The VBNC State: Unlocking the Mechanisms of Extreme Antibiotic Tolerance in Dormant Bacteria
This article provides a comprehensive analysis of the Viable But Non-Culturable (VBNC) state, a critical survival mechanism in bacteria characterized by a complete loss of culturability on standard media coupled...
The VBNC State: Unlocking the Mechanisms of Extreme Antibiotic Tolerance in Dormant Bacteria
Abstract
This article provides a comprehensive analysis of the Viable But Non-Culturable (VBNC) state, a critical survival mechanism in bacteria characterized by a complete loss of culturability on standard media coupled with significantly enhanced tolerance to antimicrobials. Aimed at researchers and drug development professionals, we explore the fundamental physiological and molecular hallmarks that differentiate VBNC cells from their culturable counterparts, with a focus on mechanisms driving multi-antibiotic tolerance. The content details advanced methodological approaches for inducing, detecting, and quantifying VBNC cells, overcoming the limitations of conventional culture-based assays. We further investigate the molecular underpinnings of this robust tolerance, including toxin-antitoxin systems, metabolic downregulation, and stress response pathways, while contrasting the VBNC state with persister cells and genetic antibiotic resistance. The synthesis of current knowledge highlights the VBNC state as a major contributor to recurrent infections and antibiotic treatment failure, urging the development of novel therapeutic strategies that target this dormant bacterial population.
VBNC State Fundamentals: Defining a Stealth Survival Strategy and Its Public Health Threat
The viable but nonculturable (VBNC) state represents a unique survival strategy employed by numerous bacterial species when confronted with adverse environmental conditions. Cells in the VBNC state undergo a dramatic physiological transformation, losing the ability to form colonies on conventional growth media while maintaining metabolic activity and viability. This review comprehensively examines the VBNC state, with particular emphasis on its profound implications for antibiotic susceptibility and public health. We systematically compare the antibiotic tolerance of VBNC cells against their culturable counterparts, present detailed experimental protocols for VBNC induction and detection, and analyze the molecular mechanisms underlying this dormant state. The findings synthesized herein reveal that VBNC cells exhibit significantly enhanced tolerance to antimicrobial agents, presenting substantial challenges for clinical treatment, food safety, and public health surveillance.
The VBNC State: A Survival Paradox
Definition and Historical Context
The viable but nonculturable (VBNC) state is defined as a dormant condition in which bacteria are alive and metabolically active but cannot form colonies on standard laboratory media that normally support their growth [1] [2]. This state was first explicitly described in 1982 by Xu et al., who observed that marine Vibrio species maintained viability despite losing culturability under certain conditions [2]. The VBNC state represents a distinct survival strategy, different from sporulation or stationary-phase dormancy, employed primarily by non-spore-forming bacteria to withstand potentially lethal environmental stresses [2] [3].
Induction Conditions and Characteristics
Bacteria enter the VBNC state in response to various environmental stresses, including but not limited to:
- Nutrient starvation [1] [2]
- Temperature extremes (both high and low) [1] [2]
- Osmotic stress [1] [2]
- Oxygen availability fluctuations [2]
- Chlorination and other disinfectant treatments [4]
- Exposure to antibiotics [3]
- Extreme pH levels [2]
The transition to the VBNC state is accompanied by significant physiological and morphological changes. Cells typically undergo reductive division, resulting in smaller, rounded morphology [1]. They demonstrate reduced nutrient transport, lower rates of respiration, decreased synthesis of macromolecules, and significantly reduced metabolic activity [1] [2]. Despite these reductions in metabolic processes, VBNC cells maintain cellular integrity, possess high ATP levels, exhibit membrane potential, and retain their plasmids [2]. Perhaps most significantly from a public health perspective, many pathogens retain virulence potential while in the VBNC state and can resuscitate when environmental conditions become favorable [1] [2].
Detection Methodologies: Beyond Conventional Culturing
Limitations of Culture-Based Methods
Conventional culture-based detection methods, including standard plate counts, fail to detect VBNC cells, leading to false-negative results in clinical, food safety, and environmental monitoring contexts [5] [2] [3]. This limitation poses significant public health risks, as VBNC pathogens may remain undetected in water supplies, food products, and clinical specimens [2]. The inability of culture-based methods to detect VBNC cells has been implicated in several disease outbreaks where standard testing failed to identify pathogens [2].
Advanced Detection Techniques
To address the limitations of culture-based methods, researchers have developed various molecular and technological approaches for VBNC cell detection:
Table 1: Advanced Methods for VBNC Cell Detection
| Method | Principle | Target Organisms | Sensitivity | Applications |
|---|---|---|---|---|
| PMA/ddPCR | Propidium monoazide dye penetration inhibition + digital PCR | Klebsiella pneumoniae | Absolute quantification without standard curve | Clinical samples, fecal specimens [6] |
| vqPCR | Viable quantitative PCR with DNA intercalating dyes | Vibrio parahaemolyticus, V. cholerae | 20 fg DNA (3.5 cells) for V. parahaemolyticus | Retail seafood safety testing [5] |
| AI-Enabled Hyperspectral Microscopy | Spectral profile analysis via deep learning | E. coli K-12 | 97.1% classification accuracy | Rapid food safety screening [7] |
| Flow Cytometry with Viability Staining | Membrane integrity assessment via fluorescent dyes | Various bacteria | Varies by dye and instrument | Environmental monitoring [1] [8] |
| Transcriptomic Analysis (RNA-seq) | Global gene expression profiling | E. coli, Vibrio parahaemolyticus | Gene-level expression changes | Mechanism studies [9] [4] |
Detailed Protocol: PMA-ddPCR for VBNC Quantification
The PMA-ddPCR method represents one of the most advanced approaches for absolute quantification of VBNC cells without requiring a standard curve [6]:
Reagents and Equipment:
- Propidium monoazide (PMA) stock solution (e.g., Biotium, Hayward, CA, USA)
- DNA extraction kit (e.g., Wizard Genomic DNA Purification Kit, Promega)
- ddPCR system with droplet generator and reader
- Halogen light source (650W)
- Species-specific primers for single-copy genes
Procedure:
- PMA Treatment Optimization:
- Test PMA concentrations ranging from 5 μM to 200 μM
- Incubate samples with PMA in the dark for 5-30 minutes at room temperature
- Expose to halogen light source (20cm distance) for 15 minutes with samples on ice
- Determine optimal PMA concentration and incubation time that effectively suppress DNA amplification from dead cells
DNA Extraction:
- Extract genomic DNA from 200 μL cell suspensions using purification kit
- Elute DNA in appropriate preservation solution
- Store at 4°C if processing immediately or at -20°C for long-term storage
Droplet Digital PCR:
- Prepare reaction mixture with template DNA, ddPCR supermix, and primers targeting at least three single-copy genes (e.g., KP, rpoB, adhE for K. pneumoniae)
- Generate droplets using droplet generator
- Perform PCR amplification with optimized thermal cycling conditions
- Read droplets using droplet reader
- Analyze data using Poisson statistics to obtain absolute copy numbers without standard curves
Validation:
- Compare results with culture-based methods for culturable cells
- Confirm VBNC state by absence of growth on appropriate media
- Use fluorescence microscopy with live/dead staining as correlative method
Genetic Regulation of the VBNC State
The transition into the VBNC state involves complex genetic regulation. Transcriptomic analyses of VBNC cells have revealed significant alterations in gene expression patterns. In E. coli, genes related to fimbrial-like adhesin protein, putative periplasmic pilin chaperone, transcriptional regulation, antibiotic resistance, and stress response are significantly regulated in the VBNC state [4]. Similarly, proteomic studies of Vibrio parahaemolyticus have identified 429 differentially expressed proteins during resuscitation compared to VBNC cells, with 330 up-regulated and 99 down-regulated proteins [9].
Type II toxin-antitoxin (TAS) systems play a crucial role in the genetic control of VBNC formation [3]. These systems typically contain two genes encoding a stable toxin and an unstable antitoxin. Under stress conditions, antitoxins are degraded by cellular proteases, releasing toxins that cause a sharp decrease in translation, replication, and cell growth, thereby inducing the VBNC state [3]. Additional global regulators, including rpoS and oxyR, also contribute to this complex regulatory network [3].
Signaling Pathways in VBNC State Transitions
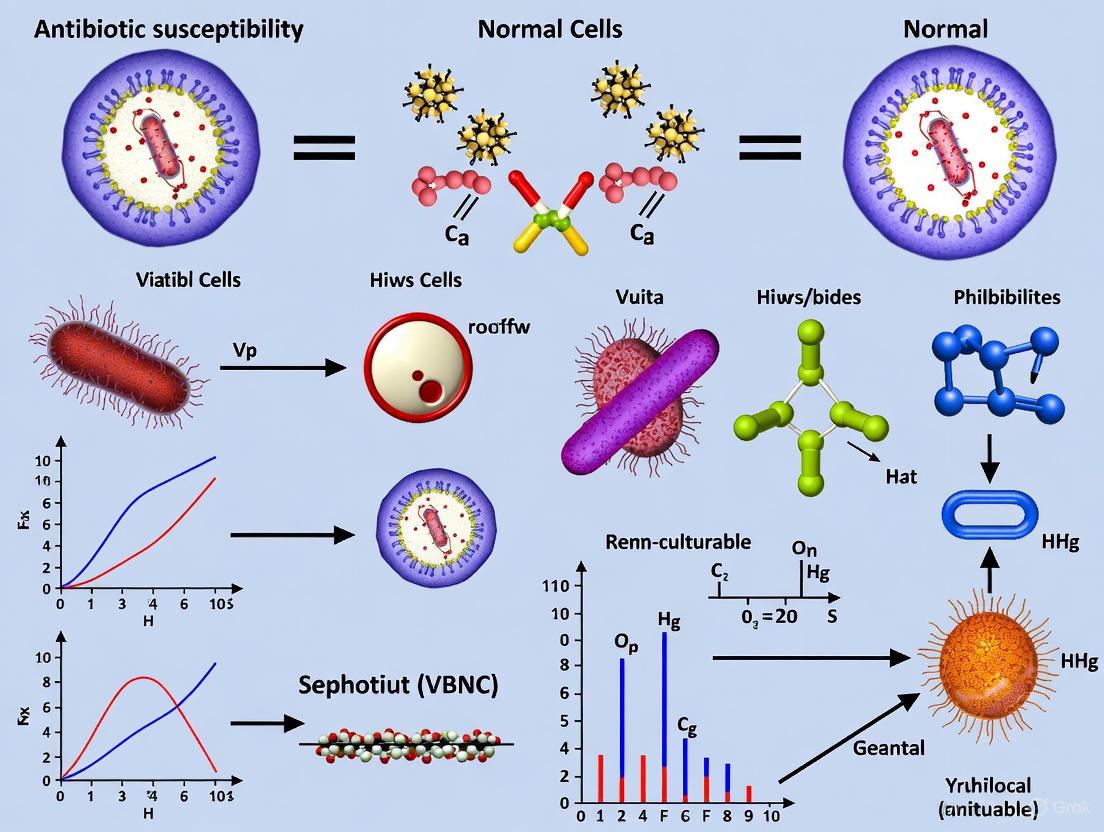
The following diagram illustrates the key molecular pathways involved in VBNC induction and resuscitation:
Antibiotic Susceptibility: VBNC vs Normal Cells
Comparative Antibiotic Tolerance Profiles
The antibiotic tolerance of VBNC cells represents one of the most significant characteristics of this physiological state. Multiple studies have demonstrated that VBNC cells exhibit dramatically enhanced tolerance to diverse classes of antibiotics compared to their culturable counterparts.
Table 2: Comparative Antibiotic Susceptibility of VBNC vs Normal Cells
| Bacterial Species | Induction Method | Antibiotic Challenge | Normal Cell Response | VBNC Cell Response | Proposed Mechanism |
|---|---|---|---|---|---|
| Escherichia coli [4] | Low-level chlorination (0.5 mg/L) | Ampicillin (200 μg/mL), Ofloxacin (5 μg/mL) | Susceptible at standard MIC | Tolerant (~128× MIC Amp, ~64× MIC Ofx) | Reduced metabolic activity, membrane modifications, stress response gene activation |
| Vibrio vulnificus [3] | Low temperature storage | Multiple antibiotic classes | Susceptible at standard MIC | Highly tolerant to various antibiotics | Toxin-antitoxin system mediated dormancy, general stress response |
| Klebsiella pneumoniae [6] | Artificial seawater at 4°C | Ciprofloxacin (3-18 μg/mL) | Inhibited growth | Maintained resuscitation capability after antibiotic removal | Reduced membrane permeability, metabolic shutdown |
| Multiple species [3] | Various environmental stresses | Broad-spectrum antibiotics | Growth inhibition | Significantly enhanced tolerance | Phenotypic plasticity without genetic changes |
Molecular Basis of Antibiotic Tolerance in VBNC Cells
The extraordinary antibiotic tolerance of VBNC cells stems from multiple interconnected physiological and molecular adaptations:
Metabolic Downregulation: The significantly reduced metabolic activity in VBNC cells decreases the efficacy of many antibiotics that target active cellular processes [3]. Since most antibacterial agents require some degree of metabolic activity for their mechanisms of action, the dormant state of VBNC cells provides inherent protection.
Membrane Modifications: VBNC cells undergo substantial changes in their cell envelope, including increased cross-linking in peptidoglycan, modifications to membrane fatty acid composition, and alterations in outer membrane protein profiles [2] [4]. These changes reduce membrane permeability, limiting antibiotic penetration into the cell.
Stress Response Activation: Transcriptomic analyses have revealed that VBNC cells upregulate various stress response genes, including those encoding chaperones, oxidative stress defense proteins, and DNA repair enzymes [4]. This enhanced stress response capability contributes to the increased antibiotic tolerance.
Toxin-Antitoxin System Mediated Dormancy: The activation of type II toxin-antitoxin systems leads to the specific inhibition of essential cellular processes, including translation and replication [3]. This regulated dormancy directly counteracts the mechanisms of many bacteriostatic and bactericidal antibiotics.
Research Reagent Solutions for VBNC Studies
Table 3: Essential Research Reagents for VBNC Studies
| Reagent/Category | Specific Examples | Function in VBNC Research | Application Notes |
|---|---|---|---|
| Viability Stains | LIVE/DEAD BacLight kit, SYTO 9/propidium iodide | Differentiate viable/damaged cells based on membrane integrity | Combine with microscopy or flow cytometry; cannot confirm culturability [10] [8] |
| DNA Binding Dyes | Propidium monoazide (PMA), Ethidium monoazide (EMA) | Selective amplification from viable cells with intact membranes | PMA preferred over EMA due to lower cytotoxicity to viable cells [5] [6] |
| Growth Media | Tryptic Soy Broth/Agar with modifications | Culturability assessment and resuscitation studies | May require additives (catalase, pyruvate) to reduce H₂O₂ stress [9] [3] |
| Induction Chemicals | Lutensol A03 with ammonium carbonate, Hydrogen peroxide, Peracetic acid | Controlled VBNC state induction | Lutensol/ammonium carbonate enables rapid induction (1 hour) for V. parahaemolyticus and V. cholerae [5] |
| Molecular Biology Kits | DNA/RNA extraction kits, Proteomic preparation kits | Downstream molecular analyses | Critical for transcriptomic and proteomic studies of VBNC mechanisms [9] [4] |
| PCR Reagents | qPCR/ddPCR master mixes, Species-specific primers | Detection and quantification of VBNC cells | Target single-copy genes; ddPCR enables absolute quantification without standard curves [6] |
Discussion and Future Perspectives
The VBNC state represents a significant challenge in clinical microbiology, food safety, and public health. The dramatically enhanced antibiotic tolerance of VBNC cells, combined with their ability to evade detection by conventional culture-based methods, creates a perfect storm for persistent infections and undetected contamination. The molecular mechanisms underlying VBNC formation—including toxin-antitoxin system activation, global transcriptomic reprogramming, and membrane modifications—provide insights into potential strategies for combating this dormant state.
Future research should focus on developing therapeutic approaches that specifically target VBNC cells, potentially by interfering with resuscitation signals or exploiting unique vulnerabilities of the dormant state. Additionally, the integration of advanced detection methods like PMA-ddPCR and AI-enabled hyperspectral microscopy into routine screening protocols could significantly improve our ability to identify VBNC pathogens in clinical, food, and environmental samples.
The systematic comparison of antibiotic susceptibility between VBNC and normal cells presented in this review underscores the critical need to consider phenotypic heterogeneity and dormancy states when designing antibiotic treatment regimens and public health interventions. As our understanding of the VBNC state continues to evolve, so too must our approaches to detecting and combating these elusive bacterial populations.
The viable but non-culturable (VBNC) state represents a critical survival strategy adopted by numerous bacterial species when confronted with adverse environmental conditions [11]. In this dormant state, bacteria lose the ability to form colonies on routine culture media—the gold standard of microbiological detection—while maintaining metabolic activity and cellular integrity [3] [12]. This phenomenon presents substantial challenges for clinical diagnostics, public health protection, and food safety, as VBNC cells evade conventional detection methods yet retain virulence potential and can resuscitate when conditions improve [11] [13].
The significance of the VBNC state extends beyond microbial ecology to direct clinical implications, particularly regarding antibiotic susceptibility profiles. Research has demonstrated that bacterial pathogens in the VBNC state exhibit markedly increased tolerance to antimicrobial treatments, including antibiotics to which their culturable counterparts remain susceptible [3] [12] [14]. This review systematically examines the environmental factors and clinical interventions that induce the VBNC state, compares the antibiotic susceptibility of VBNC cells versus their normal counterparts, and explores the molecular mechanisms underlying this altered phenotype, providing researchers with essential methodological frameworks for investigating this clinically relevant bacterial adaptation.
VBNC State Inducers and Experimental Conditions
Bacteria enter the VBNC state through diverse induction pathways, which can be broadly categorized into environmental stresses and clinical interventions. The table below summarizes key inducers, experimental parameters, and representative bacterial species documented to enter the VBNC state under these conditions.
Table 1: Key Inducers of the VBNC State and Experimental Conditions
| Inducer Category | Specific Inducer | Experimental Conditions | Representative Bacteria | Reference |
|---|---|---|---|---|
| Environmental Stresses | Low Temperature | 4°C in artificial seawater or sterile water | Vibrio vulnificus, E. coli O157:H7 | [11] [12] |
| Nutrient Starvation | Dilute media or sterile water | E. coli, Klebsiella pneumoniae | [11] | |
| Osmotic Stress | 7% NaCl solution | Campylobacter jejuni | [15] | |
| Unfavorable pH | Acidic or alkaline conditions | Staphylococcus aureus | [11] | |
| Clinical/Disinfection Interventions | Chlorine | 10 mg/L free chlorine, 1 min exposure | Listeria monocytogenes | [13] |
| Sub-lethal Photocatalysis | TiO2 nanotubes, 365 nm LED lamp | Antibiotic-resistant E. coli | [16] | |
| UV Radiation | Varying doses and exposure times | E. coli, Pseudomonas aeruginosa | [11] | |
| Antibiotics | Lethal doses of various antibiotic classes | Multiple species | [12] |
The induction of the VBNC state is not limited to a few species but has been documented in over 100 bacterial species to date, including significant human pathogens such as Escherichia coli, Vibrio cholerae, Legionella pneumophila, Listeria monocytogenes, and Mycobacterium tuberculosis [11]. The timeline for induction varies significantly, from rapid induction (less than 48 hours for C. jejuni under osmotic stress) to more gradual transitions (days or weeks for starvation at low temperatures) [11] [15].
Antibiotic Susceptibility: VBNC vs Normal Cells
A critical aspect of the VBNC state with profound clinical implications is the dramatic alteration in bacterial susceptibility to antimicrobial agents. The table below compares the antibiotic susceptibility profiles of VBNC cells with their normal, culturable counterparts, highlighting the increased tolerance observed in the VBNC state.
Table 2: Antibiotic Susceptibility Profile Comparison Between Normal and VBNC Bacterial Cells
| Characteristic | Normal (Culturable) Cells | VBNC Cells | Experimental Evidence |
|---|---|---|---|
| General Antibiotic Susceptibility | Susceptible to lethal doses | Highly tolerant to lethal doses | Biphasic killing curves; sustained viability post-treatment [12] |
| Underlying Mechanism | Genetic resistance (where present) | Phenotypic tolerance (non-heritable) | Non-genetic basis; reverts upon resuscitation [3] [12] |
| Metabolic Activity | Active metabolism and growth | Greatly reduced metabolic activity | Reduced translation, replication, and cell growth [3] [14] |
| Culturability Post-Exposure | Killed by effective antibiotics | Remain non-culturable but viable | Retain membrane integrity and viability [12] |
| Resuscitated Cells | N/A | Show higher antibiotic resistance than wild-type | Resuscitated E. coli showed increased antibiotic resistance [16] |
The antibiotic tolerance observed in VBNC cells is primarily attributed to their dormant state and dramatically reduced metabolic activity [3]. Since many antibiotics target active cellular processes such as cell wall synthesis, protein production, and DNA replication, the near-complete cessation of these processes in VBNC cells renders these antimicrobials ineffective [12] [14]. This tolerance is phenotypic and transient rather than resulting from genetic mutations, distinguishing it from conventional antibiotic resistance [12].
Molecular Mechanisms and Signaling Pathways
The transition into and maintenance of the VBNC state is governed by sophisticated molecular mechanisms that regulate bacterial physiology in response to stress. The diagram below illustrates the key signaling pathways and molecular events involved in VBNC state induction and the consequent antibiotic tolerance.
Diagram 1: Molecular mechanisms and signaling pathways in VBNC state induction and antibiotic tolerance. The diagram illustrates how environmental stresses and clinical interventions trigger specific molecular events leading to VBNC state entry and associated antibiotic tolerance.
The molecular events depicted in the diagram include several key processes:
Reactive Oxygen Species (ROS) Accumulation: Multiple stresses induce oxidative damage, triggering defense responses that contribute to dormancy [16]. Repair of oxidative damage, coupled with changes in energy allocation centered around intracellular ATP levels, serves as a driving force for subsequent resuscitation [16].
Toxin-Antitoxin (TA) System Activation: Under stress conditions, unstable antitoxins are degraded, freeing toxins that inhibit essential cellular processes including translation, replication, and cell growth [3] [14]. These systems are genetically programmed modules that respond to environmental cues by dramatically slowing bacterial metabolism [14].
Metabolic Downregulation: The combined action of ROS accumulation and TA system activation leads to dramatic reduction in metabolic activity, which directly contributes to antibiotic tolerance by reducing the cellular targets of antimicrobial agents [3] [12].
The molecular control of the VBNC state shares significant overlap with mechanisms governing bacterial persistence, suggesting these phenomena exist on a continuum of bacterial dormancy rather than representing entirely distinct states [12] [14].
Detection Methodologies and Experimental Protocols
Accurate detection and quantification of VBNC cells presents significant methodological challenges, as these cells cannot be cultured using conventional techniques. The table below summarizes key methodologies employed in VBNC research, along with their principles, experimental workflows, and applications.
Table 3: Methodologies for VBNC Cell Detection and Quantification
| Method Category | Specific Method | Principle | Experimental Protocol | Applications |
|---|---|---|---|---|
| Viability Staining | LIVE/DEAD BacLight | Membrane integrity detection using SYTO9/PI | Stain application, incubation, microscopy/flow cytometry | Differentiation of live/dead cells; can overestimate VBNC in complex matrices [11] [13] |
| Molecular Methods | PMA-qPCR | PMA dye penetrates dead cells; inhibits DNA amplification | PMA treatment (20 μM), photoactivation, DNA extraction, qPCR | Specific detection of viable cells; quantification of VBNC cells [13] [15] |
| Molecular Methods | EMA/PMAxx-qPCR | Combined dye approach for enhanced discrimination | EMA (10 μM) + PMAxx (75 μM), 40°C for 40 min, light activation | Improved VBNC detection in complex water matrices [13] |
| Advanced Molecular | ddPCR with PMA | Absolute quantification without standard curve | Oil-enveloped bacterial cells, PMA treatment, droplet digital PCR | Highly accurate VBNC quantification; Vibrio cholerae detection [17] |
| Functional Assays | DVC (Direct Viable Count) | Cell elongation in presence of antibiotics | Nalidixic acid + nutrients, incubation, microscopy | Detection of viable cells based on growth potential [11] |
The experimental workflow for investigating VBNC state induction and antibiotic susceptibility typically follows a logical sequence of steps, as illustrated in the diagram below.
Diagram 2: Experimental workflow for VBNC state induction and antibiotic susceptibility profiling. The diagram outlines the key phases in investigating VBNC cells, from initial induction through antibiotic exposure to resuscitation profiling.
Critical considerations for VBNC research methodologies include:
Method Validation: No single method perfectly detects VBNC cells in all contexts. Flow cytometry, for instance, while often recommended, may overestimate dead cells in complex matrices like process wash water [13].
Matrix Effects: The composition of the sample matrix significantly influences method performance. The combination of EMA and PMAxx dyes has shown particular effectiveness in complex water matrices with high organic matter content [13].
Culture-Based Confirmation: Despite their limitations, culture methods remain essential for confirming non-culturability and demonstrating resuscitation potential.
The Scientist's Toolkit: Essential Research Reagents
Research into the VBNC state requires specialized reagents and methodologies to accurately detect, quantify, and characterize these dormant cells. The table below outlines essential research reagents and their specific applications in VBNC studies.
Table 4: Essential Research Reagents for VBNC Cell Investigation
| Reagent Category | Specific Reagent | Function/Application | Example Usage | Considerations |
|---|---|---|---|---|
| Viability Dyes | PMA (Propidium Monoazide) | Penetrates compromised membranes; inhibits DNA amplification from dead cells | PMA-qPCR for viable cell quantification (20 μM) | Requires photoactivation; concentration must be optimized [13] [15] |
| Viability Dyes | PMAxx | Enhanced version of PMA with improved dead cell DNA binding | Combined with EMA for complex matrices | More effective than PMA alone in certain applications [13] |
| Viability Dyes | EMA (Ethidium Monoazide) | DNA intercalating dye; penetrates via efflux pumps | EMA/PMAxx combination (10 μM EMA) | Can penetrate some viable cells; use with caution [13] |
| Viability Dyes | SYTO9/PI (LIVE/DEAD BacLight) | Dual staining for membrane integrity | Fluorescence microscopy/flow cytometry | Can overestimate VBNC in complex samples [11] [13] |
| Molecular Biology | qPCR Reagents | Detection and quantification of bacterial DNA | Species-specific gene amplification | Cannot differentiate viable/dead cells without viability dyes [15] |
| Molecular Biology | ddPCR Reagents | Absolute quantification without standard curves | VBNC cell enumeration with PMA | Higher accuracy than qPCR; no standard curve needed [17] |
| Induction Agents | TiO2 Nanotubes | Photocatalytic induction of VBNC state | Sub-lethal photocatalysis stress | Controlled induction for mechanistic studies [16] |
| Culture Media | Resuscitation Media | Nutrient-rich media for VBNC cell recovery | Testing resuscitation potential | Composition varies by bacterial species [11] |
The selection of appropriate reagents depends heavily on the specific research objectives and the bacterial species under investigation. For instance, PMA-qPCR has been successfully optimized for VBNC Campylobacter jejuni detection with a limit of detection of 2.43 log CFU/mL in pure culture and 3.12 log CFU/g in spiked chicken breasts [15]. Similarly, ddPCR with PMA treatment has shown enhanced sensitivity for absolute quantification of VBNC Vibrio cholerae cells without requiring DNA extraction [17].
The VBNC state represents a sophisticated bacterial survival strategy with far-reaching implications for clinical medicine, public health, and food safety. Through systematic investigation of VBNC inducers—from environmental stresses to clinical interventions—researchers have uncovered profound alterations in antibiotic susceptibility profiles that complicate treatment and eradication protocols. The experimental methodologies and research reagents detailed in this review provide essential tools for advancing our understanding of this complex phenomenon.
Future research directions should focus on elucidating the precise molecular switches that control entry into and exit from the VBNC state, developing standardized detection methods applicable across diverse clinical and environmental samples, and identifying therapeutic approaches that either prevent VBNC state induction or effectively target dormant bacterial populations. As evidence accumulates regarding the increased antibiotic resistance of resuscitated VBNC cells [16] [18], addressing the challenge posed by this dormant state becomes increasingly urgent for effective antimicrobial stewardship and public health protection.
The viable but non-culturable (VBNC) state is a unique survival strategy adopted by many bacteria in response to adverse environmental conditions [19]. When bacteria enter this state, they lose the ability to form colonies on routine culture media—the standard method for detecting viability—while maintaining metabolic activity and cellular integrity [20]. This phenomenon has profound implications for public health, food safety, and clinical medicine, as VBNC pathogens cannot be detected by conventional methods but may retain virulence and resuscitate under favorable conditions [19] [20]. Within the context of antibiotic susceptibility research, understanding the fundamental hallmarks of VBNC cells is crucial, as these dormant cells exhibit dramatically increased tolerance to antimicrobial treatments compared to their normal, culturable counterparts [3] [4]. This guide systematically compares the morphological, physiological, and metabolic characteristics of VBNC cells against normal bacterial cells, providing researchers with a comprehensive framework for investigating this elusive bacterial state.
Defining the VBNC State
The VBNC state represents a distinct survival state fundamentally different from both normal cellular activity and cell death. First described in 1982 for Escherichia coli and Vibrio cholerae [20], the VBNC condition is now recognized in numerous human bacterial pathogens [19] [21]. While VBNC cells are unable to proliferate on conventional media that typically support their growth, they maintain viability markers including membrane integrity, metabolic activity, gene expression, and the potential for resuscitation [20]. This state is typically induced by various environmental stresses such as nutrient starvation, temperature extremes, improper osmotic pressure, oxygen concentrations, and exposure to disinfectants or antibiotics [3] [20].
It is important to distinguish VBNC cells from other non-growing states. Unlike persister cells, which are also dormant and antibiotic-tolerant but represent a phenotypic variant within a growing population, VBNC cells encompass the entire population under specific conditions and exhibit a more comprehensive shutdown of growth functions [20]. Additionally, while dead cells have compromised membranes and no metabolic activity, VBNC cells maintain membrane integrity and continue limited metabolic functions [20]. The entry into the VBNC state is not a degenerative process but rather an adaptive strategy that enables long-term survival under unfavorable conditions, with the ability to resuscitate when conditions improve [19] [20].
Morphological and Structural Hallmarks
Cell Size and Shape Transformations
VBNC cells undergo significant morphological changes that distinguish them from their culturable counterparts. The most consistent alteration is a reduction in cell size, leading to an increased surface area to volume ratio, which is thought to minimize energy requirements for maintenance [20]. For example, Campylobacter jejuni transitions from its characteristic spiral shape in the exponential phase to a coccoid form in the VBNC state [20]. Similarly, Vibrio cholerae and Burkholderia pseudomallei change from rods during exponential growth to cocci in the VBNC state [20].
Quantitative analysis reveals substantial changes in cellular dimensions. Studies on Campylobacter jejuni demonstrated a notable increase in cell volume during the VBNC state, with average cell volumes measuring 1.73 μL/mg protein for culturable forms compared to 10.96 μL/mg protein after 30 days of incubation in microcosm water [21]. This dramatic size change represents a more than six-fold increase in volume, reflecting fundamental structural reorganization.
Table 1: Morphological Changes in VBNC Cells Compared to Normal Cells
| Bacterial Species | Normal Cell Morphology | VBNC Cell Morphology | Documented Size Changes |
|---|---|---|---|
| Campylobacter jejuni | Spiral rods | Coccoid | Volume increase from 1.73 to 10.96 μL/mg protein [21] |
| Vibrio cholerae | Rod-shaped | Coccoid | Cell dwarfing commonly observed [20] |
| Escherichia coli | Rod-shaped | Smaller rods/spheres | No remarkable size change under chlorination [4] |
| Salmonella enterica | Rod-shaped | Spherical | Shape change from rod to sphere [22] |
Cell Wall and Membrane Modifications
The structural components of VBNC cells undergo significant modifications that contribute to their enhanced resilience. Changes in the outer membrane proteome have been documented in several species, with these alterations being highly dependent on the specific conditions used to induce the VBNC state [20]. In E. coli, differential expression of three outer membrane proteins (Omp)—antigen 43 β-subunit, TolC, and OmpT—was observed in cells exposed to nutrient-limited conditions, with the most dramatic changes (106 modulated proteins) occurring in cells exposed to natural seawater and light [20].
Fatty acid composition also undergoes marked changes during VBNC transition. Vibrio vulnificus shows significant increases in the percentage of unsaturated fatty acids and fatty acids with less than 16 carbons when entering the VBNC state, with notable changes in the percentages of hexadecanoic, hexadecenoic, and octadecanoic acids [20]. Additionally, enhanced peptidoglycan cross-linking has been observed in VBNC cells of Enterococcus faecalis, potentially contributing to increased resistance to environmental stresses [20].
These structural modifications have functional consequences. E. coli O157:H7 induced into the VBNC state by L-malic acid at low temperature showed maintained basic function of the cell membrane despite reduced cell size and respiratory activity [22]. Meanwhile, chlorination-induced VBNC E. coli displayed increased membrane permeability while maintaining cellular integrity [4].
Physiological and Metabolic Alterations
Metabolic Activity and Energy Conservation
VBNC cells exhibit a pronounced downshift in metabolic activity as a central survival strategy. While they maintain detectable metabolic functions, the overall metabolic rate is significantly reduced compared to normal cells [20]. This metabolic reconfiguration serves to conserve energy and enhance survival under adverse conditions. However, the degree of metabolic reduction varies depending on the inducing stressor, as demonstrated by studies using different detection methods. When assessed using 5-cyano-2,3-ditolyl tetrazolium chloride combined with flow cytometry (CTC-FCM), the respiratory activity of UV-induced VBNC bacteria showed minimal variation unless exposed to very high UV doses (200 mJ/cm²) [23]. In contrast, when measured by D₂O-labeled Raman spectroscopy—which assesses overall metabolic activity through microbial deuterium incorporation—a clear dose-response relationship was observed, with higher UV doses resulting in progressively lower metabolic activity [23].
The adenylate energy charge (AEC), a key indicator of cellular energy status, undergoes dramatic changes in VBNC cells. In Campylobacter jejuni, the AEC drops significantly from normal levels to between 0.66 and 0.26 after just one day of incubation in microcosm water [21]. After 30 days, AMP becomes the only detectable nucleotide in these cells, indicating a severely compromised energy state [21]. This reduction in energy charge reflects the transition to a maintenance-only metabolic mode.
Table 2: Metabolic and Physiological Parameters in VBNC vs Normal Cells
| Parameter | Normal Cells | VBNC Cells | Detection Methods |
|---|---|---|---|
| Adenylate Energy Charge | High (typically >0.8) | Low (0.66-0.26) to only AMP detectable [21] | HPLC measurement of ATP, ADP, AMP |
| Respiratory Activity | High | Reduced but detectable [23] [22] | CTC-FCM |
| Overall Metabolic Activity | High | Significantly reduced, heterogeneous [23] | D₂O-labeled Raman Spectroscopy |
| Membrane Potential | High | Significantly lower [21] | Fluorometric assays |
| Internal pH Maintenance | Normal (0.6-0.9 pH unit difference) | Progressive decrease [21] | Internal pH probes |
Gene Expression and Protein Synthesis
VBNC cells undergo comprehensive reprogramming of gene expression that underlies their physiological adaptations. Transcriptomic analyses reveal significant alterations in expression patterns across multiple functional categories. In Vibrio cholerae, 58 genes related to regulatory functions, cellular processes, energy metabolism, transport, and binding were induced by more than 5-fold in the VBNC state [20]. Conversely, another study reported reduced expression of 16S rRNA and mRNA levels of tuf, rpoS, and relA genes, which are responsible for protein synthesis and stress responses [20].
The expression of specific outer membrane proteins shows marked changes during VBNC transition. In E. coli, ompW expression is significantly induced in VBNC cells [20]. This protein may play a role in stress adaptation, though its exact function in the VBNC state requires further elucidation. Additionally, ribosomal activity is substantially reduced in VBNC cells, with decreased expression levels of ribosome-associated proteins including ribosomal-associated inhibitor (RaiA), 40S ribosomal subunit (S6), and bacterioferritin comigratory protein (Bcp) compared to normal cells [19].
Proteomic profiles of VBNC cells reflect their metabolic reorientation. Food isolates of E. coli O157 in the VBNC state showed decreased levels of oxidation-responsive factors (AhpCF and AceF) but exhibited a distinct increase in outer-membrane protein W (OmpW) levels [19]. Vibrio parahaemolyticus in the VBNC state up-regulates proteins associated with transcription, translation, ATP synthase, gluconeogenesis-related metabolism, and antioxidants [19]. This selective preservation of certain metabolic pathways while downregulating others appears to be a conserved feature of the VBNC state.
Homeostasis and Membrane Functions
The maintenance of cellular homeostasis is fundamentally altered in VBNC cells. Ion gradient maintenance is significantly compromised, with VBNC cells of Campylobacter jejuni showing substantially reduced internal potassium content compared to culturable forms [21]. The membrane potential is also significantly lower in the VBNC state, further indicating disruption of normal energy-transducing functions [21].
The ability to regulate internal pH is markedly impaired in VBNC cells. While culturable Campylobacter jejuni cells maintain a difference of 0.6 to 0.9 pH units between internal and external pH values, this difference decreases progressively with incubation time in microcosm water in VBNC cells [21]. This failure of pH homeostasis reflects the compromised energy status and reduced membrane function in VBNC cells.
Despite these alterations, VBNC cells maintain membrane integrity, which distinguishes them from dead cells. Studies using viability stains based on membrane integrity, such as the LIVE/DEAD BacLight assay, confirm that VBNC cells maintain an intact membrane that excludes certain dyes [20] [4]. However, increased membrane permeability has been documented in some VBNC cells induced by specific stressors, such as chlorination in E. coli [4].
Experimental Assessment Methodologies
Detection and Enumeration Techniques
Accurate detection of VBNC cells requires specialized methodologies that bypass the limitations of conventional culture-based approaches. The most widely used techniques combine viability indicators with direct microscopic or flow cytometric enumeration.
The CTC-DAPI staining method allows simultaneous assessment of respiratory activity and total cell count. In this protocol, 5-cyano-2,3-ditolyl tetrazolium chloride (CTC) is used as an indicator of respiratory activity—respiring cells reduce CTC to insoluble, fluorescent formazan crystals [21]. DAPI (4',6-diamino-2-phenylindole) stains all cells fluorescent blue by binding to DNA [21]. The specific protocol involves:
- Incubating samples with CTC (final concentration 2-5 mM) for 60-90 minutes at appropriate temperature
- Fixing with neutral-buffered formalin (final concentration 2%) for 15 minutes
- Staining with DAPI (final concentration 1-5 μg/mL) for 5-10 minutes
- Filtering through black polycarbonate membranes (0.2 μm pore size)
- Enumeration using epifluorescence microscopy or flow cytometry [21]
D₂O-labeled Raman spectroscopy provides an alternative approach for assessing metabolic activity at both population and single-cell levels. The experimental workflow consists of:
- Incubating bacterial cells in deuterium oxide (D₂O)-supplemented medium (typically 20-30% D₂O)
- Allowing incorporation of deuterium into newly synthesized biomolecules for 6-24 hours
- Fixing cells with paraformaldehyde (2-4%) for stability
- depositing cells on aluminum-coated slides for analysis
- Measuring Raman spectra with a confocal Raman microscope
- Calculating the CD/(CD+CH) ratio from the C-D (2040-2300 cm⁻¹) and C-H (2800-3100 cm⁻¹) bands as an index of metabolic activity [23]
Standardized protocols for inducing and resuscitating VBNC states are essential for experimental reproducibility across studies.
Microcosm water induction provides a controlled environment for VBNC formation:
- Grow bacterial cultures to late exponential or stationary phase
- Harvest cells by gentle centrifugation (3000 × g, 10 minutes)
- Wash twice in sterile water or saline to remove residual nutrients
- Resuspend in filter-sterilized (0.2 μm pore size) natural water or simulated oligotrophic medium at pH 6.0-7.0
- Incubate at induction temperature (typically 4°C for mesophilic pathogens) with gentle shaking (100 rpm)
- Monitor culturability by plate counts and viability by direct methods over 15-30 days [21]
Chemical induction methods include:
- Chlorine induction: Expose cells to 0.5 mg/L chlorine for 6 hours at room temperature [4]
- L-malic acid induction: Treat cells with 0.12-0.25 mM L-malic acid at 4°C for extended periods [22]
- Sub-lethal photocatalysis: Expose cell suspensions to TiO₂ nanotubes illuminated with 365 nm LED lamp (100 mW/cm²) for 1-10 hours [16]
Resuscitation protocols typically involve:
- Transferring VBNC cells to nutrient-rich media such as Brain Heart Infusion or LB broth
- Incubating at optimal growth temperatures
- Monitoring culturability restoration over 24-48 hours [16] [4]
- For challenging strains, adding resuscitation-promoting factors (Rpfs) or using host systems like embryonated eggs [19] [20]
Diagram 1: VBNC State Transitions and Assessment Methods. This workflow illustrates the induction of the VBNC state by environmental stressors, the key methods for detection, and the potential for resuscitation under favorable conditions.
The Scientist's Toolkit: Essential Research Reagents
Table 3: Essential Research Reagents for VBNC Cell Studies
| Reagent/Category | Specific Examples | Research Function | Key Applications |
|---|---|---|---|
| Viability Stains | CTC, DAPI, SYTO 9, PI | Differentiate viable cells based on membrane integrity and metabolic activity | Direct viable counts, respiratory activity assessment [21] [23] |
| Molecular Biology Reagents | PCR/qPCR reagents, RNA-seq kits | Detect gene expression and virulence genes in VBNC cells | Transcriptomic analysis, virulence gene detection [19] [4] |
| Metabolic Labels | Deuterium oxide (D₂O) | Track metabolic activity through deuterium incorporation | Raman spectroscopy metabolic assessment [23] |
| Induction Media | Microcosm water, oligotrophic buffers | Simulate natural stressful conditions for VBNC induction | Controlled VBNC state formation [21] [22] |
| Resuscitation Promoters | Rpf proteins, nutrient broths, host cell systems | Reactivate VBNC cells to culturable state | Resuscitation studies, virulence assessment [19] [16] |
| Antibiotics | Ampicillin, ofloxacin, other antimicrobials | Assess antibiotic tolerance of VBNC cells | Antibiotic susceptibility testing [3] [4] |
Implications for Antimicrobial Susceptibility
The morphological, physiological, and metabolic shifts in VBNC cells have profound implications for their antibiotic susceptibility profiles. VBNC cells exhibit dramatically increased tolerance to a wide range of antimicrobial agents compared to their normal, culturable counterparts [3]. This enhanced tolerance presents significant challenges for clinical treatment and public health interventions.
The mechanisms underlying this tolerance are multifaceted. The greatly reduced metabolic activity and downregulated cellular processes in VBNC cells decrease the efficacy of many antibiotics that target active cellular functions [3]. Additionally, structural changes such as increased peptidoglycan cross-linking and membrane modifications may reduce permeability to antimicrobial agents [20]. Research has demonstrated that E. coli in the VBNC state can persist in the presence of extremely high antibiotic concentrations—up to 200 μg/mL ampicillin and 5 μg/mL ofloxacin (approximately 128× and 64× the MIC, respectively) [4]. Similarly, Vibrio vulnificus in the VBNC state exhibits enhanced tolerance to heat, oxidative stress, osmotic stress, pH fluctuations, ethanol, antibiotics, and heavy metals [20].
This antibiotic tolerance has direct clinical relevance. After resuscitating from the VBNC state, E. coli cells showed higher antibiotic resistance than wild-type cells [16]. The persistence of VBNC pathogens in clinical settings may contribute to recurrent infections and treatment failures, particularly in biofilm-associated infections where dormant cells are protected from antimicrobial therapies [24]. Understanding the unique hallmarks of VBNC cells is therefore essential for developing strategies to combat these persistent bacterial populations.
The viable but nonculturable (VBNC) state is a dormant survival strategy adopted by numerous bacterial species when confronted with environmental stress [25]. Cells in this state are characterized by a loss of culturability on routine laboratory media, while maintaining metabolic activity and pathogenic potential [12] [20]. The resuscitation of these dormant cells back to an active, culturable state represents a significant public health threat, contributing to recurrent infections, foodborne illness outbreaks, and antimicrobial treatment failures [26] [25]. This phenomenon is of particular concern within the context of antibiotic resistance, as research indicates that resuscitated VBNC cells can exhibit enhanced antibiotic resistance compared to their pre-dormant counterparts [16] [18]. Understanding the mechanisms governing this transition is therefore critical for developing novel therapeutic strategies to control persistent and chronic infections. This guide objectively compares the antibiotic susceptibility profiles of VBNC and normal cells, supported by experimental data and detailed methodologies from current research.
VBNC State vs. Antibiotic Persistence: A Critical Distinction
While both the VBNC state and antibiotic persistence represent dormant, stress-tolerant phenotypes, they are distinct physiological states. It is essential to differentiate them, particularly in experimental design and data interpretation.
Table: Distinguishing VBNC Cells from Antibiotic Persisters
| Characteristic | VBNC State | Antibiotic Persisters |
|---|---|---|
| Culturability | Complete loss on standard media [25] | Retained, population exhibits biphasic killing [12] |
| Induction Stress | Wider range of moderate, long-term stresses (starvation, temperature, disinfection) [25] | Often specific stresses, notably antibiotics [12] |
| Metabolic Activity | Low but measurable [25] [20] | Low, can be below detection limit [12] |
| Resuscitation Trigger | Requires specific stimuli (e.g., nutrient addition, stress removal, Rpf) [26] [25] | Often resumes growth upon antibiotic removal [12] |
| Population Dynamics | Entire population becomes nonculturable [16] | A small, tolerant subpopulation within a larger susceptible one [12] |
The relationship between these states is sometimes described as a dormancy continuum, where active cells may first transition into persisters, which can then enter the deeper dormancy of the VBNC state under prolonged stress [12] [27].
Quantitative Comparison of Antibiotic Susceptibility
Experimental data consistently demonstrates that VBNC cells possess a significantly higher tolerance to antibiotics and other chemical stresses compared to their culturable, normal-state cells. The following table synthesizes key findings from recent studies.
Table: Experimental Comparison of Stress Resistance in VBNC vs. Normal Cells
| Bacterial Species | Inducing Stress | Key Experimental Finding | Reference |
|---|---|---|---|
| E. coli (ARB & ASB) | Sub-lethal photocatalysis | Resuscitated cells showed higher antibiotic resistance than wild-type cells. | [16] [18] |
| Vibrio vulnificus | Multiple | VBNC cells exhibited higher resistance to heat, low pH, ethanol, antibiotics, heavy metals, and oxidative/osmotic stress than exponential-phase cells. | [20] |
| Enterococcus faecalis | Starvation/Oligotrophy | VBNC cells showed increased tolerance to antibiotics including ampicillin and vancomycin. | [20] |
| Campylobacter jejuni | Not Specified | VBNC cells demonstrated greater tolerance to chlorine and antibiotics. | [20] |
| E. coli O157:H7 | Copper | VBNC state induced by copper could be reversed by chelating agents, demonstrating tolerance during dormancy. | [26] |
The intrinsic tolerance of VBNC cells is attributed to their drastically reduced metabolic activity, which renders many bactericidal antibiotics that target active cellular processes ineffective [12] [20]. Furthermore, structural changes like increased peptidoglycan cross-linking can enhance physical robustness [20].
To provide a reproducible methodology for researchers, the following workflow details a protocol adapted from a key study on antibiotic-resistant bacteria (ARB) [16] [18].
Key Experimental Steps and Notes
- Bacterial Strains and VBNC Induction: The protocol utilizes both antibiotic-resistant (ARB) and antibiotic-susceptible bacteria (ASB) E. coli strains. VBNC state is induced via sub-lethal photocatalysis using a TiO₂ nanotube system under LED light (365 nm) for 1-10 hours. The "sub-lethal" condition is critical, as it causes damage without immediate cell death, triggering the dormancy response [16].
- Confirmation of VBNC State: A definitive confirmation requires demonstrating zero culturable cells (CFU/mL = 0) on agar plates that normally support growth, coupled with positive signals from viability assays (e.g., LIVE/DEAD staining showing membrane integrity) [25]. A decrease in cell length is a common morphological indicator [16] [20].
- Resuscitation and Analysis: Resuscitation is initiated by removing the inductive stress, typically by transferring cells to a nutrient-rich medium like LB broth, and incubating at an optimal growth temperature (e.g., 37°C for E. coli) for 5-20 days. The recovery of culturability is monitored by plate counts. Analysis of resuscitated cells should include antibiotic resistance profiling to compare with pre-dormancy levels, often showing increased resistance [16] [18]. Molecular techniques like qPCR can be used to assess the repair of oxidative damage, a key driver of resuscitation [16].
The resuscitation of VBNC cells is not a simple reversal of the entry process but an active biological event driven by specific molecular pathways. The current research highlights several key mechanisms.
The primary drivers for resuscitation include the repair of oxidative damage and changes in energy allocation, with intracellular ATP and metabolic activity being the major force [16] [26]. This process requires de novo synthesis of proteins and cell wall components, as inhibitors like chloramphenicol and penicillin can block resuscitation [26]. In some species, specific signaling molecules like Resuscitation Promoting Factors (Rpfs) or autoinducers are involved, suggesting a regulated process [26].
The Scientist's Toolkit: Essential Research Reagents
The following table catalogues key reagents and their applications for studying the VBNC state and resuscitation.
Table: Essential Reagents for VBNC State Research
| Reagent / Material | Function / Application | Experimental Example |
|---|---|---|
| TiO₂ Nanotubes | A catalyst for inducing VBNC state via sub-lethal photocatalysis. | Used with LED light to generate oxidative stress, inducing VBNC state in E. coli [16]. |
| LIVE/DEAD Staining Kits (e.g., with SYBR Green/PI) | Differentiating viable cells (with intact membranes) from dead cells. | Confirming viability of nonculturable cells during VBNC state confirmation [25] [20]. |
| ATP Assay Kits | Quantifying intracellular ATP levels as a direct measure of metabolic activity. | Demonstrating that VBNC cells maintain high ATP levels, a key criterion and driver for resuscitation [16] [20]. |
| Resuscitation Promoting Factors (Rpfs) | Bacterial cytokine-like proteins that stimulate resuscitation from dormancy. | Added to resuscitation medium to promote the recovery of VBNC cells in certain species [26]. |
| Sodium Pyruvate / Catalase | Peroxidase supplements that degrade residual hydrogen peroxide in media. | Used to exclude the possibility that regrowth is from H₂O₂-sensitive culturable cells, thereby confirming true resuscitation [26]. |
| Specific Antibiotics (e.g., Ampicillin) | Selective agents to inhibit the growth of any remaining culturable cells. | Added to resuscitation medium to ensure that observed growth originates from VBNC cells, not a few residual culturable cells [26]. |
| qPCR Reagents | Quantifying gene expression changes during induction and resuscitation. | Analyzing expression of genes related to oxidative damage repair, stress response, and virulence [16] [18]. |
The phenomenon of bacterial resuscitation from the VBNC state presents a formidable challenge in clinical and environmental microbiology. The experimental data clearly demonstrates that this is not a regrowth artifact but a genuine return from a deep state of dormancy, often resulting in cells with enhanced resistance traits [16] [18]. The molecular mechanisms, while not fully elucidated, involve active repair processes and metabolic rewiring [16] [26]. For researchers and drug development professionals, acknowledging this survival strategy is paramount. Future therapeutic development must move beyond targeting actively growing cells and consider strategies to either prevent entry into the VBNC state, permanently eradicate dormant cells, or interfere with the resuscitation machinery itself. Standardized methodologies, as outlined in this guide, are essential for generating reproducible and comparable data to advance our understanding and overcome this hidden reservoir of bacterial persistence and antibiotic resistance.
Beyond Plate Counts: Advanced Methodologies for VBNC Cell Detection and Antibiotic Susceptibility Profiling
Standard antimicrobial efficacy testing, reliant on culture-based methods, operates with a significant blind spot: the inability to detect bacteria in the viable but non-culturable (VBNC) state. This dormant survival strategy is induced by various environmental stresses, including sub-lethal antibiotic exposure, disinfectants, and food processing conditions. VBNC cells maintain metabolic activity and virulence potential while losing cultivability on routine media, leading to a critical underestimation of microbial risk and therapeutic failure. This guide compares the antimicrobial susceptibility profiles of VBNC cells to their normal, culturable counterparts, synthesizing experimental data to highlight the limitations of conventional testing and the advanced methodologies required to evaluate the true efficacy of antimicrobial interventions.
The VBNC State: A Survival Strategy Beyond Culturability
The viable but non-culturable (VBNC) state is a survival mechanism employed by numerous bacterial species in response to adverse environmental conditions. Cells in this state are defined by their loss of cultivability on media that normally support their growth, while maintaining viability, metabolic activity, and the potential to resuscitate when conditions become favorable [25]. This state can be induced by a wide array of stresses common in clinical, industrial, and natural environments, including nutrient starvation, temperature shifts, osmotic challenges, and exposure to sub-lethal concentrations of biocides and antibiotics [12] [25].
Critically, the VBNC state is fundamentally different from bacterial persistence. While both represent non-growing phenotypes, persister cells remain culturable and their phenotype is typically reversible upon removal of the antibiotic. In contrast, VBNC cells are non-culturable and require specific resuscitation signals to return to a growth-capable state [12] [25]. The formation of VBNC cells is now recognized as a nearly universal strategy across bacterial species, posing a significant challenge to public health by contributing to recurrent infections and the undetected spread of antibiotic resistance [12].
Comparative Susceptibility: VBNC vs. Normal Cells
The following tables summarize experimental data from key studies, demonstrating the markedly increased tolerance of VBNC cells to antimicrobials compared to their culturable counterparts.
Table 1: Antibiotic Tolerance of VBNC E. coli Induced by Different Stressors
| Inducing Stressor | Antibiotic Challenge | Response of Culturable (Normal) Cells | Response of VBNC Cells | Experimental Reference |
|---|---|---|---|---|
| Low-Level Chlorination (0.5 mg/L) | Ampicillin (200 µg/mL); Ofloxacin (5 µg/mL) | Susceptible (Standard MIC) | High tolerance to ~128x and ~64x MIC, respectively | [4] |
| Sub-Lethal Photocatalysis | Not Specified | Susceptible (Standard MIC) | Resuscitated cells showed higher antibiotic resistance than wild-type | [28] |
| General VBNC State Induction | Various Antibiotics | Susceptible (Standard MIC) | Exhibit drastically increased tolerance and persistence | [3] [12] |
Table 2: Antimicrobial Tolerance of VBNC Pathogens Beyond E. coli
| Bacterial Species | VBNC Inducing Condition | Antimicrobial Challenge | Key Finding on VBNC Tolerance | Experimental Reference |
|---|---|---|---|---|
| Vibrio vulnificus | Starvation, Cold | Heat, Oxidative Stress, Osmotic Stress, Antibiotics, Heavy Metals | Protected against a variety of potentially lethal environmental challenges | [4] |
| Campylobacter jejuni | Acid, Cold, Osmotic (Poultry Processing) | Carvacrol, Diallyl Sulfide, Al₂O₃ Nanoparticles | High level of persistence to plant-based antimicrobials; only high conc. of Al₂O₃ NPs achieved >1 log reduction | [29] |
| Various (E. coli, E. faecalis, V. vulnificus) | Multiple | Various Antibiotics | Greater resistance to antibiotics compared to culturable counterparts | [29] |
Methodologies for Investigating VBNC Susceptibility
Conventional antimicrobial susceptibility testing (AST) relies on culture-based methods like broth microdilution and disk diffusion, which measure growth inhibition. These methods are intrinsically incapable of detecting VBNC cells, leading to a complete oversight of this resistant subpopulation [3]. Researchers must therefore employ a combination of viability markers and molecular techniques to assess the antimicrobial effects on VBNC states.
Key Experimental Protocols
1. Induction of the VBNC State:
- Stressor Application: Expose a mid-logarithmic phase bacterial culture to a sub-lethal stressor. Common inducers include:
- Monitoring Induction: Monitor the culture daily using plate counts. The VBNC state is considered induced when the colony-forming unit (CFU) count drops to zero on appropriate solid media, while viability is confirmed via methods below [25].
2. Viability Staining and Flow Cytometry:
- Procedure: Stain the bacterial suspension with fluorescent dyes. A common combination is SYTO 9 (green, stains all cells) and propidium iodide (PI) (red, penetrates only cells with damaged membranes).
- Analysis: Analyze using flow cytometry. VBNC cells are characterized as SYTO 9 positive / PI negative, indicating an intact membrane and viability despite non-culturability [4] [13]. This method can be hampered by complex matrices like process wash water, which may cause overestimation of dead cells [13].
3. Viability Quantitative PCR (v-qPCR):
- Principle: This method uses photoreactive dyes like propidium monoazide (PMAxx) or ethidium monoazide (EMA) that penetrate membrane-compromised (dead) cells and bind covalently to DNA, inhibiting its amplification in PCR.
- Protocol:
- Treat the sample with a optimized combination of dyes (e.g., 10 µM EMA and 75 µM PMAxx).
- Incubate in the dark (e.g., 40°C for 40 min).
- Expose to a high-intensity light source for 15 minutes to photo-activate the dyes.
- Extract DNA and perform qPCR.
- Output: The quantified DNA originates only from cells with intact membranes (viable and VBNC cells), allowing their distinction from free DNA and dead cells [13]. This method has been successfully validated in industrial settings.
4. Time-Kill Assay for VBNC Cells:
- Procedure: This is a key method for evaluating the activity of antimicrobials against non-growing VBNC cells [29].
- Expose a confirmed VBNC population to the antimicrobial agent over a set time.
- At intervals, sample and neutralize the antimicrobial.
- Use v-qPCR or flow cytometry (not plate counts) to quantify the remaining viable cell count.
- Analysis: Plot the log reduction of viable cells over time to determine the bactericidal activity of the antimicrobial against the VBNC population [29].
Visualizing the VBNC Investigation Workflow
The following diagram illustrates the core experimental workflow for inducing, confirming, and challenging the VBNC state, highlighting the parallel tracks of conventional and VBNC-aware methodologies.
Diagram 1: Workflow for VBNC State Investigation and Antimicrobial Challenge.
Molecular Mechanisms of VBNC Tolerance
The elevated antimicrobial tolerance of VBNC cells is not primarily due to acquired genetic resistance mutations. Instead, it is a consequence of their dormant physiology and specific molecular adaptations.
- Reduced Metabolic Activity: The dramatic downshift in metabolic processes and cell division means that VBNC cells are not actively engaging with many cellular targets of antibiotics (e.g., cell wall synthesis, protein synthesis) [3] [12].
- Cellular Damage Repair: Resuscitation from the VBNC state is driven by the repair of stress-induced damage, such as oxidative lesions. Intracellular ATP levels and metabolic activity are critical forces powering this resuscitation, highlighting a key survival mechanism [28].
- Transcriptional Reprogramming: Transcriptomic analyses reveal that VBNC cells undergo significant gene expression changes. This includes upregulation of genes related to stress responses, transcriptional regulation, and antibiotic resistance, which collectively render the cells more tolerant to adverse conditions [4].
- Toxin-Antitoxin Systems: Type II toxin-antitoxin (TAS) systems are genetic modules that contribute to dormancy. Under stress, unstable antitoxins are degraded, allowing stable toxins to inhibit essential cellular processes like translation and replication, thereby inducing a dormant, highly tolerant state [3].
The Scientist's Toolkit: Essential Research Reagents and Materials
Table 3: Key Reagents and Equipment for VBNC and Antimicrobial Susceptibility Research
| Tool / Reagent | Function in VBNC Research | Example Application |
|---|---|---|
| PMAxx / EMA Dyes | Viability dyes for v-qPCR; selectively inhibit DNA amplification from dead cells. | Differentiation between viable (VBNC) and dead cells in a sample [13]. |
| SYTO 9 / Propidium Iodide (PI) | Fluorescent nucleic acid stains for cell viability analysis via microscopy/flow cytometry. | Determining membrane integrity; VBNC cells are SYTO 9+/PI- [4]. |
| Chlorine (Sodium Hypochlorite) | Chemical stressor for inducing the VBNC state at low concentrations (e.g., 0.5 mg/L). | Mimicking disinfection conditions in water distribution systems [4]. |
| Quantitative PCR (qPCR) System | For quantifying gene expression and viable cell load via v-qPCR. | Quantifying total and viable bacterial populations and expressing virulence/antibiotic resistance genes [28] [4]. |
| Flow Cytometer | Multiparameter analysis of cell physiology and viability at the single-cell level. | Rapid quantification of subpopulations (culturable, VBNC, dead) based on staining [13]. |
| TiO2 Nanotubes & LED Lamp | System for applying sub-lethal photocatalytic stress. | Inducing VBNC state via oxidative stress in a controlled manner [28]. |
| Scanning Electron Microscope (SEM) | High-resolution imaging of cell morphology and surface damage. | Observing physical changes and membrane damage in VBNC cells [28] [4]. |
The evidence is clear: standard, culture-based antimicrobial efficacy testing provides an incomplete and often misleading picture by failing to account for the VBNC state. This blind spot has profound implications, from the overestimation of disinfection efficacy in water and food processing to the misunderstanding of chronic and recurrent infections in clinical settings. The elevated and multi-faceted tolerance of VBNC cells to antimicrobials underscores the necessity for the scientific community to adopt more sophisticated, culture-independent tools. Integrating viability-PCR, flow cytometry, and transcriptomic analyses into routine assessment protocols is no longer a niche pursuit but a critical step towards accurately evaluating antimicrobial interventions and developing strategies to counter this resilient survival mechanism.
The viable but non-culturable (VBNC) state represents a dormant, low-metabolic condition that numerous bacterial pathogens adopt to survive environmental stresses, including sublethal antibiotic exposure. Cells in the VBNC state maintain membrane integrity and metabolic activity but fail to grow on conventional culture media, the gold standard for viability assessment in clinical microbiology [30] [31]. This creates a critical blind spot in therapeutic development, as standard antibiotic susceptibility tests that rely on culturability may falsely classify dormant VBNC populations as susceptible, overlooking a significant reservoir of persistent bacteria with potential resuscitation capacity. Research indicates that VBNC cells can retain virulence and resuscitate under favorable conditions, posing a substantial risk for recurrent infections and treatment failure [32] [31]. Consequently, methodologies capable of detecting and quantifying these elusive populations are essential for advancing our understanding of true antibiotic efficacy and developing strategies to eradicate persistent bacterial reservoirs.
Flow cytometry combined with viability staining has emerged as a powerful tool to dissect bacterial heterogeneity at the single-cell level, simultaneously discriminating live, dead, and VBNC populations within a sample. This guide compares the performance of key staining approaches and flow cytometric methods against traditional techniques, providing researchers with the experimental data and protocols needed to integrate these powerful tools into antimicrobial susceptibility research.
Comparative Analysis of Viability Assessment Methods
Performance Metrics of Key Technologies
The following table summarizes the core principles, advantages, and limitations of the primary methods used for bacterial viability assessment, highlighting their distinct capabilities regarding VBNC detection.
Table 1: Comparison of Methods for Differentiating Live, Dead, and VBNC Bacterial Cells
| Method | Principle | Detects VBNC? | Key Advantages | Major Limitations |
|---|---|---|---|---|
| Plate Culture (CFU) [30] | Bacterial proliferation on solid media | No | Regulatory gold standard; simple; provides isolates for further study | Time-consuming (1-7 days); misses VBNC cells |
| Live/Dead Staining + Flow Cytometry [33] [31] | Membrane integrity using nucleic acid dyes (e.g., SYTO9/PI) | Yes | Rapid (<1 hour); high-throughput; single-cell data; distinguishes viable (including VBNC) from dead | Cannot assess culturability directly; requires specialized instrument |
| Viability PCR (v-PCR) [34] [32] | Dyes (PMA/EMA) penetrate compromised membranes and inhibit DNA amplification | Yes | Specific detection of viable cells (with intact membranes); fast; sensitive | Complex sample matrix can interfere; may not detect all VBNC cells |
| Metabolic Activity Assays [30] | Uptake and enzymatic conversion of fluorogenic substrates (e.g., FDA, CFDA) | Yes | Measures metabolic activity, a key viability marker | Signal can be low in dormant VBNC cells; sensitive to pH |
| Flow Cytometry-Cell Sorting + qPCR [32] | Cell sorting based on viability staining followed by species-specific qPCR | Yes | Quantifies specific VBNC pathogens in complex samples | Technically complex and expensive; multi-step protocol |
Quantitative Data: Flow Cytometry vs. Culture-Based Enumeration
Discrepancies between flow cytometry and plate counts provide direct evidence of the VBNC population. The following table compiles experimental data from recent studies highlighting the superior detection capability of flow cytometry.
Table 2: Experimental Recovery of Viable Bacteria: Flow Cytometry (FC) vs. Plate Count (PC)
| Bacterial Species / Sample Type | Treatment / Condition | Viable Count (FC) | Culturable Count (PC) | Inferred VBNC Population | Citation |
|---|---|---|---|---|---|
| Listeria monocytogenes (Process Wash Water) | Chlorine (10 mg/L) | Maintained at ~105 AFU/ml* | Reduced to 0 CFU/ml | ~105 cells/ml | [34] |
| Multi-species Probiotic Blends | Various storage stresses | 101.8% of input viable cells recovered | 81.4% of input viable cells recovered | 20.4% of total population | [33] |
| Escherichia coli (Plasma-Activated Water) | Plasma exposure | <1 log reduction | ~7 log reduction | Significant proportion entered VBNC | [35] |
| Legionella pneumophila (Water Systems) | Environmental stress & disinfection | Detectable via FCM-qPCR | Not detectable by culture | Present and potentially infectious | [32] |
*AFU: Active Fluorescent Units, a viability metric from flow cytometry.
Core Staining Mechanisms and Experimental Protocols
Mechanism of Dual Staining for Flow Cytometry
The most common approach for viability assessment uses a combination of membrane-permeant and membrane-impermeant fluorescent nucleic acid stains. The workflow and decision process for this method is outlined below.
Key Research Reagent Solutions
The following table details essential reagents and their functions for performing viability staining and flow cytometry.
Table 3: Essential Reagents for Viability Staining and Flow Cytometry
| Reagent / Kit | Primary Function | Key Features | Example Application |
|---|---|---|---|
| Live/Dead BacLight Kit [35] [31] | Differential staining based on membrane integrity | Contains SYTO9 and PI; works for a broad spectrum of bacteria | Enumeration of VBNC Listeria monocytogenes after chlorine treatment [31] |
| Fixable Viability Dyes (FVD) [36] | Covalently labels dead cells with compromised membranes | Dyes are cross-linked to proteins; compatible with fixation/permeabilization | Complex protocols involving intracellular staining or sample archiving |
| Propidium Iodide (PI) [36] [33] | Impermeant stain to identify dead cells | Red fluorescence; must be present in buffer during acquisition | Standard live/dead staining in combination with a green permeant dye like SYTO24 [33] |
| PMA/EMA Dyes [34] [32] | Selective DNA labeling for viability PCR (v-PCR) | Penetrate dead cells; bind DNA upon photoactivation to inhibit PCR | Detecting VBNC Legionella in complex water samples when combined with qPCR [32] |
| SYTO 9 / SYTO 24 Dyes [33] [31] | Permeant stain to label all cells | Green fluorescence; can be displaced by PI in dead cells | Standard live/dead staining in combination with PI [33] [31] |
Standard Protocol: Viability Staining for Flow Cytometry
This protocol is adapted from the ISO 19344|IDF 232 standard for microbial enumeration and is suitable for most bacteria [33].
Materials:
- Phosphate-buffered saline (PBS), azide- and protein-free
- Flow cytometry staining buffer
- Fluorescent dyes: SYTO 24 (or SYTO 9) and Propidium Iodide (PI)
- Flow cytometer with a 488 nm blue laser
Experimental Procedure:
- Sample Preparation: Prepare a single-cell suspension and wash cells twice in azide-free PBS.
- Cell Concentration: Resuspend the cell pellet at a concentration of 1–5 × 10^7 cells/mL in PBS or maximum recovery diluent.
- Staining: Add 100 μL of cell suspension to a mixture of 880 μL diluent and 10 μL of each fluorescent dye (e.g., 0.1 mM SYTO 24 and 0.2 mM PI).
- Incubation: Incubate the mixture for 15 minutes at 37°C in the dark.
- Flow Cytometry Analysis: Vortex the sample and analyze immediately on the flow cytometer. Use the following settings as a starting point:
- Fluidics: Medium flow rate (∼35 μL/min)
- Threshold: Set on Forward Scatter (FSC-H > 2500) and Green Fluorescence (SYTO24-H > 1000) to exclude background noise.
- Detection: Collect green fluorescence (FL-1 detector, ~530 nm) for SYTO 24 and red fluorescence (FL-3 detector, >670 nm) for PI.
Data Interpretation:
- Viable cells (AFUs): Green fluorescence only (SYTO 24 positive).
- Non-viable cells (n-AFUs): Red fluorescence (PI positive). Note that cells stained with both dyes are also considered non-viable.
- VBNC Population Calculation: The VBNC population is inferred by subtracting the culturable count (CFU/mL) from the viable count obtained by flow cytometry (AFU/mL) [33].
Advanced Applications and Integrated Workflows
Flow Cytometry-Cell Sorting and qPCR for Specific VBNC Pathogen Detection
For complex samples like water or sputum, a combination of flow cytometry and molecular methods is required to quantify specific VBNC pathogens. The "Viability-based Flow Cytometry-Cell Sorting and qPCR" (VFC+qPCR) assay is a powerful solution [32].
Workflow:
- Viability Staining & Sorting: Environmental samples are stained with a viability dye (e.g., SYTO9). The flow cytometer is then used to sort the viable (green fluorescent) cell population.
- DNA Extraction and qPCR: DNA is extracted from the sorted viable cells and subjected to a species-specific qPCR assay (e.g., targeting Legionella pneumophila).
- Quantification: The genomic load of the viable, non-culturable pathogen is quantified from the standard qPCR curve.
Significance: This method confirmed that standard culture pre-treatment procedures (acid/heat shock) can themselves induce a VBNC state in a portion of the population, leading to significant underestimation of the risk posed by pathogens like Legionella [32].
Investigating Antibiotic Susceptibility in VBNC Cells
Integrating viability staining with antibiotic exposure studies allows researchers to track the population dynamics of live, dead, and VBNC cells in response to therapeutic agents.
Experimental Framework:
- Expose bacterial cultures to a range of antibiotic concentrations and contact times.
- At various time points, aliquot samples for parallel analysis:
- Flow Cytometry: Analyze with viability stains to determine the proportion of live, VBNC, and dead cells.
- Plate Counting: Determine the culturable fraction.
- Correlate the data to identify antibiotic concentrations that eliminate culturability but leave a persistent VBNC population.
- Further investigate the VBNC population sorted by flow cytometry for their potential to resuscitate and for transcriptomic or proteomic profiles that underpin their tolerance.
This integrated approach moves beyond the simple "susceptible" or "resistant" dichotomy and is crucial for understanding the role of VBNC cells in chronic and recurrent infections, ultimately guiding the development of more effective anti-persister therapies.
The accurate profiling of gene expression and metabolic activity is a cornerstone of modern molecular biology, particularly in complex fields such as the study of antibiotic-resistant bacteria. A prominent challenge in environmental and clinical microbiology is the phenomenon of the viable but nonculturable (VBNC) state, a dormant survival strategy adopted by bacteria, including antibiotic-resistant strains (ARB), under stress. VBNC cells evade traditional culture-based detection yet retain pathogenicity and the capacity to resuscitate, posing a significant public health risk [16]. Discerning the metabolic differences between VBNC and normal cells is crucial for understanding the mechanisms of antibiotic susceptibility and developing effective countermeasures. This guide objectively compares the performance of RNA sequencing (RNA-seq) and PCR-based methodologies in probing these subtle physiological states, providing researchers with a framework for selecting appropriate tools for investigating bacterial dormancy and resuscitation.
Technical Comparison of Detection Methodologies
The selection of a molecular detection strategy involves careful consideration of experimental goals, with a fundamental trade-off between the targeted, quantitative capabilities of PCR and the comprehensive, discovery-oriented nature of RNA-seq.
Table 1: Comparison of PCR and RNA-Seq for Gene Expression and Metabolic Profiling
| Feature | Quantitative PCR (qPCR) | RNA Sequencing (RNA-Seq) |
|---|---|---|
| Primary Application | Targeted quantification of known genes [16] | Untargeted, genome-wide discovery of transcript abundance and novel RNAs [37] [38] |
| Throughput | Low to medium (tens to hundreds of targets) | High (entire transcriptome) |
| Quantitative Nature | Relative or absolute quantification of specific transcripts | Relative expression within a sample (e.g., RPKM) [38] |
| Sensitivity | High, suitable for low-abundance targets | Can detect low-abundance and non-coding RNAs, enhanced by nuclear RNA sequencing [37] |
| Key Technical Consideration | PCR duplication rates can be high for low-input samples, requiring Unique Molecular Identifiers (UMIs) for accurate quantification [39] | Library preparation (stranded vs. unstranded, ribosomal depletion) significantly impacts data interpretation and cost [38] |
| Suitability for VBNC Research | Ideal for validating specific metabolic or stress response genes during induction and resuscitation [16] | Optimal for uncovering global transcriptional shifts and unknown metabolic pathways during VBNC state entry and exit |
RNA-seq does not measure absolute RNA counts but rather relative expression within a sample, and its ability to detect different RNA biotypes—such as messenger RNA (mRNA), long non-coding RNA (lncRNA), and micro RNA (miRNA)—is entirely dependent on the library preparation method used [38]. For instance, standard poly(A) enrichment methods will miss non-polyadenylated RNAs, necessitating ribosomal depletion protocols for a more complete transcriptomic picture.
Experimental Data: Platform Performance and PCR Artifacts
The reliability of RNA-seq data is contingent on the specifics of the experimental workflow, including the sequencing platform and library preparation parameters. A recent 2025 study systematically evaluated these factors, providing critical performance data.
Table 2: Experimental Performance Data of Sequencing Platforms with Converted Illumina Libraries [39]
| Sequencing Platform | Average Phred Quality Score | Mismatch Rate (vs. GRCh38.p13) | Primer Dimer Content (Low Input <15 ng) | Effect of Library Conversion on PCR Duplicates |
|---|---|---|---|---|
| Illumina NovaSeq 6000 | 36-43 | 0.0003 - 0.001 | 5.6% to 70.1% | Baseline (Native library) |
| Illumina NovaSeq X | 36-43 | 0.0003 - 0.001 | 10-25% higher than NovaSeq 6000 | Baseline (Native library) |
| Element Biosciences AVITI | 36-43 (Highest) | 0.0003 - 0.001 | 0.009% to 3.3% | Increased rate for very low input (<15 ng) |
| Singular Genomics G4 | 36-43 | ~50% higher than others | 0.009% to 3.3% | Increased rate for very low input (<15 ng) |
The study demonstrated that the rate of PCR duplicates is a combined effect of RNA input and PCR cycle number. For inputs below 125 ng, 34–96% of reads were discarded as duplicates, with the percentage increasing at lower input amounts [39]. This is critical for VBNC studies, where sample input is often limited. The use of Unique Molecular Identifiers (UMIs) is therefore highly recommended for such scenarios to distinguish technical duplicates from biologically identical reads [39].
Detailed Protocol: Impact of PCR Cycles on RNA-Seq Libraries
Objective: To assess the impact of RNA input amount and PCR cycle number on PCR duplication rate and gene detection sensitivity in RNA-seq libraries [39].
Methodology:
- Library Preparation: Generate libraries from human liver RNA (1 ng to 1000 ng) using the NEBNext Ultra II Directional RNA Library Prep Kit.
- PCR Amplification: Amplify samples using low, mid, and high cycle numbers, adjusted according to the input amount.
- Library Conversion: For sequencing on AVITI and G4 platforms, convert a subset of Illumina-prepared libraries, a process that introduces additional PCR cycles.
- Sequencing & Analysis: Sequence samples across NovaSeq 6000, NovaSeq X, AVITI, and G4 platforms. Subsample to 2 million reads per sample. Perform deduplication analysis and quantify detected genes.
Key Outcome: For input amounts above 10 ng but below 125 ng, a strong negative correlation exists between input amount and PCR duplicate rate, and a positive correlation exists between PCR cycle number and duplicate rate. The highest data quality is achieved using the lowest recommended number of PCR cycles [39].
Application in VBNC Antibiotic Susceptibility Research
The induction and resuscitation of VBNC bacteria present a unique application for these molecular tools. A 2025 study on E. coli illustrates a targeted experimental approach.
Objective: To elucidate the regulatory formation of the VBNC state in antibiotic-resistant E. coli induced by sub-lethal photocatalysis and its resuscitation mechanism [16] [18].
Methodology:
- VBNC Induction: Subject ARB E. coli (e.g., DH5α (MCR)) and antibiotic-susceptible bacteria (ASB) to sub-lethal photocatalysis using a TiO2 nanotube system illuminated with a 365 nm LED lamp (100 mW/cm²).
- Viability Monitoring: Track culturability via plate counts and total cell counts via viability assays. A strain is considered VBNC when culturable cells are undetectable but viable cells remain.
- Resuscitation: Remove the environmental stress (photocatalysis) and monitor cultures over 20 days for recovery of culturability.
- Molecular Analysis:
- qPCR: Quantify expression of genes related to oxidative stress repair and energy metabolism during resuscitation [16].
- Morphological Analysis: Use Scanning Electron Microscopy (SEM) to measure changes in cell length (VBNC cells are shorter, resuscitated cells recover length) [16].
- Metabolic Activity: Assess using Laser Confocal Raman Microspectroscopy.
- Phenotypic Confirmation: Compare the antibiotic resistance of resuscitated cells to wild-type cells.
Key Findings: Sub-lethal photocatalysis induced >10⁸ CFU/mL of E. coli into the VBNC state within 1 hour. These cells resuscitated after 5-10 days, with a peak around 20 days. The resuscitated cells exhibited recovered culturability, growth, and cell length, but showed higher antibiotic resistance than wild-type cells. The resuscitation was driven by repaired oxidative damage and changes in intracellular ATP and metabolic activity [16].
Advanced Profiling: Direct Interrogation of Metabolic Activity
While standard RNA-seq reflects steady-state transcript levels, techniques focusing on newly synthesized RNA provide a more direct window into transcriptional and metabolic activity, which is particularly valuable for studying dynamic processes like VBNC resuscitation.
Detailed Protocol: Metabolic Labeling of Newly Synthesized Nuclear RNA
Objective: To profile newly synthesized nuclear RNA as a direct measure of transcriptional activity, enabling the detection of unstable and low-abundance nuclear RNAs [37].
Methodology:
- In Vivo Labeling: Pulse-label maize root tips (or other tissues) with the cell-permeable uracil analog 5-ethynyl uridine (EU) for 1 hour.
- Nuclei Isolation: Fix the tissue and isolate nuclei via mechanical chopping to minimize cytoplasmic RNA contamination.
- RNA Extraction & Affinity Purification: Extract total nuclear RNA. Use click chemistry to biotinylate EU-labeled RNA and isolate it using streptavidin beads.
- Library Construction & Sequencing: Prepare stranded RNA-seq libraries from the EU-labeled nuclear RNA (EU-nuclear RNA) and, for comparison, from the total nuclear RNA and total cellular RNA populations.
Key Outcome: The transcript abundance profiles of protein-coding genes in nuclear RNA and EU-nuclear RNA were tightly correlated (R² = 0.767) but distinct from cellular RNA (R² = 0.170-0.293). Nuclear RNA fractions are enriched for pre-mRNA and intronic sequences, providing a superior resource for detecting transcriptional activity and non-coding RNAs compared to standard cellular RNA-seq [37].
The Scientist's Toolkit: Essential Research Reagents
The following reagents and kits are fundamental for implementing the protocols discussed in this guide.
Table 3: Key Research Reagent Solutions for Transcriptomics and VBNC Studies
| Reagent / Kit | Function / Application |
|---|---|
| NEBNext Ultra II Directional RNA Library Prep Kit | A widely used kit for preparing strand-specific RNA-seq libraries from a range of input amounts [39]. |
| 5-Ethynyl Uridine (EU) | A uracil analog for metabolic labeling of newly synthesized RNA, enabling the isolation of nascent transcripts via click chemistry [37]. |
| TiO2 Nanotubes | A photocatalyst used in experimental systems to induce oxidative stress and drive bacteria into the VBNC state [16]. |
| Ribosomal RNA Depletion Kits | Probes (e.g., magnetic bead-based or RNAseH-mediated) to remove abundant rRNA, increasing sequencing depth for non-ribosomal transcripts [38]. |
| Unique Molecular Identifiers (UMIs) | Short random nucleotide sequences added to each RNA molecule during library prep to accurately identify and count PCR duplicates [39]. |
The viable but non-culturable (VBNC) state is a dormant survival strategy employed by many bacterial pathogens when faced with environmental stress. Cells in this state are characterized by a complete loss of culturability on routine media that would normally support their growth, while maintaining viability and metabolic activity [25]. This phenomenon presents a critical diagnostic challenge, as standard antimicrobial efficacy testing relies heavily on culture-based methods like colony forming unit (CFU) counts [3]. Consequently, bacteria in the VBNC state escape detection by conventional clinical microbiology techniques, leading to an underestimation of microbial risk and the potential for treatment failure.
The public health significance of this problem is substantial. VBNC cells exhibit drastically increased tolerance to a wide range of antimicrobials, including antibiotics, disinfectants, and sanitizers [3] [40]. When favorable conditions return, these cells can resuscitate, potentially causing recurrent infections and contributing to the spread of antibiotic resistance [16] [18]. Understanding and accurately quantifying the antibiotic tolerance of VBNC cells is therefore essential for developing more effective treatment strategies and interventions against persistent bacterial infections.
Detection and Viability Assessment of VBNC Cells
Before any assessment of antibiotic efficacy can begin, researchers must first reliably induce, detect, and quantify VBNC cells using culture-independent methods. The confirmation of VBNC state involves two key criteria: demonstrating non-culturability (CFU = 0) and confirming cellular viability through measures of metabolic activity and membrane integrity [25].
Table 1: Core Methods for Detecting and Confirming the VBNC State
| Method Category | Specific Technique | Measurement Principle | Key Application in VBNC Research |
|---|---|---|---|
| Membrane Integrity | Flow Cytometry with Live/Dead Stains (e.g., SYTO 9/PI) | Distinguishes cells with intact vs. damaged membranes | Quantifying the proportion of viable cells within a population [4] [41] |
| Molecular Viability | PMA-ddPCR or PMA-qPCR | Selective amplification of DNA from cells with intact membranes | Absolute quantification of viable cell numbers without culture [41] |
| Metabolic Activity | ATP Assays, Laser Confocal Raman Microspectroscopy | Measures cellular energy levels and metabolic fingerprints | Confirming ongoing metabolic activity in non-culturable cells [16] [25] |
| Morphological Analysis | Scanning Electron Microscopy (SEM), Transmission Electron Microscopy (TEM) | Visualizes cell size, shape, and membrane integrity | Observing physical changes and damage in VBNC cells [16] [4] |
A standardized experimental workflow is crucial for credible research in this field. The process begins with the induction of the VBNC state using a specific stressor, followed by confirmation of non-culturability and viability, after which antibiotic tolerance assays can be performed.
Figure 1: Standardized experimental workflow for inducing the VBNC state and assessing antibiotic tolerance, incorporating critical viability confirmation steps.
Established Frameworks for Quantifying Antibiotic Tolerance
The MDK99 Framework for Tolerance Quantification
For growing cells, the Minimum Inhibitory Concentration (MIC) is the gold standard for assessing antibiotic efficacy. However, for non-growing, dormant cells like those in the VBNC state, this metric is insufficient. A complementary framework proposes the Minimum Duration for Killing 99% of the population (MDK99) as a key metric for quantifying antibiotic tolerance [42]. This metric is evaluated by monitoring the reduction of viable cells over time during antibiotic exposure, allowing researchers to determine the time required to achieve a 99% reduction in viability, typically using culture-independent detection methods for VBNC cells.
Experimental Data on VBNC Antibiotic Tolerance
Application of these quantification principles has revealed the profound tolerance of VBNC cells. Studies using various induction methods and bacterial species have consistently demonstrated this phenomenon.
Table 2: Documented Antibiotic Tolerance of VBNC Cells from Experimental Studies
| Bacterial Species | VBNC Induction Method | Antibiotic Challenge | Tolerance Observed | Detection Method | Source |
|---|---|---|---|---|---|
| Escherichia coli | Low-Level Chlorination (0.5 mg/L) | Ampicillin (200 μg/mL), Ofloxacin (5 μg/mL) | Persistence at 128x and 64x MIC, respectively | Flow Cytometry, PCR [4] | |
| E. coli (ARB & ASB) | Sub-Lethal Photocatalysis | Not Specified | Higher antibiotic resistance in resuscitated cells | Plate Count, qPCR [16] | |
| Klebsiella pneumoniae | Low Temperature (4°C), Ciprofloxacin | Ciprofloxacin | Inhibited resuscitation but maintained viability | PMA-ddPCR [41] | |
| General Pathogens | Various (Starvation, Temperature, Biocides) | Multiple classes of antibiotics | "Drastically increased tolerance" | Reviewed Methods [3] |
The data show that VBNC E. coli induced by low-level chlorination, a condition relevant to drinking water distribution systems, can survive concentrations of ampicillin and ofloxacin that are 128 and 64 times their MIC, respectively [4]. Furthermore, research on antibiotic-resistant bacteria (ARB) has demonstrated that sub-lethal photocatalysis, a promising water disinfection strategy, can inadvertently induce the VBNC state, and the resuscitated cells can exhibit even higher antibiotic resistance than their wild-type counterparts [16] [18].
The extreme antibiotic tolerance of VBNC cells is not due to acquired genetic resistance but is a consequence of their dormant, metabolically downregulated state. The primary mechanism involves a massive reduction in metabolic activity, which negates the efficacy of most conventional antibiotics that target active cellular processes like cell wall synthesis, protein production, and DNA replication [3] [40].
At the molecular level, entry into the VBNC state is often regulated by complex genetic networks. Type II Toxin-Antitoxin (TA) systems are well-described mediators of this process. Under stress, unstable antitoxins are degraded, allowing stable toxins to induce a state of persistence and dormancy, dramatically increasing antimicrobial tolerance [3]. Additionally, global stress regulators like rpoS and oxyR play crucial roles in the response [3]. The process of resuscitation is driven by the repair of oxidative damage and a reallocation of energy, with intracellular ATP levels and metabolic activity being the major forces that power the return to a culturable state [16] [18].
Figure 2: Molecular mechanisms governing the induction of the VBNC state and subsequent resuscitation, highlighting the role of toxin-antitoxin systems and metabolic downregulation in conferring tolerance.
The Scientist's Toolkit: Essential Reagents and Methods
Successfully researching the antibiotic tolerance of VBNC cells requires a specific set of reagents and methodologies that move beyond traditional microbiology.
Table 3: Key Research Reagent Solutions for VBNC Tolerance Studies
| Reagent / Tool | Core Function | Application Example in VBNC Research |
|---|---|---|
| PMA (Propidium Monoazide) | DNA-binding dye that penetrates only membrane-compromised cells; inhibits PCR amplification. | Used in PMA-qPCR and PMA-ddPCR to selectively quantify intact, viable VBNC cells without culture [41]. |
| Live/Dead Staining Kits (e.g., SYTO 9/PI) | Fluorescent stains differentiating cells based on membrane integrity. | Visualizing and quantifying the proportion of viable VBNC cells via fluorescence microscopy or flow cytometry [4] [41]. |
| ATP Assay Kits | Measures intracellular adenosine triphosphate (ATP) levels as an indicator of metabolic activity. | Confirming the viability and metabolic state of non-culturable cells [16] [25]. |
| Specific Antibiotic Formulations | Pharmaceutical-grade antibiotics for in vitro challenge experiments. | Used at high, clinically relevant concentrations to challenge VBNC cells and quantify their survival over time (MDK99) [42] [4]. |
| VBNC Induction Stressors | Chemicals or equipment to apply sub-lethal stress (e.g., chlorine, H2O2, cold shock). | Inducing the VBNC state in model organisms to create experimental populations for tolerance testing [16] [4]. |
| ddPCR or qPCR Systems | Digital PCR or quantitative PCR platforms for absolute nucleic acid quantification. | Absolute quantification of viable cell numbers using viability dyes (PMA) and specific genetic targets [41]. |
The study of antibiotic efficacy against VBNC cells remains a significant challenge at the forefront of clinical microbiology. The experimental frameworks outlined here, centered on culture-independent viability assessment and metrics like MDK99, provide a path forward. A clear understanding of the molecular mechanisms, particularly the role of toxin-antitoxin systems and metabolic dormancy, is crucial for developing strategies to overcome this tolerance.
Future research must focus on standardizing these detection and quantification methods across laboratories. Furthermore, there is a pressing need to discover and develop novel anti-infective agents or combination therapies that can effectively target and eradicate the dormant VBNC subpopulation, thereby preventing disease recurrence and mitigating the long-term health risks these cells pose.
Decoding the Shield: Molecular Mechanisms of Enhanced Antibiotic Tolerance in VBNC Bacteria
The persistent challenge of bacterial infections often lies not in antibiotic resistance, but in antibiotic tolerance—a transient, non-heritable ability to survive treatment without genetic mutation. Within this context, the viable but non-culturable (VBNC) state represents a profound survival strategy adopted by numerous bacterial pathogens when confronted with adverse environmental conditions. VBNC cells are defined as bacteria that have lost the ability to grow on routine laboratory media on which they would normally proliferate, yet maintain viability, metabolic activity, and the capacity to resuscitate when conditions improve [12] [20]. This state stands in contrast to normal, culturable cells that are readily detectable and susceptible to conventional antibiotic treatments.
The study of VBNC states has gained critical importance in clinical microbiology and pharmaceutical development due to its direct implications for persistent and recurrent infections. Research indicates that VBNC cells exhibit significantly enhanced tolerance to multiple stressors, including antibiotics, compared to their culturable counterparts [20] [43]. The thesis driving current research proposes that metabolic drastic downregulation serves as the core mechanism enabling this exceptional insensitivity. Understanding the physiological and molecular basis of this phenomenon is essential for developing novel therapeutic strategies that can effectively target these dormant, recalcitrant cells and potentially overcome a significant barrier in infectious disease treatment.
Comparative Analysis: VBNC vs. Normal Cells in Antibiotic Challenge
Quantitative Evidence of Enhanced Antibiotic Tolerance
The extraordinary antibiotic tolerance of VBNC cells is quantitatively demonstrated through direct experimental challenges. The data reveal survival rates that are orders of magnitude higher than those observed in normal, culturable cells under identical antibiotic pressure.
Table 1: Comparative Antibiotic Tolerance of VBNC vs. Normal Escherichia coli Cells
| Bacterial State | Antibiotic Challenge | Concentration (vs. MIC) | Survival Outcome | Reference |
|---|---|---|---|---|
| VBNC E. coli | Ampicillin | 128× MIC | Maintained viability | [43] |
| VBNC E. coli | Ofloxacin | 64× MIC | Maintained viability | [43] |
| Normal E. coli | Ampicillin | 1× MIC | >99% killing | [43] |
| Normal E. coli | Ofloxacin | 1× MIC | >99% killing | [43] |
| VBNC Vibrio vulnificus | Multiple antibiotics | Various | Higher resistance | [20] |
| Normal V. vulnificus | Multiple antibiotics | Various | Susceptible | [20] |
Beyond specific antibiotic challenges, VBNC cells display broad-spectrum tolerance to physical and chemical stressors. Studies document that VBNC cells of pathogens like Vibrio vulnificus exhibit significantly higher resistance to heat, low pH, ethanol, heavy metals, and oxidative stress compared to their exponentially growing counterparts [20]. This generalized tolerance profile supports the hypothesis of a fundamental physiological reprogramming rather than specific resistance mechanisms.
Metabolic Characteristics Underlying Tolerance
The exceptional survival capabilities of VBNC cells are underpinned by profound metabolic alterations that distinguish them from normal cells. While VBNC cells exhibit significantly reduced metabolic rates overall, research reveals they maintain specific energy-producing pathways that are critical for survival.
Table 2: Metabolic Profile Comparison Between VBNC and Normal Bacterial Cells
| Metabolic Parameter | VBNC Cells | Normal Cells | Functional Significance |
|---|---|---|---|
| Overall metabolic rate | Drastically reduced | High | Reduces antibiotic target activity |
| Energy metabolism | Active but rewired | Fully active | Maintains essential cellular functions |
| ATP levels | Lower than normal cells but maintained | High | Sustains basal homeostasis |
| Membrane potential | Maintained | High | Preserves viability |
| Protein synthesis | Significantly reduced | Active | Limits drug targets |
| Oxidative phosphorylation | Critical for survival | Primary energy pathway | Essential for VBNC maintenance |
| TCA cycle activity | Active in some VBNC types | Highly active | Supports energy and precursor production |
Research on Escherichia coli persisters (conceptually related to VBNC cells) indicates that the global metabolic regulator Crp/cAMP redirects metabolism from anabolism to oxidative phosphorylation, with the tricarboxylic acid (TCA) cycle, electron transport chain, and ATP synthase remaining critical for survival [44]. This metabolic rewiring, rather than complete metabolic shutdown, appears crucial for maintaining the VBNC state and associated antibiotic tolerance.
Experimental Protocols for Investigating VBNC Antibiotic Tolerance
VBNC Induction and Verification Methods
Establishing reliable VBNC models is fundamental to studying their antibiotic insensitivity. Multiple induction methods have been standardized across laboratories:
Low-Level Chlorination Induction (for E. coli):
- Expose mid-logarithmic phase cells (approximately 10⁸ CFU/mL) to 0.5 mg/L chlorine in buffer
- Incubate at room temperature for 6 hours with gentle agitation
- Monitor culturability by plating on non-selective media daily
- Confirm VBNC state when no colonies form on plates after 48 hours incubation, while viability is maintained as determined by PMA-qPCR or fluorescence microscopy [43]
Antibiotic-Mediated Induction (for C. sakazakii):
- Harvest logarithmic-phase cells by centrifugation (4,000 × g, 15 min, 4°C)
- Resuspend in ampicillin solution (400 µg/mL in 0.9% saline) at approximately 10⁸ CFU/mL
- Incubate at 25°C for 10 days
- Verify VBNC state by absence of growth on LB agar plates combined with positive viability staining [45]
Nutrient Starvation at Low Temperature:
- Wash logarithmic-phase cells and resuspend in minimal media or saline
- Incubate at 4°C for extended periods (days to weeks)
- Regularly monitor culturability and viability [20]
VBNC verification requires both culturability assessment (through plate counts) and viability determination using methods such as:
- PMA-qPCR (detecting DNA from membrane-intact cells)
- Fluorescence microscopy using live/dead staining kits
- Flow cytometry with metabolic probes
- ATP quantification [6] [3]
Antibiotic Tolerance Assessment Protocols
Standardized protocols for evaluating antibiotic tolerance in VBNC states include:
High-Concentration Antibicide Exposure:
- Expose VBNC and control culturable cells to antibiotics at concentrations significantly above MIC (e.g., 200 µg/mL ampicillin, 5 µg/mL ofloxacin for E. coli)
- Incubate for predetermined periods (typically 24 hours)
- Neutralize antibiotics using appropriate methods (dilution, enzymatic inactivation)
- Assess viability using both culturability (plating) and viability stains (PMA-qPCR) [43]
Time-Kill Kinetics Assay:
- Monitor viability at multiple time points during antibiotic exposure
- Establish biphasic killing curves characteristic of persistent populations
- Compare rates of killing between VBNC and normal cells [12]
Resuscitation Potential Post-Treatment:
- Remove antibiotics after exposure through washing or dilution
- Incubate in nutrient-rich media under optimal growth conditions
- Monitor for return of culturability indicating resuscitation
- Compare resuscitation frequency between antibiotic-treated and untreated VBNC cells [43] [20]
Molecular Mechanisms: Metabolic Downregulation as the Core Driver
The exceptional antibiotic tolerance of VBNC cells is orchestrated through sophisticated molecular mechanisms that center on metabolic reprogramming. The diagram below illustrates the integrated signaling pathways and regulatory networks that establish and maintain the VBNC state.
The molecular basis for metabolic downregulation involves several key systems:
Toxin-Antitoxin (TA) Systems: Under stress conditions, unstable antitoxins are degraded, freeing toxins that dramatically reduce translation, replication, and cell growth. This directly induces the persistent/VBNC state and dramatically increases antimicrobial tolerance [3].
CRP/cAMP-Mediated Metabolic Reprogramming: Carbon starvation activates adenylate cyclase (CyaA), increasing cAMP levels. The cAMP-Crp complex then redirects metabolism from anabolism to oxidative phosphorylation, maintaining energy metabolism while reducing biosynthetic activities [44].
Global Stress Response: The alternative sigma factor RpoS coordinates the expression of numerous stress response genes, contributing to the general downregulation of metabolic processes and enhancing multidrug tolerance [12] [20].
Structural and Physiological Adaptations: VBNC cells typically undergo morphological changes including reduction in cell size and conversion to coccoid forms. These changes decrease surface area to volume ratio, potentially minimizing energy requirements. Additionally, increased peptidoglycan cross-linking and alterations in membrane fatty acid composition contribute to enhanced physical and chemical resistance [20].
The Scientist's Toolkit: Essential Research Reagents and Solutions
Investigating VBNC states and their antibiotic insensitivity requires specialized reagents and methodologies that enable detection, quantification, and molecular analysis of these non-culturable cells.
Table 3: Essential Research Reagents for VBNC Investigation
| Reagent/Solution | Application | Function/Principle | Representative Example |
|---|---|---|---|
| PMA/PMAxx | Viability PCR | Crosslinks DNA in membrane-compromised cells, preventing amplification of dead cells | 20 µM PMAxx, 10-min dark incubation, 15-min photolysis [6] [45] |
| Live/Dead Staining Kits | Microscopy/FCM | Distinguishes membrane-intact (viable) from membrane-damaged (dead) cells | SYTO 9/propidium iodide combination [43] |
| Chlorination Solution | VBNC Induction | Indces VBNC state through oxidative stress | 0.5 mg/L chlorine for E. coli [43] |
| Catalase/Pyruvate | Resuscitation Media | Neutralizes H2O2 in media that inhibits VBNC growth | Enables culturability recovery in V. vulnificus [3] |
| ATP Assay Kits | Metabolic Activity | Quantifies cellular ATP levels as viability indicator | Detection in L. monocytogenes after long-term VBNC [20] |
| RNA Protection Buffers | Transcriptomics | Preserves labile mRNA for gene expression studies | RNA-seq analysis of VBNC E. coli [43] |
| Antibiotic Neutralizers | Tolerance Assays | Inactivates antibiotics after exposure to allow viability assessment | Enzymatic inactivation or dilution methods [43] |
Advanced detection methodologies have been developed to overcome the limitations of culture-based techniques:
Molecular Detection with Viability Markers:
- Propidium monoazide (PMA) and PMAxx selectively penetrate membrane-compromised cells and covalently bind DNA upon light exposure, preventing PCR amplification
- This allows selective quantification of membrane-intact (viable) cells via qPCR or ddPCR [6]
Digital Droplet PCR (ddPCR):
- Provides absolute quantification of target genes without standard curves
- Particularly valuable for samples with low bacterial concentrations
- Enumerates viable cells when combined with PMA treatment [6]
Flow Cytometry with Metabolic Probes:
- Detects respiratory activity or membrane potential as viability indicators
- Enables high-throughput analysis of heterogenous populations
- Reveals subpopulations with varying metabolic states [3]
RNA Sequencing for Transcriptomic Analysis:
- Identifies global gene expression patterns in VBNC cells
- Reveals upregulated stress response and downregulated biosynthetic genes
- Elucidates mechanisms of antibiotic tolerance at molecular level [43]
The comprehensive analysis of VBNC states confirms that metabolic drastic downregulation serves as the core driver of antibiotic insensitivity in these dormant bacterial forms. The experimental evidence demonstrates that VBNC cells exhibit exceptional tolerance to antibiotic concentrations that rapidly eliminate normal, culturable cells. This tolerance stems from a fundamental physiological reprogramming centered on reduced metabolic activity, rewired energy production, and maintenance of critical cellular functions through specific persistent pathways.
The implications for drug development are substantial. Conventional antibiotics primarily target active cellular processes, rendering them largely ineffective against VBNC cells with downregulated metabolism. Future therapeutic strategies must account for this phenotypic plasticity by developing compounds that either prevent entry into the VBNC state, target the unique metabolic pathways that maintain VBNC viability, or effectively stimulate resuscitation under controlled conditions where cells become susceptible again to conventional antibiotics.
Research gaps remain in understanding the heterogeneity within VBNC populations, the precise signals governing resuscitation, and the clinical significance of VBNC cells in chronic and recurrent infections. Addressing these questions will require continued innovation in detection methodologies and analytical approaches that can probe the physiology of these elusive cells at single-cell resolution. The ongoing study of VBNC states promises not only to advance fundamental understanding of bacterial dormancy but also to inform novel therapeutic interventions against persistent infections that evade current antibiotic treatments.
The Role of Toxin-Antitoxin (TAS) Systems in Inducing and Maintaining Dormancy
Toxin-antitoxin systems (TAS) are small genetic modules ubiquitous in bacterial genomes that play a crucial role in stress response and survival mechanisms [46]. These systems consist of a stable toxin protein that can disrupt essential cellular processes and an unstable antitoxin that neutralizes the toxin under normal growth conditions [47] [48]. Under stressful conditions, including antibiotic exposure and nutrient limitation, the labile antitoxin is degraded, freeing the toxin to arrest cell growth and induce a dormant state [49] [50]. This transition to dormancy is increasingly recognized as a critical factor in the context of the "viable but non-culturable" (VBNC) state, a condition where bacteria lose culturability on routine media but maintain viability and metabolic activity, displaying significantly enhanced antibiotic tolerance compared to their normal, growing counterparts [12] [3]. Understanding the molecular mechanisms by which TAS orchestrate this physiological switch is fundamental to addressing the challenges of persistent infections and antibiotic treatment failures.
Classification and Mechanisms of Toxin-Antitoxin Systems
Toxin-antitoxin systems are classified into eight types (I-VIII) based on the nature and mode of action of the antitoxin component [46]. Among these, Type I, II, and V systems have been most extensively studied for their roles in bacterial dormancy and stress response.
Table 1: Classification of Major Toxin-Antitoxin Systems Relevant to Dormancy
| Type | Toxin Nature | Antitoxin Nature | Mechanism of Antitoxin Action | Example Systems |
|---|---|---|---|---|
| Type I | Small hydrophobic protein | Antisense RNA | Binds toxin mRNA, preventing translation and targeting duplex for degradation [48] | hok-sok, tisB-istR [50] |
| Type II | Protein | Protein | Forms tight complex with toxin, blocking active site; degraded under stress [48] [49] | mazEF, relBE, vapBC, hipBA [47] [50] |
| Type V | Protein | Protein | Specifically cleaves toxin mRNA [48] | ghoTS [50] |
Type II TAS are particularly noteworthy for their abundance and well-characterized role in stress-induced dormancy. In these systems, the toxin and antitoxin proteins form a tight complex that represses the TA operon's transcription. Under normal conditions, antitoxins are produced in excess, ensuring toxin neutralization [49]. However, during stress, cellular proteases such as Lon and ClpXP are activated, leading to the preferential degradation of the unstable antitoxin. This frees the more stable toxin to act on its cellular targets, which include mRNA, tRNA, DNA replication machinery, and cell wall precursors, ultimately leading to growth arrest and a dormant state [47] [48] [46].
The Interplay Between TAS, Dormancy, and the VBNC State
From Growth Arrest to the VBNC State
The dormancy induced by TAS activation represents a continuum of metabolic downregulation. On one end are persister cells—a small, transiently dormant subpopulation tolerant to antibiotics but capable of resuscitation once the stress is removed [12] [50]. On the deeper end lies the VBNC state, where cells completely lose cultivability on standard media but retain viability, membrane integrity, and metabolic activity [12] [4]. Evidence suggests TAS are pivotal in facilitating entry into both these states. For instance, the hipBA system in E. coli is a well-documented genetic locus controlling persistence [3], while multiple TAS are upregulated during the induction of the VBNC state by stressors like chlorination [51].
The core benefit of this TAS-mediated dormancy is profound antibiotic tolerance. Most clinical antibiotics target active cellular processes like cell wall synthesis, transcription, and translation. By halting these processes, dormant VBNC cells become refractory to antibiotic killing, a phenomenon distinct from genetically encoded antibiotic resistance [12] [3]. This tolerance poses a significant clinical threat, as it can lead to recurrent infections once conditions become favorable and bacterial cells resuscitate [4].
Comparative Antibiotic Susceptibility: Normal vs. VBNC Cells
Quantitative data highlights the stark contrast in survival between normal and VBNC bacterial populations when exposed to antibiotics. The following table summarizes experimental findings from key studies.
Table 2: Antibiotic Susceptibility Profile of Normal Culturable vs. VBNC Bacterial Cells
| Bacterial Species | Inducing Stress | Antibiotic Challenge | Normal Cell Survival | VBNC Cell Survival | Reference |
|---|---|---|---|---|---|
| E. coli | Low-level chlorination (0.5 mg/L) | Ampicillin (200 µg/mL); Ofloxacin (5 µg/mL) | Not detectable (non-viable) | Maintained viability and metabolic activity [4] | |
| E. coli K12 (RP4 plasmid) | UV/Chlorine | Kanamycin, Tetracycline, Ampicillin | Culturable count reduced to 0 CFU | Retained antibiotic resistance determinants; capable of resuscitation into culturable, resistant cells [51] | |
| Vibrio vulnificus | Starvation, Low temperature | Various antibiotics, Heat, Oxidative stress | Significant killing | Enhanced tolerance and survival against multiple stresses [12] |
Experimental Analysis of TAS and VBNC States
Standard Protocols for Investigating TAS Function
To establish a causal link between TAS activation and dormancy, researchers employ well-defined molecular genetics protocols.
Protocol 1: Functional Validation of a Putative TAS
- Cloning and Expression: The putative toxin and antitoxin genes are cloned into an inducible expression vector. Two constructs are created: one for the toxin gene alone (
pT), and another for the toxin-antitoxin pair (pTA) where the antitoxin is expressed from its native promoter [52]. - Induced Expression: The constructs are transformed into a bacterial host (e.g., Clostridioides difficile 630Δerm). Toxin expression is induced in mid-exponential phase cultures using an inducer like anhydrotetracycline (ATc) [52].
- Phenotypic Assessment:
- Growth Kinetics: Bacterial growth is monitored by measuring optical density (OD) over time. Cultures with
pTare expected to show immediate growth arrest upon induction, whilepTAcultures should grow normally as the antitoxin neutralizes the toxin [52]. - Viability Counts: Colony-forming units (CFUs) are quantified by plating serial dilutions on non-selective media. A drop in CFUs upon toxin induction indicates a bactericidal effect, while stable CFUs alongside dropping OD suggests a bacteriostatic effect [52].
- Morphological Analysis: Cells are examined by light microscopy. Toxin overexpression often leads to morphological changes, such as filamentation, observed in about 10% of cells expressing type I toxins in C. difficile [52].
- Growth Kinetics: Bacterial growth is monitored by measuring optical density (OD) over time. Cultures with
Protocol 2: Investigating VBNC State in E. coli via Low-Level Chlorination
- VBNC Induction: A culture of E. coli is exposed to a low concentration of chlorine (e.g., 0.5 mg/L) for a defined period (e.g., 6 hours) to induce the VBNC state [4].
- Culturability and Viability Assessment:
- Antibiotic Tolerance Testing: VBNC cells are exposed to high concentrations of antibiotics (e.g., 128x or 64x MIC). Survival is determined by measuring the persistence of metabolic activity using the viability assays above, as CFU counts are no longer applicable [4].
- Resuscitation Attempt: VBNC cells are transferred to a rich, nutrient medium without antibiotics and monitored for the reappearance of culturable cells on plates, indicating escape from the VBNC state [4].
Molecular Pathway of TAS-Mediated VBNC Induction
The following diagram illustrates the coordinated molecular pathway through which environmental stresses trigger TAS activation and lead to the VBNC state, integrating key regulatory systems like the stringent response.
Diagram Title: Integrated Pathway of Stress-Induced VBNC State Formation
The Scientist's Toolkit: Essential Reagents for TAS and VBNC Research
Studying TAS and the VBNC state requires a combination of molecular biology tools, specialized culture techniques, and advanced analytical methods. The table below lists key reagents and their applications in this field.
Table 3: Essential Research Reagents and Tools for TAS and VBNC Studies
| Reagent / Tool | Function / Application | Example Use Case |
|---|---|---|
| Inducible Expression Vectors (e.g., pRPF185 with Ptet) | Controlled overexpression of toxin genes for functional validation [52]. | Demonstrating growth arrest upon toxin induction in C. difficile [52]. |
| Anhydrotetracycline (ATc) | Inducer for tetracycline-regulated promoters in cloning vectors. | Titrating toxin expression levels to study dose-dependent effects on dormancy [52]. |
| Vital Stains (SYTO 9, Propidium Iodide) | Differentiate viable and dead cells based on membrane integrity and metabolic activity via fluorescence microscopy or flow cytometry [4]. | Quantifying the proportion of VBNC cells in a population after chlorine treatment [4]. |
| Chlorine (Sodium Hypochlorite) | Chemical stressor to induce the VBNC state in model organisms like E. coli [4] [51]. | Mimicking disinfection stress in water systems to study VBNC formation and antibiotic tolerance [4]. |
| Catalase / Pyruvate | Scavengers of hydrogen peroxide (H₂O₂) in culture media. | "Rescuing" culturability of some VBNC cells by neutralizing H₂O₂ in standard media, revealing one mechanism of non-culturability [3]. |
| RNA-seq Transcriptomics | Genome-wide analysis of gene expression patterns. | Identifying upregulation of TAS and stress response genes in VBNC cells compared to culturable cells [4] [51]. |
Toxin-antitoxin systems are master molecular regulators that enable bacteria to survive lethal stresses by inducing a dormant state, with the VBNC condition representing a profound depth of dormancy. The experimental data clearly demonstrates that this state confers a dramatic increase in tolerance to conventional antibiotics, a phenomenon that standard susceptibility tests, reliant on culturable cells, completely miss. Future research must focus on unraveling the precise molecular "signals" that trigger resuscitation, identifying specific inhibitors of TAS activation, and developing novel therapeutic agents that target the unique physiology of dormant cells. Overcoming the challenge of VBNC cells and their associated antibiotic tolerance is paramount for improving the treatment of persistent and recurrent bacterial infections.
The escalating global health crisis of antimicrobial resistance demands a paradigm shift in our understanding of bacterial survival mechanisms. Central to this challenge is the viable but non-culturable (VBNC) state, a dormant condition wherein bacteria maintain metabolic activity but lose cultivability on standard media, conferring tolerance to antibiotic treatments and environmental stressors [53]. This state represents a critical frontier in the battle against persistent infections, as VBNC cells function as a reservoir for relapse and resistance dissemination.
Transcriptomic technologies have revolutionized our ability to decode the molecular underpinnings of bacterial dormancy and stress adaptation. By providing a comprehensive, systems-level view of gene expression changes, RNA sequencing (RNA-Seq) reveals the precise regulatory networks that bacteria deploy to survive lethal threats. This article synthesizes recent transcriptomic findings to construct a comparative landscape of stress responses in VBNC versus normal bacterial cells, offering researchers a foundational framework for developing novel anti-infective strategies targeted at the deepest levels of bacterial persistence.
Comparative Transcriptomic Profiles: VBNC vs. Normal Cells
Global Expression Changes Across Bacterial Species
The transition to the VBNC state triggers extensive transcriptional reprogramming across diverse bacterial species. The table below summarizes key differential expression patterns observed in transcriptomic studies:
Table 1: Core Transcriptional Changes in VBNC Cells Across Bacterial Species
| Bacterial Species | VBNC Inducer | Upregulated Processes/Genes | Downregulated Processes/Genes | Reference |
|---|---|---|---|---|
| Bacillus subtilis | Osmotic stress + Kanamycin | ICEBs1 conjugative element, Queuosine biosynthesis (queC-queF operon), Proline catabolism | General metabolic activity, Growth-related genes | [53] |
| E. coli O157:H7 | Low temperature (-20°C) | Ion transport, Protein synthesis, Transmembrane transport (SecY, FtsY, Ffh) | Central carbon metabolism, Energy production | [54] |
| Lacticaseibacillus paracasei Zhang | Osmotic + Cold stress | Protein transport, Glycolysis, Phosphatidylglycerol metabolism, Propionate metabolism | Cell division, Ribosome biogenesis | [55] |
| Multiple Pathogens | Cross-stress conditions | RpoS regulon, Carbon metabolism, Amino acid biosynthesis, Purine metabolism | - | [56] |
Universal Stress Response Signatures
Network biology approaches analyzing five opportunistic pathogens have identified a conserved set of 31 hub-bottleneck proteins that function as central mediators of cross-stress response, regardless of the specific stressor or bacterial species [56]. These proteins operate within the RpoS-mediated general stress regulon and are interconnected with 20 common metabolic pathways, with carbon metabolism exhibiting the highest crosstalk with amino acid biosynthesis and purine metabolism pathways. This core stress response network represents a universal protection mechanism that enhances bacterial survivability under adverse conditions, including antibiotic exposure.
Methodological Framework for VBNC Transcriptomics
Standardized VBNC Induction and Validation Protocols
Transcriptomic analysis of VBNC states requires rigorous methodological standardization to ensure reproducible and meaningful results. The following workflow outlines the critical stages for reliable VBNC transcriptomic studies:
VBNC Induction Methods:
- Osmotic/Antibiotic Combination: For B. subtilis, pre-exposure to 0.6 M NaCl followed by lethal-dose kanamycin treatment effectively induces VBNC state [53].
- Low-Temperature Stress: E. coli O157:H7 enters VBNC state after 152 days at -20°C in food matrices [54].
- Sub-lethal Photocatalysis: Effective for inducing VBNC state in antibiotic-resistant E. coli within 1 hour of treatment [16] [18].
- Combined Cold/Acidic Conditions: L. paracasei Zhang transitions to VBNC state at pH 3.8 and 4°C over 210 days [57].
State Validation Techniques:
- Culturability Testing: Serial dilution and plating on appropriate solid media (e.g., LB agar, MRS agar) with confirmation of non-culturability after repeated attempts [53] [57].
- Membrane Integrity: Live/dead staining using BacLight Bacterial Viability Kit with SYTO 9 and propidium iodide [57].
- Metabolic Activity: Direct viable count (DVC) assay with nalidixic acid to inhibit DNA replication while detecting substrate absorption capability [54].
RNA Sequencing and Data Analysis Pipeline
Table 2: Essential Research Reagents for VBNC Transcriptomic Studies
| Reagent/Category | Specific Examples | Function/Application |
|---|---|---|
| RNA Extraction Kits | Bacterial Total RNA Extraction kit (Sigma-Aldrich) | High-quality RNA isolation from bacterial cells |
| rRNA Depletion | Ribo-zero rRNA kit (Epicenter Inc.) | Enrichment of mRNA by ribosomal RNA removal |
| cDNA Synthesis | SuperScript Double-Stranded cDNA Synthesis kit (Invitrogen) | Library construction for sequencing |
| Sequencing Platforms | Illumina HiSeq 2500 | High-throughput transcriptome sequencing |
| Viability Stains | Live/Dead BacLight Bacterial Viability Kit (Molecular Probes) | Differentiation of viable vs. dead cells |
| Reference Genomes | E. coli O157:H7 EDL933 (NC_002655.2) | Read alignment and expression quantification |
Bioinformatic Analysis Workflow:
- Quality Control: FastQC for raw read quality assessment and adapter trimming.
- Read Alignment: Mapping to reference genomes using TopHat2 or Bowtie2 with ≤2 base mismatches allowed [54].
- Expression Quantification: Calculation of FPKM (Fragments Per Kilobase Million) values for gene expression levels.
- Differential Expression: Identification of significantly altered genes using thresholds (typically |log2FC| ≥ 1 and FDR ≤ 0.05) [56].
- Functional Enrichment: GO term and KEGG pathway analysis using tools like KOBAS 3.0 to identify biological processes and metabolic pathways significantly enriched in VBNC cells [56] [54].
Molecular Mechanisms of VBNC Formation and Maintenance
Conserved Genetic Programs and Metabolic Rearrangements
The transition to the VBNC state activates a sophisticated genetic program for survival under energy-limited conditions. Transcriptomic analyses consistently reveal downregulation of ribosomal genes and protein synthesis machinery, indicating a fundamental shift from growth to maintenance metabolism [53] [55]. Concurrently, energy-intensive processes like cell division are suppressed, redirecting limited cellular resources toward essential preservation functions.
A key survival strategy involves rewiring of central carbon metabolism. In L. paracasei Zhang, propionate metabolism emerges as a significantly upregulated pathway under osmotic and cold stress, potentially serving as an alternative energy source when primary metabolic routes are compromised [55]. This metabolic flexibility is further enhanced by increased expression of transporters for nutrients like proline in B. subtilis, enabling VBNC cells to scavenge alternative nutrient sources from their environment [53].
Stress Response Pathways and Protein Homeostasis
The molecular architecture of VBNC formation centers on the activation of specialized stress response pathways that maintain protein homeostasis and cellular integrity under adverse conditions:
The queuosine biosynthesis pathway (queC-queF operon) is significantly upregulated in VBNC B. subtilis cells, representing a crucial mechanism for maintaining translation accuracy under stress [53]. Queuosine-modified tRNAs minimize translation errors during antibiotic-induced protein misfolding, thereby promoting bacterial survival. Experimental evidence demonstrates that mutants deficient in queuosine biosynthesis (∆queG) show increased susceptibility to kanamycin, confirming the pathway's importance in antibiotic tolerance [53].
Conjugative genetic elements like ICEBs1 are strongly induced in VBNC cells, potentially facilitating DNA exchange and genetic adaptation under antibiotic pressure [53]. This response is likely triggered by antibiotic-induced oxidative stress and DNA damage, activating the SOS response and potentially accelerating the acquisition of resistance genes in dormant populations.
Research Implications and Future Directions
Diagnostic and Therapeutic Applications
The transcriptomic signatures identified in VBNC cells present promising targets for novel therapeutic interventions. Rather than targeting growth processes, which are largely inactive in dormant cells, effective strategies might focus on disrupting the maintenance mechanisms and resuscitation pathways essential for VBNC survival and recovery. The conserved stress response network centered around RpoS and its regulon offers particularly attractive targets for broad-spectrum approaches against persistent infections [56].
From a diagnostic perspective, detecting the unique gene expression patterns associated with VBNC states could enable early identification of dormant bacterial populations in clinical, industrial, and environmental settings. This would address the critical limitation of conventional culture-based methods, which significantly underestimate viability by failing to detect VBNC cells [57].
Industrial and Environmental Considerations
Understanding bacterial stress responses has significant implications beyond clinical medicine. In industrial fermentation processes utilizing bacteria for biofuel and chemical production, controlling stress responses may enhance production yields by optimizing cell growth and metabolic activity [58]. Conversely, in water disinfection systems, recognition that sub-lethal treatments can induce VBNC states highlights the need for more effective eradication strategies that prevent bacterial persistence and subsequent resuscitation [16].
Transcriptomic technologies have unveiled the complex genetic landscape of bacterial dormancy, revealing both universal stress adaptation mechanisms and species-specific survival strategies. The VBNC state represents a sophisticated survival phenotype characterized by metabolic downshift, activation of maintenance programs, and rewiring of central metabolic pathways. These transcriptomic insights provide a roadmap for developing next-generation antimicrobials that target the core persistence mechanisms shared across diverse bacterial pathogens. As we deepen our understanding of these universal protection strategies, we move closer to overcoming the formidable challenge of treatment-resistant infections and mitigating the global threat of antimicrobial resistance.
In the ongoing struggle for survival against antimicrobial agents and environmental stresses, bacteria have evolved sophisticated adaptations centered on their primary barriers: the cell membrane and the cell wall. These structures, which serve as the first line of defense, undergo significant functional and structural modifications that enable bacterial persistence. Particularly within the context of the viable but non-culturable (VBNC) state—a dormant condition that allows bacteria to survive under adverse conditions—these adaptations manifest as reduced membrane permeability and enhanced cell wall fortification. This physiological transformation presents a substantial challenge in clinical and environmental settings, as VBNC cells not only evade conventional detection methods but also exhibit markedly increased tolerance to antibiotics that typically eliminate their normal, metabolically active counterparts [16] [18] [41].
Understanding these adaptations is crucial for developing strategies to combat persistent infections and the spread of antibiotic resistance. This guide provides a comparative analysis of the performance differences between VBNC cells and normal cells, detailing the experimental approaches used to characterize these resilient biological states.
Comparative Analysis: VBNC Cells vs. Normal Cells
The transition to the VBNC state is characterized by a comprehensive reprogramming of the cell envelope, leading to distinct phenotypic differences compared to normal cells. The tables below summarize the key adaptations and their functional consequences.
Table 1: Comparative Characteristics of Normal vs. VBNC Bacterial Cells
| Characteristic | Normal Cells | VBNC Cells | Functional Consequence |
|---|---|---|---|
| Culturability | Culturable on standard media | Non-culturable on standard media [16] [18] [41] | Evasion of conventional detection methods |
| Metabolic Activity | Fully active | Low but detectable [41] | Survival without growth |
| Cell Morphology | Normal length | Decreased cell length [16] | Reduced biosynthetic activity |
| Membrane Permeability | Baseline level | Significantly reduced [59] | Barrier to antimicrobial entry |
| Antibiotic Resistance | Baseline susceptibility (wild-type) | Higher resistance than wild-type [16] [18] | Treatment failure and relapse |
| Resuscitation Potential | N/A | Can resuscitate when stress is removed [16] [18] | Risk of recurrent infection |
Table 2: Quantitative Evidence of VBNC Adaptations and Resilience
| Experimental Finding | Quantitative Result | Significance |
|---|---|---|
| VBNC Induction by Sub-lethal Photocatalysis | >10⁸ CFU/mL E. coli entered VBNC state within 1 hour [16] [18] | Rapid and widespread state transition under stress |
| Resuscitation Timeframe | Resuscitation observed 5-20 days after stress removal [16] | Persistence and potential for delayed infection |
| Post-Resuscitation Antibiotic Resistance | Resuscitated cells showed higher antibiotic resistance than wild-type [16] [18] | Adaptation provides a lasting survival advantage |
| Membrane Permeability in S. aureus | Protoplasts (wall-free) showed reduced membrane permeability and altered lipid composition [59] | Direct evidence of membrane adaptation as a defense mechanism |
Experimental Protocols for Studying VBNC Adaptations
Induction and Validation of the VBNC State
The reliable induction and confirmation of the VBNC state are foundational to its study. The following protocol, adapted from studies on E. coli and Klebsiella pneumoniae, outlines a standardized approach [16] [41].
- VBNC Induction via Sub-lethal Stress: Bacterial cultures are grown to mid-logarithmic phase and then subjected to a sub-lethal stressor. For example, cultures are exposed to sub-lethal photocatalysis using a TiO₂ catalyst illuminated with a 365 nm LED lamp (100 mW/cm²) for a defined period (e.g., 1-10 hours) [16]. Alternatively, low-temperature incubation (e.g., at 4°C in artificial seawater) for extended periods (e.g., 50 days) can also induce the VBNC state [41].
- Culturability Assay: The gold standard for confirming VBNC entry is the loss of culturability. Throughout the induction process, aliquots of the bacterial suspension are periodically plated onto rich nutrient agar plates (e.g., Luria-Bertani agar). The VBNC state is considered achieved when no colonies form on the plates after 48 hours of incubation at an optimal growth temperature (e.g., 37°C) [41].
- Viability and Morphological Validation: The lack of growth on plates does not confirm viability. Therefore, concurrent viability assays are essential. This can be done using live/dead staining kits (e.g., using propidium monoazide) in conjunction with fluorescence microscopy or flow cytometry. Furthermore, morphological changes, such as a decrease in cell length, can be visualized and quantified using scanning electron microscopy (SEM) [16].
Absolute Quantification of VBNC Cells Using PMA-ddPCR
Accurately quantifying VBNC cells, which do not form colonies, requires advanced molecular techniques. Droplet Digital PCR (ddPCR) combined with propidium monoazide (PMA) treatment has emerged as a powerful method for the absolute quantification of viable cells [41].
- PMA Treatment Optimization: PMA is a dye that penetrates only cells with compromised membranes (dead cells) and covalently cross-links to their DNA, preventing its amplification. Optimal PMA concentration and incubation conditions must be determined. A typical optimization involves testing final PMA concentrations ranging from 5 μM to 200 μM. The sample is incubated in the dark for 5-30 minutes, followed by a 15-minute exposure to a high-intensity halogen light source to photo-activate the dye [41].
- Droplet Digital PCR (ddPCR): Following PMA treatment and DNA extraction, the sample is partitioned into thousands of nanoliter-sized droplets in a ddPCR system. Each droplet acts as an individual PCR reaction chamber. The PCR targets single-copy genes (e.g., rpoB, adhE for K. pneumoniae). The system counts the number of fluorescence-positive droplets, and the absolute concentration of viable cell gene copies is calculated using Poisson statistics, without the need for a standard curve [41].
- Experimental Workflow: The diagram below illustrates the integrated workflow for inducing and quantifying VBNC cells.
Single-Cell Analysis of Antimicrobial Tolerance
Bulk population studies can mask the presence of tolerant subpopulations. Microfluidic gel encapsulation enables the observation of heterogeneity in bacterial responses to antibiotics at the single-cell level [60].
- Microfluidic Gel Encapsulation: A suspension of bacteria is mixed with a low-melting-point agarose gel (e.g., 3%) and applied to a micropatterned substrate to create thin gel pads, effectively trapping individual cells for time-lapse imaging [60].
- Time-Kill Kinetics in Physiological Media: The gel-encapsulated cells are perfused with antimicrobials dissolved in a physiologically relevant medium (e.g., human urine for uropathogens) at concentrations mimicking in vivo conditions. The system is maintained at 37°C on a microscope stage [60].
- Single-Cell Imaging and Analysis: Time-lapse microscopy is used to monitor individual cells over several hours. This allows for the direct observation of heterogeneous responses, including the formation of persister cells (which resume growth after antibiotic removal) and the identification of VBNC cells (which remain viable but do not divide) [60].
Molecular Mechanisms of Adaptation
The phenotypic adaptations of VBNC cells are underpinned by specific molecular changes to the cell envelope. The diagram below synthesizes the key signaling and regulatory pathways involved in this adaptive response.
The primary goal of these molecular changes is to maintain membrane homeostasis under stress. By reducing fluidity and permeability, the cell creates a formidable barrier that restricts the influx of toxic molecules, including antibiotics [59] [61]. Concurrent fortification of the cell wall provides an additional layer of defense, protecting the underlying membrane from damage. These coordinated adaptations are a hallmark of the VBNC state and are supported by findings that VBNC E. coli cells resuscitate by repairing oxidative damage and reallocating energy, underscoring the critical role of membrane and wall integrity in survival and recovery [16].
The Scientist's Toolkit: Essential Research Reagents
Studying membrane and wall adaptations requires a specific set of reagents and tools. The following table details key solutions used in the experiments cited in this guide.
Table 3: Essential Research Reagents for Studying Membrane and Wall Adaptations
| Research Reagent / Tool | Function / Application | Example Use Case |
|---|---|---|
| Propidium Monoazide (PMA) | DNA intercalating dye that penetrates only membrane-compromised (dead) cells; allows selective amplification of DNA from viable (VBNC) cells [41] | Differentiating viable VBNC cells from dead cells in qPCR/ddPCR assays |
| Droplet Digital PCR (ddPCR) | Microfluidic-based platform for absolute quantification of nucleic acid targets without a standard curve; provides high precision for low-abundance targets [41] | Absolute quantification of gene copy numbers from VBNC cells using single-copy genes (e.g., rpoB) |
| Lysostaphin | Enzyme that specifically digests the peptidoglycan cell wall of Staphylococcus species. | Preparation of protoplasts (wall-free cells) to study membrane-specific functions without the wall's protective influence [59] |
| Artificial Seawater (ASW) | Defined, nutrient-poor medium that induces starvation stress. | Long-term incubation to induce the VBNC state in bacterial cultures (e.g., for K. pneumoniae) [41] |
| Microfluidic Gel Encapsulation Chips | Micropatterned substrates for trapping individual bacterial cells in a thin gel layer. | Single-cell time-lapse analysis of growth and killing kinetics in response to antimicrobials [60] |
| TiO₂ Nanotubes | Photocatalyst that generates reactive oxygen species under UV light. | Inducing VBNC state in E. coli via sub-lethal photocatalytic stress [16] |
VBNC vs. Resistance vs. Persistence: Demystifying the Spectrum of Bacterial Survival
In the ongoing battle against antibiotic resistance, the scientific community is confronted with two fundamentally different bacterial survival strategies: the Viable but Non-Culturable (VBNC) state, a phenotypic condition of dormancy and tolerance, and heritable genetic resistance, driven by mutational changes or acquisition of resistance genes. While both phenomena result in treatment failures, their underlying mechanisms, detection requirements, and clinical implications differ substantially. The VBNC state represents a temporary, reversible condition where bacteria lose culturability on standard media but maintain viability, metabolic activity, and often enhanced tolerance to multiple stressors, including antibiotics [62]. In contrast, genetic antibiotic resistance arises from stable genetic changes that enable bacteria to grow in the presence of antibiotics through specific biochemical resistance mechanisms [63]. Understanding this distinction is critical for developing effective countermeasures, as interventions that target genetically resistant bacteria may prove ineffective against VBNC populations, and vice versa. This guide systematically compares these phenomena to equip researchers with the conceptual framework and methodological tools needed to address both challenges in parallel.
Fundamental Mechanisms: Dormancy Versus Genetic Change
The VBNC State: A Phenomenon of Physiological Adaptation
The VBNC state constitutes a survival strategy triggered by environmental stresses, including antibiotic exposure, nutrient starvation, and disinfection treatments. Bacteria in the VBNC state undergo significant physiological reprogramming characterized by reduced metabolic activity, dwarfing and rounding of cells, and strengthened cell walls through increased peptidoglycan cross-linking [62]. These changes collectively contribute to a non-replicating, dormant phenotype that exhibits broad-spectrum tolerance to antimicrobials without genetic alteration.
Key molecular mechanisms regulating VBNC entry include:
- Stress response systems: General stress response (rpoS), SOS response, and oxidative stress response (oxyR) pathways are activated [64] [3]
- Toxin-antitoxin (TA) systems: These genetic modules promote dormancy by degrading cellular components essential for growth, such as mRNA and proteins [3]
- Metabolic downregulation: Drastic reduction in energy metabolism and protein synthesis [62]
- Membrane modifications: Changes in membrane fluidity and composition, including increased unsaturated fatty acids [62]
Notably, VBNC cells maintain the potential for resuscitation when favorable conditions return, posing a significant risk for recurrent infections [28] [62].
Genetic Antibiotic Resistance: Heritable Defense Mechanisms
Genetic antibiotic resistance results from stable genetic changes that confer specific resistance mechanisms, which are heritable and enable bacterial proliferation despite antibiotic presence. The primary genetic strategies include:
- Chromosomal mutations: Spontaneous mutations in genes encoding antibiotic targets, transport systems, or regulatory elements [63] [65]. For example, mutations in the rpoB gene confer rifampicin resistance in Escherichia coli, while alterations in DNA gyrase confer resistance to fluoroquinolones [64] [63].
- Horizontal gene transfer: Acquisition of resistance genes through conjugation (plasmid transfer), transduction (phage-mediated transfer), or transformation (uptake of free DNA) [63] [65] [66]. This facilitates rapid dissemination of resistance determinants such as β-lactamase genes across bacterial populations.
The major biochemical mechanisms employed include:
- Antibiotic inactivation: Enzymatic modification or destruction of antibiotics (e.g., β-lactamases) [63]
- Target modification: Alteration of antibiotic binding sites to reduce drug affinity [63] [65]
- Efflux pumps: Enhanced export of antibiotics from the cell [63]
- Reduced permeability: Decreased antibiotic entry through cell envelope modifications [63]
Table 1: Fundamental Characteristics of VBNC State Versus Genetic Resistance
| Characteristic | VBNC State | Genetic Resistance |
|---|---|---|
| Nature of survival | Phenotypic tolerance | Genotypic resistance |
| Genetic basis | No genetic changes required | Chromosomal mutations or acquired genes |
| Reversibility | Resuscitation possible under favorable conditions | Stable and heritable |
| Detection methods | Viability assays (without culturability) | Culture-based AST, molecular detection |
| Metabolic state | Dormant or significantly reduced activity | Active replication |
| Primary mechanisms | Stress responses, TA systems, metabolic shutdown | Drug inactivation, target alteration, efflux pumps |
| Cross-resistance pattern | Broad, non-specific tolerance | Often specific to antibiotic classes |
Experimental Approaches: Methodological Considerations and Protocols
Induction and Detection of VBNC Cells
VBNC Induction Protocols:
- Chemical induction: Exposure to low-level chlorine (0.5 mg/L for 6 hours) or other disinfectants effectively induces VBNC state in E. coli while maintaining cell viability [4] [67].
- Sub-lethal photocatalysis: Treatment with TiO2 nanotubes under 365 nm LED illumination (100 mW/cm²) for 6-10 hours induces VBNC state in both antibiotic-resistant and susceptible E. coli strains [28].
- Multiple stressor application: Combined stressors such as UV/chlorine in water treatment systems can induce VBNC state in antibiotic-resistant E. coli, with variations observed based on resistance determinants (plasmid-borne vs. chromosomal) [64].
Detection and Quantification Methods:
- Viability staining: Combine fluorescent dyes such as SYTO 9 (membrane-permeable, labels live cells) with propidium iodide (membrane-impermeable, labels dead cells) to distinguish viable VBNC populations from dead cells using flow cytometry or fluorescence microscopy [4] [3].
- Molecular activity assays: Detect metabolic activity via ATP assays (e.g., bacTiter-Glo assay) or redox detection (e.g., CTC reduction assay) [3] [62].
- mRNA detection: Identify viable cells through reverse transcription quantitative PCR (RT-qPCR) targeting stress-induced genes (e.g., ompW, rpoS) or metabolic genes, as mRNA degrades rapidly in dead cells [64] [4] [3].
- Direct viable count (DVC): Incubate samples with nutrients and antibiotics that inhibit cell division, then detect elongated, metabolically active cells that cannot form colonies [4].
Figure 1: Experimental Workflow for VBNC State Induction, Detection, and Resuscitation
Assessment of Genetic Resistance
Standard Antimicrobial Susceptibility Testing (AST):
- Broth microdilution: Determine Minimum Inhibitory Concentration (MIC) using standardized concentrations in 96-well plates, following CLSI or EUCAST guidelines [63].
- Agar dilution: Incorporate antibiotics into solid media to establish breakpoint concentrations for resistance categorization [63].
- Gradient diffusion: Use antibiotic-impregnated strips (e.g., E-test) to establish MIC values on agar plates [63].
Molecular Detection Methods:
- PCR and qPCR: Amplify specific antibiotic resistance genes (e.g., blaCTX-M, mecA, vanA) to confirm genetic determinants [63] [67].
- Whole-genome sequencing: Comprehensive identification of resistance mutations and acquired resistance genes through genomic analysis [63].
- Microarray-based detection: Simultaneous screening for multiple resistance determinants in bacterial isolates [63].
Horizontal Gene Transfer Assessment:
- Conjugation assays: Monitor plasmid transfer between donor and recipient strains on solid surfaces or in liquid media [63] [66].
- Transduction experiments: Demonstrate bacteriophage-mediated transfer of resistance genes [63] [66].
- Natural transformation assays: Assess uptake of free DNA from the environment by competent bacteria [63] [66].
Comparative Analysis: Quantitative Experimental Data
Antibiotic Tolerance and Resistance Patterns
Table 2: Comparative Antibiotic Susceptibility Profiles of VBNC vs. Genetic Resistance
| Parameter | VBNC Cells | Genetically Resistant Cells | Experimental Context |
|---|---|---|---|
| Tolerance/Resistance Level | Survive 128× MIC of ampicillin [4] | Grow at clinical breakpoint concentrations [63] | E. coli in VBNC state vs. plasmid-mediated resistant E. coli |
| Spectrum | Broad, multi-drug tolerance [62] | Often specific to drug classes [63] | VBNC induced by low-level chlorination |
| Reversibility | Resuscitation in 5-20 days post-stress [28] | Stable without selective pressure [65] | Sub-lethal photocatalysis-induced VBNC |
| Metabolic Activity | Reduced but detectable (ATP, mRNA) [62] | Normal growth metabolism [63] | CTC reduction, ATP assays |
| Gene Expression | Stress response genes upregulated [64] [4] | Resistance genes constitutively expressed [63] | Transcriptomic analysis |
| Detection by AST | Not detected (non-culturable) [3] | Reliably detected [63] | Standard plate count vs. molecular methods |
Molecular Characterization Data
Table 3: Molecular Features of VBNC vs. Genetic Resistance Mechanisms
| Molecular Feature | VBNC State | Genetic Resistance | Detection Method |
|---|---|---|---|
| Key genetic elements | rpoS, toxing-antitoxin systems, oxidative stress genes [64] [3] | Antibiotic resistance genes (e.g., blaCTX-M, mecA), target site mutations [63] | RNA-seq, RT-qPCR, WGS |
| Gene expression changes | Downregulation of protein synthesis genes, upregulation of stress response genes [4] | Constitutive or induced expression of resistance genes [63] | Transcriptomics, RT-qPCR |
| Mobile genetic elements | Limited mobilization during dormancy [67] | Plasmids, transposons, integrons facilitate spread [63] [65] | Conjugation assays, plasmid analysis |
| Membrane composition | Increased unsaturated fatty acids, peptidoglycan cross-linking [62] | May exhibit modified porins or efflux pump overexpression [63] | Lipid analysis, proteomics |
| Genetic stability | Phenotypic state reversible upon resuscitation [28] | Genetically encoded and heritable [65] | Long-term culture, stability assays |
Figure 2: Molecular Pathways of VBNC State Formation Versus Genetic Resistance Development
The Researcher's Toolkit: Essential Reagents and Methodologies
Table 4: Essential Research Reagents and Tools for VBNC and Resistance Studies
| Reagent/Tool | Application | Function/Principle | Representative Examples |
|---|---|---|---|
| Viability stains | VBNC detection | Membrane integrity assessment | SYTO 9/PI (LIVE/DEAD BacLight) [4] [3] |
| ATP detection kits | Metabolic activity assay | Quantification of cellular ATP | BacTiter-Glo Microbial Cell Viability Assay [3] |
| CTC tetrazolium salt | Respiratory activity | Detection of electron transport chain activity | 5-cyano-2,3-ditolyl tetrazolium chloride [3] |
| Viability PCR reagents | Molecular viability detection | Selective detection of intact cells via DNA intercalation | PMA, EMA dyes + qPCR [3] |
| Specialized media | Resuscitation studies | Nutrient-rich formulations for VBNC recovery | LB broth with catalase/pyruvate [62] |
| Antibiotic test strips | AST profiling | MIC determination | E-test strips, MIC test strips [63] |
| PCR/qPCR reagents | Resistance gene detection | Amplification of specific resistance markers | Primers for blaCTX-M, mecA, vanA [63] [67] |
| Conjugation assay components | HGT studies | Plasmid transfer assessment | Filter mating setups, selective media [63] [66] |
Research Implications and Future Directions
The distinction between VBNC tolerance and genetic resistance has profound implications for antimicrobial research and development. The broad-spectrum tolerance exhibited by VBNC cells necessitates different therapeutic approaches compared to genetically resistant bacteria. While genetic resistance often responds to higher antibiotic doses or alternative drugs within the same class, VBNC cells remain unaffected due to their non-growing state and require strategies that either prevent VBNC induction or stimulate resuscitation followed by conventional treatment [28] [62].
Future research should prioritize:
- Anti-dormancy therapies: Compounds that prevent VBNC entry or force resuscitation without enhancing pathogenicity
- Dual-targeting approaches: Therapeutic strategies that simultaneously address both genetic resistance mechanisms and VBNC tolerance
- Improved diagnostic platforms: Technologies that detect VBNC cells in clinical settings to prevent underestimation of bacterial burdens
- Disinfection optimization: Methods that ensure complete bacterial inactivation without inducing VBNC state in residual populations [64] [67]
Understanding the interplay between these resistance paradigms is essential for overcoming treatment failures and developing the next generation of antimicrobial strategies. Researchers must account for both phenomena in experimental design, drug development, and clinical practice to effectively address the multifaceted challenge of antibiotic treatment failure.
Within isogenic bacterial populations exposed to stress, two distinct but related dormant subpopulations emerge as critical contributors to chronic infections and treatment failure: viable but non-culturable (VBNC) cells and persister cells [68] [3]. These phenotypic variants represent a "dormancy continuum" that enables bacterial populations to survive lethal environmental challenges, including antibiotic exposure, through non-genetic mechanisms [69] [68]. While both cell types exhibit dramatically increased tolerance to antimicrobial interventions and evade conventional culture-based detection methods, they possess fundamental differences in their physiological states and resuscitation capabilities [70] [71]. Understanding the precise positioning of VBNC and persister cells along this dormancy continuum is essential for researchers and drug development professionals seeking to combat persistent infections and address the growing threat of antibiotic tolerance [68] [3].
The clinical significance of these dormant subpopulations cannot be overstated. Persisters are increasingly recognized as the underlying cause of recurrent and chronic infections, responsible for relapse after treatment and contributing to the recalcitrance of biofilm-associated infections [68]. Meanwhile, VBNC cells represent a hidden reservoir of pathogens that can evade standard diagnostic procedures while maintaining metabolic activity and potential virulence [16] [72]. This comparative guide examines the distinctive characteristics, formation mechanisms, detection methodologies, and resuscitation behaviors of VBNC and persister cells, providing experimental data and protocols to support ongoing research in bacterial persistence and antimicrobial development.
Comparative Characteristics: VBNC vs. Persister Cells
Defining Features and Diagnostic Parameters
Table 1: Core Characteristics of VBNC and Persister Cells
| Parameter | VBNC Cells | Persister Cells |
|---|---|---|
| Culturability | Complete loss of cultivability on routine media [16] [72] | Cannot cultivate during antibiotic exposure but resume growth after stress removal [68] |
| Metabolic State | Reduced but detectable metabolic activity [16] [72] | Non-growing or slow-growing, with heterogeneous metabolic states [68] |
| Membrane Integrity | Maintain intact membrane [41] [72] | Maintain intact membrane [71] |
| Resuscitation | Require specific resuscitation signals; may need extended time [16] [72] | Spontaneously resuscitate when stress is removed [68] [71] |
| Antibiotic Susceptibility | High tolerance to multiple antibiotic classes [16] [3] | Tolerance during dormancy; susceptibility returns upon resuscitation [68] |
| Morphological Changes | Significant changes including cell rounding and cytoplasmic condensation [16] [72] | Generally retain normal morphology [73] |
| Genetic Basis | Phenotypic adaptation without genetic change [3] [72] | Phenotypic variant of wild-type population [69] [68] |
The Dormancy Continuum Concept
The relationship between VBNC and persister cells can be understood through the "dormancy continuum" model, where bacterial subpopulations occupy different positions along a spectrum of metabolic activity and resuscitability [69]. In this model, persisters represent a transitional state that may progress toward the deeper dormancy characteristic of VBNC cells under sustained stress conditions [71]. Recent research suggests these states may share adaptive mechanisms at the cellular level, as demonstrated by similar membrane lipid modifications in both Staphylococcus aureus persisters and VBNC cells when exposed to glycopeptide antibiotics [69].
The depth of dormancy varies within each category, with evidence supporting the existence of "shallow" and "deep" persistence states [68]. Similarly, VBNC cells may exhibit varying degrees of metabolic activity and resuscitation potential depending on the inducing stress and bacterial species [16] [72]. This continuum model explains the observed overlap in characteristics between these states and why clear experimental differentiation remains challenging without sophisticated methodological approaches.
Methodologies for Isolation and Characterization
Experimental Workflows for Dormant Cell Analysis
Diagram 1: Comprehensive Workflow for Dormant Cell Research
Key Detection and Quantification Methods
Table 2: Methodologies for Detecting and Analyzing Dormant Cells
| Method Category | Specific Techniques | Application | Key Findings |
|---|---|---|---|
| Viability Staining | Syto9/PI staining [72], CTC assay [72] | Differentiate live/dead cells; measure respiratory activity | 17.1% of A. baumannii cells remained viable after 4 days PSP despite zero cultivability [72] |
| Molecular Detection | PMA-qPCR [41] [6], PMA-ddPCR [41] [6] | Quantify viable cells without cultivation; absolute quantification | ddPCR with three single-copy genes enabled absolute quantification of VBNC K. pneumoniae [41] [6] |
| Microscopy Approaches | Transmission electron microscopy [16] [72], Fluorescence microscopy [71] | Morphological characterization; single-cell analysis | VBNC cells showed cytoplasmic condensation and vesicle formation versus minimal changes in persisters [16] [73] [72] |
| Flow Cytometry | Protein dilution method [71], Cell sorting | Single-cell analysis; population heterogeneity | Persisters resuscitated within 1 hour with doubling time identical to normal cells (23.3 ± 2.54 min) [71] |
| Culture-Based | Resuscitation assays [16] [72], Biphasic killing curves [69] | Confirm resuscitability; quantify persister fractions | A. baumannii VBNC cells could be resuscitated after 10 months in high-salt conditions [72] |
The Scientist's Toolkit: Essential Research Reagents
Table 3: Key Research Reagents for Dormancy Studies
| Reagent/Category | Specific Examples | Function/Application | Experimental Notes |
|---|---|---|---|
| Viability Indicators | Syto9/PI (LIVE/DEAD) [72], CTC [72], PMA [41] [6] | Membrane integrity assessment; metabolic activity; viable cell DNA detection | PMA concentration must be optimized (5-200 μM); EMA shows higher cytotoxicity [41] [6] |
| Induction Stressors | Ampicillin [71], Ciprofloxacin [41] [6], Vancomycin [69] [73], High-salt media [72] | Trigger dormancy entry; enrich dormant subpopulations | Antibiotic concentrations typically 10-100× MIC; salt concentration varies by species [69] [72] |
| Molecular Biology | Single-copy gene primers (rpoB, adhE) [41] [6], DNA purification kits | Quantitative detection of viable cells | Multiplexing 3 single-copy genes recommended for accurate quantification [41] [6] |
| Culture Media | LB broth [71], Artificial seawater [41] [6], Resuscitation buffer (PBS) [72] | Maintenance, stress induction, and resuscitation | LB medium may contain resuscitation factors for some species [72] |
| Antibiotic Neutralizers | Catalase [3], Pyruvate [3] | Counteract medium-derived stressors; improve resuscitability | Neutralizes H₂O₂ in media that prevents VBNC growth [3] |
Molecular Mechanisms and Signaling Pathways
Biochemical Pathways Governing Dormancy Transitions
Diagram 2: Molecular Regulation of Bacterial Dormancy
Key Molecular Insights from Experimental Studies
Recent research has elucidated critical molecular differences between VBNC and persister cells that explain their distinct positions along the dormancy continuum:
Energy Metabolism: Both persister and VBNC cells maintain basal ATP levels, but the allocation of this energy differs significantly. In VBNC E. coli, energy is directed toward repair of oxidative damage, which is critical for eventual resuscitation [16]. Persisters of Staphylococcus aureus similarly require ATP for their maintenance, with cellular ATP levels being a key determinant of persistence [73].
Intracellular pH Regulation: A striking difference emerges in pH homeostasis, where E. coli persisters exhibit a lower intracellular pH than both VBNC and susceptible cells even before antibiotic exposure [70]. This differential pH regulation is linked to tryptophanase (tnaA) activity and indole signaling, with ΔtnaA strains showing no pH differences between subpopulations [70].
Membrane Composition: Staphylococcus aureus cells surviving high antibiotic concentrations undergo significant membrane lipid modifications, with increased saturation of fatty acids and altered branched-chain ratios that affect membrane fluidity [69]. These changes are transmitted to daughter cells and are shared between persister and VBNC phenotypes, suggesting common adaptive mechanisms at the membrane level [69].
Oxidative Damage Repair: The ability to repair oxidative damage is a critical driver for VBNC cell resuscitation. Sub-lethal photocatalysis-induced VBNC E. coli demonstrate that repair of this damage, coupled with changes in energy allocation, provides the driving force for resuscitation [16].
The most clinically significant distinction between VBNC and persister cells lies in their resuscitation behaviors, which directly impact infection recurrence and treatment strategies:
Persister Resuscitation:
- Timing: Persister cells resuscitate rapidly upon antibiotic removal, with E. coli ampicillin persisters initiating growth within 1 hour after transfer to fresh media [71].
- Kinetics: Resuscitating persisters exhibit doubling times identical to normal cells (23.30 ± 2.54 minutes for E. coli), indicating immediate resumption of normal growth rates once the dormant state is exited [71].
- Synchronization: Flow cytometry analysis reveals that persister wake-up occurs in a synchronized manner regardless of pre-culture conditions or antibiotic exposure duration [71].
VBNC Resuscitation:
- Timing: VBNC cells require extended periods for resuscitation, with Acinetobacter baumannii demonstrating resuscitability for up to 10 months under high-salt conditions [72].
- Requirements: Successful VBNC resuscitation often requires specific signals or conditions beyond simple stress removal. For example, A. baumannii VBNC cells that could not be resuscitated in PBS or PBS with succinate were successfully revived in LB medium, indicating nutrient-specific resuscitation factors [72].
- Inhibition: Certain antibiotics like ciprofloxacin can inhibit VBNC cell recovery even after the primary stressor is removed, while still allowing maintenance of viability and metabolic functions like ethanol production in HiAlc K. pneumoniae [41] [6].
Novel approaches combining microfluidics, time-lapse microscopy, and fluorescent reporters have enabled unprecedented resolution in monitoring dormancy exits:
- Protein Dilution Method: By maintaining fluorescent protein expression during antibiotic treatment and monitoring dilution upon resuscitation, researchers can precisely track persister wake-up at single-cell resolution [71].
- Metabolic Activity Probes: Respiratory activity assays using CTC (5-cyano-2,3-ditolyl tetrazolium chloride) provide confirmation of viability in unculturable cells, with A. baumannii maintaining 34 ± 4.1% viability despite zero cultivability after 4 days post-stationary phase [72].
- Digital PCR Applications: PMA-ddPCR enables absolute quantification of resuscitating cells without standard curves, particularly valuable for tracking VBNC resuscitation dynamics in complex matrices like fecal samples [41] [6].
Research Implications and Future Directions
The positioning of VBNC and persister cells along a dormancy continuum rather than as discrete states has profound implications for antimicrobial development and clinical infection management. Research must account for the potential transition between these states and the heterogeneous nature of bacterial populations under stress.
Current evidence suggests that effective therapeutic strategies against dormant bacterial subpopulations may include:
- Metabolic Interventions: Targeting the specific energy metabolism and pH regulation mechanisms that distinguish persisters from normal cells [70] [73].
- Membrane-Active Compounds: Exploiting the modified membrane composition of both persister and VBNC cells to enhance antimicrobial penetration [69].
- Resuscitation Interference: Utilizing compounds like ciprofloxacin that inhibit VBNC recovery without affecting viability, potentially preventing resurgence of infections [41] [6].
- Combination Therapies: Pairing conventional antibiotics with anti-persister agents that target dormant cell maintenance mechanisms [68].
Future research should prioritize the development of standardized methodologies for discriminating between these dormant states in clinical samples, as current approaches remain predominantly restricted to research settings. The integration of single-cell analysis technologies with molecular detection methods offers promising avenues for both fundamental understanding and translational applications in combating persistent infections.
The viable but non-culturable (VBNC) state represents a unique survival strategy adopted by numerous bacterial pathogens when confronted with adverse environmental conditions. Cells in the VBNC state are characterized by a loss of culturability on routine microbiological media that would normally support their growth, while simultaneously maintaining metabolic activity and the potential to resuscitate under favorable conditions [8] [25]. This state is fundamentally different from bacterial persistence, as VBNC cells are defined by their non-culturability, whereas persister cells remain culturable despite being non-growing during antibiotic exposure [25]. The VBNC state can be induced by a wide array of stressors commonly encountered in medical, environmental, and food processing settings, including antibiotic pressure, nutrient starvation, temperature extremes, and osmotic stress [2].
The clinical significance of the VBNC state stems from two critical characteristics: these cells retain virulence and can cause infections upon resuscitation, and they exhibit markedly increased tolerance to antimicrobial agents, including antibiotics [2] [41]. This poses substantial challenges for clinical microbiology laboratories, which predominantly rely on culture-based methods for pathogen identification and antimicrobial susceptibility testing (AST). When bacteria enter the VBNC state, they become undetectable through conventional AST protocols, leading to underestimation of antibiotic tolerance and potential treatment failures [74] [3]. Understanding the quantitative changes in antibiotic susceptibility associated with the VBNC state is therefore essential for improving diagnostic approaches and therapeutic outcomes for persistent bacterial infections.
Methodological Approaches for Studying VBNC Antibiotic Susceptibility
Induction of the VBNC State and Viability Assessment
Research into the VBNC state requires specialized methodological approaches that differ significantly from conventional antimicrobial susceptibility testing. A key challenge lies in accurately inducing the VBNC state and distinguishing these cells from both dead cells and actively growing populations.
Table: Common Methods for VBNC Induction and Detection
| Method Category | Specific Technique | Application/Principle | Key Indicators |
|---|---|---|---|
| VBNC Induction | Long-term nutrient starvation | Incubation in artificial seawater or minimal media [41] | Loss of culturability while maintaining viability |
| Temperature stress | Shift to low temperatures (e.g., 4°C) [2] | Morphological changes (e.g., rod to cocci) | |
| Antibiotic exposure | Sub-lethal concentrations of macrolides [74] | Metabolic shutdown without cell death | |
| Viability Assessment | Membrane integrity staining | Live/Dead staining (SYTO-9/PI) [8] | Differentiates intact vs. compromised membranes |
| Metabolic activity probes | CTC reduction, ATP assays [2] [25] | Measures electron transport chain activity | |
| Molecular viability methods | PMA-qPCR/ddPCR [41] | Selectively amplifies DNA from cells with intact membranes |
The standard protocol for confirming VBNC state formation involves demonstrating a discrepancy between culturability and viability. Typically, cultures are considered to have entered the VBNC state when colony-forming units (CFUs) drop below the detection limit on routine media, while viability measurements (e.g., membrane integrity, metabolic activity) indicate that a significant portion of the population remains alive [25]. For example, in Mycobacterium avium, entry into the VBNC state is characterized by complete loss of culturability accompanied by a shift from Auramine-O positivity (indicating active metabolism) to Nile red positivity (indicating lipid accumulation) [74].
Advanced Detection and Quantification Methods
Traditional culture-based methods are insufficient for studying antibiotic susceptibility in VBNC cells, necessitating the development of alternative detection strategies:
Viability dyes with molecular methods: Propidium monoazide (PMA) and ethidium monoazide (EMA) selectively penetrate cells with compromised membranes and bind to DNA, preventing its amplification. When combined with qPCR or ddPCR, this approach allows quantification of viable cells regardless of culturability. PMA is generally preferred over EMA due to its lower cytotoxicity toward viable cells, reducing false-positive results [41]. Optimized PMA treatment protocols involve concentration testing (typically 5-200 μM) and incubation time optimization (5-30 minutes) followed by photoactivation [41].
Droplet digital PCR (ddPCR): This method provides absolute quantification of gene copy numbers without requiring standard curves, making it particularly valuable for detecting VBNC cells in complex samples like feces or clinical specimens. By targeting single-copy genes and combining with PMA treatment, ddPCR enables precise enumeration of VBNC populations [41].
Flow cytometry with functional stains: Techniques that measure membrane potential, respiratory activity, or enzyme function can distinguish VBNC cells from dead cells without relying on culturability [3] [8].
Resuscitation experiments: The definitive test for VBNC cells involves demonstrating the return to culturability following removal of the inducing stressor or application of resuscitation-promoting factors (RPFs) [74] [2]. For example, in Mycobacterium avium, addition of RPFs significantly increased the culturable population size during clarithromycin exposure and induced a shift from Nile red positivity back to auramine positivity, confirming the resuscitation of VBNC cells [74].
Quantitative Comparison of Antibiotic Susceptibility: VBNC vs Normal Cells
Minimum Inhibitory Concentration (MIC) Shifts in VBNC Populations
The antibiotic tolerance of VBNC cells is reflected in substantial changes in minimum inhibitory concentrations (MICs) compared to their culturable counterparts. However, quantifying these shifts presents methodological challenges, as standard MIC determination relies on bacterial growth inhibition—a parameter by definition absent in VBNC cells [75]. Researchers have therefore developed indirect approaches to assess the antibiotic susceptibility of VBNC populations.
Table: Documented MIC Shifts and Antibiotic Tolerance in VBNC Cells
| Bacterial Species | Antibiotic | Culturable Cells (MIC) | VBNC Cells (Apparent MIC) | Experimental Method | Reference |
|---|---|---|---|---|---|
| Mycobacterium avium | Clarithromycin | Susceptible (4 mg/L) | Highly tolerant | Time-kill kinetics with RPF resuscitation [74] | [74] |
| Klebsiella pneumoniae | Ciprofloxacin | Strain-dependent | Inhibited resuscitation | PMA-ddPCR quantification [41] | [41] |
| Escherichia coli | Various classes | Strain-dependent | Significantly increased | Resuscitation in animal models [2] | [2] |
In Mycobacterium avium, exposure to clarithromycin (at 2× MIC) steadily decreased the culturable population to below the detection limit, while stimulation with resuscitation-promoting factors (RPFs) significantly increased the size of the culturable population throughout antibiotic exposure [74]. This demonstrates that a substantial portion of the population entered a VBNC state tolerant to the antibiotic, rather than being eradicated. The tolerance mechanism involves a metabolic shutdown characterized by decreased respiratory rate and a switch to lipid accumulation, as evidenced by increased Nile red staining [74].
For high alcohol-producing K. pneumoniae, ciprofloxacin exposure inhibited the resuscitation of VBNC-state cells while maintaining their viability and ethanol production capability after antibiotic removal [41]. This indicates that the antibiotic effect on VBNC cells differs fundamentally from its effect on actively growing populations—rather than killing the cells, ciprofloxacin primarily prevents their resuscitation while leaving the dormant population intact.
Time-Kill Kinetics and Heterogeneous Responses
Time-kill curve analyses provide more comprehensive insights into antibiotic pharmacodynamics against VBNC populations compared to single-timepoint MIC determinations. These analyses often reveal bimodal or multimodal patterns indicating heterogeneous subpopulations with different susceptibility profiles [60]. Such heterogeneity is masked in traditional AST but becomes apparent when measuring bacterial responses over time in physiologically relevant media.
Advanced microfluidic platforms now enable single-cell analysis of antibiotic tolerance and VBNC state formation. These systems can capture both growth and killing kinetics while allowing medium exchange to assess regrowth potential after antibiotic removal—a key characteristic distinguishing persistent cells from VBNC cells [60]. Studies using these approaches have demonstrated substantial intercellular heterogeneity in bacterial responses to antibiotics in physiological fluids like urine, with patterns that differ significantly from those observed in standard laboratory media [60].
Diagram: Methodological Approaches for VBNC Susceptibility Testing. Conventional culture-based AST fails to detect VBNC cells, requiring specialized viability staining, molecular methods, and resuscitation experiments for proper characterization of their antibiotic susceptibility profiles.
Molecular Mechanisms Underlying Antibiotic Tolerance in VBNC Cells
Physiological and Metabolic Adaptations
The dramatically increased antibiotic tolerance of VBNC cells stems from comprehensive physiological restructuring that limits antibiotic uptake and target engagement:
Metabolic shutdown: VBNC cells exhibit severely reduced metabolic activity, decreasing the activity of essential metabolic pathways targeted by many antibiotics [74] [2]. For instance, transcriptomic studies of Mycobacterium avium exposed to macrolides revealed indications of respiratory shutdown and metabolic dormancy [74].
Membrane modifications: The cytoplasmic membranes of VBNC cells undergo extensive modifications to fatty acid composition, potentially reducing permeability to antibiotics [2]. These changes are accompanied by alterations in outer-membrane protein profiles and increased cross-linking in the cell wall peptidoglycan, creating additional barriers to antibiotic penetration [2].
Stress response activation: Entry into the VBNC state is regulated by stress response systems, including the RpoS regulon and toxin-antitoxin (TA) systems [3]. Under stress conditions, degradation of unstable antitoxins releases toxins that sharply decrease translation, replication, and cell growth, inducing persistence and potentially the VBNC state [3].
DNA protection: VBNC cells maintain DNA integrity and genetic material, including plasmids, allowing for potential resuscitation and expression of resistance genes when conditions improve [2].
The transition from VBNC back to actively growing states involves a gradual reversal of the physiological adaptations that confer antibiotic tolerance. Resuscitation-promoting factors (RPFs) play a key role in this process by stimulating metabolic reactivation [74]. In Mycobacterium avium, RPF addition during antibiotic exposure induced a shift from lipid-loaded (Nile red-positive) VBNC cells back to actively metabolizing (auramine-positive) cells, accompanied by restored susceptibility to clarithromycin [74].
The resuscitation process appears to follow a biphasic pattern, with an initial lag phase where cells remain non-culturable but undergo metabolic activation, followed by a rapid resuscitation phase where culturability is restored [25]. This transition represents a window of vulnerability to antibiotics, as resuscitating cells become metabolically active while still at low population densities. Strategic timing of antibiotic administration during this critical period may improve eradication of VBNC populations and reduce recurrence rates [74] [25].
Diagram: VBNC State Transition and Tolerance Mechanisms. Environmental stressors trigger multiple physiological adaptations that confer antibiotic tolerance, while resuscitation signals reverse these changes and restore antibiotic susceptibility.
The Scientist's Toolkit: Essential Reagents and Methods for VBNC Research
Table: Key Research Reagent Solutions for VBNC Studies
| Reagent/Method | Application in VBNC Research | Key Function | Technical Considerations |
|---|---|---|---|
| PMA (Propidium Monoazide) | Viability PCR | Distinguishes intact vs. compromised membranes by inhibiting DNA amplification from dead cells | Preferred over EMA due to lower cytotoxicity; requires concentration optimization (5-200 μM) [41] |
| Resuscitation-Promoting Factors (RPFs) | VBNC resuscitation | Stimulates metabolic reactivation and return to culturability | Culture filtrates from logarithmic phase M. tuberculosis can be used as RPF source [74] |
| Nile Red Stain | VBNC state identification | Detects lipid accumulation associated with VBNC state in mycobacteria | Increased staining indicates metabolic shift to lipid storage [74] |
| Auramine-O Stain | Metabolic activity assessment | Identifies actively metabolizing mycobacteria through acid-fast staining | Loss of staining indicates metabolic shutdown in VBNC state [74] |
| Droplet Digital PCR (ddPCR) | Absolute quantification | Precisely quantifies gene copies without standard curves; combined with PMA for viable cell counts | Targets single-copy genes (rpoB, adhE); provides direct quantification [41] |
| Microfluidic Gel Encapsulation | Single-cell analysis | Enables monitoring of heterogeneous responses to antibiotics at single-cell level | Facilitates medium exchange to assess regrowth after antibiotic removal [60] |
| Artificial Seawater (ASW) | VBNC induction | Standardized medium for inducing VBNC state through nutrient starvation | Contains 40 g/L sea salt; filter-sterilized [41] |
Research Implications and Future Directions
The documented shifts in antibiotic susceptibility between VBNC and normal cells have profound implications for clinical microbiology and antimicrobial drug development. Current AST methods, which form the basis for treatment decisions in clinical practice, systematically fail to detect VBNC populations, leading to underestimation of antibiotic tolerance and potential treatment failures [74] [3]. This is particularly problematic for chronic and recurrent infections caused by pathogens known to enter the VBNC state, including Mycobacterium avium complex, Escherichia coli, Klebsiella pneumoniae, and Vibrio cholerae [74] [2] [41].
Future research directions should focus on several critical areas:
Development of VBNC-inclusive diagnostic protocols that incorporate viability staining, molecular methods, or resuscitation steps to detect non-culturable populations in clinical specimens [41] [25].
Investigation of anti-VBNC antimicrobial agents that retain activity against dormant cells, potentially targeting maintenance metabolism or resuscitation pathways [74]. Clofazimine has been suggested as a candidate due to its action on the mycobacterial respiratory chain [74].
Standardization of VBNC terminology and research methodologies to improve comparability across studies and facilitate meta-analyses [25]. Clear differentiation between VBNC cells, persister cells, and other dormant states is essential for advancing the field.
Clinical correlation studies to establish the relationship between VBNC state formation and treatment outcomes in human infections, particularly for diseases with high recurrence rates despite appropriate antibiotic therapy [74] [2].
As recognition of the VBNC state's clinical significance grows, integrating VBNC-specific susceptibility testing into research and eventually clinical practice will be essential for addressing the persistent challenge of antibiotic-tolerant infections and improving patient outcomes.
The viable but nonculturable (VBNC) state is a unique survival strategy adopted by many bacteria in response to adverse environmental conditions [2] [11]. In this state, cells are metabolically active but cannot form colonies on routine microbiological media that would normally support their growth, rendering them undetectable through conventional culture-based methods [2] [25]. This phenomenon has profound implications for public health, food safety, and clinical medicine, as numerous human pathogens can enter this dormant state while retaining virulence potential [2] [20].
First proposed in 1982 by Xu and colleagues for Escherichia coli and Vibrio cholerae [11] [25], the VBNC state has since been identified in over 100 bacterial species, including significant pathogens such as Mycobacterium tuberculosis, Listeria monocytogenes, Salmonella spp., and Helicobacter pylori [2] [11]. The ability of these pathogens to evade detection while maintaining infectivity represents a critical challenge in infection control and environmental monitoring, necessitating advanced detection methods and revised safety protocols [13] [20].
Characteristics and Mechanisms of the VBNC State
Defining Features of VBNC Cells
Bacteria in the VBNC state exhibit distinct characteristics that differentiate them from both actively growing cells and dead cells. These features include maintenance of cell integrity, reduced metabolic activity, dwarfing (reduction in cell size), and extensive modifications to cellular components such as the cytoplasmic membrane and cell wall peptidoglycan [2] [20]. Importantly, VBNC cells maintain high ATP levels and membrane potential, retain plasmids, and continue gene expression, albeit at reduced rates compared to culturable cells [2] [25].
A key characteristic of VBNC cells is their increased resistance to various physical and chemical stresses, including antibiotics, extreme temperatures, chlorine, and other disinfectants [2] [20]. This enhanced resistance, combined with their nonculturability, creates a significant challenge for eradication in clinical and industrial settings.
The VBNC state can be induced by a wide range of environmental stresses, with the specific triggers varying among bacterial species. Common inducing factors include:
- Nutrient starvation [2] [11]
- Temperature extremes (both high and low) [2] [11]
- Osmotic stress and high salinity [2] [11]
- Sharp changes in pH [11]
- Oxidative stress [11]
- Chlorination and other disinfecting processes [2] [13]
- UV radiation and white light exposure [2] [11]
- Heavy metals and food preservatives [2] [11]
Table 1: Common Inducing Factors for the VBNC State in Bacterial Pathogens
| Inducing Factor | Example Pathogens Affected | Common Settings |
|---|---|---|
| Low temperature | Listeria monocytogenes, E. coli O157:H7 | Food refrigeration, cold water |
| Nutrient starvation | Vibrio cholerae, Shigella dysenteriae | Oligotrophic waters, processed foods |
| Chlorination | Listeria monocytogenes, Salmonella enterica | Water treatment, food processing wash water |
| Osmotic stress | Staphylococcus aureus, Klebsiella pneumoniae | High-salt foods, marine environments |
| Extreme pH | E. coli O157:H7, Salmonella typhimurium | Acidic fruit juices, fermented foods |
Resuscitation from the VBNC state occurs when favorable conditions are restored, often requiring specific stimuli that differ from the original culturing conditions [25]. For many pathogens, passage through an appropriate host organism serves as a resuscitation signal [2]. For example, VBNC cells of Vibrio cholerae and enteropathogenic E. coli have been shown to regain culturability after passage through intestinal tracts of animals [2]. The molecular mechanisms underlying both induction and resuscitation are complex and involve significant reprogramming of gene expression and metabolic pathways [2] [20].
Detection Challenges and Methodological Approaches
Limitations of Conventional Culture Methods
Traditional microbiology relies heavily on culture-based methods for detecting and enumerating bacteria. These methods are fundamentally inadequate for VBNC cells, as these organisms do not form colonies on standard media despite maintaining viability and metabolic activity [2] [25]. This limitation leads to substantial underestimation of viable bacterial populations in environmental, food, and clinical samples, creating a false sense of security when tests return "negative" results [20].
The discrepancy between direct counts and culturable counts was one of the earliest indicators of the VBNC state [2]. In natural environments, it is now recognized that less than 1% of microorganisms can be cultured using standard laboratory techniques [2], suggesting that the VBNC state may be the norm rather than the exception for many bacterial species in their natural habitats.
Advanced Detection Methodologies
Given the limitations of culture-based methods, researchers have developed alternative approaches for detecting VBNC cells. These methods typically rely on demonstrating viability through measures of metabolic activity, membrane integrity, or genetic integrity while confirming nonculturability.
Table 2: Comparison of VBNC Detection Methods
| Method | Principle | Advantages | Limitations |
|---|---|---|---|
| Direct Viable Count (DVC) | Microscopic enumeration after incubation with nutrients and DNA synthesis inhibitors | Distinguishes viable cells based on growth potential | May not detect all VBNC cells; requires microscopic expertise |
| Flow Cytometry with Vital Stains | Discrimination based on membrane integrity using fluorescent dyes (SYTO-9, PI) | Rapid, high-throughput capability | May overestimate dead cells in complex matrices; cannot distinguish culturable from VBNC |
| Viability qPCR (v-qPCR) | Selective amplification from cells with intact membranes using PMA/EMA dyes | Specific detection of cells with intact membranes; applicable to complex samples | Requires optimization for different matrices; may not eliminate all dead cell signal |
| ATP Assays | Measurement of cellular ATP levels as indicator of metabolic activity | Highly sensitive; correlates with metabolic activity | May not detect cells with very low metabolic rates |
| Gene Expression Analysis | Detection of mRNA or specific protein production | Confirms ongoing transcriptional activity | Technically challenging; requires specialized expertise |
The viability quantitative polymerase chain reaction (v-qPCR) method, which combines DNA intercalating dyes like propidium monoazide (PMA) or ethidium monoazide (EMA) with PCR amplification, has shown particular promise for detecting VBNC cells in complex matrices [13]. This approach exploits the principle that dyes like PMA and EMA can only penetrate cells with compromised membranes, characteristic of dead cells. Once inside, these dyes bind to DNA and inhibit PCR amplification, allowing selective detection of DNA from viable cells with intact membranes [13].
A recent study optimized a v-qPCR protocol using a combination of EMA and PMAxx (an improved version of PMA) for detection of VBNC Listeria monocytogenes in process wash water from the fresh-cut produce industry [13]. The optimized method used concentrations of 10 μM EMA and 75 μM PMAxx, incubation at 40°C for 40 minutes, followed by a 15-minute light exposure to activate the dyes. This protocol effectively inhibited qPCR amplification from dead cells while allowing detection of VBNC cells [13].
Diagram 1: Comprehensive Workflow for VBNC Cell Detection. The diagram illustrates the multi-method approach required to confirm the VBNC state, relying on discrepancies between viability indicators and culturability.
VBNC Cells in Clinical Settings: Complicating Infection Control
Impact on Antimicrobial Susceptibility and Treatment Outcomes
The VBNC state significantly alters bacterial susceptibility to antimicrobial agents, creating substantial challenges for clinical management of infections. VBNC cells exhibit increased antibiotic resistance compared to their culturable counterparts, primarily due to their reduced metabolic activity and enhanced stress response mechanisms [2] [60]. This phenomenon has important implications for antimicrobial susceptibility testing (AST), as standard methods rely on detection of bacterial growth in the presence of antibiotics [60].
Recent studies using precision single-cell analysis have revealed substantial heterogeneity in bacterial responses to antimicrobial treatment, with subpopulations including VBNC cells and persister cells contributing to treatment failure and relapse [60]. For example, research on uropathogenic bacteria demonstrated that traditional AST conducted in nutrient-rich media like Mueller-Hinton II broth fails to accurately predict bacterial clearance from urine, where antimicrobial concentrations can be 100-1000 times higher than in serum [60].
The microfluidic gel encapsulation platform developed for single-cell analysis enables researchers to monitor both growth and killing kinetics at the single-cell level, as well as assess the ability of surviving cells to resume growth after antimicrobial removal [60]. This approach has revealed bimodal or multimodal time-kill curves that deviate from the simple decay expected from a uniform population, highlighting the presence of tolerant subpopulations including VBNC cells [60].
Persistent and Recurrent Infections
The ability to enter the VBNC state has been directly linked to persistent and recurrent bacterial infections. Several studies have demonstrated that VBNC cells can maintain virulence properties while evading antibiotic treatment and host immune responses [2] [25]. For instance, recurrent urinary tract infections have been associated with uropathogenic E. coli cells that remain in the VBNC state, demonstrating resistance to antibiotic treatment and causing reinfection [2].
Similarly, VBNC Helicobacter pylori cells have been shown to express virulence factors such as cagA, vacA, and vreA [2], potentially contributing to the chronic nature of H. pylori infections and their association with gastric ulcers and cancer. The persistence of these pathogens in the VBNC state represents a significant challenge for complete eradication and long-term cure.
Table 3: Clinical Implications of VBNC Pathogens in Human Infections
| Pathogen | Clinical Significance | VBNC-associated Challenges |
|---|---|---|
| Escherichia coli (UPEC) | Recurrent urinary tract infections | Antibiotic resistance; resuscitation in urinary tract |
| Mycobacterium tuberculosis | Chronic tuberculosis | Persistence despite multidrug therapy; latent infections |
| Helicobacter pylori | Chronic gastritis, peptic ulcers, gastric cancer | Virulence factor expression; treatment failure |
| Legionella pneumophila | Legionnaires' disease | Survival in water systems; aerosol transmission |
| Vibrio cholerae | Cholera outbreaks | Environmental persistence; resuscitation in human gut |
VBNC Cells in Water Systems: Challenges for Water Safety
Water Treatment and Distribution Systems
Water safety monitoring traditionally relies on culture-based methods to detect indicator organisms and pathogens, creating a critical blind spot for VBNC cells [2] [20]. Numerous studies have demonstrated that VBNC states can be induced by common water treatment processes, including chlorination [2] [13], potentially leading to underestimation of microbial risks in treated water.
Research has shown that chlorine exposure can induce the VBNC state in foodborne pathogens like Listeria monocytogenes and Salmonella enterica [13]. This finding has significant implications for water reuse in agricultural and food processing settings, where the presence of VBNC pathogens in process wash water may lead to cross-contamination of fresh produce [13]. The standard practice of maintaining chlorine residuals to control microbial growth may inadvertently select for VBNC cells that evade detection while maintaining pathogenicity.
Environmental Persistence and Public Health Risks
The ability to persist in water environments in the VBNC state has been documented for many waterborne pathogens, including Vibrio cholerae, Legionella pneumophila, and Shigella species [2]. These pathogens can remain viable for extended periods while nonculturable, then resuscitate when conditions become favorable or when they enter a susceptible host [2] [20].
For example, Vibrio cholerae O1 can persist in surface waters in the VBNC state, particularly in association with crustacean copepods [2]. When these water sources are used for domestic purposes, the bacteria can resuscitate in the human intestinal tract and cause cholera outbreaks [2]. Similarly, Shigella species can undergo the VBNC state in water but regain culturalbility and pathogenicity upon entering the human body [2].
These observations challenge the current paradigm of water safety assessment and necessitate the incorporation of VBNC detection methods into routine water quality monitoring protocols, particularly for source waters used for drinking water production and recreational activities.
Research Reagents and Methodological Toolkit
Advancing research on VBNC cells requires specialized reagents and methodologies designed to assess viability independent of culturability. The following toolkit represents essential resources for investigating the VBNC state in human pathogens.
Table 4: Essential Research Reagent Solutions for VBNC Studies
| Reagent Category | Specific Examples | Function in VBNC Research |
|---|---|---|
| Viability Stains | SYTO-9, Propidium Iodide (PI), CTC, DAPI | Differentiation between live and dead cells based on membrane integrity and metabolic activity |
| DNA Binding Dyes | PMA, PMAxx, EMA | Selective inhibition of PCR amplification from dead cells with compromised membranes |
| Metabolic Indicators | 5-cyano-2,3-ditolyl tetrazolium chloride (CTC), INT | Detection of respiratory activity in viable cells |
| Culture Media Supplements | Resuscitation-promoting factors, catalase, sodium pyruvate | Enhancement of bacterial recovery from VBNC state |
| Microfluidic Systems | Gel encapsulation platforms, single-cell analysis chips | Monitoring heterogeneity in bacterial responses to stress at single-cell level |
| Molecular Biology Reagents | RNA protection buffers, reverse transcriptase, PCR reagents | Analysis of gene expression in nonculturable cells |
The integration of these reagents into standardized protocols is essential for generating comparable data across different laboratories and bacterial species. Particularly important is the combination of multiple methods to confirm the VBNC state, as no single approach can definitively distinguish VBNC cells from other physiological states [25] [13].
The VBNC state represents a significant and underestimated challenge in clinical medicine and environmental safety. The ability of bacterial pathogens to evade detection by conventional methods while maintaining virulence potential has profound implications for infection control, water safety, and public health protection. Addressing this challenge requires a paradigm shift from culture-based detection toward molecular and functional methods that can recognize viable but nonculturable cells.
Future directions in VBNC research should focus on standardizing detection methods, elucidating the genetic and metabolic mechanisms underlying VBNC induction and resuscitation, and developing novel intervention strategies that specifically target VBNC cells. Furthermore, integration of VBNC assessment into routine clinical and environmental monitoring protocols will provide a more accurate picture of microbial risks and enable more effective prevention and control measures.
As research in this field continues to evolve, it is becoming increasingly clear that a comprehensive understanding of bacterial pathogenesis and persistence must account for the VBNC state and its contributions to chronic infections, antimicrobial treatment failure, and the silent dissemination of pathogens through water and food systems.
Conclusion
The VBNC state represents a profound challenge to modern medicine, facilitating bacterial survival against antibiotic treatments and contributing to the global AMR crisis. This review synthesizes evidence that VBNC cells are not merely culturable failures but represent a distinct, highly protected physiological state governed by specific genetic and metabolic programs. Their extreme antibiotic tolerance, driven by dormancy and comprehensive stress responses, renders conventional antibiotics, which target active cellular processes, largely ineffective. The inability of standard diagnostic methods to detect these cells creates a dangerous diagnostic gap, leading to underestimated risks in clinical and environmental settings. Future research must prioritize the development of innovative therapeutic agents that either prevent entry into the VBNC state, actively kill dormant cells, or safely trigger resuscitation to re-sensitize bacteria to existing antibiotics. For the drug development community, overcoming the VBNC defense mechanism is not just an academic pursuit but a critical frontier in the ongoing battle against antimicrobial resistance.
References
- 1. Viable but nonculturable [https://en.wikipedia.org/wiki/Viable_but_nonculturable]
- 2. Viable but Nonculturable Bacteria: Food Safety and Public ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC3804398/]
- 3. How to Evaluate Non-Growing Cells—Current Strategies ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC7912045/]
- 4. Characterization and potential mechanisms of highly ... [https://www.nature.com/articles/s41598-020-58106-3]
- 5. Rapid Detection and Fast Induction of Viable but ... [https://www.sciencedirect.com/science/article/pii/S0362028X25001759]
- 6. Absolute quantification of VBNC state formation and ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12535994/]
- 7. Detection of Viable but Nonculturable E. coli Induced by ... [https://www.sciencedirect.com/science/article/pii/S0362028X2400214X]
- 8. Viable but Nonculturable - an overview [https://www.sciencedirect.com/topics/immunology-and-microbiology/viable-but-nonculturable]
- 9. Global Proteomic Analysis of the Resuscitation State of Vibrio... [https://pmc.ncbi.nlm.nih.gov/articles/PMC6517545/]
- 10. Study on the Viable but Non-culturable (VBNC) State ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC7726111/]
- 11. Overview of VBNC, a survival strategy for microorganisms [https://pmc.ncbi.nlm.nih.gov/articles/PMC9526772/]
- 12. Relationship between the Viable but Nonculturable State and ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC6153661/]
- 13. Detection and Quantification Methods for Viable but Non ... [https://www.frontiersin.org/journals/microbiology/articles/10.3389/fmicb.2020.00673/full]
- 14. Bridging the gap between viable but non-culturable and ... [https://www.sciencedirect.com/science/article/abs/pii/S0966842X14001954]
- 15. Detection and Quantification of Viable but Non-culturable ... [https://www.frontiersin.org/journals/microbiology/articles/10.3389/fmicb.2019.02920/full]
- 16. Regulatory formation of VBNC state antibiotic-resistant ... [https://www.sciencedirect.com/science/article/abs/pii/S0304389425029607]
- 17. Absolute Quantification of Viable but Nonculturable Vibrio ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC9430983/]
- 18. Regulatory formation of VBNC state antibiotic-resistant ... [https://pubmed.ncbi.nlm.nih.gov/41046676/]
- 19. Current Perspectives on Viable but Non-Culturable (VBNC) ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC4116801/]
- 20. The importance of the viable but non-culturable state in ... [https://www.frontiersin.org/journals/microbiology/articles/10.3389/fmicb.2014.00258/full]
- 21. Physiological Characterization of Viable-but-Nonculturable ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC91151/]
- 22. The effects and cell phenotype changes in Escherichia coli ... [https://www.sciencedirect.com/science/article/abs/pii/S2212429224007314]
- 23. Population and single cell metabolic activity of UV-induced ... [https://www.sciencedirect.com/science/article/pii/S0160412019307998]
- 24. Viable but non-cultivable state in oral microbiota [https://pmc.ncbi.nlm.nih.gov/articles/PMC11959090/]
- 25. Viable but nonculturable (VBNC) state, an underestimated ... [https://www.sciencedirect.com/science/article/abs/pii/S0966842X23001476]
- 26. Wake Up! Resuscitation of Viable but Nonculturable Bacteria [https://pmc.ncbi.nlm.nih.gov/articles/PMC9818539/]
- 27. Viable but non-cultivable state in oral microbiota [https://www.frontiersin.org/journals/cellular-and-infection-microbiology/articles/10.3389/fcimb.2025.1533768/full]
- 28. Regulatory formation of VBNC state antibiotic-resistant ... [https://www.sciencedirect.com/science/article/pii/S0304389425029607]
- 29. A novel mathematical model for studying antimicrobial ... [https://www.sciencedirect.com/science/article/abs/pii/S0740002025000206]
- 30. Recent Methods for the Viability Assessment of Bacterial ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC9500772/]
- 31. Detection and Potential Virulence of Viable but Non- ... [https://www.mdpi.com/2076-2607/9/1/194]
- 32. Detection and quantification of viable but non-culturable ... [https://www.frontiersin.org/journals/microbiology/articles/10.3389/fmicb.2023.1094877/full]
- 33. Insights into the enumeration of mixtures of probiotic bacteria ... [https://bmcmicrobiol.biomedcentral.com/articles/10.1186/s12866-023-02792-2]
- 34. Detection and Quantification Methods for Viable but Non- ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC7214806/]
- 35. Flow cytometry study of Escherichia coli treated with ... [https://www.frontiersin.org/journals/microbiology/articles/10.3389/fmicb.2025.1592471/full]
- 36. BestProtocols: Viability Staining Protocol for Flow Cytometry [https://www.thermofisher.com/us/en/home/references/protocols/cell-and-tissue-analysis/protocols/viability-staining-flow-cytometry.html]
- 37. Comparison of transcriptional activity profiling by metabolic ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12342705/]
- 38. Commentary: a review of technical considerations for ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12522984/]
- 39. The impact of PCR duplication on RNAseq data generated ... [https://genomebiology.biomedcentral.com/articles/10.1186/s13059-025-03613-7]
- 40. Antimicrobial Resistance of Dormant Bacterial Cells [https://www.mdpi.com/journal/antibiotics/special_issues/Bacterial_Cells]
- 41. Absolute quantification of VBNC state formation and ... [https://www.frontiersin.org/journals/cellular-and-infection-microbiology/articles/10.3389/fcimb.2025.1627943/full]
- 42. An Experimental Framework for Quantifying Bacterial ... [https://pubmed.ncbi.nlm.nih.gov/28636922/]
- 43. Characterization and potential mechanisms of highly antibiotic ... [https://www.nature.com/articles/s41598-020-58106-3?error=cookies_not_supported&code=1c49b194-0cf5-43f4-8078-5e7b05f31e7c]
- 44. Unraveling CRP/cAMP-mediated metabolic regulation in Escherichia... [https://elifesciences.org/articles/99735]
- 45. Cronobacter sakazakii survives in macrophages by resisting... VBNC [https://bmcmicrobiol.biomedcentral.com/articles/10.1186/s12866-024-03595-9]
- 46. Toxin–antitoxin systems: Classification, biological roles, ... [https://www.sciencedirect.com/science/article/pii/S0944501322001999]
- 47. Wake me when it's over - Bacterial toxin-antitoxin proteins and ... [https://pubmed.ncbi.nlm.nih.gov/27216598/]
- 48. Wake me when it's over – Bacterial toxin–antitoxin proteins ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC4909563/]
- 49. Toxin–antitoxins and sigma factors may optimize the fitness of ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12440627/]
- 50. Toxin–antitoxin systems and their role in disseminating and ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC5812544/]
- 51. Viable but non-culturable state formation and resuscitation ... [https://www.sciencedirect.com/science/article/abs/pii/S0043135424009114]
- 52. Type I toxin-antitoxin systems contribute to the ... [https://www.nature.com/articles/s42003-020-01448-5]
- 53. Transcriptome analysis and prediction of the metabolic ... [https://www.nature.com/articles/s41598-022-21102-w]
- 54. Transcriptomic Analysis of Viable but Non-Culturable ... [https://www.mdpi.com/2076-2607/7/12/634]
- 55. Osmotic and cold stress-induced viable but non-culturable ... [https://www.sciencedirect.com/science/article/abs/pii/S0958694625000470]
- 56. Analysis of stress response in multiple bacterial pathogens ... [https://www.nature.com/articles/s41598-025-91269-5]
- 57. Transcriptomic analysis of Lacticaseibacillus paracasei ... [https://www.frontiersin.org/journals/microbiology/articles/10.3389/fmicb.2023.1280350/full]
- 58. Stressed bacteria develop antibiotic resistance more easily [https://sciencenews.dk/en/stressed-bacteria-develop-antibiotic-resistance-more-easily]
- 59. Functional Interrelationships between Cell Membrane ... - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC1196293/]
- 60. Precision single cell analysis to characterize host dependent ... [https://pubs.rsc.org/en/content/articlehtml/2025/lc/d4lc00765d]
- 61. Engineering membrane and cell-wall programs for ... [https://www.sciencedirect.com/science/article/abs/pii/S1369527416300856]
- 62. The importance of the viable but non-culturable state in ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC4040921/]
- 63. Mechanisms of Antibiotic Resistance - PMC - PubMed Central [https://pmc.ncbi.nlm.nih.gov/articles/PMC4888801/]
- 64. Viable but non-culturable state formation and resuscitation ... [https://pubmed.ncbi.nlm.nih.gov/38959654/]
- 65. Genetics of Antimicrobial Resistance - NCBI - NIH [https://www.ncbi.nlm.nih.gov/books/NBK216503/]
- 66. Transfer of antibiotic resistance [https://www.reactgroup.org/toolbox/understand/antibiotic-resistance/transfer-of-antibiotic-resistance/]
- 67. Quantification and antibiotic resistance risk assessment of ... [https://www.sciencedirect.com/science/article/abs/pii/S0048969723007556]
- 68. Bacterial persisters: molecular mechanisms and ... [https://www.nature.com/articles/s41392-024-01866-5]
- 69. Phenotypic Modifications in Staphylococcus aureus Cells ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC4724715/]
- 70. Escherichia coli Persister Have a Lower Intracellular pH than... Cells [https://pmc.ncbi.nlm.nih.gov/articles/PMC8406257/]
- 71. Flow-cytometry analysis reveals persister resuscitation characteristics [https://bmcmicrobiol.biomedcentral.com/articles/10.1186/s12866-020-01888-3]
- 72. a fundamental survival strategy of Acinetobacter baumannii [https://pmc.ncbi.nlm.nih.gov/articles/PMC10653857/]
- 73. Isolation and characterization of persisters of the ... [https://www.sciencedirect.com/science/article/pii/S2589004224012276]
- 74. A viable but nonculturable state of Mycobacterium avium in ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12574950/]
- 75. Overview of Quantitative Methodologies to Understand ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC7459578/]