producers within the ESKAPE cohort, utilizes P. aeruginosa as a model to elucidate the fundamental principles of biofilm-mediated resistance, and synthesizes contemporary experimental methodologies and emerging therapeutic strategies aimed at mitigating the biofilm barrier to antibiotic penetration.
Comparative Analysis of Biofilm Formation and Antimicrobial Resistance in ESKAPE Pathogens
The ESKAPE pathogens demonstrate significant variability in their propensity to form biofilms, the composition of their extracellular matrices, and their associated antimicrobial resistance profiles. A recent comparative analysis of clinical isolates provides critical quantitative insights into these differences, underscoring the unique threat posed by each member [22].
Table 1: Comparative Biofilm Formation and Key Resistance Traits in ESKAPE Pathogens
| Pathogen | Gram Stain | Prevalence of Biofilm Formers | Strong Biofilm Producers | Key Resistance Traits | Notable Resistance Genes |
|---|---|---|---|---|---|
| E. faecium | Positive | High | Moderate | High-level MDR (90%), Vancomycin Resistance | vanB |
| S. aureus | Positive | High | Moderate | Methicillin Resistance (MRSA - 46.7%) | mecA |
| K. pneumoniae | Negative | High | High | Carbapenem Resistance (45.71%), Colistin Resistance (42.86%), ESBL | NDM, OXA-48-like |
| A. baumannii | Negative | High | High | Carbapenem Resistance (74.29%), MDR | OXA-type carbapenemases |
| P. aeruginosa | Negative | High | Moderate | Carbapenem Resistance (Lower than A. baumannii & K. pneumoniae), Intrinsic MDR | AmpC, Metallo-β-lactamases (MBLs) |
The data reveals that biofilm formation is a ubiquitous capability among ESKAPE pathogens, with a significant majority (88.5%) of clinical isolates forming biofilms, and 15.8% characterized as strong producers [22]. A particularly noteworthy finding is the correlation between biofilm formation and resistance to critical antibiotic classes, including carbapenems, cephalosporins, and piperacillin/tazobactam, suggesting a synergistic role of biofilms in disseminating and entrenching resistance [22]. The high rates of multi-drug resistance (MDR), especially in E. faecium (90%) and A. baumannii, coupled with significant carbapenem resistance in Gram-negative members, highlight the therapeutic dead ends often encountered when treating biofilm-associated infections [22].
3Pseudomonas aeruginosa: A Model for Biofilm Matrix Complexity and Antibiotic Recalcitrance
P. aeruginosa serves as an archetype for understanding biofilm biology due to its genetic tractability and the well-defined composition of its matrix, which primarily consists of the exopolysaccharides Psl, Pel, and alginate, extracellular DNA (eDNA), and proteins [25] [24] [26]. The matrix is not a mere physical barrier; it is a dynamic functional compartment that actively contributes to tolerance and resistance through multiple mechanisms.
Key Exopolysaccharides and Matrix Proteins
- Psl (Polysaccharide Synthesis Locus): A mannose-, rhamnose-, and glucose-rich polysaccharide that provides structural scaffolding for the biofilm. Psl plays a critical role in cell-surface and cell-cell adhesion during initial biofilm development [26]. Recent research has identified that the lectin LecB binds specifically to the branched mannose residues of Psl, stabilizing the biofilm matrix and enhancing cell and EPS retention [26].
- Pel (Polysaccharide Encapsulation Locus): A positively charged, N-acetyl glucosamine (GlcNAc)- and N-acetyl galactosamine (GalNAc)-rich polysaccharide that interacts with eDNA, contributing to matrix integrity and resistance to aminoglycosides [2] [26].
- Alginate: A hallmark of mucoid P. aeruginosa variants common in chronic cystic fibrosis lung infections. Alginate forms a viscous capsule that inhibits phagocytosis and scavenges reactive oxygen species (ROS), providing protection against both antibiotics and the host immune response [25] [24].
- LecB: This soluble lectin, while involved in host attachment, is also a bona fide matrix component. Its interaction with Psl represents a protein-carbohydrate interaction that is crucial for maintaining the structural stability of the biofilm [26].
- Extracellular DNA (eDNA): A universal matrix component that contributes to biofilm integrity and chelates cationic antibiotics like aminoglycosides and colistin, significantly reducing their effective concentration within the biofilm [2] [24].
Mechanisms of Antibiotic Tolerance and Resistance in Biofilms
The biofilm mode of growth confers tolerance through a multifaceted interplay of physical, physiological, and adaptive mechanisms, with P. aeruginosa exhibiting a particularly broad arsenal [24].
Diagram: Mechanisms of Biofilm-Mediated Antibiotic Resistance in P. aeruginosa
The diagram above summarizes the core mechanisms, which include:
- Physical Restriction and Inactivation: The EPS matrix acts as a diffusion barrier, slowing antibiotic penetration. Furthermore, ionic interactions between matrix components (e.g., anionic eDNA and alginate) and cationic antibiotics (e.g., tobramycin, colistin) lead to sequestration and neutralization [2] [24]. Enzymes like AmpC β-lactamase can be concentrated in the matrix, inactivating β-lactam antibiotics before they reach their cellular targets [24].
- Physiological Heterogeneity: Gradients of nutrients and oxygen within the biofilm create zones of metabolically inactive or slow-growing bacteria. Since many antibiotics target active cellular processes, these dormant cells exhibit profound tolerance and can act as "persisters," capable of re-populating the biofilm after antibiotic treatment ceases [2] [24].
- Biofilm-Specific Adaptive Responses: The biofilm lifestyle triggers the expression of specific genes. The transcriptional regulator BrlR upregulates efflux pumps (e.g., MexAB-OprM, MexEF-OprN), directly contributing to multidrug resistance [24]. The gene ndvB, involved in the synthesis of periplasmic glucans, is also upregulated in biofilms and can sequester antibiotics like aminoglycosides, preventing them from reaching their targets [24].
Experimental Methods for Analyzing Biofilm Matrix and Antibiotic Penetration
A robust methodological framework is essential for dissecting biofilm matrix composition and evaluating the efficacy of antimicrobial agents. The following section details key protocols cited in contemporary literature.
Microtiter Plate Biofilm Formation Assay
This standard method quantifies total biofilm biomass and is ideal for high-throughput screening [22].
- Procedure:
- Inoculation: Dilute an overnight bacterial culture to ~1×10^6 CFU/mL in fresh, appropriate medium. Dispense 200 µL per well into a sterile 96-well flat-bottom polystyrene microtiter plate. Include negative control wells with medium only.
- Incubation: Incubate the plate statically for 24-48 hours at the optimal growth temperature for the organism (e.g., 37°C for pathogens).
- Washing: Carefully remove the planktonic culture by inverting and flicking the plate. Gently wash the adhered biofilm twice with 200-300 µL of phosphate-buffered saline (PBS) to remove non-adherent cells.
- Fixation and Staining: Fix the biofilm with 200 µL of 99% methanol for 15 minutes. Empty the plate and allow it to air dry. Subsequently, stain the biofilm with 200 µL of 0.1% (w/v) crystal violet solution for 5-15 minutes.
- Destaining and Quantification: Rinse the plate thoroughly under running tap water to remove excess stain. After air drying, add 200 µL of 33% glacial acetic acid or 95% ethanol to destain and solubilize the crystal violet. Transfer 125 µL of the solubilized dye to a new microtiter plate.
- Measurement: Measure the optical density (OD) at 570-600 nm using a microplate reader. The OD is proportional to the biofilm biomass attached to the well surface.
Modified Carbapenem Inactivation Method (mCIM and eCIM) for Carbapenemase Detection
This phenotypic assay is critical for identifying carbapenemase-producing Gram-negative isolates, a key resistance trait in ESKAPE pathogens like K. pneumoniae and A. baumannii [22].
- Principle: The test organism is incubated with a meropenem disk. If the organism produces a carbapenemase, the enzyme will inactivate the meropenem. This is detected by a reduction in the zone of inhibition of an indicator strain.
- mCIM Procedure:
- Preparation: Create a 1-µL loop of the test organism from an overnight agar plate and emulsify it thoroughly in 2 mL of tryptic soy broth (TSB).
- Incubation with Antibiotic: Add a 10-µg meropenem disk to the broth. Incubate the suspension at 35°C ± 2°C for 4 hours ± 15 minutes.
- Testing Inactivation: After incubation, remove the meropenem disk and place it on a Mueller-Hinton agar plate that has been inoculated with a 0.5 McFarland standard of a susceptible E. coli indicator strain (e.g., ATCC 25922).
- Interpretation: Incubate the plate for 18-24 hours at 35°C. A zone diameter of ≤15 mm (or 6-15 mm with a clump of colonies within the zone) indicates a positive result for carbapenemase production. A zone diameter of ≥19 mm indicates a negative result.
- eCIM Procedure: The eCIM test is performed in parallel. EDTA, an inhibitor of Metallo-β-lactamases (MBLs), is added to a separate broth suspension of the test organism. An increase in the zone diameter of ≥5 mm for the eCIM test compared to the mCIM test confirms the production of an MBL [22].
PCR for Detection of Biofilm-Associated and Resistance Genes
Polymerase Chain Reaction (PCR) is a fundamental molecular technique for identifying the genetic determinants of biofilm formation and antibiotic resistance [22].
- Protocol for Screening Biofilm-Forming Genes:
- DNA Extraction: Purify genomic DNA from bacterial cultures using a commercial kit or standard enzymatic (lysozyme) and chemical (SDS) lysis followed by phenol-chloroform extraction and ethanol precipitation.
- PCR Reaction Setup: Prepare a 25-µL reaction mixture containing:
- 1X PCR buffer (with MgCl₂)
- 200 µM of each dNTP
- 0.2-0.5 µM of each forward and reverse primer (designed for target genes, e.g., pslA, pelA, algD for P. aeruginosa; icaA and icaD for S. aureus)
- 1.0-1.5 U of thermostable DNA polymerase (e.g., Taq polymerase)
- 50-100 ng of template DNA
- Thermal Cycling: Amplify the target DNA in a thermal cycler using a standard program:
- Initial Denaturation: 95°C for 5 minutes.
- Amplification (30-35 cycles):
- Denaturation: 95°C for 30 seconds.
- Annealing: 55-65°C (primer-specific) for 30 seconds.
- Extension: 72°C for 1 minute per kb of amplicon length.
- Final Extension: 72°C for 7 minutes.
- Analysis: Analyze the PCR products by agarose gel electrophoresis (1.5-2.0% gel), stain with ethidium bromide or a safer alternative, and visualize under UV light to confirm the presence of an amplicon of the expected size.
Emerging Strategies to Overcome Biofilm-Mediated Resistance
The profound resistance of biofilms to conventional antibiotics has necessitated the development of novel therapeutic approaches that target the biofilm structure itself.
Diagram: Emerging Anti-Biofilm Therapeutic Strategies
A highly promising strategy involves the disruption of the biofilm matrix to release resident bacteria, which subsequently enter a transient state of heightened antibiotic susceptibility. A groundbreaking approach utilizes antibodies targeting DNABII proteins (HU and IHF), which serve as structural linchpins in the biofilm matrix by binding to and stabilizing eDNA [27]. Incubation of biofilms with these antibodies causes a rapid collapse of the matrix structure, releasing "newly released" (NRel) bacteria. These NRel bacteria exhibit significantly increased sensitivity to killing by traditional antibiotics—even at sub-MIC concentrations—that were ineffective against the biofilm-embedded population [27]. This combinatorial strategy of a biofilm-disrupting agent (e.g., a humanized monoclonal antibody like HuTipMab) co-delivered with a standard antibiotic represents a paradigm shift in treating chronic, biofilm-mediated infections [27].
Other emerging strategies include the use of glycoside hydrolases to degrade polysaccharide matrix components, quorum sensing inhibitors to disrupt bacterial communication, and lectin inhibitors (e.g., glycomimetics that block LecB-Psl interactions) to destabilize the biofilm architecture [26] [16] [23].
The Scientist's Toolkit: Key Research Reagents and Materials
Table 2: Essential Research Reagents for Biofilm and Antibiotic Resistance Studies
| Reagent/Material | Function/Application | Example Use Case |
|---|---|---|
| Crystal Violet | A basic dye that binds to negatively charged surface molecules and polysaccharides in the biofilm matrix. | Staining and semi-quantification of total biofilm biomass in microtiter plate assays [22]. |
| Meropenem Disks | A carbapenem antibiotic. Serves as the substrate for detecting carbapenemase enzyme activity. | Used as the key reagent in the mCIM and eCIM tests for phenotypic detection of carbapenemase production [22]. |
| Anti-DNABII Antibodies | Monoclonal or polyclonal antibodies that target the DNABII proteins (HU/IHF). Function as a biofilm-disrupting agent. | Experimental disruption of biofilms from diverse bacterial genera to induce NRel bacteria for subsequent antibiotic killing studies [27]. |
| PCR Primers (e.g., for psl, pel, mecA, vanB) | Short, single-stranded DNA fragments designed to flank a specific gene sequence. Enable targeted amplification for genetic screening. | Detection of biofilm-forming genes (e.g., pslA) or antibiotic resistance genes (e.g., mecA for MRSA) in bacterial isolates via conventional or quantitative PCR [22]. |
| LecB-FITC (Fluorescein Isothiocyanate) | Fluorescently labeled lectin that binds specifically to mannose and fucose residues. | Visualization and quantification of LecB binding to its polysaccharide ligand Psl in the biofilm matrix using fluorophore-linked lectin assays (FLLA) [26]. |
| Tryptic Soy Broth (TSB) | A rich, general-purpose nutrient medium that supports the growth of a wide variety of fastidious and non-fastidious organisms. | Standard liquid medium for growing planktonic cultures and for promoting robust biofilm formation in in vitro assays [22]. |
The ESKAPE pathogens, with Pseudomonas aeruginosa as a preeminent model, demonstrate that the biofilm matrix is a central organizer of antimicrobial recalcitrance. The synergistic interplay of physical barrier function, physiological heterogeneity, and biofilm-specific adaptive responses creates a formidable defense system that renders traditional monotherapies largely ineffective. The quantitative data and mechanistic insights consolidated in this whitepaper underscore the critical need to shift the therapeutic paradigm from simply killing bacteria to disrupting their communal architecture. The experimental methodologies detailed herein provide a foundational toolkit for ongoing research, while the emergence of innovative strategies, particularly matrix-disrupting agents like anti-DNABII antibodies used in combination with antibiotics, offers a promising path forward. Future research must continue to decode the intricate biology of biofilm matrices, validate these novel combinatorial approaches in clinical settings, and accelerate the development of next-generation therapeutics capable of penetrating and dismantling these bastions of bacterial resistance.
The extracellular polymeric substance (EPS) matrix of biofilms has traditionally been viewed as a physical barrier that restricts antibiotic penetration. However, emerging research reveals that matrix components serve sophisticated functional roles that extend far beyond structural support. The biofilm matrix represents a dynamic, functionally active compartment that actively contributes to antimicrobial resistance through molecular interactions, enzymatic degradation, and physiological regulation of embedded microbial communities [16] [2]. This paradigm shift in understanding matrix functionality is critical for developing effective strategies against biofilm-associated infections, which account for approximately 65% of all microbial infections and demonstrate up to 1000-fold greater antibiotic tolerance compared to their planktonic counterparts [28].
The matrix is composed of a complex mixture of polysaccharides, proteins, extracellular DNA (eDNA), lipids, and other biopolymers that vary depending on microbial species and environmental conditions [2]. Rather than serving merely as a passive scaffold, these components form a chemically active interface that modulates antibiotic penetration, inactivates antimicrobial agents, facilitates intercellular communication, and promotes genetic exchange. This review synthesizes current understanding of the functional roles of matrix components, with particular emphasis on mechanisms that contribute to antibiotic penetration resistance, to inform the development of next-generation anti-biofilm therapeutics.
Multifunctional Roles of Major Matrix Components
Extracellular DNA (eDNA): A Polyfunctional Virulence Factor
eDNA serves critical functions beyond structural integrity, including cation chelation, antibiotic binding, and facilitation of horizontal gene transfer. The phosphodiester backbone of eDNA confers a net negative charge that enables electrostatic interactions with cationic antimicrobial peptides (AMPs) and aminoglycoside antibiotics [2]. Studies demonstrate that eDNA can bind tobramycin, significantly reducing its effective concentration within deeper biofilm regions [2]. In Pseudomonas aeruginosa biofilms, eDNA works synergistically with host-derived DNA in cystic fibrosis lungs to create a physical shield that protects bacterial communities from both antibiotics and immune cells [2].
Table 1: Functional Roles of eDNA in Biofilm Matrix
| Function | Mechanism | Impact on Resistance | Experimental Evidence |
|---|---|---|---|
| Antibiotic Binding | Electrostatic interactions with cationic antibiotics | Reduced antibiotic penetration & efficacy | Fluorescence quenching assays show tobramycin-eDNA complex formation [2] |
| Cation Chelation | Binding of Mg²⁺ and Ca²⁺ ions | Activation of cationic antimicrobial peptide resistance pathways | Induces pmr operon in P. aeruginosa, increasing lipid A modification [2] |
| Genetic Material | Horizontal gene transfer substrate | Dissemination of resistance genes | Transformation efficiency increases 10-1000x in biofilms vs. planktonic cells [18] |
| Neutrophil Protection | Physical barrier formation | Protection from neutrophil extracellular traps (NETs) | NET-associated host DNA complements bacterial eDNA shielding [2] |
Exopolysaccharides: Architecturally Active Polymers
Exopolysaccharides constitute the volumetric majority of most biofilm matrices and serve multiple functional roles beyond scaffolding. These polymers create a highly hydrated environment that restricts antibiotic diffusion through molecular sieving and binding interactions. Specifically, the negatively charged groups on alginate (in P. aeruginosa) and poly-N-acetylglucosamine (PNAG) in staphylococcal biofilms can bind positively charged aminoglycosides, effectively sequestering them before they reach cellular targets [16] [28]. The viscous polysaccharide network also establishes chemical gradients that generate heterogeneous metabolic activity, contributing to persister cell formation and phenotypic tolerance [18].
Matrix Proteins: Enzymatic Defense Systems
Biofilm matrices contain diverse protein components that actively contribute to resistance mechanisms. Enzymatic resistance factors such as β-lactamases can be retained within the matrix, creating a front-line defense system that inactivates antibiotics before they penetrate to cellular targets [29]. Pseudomonas aeruginosa biofilms, for instance, release β-lactamases into the matrix that hydrolyze penicillins and cephalosporins, with catalytic efficiency (kcat/Km) reaching up to 10⁶ M⁻¹s⁻¹ for enzymes like TEM-52 and CTX-M-15 [29]. Other matrix proteins function as structural elements that bind eDNA and polysaccharides, while some actively modify the matrix environment to maintain conditions favorable for bacterial survival.
Advanced Experimental Approaches for Investigating Matrix Functionality
Methodologies for Assessing Antibiotic-Matrix Interactions
Understanding the functional roles of matrix components requires sophisticated experimental approaches that quantify interactions between antibiotics and specific matrix constituents:
Fluorescent Probe Binding Assays: This technique utilizes fluorescence-labeled antibiotics or matrix components to quantify binding interactions. When tobramycin conjugated with FITC binds to eDNA, fluorescence quenching occurs, allowing calculation of binding constants through Stern-Volmer analysis [2]. The protocol involves: (1) preparing biofilm matrix extracts or purified matrix components; (2) adding serial dilutions of fluorescently-labeled antibiotics; (3) measuring fluorescence intensity changes using a plate reader; (4) calculating binding constants from quenching curves.
Diffusion Chamber Systems: These systems measure antibiotic penetration rates through intact biofilms using a two-compartment model separated by a biofilm-grown membrane. The methodology includes: (1) growing biofilms on permeable membranes; (2) placing membrane between antibiotic-containing and antibiotic-free chambers; (3) sampling from the antibiotic-free chamber at timed intervals; (4) quantifying antibiotic concentration via HPLC or bioassay; (5) calculating diffusion coefficients using Fick's law [28].
Enzymatic Activity Assays in Biofilm Supernatants: These assays detect and quantify antibiotic-degrading enzymes within the matrix environment. The protocol involves: (1) collecting biofilm supernatants and concentrated matrix extracts; (2) incubating with specific antibiotic substrates; (3) measuring substrate degradation via spectrophotometry or HPLC; (4) determining enzyme kinetics (Km, Vmax) under conditions mimicking the biofilm microenvironment [29].
Genetic Approaches for Elucidating Matrix Function
Genetic techniques enable researchers to dissect the contribution of specific matrix components to antibiotic resistance:
Targeted Gene Knockout with CRISPR-Cas9: This approach creates isogenic mutants lacking specific matrix components to assess their functional contributions. The methodology includes: (1) designing gRNAs targeting genes of interest (e.g., pelA, pslG, algD for polysaccharide synthesis); (2) preparing CRISPR-Cas9 ribonucleoprotein complexes; (3) delivering complexes via conjugation or electroporation; (4) verifying gene deletion via PCR and sequencing; (5) comparing antibiotic susceptibility between mutant and wild-type biofilms using minimum biofilm eradication concentration (MBEC) assays [30].
Gene Expression Profiling in Biofilm Subregions: Spatial mapping of gene expression within biofilms reveals compartmentalized functional specialization. The protocol involves: (1) growing biofilms under controlled conditions; (2) cryosectioning or laser capture microdissection to isolate specific biofilm regions; (3) RNA extraction and reverse transcription; (4) quantifying expression of matrix-related genes via qRT-PCR or RNA-seq; (5) correlating expression patterns with functional properties of different biofilm zones [2].
Diagram 1: Multifunctional roles of eDNA in antibiotic resistance. The diagram illustrates how extracellular DNA (eDNA) contributes to resistance through charge-based antibiotic binding, horizontal gene transfer, cation chelation triggering adaptive responses, and quorum sensing activation in biofilms.
Quantitative Analysis of Matrix-Mediated Resistance Mechanisms
Table 2: Antibiotic Penetration Parameters Through Biofilm Matrix Components
| Antibiotic Class | Specific Antibiotic | Matrix Component | Reduction in Effective Concentration | Primary Mechanism | Experimental System |
|---|---|---|---|---|---|
| Aminoglycosides | Tobramycin | eDNA | 60-80% | Charge-based sequestration | P. aeruginosa flow cell biofilm [2] |
| β-lactams | Ampicillin | β-lactamase in matrix | 90-95% | Enzymatic degradation | S. aureus biofilm model [29] |
| Fluoroquinolones | Ciprofloxacin | Alginate polysaccharide | 40-60% | Diffusion limitation | P. aeruginosa alginate beads [28] |
| Glycopeptides | Vancomycin | PNAG polysaccharide | 50-70% | Molecular sieving | S. epidermidis biofilm [16] |
| Antimicrobial Peptides | Colistin | eDNA & polysaccharides | 70-90% | Charge neutralization | A. baumannii wound biofilm [29] |
The data presented in Table 2 demonstrates that different matrix components selectively impact various antibiotic classes through distinct mechanisms. The reduction in effective concentration represents the percentage decrease in antibiotic concentration reaching cellular targets compared to the applied external concentration.
The Scientist's Toolkit: Essential Research Reagents for Matrix Studies
Table 3: Key Research Reagents for Investigating Biofilm Matrix Functions
| Reagent/Category | Specific Examples | Functional Application | Key Considerations |
|---|---|---|---|
| Matrix-Degrading Enzymes | DNase I, Dispersin B, Alginate lyase | Selective degradation of specific matrix components (eDNA, PNAG, alginate) | Purity and activity validation; control for cellular toxicity [18] |
| Fluorescent Probes | FITC-labeled antibiotics, ConA, SYTO dyes | Visualization of antibiotic penetration and matrix architecture | Photostability; minimal perturbation of native structure [2] |
| Quorum Sensing Inhibitors | Synthetic AHL analogs, RNAIII-inhibiting peptides | Disruption of cell-to-cell communication and matrix regulation | Species-specificity; potential off-target effects [18] |
| Genomic Editing Tools | CRISPR-Cas9 systems, Transposon mutagenesis kits | Targeted manipulation of matrix biosynthesis genes | Delivery efficiency; pleiotropic effects assessment [30] |
| Nanoparticle Systems | Gold, silver, zinc oxide nanoparticles | Penetration enhancement; antimicrobial activity assessment | Size-controlled synthesis; biocompatibility testing [30] |
Signaling Pathways Regulating Matrix Production and Function
Matrix production is dynamically regulated through complex signaling networks that respond to environmental cues and population density. Understanding these regulatory pathways is essential for developing strategies to manipulate matrix composition and function.
Diagram 2: Regulatory pathways controlling biofilm matrix production. The diagram illustrates how quorum sensing (via autoinducers) and second messenger systems (like c-di-GMP) integrate population density and environmental stress signals to regulate matrix gene expression, creating a feedback loop that enhances antibiotic tolerance.
Quorum sensing (QS) systems represent the master regulatory circuitry controlling matrix production in response to population density. Gram-negative bacteria typically employ acyl-homoserine lactone (AHL) systems, while Gram-positive species use autoinducing peptide (AIP) signals [18]. These systems function through a cascade beginning with: (1) autoinducer synthesis and accumulation in the extracellular environment; (2) receptor binding at threshold concentrations; (3) activation of transcriptional regulators; (4) expression of matrix biosynthesis operons; and (5) increased production of polysaccharides, proteins, and eDNA release mechanisms.
The second messenger cyclic diguanylate monophosphate (c-di-GMP) serves as a central integrator of environmental signals for matrix regulation. High intracellular c-di-GMP levels promote matrix production and biofilm formation through allosteric activation of effector proteins that control the expression of matrix components [2]. The c-di-GMP network interfaces with QS systems to fine-tune matrix production in response to diverse environmental inputs, including nutrient availability, oxygen tension, and sub-inhibitory antibiotic concentrations.
The biofilm matrix represents a sophisticated functional compartment that actively contributes to antibiotic resistance through multiple mechanisms beyond mere physical obstruction. The integrated functions of eDNA, exopolysaccharides, and matrix proteins create a dynamic microenvironment that modulates antibiotic penetration, inactivates antimicrobial agents, facilitates genetic exchange, and regulates microbial physiology. Understanding these multifunctional roles is essential for developing effective strategies to combat biofilm-associated infections.
Future research directions should focus on spatial mapping of matrix component distribution and function within different biofilm regions, elucidating how matrix composition adapts in response to antimicrobial pressure, and developing targeted matrix-disrupting agents that can enhance conventional antibiotic efficacy. The integration of advanced techniques such as CRISPR-based editing with nanoparticle delivery systems holds particular promise for precisely manipulating matrix functions and overcoming treatment-resistant infections [30]. As our understanding of matrix functionality continues to evolve, so too will our ability to design innovative therapeutic approaches that address the multifactorial nature of biofilm-mediated resistance.
Tools of the Trade: Methodologies for Quantifying Penetration and Resistance
Biofilms are structured microbial communities encased in a self-produced extracellular polymeric substance (EPS) matrix that confers significant protection against antimicrobial agents [16] [2]. This matrix, composed of polysaccharides, proteins, nucleic acids, and lipids, creates a diffusion barrier that restricts antibiotic penetration and establishes heterogeneous microenvironments within the biofilm structure [18]. The inherent resistance of biofilms to conventional antibiotics represents a critical challenge in clinical settings, particularly for medical implant-associated infections and chronic conditions such as cystic fibrosis [2] [31].
Reaction-diffusion mathematical frameworks provide powerful tools for quantifying and predicting the complex spatiotemporal dynamics of antibiotic transport and efficacy within biofilms. These models bridge the gap between empirical observations and predictive understanding by explicitly coupling the physical process of antibiotic diffusion with biochemical reactions, including bacterial consumption, inactivation, and phenotypic adaptation [32] [31]. By simulating how antibiotics penetrate the biofilm matrix and interact with bacterial populations under varying conditions, these models offer invaluable insights for designing more effective treatment strategies against biofilm-associated infections.
Theoretical Foundations of Reaction-Diffusion in Biofilms
Core Principles and Governing Equations
Reaction-diffusion models conceptualize biofilms as porous structures where antimicrobial compounds move via molecular diffusion while simultaneously undergoing biochemical interactions. The fundamental governing equation for antibiotic transport within a biofilm can be expressed as:
∂C/∂t = ∇ · (D∇C) - R(C,S) - μC
Where C represents antibiotic concentration, D is the effective diffusion coefficient through the biofilm matrix, R(C,S) describes the reaction term accounting for antibiotic consumption or inactivation, and μ represents first-order degradation rate [32] [31]. The diffusion coefficient D is typically reduced within biofilms compared to aqueous environments due to the obstructive presence of EPS matrix components, with reported values ranging from 30% to 70% of their values in water [31].
The reaction term R(C,S) often follows Michaelis-Menten or Monod kinetics, reflecting concentration-dependent antibiotic uptake or inactivation by bacterial cells:
R(C,S) = Rmax · (C/(Ks + C)) · (S/(K_s + S))
Where Rmax represents the maximum consumption rate, Ks is the half-saturation constant, and S denotes nutrient concentration [32]. This formulation captures the nonlinear relationship between antibiotic concentration and bacterial consumption, which is particularly important for modeling concentration-dependent antibiotics like aminoglycosides.
Integration with Bacterial Population Dynamics
Advanced reaction-diffusion frameworks couple antibiotic transport with bacterial population dynamics, accounting for metabolic heterogeneity and phenotypic transitions within biofilms. A continuum approach typically models proliferative bacteria (Bp), persister cells (Bq), dead cells (B_d), and extracellular polymeric substances (EPS) through a system of partial differential equations:
∂Bp/∂t = ∇ · (DB ∇Bp) + μmax · (S/(KS + S)) · (C/(KC + C)) · Bp - kswitch C · Bp + krevert · B_q
∂Bq/∂t = ∇ · (DB ∇Bq) + kswitch C · Bp - krevert · B_q
∂EPS/∂t = ∇ · (DEPS ∇EPS) + kEPS · μmax · (S/(KS + S)) · Bp - kdegrad · EPS
Where DB and DEPS represent diffusion coefficients for biomass and EPS respectively, μmax is the maximum growth rate, kswitch and krevert are phenotypic switching rates, and kEPS is the EPS production rate [31]. This formulation enables the model to capture the emergence of nutrient-limited persister cells that exhibit elevated antibiotic tolerance, a key mechanism of biofilm resilience.
Table 1: Key Parameters in Biofilm Reaction-Diffusion Models
| Parameter | Symbol | Typical Range | Units | Biological Significance |
|---|---|---|---|---|
| Effective Diffusion Coefficient | D | 0.3-0.7 × D_water | cm²/s | Matrix restriction on molecular mobility |
| Maximum Growth Rate | μ_max | 0.1-0.8 | h⁻¹ | Bacterial division under ideal conditions |
| Half-Saturation Constant | K_S | 0.01-0.5 | mg/L | Nutrient affinity and utilization efficiency |
| Antibiotic Consumption Rate | R_max | 0.01-1.0 | mg/L·h | Metabolic uptake/inactivation capacity |
| Phenotypic Switching Rate | k_switch | 0.001-0.1 | h⁻¹ | Transition to dormant persister state |
| EPS Production Rate | k_EPS | 0.05-0.3 | - | Matrix synthesis per biomass growth |
Computational Implementation and Methodologies
Numerical Solution Approaches
Solving coupled reaction-diffusion equations for biofilm systems requires specialized numerical methods due to the moving boundary problem presented by biofilm growth and the stiffness introduced by multiple timescales. The finite-difference method (FDM) provides a straightforward approach for one-dimensional simulations, discretizing the spatial domain into uniform grids and approximating derivatives using difference quotients [32]. For more complex geometries, finite-element (FEM) or finite-volume methods (FVM) offer greater flexibility in handling irregular boundaries and heterogeneous material properties [31].
A typical implementation workflow includes:
- Spatial discretization of the computational domain
- Temporal discretization using implicit or semi-implicit schemes
- Iterative solution of the resulting algebraic system
- Application of boundary conditions (Dirichlet, Neumann, or Robin)
- Adaptive time-stepping to maintain numerical stability
Implementation verification through mass balance checks and convergence analysis represents a critical step in ensuring solution accuracy [33] [31].
Experimental Protocol for Model Parameterization
Validating reaction-diffusion models requires quantitative measurements of key parameters under controlled conditions. The following protocol outlines a comprehensive approach for parameter estimation:
Diffusion Coefficient Determination:
- Cultivate biofilms of specified thickness (100-500 μm) using a flow-cell reactor system
- Introduce fluorescently-labeled antibiotic analogs (e.g., fluorescent tobramycin) at known concentrations
- Monitor spatiotemporal fluorescence distribution using confocal laser scanning microscopy (CLSM)
- Calculate effective diffusion coefficients by fitting concentration profiles to Fick's second law using inverse modeling techniques
Antibiotic Consumption Kinetics:
- Establish planktonic cultures under nutrient conditions matching biofilm environments
- Expose cultures to antibiotic concentration series (0.1-100× MIC)
- Sample at regular intervals (0, 15, 30, 60, 120 min) for antibiotic quantification via HPLC-MS
- Determine Rmax and Ks by nonlinear regression of depletion curves
Phenotypic Switching Rates:
- Engineer reporter strains with fluorescent markers for persister-specific promoters
- Track single-cell fluorescence in microfluidic devices under antibiotic exposure
- Quantify transition probabilities between proliferative and persister states using Markov chain analysis
This experimental framework generates the quantitative inputs necessary for parameterizing and validating reaction-diffusion models of antibiotic penetration in biofilms [31] [34].
Advanced Modeling Frameworks and Applications
Integration with Machine Learning Approaches
Modern modeling frameworks increasingly combine reaction-diffusion principles with machine learning to enhance predictive accuracy, particularly for complex, multivariate biofilm systems. Recent research has demonstrated successful prediction of antibiotic susceptibility in Pseudomonas aeruginosa biofilms using machine learning models trained on analytical data including whole-genome sequencing (WGS), matrix-assisted laser desorption/ionization-time of flight mass spectrometry (MALDI-TOF MS), isothermal microcalorimetry (IMC), and multi-excitation Raman spectroscopy (MX-Raman) [34].
For predicting minimal inhibitory concentration (MIC) and biofilm prevention concentration (BPC) values, ordinal regression models achieve notable accuracy:
Table 2: Machine Learning Prediction Performance for Antibiotic Susceptibility
| Analytical Method | MIC Prediction Accuracy±1 | BPC Prediction Accuracy±1 | Key Predictors |
|---|---|---|---|
| MALDI-TOF MS | 97.83% | 73.91% | Proteomic fingerprints |
| Multi-excitation Raman | 89.13% | 80.43% | Biochemical composition |
| Whole-Genome Sequencing | 89.13% | 76.09% | Genetic mutations |
| Isothermal Microcalorimetry | 91.30% | 76.09% | Metabolic heat profiles |
These integrated approaches leverage the mechanistic understanding provided by reaction-diffusion frameworks while incorporating data-driven pattern recognition to address the complex heterogeneity of clinical biofilm isolates [34].
Membrane Carbonated Microalgal Biofilm Photobioreactor (MC-MBPBR) Model
A sophisticated application of reaction-diffusion modeling appears in the membrane carbonated microalgal biofilm photobioreactor (MC-MBPBR) system, which simulates counter-current diffusion of CO₂ and nutrients in membrane-attached biofilms. The governing equations for this system incorporate simultaneous diffusion and reaction of multiple substrates:
∂SCO₂/∂t = DCO₂ · (∂²SCO₂/∂x²) - (μmax/Y) · (SCO₂/(KCO₂ + SCO₂)) · (SN/(KN + SN)) · (SP/(KP + S_P)) · X
∂SN/∂t = DN · (∂²SN/∂x²) - (μmax/YN) · (SCO₂/(KCO₂ + SCO₂)) · (SN/(KN + SN)) · (SP/(KP + SP)) · X
∂SP/∂t = DP · (∂²SP/∂x²) - (μmax/YP) · (SCO₂/(KCO₂ + SCO₂)) · (SN/(KN + SN)) · (SP/(KP + SP)) · X
Where SCO₂, SN, and SP represent CO₂, nitrogen, and phosphorus concentrations respectively, Di denotes their diffusion coefficients, Y terms represent yield coefficients, and X is biomass concentration [32]. This multi-substrate approach more accurately captures the nutrient-dependent growth limitations that influence antibiotic efficacy in biofilms.
The Scientist's Toolkit: Essential Research Reagents and Materials
Table 3: Key Research Reagents for Biofilm Reaction-Diffusion Studies
| Reagent/Material | Function | Application Example | Technical Considerations |
|---|---|---|---|
| Synthetic Cystic Fibrosis Medium 2 (SCFM2) | Physiologically relevant biofilm growth medium | Culturing P. aeruginosa biofilms with in vivo-like phenotype [34] | Mimics nutrient composition of CF airway surface liquid |
| Fluorescent antibiotic conjugates (e.g., BODIPY-tobramycin) | Visualization of antibiotic penetration | Quantifying spatiotemporal distribution via CLSM | Must validate that labeling doesn't alter antibacterial activity |
| Microfluidic flow cells | Controlled hydrodynamic environment | Studying biofilm development under defined shear stress | Enables real-time microscopy during biofilm growth |
| Permeabilized cellulose membranes | Support for biofilm growth in MC-MBPBR systems | Studying counter-current diffusion in membrane-attached biofilms [32] | Porosity affects nutrient exchange and biofilm structure |
| Recombinant reporter strains (GFP, RFP) | Visualizing subpopulations and metabolic states | Tracking phenotypic switching in situ | Promoter selection critical for relevant expression patterns |
| DNase I & Dispersin B | Matrix-degrading enzymes | EPS disruption to enhance antibiotic penetration [18] | Enzyme specificity determines efficacy against matrix components |
| Customized ordinal regression algorithms | Machine learning prediction of susceptibility | Integrating multi-omics data for BPC prediction [34] | Requires training on comprehensive experimental datasets |
Model Validation and Corroboration with Experimental Data
Robust validation represents an essential yet often overlooked component of biofilm reaction-diffusion modeling. The TRACE framework (Transparent and Comprehensive Ecological modeling) outlines rigorous criteria for model evaluation, including problem formulation, model description, data evaluation, conceptual model evaluation, implementation verification, model output verification, model analysis, and model output corroboration [33]. Despite these guidelines, a systematic review of antimicrobial resistance transmission models found that only 39 of 170 studies adequately described model verification procedures, and fewer than 25% performed comprehensive output corroboration with external datasets [33].
Effective validation strategies for biofilm reaction-diffusion models include:
- Quantitative comparison with concentration profiles obtained through microsensor measurements or CLSM imaging of fluorescent antibiotics
- Sensitivity analysis to identify parameters with greatest influence on model predictions (e.g., diffusion coefficients, growth rates)
- Cross-validation using separate datasets for parameter estimation and model testing
- Prospective prediction of treatment outcomes in experimental systems not used during model development
Model validation should specifically test the prediction of critical biofilm characteristics such as optimal intervention timing coinciding with persister population peaks, which reaction-diffusion models have identified as key determinants of treatment success [31].
Reaction-diffusion frameworks provide mathematically rigorous foundations for predicting antibiotic penetration and efficacy in bacterial biofilms. By explicitly coupling transport limitations with biochemical reactions and phenotypic adaptations, these models illuminate the complex interplay between antibiotic properties, biofilm matrix composition, and bacterial responses that underlie treatment failure. The integration of these mechanistic models with machine learning approaches trained on multi-omics datasets represents a promising frontier for improving predictive accuracy and clinical relevance.
Future advancements in biofilm reaction-diffusion modeling will likely focus on incorporating additional layers of biological complexity, including multi-species interactions, immune system effects, and spatial heterogeneity at micron scales. Additionally, addressing current gaps in model validation through standardized benchmarking and external corroboration will be essential for translating theoretical predictions into clinically actionable insights. As these models continue to evolve, they will play an increasingly vital role in guiding the development of novel anti-biofilm strategies and optimizing treatment regimens for persistent biofilm-associated infections.
Experimental Techniques for Measuring Antibiotic Diffusion Kinetics
The efficacy of an antibiotic is fundamentally constrained by its ability to reach its cellular target at a sufficient concentration. This is particularly critical in the context of biofilm-associated infections, where the extracellular polymeric substance (EPS) matrix can severely hinder antibiotic penetration, leading to markedly elevated minimum inhibitory concentrations (MICs)—often 100-800 times greater than those required for planktonic cells [35]. Understanding and quantifying antibiotic diffusion kinetics is therefore essential for developing effective treatments against these recalcitrant infections. This guide synthesizes current methodologies for analyzing antibiotic movement through biofilms and other biological matrices, providing a technical resource for researchers engaged in the fight against antimicrobial resistance.
Established and Emerging Analytical Techniques
A range of techniques, from classical diffusion assays to advanced spectroscopic and computational methods, are employed to quantify antibiotic diffusion. The choice of method depends on the required resolution, the need for in-situ measurement, and whether quantitative or qualitative data is sufficient.
Table 1: Core Techniques for Measuring Antibiotic Diffusion Kinetics
| Technique | Principle | Spatial Resolution | Key Measurable Parameters | Primary Applications |
|---|---|---|---|---|
| Diffusion Cell Systems [36] | Measures solute flux across a biofilm membrane under a concentration gradient. | Bulk measurement (entire biofilm) | Diffusion coefficients, permeability coefficients, flux rates. | Studying antibiotic transport in counter-diffusion biofilms (e.g., MABR). |
| FRAP (Fluorescence Recovery After Photobleaching) | A region of fluorescently-tagged molecules is bleached; recovery via diffusion is monitored. | Microscopic (µm-scale) | Effective diffusion coefficient (D_eff), mobile/immobile fractions. | Quantifying mobility of labeled antibiotics within biofilm EPS in real-time. |
| Raman Spectroscopy [37] | Inelastic light scattering provides a molecular fingerprint based on vibrational modes. | Microscopic (µm-scale) | Molecular binding, complex formation, diffusion barriers. | Label-free analysis of antibiotic-matrix interactions; identification of binding. |
| Molecular Dynamics (MD) Simulation [38] | Computational simulation of atom-level interactions and trajectories over time. | Atomic (Ångstrom-scale) | Interaction energy, binding affinity, diffusion pathways, free energy. | Predicting antibiotic-organic matter interactions and penetration barriers. |
Diffusion Cell Assays
Principle and Workflow: Diffusion cells, such as Franz or Side-Bi-Side cells, are classical apparatuses used to study solute transport across a barrier. In biofilm research, a biofilm is typically grown or placed on a membrane that separates a donor compartment (containing the antibiotic solution) from a receptor compartment. The concentration of the antibiotic in the receptor compartment is measured over time, allowing for the calculation of key kinetic parameters [36].
Key Protocol Steps:
- Biofilm Preparation: Grow a standardized biofilm on a semi-permeable membrane support.
- Assembly: Mount the biofilm-membrane assembly between the donor and receptor chambers of the diffusion cell. The receptor chamber is often filled with a buffer like PBS to maintain sink conditions.
- Sampling: Introduce the antibiotic at a known concentration into the donor chamber. Periodically withdraw samples from the receptor chamber.
- Analysis: Quantify antibiotic concentration in the samples using HPLC, MS, or other analytical methods.
- Data Calculation: Plot the cumulative amount of drug permeated versus time. The steady-state flux (Jss) can be determined from the linear portion of the plot, and the apparent permeability coefficient (Papp) can be calculated using the formula:
Papp = (dQ/dt) / (A * C0), where dQ/dt is the flux, A is the diffusion area, and C0 is the initial donor concentration.
Fluorescence Recovery After Photobleaching (FRAP)
Principle and Workflow: FRAP is a powerful technique for measuring the two-dimensional lateral diffusion of fluorescent molecules within a defined region, such as a biofilm section.
Key Protocol Steps:
- Labeling: The antibiotic of interest is conjugated to a fluorescent tag (e.g., FITC, Rhodamine). It is critical to validate that the tagging does not alter the antibiotic's biological activity or diffusion properties.
- Bleaching: A high-intensity laser is used to permanently bleach the fluorophores in a small, defined region of the biofilm.
- Recovery: The recovery of fluorescence in the bleached area, due to the influx of unbleached, mobile molecules from the surrounding regions, is monitored with a low-intensity laser using confocal laser scanning microscopy (CLSM).
- Data Analysis: The fluorescence recovery curve is fitted to an appropriate diffusion model to calculate the effective diffusion coefficient (D_eff) and the mobile fraction of the molecules.
Spectroscopic Methods: Raman Spectroscopy
Principle and Workflow: Techniques like Raman spectroscopy and FTIR are label-free methods that can probe antibiotic-matrix interactions, which directly influence diffusion kinetics [37].
Key Protocol Steps:
- Sample Preparation: Prepare biofilm samples, potentially alongside control samples of the antibiotic and matrix components alone.
- Spectral Acquisition: Acquire spectra from the pure antibiotic, the biofilm matrix, and the biofilm after exposure to the antibiotic.
- Data Analysis: Identify spectral shifts, the appearance of new peaks, or the disappearance of existing peaks in the biofilm-antibiotic sample compared to the controls. These changes indicate molecular binding or complex formation. For instance, a shift in the peak corresponding to an amine group suggests that the antibiotic is interacting with a negatively charged component like eDNA in the matrix [2] [10].
Computational Modeling: Molecular Dynamics (MD) Simulation
Principle and Workflow: MD simulation provides atomic-level insight into the interactions that govern diffusion, complementing empirical data [38].
Key Protocol Steps:
- System Construction: Build all-atom or coarse-grained models of the antibiotic molecule and the major components of the biofilm EPS (e.g., proteins, polysaccharides, eDNA) based on experimental data or literature.
- Equilibration: Solvate the system in water and add ions to achieve physiological salinity. Energy-minimize and equilibrate the system under constant temperature and pressure.
- Production Run: Run the simulation for hundreds of nanoseconds to microseconds, tracking the position and energy of all atoms.
- Trajectory Analysis: Analyze the simulation trajectory to calculate:
- Interaction Energy: The strength of binding between the antibiotic and matrix molecules.
- Mean Squared Displacement (MSD): Used to compute the diffusion coefficient of the antibiotic within the matrix environment.
- Radial Distribution Function (g(r)): Reveals the preferred distances between atoms of the antibiotic and matrix, indicating binding sites.
The Scientist's Toolkit: Essential Research Reagents and Materials
Successful execution of these techniques requires a suite of specialized reagents and instruments.
Table 2: Key Research Reagent Solutions for Diffusion Kinetics Studies
| Item/Category | Function in Experiment | Specific Examples & Notes |
|---|---|---|
| Membrane Bioreactor Systems | Provides a controlled environment for growing structured biofilms with defined counter-diffusion characteristics for realistic diffusion studies [36]. | Membrane Aerated Biofilm Reactors (MABRs); allows separate control of electron donors and acceptors. |
| Fluorescent Tags/Probes | Labels antibiotics for direct visualization and quantification via microscopy techniques (e.g., FRAP, CLSM). | FITC, Rhodamine B, Cyanine dyes (Cy3, Cy5); must verify tagged antibiotic retains native activity. |
| Chromatography & Mass Spectrometry | Precisely quantifies antibiotic concentration in complex solutions from diffusion assays or extracted from biofilm layers. | High-Performance Liquid Chromatography (HPLC), Liquid Chromatography with tandem mass spectrometry (LC-MS/MS) [37]. |
| Biofilm Matrix Components | Used in model systems to study specific antibiotic-matrix interactions that impede diffusion. | Purified alginate (from P. aeruginosa), Poly-N-acetylglucosamine (PNAG), extracellular DNA (eDNA), proteins [10]. |
| Molecular Modeling Software | Enables atomic-level simulation of antibiotic diffusion and interaction with biofilm matrix components. | GROMACS, AMBER, NAMD; used for MD simulations to calculate interaction energies and pathways [38]. |
Conceptualizing Diffusion Resistance in Biofilms
The following diagram illustrates the multi-faceted mechanisms that collectively hinder antibiotic penetration in biofilms, integrating concepts from the experimental techniques described.
Diagram 1: Biofilm antibiotic diffusion resistance mechanisms. The diagram shows how an antibiotic faces sequential barriers including physical EPS blocking, molecular binding, active efflux, and heterogeneous metabolic zones leading to persistent cells, ultimately resulting in inadequate concentration at the target site.
Experimental Workflow for Comprehensive Analysis
A robust investigation of antibiotic diffusion kinetics often combines multiple techniques, moving from macroscopic observation to molecular-level insight. The following workflow outlines a integrated approach.
Diagram 2: Integrated workflow for diffusion kinetics. The process flows from defining the research question, to macroscopic screening with diffusion cells, spatial visualization with FRAP or Raman, mechanistic analysis with MD simulation, and finally data integration for a comprehensive model.
The challenge of antibiotic diffusion in biofilms is a multi-scale problem, requiring an integrated methodological approach. No single technique can fully elucidate the complex interplay of physical barriers, chemical interactions, and bacterial adaptations that define penetration resistance. The future of this field lies in the intelligent combination of these established and emerging technologies. Correlating bulk transport data from diffusion cells with high-resolution spatial mapping from FRAP and Raman, and validating these findings with predictive computational models from MD simulations, will provide the comprehensive understanding needed to develop novel strategies to disrupt the biofilm barrier and restore the efficacy of existing antibiotics.
The extracellular matrix of microbial biofilms is a highly complex scaffold, characterized by a multitude of structurally and chemically heterogeneous microenvironments [39]. This matrix provides mechanical stability to the biofilm and protects microorganisms from desiccation, while simultaneously acting as a formidable barrier against adverse chemical and biological influences, including antibiotics, antiseptics, and host immune defenses [39]. If the biofilm is a microbial city, then the matrix is its infrastructure [39]. The matrix's composition—an intricate network of polysaccharides, proteins, nucleic acids, and lipids—creates a diffusion-limiting environment that significantly reduces antibiotic penetration and efficacy, contributing to the up to 1000-fold increased resistance observed in biofilm-associated infections compared to their planktonic counterparts [40]. Understanding this architectural complexity is therefore paramount for developing effective therapeutic strategies against persistent biofilm-mediated infections. Advanced imaging technologies, particularly Confocal Laser Scanning Microscopy (CLSM), Scanning Electron Microscopy (SEM), and Transmission Electron Microscopy (TEM), provide researchers with the necessary tools to visualize, quantify, and ultimately disrupt this protective barrier.
Confocal Laser Scanning Microscopy (CLSM): Visualizing 3D Architecture in Real Time
Confocal Laser Scanning Microscopy has established itself as a cornerstone technique in biofilm research due to its capability for in situ, real-time visualization of fully hydrated, living specimens, thereby preserving the native three-dimensional structure of biofilms [39] [41]. CLSM operates by exciting fluorescence signals from different planes within the sample using laser light, and through a system of pinholes, it eliminates out-of-focus light, resulting in high-resolution optical sections that can be reconstructed into a 3D model of the entire biofilm [42].
Key Applications in Matrix and Antibiotic Penetration Research
The application of CLSM extends beyond mere structural observation to functional and quantitative analysis:
- Matrix Component Localization: Fluorescently labeled lectins (e.g., Con A, WGA) are widely employed to target and visualize specific sugar residues within the exp polysaccharide (EPS) matrix, revealing the heterogeneous distribution of matrix components [39].
- Viability and Metabolic Activity: Using pathogen-specific probes labeled with different fluorescent dyes, such as the LIVE/DEAD BacLight Bacterial Viability Kit (SYTO9/PI), CLSM can discriminate between live and dead bacterial cells and localize their spatial distribution within the biofilm architecture, a crucial metric for evaluating antimicrobial efficacy [41] [43] [44].
- Solute Diffusion and Antibiotic Penetration: Techniques like Fluorescence Recovery After Photobleaching (FRAP) allow researchers to measure the local diffusion coefficients of molecules within the biofilm matrix, providing critical data on the penetration barriers that antibiotics must overcome [39].
- Quantitative Structural Analysis: When combined with image analysis software, CLSM can extract quantitative parameters such as biovolume, thickness, roughness, and surface-to-volume ratio [39] [42]. These metrics are essential for conducting comparative studies on the effects of anti-biofilm treatments.
Experimental Protocol: CLSM for Biofilm Viability and Structure
A representative protocol for evaluating anti-biofilm treatments, as derived from recent studies, involves the following steps [43] [44]:
- Biofilm Growth: Grow biofilms under desired conditions (e.g., in flow cells, on glass-bottom dishes, or silicone tubes) for a specified period (commonly 24-72 hours).
- Treatment Application: Expose biofilms to the therapeutic agent (e.g., antibiotics, shockwaves, or antibiotic-loaded microbubbles).
- Staining: Gently rinse the biofilm with a buffer like phosphate-buffered saline (PBS) to remove non-adherent cells. Apply fluorescent stains:
- For viability: Stain with a mixture of SYTO9 (green, membrane-permeant, labels all cells) and propidium iodide (red, membrane-impermeant, labels dead cells with compromised membranes) and incubate for 15-20 minutes in darkness [43] [44].
- For matrix: Incubate with fluorescently conjugated lectins or other matrix-specific probes.
- Image Acquisition: Observe the biofilm using a CLSM system (e.g., Leica Stellaris 5). Acquire z-stack images through the entire biofilm depth with a suitable step size (e.g., 1 µm) to enable 3D reconstruction.
- Image Analysis: Utilize specialized software (e.g., ImageJ, COMSTAT2, daime, BiofilmQ) to quantify parameters like biofilm thickness, live/dead cell ratios, and biovolume [42].
Table 1: Key Image Analysis Software for CLSM Biofilm Data
| Software Name | User Interface | Key Capabilities | Key Limitations |
|---|---|---|---|
| COMSTAT2 [42] | ImageJ Plugin (GUI) | Quantifies biovolume, thickness distribution, roughness, surface area. | Unable to calculate surface-to-volume ratio. |
| BiofilmQ [42] | MATLAB-based (GUI) | Measures fluorescence, architectural, and spatial properties; data visualization. | Requires MATLAB license; needs high-spec computer. |
| daime [42] | Standalone (GUI) | Segmentation, noise reduction; can analyze conventional micrographs. | — |
| ImageJ/FIJI [42] | Open-source (GUI) | Highly flexible with numerous plugins for general image analysis. | Requires plugin installation for specialized biofilm metrics. |
Scanning Electron Microscopy (SEM): Revealing Ultrastructural Details
Scanning Electron Microscopy provides high-resolution, topographical images of biofilm surfaces, revealing the ultrastructural organization of cells and the extracellular matrix with unparalleled detail and a significant depth of field [41]. Conventional SEM requires samples to be fixed, dehydrated, and coated with a conductive material, which can introduce artifacts such as EPS collapse and overall biofilm shrinkage [41]. Despite this, its combined ability to image at a wide range of magnifications (20 to 30,000x) with high resolution (50 to 100 nm) makes it an invaluable tool, particularly for comparative analyses of biofilm morphology before and after treatment [41].
Advanced SEM Modalities for Enhanced Preservation
To overcome the limitations of conventional SEM preparation, several advanced modalities have been developed:
- Cryo-SEM: This technique involves rapid cryo-fixation of the hydrated biofilm, followed by examination under frozen conditions. It is widely recognized for providing the best preservation of the biofilm's native architecture, as it avoids the damaging dehydration steps of chemical fixation [41] [45].
- Environmental SEM (ESEM): ESEM allows for the observation of partially hydrated, uncoated biofilms under low-pressure and humid conditions, minimizing preparation artifacts and enabling the study of biofilms in a state closer to their natural environment [41].
- Variable Pressure SEM (VP-SEM): Similar to ESEM, VP-SEM operates at higher pressures, reducing the need for extensive conductive coating and thereby better preserving delicate structures [41].
Experimental Protocol: SEM for Biofilm Morphology
A standardized protocol for conventional SEM biofilm imaging is outlined below [45] [46]:
- Primary Fixation: Fix biofilm samples (grown on a relevant substrate, e.g., a glass coverslip) in a buffered 2.5% glutaraldehyde solution for a minimum of 2 hours at 4°C.
- Washing: Rinse the fixed samples gently but thoroughly with a buffer (e.g., PBS or cacodylate buffer) to remove excess fixative.
- Post-Fixation (Optional): To improve the preservation of certain matrix components and lipid structures, post-fix with 1% osmium tetroxide for 1-2 hours [45].
- Dehydration: Gradually dehydrate the sample using a graded ethanol series (e.g., 30%, 50%, 80%, 95%, 100%, 100%) to remove all water. A microwave processor can be used to accelerate this process [45].
- Drying: Critical Point Dry the samples using liquid CO₂. This technique avoids the surface tension forces associated with air drying, which can collapse delicate matrix structures.
- Mounting and Coating: Mount the dried samples on aluminum stubs using conductive adhesive tape and sputter-coat with a thin layer (e.g., 10-20 nm) of gold or gold/palladium to render the sample conductive.
- Imaging: Observe and acquire images using an SEM (e.g., Thermo Scientific Apreo S) at accelerating voltages typically between 5-15 kV [46].
Transmission Electron Microscopy (TEM): Nanoscale Insights into Matrix Organization
Transmission Electron Microscopy offers the highest resolution of the three techniques, capable of visualizing the nanoscale organization of the biofilm matrix and its intimate association with bacterial cells [45]. Unlike SEM, which provides surface topography, TEM transmits electrons through an ultra-thin section of the sample, yielding detailed information on the internal structure of cells and the fine fibrillar network of the EPS [45]. This makes TEM particularly powerful for studying microbe-mineral interactions, the presence of amyloid-like fibers, and the precise localization of matrix components at the nanometer scale.
Protocol Optimization for EPS Visualization
Sample preparation is critical for successful TEM imaging of biofilms. A comparative study of three protocols revealed key insights [45]:
- Cryofixation (Protocol 1): Using high-pressure freezing followed by freeze-substitution, this method provides the best overall preservation of cellular ultrastructure, minimizing the artifacts introduced by chemical fixation.
- Routine Chemical Fixation (Protocol 2): Involving primary fixation with glutaraldehyde and post-fixation with osmium tetroxide, this is a standard but less optimal method for EPS preservation.
- Enhanced Staining (Protocol 3): Chemical fixation followed by an extensive staining regimen including tannic acid, uranyl acetate, osmium tetroxide, and ruthenium red provided the best visualization of the extracellular polymeric substances (EPS), despite potential cellular artifacts. Ruthenium red is particularly crucial as it binds to and stabilizes acidic polysaccharides within the matrix [45].
Experimental Protocol: TEM with Enhanced EPS Staining
The following protocol, adapted from geomicrobiology studies, is optimized for EPS visualization [45]:
- Primary Fixation: Fix biofilm samples in a mixture of 2.5% glutaraldehyde and 0.15% ruthenium red in a 0.1 M buffer (e.g., cacodylate buffer) for 2 hours at room temperature.
- Washing: Wash the samples with 0.1 M buffer containing 0.15% ruthenium red.
- Secondary Fixation and Staining: Post-fix with a mixture of 1% osmium tetroxide and 0.15% ruthenium red in the same buffer for 2 hours at room temperature.
- Dehydration: Dehydrate the samples through a graded ethanol series.
- Embedding: Infiltrate and embed the sample in a resin, such as Spurr's or Epon, and polymerize at 60°C for 24-48 hours.
- Sectioning and Post-Staining: Use an ultramicrotome to cut ultrathin sections (60-90 nm). Mount sections on grids and post-stain with uranyl acetate and lead citrate to enhance contrast.
- Imaging: Observe grids using a TEM at accelerating voltages of 80-120 kV.
Integrated Workflow and Data Correlation
For a comprehensive understanding of biofilm matrix architecture and its role in antibiotic resistance, an integrated approach that correlates data from CLSM, SEM, and TEM is most powerful. The following workflow visualizes a typical integrated experimental design for evaluating an anti-biofilm treatment, synthesizing the protocols described in this guide.
(Correlative Imaging Workflow for Anti-biofilm Studies)
The Scientist's Toolkit: Essential Reagents and Materials
Successful imaging relies on a suite of specialized reagents and materials. The following table catalogs key solutions used in the protocols discussed.
Table 2: Research Reagent Solutions for Biofilm Imaging
| Reagent/Material | Function | Application Examples |
|---|---|---|
| Glutaraldehyde [45] [43] | Primary fixative that cross-links proteins, stabilizing the 3D structure of cells and matrix. | Used in initial fixation for both SEM and TEM sample preparation. |
| Osmium Tetroxide (OsO₄) [41] [45] | Secondary fixative that stabilizes lipids and acts as a heavy metal stain, providing electron density. | Post-fixation in TEM and some SEM protocols to enhance contrast and preserve membranes. |
| Ruthenium Red [45] | A polycationic dye that binds to and stabilizes acidic polysaccharides (e.g., in EPS). | Added to primary and secondary fixatives in TEM protocols specifically designed for EPS visualization. |
| Uranyl Acetate [45] | Heavy metal salt used as a stain to scatter electrons, enhancing contrast in TEM. | Used as a post-staining agent for ultrathin TEM sections. |
| SYTO9/Propidium Iodide [43] [44] | Fluorescent nucleic acid stains for differentiating live (green) and dead (red) bacterial cells. | Used in CLSM for viability assessment after antimicrobial treatment. |
| Fluorescent Lectins [39] | Carbohydrate-binding proteins conjugated to fluorophores to target specific sugar residues in EPS. | Used in CLSM to label and visualize the polysaccharide component of the biofilm matrix. |
| Tannic Acid [45] | A mordant that improves the binding of heavy metal stains, enhancing contrast for TEM. | Included in enhanced staining protocols for TEM to improve visualization of fine details. |
The strategic application of CLSM, SEM, and TEM provides a multi-scale, complementary toolkit for deconstructing the complex architecture of the biofilm matrix. CLSM offers unparalleled capability for the functional, 3D analysis of living biofilms, SEM reveals the topographical landscape of the biofilm surface, and TEM delivers nanoscale resolution of the matrix infrastructure. Together, these techniques are indispensable for elucidating the fundamental mechanisms of antibiotic penetration resistance. As these imaging technologies continue to advance—with improvements in cryo-techniques, super-resolution microscopy, and automated image analysis—they will undoubtedly uncover new vulnerabilities in the biofilm fortress, paving the way for novel therapeutic strategies to combat persistent biofilm-related infections.
In Vitro and In Vivo Models for Studying Biofilm-Associated Infections
Biofilm-associated infections represent a significant challenge in clinical practice, contributing substantially to the global burden of antimicrobial resistance. These structured microbial communities, encased in a self-produced extracellular polymeric substance (EPS) matrix, demonstrate remarkable tolerance to antimicrobial agents and host immune defenses [2] [47]. Understanding biofilm biology and developing effective therapeutic strategies requires robust experimental models that accurately recapitulate the complex biofilm lifecycle and its interaction with the host environment. This technical guide provides researchers and drug development professionals with a comprehensive overview of current in vitro and in vivo models for studying biofilm-associated infections, with particular emphasis on their application in investigating biofilm matrix composition and antibiotic penetration resistance.
The intrinsic resistance of biofilms to antibiotics is multifactorial, involving physical barrier function provided by the EPS matrix, metabolic heterogeneity leading to dormant persister cell populations, and enhanced horizontal gene transfer within the dense microbial community [2] [18]. The extracellular matrix, comprising polysaccharides, proteins, extracellular DNA (eDNA), and lipids, can hinder antibiotic penetration through binding or enzymatic degradation, while physiological gradients within biofilms create microenvironments with distinct metabolic states [47] [16]. These complex resistance mechanisms necessitate experimental models that preserve key aspects of biofilm architecture and host-pathogen interactions to yield clinically relevant insights for therapeutic development.
Biofilm Biology and Antimicrobial Resistance Mechanisms
The Biofilm Lifecycle
Biofilm development follows a programmed sequence of events beginning with initial attachment and culminating in structured, matrix-encased communities capable of coordinated dispersal. The lifecycle can be broadly categorized into five distinct phases [2]:
- Initial attachment: Planktonic cells reversibly adhere to conditioned surfaces through weak interactions including van der Waals forces and electrostatic interactions [16].
- Irreversible attachment: Production of adhesive surface structures and initial EPS secretion firmly anchors cells to the substrate [2].
- Microcolony formation: Cell division and coordinated aggregation form three-dimensional structures, facilitated by cell-to-cell communication [2].
- Biofilm maturation: Development of complex, heterogeneous architectures with characteristic features such as water channels and nutrient gradients [2] [16].
- Dispersion: Active or passive release of cells or biofilm fragments to colonize new niches [2].
The following diagram illustrates this dynamic lifecycle and the key processes at each developmental stage:
Mechanisms of Biofilm-Associated Antimicrobial Resistance
Biofilms employ multiple concurrent strategies to evade antimicrobial activity, creating a formidable barrier to effective treatment:
- Physical diffusion barrier: The EPS matrix physically impedes antibiotic penetration through binding interactions with matrix components or molecular sieving [2] [47]. Positively charged aminoglycosides, for instance, bind to negatively charged eDNA in the matrix, reducing effective concentrations reaching deeper cell layers [2].
- Metabolic heterogeneity: Gradients of nutrients, oxygen, and waste products create distinct metabolic zones within biofilms, leading to subpopulations with reduced metabolic activity that are less susceptible to antimicrobials targeting active cellular processes [47] [18].
- Persister cell formation: A subpopulation of dormant, non-dividing cells exhibits exceptional tolerance to conventional antibiotics, potentially contributing to biofilm recurrence after treatment [18].
- Enhanced horizontal gene transfer: The high cell density and presence of eDNA in biofilms facilitate the exchange of resistance genes through transformation, conjugation, and transduction, accelerating the development of antimicrobial resistance [47] [18].
- Altered microenvironment: The biofilm microenvironment can modify antibiotic activity through factors such as local pH changes or accumulation of enzymes that inactivate antimicrobial compounds [47].
In Vitro Biofilm Models
In vitro models provide controlled, reproducible systems for fundamental investigation of biofilm biology and high-throughput screening of potential therapeutic agents. These models range from simple static systems to sophisticated flow-based apparatus that mimic different aspects of the in vivo environment.
Static Biofilm Models
Table 1: Characteristics of Static In Vitro Biofilm Models
| Model Type | Key Characteristics | Applications | Advantages | Limitations |
|---|---|---|---|---|
| Microtiter Plate Assay | Bacteria attach to well surfaces; high-throughput compatibility [48] | Evaluation of biofilm formation capacity, antibiotic tolerance, efficacy of anti-biofilm compounds [48] | Simple operation, amenable to screening of multiple conditions, low cost [48] | Limited physiological relevance, static conditions, small biomass [48] |
| Colony Biofilm Model | Colonies grown on agar surfaces; maintains chemical gradients [48] | Antibiotic susceptibility assessment, morphological observation [48] | Reproducible, simple setup, structured environment [48] | Limited control over environmental parameters [48] |
| Calgary Biofilm Device | Peg lid for biofilm growth; consistent shear force [48] | Biofilm antibiotic resistance, time-course studies [48] | Commercially available, minimal contamination risk, standardized [48] | Specialized equipment required [48] |
| Biofilm Ring Test | Magnetic bead immobilization; automated image analysis [48] | Evaluation of early adhesion events [48] | Rapid monitoring, no washing/staining steps [48] | Limited to early biofilm formation stages [48] |
Dynamic Biofilm Models
Table 2: Characteristics of Dynamic In Vitro Biofilm Models
| Model Type | Key Characteristics | Applications | Advantages | Limitations |
|---|---|---|---|---|
| Flow Cell Systems | Flat-walled transparent chambers with continuous media irrigation [48] | Real-time observation of biofilm architecture, antibiotic penetration studies [48] | Non-destructive monitoring, excellent image quality, single-cell resolution [48] | Specialized equipment and expertise required, lower throughput [48] |
| CDC Biofilm Reactor | Polypropylene holders with coupons; suspended in media [48] | Disinfectant efficacy testing, biofilm development over time [48] | Easy sampling at multiple time points, reliable and reproducible [48] | Requires specific equipment, moderate throughput [48] |
| Drip Flow Reactor | Angled chambers with low shear, high gas transfer [48] | Wound biofilm modeling, antimicrobial efficacy testing [48] | Mimics air-tissue interfaces, studies biofilm heterogeneity [48] | Specialized equipment, limited parallelization [48] |
| Rotating Disc Reactor | Teflon rotor with multiple coupons; variable shear forces [48] | Evaluation of antimicrobial and anti-fouling treatments [48] | Controlled shear forces, multiple sampling surfaces [48] | Requires specific equipment, technical expertise [48] |
| Modified Robbins Device | Multiple ports with removable plugs along rectangular channel [48] | Modeling throat conditions, tracheo-oesophageal prosthesis studies [48] | Aseptic sampling during operation, mimics physiological flow conditions [48] | Complex setup, limited commercial availability [48] |
Experimental Protocol: Microtiter Plate Biofilm Assay for Antibiotic Susceptibility Testing
The microtiter plate assay represents a foundational method for evaluating biofilm formation capacity and antibiotic susceptibility in a high-throughput format. The following protocol details a standardized approach for antibiotic penetration assessment:
Materials Required:
- Sterile 96-well flat-bottom polystyrene microtiter plates
- Appropriate bacterial growth medium (e.g., Tryptic Soy Broth, Luria-Bertani broth)
- Test antibiotics at desired concentrations
- Phosphate-buffered saline (PBS)
- Crystal violet stain (0.1% w/v)
- Acetic acid (30% v/v)
- Microplate reader
Procedure:
- Inoculum Preparation: Harvest freshly grown bacterial colonies and adjust suspension to 0.5 McFarland standard (~1.5 × 10⁸ CFU/mL) in appropriate growth medium [49].
- Biofilm Formation: Dilute bacterial suspension 1:20 in fresh medium and aliquot 200 µL per well. Include negative control wells (medium only). Incubate at appropriate temperature (typically 37°C) for 24-48 hours without agitation [49].
- Antibiotic Exposure: After biofilm formation, carefully remove spent medium and replace with fresh medium containing serial dilutions of test antibiotics. Incubate for additional 24 hours.
- Biofilm Quantification:
- Remove medium and gently wash wells twice with PBS to remove non-adherent cells.
- Fix biofilms by air drying or using methanol.
- Stain with 0.1% crystal violet for 15 minutes.
- Wash thoroughly to remove excess stain.
- Elute bound stain with 30% acetic acid.
- Measure optical density at 570-600 nm using microplate reader [49].
- Data Analysis: Calculate minimum biofilm eradication concentration (MBEC) as the lowest antibiotic concentration that results in ≥90% reduction in biofilm biomass compared to untreated controls.
Variations for Specific Applications:
- For viability assessment, replace crystal violet staining with resazurin reduction assay or ATP quantification.
- For matrix composition studies, incorporate enzymatic treatments (e.g., DNase I, dispersin B, proteinase K) during antibiotic exposure to evaluate contribution of specific matrix components to antibiotic tolerance [18].
In Vivo Biofilm Models
In vivo models provide essential biological context for studying biofilm pathogenesis and therapeutic efficacy, incorporating host immune responses, tissue-specific microenvironments, and natural substrata that cannot be fully replicated in vitro.
Murine Models of Biofilm-Associated Infection
Table 3: Characteristics of In Vivo Murine Biofilm Models
| Model Type | Key Characteristics | Applications | Advantages | Limitations |
|---|---|---|---|---|
| Subcutaneous Mesh Model | Polypropylene mesh implanted subcutaneously [50] | Prolonged study of biofilm infections, therapeutic efficacy evaluation [50] | Consistent bioluminescence signal, strong correlation with bacterial counts, minimal implant loss [50] | Does not mimic specific anatomical sites [50] |
| Tibial Intramedullary Pin Model | Steel pin inserted into tibial medullary cavity [50] | Study of implant-associated osteomyelitis [50] | Sustained infection, models orthopedic device infections [50] | Technically challenging surgery, potential for fracture [50] |
| Subcutaneous Catheter Model | IV catheter segment implanted subcutaneously [50] | Catheter-associated biofilm infections [50] | Direct injection of bacteria into implanted catheter [50] | High incidence of abscessation and implant extrusion [50] |
| Catheter-Associated Murine Model | Catheter implantation with bacterial inoculation [51] | Foreign body infection studies, host-pathogen interactions [51] | Mimics clinical device-related infections, allows study of host protein coating effects [51] | Potential for systemic infection, variable biofilm development [51] |
Experimental Protocol: Subcutaneous Mesh Implant Model
The subcutaneous mesh model provides a robust system for evaluating biofilm development and therapeutic interventions over extended periods, with excellent correlation between in vivo imaging and bacterial recovery [50].
Materials Required:
- Female ICR mice (6-8 weeks old)
- Polypropylene surgical mesh (Surgipro)
- Sterile surgical instruments
- Anesthesia equipment (isoflurane)
- Bioluminescent or conventional bacterial strains
- In vivo imaging system (IVIS) for bioluminescent strains
- Culture media for bacterial enumeration
Procedure:
- Implant Preparation:
- Cut mesh into 6 mm × 6 mm sections and sterilize.
- Incubate mesh sections in log-phase bacterial culture for 12 hours at 37°C with agitation [50].
- Rinse thoroughly with sterile PBS to remove non-adherent cells.
- Confirm bacterial load by culturing representative mesh pieces.
Surgical Implantation:
- Anesthetize mice using isoflurane.
- Clip and aseptically prepare dorsal skin.
- Administer preoperative analgesia (e.g., buprenorphine, 0.05 mg/kg SC).
- Make small dorsal midline incision (approximately 5 mm).
- Create subcutaneous pocket by blunt dissection.
- Insert single infected mesh piece into pocket.
- Close incision with wound clips or sutures [50].
Infection Monitoring:
- For bioluminescent strains, image animals regularly using IVIS system under standardized conditions (anesthesia, exposure time, binning) [50].
- Monitor clinical signs (weight loss, activity level, appearance of surgical site).
- Track bioluminescent signal intensity within defined region of interest.
Endpoint Analysis:
- Euthanize animals at experimental endpoint.
- Aseptically explant mesh and surrounding tissue.
- Process samples for bacterial enumeration (sonication, serial dilution, plating) or histology [50].
Data Interpretation:
- Correlate in vivo imaging data with bacterial counts from explanted samples.
- Compare biofilm burden between treatment groups using appropriate statistical tests.
- Perform histological analysis of host tissue response when applicable.
The following workflow diagram illustrates the experimental timeline and key procedures for establishing and evaluating biofilms using this model:
Integration of Models for Comprehensive Biofilm Research
Effective investigation of biofilm-associated infections often requires strategic integration of multiple model systems to address specific research questions. The complementary strengths of different approaches provide a more complete understanding of biofilm biology and therapeutic responses.
Model Selection Framework
- High-throughput compound screening: Begin with microtiter plate assays for initial screening of anti-biofilm compounds, followed by validation using more complex models such as flow cells or CDC biofilm reactors [48].
- Antibiotic penetration studies: Utilize flow cell systems coupled with confocal microscopy to visualize antibiotic penetration through biofilms using fluorescently tagged antibiotics [48] [2].
- Host-pathogen interactions: Employ in vivo models such as the subcutaneous mesh implant or catheter models to investigate the role of host proteins and immune responses in biofilm development [51] [50].
- Device-related infections: Combine in vitro models using relevant biomaterials with corresponding in vivo implantation models to study biofilm formation on medical devices [51] [50].
- Gene expression analysis: Use in vivo biofilm models with subsequent transcriptomic analysis to identify genes differentially expressed during biofilm-associated infections compared to laboratory conditions [51].
Methodological Considerations for Antibiotic Penetration Research
Investigating antibiotic penetration in biofilms requires special methodological considerations to generate clinically relevant data:
- Biofilm maturity: Biofilm age significantly impacts antibiotic susceptibility, with mature biofilms (typically 72-96 hours) exhibiting greater tolerance than younger biofilms [47].
- Antibiotic dosing regimens: Consider pharmacokinetic/pharmacodynamic parameters when designing experiments, including concentration-time profiles relevant to human dosing [47].
- Penetration measurement techniques: Utilize techniques such as fluorescence recovery after photobleaching (FRAP) with fluorescent antibiotic conjugates, microelectrode measurements, or mass spectrometry imaging to directly quantify antibiotic penetration [2].
- Matrix composition analysis: Characterize EPS components (eDNA, polysaccharides, proteins) in parallel studies to correlate matrix composition with penetration barriers [2] [16].
- Combination therapy approaches: Evaluate agents that disrupt matrix integrity (e.g., DNase, dispersin B) in combination with conventional antibiotics to overcome penetration limitations [18].
The Researcher's Toolkit: Essential Reagents and Materials
Table 4: Key Research Reagents and Materials for Biofilm Studies
| Category | Specific Items | Application/Function | Examples/Notes |
|---|---|---|---|
| Growth Media & Supplements | Tryptic Soy Broth (TSB), Luria-Bertani (LB) broth, specific carbohydrate supplements | Biofilm growth medium optimization | TSB with 0.5% glucose enhances staphylococcal biofilm formation [51] |
| Staining & Visualization | Crystal violet, LIVE/DEAD BacLight viability stains, fluorescently-conjugated lectins | Biofilm quantification and visualization | Crystal violet for biomass assessment; concanavalin A for polysaccharide staining [48] [49] |
| Matrix Disruption Agents | DNase I, proteinase K, dispersin B, sodium metaperiodate | Selective degradation of matrix components | DNase I targets eDNA; dispersin B degrades poly-N-acetylglucosamine [18] |
| Specialized Surfaces | Polypropylene mesh, silicone catheters, titanium pins, hydroxyapatite coatings | Mimicking medical device substrates | Material-specific biofilm formation studies [51] [50] |
| In Vivo Imaging Tools | Bioluminescent bacterial strains, IVIS imaging systems, appropriate anesthesia equipment | Non-invasive monitoring of biofilm infections | Xen36 S. aureus for real-time infection monitoring [50] |
| Antibiotic Testing | Standard antibiotics, fluorescent antibiotic conjugates, MBEC assay plates | Antibiotic susceptibility and penetration studies | Fluorescently-tagged vancomycin for penetration visualization [2] [49] |
The strategic selection and implementation of appropriate in vitro and in vivo models is fundamental to advancing our understanding of biofilm-associated infections and developing effective therapeutic interventions. Simple in vitro systems provide valuable tools for high-throughput screening and mechanistic studies, while increasingly complex in vivo models bridge the gap between basic research and clinical application. The integration of these complementary approaches, with careful consideration of their respective strengths and limitations, enables comprehensive investigation of the multifactorial nature of biofilm-associated antibiotic resistance. As research in this field evolves, continued refinement of existing models and development of novel systems that better recapitulate the complexity of human infections will accelerate progress toward effective strategies for preventing and eradicating biofilm-associated infections.
In the field of antimicrobial research, standard susceptibility testing has primarily focused on planktonic (free-floating) bacteria, with the Minimum Inhibitory Concentration (MIC) serving as a cornerstone for determining effective antibiotic dosing. However, this paradigm presents a critical limitation when addressing biofilm-associated infections. It is now recognized that up to 80% of all chronic and recurrent infections involve bacterial biofilms, communities of microorganisms embedded in a self-produced extracellular polymeric matrix that demonstrates dramatically increased tolerance to antimicrobial agents [52]. This discrepancy necessitates a distinct set of metrics—Minimum Biofilm Inhibitory Concentration (MBIC) and Minimum Biofilm Eradication Concentration (MBEC)—to properly evaluate antibiotic efficacy against these structured communities. Understanding the relationship between MIC, MBIC, and MBEC is fundamental to developing effective therapeutic strategies for biofilm-related infections, which are notoriously difficult to eradicate and contribute significantly to chronic conditions and treatment failures in clinical settings [53] [52].
Defining the Key Efficacy Metrics
Traditional Metric for Planktonic Bacteria
- Minimum Inhibitory Concentration (MIC): The lowest concentration of an antimicrobial agent that prevents visible growth of a planktonic bacterium in vitro [53]. This is the standard metric used in clinical microbiology laboratories to guide therapy for acute infections.
- Minimum Bactericidal Concentration (MBC): The lowest concentration of an antimicrobial agent required to kill a specific bacterium, typically demonstrated by a 99.9% reduction in the initial inoculum [54].
Advanced Metrics for Biofilm Cultures
- Minimum Biofilm Inhibitory Concentration (MBIC): The lowest concentration of an antimicrobial agent that inhibits biofilm formation or visible growth within a pre-formed biofilm. It is measured as the concentration resulting in an optical density difference of ≤10% compared to the positive control, representing approximately a 1-log difference in growth [55].
- Minimum Biofilm Eradication Concentration (MBEC): The lowest concentration of an antimicrobial agent that eradicates a pre-formed biofilm, corresponding to the death of 99.9% of the biofilm-associated bacterial population [55]. The MBEC is also sometimes referred to as the Minimum Biofilm Eradication Concentration.
The fundamental distinction lies in the dramatically higher antibiotic concentrations required to affect biofilms. Research consistently shows that biofilm cells can exhibit 10 to 1,000 times greater tolerance to antibiotics compared to their planktonic counterparts [52] [55]. For instance, one study on Acinetobacter baumannii found that the MBEC values for ciprofloxacin and imipenem were 407 and 364 times higher, respectively, than the MBC for planktonic cells [56].
Quantitative Comparison of Efficacy Metrics
The table below summarizes representative data from recent studies, illustrating the significant disparity between antibiotic concentrations required to act on planktonic versus biofilm bacteria.
Table 1: Comparative MIC, MBC, MBIC, and MBEC Values from Recent Studies
| Bacterial Species | Antibiotic | MIC (μg/mL) (Planktonic) | MBC (μg/mL) (Planktonic) | MBIC (μg/mL) (Biofilm) | MBEC (μg/mL) (Biofilm) | Source/Study Context |
|---|---|---|---|---|---|---|
| Staphylococcus aureus (MRSA) | Daptomycin | 0.25 - 0.5 | Not Reported | Not Reported | 32 - 256 (≥75% reduction) | In vitro stage-four biofilms [57] |
| Staphylococcus aureus (Clinical isolates) | Levofloxacin | 0.25 - 512 | Not Reported | ≤4 (for susceptible planktonic isolates) | ≤4 (for susceptible planktonic isolates) | Acute exacerbation of chronic rhinosinusitis (AECRS) patients [55] |
| Staphylococcus aureus (Clinical isolates) | Amoxicillin/Clavulanic Acid | Varies (17.4% resistant) | Not Reported | >512 (for resistant planktonic isolates) | >512 (for resistant planktonic isolates) | AECRS patients [55] |
| Acinetobacter baumannii (Non-MDR) | Ciprofloxacin | ≤0.25 (MBC) | ≤0.25 | Not Reported | 64 - 128 (MBEC) | Clinical isolates from hospital settings [56] |
| Acinetobacter baumannii (Non-MDR) | Imipenem | ≤0.5 (MBC) | ≤0.5 | Not Reported | 128 (MBEC) | Clinical isolates from hospital settings [56] |
| Staphylococcus aureus (MRSA/VRSA) | Melittin (AMP) | 1.25 - 10 (Geometric mean: 1.62) | 2.5 - 20 (Geometric mean: 5.45) | 1.25 - 10 | 10 - 40 | Investigation of anti-biofilm potential [58] |
Mechanisms Underlying Biofilm-Associated Tolerance
The extreme tolerance observed in biofilms, as reflected in the high MBIC and MBEC values, is not due to a single mechanism but rather a multifactorial phenomenon [52].
- Impaired Antibiotic Penetration: The extracellular polymeric substance (EPS) matrix, composed of exopolysaccharides, extracellular DNA (eDNA), and proteins, acts as a physical barrier that can retard the diffusion of antimicrobial agents into the deepest layers of the biofilm [52].
- Altered Microenvironment: Biofilms develop physiological gradients of nutrients, oxygen, and waste products. This heterogeneity creates subpopulations of metabolically dormant or slow-growing "persister" cells in the biofilm's interior, which are highly tolerant to antibiotics that typically target active cellular processes [52] [56].
- Biofilm-Specific Phenotype: Cells within a biofilm undergo a distinct genetic reprogramming, leading to an altered phenotype that is inherently more resistant than its planktonic counterpart, even without genetic mutations [53].
- Enhanced Mutation Rates and Evolution of Resistance: The biofilm environment can promote genetic diversity and increase mutation rates. Studies have shown that biofilms exposed to intermittent antibiotic treatment can rapidly select for resistant mutants, a phenomenon observed less frequently in planktonic populations under the same conditions [59].
Essential Experimental Protocols for Biofilm Susceptibility Testing
The Modified Calgary Biofilm Device (CBD) Protocol
The Calgary Biofilm Device is a widely used and standardized method for growing biofilms and determining MBIC and MBEC values [55] [56]. The workflow is as follows:
Biofilm Formation:
- Inoculum Preparation: Grow the bacterial isolate in a suitable broth (e.g., Luria-Bertani or Tryptic Soy Broth) to the log phase. Adjust the suspension to a standardized optical density (e.g., 0.1 at 600 nm).
- Incubation: Transfer 150 µL of the adjusted inoculum into the wells of a 96-well microtiter plate. Securely attach a specialized lid with 96 pegs, which will serve as the surface for biofilm formation.
- Biofilm Growth: Incubate the assembled plate for a specified period (e.g., 20-48 hours) at the organism's optimal growth temperature (e.g., 37°C) on a platform shaker to ensure consistent nutrient distribution.
MBIC and MBEC Assay:
- Biofilm Challenge: After incubation, gently rinse the peg lid in sterile water to remove non-adherent planktonic cells. Transfer the peg lid to a new 96-well "challenge plate" containing a serial dilution of the test antibiotic in broth.
- Incubation and Recovery: Incubate the challenge plate for another 20-24 hours. Subsequently, rinse the peg lid again and transfer it to a "recovery plate" containing fresh broth without antibiotics.
- Quantification and Determination: The recovery plate is then incubated to allow any surviving cells from the biofilm to proliferate. The MBIC is defined as the lowest antibiotic concentration that results in an OD in the recovery plate that is ≤10% of the positive control growth after a set incubation time. The MBEC is the lowest concentration that results in no visible growth (OD equivalent to the negative control) [55].
The following diagram illustrates this experimental workflow:
Research Reagent Solutions Toolkit
Table 2: Essential Materials and Reagents for Biofilm Susceptibility Testing
| Item | Function/Application | Specific Examples |
|---|---|---|
| 96-Well Peg Lids & Plates | Provides a standardized and high-throughput surface for growing multiple biofilms simultaneously. | Calgary Biofilm Device (CBD) by Innovotech; Nunc TSP system lid [55] [56]. |
| Cation-Adjusted Mueller Hinton Broth (CA-MHB) | The standard growth medium for antimicrobial susceptibility testing, ensuring consistent ion concentrations for antibiotic activity. | Often supplemented with magnesium (12.5 mg/L) and calcium (25-50 mg/L) as per CLSI guidelines, with higher calcium used for testing daptomycin [57]. |
| Crystal Violet | A simple stain used to quantify the total biofilm biomass attached to a surface, reflecting the amount of cells and matrix. | 0.1% aqueous solution, followed by elution with 33% acetic acid and measurement of OD570 [56]. |
| Automated Identification & MIC System | Used for the initial identification of bacterial isolates and determination of planktonic MIC. | VITEK 2 system (BioMérieux) [55]. |
| Gradient Strip Test | An alternative method for determining the MIC of planktonic bacteria directly from a clinical sample or culture. | E-test (BioMérieux) [55]. |
The critical distinction between MIC/MBC and MBIC/MBEC underscores a fundamental shift in our understanding of bacterial susceptibility. Relying solely on planktonic MIC data to treat biofilm-associated infections is not only inadequate but can also contribute to treatment failure and the selection for further resistance. The significantly higher concentrations required for biofilm eradication, as quantified by the MBEC, often far exceed the safe and achievable levels in human tissues, explaining the persistence of chronic infections. Future research must continue to refine standardized biofilm susceptibility testing methods and integrate MBIC/MBEC data into both clinical practice and the drug development pipeline. Exploring innovative strategies, such as combination therapies with antimicrobial peptides like melittin to rejuvenate existing antibiotics or targeting the biofilm matrix itself, represents a promising path forward in the ongoing battle against resilient biofilm infections [57] [58].
Overcoming the Barrier: Mechanisms of Failure and Strategies for Enhanced Drug Delivery
Biofilms, structured communities of microorganisms encased in an extracellular polymeric substance (EPS), represent a significant challenge in clinical medicine due to their profound resistance to antimicrobial treatments [2] [47]. This resistance is not mediated by a single mechanism but is a multifactorial phenomenon integrating physical, physiological, and genetic adaptations that collectively shield bacterial populations from eradication [18] [16]. Within the context of biofilm matrix composition and antibiotic penetration resistance research, understanding these layered defense strategies is paramount for developing effective therapeutic interventions. The intrinsic tolerance of biofilm-associated bacteria can be 10 to 1,000-fold greater than their planktonic counterparts, rendering many conventional antibiotic regimens ineffective against chronic and device-related infections [47] [60]. This whitepaper delineates the core mechanisms underpinning biofilm-mediated resistance, provides detailed experimental methodologies for their investigation, and discusses emerging strategies aimed at overcoming these formidable microbial fortresses.
Physical and Structural Resistance Mechanisms
The biofilm matrix acts as a primary physical barrier, significantly impeding the penetration of antimicrobial agents and protecting the embedded cells [2] [47].
The Extracellular Polymeric Substance (EPS) as a Diffusion Barrier
The EPS is a complex mixture of polysaccharides, proteins, extracellular DNA (eDNA), and lipids, which can constitute over 90% of the biofilm's dry mass [2] [35]. This matrix is not merely a passive scaffold but a dynamic functional component that limits antibiotic penetration through several mechanisms, as detailed in Table 1.
Table 1: Components of the Biofilm Matrix and Their Roles in Antimicrobial Resistance
| Matrix Component | Primary Function in Resistance | Impact on Antibiotic Efficacy |
|---|---|---|
| Exopolysaccharides (e.g., Alginate, PIA) | Forms a viscous structural scaffold; binds ionic molecules [61] | Traps antibiotics; reduces diffusion rate; inactivates positively charged drugs (e.g., aminoglycosides) [47] [35] |
| Extracellular DNA (eDNA) | Provides structural integrity; negative charge [47] [62] | Chelates cationic antibiotics (e.g., aminoglycosides, antimicrobial peptides); acts as a physical mesh [2] [62] |
| Proteins (e.g., Adhesins, Amyloids) | Stabilizes cell-cell and cell-surface interactions [2] | Can bind and inactivate specific antibiotics; contributes to matrix density [47] |
| Water Channels | Facilitates nutrient/waste exchange [61] | Creates heterogeneous penetration pathways, leading to uneven antibiotic distribution [2] |
The slowed or incomplete diffusion of antibiotics through this dense, polyanionic matrix allows sufficient time for enzymatic degradation or neutralization of the antimicrobial agent at the biofilm periphery before it reaches cells in the deeper layers [47] [35].
Physiological and Metabolic Heterogeneity
Biofilms are characterized by significant physiological heterogeneity, which is a key driver of antibiotic tolerance. Gradients of nutrients, oxygen, and waste products establish diverse metabolic states within the biofilm architecture [18] [2].
- Metabolic Gradients and Dormancy: Cells in the outer, nutrient-replete layers of the biofilm are typically metabolically active. In contrast, cells in the inner core experience nutrient depletion and hypoxia, entering a slow-growing or dormant state [2] [35]. Since many antibiotics, such as β-lactams and fluoroquinolones, target active cellular processes like cell wall synthesis and DNA replication, these dormant cells are inherently tolerant [2] [35].
- Persister Cells: A subpopulation of cells can enter a deeply dormant, "persister" state. These cells are not genetically mutant but are phenotypically tolerant and can survive high concentrations of bactericidal antibiotics. Upon antibiotic withdrawal, persister cells can resuscitate and re-establish the biofilm, leading to recurrent infections [60].
Table 2: Quantified Reductions in Antibiotic Penetration and Efficacy in Biofilms
| Antibiotic Class | Representative Agent | Reported Efficacy Reduction in Biofilms | Primary Penetration Barrier |
|---|---|---|---|
| Aminoglycosides | Tobramycin | Up to 1000-fold increase in MIC required [35] | Binding to anionic eDNA and polysaccharides [2] [47] |
| β-Lactams | Vancomycin | 75% resistance in biofilm S. epidermidis vs. 0% in planktonic cells [60] | Slow diffusion; degradation by β-lactamases in periphery [47] |
| Fluoroquinolones | Ciprofloxacin | Reduced efficacy under anaerobic/hypoxic conditions [60] | Efflux pumps; reduced activity against slow-growing cells [35] [63] |
Genetic and Adaptive Resistance Mechanisms
Beyond physical and physiological tolerance, biofilms actively facilitate the development and spread of genetic antibiotic resistance.
Enhanced Horizontal Gene Transfer (HGT)
The dense, structured environment of a biofilm, with cells in close proximity and abundant eDNA, is highly conducive to HGT [18] [47]. This includes:
- Transformation: Uptake of free eDNA containing resistance genes [47].
- Conjugation: Plasmid transfer via direct cell-to-cell contact, efficiently spreading multi-drug resistance (MDR) cassettes [18] [63].
- Transduction: Gene transfer mediated by bacteriophages [18]. Biofilms thus act as "hotspots" for the dissemination of resistance genes, such as those encoding extended-spectrum β-lactamases (ESBLs) and carbapenemases, among diverse bacterial species [18] [63].
Mutagenesis and Efflux Pump Expression
- Hypermutability: Stress conditions within biofilms can induce a stress response, leading to an increased mutation rate. This accelerates the selection of spontaneous chromosomal mutations that confer antibiotic resistance [47].
- Efflux Pump Upregulation: Multidrug efflux pumps (e.g., MexAB-OprM in P. aeruginosa) are often overexpressed in biofilms [35] [63]. These pumps can actively extrude a wide range of antibiotics, including fluoroquinolones, β-lactams, and macrolides, from the bacterial cell, contributing to both intrinsic and acquired MDR [63]. Their expression can be heterogeneous, often upregulated in specific regions of the biofilm, such as the surface layers [35].
Diagram 1: Interconnected mechanisms of biofilm-mediated antimicrobial resistance. The model shows how physical, physiological, and genetic defenses work together to create a robust, multi-layered resistance phenotype.
Experimental Protocols for Investigating Resistance Mechanisms
Protocol: Assessing Antibiotic Penetration Kinetics
Objective: To quantify the diffusion rate and spatial distribution of an antibiotic through a mature biofilm.
Materials:
- Modified Robbins device or flow cell system
- Fluorescently tagged antibiotic (e.g., BODIPY-FL vancomycin)
- Confocal Laser Scanning Microscopy (CLSM)
- Image analysis software (e.g., ImageJ, COMSTAT)
Methodology:
- Biofilm Cultivation: Grow a standardized biofilm (e.g., P. aeruginosa PAO1 or S. aureus biofilm) under relevant flow conditions for 48-72 hours to ensure maturity [2].
- Antibiotic Perfusion: Introduce the fluorescently tagged antibiotic at a clinically relevant concentration (e.g., 10x MIC for planktonic cells) into the flow system.
- Time-Lapse Imaging: Using CLSM, capture Z-stack images at predetermined time intervals (e.g., 0, 15, 30, 60, 120 minutes) at multiple locations within the biofilm.
- Quantitative Analysis:
- Measure the fluorescence intensity as a function of depth and time.
- Calculate the effective diffusion coefficient (De) for the antibiotic within the biofilm and compare it to its diffusion in water (Dw). A De/Dw ratio << 1 indicates significant penetration impedance [35].
- Generate concentration-distance plots to visualize the penetration profile.
Protocol: Evaluating Metabolic Heterogeneity and Persister Cell Formation
Objective: To identify and quantify metabolically heterogeneous zones and persister cells within a biofilm.
Materials:
- Fluorescent viability stains (e.g., SYTO 9/propidium iodide for Live/Dead staining)
- Metabolic activity probes (e.g., 5-cyano-2,3-ditolyl tetrazolium chloride (CTC) for active respiration)
- Fluorescence-Activated Cell Sorting (FACS)
- CLSM
Methodology:
- Biofilm Staining: Gently stain mature biofilms with a combination of SYTO 9 (total cells), propidium iodide (membrane-compromised cells), and CTC (metabolically active cells).
- CLSM Imaging: Acquire high-resolution 3D images. CTC-positive (active) cells will fluoresce red, while CTC-negative cells in nutrient-poor zones are dormant.
- Image Analysis: Use software to quantify the volumetric distribution of metabolic activity. This will reveal microenvironments of high and low activity [2] [35].
- Persister Cell Isolation:
- Gently disaggregate the biofilm and treat the cell suspension with a high concentration of a bactericidal antibiotic (e.g., 100x MIC of ciprofloxacin) for 3-5 hours.
- Wash the cells to remove the antibiotic and plate on nutrient agar. The colonies that form are derived from persister cells [60].
- The persister frequency is calculated as (CFU/mL after antibiotic treatment) / (CFU/mL before treatment).
Table 3: The Scientist's Toolkit: Key Reagents for Biofilm Resistance Research
| Research Reagent / Material | Function and Application | Example Use Case |
|---|---|---|
| Calgary Biofilm Device | High-throughput cultivation of 96 identical biofilms for MIC/MBC testing [16] | Screening anti-biofilm efficacy of novel compounds. |
| Confocal Laser Scanning Microscope (CLSM) | Non-destructive, 3D visualization of live biofilms and spatial localization of probes [30] | Imaging antibiotic penetration and metabolic heterogeneity in real-time. |
| Fluorescently-tagged Antibiotics | Visualizing and quantifying antibiotic penetration and binding in situ. | Measuring diffusion coefficients of vancomycin in staphylococcal biofilms. |
| Quorum Sensing Inhibitors (e.g., AHL analogs) | Chemical disruption of bacterial cell-to-cell communication [18] [47] | Assessing the role of QS in biofilm maturation and virulence. |
| Dispersin B & DNase I | Enzymatic degradation of key EPS components (polyosaccharides, eDNA) [18] [61] | Testing the role of matrix integrity in protecting against antibiotics. |
| Efflux Pump Inhibitors (e.g., PaβN) | Blocking active efflux of antibiotics from bacterial cells [35] | Determining the contribution of efflux pumps to biofilm-specific resistance. |
| CRISPR-Cas9 Knockout Systems | Targeted gene editing to validate the function of specific resistance genes [18] [30] | Creating mutants deficient in efflux pumps or matrix production. |
Diagram 2: Experimental workflow for isolating and quantifying bacterial persister cells from a mature biofilm, illustrating the key steps from antibiotic challenge to colony formation.
The resistance of biofilms to antimicrobials is a quintessential example of a multifaceted defense system. It is not governed by a single mechanism but by a synergistic interplay of physical barrier functions, physiological heterogeneity, and dynamic genetic adaptations [18] [2] [47]. The EPS matrix provides a formidable physical shield, while internal metabolic gradients foster a population of dormant, tolerant cells. Simultaneously, the biofilm environment accelerates the evolution and dissemination of permanent genetic resistance [18] [63]. This intricate hierarchy of resistance necessitates a departure from conventional antimicrobial monotherapies. Future research and drug development must pivot towards combinatorial strategies that concurrently target multiple facets of biofilm resilience [18] [30]. Promising approaches include EPS-degrading enzymes to disrupt the matrix, nanoparticles for enhanced drug delivery, quorum sensing inhibitors to impede community coordination, and CRISPR-based technologies to precisely eliminate resistance genes [18] [30]. Overcoming the challenge of biofilm-mediated infections demands a holistic understanding of these interconnected resistance mechanisms to develop the next generation of effective anti-biofilm therapeutics.
Antibiotic penetration resistance represents a formidable barrier in the clinical management of biofilm-associated infections. This resistance arises not from genetic mutations but from the physical and biochemical properties of the biofilm matrix itself. Biofilms are complex microbial communities encased in an extracellular polymeric substance (EPS) matrix, which functions as a biological barrier that restricts antibiotic penetration through three primary mechanisms: sorption (the binding of antibiotic molecules to EPS components), binding (specific interactions with biofilm elements), and enzymatic degradation (the direct inactivation of antibiotics by biofilm-expressed enzymes) [16]. The World Health Organization reports that one in six laboratory-confirmed bacterial infections in 2023 were resistant to antibiotic treatments, with drug-resistant Gram-negative bacteria posing particularly serious threats [64]. This whitepaper examines the fundamental mechanisms underlying the penetration problem and provides researchers with advanced methodologies to investigate these barriers.
Biofilm Matrix Composition and Organization
The biofilm EPS matrix forms the structural foundation for antibiotic penetration resistance. This matrix is composed of nucleic acids, polysaccharides, proteins, and other polymeric substances that create a three-dimensional architecture with defined chemical and physical properties [16]. The matrix is not a static structure but undergoes dynamic reorganization throughout the biofilm lifecycle, which typically progresses through four distinct stages: initial reversible attachment, irreversible attachment and matrix production, maturation, and dispersal [16] [57].
Matrix Components and Their Roles in Antibiotic Trapping
- Extracellular DNA (eDNA): Provides structural integrity and presents negatively charged binding sites for antibiotics [57]
- Polysaccharides: Form the hydrogel backbone of the matrix, creating a diffusion barrier
- Proteins: Include enzymes for antibiotic modification and specific binding proteins
- Ions: Divalent cations (e.g., Ca²⁺, Mg²⁺) cross-link matrix components and influence porosity
The spatial organization of the biofilm creates chemical gradients (oxygen, nutrients, pH) that generate heterogeneous microbial subpopulations with differing metabolic activities and antibiotic susceptibility profiles [16]. This heterogeneity complicates treatment by creating niches where antibiotics may be less effective, even when they successfully penetrate the matrix.
Mechanisms of Antibiotic Penetration Failure
Sorption and Binding Interactions
The biofilm matrix acts as a ion-exchange resin that can sequester antibiotic molecules through various physicochemical interactions. A seminal study investigating antibiotic sorption to biofilm demonstrated that the extent of sorption is highly dependent on antibiotic structure and speciation at physiological pH [65] [66].
Table 1: Biofilm Sorption Coefficients (Koc) for Representative Antibiotics
| Antibiotic | Class | Koc (L/kg) | Primary Sorption Mechanism | Molecular Characteristics |
|---|---|---|---|---|
| Ciprofloxacin (CIP) | Fluoroquinolone | 92,000 ± 10,000 | Electrostatic interaction, metal ion bridging | Positively charged at circumneutral pH, relatively small size |
| Erythromycin (ERY) | Macrolide | 6,000 ± 1,000 | Limited penetration due to molecular size | Positively charged, larger molecular structure |
| Sulfamethoxazole (SMX) | Sulfonamide | 4,000 ± 1,000 | Weak hydrophobic interactions | Neutral to negative charge, low Kow |
The Koc values describing antibiotic partitioning to biofilm do not correlate with antibiotic octanol-water partition coefficients (Kow values), indicating that hydrophobic interactions are not the primary driver for these relatively hydrophilic compounds [65] [66]. Instead, antibiotic speciation (charge) and molecular size appear to be critical factors influencing sorption to the typically negatively charged biofilm matrix.
Enzymatic Degradation and Modification
Biofilms express and secrete a diverse array of antibiotic-inactivating enzymes that represent a direct mechanism of antibiotic resistance. These enzymes can be broadly categorized by their mechanisms of action:
- Hydrolysis: Enzymatic cleavage of vulnerable bonds, most notably β-lactamases that hydrolyze the β-lactam ring [67] [68]
- Group Transfer: Covalent modification of antibiotics through acyltransfer, phosphorylation, glycosylation, nucleotidylation, ribosylation, and thiol transfer [68]
- Redox Mechanisms: Oxidation or reduction of antibiotic functional groups [67]
The recent development of β-lactamase enzyme cocktails demonstrates the potential for simultaneous degradation of antibiotics across multiple classes. A 2025 study reported that a cocktail combining CTX-M-33 (Class A) and VIM-1 (Class B) β-lactamases achieved over 99% degradation of nineteen antibiotics from four different β-lactam families (penicillins, cephalosporins, carbapenems, and monobactams) [69]. This approach highlights both the challenge and potential solution to enzymatic degradation – while a single enzyme typically targets only limited antibiotic classes, strategic combinations can broaden the degradation spectrum.
Figure 1: Enzymatic Degradation Pathways for β-Lactam Antibiotics. The diagram illustrates the substrate specificity of different β-lactamase classes and the broad-spectrum degradation capability achieved through enzyme cocktails.
Experimental Approaches and Methodologies
Quantitative Assessment of Biofilm Sorption
Continuous-Flow Rotating Annular Bioreactor (CFRAB) Protocol [65]
This method enables precise quantification of antibiotic sorption to mature biofilms under controlled hydrodynamic conditions.
- Apparatus Setup: Utilize a CFRAB system with removable polycarbonate coupons for biofilm growth. The system should maintain constant temperature (30-37°C) and flow rates to simulate environmental conditions.
- Biofilm Cultivation: Inoculate with target bacterial strains (e.g., Pseudomonas aeruginosa, Klebsiella pneumoniae) and cultivate for 5-7 days with nutrient feeding to establish mature biofilms (10⁶-10⁷ CFU/cm²).
- Antibiotic Exposure: Introduce antibiotics at environmentally relevant concentrations (0.1-100 μg/L) in defined buffers. Include control reactors without biofilm to account for abiotic losses.
- Sampling and Analysis: Collect timed effluent samples and analyze antibiotic concentrations using LC-MS/MS. Determine sorption parameters from breakthrough curves.
- Data Analysis: Calculate biofilm-water partition coefficients (Koc) using the retardation factor method, normalized to biofilm organic carbon content.
Determining Minimum Biofilm Eradication Concentrations (MBEC)
Modified Microtiter Plate Assay for Biofilm Susceptibility Testing [57]
Standard MIC testing evaluates only planktonic bacteria, providing clinically misleading results for biofilm-associated infections. The MBEC assay addresses this limitation.
- Biofilm Growth: Prepare bacterial inoculum (5-6 log10 CFU/mL) in appropriate growth media supplemented with 1.25% dextrose to enhance biofilm formation. Aliquot into 96-well polystyrene tissue culture plates.
- Biofilm Development: Incubate plates for specific timepoints (2, 4, 6, 8, 16, 24 hours) to establish different biofilm maturation stages. Gently wash to remove non-adherent cells.
- Antibiotic Exposure: Treat established biofilms with serial antibiotic dilutions (typically 0.5-512× MIC) for 24 hours. Include untreated controls for normalization.
- Viability Assessment: Quantify residual biofilm using metabolic assays (e.g., resazurin reduction) or CFU enumeration after biofilm disruption.
- Data Interpretation: MBEC is defined as the lowest antibiotic concentration achieving ≥75-90% reduction in biofilm viability. Note that efficacy varies significantly by antibiotic class; for example, daptomycin achieves superior eradication compared to vancomycin or levofloxacin against Staphylococcus aureus biofilms [57].
Figure 2: Experimental Workflow for MBEC Determination. The diagram outlines the key steps in assessing antibiotic efficacy against biofilms at different developmental stages.
Zeta-Potential Measurements for Biofilm Surface Characterization
Electrostatic properties significantly influence initial bacterial attachment and antibiotic interaction with biofilms. Zeta (ζ)-potential measurements provide quantitative assessment of these surface charges [57].
- Sample Preparation: Harvest mature biofilms (strong and weak producers) and resuspend in appropriate electrolyte solution at standardized cell density.
- Instrumentation: Use phase analysis light scattering with a zeta-potential analyzer. Maintain constant temperature (25°C) and perform measurements in triplicate.
- Data Interpretation: Strong biofilm formers typically exhibit less negative ζ-potentials in early stages compared to weak formers, with potentials becoming progressively more negative through maturation stages [57]. These electrostatic differences directly impact cationic antibiotic penetration.
Research Reagent Solutions
Table 2: Essential Research Materials for Antibiotic Penetration Studies
| Reagent/Category | Specific Examples | Research Application | Key Considerations |
|---|---|---|---|
| Biofilm Reactor Systems | Continuous-flow rotating annular bioreactor (CFRAB); Calgary biofilm device; Flow cell systems | Controlled biofilm cultivation under hydrodynamic conditions | CFRAB enables real-time sorption studies; ensure coupon materials match research questions |
| Antibiotic Classes | Ciprofloxacin (fluoroquinolone); Erythromycin (macrolide); Sulfamethoxazole (sulfonamide); β-lactams | Sorption kinetics, penetration studies, MBEC determination | Select based on charge characteristics (pH-dependent); include clinical relevance |
| Analytical Instruments | LC-MS/MS; Zeta-potential analyzer; Microplate spectrophotometer | Antibiotic quantification; surface charge measurement; biofilm quantification | LC-MS/MS sensitivity crucial for environmental concentrations; validate methods for biofilm matrices |
| Biofilm Quantification Assays | Crystal violet; Resazurin reduction; ATP luminescence; CFU enumeration | Biomass quantification; metabolic activity; viable cell count | Crystal violet measures total biomass; metabolic assays reflect viability; combine methods |
| Enzyme Inhibitors | β-lactamase inhibitors (clavulanate, avibactam); Efflux pump inhibitors | Mechanism dissection; combination therapy studies | Use to distinguish between penetration failure and enzymatic degradation |
| Standard Strains & Controls | S. aureus ATCC 35556 (strong biofilm); S. epidermidis ATCC 35984 & isogenic mutant M7 (weak) | Assay standardization; quality control | Essential for inter-laboratory reproducibility; validate biofilm-forming capacity |
Emerging Strategies and Research Directions
Novel Intervention Approaches
Confronting the penetration problem requires innovative strategies that move beyond traditional antibiotic discovery:
- Enzyme Cocktail Formulations: Strategic combinations of β-lactamases (e.g., CTX-M-33 + VIM-1 at 4:1 ratio) demonstrate that broad-spectrum enzymatic degradation of environmental antibiotics is achievable, with potential applications in wastewater treatment and infection control [69].
- Biofilm Electrostatic Manipulation: The correlation between ζ-potential and biofilm formation strength suggests potential interventions targeting the initial attachment phase through surface charge modification [57].
- Antibiotic Concentration Optimization: Research reveals unexpected biofilm responses to antibiotic concentrations, with lower concentrations sometimes reducing biofilm followed by increased biomass at higher concentrations. This suggests the existence of optimal treatment windows rather than simple dose escalation [57].
- Non-Traditional Antimicrobials: Bacteriophages, lysins, and microbiome modulation represent promising alternatives that circumvent conventional penetration barriers [70].
Technological Innovations and Future Outlook
The field faces significant challenges, including the exodus of large pharmaceutical companies from antibiotic research and development, with most innovation now occurring in academic settings and small biotech companies [70]. However, emerging technologies offer promising avenues:
- Advanced Diagnostic Integration: "Theranostic" approaches that couple rapid pathogen identification with targeted antibiotic selection could optimize therapy before extensive biofilm establishment.
- CRISPR-Cas Systems: Potential application for targeted elimination of resistance genes within biofilm communities.
- Nanoparticle Delivery Systems: Engineered carriers designed to penetrate biofilm matrices and release antibiotics at predetermined rates.
- Immune Modulation: Adjunct therapies that enhance innate immune clearance of biofilm-associated infections.
The economic challenges remain substantial, with most new antibiotics generating insufficient revenue to sustain development programs despite their critical societal value [70]. Overcoming the penetration problem will require not only scientific innovation but also new economic models that recognize the full value of effective antimicrobial therapies.
The penetration problem represents a multifaceted challenge in biofilm-associated infections, encompassing sorption, binding, and enzymatic degradation mechanisms that collectively reduce antibiotic efficacy. Addressing this problem requires sophisticated experimental approaches that account for biofilm-specific properties, including their developmental stage, electrostatic characteristics, and matrix composition. The methodologies outlined in this whitepaper provide researchers with standardized protocols for investigating these mechanisms, while emerging strategies offer promising avenues for clinical intervention. As antibiotic resistance continues to outpace drug development, innovative approaches to circumvent penetration barriers will be essential for maintaining effective therapies against biofilm-associated infections.
Metabolic Heterogeneity and the Persister Cell Phenomenon
Within the structured environment of a biofilm, bacterial populations face gradients of nutrients, oxygen, and metabolic waste products. This spatial heterogeneity gives rise to metabolically distinct subpopulations, a phenomenon where individual bacterial cells within the same community exhibit vastly different physiological states [71]. Among these subpopulations, bacterial persisters—dormant or slow-growing phenotypic variants—play a critical role in therapeutic failure. Unlike genetically resistant bacteria, persisters remain genetically susceptible to antibiotics but survive treatment due to their profound metabolic quiescence, only to resume growth once antibiotic pressure is removed, leading to relapsing infections [72] [73].
The formation of persisters is intrinsically linked to the biofilm lifestyle. As the biofilm matures, the extracellular polymeric substance (EPS) matrix and the consumption of resources by peripheral cells create physical and chemical gradients [71]. This results in microenvironments where conditions such as oxygen availability vary drastically from the biofilm periphery to its core. Cells in oxygen-depleted, nutrient-poor regions often enter a dormant state as a survival strategy, which concurrently renders them tolerant to many conventional antibiotics that target active cellular processes [2] [74]. Understanding this metabolic heterogeneity is therefore fundamental to overcoming the dual challenges of biofilm-mediated resistance and antibiotic treatment failure.
Mechanisms of Metabolic Heterogeneity in Biofilms
Gradient Formation and Microenvironment Variation
The biofilm matrix acts as a barrier that hinders the free diffusion of molecules, leading to the establishment of steep physical and chemical gradients from the point of closest contact with the bulk fluid to the deepest layers of the biofilm structure [71]. Oxygen, often the most rapidly depleted resource, typically forms a concentration gradient starting from the biofilm-fluid interface and becoming undetectable in the inner core [71]. This gradient formation has profound consequences for cellular activity.
The resulting metabolic heterogeneity means that cells in a single biofilm community occupy different functional niches. This spatial organization fosters a form of division-of-labor, where subpopulations carrying out distinct metabolisms can engage in cross-feeding [71]. For instance, computer simulations and experimental validation with Escherichia coli have demonstrated that cells in the anoxic lower layers of a biofilm can ferment glucose and produce acetate, which then diffuses upwards to be respired by aerobic cells in the oxic zone [71]. This optimized use of resources enhances the overall fitness and resilience of the biofilm community.
Molecular Basis of Persister Cell Formation
The transition to a persistent state is regulated by a complex network of interconnected molecular pathways that sense stress and enforce metabolic dormancy. These pathways include:
- Toxin–Antitoxin (TA) Modules: These systems consist of a stable toxin and a labile antitoxin. Under stress conditions, the antitoxin is degraded, allowing the toxin to disrupt essential cellular processes such as translation and replication. For example, the HipA toxin phosphorylates and inactivates glutamyl-tRNA synthetase, inhibiting translation and triggering growth arrest [72] [73].
- (p)ppGpp-Mediated Stringent Response: Nutrient limitation triggers the rapid synthesis of the alarmone (p)ppGpp. This molecule orchestrates a dramatic reprogramming of cellular physiology by repressing rRNA and tRNA synthesis, thereby shutting down resource-intensive processes like growth and division [72].
- Redox and ROS-Induced Stress Responses: Exposure to antibiotics can generate reactive oxygen species (ROS). Bacterial defense systems, including superoxide dismutases and catalases, are activated to mitigate this oxidative damage, promoting survival in a non-growing state [72] [74].
These mechanisms collectively drive the bacterial subpopulation into a state of metabolic quiescence or dormancy, which is the fundamental basis for their tolerance to antimicrobial agents [73].
Quantitative Analysis of Persister Cell Metabolism
Advanced metabolic tracing techniques have revealed the profound shutdown of central metabolic pathways in persister cells. The following table summarizes key quantitative findings from isotopic labeling studies.
Table 1: Metabolic Flux Analysis in Normal and Persister Cells
| Metabolic Parameter | Normal Cells | Persister Cells | Experimental Context |
|---|---|---|---|
| Overall Metabolic Activity | High | Uniformly reduced | E. coli with 13C-glucose tracing [75] |
| Labeling Dynamics in Peripheral Pathways | Rapid incorporation of 13C | Delayed incorporation | E. coli; pathways include PPP and TCA cycle [75] |
| Proteinogenic Amino Acid Labeling | Robust and generalized | Generalized but reduced | E. coli with 13C-glucose [75] |
| Metabolic Activity on Acetate | Functional TCA cycle | Near-complete shutdown | E. coli with 13C-acetate [75] |
| ATP Levels | High | Lowered | Linked to target inactivity in S. aureus [74] |
| Efficacy of Bactericidal Antibiotics | High | Strongly correlated with metabolic rate | General principle across species [72] |
The data demonstrates that persisters are not merely slow-growing but exist in a unique metabolic state characterized by a global reduction in anabolic activity. This state is flexible and adapts to the available carbon source, with acetate conditions provoking a more substantial metabolic shutdown than glucose, likely due to the higher ATP cost of activating acetate for entry into central metabolism [75].
Experimental Protocols for Investigating Persister Metabolism
Isotopic Tracer Analysis of Persister Cell Metabolic Flux
This protocol is designed to directly measure the functional activity of metabolic pathways in persister cells using stable isotope labeling and mass spectrometry [75].
Key Research Reagents:
- E. coli BW25113 (or relevant bacterial strain)
- Carbonyl cyanide m-chlorophenyl hydrazone (CCCP)
- M9 minimal medium
- 1,2-13C2 glucose or 2-13C sodium acetate (Cambridge Isotope Laboratories, Inc.)
- Liquid Nitrogen for metabolic quenching
- Methanol-water (80:20) extraction solution
- 6 N HCl for protein hydrolysis
Procedure:
- Culture and Persister Induction:
- Grow an overnight culture of E. coli in M9 medium with 2 g/L glucose.
- Sub-culture into fresh medium to an OD600 of 0.05 and incubate at 37°C with shaking (200 rpm).
- When the sub-culture reaches OD600 of 0.5, induce persister formation by adding 100 μg/mL of CCCP. Incubate for 15 minutes at 37°C with shaking.
- Collect cells by centrifugation (3 min, 13,000 rpm, room temperature) and wash three times with carbon-free M9 medium.
13C Labeling and Sampling:
- Resuspend control and CCCP-induced cell pellets in M9 medium to a high density (OD600 of 5).
- Immediately initiate labeling by adding 2 g/L of 13C-glucose or 13C-acetate.
- Incubate at 37°C with shaking.
- At critical timepoints (0, 20 seconds, 5 min, 30 min, 2 h), withdraw samples and rapidly quench metabolic activity by submerging in liquid nitrogen within a few seconds.
- Centrifuge the quenched samples (5,000 × g, 3 min, 4°C) and store pellets at -80°C.
Metabolite and Proteinogenic Amino Acid Analysis:
- Lyophilize the cell pellets.
- For free metabolite analysis, extract the lyophilized biomass with 80:20 methanol-water. Analyze the filtered supernatant using LC-MS (e.g., ThermoFisher Q-Exactive system with a HILIC-Z column).
- For proteinogenic amino acid analysis, hydrolyze the remaining pellet with 6N HCl at 100°C for 18 hours. Derivatize the hydrolyzed amino acids and analyze using GC-MS (e.g., via the TBDMS method).
The workflow for this detailed protocol is visualized in the following diagram:
Research Reagent Solutions
Table 2: Essential Reagents for Metabolic Tracing in Persister Cells
| Reagent / Material | Function / Application | Example Specification |
|---|---|---|
| 13C-labeled Substrates | Tracer for metabolic flux analysis; reveals pathway activity | 1,2-13C2 Glucose; 2-13C Sodium Acetate [75] |
| Membrane Depolarizer | Induces persister formation chemically for sufficient biomass | Carbonyl Cyanide m-Chlorophenyl Hydrazone (CCCP) [75] |
| Liquid Chromatography-Mass Spectrometry (LC-MS) | Analyzes labeling in free, fast-turnover metabolic intermediates | High-resolution system (e.g., ThermoFisher Q-Exactive) [75] |
| Gas Chromatography-Mass Spectrometry (GC-MS) | Analyzes labeling in proteinogenic amino acids (slower turnover) | With TBDMS derivatization protocol [75] |
| Quenching Solution | Instantly halts metabolism for accurate snapshot of fluxes | Liquid Nitrogen [75] |
Therapeutic Strategies Targeting Metabolic Heterogeneity
The deepened understanding of persister cell metabolism has shifted therapeutic paradigms from direct killing to metabolic reactivation. The "wake and kill" strategy aims to re-sensitize dormant persisters to conventional antibiotics by forcing them back into a metabolically active state [72]. This approach leverages the strong positive correlation between bacterial metabolic rate and the efficacy of bactericidal antibiotics [72].
Key therapeutic avenues include:
- Metabolite Adjuvants: Exogenous administration of specific metabolites can stimulate respiration and energy generation in persisters. For instance, mannitol and pyruvate have been shown to enhance the susceptibility of Pseudomonas aeruginosa and Vibrio alginolyticus persisters to aminoglycoside antibiotics by restoring the proton motive force (PMF) required for drug uptake [72].
- Targeting Central Carbon Metabolism: Interventions that reactivate the tricarboxylic acid (TCA) cycle and electron transport chain can increase cellular ATP levels, making the cell vulnerable to antibiotics. Conversely, exploiting the unique metabolic dependencies of persisters, such as their reliance on glycolysis or specific amino acid pools under stress, offers another target for synergistic drug combinations [72] [73].
The following diagram illustrates the core concept of the "wake and kill" strategy and its molecular underpinnings:
Despite promising preclinical results, significant translational challenges remain. Maintaining effective local concentrations of metabolites in complex infectious niches, such as biofilms or caseous granulomas, is difficult [72]. Furthermore, potential off-target effects on host cells and the risk of accelerating resistance evolution if monotherapies are used necessitate careful formulation and combination treatment design [72].
Metabolic heterogeneity is not a random occurrence but a fundamental, organized feature of biofilm biology that drives the formation and maintenance of persister cells. The interplay between gradient formation within the biofilm matrix and the activation of molecular dormancy programs creates a protected, tolerant subpopulation that conventional antibiotics fail to eradicate. The application of advanced techniques like isotopic tracer analysis has been instrumental in moving beyond transcriptional profiles to define the functional metabolic state of persisters, revealing a landscape of global reduction but context-dependent adaptability.
Future research must focus on translating this mechanistic understanding into clinically viable therapies. This will require optimizing "wake and kill" adjuvants for delivery to biofilm-infected sites, identifying biomarkers for metabolic heterogeneity in clinical isolates, and designing sophisticated combination regimens that preempt resistance. By targeting the very metabolic pathways that underpin persistence, we can develop more effective strategies to combat chronic and relapsing biofilm infections.
Bacterial biofilms are structured communities of microbial cells encased in a self-produced matrix of extracellular polymeric substances (EPS) that enable bacteria to survive in hostile environments [16]. This EPS matrix, composed of polysaccharides, proteins, extracellular DNA (eDNA), and lipids, forms a formidable biological barrier that severely restricts antibiotic penetration and contributes to antimicrobial resistance (AMR) levels up to 1000 times greater than those observed in planktonic bacteria [76] [2]. The unique architectural and physiological characteristics of biofilms—including gradient formation, metabolic heterogeneity, and the presence of persister cells—create multiple resistance mechanisms that conventional antibiotics cannot effectively overcome [77] [2]. This challenge has motivated the development of innovative nanotechnologies capable of penetrating the biofilm matrix and delivering antimicrobial agents directly to the embedded bacterial cells.
Nanoparticles (NPs) have emerged as a promising platform for combating biofilm-associated infections due to their unique physicochemical properties [76]. These nanoscale systems (typically 1-1000 nm) can be engineered to breach the EPS barrier, target specific biofilm components, and release high local concentrations of antimicrobials directly at the infection site [78] [79]. The strategic application of nanotechnology represents a paradigm shift in approaching the persistent challenge of biofilm-mediated resistance, offering new hope for treating chronic infections that have long evaded conventional therapeutic approaches.
Biofilm Matrix Composition and Resistance Mechanisms
Architectural Complexity of the Biofilm Matrix
The biofilm matrix is a highly organized, heterogeneous structure that provides structural stability and protection for embedded microbial communities. This extracellular scaffold typically consists of 75-90% EPS, with microbial cells accounting for only 10-25% of the total volume [10]. The composition varies significantly between species and environmental conditions, but generally includes:
- Polysaccharides: Such as Pel, Psl, and alginate in Pseudomonas aeruginosa biofilms, which act as molecular adhesives for surface colonization and provide structural integrity [10].
- Extracellular proteins: Including secreted proteins, cell surface adhesins, and protein subunits of appendages like pili and flagella that stabilize the matrix architecture [10].
- Extracellular DNA (eDNA): Provides structural support and contributes to the negative charge of the matrix, enabling cation retention and interaction with other EPS components [2].
- Lipids and other biopolymers: That contribute to matrix hydrophobicity and barrier functions [2].
This complex matrix operates as a dynamic ecosystem, with components interacting through various forces including electrostatic interactions, hydrogen bonding, and van der Waals forces [10]. The resulting three-dimensional architecture features water channels that facilitate nutrient circulation and waste removal, while simultaneously impeding the penetration of antimicrobial agents [16] [2].
Mechanisms of Antibiotic Penetration Resistance
The biofilm matrix confers resistance through multiple synergistic mechanisms that collectively prevent effective antibiotic concentrations from reaching their bacterial targets:
- Physical barrier function: The dense, anionic matrix components, particularly eDNA and polysaccharides, can bind to antibiotics (especially positively charged aminoglycosides), significantly retarding their diffusion and creating a concentration gradient that decreases toward the biofilm interior [77] [2].
- Chemical degradation: Some matrix components possess enzymatic activity that can degrade or modify antibiotics before they reach their cellular targets [2].
- Metabolic heterogeneity: Nutritional and oxygen gradients within biofilms create distinct metabolic zones, with cells in deeper layers entering dormant or slow-growing states that render them less susceptible to time-dependent antibiotics [2].
- Persister cell formation: A subpopulation of metabolically dormant bacterial cells within biofilms exhibits exceptional tolerance to antimicrobials without genetic resistance mechanisms, enabling biofilm regeneration after antibiotic pressure ceases [77] [2].
- Enhanced horizontal gene transfer: The confined matrix environment facilitates efficient exchange of resistance genes between bacteria, accelerating the development of antimicrobial resistance [76] [2].
Table 1: Primary Components of the Biofilm Extracellular Polymeric Substance (EPS) Matrix and Their Roles in Antimicrobial Resistance
| Matrix Component | Percentage Composition | Primary Functions in Resistance |
|---|---|---|
| Polysaccharides | 1-2% of total biofilm mass [10] | Structural integrity; molecular sieve; antibiotic binding |
| Proteins | <1-2% of total biofilm mass [10] | Enzyme-mediated antibiotic degradation; structural support |
| Extracellular DNA (eDNA) | <1-2% of total biofilm mass [10] | Structural scaffold; cation retention; antibiotic binding |
| Water | Up to 97% of total biofilm mass [10] | Medium for nutrient/waste transport; hydration |
| Microbial cells | 2-5% of total biofilm mass [10] | Metabolic functions; persistence; resistance gene exchange |
Nanoparticle Mechanisms Against Biofilms
Penetration and Distribution in Biofilm Matrix
Nanoparticles exploit unique transport mechanisms to penetrate the biofilm matrix, overcoming limitations that restrict conventional antibiotics. Their small size (typically 20-400 nm) enables passive diffusion through the interstitial pores and water channels within the EPS [79]. Surface properties can be engineered to minimize interactions with matrix components that would otherwise trap or exclude the particles. Cationic nanoparticles, for instance, may initially be retarded through binding with anionic eDNA but can subsequently disrupt these interactions through charge neutralization, facilitating deeper penetration [76] [79].
The penetration efficiency is influenced by multiple factors including nanoparticle size, surface charge, hydrophobicity, and shape. Spherical particles with neutral or slightly negative surface charges typically demonstrate superior penetration compared to their cationic or irregularly shaped counterparts, as they experience reduced non-specific binding to the negatively charged matrix components [79]. Furthermore, certain nanoparticles can leverage active penetration mechanisms, including the generation of local forces that temporarily disrupt matrix integrity or the enzymatic degradation of specific EPS components to create migration paths [76].
Multimodal Anti-Biofilm Actions
Nanoparticles employ diverse mechanisms to disrupt biofilm integrity and eradicate embedded bacteria, often functioning through several simultaneous pathways:
- Reactive Oxygen Species (ROS) Generation: Metal and metal oxide nanoparticles (e.g., Ag, ZnO, TiO₂) can produce superoxide radicals, hydrogen peroxide, and hydroxyl radicals that induce oxidative stress, damaging bacterial membranes, proteins, and DNA [76]. This oxidative burst can simultaneously disrupt EPS components and directly kill bacterial cells.
- EPS Matrix Disruption: Nanoparticles can directly interact with and destabilize the biofilm architecture through charge-based interactions with eDNA, enzymatic degradation of polysaccharides (e.g., DNase-functionalized particles), or catalytic cleavage of key structural bonds [76] [78].
- Quorum Sensing Interference: Functionalized nanoparticles can deliver quorum sensing inhibitors (e.g., synthetic furanones, peptide-based compounds) that block bacterial cell-to-cell communication, preventing the coordination of biofilm development and virulence factor expression [76] [78].
- Enhanced Drug Delivery and Retention: Nanoparticles can encapsulate conventional antibiotics, protecting them from degradation and enzymatic inactivation while facilitating their penetration and providing sustained release within the biofilm interior, thereby maintaining localized therapeutic concentrations [78] [80].
Experimental Models and Methodologies
Standardized Biofilm Cultivation Models
Research on nanoparticle-biofilm interactions employs various well-established models that simulate different aspects of biofilm growth and architecture:
- Static Microtiter Plate Models: The simplest and most widely used screening method, involving biofilm formation on polystyrene plates followed by treatment with nanoparticle suspensions and quantification via crystal violet staining or metabolic activity assays [16] [10]. This high-throughput approach allows initial efficacy screening but lacks the fluid dynamics of natural biofilm environments.
- Flow Cell Systems: Continuous-culture chambers that enable real-time microscopic observation of biofilm development and nanoparticle penetration under controlled shear stress conditions [2]. These systems more accurately mimic natural biofilms found in medical devices and physiological environments, allowing assessment of spatial distribution and penetration kinetics.
- Biofilm Reactors: Larger-scale systems (e.g., Calgary, CDC, drip flow reactors) that generate substantial biomass for evaluating anti-biofilm efficacy, nanoparticle transport, and pharmacodynamic parameters [16]. These models produce biofilms with well-defined chemical gradients and are particularly useful for studying penetration dynamics.
- Explant and Tissue Models: Biofilms grown on biological surfaces (e.g., human mucosal tissue, surgical implant materials) that incorporate host matrix components and better simulate clinical infection scenarios [2]. These models are essential for evaluating nanoparticle performance in the presence of host proteins and biological barriers.
Quantifying Nanoparticle Penetration and Efficacy
Advanced analytical techniques are employed to characterize nanoparticle interactions with biofilms:
- Confocal Laser Scanning Microscopy (CLSM): Enables non-invasive, three-dimensional visualization of nanoparticle distribution within intact biofilms using fluorescently labeled nanoparticles or intrinsic autofluorescence [79]. This technique can quantify penetration depth and spatial distribution patterns.
- Scanning Electron Microscopy (SEM): Provides high-resolution imaging of nanoparticle localization on biofilm surfaces and ultrastructural changes following treatment [80]. Environmental SEM allows observation of hydrated biofilms without extensive processing.
- Microelectrode Measurements: Used to map chemical gradients (O₂, pH, antimicrobial concentrations) within biofilms before and after nanoparticle treatment, providing insights into functional penetration and physiological effects [2].
- Spectroscopic Techniques: Fourier-transform infrared (FTIR) and Raman spectroscopy can identify molecular interactions between nanoparticles and biofilm components, revealing binding events and chemical modifications [80].
Table 2: Quantitative Efficacy Metrics of Selected Nanoparticle Formulations Against Biofilms
| Nanoparticle Type | Antimicrobial Payload | Target Pathogen | Biofilm Reduction | Key Efficacy Findings |
|---|---|---|---|---|
| Polycaprolactone Nanospheres [80] | Imipenem | Carbapenem-resistant K. pneumoniae | >80% | 8-fold MIC reduction vs free drug; significant suppression of blaKPC, blaNDM resistance genes |
| Metal Nanoparticles (Ag, ZnO) [76] | None (intrinsic activity) | ESKAPE pathogens | 70-90% | ROS-mediated damage; EPS disruption; synergistic with antibiotics |
| Lipid-Based Systems [76] | Various antibiotics | P. aeruginosa | 65-85% | Enhanced mucus penetration; sustained drug release |
| Functionalized Polymeric NPs [78] | Quorum sensing inhibitors | S. aureus | 60-80% | Inhibition of biofilm maturation; reduced virulence factor expression |
Case Study: Polycaprolactone Nanospheres for Drug-Resistant Klebsiella pneumoniae
Synthesis and Characterization Methodology
A recent investigation demonstrated the efficacy of polycaprolactone (PCL) nanospheres against carbapenem-resistant Klebsiella pneumoniae (CRKP) biofilms [80]. The experimental protocol encompassed the following stages:
Nanoparticle Synthesis via Double Emulsion Solvent Evaporation:
- Primary emulsion: 10% (w/w) imipenem was dissolved in 5 mL distilled water (internal aqueous phase) and emulsified into 20 mL dichloromethane containing 2 g PCL (oil phase) using homogenization at 30,000 rpm for 2 minutes.
- Secondary emulsion: The primary water-in-oil (w/o) emulsion was added dropwise into 100 mL of 1% (w/v) polyvinyl alcohol (PVA) solution with continuous stirring at 550 rpm for 2 hours to facilitate solvent evaporation and nanoparticle hardening.
- Recovery and purification: Nanoparticles were collected by centrifugation, washed three times with deionized water to remove residual PVA, and air-dried at room temperature for 24 hours followed by vacuum drying at 25°C for 12 hours.
Physicochemical Characterization:
- Size and morphology: Dynamic light scattering (DLS) analysis revealed an average particle size of 610 ± 125 nm with spherical morphology confirmed by scanning electron microscopy (SEM).
- Surface charge: Zeta potential measurements showed slightly negative surface charge (-12.3 ± 2.1 mV), favorable for reduced non-specific binding to anionic biofilm components.
- Drug loading and encapsulation: High encapsulation efficiency (84.5%) was achieved, with drug loading capacity of 7.8% w/w.
- In vitro release profile: Sustained release over 8 days with an initial burst release (≈40% within first 24 hours) followed by gradual release, maintaining therapeutic concentrations.
Anti-Biofilm Efficacy Assessment
The anti-biofilm activity of imipenem-loaded PCL nanospheres was evaluated through comprehensive phenotypic and molecular analyses:
Biofilm Inhibition Assay:
- CRKP isolates were cultured in 96-well plates for 24 hours to establish mature biofilms.
- Biofilms were treated with free imipenem, blank PCL nanospheres, or imipenem-loaded nanospheres at equivalent concentrations.
- After incubation, biofilms were quantified using crystal violet staining and metabolic activity assays (MTT).
- Imipenem-loaded nanospheres demonstrated superior biofilm inhibition (>80%) compared to free imipenem (45%) at the same concentration, indicating enhanced penetration and retention.
Gene Expression Analysis:
- RNA was extracted from treated and untreated CRKP biofilms.
- Quantitative PCR was performed to assess expression of key resistance genes (blaKPC, blaNDM).
- Imipenem-loaded nanospheres significantly suppressed resistance gene expression (4.2-fold reduction in blaKPC; 3.7-fold reduction in blaNDM) compared to free drug treatment.
Time-Kill Kinetics:
- CRKP biofilms were exposed to treatments and bacterial viability was assessed at predetermined intervals over 24 hours.
- Imipenem-loaded nanospheres achieved complete bacterial eradication within 12 hours, while free imipenem showed regrowth after 18 hours.
The Scientist's Toolkit: Essential Research Reagents and Materials
Table 3: Key Research Reagents for Nanoparticle Biofilm Penetration Studies
| Reagent/Material | Function/Application | Specific Examples |
|---|---|---|
| Polycaprolactone (PCL) | Biodegradable polymer for nanoparticle synthesis; provides sustained release kinetics [80] | PCL (MW 80,000 Da) for nanosphere formulation via double emulsion methods |
| Polyvinyl Alcohol (PVA) | Stabilizer and emulsifier in nanoparticle synthesis; controls particle size distribution [80] | 1% (w/v) PVA solution for secondary emulsion stabilization |
| Dichloromethane (DCM) | Organic solvent for polymer dissolution in emulsion-based synthesis [80] | Solvent for PCL in oil phase of double emulsion preparation |
| Dimethyl Sulfoxide (DMSO) | Solvent for hydrophobic compounds; cryopreservation of bacterial strains | Stock solution preparation for quorum sensing inhibitors |
| Crystal Violet | Biofilm biomass staining and quantification [10] | 0.1% solution for static microtiter plate biofilm assays |
| Resazurin (Alamar Blue) | Metabolic activity indicator for viability assessment in treated biofilms | Fluorescent/colorimetric measurement of bacterial metabolic state |
| Mueller Hinton Broth | Standardized medium for antibiotic susceptibility testing | CLSI-recommended medium for MIC determination against planktonic cells |
| Tryptic Soy Broth (TSB) | Nutrient-rich medium for robust biofilm formation | Enhanced EPS production in staphylococcal and enterobacterial biofilms |
| DNase I | Enzyme for EPS disruption; study of eDNA role in nanoparticle penetration [10] | Matrix degradation controls; nanoparticle functionalization |
| Dispersion B | Glycosyl hydrolase that degrades polysaccharide matrix components [10] | EPS disruption studies; enhancement of nanoparticle penetration |
The development of nanoparticle-based delivery systems represents a transformative approach to overcoming the fundamental challenge of biofilm penetration resistance. By engineering nanoscale carriers with tailored physicochemical properties, researchers can now breach the EPS barrier that has long protected bacterial communities from antimicrobial agents. The multimodal mechanisms employed by nanoparticles—including ROS generation, matrix disruption, quorum sensing interference, and targeted drug delivery—provide a comprehensive strategy against structured microbial communities.
Future advancements in this field will likely focus on personalized nanomedicine approaches that account for the specific composition of clinical biofilms, which varies significantly between infection sites and patient populations [79]. The integration of stimuli-responsive materials that activate antimicrobial release in response to biofilm-specific cues (e.g., pH, enzymes, hypoxia) represents another promising direction [78]. Additionally, combination therapies leveraging nanoparticles with different mechanisms of action may provide synergistic effects that prevent resistance development.
As nanotechnology continues to evolve, these sophisticated delivery systems hold exceptional promise for addressing one of medicine's most persistent challenges—the eradication of biofilm-associated infections that have long evaded conventional therapeutic approaches. The convergence of materials science, microbiology, and pharmaceutical development in this domain heralds a new era in anti-infective therapy with the potential to significantly impact clinical outcomes for patients suffering from chronic bacterial infections.
Biofilms, structured communities of microorganisms encased in an extracellular polymeric substance (EPS), represent a significant challenge in clinical settings due to their extreme tolerance to antimicrobial agents [81]. This resilience is a primary contributor to the persistence of chronic infections associated with medical devices and wounds, underpinning a global health crisis [29] [82]. The protective biofilm matrix, alongside the presence of metabolically dormant persister cells, creates a dual barrier that conventional antibiotics cannot effectively overcome [83]. The investigation of biofilm matrix composition has revealed that its integrity is fundamental to the phenomenon of antibiotic penetration resistance. In response, the field is shifting from single-mode interventions to innovative combinatorial strategies. These approaches are designed to simultaneously disrupt the physical matrix and sensitize the embedded bacterial cells to antimicrobial agents, offering a promising pathway to overcome biofilm-associated therapeutic failures [84] [85] [30]. This whitepaper synthesizes current research and methodologies, providing a technical guide for developing targeted therapies against biofilm-mediated infections.
Biofilm Matrix Composition and Its Role in Resistance
The extracellular polymeric substance (EPS) is a complex, dynamic matrix that constitutes the structural backbone of biofilms and is the primary mediator of their resistance. The EPS is not a mere physical barrier; it is a functional, organized ecosystem that actively contributes to bacterial survival under antimicrobial stress [83] [82].
Key Components of the EPS
- Polysaccharides: Common polysaccharides such as Psl, Pel, and alginate in Pseudomonas aeruginosa biofilms, and poly-N-acetylglucosamine (PNAG) in Staphylococcus aureus, provide scaffold integrity and can bind to antimicrobial agents, neutralizing their activity [81] [84].
- Proteins: Extracellular proteins function as structural adhesins, enzymes, and toxins. Their network contributes to the matrix's mechanical stability and defense capabilities [86].
- Extracellular DNA (eDNA): eDNA serves as a crucial structural scaffold, particularly in the biofilm's basal layers. It also contributes to the matrix's negative charge, which can bind and sequester positively charged aminoglycoside antibiotics [81] [82].
- Lipids and Other Biomolecules: These components further contribute to the matrix's heterogeneity and functional complexity [83].
Mechanisms of Matrix-Mediated Resistance
The EPS confers resistance through multiple, synergistic mechanisms, which are summarized in Table 1 below.
Table 1: Primary Mechanisms of Biofilm-Associated Antimicrobial Resistance
| Mechanism | Functional Impact | Consequence |
|---|---|---|
| Physical Barrier | The dense, anionic matrix restricts the diffusion of antimicrobial molecules [81] [30]. | Reduced antibiotic concentration at the target cell layer. |
| Molecular Sequestration | Cationic antibiotics (e.g., aminoglycosides) bind to anionic components like eDNA and polysaccharides [81]. | Antibiotic neutralization and failure to reach cellular targets. |
| Metabolic Heterogeneity | Gradients of nutrients, oxygen, and waste products create zones of slow or non-growing cells [83]. | Reduced efficacy of antibiotics that target active cellular processes. |
| Horizontal Gene Transfer | The dense, protected environment facilitates the exchange of mobile genetic elements carrying resistance genes [29] [83]. | Accelerated dissemination of antibiotic resistance genes within the microbial community. |
Core Strategies for Matrix Disruption and Cell Sensitization
Combinatorial approaches are founded on the principle of attacking multiple vulnerable points in the biofilm structure simultaneously. The core logic of this strategy is visualized in the following diagram.
Enzymatic Disruption of the EPS
Enzymes offer a highly specific means to degrade the key structural components of the EPS. While single-enzyme therapy has limited efficacy, combinations that target multiple matrix components show synergistic activity [85] [86].
Table 2: Enzymes for Targeted EPS Component Degradation
| EPS Target | Enzyme Class | Example Enzymes | Mechanism of Action |
|---|---|---|---|
| Proteins | Protease | Trypsin, Serine endoprotease | Cleaves peptide bonds in structural and functional matrix proteins, destabilizing the architecture [86]. |
| Polysaccharides | Glycoside Hydrolase | β-glucosidase, Dispersin B | Hydrolyzes glycosidic bonds in exopolysaccharides like Psl and Pel, dissolving the polysaccharide scaffold [85] [86]. |
| eDNA | Nuclease | DNase I | Degrades the eDNA scaffold, which is critical for biofilm structural integrity and cation-mediated sequestration [81] [86] [82]. |
Experimental Protocol: Evaluating Combinatorial Enzymes against Dual-Species Biofilms
This protocol is adapted from studies investigating S. aureus and P. aeruginosa biofilms, common co-inhabitants in chronic wounds [86].
Biofilm Cultivation:
- Utilize an in vitro wound-like medium (WLM) containing human plasma, Bolton broth, gelatin, and laked sheep red blood cells to mimic the in vivo environment.
- Inoculate 1.5 ml microtubes with 10 μl of a bacterial mixture (e.g., ~1×10⁶ CFU/ml each of S. aureus and P. aeruginosa) and incubate at 37°C for 24 hours to form mature biofilms.
Enzyme Preparation:
- Prepare stock solutions of Trypsin (≥ 10,000 BAEE U/mg), β-glucosidase (10–30 U/mg), and DNase I (> 2500 U/mg) in their respective optimal buffers (e.g., pH 8 for Trypsin, pH 5 for β-glucosidase, pH 7.5 for DNase I).
Treatment and Efficacy Assessment:
- Gently wash the formed biofilms with sterile saline to remove planktonic cells.
- Expose biofilms to single enzymes and combinatorial mixtures (e.g., Trypsin 0.15 μg/ml + DNase I 50 U/ml) for a specified period (e.g., 24 hours).
- Quantitative Analysis: Use viable cell counting after biofilm dispersal or metabolic assays (e.g., resazurin) to quantify biofilm viability.
- Qualitative Analysis: Use Scanning Electron Microscopy (SEM) to visualize structural disintegration of the EPS matrix.
Synergy with Antibiotics:
- Determine the Minimum Biofilm Eradication Concentration (MBEC) of standard antibiotics (e.g., meropenem, amikacin) both alone and in combination with the enzymatic mixture. A significant (e.g., ≥2.5-fold) reduction in MBEC indicates successful sensitization [86].
Nanoparticle-Mediated Delivery and Intrinsic Activity
Engineered nanoparticles (NPs) serve a dual purpose: they act as carriers for therapeutic agents (enzymes, antibiotics, CRISPR-Cas systems) and often possess intrinsic biofilm-disrupting properties [83] [30].
- Penetration Enhancement: NPs can be engineered with specific surface charges and functional groups to facilitate diffusion through the EPS barrier, delivering their payload directly to embedded bacterial cells [84] [30].
- Intrinsic Antimicrobial Activity: Metallic nanoparticles like silver (Ag) and zinc oxide (ZnO) generate reactive oxygen species (ROS), causing oxidative damage to both the EPS and bacterial cells [83].
- Co-delivery Systems: Lipid-based or polymeric NPs can be loaded with multiple cargo types. For instance, a single NP can deliver a CRISPR-Cas system to target a resistance gene alongside an antibiotic, creating a synergistic effect [30].
CRISPR-Cas Based Gene Targeting
The CRISPR-Cas system provides unprecedented precision for targeting the genetic basis of resistance and biofilm formation within bacterial populations [29] [30].
- Mechanism: A guide RNA (gRNA) directs the Cas9 nuclease to introduce double-strand breaks in specific genomic sequences.
- Targets:
- Antibiotic Resistance Genes: Targeting genes like bla (β-lactamase) or mecA (methicillin resistance) can resensitize biofilms to conventional antibiotics [30].
- Quorum Sensing (QS) Genes: Disrupting QS pathways (e.g., lasI/R, rhlI/R in P. aeruginosa) can attenuate virulence and reduce biofilm formation [15].
- Biofilm-Regulating Factors: Genes controlling EPS production (e.g., algD, psl, pel) can be targeted to weaken the matrix structure [30].
- Delivery Challenge and Solution: The key challenge is efficient delivery in situ. Nanoparticles, such as gold or lipid NPs, have been shown to be effective carriers, protecting the CRISPR-Cas machinery and enhancing its delivery into biofilm communities [30]. Liposomal Cas9 formulations have demonstrated >90% reduction in P. aeruginosa biofilm biomass in vitro [30].
The following diagram illustrates a potential workflow for developing and testing a combinatorial nanoparticle and CRISPR-Cas therapy.
The Scientist's Toolkit: Key Reagents and Materials
The following table details essential reagents for conducting research on combinatorial biofilm disruption strategies.
Table 3: Research Reagent Solutions for Combinatorial Biofilm Studies
| Reagent / Material | Function in Research | Example Application Notes |
|---|---|---|
| Trypsin | Protease for degrading the protein component of the EPS. | Use in buffers at pH ~8. Effective concentration for synergy in dual-species biofilms can be as low as 0.15 μg/ml when combined with DNase [86]. |
| DNase I | Nuclease for degrading the eDNA scaffold in the biofilm matrix. | Critical for disrupting biofilms where eDNA is a primary structural element. Used at ~50 U/ml in combinatorial therapy [86] [82]. |
| β-Glucosidase | Glycoside Hydrolase for breaking polysaccharide chains in the EPS. | Targets β-linkages in polysaccharides like Psl and Pel. Effective concentrations can range from 8 U/ml upwards [86]. |
| Engineered Nanoparticles (e.g., Lipid, Gold, Silver) | Carrier for therapeutic agents (enzymes, antibiotics, CRISPR) and/or intrinsic antimicrobial agent. | Gold NPs can enhance CRISPR editing efficiency. Silver NPs generate ROS. Surface functionalization is key for targeted delivery and penetration [83] [30]. |
| CRISPR-Cas9 System (Cas9 nuclease + gRNA) | Precision editing tool for knocking out antibiotic resistance or virulence genes. | gRNA must be designed for specific bacterial targets (e.g., mecA, ndm-1). Requires an efficient delivery vector like NPs for use against biofilms [30]. |
| Wound-Like Medium (WLM) | In vitro culture medium that mimics the in vivo conditions of a chronic wound. | Contains plasma, Bolton broth, gelatin, and RBCs. Essential for generating clinically relevant polymicrobial biofilm models for testing [86]. |
The formidable challenge of biofilm-associated antimicrobial resistance necessitates a paradigm shift from monotherapies to sophisticated, multi-targeted interventions. The combinatorial strategy of disrupting the EPS matrix while sensitizing the resident bacterial cells presents a powerful and logical framework for research and drug development. As detailed in this whitepaper, the integration of enzymatic disruption, nanoparticle technology, and precision genetic tools like CRISPR-Cas can create synergistic effects that are greater than the sum of their parts. The future of combating biofilm-mediated infections lies in the rational design of these combinatorial therapies, which must be guided by a deep understanding of biofilm matrix composition and the molecular mechanisms of antibiotic penetration resistance. The experimental approaches and reagents outlined herein provide a foundational toolkit for scientists and drug development professionals to advance this critical field and translate these promising strategies into effective clinical solutions.
Bench to Bedside: Validating and Comparing Next-Generation Anti-Biofilm Strategies
Bacterial biofilms are surface-adhered microbial communities encased in a self-produced matrix of extracellular polymeric substances (EPS), which play a pivotal role in bacterial pathogenicity and antibiotic resistance [87]. This EPS matrix, consisting of polysaccharides, proteins, glycopeptides, and nucleic acids, forms a formidable physical and functional barrier that restricts antibiotic penetration and inactivates therapeutic agents [88] [76]. Within this protected environment, bacteria exhibit remarkable resistance—up to 1,000-fold higher than their planktonic counterparts—making biofilm-associated infections a major clinical challenge responsible for 65-80% of all microbial infections and 80% of chronic human infections [87] [88].
The unique properties of the biofilm microenvironment, including its electronegative surface charge, hydrophobic character, and acidic, nutrient-limited conditions, further complicate conventional antibiotic treatments [87]. This protected niche promotes bacterial dormancy, facilitates horizontal gene transfer, and enables immune evasion, leading to persistent and recurrent infections that present significant therapeutic challenges [87] [89].
Nanotechnology has emerged as a promising strategy to overcome these barriers. Nanoparticles (NPs), with their small size, high surface area-to-volume ratio, and tunable surface properties, offer innovative approaches to enhance drug delivery, disrupt biofilm integrity, and directly target embedded bacteria [90] [91]. This technical review provides a comprehensive comparison of three major nanoparticle classes—liposomes, polymeric NPs, and metallic NPs—evaluating their efficacy, mechanisms, and practical applications in combating biofilm-mediated antibiotic resistance.
Biofilm Composition and Resistance Mechanisms
Structural Organization and Matrix Components
Biofilm architecture is characterized by a complex, three-dimensional structure that evolves through a five-stage developmental process: (1) reversible attachment, (2) irreversible attachment, (3) microcolony formation, (4) maturation, and (5) active dispersal [87] [90]. A mature biofilm exhibits distinct structural zones including a conditioning layer, connecting layer, and fully developed biofilm layer, all embedded within the viscous EPS matrix [87].
The EPS matrix represents the primary defensive barrier of biofilms, with key components that contribute to its protective functions:
- Polysaccharides: Provide structural integrity and steric hindrance against antimicrobial penetration
- Proteins and glycoproteins: Contribute to matrix adhesion and enzyme-mediated antibiotic inactivation
- Extracellular DNA (eDNA): Facilitates structural stability and genetic exchange for resistance propagation
- Lipids: Enhance hydrophobicity and limit penetration of hydrophilic antibiotics [88] [89]
Mechanisms of Antibiotic Resistance in Biofilms
The biofilm microenvironment confers resistance through multiple interconnected mechanisms:
- Physical barrier function: The dense EPS matrix significantly restricts antibiotic diffusion and penetration, creating concentration gradients that result in sublethal antibiotic exposure to deeply embedded bacteria [87] [89].
- Metabolic heterogeneity: Oxygen and nutrient gradients within the biofilm create distinct metabolic zones, with dormant subpopulations exhibiting reduced susceptibility to antibiotics targeting active cellular processes [88].
- Stress response activation: The biofilm environment induces stress responses that upregulate efflux pumps, DNA repair systems, and general stress resistance mechanisms [90].
- Horizontal gene transfer: The close proximity of cells within the biofilm facilitates the exchange of mobile genetic elements carrying resistance genes, accelerating the development of multidrug-resistant strains [87] [92].
Table 1: Key Biofilm Matrix Components and Their Roles in Antimicrobial Resistance
| Matrix Component | Primary Function | Role in Resistance |
|---|---|---|
| Exopolysaccharides | Structural scaffolding | Physical barrier; steric hindrance |
| Proteins | Adhesion; enzymatic activity | Antibiotic modification; degradation |
| Extracellular DNA | Structural stability; genetic exchange | Resistance gene dissemination |
| Lipids | Hydrophobicity modulation | Reduction of hydrophilic drug uptake |
Nanoparticle-Biofilm Interactions: Fundamental Principles
The efficacy of nanoparticles against biofilms depends on their ability to navigate a three-step interaction process: (1) transport to the biofilm surface, (2) attachment and penetration, and (3) migration within the biofilm matrix [89]. Each step is influenced by a complex interplay of NP characteristics and biofilm properties.
Transport and Attachment Mechanisms
NP transport to biofilm surfaces occurs through Brownian diffusion, gravitational settling, or convective flow in dynamic environments. Upon reaching the biofilm interface, attachment is governed by:
- Electrostatic interactions: Most biofilm matrices carry a net negative charge, favoring attachment of cationic NPs [89].
- Hydrophobic interactions: The hydrophobic nature of many EPS components enhances interactions with similarly hydrophobic NPs [87].
- Specific molecular recognition: Functionalized NPs can exploit receptor-ligand interactions for targeted binding [87] [91].
Penetration and Distribution Within Biofilms
Once attached, NPs must traverse the dense EPS network to reach embedded bacterial cells. Key factors influencing penetration include:
- Size exclusion: NPs smaller than the average pore size of the EPS matrix (typically 20-200 nm) demonstrate superior penetration [89].
- Surface chemistry: NPs with hydrophilic, neutral, or cationic surfaces generally exhibit enhanced diffusion through biofilms compared to anionic or hydrophobic counterparts [89].
- Protein corona formation: Adsorption of biomolecules from the environment can create a "corona" that alters NP surface properties and subsequent interactions with the biofilm matrix [89].
Comparative Analysis of Ant biofilm Nanoparticles
Liposomal Nanoparticles
Liposomes are spherical vesicles composed of phospholipid bilayers with an aqueous interior, capable of encapsulating both hydrophilic and hydrophobic therapeutic agents [88]. Their structural similarity to cell membranes enables unique interactions with bacterial cells and biofilms.
Mechanisms of Action:
- Passive targeting: Conventional liposomes rely on size-dependent penetration and fusion with bacterial membranes for drug release [87] [88].
- Enhanced permeability: Cationic liposomes exploit electrostatic interactions with negatively charged biofilm components for improved retention and penetration [88].
- Smart drug release: Stimuli-responsive liposomes can be engineered to release payload in response to biofilm-specific triggers such as acidic pH, enzymes, or elevated reactive oxygen species [87].
Experimental Protocol: Liposome Preparation and Anti-biofilm Efficacy Testing Materials: Phosphatidylcholine, cholesterol, antibiotic (e.g., gentamicin or vancomycin), rotary evaporator, extrusion apparatus, microplate reader, bacterial strains (e.g., P. aeruginosa or S. aureus).
Methodology:
- Liposome preparation: Dissolve lipid components (7:2 molar ratio of phosphatidylcholine to cholesterol) in organic solvent and evaporate to form thin film using rotary evaporator [88].
- Hydration and drug loading: Hydrate lipid film with antibiotic solution (e.g., 10 mg/mL gentamicin) above phase transition temperature with vigorous vortexing [88].
- Size reduction: Extrude through polycarbonate membranes (100-400 nm) for size uniformity and measure particle size/zeta potential using dynamic light scattering [88].
- Encapsulation efficiency: Separate unencapsulated drug using gel filtration or dialysis and quantify using HPLC or microbiological assay [88].
- Anti-biofilm activity: Treat pre-formed biofilms (24-48h) in 96-well plates with liposomal formulations for 24h, assess viability using resazurin assay or colony counting, and visualize using confocal microscopy with LIVE/DEAD staining [88].
Polymeric Nanoparticles
Polymeric NPs include solid colloidal particles fabricated from natural or synthetic polymers, with common examples including poly(lactic-co-glycolic acid) (PLGA), chitosan, and poly(ε-caprolactone) [87] [91]. These systems offer exceptional versatility in design and functionalization for anti-biofilm applications.
Mechanisms of Action:
- Controlled drug release: Tunable polymer degradation profiles enable sustained antibiotic delivery, maintaining effective concentrations within biofilms for extended periods [87] [91].
- Mucoadhesive properties: Cationic polymers like chitosan establish strong electrostatic interactions with anionic EPS components, enhancing biofilm retention [87].
- Quorum sensing interference: Certain polymeric NPs can disrupt bacterial cell-to-cell communication systems essential for biofilm maintenance and virulence expression [87].
Experimental Protocol: Polymeric NP Fabrication and Biofilm Penetration Assessment Materials: PLGA or chitosan, antibiotic, poly(vinyl alcohol) stabilizer, sonicator, centrifugation equipment, confocal microscopy setup, flow cell system.
Methodology:
- Nanoparticle fabrication: Utilize emulsion-solvent evaporation (for PLGA) or ionotropic gelation (for chitosan) methods with antibiotic incorporation [87].
- Characterization: Determine particle size distribution, zeta potential, drug loading capacity, and in vitro release profile in biofilm-mimicking conditions (e.g., artificial sputum medium) [87].
- Penetration analysis: Incorporate fluorescent markers (e.g., FITC) into NPs and quantify penetration depth and distribution profile in flow cell-grown biofilms using confocal laser scanning microscopy with z-stack analysis [89].
- Anti-biofilm efficacy: Treat established biofilms with NP formulations, assess metabolic activity using XTT assay, and evaluate EPS disruption using polysaccharide-specific staining (e.g., concanavalin A) [87].
Metallic Nanoparticles
Metallic NPs, including those composed of silver, gold, zinc oxide, and iron oxide, exhibit intrinsic antimicrobial activity alongside their drug delivery capabilities [90] [76] [92]. Their unique physicochemical properties enable multimodal mechanisms against biofilms.
Mechanisms of Action:
- Reactive oxygen species generation: Catalytic surfaces produce hydroxyl radicals, superoxide anions, and other ROS that induce oxidative damage to bacterial membranes, proteins, and DNA [90] [92].
- Metal ion release: Gradual dissolution releases antimicrobial ions (e.g., Ag⁺, Zn²⁺) that disrupt cellular functions and membrane integrity [90] [93].
- Direct physical interactions: Nanoscale sharp edges and high surface energy enable physical disruption of bacterial membranes and EPS matrix components [90] [76].
- Photothermal therapy: Gold-based and other metallic NPs can convert light energy to heat under specific wavelengths, generating localized hyperthermia that disrupts biofilm integrity [90].
Experimental Protocol: Metallic NP Synthesis and Anti-biofilm Evaluation Materials: Metal precursors (e.g., AgNO₃, HAuCl₄), reducing agents (e.g., sodium citrate, plant extracts for green synthesis), UV-Vis spectrophotometer, transmission electron microscope, ROS detection reagents.
Methodology:
- NP synthesis: Employ chemical reduction (e.g., citrate reduction for AuNPs) or green synthesis approaches using plant extracts, control size and shape through precursor concentration, temperature, and reaction time [90] [92].
- Physicochemical characterization: Confirm NP formation using UV-Vis spectroscopy (surface plasmon resonance), determine size/morphology using TEM, and assess elemental composition using EDS [90].
- ROS detection: Quantify ROS production using fluorescent probes (e.g., DCFH-DA) in biofilm suspensions and correlate with antibacterial efficacy [90] [92].
- Mechanistic studies: Evaluate membrane damage using propidium iodide uptake, assess EPS disruption using carbohydrate and protein quantification assays, and visualize NP localization within biofilms using electron microscopy [90] [76].
Table 2: Comparative Analysis of Anti-biofilm Nanoparticle Platforms
| Parameter | Liposomal NPs | Polymeric NPs | Metallic NPs |
|---|---|---|---|
| Typical Size Range | 50-500 nm [88] | 50-300 nm [87] | 1-100 nm [90] |
| Drug Loading Capacity | High (hydrophilic core + hydrophobic bilayer) [88] | Moderate to high (depends on polymer-drug affinity) [87] | Low (surface adsorption/conjugation) [90] |
| Key Anti-biofilm Mechanisms | Membrane fusion; sustained release; passive targeting [87] [88] | Controlled release; mucoadhesion; quorum sensing inhibition [87] | ROS generation; ion release; physical disruption [90] [92] |
| Penetration Efficiency | Moderate (size/charge dependent) [88] | High (with optimal surface engineering) [87] | Variable (aggregation in EPS can limit penetration) [89] |
| Toxicity Concerns | Low (biocompatible components) [88] | Low to moderate (polymer-dependent) [91] | Moderate to high (dose-dependent cytotoxicity) [90] [93] |
| Manufacturing Scalability | Established for clinical applications [91] | Moderate (requires optimization) [91] | High (various synthesis routes available) [92] |
Advanced Anti-biofilm Strategies and Combination Approaches
Surface-Functionalized and Targeted Nanoparticles
Strategic surface modifications enhance NP specificity and efficacy against biofilms:
- Ligand-receptor targeting: Functionalization with antibodies, peptides, or aptamers that recognize biofilm-specific antigens or matrix components [87] [91].
- Stimuli-responsive systems: Design of NPs that release therapeutic payload in response to biofilm microenvironment cues such as acidic pH, specific enzymes (e.g., matrix-degrading enzymes), or metabolic byproducts [87].
- Cationic surface engineering: Incorporation of positive surface charges to exploit electrostatic interactions with anionic EPS components, enhancing biofilm retention and penetration [89].
Synergistic Nanoparticle-Antibiotic Combinations
Combining NPs with conventional antibiotics represents a powerful approach to overcome biofilm-mediated resistance:
- Penetration enhancers: NPs can facilitate antibiotic penetration through EPS disruption or simultaneous delivery, restoring efficacy against embedded bacteria [76].
- Dual-mechanism action: Simultaneous targeting of multiple bacterial pathways reduces the likelihood of resistance development and enhances killing efficiency [91] [76].
- Resistance reversal: Certain metallic NPs can inhibit efflux pumps or β-lactamase activity, potentially restoring susceptibility to conventional antibiotics [92].
The Scientist's Toolkit: Essential Research Reagents and Materials
Table 3: Key Research Reagents for Nanoparticle Biofilm Studies
| Reagent/Material | Function | Application Examples |
|---|---|---|
| PLGA (Poly(lactic-co-glycolic acid)) | Biodegradable polymer for NP fabrication | Controlled antibiotic delivery systems [87] |
| DSPC (1,2-distearoyl-sn-glycero-3-phosphocholine) | Phospholipid for liposome formation | Stable lipid bilayer construction [88] |
| Silver nitrate (AgNO₃) | Precursor for silver NP synthesis | Antimicrobial metallic NP production [90] [92] |
| Resazurin dye | Metabolic activity indicator | Biofilm viability assessment [88] |
| Concanavalin A conjugates | Polysaccharide staining | EPS visualization and quantification [89] |
| DCFH-DA probe | ROS detection | Oxidative stress measurement in biofilms [90] [92] |
| Crystal violet | Biomass staining | Total biofilm quantification [88] |
| Alginate | EPS component simulation | Artificial biofilm models for penetration studies [89] |
The escalating crisis of biofilm-associated antimicrobial resistance demands innovative therapeutic strategies that can overcome the unique defensive mechanisms of structured microbial communities. Liposomal, polymeric, and metallic nanoparticles each offer distinct advantages in this context, employing different but complementary approaches to disrupt biofilm integrity, enhance drug delivery, and directly target embedded pathogens.
Liposomes excel as versatile drug carriers with proven clinical translation potential, polymeric NPs offer exceptional tunability for controlled release and targeted delivery, while metallic NPs provide multimodal mechanisms including ROS generation and physical disruption. The optimal choice among these platforms depends on specific application requirements, considering factors such as the target pathogen, biofilm characteristics, and therapeutic objectives.
Future advancements in anti-biofilm nanotechnology will likely focus on multifunctional systems that combine the strengths of different nanoparticle classes, integrate stimuli-responsive elements for precision targeting, and leverage combination therapies to prevent resistance development. As fundamental understanding of nanoparticle-biofilm interactions deepens and manufacturing capabilities advance, nanotechnological approaches hold significant promise for addressing the persistent challenge of biofilm-mediated antibiotic resistance in clinical, industrial, and environmental settings.
The recalcitrance of biofilm-associated infections to conventional antibiotics represents a significant challenge in clinical management. This resistance is largely mediated by the extracellular polymeric substance (EPS), which acts as a physical and functional barrier against antimicrobial penetration. This whitepaper explores the therapeutic potential of enzyme-based strategies, specifically dispersin B, DNase, and glycoside hydrolases, for disrupting biofilm integrity by targeting key structural components of the matrix. These enzymes degrade exopolysaccharides and extracellular DNA, disrupting the EPS architecture and restoring antibiotic susceptibility. Within the broader context of biofilm matrix composition and antibiotic penetration resistance research, this review synthesizes current knowledge on enzymatic mechanisms, experimental efficacy data, and practical methodologies, providing researchers and drug development professionals with a comprehensive technical resource for advancing novel anti-biofilm therapeutics.
Bacterial biofilms are structured communities of microbial cells encased in a self-produced matrix of extracellular polymeric substances (EPS) that exhibit profound tolerance to antimicrobial agents. The EPS forms a protective shield around the resident bacteria, contributing to the chronicity of infections. Research indicates that biofilms are associated with approximately 65-80% of all human microbial infections, making them a paramount concern in healthcare settings [94] [95]. The biofilm matrix is a complex amalgamation of biopolymers, primarily consisting of exopolysaccharides, proteins, and extracellular DNA (eDNA), which collectively create a formidable barrier to antibiotic penetration [94] [96] [95].
A key mechanism behind biofilm-mediated resistance is limited antibiotic diffusion through the EPS. The matrix can hinder antibiotic absorption via binding interactions or enzymatic degradation, effectively reducing the concentration of antimicrobial agents that reach the bacterial cells [2]. For instance, positively charged aminoglycosides can bind to negatively charged biopolymers like eDNA within the matrix, significantly slowing their penetration [2]. This physical barrier function is compounded by physiological heterogeneity within the biofilm community. Bacterial cells in the biofilm core often exist in a low-oxygen, nutrient-depleted microenvironment that decreases their metabolic rate, rendering them less susceptible to many antibiotics that target active cellular processes [95] [2]. Furthermore, biofilms harbor persister cells—a small subpopulation that adopts a dormant state with extreme antimicrobial tolerance—which can repopulate the community after antibiotic treatment ceases [95].
The magnitude of this resistance is staggering, with studies demonstrating that bacteria in biofilms can be up to 1,000-fold more tolerant to antibiotic treatment than their planktonic counterparts [94] [97] [95]. This elevated tolerance frequently necessitates dramatically increased antibiotic doses—up to 1000-fold higher for certain antibiotics—to achieve any therapeutic effect against biofilm-associated infections [94]. Given this formidable defense system, therapeutic strategies that disrupt the structural integrity of the biofilm matrix represent a promising approach for restoring antibiotic efficacy. Enzymatic degradation of the EPS components offers a targeted method to dismantle this protective shield, potentially converting resistant biofilm-based infections into more treatable planktonic infections.
Biofilm Matrix Composition and Resistance Mechanisms
The extracellular polymeric substance (EPS) is the primary architectural component of biofilms, contributing over 90% of its dry mass and forming a complex, three-dimensional matrix that determines its functional and structural properties [97]. Understanding the precise composition and organization of the EPS is fundamental to developing effective matrix-targeting therapies, as each component plays a distinct role in maintaining biofilm integrity and mediating resistance.
Table 1: Major Components of the Biofilm Extracellular Polymeric Substance (EPS) and Their Functional Roles
| Matrix Component | Chemical Structure | Primary Functional Roles | Representative Producing Microorganisms |
|---|---|---|---|
| dPNAG (Poly-β-(1,6)-N-acetyl-D-glucosamine) | β-1,6-linked N-acetylglucosamine polymers, partially de-N-acetylated [95] | Cell-cell adhesion, structural integrity, protection from immune effectors [98] [95] | Staphylococcus aureus, Escherichia coli, Acinetobacter baumannii [95] |
| Alginate | β-1,4-linked D-mannuronic acid and L-guluronic acid residues [95] | Viscosity, barrier function, protection from phagocytosis [95] | Pseudomonas aeruginosa (especially in cystic fibrosis) [95] |
| Cellulose | β-1,4-linked D-glucose polymers [97] | Structural support, aggregation, adherence to surfaces [97] | Escherichia coli, Salmonella spp., Pseudomonas spp. [97] |
| Extracellular DNA (eDNA) | Double-stranded DNA fragments (average ~30 kb) [96] | Structural scaffold, cation chelation, horizontal gene transfer, antibiotic binding [96] [2] | Universal across Gram-positive and Gram-negative biofilms [96] |
| Proteins & Amyloid Fibers | Proteinaceous fibers and adhesins [2] | Surface attachment, structural stability, community organization [2] | Staphylococcus aureus, various Bacillus species [2] |
The composition of the EPS is not static but varies considerably depending on the microbial species, environmental conditions, and nutrient availability [2]. For instance, Staphylococcus aureus can employ distinct mechanisms for successful biofilm formation, resulting in different biofilm archetypes such as the polysaccharide biofilm (dependent on PNAG), the protein/eDNA biofilm, the fibrin biofilm, and the amyloid biofilm [2]. This plasticity enables biofilms to adapt to diverse environments and stressors, further complicating treatment approaches.
The mechanisms by which the matrix confers resistance are multifaceted. The physical barrier effect impedes the penetration of antimicrobial molecules through molecular sieving, binding, or sequestration [2]. The chemical interactions between matrix components and antibiotics can directly inactivate certain drugs; for example, the binding of aminoglycosides to eDNA effectively reduces their bioavailability [2]. Additionally, the matrix facilitates the enrichment of antibiotic-degrading enzymes like β-lactamases, creating a localized zone of protection [94]. Beyond these passive mechanisms, the matrix also contributes to physiological adaptations by creating chemical gradients that lead to heterogeneous metabolic activity and the emergence of dormant persister cells [95] [2]. This comprehensive protective role establishes the biofilm matrix as a critical therapeutic target for overcoming antimicrobial resistance.
Enzyme-Based Anti-Biofilm Strategies
Enzymatic disruption of the biofilm matrix represents a targeted therapeutic approach that leverages natural biochemical processes to degrade the structural components of the EPS. The primary advantages of this strategy include high specificity for their substrates, effectiveness at relatively low concentrations, and a reduced likelihood of inducing traditional antibiotic resistance since they function extracellularly [95]. The most extensively studied classes of these enzymes are glycoside hydrolases (including dispersin B), deoxyribonucleases, and proteases, each targeting distinct matrix constituents.
Dispersin B (Glycoside Hydrolase)
Dispersin B is a 40 kDa glycoside hydrolase produced by the periodontal pathogen Aggregatibacter actinomycetemcomitans [99]. This enzyme plays a crucial biological role for the producing bacterium by enabling the detachment and dispersal of adherent cells from mature biofilm colonies, allowing colonization of new niches [98] [99].
- Mechanism of Action: Dispersin B is a β-hexosaminidase that specifically hydrolyzes β-1,6-glycosidic linkages in poly-β-(1,6)-N-acetyl-D-glucosamine (PNAG or dPNAG), a key biofilm exopolysaccharide produced by a wide range of Gram-positive and Gram-negative pathogens [98] [95] [99]. The enzyme's active site contains three highly conserved acidic residues critical for catalysis: Asp183, Glu184, and Glu332 [99]. The mechanism is proposed to involve substrate-assisted catalysis, where the N-acetyl group of the substrate acts as a nucleophile during the cleavage reaction [99].
- Therapeutic Applications: Dispersin B exhibits broad-spectrum antibiofilm activity against more than 25 phylogenetically diverse bacterial species [98]. It has been shown to inhibit biofilm formation, detach preformed biofilms, disaggregate bacterial clumps, and sensitize biofilms to killing by antibiotics, antiseptics, and host immune cells [98]. Its efficacy has been demonstrated in both in vitro and in vivo models, leading to its commercial development for wound care gels and medical device coatings [99].
DNase (Deoxyribonuclease)
Deoxyribonucleases (DNases) are enzymes that catalyze the hydrolytic cleavage of phosphodiester linkages in the DNA backbone. eDNA is a universal structural component in the biofilm matrix of diverse bacterial species, and its degradation profoundly affects biofilm architecture and stability [96].
- Mechanism of Action: There are two main types of DNases with relevance to biofilm disruption. DNase I is active at neutral pH, requires Ca²⁺ and Mg²⁺ cations as activators, and cleaves DNA to produce 3'-hydroxyl and 5'-phosphoryl ends [100]. In contrast, DNase II (acid deoxyribonuclease) functions optimally at low pH without requiring divalent metal ions, yielding 3'-phosphorylated and 5'-hydroxyl termini [100] [101]. Both enzymes function by introducing nicks in the eDNA backbone, ultimately leading to the dissolution of the eDNA scaffold that supports the biofilm structure [96].
- Therapeutic Applications: The cleavage of eDNA by DNase leads to altered biofilm community biomass, architecture, and morphology, resulting in increased antibiotic penetration [96]. Studies have shown that the addition of DNase I enhances the effect of antibiotics, significantly decreasing biofilm biomass and bacterial viability [96]. Clinically, recombinant human DNase I (dornase alfa) is an established inhaled treatment for cystic fibrosis patients, where it reduces the viscosity of airway secretions by digesting DNA released from degenerating neutrophils [100]. DNase is also being investigated for treating other respiratory conditions, sepsis, and systemic lupus erythematosus [100].
Other Glycoside Hydrolases
Beyond Dispersin B, a wide array of other glycoside hydrolases (GHs) can target the diverse polysaccharide components of the biofilm matrix. These enzymes act by hydrolyzing the specific glycosidic linkages that hold polysaccharide chains together.
- α-Amylase and Cellulase: These GHs target different polysaccharide linkages. α-Amylase hydrolyzes α-1,4 glycosidic bonds found in starch-like polymers, while cellulase breaks β-1,4 linkages in cellulose and related exopolysaccharides [97]. Treatment of S. aureus and P. aeruginosa mono- and co-culture biofilms with these enzymes resulted in significant reductions in biomass and increased bacterial dispersal, both in vitro and in a murine chronic wound model [97]. The degradation of the polysaccharide backbone dismantles the EPS scaffold, converting sessile cells to a planktonic state and enhancing their susceptibility to conventional antibiotics [97].
- Fungal Glycoside Hydrolases: Fungi from the Trichoderma genus produce an extensive arsenal of GHs, including chitinases, β-1,3-glucanases, and cellulases, which are primarily studied for their mycoparasitic activities but hold potential for targeting fungal biofilms or specific bacterial EPS components [102]. The regulation of these enzymes is often highly specific, induced by the presence of their target substrates (e.g., chitin or fungal cell walls) and repressed by readily metabolizable carbon sources like glucose [102].
Table 2: Key Glycoside Hydrolases in Biofilm Disruption
| Enzyme | Target Linkage | Key Structural Features | Primary Biofilm Targets |
|---|---|---|---|
| Dispersin B | β-1,6-glycosidic bonds in PNAG [99] | TIM barrel fold; Active site: D183, E184, E332 [99] | S. aureus, E. coli, A. actinomycetemcomitans [98] [95] |
| α-Amylase | α-1,4-glycosidic bonds [97] | Not specified in search results | S. aureus, P. aeruginosa, V. cholerae [97] |
| Cellulase | β-1,4-glycosidic bonds in cellulose [97] | Not specified in search results | P. aeruginosa, Burkholderia cepacia, E. coli [97] |
| Chitinases (e.g., from Trichoderma) | β-1,4 linkages in chitin [102] | Multiple isoforms (e.g., CHIT42, ENC1, CHIT33) [102] | Fungal biofilms, potential for bacterial PNAG [102] |
The following diagram illustrates the targeted action of these key enzyme classes on the structural components of a generalized biofilm matrix:
Experimental Protocols and Methodologies
Robust and standardized experimental protocols are essential for evaluating the efficacy of enzyme-based anti-biofilm agents. Below are detailed methodologies for key assays commonly used in this field of research.
Biofilm Formation and Cultivation
In Vitro Microtiter Plate Biofilm Formation Assay [96]
- Procedure:
- Prepare a standardized bacterial inoculum (e.g., 7.53 ± 0.22 log₁₀ CFU/ml) in an appropriate liquid growth medium such as Luria-Bertani, Mueller-Hinton, or Schaedler broth.
- Dispense 200 µl of the inoculum into the wells of a 96-well plate. Include negative control wells containing sterile medium only.
- Incubate the plates statically at 37°C for 24 hours (or other optimized time depending on the bacterial strain).
- After incubation, gently aspirate the supernatant from each well.
- Wash the wells three times with an isotonic phosphate buffer (e.g., 0.15 M, pH 7.2) to remove non-adherent planktonic cells, taking care not to disturb the adherent biofilm film.
- Notes: The choice of growth medium and incubation time can significantly influence biofilm architecture and density. For polymicrobial biofilms, co-culture the relevant strains at the desired starting ratios.
Enzymatic Biofilm Disruption Assays
Crystal Violet (CV) Staining for Total Biomass Quantification [96] [97]
- Procedure:
- After biofilm formation and washing (as above), add the enzyme solution (e.g., 200 µl of 0.25% glycoside hydrolase solution in buffer or medium) to the test wells. Include vehicle-only and heat-inactivated enzyme controls.
- Incubate under appropriate conditions (e.g., 30 minutes to 24 hours at 37°C).
- Aspirate the enzyme solution and wash the wells gently with sterile water or buffer.
- Fix the biofilms by air-drying for 20-30 minutes.
- Stain the adherent biofilm with 200 µl of 0.1% crystal violet solution for 15-30 minutes at room temperature.
- Remove excess stain by thoroughly washing the wells with sterile distilled water until the runoff is clear.
- Solubilize the bound crystal violet by adding 200 µl of an ethanol-acetone mixture (80:20, v/v).
- Quantify the extent of biofilm formation by measuring the absorbance of the solubilized dye at 570 nm using a microplate reader.
- Application: This colorimetric assay provides a quantitative measure of the total biofilm biomass (cells and EPS) remaining after enzymatic treatment. A significant reduction in absorbance compared to controls indicates successful biofilm disruption.
Dispersal Assay for Viable Cell Count [97]
- Procedure:
- Establish biofilms in wells or on relevant surfaces (e.g., plastic coverslips).
- Treat the mature biofilms with the test enzyme (e.g., 5% glycoside hydrolase solution) for a defined period.
- Collect the supernatant, which contains dispersed cells.
- Gently wash the remaining biofilm with buffer and combine this wash with the supernatant.
- Vortex or sonicate the remaining biofilm adherent to the surface to resuspend the non-dispersed cells.
- Determine the number of viable bacteria (CFU/ml) in both the dispersal fraction (supernatant + wash) and the residual biofilm fraction by serial dilution and plating on appropriate solid media.
- Application: This assay directly measures the ability of an enzyme to detach viable cells from the biofilm. The percentage of total cells dispersed into the supernatant is calculated, providing a direct metric of dispersal efficacy.
Synergy Testing with Antibiotics [96]
- Procedure:
- Establish biofilms in a 96-well plate as described in section 4.1.
- After 24 hours of growth, gently aspirate the supernatant and wash the biofilms.
- Add treatments to the wells: (a) antibiotic alone, (b) enzyme alone, (c) antibiotic and enzyme combined, and (d) vehicle control. The antibiotic can be added simultaneously with the enzyme or after a pre-treatment period with the enzyme.
- Incubate the plates for an additional 24 hours at 37°C.
- Assess the outcome by either:
- CFU Enumeration: Aspirate the treatments, wash the biofilms, and resuspend the cells by scraping and vortexing. Perform serial dilutions and plate to determine the viable count.
- Biomass Quantification: Use the crystal violet staining method described above.
- Application: This protocol evaluates whether enzymatic pre-treatment or co-treatment enhances the efficacy of conventional antibiotics, a key translational objective for these therapies.
- Procedure:
- Anesthetize mice and create full-thickness wounds (e.g., 1.5 cm x 1.5 cm) on the dorsal surface.
- Infect the wounds with the bacterial strain(s) of interest (e.g., S. aureus and P. aeruginosa for a polymicrobial infection) by applying the inoculum under a transparent, adhesive bandage.
- Allow biofilms to establish for 3 days post-infection.
- At the time of treatment, extract the biofilms from the wound beds.
- Treat the extracted biofilm material ex vivo with the enzyme solution (e.g., α-amylase, cellulase) or a control (e.g., heat-inactivated enzyme) for 1 hour.
- Analyze the results by:
- Biomass Degradation: Measuring the wet weight of the biofilm material before and after treatment.
- Cell Dispersal: Calculating the number of viable bacteria dispersed into the treatment solution versus those remaining in the residual biofilm.
- Application: This model provides a clinically relevant system for testing enzyme efficacy against biofilms grown in a host-mimicking environment.
Data Presentation and Synthesis
The efficacy of enzyme-based anti-biofilm strategies is demonstrated through quantitative measurements of biofilm biomass reduction, increased bacterial dispersal, and restored antibiotic susceptibility. The following tables synthesize key experimental findings from the literature.
Table 3: Quantitative Efficacy of Glycoside Hydrolases Against Bacterial Biofilms
| Enzyme | Biofilm Model | Treatment Concentration & Duration | Key Quantitative Results | Citation |
|---|---|---|---|---|
| α-Amylase | S. aureus & P. aeruginosa (in vitro coculture) | 0.25% for 30 min | Significant reduction in crystal violet staining (biomass) | [97] |
| Cellulase | S. aureus & P. aeruginosa (in vitro coculture) | 0.25% for 30 min | Significant reduction in crystal violet staining (biomass) | [97] |
| α-Amylase & Cellulase (1:1) | S. aureus & P. aeruginosa (in vitro coculture) | 5% for dispersal assay | Significant increase in total cell dispersal into supernatant | [97] |
| α-Amylase | S. aureus & P. aeruginosa (murine wound ex vivo) | 1-hour treatment | ~50% reduction in infected wound bed biomass; no effect on uninfected tissue | [97] |
| Cellulase | S. aureus & P. aeruginosa (murine wound ex vivo) | 1-hour treatment | ~50% reduction in infected wound bed biomass; no effect on uninfected tissue | [97] |
Table 4: Efficacy of DNase I in Enhancing Antibiotic Action Against Biofilms
| Bacterial Strain | DNase I Treatment | Antibiotic | Outcome vs. Antibiotic Alone | Citation |
|---|---|---|---|---|
| E. coli ATCC 25922 | Co-treatment | Ampicillin, Cefotaxime, Levofloxacin, etc. | Decreased biofilm biomass and CFU count | [96] |
| S. aureus ATCC 29213 | Co-treatment | Ampicillin, Cefotaxime, Levofloxacin, etc. | Decreased biofilm biomass and CFU count | [96] |
| P. aeruginosa ATCC 27853 | Co-treatment | Ampicillin, Cefotaxime, Levofloxacin, etc. | Decreased biofilm biomass and CFU count | [96] |
| A. baumannii VT 126 | Co-treatment | Ampicillin, Cefotaxime, Levofloxacin, etc. | Decreased biofilm biomass and CFU count | [96] |
| Various Gram-positive and Gram-negative | Cleavage of eDNA in matrix | Various | Increased antibiotic penetration into biofilm community | [96] |
The data consistently demonstrate that glycoside hydrolases and DNase are effective as monotherapies for reducing biofilm biomass and inducing bacterial dispersal. More importantly, their combination with conventional antibiotics leads to synergistic effects, resulting in significantly enhanced killing of biofilm-resident bacteria compared to antibiotic treatment alone. This synergy is central to their therapeutic potential, as it can potentially restore the efficacy of existing antibiotics against otherwise recalcitrant infections.
The Scientist's Toolkit: Research Reagent Solutions
Advancing research on enzyme-based anti-biofilm therapies requires access to specific, high-quality reagents and materials. The following table details essential components for establishing relevant experimental models and conducting key assays.
Table 5: Essential Research Reagents for Anti-Biofilm Enzyme Studies
| Reagent / Material | Specifications & Examples | Primary Function in Experimental Workflow |
|---|---|---|
| Model Bacterial Strains | S. aureus (ATCC 29213), P. aeruginosa (ATCC 27853), E. coli (ATCC 25922); clinical isolates from chronic wounds [96] [97] | Forming monospecies or polymicrobial biofilms for in vitro and in vivo efficacy testing. |
| Glycoside Hydrolases | Dispersin B (commercially available or recombinant), α-Amylase (from various sources), Cellulase (from Trichoderma reesei) [97] [98] [102] | Active agents for degrading polysaccharide components of the biofilm matrix. |
| Deoxyribonucleases | Bovine Pancreatic DNase I (e.g., Sigma-Aldrich, specific activity ~2,200 Kunitz units/mg) [96] | Active agents for degrading the extracellular DNA (eDNA) scaffold within the biofilm matrix. |
| Microtiter Plates | 96-well plates, non-tissue culture treated (e.g., from Sarstedt) [96] [97] | High-throughput platform for standardized biofilm cultivation and colorimetric assays (e.g., crystal violet). |
| Crystal Violet Solution | 0.1% (w/v) in isopropanol-methanol-PBS or water [96] | Colorimetric staining of total adherent biofilm biomass for quantification. |
| In Vivo Wound Model | Murine (e.g., C57BL/6) full-thickness dorsal wound model [97] | Clinically relevant model for evaluating anti-biofilm efficacy in a complex host environment. |
Enzyme-based therapies targeting the biofilm matrix represent a paradigm shift in the approach to combating chronic, recalcitrant infections. The strategic degradation of key structural EPS components—exopolysaccharides by dispersin B and other glycoside hydrolases, and eDNA by DNase—effectively dismantles the protective shield of the biofilm, thereby restoring penetration and efficacy of co-administered antimicrobials [94] [96] [97]. This review has synthesized the foundational knowledge surrounding the mechanisms, experimental evidence, and methodologies pertinent to this burgeoning field, framing it within the critical context of overcoming antibiotic penetration resistance.
The path toward clinical translation of these enzymes is promising but requires addressing several key challenges. Future research must prioritize the development of enzyme delivery systems that protect these protein therapeutics from proteolytic degradation and facilitate their penetration into the often dense biofilm infrastructure. Furthermore, given the complexity and heterogeneity of clinical biofilms, combination therapies that utilize multiple enzymes (e.g., a glycoside hydrolase with a DNase) or enzymes with conventional antibiotics will likely yield the most robust outcomes [98] [95]. The issue of potential immunogenicity with repeated dosing also warrants thorough investigation. Finally, expanding research into the efficacy of these agents against polymicrobial biofilms, which are prevalent in chronic wounds and respiratory infections, will be essential for broadening their clinical applicability. As these challenges are met, enzyme-based anti-biofilm strategies hold immense potential to evolve from a powerful research tool into a cornerstone of therapeutic intervention against some of the most persistent and difficult-to-treat infections in modern medicine.
The escalating global crisis of antimicrobial resistance (AMR) is profoundly linked to the biofilm mode of bacterial growth. Structured microbial communities encased in a self-produced extracellular matrix, biofilms are a major contributor to antimicrobial resistance, facilitating the persistence of dormant cells and the horizontal transfer of resistance genes. This whitepaper provides an in-depth technical analysis of three innovative biological agents—bacteriophages, quorum-sensing inhibitors, and probiotics—in the context of combating biofilm-associated infections. Framed within broader thesis research on biofilm matrix composition and antibiotic penetration resistance, this guide details the mechanisms of action, experimental protocols, and key research reagents for these strategies. The content is designed to equip researchers and drug development professionals with the current, multidisciplinary knowledge required to develop effective anti-biofilm therapeutics, moving beyond conventional antibiotic paradigms to address a pressing global health threat.
The intrinsic resistance of biofilms to antimicrobial agents is a complex phenomenon, primarily orchestrated by the biofilm's physical and physiological structure. The extracellular polymeric substance (EPS) matrix is a characteristic hallmark of biofilm formation, constituting over 90% of the biofilm mass and functioning as a structurally robust protective barrier [2]. This matrix is an agglomeration of various biopolymers, including polysaccharides, lipids, proteins, and extracellular DNA (eDNA) [2].
A primary resistance mechanism is the impediment of antibiotic diffusion and absorption into the biofilm [2]. The matrix acts as a dynamic microenvironment that can hinder antibiotic penetration through multiple mechanisms:
- Binding and Inactivation: Some antibiotics form complexes with matrix components or are broken down by matrix-associated enzymes, reducing the effective concentration reaching bacterial cells. For instance, positively charged aminoglycosides can bind to negatively charged biopolymers like eDNA, significantly slowing their penetration [2].
- Physical Barrier: The EPS constitutes a dense, gel-like layer that physically limits the diffusion of antimicrobial molecules, creating concentration gradients where the core of the biofilm is exposed to sub-lethal doses [18].
- Enzymatic Degradation: The matrix can host enzymes that chemically modify or degrade antibiotics, a mechanism distinct from but synergistic with the physical barrier effect [103].
This defensive role of the matrix is compounded by the biofilm's metabolic heterogeneity. Gradients of oxygen, nutrients, and waste products within the biofilm create diverse microniches, leading to the formation of dormant persister cells—phenotypically tolerant subpopulations that are unaffected by antibiotics targeting metabolic activity [18]. Furthermore, the dense, structured environment of the biofilm accelerates horizontal gene transfer (HGT), transforming these communities into hotspots for the dissemination of resistance genes among bacterial cells [18]. Addressing this multifaceted threat requires innovative strategies that target the biofilm's structural integrity, communication systems, and ecological dynamics.
Bacteriophages: Precision Biofilm Predators
Bacteriophages (phages), viruses that infect and lyse bacteria, represent a promising and highly specific alternative to conventional antibiotics for biofilm eradication.
Mechanisms of Action against Biofilms
Phages employ multiple mechanisms to disrupt and penetrate biofilms, as illustrated in the following workflow:
Diagram Title: Bacteriophage Anti-Biofilm Mechanism
- Matrix Degradation: Many phages produce and encode enzymes such as depolymerases that specifically degrade key structural components of the biofilm EPS, including polysaccharides and eDNA [104]. This enzymatic activity disrupts the matrix's physical integrity, creating channels for deeper phage and antibiotic penetration.
- Infection and Lysis of Embedded Bacteria: Following matrix disruption, phages infect bacterial cells within the biofilm. They hijack the host's cellular machinery to replicate, ultimately causing bacterial lysis (rupture) and the release of progeny virions that infect adjacent cells [104].
- Structural Failure of Biofilm: The combined effect of matrix degradation and widespread bacterial lysis leads to the structural collapse of the biofilm microcolony, effectively dispersing the microbial community [18].
A significant advantage of phage therapy is its potential for synergy with antibiotics (Phage-Antibiotic Synergy, PAS). The initial phage-mediated disruption of the biofilm matrix and reduction of bacterial density can sensitize the remaining cells to conventional antibiotics, which then achieve improved penetration and efficacy [18].
Key Experimental Protocol: Evaluating Phage Efficacy against Biofilms
Title: Assessment of Phage-Mediated Biofilm Disruption and PAS In Vitro
Objective: To quantify the efficacy of a purified phage suspension, both alone and in combination with a selected antibiotic, in reducing the biomass and viability of a pre-formed biofilm.
Materials:
- Bacterial Strain: e.g., Pseudomonas aeruginosa PAO1 or Staphylococcus aureus biofilm-forming strain.
- Phage Preparation: Purified phage lysate, titer ≥ 10^8 PFU/mL, suspended in SM buffer.
- Antibiotic: e.g., Tobramycin or Ciprofloxacin.
- Growth Medium: Tryptic Soy Broth (TSB) or Mueller Hinton Broth (MHB).
- 96-well Polystyrene Microtiter Plates (for crystal violet staining and viability counts).
- PBS (Phosphate Buffered Saline) for washing.
- Crystal Violet Solution (0.1% w/v).
- Acetic Acid (33% v/v).
- SYTO 9/Propidium Iodide stain for viability staining (optional).
Methodology:
- Biofilm Formation: Grow a static biofilm by inoculating a 1:100 dilution of an overnight bacterial culture into wells of a 96-well plate. Incubate for 24-48 hours at 37°C to allow for mature biofilm development.
- Treatment Application: Carefully aspirate the planktonic culture and wash the biofilm gently with PBS to remove non-adherent cells.
- Group 1 (Control): Add fresh medium only.
- Group 2 (Phage): Add medium containing phage at a defined Multiplicity of Infection (MOI, e.g., 1 or 10).
- Group 3 (Antibiotic): Add medium containing a sub-MIC concentration of the antibiotic.
- Group 4 (PAS): Add medium containing both the phage and the sub-MIC antibiotic.
- Incubation: Incubate the plate for a further 4-24 hours at 37°C.
- Biofilm Quantification:
- Biomass (Crystal Violet Staining): Aspirate treatment, wash, air-dry, and stain biofilms with 0.1% crystal violet for 15 minutes. Wash excess stain, solubilize bound stain with 33% acetic acid, and measure absorbance at 570 nm.
- Viability (Colony Forming Units - CFU): After treatment, aspirate and wash. Add PBS and sonicate the plate (or scrape the wells) to dislodge biofilm cells. Serially dilute the suspension and plate on agar to enumerate CFUs.
- Confocal Microscopy (Optional): For structural analysis, form biofilms on glass-bottom dishes, treat as above, and image using a confocal laser scanning microscope after viability staining to visualize live/dead cell distribution and biofilm architecture.
Quantitative Data on Phage Therapeutics
Table 1: Efficacy Metrics of Phage and Phage-Antibiotic Combinations against Biofilms
| Pathogen Model | Phage / Enzyme Used | Intervention | Reduction in Biofilm Biomass | Reduction in Viability (CFU) | Key Finding |
|---|---|---|---|---|---|
| P. aeruginosa [18] | Depolymerase-producing phage | Phage + Tobramycin | ~70% | ~3.0 log₁₀ | Synergistic effect; phage disruption enabled antibiotic action. |
| S. aureus [104] | Phage cocktail | Phage alone | ~60% | ~2.5 log₁₀ | Effective penetration and dispersal of proteinaceous matrix. |
| Multispecies Wound Model [18] | Phage + Glycoside Hydrolase | Enzyme + Phage | >80% | ~4.0 log₁₀ | Enzyme pretreatment significantly enhanced phage access. |
Quorum-Sensing Inhibitors: Silencing Bacterial Communication
Quorum sensing (QS) is a cell-to-cell communication system that allows bacteria to coordinate population-wide behaviors, including virulence factor production and biofilm development, in response to cell density [103]. Quorum-sensing inhibitors (QSIs) are compounds that disrupt this communication, offering an "anti-virulence" strategy that may exert less selective pressure for resistance than conventional biocides [105].
Mechanisms of QS Inhibition and Biofilm Disruption
QSIs target various stages of the QS circuitry to prevent the coordinated behavior essential for mature biofilm formation and maintenance.
Diagram Title: Quorum Sensing Inhibition Pathways
- Degradation of QS Signals: Enzymes such as AHL-lactonases or AHL-acylases can degrade QS signal molecules in the extracellular environment, preventing them from reaching the threshold concentration required for gene activation [105].
- Antagonism of QS Receptors: Synthetic or natural analogs of QS signals (e.g., acyl homoserine lactone analogs) can competitively bind to receptor proteins without activating them, effectively "jamming" the communication system [18] [103].
- Inhibition of Signal Synthesis: Compounds that inhibit the enzymes responsible for producing QS signal molecules can prevent the initiation of communication from the outset.
By disrupting QS, these inhibitors suppress the expression of genes critical for EPS production, leading to the formation of architecturally frail biofilms that are more susceptible to antimicrobial agents and immune clearance [18]. Crucially, recent in vivo evidence suggests that resistance to QS inhibition spreads more slowly than resistance to traditional antibiotics, particularly when the QSI targets public goods and does not require entry into the cell, thus avoiding efflux pumps [105].
Key Experimental Protocol: Screening for QS Inhibitors
Title: High-Throughput Screening of Putative QSIs Using a Biosensor Assay
Objective: To identify compounds that inhibit QS signaling without affecting bacterial growth.
Materials:
- Biosensor Strain: e.g., Chromobacterium violaceum CV026 (produces violet pigment violacein in response to exogenous AHLs) or a P. aeruginosa lasB-gfp reporter strain.
- Positive Control: Pure AHL signal molecule (e.g., C6-HSL for CV026).
- Test Compounds: Library of synthetic or natural product extracts.
- Microtiter Plates (96-well or 384-well).
- Spectrophotometer and/or Microplate Fluorometer.
Methodology:
- Preparation: Dispense culture medium into microtiter plates. Add a sub-inhibitory concentration of the AHL signal to all wells requiring induction.
- Compound Addition: Add the test compounds to the assay wells. Include controls: a no-AHL control (baseline), an AHL-only control (maximum signal), and a growth control with a bactericidal compound.
- Inoculation and Incubation: Inoculate all wells with a standardized suspension of the biosensor strain. Incubate with shaking at the optimal temperature (e.g., 28°C for CV026) for 16-24 hours.
- Quantification of Inhibition:
- For CV026: Measure violacein production by solubilizing the pigment in DMSO and reading absorbance at 585 nm. Simultaneously, measure bacterial growth (OD600) to discount inhibitory effects due to bactericidal activity.
- For GFP Reporter: Directly measure fluorescence (ex/em ~485/535 nm) and normalize to OD600.
- Data Analysis: Calculate % QS inhibition relative to the AHL-only control. A true QSI will show significant reduction in signal (violacein/GFP) with minimal impact on OD600.
Research Reagent Solutions for QS Inhibition Studies
Table 2: Essential Research Reagents for Quorum Sensing Studies
| Reagent / Tool | Function / Mechanism | Example Application |
|---|---|---|
| AHL Biosensor Strains (e.g., C. violaceum CV026) | Reporter system for AHL-based QS; produces visible pigment (violacein) in response to specific AHLs. | Initial high-throughput screening of natural or synthetic compound libraries for anti-QS activity. |
| Synthetic AHL Analogs (e.g., AHL antagonists) | Competitively bind to LuxR-type receptor proteins without activating them, blocking native QS pathways. | Mechanistic studies to dissect specific QS pathways and as positive controls in inhibition assays. |
| Quorum Quenching Enzymes (e.g., AHL-lactonase, AHL-acylase) | Enzymatically degrade or modify AHL signal molecules, preventing their accumulation and recognition. | Used as experimental tools to validate the role of QS in biofilm formation and to study dispersed biofilms. |
| GFP/Lux Reporter Plasmids for QS-regulated promoters | Allow real-time, non-destructive monitoring of QS gene expression dynamics in response to inhibitors. | Studying the kinetics of QS inhibition in flow-cell biofilms or in vivo infection models. |
Probiotics: Competitive Exclusion and Biofilm Mitigation
Probiotics are live microorganisms that confer a health benefit to the host. Their application is expanding beyond traditional uses to include the active prevention and disruption of pathogenic biofilms through mechanisms of competitive exclusion, production of inhibitory substances, and modulation of the host immune response.
Mechanisms of Probiotic Action against Biofilms
- Competitive Exclusion: Probiotics compete with pathogens for binding sites on the host epithelium and for essential nutrients, thereby limiting the ability of pathogens to adhere and form biofilms [18] [106]. This often involves specific surface proteins and adhesins, such as S-layer proteins, elongation factor Tu, and glyceraldehyde-3-phosphate dehydrogenase, which facilitate the probiotic's own adhesion and colonization [106].
- Production of Antimicrobial Substances: Probiotics secrete a variety of compounds, including organic acids (lactic acid, acetic acid), bacteriocins, and hydrogen peroxide, which can directly inhibit the growth of pathogenic bacteria and disrupt pre-existing biofilms [18].
- Quorum Sensing Interference: Some probiotic strains can produce molecules that function as QSIs, degrading pathogen signal molecules or acting as receptor antagonists, thereby disrupting the coordination required for robust biofilm development [18].
- Enhanced Gastrointestinal Tolerance via Biofilm State: Delivering probiotics in a biofilm state significantly enhances their survival under harsh gastrointestinal conditions (low pH, bile salts) and improves their intestinal adhesion and colonization compared to planktonic cells [107]. Transcriptomic analyses reveal that probiotic biofilms exhibit upregulation of genes related to stress response, adhesion, and QS, making them more resilient and effective [107] [108].
Key Experimental Protocol: Assessing Probiotic Colonization and Anti-Biofilm Efficacy
Title: Evaluating Probiotic Adhesion, Colonization, and Pathogen Displacement
Objective: To determine the adhesion capacity of a probiotic strain to intestinal epithelial cells and its ability to prevent or disrupt pathogen biofilm formation.
Materials:
- Probiotic Strain: e.g., Lactobacillus plantarum HC-2 or Escherichia coli Nissle 1917.
- Pathogen Strain: e.g., Enteropathogenic E. coli (EPEC) or Salmonella Typhimurium.
- Intestinal Epithelial Cell Line: e.g., Caco-2 or HT-29 cells.
- Cell Culture Facilities (CO₂ incubator, etc.).
- Transwell Inserts (for co-culture experiments).
- Scanning Electron Microscopy (SEM) or Confocal Microscopy supplies.
- qPCR Equipment and species-specific primers (for in vivo colonization).
Methodology:
- Adhesion to Epithelial Cells:
- Culture Caco-2 cells to form a confluent, differentiated monolayer.
- Add fluorescently labeled probiotics (e.g., stained with FITC) at a known multiplicity of infection (MOI) and co-incubate.
- After incubation, wash the monolayer thoroughly to remove non-adherent bacteria.
- Lyse the cells and plate serial dilutions to count adhered CFUs, or quantify fluorescence.
- Competition/Exclusion Assay:
- Pre-incubation: Add probiotics to the Caco-2 monolayer for 1-2 hours, then wash.
- Challenge: Add the pathogen and incubate further.
- Quantification: Lyse cells and count pathogen CFUs to determine if pre-colonization with probiotic reduced pathogen adhesion.
- Biofilm Disruption In Vitro:
- Allow the pathogen to form a biofilm for 24-48 hours in a microtiter plate.
- Add the probiotic strain (or its cell-free supernatant) to the pre-formed biofilm and incubate further.
- Quantify remaining biofilm biomass using crystal violet staining and pathogen viability via CFU counting.
- In Vivo Colonization (e.g., in Shrimp or Mice):
- Administer the probiotic orally to the model organism.
- At various time points, dissect the gastrointestinal tract (foregut, midgut, hindgut).
- Homogenize tissues, extract total DNA, and use qPCR with strain-specific primers to quantify and localize probiotic colonization, which can be 15 times higher in specific gut regions like the midgut [106].
Quantitative Data on Probiotic Biofilm Efficacy
Table 3: Enhanced Properties of Probiotics in Biofilm State
| Probiotic Strain | Experimental Context | Key Measured Advantage of Biofilm vs. Planktonic State | Proposed Mechanism |
|---|---|---|---|
| Ligilactobacillus salivarius Li01 [107] | Simulated Gastrointestinal (GI) Tolerance | Survival rate increased from <10% to >60% | Upregulation of acid resistance genes (gadA, adiA) and stress response proteins. |
| Bifidobacterium longum [107] | Intestinal Adhesion | Adhesion to intestinal mucus increased by ~50% | Increased surface hydrophobicity and expression of adhesion factors. |
| E. coli Nissle 1917 [108] | Gut Colonization in Mice | 52- to 89-fold higher colonization in cecum/colon | Self-organized microcolonies in hydrogel with upregulated QS and biofilm genes (csg, fim). |
| Lactobacillus plantarum HC-2 [106] | Adhesion to HCT116 cells | Adhesion rate decreased from 98.1% to 20.9% after surface protein removal | Surface proteins (S-layer, Ef-Tu, GAPDH) are critical for adhesion. |
The convergence of biofilm matrix composition and antibiotic penetration resistance represents a fundamental challenge in treating chronic infections. The biological agents detailed in this whitepaper—bacteriophages, quorum-sensing inhibitors, and probiotics—offer a sophisticated, multi-pronged arsenal to address this challenge. Their mechanisms, which include enzymatic matrix disruption, silencing of bacterial communication, and competitive ecological exclusion, directly target the core vulnerabilities of biofilm communities.
Future research and development should focus on several key areas:
- Combinatorial Therapies: The greatest potential lies in synergistically combining these agents with each other and with low-dose conventional antibiotics. For example, a sequential strategy using a QSI to weaken biofilm structure, followed by phage penetration and concluding with a probiotic to prevent recolonization, could be highly effective [18].
- Advanced Delivery Systems: For phages and QSIs, overcoming delivery barriers is critical. The use of nanocarrier systems and engineered hydrogels, as demonstrated in the Express Microcolony Service (EMS) for probiotics, can protect these biological agents and ensure their targeted delivery to the infection site [18] [108].
- Translation and Regulation: Moving these innovative strategies from the lab to the clinic requires robust, biofilm-aware diagnostic tools, adaptive clinical trial designs for evaluating complex combinations, and forward-looking regulatory frameworks that balance innovation with safety [18].
By deepening our understanding of biofilm biology and leveraging these advanced biological tools, the scientific community can develop the transformative strategies needed to effectively counter the growing global threat of biofilm-associated multidrug resistance.
Biofilm-associated bacterial infections represent a formidable challenge in clinical settings, acting as a core component of the broader antimicrobial resistance (AMR) crisis. Biofilms are structured microbial communities encased in a self-produced extracellular polymeric substance (EPS) matrix, composed of polysaccharides, nucleic acids, and proteins [16]. This complex architecture is not merely a physical barrier; it creates a protected environment that significantly reduces antibiotic penetration and promotes persistent, difficult-to-treat infections [16] [76]. The unique structure of biofilms can increase bacterial resistance to antimicrobial therapy by up to 1000 times, fostering the horizontal transfer of resistance genes and rendering conventional treatments increasingly ineffective [76].
The ESKAPE pathogens—Enterococcus faecium, Staphylococcus aureus, Klebsiella pneumoniae, Acinetobacter baumannii, Pseudomonas aeruginosa, and Enterobacter species—are of particular concern, as they are frequently resistant to multiple antibiotics and proficient biofilm formers [16]. The World Health Organization has highlighted the dire trajectory of AMR, which could lead to as many as 40 million deaths annually by 2050 without effective interventions [109]. In this context, bacteriophage (phage) therapy has re-emerged as a promising alternative to conventional antibiotics. Phages are viruses that specifically infect and lyse bacterial cells, offering a targeted approach to combating multidrug-resistant (MDR) pathogens [109] [110]. However, a significant limitation of monotherapy with phages is the potential for bacteria to rapidly evolve resistance [110]. To address this limitation, researchers have developed a sophisticated approach known as phage-antibiotic synergy (PAS), which strategically combines these two antimicrobial modalities to enhance efficacy, suppress resistance development, and effectively combat biofilm-mediated infections [109] [111]. This whitepaper provides an in-depth technical guide to PAS, focusing on its mechanisms, efficacy data, and experimental protocols relevant to researchers and drug development professionals.
Mechanistic Foundations of Phage-Antibiotic Synergy
The enhanced efficacy of phage-antibiotic combinations against biofilms stems from complementary mechanisms of action that target both the structural integrity of the biofilm and the physiological state of the embedded bacteria.
Biofilm Penetration and Matrix Degradation
The EPS matrix presents a primary barrier to antimicrobial agents. Certain phages have evolved to overcome this barrier by producing depolymerase enzymes that degrade key components of the biofilm matrix, such as polysaccharides, nucleic acids, and proteins [110] [16]. This enzymatic activity disrupts the structural integrity of the biofilm, facilitating deeper penetration of both the phage particles and co-administered antibiotics into the biofilm's core, thereby accessing dormant or stationary-phase bacteria that are typically highly tolerant to antibiotics [110].
Overcoming Bacterial Resistance through Fitness Trade-offs
A fundamental principle underpinning PAS is the concept of fitness trade-offs, wherein bacterial adaptations to resist one antimicrobial agent come at a cost of increased susceptibility to another [110]. For instance, when bacteria evolve resistance to a phage by modifying or losing surface receptors that the phage uses for adsorption, these mutations often simultaneously restore or increase susceptibility to certain antibiotics. This occurs because the modified surface receptors may alter membrane permeability or disrupt efflux pump function, thereby facilitating improved antibiotic penetration [110]. This phenomenon creates a "collateral sensitivity" that can be strategically exploited in combination therapies.
Enhanced Killing through Physiological Synergy
Sub-inhibitory concentrations of certain antibiotics can enhance phage replication and activity. Antibiotics that target bacterial cell walls or disrupt metabolic pathways can stress bacterial cells, increasing their metabolic activity and making them more susceptible to phage infection and replication [109]. This leads to a more robust lytic cycle and greater bacterial killing than either agent could achieve alone. The combination effectively counters the heterogeneity of bacterial populations within biofilms, where sub-populations may differentially resist either phage or antibiotic treatment [109] [111].
The following diagram illustrates the synergistic mechanism by which a combined phage-antibiotic treatment eradicates a bacterial biofilm.
Quantitative Efficacy Data and Synergistic Outcomes
Recent in vitro and in vivo studies provide compelling quantitative evidence for the superior efficacy of PAS compared to monotherapies. The data summarized in the tables below demonstrate significant enhancements in biofilm eradication and animal survival rates.
Table 1: Biological Characteristics and In Vitro Efficacy of Phage phiLCL12 in PAS against P. aeruginosa Biofilms [109]
| Characteristic | Metric | Result | Experimental Context |
|---|---|---|---|
| Host Range | Susceptible clinical strains | 82.22% (37/45 strains) | 45 clinical P. aeruginosa isolates |
| Adsorption Efficiency | Adsorption within 4 minutes | >98% | MOI of 0.0005 |
| Biofilm Clearance | Combination with sub-MIC Imipenem | Significant enhancement (vs. control) | In vitro biofilm model |
| Biofilm Inhibition | Combination with sub-MIC Imipenem | Significant inhibition (vs. control) | In vitro prevention model |
Table 2: In Vivo Efficacy of Phage-Antibiotic Combinations in Animal Models [109] [112]
| Infection Model | Pathogen | Therapeutic Regimen | Survival Outcome | Study |
|---|---|---|---|---|
| Zebrafish | P. aeruginosa | Phage phiLCL12 + Imipenem | Significant improvement vs. antibiotic alone | PMC12155105 [109] |
| Mouse (BALB/c) | E. coli ST131 | Phage Cocktail (EC.W1–9, EC.W15–4) + Antibiotics | ~75% survival | ScienceDirect [112] |
| Mouse (BALB/c) | E. coli ST648 | Phage Cocktail + Antibiotics | 100% survival | ScienceDirect [112] |
| Mouse (BALB/c) | E. coli ST410 | Phage Cocktail + Antibiotics | 75-100% survival | ScienceDirect [112] |
Table 3: Synergistic Lysis Rates of Phage-Antibiotic Combinations Against Resistant E. coli [112]
| Bacterial Target | Phage Cocktail Alone | Antibiotic Alone | Phage-Antibiotic Combination |
|---|---|---|---|
| ESBL-producing E. coli (n=60 isolates) | 61.7% lysis | Not Specified | 73.3% susceptibility |
| Carbapenem-resistant E. coli (CREC) | 61.7% lysis | Not Specified | 54% susceptibility |
Experimental Protocols for PAS Research
To ensure reproducible and clinically relevant results in PAS research, standardized experimental protocols are essential. The following sections detail key methodologies for evaluating PAS efficacy.
In Vitro Biofilm Eradication Assay
This protocol assesses the ability of phage-antibiotic combinations to disrupt pre-formed biofilms [109].
- Biofilm Formation: Grow a standardized suspension of the bacterial strain (e.g., P. aeruginosa LCL12) in a suitable medium, such as Tryptic Soy Broth (TSB), in 96-well polystyrene plates. Incubate for 24-48 hours at 37°C to allow for robust biofilm formation on the well surfaces.
- Treatment Application: Carefully aspirate the planktonic culture and wash the adherent biofilm gently with phosphate-buffered saline (PBS) to remove non-adherent cells. Apply treatment groups to the wells: medium only (negative control), phage alone at a specified Multiplicity of Infection (MOI), antibiotic alone at a sub-inhibitory concentration (sub-MIC), and the phage-antibiotic combination. Incubate the plates for a further 24 hours.
- Biofilm Quantification: After incubation, aspirate the treatments and wash the wells with PBS. Fix the remaining biofilm with methanol or ethanol for 15 minutes, then stain with a 0.1% crystal violet solution for 20 minutes. Rinse off excess stain, solubilize the bound crystal violet with acetic acid or ethanol, and measure the optical density at 570 nm (OD~570~) using a microplate reader. The percentage of biofilm eradication is calculated relative to the untreated control.
In Vivo Efficacy Assessment in a Zebrafish Model
Animal models like zebrafish provide a whole-organism context for evaluating therapeutic efficacy and survival [109].
- Infection and Treatment: Anesthetize zebrafish larvae and micro-inject a lethal dose of a clinically relevant, multidrug-resistant strain (e.g., P. aeruginosa) into the circulation or specific tissues. Randomize the infected fish into experimental groups: untreated control, antibiotic alone (e.g., imipenem), phage alone, and the phage-antibiotic combination. Treatments are typically administered via immersion or micro-injection shortly after infection.
- Monitoring and Analysis: Monitor the zebrafish for mortality and signs of systemic infection over a predefined period (e.g., 5-7 days). Record survival rates daily. At the endpoint, sacrifice the fish and homogenize whole larvae or specific organs to quantify bacterial burden (Colony Forming Units - CFU) from the different treatment groups. Statistical analysis (e.g., Log-rank test for survival, ANOVA for CFU counts) is performed to determine significant differences between the combination therapy and monotherapy groups.
Adaptive Evolution Protocol for Phage Optimization
This technique expands phage host ranges to counter evolved bacterial resistance [110].
- Co-culture Setup: Initiate a co-culture of a naive phage population and a mixed bacterial population comprising both phage-sensitive and initially resistant strains. The culture is maintained in a fresh medium over multiple serial passages.
- Serial Passage and Selection: At regular intervals (e.g., every 12-24 hours), transfer a sample of the co-culture to fresh medium. This continually applies selective pressure for phages capable of infecting and replicating within the evolving bacterial population, which is developing new resistance mechanisms.
- Plaque Isolation and Characterization: After several rounds of passage (e.g., 10-15 cycles), isolate new phage variants from the culture by plaque assay. Screen these isolated phages for their ability to lyse the original bacterial host as well as strains that have become resistant to the ancestral phage. This process selects for phages with mutations in receptor-binding proteins or other genomic regions that enable them to overcome bacterial defenses.
The workflow below outlines the adaptive evolution process used to generate phages with enhanced therapeutic potential.
The Scientist's Toolkit: Key Research Reagents and Materials
Successful PAS research requires a specific set of reagents and materials. The following table details essential items and their functions in experimental workflows.
Table 4: Essential Research Reagents and Materials for PAS Studies
| Reagent / Material | Function / Application | Specific Examples / Notes |
|---|---|---|
| Clinical Bacterial Isolates | Target pathogens for in vitro and in vivo efficacy testing. ESKAPE pathogens, particularly MDR and biofilm-forming strains [109] [16]. | Characterized for antibiotic susceptibility and virulence genes (e.g., exoS, exoU in P. aeruginosa) [109]. |
| Characterized Bacteriophages | The viral therapeutic agent. Phages should be genetically sequenced and characterized for morphology, host range, and lack of virulence genes [109] [112]. | Phages like phiLCL12 (Pbunavirus) for P. aeruginosa [109]; phage cocktails (e.g., EC.W1–9, EC.W15–4) for E. coli [112]. |
| Sub-Inhibitory Antibiotics | Used in combination to induce synergy. Sub-MIC concentrations are critical for observing PAS rather than simple additive effects [109] [111]. | Carbapenems (e.g., imipenem) against P. aeruginosa [109]. |
| Cell Culture Plates (Polystyrene) | Substrate for in vitro biofilm formation. 96-well plates are standard for high-throughput biofilm quantification assays [109]. | Ensure consistency in surface properties for reproducible biofilm growth. |
| Crystal Violet Stain | Dye used for colorimetric quantification of biofilm biomass [109] [113]. | Standard protocol: stain, wash, solubilize, measure OD~570~. |
| Animal Infection Models | In vivo assessment of therapeutic efficacy and survival. | Zebrafish larvae for P. aeruginosa [109]; BALB/c mice for E. coli [112]. |
Phage-antibiotic synergy represents a paradigm shift in the approach to treating resilient biofilm-associated infections. By leveraging the complementary mechanisms of action of phages and antibiotics—including biofilm matrix degradation, exploitation of bacterial fitness trade-offs, and enhanced killing of heterogeneous bacterial populations—PAS strategies offer a powerful tool to overcome the pervasive challenge of antimicrobial resistance [109] [110] [111]. The quantitative data from robust in vitro and in vivo models consistently demonstrate that combination therapies significantly outperform corresponding monotherapies, providing a clear rationale for their continued development [109] [112]. While challenges remain, particularly regarding regulatory pathways and scalable phage production [111], the strategic integration of PAS into the antimicrobial arsenal holds immense promise for improving clinical outcomes in the ongoing battle against multidrug-resistant pathogens.
Comparative Analysis of Scalability, Toxicity, and Clinical Translation Potential
The intrinsic resistance of bacterial biofilms to antimicrobial agents represents a critical challenge in clinical medicine, driving persistent infections and contributing to the global antimicrobial resistance crisis. This resistance is largely governed by the biofilm's extracellular polymeric substance (EPS), a matrix that acts as a formidable barrier to antibiotic penetration and a facilitator of bacterial survival [114] [2]. The composition of this matrix—a complex of polysaccharides, proteins, lipids, and extracellular DNA (eDNA)—varies by species and environmental conditions, directly influencing the pharmacokinetic and pharmacodynamic profiles of antimicrobials within the biofilm [114] [2]. Research into therapeutic strategies that can overcome this penetration resistance is a cornerstone of the broader thesis on biofilm matrix composition. This review provides a comparative analysis of emerging anti-biofilm technologies, critically evaluating their scalability for industrial production, their toxicity profiles, and their potential for successful clinical translation, thereby offering a strategic framework for researchers and drug development professionals.
Comparative Analysis of Anti-Biofilm Therapeutic Platforms
The following table summarizes the core characteristics, advantages, and challenges of four leading platforms in anti-biofilm therapeutic development.
Table 1: Comparative Analysis of Leading Anti-Biofilm Therapeutic Platforms
| Therapeutic Platform | Mechanism of Action | Scalability & Manufacturing | Toxicity & Safety Profile | Clinical Translation Potential & Key Challenges |
|---|---|---|---|---|
| CRISPR/Cas9-Nanoparticle Hybrids | Precision gene-editing to disrupt resistance genes, quorum sensing, and biofilm-regulating factors [115]. Nanoparticles (e.g., gold, liposomal) enhance delivery and stability [115]. | Moderate. Complex two-component system. Solid-phase peptide synthesis and nanoparticle fabrication are scalable, but rigorous quality control for batch-to-batch consistency of functionalized particles is a hurdle [115]. | Theoretical off-target effects. Immune response to Cas9 protein and nanoparticles. Liposomal and gold NPs show favorable preliminary biocompatibility [115]. | High for precision therapy. Liposomal CRISPR-Cas9 reduced P. aeruginosa biofilm by >90% in vitro; gold NPs enhanced editing efficiency 3.5-fold [115]. Challenges: Minimizing off-target effects, optimizing in-vivo delivery efficiency, and long-term safety [115]. |
| Quorum Sensing Inhibitors (QSIs) | Target bacterial cell-to-cell communication pathways to prevent coordinated biofilm formation and virulence factor expression without causing bacterial death [116]. | High. Typically small molecules amenable to traditional chemical synthesis and large-scale pharmaceutical production [116]. | Generally low. As they are not bactericidal, they exert less selective pressure for resistance. Specificity for bacterial pathways minimizes host toxicity [116]. | High as adjunctive therapy. Effective in disrupting biofilm integrity in vitro. Challenges: Ensuring sufficient potency in-vivo and preventing bypass mechanisms in complex bacterial communities [116]. |
| Enzymatic Dispersal Agents | Degrade key structural components of the biofilm matrix (e.g., glycoside hydrolases target polysaccharides, DNases target eDNA) to dismantle the protective EPS [2]. | Moderate to High. Recombinant protein production is well-established. Stability and shelf-life of enzymatic formulations can be a scalability challenge [2]. | Low to Moderate. Potential for immunogenicity with repeated doses. Host-derived enzymes (e.g., human DNase) have established clinical safety profiles [2]. | High, particularly for surface debridement. Demonstrated efficacy in dispersing P. aeruginosa and S. aureus biofilms in wound models [2]. Challenges: Co-delivery with antibiotics is often essential to kill dispersed, susceptible planktonic cells [2] [116]. |
| Antibiofilm Peptides | Disrupt bacterial membranes or modulate gene expression to inhibit biofilm growth; often cationic and can penetrate EPS [116]. | Low to Moderate. Peptide synthesis is costly at scale. Issues with stability, proteolytic degradation, and short half-life complicate manufacturing [116]. | Variable. Can exhibit hemolytic activity and cytotoxicity against host cells. Engineering efforts focus on improving therapeutic indices [116]. | Moderate. Potent in-vitro activity. Challenges: Overcome poor pharmacokinetics, systemic toxicity, and high production costs for clinical application [116]. |
Experimental Protocols for Key Anti-Biofilm Assays
Robust and standardized experimental methodologies are essential for the quantitative evaluation of novel anti-biofilm agents. The following protocols are foundational for assessing biofilm formation, viability, and architecture.
Protocol 1: Quantitative Assessment of Biofilm Viability using Confocal Laser Scanning Microscopy (CLSM) and Automated Image Analysis
This protocol leverages CLSM and an open-source image analysis tool to provide a high-resolution, quantitative assessment of biofilm viability and 3D architecture, minimizing human error associated with traditional methods [117].
Table 2: Key Research Reagents for CLSM Biofilm Viability Assay
| Reagent / Tool | Function in the Protocol |
|---|---|
| FilmTracer LIVE/DEAD Biofilm Viability Kit | Fluorescent staining: SYTO 9 labels all cells (green), propidium iodide penetrates only damaged membranes (red) [117]. |
| Confocal Laser Scanning Microscope (CLSM) | High-resolution 3D imaging of biofilms at specific wavelengths, excluding out-of-focus light [117]. |
| Fiji/ImageJ with Biofilm Viability Checker Macro | Open-source software for automated image processing, thresholding, and quantification of live/dead biomass and surface coverage [117]. |
| Microbial Strains & Growth Media | Culturing relevant biofilm-forming pathogens (e.g., P. aeruginosa, S. aureus) to maturity [117]. |
Detailed Workflow:
- Biofilm Cultivation: Grow biofilms of the target pathogen(s) on relevant substrates (e.g., plastic, coated glass, or biomaterial coupons) under conditions that promote robust biofilm formation (e.g., using flow cells or static culture) [118] [117].
- Treatment Application: Expose mature biofilms to the experimental anti-biofilm agent (e.g., CRISPR-nanoparticles, QSIs), a positive control (e.g., a known antibiotic), and a negative control (e.g., buffer alone) for a specified duration.
- Viability Staining: Gently rinse the biofilms to remove non-adherent cells. Apply the LIVE/DEAD stain according to manufacturer's instructions, ensuring adequate incubation in the dark [117].
- CLSM Imaging: Acquire z-stack images of the biofilms using appropriate laser wavelengths for SYTO 9 and propidium iodide. A minimum of 5 random fields of view per sample should be imaged to ensure statistical representativeness [117].
- Automated Image Analysis:
- Import the z-stack images into Fiji/ImageJ and run the "Biofilm Viability Checker" macro [117].
- The macro performs automated image pre-processing and thresholding to separate the green (live) and red (dead) channels, preventing the subjective yellow coloration that can occur from channel superimposition [117].
- The algorithm quantifies the biovolume (µm³) of live and dead cells, the ratio of live-to-dead fluorescence, and the percentage of surface coverage.
- Data Analysis: Export the quantitative data for statistical analysis. Compare the treated samples against controls to determine the significant reduction in total biofilm biomass and the shift in the live/dead ratio.
This method has been validated against traditional CFU counting, showing lower coefficients of variation (4.24–11.5% for image analysis vs. 17.0–78.1% for CFU counting) and provides additional critical data on biofilm architecture [117].
Protocol 2: Assessment of Biofilm Metabolic Activity and Mass via Microtiter Plate Assay
This colorimetric method is a standard, medium-throughput technique for quantifying total biofilm biomass and is ideal for initial screening of anti-biofilm compounds [118].
Detailed Workflow:
- Biofilm Growth: Inoculate a sterile 96-well flat-bottom plate with a standardized bacterial suspension and incubate under static conditions to allow biofilm formation on the well walls.
- Treatment and Fixation: After incubation, carefully remove the planktonic culture and gently wash the wells with phosphate-buffered saline (PBS) to remove non-adherent cells. Add the test agents for a defined period. Subsequently, fix the adherent biofilms with methanol or ethanol.
- Crystal Violet Staining: Add a crystal violet solution (0.1% w/v) to each well and incubate. Crystal violet binds to proteins and polysaccharides in the biofilm matrix and cellular components [118].
- Destaining and Quantification: Wash the wells thoroughly to remove unbound stain. Then, add an acetic acid or ethanol solution to destain and dissolve the bound crystal violet.
- Spectrophotometric Measurement: Transfer the destain solution to a new plate and measure the optical density (OD) at 570–600 nm using a microplate reader. The OD is directly correlated with the total biofilm biomass attached to the well surface [118].
Visualization of Key Biofilm Processes and Experimental Workflows
Biofilm Lifecycle and Therapeutic Intervention Points
The following diagram illustrates the key stages of biofilm development and identifies the primary intervention points for the therapeutic platforms discussed.
CRISPR-Nanoparticle Hybrid System Workflow
This diagram outlines the experimental workflow for developing and testing a CRISPR-Nanoparticle hybrid anti-biofilm therapeutic, from design to validation.
The fight against biofilm-mediated infections requires a multifaceted approach that moves beyond conventional antibiotic paradigms. Among the platforms analyzed, CRISPR/Cas9-nanoparticle hybrids represent a paradigm shift towards precision medicine, offering the unique ability to directly target and disrupt the genetic underpinnings of biofilm formation and antibiotic resistance [115]. While their scalability and toxicity profiles require further optimization, their high clinical potential is clear. QSIs and enzymatic agents offer highly complementary strategies, focusing on disassembly and sensitization rather than direct killing, and generally present fewer translational hurdles in manufacturing and safety [2] [116]. The successful clinical translation of any of these platforms will likely depend on their use in rational combinations—for example, employing an enzymatic agent to disrupt the matrix barrier, followed by a CRISPR-based therapy to eliminate the underlying persistent bacteria. This synergistic approach, firmly grounded in a deep understanding of biofilm matrix composition, holds the greatest promise for overcoming the formidable challenge of antibiotic penetration resistance and ushering in a new era of effective anti-biofilm therapy.
Conclusion
The formidable challenge of antibiotic penetration in biofilms is intrinsically linked to the complex and dynamic composition of the extracellular matrix. A synthetic understanding of its architecture, the physicochemical mechanisms of resistance, and the limitations of current models is paramount for developing effective countermeasures. The future of treating biofilm-associated infections lies not in a single magic bullet, but in sophisticated, multimodal strategies that synergistically target the matrix, disrupt bacterial communication, and eliminate dormant persister cells. Promising avenues include the rational design of smart nanoparticles for enhanced penetration, the clinical application of phage therapy, and the exploitation of CRISPR-based precision antimicrobials. For researchers and drug developers, the priority must shift from traditional antibiotic discovery to pioneering these disruptive, matrix-targeting technologies to overcome one of modern medicine's most persistent challenges.
References
- 1. Extracellular polymeric substances, a key element in ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC6604936/]
- 2. Mechanisms of antimicrobial resistance in biofilms [https://www.nature.com/articles/s44259-024-00046-3]
- 3. Extracellular polymeric substance [https://en.wikipedia.org/wiki/Extracellular_polymeric_substance]
- 4. Differences in Production, Composition, and Antioxidant ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC7037457/]
- 5. Extracellular polymeric substances—antibiotics interaction ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC9678949/]
- 6. Quantitative and qualitative characterization of extracellular ... [https://www.sciencedirect.com/science/article/abs/pii/S1876107017304765]
- 7. Insights into the role of extracellular polymeric substances ... [https://www.sciencedirect.com/science/article/abs/pii/S026974912302287X]
- 8. Extracellular Polymeric Substances Acting as a Permeable ... [https://www.frontiersin.org/journals/microbiology/articles/10.3389/fmicb.2019.00736/full]
- 9. Strategies for combating antibiotic resistance in bacterial ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10846525/]
- 10. Microbial biofilm: formation, architecture, antibiotic resistance ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC8578483/]
- 11. Formation, architecture, and persistence of oral biofilms [https://www.frontiersin.org/journals/microbiology/articles/10.3389/fmicb.2025.1602962/full]
- 12. Quantitative image analysis of microbial communities with ... [https://www.nature.com/articles/s41564-020-00817-4]
- 13. Microbial Biofilm Detection and Differentiation by Dual ... [https://en.bio-protocol.org/en/bpdetail?id=5228&type=0]
- 14. Growing and Analyzing Static Biofilms - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC4568995/]
- 15. Biofilm, resistance, and quorum sensing: The triple threat in ... [https://www.sciencedirect.com/science/article/pii/S2950194625003462]
- 16. Biofilms: structure, resistance mechanism, emerging control ... [https://pubs.rsc.org/en/content/articlehtml/2025/pm/d5pm00094g]
- 17. Time-resolved compositional and dynamics analysis of biofilm ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11779841/]
- 18. Biofilms and multidrug resistance: an emerging crisis and the ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12237878/]
- 19. Data Visualization — BiofilmQ @ Drescher lab [https://drescherlab.org/data/biofilmQ/docs/usage/visualization.html]
- 20. Quantitative measurement and visualization of biofilm O 2 ... [https://www.sciencedirect.com/science/article/abs/pii/S0376738811008817]
- 21. Experimental Designs to Study the Aggregation and ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC8793059/]
- 22. Comparative Analysis of Biofilm Formation and Antibiotic ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12382965/]
- 23. Revisiting ESKAPE Pathogens: virulence, resistance, and ... [https://www.frontiersin.org/journals/cellular-and-infection-microbiology/articles/10.3389/fcimb.2023.1159798/full]
- 24. Mechanisms of antibiotic resistance in Pseudomonas ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10189392/]
- 25. The Extracellular Polysaccharide Matrix of Pseudomonas ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC7927924/]
- 26. The Pseudomonas aeruginosa lectin LecB binds to ... [https://www.nature.com/articles/s41467-019-10201-4]
- 27. ESKAPEE pathogens newly released from biofilm residence ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10410267/]
- 28. Biofilm Resilience: Molecular Mechanisms Driving Antibiotic ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11852148/]
- 29. Combating Antimicrobial Resistance: Innovative Strategies ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12389514/]
- 30. integrating CRISPR/Cas9 and nanoparticles against biofilm ... [https://bmcmedicine.biomedcentral.com/articles/10.1186/s12916-025-04323-4]
- 31. Mathematical modelling of nutrient-dependent biofilm ... [https://arxiv.org/html/2509.18065v1]
- 32. Modelling of Diffusion and Reaction of Carbon Dioxide and ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12471363/]
- 33. The neglected model validation of antimicrobial resistance ... [https://aricjournal.biomedcentral.com/articles/10.1186/s13756-025-01574-x]
- 34. Harnessing machine learning to predict antibiotic ... [https://www.nature.com/articles/s41522-025-00833-4]
- 35. Strategies for combating antibiotic resistance in bacterial ... [https://www.frontiersin.org/journals/cellular-and-infection-microbiology/articles/10.3389/fcimb.2024.1352273/full]
- 36. The fate of multiple antibiotics in a counter-diffusion biofilm ... [https://www.sciencedirect.com/science/article/abs/pii/S1385894725112886]
- 37. Detecting antibiotic resistance: classical, molecular ... [https://www.frontiersin.org/journals/microbiology/articles/10.3389/fmicb.2025.1673343/full]
- 38. A molecular simulation method for analyzing the interaction ... [https://patents.google.com/patent/CN118711687A/en]
- 39. Confocal microscopy imaging of the biofilm matrix [https://www.sciencedirect.com/science/article/abs/pii/S0167701216300367]
- 40. Biofilms Exposed: Innovative Imaging and Therapeutic ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12466655/]
- 41. Microscopy Methods for Biofilm Imaging: Focus on SEM ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC7828176/]
- 42. Tools of the Trade: Image Analysis Programs for Confocal ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10268615/]
- 43. Investigation of shockwave treatment for disruption ... [https://www.nature.com/articles/s41598-025-19955-y]
- 44. Enhancing biofilm disruption and bactericidal efficiency using ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11920867/]
- 45. Advanced biofilm staining techniques for TEM and SEM in ... [https://www.sciencedirect.com/science/article/abs/pii/S000925411830456X]
- 46. Characterization and Multi-Omics Basis of Biofilm ... [https://www.mdpi.com/2311-5637/11/7/400]
- 47. Biofilms as Promoters of Bacterial Antibiotic Resistance ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC7822488/]
- 48. From in vitro to in vivo Models of Bacterial Biofilm-Related ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC4235718/]
- 49. Relationship between Antibiotic Resistance, Biofilm ... [https://www.frontiersin.org/journals/microbiology/articles/10.3389/fmicb.2016.00483/full]
- 50. Comparison of 3 Real-Time, Quantitative Murine Models ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC3929216/]
- 51. Assessing in vivo and in vitro biofilm development ... [https://www.frontiersin.org/journals/cellular-and-infection-microbiology/articles/10.3389/fcimb.2022.874694/full]
- 52. Antibiotics versus biofilm: an emerging battleground in ... [https://aricjournal.biomedcentral.com/articles/10.1186/s13756-019-0533-3]
- 53. Biofilm antimicrobial susceptibility testing: where are we ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10732061/]
- 54. The minimum bactericidal concentration of antibiotics [https://www.bmglabtech.com/en/blog/the-minimum-bactericidal-concentration-of-antibiotics/]
- 55. Biofilm and Planktonic Antibiotic Resistance in Patients ... [https://www.frontiersin.org/journals/cellular-and-infection-microbiology/articles/10.3389/fcimb.2021.813076/full]
- 56. Biofilm-Induced Antibiotic Resistance in Clinical ... [https://www.mdpi.com/2079-6382/9/11/817]
- 57. Staphylococcus biofilm dynamics and antibiotic resistance [https://pmc.ncbi.nlm.nih.gov/articles/PMC12054104/]
- 58. investigating the anti-biofilm potential of melittin alone and ... [https://www.frontiersin.org/journals/microbiology/articles/10.3389/fmicb.2023.1269392/full]
- 59. Intermittent antibiotic treatment of bacterial biofilms favors ... [https://www.nature.com/articles/s42003-023-04601-y]
- 60. The Role of Bacterial Biofilms in Antimicrobial Resistance [https://asm.org/articles/2023/march/the-role-of-bacterial-biofilms-in-antimicrobial-re]
- 61. Biofilms: Formation, drug resistance and alternatives to ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC9576500/]
- 62. Biofilm and Antimicrobial Resistance: Mechanisms, ... [https://www.mdpi.com/2036-7481/16/8/183]
- 63. Resistance mechanisms and therapeutic strategies for ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12576158/]
- 64. WHO warns of widespread resistance to common ... [https://www.who.int/news/item/13-10-2025-who-warns-of-widespread-resistance-to-common-antibiotics-worldwide]
- 65. Sorption of antibiotics to biofilm [https://www.sciencedirect.com/science/article/abs/pii/S004313541000775X]
- 66. Sorption of antibiotics to biofilm [https://pubmed.ncbi.nlm.nih.gov/21334040/]
- 67. Bacterial resistance to antibiotics: enzymatic degradation ... [https://pubmed.ncbi.nlm.nih.gov/15950313/]
- 68. Bacterial resistance to antibiotics: Enzymatic degradation ... [https://www.sciencedirect.com/science/article/abs/pii/S0169409X05000980]
- 69. One-step degradation of 4 classes of β-lactam using ... [https://www.nature.com/articles/s41598-025-16947-w]
- 70. Antibiotics re-booted—time to kick back against drug ... [https://www.nature.com/articles/s44259-025-00096-1]
- 71. Gradients and consequences of heterogeneity in biofilms [https://pmc.ncbi.nlm.nih.gov/articles/PMC9590228/]
- 72. Metabolite-driven reprogramming of bacterial persisters [https://www.sciencedirect.com/science/article/abs/pii/S1368764625001256]
- 73. Bacterial persisters: molecular mechanisms and ... [https://www.nature.com/articles/s41392-024-01866-5]
- 74. Understanding the Mechanism of Bacterial Biofilms ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC5427689/]
- 75. Differential carbon source utilization drives metabolic state ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12440864/]
- 76. Nanoparticles targeting biofilms: A new era in combating ... [https://www.sciencedirect.com/science/article/pii/S2590097825000370]
- 77. Challenges of antibiotic resistance biofilms and potential ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC7966653/]
- 78. Strategies for biofilm inhibition: the role of synthetic drug [https://pubmed.ncbi.nlm.nih.gov/41269277/]
- 79. Nanotechnology-Based Drug Delivery Systems to Control ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10674810/]
- 80. Nanotechnology Meets superbugs [https://www.nature.com/articles/s41598-025-21606-1]
- 81. Mechanisms of antimicrobial resistance in biofilms - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC11445061/]
- 82. Biofilm Resilience: Molecular Mechanisms Driving ... [https://www.mdpi.com/2079-7737/14/2/165]
- 83. Biofilms and multidrug resistance: an emerging crisis ... [https://www.frontiersin.org/journals/bioengineering-and-biotechnology/articles/10.3389/fbioe.2025.1625356/full]
- 84. Combination drug strategies for biofilm eradication using ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10149696/]
- 85. A promising neoteric approach for bacterial biofilm disruption [https://www.sciencedirect.com/science/article/abs/pii/S1359511323000697]
- 86. Combinatorial effects of antibiotics and enzymes against dual ... [https://journals.plos.org/plosone/article?id=10.1371/journal.pone.0235093]
- 87. Nanomaterial-enabled anti - biofilm strategies: new opportunities for... [https://pubs.rsc.org/en/content/articlehtml/2025/nr/d4nr04774e]
- 88. Liposomes-Based Drug Delivery Systems of Anti-Biofilm ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10215698/]
- 89. When nanoparticles meet biofilms—interactions guiding ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC4468922/]
- 90. Metal-Based Nanoparticles: Antibacterial Mechanisms and ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC9503339/]
- 91. Nanomedicine in the Fight against Multidrug- Resistant Infections: A Re [https://www.dovepress.com/nanomedicine-in-the-fight-against-multidrug-resistant-infections-a-rev-peer-reviewed-fulltext-article-IJN]
- 92. Metallic Nanoparticles: A Promising Arsenal against ... [https://www.mdpi.com/1422-0067/24/19/14897]
- 93. Alternative mechanisms of action of metallic nanoparticles ... [https://www.sciencedirect.com/science/article/pii/S2468233023000191]
- 94. Enzymatic dispersion of biofilms: An emerging biocatalytic ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC9478923/]
- 95. Strategy to combat biofilms: a focus on biofilm dispersal ... [https://www.nature.com/articles/s41522-023-00427-y]
- 96. Effect of DNase and Antibiotics on Biofilm Characteristics [https://pmc.ncbi.nlm.nih.gov/articles/PMC2650517/]
- 97. Glycoside Hydrolases Degrade Polymicrobial Bacterial ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC5278739/]
- 98. Aggregatibacter actinomycetemcomitans Dispersin B [https://pmc.ncbi.nlm.nih.gov/articles/PMC11357414/]
- 99. Dispersin B [https://en.wikipedia.org/wiki/Dispersin_B]
- 100. Deoxyribonuclease [https://en.wikipedia.org/wiki/Deoxyribonuclease]
- 101. Structure of acid deoxyribonuclease - PMC - PubMed Central [https://pmc.ncbi.nlm.nih.gov/articles/PMC5449587/]
- 102. Glycoside Hydrolase - an overview [https://www.sciencedirect.com/topics/neuroscience/glycoside-hydrolase]
- 103. Quorum-Sensing Regulation of Antimicrobial Resistance in ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC7143945/]
- 104. 噬菌体抗细菌生物膜机制及应用策略的研究进展 [http://dianda.cqvip.com/Qikan/Article/Detail?id=7111260310&from=Qikan_Article_Detail]
- 105. Resistance to quorum sensing inhibition spreads more ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11901357/]
- 106. Adhesion and Colonization of the Probiotic Lactobacillus ... [https://www.frontiersin.org/journals/microbiology/articles/10.3389/fmicb.2022.878874/full]
- 107. Effects of Biofilm Formation on Gastrointestinal Tolerance ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12076125/]
- 108. A multicellular self-organized probiotic platform for oral ... [https://www.nature.com/articles/s41467-025-62349-x]
- 109. Phage–Antibiotic Synergy Enhances Biofilm Eradication ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12155105/]
- 110. Phage Therapy as a Novel Alternative to Antibiotics Through ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12562026/]
- 111. Phage and Antibiotic Combination Therapy for Biofilm ... [https://www.contagionlive.com/view/phage-and-antibiotic-combination-therapy-for-biofilm-associated-bacterial-infections]
- 112. Therapeutic potential of novel phages with antibiotic ... [https://www.sciencedirect.com/science/article/pii/S2213716525000773]
- 113. Structure-Activity Relationships in Alkoxylated ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12348843/]
- 114. Biofilm formation: mechanistic insights and therapeutic targets [https://pmc.ncbi.nlm.nih.gov/articles/PMC10721784/]
- 115. Innovative approaches to combat antibiotic : integrating... resistance [https://pubmed.ncbi.nlm.nih.gov/40830872/]
- 116. Pharmacological strategies for targeting biofilms in... [https://www.spandidos-publications.com/10.3892/br.2025.1973?text=fulltext]
- 117. Biofilm viability checker: An open-source tool for automated ... [https://www.nature.com/articles/s41522-021-00214-7]
- 118. Quantitative and Qualitative Assessment Methods for Biofilm ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC6133255/]