Unrecognized Human Bacterial Pathogens: Detection Challenges and Innovative Therapeutic Strategies
This article addresses the critical and growing challenge of unrecognized and drug-resistant bacterial pathogens, a pressing concern for global public health.
Unrecognized Human Bacterial Pathogens: Detection Challenges and Innovative Therapeutic Strategies
Abstract
This article addresses the critical and growing challenge of unrecognized and drug-resistant bacterial pathogens, a pressing concern for global public health. It explores the foundational science behind their emergence, including the alarming rise of 'nightmare bacteria' like NDM-producing strains. The scope extends to advanced methodological approaches for pathogen identification, such as metagenomic next-generation sequencing (mNGS) and the Tm mapping method. It further investigates the significant hurdles in developing novel therapeutics against these pathogens, analyzing the dwindling antibiotic pipeline and the promise of targeted strategies like narrow-spectrum agents and drug repurposing. Finally, the article provides a comparative validation of emerging diagnostic technologies against traditional culture, offering a comprehensive resource for researchers and drug development professionals navigating this complex field.
The Rising Tide of Stealth Pathogens: Understanding the Scale and Mechanisms of Resistance
The escalating crisis of antimicrobial resistance (AMR) represents a quintessential silent pandemic, undermining decades of progress in infectious disease control. AMR is projected to cause 10 million deaths annually by 2050 if left unaddressed, posing a severe threat to global health and modern medicine [1]. This technical brief examines the convergence of two critical fronts in this battle: the rapid emergence of pan-resistant "nightmare bacteria" and the elusive reservoir of asymptomatic human carriers who facilitate their spread. Within the context of unrecognized human bacterial pathogens research, this dynamic creates a perfect storm for stealth transmission, challenging conventional detection paradigms and therapeutic development. The intricate interplay between bacterial evolution, host-pathogen interactions, and diagnostic limitations necessitates a fundamental re-evaluation of our approaches to pathogen surveillance and containment.
The Expanding Spectrum of Resistant Pathogens
Quantitative Landscape of Resistance
Surveillance data reveal an alarming acceleration in resistance mechanisms, particularly among Gram-negative pathogens. The Centers for Disease Control and Prevention (CDC) reports that infection rates from drug-resistant "nightmare bacteria" rose almost 70% between 2019 and 2023 [2]. The rate of infections caused by bacteria carrying the New Delhi metallo-β-lactamase (NDM) gene, which confers resistance to nearly all beta-lactam antibiotics including carbapenems, rose more than fivefold (460%) during this period [2]. This is particularly concerning as NDM-carrying pathogens are susceptible to only two remaining antibiotics, both of which are expensive and require intravenous administration [2].
Table 1: Emerging High-Priority Resistant Pathogens and Their Mechanisms
| Pathogen | Resistance Mechanism | Key Genetic Determinants | Therapeutic Implications |
|---|---|---|---|
| Klebsiella pneumoniae | Carbapenem resistance | blaKPC, blaNDM, blaOXA-48 | Limited to aminoglycosides, tigecycline, fosfomycin, colistin |
| Acinetobacter baumannii | Multi-drug resistance | OXA-type carbapenemases, efflux pumps, porin mutations | Polymyxins remain last resort |
| Pseudomonas aeruginosa | Efflux pumps, enzymatic degradation | MexAB-OprM, blaCTX-M, blaVIM | Compounded resistance challenges in immunocompromised |
| Escherichia coli | Extended-spectrum β-lactamases (ESBL) | blaCTX-M, blaTEM, blaSHV | Rising resistance to fluoroquinolones |
| Staphylococcus aureus (MRSA) | Altered drug target | mecA (PBP2a) | Resistance to all β-lactams |
The molecular mechanisms driving this crisis are diverse and continuously evolving. Traditional resistance pathways include three dominant strategies: (1) target site modification (e.g., PBP2a in MRSA), (2) enzymatic degradation (e.g., β-lactamases), and (3) reduced drug accumulation via efflux pumps or membrane permeability barriers [1]. The horizontal gene transfer of resistance determinants via plasmids, transposons, and integrons further accelerates the dissemination of these traits across microbial populations [1].
The Carrier Conundrum in Disease Transmission
Asymptomatic carriers—individuals who host pathogenic organisms without displaying clinical symptoms—represent a critical blind spot in AMR containment. Mathematical models indicate that the presence of asymptomatic carriers significantly complicates disease control by undermining interventions that rely on identifying symptomatic cases [3]. For pathogens like Staphylococcus aureus and Streptococcus pneumoniae, carriers can unknowingly transmit resistant strains while remaining undetected by conventional surveillance systems [3].
The epidemiological significance of asymptomatic carriage is profound. Current models suggest that interventions targeting only symptomatically infected hosts while ignoring asymptomatic carriers are often incapable of achieving disease control, even when multiple intervention strategies are implemented simultaneously [3]. This is particularly relevant for AMR, where asymptomatic carriage may exert selective pressure that contributes to the emergence and transmission of drug-resistant strains when carriers are unknowingly treated with antibiotics [3].
Table 2: Documentated Prevalence of Asymptomatic Carriage for Key Pathogens
| Pathogen | Carriage Prevalence | Population Context | Implications for AMR Spread |
|---|---|---|---|
| Neisseria meningitidis | 10-35% | Young adults | Approaching 100% in closed populations |
| Influenza virus | 5-35% | General population | Pre-symptomatic transmission undermines control |
| Salmonella enterica ser. Typhi | 1-6% | Post-infection | Chronic carriage (exemplified by "Typhoid Mary") |
| Ebola virus | 27-71% | During outbreaks | Significant proportion never develop symptoms |
| Clostridioides difficile | >50% | Long-term care patients | Extended fecal contamination despite lack of symptoms |
Diagnostic Challenges and Methodological Advances
Limitations of Conventional Detection Paradigms
Traditional culture-based methods for bacterial identification, while inexpensive and conceptually simple, require 2-3 days for preliminary identification and more than a week for species confirmation [4]. These approaches suffer from critical limitations in sensitivity, particularly for detecting viable but non-culturable (VBNC) pathogens that may lead to false-negative results [4]. Furthermore, standard biochemical tests often fail to distinguish between closely related species with dramatically different pathogenic profiles and resistance patterns [5] [6].
The clinical implications of these diagnostic shortcomings are substantial. In cases where Escherichia marmotae is mistaken for E. coli, for instance, inappropriate broad-spectrum antibiotic therapy may be administered, exerting unnecessary selective pressure for resistance development [6]. Such misidentification underscores the critical need for species-specific diagnostic methods that can guide targeted therapeutic interventions.
Advanced Molecular Detection Platforms
Nucleic acid-based detection methods have emerged as powerful alternatives to conventional culture-based techniques. These platforms offer superior sensitivity, specificity, and rapid turnaround times, enabling pathogen-directed therapy within clinically relevant timeframes [4].
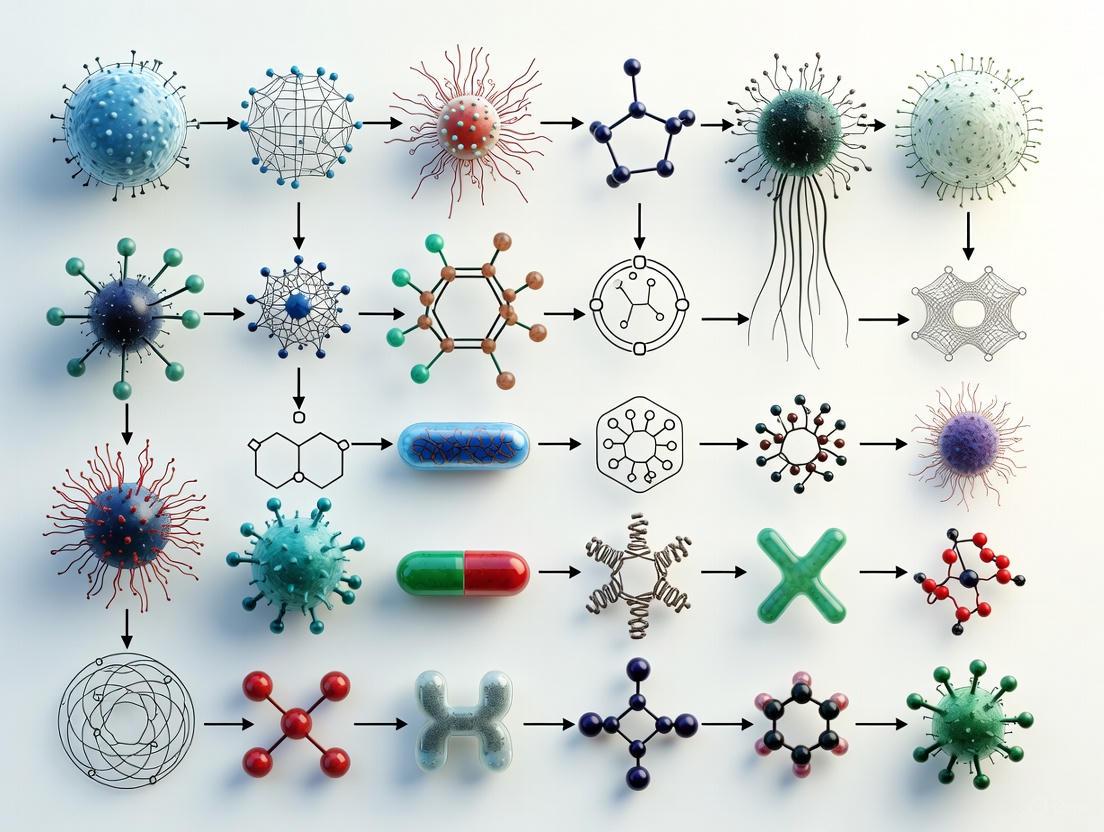
Diagram 1: Molecular Detection Workflow
Polymerase chain reaction (PCR) and its variants form the cornerstone of modern molecular detection. Simple PCR allows detection of a single bacterial pathogen by amplifying a specific target DNA sequence, while multiplex PCR (mPCR) enables simultaneous amplification of multiple gene targets, offering a more comprehensive approach to pathogen identification [4]. Real-time PCR (qPCR) provides both detection and quantification of target organisms, making it particularly valuable for surveillance applications [7].
Isothermal amplification techniques such as loop-mediated isothermal amplification (LAMP) and nucleic acid sequence-based amplification (NASBA) offer advantages in resource-limited settings by eliminating the need for thermal cyclers [4]. For complex samples containing multiple potential pathogens, oligonucleotide DNA microarrays facilitate high-throughput screening of numerous genetic targets simultaneously [4].
Novel Surveillance Approaches and Emerging Platforms
Innovative surveillance strategies are leveraging molecular techniques to monitor resistance spread. The CDC's Active Bacterial Core surveillance (ABCs) program employs laboratory- and population-based surveillance to monitor invasive bacterial infections that cause bloodstream infections, sepsis, and meningitis [8]. This system provides critical data on emerging resistance patterns and informs vaccine and public health policies.
Recent research has identified novel bacterial immune systems that may inspire future diagnostic platforms. The Panoptes system, discovered in bacteria, operates by sensing viral interference with cellular signals and launching a counterattack [9]. This sophisticated mechanism for detecting pathogen intrusion demonstrates the potential for borrowing biological recognition elements from natural systems to develop novel detection technologies.
The Scientist's Toolkit: Essential Research Reagents and Methodologies
Core Reagent Solutions for AMR Research
Table 3: Essential Research Reagents for Antimicrobial Resistance Studies
| Reagent/Category | Specific Examples | Research Application | Technical Function |
|---|---|---|---|
| Chromogenic/Fluorogenic Enzyme Substrates | Nitrocefin, X-Gluc, FDG | Detection of β-lactamase activity; bacterial enumeration | Visual detection of specific enzyme activities via color/fluorescence change |
| PCR Reagents | Specific primers (e.g., for mecA, blaNDM), dNTPs, thermostable DNA polymerase | Molecular detection of resistance genes | Amplification of specific DNA sequences for pathogen identification |
| Culture Media | Selective agars (e.g., CHROMagar, MRSA Select) | Isolation and presumptive identification of resistant pathogens | Support growth of target organisms while inhibiting competitors; color-based differentiation |
| Antibiotic Test Panels | Broth microdilution panels, Etest strips | Determination of minimum inhibitory concentrations (MICs) | Quantitative assessment of antibiotic susceptibility |
| Whole Genome Sequencing Kits | Library preparation reagents, sequencing adapters | Comprehensive analysis of resistance genes and mobile genetic elements | High-resolution characterization of resistance determinants |
Experimental Protocol: Molecular Detection of NDM-Producing Enterobacteriaceae
Principle: This protocol describes a real-time PCR (qPCR) method for detecting the blaNDM gene in clinical isolates or directly from surveillance samples, enabling rapid identification of carbapenem-resistant organisms.
Sample Preparation:
- For bacterial isolates: Inoculate 3-5 colonies into 200μL of nuclease-free water and heat at 95°C for 10 minutes. Centrifuge at 12,000 × g for 2 minutes, and use supernatant as template.
- For direct specimen testing: Extract nucleic acids using a commercial kit with optional DNase treatment if RNA detection is required.
qPCR Reaction Setup:
- Prepare master mix containing:
- 10μL of 2× qPCR master mix
- 1μL of forward primer (10μM): 5'-GGGCAGTCGCTTCCAACGGT-3'
- 1μL of reverse primer (10μM): 5'-GTAGTGCTCAGTGTCGGCAT-3'
- 0.5μL of probe (10μM): 5'-[FAM]ACTCGCAAGACTGCTACCC-[BHQ1]-3'
- 2.5μL of nuclease-free water
- Add 5μL of template DNA to 15μL of master mix
- Include positive control (plasmid with blaNDM insert) and negative control (nuclease-free water)
Amplification Parameters:
- Initial denaturation: 95°C for 3 minutes
- 40 cycles of:
- Denaturation: 95°C for 15 seconds
- Annealing/Extension: 60°C for 60 seconds (collect fluorescence)
- Analysis: Determine Cq values with threshold set in exponential phase of amplification
Interpretation: Cq values ≤35 indicate presence of blaNDM gene. Confirm positive results with melting curve analysis if using SYBR Green chemistry.
Conceptual Framework for Pathogen Emergence and Detection
The complex interplay between bacterial evolution, transmission dynamics, and detection capabilities can be visualized as a cyclical process that drives the silent spread of resistant pathogens.
Diagram 2: AMR Transmission Cycle
This framework illustrates how diagnostic limitations perpetuate a cycle of resistance amplification. Asymptomatic carriers facilitate silent transmission, while diagnostic gaps enable continued spread until treatment failures trigger recognition of the problem. Each iteration of this cycle expands the reservoir of resistant organisms and further complicates containment efforts.
The convergence of expanding resistance mechanisms and widespread asymptomatic carriage represents a critical challenge in microbial pathogenesis research. The silent transmission of resistant pathogens through unrecognized carriers underscores the urgent need for innovative detection technologies that can identify both the pathogens and their resistance determinants within clinically relevant timeframes.
Future research directions must include the development of point-of-care diagnostic platforms that integrate multiplexed detection of pathogens and their resistance profiles, enabling targeted therapy while minimizing unnecessary antibiotic exposure. Furthermore, a deeper understanding of the host-pathogen interactions that permit asymptomatic carriage may reveal novel therapeutic targets for disrupting transmission networks.
The escalating threat of nightmare bacteria necessitates a paradigm shift in our approach to resistance containment—from reactive treatment to proactive detection and interruption of transmission chains. By leveraging advanced molecular technologies and embracing comprehensive surveillance strategies, the scientific community can mount a more effective defense against this invisible pandemic.
The relentless evolution of antimicrobial resistance (AMR) represents one of the most pressing challenges in modern medicine, particularly with the emergence and global spread of carbapenem-resistant Enterobacterales (CRE). Among these, New Delhi metallo-β-lactamase-producing CRE (NDM-CRE) constitutes a critical threat due to their extensive resistance profiles and association with severe morbidity and mortality. Recent epidemiological data from the United States Centers for Disease Control and Prevention (CDC) reveals a disturbing trend: between 2019 and 2023, NDM-CRE infections surged by approximately 460% in the United States [10] [11] [12]. This unprecedented increase has transformed NDM-CRE from a historically uncommon pathogen in the U.S. into a predominant clinical concern, with incidence rates now comparable to the previously dominant Klebsiella pneumoniae carbapenemase (KPC) variants [13].
This whitepaper contextualizes the dramatic rise of NDM-CRE within the broader framework of unrecognized human bacterial pathogens research. We present a comprehensive technical analysis of the epidemiological landscape, molecular mechanisms of resistance, detection methodologies, and therapeutic challenges associated with NDM-CRE. The objective is to provide researchers, scientists, and drug development professionals with an integrated resource that bridges surveillance data with experimental and clinical insights, ultimately guiding future research priorities and intervention strategies against these formidable pathogens.
Epidemiological Landscape: Quantifying the Surge
Data compiled through the CDC's Antimicrobial Resistance Laboratory Network from 2019 to 2023 demonstrates a sharp upward trajectory in carbapenemase-producing CRE (CP-CRE), primarily fueled by the rise of NDM-producing strains. The following table summarizes the key quantitative findings from the recent CDC report published in the Annals of Internal Medicine [10] [13].
Table 1: Trends in Carbapenem-Resistant Enterobacterales in the United States (2019-2023)
| Metric | 2019-2023 Change | Key Statistics & Notes |
|---|---|---|
| Overall CP-CRE Incidence | Increased by 69% | Age-adjusted incidence rate ratio (aIRR) = 1.69 (95% CI, 1.61-1.78) [13]. |
| NDM-CRE Incidence | Increased by ~460% | Age-adjusted incidence rate ratio (aIRR) = 5.61 (95% CI, 4.96-6.36). This was the steepest increase among all carbapenemases [13]. |
| OXA-48-like-CRE Incidence | Increased by 5% | Age-adjusted incidence rate ratio (aIRR) = 1.5 (95% CI, 1.17-1.94) [13]. |
| KPC-CRE Incidence | Not specified in data | By 2023, NDM-CRE incidence became similar to KPC-CRE, previously the most common type in the U.S. [13]. |
| Historical Burden (2020) | ~12,700 CRE infections, ~1,100 deaths | From CDC's 2022 special report, provided for context on overall CRE impact [10] [14]. |
| Common NDM-CRE Infections | Pneumonia, bloodstream, urinary tract, wound infections | Infections are extremely difficult to treat and associated with high morbidity and mortality [10]. |
This surveillance data, representing 35% of the U.S. population, likely underestimates the true burden due to the absence of several high-population states and incomplete carbapenemase testing in many clinical laboratories [11] [13]. The rise of NDM-CRE is not isolated to the U.S.; it is part of a global phenomenon. A 2025 study by the Global Antibiotic Research & Development Partnership (GARDP) highlighted critical treatment gaps in low- and middle-income countries (LMICs), where only 6.9% of patients with drug-resistant Gram-negative infections received appropriate antibiotics [15].
The Pathogen: Biochemical and Genetic Mechanisms of NDM-CRE
Classification and Enzyme Function
NDM (New Delhi metallo-β-lactamase) is a transferable molecular class B metallo-β-lactamase (MβL). Unlike class A, C, and D β-lactamases that utilize a serine residue in their active site, class B enzymes are zinc-dependent metalloenzymes [16] [17]. The "metallo-" designation refers to the requirement for one or two zinc ions (Zn²⁺) in the active site to hydrolyze the β-lactam ring [16]. The gene encoding the most common variant, blaNDM-1, was first identified in 2008 in a Klebsiella pneumoniae isolate from a Swedish patient previously hospitalized in New Delhi, India [17].
NDM enzymes confer resistance by efficiently hydrolyzing a broad spectrum of β-lactam antibiotics. Their activity profile encompasses:
- Penicillins
- Cephalosporins
- Carbapenems (meropenem, imipenem, ertapenem)
Notably, NDM enzymes are not active against the monobactam aztreonam [17]. However, this intrinsic susceptibility is often negated in clinical isolates because NDM-producing organisms frequently co-harbor other resistance mechanisms, such as extended-spectrum β-lactamases (ESBLs), which hydrolyze aztreonam [16] [18].
Genetic Architecture and Horizontal Transfer
The rapid global dissemination of NDM is largely facilitated by its location on mobile genetic elements, particularly plasmids [16] [18] [17]. The blaNDM gene is often embedded within a complex genetic environment flanked by insertion sequences (IS), such as ISAba125, which contribute to its mobilization and expression [17] [19].
Table 2: Key Genetic and Biochemical Features of NDM Carbapenemases
| Feature | Description |
|---|---|
| Ambler Class | Class B (Metallo-β-lactamase, MβL) [16] [17]. |
| Active Site | Zinc-dependent hydrolase (subclasses B1/B3: two Zn²⁺ ions; B2: one Zn²⁺ ion) [16]. |
| Genetic Location | Plasmid-borne, facilitating horizontal gene transfer [18] [17]. |
| Common Flanking Elements | Insertion sequences (e.g., ISAba125, IS5, IS26) [17] [19]. |
| Primary Hydrolysis Spectrum | Penicillins, Cephalosporins, Carbapenems [17]. |
| Notable Exception | No hydrolysis of Aztreonam (a monobactam) [17]. |
| Inhibitor Susceptibility | Resistant to all commercially available β-lactamase inhibitors (e.g., clavulanic acid, avibactam) [16] [17]. |
This genetic mobility allows blaNDM to spread not only among clinical strains of K. pneumoniae and E. coli but also across other members of the Enterobacterales order, and even into environmental bacteria, creating vast reservoirs of resistance [17] [19].
The following diagram illustrates the core genetic structure surrounding the blaNDM gene and its role in the primary resistance mechanism.
Detection and Diagnostic Challenges
A critical factor contributing to the silent spread of NDM-CRE is the widespread lack of routine carbapenemase testing in clinical laboratories [10] [11]. Many labs confirm carbapenem resistance but do not perform specific tests to identify the presence of a carbapenemase, much less differentiate its type. This diagnostic gap has significant clinical consequences:
- Delayed Targeted Therapy: Without knowing the carbapenemase type (e.g., NDM vs. KPC), clinicians may select initially ineffective antibiotics [10].
- Missed Opportunities for Infection Control: Failure to rapidly identify NDM-CRE carriers impedes the timely implementation of contact precautions to prevent transmission [10] [14].
Recommended Testing Methodologies
The CDC urges prompt carbapenemase testing whenever a CRE infection is identified [10]. The following table outlines key methods used in identification and their applications in both research and clinical settings.
Table 3: Diagnostic and Research Methods for NDM-CRE Detection
| Method Category | Examples & Specific Techniques | Primary Application & Function |
|---|---|---|
| Phenotypic Detection | CARBA NP test (colorimetric) [16].mSuperCARBA agar (chromogenic) [19].Antibiotic Susceptibility Testing (AST) with MIC determination [19]. | Rapid, functional confirmation of carbapenemase production.Screening and selective isolation of presumptive CP-CRE from complex samples (e.g., wastewater, clinical specimens). |
| Genotypic Detection | PCR for major carbapenemase genes (e.g., blaNDM, blaKPC, blaVIM, blaOXA-48) [19].Whole-Genome Sequencing (WGS) (e.g., PacBio, Illumina) [19]. | Gold-standard for identifying specific carbapenemase genes.Comprehensive analysis of resistance genes, plasmid structures, virulence factors, and strain typing (MLST). |
| Public Health Support | Testing through public health laboratories (e.g., CDC's Antimicrobial Resistance Laboratory Network) [10]. | Confirmatory testing and surveillance when clinical labs lack capacity. |
The experimental workflow for the surveillance and characterization of NDM-CRE, as used in research settings, is summarized below. This workflow integrates both phenotypic and genotypic methods to fully understand the pathogen's properties and spread.
The Scientist's Toolkit: Essential Research Reagents and Materials
Research into NDM-CRE relies on a suite of specialized reagents and tools to isolate, identify, and characterize these pathogens. The following table details key materials essential for experimental work in this field.
Table 4: Key Research Reagent Solutions for NDM-CRE Investigation
| Research Reagent / Material | Function & Application in NDM-CRE Research |
|---|---|
| Chromogenic Agar (e.g., mSuperCARBA) | Selective isolation of presumptive carbapenemase-producing organisms from complex samples like clinical specimens or wastewater. Contains chromogenic substrates that produce colored colonies upon enzyme activity [19]. |
| Cation-Adjusted Mueller-Hinton Broth (CAMHB) | The standard medium for performing antibiotic susceptibility testing (AST), including minimum inhibitory concentration (MIC) determinations, following CLSI guidelines [19]. |
| PCR Reagents & Primers | Specific primers for carbapenemase genes (blaNDM, blaKPC, blaVIM, blaOXA-48) are used for rapid genotypic screening and confirmation [19]. |
| Whole-Genome Sequencing Kits | Reagents for next-generation sequencing platforms (e.g., PacBio, Illumina) enable comprehensive genomic analysis, including strain typing, plasmid epidemiology, and resistance gene detection [19]. |
| Antibiotic Disks/Powders | Standardized antibiotics for AST and MIC testing are crucial for defining resistance profiles and evaluating the efficacy of new therapeutic compounds [19]. |
Therapeutic Landscape and Future Directions
The treatment of NDM-CRE infections is severely constrained because NDM enzymes are not inhibited by any currently marketed β-lactamase inhibitors [16]. While ceftazidime-avibactam is effective against class A KPC enzymes, it is inactive against class B metallo-β-lactamases like NDM [16] [18]. This leaves clinicians with a limited arsenal, often relying on older, more toxic antibiotics such as polymyxins (e.g., colistin), tigecycline, and fosfomycin [18] [17]. However, efficacy is variable, and these agents often fail in serious infections like bacteremia and pneumonia [18].
The pipeline for novel agents active against NDM is a critical area of development. Promising strategies include:
- Novel β-Lactamase Inhibitors: Compounds like xeruborbactam (a bicyclic boronate) are in clinical development and show promise as pan-β-lactamase inhibitors, including activity against NDM and other metallo-β-lactamases [16].
- Siderophore-Antibiotic Conjugates: These constructs, such as cefiderocol, exploit bacterial iron uptake systems to enhance antibiotic penetration into the cell, showing activity against some NDM-producing strains [16] [18].
- Combination Therapies: Rational combinations of existing antibiotics, sometimes including aztreonam to exploit the "Achilles' heel" of NDM, are being explored to overcome resistance [18] [17].
Beyond drug development, strengthening infection prevention and control (IPC) measures in healthcare settings is paramount to curbing the spread of NDM-CRE. The CDC emphasizes consistent hand hygiene, wearing gloves and gowns during patient care (Contact Precautions), and rigorous environmental cleaning and disinfection [10] [13]. Furthermore, enhancing surveillance and diagnostic capacity to enable rapid detection and implementation of these precautions is a foundational component of any public health response to this growing threat [10] [11].
The 460% surge in NDM-CRE infections over a mere four-year period is a stark warning of the rapid evolution and dissemination of unrecognized bacterial pathogens. This whitepaper has delineated the multifaceted nature of the NDM-CRE threat, integrating quantitative epidemiology, molecular genetics, diagnostic challenges, and therapeutic limitations. The rise of NDM-CRE underscores the critical importance of a "One Health" approach, recognizing the interconnectedness of human health, animal health, and the environment in the spread of resistance genes [16] [19].
For the research community, the path forward demands a concerted effort on several fronts: (1) the development and deployment of rapid, accessible diagnostic tests to distinguish carbapenemase types; (2) accelerated discovery of novel therapeutic agents, particularly broad-spectrum β-lactamase inhibitors effective against metallo-enzymes; and (3) enhanced genomic surveillance to track the evolution and spread of high-risk NDM-CRE clones and plasmids. Addressing the NDM-CRE crisis requires a synergistic effort between basic researchers, clinical scientists, public health agencies, and drug developers to prevent a regression to the pre-antibiotic era for an increasing number of patients.
The relentless evolution of antimicrobial resistance (AMR) represents one of the most pressing challenges to modern medicine and public health. Within the broader context of unrecognized human bacterial pathogens research, understanding the drivers of resistance is paramount for developing effective countermeasures. The World Health Organization identifies bacterial AMR as directly responsible for 1.27 million global deaths annually and a contributing factor to 4.95 million deaths, underscoring the scale of this crisis [20]. The complex interplay between antibiotic misuse, horizontal gene transfer mechanisms, and disruptive global events like the COVID-19 pandemic has accelerated the emergence and dissemination of resistant pathogens. This whitepaper provides a technical examination of these core drivers, offering researchers and drug development professionals a comprehensive analysis of the mechanisms, transmission pathways, and methodologies essential for combating AMR. The pandemic undid years of progress, with U.S. hospitals witnessing significant increases in healthcare-associated, antimicrobial-resistant infections [21]. As we explore the molecular machinery of resistance dissemination and the quantitative assessment of antimicrobial use, this review aims to equip the scientific community with the knowledge and tools necessary to address this escalating threat through enhanced surveillance, stewardship, and innovative research approaches.
Antibiotic Misuse and Selective Pressure
Mechanisms of Antimicrobial Action and Resistance
Antimicrobial agents target essential bacterial cellular processes through distinct mechanisms of action, which corresponding resistance mechanisms have evolved to counteract. Table 1 summarizes the primary antibiotic classes, their cellular targets, and the resistance strategies employed by bacterial pathogens.
Table 1: Antimicrobial Mechanisms of Action and Corresponding Bacterial Resistance Strategies
| Mechanism of Action | Antimicrobial Classes | Primary Resistance Mechanisms | Example Pathogens with Intrinsic Resistance |
|---|---|---|---|
| Inhibit Cell Wall Synthesis | β-Lactams, Carbapenems, Cephalosporins, Penicillins, Glycopeptides | Drug inactivation (e.g., β-lactamases), Target modification, Reduced permeability | Enterococci (cephalosporins), Listeria monocytogenes (cephalosporins) [22] |
| Depolarize Cell Membrane | Lipopeptides | Membrane modification, Efflux pumps | All Gram-negative bacteria (lipopeptides) [22] |
| Inhibit Protein Synthesis | Aminoglycosides, Tetracyclines, Macrolides, Chloramphenicol | rRNA methylation, Efflux pumps, Enzymatic modification | Bacteroides spp. (aminoglycosides), E. coli (macrolides) [22] |
| Inhibit Nucleic Acid Synthesis | Quinolones, Fluoroquinolones | Target mutations (gyrase, topoisomerase), Efflux pumps | Serratia marcescens (macrolides) [22] |
| Inhibit Metabolic Pathways | Sulfonamides, Trimethoprim | Bypass pathways, Target enzyme mutations | Pseudomonas aeruginosa (sulfonamides) [22] |
The improper stewardship of antimicrobial agents, including increased consumption in humans and animals, along with inappropriate prescribing practices, has created selective pressure that favors resistant organisms [22]. Patients with the highest exposure to antimicrobials are at greatest risk for infection with drug-resistant bacteria, creating a vicious cycle of escalating resistance [22].
Quantitative Evaluation of Antimicrobial Use
Accurate assessment of antimicrobial use patterns is fundamental to antimicrobial stewardship programs (ASPs). Quantitative evaluation employs standardized metrics to measure the volume and frequency of antimicrobial consumption, enabling correlation with resistance development and assessment of intervention effectiveness [23].
Table 2: Core Metrics for Quantitative Evaluation of Antimicrobial Use
| Metric | Definition | Calculation Method | Advantages | Limitations |
|---|---|---|---|---|
| Defined Daily Dose (DDD) | The average maintenance daily dose for adults using a specific antimicrobial for its primary indication [23] | (Total antimicrobial weight in grams) / (Standard DDD value) | Easy data collection (no patient-specific data needed), Applicable to children | Not applicable to pediatric populations, Inaccurate with renal impairment or combination therapy |
| Days of Therapy (DOT) | The sum of the number of days each patient receives antimicrobial therapy, regardless of dose [23] | Count of days each antimicrobial agent was administered to a patient | More intuitive than DDD, Better reflects actual exposure | Requires patient-specific data, Labor-intensive to collect |
| Standardized Antimicrobial Administration Ratio (SAAR) | A risk-adjusted benchmark comparing observed versus predicted antimicrobial use [23] | Complex statistical modeling based on patient demographics and facility factors | Allows comparison between facilities, Adjusts for case mix | Requires sophisticated data infrastructure and analysis |
The WHO Access, Watch, and Reserve (AWaRe) classification system further supports antimicrobial use evaluation by categorizing drugs based on their potential to develop resistance. "Access" group antibiotics feature narrow spectra and good safety profiles, "Watch" agents have broader spectra and higher resistance potential, while "Reserve" antibiotics are last-resort options for multidrug-resistant infections [23].
Horizontal Gene Transfer: The Molecular Architecture of Resistance Dissemination
Mechanisms of Genetic Exchange
Horizontal gene transfer (HGT) enables bacteria to acquire resistance genes from phylogenetically distinct species, dramatically accelerating the spread of AMR beyond vertical inheritance. The three primary HGT mechanisms operate through distinct molecular pathways with characteristic components and efficiencies.
Conjugation represents the most efficient and clinically significant mechanism for disseminating antibiotic resistance genes among bacteria [24]. This contact-dependent process involves the direct transfer of mobile genetic elements (primarily plasmids) through a specialized conjugation pilus or pore formation between adjacent cells [24]. The molecular machinery typically includes an origin-of-transfer sequence (oriT), relaxase enzyme, and type IV secretion system components that mediate DNA processing and transport. Recent research demonstrates that some plasmids require "helper" plasmids to provide the necessary conjugation machinery in trans [25]. Notably, conjugation occurs at substantial rates even in the absence of antibiotic selective pressure, facilitated by certain non-antibiotic pharmaceuticals like ibuprofen and propranolol through reactive oxygen species generation [25].
Transformation involves the uptake and genomic integration of extracellular DNA from lysed donor bacteria by naturally competent recipient cells [24]. Pathogens such as Neisseria gonorrhoeae, Vibrio cholerae, and Streptococcus pneumoniae efficiently acquire resistance determinants through this mechanism [24]. The process requires a state of genetic competence, typically regulated by quorum-sensing systems, and expression of DNA-binding and transport proteins. Evidence suggests that even traditionally non-competent bacteria like Escherichia coli may undergo natural transformation in specific environments such as the gut [24].
Transduction utilizes bacteriophages as vectors to transfer chromosomal or extrachromosomal DNA between bacterial cells [24]. During the lytic cycle, phage particles occasionally package host DNA instead of viral genomes, creating transducing particles that inject this DNA into subsequent hosts. Generalized transduction can transfer any bacterial gene, while specialized transduction moves specific genomic regions. This mechanism is particularly relevant in Staphylococcus aureus, where phages mediate the transfer of the methicillin resistance gene (mecA) [24]. Recent mouse model studies confirm that transduction significantly contributes to genetic diversity and resistance emergence in gut-colonizing E. coli [24].
Other transfer mechanisms include membrane vesicles (MVs), which are 20-400 nm particles secreted by Gram-negative bacteria that can package and deliver antibiotic resistance genes [24]. Studies confirm that Acinetobacter baumannii and E. coli can transfer β-lactamase genes through MVs [24].
Diagram 1: Pathways of Horizontal Gene Transfer in Bacteria. This diagram illustrates the four primary mechanisms (conjugation, transformation, transduction, and membrane vesicle transfer) by which antibiotic resistance genes disseminate between bacteria, highlighting the genetic materials and specialized structures required for each process.
In Vivo Models for Studying HGT
While traditional knowledge of HGT derives from in vitro studies, recent research emphasizes the critical importance of in vivo models that better mimic realistic conditions in human and animal hosts [24]. The mammalian gastrointestinal tract provides a particularly efficient environment for HGT due to high bacterial density, nutrient availability, and complex microbial community interactions.
Experimental studies using mouse models have demonstrated the transfer of broad host-range plasmids like P3 from Salmonella enterica serovar Typhimurium to diverse recipient bacteria belonging to the Gammaproteobacteria class, including human gut commensals [25]. This transfer occurred efficiently even without antibiotic selective pressure, highlighting the concerning potential for resistance dissemination in natural environments [25]. The "plasmid paradox" – why bacteria maintain and transfer plasmids without apparent selective advantage – remains an active research area, with hypotheses including unknown fitness benefits or "selfish DNA" behavior [25].
Methodologically, these in vivo studies involve infecting mice with recipient bacterial species followed by donor strains 24 hours later, then monitoring bacterial populations and plasmid transfer frequencies through fecal analysis over several days [25]. Such approaches provide invaluable insights into the dynamics of resistance gene spread in realistic biological contexts, enabling more accurate risk assessment and intervention development.
Research Reagents and Methodologies
Table 3: Essential Research Reagents for Studying Horizontal Gene Transfer
| Reagent/Category | Specific Examples | Research Application | Key Function in HGT Studies |
|---|---|---|---|
| Model Plasmids | P3 (streptomycin/sulfonamide resistance), RP4 (broad-host-range), pRSF1010 | Conjugation efficiency, Host range studies | Tracking mobilization, Helper plasmid requirements, Fitness costs [25] |
| Bacterial Strains | Salmonella enterica SL1344, Escherichia coli MG1655, Acinetobacter baumannii | Donor/recipient systems, Persister cell studies | Demonstrating intra-species and inter-genera transfer, Environmental persistence [25] |
| Animal Models | Mouse gastrointestinal model, Galleria mellonella infection model | In vivo HGT dynamics, Host-pathogen interactions | Simulating human infection environments, Studying transfer in realistic conditions [24] [25] |
| Selection Agents | Streptomycin, Sulfonamides, Carbapenems, β-lactam/β-lactamase inhibitor combinations | Selective plating, Competition assays | Quantifying transfer frequencies, Monitoring plasmid stability and persistence [25] |
| Molecular Tools | PCR primers for resistance genes, Sequencing platforms, Fluorescent reporter tags | Detection and quantification, Molecular characterization | Tracking specific resistance elements, Visualizing transfer events, Phylogenetic analysis [24] |
The Impact of the COVID-19 Pandemic on AMR
Pandemic-Related Setbacks in Antimicrobial Resistance Control
The COVID-19 pandemic fundamentally disrupted global healthcare systems and inadvertently reversed years of progress in combating AMR. According to CDC reports, the United States lost significant ground in controlling antimicrobial resistance during 2020, with nearly 40% of the estimated 29,400 deaths from antimicrobial-resistant infections being healthcare-acquired [21]. The diversion of resources toward pandemic response created ideal conditions for resistant pathogens to flourish unchecked.
Table 4 summarizes the profound impacts of the pandemic on AMR epidemiology and control efforts across healthcare settings.
Table 4: Documented Impacts of the COVID-19 Pandemic on Antimicrobial Resistance
| Impact Category | Specific Findings | Magnitude of Change | Primary Contributing Factors |
|---|---|---|---|
| Healthcare-Associated Infections | Resistant hospital-onset infections and deaths | ≥15% increase (2019-2020) [21] | Sicker patients, prolonged device use, staffing shortages, PPE challenges |
| Antifungal Resistance | Candida auris infections | 60% overall increase (2020) [21] | Enhanced transmission in COVID-19 units, strained infection control |
| Carbapenem-Resistant Organisms | NDM gene-mediated infections | 460% increase (2019-2023) [2] [26] | Antibiotic overuse in COVID-19, decreased stewardship oversight |
| Gram-Negative Resistance | ESBL, CRE, MDR Pseudomonas/Acinetobacter | Incidence rate ratio: 1.64 (95% CI: 0.92-2.92) [27] | High antibiotic prescribing despite low bacterial co-infection rates |
| Antibiotic Prescribing | Inpatient COVID-19 management | ~80% of hospitalized patients received antibiotics (2020) [21] [27] | Diagnostic uncertainty, concern for bacterial co-infections |
A comprehensive meta-analysis of 28 studies found that the pandemic likely hastened the emergence and transmission of AMR, particularly for Gram-negative organisms in hospital settings [27]. Although the changes were not always statistically significant in pooled analyses, the consistent direction of effect across diverse healthcare environments confirms a genuine worsening of the AMR landscape attributable to pandemic-related disruptions.
Mechanisms of Pandemic-Driven Resistance Acceleration
Several interconnected mechanisms drove the alarming escalation of AMR during the COVID-19 pandemic:
Inappropriate Antibiotic Use: Despite the viral etiology of COVID-19, antibiotics were prescribed to nearly 80% of hospitalized patients during the initial pandemic waves [21] [27]. This reflected initial diagnostic challenges in distinguishing COVID-19 pneumonia from community-acquired bacterial pneumonia, coupled with concerns about bacterial co-infections. Ceftriaxone and azithromycin were the most frequently prescribed agents, with azithromycin use in nursing homes reaching 150% higher in April 2020 compared to the same month in 2019 [21].
Compromised Infection Prevention and Control: Overwhelmed healthcare systems experienced critical shortages of personal protective equipment, increased patient-to-staff ratios, and reduced capacity for maintaining standard infection control protocols [21] [27]. Outbreak investigations identified numerous instances of antimicrobial-resistant pathogen transmission within COVID-19 units, with CDC and public health partners responding to more than 20 such outbreaks in specialized treatment units [21].
Diverted Public Health Resources: Antimicrobial stewardship programs were deprioritized as clinical staff were redeployed to COVID-19 response duties [21]. Simultaneously, public health personnel were diverted from AMR surveillance and containment activities, creating significant data gaps, with the CDC's Antimicrobial Resistance Laboratory Network receiving and testing 23% fewer specimens in 2020 compared to 2019 [21]. This surveillance breakdown allowed community transmission of resistant organisms to proceed undetected.
Methodologies for Tracking and Predicting AMR Evolution
Experimental Workflow for AMR Surveillance
Systematic monitoring of antimicrobial resistance patterns requires standardized methodologies for data collection, analysis, and interpretation. The following workflow represents best practices for comprehensive AMR surveillance:
Diagram 2: AMR Surveillance and Prediction Workflow. This comprehensive workflow outlines the sequential steps from sample collection through data analysis that enables systematic monitoring of resistance patterns and informed intervention strategies.
Predictive Modeling of Resistance Evolution
The emerging field of evolutionary prediction applies quantitative, systems-based approaches to forecast AMR development. These models integrate multiscale data from microbial evolution experiments to quantify both evolutionary predictability (the existence of a probability distribution of outcomes) and evolutionary repeatability (the likelihood of specific events occurring) [28].
Key considerations for predictive modeling include:
Fundamental Limitations: Evolutionary prediction faces inherent constraints from random mutations, genetic drift, and epistatic interactions that create nonlinear fitness landscapes [28]. The characteristic timescale for prediction (τe) represents the practical horizon beyond which forecasts become unreliable due to accumulating stochasticity and model errors [28].
Promising Approaches: Despite challenges, successful prediction of resistance mutations has been demonstrated in both yeast and bacterial systems. Metabolic fitness landscapes have proven valuable for predicting antibiotic resistance, while in silico mutational scanning has anticipated SARS-CoV-2 antiviral resistance mutations [28]. These approaches leverage high-replicate evolution experiments coupled with whole-genome sequencing to map genotype-phenotype relationships.
Stochastic Population Dynamics: Advanced modeling incorporates resource competition between nongenetically resistant and genetically resistant subpopulations, revealing that nongenetic resistance facilitates survival but paradoxically slows the evolution of genetic resistance [28]. Such insights refine our understanding of resistance trajectories and inform combination therapy strategies.
The integration of quantitative systems biology with real-time surveillance data offers the most promising path toward predictive management of the AMR crisis, potentially enabling preemptive interventions before resistance becomes established in clinical settings.
The convergence of antibiotic misuse, efficient horizontal gene transfer mechanisms, and the disruptive impact of the COVID-19 pandemic has created a perfect storm that continues to accelerate the global antimicrobial resistance crisis. The intricate molecular machinery of plasmid-mediated conjugation, even in the absence of antibiotic selection pressure, underscores the formidable challenge containment presents. Quantitative assessment of antimicrobial use patterns through DDD and DOT metrics provides essential surveillance data, while in vivo models reveal the startling efficiency of resistance gene dissemination in biological environments. The pandemic-related setbacks demonstrate the fragility of previous progress and underscore the need for resilient stewardship programs that can withstand healthcare disruptions. Moving forward, integrating quantitative systems biology approaches with enhanced surveillance methodologies offers the most promising path toward predicting and preempting resistance evolution. For researchers and drug development professionals focused on unrecognized human bacterial pathogens, these insights highlight the critical importance of developing novel antimicrobials that circumvent existing resistance mechanisms while implementing robust infection control practices to limit dissemination. Only through a comprehensive understanding of these interconnected drivers can we hope to mitigate the escalating threat of antimicrobial resistance to global health security.
The paradigm of human bacterial pathogens has shifted dramatically over the past half-century. Since the 1950s, the medical community has faced a continuous emergence of bacterial pathogens, now recognized as a major microbiologic public health threat [29]. These pathogens transcend traditional clinical boundaries, spreading through community and environmental routes while demonstrating a remarkable capacity to establish chronic, persistent infections that evade standard diagnostic and therapeutic interventions. This whitepaper examines the dual threats of community transmission and chronic bacterial infections within the broader context of unrecognized human bacterial pathogens research, addressing critical gaps in our understanding of their epidemiology, pathogenic mechanisms, and detection methodologies.
The emergence of novel bacterial species and more virulent strains of known species represents a significant challenge. Between 1973 and 2010, at least 26 major emerging and reemerging bacterial pathogens have been identified, with most originating either from animal reservoirs (zoonoses) or water sources [29]. This trend continues unabated, complicated by factors including development of new diagnostic tools, increased human exposure due to sociodemographic and environmental changes, and the emergence of more virulent bacterial strains particularly affecting immunocompromised populations [29].
Mechanisms of Community Spread and Persistence
Zoonotic and Environmental Transmission Pathways
Community spread of bacterial pathogens occurs primarily through zoonotic transmission and environmental contamination. Analysis of major emerging bacterial diseases reveals that a significant majority have animal origins or persist in water systems, creating resilient reservoirs that facilitate ongoing human exposure [29]. These transmission pathways enable pathogens to bypass conventional clinical containment measures.
Table: Major Emerging Bacterial Pathogens (1973-2010) and Their Transmission Routes
| Year Emerged | Bacterial Species | Primary Disease Association | Transmission Route |
|---|---|---|---|
| 1973 | Campylobacter spp. | Diarrhea | Zoonosis (poultry, cattle) |
| 1976 | Legionella pneumophila | Lung infection | Water (amoebae) |
| 1982 | Borrelia burgdorferi | Lyme disease | Zoonosis (ticks) |
| 1982 | Escherichia coli O157:H7 | Hemorrhagic colitis | Zoonosis (contaminated food) |
| 1987 | Ehrlichia chaffeensis | Human ehrlichiosis | Zoonosis (ticks) |
| 1992 | Bartonella henselae | Cat-scratch disease | Zoonosis (cats) |
| 2010 | Neoehrlichia mikurensis | Systemic inflammatory response | Zoonosis (ticks) |
Molecular Mechanisms of Chronic Persistence
The establishment of chronic bacterial infections involves sophisticated adaptive mechanisms that allow pathogens to evade host immune responses and antimicrobial treatments. Research on infection-associated chronic illnesses (IACCIs) has revealed multiple persistence mechanisms, including:
- Immune evasion through antigenic variation: Pathogens alter surface proteins to avoid immune recognition.
- Intracellular sequestration: Bacteria establish protected niches within host cells.
- Biofilm formation: Microbial communities encased in extracellular matrix provide physical protection.
- Metabolic dormancy: Reduced metabolic activity decreases antibiotic susceptibility.
Animal model studies of Lyme disease demonstrate that Borrelia burgdorferi can persist following conventional single antibiotic treatments, with combination therapies proving more effective in clearing infection [30]. This suggests that bacterial persistence, rather than continued immune stimulation, may underlie some chronic manifestations.
Diagnostic Challenges and Advanced Detection Methodologies
Limitations of Conventional Diagnostic Approaches
Traditional culture-based methods for bacterial identification and quantification face significant limitations in detecting emerging and chronic pathogens. These methods are inherently slow, with growth times ranging from approximately 1 day for Listeria monocytogenes to 30-50 days for Mycobacterium avium subsp. paratuberculosis [31]. This diagnostic delay critically impacts patient outcomes, particularly in sepsis where appropriate antibiotic administration within hours significantly reduces mortality [32]. Furthermore, standard biomarkers of sepsis such as procalcitonin, presepsin, and C-reactive protein reflect the host's immune response rather than direct pathogen presence, inevitably causing a time-lag that impedes accurate severity assessment [32].
Advanced Molecular Detection and Quantification Platforms
Novel molecular approaches have emerged to address the limitations of conventional diagnostics, enabling rapid identification and quantification of unknown pathogenic bacteria directly from clinical samples.
Digital PCR for Pathogen Quantification
Digital PCR (dPCR) represents a significant advancement over quantitative PCR (qPCR) for pathogen quantification. Unlike qPCR, which requires calibration curves with known standards, dPCR is based on sample partitioning so that individual nucleic acid molecules undergo end-point PCR amplification in separate partitions. Target concentration is then estimated through Poisson distribution analysis [31]. This approach demonstrates greater robustness and reduced sensitivity to PCR inhibitors compared to qPCR [31].
Comparative studies evaluating dPCR and qPCR for quantifying bacterial pathogens (Listeria monocytogenes, Francisella tularensis, and Mycobacterium avium subsp. paratuberculosis) found that while both dPCR systems tested (QX200 and QuantStudio 3D) quantified similar bacterial amounts, qPCR showed both over- and under-estimation compared to dPCR [31]. The maximum difference among PCR approaches was <0.5 Log10, while cultural methods underestimated the number of bacteria by one to two Log10 for Francisella tularensis and Mycobacterium avium subsp. paratuberculosis [31].
Tm Mapping Method for Rapid Identification
The Tm mapping method enables rapid identification and quantification of unknown pathogenic bacteria within four hours of blood collection [32]. This innovative approach combines nested PCR using seven bacterial universal primer sets with melting temperature (Tm) analysis to create species-specific Tm mapping shapes compared against an established database.
The methodology employs a eukaryote-made thermostable DNA polymerase free from bacterial DNA contamination, eliminating false-positive results that plague conventional bacterial universal PCR [32]. For accurate quantification, the method incorporates a standard curve formed by Ct values of quantification standards (E. coli DNA) with known concentrations, with final bacterial concentrations corrected according to the 16S ribosomal RNA operon copy number of the identified pathogen [32].
Table: Research Reagent Solutions for Bacterial Pathogen Detection
| Research Reagent | Function/Application | Technical Considerations |
|---|---|---|
| Eukaryote-made thermostable DNA polymerase | Sensitive bacterial DNA amplification without bacterial DNA contamination | Manufactured using eukaryotic (yeast) host cells; eliminates false positives from reagent contamination [32] |
| Mixed 1st PCR forward primers | Accurate quantification regardless of bacterial species | Combines primers targeting minor sequence variations in 16S conserved region (1:1 ratio) [32] |
| Proteinase K with lysing beads | Maximize DNA extraction efficiency from bacterial cells | Maintains constant extraction efficiency across bacterial species; assists in lysing bacterial cell walls [32] |
| Bacterial universal primer sets (7 sets) | Broad-range detection of pathogenic bacteria | Targets highly conserved regions in bacterial 16S ribosomal RNA gene; enables detection of >100 bacterial species [32] |
| Quantification standards (E. coli DNA) | Absolute quantification reference | Precisely quantified by flow cytometry; enables standard curve generation for conversion of Ct values to bacterial counts [32] |
Tm Mapping Method Workflow for Bacterial Identification
Chronic Bacterial Infections and Host-Pathogen Interactions
Immune Dysregulation in Infection-Associated Chronic Illnesses
Chronic bacterial infections can trigger complex host-mediated responses that persist long after the initial infection. Infection-associated chronic conditions and illnesses (IACCIs) encompass various health consequences that occur after an acute infection, including organ damage, autoimmune conditions, and persistent systemic symptoms such as debilitating fatigue, postexertional malaise, cognitive impairment, and sleep disorders [33].
Research on long COVID and myalgic encephalitis/chronic fatigue syndrome (ME/CFS) reveals evidence for immune dysregulation and autoimmunity in infection-triggered chronic illnesses. Studies show correlation between autoantibody levels to the autonomic nervous system and symptom severity in patients with infection-triggered ME/CFS [30]. Approximately 50% of long COVID patients meet diagnostic criteria for ME/CFS, suggesting common mechanistic pathways [30].
Latent Viral Reactivation and Bacterial Coinfections
The role of latent viral reactivation in chronic bacterial illness manifestations represents an emerging research frontier. Evidence suggests that Epstein-Barr virus (EBV) reactivation is associated with long COVID development, with higher EBV titers correlating with more symptomatic phenotypes [30]. Interestingly, cytomegalovirus (EBV) seropositivity demonstrates a protective association, decreasing odds of developing long COVID [30]. This differential effect may stem from distinct immunoregulatory mechanisms employed by these herpesviruses.
Host-Pathogen Interactions in Chronic Infection Development
Research Implications and Future Directions
The growing recognition of chronic bacterial manifestations necessitates re-evaluation of therapeutic approaches. The limitations of single antibiotic regimens for persistent infections highlight the potential need for combination therapies targeting different bacterial persistence mechanisms [30]. Furthermore, the correlation between autoantibody levels and symptom severity suggests potential benefit from immunomodulatory approaches in selected patient populations.
Future research priorities should include:
- International surveillance networks to track emerging bacterial pathogens and their transmission dynamics
- Advanced persistence models to elucidate mechanisms of bacterial chronicity
- Rapid diagnostic implementation to reduce time to targeted antimicrobial therapy
- Host-directed therapies to address immune dysregulation in chronic manifestations
- Biomarker discovery to identify patients at risk for chronic sequelae
The financial allocation for gathering international data on waterborne and zoonotic emerging diseases is increasingly urgent to provide better understanding of their clinical relevance and public health impact [29]. As detection methodologies continue to advance, the number of recognized bacterial pathogens contributing to chronic human illness will likely expand, necessitating ongoing collaboration between clinical, microbiological, and public health disciplines.
The rise of antimicrobial resistance (AMR) represents one of the most pressing global health threats of the 21st century, often described as a "silent pandemic" unfolding outside public view. Bacterial AMR was directly responsible for 1.27 million global deaths in 2019 and contributed to 4.95 million deaths, with recent estimates projecting over 8 million annual resistance-associated deaths by 2050 [34] [20]. This escalating health crisis coincides with a paradoxical trend: the progressive decline in development of new antibacterial treatments. The antibiotic pipeline, once robust during the "golden era" of antibiotic discovery (1940s-1960s) that yielded more than 20 new antibiotic classes, has entered what is now termed an "antibiotic discovery void" [34]. Since 1987, only five novel classes of antibiotics have been marketed, and the clinical pipeline contains alarmingly few innovative agents targeting the World Health Organization's (WHO) most critical priority pathogens [34] [35].
This whitepaper analyzes the complex interplay between scientific innovation barriers and economic disincentives that have created this dangerous innovation gap. Within the broader context of unrecognized human bacterial pathogens research, we examine how existing discovery paradigms have largely failed to address the threat of resistant infections, particularly those caused by Gram-negative bacteria identified in the WHO's 2024 Bacterial Priority Pathogens List [36]. We further explore promising alternative approaches, detailed experimental methodologies for pathogen identification, and essential research tools that may help revitalize the field.
The Current Antibacterial Development Landscape
Quantitative Analysis of the Clinical and Preclinical Pipeline
The antibacterial pipeline remains critically anemic, particularly for innovative agents targeting priority pathogens. Table 1 summarizes the current state of antibacterial agents in development based on WHO's 2024 analysis [37] [38].
Table 1: Current Antibacterial Clinical Development Pipeline (2024 WHO Data)
| Pipeline Category | Number of Agents | Innovative Agents | Targeting WHO Critical Pathogens | Notes |
|---|---|---|---|---|
| Total Clinical Pipeline | 90 | 15 | 5 | Down from 97 in 2023 |
| Traditional Antibiotics | 50 | 12 | 4 | Mostly β-lactamase inhibitor combinations |
| Non-traditional Agents | 40 | 3 | 1 | Bacteriophages, antibodies, microbiome modulators |
| Preclinical Pipeline | 232 | ~90% from small firms | N/A | Significant economic hurdles for development |
The decline in innovative candidates is particularly alarming. Of the 32 antibiotics under development to address infections from the Bacterial Priority Pathogens List, only 12 can be considered innovative, with just 4 of these active against at least one WHO 'critical' pathogen [38]. The critical priority category includes carbapenem-resistant Acinetobacter baumannii, carbapenem-resistant Enterobacterales, third-generation cephalosporin-resistant Enterobacterales, and rifampicin-resistant Mycobacterium tuberculosis [37]. Since 2017, only 13 new antibiotics have obtained marketing authorization, with just two representing a new chemical class deemed truly innovative [38].
The WHO Bacterial Priority Pathogens List 2024: A Strategic Framework
The 2024 WHO Bacterial Priority Pathogens List (BPPL) serves as a critical strategic framework for directing research and development efforts. Developed using a multicriteria decision analysis framework that incorporated eight criteria including mortality, non-fatal burden, incidence, 10-year resistance trends, and antibacterial pipeline status, the list represents the most evidence-based prioritization of bacterial threats [36]. Table 2 outlines the highest priority pathogens from the 2024 BPPL [36].
Table 2: WHO Bacterial Priority Pathogens List 2024 - Critical and High Priority Pathogens
| Priority Tier | Pathogen | Resistance Profile | Total Score (%) | R&D Urgency |
|---|---|---|---|---|
| Critical | Klebsiella pneumoniae | Carbapenem-resistant | 84% | Highest |
| Critical | Acinetobacter baumannii | Carbapenem-resistant | 82% | Highest |
| Critical | Mycobacterium tuberculosis | Rifampicin-resistant | 80% | Highest |
| Critical | Escherichia coli | Carbapenem-resistant | 78% | Highest |
| High | Salmonella enterica serotype Typhi | Fluoroquinolone-resistant | 72% | High |
| High | Shigella spp. | Fluoroquinolone-resistant | 70% | High |
| High | Pseudomonas aeruginosa | Carbapenem-resistant | 68% | High |
| High | Neisseria gonorrhoeae | Extended-spectrum cephalosporin-resistant | 64% | High |
| High | Staphylococcus aureus | Methicillin-resistant | 62% | High |
The 2024 BPPL highlights the persistent threat of antibiotic-resistant Gram-negative bacteria, which dominate the critical priority tier. Notably, the list also emphasizes the disproportionate burden of community-acquired infections in resource-limited settings, with pathogens like fluoroquinolone-resistant Salmonella and Shigella species ranking as high priority [36].
Economic and Regulatory Barriers to Antibiotic Development
Market Failures in Antibiotic Development
The economic model for antibiotic development is fundamentally broken, creating what has been termed a "market failure" that drives pharmaceutical companies away from this critical field. The root causes are multifaceted:
- Poor Return on Investment: Antibiotics are typically used for short durations (days to weeks), unlike medications for chronic conditions that generate sustained revenue. The direct net present value of an antibiotic is close to zero, with most new antibiotics generating only $15-50 million in annual US sales, far below the estimated $300 million needed for sustainability [35].
- High Development Costs with Low Success Rates: The mean cost for developing systemic anti-infectives is approximately $1.3 billion, matching the average across all drug classes, despite a better Phase 1 to approval success rate (25% versus 14% average) [35]. Post-approval costs add an additional $240-622 million over five years [35].
- Stewardship Versus Commercialization Conflict: Appropriate antibiotic stewardship practices that preserve efficacy by limiting use directly conflict with traditional pharmaceutical commercialization models that rely on widespread use to recoup investment [35].
This economic reality has triggered a massive exodus of major pharmaceutical companies from antibiotic research. Since the 1990s, 18 major pharmaceutical companies have exited the field, with even those maintaining active programs beyond this period—GSK, Novartis, Sanofi, and AstraZeneca—shifting away between 2016 and 2019 [34]. The devastating consequence has been a "brain drain" of specialized expertise, with only approximately 3,000 AMR researchers currently active worldwide [35].
Clinical Trial Challenges and Regulatory Hurdles
Clinical trials for new antibiotics face unique methodological and operational challenges that further complicate development:
- Patient Recruitment Difficulties: Trials for antibiotics targeting resistant infections require specific patient populations that are relatively rare at individual sites. The plazomicin trial against carbapenem-resistant Enterobacterales screened 2,000 patients but successfully enrolled only 39, at an estimated cost of $1 million per recruited patient [35].
- Non-inferiority Trial Designs: Antibiotics typically must demonstrate non-inferiority to existing therapies rather than superiority, requiring large sample sizes that increase costs and prolong development timelines [35].
- Operational Complexities: Patients with resistant infections often have comorbidities or receive concomitant antimicrobial drugs, complicating the assessment of treatment benefit for investigational drugs [39].
The lengthy pathway from preclinical development to approval—approximately 10-15 years—combined with these clinical trial challenges creates a perfect storm that deters investment in antibiotic development [40].
Innovative Approaches and Methodologies
Meta-Genomics for Pathogen Discovery and Characterization
The investigation of unrecognized bacterial pathogens requires moving beyond traditional culture-dependent methods, which have significant limitations for novel pathogen discovery. Meta-genomics represents a powerful culture-independent approach for comprehensive pathogen identification and characterization [41]. The experimental workflow, illustrated in Figure 1, enables unbiased detection of previously unknown bacterial pathogens in clinical and environmental samples.
Figure 1: Meta-Genomics Pathogen Discovery Workflow
The meta-genomics workflow involves two primary approaches: untargeted shotgun sequencing of all nucleic acids in a sample, and targeted sequencing of known pathogens. For novel pathogen discovery, the de novo shotgun meta-genomics pipeline is particularly valuable as it enables identification of unknown sequences without relying on reference genomes [41]. Critical steps in this process include:
- Initial Assembly: Using algorithms such as SPAdes, Lasergene, or Flye to generate contiguous sequence blocks ("contigs") from overlapping sequencing reads [41].
- Resolution of Genomic Repeats: Employing long-read sequencing platforms to address repetitive genomic regions that challenge short-read technologies [41].
- Genome Polishing: Running assembled genomes through multiple algorithms (Arrow, FreeBayes, Racon) to correct misassemblies, mismatches, and indels [41].
- Functional Annotation: Comparing polished genomes against known sequence databases using tools like UBLAST to annotate conserved elements and assess phylogenetic relatedness [41].
A critical evaluation of assemblers using mock microbial communities concluded that long-read data alone can generate accurate and complete genomes, with software selection significantly impacting quality. Meta-genomics-specific tools such as metaFlye, Raven, and Canu generally outperform general-purpose assemblers [41].
Multi-Omics and Non-Traditional Therapeutic Approaches
Beyond traditional antibiotics, innovative therapeutic strategies are emerging that offer promising alternatives for tackling resistant infections:
- Bacteriophages and Lysins: Bacteriophages (viruses that infect specific bacteria) and lysins (enzymes that degrade bacterial cell walls) represent precision antibacterial approaches with potentially lower resistance development [37] [35].
- Monoclonal Antibodies: Pathogen-specific antibodies can neutralize bacterial toxins or enhance immune clearance of pathogens, though development costs remain high [37].
- Microbiome Modulation: Fecal-based products for restoring gut microbiota have shown success in preventing recurrent Clostridioides difficile infection, with three such products recently authorized [38].
- Anti-virulence Agents: Rather than killing bacteria, these agents disrupt virulence mechanisms (e.g., toxin production, adhesion, quorum sensing), potentially reducing selective pressure for resistance [35].
- Immune Modulators: Agents that enhance host immune responses to infections represent a complementary approach to direct antibacterial activity [35].
These non-traditional approaches comprised 40 of the 90 agents in the clinical pipeline in the 2024 WHO analysis, indicating growing interest in these alternative modalities [37].
The Scientist's Toolkit: Essential Research Reagents and Platforms
Table 3 details key research reagents and platforms essential for investigating unrecognized bacterial pathogens and developing novel antibacterial strategies.
Table 3: Research Reagent Solutions for Bacterial Pathogen Investigation
| Reagent/Platform | Function | Application in Pathogen Research |
|---|---|---|
| CRISPR-Cas Systems | Gene editing and bacterial identification | Pathogen gene function validation, diagnostic development |
| Bacterial Phenotype Microarrays | High-throughput phenotypic screening | Metabolic profiling, antibiotic susceptibility testing |
| Omics Libraries | Focused compound collections | Screening for novel antibacterial activity |
| CARB-X Compound Libraries | Rationally designed focused libraries | Gram-negative antibacterial drug discovery |
| AR Isolate Bank (CDC/FDA) | Quality-controlled resistant isolates | Preclinical development challenge sets |
| Monoclonal Antibody Platforms | Pathogen-specific antibody generation | Therapeutic and diagnostic applications |
| Bacteriophage Libraries | Diverse phage collections | Phage therapy development |
| Synthetic Biology Toolkits | Genetic circuit construction | Engineered diagnostic and therapeutic bacteria |
| Microbiome Modulators | Defined bacterial consortia | Restorative therapy for infection prevention |
| AI/ML Screening Platforms | Predictive compound screening | Identification of novel antibacterial candidates |
These research tools, many supported by government initiatives like the NIH Chemistry Center for Combating Antibiotic-Resistant Bacteria (CC4CARB), provide critical resources for overcoming historical challenges in antibacterial discovery [39]. The CC4CARB specifically focuses on synthesizing and distributing rationally designed, focused libraries free-of-charge to the global scientific community for Gram-negative antibacterial drug discovery programs [39].
Bacterial Resistance Mechanisms and Therapeutic Targeting
Understanding the molecular basis of antibiotic resistance is fundamental to designing effective countermeasures. Figure 2 illustrates the primary mechanisms of bacterial resistance and corresponding therapeutic targeting strategies.
Figure 2: Bacterial Resistance Mechanisms and Corresponding Therapeutic Strategies
The five primary resistance mechanisms—enzymatic inactivation, target modification, efflux pumps, permeability barriers, and biofilm formation—represent evolutionary adaptations that bacteria employ to survive antibiotic exposure. Innovative therapeutic approaches must address these specific mechanisms, often through combination strategies that include both direct antibacterial activity and resistance-countering adjuvants [34] [20].
Addressing the innovation gap in antibiotic development requires a multifaceted approach that combines scientific advancement with economic and policy reforms. Promising pathways include:
- Pull Incentives: Implement market entry rewards and subscription-based payment models that delink antibiotic reimbursement from volume of use, creating sustainable economic models for antibiotic development [35] [39].
- Public-Private Partnerships: Expand initiatives like CARB-X (Combating Antibiotic-Resistant Bacteria Biopharmaceutical Accelerator) that provide funding and technical support for early-stage antibacterial research [39].
- Regulatory Modernization: Develop streamlined regulatory pathways for non-traditional antibacterial agents and novel clinical trial designs that efficiently demonstrate efficacy against resistant infections [35] [39].
- Global Coordination: Enhance international collaboration through the Quadripartite Joint Secretariat (FAO, UNEP, WHO, WOAH) to implement a comprehensive One Health approach to AMR that addresses human, animal, and environmental dimensions [20].
- Diagnostic Integration: Accelerate development and deployment of rapid diagnostic tests to enable targeted antibiotic use and facilitate clinical trials for pathogen-specific agents [37].
The second UN High-level Meeting on AMR in 2024 resulted in a political declaration pledging to reduce AMR-associated deaths by 10% by 2030, with calls for catalytic funding of $100 million to help 60% of countries globally secure funds to execute AMR plans by 2030 [34]. Such commitments, if backed by sustained investment and implementation, represent crucial steps toward revitalizing the antibiotic pipeline and securing effective treatments for future generations.
The innovation gap in antibiotic development is both a scientific and economic challenge of unprecedented complexity. By leveraging novel discovery methodologies, embracing non-traditional therapeutic approaches, and implementing sustainable economic models, the global research community can begin to bridge this gap and address the escalating threat of antimicrobial resistance.
Beyond Culture: Advanced Genomic and Molecular Tools for Pathogen Discovery
The study of unrecognized human bacterial pathogens represents a critical frontier in public health and infectious disease research. Conventional, culture-dependent diagnostic methods, long considered the "gold standard," are inherently limited for this task, as they require a priori knowledge of a pathogen to select the appropriate growth conditions and subsequent tests [42] [43]. It is estimated that the cause of severe infections like meningoencephalitis remains unknown in approximately 50% of cases using these traditional methods, significantly hindering clinical management and effective response to emerging threats [44]. This diagnostic ceiling creates a pressing need for hypothesis-free tools that can comprehensively characterize the microbial content of a clinical sample.
Metagenomic Next-Generation Sequencing (mNGS) is a culture-independent, agnostic sequencing technology that has emerged to meet this challenge. By simultaneously sequencing all nucleic acids (DNA and RNA) in a sample, mNGS allows for the detection and identification of any bacteria, virus, fungus, or parasite present without any prior suspicion [45] [43]. This capability is indispensable for research on unrecognized bacterial pathogens, enabling the discovery of novel organisms, the detection of fastidious or slow-growing bacteria that evade culture, and the accurate characterization of complex polymicrobial infections [44] [46]. As public health crises repeatedly emphasize, the rapid deployment of agnostic diagnostics at the start of an outbreak is a cornerstone of an effective response to emerging pathogens [45].
The mNGS Workflow: From Sample to Result
The journey from a complex clinical sample to actionable pathogen data involves a multi-step process designed to maximize the recovery of microbial signals.
Wet-Lab Experimental Protocol
The following workflow diagram outlines the key stages of the mNGS process, highlighting critical decision points that influence assay performance.
Figure 1: The mNGS Experimental Workflow. This diagram outlines the key stages in a clinical metagenomic next-generation sequencing assay, from sample collection to final bioinformatic analysis, with approximate processing times for optimized protocols [47].
Detailed Methodology for Key Experimental Steps:
Sample Collection & Input: Samples are collected in a sterile manner from sterile sites (e.g., Cerebrospinal Fluid - CSF, tissue) or non-sterile sites (e.g., upper respiratory swabs, bronchoalveolar lavage - BAL). An input volume of 450 µL is typical for optimized protocols. The sample matrix can significantly impact diagnostic performance and must be considered during interpretation [45] [47].
Nucleic Acid Extraction: Total nucleic acid is extracted, followed by DNase treatment to isolate total RNA, enabling the detection of RNA viruses and bacterial transcripts. For DNA-focused assays, differential lysis and methylated DNA depletion can be used to reduce host background [47] [44].
Library Preparation: This critical step involves:
- cDNA Synthesis: RNA is reverse-transcribed to DNA using reverse transcriptase. Optimized protocols can reduce incubation times to 15 minutes [47].
- Host Depletion: Techniques to remove human ribosomal RNA (rRNA) are employed, with protocols available that take as little as 15 minutes. This step is crucial for enriching microbial content and improving sensitivity [47].
- Library Construction: Adapters are ligated to the DNA fragments, which are then amplified via PCR. This step can be performed on an automated instrument in approximately 6.5 hours, reducing hands-on time and improving reproducibility [47].
Sequencing: Prepared libraries are sequenced using high-throughput platforms. Common instruments include Illumina (e.g., NextSeq, MiniSeq) for short-read sequencing or Oxford Nanopore Technologies (ONT) devices for long-read, real-time sequencing. The choice between short- and long-read technologies involves a trade-off between accuracy, read length, turnaround time, and cost [47] [48].
The Scientist's Toolkit: Essential Research Reagents
Successful execution of the mNGS workflow relies on a suite of critical reagents and controls, each serving a specific function to ensure data quality and reliability.
Table 1: Key Research Reagent Solutions for mNGS
| Reagent / Solution | Function | Example & Brief Explanation |
|---|---|---|
| Internal Control (MS2 Phage) | Qualitative process control. | MS2 phage is spiked into the sample at the start of extraction. Its consistent detection verifies successful nucleic acid extraction, library prep, and sequencing, and helps evaluate background noise [47]. |
| Quantitative Control (ERCC Mix) | Generation of standard curve for viral load quantification. | The External RNA Controls Consortium (ERCC) RNA Spike-In Mix consists of exogenous RNA transcripts at known concentrations. It enables absolute quantification of pathogens in copies/mL by comparing sample data to the external positive control [47]. |
| External Positive Control | Assay performance and run validation. | A commercial reference panel (e.g., Accuplex) containing quantified viruses (e.g., SARS-CoV-2, Influenza, RSV) spiked into a negative matrix. It confirms the assay's detection capability in each run [47]. |
| Host Depletion Reagents | Enrichment of microbial sequences. | Kits targeting human rRNA (e.g., Illumina Ribo-Zero). Removing abundant host nucleic acids dramatically increases the proportion of microbial reads, improving sensitivity, especially in low-biomass samples [47] [49]. |
| Curated Reference Databases | Accurate taxonomic classification of sequences. | FDA-ARGOS and other curated databases provide high-quality, reference-grade microbial genomes. "Tagging" these genomes in the analysis pipeline ensures reliable and standardized pathogen identification [47]. |
Analytical Performance and Validation
For a diagnostic tool to be adopted in research and clinical practice, its analytical performance must be rigorously characterized. Recent validation studies demonstrate the maturing capabilities of mNGS.
Table 2: Quantitative Performance Metrics of a Validated mNGS Assay
| Performance Metric | Result | Experimental Protocol & Significance |
|---|---|---|
| Limit of Detection (LoD) | 543 copies/mL (mean for respiratory viruses) [47] | Negative nasopharyngeal swab matrix was spiked with a quantified reference panel (Accuplex) and diluted. LoD was determined by 95% probit analysis, showing sensitivity comparable within one log to specific RT-PCR assays [47]. |
| Linearity | 100% calculated linearity [47] | A linearity panel was generated using five log dilutions of a high-titer SARS-CoV-2 positive sample. Duplicates/triplicates across dilutions showed a log10 deviation of <0.52, confirming accurate viral load quantification across a wide dynamic range [47]. |
| Sensitivity & Specificity | 93.6% Sensitivity, 93.8% Specificity (vs. multiplex RT-PCR) [47] | Performance was evaluated against gold-standard clinical testing. After discrepancy testing and clinical adjudication, overall predictive agreement increased to 97.9%, superior to that of RT-PCR (95.0% agreement) [47]. |
| Real-World Diagnostic Yield | 14.4% Positivity Rate (of 4,828 CSF samples) [44] | A 7-year performance study of clinical mNGS testing for CNS infections identified a pathogen in 697 samples. The test showed higher sensitivity (63.1%) than indirect serologic testing (28.8%) and direct detection from non-CSF samples (15.0%) [44]. |
Computational Framework for Pathogen Detection and Discovery
The raw sequencing data generated by mNGS requires sophisticated computational analysis to distinguish pathogenic signals from a background of host and commensal nucleic acids. The following diagram illustrates the bioinformatic pipeline designed for both detection and novel discovery.
Figure 2: The SURPI+ Computational Pipeline for Pathogen Detection. This enhanced bioinformatics workflow, as used in validated assays, incorporates both reference-based alignment and novel methods for identifying sequence-divergent organisms [47].
Key Enhancements in Modern mNGS Pipelines:
- Viral Load Quantification: The pipeline uses the spiked-in ERCC controls to generate a standard curve, allowing for absolute quantification of detected pathogens in copies per milliliter (cp/mL). This quantitative data has been shown to correlate with infection severity, providing clinically relevant information beyond simple detection [47].
- Novel Pathogen Discovery: A critical feature for research on unrecognized pathogens is the ability to detect novel, sequence-divergent viruses. The custom algorithm involves de novo assembly of metagenomic reads that do not align to known references, followed by translated nucleotide alignment against a viral protein database. This allows for identification based on homology at the amino acid level. In silico analysis demonstrated that after removing all human viral sequences from the database, 100% of 70 representative human viral pathogens could still be identified through homology to related animal or plant viruses [47].
- Comprehensive Profiling: Advanced pipelines can also be configured to identify markers for antimicrobial resistance (AMR) and bacterial virulence factors, providing a more complete picture of the pathogen's threat profile and potential treatment options directly from the metagenomic data [49].
Challenges and Future Directions in Bacterial Pathogen Research
Despite its transformative potential, the widespread integration of mNGS into routine research and clinical practice faces several hurdles. These include the initial high costs, lack of standardized bioinformatic pipelines, need for highly trained personnel, and challenges in interpreting findings (e.g., distinguishing contaminants from true pathogens) [42] [43] [50]. Furthermore, operationalizing mNGS within surveillance systems presents challenges in rapidly identifying appropriate use cases, ensuring reproducibility, and establishing data-sharing agreements [50].
Future developments are focused on overcoming these barriers. Key goals are the creation of a sample-to-answer system that runs in under 24 hours, compatibility with both short- and long-read sequencers, and strategies to facilitate commercialization and clinical adoption [51]. Technological advancements are rapidly driving down costs and improving accuracy, with some platforms now achieving a Q40 standard (one error in 10,000 bases) [48]. The ultimate goal is for mNGS to evolve into a routine, accessible tool that can be deployed even in resource-scarce settings, forming part of a global surveillance network crucial for the early detection and containment of novel bacterial pathogens [46].
The Tm mapping method represents a transformative approach in rapid microbiological diagnostics, enabling the identification of pathogenic bacteria directly from clinical samples within three hours of collection. This technical guide details the experimental protocols, analytical frameworks, and practical implementation of this method, with particular emphasis on its application in pediatric populations and low-biomass samples—environments where traditional culture-based methods and conventional molecular approaches face significant limitations. The method's capacity to address critical gaps in unrecognized human bacterial pathogen research is explored through its unique primer design strategy, melting temperature profiling, and specialized contamination control measures essential for reliable low-biomass analysis.
The accurate and timely identification of bacterial pathogens is particularly challenging in pediatric medicine and when investigating low-biomass environments. Traditional culture-based methods, while considered the gold standard for many infections, require several days for pathogen identification and are often inadequate for detecting fastidious or uncultivable organisms. This delay significantly impacts patient outcomes, especially in time-sensitive conditions like sepsis, and contributes to the empirical overuse of broad-spectrum antibiotics, which in turn fuels the development of antimicrobial resistance [52]. The recent rise of "nightmare bacteria" with carbapenem resistance—increasing by 460% between 2019 and 2023—underscores the urgent need for rapid, precise diagnostic tools that can guide targeted antimicrobial therapy [2].
The diagnostic challenge intensifies when working with low microbial biomass samples, such as certain pediatric tissues, blood, urine, or cerebrospinal fluid. In these environments, the inherent limitations of DNA-based sequencing approaches become critically important. The inevitable introduction of contaminating DNA from sampling equipment, reagents, or laboratory environments can disproportionately impact results, potentially leading to false positives and incorrect biological interpretations [53] [54]. This is especially problematic when investigating potential unrecognized pathogens in tissues once considered sterile, where distinguishing true signal from contamination is paramount. The pediatric urobiome, for instance, presents unique sampling and analytical challenges due to low bacterial biomass and ethical limitations in collection methods, requiring specialized approaches to avoid contamination and ensure accurate results [55].
Fundamental Principles of the Tm Mapping Method
The Tm mapping method is a novel, rapid, and cost-effective approach for identifying a broad range of pathogenic bacteria without the need for microbial culture, multiplexing, hybridization probes, or gene sequencing. Its core innovation lies in using melting temperature (Tm) profiles generated from multiple bacterial universal primer sets to create unique, species-specific identification patterns.
Workflow and Core Concept
The method operates through a streamlined four-step process designed for maximum efficiency and speed:
- DNA Extraction: Bacterial DNA is extracted directly from clinical samples (e.g., 2 mL of whole blood) [52] [56].
- Nested PCR: The DNA undergoes a nested PCR amplification using a limited set of bacterial universal primer sets (initially seven, later refined to five) targeting conserved regions of the 16S ribosomal RNA gene. This step is performed with a eukaryote-made thermostable DNA polymerase produced in yeast, which is critical for avoiding false-positive results from bacterial DNA contamination in reagents [52] [56].
- Tm Value Acquisition: The amplicons are analyzed to determine their precise melting temperatures. In the improved protocol, this step employs Imperfect-Match Linear Long Quenching Probes (IMLL Q-probes) to generate a wider variation range of Tm values, enhancing compatibility with standard real-time PCR instruments [56].
- Tm Mapping and Identification: The seven (or five) Tm values are plotted in two dimensions, creating a unique species-specific "Tm mapping shape." This shape is compared against a established database for identification [52].
Table 1: Key Phases of the Tm Mapping Workflow
| Phase | Description | Key Components | Time Frame |
|---|---|---|---|
| Sample Processing | DNA extraction from clinical samples | Whole blood, eukaryotic DNA polymerase | Within 1 hour of collection |
| Target Amplification | Nested PCR with universal primers | 5-7 bacterial universal primer sets, 16S rDNA targets | ~1.5 hours |
| Signal Generation | Melting temperature analysis | IMLL Q-Probes, real-time PCR instrumentation | ~30 minutes |
| Pathogen Identification | Database matching of Tm profiles | Custom software, species-specific Tm shape database | ~10 minutes |
| Total Time | From sample to result | ~3 hours [52] |
Algorithmic Identification and Difference Value Calculation
The identification process relies on comparing the geometric "shape" formed by the Tm values from multiple primer sets. To quantitatively assess similarity between an unknown sample and database entries, the method employs a Difference Value calculation. This metric is derived by comparing the distances of each individual Tm value from the average Tm of the profile, making the identification robust to measurement errors that affect all tubes equally (e.g., run-to-run instrument variation) [52].
The formula for calculating the Difference Value (D) is:
[ D = \sqrt{ \sum{i=1}^{7} (Xi - Y_i)^2 } ]
Where (Xi) represents the distance from the mean for the (i)-th Tm value of the unknown sample, and (Yi) represents the corresponding distance for the database entry. A Difference Value closer to zero indicates a higher degree of similarity between the unknown sample and a specific database entry [52]. The interpretative criteria for identification are based on threshold Difference Values, which must account for the tube-to-tube variation of the specific real-time PCR instrument used [56].
Diagram 1: Tm mapping method workflow for pathogen identification.
Experimental Protocols and Methodological Optimization
Standard Tm Mapping Protocol
The foundational protocol for the Tm mapping method requires meticulous attention to contamination control and measurement precision.
Sample Preparation and DNA Extraction:
- Sample Type: Whole blood (2 mL) is a validated sample type, but the method is adaptable to other sterile site samples [52].
- DNA Extraction: Use commercially available DNA extraction kits, but ensure reagents are verified for low bacterial DNA contamination. Incorporating negative extraction controls (using nuclease-free water instead of sample) is mandatory to monitor for contaminating DNA in reagents [53] [54].
- Critical Reagent: Employ a eukaryote-made thermostable DNA polymerase (manufactured in yeast) to prevent false positives from bacterial DNA contaminants commonly present in enzymes produced in bacterial systems [52] [56].
Nested PCR Amplification:
- Primary PCR: Use the first set of bacterial universal primers under standard cycling conditions to initially amplify the 16S rDNA target.
- Secondary PCR: Use the second set of primers (5-7 sets, each in a separate tube) for nested amplification. This two-step process enhances sensitivity and specificity.
- Cycling Conditions: If no amplification is observed by the 30th cycle in the second PCR, the sample can be defined as having no detectable bacteria [52].
Melting Temperature Analysis:
- Dye Chemistry: Use EvaGreen dye for stable Tm value determination and minimized tube-to-tube variation [52].
- Instrument Calibration: Use instruments with high thermal accuracy. The original method required a tube-to-tube variation of ≤ ±0.1°C (e.g., Rotor-Gene Q, LightCycler Nano) [52].
Advanced Protocol with IMLL Q-Probes
To overcome the limitation of requiring specialized instruments, an improved protocol was developed using Imperfect-Match Linear Long Quenching Probes (IMLL Q-probes).
Probe Design Strategy:
- Length: Probes are designed to be approximately 40 nucleotides long to ensure binding even in the presence of multiple mismatches [56].
- Specificity: Probes are designed to target variable regions within the 16S rDNA amplicons, generating a wide range of Tm values (spanning >20°C) across different bacterial species [56].
- Structure: Probes are bioinformatically designed to lack secondary structures (self-dimers, hairpins) by ensuring the delta G value of any potential structure is weaker than -9.0 kcal/mol, promoting linearity and preventing self-quenching [56].
Modified Workflow:
- After nested PCR with five primer sets, the amplicons from Regions 1 and 3 are divided. Each of the seven resulting amplicon aliquots is mixed with a specific IMLL Q-probe.
- The Tm values are acquired by analyzing the probe-amplicon hybrids, creating the distinctive Tm mapping shape compatible with most commercial real-time PCR instruments [56].
Table 2: Research Reagent Solutions for Tm Mapping
| Reagent / Material | Function | Technical Specifications | Application Notes |
|---|---|---|---|
| Eukaryote-Made DNA Polymerase | PCR amplification free from bacterial DNA contamination | Recombinant polymerase produced in yeast host cells | Critical for avoiding false positives in low-biomass samples [52] [56] |
| Bacterial Universal Primer Sets | Amplification of conserved 16S rDNA regions | 5-7 primer sets covering variable regions | Enables detection of >100 bacterial species [52] |
| IMLL Q-Probes | Generation of species-specific Tm signatures | ~40 nt linear probes, designed to minimize secondary structure | Enables use on standard real-time PCR instruments; creates wide Tm range [56] |
| EvaGreen Dye | Fluorescent detection for Tm analysis | Intercalating dye | Provides stable Tm values with low tube-to-tube variation [52] |
| Tm Mapping Database | Reference for pathogen identification | Contains Tm profiles of 68-107 bacterial species | Scalable database; requires periodic updating with new sequences [52] [56] |
Application in Pediatric and Low-Biomass Samples
Performance in Clinical Validation Studies
The Tm mapping method has been rigorously validated in clinical settings, demonstrating high concordance with traditional culture methods while providing results in a fraction of the time.
In a study of 200 whole blood samples from patients with suspected sepsis:
- 85% (171/200) of the Tm mapping results matched the culture results.
- Of the 130 samples negative by Tm mapping, 98% (128/130) were also negative by culture, demonstrating high negative predictive value.
- Of the 70 positive samples, 59 were suitable for identification, and 100% (59/59) showed a "match" or "broad match" with culture or sequencing results [52].
- The entire process, from blood collection to identification, was completed within three hours, compared to the 24-72 hours required for culture [52].
The limits of identification for the IMLL Q-probe method were determined to be 5 CFU/PCR tube (equivalent to 250 CFU/mL) for both Escherichia coli and Staphylococcus aureus [56].
Addressing Low-Biomass and Contamination Challenges
Low-biomass samples pose unique challenges for molecular diagnostics because contaminating DNA from reagents or the environment can constitute a significant proportion of the total DNA, leading to erroneous results [53] [54]. The Tm mapping method incorporates several strategies to mitigate these issues:
Contamination Control Measures:
- Source Decontamination: Equipment and surfaces should be decontaminated with 80% ethanol (to kill microorganisms) followed by a nucleic acid degrading solution (e.g., bleach, UV-C light) to remove trace DNA [53].
- Personal Protective Equipment (PPE): Use of gloves, masks, and clean suits to limit human-derived contamination from skin, hair, or aerosols [53].
- Negative Controls: Inclusion of multiple negative controls (e.g., empty collection vessels, swabs exposed to sampling environment, aliquots of preservation solution) processed alongside samples to identify contamination sources [53].
Analytical Specificity: While highly accurate, the method has limitations in distinguishing between some closely related species. The IMLL Q-probe method could not distinguish between Enterococcus faecalis and Enterococcus faecium or between some Staphylococcus species (aureus, hemolyticus, hominis, lugdunensis) [56]. This highlights the importance of understanding the resolution limits of the technique when investigating potential unrecognized pathogens.
Diagram 2: Low-biomass challenges and mitigation strategies for accurate diagnosis.
Integration into Unrecognized Pathogen Research
The Tm mapping method provides a valuable tool for investigating unrecognized bacterial pathogens, particularly in contexts where traditional methods have failed to establish causative links. Its application spans several critical areas of investigation:
Exploring Sterile Site Microbiomes
The method enables the study of potential microbial communities in body sites historically considered sterile, such as the urinary bladder, fetal tissues, and tumors. Research into the pediatric urobiome exemplifies this application, where low microbial biomass and ethical constraints on sample collection (e.g., avoiding suprapubic aspiration in children) complicate analysis [55]. The Tm mapping method's sensitivity and rapid turnaround make it suitable for investigating these challenging environments, potentially revealing novel pathogen associations.
Tumor Microenvironment and Treatment Resistance
Bacteria within tumors have been shown to influence cancer progression and treatment response. For example, Fusobacterium nucleatum in colorectal and oral tumors can induce a reversible quiescent state in cancer cells, helping them evade the immune system and resist chemotherapy [57]. The Tm mapping method could facilitate rapid profiling of such tumor-infiltrating bacteria, potentially identifying microbial signatures associated with treatment resistance and opening avenues for microbe-aware cancer therapies.
Antimicrobial Stewardship
By providing species-specific identification within three hours of sample collection, the Tm mapping method enables clinicians to make informed, early decisions regarding antimicrobial therapy. This is particularly crucial in pediatric sepsis and other serious infections, where inappropriate antibiotic use can have lifelong consequences. The method's rapid exclusion of bacterial etiology can prevent unnecessary antibiotic exposure, while its identification capabilities support targeted, narrow-spectrum therapy [52] [58].
The Tm mapping method represents a significant advancement in rapid molecular diagnostics, with particular relevance for pediatric infectious diseases and the investigation of low-biomass environments. Its ability to provide accurate, species-level identification of bacterial pathogens within three hours of sample collection addresses critical limitations of traditional culture-based methods and supports antimicrobial stewardship efforts. The development of IMLL Q-probes has enhanced the method's practicality by making it compatible with standard real-time PCR instrumentation.
For researchers investigating unrecognized human bacterial pathogens, the method offers a sensitive, specific, and rapid tool for exploring microbial associations in traditionally sterile sites, tumor microenvironments, and other challenging low-biomass contexts. When combined with rigorous contamination control measures and appropriate validation frameworks, the Tm mapping method can contribute substantially to our understanding of the roles—both pathogenic and protective—that bacteria play in human health and disease.
Metagenomic next-generation sequencing (mNGS) has revolutionized the detection and identification of pathogens, offering an unbiased, hypothesis-free approach to diagnosing infectious diseases. Within the realm of mNGS, two primary methodological approaches have emerged: one targeting whole-cell DNA (wcDNA) and the other targeting cell-free DNA (cfDNA). This in-depth technical guide provides a comparative analysis of these two workflows, framing the discussion within the critical context of research on unrecognized human bacterial pathogens. For researchers and drug development professionals, understanding the nuances, advantages, and limitations of each method is essential for selecting the appropriate tool to uncover elusive pathogens and combat the growing threat of antimicrobial resistance (AMR).
Performance Comparison: wcDNA vs. cfDNA mNGS
The choice between wcDNA and cfDNA mNGS involves significant trade-offs in sensitivity, specificity, and pathogen detection capability. The table below summarizes key performance metrics from recent clinical studies.
Table 1: Comparative Performance of wcDNA and cfDNA mNGS in Clinical Samples
| Performance Metric | wcDNA mNGS | cfDNA mNGS | Context and Implications |
|---|---|---|---|
| Overall Detection Rate | 83.1% (BALF samples) [59] | 91.5% (BALF samples) [59] | Higher detection rate suggests cfDNA may capture a broader spectrum of causative agents. |
| Concordance with Culture | 63.33% (body fluid samples) [60] | 46.67% (body fluid samples) [60] | wcDNA shows stronger alignment with traditional culture methods. |
| Sensitivity vs. Culture | 74.07% (body fluid samples) [60] | Not reported | Indicates wcDNA's ability to identify culture-positive infections. |
| Specificity vs. Culture | 56.34% (body fluid samples) [60] | Not reported | Lower specificity highlights need for careful result interpretation to avoid false positives. |
| Host DNA Proportion | Mean 84% [60] | Mean 95% [60] | Lower host DNA in wcDNA can improve microbial signal and sequencing efficiency. |
| Detection of Fungi/Viruses/Intracellular Bacteria | Lower detection rate for low-load pathogens [59] | Superior for low-load pathogens; 31.8% of fungi, 38.6% of viruses detected only by cfDNA [59] | cfDNA is advantageous for detecting pathogens that are difficult to culture or present in low abundance. |
The application context is critical. One study on body fluid samples concluded that "Whole-cell DNA mNGS demonstrates significantly higher sensitivity for pathogen detection and identification compared to both cfDNA mNGS and 16S rRNA NGS," particularly in abdominal infections [60]. Conversely, research on bronchoalveolar lavage fluid (BALF) for pulmonary infections found that "mNGS of cfDNA showed higher detection rate (91.5%) and total coincidence rate (73.8%) than mNGS of wcDNA (83.1% and 63.9%)" [59]. This suggests that the optimal choice may depend heavily on the sample type and the clinical syndrome.
Detailed Experimental Protocols
To ensure reproducible and reliable results, adherence to detailed, standardized protocols for both wcDNA and cfDNA mNGS is paramount. The following sections outline the core methodologies.
Sample Processing and DNA Extraction
The most fundamental difference between the two workflows lies in the initial sample processing and DNA extraction steps.
Table 2: Key Reagents and Kits for mNGS Workflows
| Research Reagent Solution | Function in Workflow | Example Kits & Instruments |
|---|---|---|
| Cell-Free DNA Extraction Kit | Isulates fragmented cfDNA from sample supernatant; critical for yield and purity. | VAHTS Free-Circulating DNA Maxi Kit (Vazyme) [60], QIAGEN QIAamp ccfDNA kit [61], MagMax cell-free DNA kit (ThermoFisher) [61] |
| Whole-Cell DNA Extraction Kit | Lyzes microbial and human cells to extract genomic DNA; includes mechanical disruption. | Qiagen DNA Mini Kit [60], QIAamp DNA Micro Kit (QIAGEN) [59] |
| DNA Library Preparation Kit | Prepares fragmented DNA for sequencing by adding adapters and indexing samples. | VAHTS Universal Pro DNA Library Prep Kit for Illumina (Vazyme) [60], QIAseq Ultralow Input Library Kit (QIAGEN) [59] |
| Nucleic Acid Quantification System | Accurately measures DNA concentration and quality before library construction. | Qubit Fluorometer (Thermo Fisher) [59] [61], BIABooster system [62] |
| Automated Nucleic Acid Extractor | Automates DNA extraction processes for improved throughput, reproducibility, and traceability. | MagNA Pure 24 (Roche), IDEAL (IDSolution), LABTurbo 24 (Taigen), Chemagic 360 (Perkin Elmer) [62] |
cfDNA mNGS Protocol
- Sample Collection and Transport: Collect body fluid (e.g., BALF, plasma, CSF) into sterile tubes. Maintain a cold chain and process samples promptly (ideally within hours) to prevent cell lysis and the release of genomic DNA into the cfDNA pool [63].
- Centrifugation: Centrifuge samples at high speed (e.g., 20,000 × g for 15 minutes) to pellet intact cells and cellular debris [60].
- cfDNA Extraction: Transfer the cell-free supernatant to a new tube. Extract cfDNA using a specialized kit designed for low-concentration, fragmented DNA. Automated systems can enhance reproducibility [62] [61].
- Quality Control: Quantify the extracted cfDNA using a fluorometer (e.g., Qubit). Assess fragment size distribution using a system like the Bioanalyzer or BIABooster to confirm the expected peak at ~160-180 base pairs and check for high molecular weight contamination [62] [63].
wcDNA mNGS Protocol
- Sample Processing: For wcDNA, the entire sample or the pellet obtained from a preliminary, lower-speed centrifugation is used. The pellet contains both human cells and microbial pathogens [59].
- Cell Lysis and DNA Extraction: Resuspend the pellet and subject it to vigorous mechanical lysis, often using bead-beating with nickel or silica beads to break open robust microbial cell walls [60].
- Nucleic Acid Purification: Extract total DNA from the lysate using a standard DNA extraction kit. This co-extracts DNA from all organisms present in the sample, including the host [60].
- Quality Control: Quantify the total DNA yield. The extracted DNA will be composed of long, intact strands, and the proportion of host DNA is typically high, which can be assessed by methods like qPCR [60] [64].
Library Preparation and Sequencing
After extraction, both workflows converge in library preparation and sequencing.
- Library Construction: Fragment the DNA (if using wcDNA) to an appropriate size and use a library preparation kit to add sequencing adapters and sample-specific barcodes. For cfDNA, which is already fragmented, the initial fragmentation step is omitted [60] [59].
- Sequencing: Sequence the libraries on a platform such as the Illumina NovaSeq. Standard parameters include a 2 × 150 paired-end configuration, generating approximately 20-30 million reads per sample to ensure sufficient depth for detecting low-abundance pathogens [60] [59]. The choice of read length (e.g., 75 bp, 150 bp) can be optimized based on the target pathogens and cost considerations, with longer reads (150-300 bp) generally providing better accuracy for bacterial identification [65].
Bioinformatic Analysis
The bioinformatic pipeline is critical for converting raw sequencing data into actionable results.
- Quality Control and Host Depletion: Remove low-quality reads and adapter sequences. Then, align reads to the human reference genome (e.g., hg38) and discard those that map to it, a process crucial for reducing background and improving sensitivity [60] [59].
- Pathogen Identification: Align the non-human reads to a comprehensive microbial genome database (e.g., from NCBI) using tools like Kraken2 or BWA [59] [65].
- Reporting Criteria: Establish stringent thresholds to distinguish true pathogens from background noise or contamination. Common criteria include:
The following diagram illustrates the core workflows for both wcDNA and cfDNA mNGS, highlighting their key differences.
Application in Research on Unrecognized Bacterial Pathogens
The global threat of antimicrobial resistance (AMR) underscores the urgent need for advanced tools like mNGS to identify and characterize novel and resistant bacterial pathogens. The World Health Organization (WHO) has highlighted critical gaps in the diagnostic pipeline, particularly the need for tools suitable for low-resource settings that can identify pathogens without prior culture [66]. Both wcDNA and cfDNA mNGS are poised to address this challenge.
- Unbiased Pathogen Discovery: mNGS does not require pre-specifying targets, making it ideal for identifying novel, unculturable, or unexpected bacterial pathogens. This is crucial for investigating infections of unknown etiology and for comprehensive surveillance of the resistome [67].
- Antimicrobial Resistance (AMR) Profiling: WGS data from mNGS can be mined for known AMR genes and mutations, providing insights into resistance mechanisms that can guide drug development. Economic analyses support the use of WGS for surveillance of bacterial pathogens on economic grounds, as the timely data can maximize the benefit from control strategies [67].
- Epidemiological Surveillance: The high resolution of mNGS enables precise strain typing and tracking of transmission pathways for resistant bacteria, such as those identified as WHO priority pathogens. Major initiatives, like the Fleming Initiative, are now combining mNGS data with AI modeling to predict how drug-resistant pathogens emerge and spread [68].
The decision to use wcDNA or cfDNA mNGS in this research context depends on the specific question. wcDNA mNGS may be superior for directly linking a viable, intact pathogen to an infection and for comprehensive genomic analysis, including plasmid and AMR gene carriage. In contrast, cfDNA mNGS may be more effective for detecting fastidious or intracellular bacteria that are difficult to culture, for monitoring response to therapy through the clearance of microbial DNA, or for diagnosing deep-seated infections from blood samples.
Both wcDNA and cfDNA mNGS workflows are powerful, high-performance tools in the arsenal of infectious disease researchers and drug developers. The comparative analysis presented in this guide demonstrates that neither method is universally superior; each has distinct strengths and limitations.
- wcDNA mNGS demonstrates high sensitivity and strong concordance with culture, making it a robust choice for many sample types, particularly those associated with abdominal infections [60]. Its main challenge is lower specificity and high background host DNA.
- cfDNA mNGS excels in detecting pathogens with low microbial loads, such as fungi, viruses, and intracellular bacteria, often yielding higher overall detection rates in pulmonary infection studies [59]. It is less affected by DNA degradation from extraction but is more susceptible to high host DNA background.
For researchers focused on unrecognized bacterial pathogens and AMR, the choice of workflow must be guided by the specific clinical question, sample type, and resources. As the field advances, the combination of both approaches or their selective application based on the clinical context may offer the most comprehensive path forward. Furthermore, ongoing innovations in automated extraction, sequencing efficiency (e.g., optimized read lengths) [65], and bioinformatic algorithms will continue to enhance the sensitivity, speed, and accessibility of mNGS, solidifying its role as a cornerstone technology in the fight against resistant and emerging bacterial threats.
The landscape of human infectious diseases is continually evolving, with metagenomic technologies increasingly uncovering novel pathogens previously unrecognized in human clinical contexts. Among these emerging agents, circoviruses have recently demonstrated pathogenic potential in immunocompromised human hosts, representing a significant development in the field of unrecognized human pathogens. Circoviruses are small, single-stranded DNA viruses with circular genomes that were previously known primarily as veterinary pathogens, particularly in swine and birds. The recent identification of human circovirus 1 (HCirV-1) in patients with hepatitis underscores the critical importance of advanced diagnostic methodologies in elucidating the etiology of unexplained clinical syndromes [69] [70].
This technical guide examines the seminal case of HCirV-1 discovery in an immunocompromised patient with hepatitis, framing it within the broader context of pathogen discovery research. We present detailed experimental protocols, analytical frameworks, and reagent solutions that enabled the identification and characterization of this novel human pathogen, providing researchers with a comprehensive toolkit for similar investigations into unrecognized human bacterial pathogens and viral agents.
Clinical Case Presentation and Epidemiological Context
Index Case: Immunocompromised Patient with Unexplained Hepatitis
The initial detection of human circovirus occurred in a 66-year-old female patient in Switzerland with a 20-year history of rheumatoid arthritis requiring sustained immunosuppressive therapy including prednisolone, rituximab, and methotrexate [69]. The patient presented in July 2022 with sudden elevation of hepatic transaminases that peaked in September 2022, with laboratory findings notable for negative serologic tests for hepatitis viruses A, B, C, and E, and absence of autoantibodies suggestive of autoimmune hepatitis [69].
Histopathological analysis of an October 2022 liver biopsy revealed acute and subacute hepatitis with a periportal mixed inflammatory infiltrate consisting of lymphocytes, histiocytes, plasma cells, and neutrophilic and eosinophilic granulocytes [69]. The pathologist categorized the changes as most consistent with infectious hepatitis, while drug-related and autoimmune etiologies were deemed highly unlikely. Transaminase levels gradually decreased and eventually normalized by July 2023, indicating a self-limiting course despite the patient's immunocompromised status [69].
Epidemiological Findings and Confirmed Cases
Subsequent investigations have expanded our understanding of HCirV-1 occurrence and prevalence:
Table 1: Documented Cases of Human Circovirus Infection
| Case Location | Patient Population | HCirV-Positive (%) | Clinical Context | Key Findings |
|---|---|---|---|---|
| Hong Kong [71] | 278 hepatitis patients | 8 (2.9%) | Unexplained hepatitis | 4/8 immunocompromised; persistent infection documented |
| Hong Kong [71] | 184 asymptomatic controls | 0 (0%) | Routine screening | No HCirV detected in absence of hepatitis |
| France [69] | Heart-lung transplant recipient | 1 case | Unexplained hepatitis | HCirV mRNA detected in hepatocytes |
| China [69] | Intravenous drug users with HIV/HCV | 2 cases | Co-infection context | First reported human circovirus detections |
The Hong Kong study demonstrated a statistically significant association between HCirV infection and hepatitis (p<0.05), with 50% of infected patients being immunocompromised, mirroring the index case [71]. Alternative causes of hepatitis were clearly identifiable in only 2 of the 8 HCirV-positive patients, suggesting HCirV as a probable causative agent in the remaining cases [71].
Experimental Protocols and Methodologies
Metagenomic Next-Generation Sequencing (mNGS)
The identification of HCirV-1 was achieved through a comprehensive mNGS workflow applied to the patient's liver biopsy tissue [69]. This approach enables unbiased detection of pathogenic nucleic acids without prior knowledge of potential causative agents.
Protocol Details:
- Sample Processing: Formalin-fixed paraffin-embedded (FFPE) liver biopsy tissue subjected to DNA and RNA extraction using commercial kits (QIAamp DNA FFPE Tissue Kit, Qiagen)
- Library Preparation: Dual DNA and RNA libraries prepared using Illumina Nextera XT DNA Sample Preparation Kit with modifications for FFPE-derived nucleic acids [69] [72]
- Sequencing Parameters: Illumina platform with 60-150 bp paired-end reads, targeting 20-50 million reads per sample
- Bioinformatic Analysis:
- Quality filtering and adapter trimming using Trimmomatic
- De novo assembly using SPAdes or MEGAHIT
- Taxonomic classification against comprehensive microbial databases using Kraken2 or BLAST
- Genome binning and annotation using Prokka or similar tools
The initial analysis identified sequence reads with similarity to porcine circovirus 3 (PCV3), but subsequent reanalysis against the newly published HCirV-1 genome (HCirV-1-FR) demonstrated greater identity with the human strain [69]. This highlights the importance of maintaining current, comprehensive reference databases for pathogen identification.
Specific PCR Assays for Detection and Quantification
Following initial mNGS detection, specific PCR assays were developed for confirmation and viral load monitoring:
Primer Design:
- Two primer sets were utilized: one specific to the French HCirV-1 strain (HCirV-1-FR) and a second broader set targeting the expanding clade of human circoviruses, including strains from China [69]
- Targets included both replicase (rep) and capsid (cap) genes to ensure detection specificity
Quantitative PCR Protocol:
- Reaction Composition: 20μL containing 1X LightCycler 480 Probes Master (Roche), 0.5μM each primer, 0.2μM probe, and 5μL template DNA
- Amplification Conditions: 95°C for 10 min, followed by 45 cycles of 95°C for 15 sec and 60°C for 30 sec [71]
- Quantification Standard: Serial dilutions of plasmid containing target amplicon for absolute quantification
- Analytical Sensitivity: Limit of detection of 10-100 copies/mL depending on sample type [71]
The HCirV-1 viral load in the index case's liver biopsy was remarkably high at 3.39 × 10^9 genome copies/g tissue, supporting an active viral replication process [69].
In Situ Hybridization for Cellular Localization
RNAscope in situ hybridization (Bio-Techne) was employed to localize HCirV-1 nucleic acids within liver tissue and confirm cellular tropism [69].
Protocol Details:
- Probe Design: Double-Z oligonucleotide probes targeting HCirV-1-CH rep gene transcripts
- Tissue Processing: 5μm FFPE sections mounted on charged slides
- Hybridization Conditions:
- Protease pretreatment for 30 min at 40°C
- Target probe hybridization for 2 hours at 40°C
- Amplification steps per manufacturer protocol
- Fast Red chromogenic detection
- Controls: Included normal liver tissues (n=3) and hepatitis B/C-infected liver tissues (n=4) as negative controls
This technique demonstrated HCirV-1 nucleic acids in approximately 40% of hepatocytes, with strongest positivity co-localizing with nuclei, consistent with nuclear replication of circoviruses [69].
Viral Persistence and Shedding Assessment
Longitudinal monitoring of viral dynamics was conducted through systematic sampling of multiple body compartments:
Table 2: HCirV-1 Persistence and Viral Load Dynamics in Index Case
| Sample Type | Timepoint Post-Diagnosis | Viral Load (copies/mL) | Significance |
|---|---|---|---|
| Liver biopsy | Acute phase (Oct 2022) | 3.63 × 10^9/g | Primary site of infection |
| Blood | 2 months (Dec 2022) | 1.15 × 10^7/mL | Established viremia |
| Blood | 17-21 months (Dec 2023-Apr 2024) | ~10^7/mL | Persistent high-level viremia |
| Stool | 17-21 months | ~10^4/mL | Active shedding |
| Urine | 17-21 months | ~10^4/mL | Active shedding |
| Saliva | 21 months (Apr 2024) | ~10^3/mL | Low-level shedding |
The persistence of high viral loads in blood for >21 months without significant genomic changes indicates chronic infection with continuous viral replication in an immunocompromised host [69].
Experimental Workflow Visualization
Figure 1: Comprehensive Workflow for Novel Circovirus Identification. This diagram illustrates the stepwise process from initial clinical presentation to pathogen discovery and characterization, highlighting key decision points and methodological approaches.
Research Reagent Solutions and Essential Materials
Table 3: Key Research Reagents for Circovirus Detection and Characterization
| Reagent/Category | Specific Examples | Application & Function | Technical Notes |
|---|---|---|---|
| Nucleic Acid Extraction | QIAamp DNA Blood Mini Kit (Qiagen), QIAamp DNA FFPE Tissue Kit | Isolation of viral DNA from clinical samples | FFPE protocols require specialized treatment for cross-linked DNA |
| Library Preparation | Nextera XT DNA Sample Preparation Kit (Illumina) | Preparation of sequencing libraries from low-input DNA | Modified protocols needed for degraded FFPE-derived DNA [72] |
| Sequencing Platforms | Illumina MiSeq, NextSeq | High-throughput sequencing | Short-read technologies sufficient for small circovirus genomes |
| Specific PCR Reagents | LightCycler 480 Probes Master (Roche), custom primers/probes | Target-specific detection and quantification | Primer design should account for known strain variation |
| In Situ Hybridization | RNAscope Kit (Bio-Techne), custom HCirV-1 probes | Cellular localization of viral nucleic acids | Double-Z probe design enhances specificity and signal amplification |
| Cloning & Expression | pGEM-T Easy Vector (Promega), pCMV-Myc/FLAG vectors | Genome sequencing, protein expression | Essential for functional studies of rep and cap genes |
| Bioinformatic Tools | Kraken2, BLAST, MAFFT, IQ-TREE | Taxonomic classification, genome analysis, phylogenetics | Custom database maintenance crucial for novel pathogen detection |
Genomic Characterization and Phylogenetic Analysis
The complete genome of the Swiss HCirV-1 strain (HCirV-1-CH) was deposited in GenBank (accession no. OR905605) and comparative analysis revealed important relationships with other circoviruses [69].
Genomic Features:
- Genome Organization: Characteristic circovirus ambisense organization with two major open reading frames
- ORF1: Encodes replication-associated protein (Rep)
- ORF2: Encodes capsid protein (Cap)
- Intergenic Region: Contains stem-loop structure with nonanucleotide motif essential for rolling-circle replication
Comparative Genomics:
- HCirV-1-CH vs. HCirV-1-FR: 83.6% full-genome nucleotide identity
- Rep Gene: 91.2% nucleotide identity, 95.6% amino acid identity (high conservation)
- Cap Gene: 69.4% nucleotide identity, 64.1% amino acid identity (significant divergence)
- Phylogenetic Position: HCirV-1 strains form a distinct clade separate from animal circoviruses, but cluster closely with circovirus sequences from drug users in China [69]
The significant divergence in the capsid gene, which encodes the primary antigenic determinant, suggests potential immune evasion capabilities and adaptation to human host factors.
Pathogenesis and Host-Pathogen Interactions
Hepatic Tropism and Cellular Binding
Experimental evidence strongly supports specific hepatic tropism of HCirV-1. Binding assays using HCirV-1-derived virus-like particles (VLPs) demonstrated specific binding to human hepatoma cell lines (PLC/PRF/5 and Hep-G2) but not to A549 lung epithelial cells [71]. This hepatic tropism was further confirmed by in situ hybridization showing viral nucleic acids primarily in hepatocytes [69].
The host immune status appears to be a critical factor in HCirV-1 pathogenesis. The index case had significant immunodeficiency characterized by B-cell deficiency (due to rituximab therapy), hypogammaglobulinemia, and complement system dysfunction via the mannose-binding lectin pathway [69]. These factors likely contributed to the establishment of persistent infection with high viral loads.
Parallels with Porcine Circovirus Pathogenesis
Insights from veterinary circovirus research provide valuable context for understanding human infection:
Table 4: Comparative Features of Circovirus Infections Across Species
| Feature | Porcine Circovirus 2 (PCV2) | Human Circovirus 1 (HCirV-1) |
|---|---|---|
| Primary Target Cells | Lymphocytes, macrophages, hepatocytes | Hepatocytes (demonstrated tropism) |
| Clinical Manifestations | PMWS, hepatitis, PDNS, respiratory disease | Hepatitis, mononucleosis-like syndrome |
| Persistent Infection | Common, with prolonged shedding | Documented >21 months in immunocompromised |
| Viral Shedding | Feces, urine, respiratory secretions | Blood, stool, urine, saliva (demonstrated) |
| Immunocompromise Role | Predisposing factor for severe disease | Appears essential for symptomatic infection |
PCV2 provides a relevant model for understanding HCirV-1 persistence and transmission dynamics, particularly its exceptional ability to cause persistent infections and shed in bodily fluids, enabling rapid spread in populations [69].
Discussion and Research Implications
Public Health and Diagnostic Considerations
The discovery of HCirV-1 as a human pathogen has several important implications:
- Unexplained Hepatitis: HCirV-1 should be considered in the differential diagnosis of unexplained hepatitis, particularly in immunocompromised patients where conventional hepatitis etiologies have been excluded
- Blood Safety: While transfusion transmission was ruled out in the index case, the high viral loads in blood and persistence raise concerns about blood product safety [69]
- Environmental Surveillance: Wastewater testing for HCirV-1 could elucidate regional distribution and prevalence, as suggested by parallels with porcine circovirus epidemiology [69]
- Zoonotic Potential: The evolutionary origins and potential animal reservoirs of HCirV-1 require further investigation, though no direct animal contact was identified in the index case
Future Research Directions
Several critical research questions remain unresolved:
- Transmission Routes: Precise mechanisms of transmission require elucidation
- Animal Reservoirs: Potential zoonotic origins need investigation
- Spectrum of Disease: The full clinical spectrum of HCirV-1 infection in both immunocompromised and immunocompetent hosts remains undefined
- Treatment Strategies: Antiviral options and potential vaccine development require exploration
The diagnostic approach outlined in this guide provides a template for future investigations into unrecognized human pathogens, demonstrating the power of integrated clinical observation, metagenomic technologies, and careful laboratory validation in advancing our understanding of infectious diseases.
The identification of HCirV-1 as a cause of hepatitis in immunocompromised patients represents a significant achievement in pathogen discovery and underscores the ongoing relevance of investigating unrecognized human pathogens. This case study demonstrates the critical importance of maintaining an open-minded diagnostic approach when faced with unexplained clinical syndromes, particularly in vulnerable patient populations.
The methodologies and reagents detailed in this technical guide provide a roadmap for researchers investigating similar novel pathogens, emphasizing the integrated application of clinical observation, modern sequencing technologies, and careful laboratory validation. As metagenomic technologies continue to evolve and become more accessible, our capacity to identify novel pathogens in clinical contexts will expand, potentially transforming our understanding of infectious diseases and enabling more precise diagnostic and therapeutic approaches.
The rapid and accurate identification of bacterial pathogens is a cornerstone of modern public health and clinical microbiology. This technical guide delineates a comprehensive bioinformatic pipeline, framed within research on unrecognized human bacterial pathogens, that transforms raw sequencing data into actionable reports for researchers and drug development professionals. By integrating established quality control measures, state-of-the-art assembly techniques, machine learning-based pathogen prediction, and systems biology approaches for functional annotation, the pipeline facilitates the discovery and characterization of novel pathogenic entities. The guide provides detailed methodologies, structured data presentations, and essential workflow visualizations to equip scientists with the tools necessary to navigate the complexities of genomic data and contribute to the urgent fight against antimicrobial resistance (AMR) and emerging infectious diseases.
Despite significant advances in molecular biology and genomics, infectious diseases caused by pathogenic microorganisms remain a severe global threat to human health [73]. The challenge is compounded by the continuous evolution of pathogens and the alarming rise of antimicrobial resistance (AMR). A 2022 systematic analysis in The Lancet revealed that AMR was directly responsible for approximately 1.27 million deaths and contributed to nearly 4.95 million other deaths globally in 2019 alone [73]. By 2022, approximately 1.3 million deaths were linked to antibiotic resistance, and projections suggest that by 2050, antibiotic-resistant infections could cause 10 million deaths annually without intervention [73].
The discovery and characterization of unrecognized human bacterial pathogens are critical for addressing this crisis. Traditional culture-based methods for identifying pathogenic bacteria are often characterized by prolonged timeframes, intricate procedures, and suboptimal sensitivity. For instance, culturing mycobacterial strains can require 30 to 40 days [73]. Molecular techniques like PCR, while faster, are typically targeted and may miss novel or unexpected pathogens. High-throughput sequencing technologies circumvent these limitations but generate vast amounts of complex data, necessitating robust, automated bioinformatic pipelines to translate this data into biologically meaningful and clinically actionable information. This guide outlines such a pipeline, emphasizing its application within a research context focused on discovering and understanding previously unrecognized bacterial pathogens.
A bioinformatic pipeline for pathogen reporting is a multi-stage process that systematically converts raw sequencing reads into a comprehensive report on the pathogenic potential of a sample. The overall workflow, from sample to final report, can be visualized as follows:
Stage 1: Quality Control and Preprocessing
The initial and critical stage of any bioinformatic analysis involves assessing and ensuring the quality of the raw sequencing data. This step identifies technical artifacts and prevents erroneous conclusions downstream.
Understanding Raw Data and Quality Metrics
Sequencing data is typically delivered in the FASTQ format. Each sequence read is represented by four lines: a sequence identifier starting with "@", the nucleotide sequence, a separator line starting with "+", and a quality score string for each base [74]. The quality score, encoded as a single ASCII character, represents the probability (P) that a base was called incorrectly. It is calculated as the Phred score: Q = -10 log₁₀(P) [74].
Table 1: Interpretation of Phred Quality Scores
| Phred Quality Score | Probability of Incorrect Base Call | Base Call Accuracy |
|---|---|---|
| 10 | 1 in 10 | 90% |
| 20 | 1 in 100 | 99% |
| 30 | 1 in 1,000 | 99.9% |
| 40 | 1 in 10,000 | 99.99% |
Experimental Protocol: Quality Assessment and Trimming
Tools: FastQC, FASTQE, Cutadapt, Trimmomatic, MultiQC [74].
Detailed Methodology:
Quality Assessment: Run FastQC on the raw FASTQ file(s). FastQC generates an HTML report summarizing key metrics, including:
- Per Base Sequence Quality: Visualizes the average quality score at each position across all reads. A drop in quality towards the ends of reads is common.
- Sequence Quality Distribution: Shows the overall distribution of average read qualities.
- Per Base Sequence Content: Checks for overrepresented nucleotides, which can indicate contamination or adapter content.
- Adapter Content: Measures the proportion of reads containing adapter sequences. FASTQE provides a rapid, emoji-based visualization of quality, offering an immediate impression of data quality [74].
Quality Trimming/Filtering: Based on the FastQC report, use a tool like Cutadapt to perform the following:
- Remove adapter sequences: Provide the adapter sequence used in your library preparation.
- Trim low-quality bases: Typically, bases below a quality threshold (e.g., Q20) are trimmed from the 3' end. A sliding window approach can be used, where a window is trimmed if its average quality falls below the threshold.
- Remove short reads: After trimming, discard reads that fall below a minimum length (e.g., 50-75 bp), as they can be problematic for assembly.
Post-Trimming Assessment: Run FastQC again on the trimmed FASTQ files to confirm the success of the cleaning process.
Report Generation: Use MultiQC to aggregate results from multiple tools (e.g., FastQC on raw and trimmed data, Cutadapt statistics) into a single, unified report, facilitating easy comparison across multiple samples.
The quality control process, from raw data to cleaned data, is summarized below:
Stage 2: Genome Assembly and Gene Prediction
Once the data is cleaned, the next step is to reconstruct the genomic sequences and identify the genes present.
De Novo Genome Assembly
For samples containing novel or unrecognized pathogens, a reference genome may not be available. In such cases, de novo assembly is used to reconstruct the genome from the short sequencing reads without a guide. This process involves finding overlaps between reads to build longer contiguous sequences (contigs). Assemblers like SPAdes are commonly used for this purpose, especially for bacterial genomic data [75].
Gene Prediction and Open Reading Frame (ORF) Calling
With the assembled contigs, the next step is to identify potential protein-coding genes. This is performed by gene prediction tools such as Prodigal, which scans the contigs for Open Reading Frames (ORFs) [75]. Prodigal uses dynamic programming to identify regions with sequence patterns consistent with bacterial genes, such as ribosome binding sites and start/stop codons. The output is a file (often in FASTA or GFF format) containing the predicted nucleotide or amino acid sequences of all putative proteins in the sample.
Stage 3: Pathogenicity Prediction and Functional Annotation
This is the core analytical stage where the pipeline assesses the pathogenic potential of the identified genes and annotates their functions.
Machine Learning-Based Pathogen Prediction
Homology-based approaches (e.g., BLAST) have limitations in identifying novel virulence factors with low sequence similarity to known proteins. Machine learning (ML) classifiers trained on specific features of pathogenic proteins offer a powerful alternative [75].
Tools like MP4 leverage the differences in the protein profiles of pathogenic and non-pathogenic bacteria. MP4 uses a Support Vector Machine (SVM) model trained on dipeptide frequency and other protein features (pepstats) to classify proteins into three functional classes relevant to pathogenesis [75]:
Table 2: Pathogenic Protein Classes Predicted by Machine Learning Models
| Class | Description | Example Proteins |
|---|---|---|
| Class 1 | Non-pathogenic proteins | Housekeeping genes, metabolic enzymes |
| Class 2 | Antibiotic Resistance Proteins and Toxins | Beta-lactamases, enterotoxins |
| Class 3 | Secretory System Associated and Capsular Proteins | Type III secretion system apparatus, capsule biosynthesis proteins |
The MP4 classifier has been reported to achieve an accuracy of 81.72% on blind datasets and 79% and 72% on two independent real datasets, demonstrating its utility for functional annotation of hypothetical proteins from novel genomes and metagenomes [75].
Experimental Protocol: Running the MP4 Classifier
Input: The amino acid sequences of predicted proteins (from Prodigal) in FASTA format.
Detailed Methodology:
- Data Preparation: Ensure your input FASTA file contains the protein sequences you wish to classify.
- Feature Extraction: The MP4 tool automatically calculates the input features for its model. These include:
- Dipeptide Frequency: This provides global information on the protein's amino acid composition and local order, calculated as: (Total number of a specific dipeptide / Total number of all possible dipeptides) * 100 [75].
- Pepstats Features: A set of statistical measures of the protein sequence, such as molecular weight, isoelectric point, and amino acid composition.
- Classification: The pre-trained SVM model processes the feature vector for each protein.
- Output Interpretation: The tool provides a classification for each protein (Class 1, 2, or 3) along with a probability score. A higher probability indicates greater confidence in the prediction. The results can be used to calculate a Pathogenicity Index for a sample: (Number of Class 2 sequences + Number of Class 3 sequences) / Total number of sequences [75]. This index helps differentiate pathogenic from non-pathogenic strains.
Systems Biology and Network Analysis
To move beyond a simple list of virulence factors, a systems biology approach is essential. This involves integrating omics data (genomics, transcriptomics) to model the complex interactions between the pathogen and its host [76]. Computational methods can be used to infer and analyze PHI regulatory, metabolic, and protein-protein interaction networks. These network-based analyses can elucidate the dynamic mechanisms of infection and identify critical hubs or pathways that may serve as potential targets for novel therapeutic interventions [76].
The Scientist's Toolkit: Essential Research Reagents and Materials
Table 3: Key Reagents and Tools for Pathogen Bioinformatics Research
| Item | Function/Brief Explanation |
|---|---|
| Sequencing Platform | Generates raw short-read (Illumina) or long-read (Oxford Nanopore, PacBio) data in FASTQ format. |
| High-Performance Computing Cluster | Essential for running computationally intensive tasks like genome assembly and ML classification. |
| Curated Protein Databases | Databases like VFDB, PATRIC, and CARD provide reference data for training ML models and validating predictions [75]. |
| Bioinformatic Suites | Platforms like Galaxy provide a user-friendly, web-based interface for executing many of the tools mentioned without requiring command-line expertise [74]. |
| R/Bioconductor | A free, open-source software project providing 934+ software packages for the advanced statistical analysis and comprehension of high-throughput genomic data [76]. |
The bioinformatic pipeline described herein provides a robust, scalable framework for transforming raw sequencing data into actionable intelligence on bacterial pathogens. By integrating rigorous quality control, sophisticated assembly, and predictive machine learning within a systems biology context, this approach is particularly potent for research aimed at uncovering and characterizing unrecognized human pathogens. As sequencing technologies continue to evolve and AI models become more refined, these pipelines will play an increasingly vital role in accelerating pathogen discovery, informing drug development, and ultimately mitigating the global burden of antimicrobial resistance and infectious diseases.
Overcoming Diagnostic and Therapeutic Dead Ends in a Post-Antibiotic Era
Within the broader research on unrecognized human bacterial pathogens, metagenomic next-generation sequencing (mNGS) has emerged as a transformative diagnostic tool. Its hypothesis-free nature allows for the detection of novel, fastidious, and co-infecting pathogens that traditional culture and targeted molecular assays routinely miss [77]. However, the clinical application of mNGS in diagnosing bacterial pathogens faces two significant technical hurdles: the overwhelming background of host DNA and persistent specificity challenges in bioinformatic analysis. High host nucleic acid concentration in clinical specimens drastically reduces sequencing coverage of microbial genomes, while difficulties in distinguishing true pathogens from background contamination or commensal organisms complicate clinical interpretation [77] [78]. This technical guide provides an in-depth examination of these challenges and outlines validated experimental protocols and analytical frameworks to overcome them, thereby enhancing the reliability of mNGS in the pursuit of discovering and characterizing unrecognized bacterial pathogens.
The Core Challenge: Host DNA Interference
The high abundance of host DNA in clinical samples presents the most significant technical barrier to sensitive pathogen detection via mNGS. In samples such as bronchoalveolar lavage fluid (BALF) and blood, host-derived sequences can constitute over 95% of the total sequencing reads, drastically reducing the effective depth of coverage for microbial genomes and elevating the limit of detection for pathogens [77] [79]. This interference is particularly detrimental for the identification of low-abundance bacterial pathogens, which are often the focus of research into unrecognized infectious agents.
The following table summarizes the impact of host DNA in different clinical sample types:
Table 1: Host DNA Content and Impact Across Clinical Specimens
| Sample Type | Typical Host DNA Proportion | Primary Impact on mNGS | Relevant Pathogen Groups Most Affected |
|---|---|---|---|
| BALF | >95% [79] | Severely reduced microbial sequencing depth; false negatives for low biomass infections. | Intracellular bacteria, fastidious organisms. |
| Blood | >99% in plasma [78] | Extreme dilution of microbial signal; requires ultra-deep sequencing. | Bartonella spp., blood-stream infections with low colony-forming units. |
| Cerebrospinal Fluid | Variable; often lower | Critical impact due to typically low pathogen load in neurological infections. | Mycobacterium tuberculosis, emerging neurotropic bacteria. |
| Tissue Biopsies | >99% [77] | Masking of intracellular pathogens; difficulty in detecting integrated sequences. |
The relationship between host DNA burden, sequencing effort, and pathogen detection sensitivity forms the core diagnostic challenge. One study demonstrated that removing host DNA could significantly enhance the sensitivity of mNGS for detecting SARS-CoV-2 in swab samples, a principle that directly applies to bacterial pathogen detection [80]. Without effective host depletion, the sequencing effort required to detect a single bacterial genome escalates exponentially, making diagnostic procedures cost-prohibitive and technically demanding.
Table 2: Relationship Between Host DNA, Sequencing Depth, and Detection Sensitivity
| Host DNA Proportion | Required Total Reads for 10x Pathogen Coverage | Effective Limit of Detection (Pathogen Reads) | Suitable for Detecting |
|---|---|---|---|
| 99.9% | 100 million | 0.1% | High-abundance pathogens; acute infections. |
| 99% | 10 million | 1% | Moderate-abundance pathogens. |
| 95% (post-depletion) | 1-2 million | 5% | Low-abundance and intracellular pathogens. |
| <90% (efficient depletion) | <1 million | 10% | Very low-abundance and novel pathogens. |
Host Depletion and Pathogen Enrichment Strategies
Overcoming the host DNA background requires a multi-faceted approach involving both wet-lab and computational techniques. The primary wet-lab methods focus on physically separating host cells from microbes, selectively lysing host cells, or enzymatically degrading host nucleic acids.
Wet-Lab Methodologies
1. Differential Centrifugation and Filtration: This protocol leverages size differences between human cells and bacteria. Initial low-speed centrifugation pellets human cells while leaving most bacteria in suspension. The supernatant is then subjected to membrane filtration (e.g., 0.45-0.8 µm pores) to capture microbial cells. DNA is subsequently extracted from the filtered fraction, significantly enriching for microbial DNA [78].
Detailed Protocol:
- Homogenize the sample in a sterile saline buffer.
- Centrifuge at 500 x g for 10 minutes at 4°C to pellet host cells and debris.
- Carefully transfer the supernatant to a new tube.
- Pass the supernatant through a sterile membrane filter with a pore size of 0.45 µm.
- Wash the filter with PBS to remove residual host DNA.
- Either extract DNA directly from the filter or lyse the captured microbial cells for DNA extraction.
2. Selective Lysis of Host Cells: This method uses mild detergents or enzymatic treatments to disrupt eukaryotic cell membranes while leaving bacterial cells intact due to their robust cell walls.
Detailed Protocol:
- Resuspend the sample in a lysis buffer containing 0.1% Triton X-100 or saponin.
- Incubate on ice for 15-30 minutes with gentle agitation.
- Centrifuge at low speed to pellet the intact bacterial cells.
- Wash the pellet with PBS to remove host DNA released during lysis.
- Proceed with standard DNA extraction from the bacterial pellet.
3. Enzymatic Host DNA Depletion: Commercial kits are available that selectively digest methylated eukaryotic DNA (e.g., NEBNext Microbiome DNA Enrichment Kit). This approach is particularly useful for samples where physical separation is difficult.
Detailed Protocol from COVID-19 Study [80]:
- Extract total nucleic acid from a 200 µl swab sample.
- Mix 33µl of nucleic acid with 3µL DNA enzyme and DNA enzyme buffer to digest DNA and enrich for RNA (for RNA pathogens).
- For DNA-focused analysis, use methylation-dependent restriction enzymes.
- Incubate at 37°C for 1 hour.
- Purify the remaining nucleic acids using magnetic beads.
- Proceed to library preparation.
4. Probe-Based Hybridization Capture: This targeted enrichment method uses biotinylated oligonucleotide probes complementary to microbial genomes or universal bacterial genes (e.g., 16S rRNA) to selectively pull down pathogen-derived sequences from a total DNA library [81].
Computational Host Depletion
After sequencing, bioinformatic subtraction of reads aligning to the human reference genome (e.g., GRCh38) is a standard and essential step. This process, while computationally intensive, removes the remaining host-derived sequences from downstream microbial analysis [80] [82]. The unmapped reads are then used for pathogen detection.
The following diagram illustrates a comprehensive workflow integrating both laboratory and computational host depletion methods:
Specificity Challenges and Bioinformatics Solutions
Even after successful host depletion, distinguishing true pathogens from environmental contamination, database errors, and commensal flora remains a critical specificity challenge. This requires a robust bioinformatics pipeline and careful interpretation.
Bioinformatic Workflow for Specific Pathogen Identification
A standardized bioinformatics pipeline is essential for reproducible and specific pathogen detection. The following workflow, adapted from recent studies, outlines the key steps [80] [79] [82]:
- Quality Control and Adapter Trimming: Tools like FastQC and Trimmomatic are used to assess read quality and remove adapters and low-quality bases [80] [82].
- Host Read Subtraction: As described in Section 3.2, reads aligning to the host genome are removed.
- Taxonomic Classification: Non-host reads are classified against a comprehensive microbial database using tools like Kraken2. The database must be carefully curated to include relevant bacterial species and avoid false-positive matches [79].
- Validation and Alignment: Classified reads of interest are realigned using more precise aligners like Bowtie2 or via BLAST against the nucleotide database for final validation, especially when classification tools disagree [79].
- Clinical Correlation and Interpretation: This is the most critical step for ensuring specificity. Detected microbes are categorized based on clinical, radiologic, and laboratory findings. One common framework divides findings into four categories [79]:
- Definite: Microbe known to cause the clinical syndrome with no alternative explanation.
- Probable: Microbe plausibly linked to the syndrome, with supportive clinical context.
- Possible: Microbe with uncertain role; may be a commensal or contaminant.
- Unlikely: Microbe judged to be a contaminant or commensal with no pathogenic role.
Only "definite" and "probable" findings should be considered positive for clinical diagnosis, a crucial guardrail against over-interpretation.
Reagent and Laboratory Controls
Specificity is impossible to ensure without rigorous controls throughout the process. The following table lists essential research reagents and controls required for a reliable mNGS experiment:
Table 3: Research Reagent Solutions for mNGS Specificity
| Reagent/Control Type | Function | Example | Role in Addressing Specificity |
|---|---|---|---|
| Negative Template Control (NTC) | Deters reagent or laboratory contamination. | Sterile deionized water taken through entire extraction and sequencing workflow [79]. | Any microbe detected in the NTC is likely a contaminant and should be filtered from patient samples. |
| Internal Control (Spike-in) | Monitors extraction and amplification efficiency. | Defined quantity of synthetic or non-human pathogen (e.g., phage DNA) [79]. | Ensures the workflow is functionally capable of detection, preventing false negatives. |
| Microbial Reference Materials | Validates assay sensitivity and specificity. | Mock microbial communities with known composition (e.g., ZymoBIOMICS). | Benchmarks the performance of the bioinformatic pipeline and wet-lab methods. |
| DNA/RNA Extraction Kits | Isolates nucleic acids from diverse sample types. | Automated nucleic acid extraction instruments with配套 reagents [80]. | Standardizes input material and reduces batch-to-batch variability. |
| Library Preparation Kits | Prepares sequencing libraries from low-input DNA/RNA. | PMseq RNA infectious pathogens detection kit; Total DNA Library Preparation Kit [80] [79]. | Ensures efficient and unbiased conversion of nucleic acids to a sequencer-compatible library. |
| Curated Microbial Databases | Provides a reference for taxonomic classification. | Custom databases integrating NCBI RefSeq, pathogen-specific genomes. | A comprehensive, well-annotated database is fundamental for accurate taxonomic assignment and avoiding misclassification. |
Case Study: Integrated Approach for Unrecognized Pathogen Detection
A recent prospective study on patients with lung lesions exemplifies the dual utility of mNGS. The study used BALF samples to simultaneously detect pathogens and host copy number variations (CNVs) for cancer diagnosis. The mNGS workflow demonstrated a significantly higher sensitivity for infection diagnosis compared to conventional microbiological tests (56.5% vs. 39.1%) [79]. This was achieved despite the high host DNA background in BALF.
Key Experimental Protocol from the Study [79]:
- Sample Collection: BALF (> 5 mL) was collected and immediately transported on dry ice.
- DNA Extraction and Library Prep: Used an automated system with a Total DNA Library Preparation Kit.
- Sequencing: Illumina NextSeq500, generating 10–20 million reads per sample.
- Bioinformatic Analysis:
- Reads were aligned to the human reference genome (hg19). Unique, mapped reads were used for host CNV analysis.
- Unmapped reads (computationally host-depleted) were aligned to a manually curated microbial database using Kraken2 for classification.
- Potential pathogens were identified based on clinical phenotype and reviewed by senior clinicians.
This case study highlights how a standardized protocol combining laboratory processing and computational analysis can overcome host background issues to provide clinically actionable diagnostic information, even in complex diagnostic scenarios where infection must be distinguished from malignancy.
The challenges of high host DNA background and diagnostic specificity in mNGS are significant but surmountable. A combination of advanced wet-lab depletion techniques, rigorous bioinformatic subtraction, and careful clinical interpretation is essential for unlocking the full potential of mNGS in the search for unrecognized bacterial pathogens. As host depletion methods become more efficient and bioinformatic tools more sophisticated, the sensitivity and specificity of mNGS will continue to improve. For the research community, adhering to standardized protocols, implementing comprehensive controls, and maintaining a skeptical, correlation-driven approach to interpretation are the keys to successfully employing this powerful tool. Overcoming these diagnostic hurdles will not only enhance clinical diagnosis but also accelerate the discovery and characterization of the next generation of human bacterial pathogens.
The escalating crisis of antimicrobial resistance (AMR) poses one of the most severe threats to global public health, with multidrug-resistant (MDR) pathogens causing millions of deaths annually and potentially rendering routine infections fatal [83] [84]. The traditional antibiotic development pipeline has proven insufficient to address this challenge, characterized by prolonged timelines exceeding 10-15 years, costs surpassing $1 billion, and diminishing commercial incentives for pharmaceutical companies [85] [86]. Within this landscape, drug repurposing has emerged as a strategic, pragmatic, and cost-effective approach to rapidly identify novel antibacterial agents from existing pharmacopoeias [85] [87].
Drug repurposing, defined as identifying new therapeutic uses for approved or investigational drugs beyond their original medical indications, offers significant advantages over traditional drug discovery [85] [86]. These advantages include reduced development timelines by approximately 50%, cost savings of over $1 billion per approved drug, lower risk of unforeseen toxicity, and a higher probability of regulatory success [86] [83]. For MDR pathogens, this approach is particularly valuable as repurposed drugs often act via mechanisms distinct from conventional antibiotics, potentially bypassing existing resistance pathways and revitalizing our therapeutic arsenal against superbugs [83] [88].
This technical review examines the methodological frameworks, promising candidates, experimental protocols, and implementation challenges of drug repurposing against MDR bacterial pathogens, with particular focus on its integration into broader research on unrecognized human bacterial pathogens.
Methodological Approaches to Antibacterial Drug Repurposing
Antibacterial drug repurposing employs complementary computational and experimental strategies that can be systematically implemented to identify and validate new therapeutic applications for existing drugs.
Computational Approaches
Computational methods enable the high-throughput screening of extensive drug libraries against bacterial targets, leveraging established algorithms and datasets to generate repurposing hypotheses.
Machine Learning-Based Methods: ML models integrate molecular fingerprints, docking results, and multi-omics datasets to predict repurposing candidates. Deep neural networks optimized via ensemble learning have successfully identified compounds like SU3327 as effective against Escherichia coli from screens of >107 million molecules [85]. Algorithms combining FP2 molecular fingerprints with Random Forest, support vector machine, or multi-layer perception approaches have revealed novel antibacterial structures, suggesting unexplored pathways against MDR pathogens [85].
Structure-Based Virtual Screening: This approach identifies molecules with high target affinity and specificity through computational docking. For instance, fenoprofen, a nonsteroidal anti-inflammatory drug (NSAID), was repurposed as a SaeR inhibitor in Staphylococcus aureus via virtual screening [85]. Similarly, combined docking, molecular dynamics simulations, and QM/MM calculations revealed Lumacaftor's strong binding to the Staphylococcus FemX enzyme, highlighting its therapeutic potential [85].
Signature-Based Matching: This method compares a drug's characteristic profiles with pharmacological agents or clinical phenotypes through multi-omics datasets, adverse event reports, and structural chemistry analyses [85]. For example, researchers integrated S. aureus endophthalmitis transcriptomics with connectivity map analysis, predicting clofilium tosylate and glybenclamide as antimicrobial agents that reverse infection-associated gene signatures [85].
The workflow below illustrates how these computational approaches integrate into a systematic repurposing pipeline:
Experimental Approaches
Experimental validation remains essential for confirming computational predictions and elucidating mechanisms of action against MDR pathogens.
Target-Based Screening: This methodology focuses on specific bacterial targets including cell wall biosynthesis, protein synthesis, nucleic acid metabolism, membrane stability, essential metabolic pathways, and bacterial-specific enzymes [85]. While offering operational simplicity and mechanism-driven discovery with clear therapeutic rationale, this approach faces limitations including target dependency, challenges in novel target identification, high false-positive rates, and potentially narrowed therapeutic scope that may accelerate resistance development [85].
Phenotype-Based Screening: This strategy evaluates compound effects through direct observation of bacterial growth inhibition and viability changes without requiring prior knowledge of specific molecular targets [85]. This approach eliminates target hypothesis-driven screening bias and is particularly effective for identifying multi-target agents. It is adaptable to high-throughput formats but presents challenges in lead optimization due to unclear mechanisms of action and potential off-target effects [85].
Animal Models for Validation: Animal models constitute indispensable tools for the preclinical evaluation of novel antimicrobial compounds. Murine models (mice and rats) are commonly utilized owing to their physiological parallels with humans, facilitating the assessment of drug efficacy, pharmacokinetics, toxicity profiles, and antimicrobial resistance development [85]. Alternative models such as zebrafish, Caenorhabditis elegans, and fruit flies enable rapid and cost-effective screening [85].
The following diagram illustrates the integrated experimental workflow for validating repurposing candidates:
Promising Drug Repurposing Candidates Against MDR Pathogens
Comprehensive screening efforts have identified numerous approved drugs with significant potential for repurposing against MDR pathogens, particularly focusing on the critical ESKAPE pathogens (Enterococcus faecium, Staphylococcus aureus, Klebsiella pneumoniae, Acinetobacter baumannii, Pseudomonas aeruginosa, and Enterobacter species) [83]. These candidates generally fall into two categories: direct antibacterial agents exhibiting intrinsic bactericidal/bacteriostatic activity, and antimicrobial adjuvants including host-directed therapies, antivirulence drugs, and antiresistance drugs [85].
Table 1: Promising Repurposed Drug Candidates Against MDR Pathogens
| Drug Candidate | Original Indication | Target Pathogens | MIC Range | Proposed Antimicrobial Mechanism |
|---|---|---|---|---|
| Auranofin | Rheumatoid Arthritis | S. aureus (including MRSA) | 0.0625-0.5 μg/mL | Inhibits thioredoxin reductase, disrupts redox balance, impairs selenoprotein biosynthesis [85] |
| Ibuprofen | NSAID | S. aureus, E. coli | 500-1,600 mg/L | Cytoplasmic membrane destabilization, potassium ion efflux, altered surface properties [85] |
| Niclosamide | Antihelminthic | ESKAPE pathogens | Variable | Induces oxidative stress, inhibits ATP production, synergistic with polymyxins [83] [88] |
| Ciclopirox | Antifungal | A. baumannii, E. coli, K. pneumoniae, P. aeruginosa | 5-15 μg/mL | Iron chelation, LPS synthesis inhibition, immunomodulation via NLRP3 inflammasome inhibition [88] |
| Pentamidine | Antiparasitic | Multiple Gram-negative | Adjuvant | LPS interaction, increased membrane permeability, antibiotic sensitization [88] |
| Diclofenac | NSAID | Under investigation | Under investigation | Under investigation [85] |
| Thalidomide | Immunomodulatory | Limited direct activity (E. coli MIC=712.5 μg/mL) | Not applicable | Host-directed therapy via TNFα inhibition, benefits in sepsis models [88] |
Direct Antibacterial Agents
Anti-inflammatory Drugs: Auranofin, a gold-containing compound approved for rheumatoid arthritis, demonstrates potent antibacterial activity against multiple S. aureus strains through inhibition of thioredoxin reductase, which disrupts the bacterial redox balance and increases cellular sensitivity to oxidative stress [85]. Its efficacy has been confirmed in multiple animal models, and synergistic interactions have been observed with antibiotics including linezolid, fosfomycin, and ciprofloxacin [85]. Ibuprofen, an NSAID, exhibits inhibitory effects against multiple bacterial species including S. aureus through cytoplasmic membrane destabilization, causing potassium ion efflux and altered surface properties [85].
Antimicrobial Agents: Drugs originally developed against other microbial pathogens frequently demonstrate cross-kingdom antibacterial activity. Ciclopirox, a topical antifungal, shows direct antibacterial activity against clinical isolates of A. baumannii, E. coli, K. pneumoniae, and P. aeruginosa through iron chelation and interference with LPS synthesis [88]. Niclosamide, an anthelmintic, induces oxidative stress and inhibits ATP production in bacterial cells, demonstrating synergy with polymyxins against Gram-negative pathogens [88].
Host-Directed Therapies (HDT) and Adjuvants
Host-directed therapies represent a paradigm shift in antimicrobial strategy by modulating host immune responses rather than directly targeting pathogens, thereby reducing selective pressure for resistance development [84] [88].
Phosphoinositide 3-Kinase (PI3K) Inhibitors: Pathogenic bacteria utilize PI3K to enhance their uptake into host cells, inhibit phagosome maturation, and prevent lysosomal fusion, thereby protecting them from host immune killing and impairing antibiotic efficacy [88]. Combining PI3K inhibitors with antibiotic therapy may improve treatment outcomes for intracellular bacteria and facilitate more effective bacterial clearance [88].
Immunomodulatory Agents: Thalidomide, despite limited direct antibacterial activity, demonstrates benefits in rat sepsis models infected with MDR P. aeruginosa or E. coli through its immunomodulatory activity as a TNFα inhibitor [88]. This host-directed approach modulates the excessive inflammatory response characteristic of severe sepsis without directly targeting the pathogen.
Drugs Affecting NETosis and Iron Metabolism: Therapeutic approaches that enhance immune system activity against bacteria or prevent bacterial utilization of critical host-supplied substances such as iron represent important adjuvant strategies [88]. Iron metabolism manipulation through drugs like ciclopirox simultaneously exerts direct antibacterial effects through chelation while modulating host iron availability to pathogens.
Experimental Protocols for Drug Repurposing
Robust experimental methodologies are essential for validating repurposing candidates and elucidating their mechanisms of action against MDR pathogens.
Protocol for Phenotype-Based Screening
Objective: To identify compounds that inhibit bacterial growth or viability without prior knowledge of specific molecular targets [85].
Materials:
- Bacterial strains: Reference strains and clinical isolates of target MDR pathogens
- Compound library: FDA-approved drugs or investigational compounds
- Culture media: Appropriate broth and agar for each bacterial species
- Microtiter plates: 96-well or 384-well format for high-throughput screening
- Plate reader: Spectrophotometer for optical density measurements
Procedure:
- Prepare logarithmic-phase bacterial inocula adjusted to approximately 5 × 10^5 CFU/mL in appropriate broth.
- Dispense 100 μL aliquots of bacterial suspension into microtiter plates.
- Add test compounds to achieve final concentrations typically ranging from 0.5 to 256 μg/mL.
- Include appropriate controls: growth control (bacteria without compounds), sterility control (media only), and reference antibiotics.
- Incubate plates at appropriate temperature (usually 35-37°C) for 16-20 hours.
- Measure optical density at 600 nm to determine bacterial growth inhibition.
- Calculate minimum inhibitory concentration (MIC) as the lowest compound concentration that inhibits visible growth.
- For bacteriostatic vs. bactericidal determination, subculture wells with no visible growth onto antibiotic-free agar plates to assess viability.
Advanced Applications: For biofilm inhibition assays, allow biofilms to form on plates before compound addition, then quantify biomass using crystal violet staining or metabolic activity assays [85].
Protocol for Checkerboard Synergy Assays
Objective: To evaluate synergistic interactions between repurposed drugs and conventional antibiotics [83].
Materials:
- Bacterial strains: MDR clinical isolates
- Compounds: Repurposed drug candidate and conventional antibiotics
- Culture media: Cation-adjusted Mueller-Hinton broth
- Microtiter plates: 96-well format
Procedure:
- Prepare serial dilutions of the antibiotic in horizontal direction across the microtiter plate.
- Prepare serial dilutions of the repurposed drug candidate in vertical direction.
- Add bacterial suspension to achieve final inoculum of 5 × 10^5 CFU/mL in each well.
- Incubate plates at 35°C for 16-20 hours.
- Determine MICs for each drug alone and in combination.
- Calculate fractional inhibitory concentration index (FICI) using the formula: FICI = (MIC of drug A in combination/MIC of drug A alone) + (MIC of drug B in combination/MIC of drug B alone)
- Interpret results: FICI ≤ 0.5 indicates synergy; >0.5 to ≤1 indicates additive effect; >1 to ≤4 indicates indifference; >4 indicates antagonism [83].
Protocol for In Vivo Efficacy Testing
Objective: To evaluate efficacy of repurposed drugs in animal infection models [85].
Materials:
- Animals: Typically murine models (mice or rats), occasionally alternative models like zebrafish or Galleria mellonella
- Bacterial strains: Bioluminescent engineered strains facilitate in vivo imaging
- Compounds: Repurposed drug candidate, formulation reagents
- Equipment: Injection equipment, in vivo imaging system (if using bioluminescent strains)
Procedure:
- Establish infection model: Common models include neutropenic thigh infection, pneumonia, sepsis, or biofilm-associated device infection.
- Administer bacterial inoculum via appropriate route (intraperitoneal, intravenous, intranasal, or subcutaneous).
- Randomize animals into treatment groups: untreated control, repurposed drug alone, standard antibiotic alone, combination therapy.
- Initiate treatment at predetermined timepoints post-infection, typically 1-2 hours for acute models or 24-48 hours for established infection models.
- Administer compounds via appropriate route (oral, intravenous, intraperitoneal) at clinically relevant doses.
- Monitor survival outcomes, bacterial burden in target organs (quantified by CFU enumeration), and clinical signs of infection.
- Collect tissues for histopathological analysis to assess tissue damage and inflammatory response.
- Analyze pharmacokinetic/pharmacodynamic (PK/PD) parameters to establish exposure-response relationships.
The Scientist's Toolkit: Essential Research Reagents and Solutions
Successful implementation of drug repurposing research requires specific reagents and methodological tools tailored to antibacterial discovery.
Table 2: Essential Research Reagents for Antibacterial Drug Repurposing
| Reagent/Category | Specific Examples | Function/Application | Key Considerations |
|---|---|---|---|
| Bacterial Strains | Reference strains (ATCC), clinical MDR isolates, genetically engineered mutants | Phenotypic screening, mechanism studies, resistance assessment | Include diverse genetic backgrounds; verify resistance profiles; use quality-controlled repositories |
| Cell Culture Media | Mueller-Hinton broth, cation-adjusted MH broth, RPMI for host cells | Standardized antimicrobial susceptibility testing, biofilm models, host-pathogen interaction studies | Follow CLSI guidelines for preparation; validate performance with quality control strains |
| Compound Libraries | FDA-approved drug libraries, bioactive compound collections | High-throughput screening, structure-activity relationship studies | Ensure compound integrity through proper storage; include appropriate controls; verify solubility |
| Analytical Tools | LC-MS/MS, spectrophotometers, fluorescence plate readers | Compound quantification, bacterial growth kinetics, reporter assays | Validate detection methods; establish linear ranges; implement robust data analysis pipelines |
| Animal Models | Murine models, zebrafish, Galleria mellonella | In vivo efficacy testing, pharmacokinetic studies, host-pathogen interactions | Adhere to ethical guidelines; standardize inoculum preparation; include appropriate sample sizes |
Pathway to Clinical Translation and Concluding Perspectives
The translation of repurposed drugs from laboratory findings to clinical application faces several significant challenges despite the accelerated development pathway. Regulatory pathways for repurposed drugs, while more streamlined than for novel chemical entities, still require robust clinical validation of efficacy and safety for the new indication [86]. Intellectual property considerations present complex challenges, with various strategies available including new formulation patents, method-of-use patents, and regulatory exclusivity periods [86].
Clinical development must address specific considerations for repurposed anti-infectives, including appropriate patient populations with MDR infections, determination of optimal dosing regimens that may differ from original indications, and identification of relevant endpoints that demonstrate clinical superiority or non-inferiority to standard care [83]. The CURE ID platform and similar initiatives aim to collect real-world treatment experiences to inform clinical trial design and regulatory decisions, particularly for rare and orphan diseases where traditional trials are challenging [89].
Future directions in antibacterial drug repurposing will likely emphasize several key areas: First, the integration of multi-omics approaches (genomics, transcriptomics, proteomics, metabolomics) to provide comprehensive insights into drug mechanisms and host-pathogen interactions [41]. Second, the development of innovative delivery systems, such as inhaled formulations for respiratory infections or catheter coatings for device-related infections, to enhance targeted exposure while minimizing systemic toxicity [85] [83]. Third, the application of artificial intelligence and machine learning to analyze complex datasets and predict novel drug-pathogen interactions with increasing accuracy [87].
In conclusion, drug repurposing represents a viable, efficient, and strategically important approach to expanding our therapeutic arsenal against MDR pathogens. By leveraging existing pharmacological agents with well-characterized safety profiles, this strategy can significantly reduce the time and cost required to address the escalating AMR crisis. As technological advances in computational prediction, high-throughput screening, and multi-omics integration continue to mature, drug repurposing will play an increasingly vital role in the global response to antimicrobial resistance, complementing traditional antibiotic development and providing much-needed alternatives for treating infections caused by multidrug-resistant superbugs.
The escalating crisis of antimicrobial resistance (AMR) demands a paradigm shift from broad-spectrum therapeutic strategies to precision-targeted approaches. This whitepaper examines the cutting-edge development of narrow-spectrum antibiotics and engineered live biotherapeutic products (LBPs) within the context of unrecognized human bacterial pathogens. These innovative solutions promise to combat resistant infections with unprecedented specificity, preserving the native microbiome and reducing selective pressure for resistance. We detail the mechanistic action of newly discovered antibacterial proteins, AI-accelerated drug discovery pipelines, and sophisticated synthetic biology platforms for engineered therapeutics. The integration of these technologies represents a transformative frontier in our ability to precisely detect, target, and eliminate bacterial pathogens, offering a sustainable framework for addressing the global AMR threat.
The Scientific Rationale for a Narrow-Spectrum Approach
Traditional broad-spectrum antibiotics function as non-discriminative "nukes," effectively eliminating pathogenic bacteria but simultaneously decimating commensal microbes that are critical for human health. This collateral damage disrupts the host's microbiome, creating ecological vacancies that can be exploited by invasive, drug-resistant species—a phenomenon particularly problematic in conditions like inflammatory bowel disease (IBD) [90]. In contrast, narrow-spectrum interventions are founded on the principle of precision strike, targeting only specific pathogens or their essential virulence functions.
This targeted approach offers several distinct advantages in the context of unrecognized and resistant pathogens:
- Reduced Selective Pressure: By sparing the vast majority of the microbiota, narrow-spectrum therapies minimize the selective pressure that drives the evolution and dissemination of broad-spectrum resistance mechanisms.
- Preservation of Microbiome Integrity: A healthy microbiome serves as a protective barrier against colonization by pathogens. Precision therapies maintain this natural defense system.
- Synergy with Diagnostics: The effectiveness of narrow-spectrum agents is amplified when coupled with rapid, precise diagnostic tools that identify the causative pathogen, enabling a tailored therapeutic response.
Breakthroughs in Novel Narrow-Spectrum Agents
A Novel Class of Broad-Spectrum Antibacterial Proteins
Conventional understanding held that bacterially derived antibacterial proteins, which are toxic proteins used in inter-bacterial warfare, typically act only against a narrow range of closely related species due to their dependence on specific surface receptors. However, recent research has uncovered a remarkable exception.
Key Discovery: Investigators at McMaster University have characterized a family of antibacterial proteins that exhibit potent, receptor-independent activity against a broad range of bacteria [91]. This finding fundamentally challenges long-standing dogma in the field.
Quantitative Efficacy Data: Table 1: Pathogen Susceptibility to Novel Antibacterial Proteins
| Pathogen Tested | Associated Disease | Efficacy of Antibacterial Protein |
|---|---|---|
| Listeria | Listeriosis | Eliminated bacterial colonies within 24 hours [91] |
| Staphylococcus | Staph infections | Eliminated bacterial colonies within 24 hours [91] |
| Enterococcus | Urinary tract infections | Eliminated bacterial colonies within 24 hours [91] |
Mechanism of Action: Unlike previously known proteins that require a specific molecular "receptor" for entry or a forced-injection mechanism (secretion system), these newly discovered proteins operate through a unique, energy-dependent process [91]. They are secreted freely into the environment alongside a helper protease enzyme. This protease activates the proteins, enabling them to traverse the membrane of susceptible bacteria directly, without needing a receptor or physical contact between bacterial cells. This novel mechanism explains their ability to target a phylogenetically diverse set of pathogens.
AI-Guided Discovery of a Precision Anti-Inflammatory Antibiotic
The application of artificial intelligence (AI) is dramatically accelerating the discovery and development of new antibiotics, as exemplified by the identification of enterololin, a narrow-spectrum antibiotic for IBD.
Therapeutic Profile: Enterololin is a narrow-spectrum antibiotic designed to selectively target the Enterobacteriaceae family (which includes disease-exacerbating E. coli) while sparing the broader gut microbiome [90]. This makes it a promising therapeutic candidate for Crohn's disease and other IBDs.
AI's Role in Mechanism of Action (MOA) Elucidation: Beyond identifying candidate molecules, AI was used to predict the drug's MOA—a traditionally slow and expensive step in drug development. The AI model DiffDock predicted that enterololin inhibits the LolCDE protein complex, an essential machinery for the survival of certain bacteria [90]. This AI-generated hypothesis was subsequently validated through traditional laboratory experiments, which confirmed the target.
Impact of AI on Development Efficiency: This AI-guided approach yielded a dramatic reduction in both time and cost. The standard MOA study, which typically takes up to two years and costs around $2 million, was completed in just six months for $60,000 [90]. This showcases a powerful new model for streamlining the antibiotic development pipeline.
Engineered Live Biotherapeutic Products (LBPs)
LBPs are genetically modified bacteria designed to function as living in-situ drug delivery systems, providing site-specific deployment of therapeutic payloads to enhance efficacy and minimize off-target effects [92] [93].
Bacteriocin-Based Antimicrobial Platforms
Bacteriocins are ribosomally synthesized antimicrobial peptides naturally produced by bacteria to inhibit competitors. A common chassis for engineering is the safe E. coli strain Nissle 1917 (EcN), which can be outfitted to produce and secrete a tailored arsenal of bacteriocins [92].
Table 2: Engineered Bacteriocin Therapies for Pathogen Control
| Engineered Chassis | Secreted Bacteriocin | Target Pathogen(s) | Activation/Control Mechanism |
|---|---|---|---|
| E. coli Nissle 1917 | Microcin J25 (MccJ25) | Pathogenic E. coli, Salmonella [92] | Constitutive expression [92] |
| E. coli Nissle 1917 | Microcin I47 (MccI47) | ESBL E. coli, Carbapenem-resistant Klebsiella pneumoniae [92] | Constitutive expression [92] |
| E. coli Nissle 1917 | Microcin 47 (Mcc47) | Pathogenic E. coli, Salmonella [92] | Sensing of tetrathionate (an inflammatory metabolite) [92] |
| E. coli Nissle 1917 | Heterologous Bacteriocins | Vancomycin-resistant Enterococci (VRE), Pseudomonas aeruginosa [92] | Use of an E. coli microcin secretion system [92] |
Nanobody Delivery Platforms
Single-domain antibodies, or nanobodies (Nbs), are small (~15 kDa) proteins that can be engineered to bind and neutralize specific pathogen virulence factors. Multiple platforms have been developed for their localized delivery to the gut.
- Surface Display on Gram-Positive Bacteria: Lactobacillus paracasei can be engineered to display viral-neutralizing Nbs on its surface by fusing the Nb to exposed domains of cell wall proteins. This approach has shown efficacy in reducing disease severity and viral load in mouse models of rotavirus infection [92].
- Surface Display on Gram-Negative Bacteria: In E. coli, Nbs can be displayed by fusing them to:
- Secretion via Engineered Systems: The PROT3EcT platform uses commensal E. coli equipped with a modified, tipless Type III Secretion System (T3SS) to directly secrete Nbs into the gut environment. A variant secreting a Nb that blocks an essential EHEC virulence protein delayed infection onset in a mouse model [92].
Detailed Experimental Protocols
Protocol: In Vitro Efficacy Testing of Novel Antibacterial Proteins
This protocol is adapted from the methodology used to characterize the novel antibacterial proteins from McMaster University [91].
Objective: To assess the bactericidal activity of a purified antibacterial protein preparation against a panel of pathogenic bacteria.
Materials:
- Reagent 1: Purified antibacterial protein solution (with associated protease).
- Reagent 2: Lawn of target pathogen (e.g., Listeria, Staphylococcus, Enterococcus) grown to mid-log phase.
- Reagent 3: Solid agar growth media appropriate for the target pathogen.
- Reagent 4: Buffer control.
Methodology:
- Lawn Preparation: Standardize the optical density of the bacterial pathogen culture and spread it evenly onto the surface of the solid agar plate to create a confluent "lawn" of growth.
- Application of Agent: Apply a known volume of the purified antibacterial protein solution directly onto the center of the prepared bacterial lawn.
- Incubation: Incubate the plate at the optimal growth temperature for the pathogen (typically 37°C) for 18-24 hours.
- Analysis: Examine the plate for a zone of clearance (plaque) where bacterial growth has been eliminated. The size and clarity of the zone indicate the potency of the antibacterial protein.
Protocol: Validating AI-Predicted Mechanism of Action
This protocol outlines the validation process for an AI-predicted drug target, as demonstrated for enterololin [90].
Objective: To experimentally confirm that a candidate antibiotic (e.g., enterololin) functions through a specific, AI-predicted molecular target (e.g., the LolCDE complex).
Materials:
- Reagent 1: The candidate antibiotic (enterololin).
- Reagent 2: Bacterial strains: a wild-type strain and an isogenic mutant strain with modifications in the predicted target (e.g., LolCDE complex).
- Reagent 3: Growth medium (e.g., Mueller-Hinton broth).
- Reagent 4: Microdilution plates.
Methodology:
- Minimum Inhibitory Concentration (MIC) Determination:
- Prepare serial two-fold dilutions of the candidate antibiotic in a liquid growth medium within a microdilution plate.
- Inoculate each well with a standardized inoculum (~5 x 10^5 CFU/mL) of either the wild-type or the target-modified mutant strain.
- Incubate the plates at 37°C for 16-20 hours.
- Data Analysis:
- The MIC is defined as the lowest concentration of antibiotic that completely inhibits visible growth.
- Key Validation: A significantly higher MIC (indicating resistance) in the mutant strain compared to the wild-type strain provides strong genetic evidence that the antibiotic's activity is dependent on the integrity of the predicted target pathway.
The Scientist's Toolkit: Research Reagent Solutions
Table 3: Essential Research Reagents for Developing Precision Antimicrobials
| Reagent / Tool | Function in Research | Specific Example / Application |
|---|---|---|
| Engineered Bacterial Chassis | Safe, customizable platform for therapeutic delivery. | E. coli Nissle 1917 (EcN); Lactobacillus species [92] [93]. |
| Bacteriocin Gene Clusters (BGCs) | Genetic source for antimicrobial peptides with targeted activity. | Microcin J25, I47, and Mcc47 for targeting Enterobacteriaceae [92]. |
| Nanobodies (Nbs) | Small, high-affinity binding proteins to neutralize virulence factors. | Nb against EHEC virulence protein delivered via PROT3EcT platform [92]. |
| Specialized Secretion Systems | Enable display or secretion of therapeutic payloads from engineered bacteria. | Type III Secretion System (PROT3EcT); Curli fiber (CsgA) display system [92]. |
| Intracellular Sensing Promoters | Control transgene expression specifically inside host cells. | Salmonella SPI-2 promoters (e.g., PsseA, PsseJ) for intracellular activation [94]. |
| Bacterial Lysis Proteins | Facilitate escape of therapeutic cargo from bacteria into host cells. | Phage-derived protein E and pore-forming HlyE for vacuole escape [94]. |
Technical Diagrams of Key Systems
Bacterial Secretion and Pathogen Neutralization
Diagram: Engineered bacteria use surface display or secretion systems to deliver therapeutic payloads that neutralize pathogen virulence factors.
AI-Guided Antibiotic Discovery Workflow
Diagram: AI rapidly predicts a drug's mechanism of action, which is then validated through traditional laboratory experiments.
The field of precision antimicrobials is advancing on multiple fronts. Beyond the strategies discussed, technologies like engineered bacterial-viral consortia (e.g., CAPPSID, where bacteria deliver oncolytic viruses to tumors) and CRISPR/Cas-based pathogen targeting are expanding the toolkit for complex infections and microbiome editing [92] [94]. The growing threat of antifungal resistance, highlighted by WHO's "critical priority" fungal pathogens, further underscores the need to extend these precision principles beyond bacteria [95].
Conclusion: The paradigm is irrevocably shifting from indiscriminate bombardment to intelligent, targeted warfare against bacterial pathogens. The convergence of foundational microbiology, synthetic biology, and artificial intelligence is producing a new generation of narrow-spectrum antibiotics and engineered living medicines. These tools offer the potential to treat resistant infections more effectively, preserve our protective microbiomes, and steward the longevity of our antimicrobial resources. For researchers and drug development professionals, the future lies in the continued refinement of these precision strike capabilities, demanding interdisciplinary collaboration to translate these powerful concepts from the laboratory bench to the patient bedside.
The escalating crisis of antimicrobial resistance represents one of the most severe threats to global health systems, with Gram-negative pathogens such as Escherichia coli, Klebsiella pneumoniae, Pseudomonas aeruginosa, and Acinetobacter baumannii having evolved resistance to most clinically available antibiotics [96]. The World Health Organization has classified these drug-resistant pathogens as a critical priority, underscoring the urgent need for novel antibiotics with new mechanisms of action that circumvent existing resistance pathways [96]. For Gram-negative bacteria specifically, the problem is exacerbated by their highly restrictive permeability barrier, which limits the penetration of most compounds [96]. Notably, the last class of antibiotics acting against Gram-negative pathogens was developed in the 1960s, followed by decades of discovery limited largely to narrow-spectrum compounds [96]. This review examines two groundbreaking antibiotic classes—teixobactin and darobactin—that employ novel mechanisms of action to target highly conserved bacterial structures, thereby presenting significant barriers to resistance development and offering promising therapeutic avenues against multidrug-resistant pathogens.
Teixobactin: A Dual-Pronged Attack on the Cell Envelope
Discovery and Structural Features
Teixobactin, isolated from the previously uncultured soil bacterium Eleftheria terrae, represents the first member of a new class of antibiotics with a unique chemical scaffold and a notable lack of detectable resistance [97] [98]. This macrocyclic depsipeptide natural product is an undecapeptide containing five non-canonical amino acids, including four D-amino acids and the rare cationic L-allo-enduracididine localized in a C-terminal depsi-cycle [97] [99]. Its structure consists of 11 amino acids forming a 13-membered macrocycle between the side chain of D-Thr8 and the C-terminus [100]. The complex synthesis of teixobactin, particularly the challenging L-allo-enduracididine precursor, has prompted the development of active analogues such as Leu10-teixobactin, which exhibits comparable activity and is widely used in research [100].
Unique Dual Mechanism of Action
Teixobactin employs an unprecedented two-pronged attack on the bacterial cell envelope, simultaneously inhibiting cell wall biosynthesis and compromising membrane integrity [97].
Target Sequestration Mechanism: Teixobactin specifically binds to the essential cell wall precursors lipid II (involved in peptidoglycan biosynthesis) and lipid III (involved in teichoic acid biosynthesis) [98] [101]. The unique C-terminal enduracididine headgroup of teixobactin specifically recognizes the conserved pyrophosphate-sugar moiety of lipid II, while the N-terminus coordinates the pyrophosphate of another lipid II molecule [97]. This configuration enables the formation of a β-sheet of teixobactin molecules bound to lipid II, creating stable supramolecular fibrillar structures on membrane surfaces [97] [98]. These fibrillar complexes sequester lipid II, making it unavailable for peptidoglycan biosynthesis and effectively halting cell wall construction [98].
Membrane Disruption Mechanism: The supramolecular structures formed by teixobactin and lipid II compromise bacterial membrane integrity through a sophisticated physical mechanism [97]. High-speed atomic force microscopy and molecular dynamics simulations reveal that these fibrillar structures initially form on the membrane surface but subsequently descend into the membrane bilayer, causing substantial membrane thinning of approximately 0.5 nm [97]. This membrane perturbation occurs because the supramolecular structure displaces phospholipids and concentrates the long hydrophobic tails of lipid II within the complex, collectively contributing to membrane disruption [97].
Table 1: Key Experimental Findings on Teixobactin's Mechanism of Action
| Experimental Approach | Key Findings | Significance |
|---|---|---|
| Solid-state NMR spectroscopy | Teixobactin forms antiparallel β-sheets upon binding lipid II; ring motif coordinates lipid II pyrophosphate | Reveals atomic-level interaction interface and oligomerization mechanism [97] [98] |
| Metabolomics profiling | Perturbation of membrane lipids, peptidoglycan, and teichoic acid biosynthesis pathways; suppression of D-alanyl-D-lactate | Confirms dual action on cell wall synthesis and membrane integrity; explains lack of cross-resistance with vancomycin [100] |
| High-speed atomic force microscopy | Fibril formation on membranes containing lipid II; membrane thinning of ~0.5 nm | Visualizes real-time formation of supramolecular structures and membrane disruption [97] |
| Fluorescence microscopy | Micron-sized cluster formation on membranes; compact clusters in bacteria within 15-45 minutes | Demonstrates rapid target sequestration in biological systems [97] [98] |
Resistance Profile
A distinctive characteristic of teixobactin is its remarkable resistance to resistance development [101]. Notably, Staphylococcus aureus did not develop resistance to teixobactin after 27 consecutive passages in the presence of the drug [101]. This resistance-resistant profile stems from teixobactin's targeting of non-proteinogenic cell wall precursors (lipid II and lipid III) that are not directly encoded by DNA but are products of multi-enzyme pathways [101]. The conserved nature of the pyrophosphate-sugar binding motif makes it difficult for bacteria to achieve sufficient structural modification through simple mutations, while the dual-targeting approach further elevates the barrier to resistance development [97] [101].
Darobactin: Targeting the Gram-Negative Outer Membrane
Discovery and Structural Features
Darobactin represents a recently discovered antibiotic class with potent activity against Gram-negative pathogens, addressing a critical gap in the antibiotic arsenal [96]. This novel compound was identified through a screen of Photorhabdus symbionts from entomopathogenic nematode microbiomes, based on the rationale that bacterial symbionts of animals might produce antibiotics with properties suitable for development into human therapeutics [96]. Darobactin is a modified heptapeptide (W-N-W-S-K-S-F) with an unusual structure containing two fused rings that form post-translationally: an unprecedented aromatic-aliphatic ether linkage between the C7 indole of W1 and the β-carbon of W3, and a carbon-carbon bond between the C6 indole of W3 and the β-carbon of K5 [96]. The formation of a carbon-carbon bond between two unactivated carbons is particularly unique for an antibiotic [96].
Biosynthetic Pathway
Darobactin is ribosomally synthesized as a precursor peptide, representing a new class of ribosomally synthesized and post-translationally modified peptide (RiPP) natural products [96]. The darobactin biosynthetic operon (darABCDE) includes DarA, which encodes the precursor peptide; DarE, a radical SAM enzyme that catalyzes the formation of both unusual cross-links; and DarB, DarC, and DarD, which form an ABC-type transenvelope exporter [96]. The darobactin operon is naturally silent under standard laboratory conditions, requiring extended fermentation (10-14 days) for detection, which likely explains why it was overlooked in previous screens [96]. Genomic analyses have revealed the existence of multiple darobactin analogs (darobactin B-E) in various bacterial species, including Yersinia pestis, suggesting this class represents a family of naturally occurring antibiotics [96].
Novel Mechanism: BamA Inhibition
Darobactin exerts its antibacterial activity through a novel mechanism involving targeting BamA, an essential outer membrane protein in Gram-negative bacteria [96]. BamA functions as a chaperone and translocator that folds and inserts outer membrane proteins, making it essential for bacterial viability and outer membrane integrity [96]. Mutants resistant to darobactin consistently map to the bamA gene, confirming it as the primary target [96]. By inhibiting BamA function, darobactin compromises the integrity of the outer membrane, a structure that normally protects Gram-negative bacteria from antimicrobial compounds [96]. This mechanism is particularly significant because it represents the first known antibiotic class to target this essential component of the Gram-negative outer membrane assembly machinery.
Table 2: Comparative Analysis of Teixobactin and Darobactin
| Property | Teixobactin | Darobactin |
|---|---|---|
| Source | Uncultured soil bacterium Eleftheria terrae [97] | Nematode symbionts Photorhabdus spp. [96] |
| Chemical Class | Macrocyclic depsipeptide [99] | Modified ribosomally synthesized peptide (RiPP) [96] |
| Molecular Target | Lipid II and lipid III [97] [101] | BamA outer membrane protein [96] |
| Spectrum | Gram-positive bacteria [100] | Gram-negative pathogens [96] |
| Resistance Development | Not detected in laboratory settings [101] | Resistance maps to target mutations [96] |
| Key Structural Feature | L-allo-enduracididine [97] | Dual fused rings with C-C and C-O-C bridges [96] |
Experimental Methodologies for Mechanism Elucidation
Solid-State NMR Spectroscopy for Membrane Protein Complexes
Solid-state NMR (ssNMR) spectroscopy has proven indispensable for elucidating the mechanisms of both teixobactin and darobactin at atomic resolution under native membrane conditions [97] [98]. For teixobactin studies, researchers incorporate uniformly ¹³C,¹⁵N-labeled antibiotic (produced via native host cultivation or synthetic labeling) into lipid bilayers containing the target molecules (lipid II or lipid III) [97] [98]. Key experiments include:
- 2D ¹³C-¹³C correlation spectra: Employ dipolar-based magnetization transfer (PARISxy) to identify through-space correlations between teixobactin and labeled lipid II, defining the binding interface [97].
- 2D ¹H-³¹P spectra: Determine coordination between antibiotic backbone protons and the lipid II pyrophosphate moiety through heteronuclear correlation experiments with varying contact times (1-2 ms) [97] [98].
- 3¹P chemical shift analysis: Monitor changes in lipid II pyrophosphate signals upon antibiotic binding to confirm direct interaction [98].
- Mobility-edited experiments: Differentiate rigid (complex-bound) and mobile components to determine membrane topology [98].
This approach revealed that teixobactin's ring motif (residues Thr8-Ile11) directly coordinates the lipid II pyrophosphate, while the N-terminus forms β-strands that mediate oligomerization [97] [98].
Metabolomics for Pathway Analysis
Metabolomic profiling provides systems-level insights into the bacterial response to antibiotic treatment, as demonstrated in studies of teixobactin's mechanism [100]. The standard protocol involves:
- Bacterial treatment: Expose MRSA cultures (e.g., S. aureus ATCC 700699) to sub-MIC concentrations of teixobactin analogue (e.g., 0.5 μg/mL Leu10-teixobactin) for defined intervals (1, 3, and 6 hours) [100].
- Metabolite extraction: Use quenching solutions (cold methanol) to rapidly halt metabolism, followed by extraction with appropriate solvent systems [100].
- LC-MS analysis: Employ untargeted liquid chromatography-mass spectrometry with reverse-phase columns to separate and detect intracellular metabolites [100].
- Data analysis: Utilize multivariate statistical methods (PCA, OPLS-DA) to identify significantly perturbed metabolic pathways, including cell envelope precursors, central carbon metabolism, and amino acid biosynthesis [100].
This approach confirmed teixobactin's profound impact on cell envelope biosynthesis, revealing perturbations in peptidoglycan precursors (lipid I, lipid II), teichoic acid precursors (lipid III), and membrane lipids, while simultaneously suppressing key intermediates involved in vancomycin resistance [100].
High-Speed Atomic Force Microscopy for Real-Time Visualization
High-speed atomic force microscopy (HS-AFM) enables direct visualization of antibiotic action on membrane surfaces in real time [97]. The methodology includes:
- Membrane preparation: Create supported lipid bilayers containing incorporated lipid II (typically 1-5 mol%) [97].
- Image acquisition: Perform HS-AFM in liquid phase at room temperature with high scan rates (1-2 frames per second) using ultrashort cantilevers [97].
- Antibiotic addition: Introduce teixobactin directly to the imaging chamber while continuously scanning membrane surfaces [97].
- Topographical analysis: Measure height profiles of membrane surfaces before and after fibril formation to quantify membrane thinning [97].
This technique directly captured the formation of teixobactin-lipid II fibrils (height: 0.8 ± 0.1 nm) and their subsequent reorganization into fibrillar sheets that embedded into the membrane, causing ~0.5 nm membrane thinning [97].
Genetic Approaches for Target Identification
For darobactin, genetic screening identified the molecular target through resistance mapping [96]. The experimental workflow involves:
- Mutant generation: Isolate spontaneous darobactin-resistant mutants through serial passage in sub-inhibitory antibiotic concentrations [96].
- Whole-genome sequencing: Sequence resistant strains and compare to parent strain to identify mutations [96].
- Target validation: Introduce identified mutations into susceptible strains via allelic exchange to confirm causality [96].
- Operon analysis: Identify biosynthetic genes through genome mining and confirm involvement via knockout/complementation [96].
This approach revealed that darobactin resistance mutations consistently mapped to bamA, encoding an essential outer membrane protein, thereby identifying it as the primary target [96].
The Scientist's Toolkit: Essential Research Reagents
Table 3: Key Reagents for Studying Novel Antibiotic Mechanisms
| Reagent/Category | Specific Examples | Research Application |
|---|---|---|
| Isotope-Labeled Antibiotics | ¹³C,¹⁵N-teixobactin; ¹³C,¹⁵N-darobactin precursors | Solid-state NMR studies for structural characterization and binding interface mapping [97] [98] |
| Fluorescent Probes | Atto 550-tagged lipid II; NBD-labeled lipid II; pyrene-tagged lipid II | Visualization of target sequestration and oligomerization via fluorescence microscopy and spectroscopy [97] [98] |
| Membrane Model Systems | DOPC liposomes; giant unilamellar vesicles (GUVs); supported lipid bilayers | Biophysical studies of antibiotic-membrane interactions under controlled conditions [97] [98] |
| Bacterial Strains | MRSA ATCC 700699; E. coli MG1655; Photorhabdus khanii HGB1456 | Antimicrobial activity assessment; resistance development studies; natural product production [96] [100] |
| Specialized Enzymes | Radical SAM enzymes (DarE homologs); peptidoglycan glycosyltransferases | Mechanistic studies of biosynthesis and molecular target activity [96] |
Visualizing Mechanisms and Methodologies
Teixobactin's Dual Mechanism of Action
Darobactin Biosynthesis and Mechanism
Research Gaps and Future Directions
While teixobactin and darobactin represent significant breakthroughs in antibiotic discovery, several research gaps remain. For teixobactin, the limited activity against Gram-negative pathogens presents a major constraint, though its unique resistance-resistant properties make it an excellent candidate for further optimization against Gram-positive infections [99]. Structure-activity relationship studies have identified key residues for activity, informing the design of analogues with improved pharmacological properties [99]. For darobactin, the naturally low production yield and challenges in chemical synthesis present hurdles for large-scale development, while its exclusive Gram-negative spectrum limits broad-spectrum applications [96]. Future research should focus on leveraging the novel mechanisms of these compounds to develop broader-spectrum analogues, exploring potential synergistic combinations with existing antibiotics, and further elucidating the structural basis of their target interactions to enable rational drug design. The ongoing exploration of uncultured bacteria and symbiotic microbiomes continues to reveal promising antimicrobial candidates with unprecedented mechanisms, offering hope in the battle against multidrug-resistant pathogens [96] [102].
The Scale of the Crisis: A Dwindling Pipeline amid Rising Resistance
The World Health Organization (WHO) reports a 40 percent jump in global antibiotic resistance between 2018 and 2023, finding that approximately one in six laboratory-confirmed bacterial infections were resistant in 2023 [103]. This escalating threat is met with a clinical pipeline that is both shrinking and lacking in innovation. As of 2025, only 90 antibacterial agents are in clinical development, down from 97 in 2023. Among these, a mere 15 are considered innovative, and only 5 are effective against WHO "critical priority" pathogens such as carbapenem-resistant Acinetobacter baumannii (CRAB) [37]. This combination of rising resistance and a failing innovation pipeline represents a fundamental threat to modern medicine, undermining the treatment of routine infections and the safety of surgical procedures, from C-sections to cancer chemotherapy [103] [104].
Table: Key Metrics of the Antibacterial Clinical Pipeline (2025)
| Metric | 2023 | 2025 | Context & Implication |
|---|---|---|---|
| Total Agents in Clinical Pipeline | 97 | 90 | Highlights a shrinking global effort [37] |
| Innovative Agents | N/A | 15 | Majority are modifications of existing classes [37] |
| Agents Targeting Critical WHO Pathogens | N/A | 5 | Insufficient focus on the most urgent threats [37] |
| Preclinical Agents | N/A | 232 | Early innovation is high-risk and dominated by small firms (90%) [37] |
The economic burden of Antimicrobial Resistance (AMR) is staggering, with treatment for resistant infections adding up to $29,000 per patient in hospital settings [105]. The "antibiotic discovery void" persists; since 2000, only five novel classes of antibiotics have been marketed, and no new class has been developed for Gram-negative bacteria in over 50 years [105] [106]. This innovation drought is particularly alarming given the rapid evolution of bacterial pathogens, which can develop resistance to a new antibiotic within a year of its introduction [106].
Analyzing the Economic and Regulatory Barriers to Development
The Broken Commercial Model
The core economic problem is that the net present value of a new antibiotic is close to zero, making it impossible for companies to recoup research and development (R&D) investments [107] [104]. This market failure stems from several interconnected factors:
- Short Treatment Duration & Stewardship: Unlike drugs for chronic conditions, antibiotics are typically used for short courses. Furthermore, to preserve their efficacy, new antibiotics are often held in reserve as "last-line" treatments, deliberately limiting their use and sales volume [104]. This creates a perverse incentive structure where a successful, life-saving antibiotic is intentionally not marketed aggressively.
- Inadequate Revenue vs. Development Cost: The average revenue for a new antibiotic in its first eight years on the market is approximately $240 million in total, with the U.S. accounting for 84% of sales [107]. This revenue is insufficient against mean development costs of $1.3 billion for systemic anti-infectives [107]. Post-approval costs for manufacturing, marketing, and regulatory compliance can add another $240-622 million over five years, pushing companies into bankruptcy even after gaining regulatory approval, as seen with Achaogen after it received approval for plazomicin [107].
- High Cost of Clinical Trials: Trials for antibiotics, particularly those targeting resistant infections, are exceptionally challenging and expensive. The Achaogen trial for plazomicin against CRE infections was estimated to cost $1 million per recruited patient after screening 2,000 patients to enroll only 39 [107]. Regulatory requirements for non-inferiority trials often demand thousands of patients across multiple sites, further driving up costs [107].
Table: Comparative Analysis of Antibiotic R&D Economic Challenges
| Factor | Impact on Antibiotic R&D | Contrast with Other Drug Classes (e.g., Oncology) |
|---|---|---|
| Return on Investment (ROI) | Negative or near-zero net present value [107] | High; chronic use and premium pricing drive sustained revenue [105] |
| Market Size & Utilization | Deliberately restricted by stewardship [104] | Encouraged for widespread and long-term use |
| Clinical Trial Cost & Complexity | Extremely high; difficult to enroll patients with resistant infections [107] | While costly, patient recruitment is generally more straightforward |
| Success Reward | High risk of commercial failure and bankruptcy post-approval [107] | Commercial success and blockbuster sales are common goals |
The "Brain Drain" and Corporate Exodus
The economic disincentives have triggered a mass exodus of large pharmaceutical companies from antibiotic R&D. Since the 1990s, 18 major pharmaceutical companies have exited the field, including AstraZeneca, Novartis, and Sanofi [105]. This has resulted in a devastating "brain drain"; it is estimated that only about 3,000 AMR researchers remain active globally [107]. The antibiotic INDs (Investigational New Drug applications) filed by large companies have plummeted from over 75% of the total in the 1980s to under 20% in the 2010s [107]. The ecosystem is now reliant on small biotech firms and academia, entities that lack the capital to bring a drug through late-stage clinical trials and onto the global market [37].
Regulatory and Reimbursement Hurdles
The regulatory pathway for antibiotics, while containing expedited designations, often falls behind other antimicrobials in utilization [108]. Furthermore, the reimbursement model is fundamentally misaligned with public health needs. Insurance companies are often reluctant to cover newer, more expensive antibiotics as a first-line treatment, preferring older, generic alternatives [104]. This creates a "valley of death" where a newly approved drug, despite its clinical need, generates insufficient revenue to sustain the company that developed it.
Pathways to Overcoming the Roadblocks
Policy and Economic Solutions: "Push" and "Pull" Incentives
Experts and global bodies agree that a multi-pronged strategy combining "push" and "pull" incentives is essential to revitalize the antibiotic pipeline [103].
- Push Funding: These mechanisms lower the upfront costs and risks of R&D. Organizations like CARB-X (Combating Antibiotic-Resistant Bacteria Biopharmaceutical Accelerator) provide funding and expert support to early-stage projects. Since 2016, CARB-X has distributed over $450 million, helping push three new products to market and a dozen more into clinical trials [103]. Sustained public funding for such push mechanisms is a critical first step [103].
- Pull Incentives: These are designed to create a predictable and sufficient market reward for successfully bringing a new antibiotic to market. This is widely seen as the most critical intervention to repair the broken commercial model. Models include revenue guarantees and subscription-style models, such as the UK's NHS pilot, where developers are paid an annual subscription fee for access to a drug, delinked from the volume of sales [103] [106]. The proposed PASTEUR Act in the U.S. is a similar delinked pull incentive [108].
Scientific Innovation and Alternative Approaches
Beyond traditional small molecules, the field is exploring non-traditional therapies to overcome resistance. The current clinical pipeline includes 40 non-traditional agents, such as bacteriophages, lysins, antibodies, and microbiome-modulating therapies [107] [37].
A key regulatory breakthrough for one such alternative, phage therapy, occurred in France with the authorization of a personalized phage therapy platform for veterinary use [109]. Unlike traditional drug approval for a single, static formulation, this platform approach establishes a validated framework for producing tailored phage combinations. This allows the medicine to evolve alongside bacterial resistance, a significant step forward for biological medicines [109].
Promising clinical-stage candidates are also emerging. Roche's zosurabalpin, the first new class of antibiotic in 50 years to target CRAB, is advancing into Phase 3 trials. It works by disrupting the transport of lipopolysaccharide, a key component of the bacteria's protective outer membrane [106]. Another candidate, Venatorx's cefepime-taniborbactam, a beta-lactam/beta-lactamase inhibitor combination, showed promise in Phase 3 trials for complicated UTIs, despite a recent FDA rejection citing manufacturing concerns [106].
The Critical Role of Public Funding and Diagnostics
Government-funded research is an irreplaceable component of the antibiotic R&D ecosystem. It supports basic research into bacterial mechanisms and funds high-risk inquiries that lack immediate profit potential [110]. Recent cuts to the U.S. National Institutes of Health (NIH) budget, including the termination of grants with foreign subawards, threaten to disproportionately impact antibiotic research, which is heavily reliant on public funding [104] [110]. This comes at a time when AMR is projected to cause 10 million deaths annually by 2050 if left unchecked [105].
Strengthening diagnostic capacity is another critical pillar. Rapid, point-of-care diagnostics are essential for implementing effective antibiotic stewardship, as they enable clinicians to distinguish between bacterial and viral infections and to select the most appropriate antibiotic quickly [103] [37]. Without these tools, even the most innovative antibiotics will be used empirically, accelerating the development of resistance.
The Scientist's Toolkit: Key Reagents for Antibiotic Discovery
Table: Essential Research Reagents and Tools for Modern Antibiotic R&D
| Reagent / Tool | Core Function | Application in Antibiotic Discovery |
|---|---|---|
| Actinomycetes & Soil Microbe Libraries | Natural product screening for novel compounds [105] | Rediscovery of antibiotics using platforms like the Waksman platform; source of new chemical scaffolds [105]. |
| Specialized Growth Media | To culture fastidious environmental bacteria [104] | Enables the "unculturable" majority of soil microbes to be grown in the lab, expanding the pool of discoverable antibiotics [104]. |
| CRISPR-Cas Systems | Gene editing and target validation [107] | Used to elucidate bacterial gene function and identify new, essential targets for antibiotic development [107]. |
| Lipopolysaccharide (LPS) Transport Assays | Measure disruption of outer membrane synthesis [106] | Critical for characterizing novel antibiotics like zosurabalpin that target Gram-negative outer membrane biogenesis [106]. |
| Bacteriophage Libraries | Collections of bacteria-specific viruses [109] | Sourced for developing personalized phage therapy cocktails to treat multi-drug resistant infections [109]. |
| Beta-Lactamase Enzymes | Enzymes that confer resistance to beta-lactam antibiotics [106] | Used in screens to identify and characterize new beta-lactamase inhibitors (e.g., taniborbactam, vaborbactam) [106]. |
The abandonment of antibiotic R&D by the pharmaceutical industry is a rational response to profound economic and regulatory roadblocks. The combination of scientific difficulty, a broken commercial model that fails to reward innovation, and a dwindling specialized workforce has created a perfect storm. The consequences are dire: a dangerously thin pipeline incapable of addressing the rapid rise of pan-resistant infections. Reversing this trend requires a concerted, global effort that includes robust "push" and "pull" financial incentives, regulatory innovation for both traditional and non-traditional therapies, and sustained public investment in basic research. Without such a comprehensive strategy, the world risks a return to the pre-antibiotic era, where routine infections and minor surgeries once again become life-threatening events.
Benchmarking Breakthroughs: Validating New Diagnostics Against Gold Standards
The precise and timely identification of pathogens in clinical body fluid samples is a cornerstone of effective infectious disease management, yet it remains a significant diagnostic challenge. Traditional culture-based methods, long considered the gold standard, are increasingly being supplemented or supplanted by molecular techniques, most notably metagenomic next-generation sequencing (mNGS). This technical guide provides a comprehensive comparison of the sensitivity and specificity of mNGS versus culture techniques, framing this evolution within the broader research context of identifying previously unrecognized human bacterial pathogens. For researchers and drug development professionals, understanding these diagnostic performance characteristics is critical for advancing both clinical diagnostics and fundamental pathogen discovery.
The limitations of conventional culture are particularly pronounced when investigating rare or novel pathogens. As highlighted by research into rare human pathogenic bacteria, "routine clinical diagnostics are geared towards detecting the known human pathogenic bacteria," which creates considerable problems when encountering novel species whose clinical relevance is unknown [111]. Culture-based methods inherently fail to detect uncultivable or fastidious organisms, and their efficacy is substantially diminished by prior antibiotic exposure [112]. These limitations directly impede research progress into the vast diversity of unrecognized pathogens, estimated to include between 10⁷ and 10⁹ unknown bacterial species [111].
mNGS offers a culture-independent approach that can detect a broad spectrum of pathogens directly from clinical samples, including viruses, fungi, parasites, and bacteria that cannot be cultivated by standard methods. This capability makes it particularly valuable for hypothesis-free pathogen detection in cases where conventional methods have failed or when investigating potential emerging pathogens. However, the adoption of mNGS necessitates a thorough understanding of its analytical performance compared to established methods, specifically regarding sensitivity and specificity across diverse sample types and clinical scenarios.
Performance Comparison: Quantitative Data Analysis
Numerous recent studies have directly compared the diagnostic performance of mNGS and culture methods across various body fluid sample types. The table below summarizes key quantitative findings from contemporary research, providing researchers with a consolidated view of the current evidence base.
Table 1: Comparative Diagnostic Performance of mNGS vs. Culture in Clinical Body Fluid Samples
| Study & Sample Type | Sensitivity (%) | Specificity (%) | Positive Predictive Value (%) | Negative Predictive Value (%) | Sample Size (n) |
|---|---|---|---|---|---|
| Febrile Patients (Multiple Sample Types) [112] | 58.01 (mNGS) vs. 21.65 (Culture) | 85.40 (mNGS) vs. 99.27 (Culture) | 87.01 (mNGS) vs. 98.84 (Culture) | 54.67 (mNGS) vs. 42.90 (Culture) | 368 patients |
| Spinal Infections (Meta-Analysis) [113] | 81 (mNGS) vs. 34 (TCT) | 75 (mNGS) vs. 93 (TCT) | - | - | 770 patients (10 studies) |
| Clinical Body Fluids (wcDNA mNGS) [60] | 74.07 | 56.34 | - | - | 125 samples |
| Organ Preservation & Wound Drainage Fluids [114] | Positive Rate: 47.5% (mNGS) vs. 24.8% (Culture) in preservation fluids; 27.0% (mNGS) vs. 2.1% (Culture) in drainage fluids | - | - | - | 141 patients |
The consistent theme across these studies is the markedly higher sensitivity of mNGS compared to culture-based methods, with a corresponding trade-off of generally lower specificity. In the study of febrile patients, mNGS demonstrated nearly three times the sensitivity of culture (58.01% vs. 21.65%), enabling pathogen detection in many cases where culture failed [112]. This enhanced detection capability is particularly valuable for identifying uncultivable or difficult-to-cultivate species and in patients with prior antibiotic exposure, where culture performance is notably compromised.
The meta-analysis of spinal infections provides particularly compelling evidence, synthesizing data from 10 studies involving 770 patients. The pooled sensitivity of mNGS was 0.81 (95% CI, 0.74–0.87) compared to just 0.34 (95% CI, 0.27–0.43) for traditional tissue culture techniques (TCT) [113]. The area under the summary receiver operating characteristic curve (AUC) was 0.85 for mNGS versus 0.59 for TCT, indicating superior overall diagnostic accuracy of the molecular approach.
The specificity differential is equally important for researchers to consider. Culture methods maintain exceptionally high specificity (99.27% in febrile patients; 93% in spinal infection meta-analysis), meaning false positives are rare [112] [113]. mNGS specificity is more variable, ranging from 56.34% in body fluid samples to 85.40% in febrile patients [112] [60]. This lower specificity reflects the technique's ability to detect background DNA, contaminants, colonizing organisms, and non-viable pathogens, all of which can complicate result interpretation without clinical correlation.
Table 2: Performance Variation by Sample Type and Pathogen Category
| Factor | Impact on mNGS Performance | Impact on Culture Performance | Clinical/Research Implications |
|---|---|---|---|
| Prior Antibiotic Use | Minimal impact; detected pathogen DNA persists | Significant reduction in sensitivity; antibiotics inhibit microbial growth | mNGS particularly valuable for patients with pre-treatment |
| Pathogen Type | Superior for viruses, atypical bacteria, uncultivable species | Limited to cultivable bacteria and fungi | mNGS enables detection of full pathogen spectrum |
| Sample Type (Body Fluids) | Varies by DNA content; higher host DNA reduces sensitivity | Dependent on viable pathogen concentration | Plasma cfDNA reduces host background vs. whole blood |
| Gram-positive Bacteria | Lower detection rate for some Gram-positive organisms (22.2% concordance in one study) [114] | Standard performance for cultivable Gram-positive species | Complementary approaches needed for comprehensive detection |
| Fungal Pathogens | Variable detection (55.6% concordance in one study) [114] | Gold standard for cultivable fungi; limited for atypical species | Culture may supplement mNGS for fungal detection |
The performance of both methods is further influenced by sample type and the biological characteristics of the pathogen. Research comparing whole-cell DNA (wcDNA) mNGS to cell-free DNA (cfDNA) mNGS in body fluids found that wcDNA mNGS demonstrated significantly higher sensitivity for pathogen detection compared to both cfDNA mNGS and 16S rRNA NGS [60]. This has important implications for protocol selection in research settings.
For bacterial detection, the cell wall structure appears to influence mNGS performance. One study in transplant patients found that while mNGS detected 79.2% of Gram-negative bacteria (Enterobacteriaceae and non-fermenting bacteria) identified by culture, it detected only 22.2% of Gram-positive bacteria [114]. This suggests that DNA extraction efficiency may vary between these bacterial classes, an important consideration for researchers optimizing detection protocols.
Experimental Methodologies
Conventional Culture Protocols
Traditional culture remains the benchmark against which molecular methods are compared, providing viable isolates for further characterization and drug susceptibility testing. Standard culture protocols involve inoculating clinical body fluid samples onto appropriate media and incubating under conditions suitable for pathogen growth.
Sample Processing Protocol:
- Inoculation: Body fluid samples are directly inoculated into aerobic and anaerobic culture bottles (e.g., BD BACTEC Plus Aerobic/F bottles and BD BACTEC Lytic Anaerobic/F bottles) [112] [114].
- Incubation: Culture bottles are incubated for up to 5 days using automated continuous monitoring systems (e.g., BD BACTEC FX instrument) [114].
- Subculture: Positive cultures are Gram stained and subcultured onto specialized agar plates (blood agar, chocolate agar, MacConkey agar) based on Gram stain results [112].
- Identification: Isolated colonies are identified using matrix-assisted laser desorption ionization-time of flight mass spectrometry (MALDI-TOF MS) [112] [114].
- Antibiotic Susceptibility Testing: Identified bacterial pathogens are subjected to antibiotic susceptibility testing using systems such as VITEK II with appropriate susceptibility cards to determine minimum inhibitory concentrations (MICs) [112].
The major advantages of culture include its ability to provide isolates for further research and its high specificity. However, its limitations are substantial: typically requiring 1-5 days for results, inability to detect uncultivable pathogens, and significantly reduced sensitivity in patients who have received antibiotic therapy [112].
Metagenomic Next-Generation Sequencing Protocols
mNGS protocols for body fluid samples involve multiple critical steps from sample preparation to bioinformatic analysis, each of which can influence the sensitivity and specificity of the assay.
Sample Processing and DNA Extraction:
- Sample Collection: Body fluids (blood, cerebrospinal fluid, bronchoalveolar lavage fluid, puncture fluids, tissues) are collected aseptically [112].
- Transport and Storage: Samples are transported at appropriate temperatures (6°C to 35°C for blood; -20°C or dry ice for other fluids) to preserve nucleic acid integrity [112].
- DNA Extraction: Various extraction kits are employed depending on the sample type. The QIAamp DNA Micro Kit is commonly used for DNA extraction from 200 μL of sample [112]. For cell-free DNA analysis from plasma, samples are centrifuged at 16,000×g for 10 minutes before extraction [115].
Library Preparation and Sequencing:
- Library Construction: DNA libraries are prepared using kits such as the VAHTS Universal Pro DNA Library Prep Kit for Illumina or QIAseq Ultralow Input Library Kit, involving fragmentation, end repair, adapter ligation, and PCR amplification [112] [60].
- Quality Control: Library quality is assessed using fluorometric methods (Qubit Fluorometer) and bioanalyzers (Agilent 2100 Bioanalyzer) [112].
- Sequencing: Qualified libraries are sequenced on platforms such as the Illumina Nextseq 550 or NovaSeq with 2×150 paired-end configuration, generating approximately 8 GB of data per sample (∼26.7 million reads) [112] [60].
Bioinformatic Analysis:
- Quality Control: Raw data undergoes adapter trimming and low-quality read removal using tools like Fastp [115].
- Host DNA Depletion: Human sequences are removed by alignment to the human reference genome (hg38) using BWA-MEM or Bowtie2 [112] [114].
- Pathogen Identification: Non-host reads are aligned against comprehensive microbial genome databases using Kraken2 or BLASTN against the NCBI nt database [112] [114].
- Result Interpretation: Positive criteria typically include: read counts significantly exceeding negative controls, mapping to multiple genomic regions, and exclusion of common contaminants [60].
Figure 1: mNGS Workflow for Body Fluid Samples
The Scientist's Toolkit: Essential Research Reagents and Materials
The successful implementation of mNGS for pathogen detection requires specific reagents and instruments that collectively enable the sensitive and specific identification of microbial organisms in complex clinical samples. The following table details key components of the methodological pipeline.
Table 3: Essential Research Reagents and Materials for mNGS-Based Pathogen Detection
| Category | Specific Product/Platform | Research Application | Performance Considerations |
|---|---|---|---|
| Nucleic Acid Extraction | QIAamp DNA Micro Kit (QIAGEN) | DNA extraction from low-biomass samples | High recovery efficiency for microbial DNA |
| Library Preparation | VAHTS Universal Pro DNA Library Prep Kit for Illumina (Vazyme) | Library construction from low-input DNA | Maintains complexity of metagenomic samples |
| Sequencing Platforms | Illumina Nextseq 550, NovaSeq | High-throughput sequencing | 2×150 bp configuration common for metagenomics |
| Bioinformatic Tools | BWA-MEM, Bowtie2, Kraken2, BLASTN | Host sequence removal, taxonomic classification | Database comprehensiveness critical for sensitivity |
| Quality Control Instruments | Qubit Fluorometer, Agilent 2100 Bioanalyzer | Quantification and qualification of nucleic acids | Essential for assessing library quality |
| Reference Databases | NCBI nt database, Custom pathogen databases | Taxonomic classification of sequencing reads | Breadth directly impacts novel pathogen detection |
Research Implications and Future Directions
The enhanced sensitivity of mNGS compared to culture has profound implications for research on unrecognized human bacterial pathogens. The ability to detect microbial DNA without prior cultivation enables researchers to identify and characterize previously unknown infectious agents, expanding our understanding of the human microbiome and its relationship to disease.
mNGS has demonstrated particular value in detecting atypical pathogens that evade conventional methods. Studies have identified "clinically atypical pathogens, mainly Mycobacterium, Clostridium tetanus, and parasites, that can solely be detected via mNGS" [114]. This capability is revolutionizing our approach to diagnostic microbiology and expanding the catalog of known human pathogens.
The research applications extend beyond clinical diagnostics to broader microbial discovery. As noted in research on rare pathogens, "when starting to do research on rare pathogens, it is advisable to first establish a collection of the species of interest derived from clinical samples" [111]. mNGS facilitates this process by enabling detection of organisms that cannot be cultivated by standard methods. Genome-based methods such as "digital DNA-DNA hybridisation or calculation of the average nucleotide identity (ANI)" can then be applied for precise taxonomic classification of these novel organisms [111].
Future methodological developments will likely focus on addressing current limitations, particularly the challenge of high host DNA background that reduces sensitivity. Approaches such as targeted enrichment of microbial sequences and improved algorithms for distinguishing pathogens from contaminants will enhance the utility of mNGS for both clinical and research applications. As these technologies mature, they will increasingly enable the comprehensive characterization of the human pathobiome and facilitate the discovery of novel infectious agents associated with human disease.
Figure 2: Diagnostic Approaches for Pathogen Discovery
In the rapidly evolving field of unrecognized human bacterial pathogens research, the speed and accuracy of diagnostic methods are paramount. The delay in identifying novel or fastidious pathogens directly impacts patient outcomes, antimicrobial stewardship, and public health responses. While traditional microbial culture has been the cornerstone of bacteriology for over a century, its prolonged turnaround time and limitations in detecting unculturable or novel organisms present significant challenges for contemporary research and clinical practice [77].
The emergence of molecular and genomic technologies has revolutionized pathogen detection, offering complementary approaches with potentially faster results. Among these, metagenomic next-generation sequencing (mNGS) enables hypothesis-free detection of a broad array of pathogens directly from clinical specimens, while targeted molecular (Tm) methods like digital droplet PCR (ddPCR) and targeted NGS (tNGS) provide rapid, focused detection of specific pathogens [116] [117]. Understanding the comparative performance characteristics—particularly turnaround time—of these approaches is essential for researchers and drug development professionals working to uncover and characterize novel bacterial pathogens.
This technical analysis provides a systematic comparison of the turnaround times for Tm mapping, mNGS, and culture methods, contextualized within the framework of unrecognized human bacterial pathogen research. We present quantitative data on diagnostic performance, detailed experimental protocols, and analytical frameworks to guide methodological selection for research applications.
Comparative Analysis of Turnaround Times
The turnaround time from sample collection to actionable result represents a critical metric for evaluating diagnostic methods in pathogen research. The following analysis synthesizes data from recent studies across various clinical and research contexts to provide a comprehensive comparison of culture, mNGS, and Tm mapping methods.
Table 1: Comparative Turnaround Times and Performance of Diagnostic Methods
| Method | Average Turnaround Time | Key Advantages | Key Limitations | Sensitivity Range | Specificity Range |
|---|---|---|---|---|---|
| Culture | 2-4 days [118] | Gold standard, provides live isolates for further testing | Limited to culturable organisms; affected by prior antibiotics | 36-65.8% [119] [117] | 100% [117] |
| mNGS | 16-24 hours [117] | Hypothesis-free, detects novel/rare pathogens | High cost; host DNA interference; complex bioinformatics | 86-89.7% [119] [117] | 83-94.2% [119] [117] |
| Tm Mapping (ddPCR) | 12.4 ± 3.8 hours [116] | High sensitivity, quantitative, minimal host DNA interference | Requires prior knowledge of target pathogens | 78.7% [116] | Not specified |
| Tm Mapping (tNGS) | 11-13 hours [117] | Cost-effective, focused analysis, reduced host interference | Limited to predefined targets | 89.7% [117] | 94.2% [117] |
| Rapid mNGS (Nanopore) | ~4 hours [118] | Ultra-fast, potential for point-of-care application | Requires optimization for specific sample types | 99% accuracy for pathogen ID [118] | 90% for AMR profiling [118] |
The data reveal a clear continuum of speed versus breadth in pathogen detection methods. Traditional culture methods, while providing the gold standard for viability and antibiotic susceptibility testing, require the longest turnaround times—typically 2-4 days for complete identification and susceptibility profiling [118]. This prolonged timeframe presents significant limitations for rapid intervention in research on novel pathogens.
Standard mNGS workflows offer a substantial improvement in speed, with turnaround times of 16-24 hours [117], while simultaneously providing hypothesis-free detection capable of identifying novel, rare, or unexpected pathogens. The comprehensive nature of mNGS comes with trade-offs, including higher costs, bioinformatic complexity, and interference from host nucleic acids [77].
Tm mapping approaches, including tNGS and ddPCR, occupy an intermediate position, offering faster results than comprehensive mNGS (11-13 hours for tNGS [117] and 12.4±3.8 hours for ddPCR [116]) while maintaining high sensitivity and specificity. These methods are particularly valuable in research contexts where specific pathogen targets are known, and rapid, quantitative results are prioritized.
Most notably, optimized rapid mNGS protocols leveraging technologies like nanopore sequencing have demonstrated the potential to dramatically reduce turnaround times to approximately 4 hours while maintaining high accuracy [118]. Such advances highlight the evolving landscape of pathogen detection and its implications for research on unrecognized bacterial pathogens.
Experimental Protocols and Methodologies
Conventional Culture Protocol
Objective: To isolate and identify bacterial pathogens from clinical specimens using standard culture techniques.
Materials and Reagents:
- Culture media (blood agar, chocolate agar, MacConkey agar)
- Sterile culture tubes and plates
- Incubators (35±2°C, with 5-10% CO₂ as needed)
- Automated identification systems (MALDI-TOF, VITEK)
- Antibiotic susceptibility testing materials
Procedure:
- Sample Processing: Inoculate clinical specimens (e.g., urine, tissue, fluid) onto appropriate culture media using standardized loops or swabs [120].
- Incubation: Place inoculated media in incubators at optimal temperatures for 18-24 hours; extend for fastidious organisms [120].
- Colony Evaluation: Examine plates for growth; identify morphologically distinct colonies.
- Subculture: Purify colonies of interest on fresh media for further analysis.
- Species Identification: Employ Gram staining, biochemical tests, or automated systems (e.g., MALDI-TOF) [120].
- Antibiotic Susceptibility Testing: Perform disk diffusion, E-test, or automated systems following CLSI guidelines.
Time Analysis: Time to positive culture (TTPC) averages 15.1±10.4 hours [116], with total time from sample harvesting to final results (THTR) averaging 22.6±9.4 hours [116]. Complete identification and susceptibility profiles typically require 48-72 hours [118].
Metagenomic Next-Generation Sequencing (mNGS) Protocol
Objective: To comprehensively detect and identify bacterial pathogens directly from clinical specimens without prior cultivation.
Materials and Reagents:
- Nucleic acid extraction kits (e.g., QIAamp DNA Microbiome Kit)
- Host DNA depletion reagents (e.g., Naxtra Blood kit)
- Library preparation kits (e.g., Nextera XD)
- Sequencing platforms (Illumina, Nanopore)
- Bioinformatics pipelines (IDSeq, PathoScope)
Procedure:
- Sample Processing: Concentrate pathogens from clinical specimens via centrifugation or filtration; implement host DNA depletion using salt-activated nucleases (e.g., MSAN or HLSAN) [118].
- Nucleic Acid Extraction: Extract total DNA/RNA using optimized kits; quantify yield and quality [118].
- Library Preparation: Fragment DNA, add adapters, and amplify using validated kits [77].
- Sequencing: Process libraries on appropriate NGS platforms (short-read: Illumina; long-read: Nanopore) [77].
- Bioinformatic Analysis:
- Quality control and filtering of raw reads
- Host sequence subtraction
- Taxonomic classification against microbial databases
- Antimicrobial resistance gene detection [77]
Time Analysis: Total time from sample harvesting to result (THTR) averages 16.8±2.4 hours [116]. Rapid nanopore protocols can reduce this to approximately 4 hours with optimized host depletion [118].
Targeted Molecular (Tm) Mapping Protocol
Objective: To achieve rapid, sensitive detection of specific bacterial pathogens using focused molecular assays.
Digital Droplet PCR (ddPCR) Materials and Reagents:
- ddPCR supermix
- Droplet generation oil and cartridges
- Target-specific primers and probes
- Droplet reader and analyzer
Procedure:
- Sample Preparation: Extract nucleic acids from clinical specimens; minimal processing required due to resistance to host DNA interference [116].
- Reaction Setup: Combine sample with ddPCR supermix and target-specific primers/probes [116].
- Droplet Generation: Partition reactions into ~20,000 nanoliter-sized droplets [116].
- Amplification: Perform PCR cycling with endpoint detection.
- Quantification: Count positive and negative droplets; calculate original target concentration using Poisson statistics [116].
Time Analysis: THTR averages 12.4±3.8 hours, significantly faster than mNGS (p<0.01) [116].
Targeted NGS (tNGS) Materials and Reagents:
- Target-specific primer panels
- Multiplex PCR reagents
- Library preparation kits
- Sequencing platforms (Illumina, Nanopore)
Procedure:
- Target Enrichment: Perform multiplex PCR with pathogen-specific primers (e.g., Fi-tNGS panel for 64 fungal species) [117].
- Library Preparation: Process amplicons with streamlined kits [117].
- Sequencing: Run on appropriate platforms with reduced depth requirements.
- Analysis: Use simplified bioinformatics pipelines for target identification [117].
Time Analysis: Turnaround time of 11-13 hours, significantly faster than mNGS (16-24 hours) [117].
Technological Workflows and Pathway Analysis
The following diagrams illustrate the core workflows and technological relationships between the different diagnostic methods discussed in this analysis.
Diagnostic Method Workflow Comparison
Diagram 1: Comparative workflows and turnaround times for culture, mNGS, and Tm mapping methods. Tm mapping approaches show significantly compressed timelines compared to traditional methods.
Bacterial Defense Systems Against Viral Attack
Research into unrecognized bacterial pathogens must consider the complex evolutionary arms race between bacteria and their viruses (phages), as these defense mechanisms represent both research challenges and opportunities for discovery.
Diagram 2: Bacterial defense mechanisms against viral attack. Understanding these systems is crucial for researching unrecognized pathogens, as they represent evolutionary adaptations that can complicate detection and cultivation.
Essential Research Reagent Solutions
The following table outlines key reagents and materials essential for implementing the diagnostic methods discussed, with particular emphasis on their applications in research on unrecognized bacterial pathogens.
Table 2: Research Reagent Solutions for Pathogen Detection Methods
| Reagent/Material | Function | Application Notes |
|---|---|---|
| Salt-Activated Nucleases (MSAN/HLSAN) | Selective host DNA depletion | Critical for improving microbial signal in low-biomass samples; MSAN shows slightly better performance than HLSAN [118] |
| Multiplex PCR Primer Panels | Targeted amplification of pathogen sequences | Enables tNGS; Fi-tNGS example targets 64 fungal species [117] |
| Droplet Generation Oil & Cartridges | Partitioning samples for ddPCR | Essential for absolute quantification without standards; resistant to PCR inhibitors [116] |
| Nanopore Flow Cells | Real-time sequencing | Enables rapid (4-hour) mNGS; suitable for point-of-care applications [118] |
| Bioinformatic Pipelines (IDSeq, PathoScope) | Taxonomic classification | Critical for mNGS; requires standardization and database curation [77] |
| Host Depletion Kits (e.g., Naxtra Blood) | Removal of human DNA | Improves sequencing efficiency; commercial kits show variable performance [118] |
| Long-read Sequencing Reagents | Assembly of complex genomic regions | Enables detection of giant DNA elements like Inocles (350 kbp) [121] |
Implications for Unrecognized Bacterial Pathogen Research
The comparative analysis of turnaround times across diagnostic methods reveals significant implications for research on unrecognized human bacterial pathogens. The speed advantage of Tm mapping and mNGS approaches enables more rapid hypothesis generation and testing when investigating novel microbial threats.
The discovery of massive extrachromosomal DNA elements called "Inocles" in oral bacteria underscores the limitations of traditional methods and the potential of advanced sequencing technologies [121]. These giant genetic elements (averaging 350 kilobase pairs) had remained undetected by conventional sequencing due to their size and complexity, requiring long-read sequencing approaches for identification. This finding highlights how methodological choices directly impact our ability to uncover novel biological entities.
Similarly, research on bacterial defense systems against phage predation has revealed hundreds of previously unknown antiphage genes, many with unknown functions [122]. The recent discovery of the Panoptes system—a bacterial immune mechanism that senses viral interference and launches counterattacks—exemplifies how novel pathogen biology continues to emerge through contemporary research approaches [9]. These defense systems not only represent fascinating biological mechanisms but also potential tools for biotechnology and therapeutic development.
The integration of rapid diagnostic methods with research on bacterial pathogenesis is creating new paradigms for pathogen discovery. For instance, the development of species-specific PCR tests to distinguish Escherichia marmotae from E. coli demonstrates how targeted molecular approaches enable more precise tracking and study of emerging pathogens [6]. Such differentiation was previously challenging with conventional methods but is crucial for understanding the epidemiology and pathogenicity of closely related species.
The landscape of pathogen detection is evolving rapidly, with significant implications for research on unrecognized bacterial pathogens. While culture methods remain essential for obtaining viable isolates and performing phenotypic antibiotic susceptibility testing, their prolonged turnaround times limit their utility in rapid pathogen discovery and response scenarios.
Metagenomic NGS offers a powerful hypothesis-free approach with dramatically improved detection capabilities for novel, fastidious, and polymicrobial infections, with standard turnaround times of 16-24 hours and emerging rapid protocols reducing this to approximately 4 hours. Targeted mapping approaches, including tNGS and ddPCR, provide an optimal balance of speed (11-13 hours) and sensitivity for focused research applications where pathogen targets are predefined.
The continuing advancements in sequencing technologies, host DNA depletion methods, and bioinformatic analyses promise to further accelerate pathogen discovery while reducing costs. For researchers investigating unrecognized human bacterial pathogens, a strategic approach that combines the comprehensive capability of mNGS with the rapid, sensitive detection of Tm mapping methods will maximize both the breadth and speed of discovery, ultimately enhancing our ability to identify and characterize novel microbial threats to human health.
Within the broader thesis on unrecognized human bacterial pathogens, the limitations of traditional diagnostic methods become a significant bottleneck for both research and clinical practice. Nearly half of all patients with pulmonary infections lack definitive identification of a causative pathogen, compelling reliance on empirical antibiotic therapies that contribute to the emergence of drug-resistant "nightmare bacteria," cases of which have surged dramatically in recent years [123] [2]. This escalating public health threat underscores the urgent need for diagnostic technologies with higher sensitivity and broader detection capabilities. Next-generation sequencing technologies, particularly targeted next-generation sequencing (tNGS), are emerging as powerful tools that can overcome the limitations of traditional methods, offering researchers and drug development professionals a more precise window into the hidden world of microbial pathogens and their resistance mechanisms [123] [124].
Quantitative Showdown: tNGS vs. Traditional Methods
A direct comparison of pathogen detection rates reveals the superior performance of novel sequencing-based methods. A prospective 2025 study involving 166 patients with suspected pulmonary infections provided a clear, quantitative assessment of this advantage, testing samples including bronchoalveolar lavage fluid (BALF), fresh tissue, pleural effusion, and sputum [123].
Table 1: Comparative Pathogen Detection Performance
| Metric | Traditional Pathogen Detection (TPD) | Targeted NGS (tNGS) | Statistical Significance |
|---|---|---|---|
| Overall Positive Detection Rate | 32.53% (54/166 samples) | 81.33% (135/166 samples) | p < 0.001 |
| Total Number of Pathogen Species Identified | 14 | 65 | Not Applicable |
| Spectrum of Detection | Bacteria (including M. tuberculosis) and Fungi | 35 Bacterial Species, 10 Fungal Species, 18 Viral Species, M. pneumoniae, C. pneumoniae | Not Applicable |
| Capability for Mixed Infection Detection | Limited | Enhanced | Not Applicable |
| Additional Output | Not Available | 16 Antibiotic Resistance Genes (ARGs) | Not Applicable |
Beyond the stark difference in detection rates, tNGS dramatically expanded the identifiable spectrum of pathogens. While traditional methods were confined to 11 bacterial and 2 fungal species (plus Mycoplasma pneumoniae), tNGS identified 35 bacterial species, 10 fungal species, and 18 viral species, in addition to Mycoplasma pneumoniae and Chlamydia pneumoniae [123]. This capability is critical for uncovering the full diversity of pathogens, including viruses, which are entirely missed by standard cultures. Furthermore, tNGS proved significantly more efficient at detecting mixed infections, a complex clinical scenario that traditional methods often fail to resolve. A crucial advantage for antimicrobial stewardship and drug development is the technology's ability to concurrently identify antibiotic resistance genes, with the study reporting the detection of 16 such genes [123].
Inside the Experiment: Detailed Methodologies
Traditional Pathogen Detection Protocols
The traditional methods used as a comparator in the study represent standard clinical microbiology practices [123]:
- Mycobacterium tuberculosis Detection: Acid-fast staining was used for initial microscopic screening. Simultaneously, samples were inoculated onto Löwenstein-Jensen culture medium and incubated at 37°C for 4 to 8 weeks, with periodic observation of colony morphology for identification.
- Other Bacteria and Fungi: Pure cultures were prepared into standard suspensions and analyzed using the VITEK-2 system. This instrument identifies organisms based on reactions to biochemical substrates, comparing results against a built-in microbial database.
- Quality Control: Positive controls (E. coli ATCC 25922) and negative controls (sterile saline) were implemented to ensure reliability.
Targeted NGS (tNGS) Workflow
The tNGS protocol is a multi-stage process that combines molecular biology with high-throughput bioinformatics [123].
Table 2: Research Reagent Solutions for tNGS Workflow
| Reagent / Tool | Function in the Protocol |
|---|---|
| RNA/DNA Isolation Kit (Beyotime) | Extraction of total nucleic acids (DNA and RNA) from processed samples. |
| 300+ Pathogen-Targeted Gene Detection Kit (Pathogeno) | Core reagent containing a specific primer panel for multiplex PCR amplification of pathogen and ARG targets. |
| Illumina MiniSeq Platform | High-throughput sequencer to generate massive numbers of short DNA reads. |
| Trimmomatic (v0.39) | Bioinformatics tool for raw read preprocessing and adapter trimming. |
| Kraken2 (v2.1.2) | Taxonomic classification system that assigns sequenced reads to specific pathogens using the NCBI RefSeq database. |
| ResFinder (v4.1) / CARD Database | Tool and database for identifying antimicrobial resistance genes in the sequenced data. |
The following diagram illustrates the key stages of the tNGS workflow, from sample to final report.
Diagram 1: tNGS workflow from sample to result
Key Experimental Steps [123]:
- Sample Pretreatment: Varied by sample type. BALF was centrifuged to pellet cells; fresh tissue was homogenized and centrifuged; pleural effusion was centrifuged for pathogen enrichment; sputum was lysed with dithiothreitol (DTT) and washed.
- Nucleic Acid Extraction: Total DNA and RNA were co-extracted using a commercial kit.
- Library Construction: A two-round PCR protocol was used.
- First Round (Multiplex PCR): Specific primers from the detection kit targeted conserved regions of pathogens and antibiotic resistance genes (ARGs). Products were purified.
- Second Round (Indexing PCR): Primers with sequencing adapters and sample-specific barcodes were used. Final libraries were quality-controlled for fragment size and concentration.
- Sequencing: Libraries were sequenced on an Illumina MiniSeq platform.
- Bioinformatic Analysis:
- Quality Control: Raw reads were filtered for length and quality.
- Pathogen Identification: Filtered reads were classified using Kraken2 against a microbial genome database.
- ARG Detection: Reads were aligned against ARG references using ResFinder.
- Positivity Criteria: Strict thresholds were applied, requiring a minimum number of reads and/or a significant fold-change over negative controls.
Implications for Research and Public Health
The enhanced detection capabilities of tNGS have profound implications for the research on unrecognized pathogens and the broader fight against antimicrobial resistance.
Revealing the Hidden Microbiome and Resistance Landscape
The ability of tNGS to identify a wider spectrum of pathogens, including viruses and fastidious bacteria, directly addresses the challenge of unrecognized human bacterial pathogens [123]. By providing a more comprehensive etiological profile, especially in cases of mixed infection, this technology generates richer data for understanding microbial ecology in human disease. Concurrently, the detection of antibiotic resistance genes alongside pathogens offers invaluable insights for surveillance. Public health systems, such as the NCBI Pathogen Detection platform, already integrate genomic data to track the spread of resistant organisms and their resistance mechanisms [125]. The rise of "nightmare bacteria" carrying difficult-to-treat resistance genes like NDM underscores the critical importance of such advanced surveillance tools [2].
Informing Drug Development and Basic Science
For drug development professionals, tNGS data can guide the development of new antimicrobials and vaccines by identifying prevalent and emerging pathogen targets, as well as common resistance patterns. Furthermore, the discovery of novel bacterial defense systems, such as the recently identified Panoptes system that protects bacteria from viral predators (phages), opens new avenues for therapeutic intervention [9]. Understanding these fundamental mechanisms of bacterial survival and immunity can inspire entirely new classes of anti-infective agents.
The evidence clearly demonstrates a decisive "showdown" victory for targeted next-generation sequencing over traditional pathogen detection methods. With its significantly higher sensitivity, broader detection spectrum, and unique ability to identify mixed infections and antibiotic resistance genes, tNGS is an indispensable tool for modern infectious disease research [123]. Its adoption is pivotal for advancing our understanding of unrecognized bacterial pathogens, improving public health surveillance in the face of rising antimicrobial resistance, and ultimately informing the development of next-generation therapeutic strategies [2] [9].
The landscape of clinical microbiology is continuously evolving, with an increasing number of bacterial species being recognized as human pathogens. The vast number of unknown bacteria is estimated to range between 10^7 and 10^9, ensuring that routine clinical diagnostics increasingly encounter rare and novel species [111]. These unrecognized and rare bacterial pathogens present a significant challenge for antimicrobial stewardship programs (ASPs) and directly impact patient outcomes. Accurate and timely identification is a critical requisite for early, adequate antibiotic treatment, yet many newly described and rare species fall outside the detection scope of conventional phenotypic identification (CPI) methods [126]. The clinical relevance of these organisms is often difficult to ascertain from sporadic case reports alone, complicating therapeutic decisions [111]. This whitepaper examines the transformative impact of advanced diagnostic technologies, particularly matrix-assisted laser desorption ionization–time of flight (MALDI-TOF) mass spectrometry (MS) and metagenomic next-generation sequencing (mNGS), on pathogen identification, antimicrobial stewardship, and ultimately, patient care within the broader context of researching unrecognized human bacterial pathogens.
Advanced Diagnostic Technologies and Their Methodologies
MALDI-TOF Mass Spectrometry
MALDI-TOF MS has revolutionized routine bacterial identification in clinical laboratories over the past decade. This method involves the direct analysis of bacterial colonies to generate a unique protein spectral fingerprint that is compared against an extensive database of reference spectra [126].
- Experimental Protocol: The standard methodology for MALDI-TOF MS identification is as follows [126]:
- Sample Preparation: A single bacterial colony is smeared directly onto a steel target plate.
- Matrix Application: The sample is overlaid with 2 µL of matrix solution (saturated α-cyano-4-hydroxycinnamic acid in 50% acetonitrile and 2.5% trifluoroacetic acid).
- Spectrum Acquisition: The plate is inserted into the mass spectrometer (e.g., MALDI-TOF MS AutoFlex II or MicroFlex LT). Laser desorption and ionization generate a mass spectrum, typically focusing on the first 100 peaks of ribosomal proteins.
- Data Analysis: MALDI Biotyper 3.0 software compares the sample spectrum against a validated database. An isolate is considered correctly identified at the species level if two spectra achieve a score of ≥1.9. For scores <1.9, a second run with four additional spectra is performed.
- Database Construction: To enhance the identification of rare species, the primary commercial database (e.g., Bruker database containing 3,993 microorganism spectra) must be updated with a laboratory-owned collection of spectra from clinical isolates that have been definitively identified by molecular techniques such as 16S rRNA gene sequencing. A consensus spectrum is created from 12 spots per isolate across two independent runs to ensure reproducibility [126].
Metagenomic Next-Generation Sequencing (mNGS)
Metagenomic Next-Generation Sequencing is an unbiased, high-throughput sequencing technique that allows for the detection of all nucleic acids in a clinical sample, enabling the identification of pathogens without prior knowledge or cultivation.
- Experimental Protocol: A typical mNGS workflow for bacterial identification from clinical samples includes [127]:
- Nucleic Acid Extraction: DNA is extracted from samples (e.g., blood, tissue, cerebrospinal fluid) using a commercial kit (e.g., TIANamp Micro DNA Kit).
- Library Preparation: Libraries are constructed using a kit such as the Nextera XT, followed by quality control with Qubit and Agilent 2100 Bioanalyzer.
- Sequencing: Sequencing is performed on a platform like the Illumina NextSeq-550Dx.
- Bioinformatic Analysis:
- Quality Control: Adapter contamination, low-quality, and low-complexity reads are removed using tools like fastp and Komplexity.
- Host Depletion: Human host DNA sequences are filtered out by mapping to a human reference genome (GRCh38) with Bowtie2.
- Pathogen Identification: The remaining data is aligned to comprehensive microbial genome databases.
- Positive Detection Criteria: The criteria are pathogen-specific [127]:
- Bacteria/Fungi: Specifically mapped read number (SMRN) ranks in the top 10 for its kind, OR the standardized SMRN (SDSMRN = SMRN × 20 million/total reads) is >1.
- Viruses: SDSMRN ranks in the top 3 AND SDSMRN >5.
- Mycobacterium, parasites: SDSMRN >1, OR it positions first within the top 20 genus with the highest SDSMRN.
The Diagnostic Pathway and Workflow Integration
The following diagram illustrates the integrated diagnostic pathway for identifying rare and unrecognized bacterial pathogens, combining traditional and advanced methods.
Quantitative Impact on Diagnostic Performance
Advanced diagnostic technologies significantly improve the ability to identify a wider range of pathogens with greater speed and accuracy compared to conventional methods. The data below summarize their quantitative performance.
Table 1: Comparative Diagnostic Performance of Identification Techniques
| Metric | Conventional Phenotypic Identification (CPI) | MALDI-TOF MS | Metagenomic NGS (mNGS) |
|---|---|---|---|
| Species Identified/10,000 isolates | 19 [126] | 36 [126] | Not directly comparable (unbiased detection) |
| Sensitivity for Infection | 47.28% (for culture) [127] | 81.52% (vs. culture) [127] | 81.52% (in FUO diagnosis) [127] |
| Specificity for Infection | 84.81% (for culture) [127] | 73.42% (vs. culture) [127] | 73.42% (in FUO diagnosis) [127] |
| Re-identifications Required/10,000 isolates | 35.2 [126] | 4.5 [126] | Not Applicable |
| Time to Identification | Baseline | 55x faster than CPI [126] | Varies (days) |
| Cost of Identification | Baseline | 5x cheaper than CPI [126] | Higher cost |
Table 2: Impact of mNGS on Clinical Management in Fever of Unknown Origin (FUO) [127]
| Parameter | Value | Clinical Implication |
|---|---|---|
| Total FUO Patients | 263 | Single-center retrospective study |
| Final Infectious Disease (ID) Diagnosis | 184 (69.96%) | Confirms infection as leading FUO cause |
| mNGS True Positives | 150 | Correctly identified causative pathogen |
| Clinical Management Positively Affected | 128 (48.67%) | Direct impact on therapeutic decisions |
| Most Common Pathogen (A. baumannii) | Identified by mNGS | Expands detected pathogen spectrum |
Direct Impact on Antimicrobial Stewardship and Patient Outcomes
Integration into the "Six D's" of Antimicrobial Stewardship
Antimicrobial Stewardship Programs aim to optimize antimicrobial use. Microbiology laboratories and clinical microbiologists are critical leaders in these efforts, and their role can be summarized by the "six D's" of antimicrobial stewardship [128].
Table 3: The Role of Advanced Diagnostics in the "Six D's" of Antimicrobial Stewardship [128]
| Stewardship Element | Role of Advanced Diagnostics (MALDI-TOF MS & mNGS) |
|---|---|
| Diagnosis | Rapid, accurate pathogen identification from critical specimens (e.g., positive blood cultures); unbiased detection via mNGS in culture-negative cases. |
| Drug | Provision of cumulative susceptibility reports to guide empirical therapy; rapid detection of resistance markers (e.g., carbapenemases, colistin resistance) via mNGS. |
| Dose | Collaboration with pharmacists to report MICs for pharmacokinetic/pharmacodynamic (PK/PD) dosing optimization. |
| De-escalation | Enables early de-escalation from broad-spectrum to targeted therapy upon definitive pathogen identification. |
| Duration | Use of biomarker testing in conjunction with microbial clearance to inform appropriate therapy duration. |
| Debridement/Drainage | Guidance on obtaining adequate specimens (e.g., tissue/fluid vs. swabs) and prioritizing cultures from sterile sites. |
Economic and Operational Efficiency
The adoption of MALDI-TOF MS presents substantial economic and operational advantages for clinical laboratories. Studies have demonstrated that this technology reduced the time required for bacterial identification by 55-fold and 169-fold compared to conventional phenotypic identification and gene sequencing, respectively [126]. Furthermore, the associated costs were reduced by 5-fold and 96-fold in the same comparisons, making it a highly cost-effective tool for routine use [126]. The efficiency is further underscored by the dramatic reduction in misidentifications requiring confirmation; MALDI-TOF MS necessitated only 4.5 re-identifications per 10,000 isolates, compared to 35.2 per 10,000 with conventional methods [126].
Enhancing Outcomes in Specific Clinical Scenarios
The clinical utility of these technologies is most apparent in complex scenarios:
- Fever of Unknown Origin (FUO): mNGS significantly improves the detection of the pathogen spectrum in infection-caused FUO, with one study showing it positively affecting the clinical management of nearly half (48.67%) of patients [127].
- Rare Pathogen Identification: MALDI-TOF MS, especially with customized databases, has proven to be a powerful tool for identifying rare bacterial species implicated in human infectious diseases. It allows for the rapid recognition of species with fewer than 10 reports in PubMed, facilitating the study of their clinical burden and serving as a viable alternative to more costly and time-consuming molecular methods [126] [111].
The Scientist's Toolkit: Essential Research Reagents and Materials
Research into unrecognized pathogens relies on a specific set of reagents and tools for identification, characterization, and analysis.
Table 4: Essential Research Reagents and Materials for Pathogen Research
| Item | Function/Application | Examples/Notes |
|---|---|---|
| MALDI-TOF MS System | High-throughput protein spectral analysis for bacterial identification. | Bruker MicroFlex LT/MALDI Biotyper; Requires a validated spectral database [126]. |
| Matrix Solution | Critical for co-crystallization with analyte in MALDI-TOF MS. | Saturated α-cyano-4-hydroxycinnamic acid (CHCA) in 50% acetonitrile, 2.5% TFA [126]. |
| Next-Generation Sequencer | Unbiased sequencing of all nucleic acids in a sample for pathogen detection. | Illumina NextSeq-550Dx; used for mNGS [127]. |
| DNA Extraction Kit | Isolation of high-quality microbial DNA from complex clinical samples. | TIANamp Micro DNA Kit (TIANGEN Biotech) [127]. |
| Bioinformatic Tools | Analysis of mNGS data: quality control, host depletion, taxonomic assignment. | fastp (QC), Bowtie2 (host depletion), alignment to microbial databases [127]. |
| 16S rRNA & rpoB Primers | Amplification and sequencing of phylogenetic marker genes for molecular identification. | Used for definitive confirmation of rare/novel species [126]. |
| Special Stains | Microscopic detection of bacteria in tissues. | Warthin-Starry silver stain, Gimenez stain [129]. |
| Automated Identification Systems | Conventional phenotypic identification (baseline for comparison). | Vitek 2 System, API Strips (bioMérieux) [126]. |
The field of pathogen diagnostics is rapidly evolving, with several promising technologies on the horizon. Phage therapy has shown significant success in compassionate use cases against multi-drug resistant (MDR) Gram-negative infections, including those caused by Pseudomonas aeruginosa and Acinetobacter baumannii [130]. Artificial intelligence is poised to bridge the gap between disease understanding and drug design, with machine learning models like Random Forest and Support Vector Machines being applied to virtual screening, toxicity prediction, and bioactivity assessment [131]. Furthermore, genomic surveillance combined with patient mobility data and inference modeling is being used to identify asymptomatic carriers of antimicrobial-resistant organisms (AMROs) in hospitals, enabling more effective, targeted interventions to reduce the burden of healthcare-associated infections [132].
In conclusion, the integration of advanced diagnostic technologies like MALDI-TOF MS and mNGS into clinical practice is fundamental to modern antimicrobial stewardship and the management of infections caused by both common and unrecognized pathogens. These tools provide rapid, accurate, and often cost-effective pathogen identification, which directly facilitates early, targeted antimicrobial therapy, reduces unnecessary broad-spectrum antibiotic exposure, and ultimately improves patient outcomes. As research continues, the synergy between advanced diagnostics, novel therapeutics like phage therapy, and AI-driven analytics will be crucial in addressing the ongoing challenges of antimicrobial resistance and emerging infectious diseases.
The gold standard of bacterial culture, a cornerstone of clinical microbiology for over a century, is increasingly revealing its limitations in the face of modern diagnostic challenges. Culture-negative infective endocarditis (CNE) exemplifies this crisis, occurring in up to 30% of infective endocarditis (IE) cases where traditional blood cultures fail to identify a causative organism, often due to prior antibiotic administration or the presence of fastidious pathogens [133]. This diagnostic gap has profound implications, leading to diagnostic delays, prolonged empirical therapy with broad-spectrum antibiotics, and significant impacts on patient outcomes [133]. Within the broader context of unrecognized human bacterial pathogens research, these discrepancies are not merely diagnostic failures but represent critical opportunities to discover novel pathogens, understand emerging resistance patterns, and develop more precise diagnostic frameworks. The rise of drug-resistant "nightmare bacteria," with cases of carbapenem-resistant infections increasing by nearly 70% between 2019 and 2023, further underscores the urgent need for advanced diagnostic capabilities that can outpace conventional methods [2] [26].
Methodological Comparisons: Traditional vs. Novel Diagnostic Platforms
Performance Characteristics of Diagnostic Modalities
The evolution of diagnostic techniques for bloodstream infections reveals a trajectory toward greater sensitivity, speed, and comprehensiveness. Table 1 summarizes the key performance metrics of major diagnostic platforms, highlighting the comparative advantages of novel molecular methods.
Table 1: Comparative Analysis of Diagnostic Methods for Bloodstream Pathogen Detection
| Diagnostic Method | Sensitivity (Pooled or Reported) | Specificity (Pooled or Reported) | Typical Detection Time | Pathogen Coverage Scope | Key Limitations |
|---|---|---|---|---|---|
| Blood Culture | 40-60% [133] | High [133] | 2-5 days [134] | Broad range of bacteria and fungi | Greatly reduced by prior antibiotic use; slow [133] |
| Semi-Quantitative Catheter Culture | 85% (95% CI 79–90%) [135] | 84% (95% CI 79–88%) [135] | 2-3 days | Microorganisms on external catheter surface | Misses endoluminal colonization [136] |
| Quantitative Catheter Culture | 85% (95% CI 79–90%) [135] | 95% (95% CI 91–97%) [135] | 2-3 days | Exo- and endo-luminal organisms | More complex methodology [136] |
| Digital PCR (dPCR) | Significantly higher than culture [134] | High [134] | 3-6 hours [134] | Pre-designed panel of bacteria, fungi, viruses | Limited to targets with available primers/probes [134] |
| Metagenomic NGS (mNGS) | 90-95% [133] | High [133] | 24-48 hours [133] | Comprehensive, untargeted detection of bacteria, fungi, viruses | High cost, complex data interpretation, contamination risk [133] |
Head-to-Head Comparative Studies
Recent direct comparisons illuminate the stark sensitivity gap between traditional and novel methods. A 2025 retrospective study of 149 patients with suspected bloodstream infections found that digital PCR (dPCR) detected 63 pathogenic strains from 42 positive specimens, whereas routine blood culture identified only 6 strains from 6 positive specimens [134]. This represents a seven-fold increase in pathogen detection using dPCR. Furthermore, dPCR identified 14 cases of polymicrobial infections that were missed by culture, highlighting its superior capability to reveal complex infection profiles [134]. The average detection time for dPCR was 4.8 hours, compared to 94.7 hours for blood culture, providing a critical time advantage for clinical decision-making [134].
For catheter-related infections, a meta-analysis of 45 studies found that while semi-quantitative and quantitative techniques demonstrate similar sensitivity (85% for both), quantitative methods show superior specificity (95% vs. 84%) [135]. This makes quantitative cultures particularly valuable for confirming CR-BSIs with a high degree of certainty, though semi-quantitative methods remain widely used due to their simpler methodology [136].
Experimental Protocols for Diagnostic Validation
Metagenomic Next-Generation Sequencing (mNGS) Workflow
The application of mNGS for pathogen identification requires a meticulously controlled experimental pipeline, particularly when validating results that diverge from culture.
- Sample Preparation and Nucleic Acid Extraction: For blood samples, collect venous blood in EDTA tubes. Separate plasma via centrifugation at 1,600 × g for 10 minutes. Extract nucleic acids (DNA and RNA) using commercial kits (e.g., Pilot Gene Technology nucleic acid purification kits) and automated systems (e.g., Auto-Pure10B) [134]. For tissue samples (e.g., heart valves), homogenize the tissue first, then proceed with extraction. Include negative control extractions to monitor for contamination.
- Library Preparation and Sequencing: Convert extracted nucleic acids into sequencing libraries using kits that facilitate both DNA and RNA sequencing (e.g., Illumina Nextera XT). For RNA viruses, include a reverse transcription step. Use dual-index barcoding to enable sample multiplexing. Sequence on platforms such as Illumina NextSeq or NovaSeq to achieve sufficient depth (typically 5-20 million reads per sample) [133].
- Bioinformatic Analysis:
- Quality Control and Host Depletion: Use Trimmomatic or FastP to remove adapter sequences and low-quality reads. Align reads to the human reference genome (hg38) using BWA or Bowtie2 and remove aligning reads to deplete host background.
- Pathogen Identification: Classify remaining non-host reads against comprehensive microbial databases (NCBI RefSeq, GenBank) using tools like Kraken2 or Centrifuge. For more precise alignment, use BWA or Bowtie2 against a curated pathogen genome database.
- Result Interpretation: Establish a threshold for positive identification (e.g., ≥ 10 reads mapping to a specific pathogen, or ≥ 3 times background) while considering the negative controls. Integrate host response biomarkers (e.g., CRP, procalcitonin) for clinical correlation [133].
Digital PCR (dPCR) Protocol for Blood Pathogen Detection
Digital PCR provides absolute quantification of pathogen DNA, making it ideal for validating low-burden infections missed by culture.
- Sample Preparation: Extract DNA from 100 μL of plasma using a nucleic acid extraction kit (e.g., from Pilot Gene Technology) and an automated purification system [134].
- Droplet Generation and PCR Setup: Add 15 μL of extracted DNA to a master mix containing fluorescent probes and primers specific to the target pathogen panel. Load the reaction mixture into a droplet generator (e.g., Pilot Gene droplet digital PCR system) to create thousands of nanoliter-sized droplets, effectively partitioning the sample.
- Amplification and Reading: Perform endpoint PCR amplification on the droplet emulsion. Transfer the PCR-amplified cartridge to a droplet reader which counts the fluorescent-positive and negative droplets for each channel (e.g., FAM, VIC, ROX, Cy5, Cy5.5, A425).
- Data Analysis: Use manufacturer-supplied software (e.g., Gene PMS) to apply Poisson statistics to the droplet counts, providing absolute quantification of the target pathogen DNA in copies/mL without the need for a standard curve [134].
The Scientist's Toolkit: Essential Research Reagents and Materials
Table 2: Key Reagents and Materials for Advanced Pathogen Diagnostics
| Item Name | Function/Application | Example Use Case |
|---|---|---|
| Nucleic Acid Extraction Kit | Purification of DNA/RNA from clinical samples (blood, tissue). | Initial sample processing for mNGS or dPCR to isolate pathogen nucleic acid [134]. |
| mNGS Library Prep Kit | Preparation of sequencing libraries from purified nucleic acids. | Converting extracted DNA/RNA into a format compatible with NGS platforms (e.g., Illumina) [133]. |
| dPCR Pathogen Panel | Multiplex probe-based assay for simultaneous pathogen detection. | Absolute quantification of a predefined set of bacterial, fungal, or viral targets in blood [134]. |
| Bioinformatic Databases (e.g., RefSeq) | Curated genomic reference databases for pathogen identification. | Taxonomic classification of non-host sequencing reads in mNGS analysis [133]. |
| Automated Nucleic Acid Purification System | High-throughput, consistent extraction of nucleic acids. | Standardized processing of multiple clinical samples for large-scale studies [134]. |
Interpretation Framework: Resolving Diagnostic Discrepancies
When novel diagnostics and culture results diverge, a systematic framework is essential for interpreting findings and guiding further research or clinical action.
- Assay Limitations and Artifacts: First, rule out technical false positives in molecular tests. Review the cycle threshold (Ct) values in PCR, read counts and genome coverage in mNGS, and ensure they significantly exceed those of negative controls. Contamination during sample processing or from reagents is a common culprit in low-biomass samples [133].
- Viability and Clinical Significance: A positive molecular test coupled with a negative culture may indicate non-viable organisms, non-replicating persister cells, or residual nucleic acid fragments from a prior, cleared infection. Correlate results with clinical symptoms, host immune response biomarkers (e.g., CRP, procalcitonin), and imaging findings to determine clinical significance [133] [134].
- Therapeutic Implications: The identification of pathogens through molecular methods can directly inform antibiotic stewardship. For example, detecting a rare or fastidious pathogen like Tropheryma whipplei or Bartonella species via mNGS allows for a targeted, narrow-spectrum therapy, reducing the reliance on broad-spectrum empirical regimens [133].
The divergence between novel diagnostics and traditional culture is not a failure of technology but a reflection of its enhanced sensitivity and the complex biology of bacterial pathogens. The research landscape is moving toward the integration of multiple diagnostic modalities. Future frameworks will combine the comprehensive detection of mNGS, the precise quantification of dPCR, and emerging technologies like host-response biomarker profiling and AI-driven bioinformatic interpretation to resolve discrepancies with greater confidence [133]. For researchers investigating unrecognized bacterial pathogens, these diagnostic gaps represent the frontier of discovery. Standardizing methodologies, improving regulatory pathways, and ensuring equitable access to these advanced tools will be essential to fully leverage their potential, ultimately transforming diagnostic puzzles into opportunities for precision medicine and improved patient outcomes [133].
Conclusion
The battle against unrecognized bacterial pathogens is multifaceted, demanding an integrated approach that spans enhanced surveillance, rapid and precise diagnostic technologies, and innovative therapeutic models. The foundational data reveals an undeniable and accelerating crisis, particularly with carbapenem-resistant strains. Methodologically, tools like mNGS and Tm mapping are revolutionizing pathogen detection, offering speed and sensitivity far beyond traditional culture, though issues of cost and interpretation remain. The troubleshooting of therapeutic development is paramount, with strategies like drug repurposing and narrow-spectrum agents offering promising pathways amidst a sparse pipeline. Validation studies confirm that these new diagnostics are not merely adjuncts but are becoming essential components of clinical microbiology. Future directions must focus on closing the innovation gap through new economic models for antibiotic development, expanding genomic databases for pathogen identification, and fully leveraging a One Health approach to mitigate the silent pandemic of antimicrobial resistance.
References
- 1. The Global Challenge of Antimicrobial Resistance [https://pmc.ncbi.nlm.nih.gov/articles/PMC12284435/]
- 2. 'Nightmare bacteria' cases are increasing in the U.S. [https://www.nbcnews.com/health/health-news/nightmare-bacteria-cases-are-increasing-us-rcna233398]
- 3. Implications of asymptomatic carriers for infectious disease ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC5830799/]
- 4. Rapid methods for the detection of foodborne bacterial ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC4290631/]
- 5. Methods for the detection and identification of pathogenic ... [https://pubs.rsc.org/en/content/articlehtml/2017/cs/c6cs00693k]
- 6. New test developed at Wayne State may explain why an E ... [https://today.wayne.edu/medicine/news/2025/10/10/new-test-developed-at-wayne-state-may-explain-why-an-e-coli-lookalike-bacteria-goes-undetected-67389]
- 7. Quantitative Assessment of Microbial Pathogens and ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC9769927/]
- 8. ABCs Bact Facts Interactive Data Dashboard [https://www.cdc.gov/abcs/bact-facts/data-dashboard.html]
- 9. UCI Scientists Help Uncover a New Bacterial Defense System ... [https://www.bio.uci.edu/uci-scientists-help-uncover-a-new-bacterial-defense-system-against-viruses/]
- 10. CDC Report Finds Sharp Rise in Dangerous Drug ... [https://www.cdc.gov/media/releases/2025/2025-cdc-report-finds-sharp-rise-in-dangerous-drug-resistant-bacteria.html]
- 11. NDM-Carbapenem-Resistant Enterobacterales Infections ... [https://www.contagionlive.com/view/ndm-cre-infections-rise-460-in-us-cdc-annals-analysis-finds]
- 12. NDM-CRE Infections Rise 460% in US, CDC/Annals ... [https://atlasidp.com/ndm-cre-infections-rise-460-in-us-cdc-annals-analysis-finds/]
- 13. 'Nightmare bacteria' cases surged in US from 2019 to 2023 [https://www.healio.com/news/primary-care/20250924/nightmare-bacteria-cases-surge-in-us-from-2019-to-2023]
- 14. CDC Report Finds Sharp Rise in Dangerous Drug ... [https://www.amr-insights.eu/cdc-report-finds-sharp-rise-in-dangerous-drug-resistant-bacteria-changes-in-carbapenemase-producing-carbapenem-resistant-enterobacterales-2019-to-2023/]
- 15. GARDP research reveals that people with multidrug ... [https://gardp.org/gardp-research-reveals-that-people-with-multidrug-resistant-infections-in-low-and-middle-income-countries-dont-have-access-to-appropriate-treatment/]
- 16. Challenges of Carbapenem-Resistant Enterobacteriaceae ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12189368/]
- 17. Review The emerging NDM carbapenemases [https://www.sciencedirect.com/science/article/abs/pii/S0966842X11001776]
- 18. Emerging Carbapenem-Resistant Enterobacteriaceae ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC8544126/]
- 19. Emergence of High Level Carbapenem and Extensively ... [https://www.frontiersin.org/journals/microbiology/articles/10.3389/fmicb.2021.645411/full]
- 20. Antimicrobial resistance [https://www.who.int/news-room/fact-sheets/detail/antimicrobial-resistance]
- 21. COVID-19 & Antimicrobial Resistance [https://www.cdc.gov/antimicrobial-resistance/data-research/threats/COVID-19.html]
- 22. An overview of the antimicrobial resistance mechanisms ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC6604941/]
- 23. Quantitative and qualitative evaluation of antimicrobial usage [https://pmc.ncbi.nlm.nih.gov/articles/PMC11076899/]
- 24. The Spread of Antibiotic Resistance Genes In Vivo Model [https://pmc.ncbi.nlm.nih.gov/articles/PMC9314185/]
- 25. Plasmids and the Spread of Antibiotic Resistance Genes [https://asm.org/articles/2023/january/plasmids-and-the-spread-of-antibiotic-resistance-g]
- 26. CDC report says 'nightmare bacteria' cases are increasing ... [https://www.pbs.org/newshour/health/cdc-report-says-nightmare-bacteria-cases-are-increasing-in-u-s]
- 27. Antibiotic resistance associated with the COVID-19 pandemic [https://pmc.ncbi.nlm.nih.gov/articles/PMC9733301/]
- 28. Quantitative systems-based prediction of antimicrobial ... [https://www.nature.com/articles/s41540-023-00304-6]
- 29. Emerging bacterial pathogens: the past and beyond - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC7128729/]
- 30. Common Mechanistic Factors of Infection-Associated Chronic ... [https://www.ncbi.nlm.nih.gov/books/n/nap27462/ch3/]
- 31. Comparison among the Quantification of Bacterial ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC5487435/]
- 32. Novel rapid method for identifying and quantifying ... [https://www.nature.com/articles/s41598-023-50864-0]
- 33. Progress Toward Understanding Infection-Associated ... [https://wwwnc.cdc.gov/eid/article/31/14/25-1187]
- 34. Current economic and regulatory challenges in developing ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12159177/]
- 35. Antibiotics re-booted—time to kick back against drug ... [https://www.nature.com/articles/s44259-025-00096-1]
- 36. The WHO Bacterial Priority Pathogens List 2024 [https://pmc.ncbi.nlm.nih.gov/articles/PMC12367593/]
- 37. Reports identify weakness in global pipeline for new ... [https://www.cidrap.umn.edu/antimicrobial-stewardship/reports-identify-weakness-global-pipeline-new-antibiotics-diagnostics]
- 38. WHO releases report on state of development ... [https://www.who.int/news/item/14-06-2024-who-releases-report-on-state-of-development-of-antibacterials]
- 39. Novel Antimicrobial Drug Development and Access - NCBI - NIH [https://www.ncbi.nlm.nih.gov/books/NBK611093/]
- 40. Lack of innovation set to undermine antibiotic performance ... [https://www.who.int/news/item/22-06-2022-22-06-2022-lack-of-innovation-set-to-undermine-antibiotic-performance-and-health-gains]
- 41. Opportunities and Challenges of Multiomics for Discovery and ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12538332/]
- 42. Clinical metagenomics—challenges and future prospects - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC10337830/]
- 43. Clinical metagenomics—challenges and future prospects [https://www.frontiersin.org/journals/microbiology/articles/10.3389/fmicb.2023.1186424/full]
- 44. Seven-year performance of a clinical metagenomic next- ... [https://www.nature.com/articles/s41591-024-03275-1]
- 45. Agnostic Sequencing for Detection of Viral Pathogens - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC10035330/]
- 46. Metagenomic pathogen sequencing in resource-scarce ... [https://www.frontiersin.org/journals/epidemiology/articles/10.3389/fepid.2022.926695/full]
- 47. Laboratory validation of a clinical metagenomic next ... [https://www.nature.com/articles/s41467-024-51470-y]
- 48. The Latest Developments in Sequencing Technologies [https://frontlinegenomics.com/the-latest-developments-in-sequencing-technologies/]
- 49. Academic and clinical perspectives of metagenome ... [https://bmcinfectdis.biomedcentral.com/articles/10.1186/s12879-025-10820-x]
- 50. Challenges and Opportunities in Pathogen Agnostic ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10902267/]
- 51. Next-generation sequencing (NGS) diagnostic - BARDA DRIVe [https://drive.hhs.gov/ngs.html]
- 52. Melting Temperature Mapping Method: A Novel ... [https://www.nature.com/articles/srep12543]
- 53. Guidelines for preventing and reporting contamination in ... [https://www.nature.com/articles/s41564-025-02035-2]
- 54. challenges of low microbial biomass samples during ... [https://pubmed.ncbi.nlm.nih.gov/31944633/]
- 55. Synthesis of current pediatric urinary microbiome research [https://www.frontiersin.org/journals/pediatrics/articles/10.3389/fped.2024.1396408/full]
- 56. Melting temperature mapping method using imperfect ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11094154/]
- 57. Study reveals how bacteria in tumors drive treatment ... [https://www.mdanderson.org/newsroom/research-newsroom/study-reveals-how-bacteria-in-tumors-drive-treatment-resistance-.h00-159780390.html]
- 58. Rapid microbiological diagnostic test in the Primary Care ... [https://www.pediatriaintegral.es/2023-english/rapid-microbiological-diagnostic-test-in-the-primary-care-pediatric-consultation/]
- 59. Comparison of metagenomic next-generation sequencing ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC9684712/]
- 60. analysis of metagenomic Comparative - next ... generation sequencing [https://pmc.ncbi.nlm.nih.gov/articles/PMC11934473/]
- 61. Comparison of three commercially available circulating cell ... [https://www.biochain.com/blog/comparison-of-three-commercially-available-circulating-cell-free-dna-ccfdna-extraction-methods-through-low-coverage-whole-genome-sequencing/]
- 62. Qualitative and quantitative comparison of cell-free DNA and ... [https://translational-medicine.biomedcentral.com/articles/10.1186/s12967-020-02671-8]
- 63. Quantitative PCR–Based Method to Assess Cell-Free DNA ... [https://www.sciencedirect.com/science/article/pii/S1525157822000745]
- 64. Cell-free DNA as a potential alternative to genomic ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12408905/]
- 65. analysis of read length impact on cost and performance | BMC ... [https://bmcgenomics.biomedcentral.com/articles/10.1186/s12864-024-10778-1]
- 66. WHO releases new reports on new tests and treatments in ... [https://www.who.int/news/item/02-10-2025-who-releases-new-reports-on-new-tests-and-treatments-in-development-for-bacterial-infections]
- 67. A systematic review of economic evaluations of whole- ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC9997737/]
- 68. GSK and Fleming Initiative scientists unite to target AMR ... [https://www.gsk.com/en-gb/media/press-releases/gsk-and-fleming-initiative-scientists-unite-to-target-amr-with-advanced-ai/]
- 69. Circovirus Hepatitis in Immunocompromised Patient ... [https://wwwnc.cdc.gov/eid/article/30/10/24-0678_article]
- 70. Circovirus Hepatitis in Immunocompromised Patient, ... [https://pubmed.ncbi.nlm.nih.gov/39320240/]
- 71. Human Circovirus in Patients with Hepatitis, Hong Kong [https://wwwnc.cdc.gov/eid/article/30/12/24-1114_article]
- 72. Rapid identification of unknown pathogens in ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC6538980/]
- 73. Application of machine learning based genome sequence ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11480060/]
- 74. Sequence analysis / Quality Control / Hands-on [https://training.galaxyproject.org/training-material/topics/sequence-analysis/tutorials/quality-control/tutorial.html]
- 75. MP4: a machine learning based classification tool for ... [https://bmcbioinformatics.biomedcentral.com/articles/10.1186/s12859-022-05061-7]
- 76. A review on computational systems biology of pathogen–host ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC4391036/]
- 77. Metagenomic Next-Generation Sequencing in Infectious ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12384723/]
- 78. Advances in Host Depletion and Pathogen Enrichment ... [https://www.sciencedirect.com/science/article/pii/S1525157824001284]
- 79. Metagenomic next-generation sequencing for concurrent ... [https://www.nature.com/articles/s41598-025-18812-2]
- 80. Clinical characteristics of the host DNA-removed ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC9705594/]
- 81. Guidelines for Validation of Next-Generation Sequencing– ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC6941185/]
- 82. Data Processing and Visualization for Metagenomics [https://carpentries-lab.github.io/metagenomics-analysis/]
- 83. A bibliometric analysis and systematic review of drug ... [https://www.frontiersin.org/journals/microbiology/articles/10.3389/fmicb.2025.1669585/full]
- 84. Current Treatment Strategies Against Multidrug-Resistant ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC9633024/]
- 85. Drug Repurposing: An Emerging Strategy in Staphylococcus ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12603381/]
- 86. From Lab to Clinic: Success Stories of Repurposed Drugs in ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12535746/]
- 87. Effective alternative strategies to combat challenges ... [https://www.sciencedirect.com/science/article/pii/S1876034125004071]
- 88. Repurposing Approved Drugs Against Gram-Negative ... [https://www.mdpi.com/2076-2607/13/9/2115]
- 89. Drug Repurposing Provides Big Impact for Patients [https://c-path.org/story/drug-repurposing-provides-big-impact-for-patients/]
- 90. AI serves as a tool to fight drug resistance and accelerate ... [https://www.news-medical.net/news/20251003/AI-serves-as-a-tool-to-fight-drug-resistance-and-accelerate-new-antibiotic-development.aspx]
- 91. McMaster researchers discover antibiotic proteins that kill a ... [https://healthsci.mcmaster.ca/mcmaster-researchers-discover-antibiotic-proteins-that-kill-a-broad-range-of-bacteria/]
- 92. Living Engineered Bacterial Therapeutics: Emerging ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11584976/]
- 93. Engineering live bacterial therapeutics to treat human ... [https://www.sciencedirect.com/science/article/pii/S2452310023000495]
- 94. Engineered bacteria launch and control an oncolytic virus [https://www.nature.com/articles/s41551-025-01476-8]
- 95. 全球四大关键真菌病原体四十年研究进展与展望:抗真菌耐药机制 ... [https://www.ebiotrade.com/newsf/2025-8/20250831002327077.htm]
- 96. A new antibiotic selectively kills Gram-negative pathogens [https://pmc.ncbi.nlm.nih.gov/articles/PMC7188312/]
- 97. Teixobactin kills bacteria by a two-pronged attack on the ... [https://www.nature.com/articles/s41586-022-05019-y]
- 98. Mode of action of teixobactins in cellular membranes [https://www.nature.com/articles/s41467-020-16600-2]
- 99. Teixobactin: A Paving Stone toward a New Class of ... [https://pubmed.ncbi.nlm.nih.gov/32520557/]
- 100. The Killing Mechanism of Teixobactin against Methicillin ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC7253363/]
- 101. Teixobactin - an overview [https://www.sciencedirect.com/topics/pharmacology-toxicology-and-pharmaceutical-science/teixobactin]
- 102. Research reveals hidden antibiotics in non-immune proteins [https://english.elpais.com/science-tech/2024-10-29/research-reveals-hidden-antibiotics-in-non-immune-proteins.html]
- 103. WHO Reports 40 Percent Jump in Antibiotic-Resistant ... [https://www.bu.edu/articles/2025/antibiotic-resistant-infection-bu-based-nonprofit-fightback/]
- 104. Without Federal Funding, Antibiotics Research May Lag [https://undark.org/2025/07/30/antibiotics-funding-lag/]
- 105. Current economic and regulatory challenges in developing ... [https://www.nature.com/articles/s44259-025-00123-1]
- 106. First antibiotic in 50 years to tackle superbug nears approval [https://www.labiotech.eu/trends-news/antibiotic-development-landscape/]
- 107. Antibiotics re-booted—time to kick back against drug ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12125309/]
- 108. Antibacterial R&D is very hard! Two great pipeline reviews ... [https://amr.solutions/2025/04/04/antibacterial-rd-is-very-hard-two-great-pipeline-reviews-an-industry-level-view/]
- 109. Alternatives to antibiotics in the fight against superbugs [https://www.weforum.org/stories/2025/10/this-regulatory-shift-is-unlocking-alternatives-to-antibiotics-in-the-fight-against-superbugs/]
- 110. Government-Funded Health and Biomedical Research Is ... [https://nam.edu/perspectives/government-funded-health-and-biomedical-research-is-irreplaceable/]
- 111. Characterization of rare and recently first described human ... [https://www.frontiersin.org/journals/cellular-and-infection-microbiology/articles/10.3389/fcimb.2023.1212627/full]
- 112. Comparison of metagenomic next-generation sequencing and ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10964532/]
- 113. Metagenomic next-generation sequencing (mNGS) versus ... [https://www.nature.com/articles/s41598-025-06759-3]
- 114. Comparison of pathogen detection performance between ... [https://www.frontiersin.org/journals/cellular-and-infection-microbiology/articles/10.3389/fcimb.2025.1563962/full]
- 115. Comparison of metagenomic next-generation sequencing and ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10847245/]
- 116. Comparison of microbial culture, metagenomic next ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12343261/]
- 117. An innovative fungal-specific targeted next-generation ... [https://translational-medicine.biomedcentral.com/articles/10.1186/s12967-025-06784-w]
- 118. Accurate and rapid turnaround of four hours for diagnosis ... [https://www.medrxiv.org/content/10.1101/2025.04.24.25326310v1.full-text]
- 119. Diagnostic Performance of Metagenomic Next-Generation ... [https://pubmed.ncbi.nlm.nih.gov/41109936/]
- 120. The application value and challenges of metagenomic next ... [https://www.frontiersin.org/journals/medicine/articles/10.3389/fmed.2025.1686503/full]
- 121. Surprising giant DNA discovery may be linked to gum ... [https://www.sciencedaily.com/releases/2025/09/250912195128.htm]
- 122. The secret lives of bacteria: How they evade viral attack [https://www.utsouthwestern.edu/newsroom/articles/year-2025/aug-bacteria-evad-viral-attack.html]
- 123. Utilization of targeted sequencing for etiological diagnosis of ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12586106/]
- 124. Targeted next-generation sequencing (tNGS) [https://www.sciencedirect.com/science/article/pii/S1876034125002850]
- 125. Home - Pathogen Detection - NCBI - NIH [https://www.ncbi.nlm.nih.gov/pathogens/]
- 126. Identification of Rare Pathogenic Bacteria in a Clinical ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC3697718/]
- 127. The value of metagenomic next-generation sequencing in ... [https://www.nature.com/articles/s41598-025-86295-2]
- 128. Antimicrobial Stewardship: How the Microbiology Laboratory ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC5217798/]
- 129. Traditional and Molecular Techniques for the Study of ... [https://wwwnc.cdc.gov/eid/article/8/2/01-0141_article]
- 130. Emerging antimicrobial therapies for Gram-negative ... [https://www.nature.com/articles/s44259-025-00087-2]
- 131. From understanding diseases to drug design: can artificial ... [https://link.springer.com/article/10.1007/s10462-024-10714-5]
- 132. Inferring asymptomatic carriers of antimicrobial-resistant ... [https://www.nature.com/articles/s41467-025-65241-w]
- 133. Unveiling the Future of Infective Endocarditis Diagnosis [https://pmc.ncbi.nlm.nih.gov/articles/PMC12373624/]
- 134. Comparative analysis between digital PCR and blood ... [https://www.frontiersin.org/journals/medicine/articles/10.3389/fmed.2025.1615409/full]
- 135. a systematic review and meta-analysis of diagnostic accuracy ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC7439295/]
- 136. Diagnostic accuracy of semi-quantitative and quantitative ... [https://bmcinfectdis.biomedcentral.com/articles/10.1186/1471-2334-14-283]